Abstract
Background:
In 2014, the price of intravenous (IV) acetaminophen more than doubled. This study determined whether increased IV acetaminophen cost was associated with decreased utilization and increased opioid use for children undergoing appendectomy.
Methods:
A multicenter retrospective cohort study using the Pediatric Health Information System® database between 2011–2017 was performed. Healthy children 2–18y undergoing appendectomy at 46 children’s hospitals in the United States were identified. IV acetaminophen use, opioid use and pharmacy costs were assessed. Multivariable mixed-effects modeling was used to determine the association between postoperative opioid use, IV acetaminophen use, and postoperative length-of-stay (LOS).
Results:
Overall, 110,019 children undergoing appendectomy were identified with 22.5% (N=24,777) receiving IV acetaminophen. Despite the 2014 price increase, IV acetaminophen use increased from 3% in 2011 to 40.1% in 2017 (p<0.001), but at a significantly reduced rate. After 2014, adjusted median pharmacy charges decreased from $3,326.5 (IQR:$1,717.5$6,710.8) to $3,264.1 (IQR:$1,782.8-$5,934.7, p<0.001) for children who received IV acetaminophen. In 94,745 children staying ≥1 day after surgery, postoperative opioid use decreased from 73.6% in 2011 to 58.6% in 2017 (p<0.001). Use of IV acetaminophen alone compared to opioids alone after surgery resulted in similar predicted mean postoperative LOS.
Conclusions:
In children undergoing appendectomy, IV acetaminophen use continued to rise, but at a slower rate after a price increase. Furthermore, adjusted pharmacy charges were lower for children receiving IV acetaminophen, possibly secondary to a concurrent decrease in postoperative opioid use. These findings suggest IV acetaminophen may be more broadly utilized regardless of perceived costs to minimize opioid use after surgery.
Keywords: intravenous acetaminophen, appendicitis, pediatric, opioid, cost
Article Summary
For children who underwent an appendectomy from 2011–2017, use of IV acetaminophen increased at a lower rate after a significant price increase in 2014. However, overall adjusted pharmacy costs actually decreased over time, possibly due to a concurrent decrease in postoperative opioid use.
Introduction
In 2017, the opioid epidemic was declared a national emergency,1 resulting in efforts to incorporate multi-modal analgesics to decrease opioid use postoperatively.2–4 For children undergoing surgery, opioid use is associated with considerable risks, including, sedation, vomiting, constipation, respiratory depression, and a high addictive potential.5 In 2010, the Food and Drug Administration approved intravenous (IV) acetaminophen to be used to treat pain in children and adults.6 Clinicians subsequently began using it for postoperative pain as a non-opioid analgesic in an attempt to reduce opioid use.7 Several studies have demonstrated decreased length of stay, improved pain control, decreased opioid use, and decreased overall hospital costs related to IV acetaminophen use,7–9 including a recent systematic review.10 However, in 2014 the cost of IV Acetaminophen more than doubled from $14 to $35 per onegram vial. As a result, hospitals began limiting use of IV acetaminophen in an effort to reduce costs.11,12
Appendectomy is the most common surgery performed in hospitalized children.13 Children undergoing appendectomy for acute appendicitis require inpatient hospitalization and are typically managed with various analgesia strategies, often including opioids.14–18 It is unknown whether the price increase for IV acetaminophen impacted overall utilization of IV acetaminophen and/or opioids for children undergoing appendectomy. This study was conducted to determine if the increased price of IV acetaminophen was associated with decreased inpatient utilization and consequently associated with increased opioid use for children undergoing appendectomy. We hypothesized that when the cost of IV acetaminophen increased, IV acetaminophen utilization would decrease, and opioid use would increase in response. Furthermore, we hypothesized that any increased opioid use would be associated with prolonged postoperative length of stay.
Methods
Study Design, Participants, and Data Collection Procedures
Institutional Review Board approval was obtained from the Children’s Hospital of Los Angeles. We performed a retrospective cohort study using the Pediatric Health Information System® (PHIS). The PHIS database is maintained by the Children’s Hospital Association (CHA; Lenexa, KS) and includes clinical and resource utilization data for both inpatient and outpatient encounters for children’s hospitals throughout the United States. All data is deidentified prior to its release for analysis. Data quality is monitored by the PHIS data quality program with issuance of quarterly data quality reports, chart audits, and feedback to participating hospitals.
All pediatric patients between the ages of 2 to 18 years with a diagnosis of acute appendicitis (ICD-9-CM 540, 540.9, 541, 542 or ICD-10-CM K35.3, K35.30, K35.31, K35.8, K35.80, K35.89, K35.890, K35.891, K36, K37) or perforated appendicitis (ICD-9-CM 540.0, 540.1 or ICD-10-CM K35.2, K35.20, K35.21, K35.32, K35.33) who underwent an open appendectomy (ICD-9-CM 47.0, 47.09 or ICD-10-CM 0DBJ0ZZ, 0DTJ0ZZ) or laparoscopic appendectomy (ICD-9-CM 47.01 or ICD-10-CM 0DBJ4ZZ, 0DTJ4ZZ) from 1/1/2011 – 12/31/2017 were identified. Hospitals that only contributed data after the 2014 price increase were omitted. Patients with a complex chronic condition, defined as a medical condition expected to last at ≥12 months and involve either several organ systems or one organ system severely enough to require specialty care,19 those without pharmacy data, and those with missing insurance or gender data were excluded. Patient demographic data included age, sex, gender, race, ethnicity, and insurance status. Hospital characteristics included United States census region (Midwest, Northeast, South, and West) and hospital number.
Definition of Analgesic Exposure
Pain medications of interest included opioids and IV acetaminophen. Analgesia use was determined from PHIS pharmacy billing data using generic pharmacy codes which are timestamped for date of exposure. Of note, while dosage strength is captured by PHIS, frequency of administration is not captured.
