Abstract
Objectives
Our aim was to review medication-related incidents reported to a hospital voluntary incident reporting system to identify and quantify the magnitude of wrong dose errors.
Methods
The study was a retrospective review of medication-related incidents reported over a 7-year period at a large acute teaching hospital in the UK, providing secondary and tertiary care for a range of clinical specialties. Medication-related incident reports submitted from all clinical settings were reviewed. Incidents submitted under the categories ‘wrong dose’, ‘wrong dose preparation’, ‘wrong rate’ or ‘wrong quantity’ and describing situations where incorrect doses were prescribed, dispensed or administered were analysed. Magnitudes of medication overdoses and underdoses reported from adult and paediatric settings were calculated. Stage of the medicines process and drug classes most commonly involved in wrong dose errors were described.
Results
Of 12 006 reported medication incidents, 1568 described ‘wrong-dose’ errors: 702 (44.8%) were prescribing errors, 223 (14.2%) were dispensing errors and 643 (41%) were administration errors. Overdoses were reported more frequently than underdoses. 926 (59%) of reported wrong dose errors were overdoses, 464 (29.6%) were underdoses; the magnitude could not be determined in 178 (11.4%) of reports. Twofold and 10-fold overdoses and underdoses were the most commonly reported error magnitude, although dosing errors across a wide range of magnitudes were reported. Incidents were reported from paediatric wards (491, 31.3%), non-paediatric wards and clinical settings (880, 56.1%) and pharmacy (197, 12.6%). Prescribing errors (702, 45.9%) were reported more commonly than administration (643, 41%) and dispensing errors (223, 14.2%). Drugs acting on the central nervous system, cardiovascular drugs and anti-infectives were the drug classes most commonly involved.
Conclusions
Wrong dose errors occur across all inpatient settings. Wrong dose errors of all magnitudes are possible, but twofold and 10-fold errors occur most frequently. Drug classes involved in wrong dose incidents reported to a voluntary reporting system in a large acute hospital are similar to those identified using other methodologies. Harms and potential harms associated with specific drugs and error magnitudes need to be identified to inform quality improvement work to reduce the risk of patient harm.
Keywords: clinical governance, risk management, drug overdose, inpatients, medication error, patient safety
Background
Voluntary incident reporting systems are key to identifying and learning from adverse events and medical error including errors in medicines use. Landmark publications1–3 advocated the implementation of national reporting systems to collate and analyse data on patient safety incident reports from healthcare organisations. All National Health Service (NHS) organisations in England and Wales are required to report patient safety incidents to the National Reporting and Learning System (NRLS) set up in 2003 by the Department of Health. Medication safety incident reports have been used by the National Patient Safety Agency and NHS England Patient Safety to highlight risks and make recommendations for safer medicines use through publication of alerts, rapid response reports and signals. As well as being aware of and managing risks highlighted at a national level, organisations need to be responsive to local medication safety incidents to reduce the risk of potential future harm.
While voluntary incident reporting systems have become well established over the last decade or more, particularly in large acute hospitals, they cannot be relied on to provide quantitative data on the incidence of adverse events. Voluntary incident reporting detects fewer incidents than other methodologies.4 5 Use of voluntary reporting schemes relies on recognition that an adverse event has occurred and that it is reportable, practitioners’ willingness to report, knowledge of how to report and ease of access to an easy to use reporting system. However, incident reports provide an ongoing source of information to monitor known drug-related risks and identify new concerns and themes associated with specific drugs and processes that can be addressed.
Despite their widespread use, there are few published papers describing themes and trends within data sets of adverse drug events, although several reviews of incidents reported to the NRLS have been published.6–9 Among these reviews, ‘wrong dose’ is one of the most frequently reported categories. Recently, wrong dose errors were described as one of the ‘giant’ risks to medication safety deserving more detailed analysis and learning.10
Our organisation is a 1000-bed, UK teaching hospital with secondary and tertiary care specialties, including paediatrics. Datix is the electronic reporting system used to report patient safety incidents. Patient safety incidents associated with medicines are reviewed by our Medication Safety Committee and ‘wrong-dose’ incidents, including 10-fold incidents, are regularly reported. We conducted a retrospective review of reported medication incidents associated with ‘wrong dose’ errors to determine the numbers and magnitudes of those dose errors to inform future risk management strategies.
