Abstract
Background:
Powered hand exoskeletons are an emerging technology that have shown promise in assisting individuals with impaired hand function. A number of hand exoskeleton designs have been described in the literature; however, the majority have not been supported by patient-oriented criteria.
Objective:
The aim of this study was to define preliminary end-user needs and expectations for an assistive hand exoskeleton.
Study design:
Explorative interview and case series.
Methods:
Six clinicians and eight individuals with impaired hand function were interviewed in small groups or individually. A standardized list of questions was used to elicit feedback on specific design criteria or promote the discovery of new criteria. In addition, three participants with impaired hand function returned for a second session where hand characteristics, such as range of motion and force required to flex/extend fingers, were recorded to further quantify design requirements.
Results:
Interview responses indicated that there was general consensus among participants on criteria relating to important grasp patterns, grip strength, wear time, and acceptable bulk/weight. However, interview responses and hand characteristics also revealed important differences between individuals with impaired hand function.
Conclusion:
Qualitative and quantitative data were collected to develop an understanding of end-user design requirements for assistive hand exoskeletons. Although the data collected were helpful in identifying some preliminary criteria, differences between participants exist and identifying a universal set of criteria applicable across individuals with impaired hand function is challenging. This work reinforces the importance of involving users of rehabilitation technology in the device development process.
Keywords: Upper limb orthotics, hand exoskeleton, design criteria, mixed methods
Background
The human hand is an intricate appendage that is vital for interacting with the environment, a fact that is emphasized when dextrous hand function is impaired. Limited hand function significantly impedes the ability of an individual to perform activities of daily living and impacts quality of life. Stroke is one of the leading causes of impaired hand function, with over 80 million stroke survivors globally,1 and nearly 80% experiencing upper limb motor deficits.2 Furthermore, there are an estimated 27 million people living with spinal cord injury,3 with a significant proportion experiencing impaired upper limb function.4 Beyond these clinical populations, numerous peripheral neurological disorders and traumatic injuries can also compromise hand function.
Powered hand exoskeletons are an emerging technology that have demonstrated promise in alleviating functional challenges associated with hand impairment or weakness.5,6 These systems attach to segments of the hand and actively assist digit flexion and extension to aid in the performance of functional grasping tasks by applying forces to the user’s digits. Therefore, they help restore movement by guiding the digits to specific positions or grasping patterns; movement that would typically be challenging or impossible to independently achieve and maintain.
Several hand exoskeleton designs have been described in scientific literature.5–12 However, the majority have not been tested in clinical patient populations or translated beyond the laboratory. Those that have are costly and often operate in a purely therapeutic capacity, being tethered to a computer. To date, the only commercially-available assistive device that allows the user to be untethered and perform day-to-day tasks is the MyoPro Motion (Myomo, Inc.).5,13 This device includes multiple joints (elbow, wrist, and hand) and one grasp pattern (tripod) and is marketed as a powered upper limb orthosis, rather than a dedicated hand exoskeleton. While the MyoPro and other devices are promising, the functional benefits of hand exoskeletons remain largely inaccessible to clinicians and patients. Furthermore, designs for exoskeletons are quite varied and it is not clear which populations would benefit from them. Ideally, a clinically accessible powered hand exoskeleton would adhere to a set of well-defined design specifications derived from the input of end users, specifically patients and clinicians.
The purpose of this pilot study was to define preliminary design requirements for an assistive powered hand exoskeleton that would be acceptable for clinical or long-term use according to patients and clinicians. Requirements were determined by interviewing individuals with hand impairment and clinicians who work with such patients. Further design criteria were gathered by characterizing hand function of three participants with hand impairments. The intent was to provide critical information to developers of these devices with guidance toward which criteria are important to assess in different patient populations.
Methods
Participants
Purposive sampling was used to identify individuals with impaired hand function and experienced clinicians through a local rehabilitation hospital. Clinician participants were recruited through the clinical technology lead at the hospital. These participants helped to identify and approach potential participants with hand impairment. If they consented to have their information shared, the research team contacted them through email or phone. Inclusion criteria for participants with impaired hand function were adults (18–75 years) with non-progressive or static hand impairment. Exclusion criteria were cognitive impairments or language barriers that would inhibit their ability to comprehend and respond to the interview questions in English.
Interview sessions
Interview sessions were conducted to understand end-user objectives for an assistive hand exoskeleton. Interview questions (Supplemental Digital Content 1, http://links.lww.com/POI/A24) were divided into two sections: (1) design criteria questions, aimed at understanding specific design expectations and requirements and (2) open-ended discussion questions, intended to promote exploration and discussion of new criteria from the end-user’s perspective. Present at each interview were one researcher (the interviewer), who was a graduate student with a background in biomedical engineering; the interviewee(s); and one or two other lab members (biomedical engineering graduate student and clinical/research engineer) to assist with recording the interview and taking detailed notes. The interview responses were typed out in real time by a researcher, and audio/video recordings were used to review their accuracy. The interview notes were analyzed for content, summarizing the participant’s responses to each interview question. This summary was examined by an engineering graduate student to identify recurrent responses and responses which were most relevant for defining the design criteria for a hand exoskeleton.
Hand function characterization sessions
Follow-up data collection sessions were completed with three participants with hand impairment purposively selected as having different diagnostic causes of hand impairment, being likely to benefit from a hand exoskeleton, and being available for the additional data collection session. These sessions were aimed at quantifying the characteristics of their affected limb that might be relevant to the design of a hand exoskeleton. Present at these sessions were two engineering graduate students and one clinical/research engineer. A physiatrist and occupational therapist advised on the protocol.
