Abstract
Background
Post‐dural (post‐lumbar or post‐spinal) puncture headache (PDPH) is one of the most common complications of diagnostic, therapeutic or inadvertent lumbar punctures. Many drug options have been used to prevent headache in clinical practice and have also been tested in some clinical studies, but there are still some uncertainties about their clinical effectiveness.
Objectives
To assess the effectiveness and safety of drugs for preventing PDPH in adults and children.
Search methods
The search strategy included the Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library 2012, Issue 5), MEDLINE (from 1950 to May 2012), EMBASE (from 1980 to May 2012) and CINAHL (from 1982 to June 2012). There was no language restriction.
Selection criteria
We considered randomised controlled trials (RCTs) that assessed the effectiveness of any drug used for preventing PDPH.
Data collection and analysis
Review authors independently selected studies, assessed risks of bias and extracted data. We estimated risk ratios (RR) for dichotomous data and mean differences (MD) for continuous outcomes. We calculated a 95% confidence interval (CI) for each RR and MD. We did not undertake meta‐analysis because participants' characteristics or assessed doses of drugs were too different in the included studies. We performed an intention‐to‐treat (ITT) analysis.
Main results
We included 10 RCTs (1611 participants) in this review with a majority of women (72%), mostly parturients (women in labour) (913), after a lumbar puncture for regional anaesthesia. Drugs assessed were epidural and spinal morphine, spinal fentanyl, oral caffeine, rectal indomethacin, intravenous cosyntropin, intravenous aminophylline and intravenous dexamethasone.
All the included RCTs reported data on the primary outcome, i.e. the number of participants affected by PDPH of any severity after a lumbar puncture. Epidural morphine and intravenous cosyntropin reduced the number of participants affected by PDPH of any severity after a lumbar puncture when compared to placebo. Also, intravenous aminophylline reduced the number of participants affected by PDPH of any severity after a lumbar puncture when compared to no intervention, while intravenous dexamethasone increased it. Spinal morphine increased the number of participants affected by pruritus when compared to placebo, and epidural morphine increased the number of participants affected by nausea and vomiting when compared to placebo. Oral caffeine increased the number of participants affected by insomnia when compared to placebo.
The remainder of the interventions analysed did not show any relevant effect for any of the outcomes.
None of the included RCTs reported the number of days that patients stayed in hospital.
Authors' conclusions
Morphine and cosyntropin have shown effectiveness for reducing the number of participants affected by PDPH of any severity after a lumbar puncture, when compared to placebo, especially in patients with high risk of PDPH, such as obstetric patients who have had an inadvertent dural puncture. Aminophylline also reduced the number of participants affected by PDPH of any severity after a lumbar puncture when compared to no intervention in patients undergoing elective caesarean section. Dexamethasone increased the risk of PDPH, after spinal anaesthesia for caesarean section, when compared to placebo. Morphine also increased the number of participants affected by adverse events (pruritus and nausea and vomiting)
There is a lack of conclusive evidence for the other drugs assessed (fentanyl, caffeine, indomethacin and dexamethasone).
These conclusions should be interpreted with caution, owing to the lack of information, to allow correct appraisal of risk of bias and the small sample sizes of studies.
Keywords: Adult, Child, Female, Humans, Male, Aminophylline, Aminophylline/administration & dosage, Analgesics, Analgesics/administration & dosage, Caffeine, Caffeine/administration & dosage, Cosyntropin, Cosyntropin/administration & dosage, Dexamethasone, Dexamethasone/administration & dosage, Dexamethasone/adverse effects, Drug Administration Routes, Fentanyl, Fentanyl/administration & dosage, Indomethacin, Indomethacin/administration & dosage, Morphine, Morphine/administration & dosage, Morphine/adverse effects, Post‐Dural Puncture Headache, Post‐Dural Puncture Headache/prevention & control, Randomized Controlled Trials as Topic, Spinal Puncture, Spinal Puncture/adverse effects
Plain language summary
Drugs for preventing headache after a lumbar puncture
Lumbar puncture is an invasive procedure that medical personnel use to get a sample of cerebrospinal fluid for diagnostic purposes (e.g. to diagnose meningitis or subarachnoid haemorrhage) by inserting a needle into the lower spinal region. It can also be used to inject medications such as anaesthetics and analgesics (to perform regional anaesthesia), chemotherapy or radiological contrast agents.
Post‐dural puncture headache (PDPH) is the most common complication of a lumbar puncture. The symptoms are a constant headache that worsens in the upright position and improves when lying down and resolves spontaneously within five to seven days. Several interventions have been used before, during or immediately after lumbar puncture to prevent PDPH, but there are still uncertainties about their clinical effectiveness, especially regarding drug treatments. Therefore, the aim of this review was to determine the effectiveness of these medications to prevent PDPH in children and adults.
