Abstract
Acute compartment syndrome (ACS) of the lower extremity is a surgical emergency, often secondary to severe crush injury, and requires immediate fascial release. In treatment of ACS, the underlying fascia is left unrepaired and the subsequent fascial defect does not generally cause negative consequences. Here, we present a 24-year-old man who developed symptomatic muscle herniation 3-years after undergoing fascial release secondary to ACS of the anterior thigh. Given the size of the defect, reconstruction was performed using Acellular Dermal Matrix (ADM). The patient did well, with no complications 6 months postoperatively. Symptomatic muscle herniation following fasciotomy can be treated with hernia reduction and fascial repair. When primary closure is not possible, Acelluar Dermal Matrix (ADM) is an option for successful fascial reconstruction.
Keywords: Acute compartment syndrome, Fasciotomy, Thigh hernia, Acellular dermal matrix, Lower extremity trauma
Introduction
ACS is a surgical emergency requiring immediate fascial release to avoid irreversible muscle ischemia and subsequent myonecrosis [1]. ACS is primarily a clinical diagnosis but can be confirmed with manometry [1]. Patients treated promptly often go on to experience full recovery with little functional deficit [1].
The management of the resulting surgical wound after release varies. In almost all patients with ACS of the extremities, the fascia and skin are left open initially to ensure the compartment syndrome is adequately treated [1]. Later, the skin is closed either primarily if swelling permits or using a skin graft to cover exposed muscle [2]. In some instances, patients may be managed with a negative pressure dressing as a bridge to primary closure or as a means to accelerate closure by secondary intention [3].
In these closure techniques, little thought is given to the consequence of leaving the fascia unrepaired after initial release. In this case report, the authors present a patient who suffered symptomatic muscle herniation as a late presenting sequela of ACS of the anterior thigh. We discuss the diagnosis of this rare complication and critical considerations in its surgical management.
Case report
A healthy 24-year-old man presented to our office for evaluation of a painful mass on the left thigh. The patient had a notable history of ACS following a crush injury to his left lower extremity due to an ATV accident in 2018. At his initial injury, the patient suffered no fractures, but he had severe tenderness along the anterior compartment of the left thigh as well as a tense compartment. As a result, the patient urgently underwent fasciotomies of the thigh compartments.
During the original procedure, both the anterior and posterior thigh compartments were released using a lateral and posterior incision. After release, the thigh musculature appeared viable and the thigh was soft. The patient was managed in a delayed fashion with eventual skin closure one week later. Following surgery, the patient had no motor or sensory deficits, cleared physical therapy, and reported feeling well.
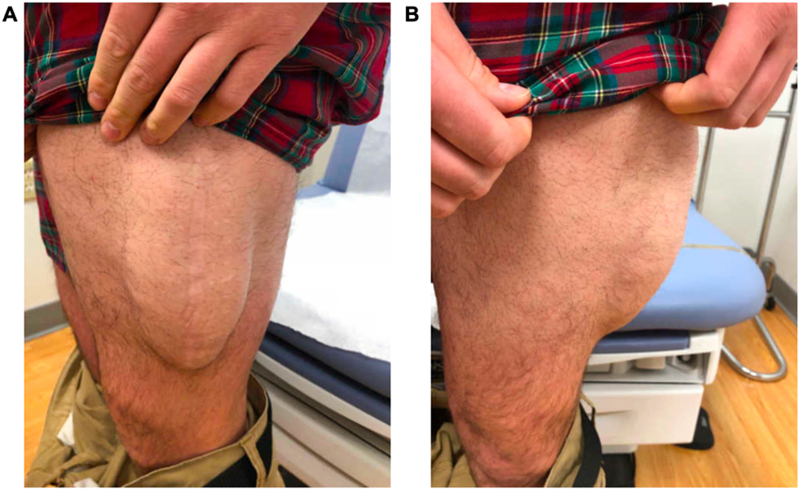
Approximately three years later, the patient returned with a painful mass along his left thigh at the site of his anterior thigh fasciotomy. He reported pain with walking and exercise. Physical exam revealed bulging at the periphery of the vastus lateralis muscle at the mid-thigh (Fig. 1). This finding was highly suggestive for muscle herniation at his previous fasciotomy site and was confirmed with a computed tomography (CT) scan.
Fig. 1.
Thigh hernia at site of anterior compartment fasciotomy.
