Abstract
Context:
The prevalence of symptomatic lumbar disc herniation (LDH) in athletes can be as high as 75%. For elite athletes diagnosed with LDH, return to play (RTP) is a major concern, and thus comparing surgical with nonoperative care is essential to guide practitioners and athletes, not just in terms of recovery rates but also speed of recovery.
Objective:
The purpose of this systematic review is to provide an update on RTP outcomes for elite athletes after lumbar discectomy versus nonoperative treatment of LDHs.
Data Sources:
A search of the literature was conducted using 3 online databases (MEDLINE, EMBASE, and PubMed) to identify pertinent studies.
Study Selection:
Yielded studies were screened according to the inclusion criteria.
Study Design:
Systematic review with meta-analysis.
Level of Evidence:
Level 4.
Data Extraction:
Relevant data were extracted. A meta-analysis was performed comparing RTP rate for all comparative studies.
Results:
Twenty studies met the inclusion criteria and were included in this review. Overall, 663 out of 799 patients (83.0%) returned to play in the surgical group and 251 out of 308 patients (81.5%) returned to play in the nonoperative group. No statistically significant difference for RTP rate was found (odds ratio, 1.39; 95% CI, 0.58-3.34; P = 0.46; I2, 71%). The mean time to RTP for patients undergoing lumbar discectomy was 5.19 months (range 1.00-8.70 months), and 4.11 months (range 3.60-5.70 months) for those treated conservatively.
Conclusion:
There was no significant difference in RTP rate between athletes treated with operative or nonoperative management of LDHs, nor did operative management have a faster time to RTP. Athletes should consider the lack of difference in RTP rate in addition to the potential risks associated with spinal surgery when choosing a treatment option. Future randomized controlled trials are needed on this topic to allow for high-powered conclusions.
Keywords: athlete, return to play, discectomy, nonoperative treatment
Imaging findings of lumbar disc herniations (LDHs) and spinal degeneration are widely prevalent in both asymptomatic and symptomatic populations.4 When symptomatic, LDH can cause significant pain and functional impairment, negatively affecting quality of life.8 While both surgical and nonsurgical treatments are available, most cases of LDH can be treated successfully with nonoperative treatment.3 It is suggested that surgical intervention may provide improved short-term outcomes such as more rapid resolution of symptoms and decreased recovery period.3,23 Generally, treatment consists of 6 to 8 weeks of nonoperative treatment prior to considering surgical intervention, assuming no significant or progressive neurological deficits.3 One study suggested that it was unnecessary to obtain imaging results for the first 4 to 6 weeks since almost 70% of patients will improve over this time period with nonoperative care.5 In the general population, multiple randomized controlled trials evaluated the efficacy of lumbar discectomy with nonoperative treatment.29,45 The Spine Patient Outcomes Research Trial by Weinstein et al45 is a randomized controlled trial that reported minimal differences between open discectomy and nonsurgical care over a 2-year follow-up period. Similar results were found by Österman et al29; specifically, that there were no significant differences between microdiscectomy and nonsurgical treatment in terms of quality of life after both interventions.
LDH in elite athletes creates a very different clinical picture from the average population, as such individuals constantly put their bodies through severe strain and push themselves to the edges of their physical capacity. The prevalence of symptomatic disc degeneration in elite athletes is significantly higher than in nonathletes (75% vs 31%).28,40 While both operative and conservative treatment options appear reasonable, operative treatment is often the treatment of choice based on the severity of the injury leading to LDH, with the theoretical aim of maximizing the potential and speed of return to sports. Historically, open discectomy was the primary surgery of choice for LDH; however, with advancement of technology and surgical techniques, microscopic lumbar discectomy (MLD) is currently the gold standard.6 Further developments, such as microendoscopic discectomy (MED) and percutaneous endoscopic discectomy (PED), are becoming increasingly utilized.19 With MLD, a microscope and sequential tubular dilation allow for visualization through smaller incisions, whereas MED and PED require an endoscope.6,19 Nonoperative treatment involves the use of physical therapy and anti-inflammatory medications.19 While surgery is proposed to increase rate of return to play (RTP) and reduced time to RTP, it is increasingly suggested that nonoperative treatment may result in similar outcomes.31
Two previous systematic reviews evaluating microdiscectomy in athletes found similar outcomes of RTP for surgical in comparison with nonoperative care.30,31 Since these reviews, however, at least 6 additional studies have been published and previous reviews also failed to explore outcomes by surgery type.30,31 The purpose of this systematic review is to provide an updated comprehensive analysis regarding RTP findings for elite athletes after nonoperative and surgical treatment of LDH, with type of surgery taken into account. Findings will improve the decisions care providers make when managing this clinical scenario.
