Abstract
Background
Given the pressure on modern healthcare systems, eHealth can offer valuable opportunities. However, understanding the potential and challenges of eHealth in daily practice can be challenging for many general practitioners (GPs) and their staff.
Objectives
To critically appraise five widely used eHealth applications, in relation to safe, evidence-based and high-quality eHealth. Using these applications as examples, we aim to increase understanding of eHealth among GPs and highlight the opportunities and challenges presented by eHealth.
Discussion
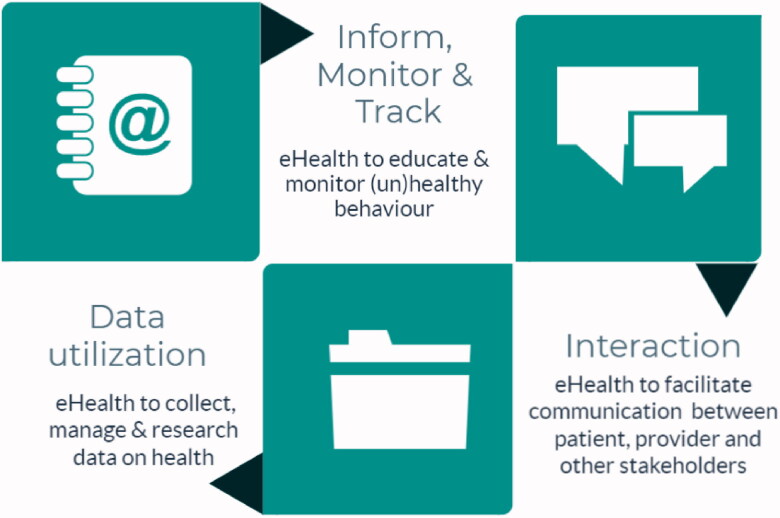
eHealth applications can support patients while increasing efficiency for GPs. A three-way division (inform, monitor, track; interaction; data utilisation) characterises many eHealth applications, with an increasing degree of complexity depending on the domain. All applications provide information and some have extra functionalities that promote interaction, while data analysis and artificial intelligence may be applied to support or (fully) automate care processes. Applications in the inform domain are relatively easy to use and implement but their impact on clinical outcomes may be limited. More demanding applications, in terms of privacy and ethical aspects, are found in the data utilisation domain and may potentially have a more significant impact on care processes and patient outcomes. When selecting and implementing eHealth applications, we recommend that GPs remain critical regarding preconditions on safe, evidence-based and high-quality eHealth, particularly in the case of more complex applications in the data utilisation domain.
Keywords: eHealth, primary care, challenges, opportunities
KEY MESSAGES
eHealth applications show varying degrees of complexity; while all applications generally provide information, additional features may support interaction and in advanced applications data analysis can automate processes.
High-risk and high-gain: the higher the complexity, the higher the potential impact.
Scientific evidence on effectiveness is often lacking or of insufficient quality.
Introduction
eHealth in primary care
Healthcare worldwide faces a heavier and increasingly complex workload due to an ageing population and a rise in multimorbidity [1]. Primary care bears the full brunt of this pressure because it is usually the first port-of-call for the general population [2]. This increasing pressure creates a necessity for a more efficient organisation and better distribution of care [3]. Inherent to this change are general practitioners (GPs) and their staff who have to deal with changing patient-provider relationships. Tailored care that focuses on a patient’s autonomy, self-management and self-efficacy is becoming increasingly important [4]. The COVID-19 pandemic further underlines the need for a transformation of care, as continuity of care should be secured even in times of limited access to face-to-face care [5].
eHealth has been proposed as a valuable tool to support healthcare and ensure universal health coverage [1]. According to Shaw et al. (Figure 1) [6], eHealth has three main functions: (1) ‘Inform, monitor and track’ to observe and study health parameters; (2) ‘Interaction’ to support communication; and (3) ‘Data utilisation’ to collect, manage, and use health data [1]. In daily practice, eHealth applications ranging from mobile phone applications to telemonitoring systems often encompass multiple domains.
Figure 1.
