Abstract
AIM
To study the effect of topical dorzolamide 2% on macular thickness reduction in diabetic cystoid macular edema (CME).
METHODS
This was a prospective, non-randomized, open study including eyes with diabetic macular edema (DME). All eyes received topical dorzolamide 2% three times daily for one month. Changes in best-corrected visual acuity (BCVA), and central macular thickness (CMT) by optical coherence tomography) were evaluated at 1wk, 1, and 3mo post-treatment.
RESULTS
Ninety-three eyes (84 patients) were included. Mean±SD (logMAR) BCVA improved significantly from 1.08±0.26 pretreatment to 0.66±0.24 at 1mo and 0.87±0.26 at 3mo post-treatment (P<0.001 both). The mean±SD CMT was significantly reduced from 535.27±97.4 µm at baseline to 357.43±125.8 µm at 1mo and 376.23±114.5 µm at 3mo post-treatment (P<0.001 both). No significant ocular or systemic side effects were recorded.
CONCLUSION
Topical dorzolamide 2% results in significant improvement of mean BCVA and reduction of mean CMT at 3mo post-treatment. It can be used as an effective, affordable, and safe therapy for treatment of non-refractory diabetic CME.
Keywords: cystoid macular edema, diabetic maculopathy, dorzolamide, retina
INTRODUCTION
Diabetic macular edema (DME) is among the most prevalent causes of visual loss in diabetic retinopathy[1], whereas its global occurrence ratio is about 6.8% among diabetic patients[2]. The exact pathophysiology of DME is still unclear, but it is believed to be multifactorial and complicated, caused mainly by blood-retinal barrier (BRB) disruption due to functional damage and necrosis of retinal capillaries. This disruption of BRB leads to abnormal leakage and accumulation of intravascular fluid into the neurosensory retina and in the intraretinal layers of the macula[3]. The resulting macular thickening deforms photoreceptors, thus causing vision loss[4].
Laser photocoagulation has been proved effective in minimizing blindness from DME by at least 60%[5]. However, it is usually associated with retinal necrosis resulting in a reduction of pericentral-sensitivity[6]. That is why treatment should also include drugs capable of reduction or elimination of the edema without permanent destruction of the retinal anatomy.
Earlier studies concluded the benefits of intravitreal triamcinolone acetonide injection in the treatment of DME either alone or versus laser therapy[7]. Despite these benefits, the associated high incidences of cataracts and consistent intraocular pressure (IOP) increase are considered major drawbacks of intravitreal triamcinolone acetonide therapy[8].
Currently, anti-vascular endothelial growth factor (anti-VEGF) substances are widely used and have revolutionized diabetic retinopathy treatment. They have been demonstrated as effective alternatives to laser photocoagulation and have replaced it as first-line therapy[9]. Although the results of anti-VEGF agents in diabetic retinopathy are promising, each intravitreal injection has the risk of post-injection and/or drug-class-associated devastating adverse effects as endophthalmitis[10], intraocular inflammation[11], IOP elevation[12], and systemic side events[13].
Systemic carbonic anhydrase inhibitors (CAIs) have been efficient in treating maculopathy present in retinal diseases as uveitis[14], retinitis pigmentosa[15], or postoperatively after cataract surgery[16], as well as that associated with epiretinal membranes[17]. However, the use of systemic CAIs is further limited by frequent and hazardous side effects[18] which are thought to result from inhibition of intracellular carbonic anhydrase (CA) isoenzymes[19]. Dorzolamide, a topical CAIs, well-tolerated and effective as an ocular hypotensive drug[20], has been used for macular edema due to retinitis pigmentosa[21]–[22], retinoschisis[23], and choroideremia[24]. It has a comparable effect to acetazolamide in macular edema due to retinitis pigmentosa[25]. In fact, few studies[26]–[27] have investigated the efficacy of CAIs, especially the topical dorzolamide, in resolving cystoid macular edema (CME) in diabetic retinopathy. This study was carried out to study the efficacy of topical dorzolamide 2% in the treatment of CME in diabetes patients.
