Abstract
One in seven US households with children are food insecure. The health effects of household food insecurity (HFI) are well documented, but its association with childhood weight status remains unclear. We aimed to assess this association and to describe correlates of HFI in children. We conducted a cross-sectional study of 3,019 low-income children aged 2–17 years. Data were extracted via chart review. HFI was assessed using the Hunger Vital Sign screener. Body mass index (BMI) was calculated from documented clinical measurements. We used adjusted linear and logistic regression to assess the association of HFI with BMI z-score (BMIz) and weight status. We used logistic regression to examine correlates of HFI including age, race/ethnicity, tobacco exposure, number of parents and siblings living at home, weight status, and census-tract poverty rate and food access. Of participants whose HFI status was documented, 91% were food secure and 9% were food insecure. The mean (SD) BMIz was 0.81 (1.11). 55% of children were healthy weight, 18% overweight, and 26% obese. In adjusted analyses, HFI was not associated with BMIz but was associated with decreased odds of obesity (OR 0.56; 95% CI 0.36–0.87). Tobacco exposure (1.63; 1.10–2.44), additional siblings (1.16; 1.04–1.30), and residence census tract with high poverty rate (1.02; 1.01–1.03) were all associated with HFI. We concluded that food-insecure children were less likely to have obesity and had differences in household makeup, exposures, and residential location compared to food-secure children. Clinicians should understand these relationships when counseling families about weight status and food insecurity.
Keywords: food insecurity, obesity, pediatrics, socioeconomics, body mass index, weight
INTRODUCTION
In 2017, one in seven US households with children met the United States Department of Agriculture’s (USDA) definition for food insecurity, “a household in which adequate food is limited by lack of money and other resources.”1 Children living with household food insecurity (HFI) are at increased risk of poor health outcomes. These include but are not limited to developmental delay, aggression, depression, predisposition to chronic disease in adulthood, and increased hospitalization rates.2–5 As the USDA definition suggests, HFI is a resource-constrained condition associated with low socioeconomic status. Households characterized by low-income, minority race, or single-parent status are at increased risk of having HFI.6,7
Like HFI, pediatric obesity is associated with low socioeconomic status. By 9 months of age the risk of having obesity begins to diverge by socioeconomic grouping, and by 4 years of age, children living in a low-income household have 3–4 times the odds of having obesity.8,9 Similar to HFI, households characterized by low-income, minority race, or single-parent status are at increased risk of having children with obesity.9–12
However, despite their similar associations with low socioeconomic status, the association between HFI and weight status in children, as opposed to certain adult populations, remains uncertain. In adult women a link has been described between HFI and weight accumulation leading to obesity.7–9 However, in the two decades since the seminal case report by Dietz describing a correlation in a female child from Boston,10 studies have demonstrated conflicting results, ranging from a positive to a negative to no association between HFI and weight status in children.3,4,11,13–17
Though most of these numerous studies have evaluated this association using population-level screening measures, there is limited data evaluating it in a clinical setting and no studies have incorporated the new individualized Hunger Vital Sign clinical screening measure into this analysis.19 As the American Academy of Pediatrics (AAP) has recommended that all pediatricians routinely screen for HFI,19 understanding the relationship between HFI and childhood weight status could help clinicians tailor recommendations to improve care for individual patients from low-income populations. Therefore, our primary aim was to examine the association between HFI and weight status in a population of children ages 2–18 years old in a pediatric primary care clinic that serves a predominantly low-income population. Additionally, though numerous individual risk factors for HFI have been established, it is less clear how neighborhood factors are associated with HFI in low-income children. Therefore, our secondary aims were to utilize demographic data to describe associations between child, parent, and family characteristics and HFI and to utilize Geographic Information Systems (GIS) to describe associations between neighborhood characteristics and HFI.
METHODS
Study Overview
We conducted a retrospective chart review of children ages 2–18 years old who attended a well-child visit between March 1, 2016 and February 28, 2017 at our institution’s pediatric residency continuity clinic. This clinic receives about 19,000 visits annually, including 11,000 well child visits and 8,000 acute care visits, and serves primarily a low-income, urban, Medicaid-insured population. All clinic visits for families or patients with low English proficiency are conducted by a certified bilingual provider or with the use of an in-person or video/phone interpreter.
We utilized automated and manual chart review to identify relevant visits and extract data from the electronic health record. Study personnel (SHW, CLB, SB, DP) were trained on a standardized REDCap data abstraction form. Inter-rater reliability testing was performed with a subset of 5% of charts. Cohen’s kappa was calculated at > 0.80. After inter-rater reliability was demonstrated, these same study personnel divided all remaining charts and independently extracted data into the REDCap form. Any questions or disagreements were discussed as a group and a final consensus was achieved. The study was approved by the Institutional Review Board of Wake Forest School of Medicine.
Participants
Data were obtained from 3,019 children. Children were included for review if they 1) were age 2–18 years old and 2) presented for a well-child check at our institution’s pediatric residency continuity clinic between March 1, 2016 and February 28, 2017. Visits were identified as a well visit if they were appropriately coded according to the International Classification of Diseases, Ninth Revision (ICD-9) and International Classification of Diseases, Tenth Revision (ICD-10) codes. We excluded children less than 2 years of age because weight status is not well defined for this age group by the Center for Disease Control and Prevention (CDC) standardized body mass index (BMI)-for-age growth charts. Food insecurity status was not documented on 331 children, leaving a final sample size of 2,668 participants for our analysis.