Study type and methodology
The study was a retrospective analysis of ‘wrong dose’ medication safety incidents involving prescribing, dispensing or administration reported in a large NHS acute teaching hospital in England over a 7-year period. The study was approved by the trust as a retrospective audit. In our hospital, medicines are supplied to wards from a centralised pharmacy. Commonly used medicines and medicines required in urgent and emergency situations are supplied and stored as ward stock. Less frequently prescribed and high-risk medicines are dispensed for individual patients against prescriptions. Almost all medicines are administered by nursing staff. Injectable medicines are prepared and administered by nurses who have received training and have been deemed competent in the use of injectable medicines. Medicines are prescribed and administration is documented within the Electronic Prescribing and Medicines Administration section of the electronic patient record, which is reviewed by pharmacists.
Incidents reported to the hospital’s incident reporting system (Datix) between 1 April 2008 and 31 March 2015 were downloaded into spreadsheets using Microsoft Excel. Incidents reported from all clinical settings were included.
A dose is defined as ‘a definite quantity of a medicine given or prescribed to be given at one time’.11 For the purpose of this review, we defined a ‘wrong dose’ error as the administration or dispensing of a drug in a dose other than the prescribed dose and a prescribed dose that differs from the expected dose for the patient and clinical situation according to current practice.
Reported incidents categorised as ‘wrong dose’, ‘wrong dose preparation’, ‘wrong rate’ and ‘wrong quantity’ were reviewed independently by a senior clinical pharmacist and a consultant medication safety pharmacist. Incidents describing situations that involved a wrong drug dose were included. Wrong dose errors reported as incidents but which did not reach the patient were also included.
Incidents containing no reference to a drug dosing error were excluded from further analysis. Duplicate reports were also excluded. Drugs administered by intermittent infusion where the right dose was administered over the wrong period of time were excluded, for example, 1.5 g vancomycin administered over 30 min instead of 90 min. Drugs prescribed to be administered by continuous infusion where the rate of administration of the drug expressed as dose/time was wrong were included as wrong dose errors, for example, a heparin 1000 unit/mL infusion administered at 1.3 mL/hour instead of 1 mL/hour.
Where reports described dosing errors for more than one drug the report was duplicated and magnitude of error was analysed separately for each drug.
Wrong dose preparation errors were included as a subset of administration errors where the dose has been prepared on the ward by nursing staff prior to administration or as dispensing errors if the dose has been prepared by the pharmacy department prior to being issued as a dispensed item.
Reports were analysed by both investigators independently for suitability for inclusion. Calculations of magnitude of error were made independently then compared. Differences were discussed to ensure the descriptions of incidents had been correctly interpreted. Error magnitudes were then recalculated if necessary to reach agreement.
Included incidents were analysed for details of the stage of the medicines process (either prescribing, dispensing or administration to patients), the drug class involved as defined by the chapter system in the British National Formulary12 and actual and intended drug dose. Where actual and intended drug doses had been included in the incident report, the magnitude of error was calculated according to the following formula:
Where actual and/or intended doses were not specified, the magnitude of error was recorded as unknown, but the report was included for analysis against other criteria. Where the magnitude of error was greater than one, errors were described as ‘overdoses’. Where the magnitude of error was less than one, errors were described as ‘underdoses’.
Descriptive statistics were used to report the findings.
Results
Results overview
Between April 2008 and March 2015, 12 006 medication safety incidents were reported to the trust incident reporting database. Two thousand and seventeen reports (2017/12 006, 16.8%) described wrong dose incidents including 1509 (74.8%) categorised as ‘wrong dose’, 216 (18%) as ‘wrong dose preparation’, 207 (17.2%) as ‘wrong rate’ and 85 (7%) as ‘wrong quantity’.