SUBJECTS AND METHODS
Ethical Approval
The study protocol was reviewed and approved by the Ethical Committee of Mansoura University, Faculty of Medicine, and was performed in accordance with the rules of the Helsinki Declaration (R/16.04.65). The study was registered in UMIN clinical trial register system (ID issued: UMIN 000022608 Receipt No: R000026059). Written informed consent was obtained from all patients after a clear explanation of the purpose of the study, the nature of the procedure, conceivable benefits, and possible risks.
This was a prospective, nonrandomized, open, and interventional study carried out on diabetic patients with CME recruited at Mansoura Ophthalmolic Center, Mansoura University in Mansoura city, Egypt.
Patients' Selection
Inclusion criteria
The study included adult diabetic patients (both type 1 and 2) recently diagnosed with diabetic CME (of duration less than 3mo). CME was diagnosed by slit lamp biomicroscopy with non-contact lens, fluorescein angiography, and optical coherence tomography (OCT; Topcon Corp, Tokyo, Japan).
Exclusion criteria
Patients were excluded from the study if they had: 1) advanced diabetic retinopathy; 2) serous retinal detachment; 3) vitreo-retinal traction syndrome; 4) Mixed maculopathy (macular ischemia by angiography ); 5) prior laser therapy or intravitreal injections (IVI); 6) additional ocular diseases, including uveitis, glaucoma, or neoplasms; 7) history of other medications with potential effect on the visual acuity and/or retinal function.
Initial assessment
All subjects underwent an ophthalmic examination that included: 1) best-corrected Snellen visual acuity (BCVA) measurement; 2) standard slit-lamp biomicroscopy; 3) IOP measurement by Goldmann applanation tonometry; 4) dilated fundus examination using non-contact Volk 90 lens, and indirect ophthalmoscope; 5) the severity and the level of diabetic retinopathy were evaluated through the fundus examination and fluorescein angiography based on the International Clinical Diabetic Retinopathy Disease Severity Scale[28]; 6) OCT: 3D-OCT 2000 (Topcon Corp, Tokyo, Japan) was used in this study for macular scanning. It was performed at a resolution of 512×128 with six linear scans oriented radially 30° apart and centered on the fovea. Central macular and foveal thicknesses were measured within a 6 mm diameter circle centered on the foveola and the circular map was subdivided into 9 regions. The 6 mm ring was divided into 3 rings, with the inner ring 1 mm in diameter, the middle ring 2 mm and the outer ring 3 mm in diameter. It was corresponding to the foveal, perifoveal, and parafoveal areas respectively. Color-coded graphs and numerical maps were used for quantitative evaluation. CME was diagnosed as an absence of central foveal contour, diffuse thickening of the foveal/or perifoveal area more than 250 µm, and a presence of intraretinal cysts. Scans with the image quality of 55 or more were included for analysis; 7) all participant's glycemic control was ascertained pretreatment and at 3mo post-treatment through glycosylated hemoglobin A1C (HbA1c) measurement.
Treatment protocol
This comprised administration of topical dorzolamide 2% eye drops (Trusopt 2% eye drops, Merck & Co., Inc., NJ, USA) three times daily for 30d.
Post-treatment evaluation and follow-up schedule
The first follow-up visit was at one week, then each patient was seen after one month, and three months to evaluate the patient's response to treatment. At each follow-up visit, BCVA, IOP, fundus biomicroscopy, and OCT images were obtained and recorded.
Study outcomes and data analysis
The main primary outcome was the changes in macular morphology post-treatment. OCT findings were evaluated by measuring the changes in the central foveal zone (CFZ) thickness and then all study participants were graded as responders or non-responders. The non-responders to the topical dorzolamide 2% were further classified as non-responders without worsening, or non-responders with worsening.
Secondary outcomes measurements included changes in BCVA, HbA1c variables, and IOP. Snellen visual acuity measurements were converted into logMAR equivalents for statistical analysis.
Statistical Analysis
The baseline and the outcome data were classified, scheduled, and then analyzed using the computer program SPSS (Statistical package for social science) version 17.0 (SPSS Inc. Chicago, Illinois, USA). To compare the mean values and changes from pretreatment values, the paired Student's t-test was used. The P value of less than 0.05 was considered statistically significant. Independent t-test was conducted to measure the difference between mean values of HbA1c variables among the responders and non-responders and to assess its impact on the treatment outcomes.