Measures
Food Insecurity
The Hunger Vital Signs (HVS) screening measure is used by our clinic to screen for HFI and therefore served as the basis for assessing food insecurity status in this study. The HVS distinguishes households at risk for food insecurity from households not at risk for food insecurity in a binary rating system. It was developed for use as a clinical screening measure and has been adopted into the AAP’s guidelines for well child visits.18,19 It has been validated in both English and Spanish language against the USDA’s Household Food Security Module (HFSM) and has shown sensitivity of 97% and specificity of 83% in detecting HFI.18,20,21 The HVS includes two questions: “Within the past 12 months we worried whether our food would run out before we got money to buy more” and “Within the past 12 months, the food we bought just didn’t last and we didn’t have the money to get more.”18 Response options include never, sometimes, or often. A response of “often” or “sometimes” to either question indicates a positive screening result. In our clinic during this time, the provider administered the HVS verbally as part of the well-child visit. Results were documented in the progress note during the visit and were retrospectively extracted via manual chart review. For the purposes of this analysis food insecurity was categorized as food secure vs. food insecure; participants for whom food insecurity was not documented were excluded from analysis.
Weight Status
We assessed weight using two measures: BMI z-score (BMIz, the number of standard deviations away from the mean BMI-for-age) and weight status category. At every well visit height and weight are measured by nursing staff using a wall-mounted stadiometer and mechanical beam scale. Clinical measurements have been shown to have good accuracy compared to height and weight obtained for research purposes.22 Height and weight from the well visit were extracted from the medical record via electronic chart review and were used to calculate BMI. BMIz and BMI percentiles were then derived using the CDC reference growth charts for age and sex.23 Weight status was subsequently classified as underweight (BMI < 5th percentile for age and sex), healthy weight (5th to <85th percentile), overweight (85th to <95th percentile) and obesity (≥ 95th percentile).
Covariates
Demographic variables including date of visit, date of birth, sex, race/ethnicity, insurance type, and residential home address were collected via automated review of each study subject’s chart. Vital signs (including height and weight) from each visit were similarly extracted. Race/ethnicity (as self-reported by the patient or guardian(s)) was categorized as White, Black, Hispanic, or other. Insurance type was classified as Medicaid or other.
Social history variables were gathered via manual chart review of the well visit documentation. These included the relationship of any adult accompanying the child at the visit (mother, father, mother and father, grandparent, aunt or uncle, sibling, other, unknown, or patient alone at visit), household size (quantified as the total number of individuals living in the same household as the child), household makeup (quantified as the distinct number of parents, step-parents, other adults, siblings, and other children living in the same household as the child), and tobacco exposure (exposure and no exposure). These data were compiled from review of the free text of the progress note, which was systematically updated by the clinician during each well visit. Tobacco exposure was recorded in two distinct locations of each well visit’s documentation. It was recorded in the visit intake after being queried by nursing, and it was recorded in the free text of the progress note after being queried by clinicians in either the general social history or the HEADSS (Home, Education/Employment, Activities, Drugs, Sexuality, Suicide/Depression) interview. For the purposes of our study, “active exposure” was defined as use of tobacco by the study participant him or herself, “passive exposure” was defined as use of tobacco by a member of the study participant’s household as documented in either of the locations within the electronic health (EHR), and “no active or passive exposure” was defined as no tobacco use by the participant or members of the household. Household income data was not available in the documentation of the EHR and therefore was not available for inclusion in the analysis. In place of household income, related surrogates were used including insurance status (Medicaid vs other) and census tract federal poverty level.
Geographic variables were collected by first geocoding each subject’s residential home address, as listed in the EHR to a corresponding latitude and longitude in order to identify its census tract, a geographical area which generally includes populations between 1,200 and 8,000 people and which is more granular and localized than a zip code area. Then, using two national data sets, we identified each census tract’s poverty rate and food access. The poverty rate was identified using the 2016 American Community Survey (ACS) 5-year estimates. ACS is a national survey conducted by the US Census Bureau that collects population estimates. A census tract’s poverty rate is defined as the percentage of households in that area that live below 100% of the federal poverty level (FPL).24 Food access was identified using the 2015 USDA Food Access Research atlas, a national data set that provides food access data for populations. Per this atlas, a census tract is considered to have low food access if at least 500 people or 33% of the population live greater than one mile from a supermarket (supermarket, supercenter, or large grocery store) in an urban area or greater than ten miles from a supermarket in a rural area.25
Statistical Analysis
We used t-tests to examine the association of HFI with BMIz and other continuous variables and Pearson’s chi-square tests to examine the association of HFI with weight status and other categorical variables. Covariates associated with HFI, BMIz, or weight status with p<0.2 in the bivariate analysis (child age, race/ethnicity, tobacco exposure, Medicaid insurance, number of parents at home, number of siblings at home, residence in a census tract with low supermarket access, and residence in a census tract with large proportion of households under 100% of the FPL), were then adjusted for in the linear and multinomial logistic regression models that examined the association of HFI with BMIz and weight status, respectively. Covariates that were not associated with HFI, BMIz, or weight status in the bivariate analysis (sex and the relationship of any adult accompanying the child at the well visit) were excluded from later analyses.
