Abstract
Objective:
In this study we compared noninvasive arterial pressure measurement using ClearSight™ vascular-unloading-technique (Edwards Lifesciences Corp, Irvine, CA) with invasive arterial pressure measurement during induction of anesthesia undergoing mayor cardiac surgery.
Design:
Prospective, monocentric.
Setting:
University hospital.
Participants:
54 patients undergoing mayor cardiac surgery.
Interventions:
During induction all patients were simultaneously monitored with invasive (reference method) and noninvasive arterial pressure measurement (test-method) over a mean time period of 27 minutes.
Measurements and Main Results:
We observed slightly lower systolic and mean arterial pressures noninvasive than invasive. For systolic arterial pressure the mean of the differences was -18,05 mmHg (p < 0,05, SD ±16,78 mmHg), the mean arterial pressure MAP -5,47 mmHg (p < 0,05, SD ±11,08 mmHg) and for diastolic pressure -1,09 mmHg (p < 0,05, SD±11,15 mmHg),. The mean of the differences in heartrate was 1,15 (p < 0,05, SD±6,9 mmHg). When considering all measured values of the invasively measured MAP and the ClearSight ™ -MAP at the same timestamp over the recording interval, an almost identical progress can be seen that indicates a sufficient mapping of the hemodynamic changes. The percentage error for mean arterial, systolic and diastolic pressure measured by ClearSight™ amounts to 25,95 %, 26,77 % and 34,16 %, respectively.
Conclusions:
We conclude that ClearSight ™ is a good option for hemodynamic monitoring during induction of anesthesia. Taking into account the limitations, non-invasive arterial blood pressure measurement offers sufficient security to safely initiate anesthesia, especially when MAP is of particular interest. The use of non-invasive arterial blood pressure measurement with ClearSight ™ during induction of anesthesia in patients scheduled for major cardiac surgery is reliable and easy to use.
Keywords: Cardiac anesthesia, clearSight, hemodynamic monitoring, induction, Nexfin, volume-clamp
INTRODUCTION
The immediate detection of hemodynamic changes in major cardiac surgery patients during the induction of anesthesia is crucial. Noninvasive blood pressure measurement (NIBP) employing an oscillometric cuff does, however, not adequately reflect rapid changes in the arterial blood pressure and is also less reliable compared to an invasive blood pressure measurement.[1,2] For this reason, many clinicians prefer preinduction arterial cannulation to establish continuous arterial blood pressure measurement. Even with the use of local anesthesia, this procedure is, however, often reported by patients to be uncomfortable or even painful. A reliable continuous NIBP system would, therefore, be useful.
The non-invasive arterial blood pressure measurement using the ClearSight™ system (Edwards Lifesciences Corp, Irvine, CA) uses a refined development of the Nexfin-technology, which has been described in detail by Kalmar et al. in 2013.[3] ClearSight™ uses an improved “vascular-unloading” method wherein noninvasive arterial blood pressure can be determined based on a method developed by Penaz and Wesseling.[4,5] Basically, continuous measurement of blood pressure is carried out on a middle phalanx of one finger using the volume clamp method. A photoplethysmograph is integrated into the cuff.[4,6,7] The cuff pressure is kept between systolic and diastolic pressure to keep the blood volume flowing through the finger artery constant as measured by the photoplethysmograph. Arterial blood pressure is measured indirectly via the cuff pressure and an algorithm that calculates a brachial arterial blood pressure curve.[8] This continuous noninvasive measurement of arterial pressure on the finger (FAP = finger arterial pressure) has also been investigated in different situations and with previous models (Finapress®, Nexfin®) in adults and children and is described as practicable and reliable.[9,10,11] However, these examinations usually describe defined time intervals during ongoing operation or also in extracorporeal circulation.[12] To our knowledge, no data are available till date on whether the “vascular- unloading” technique can be used reliably even under conditions of anesthesia induction of cardiac surgery patients, which might present with rapid hemodynamic changes.
We, therefore, conducted this study to investigate the agreement of blood pressure values measured by the ClearSight™ system (FAP) and the current “gold standard” invasive arterial pressure in patients undergoing induction of anesthesia for major cardiac surgery.