Methods
This systematic review was performed according to the guidelines outlined in the Cochrane Handbook and reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.25
Search Strategy and Eligibility
Three online databases were searched (PubMed, EMBASE, and MEDLINE) for articles related to RTP after lumbar discectomy in athletes. Search terms used to conduct this search include return to play, elite, athlete, lumbar, discectomy, and similar words (Appendix 1, available in the online version of this article). The search terms were also entered onto Google Scholar to conduct a manual search of the literature in addition to the search strategy used to yield related articles. The inclusion and exclusion criteria of this study were established a priori. The following were the inclusion criteria: (1) all levels of evidence, (2) symptomatic LDH, (3) male and female adult elite athletes, (4) RTP status reported, and (5) articles published in English. The following were the exclusion criteria: (1) pediatric patients, (2) recreational or nonprofessional athletes, (3) surgeries other than lumbar discectomies, and (4) review papers or incomplete publications such as surveys or conference proceedings.
Study Screening
Two independent blinded reviewers screened the studies from title to abstract to full text, at each stage calculating consensus and checking interrater reliability. For discrepancies at the title and abstract stages, the studies were automatically included. Any discrepancies after the full-text screening were resolved with the input from a blinded third party.
Data Extraction
Pertinent data were abstracted from the included studies by 2 blinded reviewers and recorded on a Google Spreadsheet designated a priori. Extracted data included demographics (type of study, number of patients, mean age, sex, and sports played), operation characteristics (type of procedure and operation level), RTP findings (RTP rate, time to RTP, RTP period, and RTP performance), and complications. For RTP findings, RTP rate is defined as the percentage of athletes who returned to play out of the study participants; time to RTP is defined as the time it took the players from the time of surgery or nonoperative treatment to the return to training and play; RTP period is defined as the duration of participation of the athletes in their respective sports after the surgery or nonoperative treatment; and RTP performance includes any performance parameters that the studies report, such as number of games started, player efficiency ratings, and other sports-specific performance measures to assess level of play after RTP. When the study reported the RTP period in seasons instead of years or months, a season was assumed to be 8 months for calculation of pooled results. This assumption was needed for 2 of the included studies where the sports involved were basketball and hockey in their American national leagues. The average length of the season for these 2 leagues, depending on the extent of advancement in the postseason, is around 240 days. The findings by category are reported in Appendix 2 (available online).
Study Quality Assessment
The Methodological Index for Non-Randomized Studies (MINORS) appraisal tool was used to assess the quality of the included studies.38 Scores of 0, 1, or 2 were given to each of the 12 categories on the MINORS checklist, where 0 means that the category was not included, 1 means that the category was partially covered, and 2 means that the category was fully included. A maximum score of 16 is possible for noncomparative studies and a maximum score of 24 for comparative studies. This is because 4 of the categories in the MINORS checklist only apply to comparative studies. The quality of the included studies was determined a priori based on the mean MINORS scores between the 2 reviewers as follows: a mean score of 0 to 6 indicates very low quality of evidence, 7 to 10 indicates low quality of evidence, 11 to 15 indicates fair quality of evidence, and a mean score >15 indicates good quality of evidence for nonrandomized studies.
Statistical Analysis
Descriptive statistics such as percentages, means, and measures of variance (standard deviations and 95% CIs) are presented where applicable. For interrater reliability, a kappa (κ) statistic was calculated using the percentage agreement between the 2 reviewers across all stages of screening. As for the reliability in the assessment of study quality, an intraclass correlation coefficient (ICC) was calculated for the MINORS scores of all studies. The cutoff values for agreement were determined a priori as follows: κ/ICC of 0.81 to 0.99 was considered excellent agreement; κ/ICC of 0.61 to 0.80 considered substantial agreement; κ/ICC of 0.41 to 0.60 considered moderate agreement; κ/ICC of 0.21 to 0.40 considered fair agreement, and a κ/ICC value of 0.20 or less was considered slight agreement.18 The Statistical Package for the Social Sciences (SPSS Version 23.0; IBM Corp, 2015) was used to perform these analyses.
A meta-analysis was performed for RTP rate. To perform the meta-analysis, the event rate, defined as the number of athletes who returned to play was recorded and used to compare between the surgical and nonsurgical groups. The Mantel-Haenszel test was used to generate the odds ratio (OR) and 95% CI. Heterogeneity was assessed using Cochrane Q and the I2 statistic, where high heterogeneity is indicated by a Q P value less than 0.10 and an I2 statistic greater than 50%. Cochrane RevMan Version 5.3 was used to conduct the meta-analysis.
Subgroup Analysis
The RTP findings were additionally stratified by surgery type, and the following strata were included: PED, MED, MLD, and lumbar discectomy for the surgical groups while the nonoperative group remained the same.