Opioid exposure was defined as the use of any opioid medication during the patient’s hospital stay. Opioid medications were defined according to Womer et al. who previously reviewed opioid use in hospitalized children in the PHIS.20 Opioid use was dichotomized into ‘exposed’ versus ‘unexposed’ and categorized as IV versus per os (PO). Non-opioid analgesic use of IV ketorolac was described. Of note, regional anesthetic blocks are not accurately reported in PHIS were thereby omitted from the analysis. Additionally, IV ibuprofen was used by <0.5% of the cohort and was omitted from the analysis.
Definition of Pharmacy Charges
Pharmacy charges are an estimate of what is requested by the provider for services. In the PHIS database, charges are adjusted for hospital location using the Centers for Medicare and Medicaid price and wage index. To better evaluate differences in charges we further adjusted pharmacy charges by the consumer price index (CPI) for medical care in 2017 to account for price changes and inflation over time.21 Pharmacy charge comparisons were for the entire cohort, comparing charges before and after the price increase on June 1, 2014.
Definition of Outcomes
For a subset of children who stayed ≥ 1 day(s) after surgery, we evaluated postoperative length of stay (LOS), defined as the discharge date minus the surgery date. A patient admitted and discharged the same day was defined as having a LOS equal to one day.
Statistical Analyses
Continuous variables were described using mean and standard deviation. Frequencies and percent were calculated to describe categorical variables. Patient demographic and hospital-level data were compared using bivariate analyses. Categorical and continuous variables were analyzed using Chi-square and Wilcoxon-Mann-Whitney tests, respectively. Normality for continuous variables were assessed by histograms and Q-Q plots. Pharmacy charges were stratified by IV acetaminophen exposed and unexposed patients before and after the 2014 IV acetaminophen price increase. Median and interquartile range (IQR) were reported as the data was right skewed. Pairwise comparisons of overall IV acetaminophen use by region were performed with a calculated Bonferroni correction for multiple comparisons. The Bonferroni correction was applied to adjust for multiple testing. The significance cut-off was calculated as α/n. There were six tests (regional comparisons made) and α = 0.01. Therefore, our Bonferroni corrected threshold was approximately 0.0017.
The Cochran–Armitage trend test was used to examine the trends of IV acetaminophen use and postoperative opioid use from 2011 to 2017. To further investigate the impact of the June 1, 2014 price increase on IV acetaminophen use, we conducted a segmented linear regression, a quasi-experimental method to evaluate health policies. We used this method to estimate trend in the number of patient encounters that used IV acetaminophen per month, as an aggregate outcome across hospitals. Time is a continuous variable indicating the time in months at the start of the observation period (i.e. month 1 corresponds to January 2011, and month 84 to December 2017). This alternative method of analysis uses linear regression techniques, and evaluates the structural trend growth, the impact of the price increase, and the change in trend following the price increase.22,23 As few hospitals contributed more than 100 observations per month per year, this analysis did not use mixed-effects regression and did not adjust for additional covariates.
Multivariable regression with mixed effects was used for modeling postoperative LOS. Mixed-effects modeling was used to control for unmeasured hospital characteristics that may confound any associations. Covariate selection was based on clinical assessment, availability from the PHIS databases, and variables with a significant bivariate association (p <0.01). Patient-level factors included in the regression were age, gender, race, ethnicity, and insurance type. Clinical factors included perforated appendicitis and open versus laparoscopic appendectomy. Hospital region was controlled for in the regression. A multi-level model was created in which individual patients were nested within hospitals to minimize unmeasured confounding by patient and hospital-level factors. Model fit and selection was assessed by using likelihood ratio tests, Akaike information criterion (AIC) and Bayesian information criterion (BIC).
Postoperative LOS was evaluated, and significance was tested by comparing results with natural log-transformed outcomes. Results and trends between continuous and log-transformed length of stay outcomes were consistent; we reported untransformed estimates for its ease interpretation and clinical relevancy. An additional, sensitivity analysis was conducted removing patients with LOS > 30 days, nevertheless estimates and significance trends were similar at p <0.001. To more clearly determine whether a decrease in postoperative LOS was related to an increase in IV acetaminophen use within a given hospital, a second mixed effects linear regression analysis was performed. This model assessed the relationship between the quarterly percent of patients receiving IV acetaminophen and quarterly postoperative LOS clustered by hospital and adjusted for time. Data were analyzed using SAS® software 9.4 (copyright © 2016 SAS Institute Inc., Cary, NC) and StataCorp (2017) Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. A significant association was defined at p<0.01 due to the large cohort size.
Results
Overall, 110,019 children undergoing appendectomy at 46 children’s hospitals in the United States from 2011–2017 were identified (Figure 1). Mean annual case volume at the included children’s hospitals was 341 ± 227 appendectomies per year. Within the cohort, 22.5% (N=24,777) received IV Acetaminophen (Table 1) and 98.9% (N=108,857) received opioids during hospitalization, with 94.9% receiving an opioid on the day of surgery. Use of IV opioids on the day of surgery was common (N=103,044, 93.7%) and oral opioid use less common (N=31,546, 28.7%). Conversely, oral opioid use on postoperative day 1 or later was more common (N=51,657, 47.0%) compared to postoperative IV opioid use (N=38,658, 35.1%)
Figure 1.