Conceptualisation of eHealth in primary care, derived from Shaw et al. [11].
In the first four articles of this series on eHealth, we addressed issues related to the successful uptake and use of eHealth in primary care [1,7–9]. These issues were described from various perspectives ranging from ethical aspects to education and implementation, including the six preconditions that we view as pivotal to ensure safe, evidence-based and high-quality eHealth (Box 1). However, for many GPs, it may still be challenging to maintain an up-to-date overview of the opportunities and challenges pertaining to the use of eHealth in daily practice. Therefore, this opinion paper aims to apply the six preconditions for high-quality eHealth, which are described in detail in Part 1 of the SERIES [1], to critically appraise specific and tangible eHealth applications currently in use in primary care. We intend to increase GPs’ understanding of eHealth and provide insight into the opportunities and challenges concerning the use of eHealth. Using examples illustrating the potential of eHealth, we hope to inspire and encourage GPs, while at the same time remaining reflective and critical regarding eHealth applications in daily practice.
Box 1.
Conditions to ensure safe, evidence-based and high-quality eHealth [2]
|
Contextual factors
Country-specific aspects
Adoption of eHealth differs among and within countries and is influenced by several factors, such as the details of national policy. Regarding the six preconditions (co-creation, blended care, individualisation, globalisation, evidence and ethics), there is a lack of consistent national monitoring or thorough evaluation of eHealth internationally [10]. In existing literature, several countries are mentioned repeatedly because of well-established digital health infrastructure. Denmark is considered to be an international front runner because of the combination of an advanced high-quality digital health system and an excellent nationwide Digital Health Strategy that focuses on co-creation, blended care, individualisation and ethics [11]. A comprehensive digital system enables Danish GPs, healthcare facilities, nursing homes and other facilities to cooperate better and decrease inequalities. In Australia, a national digital strategy focuses on leveraging co-creation and blended care in a digitally-savvy society, combined with a clear digital health vision that places the individual patient at the centre of care [12].
Several countries, including New Zealand, the Nordic countries and Israel, are relatively advanced in adopting eHealth and have a sound digital strategy in place that details preconditions for co-creation and blended care [12]. In New Zealand, regional systems integrate data from several primary care providers (i.e. community nurses, pharmacists and GPs) and hospitals, forming a broadly accessible data structure (depending on access rights) [13]. In the Netherlands, most primary care practices offer eHealth, although the level of use varies considerably and co-creation with the patient is still rare [14]. In Canada and the United States, GPs are increasingly adopting eHealth, including telemedicine for online consultation, a trend further boosted by COVID-19 [15]. The challenge now is to find a responsible approach to maintaining the use of eHealth as the COVID-19 pandemic recedes.
General practitioner-specific aspects
The speed of eHealth implementation depends for a large part on the willingness of physicians. While some healthcare providers can be considered early adopters and are open to using eHealth in daily practice [16], others may be more reluctant to change their routines. The expectations of general practitioners concerning the impact of eHealth on workload are sometimes conflicting, with one qualitative study stating that the majority of general practitioners thought that eHealth would reduce their workload while another large survey in the same country found that only 10% had similar expectations [17,18].
Other factors influencing the use and adoption of eHealth in daily practice relate to healthcare providers’ preferences, e.g. seeing patients face-to-face and perceptions about the (added) value of e-consultations or telemonitoring in relation to improving care and relationships with patients [19]. Legislative aspects may also play a role, as there can be uncertainty about professional responsibilities [7]. Furthermore, healthcare providers appear less inclined to use eHealth if they are worried about their job security or cost aspects, citing issues such as the extra costs of eHealth applications without compensation or the loss of revenue if the costs but not the benefits are felt at the practice level [19,20]. Differing preferences may also be linked to a lack of knowledge about and attitudes towards eHealth’s opportunities and challenges.
