Abstract
Significance
Multifocal contact lenses are being used clinically for myopia control. Center-distance designs caused myopic changes in defocus across the retina that varied by lens design, while the center-near design caused peripheral hyperopic changes. Multifocal lenses caused reductions in low-contrast vision that varied by lens design, affecting visual performance.
Purpose.
To compare changes in defocus with four multifocal contact lenses (MFCLs), three center-distance and one center-near.
Methods.
Two cohorts of twenty-five non-presbyopic myopic adults were enrolled. The first cohort was fitted with Proclear D and Biofinity D MFCL (center-distance, +2.50D add), and cohort two was fitted with NaturalVue MFCL (center-distance) and Clariti 1-Day MFCL (center-near, high add), both in random order. Over-refraction was performed to maximize visual acuity. Cycloplegic autorefraction was performed with each lens and without a lens along the line of sight and at nasal and temporal retinal locations out to 40 degrees. Data were analyzed with repeated-measures ANOVAs with post-hoc t-tests, when indicated.
Results.
Changes in defocus at each location differed between MFCL designs (lens × location; both P < .001). Clariti 1-Day caused peripheral hyperopic retinal changes (40° and 30° nasal, and 20°, 30°, 40° temporal; all P < .05). NaturalVue MFCL caused myopic changes centrally and hyperopic changes at 40° nasal and 30° temporal (all P < .05). The remaining center-distance designs caused myopic changes at multiple locations (all P < .05).
Conclusions.
After over-refraction, the center-near MFCL design caused hyperopic defocus at multiple peripheral locations, which is not hypothesized to slow myopia progression. NaturalVue MFCL caused myopic changes in defocus centrally but hyperopic changes in the far periphery. Biofinity D and Proclear D caused myopic changes in retinal defocus. Further work is warranted to determine whether defocus profile differences between the center-distance designs influence any slowing of myopia progression.
Myopia affects approximately 1.5 billion people, an estimated 22.9% of the global population.1,2 Myopia is associated with multiple potentially blinding ocular comorbidities.3–5 The higher the degree of myopia, the greater a patient’s risk of developing a visually debilitating or blinding condition.1, 6, 7 Slowing the progression of myopia may reduce this risk.8
Light focusing in front of the retina (myopic defocus), is hypothesized to slow eye growth.9–11 Conversely, light focusing behind the retina (hyperopic defocus) is hypothesized to be a growth signal. In animal models, there is evidence that defocus affects local ocular growth, with retinal regions experiencing growth based on the local defocus signal.12, 13 In animal models ranging from young chicks to infant monkeys, peripheral defocus can accelerate or slow axial elongation even in the presence of clear central vision.14, 15 In an effort to slow the progression of juvenile-onset myopia, there have been attempts to translate these findings into humans by using lenses that simultaneously cause myopic retinal defocus while providing clear foveal vision.
For many years, the standard of care for correcting myopia has been to prescribe single vision lenses. While standard corrections for myopia have not been shown to be the cause of progressing myopia, the peripheral retina of myopic eyes wearing single vision spectacles16 or spherical contact lenses17, 18 are exposed to hyperopic defocus. Consequently, optical interventions which impose myopic retinal defocus while providing good foveal vision are being investigated to determine their ability to slow myopia progression. A variety of contact lens designs, including center-distance multifocal contact lenses and orthokeratology, have shown promise in slowing myopia progression.19–23
Multifocal contact lenses, which incorporate both distance and near (plus) power into the optic zone, can either have distance power in the center of the optic zone (center distance) or plus power (add power) in the center of the optic zone (center near).24 When myopic eyes are fitted with center-distance multifocal contact lenses, the lens optics cause a myopic change in peripheral defocus.18, 25 While center-distance designs have been used in multiple myopia control studies, there have been anecdotal suggestions by some eye care providers that center-near multifocal contact lens designs could also be used for myopia control purposes since they include an add. Based on the retinal defocus hypothesis, a center-near multifocal contact lens would need to induce myopic defocus in order to slow myopia progression. With a center-near design, there is the potential that the over-refraction required to achieve acceptable distance vision could minimize or eliminate any potential myopic defocus created by the central add power in the lens. We are unaware of any on-eye investigations of the effect of a center-near design on retinal defocus after accounting for subjective over-refraction.
In non-presbyopic adults, high-contrast visual acuity with center-distance multifocal contact lenses is typically the same as with spherical equivalent spectacles26 or contact lenses.27 However, multifocal contact lens designs are reported to reduce subjective visual quality and low-contrast visual acuity compared to spherical contact lenses.27–29 As commercially-available, center-distance multifocal contact lenses are being used clinically for myopia control, it is important to understand how these designs could impact visual acuity in non-presbyopic individuals.
In this study, we compared four commercially available multifocal contact lens designs (three center-distance and one center-near) to determine their effect on retinal defocus and visual acuity. The lenses evaluated were the Biofinity Multifocal ‘D’ (CooperVision, center-distance, +2.50 add), the Proclear Multifocal ‘D’ (CooperVision, center-distance, +2.50 add), the NaturalVue Multifocal (Visioneering Technologies Inc., center-distance) and the Clariti 1-Day Multifocal (CooperVision, center-near, high add). The direct comparison using the same methodology of three of the most common commercially-available center-distance multifocal contact lenses being used off-label for myopia control in the US will be helpful for clinicians aiming to choose a lens for a myopia control application. We include the NaturalVue Multifocal in this direct comparison, for which there are little data published. While only center-distance multifocal lens designs have been studied in myopia control clinical trials, a center-near multifocal lens design was included to objectively demonstrate the difference in defocus profiles between center-near and center-distance designs after accounting for subjective over-refraction.
METHODS
Subjects
Two cohorts of non-presbyopic myopic subjects, between 18 and 39 years of age, were recruited for this study. Two separate cohorts of 25 subjects each were utilized in order to test additional multifocal designs that were available after the initial cohort completed the study. Eligible subjects had spherical equivalent refractive error of −0.50 to −6.25 diopters sphere and visual acuity of 20/30 or better (right eye) with their spherical equivalent refractive error placed in a trial frame at the spectacle plane. Any subjects with cylinder greater than −1.00 diopters at the corneal plane were excluded. Subjects with active anterior segment pathology, a history of ocular trauma or surgery, or any systemic disease that could cause variability in refraction were excluded. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board at the University of Houston. All subjects provided written informed consent prior to the initiation of testing.
Contact Lenses
The highest standard add power available in each lens was chosen for this study. All lenses were commercially available in the United States. No contact lens had a myopia control indication from the US Food and Drug Administration at the time of this study. Biofinity Multifocal D and Proclear Multifocal D contact lenses (both center-distance; CooperVision) with a +2.50 diopter add power were tested in the first cohort of subjects. In the second cohort of subjects, the NaturalVue Multifocal (center-distance; Visioneering Technologies, Inc.) and the Clariti 1-Day Multifocal with high add (center-near; CooperVision) were tested. The NaturalVue Multifocal only comes in one add power, which the manufacturer reports will satisfy all add requirements up to +3.00 diopters. The high add power on the Clariti 1-Day is reported by the manufacturer to satisfy add requirements of +2.50 diopters and higher.
Published power profiles for both the Proclear D and Biofinity D (+2.50 add) indicate these lenses have central distance power that extends to roughly 1.5 mm from the center of the lens. There is then a quick increasing in plus power between a 1.5 mm to 2.0 mm radius, though the maximum add power is less than the labelled effective add power of +2.50 diopters.24, 30 The NaturalVue Multifocal center-distance design begins increasing in plus power at a 0.5 mm radius from the lens center and reaches its highest plus power at a radius of roughly 2.6 mm from the center of the lens with a maximum measured add power that ranged from roughly +3.00 to +4.00 diopters depending on the labelled distance power. After reaching this peak of plus, the power then shifts in the more minus direction, eventually becoming more myopic at the edge of the optic zone than the central distance power.30 Conversely, the center-near Clariti 1-day (high add) has roughly 2.00 diopters of plus centrally which then drops off gradually before plateauing 2mm from the center of the lens at 1.00 diopter more minus than the labelled distance prescription.24
Outline of the Study Visit
A standardized subjective refraction with most plus/least minus to best visual acuity was performed, and the spherical equivalent was placed over the right eye in a trial frame with the left eye occluded. Photopic high-contrast and low-contrast (10% Michaelson) logMAR visual acuity was measured at four meters using Bailey-Lovie visual acuity charts to determine best acuity with spherical equivalent spectacle correction. Following previously published protocols, chart luminance was between 75 and 120 cd/m2 and was verified prior to each subject visit.31 Room lighting was standardized at each visit and was approximately 600 lux at the subject’s eye. Visual acuity of the right eye was tested with the subject starting at the top of the chart and reading each letter until three or more letters on a single line were missed. Credit was given for each correctly read letter (optotype). Pupil size was measured using a NeurOptics VIP-200 Pupillometer (NeurOptics, Inc., Irvine, CA) under the same photopic conditions under which visual acuity was tested. After visual acuity was measured with spherical equivalent spectacle correction, one of the two study contact lenses were fitted on the subject’s right eye, in random order. Subjects were masked to the lenses being tested.