RESULTS
Ninety-three patients fulfilled the inclusion criteria; however, 9 patients were excluded from the study as they did not complete the 3mo follow-up period. Accordingly, 84 patients (93 eyes) were included in the study; with a mean age of 54.22±5.8y. Patients' demographic and basic clinical data are shown in Table 1.
Table 1. Patients demographics.
| Items | Data |
| Mean age (y) | 54.22±5.8 (43-67) |
| Gender | |
| Male | 36 |
| Female | 48 |
| Laterality | |
| Unilateral | 75 |
| Bilateral | 9 |
| Severity distributiona | |
| Mild-moderate NPDR | 26 eyes |
| Severe NPDR | 55 eyes |
| Low risk PDR | 12 eyes |
aInternational Clinical Diabetic Retinopathy Disease Severity Scale[32]. NPDR: Non-proliferative diabetic retinopathy; PDR: Proliferative diabetic retinopathy.
There was a statistically significant improvement in BCVA mainly one month after treatment (Figure 1). The mean±SD baseline logMAR BCVA was 1.08±0.26. It improved to 1.02±0.28 (P=0.116), 0.66±0.24 (P<0.001), and 0.87±0.26 (P<0.001) at 1wk, 1, and 3mo after treatment respectively (Table 2). At the end of 3mo, sixty-four eyes (68.8%) had a subjective improvement in the BCVA. Twenty-two eyes (23.7%) had no change from the initial pretreatment BCVA, while 7 eyes (7.5%) showed a decline in their BCVA (Table 3). The mean±SD IOP changed from16.52±2.57 mm Hg at baseline to15.42±1.37 mm Hg at 1wk, to 14.66±1.74 mm Hg after 1mo and to 15.84±1.49 mm Hg at the end of 3mo. The changes were statistically significant (P=0.002, <0.001, <0.001) respectively (Table 4).
Figure 1. Mean BCVA prior and after treatment with topical dorzolamide 2%.
BCVA: Best corrected visual acuity.
Table 2. The mean BCVA prior and after treatment.
| Time | BCVA (logMAR), mean±SD (range) | P a |
| Baseline | 1.08±0.26 (1.5-0.8) | |
| 1wk | 1.02±0.28 (1.3-0.6) | 0.116 |
| 1mo | 0.66±0.24 (1.2-0.5) | <0.001 |
| 3mo | 0.87±0.26 (1.4-0.5) | <0.001 |
aPaired samples t-test vs baseline. BCVA: Best corrected visual acuity; SD: Standard deviation, Min: Minimum, Max: Maximum.
Table 3. Change in BCVA of 93 eyes at the end of follow-up.
| BCVA change | Number of eyes (%; n=93 eyes) |
| Worsening | 7 (7.5) |
| No change | 22 (23.7) |
| 1 line improvement | 35 (37.6) |
| ≥2 lines improvement | 29 (31.2) |
BCVA: Best corrected visual acuity.
Table 4. The mean IOP.
| Time | IOP, mean±SD (range), mm Hg | P a |
| Baseline | 16.52±2.57 (12-22) | |
| 1wk | 15.42±1.37 (12-16) | 0.002 |
| 1mo | 14.66±1.74 (11-14) | <0.001 |
| 3mo | 15.84±1.49 (12-17) | <0.001 |
aPaired samples t-test vs baseline. IOP: Intraocular pressure; SD: Standard deviation.