There was no description of a wrong dose incident within 449 (22.2%) of these reports that were excluded from the study.
Wrong dose errors occurred at all stages of the medicines process. Prescribing errors (44.77%, 95% CI 42.31 to 47.23) were reported more commonly than administration errors (41%, 95% CI 38.57 to 43.43) and dispensing errors (14.22%, 95% CI 12.49 to 15.95).
Across all three stages, overdoses were reported more commonly than underdoses but in similar proportions (table 1).
Table 1.
Numbers of ‘wrong dose’ medication incidents reported over a 7-year period (n=1568) by stage and category
| Magnitude of error | Total % |
|||
| Greater than 1 | Less than 1 | Unknown | ||
| (Overdose errors) | (Underdose errors) | |||
| Stage of the medicines process | ||||
| Prescribing | 429 | 191 | 82 | 702 |
| 27.4% | 12.2% | 5.2% | 44.8% | |
| Dispensing | 126 | 88 | 9 | 223 |
| 8% | 5.6% | 0.6% | 14.2% | |
| Administration | 371 | 185 | 87 | 643 |
| 23.7% | 11.8% | 5.5% | 41% | |
| Category of incident | ||||
| Wrong dose | 772 | 379 | 131 | 1282 |
| 49.2% | 24.2% | 8.4% | 81.8% | |
| Wong dose preparation | 54 | 38 | 13 | 105 |
| 3.4% | 2.4% | 0.8% | 6.7% | |
| Wrong rate | 81 | 37 | 28 | 146 |
| 5.2% | 2.4% | 1.8% | 9.3% | |
| Wrong quantity | 19 | 10 | 6 | 35 |
| 1.2% | 0.6% | 0.4% | 2.2% | |
| Total | 926 | 464 | 178 | 1568 |
| 59.0% | 29.6% | 11.4% | 100% | |
Magnitude of error
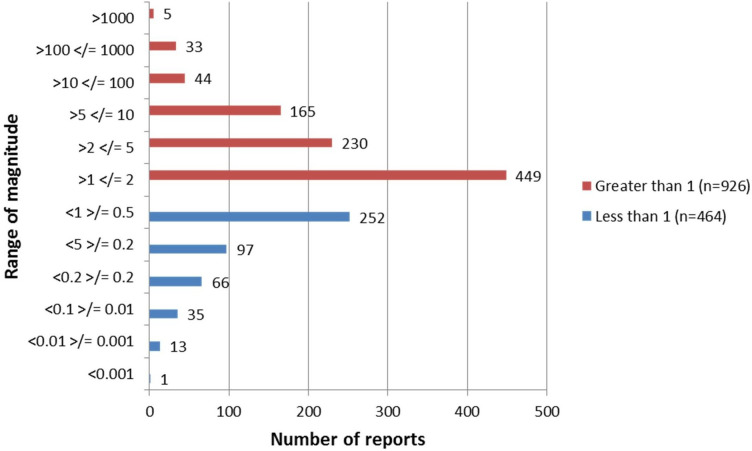
The majority of errors were overdoses (dosing errors exceeding the expected dose and with a calculated magnitude greater than 1) representing 59% of reported wrong dose errors (95% CI 56.57 to 61.43). Almost a quarter of these (209/926, 22.2%) were 10 or more times higher than expected with more than half of those being exactly tenfold errors (127/209, 60.7%). Underdoses represented 464/1568 (29.6%) of errors, of which 95 were 10 or more times lower than intended and 46/95 (48%) being exactly one-tenth of the intended dose (figure 1).
Figure 1.
Distribution of ranges of magnitudes of wrong dose medication incidents.
The magnitude of dosing error was unknown in 178/1568 (11.4%) of reports.
