Abstract
Calcific tendonitis of the gluteus medius and minimus tendons is a rare complication of hydroxyapatite deposition disease, with bilateral involvement even more so. Although patients can be asymptomatic, there is often an acute-on-chronic presentation of pain. We present a case of bilateral calcific tendonitis of the gluteus medius and minimus tendons on a background of previous bilateral rotator cuff calcific tendonitis in a middle-aged woman. This patient's long-standing history of multi-focal involvement required a multidisciplinary approach between orthopedics, rheumatology, and musculoskeletal radiology for optimal management, requiring different treatment options for different affected sites.
Keywords: Calcific, Tendonitis, Musculoskeletal, Gluteus, Tendinopathy
Introduction
Hydroxyapatite deposition disease (HADD) is a crystal arthropathy that can cause a wide spectrum of presentations including tendinopathy, bursitis and acute arthritis. Calcific tendonitis affecting the rotator cuff is a well-recognized complication of HADD however implication of the gluteus medius and minimus tendons is rare [1,2]. Patients will typically present with acute non-traumatic lateral hip pain usually on a background of previous episodes. Multiple, current or historic joint involvement is common and identified in approximately 50% of patients [3]. Treatment is aimed at symptomatic relief and ranges from simple analgesia, physiotherapy, ultrasound-guided intervention to arthroscopic removal.
Patient history and examination
This 51-year-old lady of Middle Eastern origin, presented to orthopedic clinic with severe sharp pain affecting the outer aspect of her right hip. Symptoms started suddenly one week prior to clinical presentation without any preceding trauma. The pain affected her walking and she had attempted to control her symptoms with over-the-counter nonsteroidal anti-inflammatories (NSAIDs). On clinical examination both hips demonstrated an excellent range of motion. There was no tenderness on spinal palpation. The right hip was warm and tender to touch. Pain was elicited at the right hip on performance of FABER test.
The patient had previously been investigated for bilateral hip pain a year ago, and review of previous radiographs demonstrated areas of calcification projecting at the greater trochanters. The patient also reported a previous history of left shoulder calcific tendonitis (Fig. 1) five years prior, which was treated with a bursal steroid injection. Two years prior to that she had an episode of right shoulder calcific tendonitis, which was treated, with arthroscopic removal of the calcifications.
Fig. 1.
AP projection radiograph of the right shoulder showing a large calcific deposit projecting over the site of the supraspinatus tendon (arrows) in keeping with calcific tendonitis.
A diagnosis of acute-on-chronic right calcific trochanteric bursitis was suspected. Repeat plain radiographs were requested to assess for interval change in the one year interval. The patient was advised to use a stick to offload the right hip muscles for 10 days and prescribed regular NSAIDs for the pain. The patient was also referred to the radiology department for ultrasound-guided barbotage of the calcification and steroid bursal injection.
Investigation and treatment
Routine blood tests and metabolic screen demonstrated normal renal function and bone profile with normal vitamin D levels at 58 nmol/l. Repeat radiographs of the right hip demonstrated patchy calcification at the gluteus medius insertion and trochanteric bursa (Fig. 2). Similar appearances were demonstrated on the asymptomatic left hip. Ultrasound of the right hip demonstrated a large focus of calcification within the gluteus medius and minimus tendons measuring up to 2.5 cm in maximal dimension (Fig. 3).
Fig. 2.
AP projection radiograph of the pelvis showing bilateral large deposits projecting at the insertion of the gluteus medius and minimus tendons as well as trochanteric bursa (arrows).
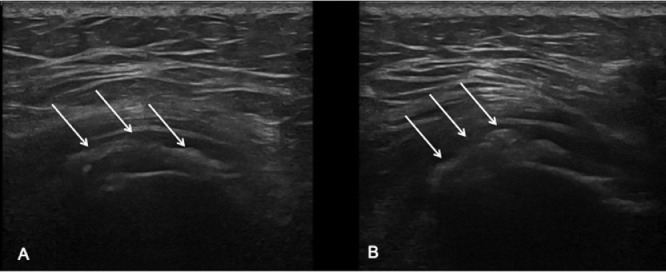
Fig. 3.
Ultrasound images of the right hip. Image A is in the transverse plane and Image B in the longitudinal plane. Large hyperechoic foci are projecting over the tendons (arrows) in keeping with calcific deposits with overlying hypoechoic rim in keeping with secondary bursitis.
The tendons demonstrated intrasubstance hypoechogenicity in keeping with secondary tendinopathy with excess fluid within the trochanteric bursa in keeping with bursitis. Ultrasound guided barbotage and steroid injection of the trochanteric bursa with 40 mg Kenalog and 5 mL of 0.5% levobupivacaine was performed and provided symptomatic relief (Fig. 4).