Results
Study Eligibility
The search strategy yielded 4157 studies from the 3 databases, in addition to 52 studies that were identified through a manual search of the literature. After duplicate removal and application of inclusion and exclusion criteria, 80 studies underwent abstract screening. After abstract screening and full-text review, 20 studies were determined to be eligible for qualitative synthesis (Figure 1). Interrater reliability for assessment of study eligibility demonstrated excellent agreement throughout all stages of screening; at the title (κ = 0.987; 95% CI, 0.983-0.991), abstract (κ = 0.850; 95% CI, 0.738-0.962), and full-text (κ = 0.950; 95% CI, 0.797-1.103) screening stages.
Figure 1.
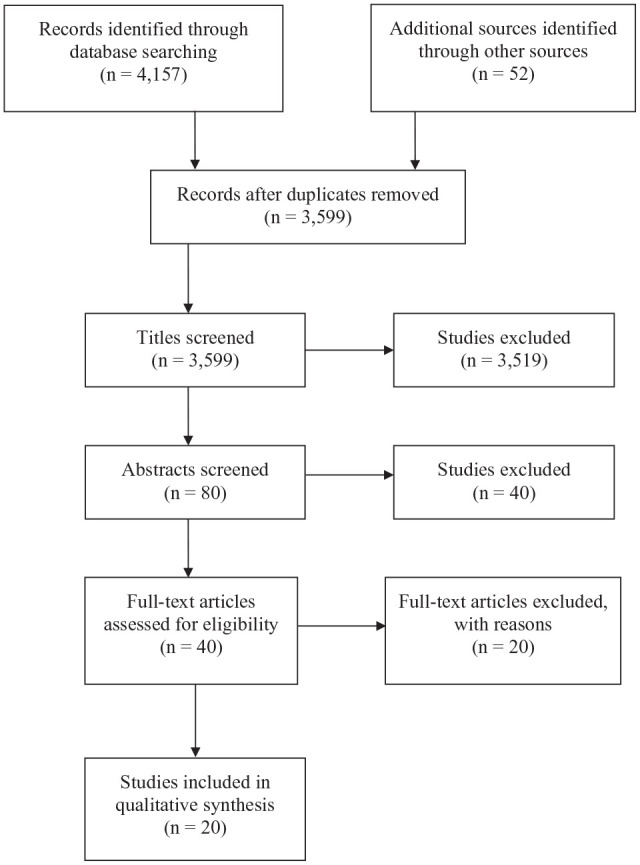
Flowchart of screening.
Study Quality Assessment
All included studies were nonrandomized level IIIB and level IV evidence (n = 20) (Appendix 3, available online). The mean MINORS score was 12.4 ± 4.0, which corresponds to fair quality of evidence. Nine of the studies were retrospective cohort studies, 2 case reports, 7 retrospective comparative studies, 1 case series, and 1 retrospective case-control study. Where lumbar discectomy was the procedure, the standard comparator was the nonsurgical group. Most included noncomparative studies had a clearly stated aim, inclusion of consecutive patients, and appropriate follow-up, but lacked an unbiased assessment of the study endpoint. Most comparative studies had an adequate control group that was contemporary and equivalent but lacked adequate statistical analyses. There was excellent interrater reliability between the reviewers for study quality (ICC, 0.89).
Study and Patient Characteristics
The included studies were conducted from 1993 to 2019 (Appendix 3, available online). There were 1181 patients across all the studies where the average age of included patients, excluding the study for which no mean age was provided,24 was 28.3 years (range: 14-49). Of the included studies, 1160 patients were men (98.2%) and 21 patients were women (1.8%). The final number of patients included in the analysis was 1107, after the exclusion of patients who did not satisfy the inclusion criteria from select studies. The most frequently played sports reported in these studies were American football, basketball, baseball, and hockey, with other played sports including soccer, volleyball, bicycle riding, rugby, tennis, and others.
Type of Procedure and Level of Operation
In total, 55 patients underwent PED, 25 patients underwent MED, 208 patients underwent MLD, and 511 patients participated in studies where the procedure was generally labeled as lumbar discectomy with no specification of technique. There were also 308 patients who were included in the nonoperative group, who were treated with physical therapy and nonsteroidal anti-inflammatory medication, if tolerated. The most common spinal levels requiring operation were the L4/L5 and L5/S1 discs, while 8 patients were reported to have the procedure done at level L3/L4 (Table 1).
Table 1.