METHODS
This prospective observational study was approved by the Ethical Committee of Hannover Medical School (No. 7363-2017) and performed during the period from November 2016 to April 2017. Written informed consent was obtained from all patients. Inclusion criteria were elective major cardiac surgery with extracorporal circulation and patient age 18 years or more. Exclusion criteria were atrial fibrillation and refusal to participate in this study. None of the included patients had Raynaud’s syndrome or peripheral vascular disease (Fontaine stadium >2). Patients were selected randomly according to the current surgical plan.
In all patients, invasive arterial blood pressure measurement was established using cannulating the radial artery by the Seldinger technique. The procedure was performed using local anesthesia (1 mL of lidocain 2%) and in sterile fashion (Arrow®GH-04120, Teleflex® Medical GmbH, Fellbach, Germany). The arterial catheter was connected to a pressure transducer (Codan pvb Critical Care GmbH, Forstinning, Germany), invasive blood pressure values were displayed on a Monitor (S5, GE Datex Ohmeda, Frankfurt, Germany), and automatically exported (1 value per min) to the electronic anesthesia protocol (ANDOKonline®, Datapec Medical Solutions, Pliezhausen, Germany).
For continuous noninvasive FAP measurement, the appropriate finger cuff from the ClearSight™ system was selected according to the manufacturer’s recommendations and placed on the intermediate phalanx of the middle or ring finger of the hand ipsilateral to the arterial catheter. After calibration of the heart reference system, the time of the ClearSight™ EV1000 system monitor (Edwards Lifesciences Corp, Irvine, CA, USA) was synchronized to the time of the electronic anesthesia protocol. Next, ClearSight™ measurement of heart rate, systolic, diastolic, and mean arterial blood pressure were started. The measured values of the FAP were saved (1 value per min) in the clinical platform EV1000 (Edwards Lifesciences Corp, Irvine, CA, USA) and exported to an Excel spreadsheet via USB interface.
Measurement of vital signs of the standard patient monitor (heart rate, systolic, diastolic, and mean arterial blood pressure) was captured automatically every minute in the abovementioned electronic anesthesia protocol.
Obvious artifacts of isolated measurement values, e.g., during arterial blood gas sampling, were excluded after finishing the measurement and before data analysis.
Induction of anesthesia was performed with etomidate, sufentanil, and atracurium. Drug doses were chosen in a weight-adapted manner according to the standard operating procedure by the respective attending anesthesiologist. Norepinephrine or glycerol trinitrate was used to treat unwanted hypertension or hypotension.
Statistical analysis: We compared data pairs of the test method (ClearSight™) with the values of the reference method (invasive arterial blood pressure measurement) for heart rate, systolic, diastolic as well as mean arterial blood pressure (1 value per min for both measurement methods). Linear regression analysis, as well as bias with its standard deviation SD (= accuracy) and the limits of agreement (= precision) according to the Bland-Altman method for repeated measures, were performed.[13,14] The percentage error was calculated as 1,96 SDbias/mean reference method. For a percentage error of less than 30%, the test method (ClearSight™) was evaluated as being interchangeable with the reference method.
RESULTS
A total of 54 patients were included. After data analysis, two patients were excluded. One patient showed extreme deviations of the data measured by FAP from the invasive arterial values so that incorrect operation or incorrect calibration of the device was assumed. FAP error messages predominantly occurred in a second patient, so that the measurement had to be stopped. The demographic data and surgical procedure data are listed in Tables 1 and 2.
Table 1.
Patients characteristics
| Sex, male / female, n (%) | 37 (70) / 15 (30) |
|---|---|
| Age, y | 71 (35-84) |
| Height, cm | 172 (150-187) |
| Body weight, kg | 84,5 (42- 16) |
Data are given as absolute numbers (percentages). Age, height, and body weight as median (min-max)
Table 2.