The fit of each contact lens was assessed to ensure adequate movement and centration. Contact lens lateral centration was assessed using a reticle in the slit lamp ocular. Nasal and temporal contact lens overlap were measured to determine horizontal decentration. After assessing the contact lens fit, a loose-lens spherical over-refraction using 0.25 diopter steps, with plus lenses being presented first, was performed to maximize distance visual acuity (maximum plus to best visual acuity). Subjects were seated 20 feet from the visual acuity chart, and all over-refractions were performed with the left eye occluded. Any over-refraction found was placed in a trial frame over the right eye with the left eye occluded. High-contrast and low-contrast logMAR visual acuity (right eye) was measured again, following the same procedure used when testing with spherical equivalent spectacle correction. The Bailey-Lovie chart set includes two high-contrast and two low-contrast charts. Subjects in each cohort needed to read a chart three different times at each contrast level – once with best correction, and once with each of the two contact lenses worn by each cohort. We alternated between charts so a subject never saw the same chart twice in a row.
After measuring best visual acuity, cycloplegia was obtained by instilling two drops of 1% tropicamide separated by five minutes. Cycloplegia was used to minimize accommodation and maximize autorefraction accuracy and repeatability during measurements.32 Twenty-five minutes after instilling the second drop of tropicamide, autorefraction measurements of the right eye (with no correction) were made along the line of sight (0°) and ±20°, ±30°, and ±40° from the line of sight using a modified Grand Seiko WAM-5500 (Grand Seiko Co.; Hiroshima, Japan). For cohort 2, additional measurements were also made at ±10° from the line of sight. This extra measurement was added due to the manufacturer reported rapid increase in plus power near the center of the NaturalVue Multifocal contact lens33–35 which was tested in cohort 2. All autorefraction measures were taken on the right eye with the left eye occluded. For each measurement, subjects turned their head, not eyes, to view a laser target projected on the wall.34, 36, 37 The autorefractor reticle was centered within the entrance pupil during measurements.38 After measurements of the eye alone, the measurements were repeated with each of the study contact lenses tested in that cohort, following the same randomized order used during acuity testing. Measurements 40° from the line of sight extend to a roughly 4.5mm radius from the center of the lens, with optic zones of most lenses ranging between 4mm to 4.5mm. The starting location for autorefraction measurements (most nasal or most temporal location) was determined by randomization.
At each retinal location, the first five autorefractor measurements that were within ±1.00 diopter of the median for the sphere and the cylinder powers were converted to vector notation (M, J0, and J45) and averaged,39 following previously published methodology.40 Relative peripheral refraction of the unaided eye and relative peripheral defocus (the eye while wearing each contact lens) were calculated by subtracting central defocus (M) from each peripheral location. The power profile of the contact lens as measured on eye by autorefraction at each retinal location was calculated by subtracting relative peripheral refraction of the uncorrected eye at each location from defocus measured while wearing each contact lens prior to cycloplegia. The over-refraction required to achieve best distance visual acuity while the subject wore each lens prior to cycloplegia was accounted for. Specifically, the subject’s spherical over-refraction when wearing that specific contact lens was subtracted from the autorefraction defocus measurements made at each retinal location while wearing that same contact lens to account for the defocus change across the retina that would result from updating the contact lens power by the over-refraction amount.
Sample Size
Sample size calculations were performed with a two-sided alpha level of 0.05 and 80% power. Previously published between-visit standard deviations (the standard deviation of the difference between measurement sessions) for off-axis autorefraction measurements with the Grand Seiko WAM-5500 were utilized.32 The highest between-visit standard deviations for repeated measurements occurred 40° nasal (± 0.37 diopters) and 40° temporal (± 0.45 diopters) on the retina from the line of sight, with the standard deviations becoming smaller the closer they were to the line of sight. Using the largest standard deviation, a sample size of 25 subjects was adequate to detect a 0.25 diopter difference in defocus.
Analyses
Repeated-measures analyses of variance were used to compare relative peripheral refraction and relative peripheral defocus in each cohort. The on-eye contact lens defocus profile as measured by autorefraction at each retinal location, J0, and J45 were also analyzed. Benjamini-Hochberg adjusted post-hoc paired t-tests were performed when appropriate to test for differences in relative defocus between the uncorrected and corrected eye, and adjusted t-tests were performed to determine changes in defocus that were significantly different than zero at each retinal location caused by the contact lens optics after accounting for subjective over-refraction.
A repeated-measures analysis of variance was used to determine the effect of each contact lens on high- and low-contrast visual acuity when compared with the spherical equivalent refraction at the spectacle plane. Benjamini-Hochberg adjusted post-hoc paired t-tests were performed, when appropriate.
RESULTS
Comparison of Cohorts, Contact Lens Fit and Over-Refraction
Two cohorts of 25 subjects each were recruited. The mean (± standard deviation) age and spherical equivalent refraction of the right eye for cohort 1 was 23.9 ± 2.1 years and −2.71 ± 1.32 diopters, and for cohort 2 was 24.8 ± 2.6 years and −2.72 ± 1.69 diopters, respectively (all P ≥ .18). Relative peripheral refraction of the uncorrected eye was not different between the two cohorts (location by cohort interaction; P = .28). There was no difference in mean (± standard deviation) pupil size between the two cohorts (cohort 1 = 4.21 ± 0.13 mm; cohort 2 = 4.24 ± 0.10 mm; P = .84).
The average most plus spherical over-refraction required to optimize distance visual acuity with each lens and mean lens decentration are shown in Table 1. The mean over-refraction for each lens ranged from −0.30 diopters for the Biofinity D to −0.03 diopters for the NaturalVue Multifocal. All lenses showed adequate movement and centration. On average, none of the four lens brands were significantly decentered on eye (all P > .08).
Table 1.
Mean (± SD) most plus spherical over-refraction and lens decentration on eye for each multifocal contact lens tested. For decentration, a negative value indicates temporal decentration.
| Contact Lens | Over-refraction (diopters) | Decentration (mm) |
|---|---|---|
| Biofinity Multifocal D (+2.50 add) | −0.30 ± 0.24 | −0.17 ± 0.48 |
| Proclear Multifocal D (+2.50 add) | −0.16 ± 0.20 | −0.05 ± 0.62 |
| NaturalVue Multifocal | −0.03 ± 0.11 | −0.11 ± 0.39 |
| Clariti 1-Day Multifocal (high add) | −0.28 ± 0.26 | −0.14 ± 0.46 |
Visual Acuity
Best corrected high- and low-contrast visual acuity with each lens brand and when subjects were tested with their spherical equivalent in the spectacle plane are shown in Table 2. For the first cohort, which included spherical equivalent spectacle lens correction, Proclear Multifocal D, and Biofinity Multifocal D, the difference between high- and low-contrast visual acuity did not depend on the lens worn during vision testing (contrast by lens interaction; P = .10). Because this interaction between lens type and contrast level was not significant, individual post-hoc comparisons between each lens and contrast level combination were not conducted, and the main effect of lens (averaged across contrast levels) and the main effect of contrast (averaged across lens types) are instead reported. There was a main effect of contrast on visual acuity, with low-contrast acuity being on average (± standard deviation) 0.20 ± 0.05 logMAR worse than high-contrast acuity across all lenses (contrast main effect; P < .001). There were also statistically significant differences in visual acuity between the three lens corrections (lens main effect; P = .018). Independent of contrast level, visual acuity was on average 0.04 logMAR better with Proclear Multifocal D than with the spherical equivalent spectacle lens and the Biofinity Multifocal D contact lens (both adjusted P < .05); however, this two-letter difference is not clinically meaningful.
Table 2.
Mean (± SD) high- and low-contrast logMAR visual acuity (VA) with spherical equivalent spectacles and each of the tested multifocal contact lenses.
| High-Contrast VA | Low-Contrast VA | |
|---|---|---|
| Cohort 1 | ||
| Spherical equivalent spectacle | 0.01 ± 0.08 | 0.19 ± 0.10 |
| Proclear D Multifocal | −0.05 ± 0.07 | 0.17 ± 0.11 |
| Biofinity D Multifocal | −0.01 ± 0.09 | 0.21 ± 0.08 |
| Cohort 2 | ||
| Spherical equivalent spectacle | 0.04 ± 0.12 | 0.19 ± 0.15 |
| NaturalVue Multifocal | 0.02 ± 0.10 | 0.27 ± 0.12 |
| Clariti 1-Day Multifocal | 0.20 ± 0.10 | 0.40 ± 0.10 |
In our second cohort that included spherical equivalent spectacle lens correction, the NaturalVue Multifocal, and the Clariti 1-Day Multifocal (center-near), the difference between high- and low- contrast visual acuity did depend on the lens worn (contrast by lens interaction; P < .001). Despite best over-refraction, high-contrast visual acuity with the Clariti 1-Day Multifocal (high add) was on average 0.15 logMAR worse (1.5 lines) than with a spherical equivalent spectacle lens (P < .001). There was no difference in high-contrast visual acuity between the NaturalVue Multifocal and spherical equivalent spectacle lens (P = .35). On average, when compared to the spherical equivalent spectacle lens, low-contrast visual acuity was worse with both multifocal lenses (NaturalVue Multifocal worse by 0.08 logMAR and Clariti 1-Day Multifocal worse by 0.21 logMAR; both P < .05). In both instances, the center-near Clariti 1-Day Multifocal with high add resulted in the largest reduction in visual acuity.