We included 10 randomised clinical trials (RCTs), with a total of 1611 participants, that assessed seven medications (epidural and spinal morphine, spinal fentanyl, oral caffeine, rectal indomethacin, intravenous cosyntropin, intravenous aminophylline and intravenous dexamethasone). Epidural morphine and intravenous cosyntropin proved to be effective at reducing the number of participants affected by PDPH of any severity after lumbar puncture compared to placebo. Aminophylline also reduced the number of participants affected by PDPH of any severity after a lumbar puncture compared to no intervention. Dexamethasone increased the risk of PDPH when compared to placebo after spinal anaesthesia for caesarean section.
Morphine also increased the number of participants affected by adverse events such as itching, nausea and vomiting. The other interventions (fentanyl, caffeine, indomethacin and dexamethasone) did not show conclusive evidence of effectiveness.
Combining data was possible only for subgroups of one study comparing different dosages of caffeine to placebo, because the other RCTs appraised diverse drugs, outcomes or populations.
A meta‐analysis (combining of data) was not possible because all the included RCTs assessed different drugs, different doses, different outcomes or different baseline participants' characteristics.
These conclusions should be interpreted carefully, given the lack of information to evaluate the risk of bias properly, and the small number of participants in the included studies.
Background
Description of the condition
Post‐dural (post‐lumbar or post‐spinal) puncture headache (PDPH) is one of the most common complications of diagnostic, therapeutic or inadvertent lumbar puncture (Bezov 2010; Davignon 2002). PDPH is defined as any headache after a lumbar puncture that worsens within 15 minutes of sitting or standing and is relieved within 15 minutes of lying down (International Headache Society 2004). Ninety per cent of PDPHs occur within three days of the procedure and 66% start in the first 48 hours (Turnbull 2003).
The pathophysiology of PDPH has not been fully described. It is well known that the puncture in the dura allows cerebrospinal fluid (CSF) to leak from the subarachnoid space, resulting in a decrease of CSF volume and pressure (Grande 2005). This CSF volume loss may cause a downwards pull on pain‐sensitive structures resulting in a headache (Ahmed 2006; Baumgarten 1987; Davignon 2002; Denny 1987; Harrington 2004). Alternatively, the loss of CSF may cause an increase in blood flow, resulting in arterial and venous vasodilation and PDPH. A third explanation involves the role of substance P and the regulation of neurokinin‐1 receptors (NK1R) (Clark 1996).
Occurrence of PDPH varies from 1% to 40%, according to the needle gauge, needle orientation, operator skill level and presence of risk factors such as age group or history of PDPH (Turnbull 2003). This frequency is related to the type of lumbar puncture. During anaesthetic procedures, such as epidural anaesthesia, PDPH is most commonly caused by an unintentional dural puncture (Thew 2008; Turnbull 2003). In contrast, in diagnostic or therapeutic lumbar puncture, the need for adequate CSF flow requires an intentional lesion that may generate the PDPH phenomenon (Kuczkowski 2006). Estimated frequencies vary from less than 10% following spinal anaesthesia (Hafer 1997; Vallejo 2000) to 36% for diagnostic lumbar puncture (Lavi 2006; Vallejo 2000) and up to 81% (Banks 2001) in obstetric patients with inadvertent dural puncture during active labour. Reported risk of inadvertent dural puncture placement during epidural anaesthesia in an obstetric population ranges from 0.04% to 6% (Berger 1998; Choi 2003). Therefore, obstetric analgesia is probably the main source of PDPH patients.
The features of PDPH are often variable. PDPH may be accompanied by neck stiffness, tinnitus, hearing loss, photophobia or nausea; other features, such as the location and duration, are also unpredictable (Lybecker 1995). Although PDPH is not a life‐threatening condition, physical activity is often restricted. Likewise patients are usually required to stay in bed the whole day, and length of stay and medical care increases (Angle 2005).
The variability of symptoms makes PDPH a diagnosis of exclusion. Other alternative diagnoses should be ruled out (e.g. viral meningitis, sinus headache or intracranial haemorrhage) (Turnbull 2003). Once PDPH is diagnosed, the initial treatment involves conservative measures such as bed rest and analgesics. If PDPH continues for more than 72 hours, a more specific treatment is indicated (Ahmed 2006). Severe PDPH may respond to some therapeutic drugs and administration of an epidural blood patch (EBP) (Lavi 2006).
How the intervention might work
Owing to the fact that no clear pathophysiology has been asserted for PDPH, many drugs options are used to prevent headache in clinical practice and in clinical trials: for example EBP mechanically blocking the leakage of CSF, postures such as a prone position, reducing pressure in the subarachnoid space and allowing a seal to form over the dura, hydration increasing CSF production (Ahmed 2006), methylxanthines, sumatriptan and caffeine increasing vasoconstriction of cerebral blood vessels or adrenocorticotropic hormone (ACTH) (Kuczkowski 2006), or epidural saline infusion (Morewood 1993) increasing intravascular volume.
