Abstract
Clinical Video Telehealth (CVT) use is increasing and allows geographically separated care; however, this separation may affect participants behaviors. Using semi-structured in-depth interviews, we asked CVT nurse practitioners (NP), staff and patients at a VA Medical Center about perspectives on how CVT effects communication and identified three themes. They remarked on the complexity of scheduling appointments, local barriers to care, and acutely ill patients. NPs discussed how CVT altered sensory collection during the physical exam and differences in building provider-patient relationships. Patients perceptions mirrored these themes. NPs identified how CVT requires different workflow, behaviors, and use of their senses. Patients expressed similar concerns with CVT.
Keywords: ambulatory care, barriers to care, clinical video telehealth, communication, nurse practitioner
Précis:
CVT changes provider’s workflow, behaviors, and use of senses to gather clinical data. Patients are aware of some the CVT’s impact on care.
INTRODUCTION
Clinical video telehealth (CVT), one aspect of the spectrum of telehealth, is a real-time videoconferencing communication technology between two clinic locations that allows the delivery of health services when the patient and provider are geographically separated. CVT use is increasing, in part, to improve access to rural and underserved populations.1,2,3,4 Telehealth has increased during the COVID-19 pandemic due to relaxed regulations and desire to provide care that does not endanger provider or patient. Nurse practitioners (NPs) are crucial to scaling up telehealth access during this unprecedented time.5 The clinical experience of CVT may be different than the experience of in-person visits. The medical interaction in CVT is technology-mediated and limited to video and audio input. Compared with in-person visits, providers in CVT visits cannot touch or smell patients, and there are also visual and auditory differences. Because of these differences, providers and patients may need to alter their communication style, etiquette, and behavior.6 Patients and providers may have more difficulty communicating and developing interpersonal relationships when they do not meet in person.7 Though studies have found similarities in provider-patient communication between CVT and in-person visits, providers’ experiences managing differences in the medical interaction in CVT is not well described.8
How providers manage the different sensory experience of CVT can influence the success of these medical encounters.9 The sensory differences inherent to medical interactions in CVT may affect interpersonal communication. Understanding providers’ perspectives about these differences may be critical to the efficacy and adoption of CVT.10 Providers who understand the sensory limitations introduced with CVT must modify their “webside manner” to improve their own and the patient’s experience.11 Providers need to modify clinical behaviors, for example, in CVT parts of the physical exam are either not performed or are delegated to the patient or remote personnel.12 Also, providers need to adapt to sensory differences in CVT because senses such as touch provide less information hence visual and auditory sensing gain more importance.
We sought to explore the experiences of providers using CVT to better understand the technical, social, and personal factors associated with using this technology in medical interactions with patients. We also sought to explore how patients’ experiences communicating in a CVT visit compare and contrast to provider experiences. Gaining insight into provider experiences using CVT may provide a foundation for developing educational initiatives to improve medical care in CVT and other telehealth visits.
METHODS
Study Design
We conducted a qualitative interview study of providers, support staff, and patients experienced with CVT medical care to understand their perspective on CVT medical visits. This study is part of a larger study to design an intervention to improve patient-provider communication in CVT settings.13 The study was approved by the VA Central Institutional Review Board (#14-22).
Participants and Setting
We identified and invited primary care and endocrinology providers and staff experienced in CVT at a single Veterans Affairs Medical Center to participate in the interviews. Provider and staff participants must have participated in at least one CVT visit with a patient with type 2 diabetes mellitus. The medical center is a large urban medical center serving a far-reaching rural community. We also conducted additional interviews with Veterans who resided in a rural area, had a diagnosis of Type 2 diabetes mellitus, HbA1c ≥ 7.0, were age 18 years or older, had at least one CVT visit, and participated in the larger study on physician-provider communication. We excluded those patients with drug induced diabetes, dementia, a terminal medical condition with life expectancy less than 6 months, those who lived in a skilled nursing facility, and those with inadequate telephone sound quality or severe hearing impairment preventing successful completion of a telephone interview. The semi-structured in-depth telephone interviews were conducted by research staff trained in qualitative interviewing (RG, DHL). Participants provided informed consent for the study prior to their interview.