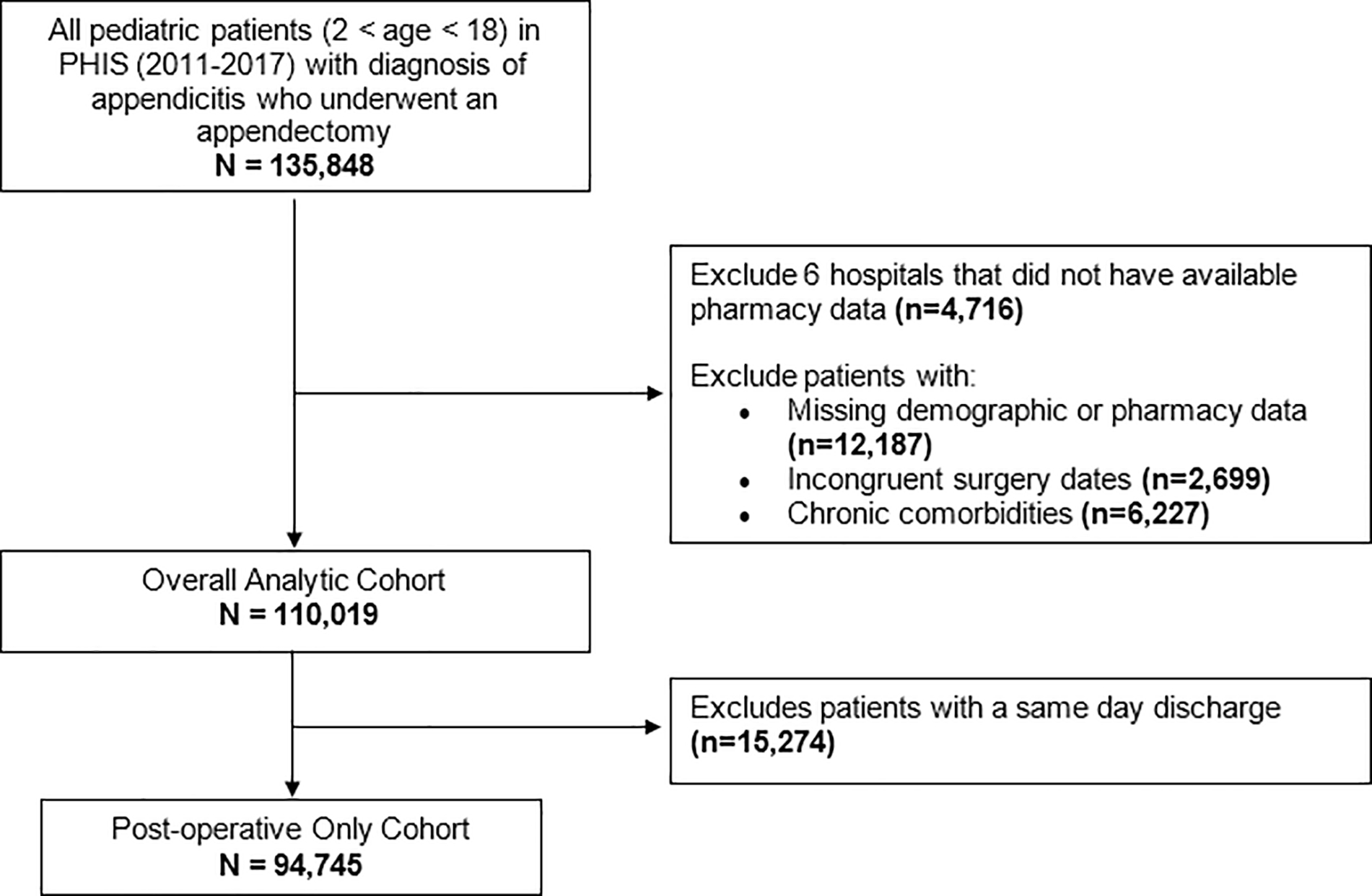
Flow Diagram of Cohort Selection
PHIS = Pediatric Health Information System
Table 1.
Overall analytic cohort of children who underwent appendectomy between 2011–2017.
| Total | IV Acetaminophen Use | |||
|---|---|---|---|---|
| N = 110,019 (%) | Yes N = 24,777 (%) |
No N = 85,242 (%) |
p-value | |
|
| ||||
| Mean age (±SD), years | 10.9 (3.7) | 10.7 (3.8) | 11.0 (3.7) | <0.001 |
| Male gender | 66,330 (60.3) | 14,833 (59.9) | 51,497 (60.4) | 0.122 |
| Ethnicity Hispanic or Latino |
37,031 (33.7) | 8,522 (34.4) | 28,509 (33.4) | <0.001 |
| Not Hispanic or Latino | 67,043 (60.9) | 15,395 (62.1) | 51,648 (60.6) | |
| Unknown | 5,945 (5.4) | 860 (3.5) | 5,086 (6.0) | |
| Race White |
77,616 (70.6) | 17,174 (69.3) | 60,442 (70.9) | <0.001 |
| Black | 7,943 (7.2) | 1,790 (7.2) | 6,153 (7.2) | |
| Asian | 2,692 (2.5) | 625 (2.5) | 2,067 (2.4) | |
| American Indian or Alaskan Native | 930 (0.9) | 62 (0.25) | 868 (1.0) | |
| Native Hawaiian or Pacific Islander | 207 (0.2) | 34 (0.14) | 173 (0.2) | |
| Other | 20,631 (18.8) | 5,092 (20.6) | 15,539 (18.2) | |
| Insurance Private |
49,672 (45.2) | 10,497 (42.4) | 39,175 (46.0) | <0.001 |
| Public | 54,722 (49.7) | 12,953 (52.3) | 41,769 (49.0) | |
| Other | 5,625 (5.1) | 1,327 (5.4) | 4,298 (5.0) | |
| Hospital Region Midwest |
21,848 (19.9) | 7,478 (30.2) | 14,370 (16.9) | <0.001 |
| Northeast | 12,119 (11.0) | 2,087 (8.4) | 10,032 (11.8) | |
| South | 45,214 (41.1) | 10,150 (40.97) | 35,064 (41.1) | |
| West | 30,838 (28.0) | 5,062 (20.4) | 25,776 (30.2) | |
| Open Appendectomy | 4,537 (4.1) | 866 (3.5) | 3,671 (4.3) | <0.001 |
| Perforated Appendicitis | 33,638 (30.6) | 10,721 (43.3) | 22,917 (26.9) | <0.001 |
Cohort race and ethnicity were consistent with previous national estimates of children with appendicitis.24,25 For children receiving IV acetaminophen, median duration of use during hospitalization was 1.0 day (IQR: 1.0–2.0). For children receiving opioids, median duration of opioid use was 2.0 days (IQR: 1.0–3.0), including opioids used on the day of surgery. On bivariate analyses, children receiving IV Acetaminophen tended to be slightly younger (10.7 vs 10.9 years; p<0.001) and more likely to have public insurance (52.3% vs 47.9%, p<0.001). Regional differences in utilization were also present. Pairwise comparisons of overall IV acetaminophen use by region were significant with the exception of Northeast versus West regions (17.2% vs. 16.4%, p-value=0.044). Children receiving IV acetaminophen were also more likely to be perforated (43.3% vs. 26.9%, p<0.001) and less likely to undergo an open operation (3.5% vs. 4.3%, p<0.001).