Peripheral Defocus
In each cohort, there were differences between relative peripheral refraction of the uncorrected eye and relative peripheral defocus measured while wearing each contact lens that depended on the lens (condition × location interaction; both P < .001; Figure 1). Compared to uncorrected relative peripheral refraction, the Proclear Multifocal D caused significant myopic shifts in relative peripheral defocus at 40° nasal, 30° nasal, and 20° temporal on the retina ranging on average from −0.65 to −0.46 diopters (all P < .05; Figure 1A). The Biofinity Multifocal D caused significant myopic shifts in relative peripheral defocus at all retinal locations ranging on average from −0.83 to −0.61 diopters (all P < .05), with the exception of 20° nasal on the retina (Figure 1A). Compared to uncorrected relative peripheral refraction, the NaturalVue Multifocal caused an average myopic shift in relative defocus at 30° nasal on the retina of −0.51 diopters, and average hyperopic shifts at 40° nasal and 30° temporal ranging from +1.33 to +1.61 diopters (all P < .05; Figure 1B). The Clariti 1-Day (center-near) Multifocal caused average hyperopic shifts in relative defocus at all locations ranging from 0.21 to 1.16 diopters (all P < .05; Figure 1B), with the exception of the 10° nasal and 20° nasal locations where there was no significant difference in defocus.
Figure 1.
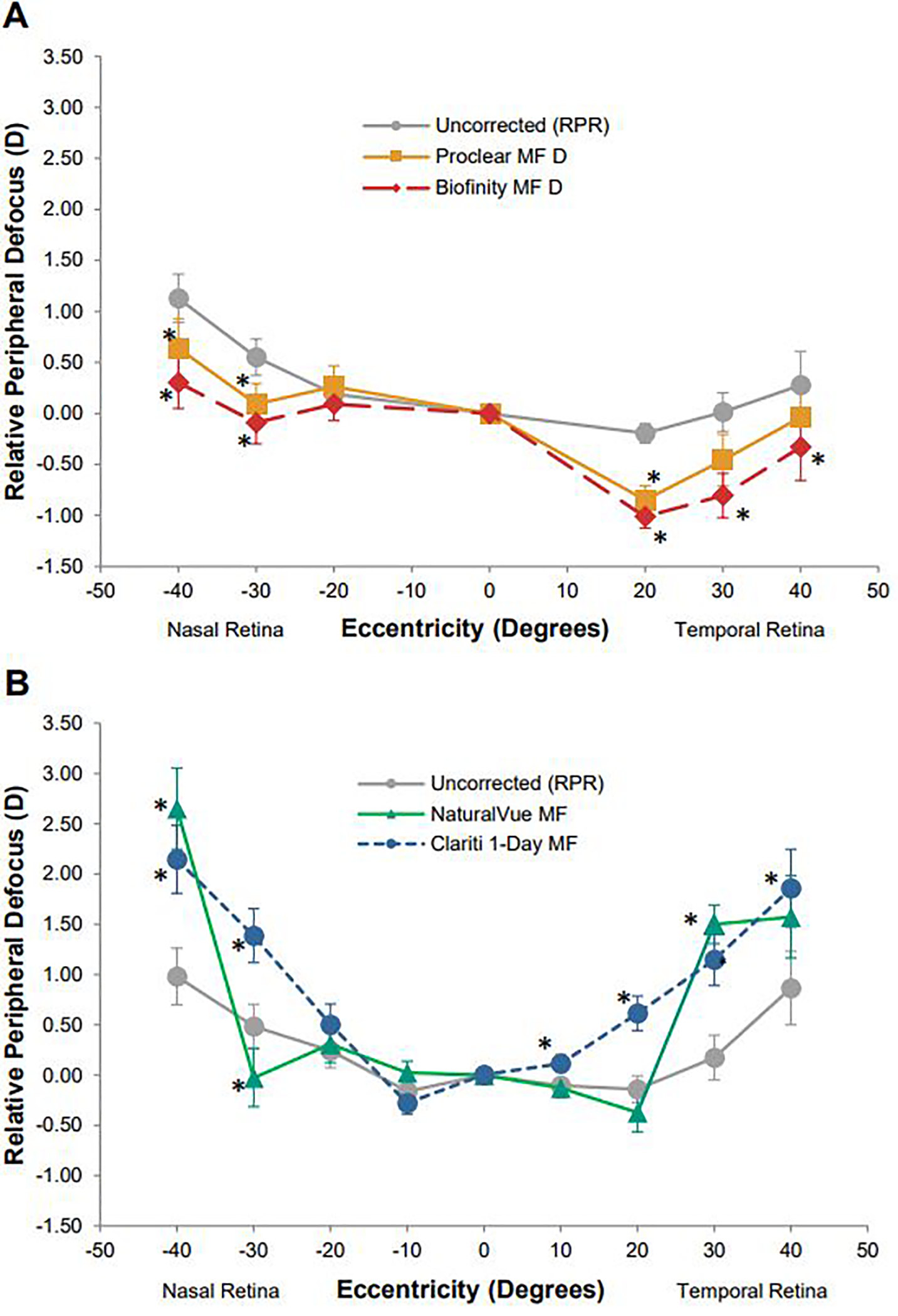
Relative peripheral defocus (measured by autorefraction) when wearing each contact lens and relative peripheral refraction of the unaided eye for A) cohort 1 wearing Biofinity Multifocal D and Proclear Multifocal D (both +2.50 diopter add powers) and B) cohort 2 wearing NaturalVue Multifocal and Clariti 1-Day Multifocal (high add). Error bars indicate the standard error. Asterisks indicate points where the relative peripheral defocus induced by a contact lens is significantly different than relative peripheral refraction of the unaided eye at that location (all P < .05).
The contact lens optical defocus profile (after accounting for over-refraction) as measured by autorefraction for each multifocal contact lens is shown in Figure 2. Zero in the figure represents a perfectly spherical image shell (i.e., an optical correction that fully eliminates central defocus but does not alter the shape of the peripheral defocus profile). The central values show defocus (M) measured by autorefraction with each multifocal lens after accounting for subjective spherical over-refraction. Despite subjects being well-corrected after over-refraction with all three center-distance multifocal designs (mean high-contrast acuity range: 0.02 logMAR to −0.05 logMAR; Table 2), a significant amount of myopic defocus caused by the contact lens optics along the line of sight was measured by autorefraction (i.e., the contact lenses optics resulted in the autorefractor measuring myopic defocus even after accounting for any subjective over-refraction required to maximize visual acuity). The average myopic defocus along the line of sight caused by the optics of the three center-distance multifocal contact lens designs ranged from −0.73 diopters to −0.89 diopters (all P < .001), showing simultaneous myopic defocus centrally on the retina from the multifocal contact lens optics. With the Clariti 1-Day center-near design, defocus along the line of sight was not significantly different than zero (P = .97)
Figure 2.
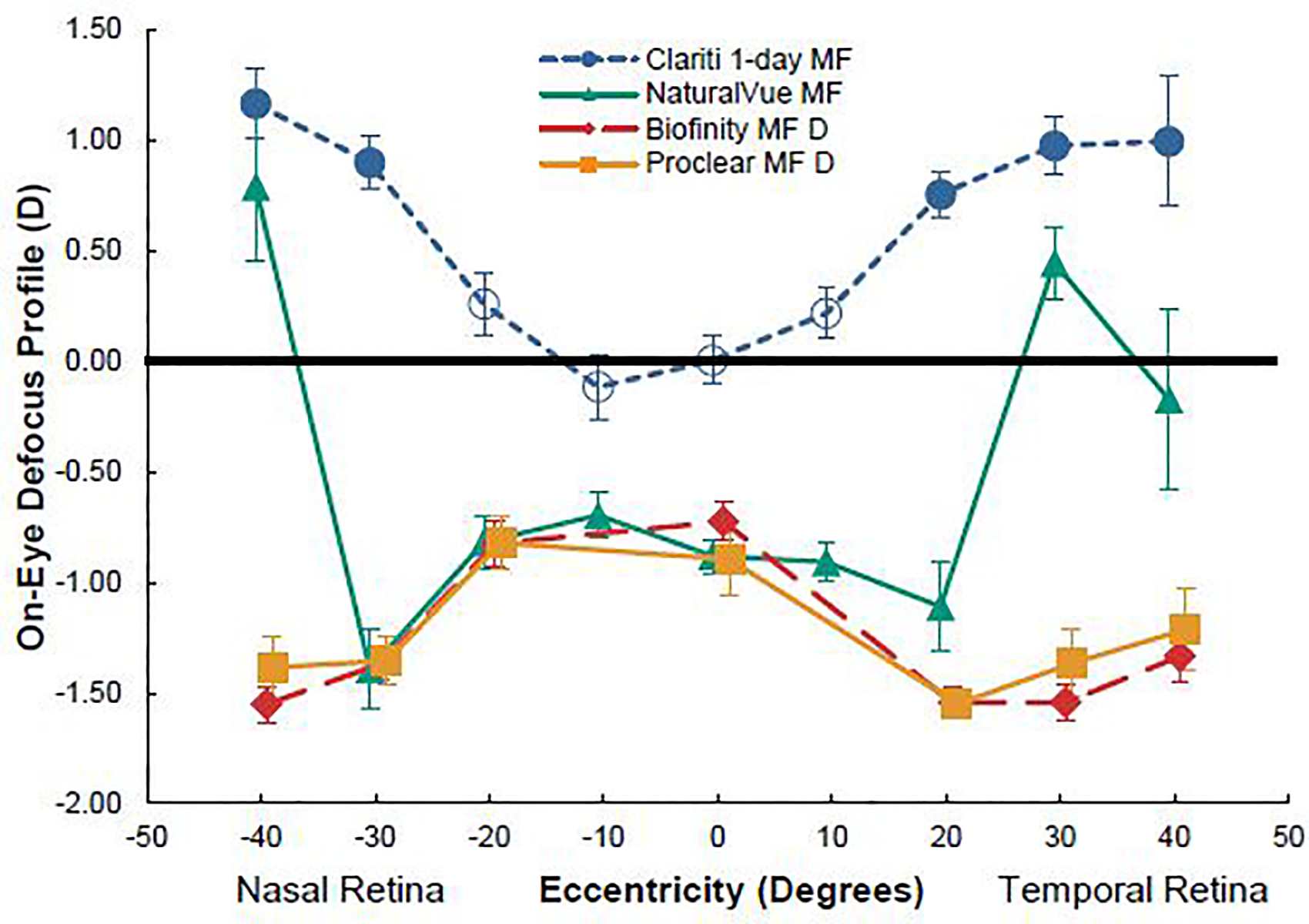
Contact lens optical defocus profile as measured by autorefraction when worn on eye (after accounting for any over-refraction). Open circles indicate points which were not significantly different from zero. The bold line at 0.00 D represents a spherical image shell normalized to the fovea.