Surgical procedures
| CABG, n (%) | 26 (50) |
|---|---|
| Valve replace / repair, n (%) | 9 (17) |
| Combined (CABG + valve), n (%) | 10 (19) |
| Others, n (%) | 7 (13) |
Data are given as absolute numbers (percentages). CABG: Coronary Artery Bypass Graft
Men outweighed 70% over women with 30%. About 50% of patients received coronary surgery, 17% heart valve surgery (aortic valve, mitral valve, or tricuspid valve), 19% underwent combined surgery (coronary and valve surgery), and 13% underwent other surgical procedures (e.g., aortic dissection, aortic aneurysm, or RV probe extraction).
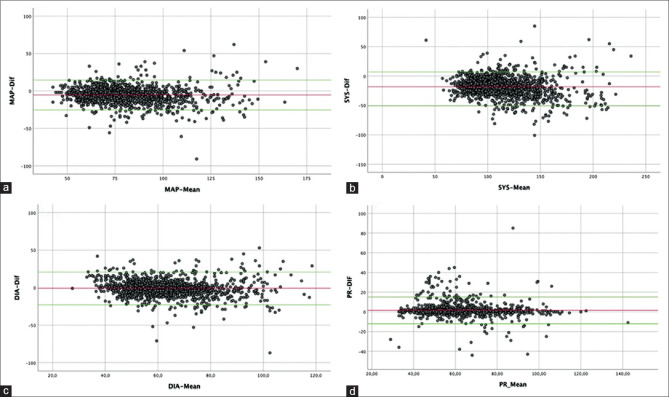
Over a mean measurement period of 27 min, the average deviation of the measured heart rate of the electrocardiography (ECG) compared to the values measured by ClearSight™ is 1.15 beats (P’. The mean average (bias) of the deviations of the measured values, which were recorded using the “;gold standard” compared to the values of the noninvasively measured pressures using FAP, are -18.05 mmHg for the systole (P < 0.05, SD ± 16.78 mmHg), the diastole -1.09 mmHg (P < 0.05, SD ± 11.15 mmHg), the mean arterial blood pressure (MAP) -’g (P < 0ss.05, SD ± 11.08 mmHg). The Bland-Altman analysis shows an acceptable range of the values obtained by the two different measurement methods [Figures 1 and 2]. When considering all measured values of the invasively measured MAP and the ClearSight™ -MAP at the same timestamp over the recording interval, almost identical progress can be seen [Figure 3] that indicates a sufficient mapping of the hemodynamic changes. The percentage error for mean arterial, systolic, and diastolic pressure measured by ClearSight™ amounts to 25,95%, 26,77%, and 34,16%, respectively [Table 3].
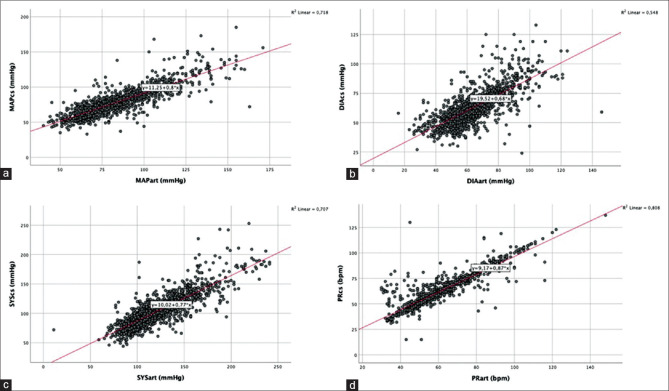
Figure 1.
(a) Scatter plot, correlation of the measured values of the mean arterial blood pressure determined by ClearSight™ (MAPcs), and invasive pressure measurement (MAPart). (b) Scatter plot, correlation of the measured values of the diastolic blood pressure determined by ClearSight ™ (DIAcs), and invasive pressure measurement (DIAart). (c) scatter plot, correlation of the measured values of the systolic blood pressure determined by ClearSight™ (SYScs), and invasive pressure measurement (SYSart). (d) Scatter plot, correlation of the measured values of the heart rate determined by ClearSight™ (PRcs) and invasive pressure measurement (PRart)
Figure 2.