Data Collection
We developed interview questions for providers, CVT staff, and patients to gain participants’ perspectives on facilitators and barriers to communicating using CVT technology in comparison with in-person visits. Facilitators and barriers to communicating included internal and external influences on the medical interaction and the non-verbal and verbal communication of providers, staff and patients (Figure 1).14 Interview questions were developed by an expert panel of physicians and scientists and from the review of the literature. The interview questions were revised after the group reviewed and discussed each of the first four interview transcripts. Providers were asked to recall their first experience conducting a CVT visit and what techniques they learned after conducting multiple CVT visits. Interview questions included the role of technology and how one accomplishes the physical exam in CVT (Supplemental Table 1). Patients were asked about their experience communicating with the provider in a CVT visit compared with an in-person visit. Interviews were audio-recorded and transcribed verbatim. Participants were recruited for interviews until we reached thematic saturation.
Figure.
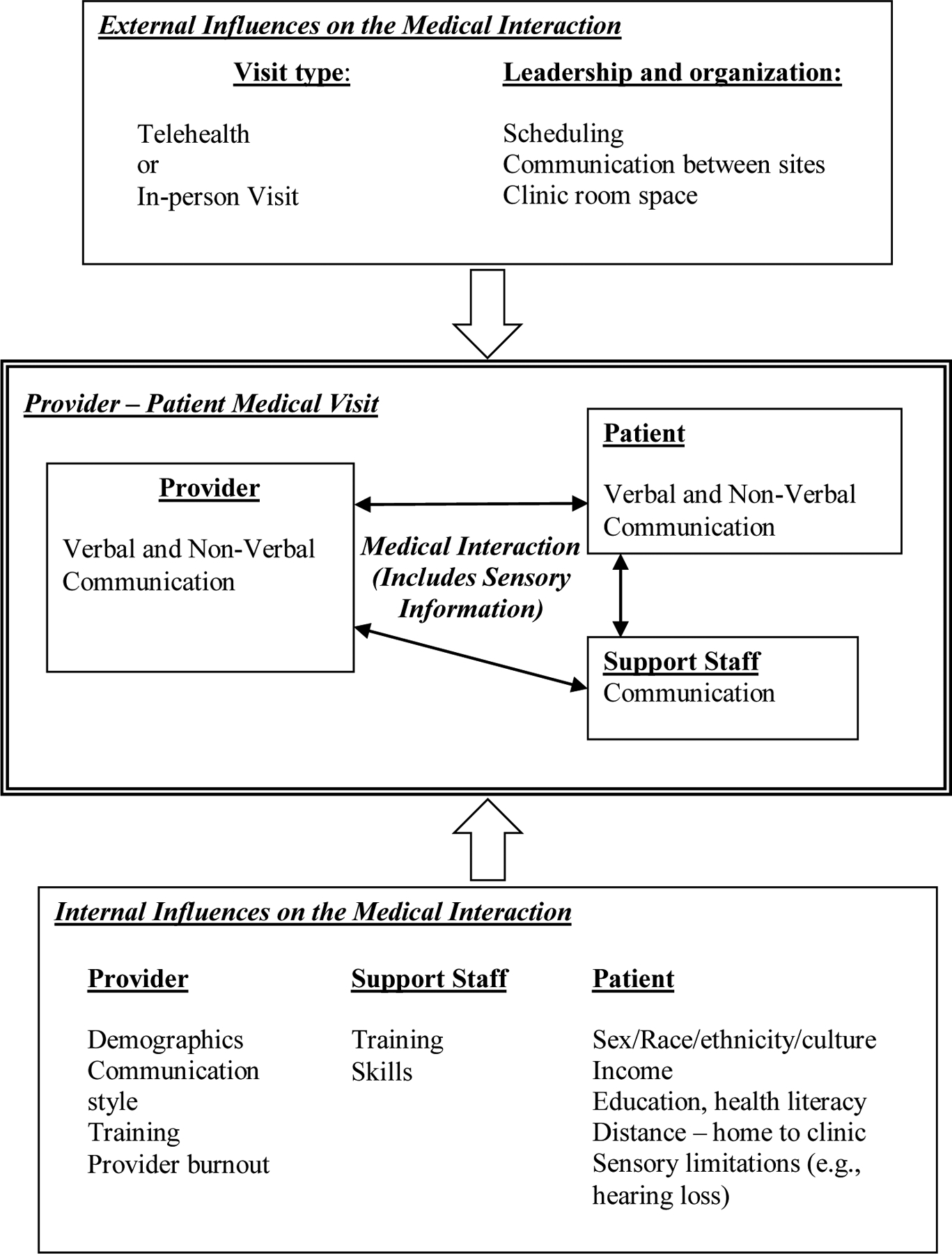
External and Internal Influences on Medical Interactions.