Hand function
Participants were asked to perform different grasp pattern movements to assess their capabilities and identify grasp patterns they would need help achieving. We recorded whether the participant was able to achieve each movement, and whether the participant’s thumb could be passively moved into opposition, if they were not able to actively do so.
Range of motion
Active and passive range of motion (RoM) were assessed using a dorsal finger goniometer14 to understand the extent to which the participant could move their fingers without assistance and the extent to which a hand exoskeleton could assist with finger motion within the available range. RoM was first assessed on the index finger, and measurements were only taken for other fingers if their RoM was dissimilar from the index. Active wrist RoM was also measured to assess the viability of a flexion sensor at the wrist as a trigger for activating a hand exoskeleton.
Grip force
Participants’ unassisted grip force was measured to quantify current capabilities. Grip strength was measured in cylinder (diameter = 70 mm), tip-to-tip, tripod, and lateral key grip patterns by grasping a load cell (Omegadyne LCM 703-5) with custom 3D printed attachments for the grip patterns. The experimenters assisted the participant to shape their hand around the load cell if required; however, they did not help them to apply force. Participants were asked to squeeze the load cell as hard as they could and then relax. Three repetitions were completed when possible.
External force required to flex/extend the index finger
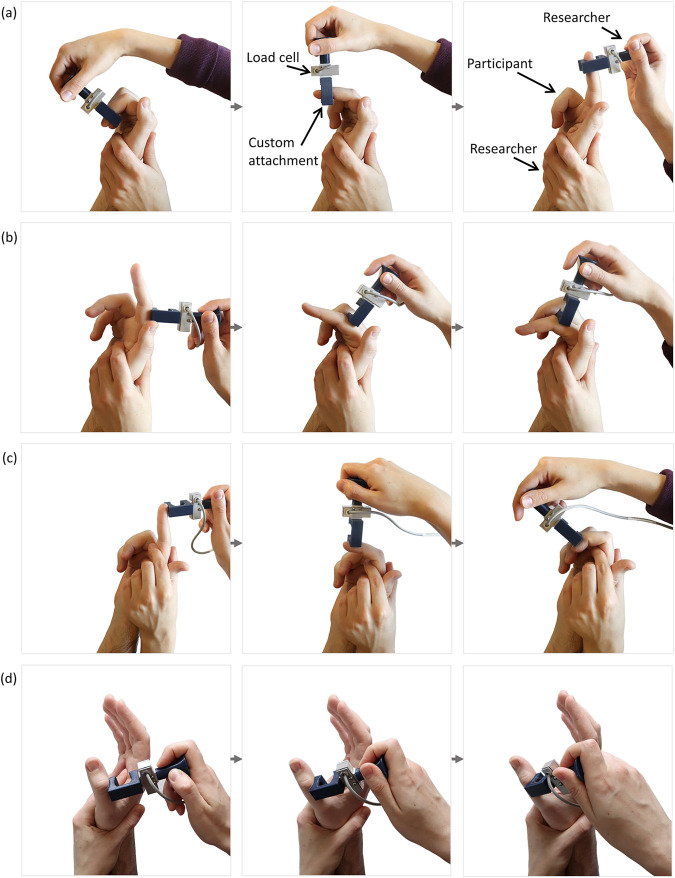
A custom load cell attachment (Figure 1) was used to measure the force required to pull the participants’ index finger into extension and push it into flexion. Hand exoskeleton grip force capabilities have been evaluated with able-bodied individuals who were instructed not to exert voluntary force7 or with individuals with flaccid hand impairment.6 Since our participant group included individuals with muscle spasticity and contracture, we wanted to gain an understanding of the forces that a hand exoskeleton would need to exert to elicit finger movement for such individuals. Three movements were examined: index finger extension (all three joints simultaneously, force applied at distal phalanx), flexion of the metacarpophalangeal (MCP) joint, and flexion of the proximal interphalangeal (PIP) and distal interphalangeal (DIP) joints while the MCP joint was stabilized. For one participant, thumb opposition was also examined by pushing on the thumb just proximal to the interphalangeal joint. The speed of each movement was controlled by the experimenter with a goal of achieving a movement time of 1–3 s. Participants were asked to relax and not assist the movement. Movement was stopped if it became uncomfortable for the participant or the experimenter felt excessive resistance. At least three repetitions were completed for each movement. The peak applied force and overall movement duration were extracted for each movement repetition.
Figure 1.
Custom load cell attachment used to move the participant’s finger while measuring the force required to assist with the movement. Movements assessed were (a) index finger extension, (b) flexion of the metacarpalphalangeal (MCP) joint on the index finger, (c) flexion of the proximal interphalangeal (PIP) and distal interphalangeal ( DIP) joints on the index finger, and (d) thumb opposition.
Forearm electromyography
To assess the feasibility of using muscle activity to trigger the activation of a hand exoskeleton, surface electromyography (EMG) was recorded from sites on each participant’s forearm flexor and extensor muscles using a Bagnoli 8-channel system (Delsys Inc). The participants were asked to complete the following movements: wrist flexion and extension, making a fist, extending all fingers, and pointing their index finger. If participants were not able to actively complete a movement, they were instructed to still imagine doing the action and express the intention. EMG signals were acquired at 1000 Hz with a hardware gain of 1000. The software gain was adjusted for each participant to achieve maximum separability of signals.