A. Left leg lateral view B. Left leg anterior view.
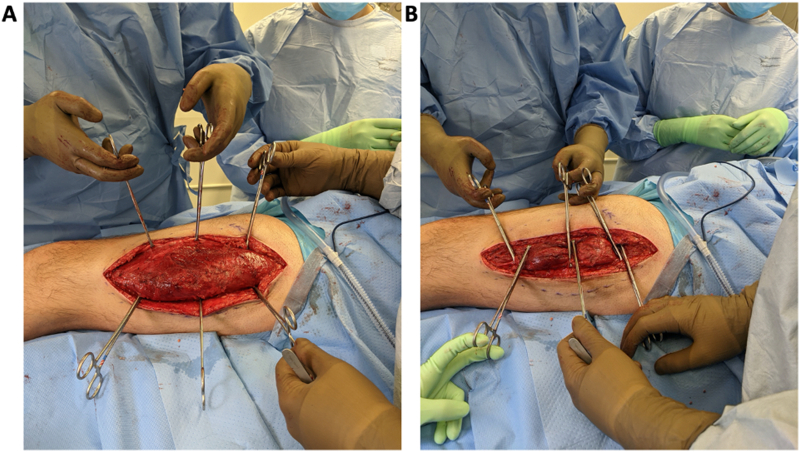
Because of the patient's considerable symptoms, surgical intervention was planned. In the operating room (OR), the previous incision was opened and dissection was carried down to the anterolateral thigh compartment, where we uncovered an area of muscle herniation which corresponded to his bulge on physical exam (Fig. 2A). The entire fascial defect measured 5 cm × 24 cm and was too large to close primarily (Fig. 2B). As a result, the decision was made to reconstruct the defect with acellular dermal matrix (ADM). The fascia was freed from the surrounding muscle, and a sheet of ADM, measuring 10 cm × 24 cm, was secured in an underlay fashion with two rows of sutures. (Fig. 3). A temporary drain was placed above the newly reconstructed fascia, and the skin was closed in a layered fashion.
Fig. 2.
A. Intraoperative photo of fascial defect B. Attempted primary closure of fascial defect.
Fig. 3.

Fascial defect after reconstruction with acellular dermal matrix (ADM).
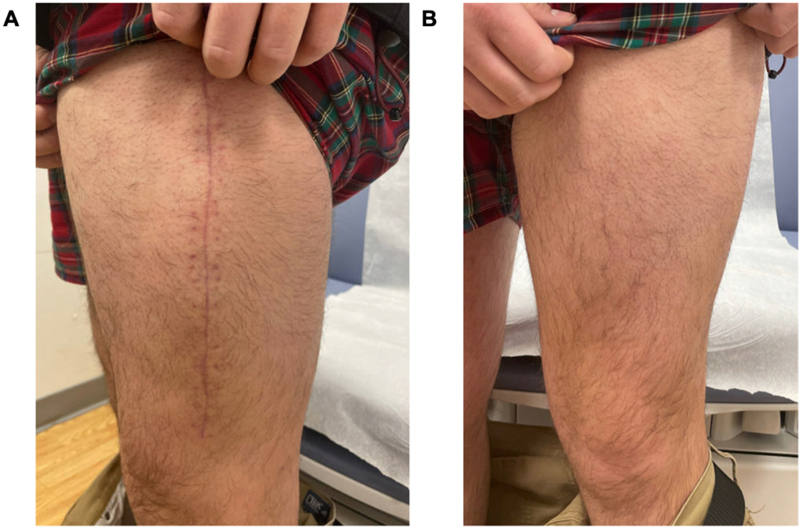
The patient did well post-operatively: he no longer had evidence of thigh muscle herniation, and his overall thigh contour was significantly improved (Fig. 4). The patient expressed resolution of his pain and his functional limitations. He worked with physical therapy and has since returned to full activity without any complications 6 months postoperatively.
Fig. 4.
Postoperative follow up with resolution of hernia bulge.
A. Left leg lateral view B. Left leg anterior view, both 6.5 weeks postoperative.
Discussion
The standard treatment for ACS is fasciotomy to prevent ischemic injury, loss of limb, and even mortality [1]. Wound closure practices vary by case; however, most often the fascia is left open to prevent recurrence [1]. The most frequent sequalae associated with fasciotomy following ACS are neurologic deficits, dry skin and pruritis [1], [4].
Muscle herniation in the leg occurs at fascial defects and often presents as chronic leg pain and neuropathy [5]. Herniation can cause chronic exertional compartment syndrome (CECS) in the lower extremities [5]. The unique aspect of this case is the occurrence of symptomatic thigh muscle herniation following fasciotomy for ACS – a post-surgical complication rarely reported in the literature.
Few studies exist describing this complication in detail, primarily because the enlarged opening following fasciotomy is believed to eliminate the risk of subsequent muscle herniation. Still, Fitzgerald et al. (2000) reported a 60 patient 8-year retrospective analysis of fasciotomy wounds and noted 13% of patients developed muscle herniation following fasciotomy [4]. Importantly, this study does not detail whether any of the herniations were symptomatic or how they were treated.
In our case, the patient's symptoms included significant pain, precluding him from performing his occupation. Thus, we pursued surgical management to reduce his pain and risk of recurrent compartment syndrome, as well as improve his stability and mobility [5]. One surgical approach to symptomatic lower extremity herniation after fasciotomy is a second fasciotomy to enlarge the initial fascial defect. This may decrease risk of recurrent compartment syndrome and ischemia to the herniated muscle [5]. Still, incomplete pain resolution and poor cosmetic outcomes are disadvantages to this approach [5]. Furthermore, pain is frequently exacerbated upon exertion, a concern for patients like ours who live active lifestyles.