Procedure and level of operation
| Author(s) | No. of Patients | Procedure | Level of Operation |
|---|---|---|---|
| Nakamae et al26 | 21 | PED | L4/5 in all patients |
| Sugimine et al39 | 2 | (1) MED (2) TELD followed by MED |
(1) MED at L3/4 (2) TELD at L4/5; MED at L5/S1 |
| Manabe et al20 | 12 | PED using thermal annuplasty | L4/5 (n = 11) L5/S1 (n = 6) |
| Minhas et al24 | 61 | (1) 34 LD (2) 27 nonoperative |
Not given |
| Abe et al1 | 1 | Foraminoplastic transforaminal PED | L5/S1 |
| Yoshimoto et al50 | 25 | MED | L3/L4 (n = 1) L4/L5 (n = 11) L5/S1 (n = 13) |
| Sairyo et al34 | 4 | PED using thermal annuplasty | L4/5 |
| Shroeder et al37 | 87 | (1) 56 surgical (a) 48 LD (b) 8 lumbar fusion (2) 31 nonoperative |
Not given |
| Earhart et al12 | 69 | (1) 40 MLD and/or laminotomy/foraminotomy (2) 29 nonoperative |
Not given |
| Watkins et al43 | 171 | (1) 85 treated with MLD, 10 excluded for retiring = 75 (2) 86 nonoperative |
1) L3/4 (n = 6) L4/5 (n = 32) L5/S1 (n = 37) |
| Weistroffer and Hsu46 | 66 | (1) 52 open or tubular LD (2) 14 nonoperative |
Not given (all 1-level LDH except one 2-level LDH) |
| Hsu et al15 | 342 | (1) 226 LD (2) 116 nonoperative |
Not given |
| Roberts et al33 | 29 | (1) 20 MLD (2) 9 nonoperative |
Not given |
| Hsu14 | 130 | (1) 96 LD (2) 34 nonoperative |
Not given |
| Savage and Hsu36 | 23 | 23 LD | Not given |
| Anakwenze et al2 | 24 | (1) 24 LD (2) 48 nonoperative |
Not given |
| Watkins et al44 | 59 | 59 MLD | Not given |
| Wang et al42 | 14 | (1) 10 single-level MLD (2) 3 two-level MLD (3) 1 single-level PED |
Not given |
| Sakou et al35 | 13 | 13 PED | L4/5 (n = 9) L5/S1 (n = 3) Both L4/5 + L5/S1 (n = 1) |
| Matsunaga et al22 | 28 | (1) 11 simple disc excision (2) 2-disc excision with spinal fusion (3) 15 PED |
Not given |
LD, lumbar discectomy; LDH, lumbar disc herniation; MED, microendoscopic discectomy; MLD, microendoscopic discectomy; PED, percutaneous endoscopic discectomy; TELD, transforaminal full endoscopic lumbar discectomy.
RTP Findings
There were 799 patients in the surgical group and 308 patients in the nonoperative group. A total of 663 patients returned to play successfully (83.0%) in the operative group versus 251 patients who returned to play in the nonoperative group (81.5%). The mean time to RTP for patients who underwent lumbar discectomy was 5.19 months (range, 1.00-8.70 months), while the mean time to RTP for the group treated nonoperatively was 4.11 months (range, 3.60-5.70 months). The average RTP period was 35.71 months (range, 6.00-57.70 months) and 38.23 months (range, 9.60-73.20 months) for the surgical and nonoperative groups, respectively.
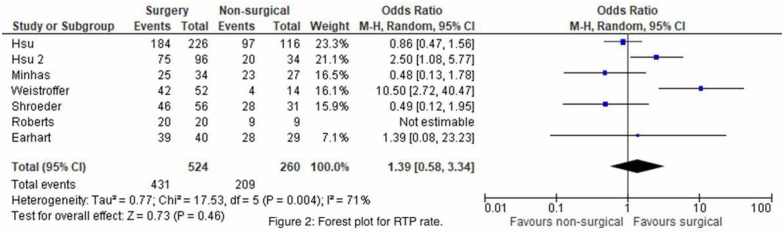
Pooled outcomes from the 7 retrospective comparative studies were evaluated.12,14,15,24,33,37,46 There was no statistically significant difference with respect to RTP rate between operative and nonoperative management of LDHs. The Mantel-Haenszel OR of RTP rate was 1.39 (95% CI, 0.58-3.34; P = 0.46), slightly in favor of surgical treatment but not statistically significant and with high heterogeneity (I2, 71%) (Figure 2). A significance test was not performed for time to RTP as there were only 2 comparative studies that reported this parameter.
Figure 2.
Forest plot for return-to-play (RTP) rate. M-H, Mantel-Haenszel.
