Abstract
Chronic obstructive pulmonary disease (COPD) is an inflammatory lung disease characterized by chronic airway obstruction and emphysema. Accumulating studies have shown that the onset and development of COPD are related to an aberrant immune response induced by the dysregulation of a number of genetic and environmental factors, while the exact pathogenesis of this disease is not well defined. Emerging studies based on tests on samples from COPD patients, animal models, pharmacological and genetic data suggest that the NLR family pyrin domain containing 3 (NLRP3) inflammasome activation is required in the lung inflammatory responses in the development of COPD. Although the available clinical studies targeting the inflammasome effector cytokine, IL-1β, or IL-1 signaling do not show positive outcomes for COPD treatment, many alternative strategies have been proposed by recent emerging studies. Here, we highlight the recent progress in our understanding of the role of the NLRP3 inflammasome in COPD and propose possible future studies that may further elucidate the roles of the inflammasome in the pathogenesis or the intervention of this inflammatory lung disease.
Keywords: inflammasome, NLRP3, IL-1, COPD, inflammation, lung
Introduction
Chronic Obstructive Pulmonary Disease (COPD)
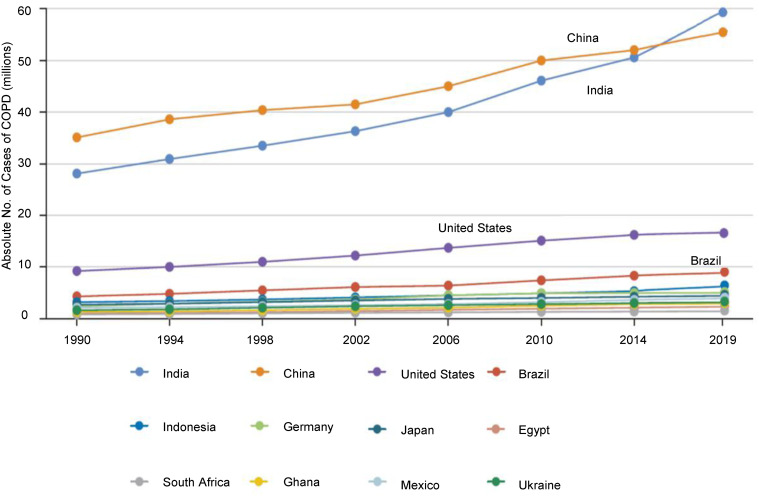
COPD is a type of obstructive lung disease equally affecting males and females, it is considered to be the fourth leading cause of death globally.1 Common COPD features include chronic airway obstruction, emphysema, chronic bronchitis, airway remodeling, and decreased lung function.1 COPD patients usually manifest long-term breathing problems, including shortness of breath and cough with sputum. With the progression of the disease, patients may display other symptoms such as physical activity limitations. According to a study in 2016,2 COPD affects nearly 2.4% of the population globally and annually causes more than 3 million deaths. COPD is a substantial problem everywhere, China and India account for more than 50% of all cases of COPD in the world (Figure 1). Although COPD-associated symptoms can be ameliorated by reducing smoking rates, improving the air quality, and usage of medicine such as inhaled corticosteroids, a treatment with enough efficacy to prevent disease progression or exacerbation is still lacking.3 Due to the higher smoking rates and aging of population, its prevalence and number of deaths are still increasing.4,5
Figure 1.
Prevalence of chronic obstructive pulmonary disease (COPD) in selected countries, 1990–2019. Data are from the Global Burden of Disease. Prevalence of chronic obstructive pulmonary disease (COPD). Available from: http://ghdx.healthdata.org/search/site/COPD.97
The most common cause of COPD is smoking,6 while other factors can also contribute to the onset of this disease, mainly including secondhand smoke, pollution and fumes, age, infections, occupational dusts/chemicals, untreated asthma and genetic factors such as deficiency of alpha-1 antitrypsin.7 The possible pathogenesis of COPD is strongly linked to chronic inflammatory responses due to the activation of many cell types such as myeloid cells and epithelial cells in response to possible irritants (such as those released from tobacco or polluted air) in the lung of genetically susceptible individuals.
Recently, Hobbs et al8 identified 22 genetic loci associated with COPD in a large cohort. Among them, 13 represented new associations with COPD, of which 9 (HHIP, CHRNA5, HTR4, FAM13A, RIN3, TGFB2, GSTCD-NPNT, CYP2A6 and IL27-CCDC101) of these 13 loci had previously been associated with measures of lung function in the general population and the remaining 4 (EEFSEC, DSP, MTCL1 and SFTPD) represented new associations with both COPD and lung function, indicating that individual genetic variation explains a small fraction of COPD susceptibility.
The activated immune cells produce pro-inflammatory cytokines, ROS, and tissue degrading proteases, which further expand the inflammation and cause tissue damage. In this process, lung epithelial cells may produce TGF-β and thus participate in fibrotic tissue remodeling. Thus, the development of COPD is a complex process that involves inflammation, aberrant activation of proteases, and uncontrolled oxidative stress.
Animal Models of COPD
Various animal models have been developed to recapitulate the hallmark features of COPD and study the molecular and cellular processes during the development of the disease. Despite the establishment of models in many species, such as rodents, dogs, guinea-pigs, monkeys and sheep, the mouse COPD model provides the greatest ability in investigating disease pathogenesis due to the advances in mouse study, such as the availability of genetically engineered/inbred strains and abundant antibodies, and the shared basic physiological processes between mouse and human.
Elastase Induced COPD Model
Previous studies have provided evidence that administration of particular proteases or chemicals can induce inflammatory responses and tissue damage in the lung, features that partially resemble COPD. Delivery of elastase (single dose oropharengeally or four times intratracheally) to the lung induces inflammatory cell infiltration and pulmonary emphysema in mice within four weeks.9,10
LPS Induced COPD Model
LPS is an endotoxin derived from gram-negative bacteria that induces production of pro-inflammatory mediators and infiltration of immune cells such as macrophages and neutrophils. This model can be induced by intranasal administration of LPS of many species such as mice and rats, which causes tissue damage and lung dysfunction associated with accumulation of white blood cells such as neutrophils in BALF, increase in pro-inflammatory cytokines and chemokines.11,12 Moreover, LPS can be used together with elastase to induce more severe lung inflammatory disease, a condition similar to COPD exacerbation.13
Ozone Induced COPD Model
Ozone is a gaseous constituent of urban air pollution generated from interaction of air pollutants such as organic compounds and nitrogen oxide. Accumulating evidence has shown that ozone plays a detrimental role in respiratory health. Ozone exerts its effects by coming into contact with cellular membranes of alveolar epithelial cells or airway macrophages, thus generating bioactive mediators, which cause oxidative stress and also affect innate immune responses.14 Ozone can also affect macrophage phagocytosis of apoptotic cells15 and cytokine production of alveolar epithelial cells,16 causing prolonged tissue damage in the lung. Long-term exposure to ozone may increase the risk of lung function reduction, emphysema development, and hospital admission in COPD patients.17,18
In animal models, acute exposure to ozone causes hyperreactivity in the airway and neutrophilic inflammation, while chronic ozone exposure induces bronchial inflammation with emphysema, a symptom that is close to that seen in COPD. For instance, in a study by Russell et al,19 the researchers showed that exposure to 3ppm of ozone for 3 hours (twice a week for 6 weeks) induced impaired lung function and airway hyperresponsiveness in male C57BL/6 mice. Moreover, ozone-treated mice manifested increased inflammatory cells such as neutrophils, macrophages, and lymphocytes, as well as pro-inflammatory cytokines such as KC, GM-CSF, TNF-α, and MIF in BAL. These changes are sensitive to ISO-1 but not dexamethasone.