Aspects concerning the complexity of eHealth applications
The complexity of an eHealth application, ranging from less complex applications in the inform domain to more complex applications in the data utilisation domain, together with the required level of care reorganisation, directly affects adoption rates [20]. Using a relatively simple eHealth application to replace a specific routine, e.g. tracking the lifestyles of patients with chronic diseases with an app rather than a paper diary, requires different abilities compared to applications that radically change work processes, e.g. 24/7 telemonitoring of patients with diabetes rather than seeing them on a quarterly basis. The lessons learned from the first four papers in the eHealth series are relevant and important to all applications, especially in the case of more complex applications [1,7–9]. Furthermore, patient factors are related to the complexity of applications and need to be considered. For example, a fair degree of (health) literacy and digital competencies are required, especially for complex applications [1]. Other factors influencing the use of eHealth include age, income and education [21]. Iterative co-creation processes with relevant target groups are essential during the development and implementation of eHealth applications.
eHealth applications
To support GPs interested in adopting eHealth, we describe five widely-used eHealth applications. Applications were eligible for inclusion in the paper if they were relevant to primary care and currently in wide use. As it was not our aim to provide a comprehensive overview of all existing applications, we selected only five applications. To cover all the domains detailed by Shaw et al., we set at least one application per domain, with the applications serving as examples to illustrate the opportunities and challenges of eHealth in primary care and as aids to help define critical aspects of concern to GPs. Using these examples, we elaborate on the preconditions for safe, evidence-based and high-quality eHealth (Box 1) and the five examples highlight how these preconditions ultimately influence the adoption and utilisation of eHealth applications.
The five included applications were selected pragmatically, based on consensus and brainstorm sessions with the co-authors. One of the authors (ET) checked the literature, websites and the application itself to extract information regarding the six preconditions for all applications. MK also reviewed the literature, websites and applications to validate the results. The next step was validation of the results by the whole author group and discussion to form the final opinion and interpretation of the findings.
The tables presented below summarise the five commonly used eHealth applications. Table 1 provides a description of the relevant domain(s) in relation to the Shaw classification. Table 2 describes preconditions for safe, evidence-based and high-quality eHealth.
Table 1.
Description of five widely used eHealth applications.
| Description | Shaw domain |
|---|---|
| Thuisarts.nl | |
| https://www.thuisarts.nl. Non-commercial public website in the Netherlands, launched by the Dutch College of General Practitioners. It provides patients with understandable and reliable medical information combined with automated (non-personal) advice. It includes the content of evidence-based guidelines on 600 topics. Each topic consists of several ‘patient situations’ (e.g. I have the flu, my child has the flu) and provides information on what to do and when to contact the GP. It includes illustrations, short videos, patient decision aids and eHealth self-management tools. It has an extremely high in-country use (24 million visitors in 2018) [37]. https://gpinfo.nl is the English version of Thuisarts.nl, covering a selection of medical topics. | Inform, monitor, track |
| Liva Healthcare | |
| https://livahealthcare.com. Innovative digital health programs to improve a variety of lifestyle behaviours by creating bonds between the lifestyle coach and the patient. The digital behavioural change programs consist of real-time personal coaching and pre-recorded videos, group-based interventions, tailored health plans, goal-tracking and self-monitoring, and fixed evidence-based curriculums personalised to support people at risk of or living with chronic conditions. Developed in Denmark in 2015 and was recently implemented in Norway, UK and Australia. | Inform, monitor, track Interaction |
| SHUTi | |
| https://www.somryst.com. An online intervention for the treatment of insomnia in adults. It is a fully automated, interactive and tailored web-based program that incorporates the primary tenets of face-to-face Cognitive Behavioural Therapy for Insomnia (CBT-I), including sleep restriction, stimulus control, cognitive restructuring, sleep hygiene and relapse prevention. Developed in the United States. | Inform, monitor, track Interaction |
