Abstract
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has infected millions of people worldwide. SARS-CoV-2 belongs to the Betacoronavirus genus, containing the mouse hepatitis virus (MHV), an extensively studied animal coronavirus. Since MHV and SARS-CoV-2 share the same genus, MHV could offer insights relative to SARS-CoV-2 studies. MHV-3 strain causes hepatitis and cellular injury, making MHV-3 infection one of the best models for this debilitating disease. Surrogate coronaviruses have been used for virus resistance and inactivation studies, and although real‐life conditions using SARS-CoV-2 should be encouraged, their use needs to be balanced with safety and costs. MHV can be manipulated under BSL2 laboratory conditions, unlike SARS-CoV-2, making it a model for studying the virucidal effects on coronaviruses. In this study, we used the betacoronavirus MHV-3 as a model to investigate the virucidal activity of an air disinfection equipment named STR Solution®, an air sterilizer with patented technology. MHV-3 was dried on different surfaces and exposed at varying distances from the STR Solution® equipment and at different exposure times. The residual infectivity was evaluated using the endpoint method. There was not a significant reduction (mean p-value = 0.4) of the viral titer under STR Solution® exposition. STR Solution® caused a slight decrease of the infectious particles’ titer (> 1 log10) only under the following conditions: polypropylene at 3 m, for 1 and 3 h (1.2 log10 reduction TCID50) and Sus domesticus skin at 0.05 m, for 1 h (1.3 log10 reduction TCID50), and at 3 m for 1 h (1.2 log10 reduction TCID50). These and other studies confirm the usefulness of this model to evaluate virucidal activity.
Keywords: MHV-3, SARS-CoV-2 model, STR solution®, Air sterilizer
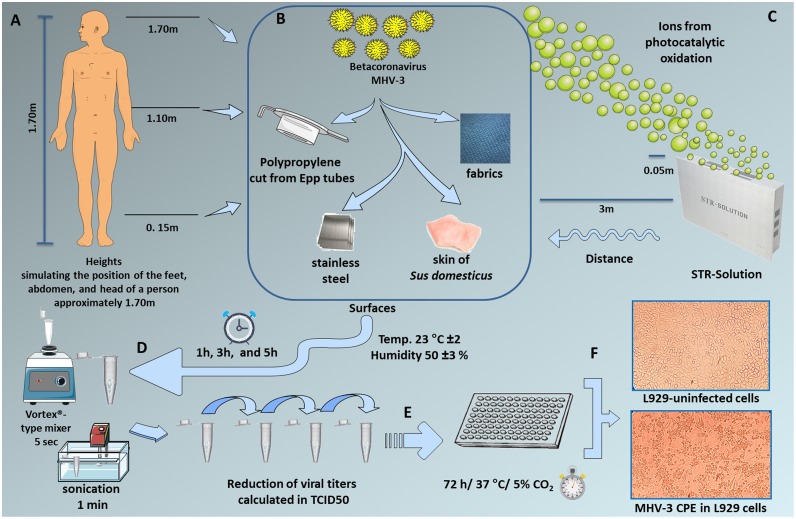
The severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) has infected millions of persons, causing the pandemic coronavirus disease 2019 (COVID-19). SARS-CoV-2 turned up in 2019 and was firstly reported in Wuhan, China (Huang et al., 2020). According to the World Health Organization (WHO, 2021), the virus rapidly spread worldwide. Researchers collaborate to develop coronavirus studies, and antiviral strategies are an area of significant focus and urgency. SARS-CoV-2 is an enveloped positive-sense RNA virus, and it is expected to be inactivated by extreme pH and temperature, halogens, radiation, peroxides, ethanol 70 % w/v, or 0.1 % sodium hypochlorite (Kampf et al., 2020; World Health Organization, 2021). Coronaviruses are classified under the order Nidovirales, family Coronaviridae, and subfamilies Letovirinae and Orthocoronavirinae, which is divided into four genera: Alphacoronavirus, Betacoronavirus, Gammacoronavirus, and Deltacoronavirus (International Committee on Taxonomy of Viruses Virus Taxonomy, 2019). SARS-CoV-2 belongs to the Betacoronavirus genus, which contains the mouse hepatitis virus (MHV) and human coronaviruses such as HCoV−OC43 and HCoV-HKU. Other human coronaviruses as HCoV-229E and HCoV-NL63, both last under the genus Alphacoronavirus (ICTV). Murine hepatitis virus (MHV) is an extensively studied animal coronavirus, and since MHV and SARS-CoV-2 share the same genus, MHV could offer insights relative to SARS-CoV-2 studies (Körner et al., 2020). MHV-1 causes severe respiratory disease, while the JHM strain of mouse hepatitis virus (JHMV) causes severe encephalitis, and MHV-3 causes hepatitis and cellular injury through the activation of the coagulation cascade, making MHV-3 infection one of the best models for this debilitating disease (Lampert et al., 1973; Levy et al., 2000; Körner et al., 2020; Weiner, 1973). Since before the COVID-19 