Statistical analysis was performed using Stata v14.2 and significance was assessed using a 2-sided test at α=0.05.
Geographic Analysis
For each subject, the geocoded EHR data, HFI, weight status, census tract poverty rate, and census tract supermarket access were modeled as individual geographic layers. Then overlay analysis and spatial data exploration were carried out to visualize distribution of variables in relation to each other. ArcGIS 10.5.1 (ESRI, Redlands, CA) was used for all geographic analyses.
RESULTS
Baseline Characteristics
Of the 2,688 included study participants, the mean (SD) age was 8.8 (4.3) years and 52% were male (Table I). Most were of minority race/ethnicity (71% Hispanic, 22% Black, 4% other, 3% white); 91% were food secure and 9% were food insecure. The mean (SD) BMI was 20.18 (5.58) and mean (SD) BMIz was 0.80 (1.11). Most participants (56%) had a healthy weight status, 17% had overweight, and 25% had obesity (17% with Class 1 obesity, 6% with Class 2 obesity, and 2% with class 3 obesity). More than half (65%) of the study population lived in a census tract with low access to a supermarket (Table 1). Of all charts reviewed (N=3,019), 89% had food security status documented. Patients were less likely to have HFI documented if they were older, Black, non-Medicaid insured, and overweight or obese (Supplemental Table 1).
Table 1.
Participant Characteristics
| Variable |
All participants n = 2,688 N (%) |
Food Secure n = 2,446 N (%) |
Food Insecure n = 242 N (%) |
|---|---|---|---|
| Male Sex | 1409 (52.4%) | 1271 (51.9%) | 138 (57.0%) |
| Age | |||
| 2–6 years old | 998 (37.1%) | 894 (36.6%) | 104 (42.9%) |
| 7–10 years old | 801 (29.8%) | 726 (29.7%) | 75 (31%) |
| 11–13 years old | 505 (18.8%) | 456 (18.6%) | 49 (20.3%) |
| 14+ years old | 384 (14.3%) | 370 (15.1%) | 14 (5.8%) |
| # Parents at home | |||
| 0 | 65 (2.7%) | 57 (2.65%) | 8 (3.7%) |
| 1 | 883 (37.2%) | 798 (37%) | 85 (39.4%) |
| 2 | 1422 (60.0%) | 1300 (60.3%) | 122 (56.5%) |
| 3 | 1 (0.04%) | 0 (0%) | 1 (0.5%) |
| # Siblings at home | |||
| 0 | 281 (10.9%) | 258 (11%) | 23 (9.8%) |
| 1 | 698 (27.1%) | 645 (27.6%) | 53 (22.5%) |
| 2 | 787 (30.6%) | 711 (30.4%) | 76 (32.2%) |
| 3+ | 807 (31.4%) | 723 (30.9%) | 84 (35.6%) |
| # Other adults at home (non-parents) | |||
| 0 | 1950 (72.5%) | 1776 (72.6%) | 174 (71.9%) |
| 1+ | 738 (27.5%) | 670 (27.4%) | 68 (28.1%) |
| # Other children at home (non-siblings) | |||
| 0 | 2307 (85.8%) | 2096 (85.7%) | 211 (87.2%) |
| 1+ | 381 (14.2%) | 350 (14.3%) | 31 (12.8%) |
| Tobacco Exposure- | |||
| Active Exposure | 4 (0.2%) | 4 (0.2%) | 0 (0%) |
| Passive Exposure | 357 (15.1%) | 300 (14.1%) | 57 (25.1%) |
| No Active or Passive Exposure | 2000 (84.7%) | 1830 (85.8%) | 170 (74.9%) |
| Insurance Type | |||
| Medicaid | 2014 (95.6%) | 1839 (95.3%) | 175 (98.9%) |
| Other | 93 (4.4%) | 91 (4.7%) | 2 (1.1%) |
| Race | |||
| White | 90 (3.4%) | 81 (3.3%) | 9 (3.7%) |
| Black | 580 (21.8%) | 520 (21.5%) | 60 (24.9%) |
| Hispanic | 1883 (70.7%) | 1723 (71.1%) | 160 (66.4%) |
| Other | 111 (4.2%) | 99 (4.1%) | 12 (4.9%) |
| Neighborhood with low access to supermarket* | 1533 (64.8%) | 1397 (64.8%) | 136 (65.4%) |
| Neighborhood Poverty Rate** | 32.3 (16.7) | 31.9 (16.7) | 35.9 (16.0) |
| BMI Category*** | |||
| Underweight | 38 (1.4$) | 35 (1.5%) | 3 (1.2%) |
| Healthy Weight | 1483 (44.9%) | 1330 (55.1%) | 153 (63.5%) |
| Overweight | 460 (17.3%) | 417 (17.3%) | 43 (17.8%) |
| Obese | 674 (25.4%) | 632 (26.2%) | 42 (17.4%) |
| BMI z-score | 0.80 (1.11) | 0.82 (1.11) | 0.65 (1.08) |
Low access is defined as living in a census tract where at least 500 people or 33% of the population live greater than one mile from a supermarket, supercenter, or large grocery store in an urban area or greater than ten miles from a supermarket, supercenter, or large grocery store in a rural area
Poverty rate is defined as the percent of households in a geographic area that live below 100% of the federal poverty level
BMI categories are defined as Underweight (BMI less than the 5th percentile for age), Healthy Weight (BMI between the 5th and 85th percentiles for age), Overweight (BMI between the 85th and 95th percentiles for age), and Obese (BMI greater than the 95th percentile for age)
Bivariate Analysis
In the bivariate analysis, food insecure participants had a lower mean BMIz than food-secure participants (0.65 vs 0.82, p=0.01). A smaller percentage of food-insecure participants had obesity compared to food secure participants (17.4% vs 26.2%, p=0.02) and a larger percentage of food-insecure participants were healthy weight compared to food-secure participants (63.5% vs 55.1%, p=0.02). Food insecure participants lived in neighborhoods with a higher proportion of households that lived below the FPL than food secure participants (mean difference 3.9%, 95% CI 1.6, 6.3).