Bland-Altman plot analysis. In each plot, the red horizontal line represents the mean difference of the measurements of invasive arterial measurement and noninvasive measurement using ClearSight ™. The two green horizontal lines represent the Limit of Agreement (1.96 x SD). (a)Bland-Altman plot, MAP-mean (calculated from (MAP invasive + MAP ClearSight)/2) vs. MAP-dif (MAP invasive - MAP ClearSight), (b) Bland-Altman-Plot, SYS-mean (calculated from (SYS invasive + SYS ClearSight)/2) vs. SYS-dif (SYS invasive - SYS ClearSight), (c) Bland-Altman-Plot, DIA-mean (calculated from (DIA invasive + DIA ClearSight)/2) vs. DIA-dif (DIA invasive - DIA ClearSight), (d) Bland-Altman-Plot, PR-mean (calculated from (PR invasive + PR ClearSight)/2) vs. PR-dif (PR invasive - PR ClearSight)
Figure 3.
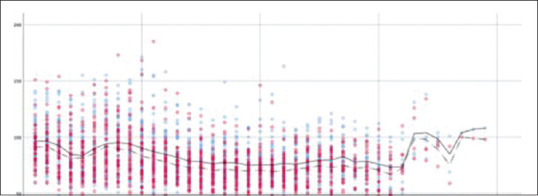
All invasively measured MAP values and all noninvasively measured MAP values over the time of registration. Blue = invasive MAP, red = noninvasive MAP; solid interpolation line: invasive MAP, dashed interpolation line: noninvasive MAP. X-axis: time (t) in minutes, Y-axis: MAP (mmHg). The dynamics are well mapped by ClearSight™, the difference of the MAP of the two measurement methods is visible
Table 3.
Bias, SD, LOA, and percentage error of ClearSight™
| Bias | SD | 95% LOA | % Error | |
|---|---|---|---|---|
| Mean arterial pressure (mmHg) | -5,47 | 11,08 | -27,20 to 16,26 | 25,96% |
| Systolic arterial pressure (mmHg) | -18,05 | 16,78 | -50,94 to 14,84 | 26,77% |
| Diastolic arterial pressure (mmHg) | -1,09 | 11,15 | - 22,94 to 20,76 | 34,16% |
| Heart rate (bpm) | +1,51 | 6,91 | -12,02 to 15,05 | 22,45% |
DISCUSSION
This study sought to investigate the performance of the ClearSight™ system, a noninvasive continuous blood pressure measurement device, during the induction of patients scheduled for major cardiac surgery. ClearSight™ measured significantly lower values compared to the current gold standard, i.e., invasive arterial measurement using arterial cannulation. Since we placed the ClearSight™ system ipsilateral to the arterial catheter, a potential impact on perfusion distal to the catheter cannot be ruled out. However, since blood flow in the palm arches is not always similar on both sides, we deliberately placed the ClearSight cuff on a finger ipsilateral to the arterial catheter. One has to keep in mind though that the potential decrease in perfusion might have caused the systematically lower systolic blood pressure values as measured by the ClearSight™ system. It is also possible that pulse pressure amplification influenced our measured values. Because the artery narrows from brachial to radially, older and ill patients may express a pulse wave that arrives earlier and deliberates due to higher pulse wave velocity. This may lead to an increase in systolic and lower diastolic blood pressure values.[15] The ClearSight™ algorithm calculates the blood pressures in the brachial artery derived from the parameters measured on the finger. Hence, the invasive blood pressure measurement obtained from the radial artery catheter used as the gold standard in our study may not optimally reflect brachial artery pressures as calculated by the ClearSight™ system.
The most important parameter for assessing peripheral perfusion is the MAP. MAP calculated by ClearSight™ was on average only 5.47 mmHg lower than measured invasive arterial MAP during induction of anesthesia. In our view, this is an acceptable difference. Gellert and Bramlage suggested heart valve interventions/surgery as a possible application for the ClearSight™ system for (REF). In this review, the bias of MAP in 16 studies from 2009 to 2018 was from -4,2 (SD 13,7) mmHg to 6,2 (SD 11,7) mmHg.,[16] which is comparable to the difference found in our study. They conclude that the ClearSight™ system can be used to accurately monitor hemodynamics during these interventions. Besides, the performance was similar to the current gold standard, i.e., invasive blood pressure measurement using arterial cannulation. The differences in diastolic blood pressure and heart rate found in our study are in our view not clinically significant.