Differences in the change in peripheral defocus caused by the multifocal contact lens optics between the center-near design and the three center-distance designs are quite apparent. For the Clariti 1-Day center-near multifocal, the changes in defocus caused by the lens optics were not different than zero across the central region from 20° nasal on the retina to 10° temporal on the retina, and were hyperopic at all more peripheral retinal locations measured (40° and 30° nasal, and 20°, 30°, 40° temporal; all P < .05). For all center-distance multifocal contact lenses, myopic changes in defocus were measured from 30° nasal to 20° temporal on the retina, including along the line of sight (Figure 2). While the Biofinity Multifocal D and the Proclear Multifocal D caused myopic changes in defocus at every retinal location measured, the NaturalVue Multifocal caused a hyperopic change in defocus at 40° nasal and 30° temporal on the retina (all P < .05) and no significant change in defocus 40° temporal on the retina.
J0 and J45 Astigmatism
In the first cohort, when evaluating differences in the amount of J0 astigmatism for uncorrected eyes and while wearing each of the contact lenses tested, there was a main effect of condition (P < .001; Figure 3A) that did not differ by retinal location (condition by location interaction; P = .09). J0 astigmatism with the Biofinity Multifocal D was (mean ± standard deviation) 0.14 ± 0.13 diopters greater than J0 of the uncorrected eye (P < .001), though this difference of less than 0.25 diopters is clinically small. There were no differences in J0 astigmatism between Proclear Multifocal D and the uncorrected eye. In the second cohort, there were differences in the amount of J0 between the uncorrected eye and when wearing each of the rotationally-symmetric contact lenses tested that depended on the retinal location measured (condition by location interaction; P < .001). For the NaturalVue Multifocal, there were two large positive changes in J0 astigmatism on average at 40° nasal and 30° temporal retina that ranged from 1.06 to 1.34 diopters, and there were much smaller (< 0.50 diopter) negative differences at 20° nasal and 10° temporal on the retina when compared to the uncorrected eye that were on average about −0.10 diopters (all P < .04; Figure 3B). Compared to the uncorrected eye, the center-near Clariti 1-Day Multifocal caused significant positive shifts in J0 astigmatism at multiple locations (all P < .001; Figure 3B), with the exception of the central, 10° nasal, 10° temporal, and 30° temporal retinal locations. The average differences in J0 astigmatism with the Clariti 1-Day Multifocal were generally small (0.50 diopters or less) versus some of the larger differences seen with the NaturalVue Multifocal.
Figure 3.
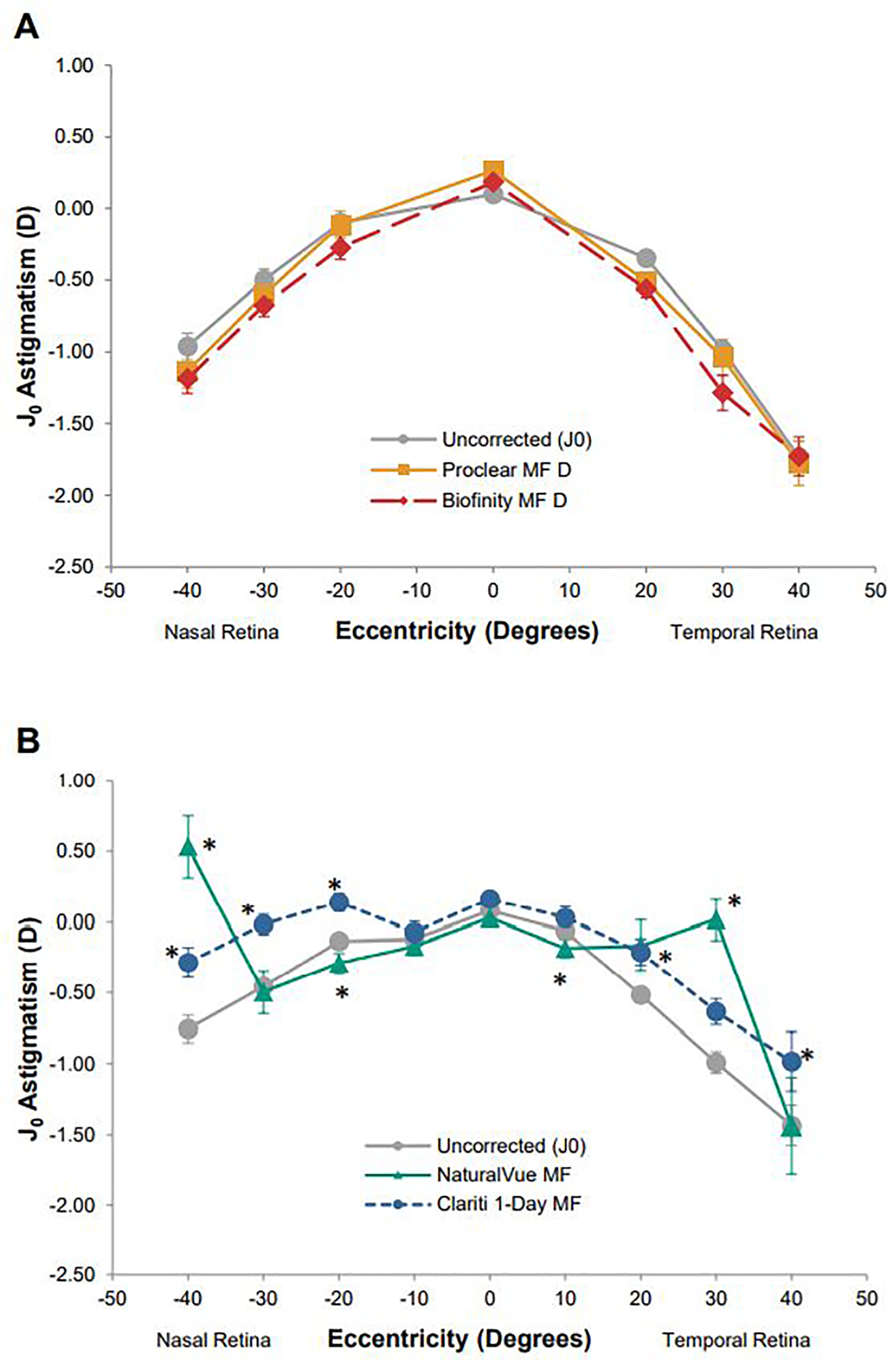
Average uncorrected J0 astigmatism and J0 astigmatism (as measured by autorefraction) when wearing each of the test contact lenses for A) cohort 1 wearing Biofinity Multifocal D and Proclear Multifocal D (both +2.50 diopter add powers) and B) cohort 2 wearing NaturalVue Multifocal and Clariti 1-Day Multifocal (high add). Error bars indicate standard error. Asterisks indicate points where J0 astigmatism while wearing a contact lens are significantly different than uncorrected J0 astigmatism at that location (all P < .05).
In both cohorts, when evaluating differences in the amount of J45 astigmatism between the uncorrected eye and while wearing each of the contact lenses tested, there was a significant interaction between condition and retinal location (condition by location interactions; both P < .007). For the first cohort, most changes caused by the lenses were clinically small (less than 0.50 diopters), with the largest change being 0.35 diopters at 20° nasal caused by the Proclear Multifocal D (P < .001; Figure 4A). Despite all changes being clinically small, the only locations without a significant difference in J45 astigmatism when wearing a study contact lens compared to the uncorrected eye were at 40° temporal and 40° nasal with the Biofinity Multifocal D. In cohort two, J45 differences when wearing the study contact lenses were again clinically small. Statistically significant, but small differences in J45 astigmatism with contact lenses compared to the uncorrected eye were only found centrally and at 20° and 10° temporal retina with the Clariti 1-Day Multifocal and at 10° temporal retina with the NaturalVue Multifocal (all P < .009, Figure 4B).