Multivariate Analysis
In adjusted linear regression analysis examining the association of HFI and BMIz we found that HFI was not significantly associated with BMIz (β −0.16; 95% CI −0.33, 0.01). In the multinomial regression model when examining weight status as a categorical variable with healthy weight as the referent, HFI was not associated with underweight (RRR: 0.49; 95% CI 0.11, 2.16) or overweight (RRR: 0.99; 0.64, 1.52) but was associated with decreased risk of having obesity (RRR: 0.56; 0.36, 0.87).
In adjusted multivariable analysis examining correlates of HFI, any tobacco exposure was associated with 1.63 times the odds of HFI (95% CI 1.10, 2.44) compared to no tobacco exposure, each additional sibling at home was associated with 1.16 times the odds of HFI (95% CI 1.04, 1.30), and living in a neighborhood with higher proportion of households living below the FPL was associated with 1.02 times the odds of HFI (95% CI 1.01, 1.03). Obesity remained negatively associated with HFI (OR 0.55, 95% CI 0.35–0.86). Age, race/ethnicity, number of parents at home, underweight or overweight weight status, and living in a neighborhood with low access to supermarkets were not associated with HFI (Table II).
Table 2.
Adjusted logistic regression models evaluating the association of HFI with weight status, age, race, tobacco exposure, household makeup, and neighborhood poverty rate, in children age 2–17
| Variable | OR (95% CI) |
|---|---|
| Age | |
| 2–6 years old | ref |
| 7–10 years old | 1.11 (0.77 – 1.61) |
| 11–13 years old | 1.14 (0.72 – 1.82) |
| 14+ years old | 0.40 (0.18 – 0.90) * |
| Race | |
| White | 2.55 (1.11 – 5.90) * |
| Black | ref |
| Hispanic | 1.11 (0.69 – 1.78) |
| Other | 0.79 (0.29 – 2.12) |
| Positive tobacco exposure | 1.63 (1.10 – 2.44) * |
| # Parents at home | 0.87 (0.62 – 1.21) |
| # Siblings at home | 1.16 (1.04 – 1.30) * |
| Neighborhood with low access to supermarket | 1.21 (0.85– 1.71) |
| Neighborhood Poverty Rate | 1.02 (1.01– 1.03) |
| BMI Category | |
| Underweight | 0.50 (0.11 – 2.22) |
| Healthy Weight | ref |
| Overweight | 0.97 (0.63 – 1.49) |
| Obese | 0.55 (0.35 – 0.86) ** |
denotes p<0.05
denotes p<0.01
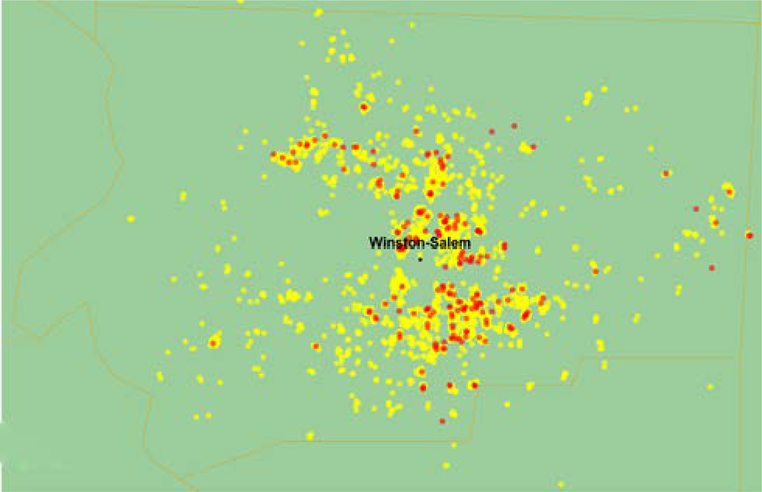
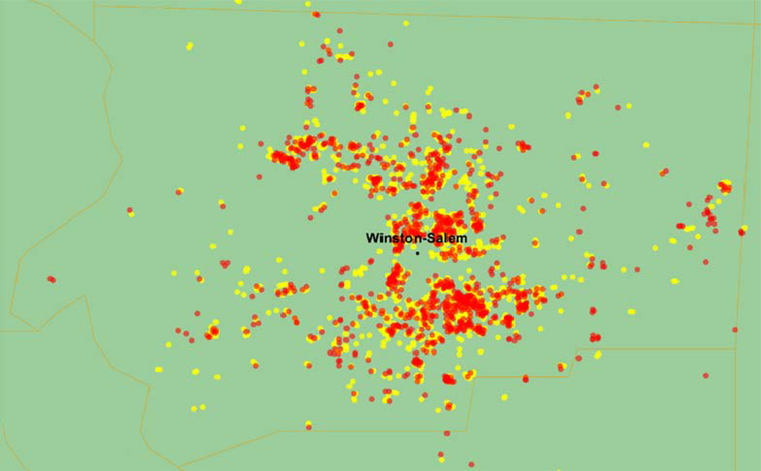
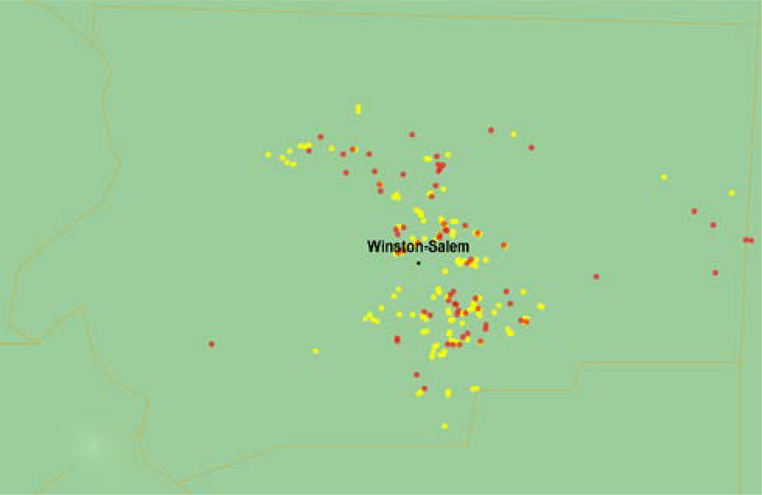
Geographic Distribution of Food Insecurity and Weight Status