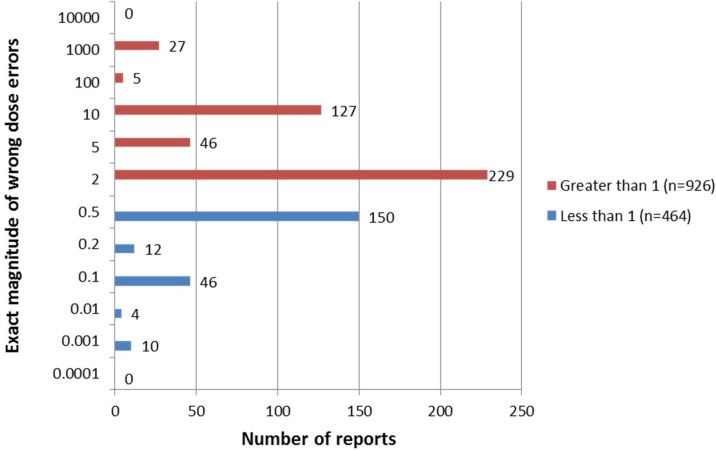
The most common error magnitudes were twofold or half (figure 2). Two hundred and twenty-nine double-dose and 150 half-doses were reported, making up 229 (14.6%) and 150 (9.6%) of all wrong dose errors.
Figure 2.
Distribution of exact magnitudes of wrong dose medication incidents.
Thousandfold overdoses and underdoses were associated with 27 and 10 reports, primarily due to the use of incorrect dose units (grams, milligrams or micrograms) at the prescribing stage.
Four hundred and ninety-one wrong dose errors occurred on paediatric wards, of which 311 (63.3%) were overdoses and 128 were underdoses (26.1%).
The number of overdoses and underdoses reported from paediatric and non-paediatric settings appeared to be similar overall, although the proportion of 10-fold errors reported from paediatric wards was higher (table 2). Tenfold overdoses were described in 12% of reports from paediatric wards compared with 6.3% from non-paediatric areas. Underdoses, where doses were one-tenth of the intended dose, were described in 3.2% of reports from paediatric wards and 2.8% from non-paediatric areas.
Table 2.
Magnitude of error on paediatric and non-paediatric wards
| Magnitude of error | All reports n=1568 | Paediatric wards only n=491 | Non-paediatric wards/clinical settings n=1077 |
| Overdose errors | |||
| Greater than 1 | 926 (59%) | 311 (63.3%) | 615 (57.1%) |
| Greater than/equal to 10 | 209 | 100 | 109 |
| Greater than/equal to 5 | 293 | 130 | 163 |
| Greater than/equal to 2 | 706 | 250 | 456 |
| Magnitude=10 | 127 | 59 (12%) | 68 (6.3%) |
| Underdose errors | |||
| Less than 1 | 464 (29.6%) | 128 (26.1%) | 336 (31.2%) |
| Less than/equal to 0.5 | 363 | 92 | 271 |
| Less than/equal to 0.2 | 127 | 55 | 72 |
| Less than/equal to 0.1 | 95 | 40 | 55 |
| Magnitude 0.1 | 46 | 16 (3.2%) | 30 (2.8%) |
| Unknown | 178 (11.4%) | 52 (10.6%) | 126 (11.7%) |
Drugs involved in wrong dose errors
Of the 1390 incidents where the magnitude of error was known, the drug involved could be identified in 1385 reports (1385/1390, 99.6%).
Three drug classes: drugs acting on the central nervous system, drugs acting on the cardiovascular system and anti-infectives accounted for 58.6% of all wrong dose errors (919/1568) and 60% (835/1390) of wrong dose errors where the magnitude was known.
Discussion
Results overview
We identified a ‘wrong dose’ error rate of 13.1% of reported medication incidents. This is similar to the findings of a retrospective review of medication safety incident data reported to the NRLS from all healthcare settings in England and Wales, which found that 15% of incidents were categorised as ‘wrong dose’.9
It is difficult to make direct comparisons between the findings of our study and other studies as there is little published data on rates of medication safety incidents reported across whole organisations. Quantitative comparisons of incident reports and reporting rates are limited due to incomplete detection and reporting of medication incidents. However, incident reports can contain useful qualitative information to identify recurring themes and trends that can be quantified using other research methodologies such as direct observation or case note review.