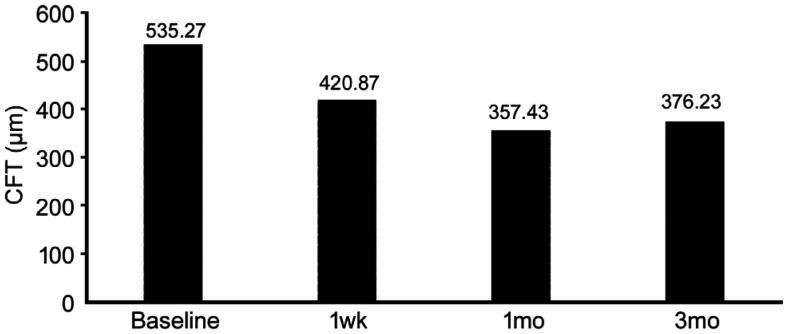
Detailed OCT images analysis showed that all post-treatment central foveal thickness (CFT) values were significantly decreased compared to baseline values (P<0.05; Figure 2). The mean±SD baseline CFT was 535.27±97.4 µm, which decreased at one week to 420.87±115.2 µm and further decreased at one month to 357.43±125.8 µm, then slightly increased to 376.23±114.5 µm at the end of 3mo, but remained significantly lower than the pretreatment value (Table 5).
Figure 2. Mean CFT prior and after treatment with topical dorzolamide 2%.
CFT: Central foveal thickness.
Table 5. The mean central foveal thickness.
| Time | Foveal thickness, mean±SD (range), µm | P a | Decrease in thickness (%) |
| Baseline | 535.27±97.4 (320-653) | ||
| 1wk | 420.87±115.2 (260-586) | <0.001 | 21.4 |
| 1mo | 357.43±125.8 (177-554) | <0.001 | 33.2 |
| 3mo | 376.23±114.5 (195-620) | <0.001 | 29.7 |
aPaired samples t-test vs baseline. SD: Standard deviation.
OCT analysis revealed that, 56 eyes (60.02%) showed improvement in response to topical dorzolamide 2% through the follow-up period (3mo), 27 eyes (29.03%) did not show any improvement and the macular thickness did not worsen, while 10 eyes (10.57%) did not show any improvement but the macular thickness worsened when compared to the baseline thickness. The mean baseline and post-treatment HbA1c values were significantly higher in non-responders as compared to responders (P<0.001; Table 6).
Table 6. The mean HbA1c among the responders and non-responders.
| HbA1c | Responders (n=56 eyes) | Non-responders (n=37 eyes) | P a |
| Baseline | 7.32±0.35 | 8.72±0.76 | <0.001 |
| Posttreatment | 7.16 ±0.35 | 8.69±0.74 | <0.001 |
aIndependent t-test. HbA1c: Glycosylated hemoglobin A1c; SD: Standard deviation.
All patients completed the follow-up period of at least 3mo (mean±SD follow-up 3.95±1.3mo; range: 3-7mo). There were no significant ocular or systemic side effects observed during the follow-up period.
DISCUSSION
The pathogenesis of DME seems to be attributable to inflammatory processes which play a main role in functional and morphological changes of DME[29]. Several previous studies have handled and evaluated the various methods for the treatment of diabetic maculopathy[3],[5]–[9],[30].
Lately, clinical interest has focused on the effect of acetazolamide, a systemic CAI, on the macular edema from various retinal disorders[14]–[17]. Unfortunately, acetazolamide may lead to serious side effects[18]–[19]. That is why it cannot be administered for a long time (3-5 days maximum). Dorzolamide is a topical CAI that can be used as an alternative prolonged therapy and can be administered to these patients constantly to prevent their visual acuity impairment[26]–[27].
It has been reported that the response to CAI therapy is better in patients with diffuse retinal pigment epithelial (RPE) disease than in those with primary retinal vascular disease, such as diabetes or retinal vein occlusion[31]. This was explained by alteration of RPE membrane-bound CAIs, which may have lost their polarized distribution due to accumulation of macular edema, with resultant stimulation of ion and fluid-removal across the RPE from the retina to the choroid[32]. However, some reports suggested that CAIs affect the BRB as they stimulate at least one ion-pump transport mechanism, resulting in an increase in passive permeability and outward-active transport across the BRB[33]. The exact mechanism for fluid transport across broken-down BRB in diabetic retinopathy remains obscure.
As the anti-inflammatory effect of dorzolamide had been reported before[34], the authors assumed that it would help in endogenous intraretinal fluid absorption through RPE and thus can improve the vision and prevente further retinal photoreceptor loss and neurodegeneration. The purpose of the current study was to evaluate the anatomical and functional effects of topical dorzolamide 2%, on CME in diabetic patients.