Figure 4.
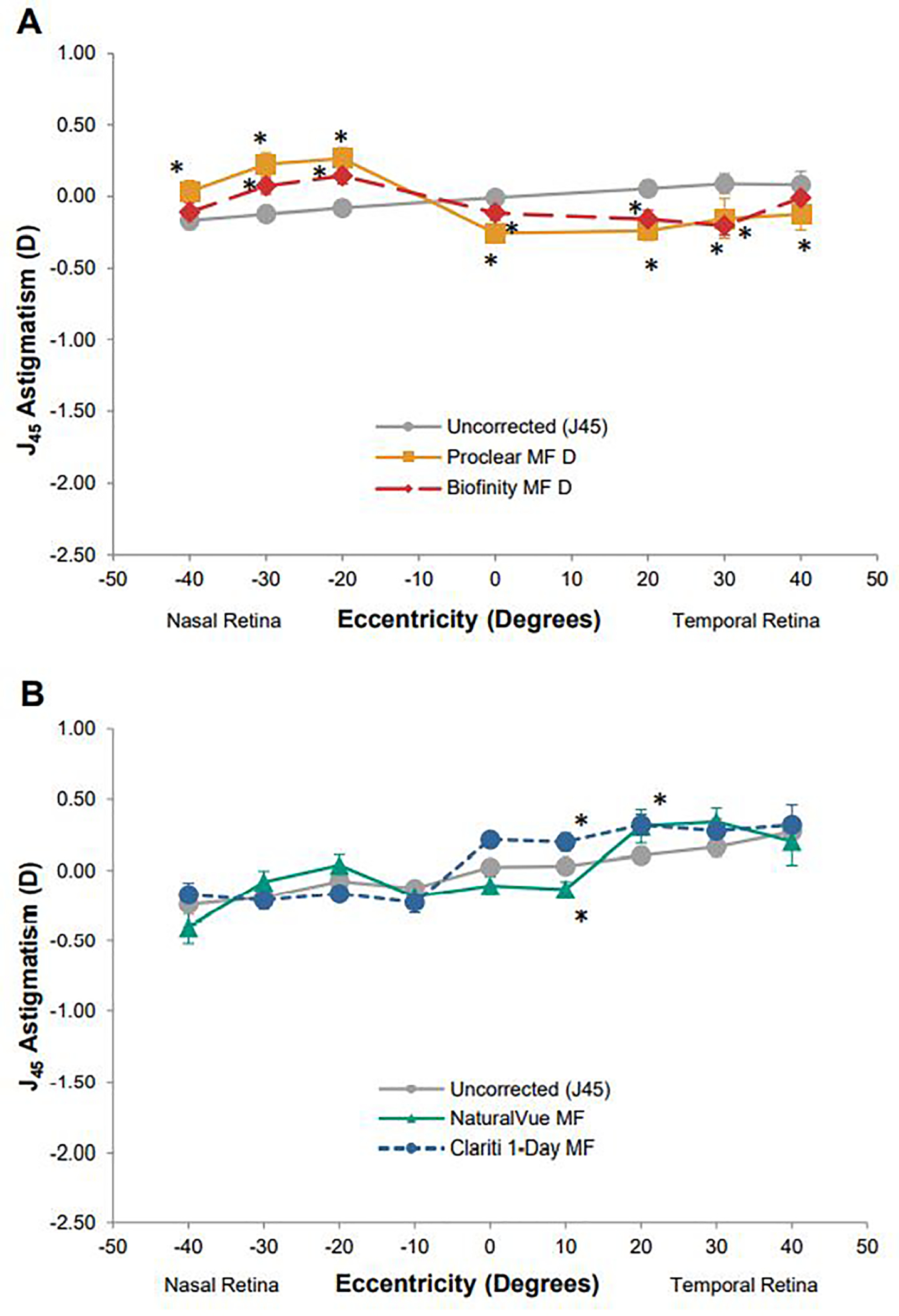
Average uncorrected J45 astigmatism and J45 astigmatism (as measured by autorefraction) when wearing each of the test contact lenses for A) cohort 1 wearing Biofinity Multifocal D and Proclear Multifocal D (both +2.50 diopter add powers) and B) cohort 2 wearing NaturalVue Multifocal and Clariti 1-Day Multifocal (high add). Error bars indicate standard error. Asterisks indicate points where J45 astigmatism induced by a contact lens are significantly different than uncorrected J45 astigmatism at that location (all P < .05).
DISCUSSION
Contact Lens Effects on Visual Acuity
Differences in visual acuity were found that depended on the contact lens design. A summary of published studies that have compared high- and low-contrast logMAR visual acuity with multifocal contact lenses versus control lenses (spherical contact lens or spectacles) is shown in Table 3.
Table 3.
Summary of research comparing logMAR Visual Acuity (VA) with multifocal contact lenses to a control lens (spherical contact lenses or spectacles). With the exception of Schulle et al. 2018 and Ruiz-Pomeda et al. 2018, all studies examined myopic adults. Over-refraction indicates if the authors reported measuring visual acuity after subjectively maximizing vision with an over-refraction.
| Multifocal Contact Lens | Add (D) | Control Lens | VA Reduction (logMAR) | Over-refraction | Citation |
|---|---|---|---|---|---|
| High-Contrast Visual Acuity | |||||
| Proclear D | High | Air Optix Aqua | 0.06 | No | Fedtke et al. 201628 |
| Proclear D | +3.00 | Proclear | 0.05 | No | Kang et al. 201727 |
| Proclear D | +2.00 | 1-Day Acuvue Moist | None | Yes | Diec et al. 201829 |
| Proclear D | +2.00 | Spectacles | None | Yes | Kollbaum et al. 201341 |
| Biofinity D | +2.50 | Spectacles | None | Yes | Schulle et al. 201826 |
| MiSight | +2.00 | Spectacles | None | Yes | Kollbaum et al. 201341 |
| MiSight | +2.00 | 1-Day Acuvue Moist | None | Yes | Diec et al. 201829 |
| MiSight | +2.00 | Air Optix Aqua | 0.05 | No | Fedtke et al. 201628 |
| MiSight | +2.00 | Spectacles | None | Yes | Ruiz-Pomeda et al. 201849 |
| Air Optix Multifocal* | High | Air Optix Aqua | 0.13 | No | Fedtke et al. 201628 |
| Proclear N* | High | Air Optix Aqua | 0.20 | No | Fedtke et al. 201628 |
| PureVision Multifocal* | High | Air Optix Aqua | 0.18 | No | Fedtke et al. 201628 |
| Low-Contrast Visual Acuity | |||||
| Proclear D | +3.00 | Proclear | 0.10 | No | Kang et al. 201727 |
| Proclear D | +2.00 | Spectacles | 0.06 | Yes | Kollbaum et al. 201341 |
| MiSight | +2.00 | Spectacles | 0.09 | Yes | Kollbaum et al. 201341 |
Indicates center-near multifocal design
In this study, the Clariti 1-Day multifocal center-near contact lens (high add) resulted in clinically meaningful reductions in high- and low-contrast logMAR visual acuity when compared with spherical equivalent lenses at the spectacle plane. Visual acuity in non-presbyopic subjects with center-near multifocal contact lenses is not widely reported in the literature. Fedtke et al. (2016) tested both center-near and center-distance multifocal contact lenses.28 The three center-near high-add multifocal designs they tested (PureVision Multifocal, AirOptix Aqua Multifocal, and Proclear Multifocal N) resulted in mean distance acuity reductions that ranged from 0.13 to 0.20 logMAR (a one- to two-line reduction) compared with a spherical contact lens. Though Fedtke et al. reported smaller reductions in visual acuity with low-add center-near multifocals, we chose a high add for the center-near Clariti 1-Day Multifocal in our study due to the suggestion that higher add powers are more efficacious for myopia control and to ensure a more equal comparison of changes in retinal defocus across center-distance and center-near multifocal lens designs.
Fedtke et al. also reported statistically significant, but clinically small, three-letter reductions in high-contrast visual acuity with the center-distance Proclear Multifocal D “high add” and the MiSight lens design compared to a spherical contact lens; however, both multifocal lenses were reported to have reduced subjective visual performance, as assessed by a participant questionnaire after one hour of wearing the lens monocularly. As one might expect, the authors found that better vision was achieved with lower add multifocals than with higher add powers.28
Using a similar contact lens to the Proclear Multifocal D, a recent study by Schulle et al. found no significant difference in high-contrast visual acuity with the Biofinity Multifocal D (+2.50 add) compared to full spectacle correction in 294 myopic children.26 A 2018 study of the Proclear Multifocal D contact lens (+2.00 add) also did not find a significant difference in high-contrast visual acuity compared to a spherical control; however, they did report a reduction in subjective visual quality with the multifocal after a five-day period of wear.29 In 2013, Kollbaum et al. compared standard spectacle correction to the Proclear Multifocal D (+2.00 add) and found that the multifocal had no effect on high-contract visual acuity; however, reductions in subjective visual performance and a reduction in low-illumination low-contrast visual acuity of approximately one line was found versus spectacle correction.41 Kang et al. compared both high- and low-contrast visual acuity with the Proclear Multifocal D (+3.00 add) to a Proclear spherical contact lenses. The +3.00 add Proclear Multifocal reduced high-contrast visual acuity by roughly two letters and low-contrast visual acuity by four letters. Additionally, the Proclear Multifocal D (+3.00 add) reduced subjective visual quality at both the dispense visit and the two-week follow-up.27 A two-year clinical trial by Sankaridurg et al. randomly assigned myopic children to one of four multifocal lenses, two different center-distance multifocal designs each with a lower and higher add power, or a single vision contact lens control group. They reported statistically significant reductions in high-contrast visual acuity for three of the four specialty multifocal contact lenses. These reductions were all less than 0.10 logMAR, with two lenses causing changes of less than 0.05 logMAR. All four multifocal lenses reduced low-contrast visual acuity by 0.11 to 0.19 logMAR (one to two lines) compared to the spherical contact lens group.42 Collectively, these studies found that high-add center-distance contact lenses provide similar high-contrast visual acuity to standard corrections, while generally reducing low-contrast visual acuity by approximately one line.