Most published studies describing medication incidents focus on single stages of the medicines process, for example, prescribing13 14 or administration,15 specific patient groups or clinical settings, for example, paediatrics16 17 and critical care,18 or wrong dose errors of specific magnitudes, for example, 10-fold errors.19 Different detection methods have been used to identify medication safety incidents,4 20 and often ‘wrong dose’ errors are not further defined.
Stage of the medicines process
The NRLS data have shown that administration errors are more frequently reported than prescribing errors (50.01% vs 18.45%).9
Our study, which focuses on wrong dose errors in the acute hospital setting, found that fewer wrong dose administration errors were reported than wrong dose prescribing errors (41% vs 44.8%).
Pharmacists are more likely to report wrong dose prescribing errors identified when clinically screening prescriptions for accuracy and appropriateness and by nurses checking doses during medicines administration than wrong dose errors occurring during administration. Indeed, over half (51.7%) of the wrong dose prescribing errors in this study were reported by pharmacists compared with 26.3% by nurses and only 8% by doctors. A study of prescribing errors in UK hospitals identified by pharmacists during prescription reviews found that more than half of the errors identified were wrong dose errors and that most serious errors were associated with wrong doses.13
Prescribing overdoses were reported more frequently than prescribing underdoses. This differs from the findings of a large prospective study of prescribing errors in 20 UK hospitals, which found that underdose prescribing errors occurred more frequently than overdoses (10.91% compared with 8.44%).14 We found a large number of wrong dose errors were reported by pharmacists suggesting that there is a potential bias towards the reporting of wrong dose prescribing errors that are easy to detect and the tendency to perceive the reporting of overdose errors as more important than reporting of underdose errors.
Wrong dose administration errors are more likely to be detected and reported by nurses than doctors or pharmacists who are unlikely to directly witness drug administration. Predictably, therefore, reporting rates of wrong dose administration errors were higher for nurses and midwives (66.87%) than for pharmacists (10.26%) and doctors (5.44%).
One observational study identified that perceptions of medication safety varied between professions and that the culture of medication safety was strongest among pharmacists. In the same study nurses, were perceived to be the highest reporters and doctors the lowest.21 Our study supports these perceptions with pharmacists and nurses being high reporters of the types of errors that they are most likely to encounter within the medicines process and doctors reporting fewest incidents.
Magnitude of error
Overdose errors were reported more frequently than underdose errors. As the data were obtained from a voluntary reporting system, it is impossible to know whether this reflects the true incidence of overdose and underdose errors or whether overdoses are more likely to be reported as they may be perceived as having more potential for patient harm.
Twofold overdoses and twofold underdoses were most commonly reported. This type of error can easily arise from selection of the wrong strength of a product where it is available in multiple strengths, or from giving the wrong number of dose units. Examples include administering 40 mg enoxaparin when 20 mg is prescribed and dispensing lansoprazole 15 mg capsules against a prescription for 30 mg capsules. Prescribing considerations can also result in double-dose errors, for example, prescribing 1000 mg of intravenous paracetamol to adults weighing less than 50 kg instead of the recommended body weight adjusted dose of 500 mg.
Thousandfold errors of overdose and underdose were reported in low numbers. Errors of this magnitude are often associated with selection of incorrect dosing units where grams and milligrams or milligrams and micrograms are confused during the prescribing process. They are more likely to occur with paper prescribing systems, which unlike electronic prescribing systems, do not guide prescribers to select the correct dosing units. They are likely to be intercepted before they are administered to patients as they create a mismatch between the dose and the available drug product of such enormity that the dose cannot easily be administered. Examples include alfacalcidol 4 mg prescribed instead of 4 µg and aciclovir 500 g instead of 500 mg.