The distribution of participant’s food insecurity status and weight status are depicted in Figure 1. Food insecurity was concentrated in neighborhoods located on the eastern side of the city (Figure 1a). In contrast, participants who had overweight/obesity were geographically dispersed throughout Forsyth County, NC (Figure 1b). Among children with food insecurity, children with overweight/obesity tended to be clustered in neighborhoods on the eastern side of the city (Figure 1c).
Fig 1a.
Distribution of Participants’ Food Insecurity Status in Forsyth County, NC. Red/Dark dots represent food-insecure participants. Yellow/Light dots represent food-secure participants. Created using ArcGIS 10.5.1 (ESRI, Redlands, CA)
Fig 1b.
Distribution of Participants’ Weight Status in Forsyth County, NC. Red/Dark dots represent overweight/obese participants. Yellow/Light dots represent healthy weight participants. Created using ArcGIS 10.5.1 (ESRI, Redlands, CA)
Fig 1c.
Among Food Insecure Participants, Distribution of Weight Status in Forsyth County, NC. Red/Dark dots represent overweight/obese participants. Yellow/Light dots represent healthy weight participants. Created using ArcGIS 10.5.1 (ESRI, Redlands, CA)
DISCUSSION
In this population of largely low-income, urban children aged 2–18 years old, we found that children with HFI had similar BMI z-scores compared to children living in food-secure households but had decreased odds of having obesity. In addition, children with HFI were more likely to have tobacco exposure, to have more siblings living at home, and to live in a neighborhood with a higher proportion of households living below 100% of the FPL.
Our primary finding of a negative association between HFI and obesity contradicts much of the established literature.7,26 However, many of these studies were secondary analyses of national food insecurity data gathered using population-level HFI screening measures such as the HFSM, a component of the Current Population Survey conducted by the US Census Bureau. Conversely, our study is the first to use the clinically oriented HVS screening measure, now recommended for use by the AAP at each well child visit. We argue that not all clinical populations are the same and conclusions or clinical practices that rely upon data from large-scale measures like the HFSM might not apply evenly across smaller, unique populations. Our results suggest that the HVS could be a tool to uncover and account for unique characteristics of a singular population, as it did with the association between HFI and obesity in our population.