Subgroup Analysis: RTP by Surgical Procedure
For the 55 patients who underwent PED, 47 patients (85.5%) returned to play. Only 2 studies labeled their surgical procedure as MED,39,50 where 21 of 25 patients (84.0%) returned to play. In addition, there were 208 patients who underwent MLD, of whom 188 (90.4%) successfully returned to play. For procedures labeled generically as lumbar discectomy, 407 of 511 patients (79.6%) successfully returned to play. In studies where the nonsurgical comparator group was present, 251 out of 308 patients (81.5%) returned to play (Appendix 4, available online).
Of the studies that reported time to RTP for patients undergoing PED, the average time to RTP was 2.06 months (range, 1.00-6.53 months). The mean time to RTP for patients undergoing MED was 2.52 months (range, 1.17-3.73 months), while for MLD patients it was 6.50 months (range, 1.00-15.00 months). None of the studies reporting on general lumbar discectomy included the time to RTP in their results, while the average time to RTP for the 2 studies with a nonoperative group that reported it was 4.11 months (range, 3.60-5.70 months).12,33
In terms of RTP period, the studies reporting on patients who underwent PED had an average of 31.75 months (range, 6.00-40.20 months). For patients who underwent MED, the mean RTP period was 22.91 months (range, 12.00-64.00 months) and for MLD it was 35.22 months (range, 12.00-57.70 months). For the studies in which the operation was labeled generically as lumbar discectomy, the average RTP period was 36.68 months (range, 21.60-49.20 months). Finally, the studies reporting on the RTP period for the nonsurgical group had an average of 38.23 months (range, 9.60-73.20 months).
Indicators of performance vary greatly across the different sports assessed in the studies, and so the appropriate parameters for each sport are presented in Appendix 4 (available online) where reported.
Discussion
Although LDH can be a painful and disheartening injury for an elite athlete, the RTP rates after operative and nonoperative management are high with no significant difference between both treatment options (OR, 1.39; 95% CI, 0.58-3.34; P = 0.46) (Figure 2). RTP after lumbar discectomy in elite athletes ranges from 79.6% to 90.4%. Despite the success of operative intervention (83.0%), nonoperative care is equally effective with regard to RTP rate (81.5%). Nonoperative treatment included education/counseling, nonsteroidal anti-inflammatory drugs if tolerated, and physical therapy, which entails functional rehabilitation, activity modification, and pain management. RTP period was also quite similar between the 2 groups. These are promising findings in support of nonsurgical treatment for athletes with LDH. Spine surgery encompasses inherent risks, including wound complications, infections, potential paralysis, or rarely even blindness from ocular pressure in the prone position.3 Therefore, if these risks can be avoided with nonoperative management while achieving similar RTP outcomes, then this should be a strong consideration for athletes deciding on their treatment plan. However, a crucial question to consider is what determines whether an athlete gets surgically treated. The severity of the injury, failure of conservative treatment, associated neurologic deficits, past surgical history of the athlete, and risks of surgery need to be considered side by side with these results to determine the appropriate treatment option.3 Since conservative management is typically the first line of care with LDHs, further exploration of pretreatment factors, such as clinical parameters and patient choice, is warranted to better determine when to recommend surgery versus continued nonsurgical treatment.
This review identified elite athletes to be treated 2.5 times more often surgically than nonoperatively. A possible explanation could be the differing pretreatment profiles between both treatment groups. Watkins et al43 analyzed the pretreatment clinical and radiological findings between the 2 groups and found that surgically treated athletes present with significantly more radicular pathologic changes. Specifically, 41% of athletes treated with a discectomy presented with radiculopathy versus 23% of nonoperative patients. More of surgically treated athletes also tested positive on the straight leg raise (56% vs 34%), crossed straight leg raise (18% vs 5%), and cram tests (35% vs 17%). Another explanation for this tendency to suggest surgical intervention is the fact that in the general population, there are high satisfaction and return-to-work rates for patients (92% and 82%, respectively).29 This might contribute to the perception that discectomies might lead to a higher proportion of RTP and faster recovery for athletes as well. Given the results of this review, however, nonoperative treatment produces similar outcomes in terms of RTP rate and time to RTP when compared with surgical intervention. This finding could be of use to practitioners as they recommend treatment for athletes, while considering pretreatment profiles and implications for RTP in the context of the quality of the presented evidence.