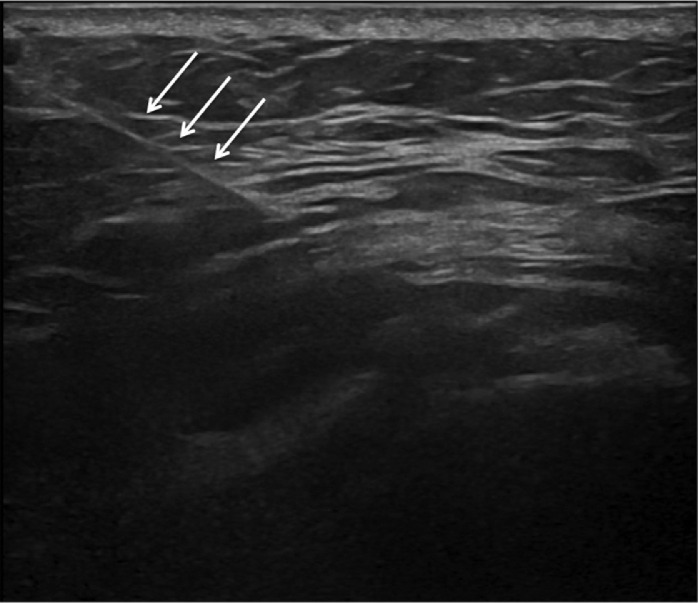
Fig. 4.
Ultrasound image of the right hip showing the ultrasound guided intervention. The needle (arrows) is guided to the level of the calcification to perform barbotage of the deposits.
Outcomes and follow-up
The patient had an excellent response to treatment with near-complete resolution of her symptoms on review after the ultrasound guided intervention.
Discussion
Crystal deposition disease refers to a spectrum of conditions induced by cellular reaction and inflammation due to deposition of microcrystals [4]. Gout, calcium pyrophosphate dihydrate (CPPD) and calcium hydroxyapatite deposition disease (HADD) are the most common crystal arthropathies. Calcium hydroxyapatite crystals can be deposited in the tendons, joints, periarticular soft tissues and bursae leading to a spectrum of symptoms secondary to bursitis, tendonitis or acute arthritis [5].
There is no gender predilection and patients will typically present between the ages of 40–70 [6]. Although the underlying etiology of HADD is not fully understood, aspiration of these deposits reveals needle-like crystals on microscopy which stain purple with Wright's stain [7]. There are well recognized associations with connective tissue disorders, renal osteodystrophy and recurrent steroid injections [8]. The majority of patients are asymptomatic with up to 45% presenting with clinical symptoms [6]. Typically HADD presents as a severely painful monoarticular arthropathy, but can be polyarticular with multiple joint involvement demonstrated in approximately 50% of patients [3]. Calcific tendonitis refers to tendinous deposition and most commonly implicates the supraspinatus tendon of the shoulders [1]. Cases affecting the gluteal muscle tendons are rare with reports of dual involvement of the gluteus medius and minimus tendon insertions more so [2]. When the hips are involved, deposits are often seen in the gluteus medius and minimus tendinous insertions as well as the associated trochanteric bursae [9].
Calcific tendonitis of the gluteal muscles typically presents acutely with non-traumatic pain along the lateral aspect of the hip [10]. Pathophysiologically the pain is thought to be due to the rupture of calcium deposits [11]. The differential diagnoses at presentation are causes of acute monoarthropathy such as gout, CPPD or septic arthritis.
Plain radiography early in the disease process demonstrates cloud-like calcification, which becomes more dense and focal with time, as in our case. The calcification is often centered on the joint capsule, closely applied tendons or within bursae [12]. The deposits are not always seen on radiography and are often better localized on ultrasound or MRI. CT is not commonly performed, but may demonstrate focal deposits conforming to the contour of the affected tendon, often described flame-shaped or comet-tail configuration, and may also demonstrate evidence of secondary cortical erosions [13,14]. On MRI, bony erosions at tendinous and ligamentous insertions may be seen, and associated bone marrow edema appearing as hyperintense signal. Calcific deposits can be more challenging to visualize on MRI and appear as well defined areas of hypointense signal on T1 and T2 weighted sequences. Ultrasound is primarily used in HADD to identify the location of the calcific deposits and to enable image guided intervention. On ultrasound the calcific foci are hyperechoic with posterior acoustic shadowing. Surrounding Doppler flow and associated edema or effusion suggest secondary inflammation, correlating accurately to the site of pain [15].
When symptomatic, treatment is aimed at relieving the associated pain. Over-the-counter analgesia, non-steroidal anti-inflammatories, physiotherapy and local steroid injections are established strategies [16]. If symptoms are ongoing and the calcific deposits are large, ultrasound-guided barbotage or arthroscopic removal may be required [2,17,18]. In our case, ultrasound-guided barbotage with steroid injection proved therapeutic.
Patient consent statement
The authors hereby confirm that written, informed consent for publication of the patient's case was obtained from the patient.
Footnotes
Competing interests: None.