Cigarette Smoking (CS) Induced COPD Model
Cigarettes contain abundant free radicals, which increase oxidative stress and cause tissue damage in the lungs. Two systems are used in inducing COPD mouse model by CS: the nose-only exposure system and the whole-body exposure system, both have been widely used to study the pathogenesis of COPD. Both systems induce pathological features of COPD, while according to Wright et al’s study,20 the nose-only system may induce more pronounced pathological changes in the lung. Another critical factor that may affect the pathological features is the exposure duration of CS. Previous studies have shown that acute exposure to CS (1 hour to 4 weeks) induces inflammatory responses in the lung,21 while the mice do not display emphysema or decreased lung function. In contrast, chronic exposure to CS (over 6 months) leads to emphysema, airway remodeling, and mild reduction of lung function. However, the long exposure time of CS restricts the use of this model. Thus, a CS model with better pathological features of COPD and shorter duration will largely facilitate the mechanistic studies of COPD associated biological processes and drug screening for therapeutic applications.
The NLRP3 Inflammasome and Its Activating Mechanisms
The NLR family pyrin domain containing 3 (NLRP3) inflammasome is a concept that describes a large molecular protein complex that acts as a platform for the maturation of pro-inflammatory cytokines, IL-1β and IL-18.22 NLRP3 is an intracellular receptor that can assemble in response to a wide variety of stimuli, such as pathogen associated molecular patterns (PAMPs) derived from invading pathogens and danger associated molecular patterns (DAMPs) released from dying cells. NLRP3 belongs to the NOD like receptor family, it contains three domains: a C-terminal leucine-rich repeat domain (LRR), a central nucleotide binding domain (NACHT) and an N-terminal pyrin domain (PYD). By sensing a PAMP or a DAMP via its LRR domain, NLRP3 NACHT domain can undergo oligomerization, then its PYD domain can bind with PYD domain of the adaptor protein ASC. Subsequently, the CARD domain of ASC recruits and binds to CARD domain of pro-caspase-1 to allow its autoactivation and cleavage. The released active form of caspase-1 cleaves pro-IL-1β and pro-IL-18 to release the mature form of these cytokines, which mediate pro-inflammatory responses in the host. The activated caspase-1 can also cleave gasdermin D to release its N terminus, which mediates a type of programmed cell death, pyroptosis.23
Mounting evidence has shown that the NLRP3 inflammasome is involved in the regulation of many physiological and pathological processes, such as infections, tissue repair, autoimmune diseases, and cancers.24 A line of recent studies has implicated the NLRP3 inflammasome in the onset and the development of COPD. Here, we will discuss the main findings reported in recent literature regarding the expression and activation of the NLRP3 inflammasome related genes in the lung tissue of both patients and animal models of COPD, the impact of NLRP3 inflammasome regulation on activity of COPD, and will propose a model with which the NLRP3 inflammasome regulates the development of COPD based on our understanding. On this basis, we provide our opinions of possible future studies that may improve our understanding about the role and impact of NLRP3 and associated cytokines in the pathogenesis of COPD.
The Expression or Activation of the NLRP3 Inflammasome Related Genes in COPD
An mRNA-based study across murine tissues showed that NLRP3 is highly expressed in the lung. The primary source of NLRP3 in the lung is the alveolar myeloid cells such as alveolar macrophages and dendritic cells,25 while the lung epithelial cells also express NLRP3 and other inflammasome associated genes.26 In COPD patients, NLRP3 is over-expressed in the lung and its expression correlates with airflow obstruction.27 In an in vitro model, Nachmias et al28 showed that the expression and activation of NLRP3 can be induced by CS extract in A549 alveolar epithelial cells. Wang et al29 evaluated the possible correlation between NLRP3 inflammasome activation and risk of acute exacerbation of COPD (AECOPD). They found that the expression levels of NLRP3 inflammasome components in peripheral blood mononuclear cells (PBMCs) and bronchial tissues from patients with AECOPD were significantly higher than those in smokers without lung diseases. Moreover, the expression of NLRP3 inflammasome associated molecules was correlated with disease activity and the common pathogen load in the lung. Thus, the systemic and local airway activity of the NLRP3 inflammasome is associated with acute exacerbation of COPD. However, these data do not distinguish whether the high activity of NLRP3 inflammasome is the cause or the result of the disease.
As a hallmark cytokine of NLRP3 inflammasome activation, IL-1β has been implicated in the pathogenesis of COPD by a number of studies. For instance, the level of IL-1β is increased in sputum and serum of COPD patients, the serum level of IL-1β correlates with disease symptoms and disease severity.30,31 Moreover, Kuschner et al32 showed that tobacco smoking enhances concentration of IL-1β in the lung, while the study by Chung et al33 found that the level of IL-1β in the lung is increased in patients with COPD. These observations suggest the possible involvement of inflammasomes in development of COPD. To further prove the in vivo function of IL-1β in COPD, Lappalainen et al34 generated IL-1β transgenic mice, whose epithelial cells expressed human IL-1β under control of a doxycycline-inducible system. After induction of IL-1β, the mice manifested lung inflammation similar to that seen in COPD patients, IL-1β induced elevation of neutrophil attractant chemokines such as KC and MIP-2 and matrix metalloproteases such as MMP-9 and MMP-12, which may be associated with the enhanced infiltration of neutrophils, macrophages and lymphocytes in the lung. These data demonstrate that overexpression of IL-1β induces pulmonary inflammation. In support to this study, Doz et al35 showed that tobacco smoke-induced lung inflammation is reduced in IL-1R deficient mice. Thus, IL-1β and IL-1R signaling are important for development of lung inflammation. However, it should be noted that the role of IL-1β in COPD is challenged by data from a study by Botelho et al36 showing that it is IL-1α, but not IL-1β, that plays a major role in the pathogenesis of COPD. While another study by Pauwels et al37 showed that neutralization of both IL-1α and IL-1β attenuated tobacco smoke-induced lung inflammation. Thus, the relative contribution of IL-1α and IL-1β needs to be further investigated in future.
IL-18 is also a hallmark cytokine that is regulated by the NLRP3 inflammasome. The level of IL-18 is elevated in blood and lungs of COPD patients,38,39 its level shows negative correlation with lung function of COPD patients, indicating a role of IL-18 in the pathogenesis of this disease. In support of these data, transgenic mice with overexpression of IL-18 manifested COPD-like symptoms,40 while in CS-induced COPD model, IL-18R deficiency ameliorated the disease severity.38 All these studies demonstrate that IL-18 contributes to the development of lung inflammation in COPD.
ASC participates in the assembly of the NLRP3 inflammasome by connecting NLRP3 and pro-caspase-1, thus the activation of the inflammasome allows ASC to form a disc-like structure, called “ASC speck”, which is considered to be a hallmark of NLRP3 inflammasome formation. Using CS-induced COPD model, Franklin et al41 found that “ASC speck” can be highly released in BALF of the lung and amplifies inflammatory response. The activation of caspase-1 has also been found to be elevated in the lungs of smokers;42 inhibition of caspase-1 prevents lung inflammation in CS-induced emphysema model.43 Thus, caspase-1 activation promotes lung inflammation.
Factors That May Affect COPD via Activating the NLRP3 Inflammasome
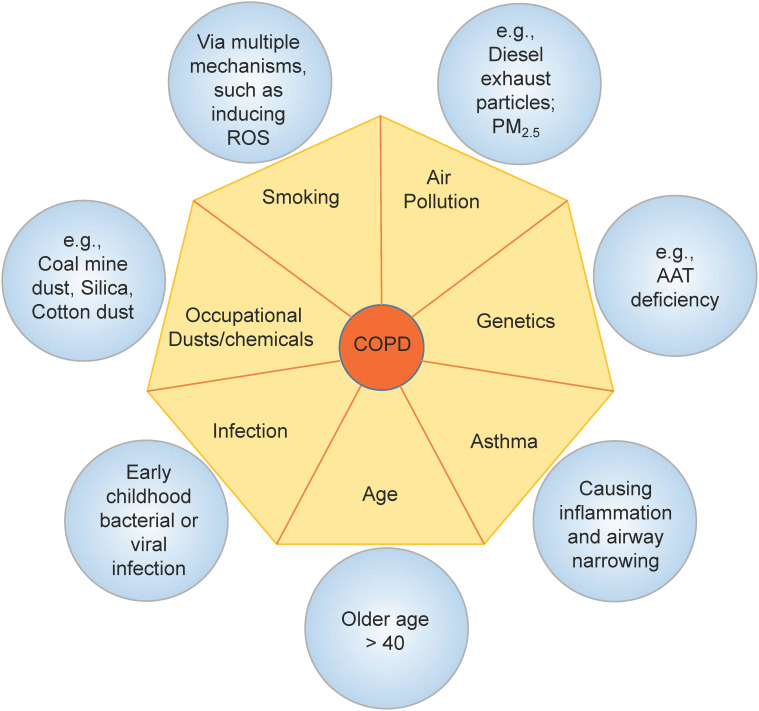
Studies have provided evidence that many factors increase the risk for developing COPD. As discussed previously, CS is the main cause of COPD, while other factors such as air pollution, occupational dusts and chemicals, age, infection, and genetic deficiency may also contribute to the pathogenesis of COPD. Among these factors, some can activate the NLRP3 inflammasome and thus may affect the development or exacerbation of COPD via regulation of the activity of the inflammasome (Figure 2).
