Abstract
This study compares the diagnostic accuracy of magnetic resonance myelography with computed tomography myelography for the identification of spinal cerebrospinal fluid leaks.
Spontaneous intracranial hypotension (SIH) is an important cause of headaches. For the initial evaluation of patients with suspected SIH, post-myelography computed tomography (CT myelography or CTM) has long been considered the gold standard for the detection of cerebrospinal fluid (CSF) leaks,1 but spine magnetic resonance imaging including heavily T2-weighted magnetic resonance myelography (MRM) may be a noninvasive alternative.2,3,4 We compared the diagnostic accuracy of MRM with CTM for the identification of spinal CSF leaks.
Methods
This study was approved by the Cedars-Sinai Medical Center institutional review board.
Using a prospectively maintained registry, we identified all patients with SIH who had MRM and CTM without any intervening treatment. Patients who had MRM and CTM performed more than 6 months apart were excluded from the study.
The diagnosis of SIH was based on International Classification of Headache Disorders, third edition (ICHD-III) criteria5 with a modification of also including patients without headaches but whose symptoms are best explained by SIH. MRM and CTM protocols are shown in the eTable in the Supplement.
Results were extracted from clinical imaging reports. All discordant studies were reviewed by one neuroradiologist and one neurosurgeon, and in case of disagreement, by a second neuroradiologist to reach consensus.
The primary end point was the noninferiority comparison of MRM and CTM. Noninferiority analysis for the proportion (risk) difference was based on the Farrington and Manning likelihood score test. We considered a noninferiority margin of 0.10 to be clinically meaningful. If the lower margin of the 90% confidence interval for difference was more than 0.10, MRM would be considered as noninferior to CTM. We used the 2-sided 95% confidence interval of the difference between the sensitivity of the MRM and sensitivity of the CTM in diagnosing CSF leak. All statistical analyses were performed using SAS, version 9.4 (SAS Institute).
Results
Six hundred sixty-seven patients underwent both CTM and MRM (Figure). Five patients had imaging performed more than 6 months apart and 86 patients underwent treatment between imaging modalities. Among the remaining 576 patients, there were 390 women and 186 men (mean age, 48.6 years [range, 13-86 years]). The mean amount of time between CTM and MRM was 6.8 days (range, 0-180 days; <72 hours: 84.1%).
Figure. Schematic Flowchart of Patient Selection.
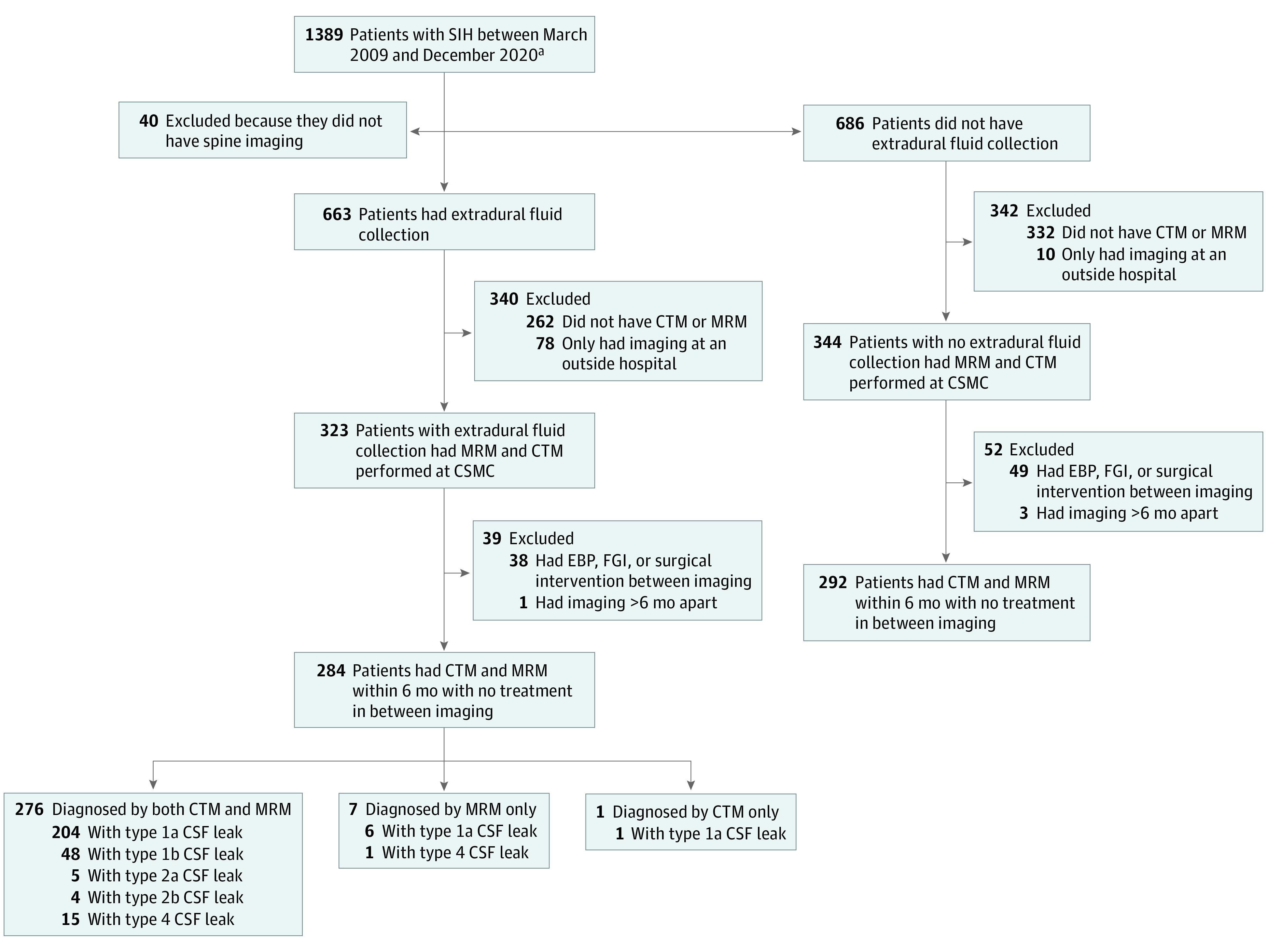
Type of cerebrospinal fluid (CSF) leak based on previously published classification of spontaneous spinal CSF leaks.6 CSMC indicates Cedars-Sinai Medical Center; CTM, post-myelography computed tomography; EBP, epidural blood patch; FGI, fibrin glue injection; MRM, spine magnetic resonance imaging with heavily T2-weighted magnetic resonance myelography; SIH, spontaneous intracranial hypotension.
aSIH diagnosed using modified International Classification of Headache Disorders, third edition criteria.5