Rogge et al. recently compared ClearSight ™ with invasive arterial blood pressure measurement in 35 patients during laparoscopic bariatric surgery.[17] The measured values were recorded at a frequency of 1/s but were started after induction of anesthesia when the patient was already transferred from the induction to the operating room. The hemodynamic changes during induction of anesthesia were not recorded in this study. Rogge et al. observed a mean deviation of the MAP of 1.1 mmHg, of the systolic pressure of 6.8 mmHg, and the diastolic pressure of 0.8 mmHg. Our investigation showed slightly higher differences between the two measurement methods. This may be since the measurement values were only registered once per minute in our investigation and thus there is a lower data density, which means that the rapid changes in blood pressure values may not be fully reflected. Rogge et al., in turn, performed an error grid analysis based on five risk levels from no risk to dangerous risk depending on whether or not a difference between the measured arterial pressure value (test method) and the reference arterial pressure value (reference method) would trigger a therapeutic intervention that can harm the patient given its reference arterial pressure value. Nearly 97,7% of the proportions of measurements for MAP are in the no-risk and low-risk zone. That means, that the deviations in measured values lead to no or benign difference in clinical interventions.[17] However, the dynamics of the course of anesthesia induction can be reproduced well with ClearSight™ even with a lower recording frequency as showed in Figure 3.
Most studies till date that have compared the Nexfin method of noninvasive arterial blood pressure measurement to the gold standard of invasive arterial blood pressure measurement have been performed during hemodynamically noncritical phases of anesthesia, during extracorporeal circulation, or in hemodynamically stable patients in the intensive care unit (ICU).[12,18,20,21,22,23] Weiss et al., however, compared the two methods during induction of anesthesia in 31 general surgery patients.[24] Data was also recorded on the ipsilateral hand, but every 5 s. They showed a fast and reliable mapping of blood pressure changes without significant time delay (<1s). The authors also considered the bias and limit of agreement (LOA) for the lowest and highest measured values. Above all, the high LOA at the lowest and highest values for systole (-28.1 mmHg to 25.4 mmHg and -60 mmHg to 39.9 mmHg, respectively) and MAP (-23.2 mmHg to 14.5 mmHg and -49.7 mmHg to 24.6 mmHg, respectively) they concluded that the Nexfin method used at that time was not suitable as a replacement for invasive arterial blood pressure measurement during anesthesia induction. Although Clearsight™ is based on the Nexfin technology used in their study, we did not see this bias in our study collective, probably due to the Clearsight™ algorithm. However, in our opinion, it must be emphasized that there is a lack of accuracy using the volume clamp method in situations with low perfusion and low cardiac output, peripheral vasoconstriction, finger edema, or chronic vascular disease. Thus, potential differences might be secondary to the sampling frequency, i.e., a lower sampling frequency might lead to higher accordance between measurement methods. Further studies are needed to determine optimal sampling frequencies using the noninvasive volume clamp method to determine continuous blood pressure.
It must be mentioned, that the duration of monitoring using noninvasive applications might be limited by blue finger syndrome, which may occur due to venous congestion distal to the probe. The Volume Clamp method should also best be avoided in a patient with Raynaud’s syndrome lest the blue finger syndrome occurs.
There are also other commercially available noninvasive continuous blood pressure monitoring devices. The continuous non-invasive arterial pressure (CNAP) system (Biopac systems, California; CNSystems Medizintechnik AG, Graz, Austria), also based on the volume-clamp-method, allows continuous noninvasive beat-by-beat recording of the arterial pressure waveform. Its algorithm is based on the “;Penaz principle,” which was described by Dr. Saugel in as early as 1973.[25] To eliminate disturbing vasomotoric effects CNAP developed further the “Penaz Principle” by using concentrically interlocking loops and a new algorithm named VERIFI-algorithm (“Vasomotoric Elimination and Reconstructed IdentiFication of the Initial set- point”).[26] CNAP as well as Clearsight ™ shows accurate and reliable NIBP, especially detecting fast changes in arterial pressure as well as intraoperative hypotension.[27,28] To our knowledge no studies yet have compared the two different approaches of noninvasive arterial pressure monitoring with each other and the current gold standard.