The mean absolute value (MAV) was calculated using a 200 ms averaging window, as commonly used for myoelectric prosthesis control.15 To gain a conservative estimate of the change in signal between resting and active contraction, differences in EMG signals were based on the maximum peak from the resting signal and the minimum value during the contraction.
Results
Six clinicians who were working as occupational therapists or hand rehabilitation specialists were recruited and enrolled in the study. Their experience ranged from 5 to 15 years and included specialization in one or more of the following patient populations: traumatic injury, brain injury, or stroke. Eight individuals with impaired hand function (two with stroke, three with spinal cord injury (SCI), and three with brachial plexus injury (BPI)) were approached by clinicians, and all eight agreed to participate.
Interview sessions
The clinicians participated in a focus group discussion. Of the eight participants with impaired hand function, six were interviewed in individual sessions (one over teleconference) and two participants with BPI were interviewed together.
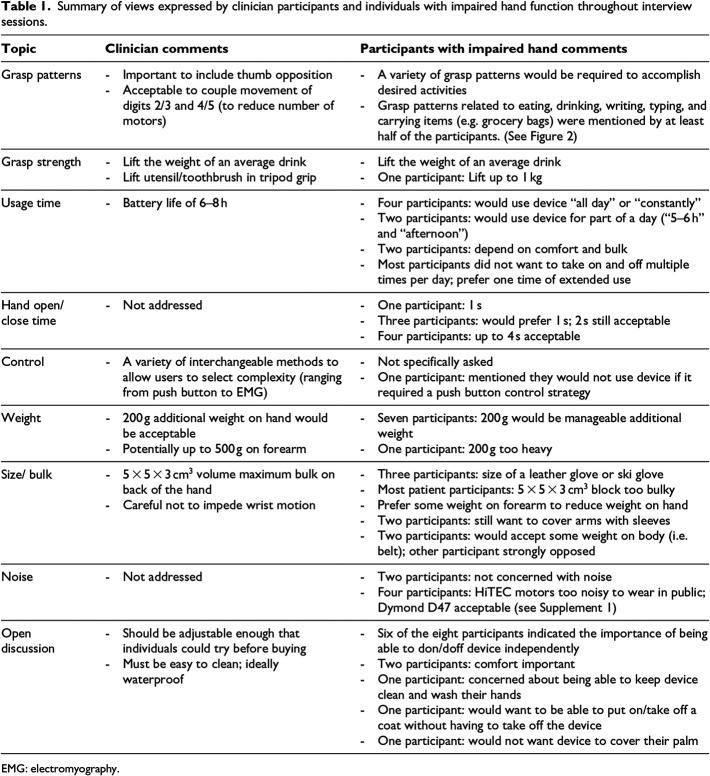
Views expressed during the interview sessions are summarized in Table 1 and Figure 2. Clinicians and participants with hand impairment mostly agreed on expectations for a hand exoskeleton regarding important grasp patterns, grip strength, wear time, and acceptable weight. However, responses also revealed differences in desired requirements. Some participants were more tolerant of a slower, bulkier, or louder device, so long as it was helpful, while others indicated that they would not use such a device. Most participants had some experience with rehabilitation devices that may have influenced their responses. Clinicians had experience with wrist and hand orthoses, and some had experience with powered therapeutic devices that move the hand and fingers. However, no clinicians had specific experience with powered assistive hand exoskeletons for use during daily life. Similarly, participants with impaired hand function did not have experience with powered exoskeletons but did have experience with other devices for supporting the wrist and hand, such as the Bioness Hand Rehabilitation System and the SaeboGlove.
Table 1.
Summary of views expressed by clinician participants and individuals with impaired hand function throughout interview sessions.
| Topic | Clinician comments | Participants with impaired hand comments |
|---|---|---|
| Grasp patterns | - Important to include thumb opposition - Acceptable to couple movement of digits 2/3 and 4/5 (to reduce number of motors) |
- A variety of grasp patterns would be required to accomplish desired activities - Grasp patterns related to eating, drinking, writing, typing, and carrying items (e.g. grocery bags) were mentioned by at least half of the participants. (See Figure 2) |
| Grasp strength | - Lift the weight of an average drink - Lift utensil/toothbrush in tripod grip |
- Lift the weight of an average drink - One participant: Lift up to 1 kg |
| Usage time | - Battery life of 6–8 h | - Four participants: would use device “all day” or “constantly” - Two participants: would use device for part of a day (“5–6 h” and “afternoon”) - Two participants: depend on comfort and bulk - Most participants did not want to take on and off multiple times per day; prefer one time of extended use |
| Hand open/close time | - Not addressed | - One participant: 1 s - Three participants: would prefer 1 s; 2 s still acceptable - Four participants: up to 4 s acceptable |
| Control | - A variety of interchangeable methods to allow users to select complexity (ranging from push button to EMG) | - Not specifically asked - One participant: mentioned they would not use device if it required a push button control strategy |
| Weight | - 200 g additional weight on hand would be acceptable - Potentially up to 500 g on forearm |
- Seven participants: 200 g would be manageable additional weight - One participant: 200 g too heavy |
| Size/ bulk | - 5 × 5 × 3 cm3 volume maximum bulk on back of the hand - Careful not to impede wrist motion |
- Three participants: size of a leather glove or ski glove - Most patient participants: 5 × 5 × 3 cm3 block too bulky - Prefer some weight on forearm to reduce weight on hand - Two participants: still want to cover arms with sleeves - Two participants: would accept some weight on body (i.e. belt); other participant strongly opposed |
| Noise | - Not addressed | - Two participants: not concerned with noise - Four participants: HiTEC motors too noisy to wear in public; Dymond D47 acceptable (see Supplemental Digital Content 1, http://links.lww.com/POI/A24) |
| Open discussion | - Should be adjustable enough that individuals could try before buying - Must be easy to clean; ideally waterproof |
- Six of the eight participants indicated the importance of being able to don/doff device independently - Two participants: comfort important - One participant: concerned about being able to keep device clean and wash their hands - One participant: would want to be able to put on/take off a coat without having to take off the device - One participant: would not want device to cover their palm |
EMG: electromyography.