When investigating trends in overall IV acetaminophen and opioid use among the entire cohort from 2011 to 2017, the annual incidence of IV acetaminophen use increased from 3% in 2011 to 40.1% in 2017 (p<0.001) while overall IV opioid use remained constant for the overall cohort (Figure 2A), overall PO opioid use decreased. For children who stayed ≥1 day after appendectomy (N=94,745), both postoperative IV and oral opioid use decreased over time while IV acetaminophen, IV ketorolac and PO acetaminophen use increased (Figure 2B).
Figure 2.
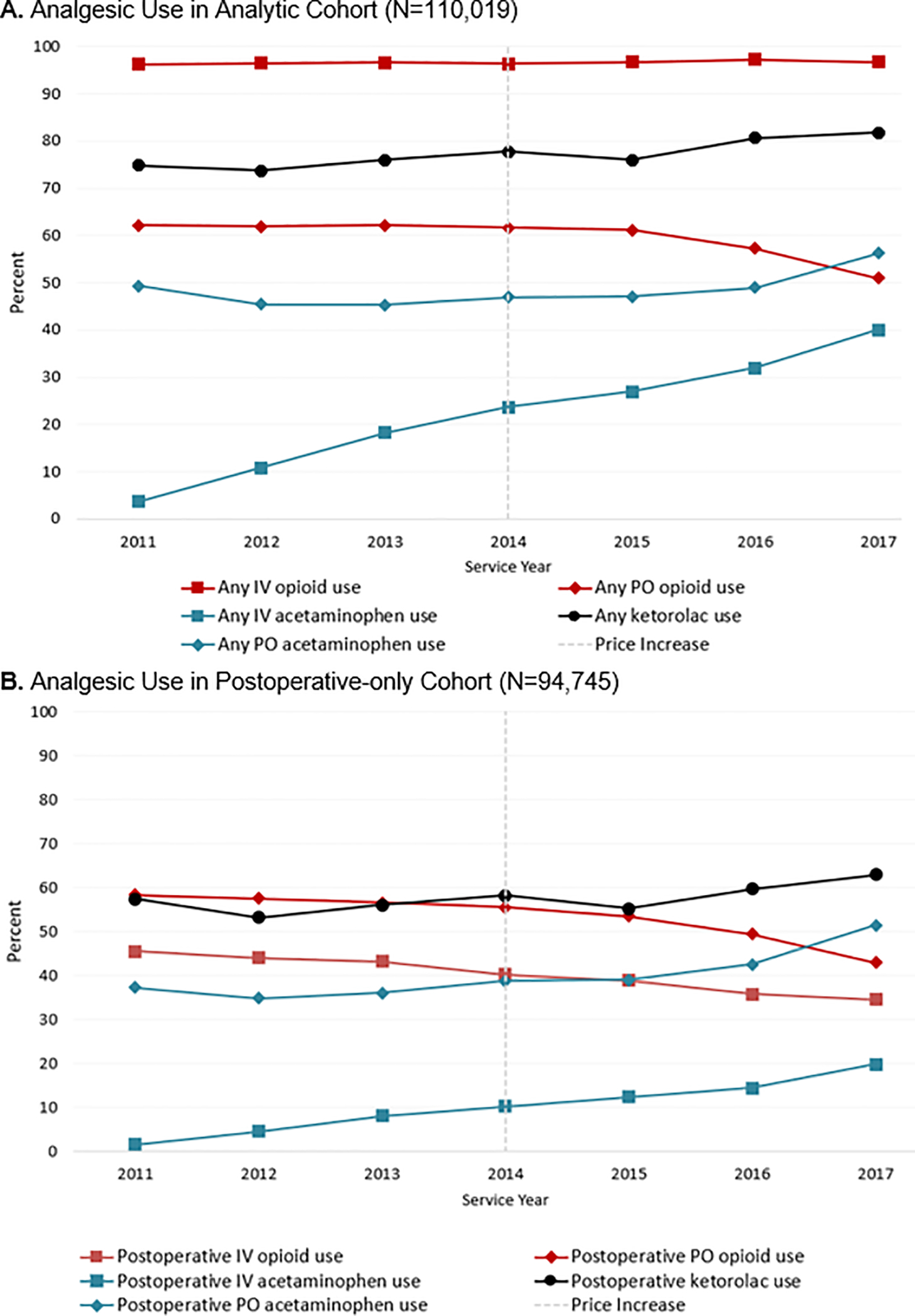
Perioperative IV Acetaminophen and Opioid Use Before and After IV Acetaminophen Price Increase (Vertical Line) in 2014.
A. Analgesic Use in Analytic Cohort (N=110,019)
B. Analgesic Use in Postoperative-only Cohort (N=94,745)
Segmented linear regression analysis evaluating the impact of the 2014 price increase on overall IV acetaminophen use revealed a significant change in the slope of the trend in acetaminophen use over time (Figure 3, Supplemental Table 1). To estimate the effect of the 2014 price increase, we can express the expected results from our segmented regression (Supplemental Table 1) at May 2015 (month 53), which is 12 months after the IV acetaminophen price increase was implemented. We estimate that had the 2014 price increase not taken effect, IV acetaminophen would have been used in 452 (95% CI: 367, 537) patients. However, 12 months after the price change, we estimate a considerable drop in IV acetaminophen use in 374 (95% CI: 236, 513) patients. The difference between these estimates is the absolute price effect, which demonstrates a decrease in IV acetaminophen use by 17.2% (95% CI: −35.8%, −4.5%).
Figure 3.