Based on analysis of the current series OCT, it was found that 56 eyes (60.2%) showed a significant improvement in central macular thickness (CMT) in response to topical dorzolamide, 29% did not show an improvement or worsening, and 10.8% showed an increase in macular thickness compared with pre-treatment values. The mean CFT was significantly lower at all post-treatment time points with the best-recorded results at one month and minimal deterioration at three months, but still better than pre-treatment levels. So, it can be assumed that sustained therapy may be required. Among the study cohort, 68.8% of eyes demonstrated a subjective improvement in the BCVA, 23.7% did not show any change from the pre-treatment BCVA value, while only 7.5% showed a decrease in their BCVA.
Several prior studies have investigated the effect of HbA1c on the treatment outcomes of diabetic edema with variable designs and conclusions. Some reported a strong correlation between the high HbA1c and the persistent macular edema[35]–[36]; by contrast, others found there was no relation[37]. In the current cohort, patients who had lower HbA1c levels either baseline or post-treatment showed a better response to treatment, suggesting that HbA1c is one of the sensitive variables to predict final treatment outcomes.
Lima-Gómez et al[27] studied the effect of topical dorzolamide, in comparison to placebo on the reduction of retinal thickness after focal laser photocoagulation in DME. They reported a significant reduction in CMT after topical dorzolamide, which was absent in eyes that received a placebo. But the reduced CMT was not followed by a significant improvement in visual acuity. In their study, topical dorzolamide was used three times daily for only three weeks. Moreover, the duration of CME was not specified; patients could have prolonged edema which would have caused irreversible functional damage to retinal photoreceptors, even if anatomical architecture has been restored. In the current study, patients with recently diagnosed diabetic edema were selected as the duration of DME, which could affect the macular cells' function either mechanically or toxically with more photoreceptor damage during the evolution of the disease.
One of the interesting questions here is the maintained response to treatment at the end of three months in spite that patients were off-treatment for two months. Understanding the pharmacokinetics of topical dorzolamide can interpret this topic point and might be a valuable guide. Following chronic topical application of dorzolamide, the drug reaches the systemic circulation and accumulates as well as its metabolite (N-desthyl) in red blood cells (RBCs). After the cease of the drug, its RBCs concentration initially shows a sudden decline followed by slower nonlinear wash-out of RBCs resulting in a prolonged half-life of the elimination phase up to four months[38].
The prolonged effect of dorzolamide is mostly related to the incomplete washout of the drug from the eye. Until now, there is no consensus regarding the complete washout period of topical anti-glaucomatous drops. According to the published literature; it varies from 4 to 8wk[39]. In the current work, the IOP decreased until the first month then started to increase again in the third month.
The current study confirms a promising effect of topical dorzolamide in visual improvement and CMT reduction within three months. To the authors' knowledge, there have not been published trials of the efficacy of topical dorzolamide 2% as a first-line treatment for diabetic CME. Recent trials investigated its additive role to the intravitreal anti-VEGFs and reported promising effects[40]–[41]. This novel study also has attempted to evaluate a less invasive approach than the intravitreal one in non-refractory diabetic edema with fewer potential complications. The absence of a randomized design and a control group are the limitations of the present study. Further randomized investigations of a larger number of cases with longer follow-up will be needed.
In conclusion, the current study suggests that topical dorzolamide 2% can be promising, effective, affordable, and safe therapy in treating non-refractory diabetic CME. The poor control of diabetes mellitus and elevated serum HbA1c might contribute to unsatisfactory treatment outcomes.
Acknowledgments
The manuscript was accepted in part at 10th International Conference on Clinical & Experimental Ophthalmology (Dubai, UAE) as oral presentation and the abstract published as a conference paper in J Clin Exp Ophthalmol. DOI: 10.4172/2155-9570.C1.048.
Conflicts of Interest: Badawi AE, None; Mokbel TH, None; Elhefney EM, None; Hagras SM, None; Abdelhameed AG, None.