Of more concern are the 127 10-fold overdoses and 46 10-fold underdoses reported representing 11% of all wrong dose incidents and 1.5% of all reported medication incidents. Almost twice as many 10-fold errors were reported from paediatric clinical areas than adult areas (15.3% vs 9.1%). Errors of this magnitude have previously been described as a risk in paediatric drug dosing where doses are calculated on an individual patient basis according to body weight.19 22 23 One UK study of 195 voluntary incident reports in a paediatric hospital identified 15 10-fold errors—8% of reports.17
There is currently no standard definition of a ‘wrong dose’ error. We included all reported ‘wrong dose’ incidents regardless of magnitude. One author describes a wrong dose prescribing error in paediatrics as a dose that is 25% greater or less than the recommended dose.24 The same author suggests that corrections to prescriptions may be perceived as dose optimisation rather than correction of an error. Therefore, we can expect that deviations in prescribed doses may be identified and corrected and not subsequently reported. Other authors have proposed limits outside which doses can be considered to be wrong, for example, infusion rates greater than 15% of the intended rate,25 gentamicin and vancomycin doses less than or greater than 10% and 20% of guideline recommended doses26 and doses of oral liquid medicines less than or greater than 17% of the dose prescribed.27
The potential for patient harm associated with wrong dose errors is difficult to predict and varies according to a range of factors including the magnitude of error, the toxicity profile of the drug itself and the patient’s clinical status and tolerance or susceptibility to the effect of the drug. All prescribed drug doses should be correct according to current clinical guidance and be dispensed and administered exactly as prescribed. Any deviations are therefore ‘wrong dose’ errors. While this increases the reporting of errors with no clinical significance, it could enable the causes of wrong dose errors to be better understood.
Defining a wrong dose error for individual drugs according to the likelihood of harm could result in a confusing list of scenarios that could reduce the numbers of errors reported. This also shifts the emphasis on reporting away from the causes of error to the outcomes of error potentially reducing the opportunities to manage and reduce the risks of recurrence.
Although several authors have defined limits against which wrong dose errors have been defined for specific studies, setting limits for routine reporting of wrong dose medication errors could be confusing for practitioners and discourage reporting.
Drugs involved in wrong dose errors
The frequencies with which wrong dose errors occur in relation to numbers of prescriptions written for each drug or drug class is not known. In our data set, drugs acting on the central nervous system, drugs acting on the cardiovascular system and anti-infectives are the drug classes most often associated with wrong dose errors. However, they are likely to be the drug classes most frequently used within the acute secondary care setting and therefore more likely to feature in medication incident reports. Previous authors have used the concept of defined daily doses to determine the relative rate of medication safety incidents with individual antimicrobial agents taking into account volumes of use.28 Comparing numbers of incident reports with the frequency of drug use helps to highlight high risk drugs where usage of the drug is low.
Our data only included incidents reported to our hospital voluntary reporting system. However, these three drug classes were also commonly associated with potentially serious errors in a large prospective study of prescribing in UK hospitals.14 This suggests that our data set may be representative of findings in other organisations and using other medication incident review methodologies.
Limitations
The study only included incidents reported to the hospital’s voluntary reporting system. It has been suggested that wrong dose errors are less likely to be self-reported than some other types of errors.29 This may be because wrong dose errors may be undetected, particularly administration errors, and also the perception that they are more likely to be seen as the fault of individuals more than other error types that can be attributed to organisation factors such as workload, training or equipment failure.
We confirmed ‘wrong dose’ incidents from incidents categorised as ‘wrong dose’, ‘wrong rate’, ‘wrong dose preparation’ and ‘wrong quantity’. We excluded incidents where there was no evidence of a wrong dose error. We only included incidents reported as medication related. Incidents involving equipment for medication administration, for example, infusion devices, and reported as medical device related incidents were not included. A small number of wrong dose incidents reported under other categories may therefore have been missed.