Figure 2.
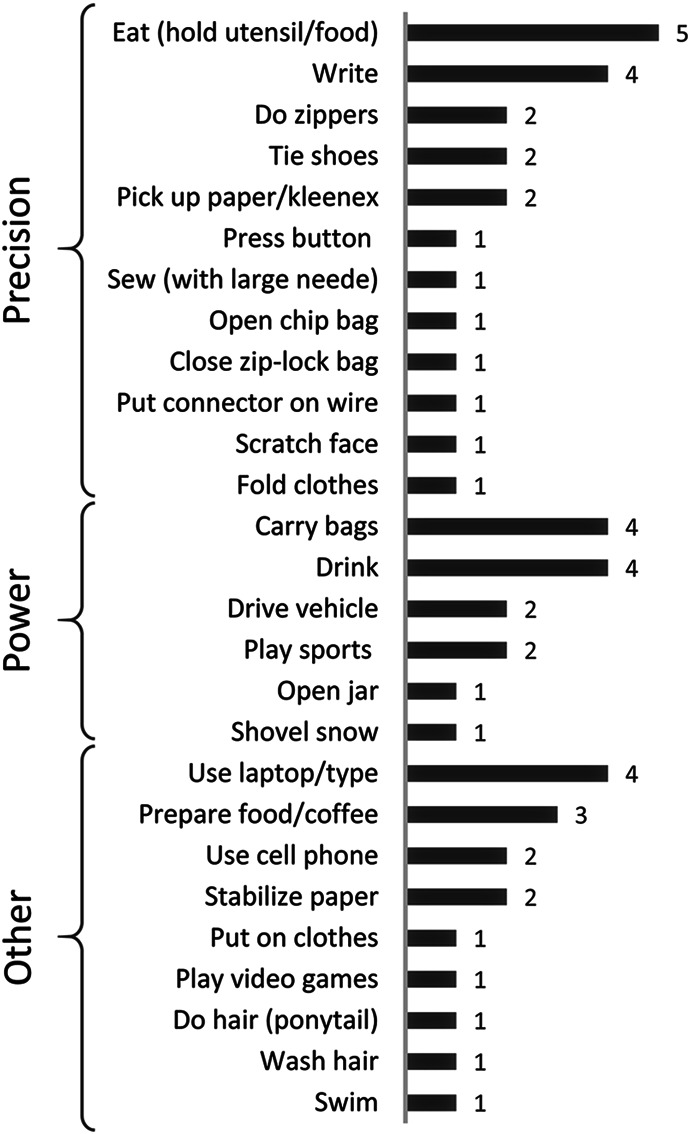
List of tasks that participants indicated they would like to perform with the help of a hand exoskeleton sorted, by grip type (precision, power, and miscellaneous) as well as the number of participants who mentioned each task.
Hand function characterization sessions
The participants who returned for hand measurements were (1) Par05: 67-year-old male with an SCI 3 years prior, affecting roots C4 through C7 (shoulder spared, limited elbow function on right arm). Measurements were taken on right (weaker) side as the participant indicated that was the hand he would prefer to use an exoskeleton with, if one were available; (2) Par06: 62-year-old male with a BPI 3 years prior, affecting the right arm; and (3) Par07: 27-year-old male with a stroke 7 years prior, affecting the right side.
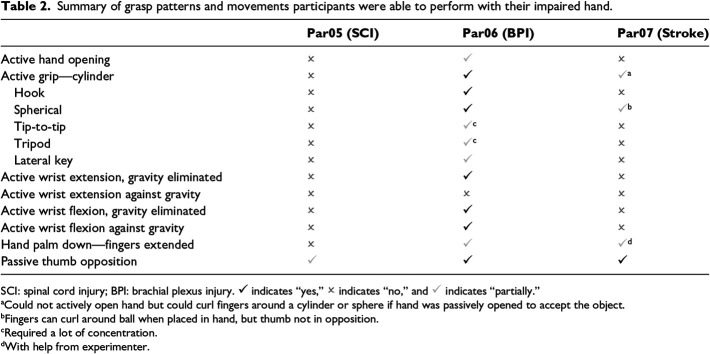
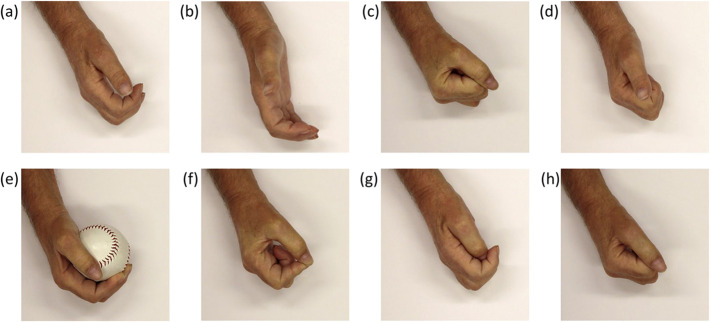
Hand function
Table 2 summarizes the grasp patterns and hand movements the participants were able to complete. Example photographs from Par06 are shown in Figure 3.