REFERENCES
- 1.Bandello F, Battaglia Parodi M, Lanzetta P, Loewenstein A, Massin P, Menchini F, Veritti D. Diabetic macular edema. Dev Ophthalmol. 2017;58:102–138. doi: 10.1159/000455277. [DOI] [PubMed] [Google Scholar]
- 2.Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–564. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haritoglou C, Maier M, Neubauer AS, Augustin AJ. Current concepts of pharmacotherapy of diabetic macular edema. Expert Opin Pharmacother. 2020;21(4):467–475. doi: 10.1080/14656566.2020.1713093. [DOI] [PubMed] [Google Scholar]
- 4.Lardenoye CW, Probst K, DeLint PJ, Rothova A. Photoreceptor function in eyes with macular edema. Invest Ophthalmol Vis Sci. 2000;41(12):4048–4053. [PubMed] [Google Scholar]
- 5.Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Ophthalmology. 1991;98(5 Suppl):766–785. [PubMed] [Google Scholar]
- 6.Lövestam-Adrian M, Agardh E. Photocoagulation of diabetic macular oedema—complications and visual outcome. Acta Ophthalmol Scand. 2000;78(6):667–671. doi: 10.1034/j.1600-0420.2000.078006667.x. [DOI] [PubMed] [Google Scholar]
- 7.Gillies MC, Simpson JM, Gaston C, Hunt G, Ali H, Zhu MD, Sutter F. Five-year results of a randomized trial with open-label extension of triamcinolone acetonide for refractory diabetic macular edema. Ophthalmology. 2009;116(11):2182–2187. doi: 10.1016/j.ophtha.2009.04.049. [DOI] [PubMed] [Google Scholar]
- 8.Bressler NM, Edwards AR, Beck RW, Flaxel CJ, Glassman AR, Ip MS, Kollman C, Kuppermann BD, Stone TW, Diabetic Retinopathy Clinical Research Network Exploratory analysis of diabetic retinopathy progression through 3y in a randomized clinical trial that compares intravitreal triamcinolone acetonide with focal/grid photocoagulation. Arch Ophthalmol. 2009;127(12):1566–1571. doi: 10.1001/archophthalmol.2009.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rajendram R, Fraser-Bell S, Kaines A, Michaelides M, Hamilton RD, Esposti SD, Peto T, Egan C, Bunce C, Leslie RD, Hykin PG. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: report 3. Arch Ophthalmol. 2012;130(8):972–979. doi: 10.1001/archophthalmol.2012.393. [DOI] [PubMed] [Google Scholar]
- 10.Daien V, Nguyen V, Essex RW, Morlet N, Barthelmes D, Gillies MC, Fight Retinal Blindness! Study Group Incidence and outcomes of infectious and noninfectious endophthalmitis after intravitreal injections for age-related macular degeneration. Ophthalmology. 2018;125(1):66–74. doi: 10.1016/j.ophtha.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 11.Cox JT, Eliott D, Sobrin L. Inflammatory complications of intravitreal anti-VEGF injections. J Clin Med. 2021;10(5):981. doi: 10.3390/jcm10050981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wingard JB, Delzell DA, Houlihan NV, Lin J, Gieser JP. Incidence of glaucoma or ocular hypertension after repeated anti-vascular endothelial growth factor injections for macular degeneration. Clin Ophthalmol. 2019;13:2563–2572. doi: 10.2147/OPTH.S232548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nuzzi R, Tridico F. Local and systemic complications after intravitreal administration of anti-vascular endothelial growth factor agents in the treatment of different ocular diseases: a five-year retrospective study. Semin Ophthalmol. 2015;30(2):129–135. doi: 10.3109/08820538.2013.835833. [DOI] [PubMed] [Google Scholar]
- 14.Schilling H, Heiligenhaus A, Laube T, Bornfeld N, Jurklies B. Long-term effect of acetazolamide treatment of patients with uveitic chronic cystoid macular edema is limited by persisting inflammation. Retina. 2005;25(2):182–188. doi: 10.1097/00006982-200502000-00011. [DOI] [PubMed] [Google Scholar]