Consistent with previous studies, we did not find a clinically meaningful difference in high-contrast visual acuity between the Proclear Multifocal D (+2.50 add), Biofinity Multifocal D (+2.50 add), or NaturalVue Multifocal when compared to spherical equivalent spectacle correction. For low-contrast visual acuity, we did not find a significant difference between spherical equivalent spectacle correction and either the Proclear Multifocal D or Biofinity Multifocal D. We did find a roughly one-line reduction in low-contrast visual acuity with the NaturalVue Multifocal, which agrees with the low-contrast results of Kang et al.27 and Sankaridurg et al.42
It is unclear why we did not measure a reduction in low-contrast visual acuity with the Proclear Multifocal D or the Biofinity Multifocal D, both fit on cohort 1, when compared to spherical equivalent spectacles, as other studies have reported roughly one-line reductions (three or more letters) in low-contrast acuity with these multifocal designs. The mean age, refractive error, and pupil size (4.21 mm) were the same between the two cohorts tested in this research. The same experimental setup was used to test both cohorts with lens randomization, and the mean spherical equivalent spectacle corrected low-contrast visual acuity in both cohorts was the same (0.19 logMAR). The mean over-refraction for each multifocal was also similar (0.30 D or less). Certain aberration modes can combine to improve or reduce visual performance.43 Both the Proclear D and Biofinity D Multifocal lenses have a similar design. One potential hypothesis for the lack of reduced low-contrast acuity with these multifocals could involve the specific design of these center-distance lenses. The central 3 mm diameter of these two lenses contain distance power, with plus power not being introduced until outside this 3 mm diameter.24, 30 In contrast, plus power is reported to begin increasing more rapidly and near the center of the lens with the center-distance NaturalVue Multifocal design,30 increasing the amount of plus power within the average pupil size measured. A second hypotheses is that the subjects’ own ocular aberrations in cohort one on average combined with the multifocal in a way that resulted in improved visual quality. Future studies would be needed to test this hypothesis. Consistent with Fedtke et al.,28 we did find that the high-add center-near multifocal design caused a significant reduction in high-contrast visual acuity. Additionally, we found that the high-add center-near multifocal contact lens tested reduced low-contrast visual acuity by more than two lines.
Contact Lens Effects on Defocus
The center-near Clariti 1-Day Multifocal design caused more hyperopic defocus with increased eccentricity (Figure 2). Despite the plus power in the center of the optic zone, on average, no central myopic defocus was measured by autorefraction in these non-presbyopic subjects after subjective over-refraction was accounted for in the autorefractor measurements. At least with this specific center-near multifocal design, the over-refraction required to best correct distance visual acuity resulted in the overall image shell being shifted in the hyperopic direction, increasing hyperopic defocus. Previous research with different center-near multifocals also found peripheral hyperopic shifts in defocus. In 2017, Fedtke et al. evaluated three center-near multifocals (Proclear Multifocal N, PureVision Multifocal, and Air Optix Aqua Multifocal). Like our results, each lens caused peripheral hyperopic shifts in defocus. However, unlike our results, Fedtke et al. reported relative myopic shifts in defocus centrally. In their study, they did not state whether an over-refraction was performed when fitting each lens, which could account for the differences between our studies. They also used an aberrometer, the Brien Holden Vision Institute EyeMapper, to measure peripheral refraction versus the autorefractor utilized in our study.44 Differences in the operating principals and sampling between these instruments, differences in the lens designs tested in each study, and differences in the contact lens fitting and over-refraction methods between studies could account for the disparity in the measurement of central myopic defocus between studies. The strong peripheral hyperopic defocus found in our data demonstrates the potential to increase hyperopic defocus when trying to optimize visual acuity when using a center-near design in a non-presbyope. The center-near defocus profile of the Clariti 1-Day would not be conducive to slowing myopia progression based on the myopic defocus hypothesis of slowing eye growth.11
All three center-distance multifocal contact lenses caused myopic defocus centrally, as measured by autorefraction, while also providing good high-contrast visual acuity. While the Proclear Multifocal D and Biofinity Multifocal D demonstrated similar peripheral myopic changes in defocus (Figure 1A and Figure 2), the NaturalVue Multifocal had a unique profile. The NaturalVue Multifocal caused a myopic change in defocus centrally (from 30° nasal to 20° temporal on the retina) but hyperopic changes in defocus in the periphery at 40° nasal and 30° temporal on the retina (Figure 1B and 2). This on-eye defocus profile has been partially replicated in recently published research.34 Jaisankar et al. reported a hyperopic shift in relative peripheral refraction with the NaturalVue Multifocal lens at 35° on the temporal retina.34 No hyperopic shift was reported on the peripheral nasal retina; however, they measured out to 35° while our study measured out to 40°. Differences in lens centration between studies could also account for the difference in power profile between studies. Since spherical contact lens designs are rotationally symmetric, it would be expected that any hyperopic change present temporally should also be present nasally. Based on recently published power profiles of the NaturalVue Multifocal showing more negative power at the edge of the optic zone than in the center of the lens, the nasal and temporal hyperopic peripheral defocus changes we found are likely due to characteristics of the lens design.30
According to the manufacturer, the NaturalVue Multifocal design has an increase in plus power of +8 to +11 diopters near the center of the lens (US patents 6474814, 7178918).33–35 This central increase in plus power was not detected in our data. The Grand Seiko autorefractor used to measure refractive values in this study has an analysis beam diameter of 2.3mm;45 therefore, instrument resolution limits could have masked detection of rapid power changes present in this particular lens design.
The implication of the hyperopic and myopic changes in defocus with the NaturalVue Multifocal as it pertains to the potential efficacy of the lens design for slowing myopia progression is not known. Based on animal models, when eyes are exposed to regions of hyperopic and myopic defocus simultaneously, eye growth is guided by the most myopic defocus present. In infant macaque monkeys presented with two planes of competing defocus, eyes typically grow toward the more myopic image plane,46 even when the myopic defocus is only one-fifth of the total area of the lens.47 This relationship has also been reported in marmosets.48 Recently published data on the MiSight lens, a center-distance dual-focus lens design, suggests that human eyes may also respond to the more myopic image plane.21, 49 Retrospective data published in which myopic children were fitted with the NaturalVue Multifocal suggest the lens design may slow progression,33 though a randomized controlled clinical trial is needed to confirm this finding.
For both the Biofinity Multifocal D and the Proclear Multifocal D, the myopic changes in relative peripheral defocus found in our study agree with previously published profiles.18, 50 In a two-year, non-randomized study, the Proclear Multifocal D resulted in a 29% reduction in myopia progression (based on axial length changes) when compared with matched historical controls.23 A recently published three-year randomized clinical trial, the Bifocal Lenses In Nearsighted Kids (BLINK) Study, found that the +2.50 add Biofinity Multifocal D significantly slowed myopia progression in children compared to both spherical soft contact lenses or a +1.50 add.51, 52 There have also been several studies of various duration investigating the effect of non-commercially available (novel) center-distance contact lens designs on myopia progression in children that have all reported various levels of success in slowing axial elongation.53–55 Together these studies indicate that center-distance multifocal contact lenses like the Proclear Multifocal D and the Biofinity Multifocal D can slow myopia progression when compared to single vision contact lenses or spectacles.
Looking only at the central defocus values measured by autorefraction along the line of sight, the center-near Clariti 1-Day Multifocal was not significantly different than zero (Figure 2). On average, the center-distance lenses all had central myopic defocus changes which ranged on average from −0.73 to −0.89 diopters after accounting for subjective over-refraction (Figure 2). While this may initially appear to represent uncorrected myopia, these central myopic changes were measured after accounting for the over-refraction necessary to optimize distance acuity, with subjects on average seeing 0.02 logMAR (20/20) or better. This central myopic defocus measured with center-distance designs could be explained by the instrument design of the Grand Seiko autorefractor utilized in this study. The Grand Seiko determines refractive error using a 2.3mm diameter annulus.45 The measured central myopic change could partially be due to the autorefractor’s measurement beam measuring through initial increases in plus power in the center-distance lenses as you move away from the center of the contact lens optic zone. Other potential factors involve the interaction of each subject’s own higher-order aberrations, pupil size, and the contact lens aberrations on overall image quality when determining the most plus over-refraction each subject selected that provided best distance visual acuity with each contact lens design. It is possible that some residual myopic defocus remained centrally with the center-distance designs, despite the participant having best distance acuity, due to the way in which the lens optics interacted with the eye’s optics and pupil size. The interaction of these same factors could also potentially explain the difference in over-refraction and measured central refractive error with the center-near design. How the eye weighs paraxial versus marginal rays will also influence a subject’s selections to optimize visual acuity during over-refraction. Future studies measuring aberrations with these lenses could further explore the effects of these lenses on objectively measured and subjective image quality.