pandemic, surrogate coronaviruses have been used for virus resistance studies. MHV-3, for example, remained infectious on steel templates for days to weeks at room temperature and HCoV-229E remained infectious for up to five days at room temperature on surface materials such as polytetrafluoroethylene, steel ceramic, and glass (Casanova et al., 2010; Lamarre and Talbot, 1989; Warnes et al., 2015). We know that real‐life conditions using SARS-CoV-2 should be encouraged, but this use should be balanced with safety and costs. Unlike SARS-CoV-2, MHV-3 can be manipulated under BSL2 laboratory conditions, making MHV-3 a model for studying the pathogenesis and immune response to coronaviruses and, as in this study, for virucidal activity. Therefore, here we used MHV-3 as a model for coronavirus to investigate the virucidal potential of an air disinfection equipment named STR Solution®. STR Solution® is an air sterilizer with patented technology. The equipment virucidal mechanism is based on volatilizing the natural sterilizer ions from photocatalytic oxidation (reviewed by Boyjoo et al., 2016) into the air in an indoor space from 100 m2 or 250 m3. This equipment is proposed as a virucidal tool to inactivate the virus in the air and on surfaces. It is sold as equipment that sterilizes the surroundings silently, making it virus-free. To evaluate the virucidal potential of the STR Solution® on viruses deposited on surfaces, we used the MHV-3 as a model. We exposed the virus particles distributed on different surfaces, varying the distance and exposure times to the STR Solution® equipment, and evaluated the residual infectious virus using the endpoint method (Reed and Muench, 1938) (Fig. 1 ). Murine fibroblast cells (L929) (ATCC CRL-6364) were used for MHV-3 replication and titration. L929 were maintained in a 5% CO2 atmosphere at 37 °C in Eagle’s Minimum Essential Medium (MEM) (Gibco BRL, Invitrogen, Carlsbad, CA, USA) supplemented with 8% fetal bovine serum (FBS) (Cultilab, Brazil), 25 μg/mL fungizone (Amphotericin B) (Cristália, São Paulo, Brazil), 500 U/mL penicillin (Cristália, São Paulo, São Paulo, Brazil) and 50 μg/mL gentamicin (Schering-Plough, São Paulo, Brazil). Clarice Arns, UNICAMP, Brazil, gently provided the MHV-3 (Garcia et al., 2021). For virus replication, the viral stock was added to 25 × 106 L929 in the T150 cell culture flask at a multiplicity of infection (MOI) of 0.01, which were incubated for 1 h adsorption at 37 °C, 5% CO2 using MEM, and after this period, MEM was supplemented with 2% FBS and incubated under the same conditions for 72 h. The cytopathic effect (CPE) was evaluated daily. When it reached 90 % of the cells, the supernatants were aspirated, centrifuged 5000 g, 10 min to remove cell debris, tittered in L929 in 96 well plates, and median tissue culture infectious dose (TCID50) was calculated using the endpoint method (Reed and Muench, 1938). The titer of the initial viral stock was 106 TCID50/mL. A test model for the virucidal efficacy of STR Solution® was developed simulating natural conditions, such as the distribution of virus on surfaces, at different distances from the equipment, under controlled temperature and humidity conditions (Fig. 1). The virucidal efficacy is dependent on the natural conditions, and various surfaces where the virus could be deposited were considered in this methodological approach. As ambient humidity and room temperature affect the virus, we controlled the room temperature around 23 °C ± 2 and 50 ± 3 % relative humidity. As surfaces, the following materials were used: polypropylene cut from Eppendorf tubes, stainless steel, polyester fabric (similar to those used to make lab coats), and skin of Sus domesticus. The dehaired skin of Sus domesticus