Evaluating RTP findings by surgical procedure, the only trend observed was one toward increased time to RTP after MLD, in comparison with PED, MED, and nonoperative care. RTP period was noticeably reduced for the 2 studies reporting on MED, at an average of 22.91 months, in comparison with the other surgeries and nonoperative group, which ranged from 31.75 to 38.23 months. A potential explanation for this is that the 2 studies using MED had incomplete follow-up.39,50
This review explores and compares various surgical techniques for the operative management of LDHs. Conventional open discectomy, originally described by Mixter and Barr in 1934, is able to alleviate clinical symptoms and assist in improving overall neurological function.17 Yasargil and Caspar developed MLD in 1977 as an alternative approach toward treating LDH,7,47 and about 20 years later in 1997, Foley and Smith13 published their article on using MED. The distinguishing feature between the 2 procedures is that MLD uses an operating microscope as the tool for visualization, whereas MED uses a tubular retractor system and a microendoscope for visualization.32 Both these procedures were developed and enhanced over the years,9,16,21,27 but MLD remained the gold standard for patients with symptomatic LDH causing radiculopathy. In 2002, Yeung and Tsou49 presented a detailed technical description of PED in 307 consecutive patients. This technique is fully endoscopic, but unlike MED, does not require the tubular retractor for visualization.48,49 It has also seen many improvements over the years before being utilized in a more widespread fashion.10,11,41 For instance, Dezawa et al10 described a hidden zone using the PED system that occurs when the herniated nucleus pulposus migrates in operation, and thus they developed a translaminar approach to address this issue.10 With these different types and developments in mind, the most commonly reported procedure for elite athletes experiencing LDH remains MLD. While MED and PED may show more promising results in the future, the sample sizes remain quite small and these procedures need to be tested against nonoperative treatment to enhance the evidence available in comparative studies.
Seven out of the 20 studies (35.0%) reported complications that occurred in their patients, all of them related to the surgical intervention. The most common complication was the recurrence of LDH at the same level of operation. This was either treated conservatively or by doing a revision discectomy. For example, the study by Weistroffer and Hsu46 on National Football League linemen reported 7 athletes who presented with a recurrent LDH and were treated with a revision discectomy. Six of those 7 linemen (85.7%) successfully returned to play after the revision surgery. The patients who did not RTP had varying reasons; some deciding to retire prematurely after their injury, some retiring for nonmedical reasons, some retiring for sustaining other injuries in addition to the lumbar herniation, and some unable to RTP, as they experienced residual pain after treatment.
The major limitation of this systematic review is that most of the included studies were of level IIIB or IV evidence and none of the studies were randomized controlled trials. This should be taken into consideration when evaluating the strength of the conclusions. Another limitation is the heterogeneity in the reporting of results between studies, which limited the number of outcomes that could be pooled. It is difficult to standardize reporting for RTP performance across different sports, given they are different in their very nature and performance entails different attributes depending on the sport. Finally, this study is limited by the fact that only 1.8% of the study population were women, as most studies were conducted on male athletes. This may warrant further investigation on female athletes to generate a more representative outlook on the management of LDH for athletes. In general, however, this study provided an important update, using the recently published evidence, on RTP outcomes for elite athletes after treatment for LDH.
Conclusion
There is no significant difference in RTP rate between elite athletes treated with operative or nonoperative management of LDHs, nor did operative management have a faster time to RTP. Despite this, LDHs in the athletic population are treated surgically with a discectomy 2.5 times more often than nonoperatively. Both treatments have high RTP rates and comparable results for time to RTP and RTP period. Given the potential risks associated with spinal surgery, athletes and providers should consider the lack of difference in RTP rate when choosing a treatment option. Future randomized controlled trials are needed on this topic to allow for high-powered conclusions.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-4-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Footnotes