Extradural fluid collections6 were diagnosed in 276 patients (47.9%) by both CTM and MRM (absolute difference, 0.01%; upper limit of 1-sided 95% CI, 3.2%; P < .001 for noninferiority) and 292 patients (50.7%) did not have an extradural CSF collection on both CTM and MRM. Eight patients (1.4%) were a mismatch, with 7 patients (1.2%) being diagnosed by MRM alone and 1 patient (0.2%) by CTM alone. A strong agreement between MRM and CTM with regard to the diagnosis of extradural CSF was found (κ, 97.2%; 95% CI, 95.3-99.1). Positive agreement was 99.6%, negative agreement was 97.7%, and overall agreement was 98.6%.
Discussion
This study shows that MRM is not inferior to CTM for the detection of extradural CSF in patients with SIH. MRM and CTM were discordant in less than 2% of patients with SIH with most of those favoring MRM over CTM.
Eliminating radiation exposure, obviating the need for lumbar puncture and intrathecal contrast injection, and decreasing resource utilization and cost are among the most important advantages of MRM over CTM. Advantages of CTM over MRM include CSF pressure measurements and exquisite bony detail of spinal tissues.
Limitations of this study include that (1) it mostly represents a selected group of patients referred to a SIH center, (2) we used digital subtraction myelography for intrathecal contrast administration rather than conventional myelography, and (3) CTM was performed after the results of MRM were available.
MRM may be a suitable alternative to CTM for the initial evaluation of patients with SIH.
eTable. MR protocol for spine MRI with heavily T2-weighted MR-myelography and CT protocol for the post-myelography CT
References
- 1.Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295(19):2286-2296. doi: 10.1001/jama.295.19.2286 [DOI] [PubMed] [Google Scholar]
- 2.Wang Y-F, Lirng J-F, Fuh J-L, Hseu S-S, Wang S-J. Heavily T2-weighted MR myelography vs CT myelography in spontaneous intracranial hypotension. Neurology. 2009;73(22):1892-1898. doi: 10.1212/WNL.0b013e3181c3fd99 [DOI] [PubMed] [Google Scholar]
- 3.Starling A, Hernandez F, Hoxworth JM, et al. Sensitivity of MRI of the spine compared with CT myelography in orthostatic headache with CSF leak. Neurology. 2013;81(20):1789-1792. doi: 10.1212/01.wnl.0000435555.13695.22 [DOI] [PubMed] [Google Scholar]
- 4.Dobrocky T, Winklehner A, Breiding PS, et al. Spine MRI in spontaneous intracranial hypotension for CSF leak detection: nonsuperiority of intrathecal gadolinium to heavily T2-weighted fat-saturated sequences. AJNR Am J Neuroradiol. 2020;41(7):1309-1315. doi: 10.3174/ajnr.A6592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. 2018;38(1):1-211. doi: 10.1177/0333102417738202 [DOI] [PubMed] [Google Scholar]
- 6.Schievink WI, Maya MM, Jean-Pierre S, Nuño M, Prasad RS, Moser FG. A classification system of spontaneous spinal CSF leaks. Neurology. 2016;87(7):673-679. doi: 10.1212/WNL.0000000000002986 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. MR protocol for spine MRI with heavily T2-weighted MR-myelography and CT protocol for the post-myelography CT