Data Analysis
Transcripts were coded using a grounded theory approach, in which open coding is used to identify key concepts emerging from the text.15 All authors discussed the key concepts, identified codes, and established a coding dictionary using the initial four provider transcripts. The authors separately read and coded each transcript and each researcher noted thematic categories throughout a particular transcript, especially in relation to the main research question of participants’ perspectives on barriers and facilitators to communicating in CVT compared with in-person visits. All authors then discussed the initial four transcripts on a line-by-line basis and provisionally agreed on and defined each code. Subsequent transcripts were coded by two authors (PS and RG), and discrepancies were resolved through discussion among all authors. As additional interviews were coded all authors met regularly to decide whether to add codes and edit codes in the coding dictionary. Atlas.ti (version 7.5.16) was used to sort and organize codes. Using the constant comparison method codes were then condensed into distinct themes. Coherence, credibility, and strength of those interpretations were achieved with multidisciplinary triangulation among the authors. Interviews were conducted until thematic saturation was achieved.
RESULTS
We invited 26 CVT health care providers, 17 CVT personnel and 16 patients who completed a CVT visit to participate in interviews. We interviewed nine CVT providers (seven of the nine providers were nurse practitioners), eight CVT staff, and nine patients. From the provider interviews, we identified three themes regarding how CVT changes providers’ work and evaluated patients’ perspectives related to those themes. The first theme identified several logistical challenges arising from coordinating visits and communicating with staff and patients across two sites. The second theme identified how CVT changed the way sensory information was collected during the physical exam. The third theme identified how differences in the sensory experience of CVT providers changed their communication style and behaviors used to build the provider-patient relationship. Patient perceptions mirrored these themes. The three themes are described below and in corresponding tables.
Theme 1: CVT is more logistically challenging because of the coordination required between multiple locations.
CVT providers identified how logistical complexities in CVT due to differences in location influence medical interactions (Table 1). Providers reported that compared with an in-person visit, appointment scheduling in CVT visits was less flexible because it requires facilities to be available at two locations rather than one. These interlocking schedules limited a provider’s ability to extend a clinic visit to match the complexity of medical problems and limited flexibility when there were delays. Providers developed work arounds to make visits more effective. They worked around the rigid scheduling by preparing the day before for visits. Perhaps because of providers preparation, patients did not feel rushed during the visit. Providers indicated there were challenges coordinating and communicating with staff at the remote site, noting concerns that the patient had to wait when there was a delay in connecting to rural clinics, but the patients did not believe the delays impacted their visit (Table 2). Other concerns were uniquely noted by providers. For example, having to work with several clinic sites, some CVT NPs reported needing contingencies to resolve issues for complicated and acutely ill patients, during and between visits (Table 1).
Table 1.
Provider Quotes
| THEME 1 – CVT IS MORE LOGISTICALLY CHALLENGING | |
|---|---|
| SUBTHEME | Illustrative quote(s) |
| Limited time flexibility during visits |
|
| Providing care for acutely ill patients |
|
| THEME 2 - CHANGES TO COLLECTING SENSORY INFORMATION FROM THE PHYSICAL EXAM | |
| SUBTHEME | Illustrative quote |
| Reliance on remote staff |
|
| THEME 3 – SENSORY CHALLENGES IN CVT TO BUILD A PATIENT-PROVIDER RELATIONSHIP | |
| SUBTHEME | Illustrative quote(s) |
| Using same technology to communicate a problem |
|
| Challenges educating patients |
|
Table 2.
Compare/Contrast Theme 1- CVT is logistically more challenging
| Provider Quotes | Patient Quotes |
|---|---|
Provider does not have a problem with audio quality.
|
Patient does not have a problem with audio and visual quality.
|
Patients may find CVT visits challenging because of sensory impairments such as difficulty hearing.
|
Although patients may have hearing impairments, they did not have a problem with audio or visual quality.
|
Theme 2: Providers changed how they collected sensory information from the physical exam.