The following author declared potential conflicts of interest: M.K. is a paid Associate Editor for Sports Health.
References
- 1.Abe M, Takata Y, Higashino K, et al. Foraminoplastic transforaminal percutaneous endoscopic discectomy at the lumbosacral junction under local anesthesia in an elite rugby player. J Med Invest. 2015;62:238-241. [DOI] [PubMed] [Google Scholar]
- 2.Anakwenze OA, Namdari S, Auerbach JD, et al. Athletic performance outcomes following lumbar discectomy in professional basketball players. Spine (Phila Pa 1976). 2010;35:825-828. [DOI] [PubMed] [Google Scholar]
- 3.Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:183-197. [DOI] [PubMed] [Google Scholar]
- 4.Brinjikji W, Diehn FE, Jarvik JG, et al. MRI findings of disc degeneration are more prevalent in adults with low back pain than in asymptomatic controls: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2015;36:2394-2399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine (Phila Pa 1976). 1992;17:1205-1212. [DOI] [PubMed] [Google Scholar]
- 6.Calikoglu C, Cakir M. Open discectomy vs. microdiscectomy: results from 519 patients operated for lumbar disc herniation. Eurasian J Med. 2018;50:178-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caspar W. A new surgical procedure for lumbar disc herniation causing less tissue damage through a microsurgical approach. In: Wüllenweber R, Kasner M, Hamer J, Klinger M, Spoerri O, eds. Lumbar Disc Adult Hydrocephalus. Springer; 1977:74-80. [Google Scholar]
- 8.Cong L, Zhu Y, Tu G. A meta-analysis of endoscopic discectomy versus open discectomy for symptomatic lumbar disk herniation. Eur Spine J. 2016;25:134-143. [DOI] [PubMed] [Google Scholar]
- 9.Destandau J. Technical features of endoscopic surgery for lumbar disc herniation: 191 patients [in French]. Neurochirurgie. 2004;50:6-10. [DOI] [PubMed] [Google Scholar]
- 10.Dezawa A, Mikami H, Sairyo K. Percutaneous endoscopic translaminar approach for herniated nucleus pulposus in the hidden zone of the lumbar spine. Asian J Endosc Surg. 2012;5:200-203. [DOI] [PubMed] [Google Scholar]
- 11.Dezawa A, Sairyo K. New minimally invasive discectomy technique through the interlaminar space using a percutaneous endoscope. Asian J Endosc Surg. 2011;4:94-98. [DOI] [PubMed] [Google Scholar]
- 12.Earhart JS, Roberts D, Roc G, Gryzlo S, Hsu W. Effects of lumbar disk herniation on the careers of professional baseball players. Orthopedics. 2012;35:43-49. [DOI] [PubMed] [Google Scholar]
- 13.Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997;3:301-307. [Google Scholar]
- 14.Hsu WK. Performance-based outcomes following lumbar discectomy in professional athletes in the National Football League. Spine. 2010;35:1247-1251. [DOI] [PubMed] [Google Scholar]
- 15.Hsu WK, McCarthy KJ, Savage JW, et al. The Professional Athlete Spine Initiative: outcomes after lumbar disc herniation in 342 elite professional athletes. Spine J. 2011;11:180-186. [DOI] [PubMed] [Google Scholar]
- 16.Kambin P, O’Brien E, Zhou L, Schaffer JL. Arthroscopic microdiscectomy and selective fragmentectomy. Clin Orthop Relat Res. 1998;347:150-167. [PubMed] [Google Scholar]
- 17.Kanno H, Aizawa T, Hahimoto K, Itoi E. Minimally invasive discectomy for lumbar disc herniation: current concepts, surgical techniques, and outcomes.Int J Orthop. 43;4:917-922. [DOI] [PubMed] [Google Scholar]
- 18.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159-174. [PubMed] [Google Scholar]
- 19.Mahesha K. Percutaneous endoscopic lumbar discectomy: results of first 100 cases. Indian J Orthop. 2015;51:36-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Manabe H, Yamashita K, Tezuka F, et al. Thermal annuloplasty using percutaneous endoscopic discectomy for elite athletes with discogenic low back pain. Neurol Med Chir (Tokyo). 2019;59:48-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matsumoto M, Watanabe K, Tuji T, et al. Microendoscopic discectomy for lumbar disc herniation with bony fragment due to apophyseal separation. Minim Invasive Neurosurg. 2007;50:335-339. [DOI] [PubMed] [Google Scholar]
- 22.Matsunaga S, Sakou T, Taketomi E, Ijiri K. Comparison of operative results of lumbar disc herniation in manual laborers and athletes. Spine. 1993;18:2222-2226. [DOI] [PubMed] [Google Scholar]
- 23.McCulloch JA. Focus issue on lumbar disc herniation: macro-and microdiscectomy. Spine. 1996;21(24)(suppl):45S-56S. [DOI] [PubMed] [Google Scholar]
- 24.Minhas SV, Kester BS, Hsu WK. Outcomes after lumbar disc herniation in the National Basketball Association. Sports Health. 2016;8:43-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moher D, Altman DG, Liberati A, Tetzlaff J. PRISMA statement. Epidemiology. 2011;22:128. [DOI] [PubMed] [Google Scholar]
- 26.Nakamae T, Fujimoto Y, Yamada K, et al. Transforaminal percutaneous endoscopic discectomy for lumbar disc herniation in athletes under the local anesthesia. J Orthop Sci. 2019;24:1015-1019. [DOI] [PubMed] [Google Scholar]