When looking at the effects these contact lenses have on J0 and J45 astigmatism, the results for the Biofinity Multifocal D found in this study (Figures 3A and 4A, respectively) agree with previously published profiles.18 Similarly, the changes in J0 and J45 astigmatism induced by the Proclear Multifocal D also agree with previously published profiles.34, 50 Temporal retinal changes in J0 astigmatism induced by the NaturalVue Multifocal (Figure 3B) were comparable with profiles published by Jaisankar et al;34 however, the nasal retinal J0 astigmatism changes they reported in their study do not completely match those found in our work. We found a positive change in J0 astigmatism in the nasal retinal periphery that they did not. Differences in lens centration and the maximum eccentricity of measurement may again explain differences between our studies. That said, changes in J45 astigmatism was small and similar between their study and ours (Figure 4B).
Study Limitations
A study limitation is that the changes in defocus were measured on young myopic adults as opposed to myopic children; however, the changes in retinal defocus caused by the lens optics are expected to be similar since the anterior segment of the eye upon which the contact lens is fitted reaches adult dimensions at roughly two years of age.56 The changes in defocus are also unique to the specific contact lenses measured. Contact lens designs other than those tested in this study would be expected to influence defocus differently. The average contact lens optical defocus profile as measured by autorefraction (after accounting for over-refraction) is also reported in this study. It is important for clinicians to note that the actual defocus experienced by a specific eye will depend on the baseline ocular shape of the eye since some eyes have more relative peripheral hyperopia than others due to variability across eyes. Measuring retinal defocus is the only way to definitively know the amount of defocus the eye is experiencing while wearing a contact lens, but these measurements are unfortunately not quickly obtained with currently available commercial instruments. The choice of autorefractor can also influence defocus measurements. The Grand Seiko measures over a 2.3mm diameter annulus, while other instruments may utilize the entire pupil when measuring refractive error. Due to the complexity of multifocal optics, the instrument measurement characteristics can influence the defocus measurements obtained.
In order to maximize repeatability of peripheral autorefraction, eyes were cyclopleged before autorefraction measurements. Despite performing an over-refraction that utilized maximum plus to best visual acuity prior to cycloplegia, it is possible that some residual accommodation might have remained after over-refraction that had the subject not been cyclopleged, might have altered the final autorefraction defocus readings. This study also did not evaluate the effects accommodation may have had on visual acuity or the defocus profiles of these lenses when looking at near. Accommodation has been hypothesized to affect myopia control efficacy with multifocal contact lenses. In one study, higher levels of accommodation when wearing multifocal lenses were associated with slower myopia progression.57 Additionally, the shape of the defocus profile is known to change in the far periphery due to accommodation; viewing a near target with accommodation causes a myopic change in the defocus profile shape in the far periphery (roughly 40 degrees or more from the line of sight) when wearing either spherical or multifocal contact lenses.18 Further work is needed to understand the effect of different center-distance multifocal contact lens designs on accommodation, the resulting near defocus profile, and their overall influence on myopia progression in children.
This study examined visual acuity in young myopic adults and the lenses were not dispensed. It is possible that myopic children wearing these lenses for longer periods of time might adapt to the aberrations of these lenses resulting in improvements in visual acuity over time.58 If that is the case, these results may underestimate the ultimate vision achieved. It is important for clinical trials determining the efficacy of any contact lens for myopia control in children to measure and report the long-term effects of any optical device on high- and low-contrast vision and other functional measures of vision that can be affected, such as reading speed.59
CONCLUSIONS
Overall, center-distance multifocal contact lenses induced myopic defocus in most peripheral locations. The center-near lens induced hyperopic defocus in most peripheral locations and did not cause any myopic changes in defocus. Additionally, the high add center-near lens tested, unlike the high add center-distance lenses, significantly degraded both high- and low-contrast visual acuity when compared to spherical equivalent spectacles. These effects on vision and defocus do not support the use of center-near lenses for myopia control. This study directly compared the visual acuity and defocus profiles out to 40 degrees eccentricity of three commercially-available center-distance multifocal contact lenses that are being used off-label in the US for myopia management using the same methodology. Information is also included on the NaturalVue Multifocal, for which there are little published data. Further work is needed to determine whether differences in the center-distance multifocal lens design influence myopia progression.
ACKNOWLEDGEMENTS
NIH/NEI grant support: T35 EY007088 and P30 EY07551. The authors thank Eric Ritchey, OD, PhD, for his assistance in figure design and Julia Benoit, PhD, for statistical advice. These data were presented, in part, at the annual meeting of the American Academy of Optometry (Orlando 2019).
Footnotes
Conflict of Interest Disclosure: No financial support was received from a corporate entity for this study. DAB serves on an advisory board for Visioneering Technologies, Inc. and receives contact lens solution from Bausch + Lomb for a National Institutes of Health–funded clinical trial.
REFERENCES
- 1.Holden B, Sankaridurg P, Smith E, et al. Myopia, an Underrated Global Challenge to Vision: Where the Current Data Takes Us on Myopia Control. Eye (Lond) 2014;28:142–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016;123:1036–42. [DOI] [PubMed] [Google Scholar]
- 3.Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and Associated Pathological Complications. Ophthalmic Physiol Opt 2005;25:381–91. [DOI] [PubMed] [Google Scholar]
- 4.Flitcroft DI. The Complex Interactions of Retinal, Optical and Environmental Factors in Myopia Aetiology. Prog Retin Eye Res 2012;31:622–60. [DOI] [PubMed] [Google Scholar]
- 5.Cho BJ, Shin JY, Yu HG. Complications of Pathologic Myopia. Eye Contact Lens 2016;42:9–15. [DOI] [PubMed] [Google Scholar]
- 6.Liu HH, Xu L, Wang YX, et al. Prevalence and Progression of Myopic Retinopathy in Chinese Adults: The Beijing Eye Study. Ophthalmology 2010;117:1763–8. [DOI] [PubMed] [Google Scholar]
- 7.Wang NK, Chen YP, Lai CC, et al. Paediatric Retinal Detachment: Comparison of High Myopia and Extreme Myopia. Br J Ophthalmol 2009;93:650–5. [DOI] [PubMed] [Google Scholar]
- 8.Bullimore MA, Brennan NA. Myopia Control: Why Each Diopter Matters. Optom Vis Sci 2019;96:463–5. [DOI] [PubMed] [Google Scholar]
- 9.Smith EL 3rd, Hung LF, Arumugam B. Visual Regulation of Refractive Development: Insights from Animal Studies. Eye (Lond) 2014;28:180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charman WN, Radhakrishnan H. Peripheral Refraction and the Development of Refractive Error: A Review. Ophthalmic Physiol Opt 2010;30:321–38. [DOI] [PubMed] [Google Scholar]
- 11.Smith EL 3rd. Prentice Award Lecture 2010: A Case for Peripheral Optical Treatment Strategies for Myopia. Optom Vis Sci 2011;88:1029–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wallman J, Gottlieb MD, Rajaram V, Fugate-Wentzek LA. Local Retinal Regions Control Local Eye Growth and Myopia. Science 1987;237:73–7. [DOI] [PubMed] [Google Scholar]
- 13.Smith EL 3rd, Hung LF, Huang J, Arumugam B. Effects of Local Myopic Defocus on Refractive Development in Monkeys. Optom Vis Sci 2013;90:1176–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu Y, Wildsoet C. The Effect of Two-Zone Concentric Bifocal Spectacle Lenses on Refractive Error Development and Eye Growth in Young Chicks. Invest Ophthalmol Vis Sci 2011;52:1078–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith EL 3rd, Hung LF, Huang J. Relative Peripheral Hyperopic Defocus Alters Central Refractive Development in Infant Monkeys. Vision Res 2009;49:2386–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin Z, Martinez A, Chen X, et al. Peripheral Defocus with Single-Vision Spectacle Lenses in Myopic Children. Optom Vis Sci 2010;87:4–9. [DOI] [PubMed] [Google Scholar]