Figure 2.
Risk factors of COPD may activate the NLRP3 inflammasome. The onset of progression of COPD can be affected by a number of factors. CS is the most common risk factor of COPD by multiple mechanisms such as generating free radicals and causing oxidative stress. Air pollutants induce production of ROS or release of cathepsins. These factors and genetic deficiency of AAT all contribute to the activation of the NLRP3 inflammasome in the lungs, which enhances the progression of COPD. Childhood lung infection and asthma may cause chronic inflammation in the lungs, which increases the risk of developing COPD.
CS
As the most common risk factor for COPD, CS can affect the activation of the NLRP3 inflammasome in various ways, it affects both priming and activating signals of the NLRP3 inflammasome. For instance, CS exposure induces release of HMGB1,44 a danger signal that activates TLR signaling and thus triggers the priming signal of inflammasome activation. CS also causes an increase of extracellular ATP (eATP), in the lungs of both COPD patients and mouse model, eATP and its receptor P2X7 have been implicated in the pathogenesis of inflammatory lung disease,45 deficiency of P2X7 attenuates CS induced neutrophilia in mice.42 Since eATP activates the NLRP3 inflammasome in many cell types, promoting eATP release might be a critical way of CS mediating the development of COPD.
Oxidative stress is a critical characteristic of COPD, it is also a key mechanism that induces lung pathology in COPD.46 Cigarettes contain abundant free radicals, including reactive oxygen species (ROS) and reactive nitrogen species (RNS), which cause tissue damage of the lung.47 Meanwhile, it has been shown that ROS is an upstream activator of the NLRP3 inflammasome.48 Thus, CS-induced ROS production may activate the NLRP3 and contribute to lung inflammatory responses in COPD patients.
In addition, COPD patients display enhanced uric acid level in both plasma and the lungs.49 Thus, uric acid may work as a predictor of COPD risk in smokers. The high level of uric acid may lead to formation of uric acid crystals, an important activator of the NLRP3 inflammasome.50,51 These findings suggest that the NLRP3 inflammasome activation induced by uric acid crystals may contribute to the development of lung pathogens in COPD patients.52
Air Pollution
Air pollution is a critical risk factor for COPD. Many different types of air pollutants such as gases, particulates, and biological molecules have been found to enhance the risk of COPD via regulating the NLRP3 inflammasome. For instance, diesel exhaust particles (DEP) are a critical component of air pollution. Uh et al’s study53 showed that DEP activate the NLRP3 inflammasome in lung tissues of mice in elastase-induced emphysema model, a process that can be inhibited by antioxidant, N-acetylcysteine. Thus, DEP may enhance the risk of COPD or other lung diseases via regulating the NLRP3 inflammasome.
Ambient fine particulate matter 2.5 (PM2.5) is another air pollution component, recent epidemiological studies provided evidence that PM2.5 enhances morbidity and mortality in COPD.54 Long-term exposure to PM2.5 exacerbates CS-induced pathology in COPD.54 Zheng et al55 performed a study to evaluate the role of PM2.5 in NLRP3 inflammasome activation and lung fibrosis, they showed that PM2.5 activates the NLRP3 inflammasome. Regarding the mechanisms involved, they showed that cathepsin B release, ROS production, and potassium efflux are required processes. Therefore, the role of PM2.5 in elevating the risk of COPD requires the activation of the NLRP3 inflammasome.
Moreover, many other common air pollutants such as ground-level ozone56 and biomass fuel smoke57 also activate the NLRP3 inflammasome and enhance risk of COPD, while whether the inflammasome activation plays a major role in COPD-like symptoms associated with these factors, still awaits further investigation. In addition, it should be noted that the air pollutant sulfur dioxide can induce COPD-like symptoms in rats,58 while this effect is not achieved by activating the NLRP3 inflammasome, since in a study conducted by Yang et al,59 the researchers showed that sulfur dioxide inhibits the activity of the NLRP3 inflammasome. Although the effect of sulfur dioxide in development of COPD and the role of NLRP3 inflammasome in sulfur dioxide induced lung pathology need to be further determined, these findings indicate a complex regulation of the NLRP3 inflammasome in the pathogenesis of COPD.
Occupational Dusts and Chemicals
Occupational dusts are the fine particles mainly generated in agriculture, forestry, and mining. Exposure to some of those dusts can increase the risk of COPD. A good example is the silica dust (also known as quartz dust) released during the processing of materials containing crystalline silica particles. It is an important occupational respiratory toxin, exposure to silica dust increases the risk of COPD.60 The inhalation of silica dust may lead to the release of crystalline silica in the lung, which is a critical activator of the NLRP3 inflammasome.61,62 Silica also enhances plasma levels of IL-18 and IL-1Ra,63 which may contribute to the lung pathology induced by silica dust. However, whether the NLRP3 inflammasome activation induced by crystalline silica plays a major role in development of COPD, needs to be determined.
Many other occupational dusts such as wood dust have been implicated in the pathogenesis of COPD. A number of studies showed that exposure to wood dust is associated with decreased lung function.64,65 Whether these dusts affect the host’s susceptibility to COPD via regulating the NLRP3 inflammasome, needs to be investigated.
Bacterial and Viral Infection
The lungs of COPD patients are more likely to be infected by bacteria or viruses, which induce increased inflammation and worse symptoms, clinically termed exacerbation of COPD.66 An example is the infection of Mycobacterium tuberculosis, a bacterium that causes tuberculosis. M. tuberculosis can affect the progression of COPD by inducing the production of matrix metalloproteinases (MMPs) via its cell wall component, lipoarabinomannan.67 MMPs then combine with other factors such as the activation of neutrophils and induce structural changes seen in COPD. Moreover, M. tuberculosis may activate the NLRP3 inflammasome and enhance the production of IL-1β and IL-18 in alveolar macrophages,68 the latter then contribute to COPD progression or exacerbation by amplifying the inflammatory responses in the lung.
In an in vitro COPD exacerbation model, Nachmias et al28 found that LPS stimulation enhances the production of pro-inflammatory cytokines, IL-8 and MCP-1, by the alveolar epithelial cell line A549 in response to the stimulation of CS extract. The combined stimulation with CS extract and LPS induces higher NLRP3 inflammasome activity and enhanced IL-1β production by A549 cells. These data demonstrate that bacterial infection derived LPS may exacerbate the inflammatory responses in COPD patients.
Viral infection may also contribute to the exacerbation of COPD. Viruses can be found in half of samples from patients with COPD exacerbations, their infection is associated with poorer clinical outcomes. Studies have shown that persistent infection with viruses such as human rhinovirus, respiratory syncytial virus, and influenza may contribute to COPD exacerbation by activating the NLRP3 inflammasome,69–71 while the exact impact of virus-inflammasome interplay on lung inflammation has not been clearly defined.
Thus, the available evidence demonstrates that both bacterial and viral infection may play a significant role in both progression and acute exacerbations of COPD by regulating the activation of the NLRP3 inflammasome. Future studies investigating the role of NLRP3 in bacteria or virus infection during COPD progression and its exacerbation may contribute to the disease therapy via regulating the activity of the NLRP3 inflammasome.