- 27.Nowitzke AM. Assessment of the learning curve for lumbar microendoscopic discectomy. Neurosurgery. 2005;56:755-762. [DOI] [PubMed] [Google Scholar]
- 28.Ong A, Anderson J, Roche J. A pilot study of the prevalence of lumbar disc degeneration in elite athletes with lower back pain at the Sydney 2000 Olympic Games. Br J Sports Med. 2003;37:263-266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Österman H, Seitsalo S, Karppinen J, Malmivaara A. Effectiveness of microdiscectomy for lumbar disc herniation: a randomized controlled trial with 2 years of follow-up. Spine. 2006;31:2409-2414. [DOI] [PubMed] [Google Scholar]
- 30.Overley SC, McAnany SJ, Andelman S, et al. Return to play in elite athletes after lumbar microdiscectomy: a meta-analysis. Spine. 2016;41:713-718. [DOI] [PubMed] [Google Scholar]
- 31.Reiman MP, Sylvain J, Loudon JK, Goode A. Return to sport after open and microdiscectomy surgery versus conservative treatment for lumbar disc herniation: a systematic review with meta-analysis. Br J Sports Med. 2016;50:221-230. [DOI] [PubMed] [Google Scholar]
- 32.Riesenburger RI, David CA. Lumbar microdiscectomy and microendoscopic discectomy. Minim Invasive Ther Allied Technol. 2006;15:267-270. [DOI] [PubMed] [Google Scholar]
- 33.Roberts DW, Roc GJ, Hsu WK. Outcomes of cervical and lumbar disk herniations in Major League Baseball pitchers. Orthopedics. 2011;34:602-609. [DOI] [PubMed] [Google Scholar]
- 34.Sairyo K, Kitagawa Y, Dezawa A. Percutaneous endoscopic discectomy and thermal annuloplasty for professional athletes. Asian J Endosc Surg. 2013;6:292-297. [DOI] [PubMed] [Google Scholar]
- 35.Sakou T, Masuda A, Yone K, Nakagawa M. Percutaneous discectomy in athletes. Spine. 1993;18:2218-2221. [DOI] [PubMed] [Google Scholar]
- 36.Savage JW, Hsu WK. Statistical performance in National Football League athletes after lumbar discectomy. Clin J Sport Med. 2010;20:350-354. [DOI] [PubMed] [Google Scholar]
- 37.Schroeder GD, McCarthy KJ, Micev AJ, Terry MA, Hsu WK. Performance-based outcomes after nonoperative treatment, discectomy, and/or fusion for a lumbar disc herniation in National Hockey League athletes. Am J Sports Med. 2013;41:2604-2608. [DOI] [PubMed] [Google Scholar]
- 38.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712-716. [DOI] [PubMed] [Google Scholar]
- 39.Sugimine Y, Sakaeda K, Yamashita K, et al. Surgical treatment of lumbar herniated nucleus pulposus combined with residual bony fragment of apophyseal ring fracture in high-level athletes: a report of two cases. J Med Invest. 2019;66:358-361. [DOI] [PubMed] [Google Scholar]
- 40.Takatalo J, Karppinen J, Niinimäki J, et al. Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine. 2009;34:1716-1721. [DOI] [PubMed] [Google Scholar]
- 41.Tsou PM, Yeung CA, Yeung AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J. 200;4:564-573. [DOI] [PubMed] [Google Scholar]
- 42.Wang JC, Shapiro MS, Hatch JD, Knight J, Dorey FJ, Delamarter RB. The outcome of lumbar discectomy in elite athletes. Spine. 1999;24:570-573. [DOI] [PubMed] [Google Scholar]
- 43.Watkins RG, 4th, Hanna R, Chang D, Watkins RG, 3rd. Return-to-play outcomes after microscopic lumbar diskectomy in professional athletes. Am J Sports Med. 2012;40:2530-2535. [DOI] [PubMed] [Google Scholar]
- 44.Watkins RG, 4th, Williams LA, Watkins RG, 3rd. Microscopic lumbar discectomy results for 60 cases in professional and Olympic athletes. Spine J. 2003;3:100-105. [DOI] [PubMed] [Google Scholar]
- 45.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441-2450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weistroffer JK, Hsu WK. Return-to-play rates in National Football League linemen after treatment for lumbar disk herniation. Am J Sports Med. 2011;39:632-636. [DOI] [PubMed] [Google Scholar]
- 47.Williams RW. Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine. 1978;3:175-182. [PubMed] [Google Scholar]
- 48.Yeung AT. The evolution of percutaneous spinal endoscopy and discectomy: state of the art. Mt Sinai J Med. 2000;67:327-332. [PubMed] [Google Scholar]
- 49.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27:722-731. [DOI] [PubMed] [Google Scholar]
- 50.Yoshimoto M, Takebayashi T, Ida K, Tanimoto K, Yamashita T. Microendoscopic discectomy in athletes. J Orthop Sci. 2013;18:902-908. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-2-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-3-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach
Supplemental material, sj-docx-4-sph-10.1177_1941738121991782 for Return to Play After Symptomatic Lumbar Disc Herniation in Elite Athletes: A Systematic Review and Meta-analysis of Operative Versus Nonoperative Treatment by Phelopater Sedrak, Mustafa Shahbaz, Chetan Gohal, Kim Madden, Ilyas Aleem and Moin Khan in Sports Health: A Multidisciplinary Approach