was obtained from a local slaughterhouse. All materials were previously decontaminated by immersion in 0.2 % sodium hypochlorite for 30 min, irradiated by ultraviolet light for 30 min, and cut into 1 cm2 pieces. After the decontamination treatment, materials were washed with sterile water. We used 10 μL containing 104 TCID50 of MHV-3, deposited onto the materials (Fig. 1B), and dried for 40 min. The MHV-3 contaminated materials and controls were exposed in front of the STR solution® at distances of 0.05 m and 3 m (Fig. 1C) at different heights, simulating the feet, (0.15 m) abdomen (1.10 m), and head (1.70 m) of a person 1.70 m (Fig. 1A) for 1 h, 3 h or 5 h (Fig. 1D). For the negative controls, viruses were exposed in environments without STR solution® at the same surfaces, times, temperature, and humidity. Besides that, the virus kept at 4 °C was tittered. After different contact times, the MHV-3 contaminated materials and the controls were resuspended in 2 mL microtubes containing 500 μL MEM and homogenized using a vortex type homogenizer for 5 s and sonicated at frequency 40 kHz for 1 min (Fig. 1D). The viruses were tittered in L929 by TCID50 assay, using series of the dilution (10−1 – 10-4) in which eight wells were infected with each dilution point, and eight wells were not infected (cell control) (Fig. 1E). The 96 wells microplate was incubated for 72 h, at 37 °C, with 5% CO2, and the CPE was evaluated daily (Fig. 1F). The reduction rate was calculated by comparing the antiviral product test specimen and the control specimen on a logarithmic scale. The controls for calculating each studied condition were maintained in an environment under the experimental conditions described above (same surfaces, times, temperature, and humidity) but without exposure to STR Solution®. Besides that, as tissue culture methods would be used to determine the virus titer, the STR Solution® may affect the L929 culture. The cytotoxic effect on L929 was evaluated, and we confirmed that STR Solution® did not affect the cells. Also, no cytotoxic effect of the used materials on L929 was detected. The cytotoxic test of the materials was performed under the same conditions as the actual test but without virus and STR solution® action. The assays were carried out in duplicate. The statistical significance was determined using the Holm-Sidak method, with alpha = 5.000 % and p values were greater than 0.05 ranging from 0.077 to 0.8. T ratio ranged from 0.179 to 4.169. STR Solution® caused a weak reduction of virus infection (> 1 log) only under the following conditions: polypropylene at 3 m, for 1 h and 3 h (1.2 Log10 reduction TCID50) and skin of Sus domesticus, at 0.05 m, for 1 h (1.3 Log10 reduction TCID50), and at 3 m for 1 h (1.2 Log10 reduction TCID50) (Table 1 ). In the current study, we found that MHV-3 was not significantly inactivated when exposed to STR Solution®. However, MHV-3 showed up as a suitable model to study virucidal activity for air disinfection. This model uses lower levels of biosafety since MHV-3 can be manipulated under BSL2 conditions and consequently lower costs and safety risks. MHV was also recommended by the Australian Government Department of Health (Australian Government Department of Health, 2021) as surrogate viruses for disinfectant efficacy tests. Ahmed et al., 2020 evaluated the virus RNA decay of MHV and SARS-CoV-2 comparatively, identified no statistically significant difference between RNA decay, and suggested it as a suitable persistence surrogate. Our method using MHV3 can also be adapted to test the virucidal activity of skin disinfectants, fabrics, and other materials, similarly as was tested for SARS-CoV-2 (Campos et al., 2020a,2020b; Campos et al., 2021).
Fig. 1.