| Babylon | |
| https://www.babylonhealth.com. AI system that can receive data about a patient’s symptoms, compare the information to a database of known conditions and illnesses, and then identify a course of action and related risk factors. It contains a virtual GP appointment, digital prescriptions, digital health check, instant symptom chequer, online view of medical records, and a chatbot. It is now an integrated part of the UK-based NHS. It can be used by patients who have registered for the service. Patients register with ‘GP at Hand’ and can then consult a digital GP within minutes of registration; however, they have to switch from their current GP practice to Babylon. Certain GPs work specifically for Babylon, with whom the patient registers. Video appointments are possible 24/7 in collaboration with 7 clinics in London and 1 clinic in Birmingham. | Inform, monitor, track Interaction Data utilisation |
| SkinVision | |
| https://www.skinvision.com/nl/. International skin cancer detection app allows patients to check suspicious skin spots themselves, promoting timely, appropriate care. It is available as either a freely downloadable app or a paid service, which various health insurers reimburse. A user can self-assess the skin cancer risk of a skin lesion by taking a photo with his/her smartphone, which is then processed by an algorithm. The user receives feedback on the risk presented by the skin lesion. SkinVision was developed by an official dermatology clinic regulated by the Dutch healthcare system, and can replace a normal dermatology consultation. Patients can also choose to send the photo to their healthcare professional, who will also receive the algorithm’s outcome as support in their diagnosis. The app also has a tracking function that can track skin spots over time. https://www.healthnavigator.org.nz/apps/f/firstcheck-app/. is a similar version from New Zealand | Inform, monitor, track Interaction Data utilisation |
AI: Artificial Intelligence; CBT: cognitive behavioural therapy; GP: general practitioner; NHS: National Health Service; UK: United Kingdom.
Table 2.
Evaluation of five widely used eHealth applications using six preconditions for high-quality eHealth.
| Co-creation | Blended care | Individual and inclusive Applicable in high and low resource setting |
Scientific evaluation | Ethics | Summary and recommendations |
|---|---|---|---|---|---|
| Thuisarts.nl | |||||
|
Intended use of Thuisarts.nl:
As patients have a better understanding of their complaints, the consultation could be more tailored. |
|
|
|
Website that informs patients and GP’s about basic medical conditions. Simple application, without a major negative impact on daily routines. However, Thuisarts.nl has not yet systematically adapted to the wishes and requirements of the end-users, which we believe is a precondition for the development of a professional and high-quality eHealth application |
| Liva Healthcare | |||||
Development by:
|
|
|
|
Liva Healthcare is an easy-to-use application to improve lifestyle, with evidence-based results on clinical outcomes, high user-satisfaction and limited resistance from doctors [38]. This eHealth tool can support behavioural changes through monitoring and providing relevant feedback. Support from family and peers also matters, and long-term success depends on ability to establish positive day-to-day support [30] |
|
| SHUTi | |||||
Development by multidisciplinary team of:
|
|
|
|
Effective and practical online solution for the treatment of insomnia in general practice. Insomnia is currently not adequately treated in the primary care setting [44] due to limited knowledge of sleep treatments [39] . Hence, contrary to international clinical guidelines that recommend CBT-I as the first line treatment for insomnia, hypnotic medication remains the primary treatment modality in the majority of the patients [45]. SHUTi is considered a viable option in the treatment of insomnia [43] | |
| Babylon | |||||
Development by:
Babylon is regulated by the Care Quality Commission in England |
|
The advantages are:
|
|
|
AI-based platform that claims to help patients to make a diagnosis. The usability is good, but there is no peer-reviewed analysis of data and a significant risk of underperforming diagnostics |
| SkinVision | |||||
Development by a multidisciplinary team:
According to existing law SkinVision is a healthcare provider and must meet established qualitative and safety requirements. Initially, it did not comply with legal requirements and, among others, had to draw up a policy plan by October 2020 [47] |
|
|
|
|
Skin cancer detection app for patients and doctors, based on an algorithm with high sensitivity and moderate specificity to detect skin cancer; there is room for improvement in terms of specificity and in terms of qualitative and safety requirements |
AI: Artificial intelligence; GP: general practitioner; QoL: quality of life.