- 15.Huang QZ, Chen R, Lin XP, Xiang ZY. Efficacy of carbonic anhydrase inhibitors in management of cystoid macular edema in retinitis pigmentosa: a meta-analysis. PLoS One. 2017;12(10):e0186180. doi: 10.1371/journal.pone.0186180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pepple KL, Nguyen MH, Pakzad-Vaezi K, Williamson K, Odell N, Lee C, Leveque TK, van Gelder RN. Response of inflammatory cystoid macular edema to treatment using oral acetazolamide. Retina. 2019;39(5):948–955. doi: 10.1097/IAE.0000000000002044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marmor MF. Hypothesis concerning carbonic anhydrase treatment of cystoid macular edema: example with epiretinal membrane. Arch Ophthalmol. 1990;108(11):1524–1525. doi: 10.1001/archopht.1990.01070130026013. [DOI] [PubMed] [Google Scholar]
- 18.Lichter PR. Reducing side effects of carbonic anhydrase inhibitors. Ophthalmology. 1981;88(3):266–269. doi: 10.1016/s0161-6420(81)35040-4. [DOI] [PubMed] [Google Scholar]
- 19.Travis DM. Renal carbonic anhydrase inhibition by benzolamide (CL 11, 366) in man. J Pharmacol Exp Ther. 1969;167(2):253–264. [PubMed] [Google Scholar]
- 20.Stewart WC, Halper LK, Johnson-Pratt L, Polis A, Hartenbaum D. Tolerability and efficacy of dorzolamide versus acetazolamide added to timolol. J Ocul Pharmacol Ther. 2002;18(3):211–220. doi: 10.1089/108076802760116133. [DOI] [PubMed] [Google Scholar]
- 21.Ikeda Y, Yoshida N, Notomi S, Murakami Y, Hisatomi T, Enaida H, Ishibashi T. Therapeutic effect of prolonged treatment with topical dorzolamide for cystoid macular oedema in patients with retinitis pigmentosa. Br J Ophthalmol. 2013;97(9):1187–1191. doi: 10.1136/bjophthalmol-2012-303005. [DOI] [PubMed] [Google Scholar]
- 22.Shimokawa S, Fujiwara K, Murakami Y, Funatsu J, Nakatake S, Yoshida N, Sonoda KH, Ikeda Y. Effect of topical dorzolamide on cystoid macular edema in retinitis pigmentosa. Ophthalmol Retina. 2020;4(10):1036–1039. doi: 10.1016/j.oret.2020.05.012. [DOI] [PubMed] [Google Scholar]
- 23.Gutiérrez-Sánchez L, Moreno-Paramo D, Ortega-Larrocea X, Villanueva-Mendoza C, Zenteno-Ruíz JC. Atipic manifestations of retinoschisis and response to dorzolamide: a case report. Revista Mexicana De Oftalmol. 2011;85(1):52–55. [Google Scholar]
- 24.Genead MA, McAnany JJ, Fishman GA. Topical dorzolamide for treatment of cystoid macular edema in patients with choroideremia. Retina. 2012;32(4):826–833. doi: 10.1097/IAE.0b013e3182215ae9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pacella E, Arrico L, Santamaria V, Turchetti P, Carbotti MR, la Torre G, Pacella F. Dorzolamide chlorhydrate versus acetazolamide in the management of chronic macular edema in patients with retinitis pigmentosa: description of three case reports. Ophthalmol Eye Dis. 2014;6:21–26. doi: 10.4137/OED.S13617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giusti C, Forte R, Vingolo EM, Gargiulo P. Is acetazolamide effective in the treatment of diabetic macular edema? A pilot study. Int Ophthalmol. 2001;24(2):79–88. doi: 10.1023/a:1016354517304. [DOI] [PubMed] [Google Scholar]
- 27.Lima-Gómez V, Bermúdez-Zapata DA, Blanco-Hernández DMR. Efficacy of dorzolamide in reducing retinal thickness after photocoagulation in diabetic macular oedema. Cirugía Y Cirujanos. 2015;83(1):3–8. doi: 10.1016/j.circir.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 28.Wilkinson CP, Ferris FL, 3rd, Klein RE, Lee PP, Agardh CD, Davis M, Dills D, Kampik A, Pararajasegaram R, Verdaguer JT, Global Diabetic Retinopathy Project Group Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology. 2003;110(9):1677–1682. doi: 10.1016/S0161-6420(03)00475-5. [DOI] [PubMed] [Google Scholar]