Experimental schematic representation of betacoronavirus MHV-3 as a model for SARS-CoV-2 to investigate the virucidal activity of equipment STR Solution®. Test model for the virucidal efficacy of STR Solution® simulating natural conditions at different heights, simulating the feet, abdomen, and head of a person 1.70 m (A). The virus stock was diluted and deposited onto the surfaces: polypropylene cut from Eppendorf tubes, stainless steel, fabrics and skin of Sus domesticus (B) at distances of 0.05 m and 3 m (C). The room temperature was controlled around 23 °C ± 2 and 50 ± 3 % relative humidity. The materials containing the viral particles were exposed at different time points (1 h, 3 h, and 5 h) to the STR solution® (D). The materials were eluted in microtubes containing FBS-free MEM and homogenized using a vortex type homogenizer for 5 s and subjected to sonication for 1 min (D). The viruses were tittered using series of the dilution (E). The 96 wells microplate was kept for 72 h, by incubation at 37 °C, 5% CO2, evaluating the cytopathic effect daily (F).
Table 1.
Reduction of viral titers calculated in TCID50.
| Contact time (h) | Distance from equipment (m) | Support surface virus | Log10 reduction TCID50 | % reduction | Virucidal | SD* |
|---|---|---|---|---|---|---|
| activity* | ||||||
| 1 | 0.05 | Fabric | <1 | <90 | WA* | 0 |
| 1 | 3 | Fabric | <1 | <90 | WA | 0 |
| 1 | 0.05 | Polypropylene | <1 | <90 | WA | 0 |
| 1 | 3 | Polypropylene | 1.2 | 96.8 | Weak | 579 |
| 1 | 0.05 | stainless steel | <1 | <90 | WA | 11,873 |
| 1 | 3 | stainless steel | 1 | 90 | Weak | 0 |
| 1 | 0.05 | skin of Sus domesticus | 1.3 | 97.5 | Weak | 131 |
| 1 | 3 | skin of Sus domesticus | 1.2 | 96.8 | Weak | 290 |
| 3 | 0.05 | Fabric | <1 | <90 | WA | 0 |
| 3 | 3 | Fabric | <1 | <90 | WA | 0 |
| 3 | 0.05 | Polypropylene | <1 | <90 | WA | 0 |
| 3 | 3 | Polypropylene | 1.2 | 96.8 | Weak | 0 |
| 3 | 0.05 | stainless steel | <1 | <90 | WA | 0 |
| 3 | 3 | stainless steel | <1 | <90 | WA | 579 |
| 3 | 0.05 | skin of Sus domesticus | <1 | <90 | WA | 0 |
| 3 | 3 | skin of Sus domesticus | <1 | <90 | WA | 19,546 |
| 5 | 0.05 | Fabric | <1 | <90 | WA | 0 |
| 5 | 3 | Fabric | <1 | <90 | WA | 0 |
| 5 | 0.05 | Polypropylene | <1 | <90 | WA | 201 |
| 5 | 3 | Polypropylene | <1 | <90 | WA | 135 |
| 5 | 0.05 | stainless steel | <1 | <90 | WA | 0 |
| 5 | 3 | stainless steel | <1 | <90 | WA | 52 |
| 5 | 0.05 | skin of Sus domesticus | <1 | <90 | WA | 73 |
| 5 | 3 | skin of Sus domesticus | <1 | <90 | WA | 119 |
SD- Standard deviation, WA- without activity.
Author contributions
G.P.O. carried out the experiment. E.G.K. proposed the experiments, analyzed the data, and wrote the manuscript together G.P.O.
Author statement
Graziele Pereira Oliveira carried out the experiment. Erna Geessien Kroon proposed the experiments, analyzed the data, and wrote the manuscript together with Graziele Pereira Oliveira.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We acknowledge HPF Surgical Ltda for the equipment loan.
References
- Ahmed W., Bertsch P.M., Bibby K., Haramoto E., Hewitt J., Huygens F., Gyawali P., Korajkic A., Riddell S., Sherchan S.P., Simpson S.L., Sirikanchana K., Symonds E.M., Verhagen R., Vasan S.S., Kitajima M., Bivins A. Decay of SARS-CoV-2 and surrogate murine hepatitis virus RNA in untreated wastewater to inform application in wastewater-based epidemiology. Environ. Res. 2020;191:110092. doi: 10.1016/j.envres.2020.110092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Australian Government Department of Health https://www.tga.gov.au/surrogate-viruses-use-disinfectant-efficacy-tests-justify-claims-against-covid-19. Accessed 08/24/2021.