Table 2.
Summary of grasp patterns and movements participants were able to perform with their impaired hand.
| Par05 (SCI) | Par06 (BPI) | Par07 (Stroke) | |
|---|---|---|---|
| Active hand opening | ✗ | ✓ | ✗ |
| Active grip—cylinder | ✗ | ✓ | ✓a |
| Hook | ✗ | ✓ | ✗ |
| Spherical | ✗ | ✓ | ✓b |
| Tip-to-tip | ✗ | ✓c | ✗ |
| Tripod | ✗ | ✓c | ✗ |
| Lateral key | ✗ | ✓ | ✗ |
| Active wrist extension, gravity eliminated | ✗ | ✓ | ✗ |
| Active wrist extension against gravity | ✗ | ✗ | ✗ |
| Active wrist flexion, gravity eliminated | ✗ | ✓ | ✗ |
| Active wrist flexion against gravity | ✗ | ✓ | ✗ |
| Hand palm down—fingers extended | ✗ | ✓ | ✓d |
| Passive thumb opposition | ✓ | ✓ | ✓ |
SCI: spinal cord injury; BPI: brachial plexus injury. ✓ indicates “yes,” ✗ indicates “no,” and ✓ indicates “partially.”
Could not actively open hand but could curl fingers around a cylinder or sphere if hand was passively opened to accept the object.
Fingers can curl around ball when placed in hand, but thumb not in opposition.
Required a lot of concentration.
With help from experimenter.
Figure 3.
Photographs of Par06’s hand (brachial plexus injury, BPI) during (a) rest, (b) active hand opening, (c) cylinder grip, (d) hook grip, (e) spherical grip, (f) tip-to-tip grip, (g) tripod grip, and (h) lateral key grip.
RoM
The participants presented quite differently with respect to active and passive RoM (Supplemental Digital Content 2, http://links.lww.com/POI/A25). Par05 (SCI) had almost no active RoM and some muscle stiffness that resisted passive motion. Passive RoM varied depending on the finger, with the index finger having the greatest RoM at the MCP compared to the other digits, but the hand could not be fully opened or fully closed due to stiffness at various joints. Par06 (BPI) could not fully extend their fingers actively, but their hand could be fully opened passively. Their hand could be closed into a fist both actively and passively, except for the little finger, which could not be flexed past approximately 40°. Par07’s hand (stroke) was closed in a fist in resting position. They were not able to actively extend their fingers. The experimenters were able to obtain passive extension with very slow application of force. Of the three participants, only Par06 was able to obtain active wrist flexion/extension.
Grip force
Par05 (SCI) was unable to apply grip force in any of the grip patterns. Par06 (BPI) was able to complete the cylinder, tip-to-tip, and lateral key grip (mean peak force of 28.6 N, 7.3 N, and 10.4 N, respectively), but not the tripod grip. Par07 (stroke) was able to complete the cylinder grip (mean peak force of 32.7 N) and one repetition of the tripod grip (1.3 N) but required help from experimenters to position the measurement device in their hand for both.
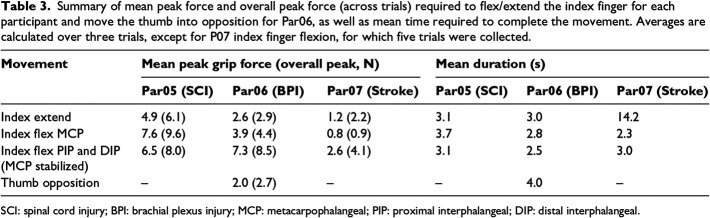
External force required to flex/extend the index finger
Peak forces required to flex and extend the index finger are summarized in Table 3. In most cases, three repetitions of the movement were conducted. For Par07 (stroke) finger extension, five repetitions were performed because of variability in muscle spasticity.
Table 3.
Summary of mean peak force and overall peak force (across trials) required to flex/extend the index finger for each participant and move the thumb into opposition for Par06, as well as mean time required to complete the movement. Averages are calculated over three trials, except for P07 index finger flexion, for which five trials were collected.
| Movement | Mean peak grip force (overall peak, N) | Mean duration (s) | ||||
|---|---|---|---|---|---|---|
| Par05 (SCI) | Par06 (BPI) | Par07 (Stroke) | Par05 (SCI) | Par06 (BPI) | Par07 (Stroke) | |
| Index extend | 4.9 (6.1) | 2.6 (2.9) | 1.2 (2.2) | 3.1 | 3.0 | 14.2 |
| Index flex MCP | 7.6 (9.6) | 3.9 (4.4) | 0.8 (0.9) | 3.7 | 2.8 | 2.3 |
| Index flex PIP and DIP (MCP stabilized) | 6.5 (8.0) | 7.3 (8.5) | 2.6 (4.1) | 3.1 | 2.5 | 3.0 |
| Thumb opposition | – | 2.0 (2.7) | – | – | 4.0 | – |
SCI: spinal cord injury; BPI: brachial plexus injury; MCP: metacarpophalangeal; PIP: proximal interphalangeal; DIP: distal interphalangeal.
The greatest force required was for flexion of the MCP on Par05 (SCI), likely due to muscle stiffness. From visual inspection of the trial-by-trial data, it appeared that force required to flex the index finger increased with each movement repetition.