Anatomical repair of the fascial defect is another potential approach. In this scenario, primary closure is often ideal to restore normal functional anatomy [6]. In our patient, primary closure was not possible because of the size of the defect. One solution here would be the use of a synthetic bridging mesh [7]. These meshes may be absorbable or permanent and offer strong tensile strength when utilized to close a fascial defect [8]. Even so, they are prone to inflammation, cannot reintegrate into the existing tissue, and often lead to hernia recurrence [7].
ADM is a newer alternative that avoids many of the pitfalls of synthetic mesh. It acts as a scaffold, allowing tissue remodeling, collagen deposition, and neovascularization [8]. In the case of symptomatic herniation, ADM may be placed beneath the fascial defect and sutured to the surrounding fascia in an underlay fashion [5]. In turn, better cosmetic outcomes and reduction of pain are seen at the edges of the defect [2].
ADM is most often used in abdominal hernias but has successfully been used for symptomatic herniation in the lower extremity, forearm, hiatal, and inguinal region [2], [6], [8], [9], [10]. In addition to improved aesthetic outcomes, patients are often able to resume active lifestyles after surgery [6]. Given the infrequency of lower extremity symptomatic herniation, few cases exist documenting adverse effects of ADM in this site. When ADM is used in abdominal hernia, Misra et al. (2008) found the most common adverse effects to be hernia recurrence (20%), graft infection (2.8%), and graft rejection (1.4%), most often occurring within a year of initial repair [8], [11]. As such, one limitation to this report is the lack of one year follow-up and the potential for complications to arise in the future.
Conclusion
In this report, the authors present a rare but important possible complication of fasciotomy for ACS. Patients presenting with increased pain and functional limitations at their fasciotomy sites may have symptomatic muscle herniation and, importantly, can be effectively treated with hernia reduction and fascial repair. Providers should consider ADM as a possible option in fascial reconstruction when primary closure is not possible.
Declaration of competing interest
None of the authors have conflicts of interest to disclose.
Acknowledgements
None.
References
- 1.Ojike N.I., Roberts C.S., Giannoudis P.V. Compartment syndrome of the thigh: a systematic review. Injury. 2010;41:133–136. doi: 10.1016/j.injury.2009.03.016. [DOI] [PubMed] [Google Scholar]
- 2.Maj E., Martell B.Kakar, Muschett D., Armstrong M. Facs, lower extremity fascial reconstruction using an acellular dermal matrix graft. Wounds. 2009;21 [PubMed] [Google Scholar]
- 3.Krticka M., Ira D., Bilik A., Rotschein P., Svancara J. Fasciotomy closure using negative pressure wound therapy in lower leg compartment syndrome. Bratisl. Lek. Listy. 2016;117:710–714. doi: 10.4149/BLL_2016_136. [DOI] [PubMed] [Google Scholar]
- 4.Fitzgerald A., Wilson Y., Quaba A., Gaston P., McQueen M. Long-term sequelae of fasciotomy wounds. Br. J. Plast. Surg. 2000;53:690–693. doi: 10.1054/bjps.2000.3444. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen J.T., Nguyen J.L., Wheatley M.J., Nguyen T.A. Muscle hernias of the leg: a case report and comprehensive review of the literature. Can. J. Plast. Surg. 2013;21:243–247. [PMC free article] [PubMed] [Google Scholar]
- 6.Kozlow J.H., Beil R.J., Chung K.C. Repair of symptomatic forearm hernias using acellular dermal matrix–two case reports. J. Hand Surg. Am. 2010;35:2053–2056. doi: 10.1016/j.jhsa.2010.07.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.FitzGerald J.F., Kumar A.S. Biologic versus synthetic mesh reinforcement: what are the pros and cons? Clin. Colon Rectal Surg. 2014;27:140–148. doi: 10.1055/s-0034-1394155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Misra S., Raj P.K., Tarr S.M., Treat R.C. Results of AlloDerm use in abdominal hernia repair. Hernia. 2008;12:247–250. doi: 10.1007/s10029-007-0319-z. [DOI] [PubMed] [Google Scholar]
- 9.Ward K.C., Costello K.P., Baalman S., Pierce R.A., Deeken C.R., Frisella M.M., Michael Brunt L., Matthews B.D. Effect of acellular human dermis buttress on laparoscopic hiatal hernia repair. Surg. Endosc. 2015;29:2291–2297. doi: 10.1007/s00464-014-3946-3. [DOI] [PubMed] [Google Scholar]
- 10.Albo D., Awad S.S., Berger D.H., Bellows C.F. Decellularized human cadaveric dermis provides a safe alternative for primary inguinal hernia repair in contaminated surgical fields. Am. J. Surg. 2006;192:e12–e17. doi: 10.1016/j.amjsurg.2006.08.029. [DOI] [PubMed] [Google Scholar]
- 11.Brunbjerg M.E., Jensen T.B., Christiansen P., Overgaard J., Damsgaard T.E. Reinforcement of the abdominal wall with acellular dermal matrix or synthetic mesh after breast reconstruction with the pedicled transverse rectus abdominis musculocutaneous flap. A prospective double-blind randomized study. J. Plast. Surg. Hand Surg. 2020:1–8. doi: 10.1080/2000656X.2020.1856673. [DOI] [PubMed] [Google Scholar]