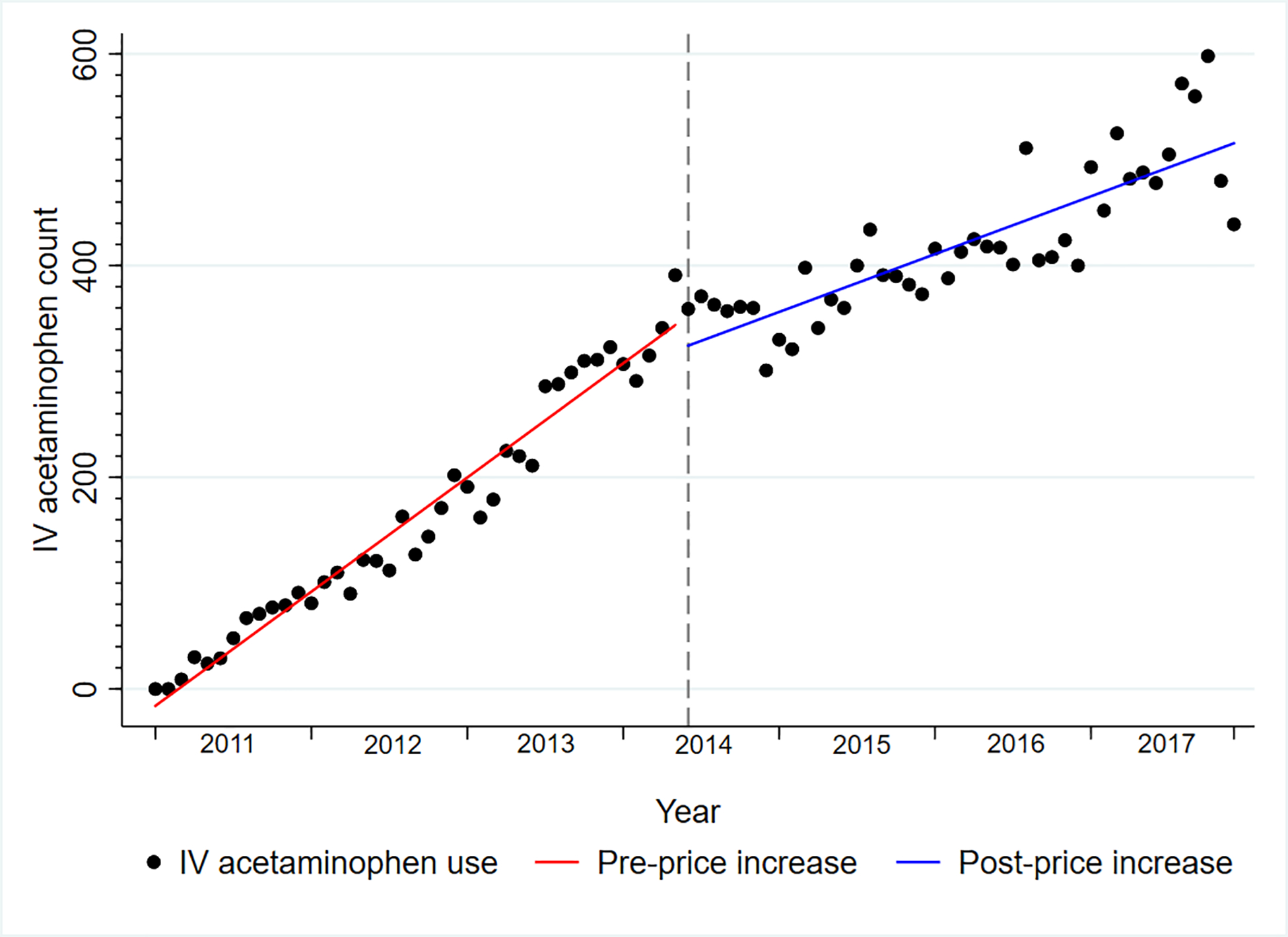
Segmented Linear Regression Evaluating the Impact of the 2014 Price Increase on the Overall use of IV Acetaminophen over Time (N=110,019)
For children who received IV acetaminophen (N=24,777), unadjusted pharmacy charges increased from $2,964.2 (IQR, $1,532.2-$5,970.3) to $3,152.6 (IQR, $1,718.4 – 5,709.1, p<0.001) following the 2014 price increase. However, after adjusting for the consumer price index (CPI), pharmacy charges significantly decreased from $3,326.5 ($1,717.5 – $6,710.8) to $3,264.1 ($1,782.8 – $5,934.7, p<0.001).
A subgroup analysis of children who stayed ≥1 day after surgery identified a cohort of 94,745 children, of which 9,445 (10.0%) received IV acetaminophen and 65,965(69.6%) received opioids after surgery. After controlling for patient and hospital-level factors, multivariable linear regression analyses revealed that postoperative opioid use after surgery was associated with a 0.68 day (95% CI: 0.57, 0.80) prolonged postoperative LOS and postoperative IV acetaminophen use was associated with a 0.84 day (95% CI: 0.67, 1.01) prolonged postoperative LOS (Table 2). A significant interaction between IV acetaminophen and IV opioid use was identified and evaluated. Use of IV acetaminophen alone compared to use of opioids alone after surgery resulted in similar predicted mean postoperative LOS (Supplemental Table 2).
Table 2.