Conclusion
This review confirms that wrong dose errors are a common type of medication safety incident across all clinical specialties. It demonstrates that wrong dose errors of all magnitudes are possible but that there are certain magnitudes that are recurring, especially twofold and 10-fold errors. Tenfold errors were not exclusive to the paediatric setting. Despite the limitations of voluntary reporting some of the themes identified within this data set, including frequently occurring magnitudes of dosing error, and errors with opioids, anticoagulants and anti-infectives are seen in studies using different error detection methodologies. This reinforces the usefulness of voluntary incident reporting as an ongoing tool for monitoring medication-related problems.
Although electronic prescribing systems, guidelines to promote the safe use of medicines and detailed policies to reduce the risk of error with high-risk medicines are all in place, dosing errors still occur. This could reflect the increasing complexity and workload in secondary care and the multitude of human and organisation factors, which can influence the performance of individuals, teams and systems on a day-to-day basis.
It must be noted that although we reviewed an apparently large number of dosing errors, these represent a very small proportion of prescriptions written and doses dispensed and administered safely and correctly every day across our organisation and the NHS as a whole. Most are isolated incidents detected and corrected before they reach the patient or occur on single occasions. For that reason, patient harm from wrong dose errors rarely occurs. However, factors contributing to wrong dose errors of common magnitudes and errors with high-risk drugs need further exploration to inform the development of organisation-wide strategies to minimise the possibility of harm.
What this paper adds.
What is already known on this subject
‘Wrong dose’ medication incidents are a frequently reported category of medication incident.
Previous published studies of ‘wrong dose’ medication incidents have focused on specific patient groups, stages of the medicines process or magnitude of error.
The range of ‘wrong dose’ magnitudes and relative frequency with which they are reported has not been previously described.
What this study adds
‘Wrong dose’ medication incidents are reported across all clinical specialities and are not exclusive to the paediatric setting.
Overdose and underdose errors of all magnitudes are possible, including thousandfold errors, but twofold and 10-fold errors are a common recurring theme.
The study demonstrates the usefulness of analysis of data within incident reporting systems to identify themes and trends over long periods of time.
Footnotes
Contributors: GFC designed the project, confirmed, analysed and interpreted the data, drafted the final paper. DM confirmed analysed and interpreted the data, reviewed and approved the final paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
No data are available.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Kohn LT, Corrigan JM, Donaldson MS, Institute of Medicine (US) Committee on Quality of Health Care in America . To err is human: building a safer health system. Washington DC: National Academy Press, 2000. [PubMed] [Google Scholar]
- 2.Britain G. An organisation with a memory : report of an expert group on learning from adverse events in the NHS Chaired by the chief medical officer. Donaldson L. London: Stationery Office, 2000. [Google Scholar]
- 3.Building a safer NHS for patients: implementing an organization with a memory. London: England: Department of Health; 2001. [Google Scholar]
- 4.Flynn EA, Barker KN, Pepper GA, et al. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm 2002;59:436–46. 10.1093/ajhp/59.5.436 [DOI] [PubMed] [Google Scholar]
- 5.Kozer E, Scolnik D, Jarvis AD, et al. The effect of detection approaches on the reported incidence of Tenfold errors. Drug Saf 2006;29:169–74. 10.2165/00002018-200629020-00007 [DOI] [PubMed] [Google Scholar]
- 6.Safety in doses: medication safety incidents in the NHS. London: National Patient Safety Agency; 2007. [Google Scholar]
- 7.Safety in doses: improving the use of medicines in the NHS. London: National Patient Safety Agency; 2009. [Google Scholar]
- 8.Review of patient safety for children and young people. London: National Patient Safety Agency; 2009. [Google Scholar]
- 9.Cousins DH, Gerrett D, Warner B. A review of medication incidents reported to the National reporting and learning system in England and Wales over 6 years (2005-2010). Br J Clin Pharmacol 2012;74:597–604. 10.1111/j.1365-2125.2011.04166.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cousins D. A failure to learn from our mistakes puts patients at risk. Clinical Pharmacist 2018;10. 10.1211/CP.2018.20205263 [DOI] [Google Scholar]
- 11.Dictionary OE. Available: http://www.oed.com/view/Entry/56940?rskey=Kz4n2w&result=1#eid [Accessed 16 Mar 2016].