For Par06 (BPI), the greatest forces were required to flex the PIP and DIP of the index finger. However, this participant was able to actively perform this movement (see hook grip in Table 2). This participant was most concerned with improving thumb opposition, which required an average peak force of 2 N.
Forces required for Par07 (stroke) were relatively low compared to the other participants. However, to overcome muscle spasticity, force had to be applied slowly over a longer period of time for finger extension (14 s on average).
Forearm EMG
Of the movements examined, wrist flexion and extension consistently produced the most promising EMG signals for all participants. A representative contraction from the wrist flexors and extensors for each participant is shown in Figure 4.
Figure 4.
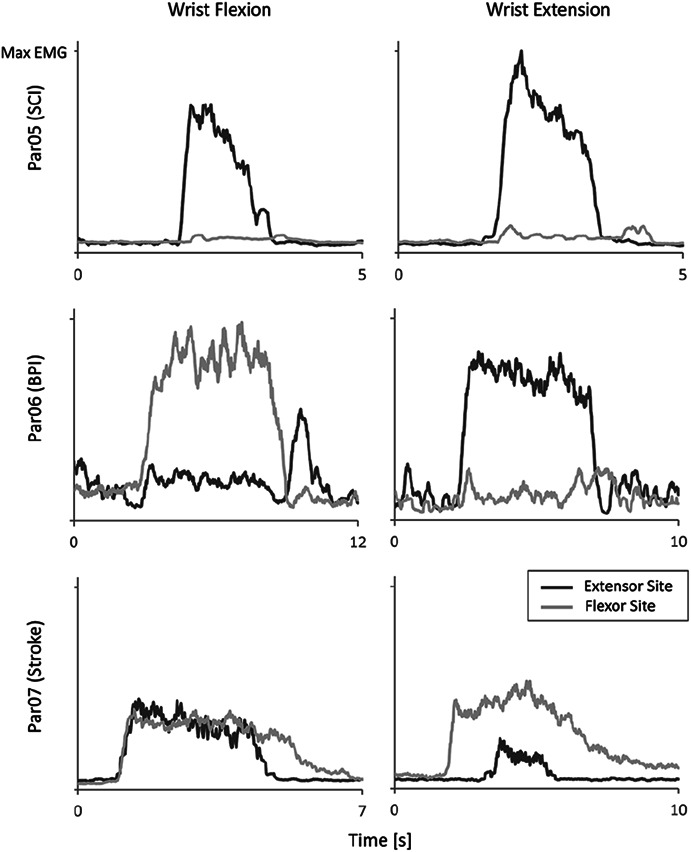
Mean absolute value of surface electromyography (EMG) signals recorded from participants’ forearms during wrist flexion (left) and extension (right) for a representative trial. Signals are normalized based on the maximum signal observed between the two channels across EMG trials. SCI: spinal cord injury, BPI: brachial plexus injury.
Participant P05 (SCI) was able to generate a voluntary extensor signal that was approximately 11 times their maximum resting signal. However, when attempting to activate their wrist flexor muscle, the pattern of EMG activity was indistinguishable from wrist extension (Figure 4). Participant P06 (BPI) was able to generate voluntary muscle signals that were at least two times their maximum resting signal for both wrist flexion and extension. Participant P07 (stroke) was able to produce a voluntary wrist flexor signal about five times larger than their resting signal but tended to co-contract their extensor muscles, although the patterns of EMG activity still appeared distinct between wrist flexion and extension movements.
Discussion
The objective of this pilot study was to ascertain preliminary end-user design requirements for an assistive powered hand exoskeleton. This was accomplished through interviews with clinicians and individuals with impaired hand function, as well as quantitative data collection with participants with hand impairment.
In the interview sessions, some recurrent responses were observed. For example, responses related to desired grasp patterns and force generation often focused on eating and drinking, highlighting these as important tasks from which design criteria could be drawn for both pinch and power grasp. In addition, most participants agreed on 200 g as an acceptable maximum weight for a wearable hand device, and they preferred being able to continually wear the device for 6 h to a full day, implying requirements for both prolonged comfort and battery life. During open discussion, six of the eight participants with impaired hand function raised the importance of being able to independently don/doff the device. While clinician responses generally aligned with individuals with impaired hand function, the topic of control requires further exploration. Clinicians, who had experience with advanced control strategies, such as myoelectric control in the context of prostheses, had concerns about the reliability of these strategies. They expressed that simpler strategies, such as a push button, should be used, especially when introducing a user to the device. Although we did not specifically ask participants with impaired hand function about control, one individual expressed a desire for intuitive control strategies (controlling the device with their “mind”) and an aversion to simple strategies, such as a push button. This points to a need for further investigation into end-user expectations with respect to potential control strategies and the impact on their willingness to accept a hand exoskeleton. The responses also revealed variability between participants with respect to their tolerance for inconveniences, such as motor noise and bulkiness, suggesting different user needs and expectations.
Detailed hand characterization sessions further confirmed variability between individuals with different diagnostic causes of hand impairment, as the three participants who returned for these sessions had substantially different levels of hand function, resting hand postures, and forces/times required for hand movement. Though it is possible that a robust hand exoskeleton could accommodate a wide variety of individuals with impaired hand function, more specific target groups may need to be identified when developing this technology. A device targeted at slowly opening the hand and helping to shape a functional grasp (as would be required for P07) may find more success without the extra machinery that would be necessary to close P05’s hand and vice versa. In addition, designing with modularity or customization options may be advantageous.