- 29.Romero-Aroca P, Baget-Bernaldiz M, Pareja-Rios A, Lopez-Galvez M, Navarro-Gil R, Verges R. Diabetic macular edema pathophysiology: vasogenic versus inflammatory. J Diabetes Res. 2016;2016:2156273. doi: 10.1155/2016/2156273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmidt-Erfurth U, Garcia-Arumi J, Bandello F, Berg K, Chakravarthy U, Gerendas BS, Jonas J, Larsen M, Tadayoni R, Loewenstein A. Guidelines for the management of diabetic macular edema by the European society of retina specialists (EURETINA) Ophthalmologica. 2017;237(4):185–222. doi: 10.1159/000458539. [DOI] [PubMed] [Google Scholar]
- 31.Cox SN, Hay E, Bird AC. Treatment of chronic macular edema with acetazolamide. Arch Ophthalmol. 1988;106(9):1190–1195. doi: 10.1001/archopht.1988.01060140350030. [DOI] [PubMed] [Google Scholar]
- 32.Wolfensberger TJ. The role of carbonic anhydrase inhibitors in the management of macular edema. Doc Ophthalmol. 1999;97(3-4):387–397. doi: 10.1023/a:1002143802926. [DOI] [PubMed] [Google Scholar]
- 33.Moldow B, Sander B, Larsen M, Lund-Andersen H. Effects of acetazolamide on passive and active transport of fluorescein across the normal BRB. Invest Ophthalmol Vis Sci. 1999;40(8):1770–1775. [PubMed] [Google Scholar]
- 34.Kawai, Ohashi H, Suzuki T, Kitagaki H, Fujisawa S. Effect of anti-glaucoma drugs on inflammatory cytokine production by human and murine peripheral blood mononuclear cells. Nippon Ganka Gakkai Zasshi. 2010;114(8):669–677. [PubMed] [Google Scholar]
- 35.Do DV, Shah SM, Sung JU, Haller JA, Nguyen QD. Persistent diabetic macular edema is associated with elevated hemoglobin A1c. Am J Ophthalmol. 2005;139(4):620–623. doi: 10.1016/j.ajo.2004.10.063. [DOI] [PubMed] [Google Scholar]
- 36.Macky TA, Mahgoub MM. The effect of glycemic control on visual and anatomic outcomes in response to therapy for diabetic macular edema. Eur J Ophthalmol. 2012:0. doi: 10.5301/ejo.5000179. [DOI] [PubMed] [Google Scholar]
- 37.Peng YJ, Tsai MJ. Impact of metabolic control on macular thickness in diabetic macular oedema. Diab Vasc Dis Res. 2018;15(2):165–168. doi: 10.1177/1479164117746023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yeh J, Kravitz D, Francis B. Rational use of the fixed combination of dorzolamide - timolol in the management of raised intraocular pressure and glaucoma. Clin Ophthalmol. 2008;2(2):389–399. doi: 10.2147/opth.s1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diaconita V, Quinn M, Jamal D, Dishan B, Malvankar-Mehta MS, Hutnik C. Washout duration of prostaglandin analogues: a systematic review and meta-analysis. J Ophthalmol. 2018;2018:3190684. doi: 10.1155/2018/3190684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fazel F, Nikpour H, Pourazizi M. Combination of intravitreal bevacizumab and topical dorzolamide versus intravitreal bevacizumab alone for diabetic macular edema: a randomized contralateral clinical trial. Biomed Res Int. 2020;2020:6794391. doi: 10.1155/2020/6794391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mirshahi A, Tadayoni R, Mohsenzadeh N, Saeidi Rezvani T, Abrishami M. Efficacy of adjuvant topical timolol-dorzolamide with intravitreal bevacizumab injection in diabetic macular edema: a contralateral eye study. J Curr Ophthalmol. 2019;31(2):168–171. doi: 10.1016/j.joco.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]