Discussion
Main findings
The goal of this opinion paper was to provide insight into and give examples of the opportunities and challenges pertaining to the use of eHealth in primary care. We will discuss five specific and tangible eHealth applications currently used in primary care. Our critical appraisal of these applications confirmed the three-way division of eHealth applications, characterised by increasing degrees of complexity. While all five applications provide information, interaction can be added to expand functionalities (Liva Healthcare and SHUTi), and data analysis and artificial intelligence can optionally be used to (fully) automate care processes (Babylon and SkinVision). Preconditions on safe and high-quality eHealth are relevant for all applications. Still, following our evaluation, we now argue that this is especially the case for more complex interventions in the data utilisation domain. In our opinion, these applications possess high-risk, high-gain potential both at the patient and GP level. To clarify, applications in the information domain, such as Thuisarts.nl, as well as some in the interaction domain, such as Liva Healthcare, can be readily recommended by any GP. Risks due to privacy or ethical issues are minimal, as no or limited data are collected and no drastic changes are made to the clinical process. While the impact on clinical outcomes of applications in the information domain may be minimal, the impact of applications in the interaction domain is likely to be much more profound. Applications in the data utilisation domain present significantly greater risk, as ethical aspects including patient safety and privacy might be at stake if an algorithm is inaccurate or data are not safely stored. On the other hand, the potential yield regarding patient outcomes and care processes is often high, e.g. diagnostic processes are performed at home instead of in a clinical setting, thereby increasing efficiency, or algorithms are used that outperform doctors in, for example, diagnostic processes and thus positively affect patient outcomes.
Impact on the care process
While patients seem very satisfied with applications that automatically use data, GP resistance tends to increase when they feel that their control of the care process is diminishing or if there is uncertainty surrounding the reliability and security of data [22,23]. Nevertheless, it is doubtful that all patients fully understand the risks of these types of applications and initial satisfaction will probably diminish following negative experiences, such as when an app ‘gets it wrong’ or after a data leak. If using an eHealth application is too disruptive to regular GP routines or if it leads to higher costs, job insecurity or loss of revenue, GPs will understandably perceive this as a barrier to using the application [19]. Moreover, the level of proficiency in the use of information technologies might also affect the use of eHealth [8]. Applications that mainly provide information to patients, such as Thuisarts.nl, are the least ‘threatening’ for GPs, offer multiple ways to support their care processes and understandably are also popular with GPs. Applications like SkinVision could radically change the diagnostic process, require GPs to have a basic understanding of AI and therefore have a greater impact on daily GP practice. Clearly, the degree of disruption to a GP practice will form a barrier to using an eHealth application [9]. The greater the disruption, the greater the need for reliable testing of technical accuracy and clinical effectiveness. GPs should also consider that implementing complex eHealth interventions might require the reorganisation of care [24]. If adopted, eHealth applications must be implemented and integrated into the daily work processes of GPs.
Scientific evaluation
While scientific evaluation of eHealth applications is essential to ensuring the safety and successful implementation of eHealth [25], scientific evidence concerning effectiveness, usability and accuracy is often lacking [26,27] or is of insufficient quality [28]. This is a particularly thorny issue in the data utilisation domain, where scientific evaluation is still in an early phase, meaning that critical external scientific evaluation is an ongoing process. The applications discussed here differ greatly in terms of supporting evidence on efficacy. Evidence concerning thuisarts.nl is available, but this focuses solely on healthcare usage [29], and no peer-reviewed evidence is available regarding, for example, usability or outcomes. Liva Healthcare and SHUTi have undergone more extensive testing, including their effects on patient outcomes and experiences [30–34]. Even though this evidence may be derived from the general population, this information is still relevant to primary care. Nonetheless, further investigation in a primary care setting would be valuable. Evidence is available regarding the accuracy and performance of SkinVision [35,36], but additional real-life studies are needed. Babylon is claimed to be effective, but there is no evidence to support this. Furthermore, it should be noted that (co)founders or employers of Thuisarts.nl, Liva Healthcare and SkinVision are co-authors of the scientific publications describing these applications. We suggest GPs remain critical towards eHealth applications in terms of available evidence and to check whether demonstrably independent experts provide effectiveness.