A few mechanisms have been proposed that could lend credence to our study’s primary finding. Biochemically, compared to adults, children have higher metabolic demand and may have decreased weight gain when food energy is scarce.27 Similarly, the perspective of life course theory, which emphasizes the long-term effects of early life events, suggests that exposure to HFI early in life can predispose to later psychosocial conditions such as anxiety, depression, and impaired familial or social interactivity, all of which can also contribute to decreased weight gain.4,28
With regards to our secondary aims, numerous mechanisms explain the family, household, and geographic characteristics found to be correlates of HFI in our urban study population. Studies examining tobacco use and HFI have suggested that households with members addicted to tobacco products may end up spending their household resources toward purchase of tobacco products rather than toward procuring food.30 Similar studies suggest that members of food insecure households might be more prone to seeking out the anorexic effects of nicotine in order to stem hunger.31 Separately, households with many children are required to stretch food and money resources across more consumers.32 It is interesting though that our secondary findings did not support an association between number of parents in the household and HFI, as this is one of the most often evidenced determinants of HFI.26,33,34
Our study’s geographic findings are interesting due to the relatively nascent utilization of this type of analysis in clinical-level healthcare. We know that the geographically-dependent conditions in which a child is born, lives, and ages have a profound impact on that child’s health and access to resources.35 Though these conditions can inform clinical evaluation and management of patients, clinicians are often unaware of these “geomarkers.”36 Our study sought to fill this knowledge gap. We found that children living in census tracts with a high prevalence of household income below the FPL were more likely to have HFI. This should come as no surprise given the broad body of evidence associating low income and HFI.6,7 Surprisingly, however, our analysis did not show any association between living in a census tract with low food access and HFI. Contrary to what logic might predict, this suggests that in our population, low household income and low food access are not mutually experienced conditions. Further research is needed to understand what census-tract level characteristics could account for these distinctions, such as types of food access available, employment opportunities, the distance from individual patients’ homes to the food access, or other factors. Separately, our analysis showed an overlapping but not identical geographic distribution between children with HFI and children with obesity, further supporting our primary finding of a negative association between HFI and weight status. Children with HFI were concentrated in neighborhoods in the eastern part of the city, while children with obesity were more dispersed throughout the city.
Our study has several strengths. The study population afforded a large sample size of greater than 3,000 subjects, allowing for a well-powered statistical analysis. Second, as previously stated, is unique in its leverage of HFI data that was gathered via a screening measure, the HVS, that is commonly employed in outpatient pediatric clinical settings and that is well-validated across both English and Spanish languages, the primary languages of participants in this study. Third, the use of GIS analysis is also unique amongst current literature examining the association between HFI and childhood weight status.
Conversely, our study has a number of limitations that must be discussed. Despite our large sample size, this was a single-site study composed primarily of an urban, African American or Hispanic, and Medicaid-insured population that was more homogenous in income and racial/ethnic identity than the general pediatric population in the United States in 2017 where an estimated 50% of children were white, non-Hispanic, and 17.5% lived in poverty (defined as having household income below 100% of the federal poverty level).37 Yet, our study population’s distribution of obese weight status (26%) was more consistent with the national trends in pediatric obesity for 2015–2016 (approximately 26.4%).38 Second, our dataset was limited by variables included in the EHR and did not include variables known to be associated with HFI such as household income, parent education, and participation in government nutritional assistance programs. A third limitation is the lower than expected rate of HFI (9%) in our study population. This is lower than 2017’s national prevalence rate of 16% and local prevalence rate of 18%, and lower than might be expected in a predominantly urban, low-income study population.1,3,7 We hypothesize two possible contributors to our study’s lower than expected prevalence. The first is that a high rate of participants (11%) did not have HFI screening documented in the well child check documentation, and it is possible that this may have skewed our study’s HFI prevalence downwards. This could have occurred if providers were less likely to screen patients in who they were busy dealing with other complex issues, as food insecurity is known to be associated with developmental delay, depression, and chronic disease.2–5 Interestingly, patients who were not screened were more likely to have overweight and obesity. The other, likely more important factor, is that during the inclusion dates of our study, our clinic administered the HVS food insecurity screening measure as a verbal measure (read to the family or patient) rather than as a written measure (provided in paper or electronic format for the family or patient to complete independently). We strongly suspect that this allowed for a reporting bias. However, this practice and therefore the data used for our study is likely not dissimilar to actual clinical practice throughout the United States, as literature has demonstrated that caregivers who are administered a verbal screening measure can under-report HFI due to fear of associated stigma.39
CONCLUSION
In this study, we found a negative association in children between HFI and obesity. We also found significant differences between food insecure and food secure children with respect to tobacco exposure, number of siblings at home, and census tract household poverty rate. As addressing HFI continues to be of paramount importance, our findings should contribute to the clinician’s index of suspicion for identifying food insecurity when certain patient, household, and neighborhood characteristics are evident. In a broader sense, as clinicians continue to grapple with the epidemics of childhood obesity and food insecurity, leveraging any associations between the two could be useful. Our study posits that advances against these problems might not dovetail. Ultimately, it contributes to the mixed evidence that exists on the association between HFI and childhood weight status and emphasizes the need for further investigation and understanding of the complex economic underpinnings of both of these conditions.
Supplementary Material
What is Already Known About this Subject:
One in seven US households with children are food insecure
Household food insecurity and obesity share many common risk factors, including low socioeconomic status
What This Study Adds:
In this low-income urban population, children who screened positive for household food insecurity had decreased odds of having obesity.
Children with food insecurity also had increased odds of having tobacco exposure, additional siblings at home, and living in a neighborhood with a high poverty rate.
Acknowledgments:
This work was supported by the National Institutes of Health (Grant Number UL1TR001420) for services received through the Clinical and Translation Science Institute, including electronic data extraction, funded by the National Center for Advancing Translational Sciences (NCATS). We also would like to acknowledge Steven Barilla for his assistance with manual chart review.