- Boyjoo Y., Sun H., Liu J., Pareek V.K., Wang S. A review on photocatalysis for air treatment: from catalyst development to reactor design. Chem. Eng. J. 2016 doi: 10.1016/j.cej.2016.06.090. [DOI] [Google Scholar]
- Campos R.K., Jin J., Rafael G.H., Zhao M., Liao L., Simmons G., Chu S., Weaver S.C., Chiu W., Cui Y. Decontamination of SARS-CoV-2 and other RNA viruses from N95 level meltblown polypropylene fabric using heat under different humidities. ACS Nano. 2020;14:14017–14025. doi: 10.1021/acsnano.0c06565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos R.K., Saada N., Rossi S.L., Weaver S.C. Thermally bonded disinfectant for self-decontamination of fabric against SARS-CoV-2. J. Hosp. Infect. 2020;106:835–836. doi: 10.1016/j.jhin.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos R.K., Mirchandani D., Rafael G., Saada N., McMahon R., Weaver S.C. SARS-CoV-2 decontamination of skin with disinfectants active during and after application. J. Hosp. Infect. 2021;111:35–39. doi: 10.1016/j.jhin.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova L.M., Jeon S., Rutala W.A., Weber D.J., Sobsey M.D. Effects of air temperature and relative humidity on coronavirus survival on surfaces. Applied Environ Microbiol. 2010;76:2712–2717. doi: 10.1128/AEM.02291-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia A.B., de Moraes A.P., Rodrigues D.M., Gilioli R., de Oliveira-Filho E.F., Durães-Carvalho R., Arns C.W. Coding-complete genome sequence of murine hepatitis virus strain 3 from Brazil. Microbiol Resour. Announc. 2021;10(15) doi: 10.1128/MRA.00248-21. e00248-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Committee on Taxonomy of Viruses Virus Taxonomy . 2019. Release, EC 51. [accessed on 27 April 2021]; Available online: https://talk.ictvonline.org/taxonomy. [Google Scholar]
- Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J. Hosp. Infect. 2020;104:246–251. doi: 10.1016/j.jhin.2020.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Körner R.W., Majjouti M., Alcazar M.A.M., Mahabir E. Of Mice and Men: The Coronavirus MHV and Mouse Models as a Translational Approach to Understand SARS-CoV-2. Viruses. 2020;12(880) doi: 10.3390/v12080880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarre A., Talbot P.J. Effect of pH and temperature on the infectivity of human coronavirus 229E. Can. J. Microbiol. 1989;35:972–974. doi: 10.1139/m89-160. [DOI] [PubMed] [Google Scholar]
- Lampert P.W., Sims J.K., Kniazeff A.J. Mechanism of demyelination in JHM virus encephalomyelitis. Acta Neuropathol. 1973;24:76–85. doi: 10.1007/BF00691421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy G.A., Liu M., Ding J., Yuwaraj S., Leibowitz J., Marsden P.A., Ning Q., Kovalinka A., Phillips M.J. Molecular and functional analysis of the human prothrombinase gene (HFGL2) and its role in viral hepatitis. Am. J. Pathol. 2000;156:1217–1225. doi: 10.1016/S0002-9440(10)64992-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed L.J., Muench H. A simple method of estimating fifty per cent endpoints. Am. J. Epidemiol. 1938;128:192–197. [Google Scholar]
- Warnes S.L., Little Z.R., Keevil C.W. Human coronavirus 229E remains infectious on common touch surface materials. mBio. 2015;6:e01697–15. doi: 10.1128/mBio.01697-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner L.P. Pathogenesis of demyelination induced by a mouse hepatitis virus (JHM virus) Arch. Neurol. 1973;28:298–303. doi: 10.1001/archneur.1973.00490230034003. [DOI] [PubMed] [Google Scholar]
- World Health Organization. 2021. https://covid19.who.int/.