Take home messages
The main advantages of the applications described in this paper, considerations that often apply to eHealth in general, are the relative ease of use for many patients, the high level of satisfaction, and the higher degree of independence and 24/7 applicability. In parallel, GPs can work more efficiently because eHealth supports patient self-management, lowering the demand for physical consultations. Nevertheless, perceived barriers for large-scale implementation include dealing with complex applications or a feeling of diminishing control of the clinical process.
In Part 1 of the SERIES, we concluded that scientific research on eHealth applications is essential, preferably performed continuously while incorporating different viewpoints [1]. With the current paper, it became clear that evidence is often limited, even in already widely-used applications. Although some research is available on the applications included here, it mainly focussed on one specific aspect and continuous assessment of effectiveness was lacking. Furthermore, some studies were performed by the developers rather than by independent scientists, which might have compromised reliability. Therefore, we recommend a critical stance regarding eHealth applications, which should include assessing any external scientific evaluation that may have been performed. Independent institutes could play a leading role in collecting and publishing this evidence. If eHealth applications are not validated by peer-reviewed scientific research, they should be implemented only with great restraint. If an application is likely to cause disruption to a GP’s routine work processes, such as the case with Babylon, we believe that effectiveness must be proven before implementation.
A limitation of this paper was the description of only five selected applications, as we wished to discuss the potential of eHealth based on specific examples. To obtain a broader overview of the availability and effectiveness of eHealth in primary care, it might be interesting to perform an umbrella review summarising published systematic reviews in this field.
Conclusion
eHealth applications in primary care appear to exhibit a three-way division, with increasing degrees of complexity ranging from relatively simple applications providing information to more complex applications that use data and/or change the organisation of care. To select viable eHealth applications for implementation in primary care, six preconditions that ensure safe, evidence-based and high-quality eHealth must be met, particularly in the case of more complex applications.
Disclosure statement
The authors declare no conflict of interest. The authors alone are responsible for the content and writing of the paper.
References
- 1.van der Kleij R, Kasteleyn MJ, Meijer E, et al. . SERIES: eHealth in primary care. Part 1: concepts, conditions and challenges. Eur J Gen Pract. 2019;25(4):179–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erler A, Bodenheimer T, Baker R, et al. . Preparing primary care for the future – perspectives from The Netherlands, England, and USA. Z Evid Fortbild Qual Gesundhwes. 2011;105(8):571–580. [DOI] [PubMed] [Google Scholar]
- 3.Fisher RF, Croxson CH, Ashdown HF, et al. . GP views on strategies to cope with increasing workload: a qualitative interview study. Br J Gen Pract. 2017;67(655):e148–e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tan SS, Goonawardene N.. Internet health information seeking and the Patient-Physician relationship: a systematic review. J Med Internet Res. 2017;19(1):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thulesius H. Increased importance of digital medicine and eHealth during the covid-19 pandemic. Scand J Prim Health Care. 2020;38(2):105–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaw T, McGregor D, Brunner M, et al. . What is eHealth (6)? development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19(10):e324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boers SN, Jongsma KR, Lucivero F, et al. . SERIES: eHealth in primary care. Part 2: exploring the ethical implications of its application in primary care practice. Eur J Gen Pract. 2020;26(1):26–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Houwink EJF, Kasteleyn MJ, Alpay L, et al. . SERIES: eHealth in primary care. Part 3: eHealth education in primary care. Eur J Gen Pract. 2020;26(1):108–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Versluis A, Van Luenen S, Meijer E, et al. SERIES: eHealth in Primary care. Part 4: addressing the challenges of implementation. Submitted to Eur J Gen Pract. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Villumsen S, Adler-Milstein J, Nøhr C.. National monitoring and evaluation of eHealth: a scoping review. JAMIA Open. 2020;3(1):132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Danish Ministery of Health, Danish Minestery of Finance, Danish Regions, et al. A coherent and trustworthy health network for all – digital health strategy 2018-2022 Odense (Denmark); 2018. [cited 2021 July 12]. Available from: https://sundhedsdatastyrelsen.dk/da/diverse/download.