Genetic Factor
CS is the major risk factor for COPD, while this disease is only developed in a minority of smokers, this fact together with studies in families and twins suggest that genetic factors also contribute to COPD progression.72 The available studies have shown that numerous genes, such as α1-antitrypsin and vitamin D-binding protein, are associated with development of COPD, their contributions to the development and progression of COPD have been described elsewhere.73 Of note, some of these genes may affect the progression of COPD via regulating the activation of the NLRP3 inflammasome. For instance, in a study conducted by Ebrahimi et al,74 the researchers found that α1-antitrypsin inhibits NLRP3 inflammasome activation in murine astrocytes, while whether a similar regulation can be observed in the lung, such as alveolar macrophages, needs further studies. Investigating the possible role of other genetic factors affecting risk of COPD in NLRP3 inflammasome activation may improve our understanding about the complex regulating network in the pathogenesis of COPD.
The NLRP3 Inflammasome in Animal Models of COPD
Couillin et al75 showed that elastase-treated mice displayed tissue destruction with emphysema and fibrosis, which is associated with an increased production of pro-inflammatory mediators including IL-1β and neutrophil infiltration in the lung. Deficiency of NLRP3 inflammasome adaptor protein, ASC, or IL-1R blockade ameliorated emphysema and inflammation in the mice. These findings suggest an involvement of NLRP3 inflammasome and IL-1 signaling in pathogenesis of elastase-induced lung inflammation.
A study by Wang et al76 evaluated the role of NLRP3 inflammasome in lung inflammation using an LPS-induced model, and they showed that MCC950, an NLRP3 inhibitor, efficiently reduced LPS-induced lung inflammation. Furthermore, LPS-induced lung inflammation can be ameliorated by administration of corticosteroids, which inhibits the activation of NF-kB signaling pathway,77 a priming signal for the activation of the NLRP3 inflammasome.22
This study suggests that the NLRP3 inflammasome may be involved in the pathogenesis of COPD, particularly those related to infection.
Ozone exposure may affect the activation of the NLRP3 inflammasome by regulating both the priming and activating steps. It has been shown that ozone modulates HSP70 activity and thus regulates TLR4 signaling,78 which acts as a priming signal to induce the transcription of NLRP3. The production of ROS induced by exposure to ozone in the lung can work as an upstream activating signal for the assembly of NLRP3 inflammasome. Additionally, exposure to ozone induces an increased expression of hypoxia inducible factor-1α (HIF-1α) target genes such as histone deacetylase 2 (HDAC2)79 and a decrease in expression and activity of the antioxidant gene nuclear erythroid-related factor 2 (Nrf2),80 both genes have been implicated in the regulation of the NLRP3 inflammasome. Indeed, ozone-treated mice show enhanced NLRP3 inflammasome activation, increased caspase-1 activity, and increased pro-inflammatory cytokine production including IL-1β.81,82 Inhibition of mitochondrial ROS or caspase-1 activity ameliorates ozone-induced lung inflammation,82 while whether deficiency of NLRP3 or related cytokines impair ozone-induced lung pathology is still not clear, genetic evidence is needed to figure out the exact role of NLRP3 in ozone-induced model of lung inflammation.
A study by Beckett et al83 reported a short-term COPD model induced by delivering CS into the nares of BALB/c mice for 1–12 weeks. Eight weeks’ exposure to CS induced airway remodeling with increased numbers of mucus-secreting goblet cells, alveolar enlargement, thickening of the airway epithelium, and decreased lung function in mice. Moreover, the pathology in mice showed glucocorticoid-resistant feature was macrophage dependent with an increased production of pro-inflammatory mediators such as TNF-α, IL-1β, and CXCL1. Enhanced level of IL-1β suggests a possible involvement of inflammasomes in the pathology of this model.
Yang et al84 studied the role of NLRP3 inflammasome in pathogenesis of COPD, using a COPD mouse model induced by tobacco inhalation, the authors showed that NLRP3 deficient mice manifested reduced disease severity and deceased IL-1 and IL-18 production in bronchoalveolar lavage fluid (BALF). These data suggest that NLRP3 is essential in development of COPD. However, in a study reported by Pauwels et al, they showed that NLRP3 and caspase-1 are not important in developing lung inflammation in mice induced by CS.37 Further studies are needed to clarify the exact contribution of NLRP3 and associated cytokines in the pathogenesis of COPD.
Polymorphisms in the NLRP3 Inflammasome Related Genes Confer Risk of COPD
Single nucleotide polymorphism (SNP) is a term to describe a single nucleotide in genomic DNA sequence which differs between members of a species or different chromosomes in an individual. It has been shown that some SNPs affect gene expression or function and are responsible for many processes such as disease susceptibility, medicinal drug responses, and genome evolution. In studies of COPD, many SNPs that have an impact on disease susceptibility have been identified,85 these SNPs may affect COPD via altering the activity of genes in inflammatory pathways and protease-antiprotease pathways. A number of recent studies identified SNPs in inflammasome-related genes, which may contribute to development of COPD. No SNP that can affect the susceptibility to COPD has been reported in human NLRP3, PYCARD (encoding ASC), and CASP1 to date, while in genes encoding the hallmark cytokines, IL1B and IL18, a number of SNPs have been identified that increase or decrease the risk of developing COPD.
IL1B gene polymorphisms have been implicated in risk of COPD, while the results from different studies are controversial. For instance, Baykara et al’s study86 showed no association between COPD and IL1B −511 and +3954 gene polymorphisms in a Turkish population. In agreement with this study, Ishii et al87 also found that polymorphisms in IL1B and IL1RN do not have a significant link to susceptibility to COPD. A meta-analysis by Xie et al88 showed that the IL1B (+3954) polymorphism does not confer risk of COPD, while the polymorphisms of the IL1B (−511, −31) and IL1RN (VNTR) enhanced the risk of developing COPD in East Asians. In another study of meta-analysis, Wang et al89 reported that the polymorphism in IL1B promoter (−511C/T) protects the host from COPD in Asian population. Shukla et al90 found that IL1RN*2/IL1RN*2 is a protective genotype for COPD in males, while the genotype seems to be a risk factor for COPD in females. They also showed that IL1B polymorphism T (−511) C does not affect host susceptibility to COPD. Lee et al’s study91 investigated the impact of SNPs in IL1B and IL1RN on the risk of COPD in a Korean population, they found that IL1B polymorphisms, −511C–>T and −31T–>C, enhanced the risk of COPD. Individuals carrying at least one IL1RN*2 allele are at lower risk of COPD. A polymorphism in IL18 was also found to have impact on susceptibility to COPD. Wang et al92 reported that an SNP in IL18 promoter (−607 C/A) enhanced the risk to develop COPD, while the other SNP −137 G/C did not show different frequency between COPD patients and healthy controls.
Thus, the impact of polymorphisms on disease risk may be affected by genetic background in different ethnic groups. However, functional studies of the impact of SNPs in IL1B and IL18 on COPD are still lacking. How they affect gene expression or inflammasome activity needs to be further investigated in the future.
Preventing COPD by Modulating the NLRP3 Inflammasome or Its Regulators
A number of recent studies have investigated the impact of preventing NLRP3 inflammasome or its effectors on COPD (summarized in Table 1). As mentioned previously, based on studies in animal models, IL-1β transgenic mice show increased COPD-like symptoms.34 IL-18 or IL-1R deficiency leads to decreased lung inflammation in CS-induced COPD model.35,38 Treatment with anakinra (IL-1 receptor antagonist) reduces lung inflammation induced by LPS.93 All these studies suggest a role of IL-1β, IL-18, and IL-1R signaling in the pathogenic progression of COPD. However, clinical trials employing an anti-human IL-1β monoclonal antibody (Canakinumab), a human IgG1 monoclonal antibody targeting IL-18 or a human IgG2 monoclonal antibody against IL-1R194 do not show significant difference for the outcomes between antibodies-treated and placebo-treated COPD patients. These results at least demonstrate that blockade of single inflammasome associated cytokine or IL-1R signaling does not protect patients from COPD. A joint blockade of IL-1β and IL-18, or IL-1α may be a possible way to prevent COPD in future clinical trials.
Table 1.