Association Between Postoperative Opioid and IV Acetaminophen Use and Postoperative LOS in Children Admitted ≥1 Day(s) after Appendectomy*
| Point Estimate | 95% CI | |
|---|---|---|
|
| ||
| Constant | −6.57 | (−56.31, 43.17) |
| Postoperative Opioid Use | 0.68 | (0.57, 0.80) |
| Postoperative IV Acetaminophen Use | 0.84 | (0.67, 1.01) |
| Age (years) | −0.02 | (−0.03, −0.02) |
| Male Gender | 0.07 | (0.04, 0.10) |
| Race White |
Ref | Ref |
| Black | 0.35 | (0.28, 0.43) |
| Asian | 0.11 | (0.02, 0.20) |
| American Indian or Alaskan Native | 0.36 | (0.12, 0.59) |
| Native Hawaiian or Pacific Islander | 0.08 | (−0.22, 0.37) |
| Other | 0.01 | (−0.05, 0.07) |
| Ethnicity Not Hispanic or Latino |
Ref | Ref |
| Hispanic or Latino | 0.08 | (0.03, 0.14) |
| Unknown | −0.02 | (−0.10, 0.10) |
| Insurance Private |
Ref | Ref |
| Public | 0.14 | (0.09, 0.18) |
| Other | 0.11 | (0.01, 0.28) |
| Hospital Region West |
Ref | Ref |
| Midwest | −0.04 | (−0.32, 0.23) |
| Northeast | −0.10 | (−0.40, 0.21) |
| South | −0.16 | (−0.41, 0.09) |
| Open Appendectomy | 0.42 | (0.12, 0.72) |
| Perforated Appendicitis | 2.73 | (2.52, 2.94) |
| Open*Perforated† | 1.49 | (1.09, 1.91) |
| Postoperative IV Acetaminophen*Postoperative Opioid Use‡ | 1.12 | (0.85, 1.40) |
| Year of procedure | 0.01 | (−0.02, 0.03) |
A second linear regression model was used to further assess the relationship between the percent of patients receiving IV acetaminophen after surgery and postoperative length of stay clustered by hospital (Supplemental Figure 1). The analysis demonstrates that there is a small increase of 0.02 days (95% CI: 0.01–0.04) in the mean postoperative LOS for a one percent increase in the percent of patients receiving postoperative IV acetaminophen within a given hospital controlling for year of surgery.
Discussion
This multicenter retrospective cohort study of children who underwent appendectomy found that despite a price increase in 2014, overall IV acetminophen use continued to increase over time, but at a slower rate than previously. When evaluating pharmacy charges over time, overall adjusted mean pharmacy charges actually decreased after the IV acetamionphen price increase. Furthermore, a significant decrease in postoperative opioid use was identified alongside the increased use of IV acetaminophen and multiple other non-opioid analgesics. However, IV acetaminophen utilization alone was found to have minimal impact on postoperative LOS. These findings suggest that IV acetaminophen may be more broadly utilized for children with appendicitis as part of a multi-modal opioid-sparing regimen, regardless pricing concerns, to enhance opioid stewardship efforts.26
While the present study did highlight increased use of IV acetaminophen despite the 2014 price increase, it also identified a significant change in rate of use after the price increase. Our model estimates that this change translates to a clinically significant decrease in IV acetaminophen utilization. Large increases in pharmaceutical pricing can be associated with decreased utilization, as observed with the recent price increase for epinephrine autoinjectors.27 However, as highlighted by Shaker et al.’s economic evaluation of community anaphylaxis treatment, value-based pricing for drugs can allow pricing to be commensurate with proven outcomes.28 Any innovation in pharmaceutical development must therefore consider a medication’s financial burden alongside possible health benefits and improved clinical outcomes, especially for vulnerable populations.
Other pediatric surgical specialties report that adding IV acetaminophen to multi-modal analgesic therapy was associated with decreased LOS and hospital costs. In a prospective study of 14 children undergoing posterior spinal fusion, Olbrecht et al. demonstrated that the addition of IV acetaminophen resulted in an opioid-sparing effect that was also associated with a decreased LOS.29 Subramanyam et al. constructed a decision analytic model for children undergoing adenoidectomy and showed that the addition of IV acetaminophen administered with opioids resulted in decreased costs, decreased utilization of rescue analgesics, and better pain control than with opioids alone.8 It may be that the decreased costs appreciated with the addition of IV acetaminophen reflect a decreased use of opioids translating to an overall savings in pharmacy costs. However, there is an element of reverse causality when evaluating postoperative length of stay and postoperative analgesic use, in that the longer a patient is in the hospital, the more likely they are to receive both opioid and non-opioid pain medications. Our previous work with using PHIS found that early use of non-opioid analgesics, including IV acetaminophen, on postoperative day 1 or 2 translated to shortened hospital LOS for children with perforated appendicitis.30 Similar findings are seen in adults, as reported by Shaffer et al., who evaluated a cohort of 2.2 million adult surgical encounters and found that the addition of IV acetaminophen translated to total hospital LOS-related cost savings of $4.5 million and decreased opioid-related complications.7 The findings of the present study imply that increased use of IV acetaminophen alone may not directly translate to shorter postoperative length of stay, but that multi-modal opioid-free approaches to postoperative pain management in children may contribute to shortened hospitalization.
Although United States Department of Health and Human Services did not declare the opioid epidemic a national emergency until 2017 after this cohort received care,1 efforts to minimize opioid prescribing in children began gaining prominence during the duration of this study and likely explain the decreases in opioid use observed and concurrent increases in non-opioid analgesic use.31 While postoperative PO opioid use decreased throughout the course of this study, it is unknown whether those decreases would be more pronounced if pricing for IV acetaminophen had remained constant. Previous work evaluating IV acetaminophen use in hospitalized children using the PHIS from 2010 to 2017 found that intravenous acetaminophen is now administered in about 1 of every 8 pediatric hospitalizations.32 While the authors correctly highlight concern about the financial impact of broadened use of an expensive pharmaceutical, their study did not evaluate how increased IV acetaminophen use impacts opioid use or overall length of hospitalization. Furthermore, it is unclear whether the pharmacy costs reported were adjusted for inflation as overall pharmacy costs in the present study demonstrated a decrease with the expansion of IV acetaminophen use. Future efforts to minimize healthcare spending by limiting non-opioid analgesics must view pharmacy costs within the broader lens of health outcomes, particularly for children who require surgery.