References
- 1.Siegal DS, Wu JS, Newman JS, del Cura JL, Hochman MG. Calcific tendinitis: a pictorial review. Can Assoc Radiol J. 2009;60(5):263–272. doi: 10.1016/j.carj.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Kandemir U, Bharam S, Philippon MJ, Fu FH. Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthrosc J Arthrosc Relat Surg. 2003;19(1):4. doi: 10.1053/jars.2003.50021. [DOI] [PubMed] [Google Scholar]
- 3.Winn RS, Melhorn JM, De Smet AA. Layering of calcifications in synovial effusions. J Can Assoc Radiol. 1981;32(1):66–68. [PubMed] [Google Scholar]
- 4.Choi MH, MacKenzie JD, Dalinka MK. Imaging features of crystal-induced arthropathy. Rheum Dis Clin North Am. 2006;32(2):427–446. doi: 10.1016/j.rdc.2006.04.001. viii. [DOI] [PubMed] [Google Scholar]
- 5.Schumacher HR, Cherian PV, Reginato AJ, Bardin T, Rothfuss S. Intra-articular apatite crystal deposition. Ann Rheum Dis. 1983;42(suppl 1):54–59. doi: 10.1136/ard.42.suppl_1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amor B, Cherot A, Delbarre F, Nunez Roldan A, Hors J. Hydroxyapatite rheumatism and HLA markers. J Rheumatol Suppl. 1977;3:101–104. [PubMed] [Google Scholar]
- 7.Faure G, Daculsi G. Calcified tendinitis: a review. Ann Rheum Dis. Aug 1983;42(suppl 1):49–53. doi: 10.1136/ard.42.suppl_1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dalinka MK, Stewart V, Bomalaski JS, Halpern M, Kricun ME. Periarticular calcifications in association with intra-articular corticosteroid injections. Radiology. 1984;153(3):615–618. doi: 10.1148/radiology.153.3.6494459. [DOI] [PubMed] [Google Scholar]
- 9.Wepfer JF, Reed JG, Cullen GM, McDevitt WP. Calcific tendinitis of the gluteus maximus tendon (gluteus maximus tendinitis) Skelet Radiol. 1983;9(3):198–200. doi: 10.1007/BF00352555. [DOI] [PubMed] [Google Scholar]
- 10.Grimaldi A, Mellor R, Hodges P, Bennell K, Wajswelner H, Vicenzino B. Gluteal tendinopathy: a review of mechanisms, assessment and management. Sports Med. 2015;45(8):1107–1119. doi: 10.1007/s40279-015-0336-5. [DOI] [PubMed] [Google Scholar]
- 11.HK Uhthoff, JW Loehr. Calcific tendinopathy of the rotator cuff: pathogenesis, diagnosis, and management. J Am Acad Orthop Surg. 1997;5(4):183–191. doi: 10.5435/00124635-199707000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Malghem J, Omoumi P, Lecouvet F, Vande Berg B. Intraosseous migration of tendinous calcifications: cortical erosions, subcortical migration and extensive intramedullary diffusion, a SIMS series. Skelet Radiol. 2015;44(10):1403–1412. doi: 10.1007/s00256-015-2165-x. [DOI] [PubMed] [Google Scholar]
- 13.Mizutani H, Ohba S, Mizutani M, Otake S, Otsuka T, Nakamura T. Calcific tendinitis of the gluteus maximus tendon with cortical bone erosion: CT findings. J Comput Assist Tomogr. 1994;18(2):310–312. doi: 10.1097/00004728-199403000-00030. [DOI] [PubMed] [Google Scholar]
- 14.Hayes CW, Rosenthal DI, Plata MJ, Hudson TM. Calcific tendinitis in unusual sites associated with cortical bone erosion. AJR Am J Roentgenol. 1987;149(5):967–970. doi: 10.2214/ajr.149.5.967. [DOI] [PubMed] [Google Scholar]
- 15.Zufferey P, So A. A pilot study of IL-1 inhibition in acute calcific periarthritis of the shoulder. Ann Rheum Dis. 2013;72(3):465–467. doi: 10.1136/annrheumdis-2012-202380. [DOI] [PubMed] [Google Scholar]
- 16.Almedghio S, Garneti N. The acute and chronic presentation of gluteus medius calcific tendinitis—a case report of two. J Orthop Case Rep. 2014;4(4):48–50. doi: 10.13107/jocr.2250-0685.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin W, Liu C-Y, Tang C-L, Hsu C-H. Acupuncture and small needle scalpel therapy in the treatment of calcifying tendonitis of the gluteus medius: a case report. Acupunct Med J Br Med Acupunct Soc. 2012;30(2):142–143. doi: 10.1136/acupmed-2012-010149. [DOI] [PubMed] [Google Scholar]
- 18.Jo H, Kim G, Baek S, Park H-W. Calcific tendinopathy of the gluteus medius mimicking lumbar radicular pain successfully treated with barbotage: a case report. Ann Rehabil Med. 2016;40(2):368–372. doi: 10.5535/arm.2016.40.2.368. [DOI] [PMC free article] [PubMed] [Google Scholar]