Potential Therapeutic Agents Targeting NLRP3 or Inflammasome Related Genes
| Agent | Target | Function | Effect | Clinical Trial or Disease Model | Reference |
|---|---|---|---|---|---|
| Anakinra | IL-1R | Blocking IL-1 signaling | Reduce lung inflammation | LPS-induced lung inflammation | [93] |
| Canakinumab | IL-1β | Blocking IL-1β signaling | No effect | Clinical trial (NCT00581945) | https://clinicaltrials.gov/ct2/show/NCT00581945 |
| MEDI2338 | IL-18 | Blocking IL-18 signaling | No effect | Clinical trial (NCT01322594) | https://clinicaltrials.gov/ct2/show/NCT01322594 |
| MEDI8968 | IL-1R1 | Blocking IL-1R signaling | No effect | Clinical trial (NCT01448850) | https://clinicaltrials.gov/ct2/show/NCT01448850 |
| MCC950 | NLRP3 | Blocking NLRP3 | Reduce lung inflammation | LPS-induced lung inflammation | [76] |
| VX-765 | Caspase-1 | Blocking caspase-1 | Reduce lung inflammation | Ozone-induced lung injury | [82] |
Moreover, based on studies by Yang et al and Xu et al,82,84 NLRP3 deficiency or caspase-1 inhibition causes a decrease of experimental COPD in mice, and the NLRP3 inhibitor, MCC950 has been demonstrated to prevent LPS-induced lung inflammation in mice.76 Therefore, it might be worthwhile to consider trials directly targeting NLRP3 or caspase-1, or GSDMD mediated pyroptosis for possible treatment of COPD.
In addition, these clinical trial studies may also suggest that other mechanisms upstream of the NLRP3 inflammasome may dominate the development of COPD. The activation of the NLRP3 inflammasome may be a secondary effect of these mechanisms. Thus, a combination strategy to block multiple molecules or signals might be required in treating COPD. For example, in a virus-induced COPD exacerbation model, Bucher et al95 showed that combined neutralization of IL-1α and IL-1β can more efficiently inhibit airway inflammation compared to individual blockade of two cytokines. In another study reported by Sichelstiel et al,96 the researchers found that blocking of IL-1β or IL-17A abrogates influenza-induced COPD exacerbation. Because of the redundancy of the two inflammatory pathways, the researchers pointed out that a combined blocking of the two cytokines might more efficiently inhibit inflammation and improve lung function.
Last but not least, COPD is a condition caused by a combination of a variety of genetic and environmental factors, the responses of patients to therapy might vary in individuals. Taking this into consideration, in future, clinical studies might improve the efficacy of the evaluation of new therapies targeting COPD.
Conclusion
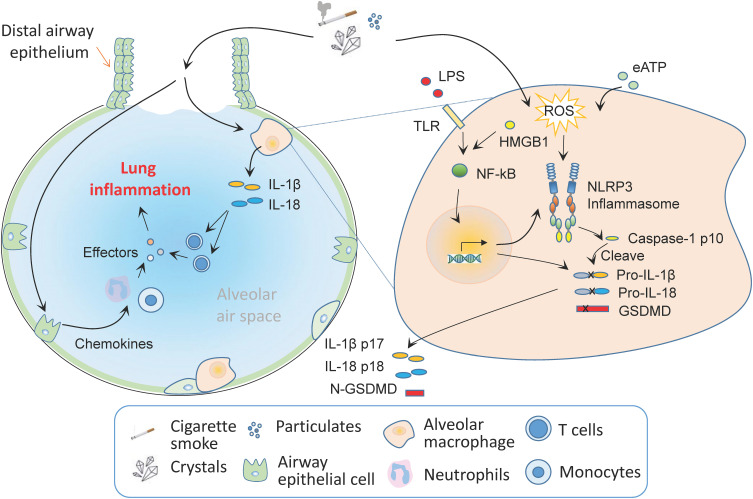
The available evidence has shown that the NLRP3 inflammasome has increased expression and activation in tissues of both COPD patients and animal models of COPD. A number of SNPs in IL-1β and IL-18 increase the risk to develop COPD. Transgene of IL-1β or IL-18 both increase lung inflammation in studies of animal models, while blocking these cytokines or IL-1R with monoclonal antibodies ameliorate lung pathologies. The exact contribution of NLRP3 inflammasome to the development of COPD is not well defined, although, based on current studies and our understanding, a possible model regarding the role of the NLRP3 inflammasome in the onset and progression of COPD may be as follows (Figure 3): COPD risk factors, such as CS or silica particulates activate the NLRP3 inflammasome in alveolar macrophages or dendritic cells, which drive the production of pro-inflammatory cytokines, IL-1β and IL-18, the latter then activate particular T cell subsets and promote lung inflammation. CS may promote the production of chemokines by airway epithelial cells, which mediate the recruitment of inflammatory cells such as neutrophils and monocytes to expand the inflammation. The effectors from these infiltrating cells such as elastase further promote inflammation and cause COPD-associated chronic tissue injury in the lungs.
Figure 3.
The role of the NLRP3 inflammasome in COPD. The exact contribution of NLRP3 inflammasome to the development of COPD is not well defined, while a variety of activators of the NLRP3 inflammasome enhance the susceptibility to the onset and progression of COPD. COPD risk factors, such as CS or silica particulates can activate the NLRP3 inflammasome in alveolar macrophages or dendritic cells, which mediates the release of pro-inflammatory cytokines, such as IL-1β and IL-18, the latter then activate particular T cell subsets and promote lung inflammation. CS may promote the production of chemokines by airway epithelial cells, which mediate the recruitment of neutrophils and monocytes. The effectors from these cells such as elastase promote lung inflammation and cause COPD-associated chronic lung injury.
Although the clinical trials testing blockade of IL-1β, IL-18 or IL-1R failed to inhibit lung pathologies in COPD patients, a number of alternative strategies such as targeting NLRP3, caspase-1 or GSDMD mediated pyroptosis, and combined blockade of multiple molecules associated with NLRP3 inflammasome or other pathways that contribute to the development of COPD are worthwhile for further investigation and trials for the control of COPD.
Funding Statement
This study was supported in part by the National Natural Science Foundation of China (32070919), Natural Science Foundation of Jiangsu Province (BK20201442), Natural Science Research Project of Jiangsu Provincial Department of Education (19KJB180021), Natural Science Foundation of Nantong University School of Medicine (TDYX2020015), and Start-up funds for young scientists of Nantong University (03083051).
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that no competing interest exists.