Providers interviewed noted a different sensory experience with the physical exam in CVT and their reliance on technology and remote staff changed how they work compared with in-person visits (Table 1). Although providers and staff described equipment such as close-up cameras and stethoscopes which have capabilities (e.g. higher sensitivity and imaging resolution) not usually available in an in-person visit, providers also noted challenges in the medical interaction such as limited views and not being able to use all their senses to examine their patient. There were challenges relying on CVT staff to complete the physical exam due to varying skills and knowledge or ability to communicate the needed sensory information. Furthermore, providers who work in multiple CVT clinics may not know each CVT staff’s qualifications. Patients were also concerned about providers’ ability to fully conduct a physical exam for findings such as a rash (Table 3).
Table 3.
Compare/Contrast Theme 2- Providers changed how they collected sensory information from a physical exam
| Provider quotes | Patient quotes |
|---|---|
Provider is concerned about doing parts of the physical exam.
|
Patient is concerned he or she cannot show the provider certain physical problems over CVT.
|
Provider relies on CVT personnel to conduct physical exams.
|
Patient is impressed with how CVT personnel help the provider conduct aspects of the physical exam.
|
TCT states CVT personnel are helpful and make the patient feel more comfortable with telehealth.
|
Patient states the CVT personnel is helpful.
|
Though CVT does not allow tactile sensing when completing a physical exam, providers learned that barriers may be reduced with qualified staff. Providers described delegating the physical exam to CVT staff who “become the hands of the doctor.” One NP provider described, “They’re like my fingers.” One patient was impressed with how the nurse was able to “carry out the wishes of the doctor” (Table 3). Some providers believed that patients received more attention during CVT visits compared to in-person visits, saying that patients could interact with both provider and the CVT staff and/or telehealth Clinical Technician (TCT) personnel. One TCT said, “they [patients] feel like it’s real one-on-one attention.” (Table 3)
Theme 3: Providers noted that CVT presented sensory challenges to building a relationship.
The CVT providers and staff in our study reported several challenges using their senses of sight, smell, hearing, and touch when communicating with patients via CVT. (Table 4). For example, the traditional greeting with a handshake that begins or continues a trusting relationship must be accomplished with verbal and non-verbal communication. Providers stated the physical distance made it difficult to develop a relationship, and patients said telehealth may not be personal enough to develop a relationship with the provider (Table 4). In addition, providers raised concern about missing patients’ body language because the typical camera view includes only the upper body. This missed body language may alter the providers’ impression of what the patient is trying to communicate. Providers noted a need to be more deliberate themselves, needing to pay more attention to their own communication behaviors than in traditional in-person visits. Providers felt that it was harder for them to maintain eye contact. Looking at the camera to make eye contact during CVT was not a natural skill. Because the camera location may be offset from the screen, the more natural behavior of looking “directly” at the patient on the screen has the effect from the patients’ perspective of making the provider appear to be looking away from the patient. Patients explained they had to speak louder to get the provider’s attention because the provider was looking away from the camera (Table 4). Another sensory challenge was not being able to readily assess if they are effectively communicating with their patients. For example, providers might miss body language indicating patients could not hear or see something. Providers had to ask patients to let them know if the technology was not working (Table 1). Nonetheless, providers and staff also suggested that telehealth may facilitate communication because patients are less stressed from issues with travel to and parking at a large hospital outpatient clinic site.
Table 4.
Compare/Contrast Theme 3- Sensory challenges in CVT to build a patient-provider relationship
| Provider quotes | Patient quotes |
|---|---|
Provider thinks physical distance makes it harder to build a relationship.
|
Patient does not think that telehealth is personal enough to express his/herself.
|
Provider needs to deliberately build a relationship with the patient.
|
Patient explains the provider is open to listen to what is going on in the patient’s life.
|
Provider states making eye contact with the patient is important.
|
Patient explains the provider was not attentive and the patient had to speak up to be heard.
|
Because CVT providers and staff perceived barriers providing education and demonstrating procedures to their telehealth patients, they developed alternative methods to educate their patients. In CVT, simply handing their patients educational handouts or an aftercare summary is not possible. Providers developed work-arounds to this challenge by sending CVT technicians the information to print locally or mailing the resources directly to the patient (Table 1). Communicating on CVT challenged usual teaching methods such as using touch and feel to demonstrate, for example, how to self-administer insulin, and patients with vision or hearing impairments sometimes struggled with communication during CVT particularly when they forgot their sensory aids. Not only does CVT impact providers’ use of their senses in a medical visit, but also impacts the patients’ sensory ability to get the most from their visit. Providers’ and staff’s comments highlighted how CVT changes the use of their senses compared to in-person visits and how these differences impose unique considerations in delivering care remotely.