This study was limited by the retrospective nature of the PHIS database. However, the large cohort size enabled us to identify and evaluate recent epidemiologic trends in IV acetaminophen use in children undergoing appendectomy, as PHIS represents approximately 20% of pediatric hospitalizations in the United States.33,34 In addition, the PHIS database does not identify frequency of analgesic administration. While dose concentrations are available, we could not determine the number of times IV acetaminophen or opioids were administered to calculate the total analgesic dosage delivered during hospitalization. There may be a dosedependent association between analgesic use and clinical outcomes that should be the target of future studies on healthcare utilization and costs of non-opioid analgesics. Also, the impact of the price increase was likely not universally applied as timing of hospital purchases after the price increase likely varied by individual pharmacy supply levels. The results to this study are also limited to children’s hospitals that are members of the CHA, most of whom are academic medical centers. Overall, IV acetaminophen utilization may vary between hospitals caring for adult and pediatric patients or community hospitals caring for children. Finally, administrative claims datasets are unable to adjust for clinical disease severity. Children with more severe appendicitis typically stay longer in the hospital and therefore may require more opioid and non-opioid analgesics. However, we excluded children with significant medical comorbidities and adjusted for perforated appendicitis, open appendectomy, and a significant interaction between open surgery and perforated appendicitis to minimize the impact of any unmeasured disease severity that would impact outcomes.
Conclusions
For children undergoing appendectomy, overall and postoperative IV acetaminophen use has continued to rise, but at a slower rate, after a recent price increase. Overall adjusted pharmacy charges decreased for children who received IV acetaminophen, possibly secondary to a decrease in postoperative opioid use. These findings underscore the importance of incorporating IV acetaminophen into opioid-sparing analgesic protocols and could contribute significant cost savings and improved outcomes for children recovering from surgery.
Supplementary Material
Supplemental Figure 1. Quarterly Percent of Children Receiving IV Acetaminophen and Quarterly Postoperative Length of Stay Clustered by Hospital for Children Admitted ≥1 Day(s) after Appendectomy (N=94,745)
Supplemental Table 1. Segmented Linear Regression Evaluating the Impact of the 2014 Price Increase on the Overall Aggregate Use of IV Acetaminophen Over Time (centered at the start of the observation period, January 2011)
Supplemental Table 2. Predicted Mean Postoperative LOS for IV Opioid and IV Acetaminophen Interaction Term
Funding/Support
Dr. Kelley-Quon is supported by grant KL2TR001854 from the National Center for Advancing Translational Science (NCATS) of the U.S. National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflict of Interest/Disclosures
The authors have no conflicts of interest or disclosures to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gostin LO, Hodge JG, Noe SA. Reframing the Opioid Epidemic as a National Emergency. JAMA. 2017;318(16):1539. doi: 10.1001/jama.2017.13358 [DOI] [PubMed] [Google Scholar]
- 2.Baxter KJ, Hafling J, Sterner J, et al. Effectiveness of gabapentin as a postoperative analgesic in children undergoing appendectomy. Pediatr Surg Int. 2018;34(7):769–774. doi: 10.1007/s00383-018-4274-9 [DOI] [PubMed] [Google Scholar]
- 3.Freedman-Weiss MR, Chiu AS, Worhunsky D, et al. An Evidence-Based Guideline Supporting Restricted Opioid Prescription after Pediatric Appendectomy. J Pediatr Surg. 2020;55(1):106–111. doi: 10.1016/j.jpedsurg.2019.09.063 [DOI] [PubMed] [Google Scholar]
- 4.Alkhoury F, Knight C, Stylianos S, et al. Prospective Comparison of Nonnarcotic versus Narcotic Outpatient Oral Analgesic Use after Laparoscopic Appendectomy and Early Discharge. Minim Invasive Surg. 2014;2014:1–3. doi: 10.1155/2014/509632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benyamin R, Trescot AM, Datta S, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105–20. http://www.ncbi.nlm.nih.gov/pubmed/18443635 [PubMed] [Google Scholar]
- 6.U.S. Food & Drug Administration. Drug Approval Package. Ofirmev (acetaminophen) Injection NDA #022450. Accessed November 14, 2019. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2010/022450_ofirmev_toc.cfm
- 7.Shaffer EE, Pham A, Woldman RL, et al. Estimating the Effect of Intravenous Acetaminophen for Postoperative Pain Management on Length of Stay and Inpatient Hospital Costs. Adv Ther. 2016;33(12):2211–2228. doi: 10.1007/s12325-016-0438-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Subramanyam R, Varughese A, Kurth CD, Eckman MH. Cost-effectiveness of intravenous acetaminophen for pediatric tonsillectomy. Anderson B, ed. Pediatr Anesth. 2014;24(5):467–475. doi: 10.1111/pan.12359 [DOI] [PubMed] [Google Scholar]
- 9.Hansen RN, Pham A, Strassels SA, Balaban S, Wan GJ. Comparative Analysis of Length of Stay and Inpatient Costs for Orthopedic Surgery Patients Treated with IV Acetaminophen and IV Opioids vs. IV Opioids Alone for Post-Operative Pain. Adv Ther. 2016;33(9):1635–1645. doi: 10.1007/s12325-016-0368-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu A, Benzon HA, Anderson TA. Evidence for the Efficacy of Systemic Opioid-Sparing Analgesics in Pediatric Surgical Populations. Anesth Analg. 2017;125(5):1569–1587. doi: 10.1213/ANE.0000000000002434 [DOI] [PubMed] [Google Scholar]
- 11.Vincent WR, Huiras P, Empfield J, et al. Controlling postoperative use of i.v. acetaminophen at an academic medical center. Am J Heal Pharm. 2018;75(8):548–555. doi: 10.2146/ajhp170054 [DOI] [PubMed] [Google Scholar]