Funding Source:
We would like to acknowledge the support of the Wake Forest Clinical and Translational Science Institute, which is supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR001420. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations:
- BMI
body mass index
- BMIz
body mass index z-score
- SES
socioeconomic status
- HFI
household food insecurity
- HVS
hunger vital sign
- USDA
United States Department of Agriculture
- CDC
Center for Disease Control and Prevention
- FPL
Federal Poverty Level
- HER
Electronic Health Record
Footnotes
Conflicts of Interest: The Authors declare that there is no conflict of interest.
REFERENCES
- 1.Coleman-Jensen A, Rabbitt MP, Gregoery CA, Singh A. Household Food Security in the United States in 2017. ERR-256, US Dep Agric Econ Res Serv Published online 2018 m. doi: 10.2139/ssrn.878333 [DOI] [Google Scholar]
- 2.Huang T, Borowski L, Liu B, et al. Pediatricians’ and family physicians’ weight-related care of children in the U.S. Am J Prev Med 2011;41(1):24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whitaker RC, Phillips SM, Orzol SM. Food Insecurity and the Risks of Depression and Anxiety in Mothers and Behavior Problems in their Preschool-Aged Children. Pediatrics. 2006;118(3):e859–e868. doi: 10.1542/peds.2006-0239 [DOI] [PubMed] [Google Scholar]
- 4.Jyoti DF, Frongillo EA, Jones SJ, Al JET. Food Insecurity Affects School Children’s Academic Performance, Weight Gain, and Social Skills. J Nutr 2005;135(12):2831–2839. [DOI] [PubMed] [Google Scholar]
- 5.Howard L. Does food insecurity at home affect non-cognitive performance at school? A longitudinal analysis of elementary student class behavior. Econ Educ Rev 2011;30(1):157–176. https://eric.ed.gov/?id=EJ908274 [Google Scholar]
- 6.Sarlio-Lahteenkorva S, Lahelma E. Food insecurity is associated with past and present economic disadvantage and body mass index. J Nutr 2001;131(11):2880–2884. [DOI] [PubMed] [Google Scholar]
- 7.Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring Mediators of Food Insecurity and Obesity: A review of recent literature. J Community Health. 2013;37(1):253–264. doi: 10.1007/s10900-011-9420-4.EXPLORING [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laraia B a. Food Insecurity and Chronic Disease. Adv Nutr 2012;4:203–212. doi: 10.3945/an.112.003277.Current [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leung CW, Williams DR, Villamor E. Very low food security predicts obesity predominantly in California Hispanic men and women. Public Health Nutr 2012;15(12):2228–2236. doi: 10.1017/S1368980012000857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dietz W. Does hunger cause obesity? Pediatrics. 1995;95(5):766–767. [PubMed] [Google Scholar]
- 11.Alaimo K, Olson C, Frongillo E Jr. Low Family Income and Food Insufficiency in Relation to Overweight in US Children Is There a Paradox? Arch Pediatr Adolesc Med 2001;155(10):1161–1167. [DOI] [PubMed] [Google Scholar]
- 12.Kaiser L, Lamp C, Johns M, Sutherlin J, Harwood J, Meglar-Quinonez H. Food Security and Nutritional Outcomes of Preschool-Age Mexican-American Children. Jounral Am Diet Assoc 2002;102(7):924–929. https://jandonline.org/article/S0002-8223(02)90210-5/pdf [DOI] [PubMed] [Google Scholar]
- 13.Willis D, Fitzpatrick K. Psychosocial factors as mediators of food insecurity and weight status among middle school students. Appetite. 2016;103:236–243. [DOI] [PubMed] [Google Scholar]
- 14.Burke M, Frongillo E Jr, Jones S, Bell B, Hartline-Grafton H. Household Food Insecurity is Associated With Greater Growth in Body Mass Index Among Female Children from Kindergarten Through Eighth Grade. J Hunger Environ Nutr 2016;11(2):227–241. [Google Scholar]
- 15.Gundersen C, Lohman BJ, Garasky S, Stewart S, Eisenmann J. Food Security, Maternal Stressors, and Overweight Among Low-Income US Children: Results From the National Health and Nutrition Examination Survey (1999–2002). Pediatrics. 2008;122(3):e529–e540. doi: 10.1542/peds.2008-0556 [DOI] [PubMed] [Google Scholar]
- 16.Spiers K, Fiese B, Team SKR. The Relationship Between Food Insecurity and BMI for Preschool Children. Matern Child Health J 2016;20(4):925–933. https://www.ncbi.nlm.nih.gov/pubmed/26662281 [DOI] [PubMed] [Google Scholar]
- 17.Rose D. Household Food Insecurity and Overweight Status in Young School Children: Results From the Early Childhood Longitudinal Study. Pediatrics. 2006;117(2):464–473. doi: 10.1542/peds.2005-0582 [DOI] [PubMed] [Google Scholar]
- 18.Hager ER, Quigg AM, Black MM, et al. Development and Validity of a 2-Item Screen to Identify Families at Risk for Food Insecurity. Pediatrics. 2010;126(1):e26–e32. doi: 10.1542/peds.2009-3146 [DOI] [PubMed] [Google Scholar]