DISCUSSION
In this qualitative study we interviewed telehealth providers, staff, and patients about experiences using CVT to describe the factors associated with using this technology. Our insights may provide a foundation for developing educational initiatives to improve medical care in CVT and other telehealth visits. We identified three themes based on providers experience that describe differences in the medical interaction between CVT and in-person visits. The first theme identified how CVT visits were more complex due to the decreased flexibility from the rigid scheduling and coordination between two clinical sites. The next two themes identified the impact of CVT on providers’ sensory experiences. The second theme describes how CVT limits providers’ use of their senses to conduct a physical exam compared with in-person visits. The third theme reflects providers’ statements concerning the increased effort needed to build a provider-patient relationship due to CVT limiting their sensory experience. Our findings suggest that communicating on telehealth is not just learning how to use an innovative technology, but includes the added challenges of coordinating visits with a less flexible schedule, relearning how to collect information about physical findings, and recognizing how sensory differences in the technology-mediated medical interaction change providers’ practices. Patients in our study also experienced parallel challenges using CVT technology and they highlighted concerns about the adequacy of the physical exam and developing trust.
Our study adds to the literature describing CVT by identifying provider’s perceptions of the complexity caused by geographic separation of the provider and patient. Unlike a traditional clinic, CVT requires scheduling rooms at two sites, one HIPAA compliant CVT enabled office for the provider and one CVT enabled clinic room with examination tools. Patient examination rooms may be scheduled sequentially with different providers. These scheduling differences limit the flexibility of providers to extend visits for complicated or late arriving patients. When there was difficulty communicating between sites, providers struggled to determine if patients were ready to be seen, resulting in late starts and shortened visits and struggled to get clinical assistance. Providers also reported increased complexity determining how to order tests for patients since each clinic’s local resources vary. Though CVT has benefits such as improved access to care, external influences on the CVT visit create challenges for the medical interaction between patient, provider, and support staff (Figure). Certain challenges providers experience affect how they work, but may not impact the patient’s CVT experience. For example, patients may not be bothered by technical delays. Patients did not express concern about the CVT personnel’s varying skills but were impressed with their ability to answer questions and carry out the NPs’ requests. However, certain challenges like lack of eye contact did impact the patient’s CVT experience. Alerting patients when they have to look away from the camera would be one way providers could improve the patient experience.
Our study also adds to the literature examining communication in telehealth by highlighting how the sensory experience is crucial to medical interactions (Figure). Communication is not just verbal, but also involves sending and receiving nonverbal cues that are observed by sight (body language), hearing (paralanguage), touch (haptics), and even smell. Providers in our study identified the importance of monitoring their own body language (making eye contact via looking at the camera) and understanding that their own observations of patients’ non-verbal communication are limited by the standard camera view of only the upper body of their patients. Providers also felt the technology created a barrier in educating their patients since they could not simply hand them written information or demonstrate using a hands-on approach. Providers with CVT experience reported changing their behaviors or creating work-arounds to overcome these challenges. For example, providers can prepare for visits beforehand to account for less time flexibility. Providers and staff also felt CVT may sometimes improve patients’ communication because they did not have to travel long distances to the urban medical center, and as a result may be less tired or stressed. Both providers and patients found it helpful to have a technician or nurse in the room because they increased attention to the patient.
CVT also affects the sensory input available for a CVT provider to physically examine their patients. Providers are limited to only two of their senses and these may be further limited by the quality of the electronic transmission. They must rely on technology and the remote staff to assist in their formal physical exam. Further, the skills and training of the staff vary from clinic to clinic. Though the technology helps, it does not fully replace an in-person exam where providers get traditional sensory inputs (e.g., touch and smell) about their patients. The providers also report missing parts of the informal physical exam such as seeing the patient walk into the room, shaking their hand, and watching their mannerisms. Patients also had concerns about the adequacy of the physical exam. Guidelines are needed to assist providers for deciding on when and the urgency of referral for an in-person examination.