- 12.Nguyen LP, Nguyen L, Austin JP. A Quality Improvement Initiative to Decrease Inappropriate Intravenous Acetaminophen Use at an Academic Medical Center. Hosp Pharm. 2020;55(4):253–260. doi: 10.1177/0018578719841054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Somme S, Bronsert M, Morrato E, Ziegler M. Frequency and Variety of Inpatient Pediatric Surgical Procedures in the United States. Pediatrics. 2013;132(6):e1466–e1472. doi: 10.1542/peds.2013-1243 [DOI] [PubMed] [Google Scholar]
- 14.Harbaugh CM, Lee JS, Hu HM, et al. Persistent Opioid Use Among Pediatric Patients After Surgery. Pediatrics. 2018;141(1):e20172439. doi: 10.1542/peds.2017-2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Manworren RCB, McElligott CD, Deraska P V., et al. Efficacy of Analgesic Treatments to Manage Children’s Postoperative Pain After Laparoscopic Appendectomy: Retrospective Medical Record Review. AORN J. 2016;103(3):317.e1–317.e11. doi: 10.1016/j.aorn.2016.01.013 [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Seipel C, Lopez ME, et al. A retrospective study of multimodal analgesic treatment after laparoscopic appendectomy in children. Lonnqvist P-A, ed. Paediatr Anaesth. 2013;23(12):1187–1192. doi: 10.1111/pan.12271 [DOI] [PubMed] [Google Scholar]
- 17.Anderson KT, Bartz-Kurycki MA, Ferguson DM, et al. Too much of a bad thing: Discharge opioid prescriptions in pediatric appendectomy patients. J Pediatr Surg. 2018;53(12):2374–2377. doi: 10.1016/j.jpedsurg.2018.08.034 [DOI] [PubMed] [Google Scholar]
- 18.Sonderman KA, Wolf LL, Madenci AL, et al. Opioid Prescription Patterns for Children Following Laparoscopic Appendectomy. Ann Surg. 2018;Publish Ah. doi: 10.1097/SLA.0000000000003171 [DOI] [PubMed] [Google Scholar]
- 19.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14(1):199. doi: 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Womer J, Zhong W, Kraemer FW, et al. Variation of Opioid Use in Pediatric Inpatients Across Hospitals in the U.S. J Pain Symptom Manage. 2014;48(5):903–914. doi: 10.1016/j.jpainsymman.2013.12.241 [DOI] [PubMed] [Google Scholar]
- 21.Dunn A, Grosse SD, Zuvekas SH. Adjusting Health Expenditures for Inflation: A Review of Measures for Health Services Research in the United States. Health Serv Res. 2018;53(1):175–196. doi: 10.1111/1475-6773.12612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27(4):299–309. doi: 10.1046/j.1365-2710.2002.00430.x [DOI] [PubMed] [Google Scholar]
- 23.Taljaard M, McKenzie JE, Ramsay CR, Grimshaw JM. The use of segmented regression in analysing interrupted time series studies: an example in pre-hospital ambulance care. Implement Sci. 2014;9(1):77. doi: 10.1186/1748-5908-9-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kokoska ER, Bird TM, Robbins JM, Smith SD, Corsi JM, Campbell BT. Racial Disparities in the Management of Pediatric Appenciditis. J Surg Res. 2007;137(1):83–88. doi: 10.1016/j.jss.2006.06.020 [DOI] [PubMed] [Google Scholar]
- 25.Naseem H-R, Dorman RM, Ventro G, Rothstein DH, Vali K. Safety of perioperative ketorolac administration in pediatric appendectomy. J Surg Res. 2017;218:232–236. doi: 10.1016/j.jss.2017.05.087 [DOI] [PubMed] [Google Scholar]
- 26.Bass KD, Heiss KF, Kelley-Quon LI, Raval M V. Opioid use in children’s surgery: Awareness, current state, and advocacy. J Pediatr Surg. Published online 2020. doi: 10.1016/j.jpedsurg.2020.02.015 [DOI] [PubMed] [Google Scholar]
- 27.Fromer L Prevention of Anaphylaxis: The Role of the Epinephrine Auto-Injector. Am J Med. 2016;129(12):1244–1250. doi: 10.1016/j.amjmed.2016.07.018 [DOI] [PubMed] [Google Scholar]
- 28.Shaker M, Greenhawt M. Association of Fatality Risk With Value-Based Drug Pricing of Epinephrine Autoinjectors for Children With Peanut Allergy. JAMA Netw Open. 2018;1(7):e184728. doi: 10.1001/jamanetworkopen.2018.4728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Olbrecht VA, Ding L, Spruance K, Hossain M, Sadhasivam S, Chidambaran V. Intravenous Acetaminophen Reduces Length of Stay Via Mediation of Postoperative Opioid Consumption After Posterior Spinal Fusion in a Pediatric Cohort. Clin J Pain. 2018;34(7):593–599. doi: 10.1097/AJP.0000000000000576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mahdi EM, Ourshalimian S, Russell CJ, Zamora AK, Kelley-Quon LI. Fewer postoperative opioids are associated with decreased duration of stay for children with perforated appendicitis. Surgery. 2020;168(5):942–947. doi: 10.1016/j.surg.2020.04.060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mazer-Amirshahi M, Mullins PM, Rasooly IR, van den Anker J, Pines JM. Trends in Prescription Opioid Use in Pediatric Emergency Department Patients. Pediatr Emerg Care. 2014;30(4):230–235. doi: 10.1097/PEC.0000000000000102 [DOI] [PubMed] [Google Scholar]
- 32.Bourgeois FT, Graham DA, Kesselheim AS, Randolph AG. Cost Implications of Escalating Intravenous Acetaminophen Use in Children. JAMA Pediatr. 2019;173(5):489. doi: 10.1001/jamapediatrics.2019.0101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kane JM, Colvin JD, Bartlett AH, Hall M. Opioid-Related Critical Care Resource Use in US Children’s Hospitals. Pediatrics. 2018;141(4):e20173335. doi: 10.1542/peds.2017-3335 [DOI] [PubMed] [Google Scholar]
- 34.Colvin JD, Hall M, Berry JG, et al. Financial Loss for Inpatient Care of Medicaid-Insured Children. JAMA Pediatr. 2016;170(11):1055. doi: 10.1001/jamapediatrics.2016.1639 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Quarterly Percent of Children Receiving IV Acetaminophen and Quarterly Postoperative Length of Stay Clustered by Hospital for Children Admitted ≥1 Day(s) after Appendectomy (N=94,745)
Supplemental Table 1. Segmented Linear Regression Evaluating the Impact of the 2014 Price Increase on the Overall Aggregate Use of IV Acetaminophen Over Time (centered at the start of the observation period, January 2011)
Supplemental Table 2. Predicted Mean Postoperative LOS for IV Opioid and IV Acetaminophen Interaction Term