Different technology for NIBP measurement is used by T-Line (Tensys Medical Inc., San Diego, CA, USA). It uses the principle of applanation tonometry and a refined algorithm for continuous calibration.[29,30,31] Studies published show acceptable values compared to invasive blood pressure measurements.[32,33,34] Cheng et al. instead point out, that the calibration in applanation tonometry is crucial and that there is substantial room for improvement of measurement accuracy.[35]
Although several studies have shown reliable NIBP monitoring in different clinical settings and by different technologies or algorithms, further studies have to establish the durability and robustness of this equivalence.
CONCLUSION
In summary, we conclude that ClearSight™ is a good option for hemodynamic monitoring during the induction of anesthesia. Given the limitations, noninvasive arterial blood pressure measurement offers sufficient security to safely initiate anesthesia, especially when MAP is of particular interest.
The use of noninvasive arterial blood pressure measurement with ClearSight™ during induction of anesthesia in patients scheduled for major cardiac surgery is reliable and easy to use. For anxious patients or expected difficult puncture conditions in the radial artery, the use of the ClearSight™ finger cuff during the anesthetic induction phase is an equivalent alternative to invasive arterial blood pressure measurement. MAP should be used for blood pressure management decisions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bur A, Herkner H, Vlcek M, Woisetschläger C, Derhaschnig U, Delle Karth G, et al. Factors influencing the accuracy of oscillometric blood pressure measurement in critically ill patients. Crit Care Med. 2003;31:793–9. doi: 10.1097/01.CCM.0000053650.12025.1A. [DOI] [PubMed] [Google Scholar]
- 2.Pace NL, East TD. Simultaneous comparison of intraarterial, oscillometric, and finapres monitoring during anesthesia. Anesth Analg. 1991;73:213–20. doi: 10.1213/00000539-199108000-00017. [DOI] [PubMed] [Google Scholar]
- 3.Kalmar A, Wesseling W, Scheeren T. Technology report: ccNexfin monitor. Nederlands Tijdschrift voor Anesthesiologie. 2013;26:4–8. [Google Scholar]
- 4.Wesseling K. A century of noninvasive arterial pressure measurement: From Marey to Penaz and Finapres. Homeostasis Health Dis. 1995;36:50–66. [Google Scholar]
- 5.Wesseling K, De Wit B, Settels J, Klawer W. On the indirect registration of finger blood pressure after Penaz. Funkt Biol Med. 1982;1:245–50. [Google Scholar]
- 6.Bartels K, Esper SA, Thiele RH. Blood pressure monitoring for the anesthesiologist: A practical review. Anesth Analg. 2016;122:1866–79. doi: 10.1213/ANE.0000000000001340. [DOI] [PubMed] [Google Scholar]
- 7.Kuck K, Baker PD. Perioperative noninvasive blood pressure monitoring. Anesth Analg. 2018;127:408–11. doi: 10.1213/ANE.0000000000002619. [DOI] [PubMed] [Google Scholar]
- 8.Imholz BP, Wieling W, van Montfrans GA, Wesseling KH. Fifteen years experience with finger arterial pressure monitoring: Assessment of the technology. Cardiovasc Res. 1998;38:605–16. doi: 10.1016/s0008-6363(98)00067-4. [DOI] [PubMed] [Google Scholar]
- 9.Kim S-H, Lilot M, Sidhu KS, Rinehart J, Yu Z, Canales C, et al. Accuracy and precision of continuous noninvasive arterial pressure monitoring compared with invasive arterial pressurea systematic review and meta-analysis. J Am Soc Anesthesiologists. 2014;120:1080–97. doi: 10.1097/ALN.0000000000000226. [DOI] [PubMed] [Google Scholar]