To the best of our knowledge, this is the first time that input from end-users on what would make a successful hand exoskeleton has been reported in the literature. However, other authors have reported limited aspects of design requirements that may be applicable to hand exoskeletons. Hume et al. identified functional requirements for finger RoM during a number of practical activities,16 which were similar to activities in our study (Figure 2). The maximum flexion angles observed by Hume et al. during their functional tasks were 73°, 86°, and 61° for the MCP, PIP, and DIP joints, respectively, and the average functional angles were 61°, 60°, and 39°, indicating that a powered hand exoskeleton would not need to fully flex the fingers to be functional. However, our study also highlighted that some individuals with impaired hand function may not have access to this functional RoM, even in passive motion, due to muscle stiffness or contracture. This must also be considered in hand exoskeleton design so as not to injure wearers by trying to move their fingers past available passive RoM.
With respect to grip force requirements, Smaby et al. documented that for a set of functional activities, “pinch force requirements ranged from 1.4 N to push a button on a remote to 31.4 N to insert a plug into an outlet.”17 Of the tasks studied by Smaby et al, “9 of 12, including stabbing food with a fork, required less than 10.5 N.” Therefore, 10 N of pinch grip force may be a reasonable goal to aim for in a hand exoskeleton. The grip force results for our study indicate that some individuals with impaired hand function may be able to generate grip force independently, but require help shaping their hand into a functional grasp pattern. Our results also emphasized that consideration should be given to the force required to move the digits and overcome resistance due to muscle stiffness or spasticity (which was up to 10 N in our study), in addition to the force required for a functional grip. Nycz et al. explored the torque required to induce finger extension in individuals with increased flexor tone due to traumatic brain injury.18 Our results suggest that this should be explored in other populations. In our study, moving the finger of the participant with flexor tone (P07-stroke) required a very low force applied over time to prevent a velocity dependent increase in tone, whereas force requirements were higher for the participant with SCI because of muscle stiffness. To gain a full appreciation of motor requirements for a hand exoskeleton, a more rigorous approach, combining force measurement and motion capture and considering moment of inertia effects, should be repeated with multiple patient populations.
We also examined the feasibility of two potential control strategies for a hand exoskeleton; a flex sensor on the wrist and forearm surface EMG. Our BPI participant had separable EMG signals that might be suitable for a dual-site control strategy (i.e. two-state amplitude modulation), whereas the SCI participant might be suitable for a single-site control strategy (i.e. three-state amplitude modulation).15 Our participant with stroke would not be suitable for dual-site EMG control due to co-contraction but may be able to use pattern recognition based on visually distinct patterns of EMG activity between wrist flexion and extension.19 This conclusion is supported by Ryser et al. who were able to achieve classification accuracies of 78.8%–99.2% for three gestures based on surface EMG in three participants post-stroke.20 These findings suggest that myoelectric control of a hand exoskeleton is feasible, although the best control strategy for each patient type may vary.
One limitation of our current study is the small sample size. While our results captured considerable differences between participants, the full range of potential hand exoskeleton users is not represented, and further exploration with a larger sample is required to gain a more complete understanding of end-user needs and expectations.
Scheduling also imposed limitations on the collection of interview data. Six of the interviews were completed individually, while one other interview and the clinician discussion were completed in small groups. Although it was our intention that all interviews be completed in small groups to allow for facilitated discussion among participants, this was not possible, and we recognize that this may have influenced responses between individual and group settings. In addition, no methods were used to confirm the trustworthiness of the qualitative data. A more thorough qualitative methodological approach may allow greater insight into patient experiences and expectations.
Hand measurement (such as surface EMG and force required to assist with finger movement) was assessed in a single arm position (forearm resting on table), which is not reflective of real-world use. These measurements may also be influenced by factors, such as temperature, rest, and medication. It is important to measure hand function characteristics based on the stability of the patient’s diagnosis, and future work could explore the repeatability of these measurements. The force measurement method also relied on the experimenter to determine the movement speed and to apply the force normal to the movement direction. Future work could benefit from the development of a methodology that limits these human factors. Despite these limitations, our study provides illuminating data in a relatively unexplored area, highlighting requirements to help shape future hand exoskeleton devices toward clinical success.
Conclusion
The results presented contain preliminary subjective and objective data relating to end-user needs and expectations for an assistive hand exoskeleton. This type of data may be helpful in identifying preliminary design requirements with respect to donning/doffing, maximum weight, desired grip patterns, grip strength, and wear time. Findings also revealed important differences between potential end-users that may make it difficult to define a single set of design criteria encompassing the needs of all individuals with hand impairment while remaining realistic for designers to achieve. This work highlights the importance of understanding end-users in the development of rehabilitation technology and including them in the design process. Future work should explore these findings with a larger sample size and investigate existing hand exoskeletons to assess how well they comply with the criteria identified.
Supplemental Material
Supplemental material, 10.1177_0309364620963943_Supplemental_material_1 for Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series by Quinn A Boser, Michael R Dawson, Jonathon S Schofield, Gwen Y Dziwenko and Jacqueline S Hebert in Prosthetics and Orthotics International
Supplemental Material
Supplemental material, 10.1177_0309364620963943_Supplemental_material_2 for Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series by Quinn A Boser, Michael R Dawson, Jonathon S Schofield, Gwen Y Dziwenko and Jacqueline S Hebert in Prosthetics and Orthotics International
Acknowledgments
The authors would like to thank the Glenrose Rehabilitation Hospital for supporting the involvement of its clinical staff in this research project, as well as James Austin for assistance with data collection.