Though few studies have evaluated the provider’s experience in the CVT setting, our findings are consistent with prior research that identified logistical barriers to CVT care including scheduling complexities, communication with staff at remote sites, and not completing a physical exam or relying on staff to complete physical exams.16–18 Studies have found that verbal communication can be significantly impacted by CVT. In a study comparing in-person to CVT visits, analysis of the recorded visits showed patients more frequently asked for physicians to repeat themselves suggesting difficulty with audio communication.19 In our study, providers commented about the importance of encouraging patients to speak up about any technical difficulties, and providers also noted the importance of verbal communication because non-verbal communication may be missed over CVT. In an experimental study comparing communication in CVT vs. in-person visits, providers were less satisfied with CVT because they could not understand what was on the patients’ mind and felt it was harder to connect with their patients and build a relationship.20 Experienced CVT providers in our study further describe the importance of developing the unique skills to be effective in seeing patients at remote locations. The current literature looking at provider experiences with CVT shows that providers that have mastered the clinical situation are satisfied with this clinical setting.21
This study had several limitations. Most of the providers interviewed were nurse practitioners, thus, it is possible our results may have differed if we interviewed more physicians. Second, the providers are all focused in internal medicine related practice, limiting our evaluation of other specialties. However, all health care providers rely on the same ability to communicate and examine patients. Third, the interviewed participants are all employees of or patients affiliated with a single Veteran Affairs Medical Center so our results might not generalize to other VA providers, non-VA providers, or other patients. Finally, we focused on care in CVT and not telehealth directly with patients on the their own smart devices, which may have different challenges. Despite these limitations, the interviews are a notable strength of this study because they provide rich data from multiple perspectives on the barriers and facilitators of communicating via CVT and provides novel insights to how CVT influences providers’ sensory experiences. Another notable strength is the perspectives our study provides on the CVT experience and its timeliness when telehealth is increasingly utilized due to the COVID-19 pandemic and will likely become a new paradigm particularly for nurse practitioners and the Veteran Affairs Health Care System.22
Our study data suggests how providers and health systems might make improvements in the quality of CVT patient-provider interactions. Logistical barriers may be reduced by improved communication and teamwork among staff at different sites. This might include occasional travel so staff could meet in person, train together, and learn specifics about distal sites. Barriers to providers providing patient education could be reduced with educational resources for patients that the provider could edit or mark-up and then print at the patient site. Providers, especially those new to CVT, could benefit from educational resources to teach best practices to navigate logistical complexities coordinating with a distant site and to develop communication styles conducive to building a relationship (e.g., “webside” manner).23 Also, learning to compensate for the inherent limitations on their senses of conducting a CVT visit and performing a physical exam with the assistance of local staff and patients.24 Furthermore, the data may help health care systems efforts to increase adoption of telehealth. Systems that prioritize reducing logistical barriers, work to improve communication between sites and respective staff, and ensure use of equipment that facilitates verbal (e.g., clear audio) and non-verbal communication (e.g., eye contact) will improve provider and patient satisfaction and desire to use telemedicine technologies such as CVT or telemedicine direct to patients’ homes. For example, health care systems might streamline ways to provide patients with written material, develop contingencies for acutely ill patients, and arrange and maintain equipment so that the provider can appear to maintain eye contact with the patient. As CVT is increasingly used to improve access for rural patients, reduce patients’ travel times, allow for social distancing, and to open other opportunities for remote medical care delivery, more providers and patients will need the specific skills to be effective in this virtual environment.
Supplementary Material
Acknowledgements:
This material is based upon work supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development grant #SDR 12-282 (PI-Gordon).
Footnotes
Publisher's Disclaimer: Disclaimer:
Publisher's Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs (VA) or the United States Government.
The data in part was presented as a poster presentation at the 2018 Annual Meeting of the Society of General Internal Medicine in Denver.
Conflicts of Interest:
The authors declare that they do not have a conflict of interest.