References
- 1.Barnes PJ. Cellular and molecular mechanisms of chronic obstructive pulmonary disease. Clin Chest Med. 2014;35:71–86. doi: 10.1016/j.ccm.2013.10.004 [DOI] [PubMed] [Google Scholar]
- 2.Disease GBD, Injury I, Prevalence C. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnes PJ. New anti-inflammatory targets for chronic obstructive pulmonary disease. Nat Rev Drug Discov. 2013;12:543–559. doi: 10.1038/nrd4025 [DOI] [PubMed] [Google Scholar]
- 4.Adhikari TB, Acharya P, Hogman M, et al. Prevalence of Chronic Obstructive Pulmonary Disease and its Associated Factors in Nepal: findings from a Community-based Household Survey. Int J Chron Obstruct Pulmon Dis. 2020;15:2319–2331. doi: 10.2147/COPD.S268110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xie M, Liu X, Cao X, Guo M, Li X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respir Res. 2020;21:49. doi: 10.1186/s12931-020-1291-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barnes PJ, Burney PG, Silverman EK, et al. Chronic obstructive pulmonary disease. Nat Rev Dis Primers. 2015;1:15076. doi: 10.1038/nrdp.2015.76 [DOI] [PubMed] [Google Scholar]
- 7.Brode SK, Ling SC, Chapman KR. Alpha-1 antitrypsin deficiency: a commonly overlooked cause of lung disease. CMAJ. 2012;184:1365–1371. doi: 10.1503/cmaj.111749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hobbs BD, de Jong K, Lamontagne M, et al. Genetic loci associated with chronic obstructive pulmonary disease overlap with loci for lung function and pulmonary fibrosis. Nat Genet. 2017;49:426–432. doi: 10.1038/ng.3752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Antunes MA, Rocco PR. Elastase-induced pulmonary emphysema: insights from experimental models. An Acad Bras Cienc. 2011;83:1385–1396. doi: 10.1590/S0001-37652011005000039 [DOI] [PubMed] [Google Scholar]
- 10.Suki B, Bartolak-Suki E, Rocco PRM. Elastase-Induced Lung Emphysema Models in Mice. Methods Mol Biol. 2017;1639:67–75. [DOI] [PubMed] [Google Scholar]
- 11.Wu W, Chen X, Liu X, Liu C, Lu G. Heliox-Driven Nebulization Has a Positive Effect on the Lung Function in Lipopolysaccharide-Induced Chronic Obstructive Pulmonary Disease Rat Model. Med Sci Monit. 2016;22:4100–4106. doi: 10.12659/MSM.896736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SY, Cho JH, Cho SS, Bae CS, Kim GY, Park DH. Establishment of a chronic obstructive pulmonary disease mouse model based on the elapsed time after LPS intranasal instillation. Lab Anim Res. 2018;34:1–10. doi: 10.5625/lar.2018.34.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kobayashi S, Fujinawa R, Ota F, et al. A single dose of lipopolysaccharide into mice with emphysema mimics human chronic obstructive pulmonary disease exacerbation as assessed by micro-computed tomography. Am J Respir Cell Mol Biol. 2013;49:971–977. doi: 10.1165/rcmb.2013-0074OC [DOI] [PubMed] [Google Scholar]
- 14.Mudway IS, Kelly FJ. Ozone and the lung: a sensitive issue. Mol Aspects Med. 2000;21:1–48. doi: 10.1016/S0098-2997(00)00003-0 [DOI] [PubMed] [Google Scholar]
- 15.Becker S, Madden MC, Newman SL, Devlin RB, Koren HS. Modulation of human alveolar macrophage properties by ozone exposure in vitro. Toxicol Appl Pharmacol. 1991;110:403–415. doi: 10.1016/0041-008X(91)90042-D [DOI] [PubMed] [Google Scholar]
- 16.Manzer R, Dinarello CA, McConville G, Mason RJ. Ozone exposure of macrophages induces an alveolar epithelial chemokine response through IL-1alpha. Am J Respir Cell Mol Biol. 2008;38:318–323. doi: 10.1165/rcmb.2007-0250OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Halonen JI, Lanki T, Yli-Tuomi T, Kulmala M, Tiittanen P, Pekkanen J. Urban air pollution, and asthma and COPD hospital emergency room visits. Thorax. 2008;63:635–641. doi: 10.1136/thx.2007.091371 [DOI] [PubMed] [Google Scholar]
- 18.Wang M, Aaron CP, Madrigano J, et al. Association Between Long-term Exposure to Ambient Air Pollution and Change in Quantitatively Assessed Emphysema and Lung Function. JAMA. 2019;322:546–556. doi: 10.1001/jama.2019.10255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Russell KE, Chung KF, Clarke CJ, et al. The MIF Antagonist ISO-1 Attenuates Corticosteroid-Insensitive Inflammation and Airways Hyperresponsiveness in an Ozone-Induced Model of COPD. PLoS One. 2016;11:e0146102. doi: 10.1371/journal.pone.0146102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wright JL, Cosio M, Churg A. Animal models of chronic obstructive pulmonary disease. Am J Physiol Lung Cell Mol Physiol. 2008;295:L1–15. doi: 10.1152/ajplung.90200.2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Churg A, Wang RD, Tai H, et al. Macrophage metalloelastase mediates acute cigarette smoke-induced inflammation via tumor necrosis factor-alpha release. Am J Respir Crit Care Med. 2003;167:1083–1089. doi: 10.1164/rccm.200212-1396OC [DOI] [PubMed] [Google Scholar]
- 22.Guo H, Callaway JB, Ting JP. Inflammasomes: mechanism of action, role in disease, and therapeutics. Nat Med. 2015;21:677–687. doi: 10.1038/nm.3893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics. Nat Rev Immunol. 2019;19:477–489. doi: 10.1038/s41577-019-0165-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bakker PJ, Butter LM, Claessen N, et al. A tissue-specific role for Nlrp3 in tubular epithelial repair after renal ischemia/reperfusion. Am J Pathol. 2014;184:2013–2022. doi: 10.1016/j.ajpath.2014.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gwyer Findlay E, Hussell T. Macrophage-mediated inflammation and disease: a focus on the lung. Mediators Inflamm. 2012;2012:140937. doi: 10.1155/2012/140937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peeters PM, Perkins TN, Wouters EF, Mossman BT, Reynaert NL. Silica induces NLRP3 inflammasome activation in human lung epithelial cells. Part Fibre Toxicol. 2013;10:3. doi: 10.1186/1743-8977-10-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Faner R, Sobradillo P, Noguera A, et al. The inflammasome pathway in stable COPD and acute exacerbations. ERJ Open Res. 2016;2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nachmias N, Langier S, Brzezinski RY, et al. NLRP3 inflammasome activity is upregulated in an in-vitro model of COPD exacerbation. PLoS One. 2019;14:e0214622. doi: 10.1371/journal.pone.0214622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang H, Lv C, Wang S, Ying H, Weng Y, Yu W. NLRP3 Inflammasome Involves in the Acute Exacerbation of Patients with Chronic Obstructive Pulmonary Disease. Inflammation. 2018;41:1321–1333. doi: 10.1007/s10753-018-0780-0 [DOI] [PubMed] [Google Scholar]
- 30.Singh B, Arora S, Khanna V. Association of severity of COPD with IgE and interleukin-1 beta. Monaldi Arch Chest Dis. 2010;73:86–87. [DOI] [PubMed] [Google Scholar]
- 31.Damera G, Pham TH, Zhang J, et al. A Sputum Proteomic Signature That Associates with Increased IL-1beta Levels and Bacterial Exacerbations of COPD. Lung. 2016;194:363–369. doi: 10.1007/s00408-016-9877-0 [DOI] [PubMed] [Google Scholar]
- 32.Kuschner WG, D’Alessandro A, Wong H, Blanc PD. Dose-dependent cigarette smoking-related inflammatory responses in healthy adults. Eur Respir J. 1996;9:1989–1994. doi: 10.1183/09031936.96.09101989 [DOI] [PubMed] [Google Scholar]
- 33.Chung KF. Cytokines in chronic obstructive pulmonary disease. Eur Respir J. 2001;34:50s–59s. doi: 10.1183/09031936.01.00229701 [DOI] [PubMed] [Google Scholar]
- 34.Lappalainen U, Whitsett JA, Wert SE, Tichelaar JW, Bry K. Interleukin-1beta causes pulmonary inflammation, emphysema, and airway remodeling in the adult murine lung. Am J Respir Cell Mol Biol. 2005;32:311–318. doi: 10.1165/rcmb.2004-0309OC [DOI] [PubMed] [Google Scholar]