- 19.Committee on Nutrition Council on Community Pediatrics. Promoting Food Security for All Children- Policy Statement. Pediatrics. 2015;136(5):e1431–e1438. doi: 10.1542/peds.2015-3301 [DOI] [PubMed] [Google Scholar]
- 20.Makelarski J, Abramsohn E, Benjamin J, Du S, Lindau S. Diagnostic Accuracy of Two Food Insecurity Screeners Recommended for Use in Health Care Settings. Am J Public Health. 2017;107(11):1812–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rooney-Otero K, Schwarzenberg SJ. Addressing Food Insecurity: A Toolkit for Pediatricians; 2017. Žiūrėta birželio; 26, 2020. www.frac.org. [Google Scholar]
- 22.Howe L, Tilling K, Lawlor D. Accuracy of height and weight data from child health records. Arch Dis Child. 2009;94(12):950–954. [DOI] [PubMed] [Google Scholar]
- 23.Rossen L, Kobernik E. Food insecurity and dietary intake among US youth, 2007–2010. Pediatr Obes. 2016;11(3):187–193. https://www.ncbi.nlm.nih.gov/pubmed/26061645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.American Community Survey. United States Census Bureau. https://www.census.gov/programs-surveys/acs/about/information-guide.html.Published online 2016 m.www.socialexplorer.com [Google Scholar]
- 25.Food Access Research Atlas. United States Department of Agriculture. Economic Research Service. Published online 2017 m.:https://www.ers.usda.gov/data-products/food-access. [Google Scholar]
- 26.Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995–2009. Obes Rev 2011;12(501):73–83. doi: 10.1111/j.1467-789X.2010.00820.x [DOI] [PubMed] [Google Scholar]
- 27.Michael Maia S, Antonio Augusto Moura da S, Rafael P-E, Gilberto K. Household food insecurity and excess weight/obesity among Brazilian women and children: a life-course approach Inseguridad alimentaria y exceso de peso/obesidad entre mujeres y niños brasileños: un enfoque para el transcurso de la vida Insegurança aliment. Cad Saude Publica 2013;29(2):219–226. http://american.summon.serialssolutions.com/2.0.0/link/0/eLvHCXMw3V1Lb9NAEF5okRASQpRHeEpz4rJKGz-SOJU4pFGroqpQ0SIhLtHaXgeD4y123dL-Ic78hv4xZnbXjgPlApy4xHa0noftb3d2dnaGMQiHgjKVDWSCY40M-kE0GoT9YNT3pcAptrucWX-1Lm21-O9_eMu7OHGXtILEE0pPnOalrUenFwXkV9oEwM-kmYHvKF23459802 [Google Scholar]
- 28.Frongillo EA, Bernal J. Understanding the Coexistence of Food Insecurity and Obesity. Curr Pediatr Rep 2014;2(4):284–290. doi: 10.1007/s40124-014-0056-6 [DOI] [Google Scholar]
- 29.Bhattacharya J, Currie J, Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. J Health Econ 2004;23(4):839–862. https://www.ncbi.nlm.nih.gov/pubmed/15587700 [DOI] [PubMed] [Google Scholar]
- 30.Cutler-Triggs C, Fryer G, Myoshi T, Weitzman M. Increased rates and severity of child and adult food insecurity in households with adult smokers. Arch Pediatr Adolesc Med 2008;162(11):1056–1062. https://www.ncbi.nlm.nih.gov/pubmed/18981354 [DOI] [PubMed] [Google Scholar]
- 31.Kim J, Tsoh J. Cigarette Smoking Among Socioeconomically Disadvantaged Young Adults in Association With Food Insecurity and Other Factors. Prev Chronic Dis 2016;13(E08). https://www.ncbi.nlm.nih.gov/pubmed/26766849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller D, Nepomnyaschy L, Ibarra G, Garasky S. Family structure and child food insecurity. Am J Public Health. 2014;104(7):e70–e76. https://ajph.aphapublications.org/doi/10.2105/AJPH.2014.302000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coleman-Jensen A, Gregory C, Singh A. Household Food Security in the United States in 2013. Dep Agric Econ Res Serv 2013;ERR 173. 2014;(173):33. doi: 10.2139/ssrn.2504067 [DOI] [Google Scholar]
- 34.Balistreri K. Family Structure, Work Patterns and Time Allocations: Potential Mechanisms of Food Insecurity among Children. Univ Kentucky Cent Poverty Res Discuss Pap Ser 2012;07. [Google Scholar]
- 35.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping neighborhood health geomarkers to clinical care decisions to promote equity in child health. Health Aff 2017;36(6):999–1005. doi: 10.1377/hlthaff.2016.1425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Beck A, Huang B, Chundur R, Kahn R. Housing Code Violation Density Associated with Emergency Department Use By Children With Asthma. Health Aff 2014;33(11):1993–2002. doi: 10.1002/cncr.27633.Percutaneous [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.US Current Population Survey, US Census Bureau and US Bureau of Labor Stastitics.
- 38.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3). doi: 10.1542/peds.2017-3459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Barnidge E, Krupsky K, LaBarge G, Arthur J. Food Insecurity Screening in Pediatric Clinical Settings: A Caregivers’ Perspective. Matern Child Health J 2020;24(1):101–109. doi: 10.1007/s10995-019-02785-6 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.