- 12.The Medical Futurist. National digital health strategies around the world: the medical futurist ; 2018. [cited 2021 July 12]. Available from: https://medicalfuturist.com/national-digital-health-strategies-around-the-world/?utm_source=The%20Medical%20Futurist%20Newsletter&utm_campaign=39368b494f-EMAIL_CAMPAIGN_2018_10_09_COPY_01&utm_medium=email&utm_term=0_efd6a3cd08-39368b494f-420590025.
- 13.HealthOne . HealthOne: share knowledge – better, safer care New Zealand. [cited 2021 July 12]. Available from: https://healthone.org.nz/.
- 14.Peeters JM, Krijgsman JW, Brabers AE, et al. . Use and uptake of eHealth in general practice: a cross-sectional survey and focus group study among health care users and general practitioners. JMIR Med Inform. 2016;4(2):e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin A, Sattler A, Smith M.. Retooling primary care in the COVID-19 era. Mayo Clin Proc. 2020;95(9):1831–1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rogers EM, Schoemaker FF.. Communication of innovations: a cross-cultural approach. 2nd ed. New York: Free Press; 1971. [Google Scholar]
- 17.de Wilt T, Versluis A, Goedhart A, et al. . General practitioners attitude towards the use of eHealth and online testing in primary care. Clinical eHealth. 2020;3:16–22. [Google Scholar]
- 18.Wouters M, Huygens M, Voogdt H, et al. Let's work together – eHealth monitor 2019 [Samen aan zet – eHealth-monitor 2019] Den Haag and Utrecht: Nictiz and NIVEL; 2019. [cited 2021 July 12]. Available from: https://www.nictiz.nl/programmas/e-health-monitor/e-health-monitor-2019/.
- 19.Odendaal WA, Anstey Watkins J, Leon N, et al. . Health workers' perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;3:CD011942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ross J, Stevenson F, Lau R, et al. . Factors that influence the implementation of e-health: a systematic review of systematic reviews (an update). Implement Sci. 2016;11(1):146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reiners F, Sturm J, Bouw LJW, et al. . Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int J Environ Res Public Health. 2019;16(4):645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iverson SA, Howard KB, Penney BK.. Impact of internet use on health-related behaviors and the patient-physician relationship: a survey-based study and review. J Am Osteopath Assoc. 2008;108(12):699–711. [PubMed] [Google Scholar]
- 23.Black AD, Car J, Pagliari C, et al. . The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med. 2011;8(1):e1000387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Greenhalgh T, Wherton J, Papoutsi C, et al. . Beyond adoption: a new framework for theorizing and evaluating nonadoption, abandonment, and challenges to the Scale-Up, spread, and sustainability of health and care technologies. J Med Internet Res. 2017;19(11):e367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scott RE, Mars M.. Principles and framework for eHealth strategy development. J Med Internet Res. 2013;15(7):e155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marcolino MS, Oliveira JAQ, D'Agostino M, et al. . The impact of mHealth interventions: Systematic review of systematic reviews. JMIR Mhealth Uhealth. 2018;6(1):e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sanyal C, Stolee P, Juzwishin D, et al. . Economic evaluations of eHealth technologies: a systematic review. PLoS One. 2018;13(6):e0198112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Olff M. Mobile mental health: a challenging research agenda. Eur J Psychotraumatol. 2015;6:27882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Spoelman WA, Bonten TN, de Waal MW, et al. . Effect of an evidence-based website on healthcare usage: an interrupted time-series study. BMJ Open. 2016;6(11):e013166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brandt CJ, Sogaard GI, Clemensen J, et al. . Determinants of successful eHealth coaching for consumer lifestyle changes: qualitative interview study among health care professionals. J Med Internet Res. 2018;20(7):e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hagatun S, Vedaa O, Harvey AG, et al. . Internet-delivered cognitive-behavioral therapy for insomnia and comorbid symptoms. Internet Interv. 