REFERENCES:
- 1.Bashshur RL, Armstrong PA, and Youssef ZI eds. Telemedicine: Explorations in the Use of Telecommunications in Health Care. Springfield, IL: Charles C Thomas; 1975. [Google Scholar]
- 2.Field MJ eds. Telemedicine: A Guide to Assessing Telecommunications for Health Care. Washington, DC: National Academy Press; 1996. [PubMed] [Google Scholar]
- 3.Park J, Erikson C, Han X, Iyer P. Are State Telehealth Policies Associated with the Use Of Telehealth Services Among Underserved Populations? Health Aff. 2018;37(12):2060–2068. [DOI] [PubMed] [Google Scholar]
- 4.Adams SV, Mader MJ, Bollinger MJ, et al. Utilization of Interactive Clinical Video Telemedicine by Rural and Urban Veterans in the Veterans Health Administration Health Care System. J Rural Health. 2019;35(3):308–318. [DOI] [PubMed] [Google Scholar]
- 5.Henderson K, Davis TC, Smith M, King M. Nurse Practitioners in Telehealth: Bridging the Gaps in Healthcare Delivery. J Nurs Pract. 2014; 10: 845–850. [Google Scholar]
- 6.Chua IS, Jackson V, Kamdar M. Webside Manner during the COVID-19 Pandemic: Maintaining Human Connection during Virtual Visits. J Palliat Med. 202023(11):1507–1509. [DOI] [PubMed] [Google Scholar]
- 7.Yudkowsky R, Valdes W, Raja S, Kiser R. Assessing residents’ telehealth communication skills using standardized patients. Med Ed. 2011;45(11):155. [DOI] [PubMed] [Google Scholar]
- 8.Dalley D, Rahman R, Ivaldi A. Health Care Professionals’ and Patients’ Management of the Interactional Practices in Telemedicine Videoconferencing: A Conversation Analytic and Discursive Systematic Review. Qual Health Res. 2020. doi: 10.1177/1049732320942346. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 9.Lupton D, Maslen S. Telemedicine and the senses: a review. Sociol Health Illn. 2017;39(8):1557–1571. [DOI] [PubMed] [Google Scholar]
- 10.Zanaboni P, Wootton R. Adoption of telemedicine: from pilot stage to routine delivery. BMC Med Inform Decis Mak. 2012;12(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gustin TS, Kott K, Rutledge C. Telehealth Etiquette Training: A Guideline for Preparing Interprofessional Teams for Successful Encounters. Nurse Educ. 2020; 45(2):88–92. [DOI] [PubMed] [Google Scholar]
- 12.Weinstein RS, Krupinski EA, Doarn CR. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med Clin Noth Am. 2018;102(3):533–544. [DOI] [PubMed] [Google Scholar]
- 13.Gordon HS, Solanki P, Bokhour BG, Gopal RK. “I’m Not Feeling Like I’m Part of the Conversation” Patients’ Perspectives on Communicating in Clinical Video Telehealth Visits. JGIM. 2020; 35(6) 1751–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Street RL. Communication in Medical Encounters: An Ecological Perspective. In Thompson TL, Dorsey AM, Miller KI, Parrott R eds., Handbook of Medical Communication. Mahwah, NJ: Lawrence Erlbaum Associates; 2003. [Google Scholar]
- 15.Chapman AL, Hadfield M, Chapman CJ. Qualitative research in healthcare: an introduction to grounded theory using thematic analysis. J R Coll Physicians Edinb 2015;45(3):201–5. [DOI] [PubMed] [Google Scholar]
- 16.Fatehi F, Gray LC, Russell AW. Telemedicine for clinical management of diabetes - a process analysis of video consultations. J Telemed Telecare. 2013;19(7):379–82. [DOI] [PubMed] [Google Scholar]
- 17.Flodgren G, Rachas A, Farmer AJ, Inzitari M, Shepperd S. Interactive telemedicine: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2015;7:1–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martinez RN, Hogan TP, Balbale S et al. Sociotechnical Perspective on Implementing Clinical Video Telehealth for Veterans with Spinal Cord Injuries and Disorders. Telemed J E Health. 2017;23:567–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Agha Z, Roter DL, Schapira RM. An Evaluation of Patient-Physician Communication Style During Telemedicine Consultations. J Med Internet Res. 2009;11: e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu W, Saxon DR, McNair B, et al. Endocrinology Telehealth Consultation Improved Glycemic Control Similar to Face-to-Face Visits in Veterans. J Diabetes Sci Technol. 2016;10:1079–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Becevic M, Boren S, Mutrux R, et al. User Satisfaction With Telehealth Study of Patients, Providers, and Coordinators. 2015;34:337–349. [DOI] [PubMed] [Google Scholar]
- 22.Gardenier D, Ballard-Hernandez J, O’Donnell M. Is telehealth here to stay? J Nurs Pract 2021 10.1016/j.nurpra.2020.12.0081555-4155/ epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rutledge CM, Kott K, Schweickert PA, et al. Telehealth and eHealth in nurse practitioner training: current perspectives. Adv Med Educ Pract. 2017;8:399–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Benziger CP, Huffman MD, Sweis RN, Stone NJ. The Telehealth Ten: A Guide for a Patient-Assisted Virtual Physical Examination. Am J Med. 2020;134:48–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