- 10.Silke B, McAuley D. Accuracy and precision of blood pressure determination with the Finapres: An overview using re-sampling statistics. J Hum Hypertens. 1998;12:403–9. doi: 10.1038/sj.jhh.1000600. [DOI] [PubMed] [Google Scholar]
- 11.Eeftinck Schattenkerk DW, Van Lieshout JJ, Van Den Meiracker AH, Wesseling KR, Blanc S, et al. Nexfin noninvasive continuous blood pressure validated against Riva-Rocci/Korotkoff. Am J Hypertens. 2009;22:378–83. doi: 10.1038/ajh.2008.368. [DOI] [PubMed] [Google Scholar]
- 12.Martina JR, Westerhof BE, Van Goudoever J, De Jonge N, Van Lieshout JJ, Lahpor JR, et al. Noninvasive blood pressure measurement by the Nexfin monitor during reduced arterial pulsatility: A feasibility study. ASAIO J. 2010;56:221–7. doi: 10.1097/mat.0b013e3181d70227. [DOI] [PubMed] [Google Scholar]
- 13.Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60. doi: 10.1177/096228029900800204. [DOI] [PubMed] [Google Scholar]
- 14.Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–82. doi: 10.1080/10543400701329422. [DOI] [PubMed] [Google Scholar]
- 15.Gizdulich P, Prentza A, Wesseling KH. Models of brachial to finger pulse wave distortion and pressure decrement. Cardiovasc Res. 1997;33:698–705. doi: 10.1016/s0008-6363(97)00003-5. [DOI] [PubMed] [Google Scholar]
- 16.Gellert G, Bramlage P. Use of the ClearSight® system for continuous noninvasive hemodynamic monitoring during heart valve interventions: Review of the literature and single-site experience. Heart Surg Forum. 2018;21:E476–83. doi: 10.1532/hsf.2177. [DOI] [PubMed] [Google Scholar]
- 17.Rogge DE, Nicklas JY, Schön G, Grothe O, Haas SA, Reuter DA, et al. Continuous noninvasive arterial pressure monitoring in obese patients during bariatric surgery: An evaluation of the vascular unloading technique (Clearsight system) Anesth Analg. 2019;128:477–83. doi: 10.1213/ANE.0000000000003943. [DOI] [PubMed] [Google Scholar]
- 18.Broch O, Bein B, Gruenewald M, Carstens A, Illies C, Schöneich F, et al. A comparison of continuous non-invasive arterial pressure with invasive radial and femoral pressure in patients undergoing cardiac surgery. Minerva Anestesiol. 2013;79:248–56. [PubMed] [Google Scholar]
- 19.Fischer MO, Avram R, Cârjaliu I, Massetti M, Gérard JL, Hanouz JL, et al. Non-invasive continuous arterial pressure and cardiac index monitoring with Nexfin after cardiac surgery. Br J Anaesth. 2012;109:514–21. doi: 10.1093/bja/aes215. [DOI] [PubMed] [Google Scholar]
- 20.Martina JR, Westerhof BE, van Goudoever J, de Beaumont EH, Truijen J, Kim Y-S, et al. Noninvasive continuous arterial blood pressure monitoring with Nexfin®. Anesthesiology. 2012;116:1092–103. doi: 10.1097/ALN.0b013e31824f94ed. [DOI] [PubMed] [Google Scholar]
- 21.Hohn A, Defosse J, Becker S, Steffen C, Wappler F, Sakka S. Non-invasive continuous arterial pressure monitoring with Nexfin® does not sufficiently replace invasive measurements in critically ill patients. Br J Anaesth. 2013;111:178–84. doi: 10.1093/bja/aet023. [DOI] [PubMed] [Google Scholar]
- 22.Vos JJ, Poterman M, Mooyaart EA, Weening M, Struys MM, Scheeren TW, et al. Comparison of continuous non-invasive finger arterial pressure monitoring with conventional intermittent automated arm arterial pressure measurement in patients under general anaesthesia. Br J Anaesth. 2014;113:67–74. doi: 10.1093/bja/aeu091. [DOI] [PubMed] [Google Scholar]