Footnotes
Associate Editor: Reza Safari
Author contribution
Study conceptualization and design: all. Data collection: QAB, MRD, JSS. Data curation and analysis: QAB. Data interpretation: QAB, MRD, JSS. Writing and editing manuscript: QAB. Reviewing and editing final manuscript: all.
Declaration of conflicting interests
The author(s) disclosed no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Natural Sciences and Engineering Research Council through an Alexander Graham Bell Canada Graduate Scholarship-Masters, as well as by the TD Bank Financial Group Health Sciences Interdisciplinary Research Studentship, and the Glenrose Rehabilitation Hospital - Research and Technology Department.
Ethical approval
All participants provided signed informed consent, and this study was approved by the University of Alberta Health Research Ethics Board (Pro00068526).
Supplemental material
Supplemental material is available in this article. Direct URL citation appears in the text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.POIjournal.org).
References
- 1.GBD 2016Stroke Collaborators. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 439–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawrence ES, Coshall C, Dundas R, et al. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke 2001; 32: 1279–1284. [DOI] [PubMed] [Google Scholar]
- 3.GBD 2016Traumatic Brain Injury and Spinal Cord Injury Collaborators. Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 56–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang Y, Ding H, Zhou H, et al. Epidemiology of worldwide spinal cord injury: a literature review. J Neurorestoratol 2018; 6: 1–9. [Google Scholar]
- 5.Peters HT Page SJ and Persch A.. Giving them a hand: wearing a myoelectric elbow-wrist-hand orthosis reduces upper extremity impairment in chronic stroke. Arch Phys Med Rehabil 2017; 98: 1821–1827. [DOI] [PubMed] [Google Scholar]
- 6.Kang BB, Choi H, Lee H, et al. Exo-glove poly II: a polymer-based soft wearable robot for the hand with a tendon-driven actuation system. Soft Robot 2019; 6: 214–227. [DOI] [PubMed] [Google Scholar]
- 7.In BH, Kang BB, Sin M, et al. Exo-glove a wearable robot for the hand with a soft tendon routing system. IEEE Robot Autom Mag 2015; 22: 97–105. [Google Scholar]
- 8.Heo P, Gu GM, Lee S, et al. Current hand exoskeleton technologies for rehabilitation and assistive engineering. Int J Precis Eng Manuf 2012; 13: 807–824. [Google Scholar]
- 9.Arata J, Ohmoto K, Gassert R, et al. A new hand exoskeleton device for rehabilitation using a three-layered sliding spring mechanism. In: Proceedings of the IEEE international conference on robotics and automation, Karlsruhe, Germany, 6–10 May 2013, pp. 3902–3907. NewYork: IEEE. [Google Scholar]
- 10.Heo P and Kim J.. Power-assistive finger exoskeleton with a palmar opening at the fingerpad. IEEE Trans Biomed Eng 2014; 61: 2688–2697. [DOI] [PubMed] [Google Scholar]
- 11.Yap HK, Lim JH, Nasrallah F, et al. Characterisation and evaluation of soft elastomeric actuators for hand assistive and rehabilitation applications. J Med Eng Technol 2016; 40: 199–209. [DOI] [PubMed] [Google Scholar]
- 12.Conti R, Meli E, Ridolfi A, et al. Kinematic synthesis and testing of a new portable hand exoskeleton. Meccanica 2017; 52: 2873–2897. [Google Scholar]
- 13.Anon. What is a MyoPro orthosis, http://myomo.com/what-is-a-myopro-orthosis (2018; accessed 29 October 2019).
- 14.Clarkson HM.Musculoskeletal assessment: joint range of motion manual muscle strength. 2nd ed.New York: LWW, 2000, pp. 239–255. [Google Scholar]
- 15.Parker P Englehart K and Hudgins B.. Myoelectric signal processing for control of powered limb prostheses. J Electromyogr Kinesiol 2006; 16: 541–548. [DOI] [PubMed] [Google Scholar]
- 16.Hume MC, Gellman H, McKellop H, et al. Functional range of motion of the joints of the hand. J Hand Surg 1990; 15A: 240–243. [DOI] [PubMed] [Google Scholar]
- 17.Smaby N, Johanson ME, Baker B, et al. Identification of key pinch forces required to complete functional tasks. J Rehabil Res Dev 2004; 41: 215–224. [DOI] [PubMed] [Google Scholar]
- 18.Nycz CJ, Meier TB, Carvalho P, et al. Design criteria for hand exoskeletons: measurement of forces needed to assist finger extension in traumatic brain injury patients. IEEE Rob Autom Lett 2018; 3: 3285–3292. [Google Scholar]
- 19.Scheme E and Englehart K.. Electromyogram pattern recognition for control of powered upper-limb prostheses: state of the art and challenges for clinical use. J Rehabil Res Dev 2011; 48: 643–659. [DOI] [PubMed] [Google Scholar]
- 20.Ryser F, Butzer T, Held JP, et al. Fully embedded myoelectric control for a wearable robotic hand orthosis. IEEE Int Conf Rehabil Robot 2017; 2017: 615–621. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 10.1177_0309364620963943_Supplemental_material_1 for Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series by Quinn A Boser, Michael R Dawson, Jonathon S Schofield, Gwen Y Dziwenko and Jacqueline S Hebert in Prosthetics and Orthotics International
Supplemental material, 10.1177_0309364620963943_Supplemental_material_2 for Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series by Quinn A Boser, Michael R Dawson, Jonathon S Schofield, Gwen Y Dziwenko and Jacqueline S Hebert in Prosthetics and Orthotics International