- 12.Committee JF. British National formulary. 68 edn. London: BMJ Group and Pharmaceutical Press, 2015. [Google Scholar]
- 13.Dean B, Schachter M, Vincent C, et al. Prescribing errors in hospital inpatients: their incidence and clinical significance. Qual Saf Health Care 2002;11:340–4. 10.1136/qhc.11.4.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ashcroft DM, Lewis PJ, Tully MP, et al. Prevalence, nature, severity and risk factors for prescribing errors in hospital inpatients: prospective study in 20 UK hospitals. Drug Saf 2015;38:833–43. 10.1007/s40264-015-0320-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kale A, Keohane CA, Maviglia S, et al. Adverse drug events caused by serious medication administration errors. BMJ Qual Saf 2012;21:933–8. 10.1136/bmjqs-2012-000946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghaleb MA, Wong I. Medication errors in paediatric patients. Arch Dis Childhood-E 2006;91. 10.1136/adc.2005.073379 [DOI] [PubMed] [Google Scholar]
- 17.Ross LM, Wallace J, Paton JY. Medication errors in a paediatric teaching hospital in the UK: five years operational experience. Arch Dis Child 2000;83:492–7. 10.1136/adc.83.6.492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thomas AN, Panchagnula U. Medication-related patient safety incidents in critical care: a review of reports to the UK national patient safety agency. Anaesthesia 2008;63:726–33. 10.1111/j.1365-2044.2008.05485.x [DOI] [PubMed] [Google Scholar]
- 19.Doherty C, Mc Donnell C. Tenfold medication errors: 5 years' experience at a university-affiliated pediatric hospital. Pediatrics 2012;129:916–24. 10.1542/peds.2011-2526 [DOI] [PubMed] [Google Scholar]
- 20.Morimoto T, Gandhi TK, Seger AC, et al. Adverse drug events and medication errors: detection and classification methods. Qual Saf Health Care 2004;13:306–14. 10.1136/qshc.2004.010611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner S, Ramsay A, Fulop N. The role of professional communities in governing patient safety. J Health Organ Manag 2013;27:527–43. 10.1108/JHOM-07-2012-0138 [DOI] [PubMed] [Google Scholar]
- 22.National Patient Safety Agency . Review of patient safety for children and young people; 2014.
- 23.Chappell K, Newman C. Potential tenfold drug overdoses on a neonatal unit. Arch Dis Child Fetal Neonatal Ed 2004;89:F483–F484. 10.1136/adc.2003.041608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghaleb MA, Barber N, Dean Franklin B, et al. What constitutes a prescribing error in paediatrics? Qual Saf Health Care 2005;14:352–7. 10.1136/qshc.2005.013797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Westbrook JI, Rob MI, Woods A, et al. Errors in the administration of intravenous medications in hospital and the role of correct procedures and nurse experience. BMJ Qual Saf 2011;20:1027–34. 10.1136/bmjqs-2011-000089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hamad A, Cavell G, Hinton J, et al. A pre-postintervention study to evaluate the impact of dose calculators on the accuracy of gentamicin and vancomycin initial doses. BMJ Open 2015;5:e006610. 10.1136/bmjopen-2014-006610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allan EL, Barker KN. Fundamentals of medication error research. Am J Hosp Pharm 1990;47:555–71. 10.1093/ajhp/47.3.555 [DOI] [PubMed] [Google Scholar]
- 28.Hamad A, Cavell G, Wade P, et al. Risk of medication safety incidents with antibiotic use measured by defined daily doses. Int J Clin Pharm 2013;35:772–9. 10.1007/s11096-013-9805-9 [DOI] [PubMed] [Google Scholar]
- 29.Kiekkas P, Aretha D, Karga M, et al. Self report may lead to underestimation of 'wrong dose' medication errors. Br J Clin Pharmacol 2009;68:963–4. 10.1111/j.1365-2125.2009.03530.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data are available.