- 35.Doz E, Noulin N, Boichot E, et al. Cigarette smoke-induced pulmonary inflammation is TLR4/MyD88 and IL-1R1/MyD88 signaling dependent. J Immunol. 2008;180:1169–1178. doi: 10.4049/jimmunol.180.2.1169 [DOI] [PubMed] [Google Scholar]
- 36.Botelho FM, Bauer CM, Finch D, et al. IL-1alpha/IL-1R1 expression in chronic obstructive pulmonary disease and mechanistic relevance to smoke-induced neutrophilia in mice. PLoS One. 2011;6:e28457. doi: 10.1371/journal.pone.0028457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pauwels NS, Bracke KR, Dupont LL, et al. Role of IL-1alpha and the Nlrp3/caspase-1/IL-1beta axis in cigarette smoke-induced pulmonary inflammation and COPD. Eur Respir J. 2011;38:1019–1028. doi: 10.1183/09031936.00158110 [DOI] [PubMed] [Google Scholar]
- 38.Kang MJ, Homer RJ, Gallo A, et al. IL-18 is induced and IL-18 receptor alpha plays a critical role in the pathogenesis of cigarette smoke-induced pulmonary emphysema and inflammation. J Immunol. 2007;178:1948–1959. doi: 10.4049/jimmunol.178.3.1948 [DOI] [PubMed] [Google Scholar]
- 39.Petersen AM, Penkowa M, Iversen M, et al. Elevated levels of IL-18 in plasma and skeletal muscle in chronic obstructive pulmonary disease. Lung. 2007;185:161–171. doi: 10.1007/s00408-007-9000-7 [DOI] [PubMed] [Google Scholar]
- 40.Hoshino T, Kato S, Oka N, et al. Pulmonary inflammation and emphysema: role of the cytokines IL-18 and IL-13. Am J Respir Crit Care Med. 2007;176:49–62. doi: 10.1164/rccm.200603-316OC [DOI] [PubMed] [Google Scholar]
- 41.Franklin BS, Bossaller L, De Nardo D, et al. The adaptor ASC has extracellular and ‘prionoid’ activities that propagate inflammation. Nat Immunol. 2014;15:727–737. doi: 10.1038/ni.2913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eltom S, Stevenson CS, Rastrick J, et al. P2X7 receptor and caspase 1 activation are central to airway inflammation observed after exposure to tobacco smoke. PLoS One. 2011;6:e24097. doi: 10.1371/journal.pone.0024097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Churg A, Zhou S, Wang X, Wang R, Wright JL. The role of interleukin-1beta in murine cigarette smoke-induced emphysema and small airway remodeling. Am J Respir Cell Mol Biol. 2009;40:482–490. doi: 10.1165/rcmb.2008-0038OC [DOI] [PubMed] [Google Scholar]
- 44.Ferhani N, Letuve S, Kozhich A, et al. Expression of high-mobility group box 1 and of receptor for advanced glycation end products in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;181:917–927. doi: 10.1164/rccm.200903-0340OC [DOI] [PubMed] [Google Scholar]
- 45.Mortaz E, Folkerts G, Nijkamp FP, Henricks PA. ATP and the pathogenesis of COPD. Eur J Pharmacol. 2010;638:1–4. doi: 10.1016/j.ejphar.2010.04.019 [DOI] [PubMed] [Google Scholar]
- 46.Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138:16–27. doi: 10.1016/j.jaci.2016.05.011 [DOI] [PubMed] [Google Scholar]
- 47.Durham AL, Adcock IM. The relationship between COPD and lung cancer. Lung Cancer. 2015;90:121–127. doi: 10.1016/j.lungcan.2015.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Harijith A, Ebenezer DL, Natarajan V. Reactive oxygen species at the crossroads of inflammasome and inflammation. Front Physiol. 2014;5:352. doi: 10.3389/fphys.2014.00352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wattanachayakul P, Rujirachun P, Charoenngam N, Ungprasert P. Chronic obstructive pulmonary disease (COPD) is associated with a higher level of serum uric acid. A systematic review and meta-analysis. Adv Respir Med. 2020;88:215–222. doi: 10.5603/ARM.2020.0119 [DOI] [PubMed] [Google Scholar]
- 50.Martinon F, Petrilli V, Mayor A, Tardivel A, Tschopp J. Gout-associated uric acid crystals activate the NALP3 inflammasome. Nature. 2006;440:237–241. doi: 10.1038/nature04516 [DOI] [PubMed] [Google Scholar]
- 51.Braga TT, Forni MF, Correa-Costa M, et al. Soluble Uric Acid Activates the NLRP3 Inflammasome. Sci Rep. 2017;7:39884. doi: 10.1038/srep39884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wanderer AA. Interleukin-1beta targeted therapy in severe persistent asthma (SPA) and chronic obstructive pulmonary disease (COPD): proposed similarities between biphasic pathobiology of SPA/COPD and ischemia-reperfusion injury. Isr Med Assoc J. 2008;10:837–842. [PubMed] [Google Scholar]
- 53.Uh ST, Koo SM, Kim Y, et al. The activation of NLRP3-inflammsome by stimulation of diesel exhaust particles in lung tissues from emphysema model and RAW 264.7 cell line. Korean J Intern Med. 2017;32:865–874. doi: 10.3904/kjim.2016.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhao J, Li M, Wang Z, et al. Role of PM2.5 in the development and progression of COPD and its mechanisms. Respir Res. 2019;20:120. doi: 10.1186/s12931-019-1081-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zheng R, Tao L, Jian H, et al. NLRP3 inflammasome activation and lung fibrosis caused by airborne fine particulate matter. Ecotoxicol Environ Saf. 2018;163:612–619. doi: 10.1016/j.ecoenv.2018.07.076 [DOI] [PubMed] [Google Scholar]
- 56.Tian L, Yan J, Li K, et al. Ozone exposure promotes pyroptosis in rat lungs via the TLR2/4-NF-kappaB-NLRP3 signaling pathway. Toxicology. 2021;450:152668. doi: 10.1016/j.tox.2020.152668 [DOI] [PubMed] [Google Scholar]
- 57.Li C, Zhihong H, Wenlong L, et al. The Nucleotide-Binding Oligomerization Domain-Like Receptor Family Pyrin Domain-Containing 3 Inflammasome Regulates Bronchial Epithelial Cell Injury and Proapoptosis after Exposure to Biomass Fuel Smoke. Am J Respir Cell Mol Biol. 2016;55:815–824. doi: 10.1165/rcmb.2016-0051OC [DOI] [PubMed] [Google Scholar]
- 58.Wagner U, Staats P, Fehmann HC, Fischer A, Welte T, Groneberg DA. Analysis of airway secretions in a model of sulfur dioxide induced chronic obstructive pulmonary disease (COPD). J Occup Med Toxicol. 2006;1:12. doi: 10.1186/1745-6673-1-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang L, Zhang H, Chen P. Sulfur dioxide attenuates sepsis-induced cardiac dysfunction via inhibition of NLRP3 inflammasome activation in rats. Nitric Oxide. 2018;81:11–20. doi: 10.1016/j.niox.2018.09.005 [DOI] [PubMed] [Google Scholar]
- 60.Hnizdo E, Vallyathan V. Chronic obstructive pulmonary disease due to occupational exposure to silica dust: a review of epidemiological and pathological evidence. Occup Environ Med. 2003;60:237–243. doi: 10.1136/oem.60.4.237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peeters PM, Eurlings IM, Perkins TN, et al. Silica-induced NLRP3 inflammasome activation in vitro and in rat lungs. Part Fibre Toxicol. 2014;11:58. doi: 10.1186/s12989-014-0058-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wu R, Hogberg J, Adner M, Ramos-Ramirez P, Stenius U, Zheng H. Crystalline silica particles cause rapid NLRP3-dependent mitochondrial depolarization and DNA damage in airway epithelial cells. Part Fibre Toxicol. 2020;17:39. doi: 10.1186/s12989-020-00370-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hedbrant A, Andersson L, Bryngelsson IL, et al. Quartz Dust Exposure Affects NLRP3 Inflammasome Activation and Plasma Levels of IL-18 and IL-1Ra in Iron Foundry Workers. Mediators Inflamm. 2020;2020:8490908. doi: 10.1155/2020/8490908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Shamssain MH. Pulmonary function and symptoms in workers exposed to wood dust. Thorax. 1992;47:84–87. doi: 10.1136/thx.47.2.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mandryk J, Alwis KU, Hocking AD. Work-related symptoms and dose-response relationships for personal exposures and pulmonary function among woodworkers. Am J Ind Med. 1999;35:481–490. doi: [DOI] [PubMed] [Google Scholar]
- 66.Sethi S. Infection as a comorbidity of COPD. Eur Respir J. 2010;35:1209–1215. doi: 10.1183/09031936.00081409 [DOI] [PubMed] [Google Scholar]