- 17.Moore KE, Benoit JS, Berntsen DA. Spherical Soft Contact Lens Designs and Peripheral Defocus in Myopic Eyes. Optom Vis Sci 2017;94:370–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berntsen DA, Kramer CE. Peripheral Defocus with Spherical and Multifocal Soft Contact Lenses. Optom Vis Sci 2013;90:1215–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (Romio) Study: A 2-Year Randomized Clinical Trial. Invest Ophthalmol Vis Sci 2012;53:7077–85. [DOI] [PubMed] [Google Scholar]
- 20.Aller TA, Liu M, Wildsoet CF. Myopia Control with Bifocal Contact Lenses: A Randomized Clinical Trial. Optom Vis Sci 2016;93:344–52. [DOI] [PubMed] [Google Scholar]
- 21.Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A 3-Year Randomized Clinical Trial of Misight Lenses for Myopia Control. Optom Vis Sci 2019;96:556–67. [DOI] [PubMed] [Google Scholar]
- 22.Lam CS, Tang WC, Tse DY, et al. Defocus Incorporated Soft Contact (Disc) Lens Slows Myopia Progression in Hong Kong Chinese Schoolchildren: A 2-Year Randomised Clinical Trial. Br J Ophthalmol 2014;98:40–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal Contact Lens Myopia Control. Optom Vis Sci 2013;90:1207–14. [DOI] [PubMed] [Google Scholar]
- 24.Kim E, Bakaraju RC, Ehrmann K. Power Profiles of Commercial Multifocal Soft Contact Lenses. Optom Vis Sci 2017;94:183–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fedtke C, Ehrmann K, Bakaraju RC. Peripheral Refraction and Spherical Aberration Profiles with Single Vision, Bifocal and Multifocal Soft Contact Lenses. J Optom 2020;13:15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schulle KL, Berntsen DA, Sinnott LT, et al. Visual Acuity and over-Refraction in Myopic Children Fitted with Soft Multifocal Contact Lenses. Optom Vis Sci 2018;95:292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kang P, McAlinden C, Wildsoet CF. Effects of Multifocal Soft Contact Lenses Used to Slow Myopia Progression on Quality of Vision in Young Adults. Acta Ophthalmol 2017;95:e43–e53. [DOI] [PubMed] [Google Scholar]
- 28.Fedtke C, Bakaraju RC, Ehrmann K, et al. Visual Performance of Single Vision and Multifocal Contact Lenses in Non-Presbyopic Myopic Eyes. Cont Lens Anterior Eye 2016;39:38–46. [DOI] [PubMed] [Google Scholar]
- 29.Diec J, Tilia D, Thomas V, Bakaraju RC. Predicting Short-Term Subjective Vision Performance of Contact Lenses Used in Myopia Control. Eye Contact Lens 2018;44:308–15. [DOI] [PubMed] [Google Scholar]
- 30.Nti AN, Ritchey ER, Berntsen DA. Power Profiles of Centre-Distance Multifocal Soft Contact Lenses. Ophthalmic Physiol Opt 2021;41:393–400. [DOI] [PubMed] [Google Scholar]
- 31.Gordon MO, Schechtman KB, Davis LJ, et al. Visual Acuity Repeatability in Keratoconus: Impact on Sample Size. Collaborative Longitudinal Evaluation of Keratoconus (Clek) Study Group. Optom Vis Sci 1998;75:249–57. [DOI] [PubMed] [Google Scholar]
- 32.Moore KE, Berntsen DA. Central and Peripheral Autorefraction Repeatability in Normal Eyes. Optom Vis Sci 2014;91:1106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper J, O’Connor B, Watanabe R, et al. Case Series Analysis of Myopic Progression Control with a Unique Extended Depth of Focus Multifocal Contact Lens. Eye Contact Lens 2018;44:e16–e24. [DOI] [PubMed] [Google Scholar]
- 34.Jaisankar D, Leube A, Gifford KL, et al. Effects of Eye Rotation and Contact Lens Decentration on Horizontal Peripheral Refraction. Ophthalmic Physiol Opt 2019;39:370–7. [DOI] [PubMed] [Google Scholar]
- 35.Visioneering Technologies Inc. (VTI). The Science of Natural Vision Meets the Science of Naturalvue® Multifocal. Available at https://vtivision.com/practitioner/products/multifocal/.Accessed: June 18, 2021.
- 36.El-Nimri NW, Walline JJ. Centration and Decentration of Contact Lenses During Peripheral Gaze. Optom Vis Sci 2017;94:1029–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lopes-Ferreira DP, Neves HI, Faria-Ribeiro M, et al. Peripheral Refraction with Eye and Head Rotation with Contact Lenses. Cont Lens Anterior Eye 2015;38:104–9. [DOI] [PubMed] [Google Scholar]
- 38.Fedtke C, Ehrmann K, Ho A, Holden BA. Lateral Pupil Alignment Tolerance in Peripheral Refractometry. Optom Vis Sci 2011;88:E570–9. [DOI] [PubMed] [Google Scholar]
- 39.Thibos LN, Wheeler W, Horner D. Power Vectors: An Application of Fourier Analysis to the Description and Statistical Analysis of Refractive Error. Optom Vis Sci 1997;74:367–75. [DOI] [PubMed] [Google Scholar]
- 40.Mutti DO, Hayes JR, Mitchell GL, et al. Refractive Error, Axial Length, and Relative Peripheral Refractive Error before and after the Onset of Myopia. Invest Ophthalmol Vis Sci 2007;48:2510–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kollbaum PS, Jansen ME, Tan J, et al. Vision Performance with a Contact Lens Designed to Slow Myopia Progression. Optom Vis Sci 2013;90:205–14. [DOI] [PubMed] [Google Scholar]
- 42.Sankaridurg P, Bakaraju RC, Naduvilath T, et al. Myopia Control with Novel Central and Peripheral Plus Contact Lenses and Extended Depth of Focus Contact Lenses: 2 Year Results from a Randomised Clinical Trial. Ophthalmic Physiol Opt 2019;39:294–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Applegate RA, Marsack JD, Ramos R, Sarver EJ. Interaction between Aberrations to Improve or Reduce Visual Performance. J Cataract Refract Surg 2003;29:1487–95. [DOI] [PubMed] [Google Scholar]
- 44.Fedtke C, Ehrmann K, Thomas V, Bakaraju RC. Peripheral Refraction and Aberration Profiles with Multifocal Lenses. Optom Vis Sci 2017;94:876–85. [DOI] [PubMed] [Google Scholar]
- 45.Fedtke C, Ehrmann K, Holden BA. A Review of Peripheral Refraction Techniques. Optom Vis Sci 2009;86:429–46. [DOI] [PubMed] [Google Scholar]
- 46.Arumugam B, Hung LF, To CH, et al. The Effects of Simultaneous Dual Focus Lenses on Refractive Development in Infant Monkeys. Invest Ophthalmol Vis Sci 2014;55:7423–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arumugam B, Hung LF, To CH, et al. The Effects of the Relative Strength of Simultaneous Competing Defocus Signals on Emmetropization in Infant Rhesus Monkeys. Invest Ophthalmol Vis Sci 2016;57:3949–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Benavente-Perez A, Nour A, Troilo D. The Effect of Simultaneous Negative and Positive Defocus on Eye Growth and Development of Refractive State in Marmosets. Invest Ophthalmol Vis Sci 2012;53:6479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ruiz-Pomeda A, Perez-Sanchez B, Valls I, et al. Misight Assessment Study Spain (Mass). A 2-Year Randomized Clinical Trial. Graefes Arch Clin Exp Ophthalmol 2018;256:1011–21. [DOI] [PubMed] [Google Scholar]
- 50.Kang P, Fan Y, Oh K, et al. The Effect of Multifocal Soft Contact Lenses on Peripheral Refraction. Optom Vis Sci 2013;90:658–66. [DOI] [PubMed] [Google Scholar]
- 51.Walline JJ, Walker MK, Mutti DO, et al. Effect of High Add Power, Medium Add Power, or Single-Vision Contact Lenses on Myopia Progression in Children: The BLINK Randomized Clinical Trial. JAMA 2020;324:571–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Walline JJ, Gaume Giannoni A, Sinnott LT, et al. A Randomized Trial of Soft Multifocal Contact Lenses for Myopia Control: Baseline Data and Methods. Optom Vis Sci 2017;94:856–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fujikado T, Ninomiya S, Kobayashi T, et al. Effect of Low-Addition Soft Contact Lenses with Decentered Optical Design on Myopia Progression in Children: A Pilot Study. Clin Ophthalmol 2014;8:1947–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paune J, Morales H, Armengol J, et al. Myopia Control with a Novel Peripheral Gradient Soft Lens and Orthokeratology: A 2-Year Clinical Trial. Biomed Res Int 2015;2015:507572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sankaridurg P, Holden B, Smith E 3rd, et al. Decrease in Rate of Myopia Progression with a Contact Lens Designed to Reduce Relative Peripheral Hyperopia: One-Year Results. Invest Ophthalmol Vis Sci 2011;52:9362–7. [DOI] [PubMed] [Google Scholar]
- 56.Wolff E, Last RJ. Anatomy of the Eye and Orbit, Including the Central Connections, Development, and Comparative Anatomy of the Visual Apparatus, 6th ed. London,: H. K. Lewis; 1968. [Google Scholar]
- 57.Cheng X, Xu J, Brennan NA. Accommodation and Its Role in Myopia Progression and Control with Soft Contact Lenses. Ophthalmic Physiol Opt 2019;39:162–71. [DOI] [PubMed] [Google Scholar]
- 58.Sawides L, de Gracia P, Dorronsoro C, et al. Adapting to Blur Produced by Ocular High-Order Aberrations. J Vis 2011;11:21, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wolffsohn JS, Kollbaum PS, Berntsen DA, et al. IMI - Clinical Myopia Control Trials and Instrumentation Report. Invest Ophthalmol Vis Sci 2019;60:M132–M60. [DOI] [PubMed] [Google Scholar]