2018;12:11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haste A, Adamson AJ, McColl E, et al. . Web-based weight loss intervention for men with type 2 diabetes: pilot randomized controlled trial. JMIR Diabetes. 2017;2(2):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Komkova A, Brandt CJ, Hansen Pedersen D, et al. . Electronic health lifestyle coaching among diabetes patients in a real-life municipality setting: observational study. JMIR Diabetes. 2019;4(1):e12140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ritterband LM, Thorndike FP, Ingersoll KS, et al. . Effect of a web-based cognitive behavior therapy for insomnia intervention with 1-year follow-up: a randomized clinical trial. JAMA Psychiatry. 2017;74(1):68–75. [DOI] [PubMed] [Google Scholar]
- 35.Freeman K, Dinnes J, Chuchu N, et al. . Algorithm based smartphone apps to assess risk of skin cancer in adults: systematic review of diagnostic accuracy studies. Br Med J. 2020;368:m127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Udrea A, Mitra GD, Costea D, et al. . Accuracy of a smartphone application for triage of skin lesions based on machine learning algorithms. J Eur Acad Dermatol Venereol. 2020;34(3):648–655. [DOI] [PubMed] [Google Scholar]
- 37.Springvloed L, Bos N, de Jong J, et al. . Thuisarts.nl – How does thuisarts.nl contribute to transparency and the best suitable care? [thuisarts.nl – Hoe draagt thuisarts.nl bij aan transparantie en de best passende zorg?]. Utrecht: NIVEL; 2019. [cited 2021 Jul 12]. Available from: https://www.nivel.nl/sites/default/files/bestanden/6-Transparantiemonitor-2018-Thuisartsnl.pdf [Google Scholar]
- 38.Johansen MY, MacDonald CS, Hansen KB, et al. . Effect of an intensive lifestyle intervention on glycemic control in patients with type 2 diabetes: a randomized clinical trial. JAMA. 2017;318(7):637–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogeil RP, Chakraborty SP, Young AC, et al. . Clinician and patient barriers to the recognition of insomnia in family practice: a narrative summary of reported literature analysed using the theoretical domains framework. BMC Fam Pract. 2020;21(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van der Zweerde T, Lancee J, Ida Luik A, et al. . Internet-Delivered cognitive behavioral therapy for insomnia: tailoring cognitive behavioral therapy for insomnia for patients with chronic insomnia. Sleep Med Clin. 2019;14(3):301–315. [DOI] [PubMed] [Google Scholar]
- 41.Archer D. SHUTi: a new insomnia treatment via the internet. 2017. [cited 2021 July 12]. Available from: https://www.psychologytoday.com/us/blog/reading-between-the-headlines/201702/shuti-new-insomnia-treatment-the-internet.
- 42.Christensen H, Batterham PJ, Gosling JA, et al. . Effectiveness of an online insomnia program (SHUTi) for prevention of depressive episodes (the GoodNight study): a randomised controlled trial. Lancet Psychiatry. 2016;3(4):333–341. [DOI] [PubMed] [Google Scholar]
- 43.Zachariae R, Lyby MS, Ritterband LM, et al. . Efficacy of internet-delivered cognitive-behavioral therapy for insomnia – a systematic review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2016;30:1–10. [DOI] [PubMed] [Google Scholar]
- 44.Grandner MA, Chakravorty S.. Insomnia in primary care: misreported, mishandled, and just plain missed. J Clin Sleep Med. 2017;13(8):937–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baglioni C, Altena E, Bjorvatn B, et al. . The European academy for cognitive behavioural therapy for insomnia: an initiative of the European insomnia network to promote implementation and dissemination of treatment. J Sleep Res. 2020;29(2):e12967. [DOI] [PubMed] [Google Scholar]
- 46.Fraser H, Coiera E, Wong D.. Safety of patient-facing digital symptom checkers. Lancet. 2018;392(10161):2263–2264. [DOI] [PubMed] [Google Scholar]
- 47.Inspectie Gezondheidszorg en Jeugd . Report of the inspection research of SkinVision in the period from January 2019 to December 2019 [Rapport van het inspectieonderzoek van SkinVision in de periode van januari 2019 tot december 2019] Utrecht: Inspectie Gezondheidszorg en Jeugd; 2020. [cited 2021 July 12]. Available from: https://www.toezichtdocumenten.igj.nl/.