- 67.Jain NK. Chronic obstructive pulmonary disease and tuberculosis. Lung India. 2017;34:468–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dorhoi A, Nouailles G, Jorg S, et al. Activation of the NLRP3 inflammasome by Mycobacterium tuberculosis is uncoupled from susceptibility to active tuberculosis. Eur J Immunol. 2012;42:374–384. doi: 10.1002/eji.201141548 [DOI] [PubMed] [Google Scholar]
- 69.Segovia J, Sabbah A, Mgbemena V, et al. TLR2/MyD88/NF-kappaB pathway, reactive oxygen species, potassium efflux activates NLRP3/ASC inflammasome during respiratory syncytial virus infection. PLoS One. 2012;7:e29695. doi: 10.1371/journal.pone.0029695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kuriakose T, Man SM, Malireddi RK, et al. ZBP1/DAI is an innate sensor of influenza virus triggering the NLRP3 inflammasome and programmed cell death pathways. Sci Immunol. 2016;5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Liu T, Zhou YT, Wang LQ, et al. NOD-like receptor family, pyrin domain containing 3 (NLRP3) contributes to inflammation, pyroptosis, and mucin production in human airway epithelium on rhinovirus infection. J Allergy Clin Immunol. 2019;144:777–787 e779. [DOI] [PubMed] [Google Scholar]
- 72.Sandford AJ, Weir TD, Pare PD. Genetic risk factors for chronic obstructive pulmonary disease. Eur Respir J. 1997;10:1380–1391. doi: 10.1183/09031936.97.10061380 [DOI] [PubMed] [Google Scholar]
- 73.Hall R, Hall IP, Sayers I. Genetic risk factors for the development of pulmonary disease identified by genome-wide association. Respirology. 2019;24:204–214. doi: 10.1111/resp.13436 [DOI] [PubMed] [Google Scholar]
- 74.Ebrahimi T, Rust M, Kaiser SN, et al. alpha1-antitrypsin mitigates NLRP3-inflammasome activation in amyloid beta1-42-stimulated murine astrocytes. J Neuroinflammation. 2018;15:282. doi: 10.1186/s12974-018-1319-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Couillin I, Vasseur V, Charron S, et al. IL-1R1/MyD88 signaling is critical for elastase-induced lung inflammation and emphysema. J Immunol. 2009;183:8195–8202. doi: 10.4049/jimmunol.0803154 [DOI] [PubMed] [Google Scholar]
- 76.Wang L, Lei W, Zhang S, Yao L. MCC950, a NLRP3 inhibitor, ameliorates lipopolysaccharide-induced lung inflammation in mice. Bioorg Med Chem. 2021;30:115954. doi: 10.1016/j.bmc.2020.115954 [DOI] [PubMed] [Google Scholar]
- 77.Yang JW, Mao B, Tao RJ, et al. Corticosteroids alleviate lipopolysaccharide-induced inflammation and lung injury via inhibiting NLRP3-inflammasome activation. J Cell Mol Med. 2020;24:12716–12725. doi: 10.1111/jcmm.15849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bauer AK, Rondini EA, Hummel KA, et al. Identification of candidate genes downstream of TLR4 signaling after ozone exposure in mice: a role for heat-shock protein 70. Environ Health Perspect. 2011;119:1091–1097. doi: 10.1289/ehp.1003326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wang Y, Chen Q, Jiao F, et al. Histone deacetylase 2 regulates ULK1 mediated pyroptosis during acute liver failure by the K68 acetylation site. Cell Death Dis. 2021;12:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wiegman CH, Li F, Clarke CJ, et al. A comprehensive analysis of oxidative stress in the ozone-induced lung inflammation mouse model. Clin Sci (Lond). 2014;126:425–440. doi: 10.1042/CS20130039 [DOI] [PubMed] [Google Scholar]
- 81.Dinarello CA. Overview of the IL-1 family in innate inflammation and acquired immunity. Immunol Rev. 2018;281:8–27. doi: 10.1111/imr.12621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Xu M, Wang L, Wang M, et al. Mitochondrial ROS and NLRP3 inflammasome in acute ozone-induced murine model of airway inflammation and bronchial hyperresponsiveness. Free Radic Res. 2019;53:780–790. doi: 10.1080/10715762.2019.1630735 [DOI] [PubMed] [Google Scholar]
- 83.Beckett EL, Stevens RL, Jarnicki AG, et al. A new short-term mouse model of chronic obstructive pulmonary disease identifies a role for mast cell tryptase in pathogenesis. J Allergy Clin Immunol. 2013;131:752–762. doi: 10.1016/j.jaci.2012.11.053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Yang W, Ni H, Wang H, Gu H. NLRP3 inflammasome is essential for the development of chronic obstructive pulmonary disease. Int J Clin Exp Pathol. 2015;8:13209–13216. [PMC free article] [PubMed] [Google Scholar]
- 85.Kumar M, Phougat N, Ruhil S, Dhankhar S, Balhara M, Chhillar AK. Genomics of Chronic Obstructive Pulmonary Disease (COPD); Exploring the SNPs of Protease-Antiprotease Pathway. Curr Genomics. 2013;14:204–213. doi: 10.2174/1389202911314030006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baykara O, Tomekce Taskiran NB, Soyyigit S, Buyru N. IL-1beta polymorphism in COPD patients in Turkish population. Tuberk Toraks. 2017;65:90–96. doi: 10.5578/tt.52778 [DOI] [PubMed] [Google Scholar]
- 87.Ishii T, Matsuse T, Teramoto S, et al. Neither IL-1beta, IL-1 receptor antagonist, nor TNF-alpha polymorphisms are associated with susceptibility to COPD. Respir Med. 2000;94:847–851. doi: 10.1053/rmed.2000.0808 [DOI] [PubMed] [Google Scholar]
- 88.Xie ZK, Huang QP, Huang J, Xie ZF. Association between the IL1B, IL1RN polymorphisms and COPD risk: a meta-analysis. Sci Rep. 2014;4:6202. doi: 10.1038/srep06202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wang YS, Liu L, Xu XY, et al. Association of interleukin-1beta −511C/T promoter polymorphism with COPD risk: a meta-analysis. Genet Mol Res. 2015;14:4477–4484. doi: 10.4238/2015.May.4.5 [DOI] [PubMed] [Google Scholar]
- 90.Shukla RK, Kant S, Bhattacharya S, Mittal B. Association of cytokine gene polymorphisms in patients with chronic obstructive pulmonary disease. Oman Med J. 2012;27:285–290. doi: 10.5001/omj.2012.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Lee JM, Kang YR, Park SH, et al. Polymorphisms in interleukin-1B and its receptor antagonist genes and the risk of chronic obstructive pulmonary disease in a Korean population: a case-control study. Respir Med. 2008;102:1311–1320. doi: 10.1016/j.rmed.2008.03.026 [DOI] [PubMed] [Google Scholar]
- 92.Wang J, Liu X, Xie J, Xu Y. Association of interleukin-18 promoter polymorphisms with chronic obstructive pulmonary disease in male smokers. Int J Immunogenet. 2013;40:204–208. doi: 10.1111/iji.12014 [DOI] [PubMed] [Google Scholar]
- 93.Hernandez ML, Mills K, Almond M, et al. IL-1 receptor antagonist reduces endotoxin-induced airway inflammation in healthy volunteers. J Allergy Clin Immunol. 2015;135:379–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Calverley PMA, Sethi S, Dawson M, et al. A randomised, placebo-controlled trial of anti-interleukin-1 receptor 1 monoclonal antibody MEDI8968 in chronic obstructive pulmonary disease. Respir Res. 2017;18:153. doi: 10.1186/s12931-017-0633-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bucher H, Mang S, Keck M, et al. Neutralization of both IL-1alpha/IL-1beta plays a major role in suppressing combined cigarette smoke/virus-induced pulmonary inflammation in mice. Pulm Pharmacol Ther. 2017;44:96–105. doi: 10.1016/j.pupt.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 96.Sichelstiel A, Yadava K, Trompette A, et al. Targeting IL-1beta and IL-17A driven inflammation during influenza-induced exacerbations of chronic lung inflammation. PLoS One. 2014;9:e98440. doi: 10.1371/journal.pone.0098440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Global Health Data Exchange. Prevalence of chronic obstructive pulmonary disease (COPD). Available from: http://ghdx.healthdata.org/search/site/COPD. Accessed August 20, 2021. [Google Scholar]