- 23.Berkelmans G, Kuipers S, Westerhof B, Spoelstra-de Man A, Smulders Y. Comparing volume-clamp method and intra-arterial blood pressure measurements in patients with atrial fibrillation admitted to the intensive or medium care unit. J Clin Monit Comput. 2018;32:439–46. doi: 10.1007/s10877-017-0044-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weiss E, Gayat E, Dumans-Nizard V, Le Guen M, Fischler M. Use of the Nexfin™ device to detect acute arterial pressure variations during anaesthesia induction. Br J Anaesth. 2014;113:52–60. doi: 10.1093/bja/aeu055. [DOI] [PubMed] [Google Scholar]
- 25.Li M, Yang L, Zhou L, Liu J, Patel S, Liu H. Non-invasive cardiac output measurement: Where are we now? J Anesth Perioperative Med (JAPM) 2018;5:221. [Google Scholar]
- 26.Fortin J, Wellisch A, Maier K. CNAP–evolution of continuous non-invasive arterial blood pressure monitoring. Biomed Tech. 2013;58 doi: 10.1515/bmt-2013-4179. (SI-1-Track-G). doi: 10.1515/bmt-2013-4179. [DOI] [PubMed] [Google Scholar]
- 27.Jeleazcov C, Krajinovic L, Münster T, Birkholz T, Fried R, Schüttler J, et al. Precision and accuracy of a new device (CNAP™) for continuous non-invasive arterial pressure monitoring: Assessment during general anaesthesia. Br J Anaesth. 2010;105:264–72. doi: 10.1093/bja/aeq143. [DOI] [PubMed] [Google Scholar]
- 28.Siebig S, Rockmann F, Sabel K, Zuber-Jerger I, Dierkes C, Brünnler T, et al. Continuous non-invasive arterial pressure technique improves patient monitoring during interventional endoscopy. Int J Med Sci. 2009;6:37–42. doi: 10.7150/ijms.6.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pressman G, Newgard P. A transducer for the continuous external measurement of a rterial blood pressure. IEEE Trans Bio-med Electronics. 1963;10:73–81. doi: 10.1109/tbmel.1963.4322794. [DOI] [PubMed] [Google Scholar]
- 30.Saugel B, Meidert AS, Langwieser N, Wagner JY, Fassio F, Hapfelmeier A, et al. An autocalibrating algorithm for non-invasive cardiac output determination based on the analysis of an arterial pressure waveform recorded with radial artery applanation tonometry: A proof of concept pilot analysis. J Clin Monit Comput. 2014;28:357–62. doi: 10.1007/s10877-013-9540-8. [DOI] [PubMed] [Google Scholar]
- 31.Stein PD, Blick EF. Arterial tonometry for the atraumatic measurement of arterial blood pressure. J Appl Physiol. 1971;30:593–6. doi: 10.1152/jappl.1971.30.4.593. [DOI] [PubMed] [Google Scholar]
- 32.Dueck R, Goedje O, Clopton P. Noninvasive continuous beat-to-beat radial artery pressure via TL-200 applanation tonometry. J Clin Monit Comput. 2012;26:75–83. doi: 10.1007/s10877-012-9336-2. [DOI] [PubMed] [Google Scholar]
- 33.Janelle GM, Gravenstein N. An accuracy evaluation of the T-Line® Tensymeter (continuous noninvasive blood pressure management device) versus conventional invasive radial artery monitoring in surgical patients. Anesth Analg. 2006;102:484–90. doi: 10.1213/01.ane.0000194873.52453.bd. [DOI] [PubMed] [Google Scholar]
- 34.Meidert A, Huber W, Müller J, Schöfthaler M, Hapfelmeier A, Langwieser N, et al. Radial artery applanation tonometry for continuous non-invasive arterial pressure monitoring in intensive care unit patients: Comparison with invasively assessed radial arterial pressure. Br J Anaesth. 2014;112:521–8. doi: 10.1093/bja/aet400. [DOI] [PubMed] [Google Scholar]
- 35.Cheng H-M, Lang D, Tufanaru C, Pearson A. Measurement accuracy of non-Invasively obtained central blood pressure by applanation tonometry: A systematic review and meta-analysis. Int J Cardiol. 2013;167:1867–76. doi: 10.1016/j.ijcard.2012.04.155. [DOI] [PubMed] [Google Scholar]