Preventive drugs should help to decrease the frequency of patients with PDPH, reduce the headache severity as much as possible, avoid the need for any therapeutic option, improve daily activity, reduce the length of hospital stay and decrease the occurrence of adverse events overall.
Why it is important to do this review
Two Cochrane systematic reviews about treatment and management of PDPH have been published using EBP (Boonmak 2010) and drugs (Basurto 2011). One Cochrane systematic review about prevention of PDPH with epidural catheter replacement and intrathecal catheter techniques is also in production (Newman 2010), alongside two published reviews using EBP (Boonmak 2010), and posture and fluids (Arevalo‐Rodriguez 2011).
Numerous preventive drugs have been proposed for treating this condition based on limited randomised controlled trials (RCTs) and case series, including: caffeine, morphine, paracetamol, fentanyl, vasopressin (Turnbull 2003) and epidural saline infusion (Morewood 1993). Therefore, there is weak evidence to support the preventive treatment of PDPH with drugs and the existing uncertainties require a systematic review to clarify their potential benefits. In addition, this review would like to inspire future guidelines as well as future good‐quality studies regarding this topic.
Objectives
To assess the effectiveness and safety of drugs for preventing PDPH in adults and children.
Methods
Criteria for considering studies for this review
Types of studies
We included RCTs (parallel or cross‐over) conducted in any setting. We excluded studies using alternation, date of birth, hospital record number or other quasi‐randomised methods of allocation of treatment.
Types of participants
Participants undergoing lumbar puncture for any of the reasons outlined: CSF sampling or pressure measurement, or both; spinal anaesthesia; myelography; intrathecal drug administration or accidental puncture of the dura during epidural anaesthesia. We included individuals of all ages and any gender.
The use of a standardised diagnostic criteria for PDPH was not required, but it should at least have been described as an orthostatic headache that worsened on standing and improved by lying down. We described the specific diagnostic criteria used in each included study.
Types of interventions
We considered any drug used for preventing PDPH. We considered interventions at any dose, formulation or route of administration given before, during or immediately after lumbar puncture.
Acceptable control groups included: placebo, no intervention, any other drug treatments, behavioural and physical therapies.
Types of outcome measures
Primary outcomes
Number of participants affected by PDPH of any severity after a lumbar puncture.
Secondary outcomes
Number of participants with severe PDPH (based on the author's definition of severity).
Number of participants with any headache, not only those explicitly described as PDPH.
Number of days that patients stayed in hospital.
Any possible adverse events of drugs taken to prevent PDPH.
Missing data (withdrawals, drop‐outs and participants lost to follow‐up).
Search methods for identification of studies
We designed the search in the context of an extensive review about prevention and treatment drugs used for PDPH. The Cochrane Central Register of Controlled Trials (CENTRAL) was our primary source for identifying studies. Our search terms were a combination of thesaurus‐based and free‐text terms covering both the procedure of interest (dural puncture performed for diagnosis, anaesthesia or myelography) and headache. For MEDLINE, EMBASE and CINAHL we used a modified version of the strategy used to search CENTRAL. We considered articles written in any language.
In addition, we searched the reference lists of all studies and review articles identified by electronic searching. We requested information about any potentially relevant studies when we contacted trialists from every included study.
Electronic searches
We searched:
CENTRAL (The Cochrane Library 2012, Issue 5);
MEDLINE (from 1950 to May 2012);
EMBASE (from 1980 to May 2012);
CINAHL (from 1982 to June 2012).
We include the complete search strategies designed for CENTRAL, MEDLINE, EMBASE and CINAHL in Appendix 1, Appendix 2, Appendix 3 and Appendix 4 respectively.
Data collection and analysis
Selection of studies
Two independent review authors (XB, SU) screened titles and abstracts of studies identified by the literature search for eligibility. We resolved disagreements through discussion. We retrieved eligible studies in full to confirm whether or not they fulfilled the inclusion criteria. Review authors were not blinded to the authors' names and institutions, journal of publication or study results at this or any stage of the review.
Data extraction and management
For included studies, we used specially designed, pre‐tested data forms to extract information from the original studies on participants, methods of randomisation and blinding, the comparison(s) of interest, the number of participants originally randomised in each arm of the study, any losses to follow‐up and the occurrence in each arm of the outcomes of interest. If information on any of these was incomplete, we attempted to obtain it by writing to the study author concerned. One review author (XB) extracted the data from studies and a second review author (SU) checked data for accuracy, resolving any disagreement by discussion. We entered data into Review Manager 5.1 (RevMan 2011).
When efficacy outcomes were reported in dichotomous form (e.g. number of people with severe PDPH, number of people with any headache, any possible adverse events of drug and missing data), we recorded the number of participants assigned to each treatment arm and the number with each outcome. For outcomes reported on a continuous scale (e.g. number of days participants stayed in hospital), we recorded data on the variance associated with their means.
If reported we recorded the frequency and type of adverse events for each treatment arm.
Assessment of risk of bias in included studies
We used The Cochrane Collaboration's tool for assessing risk of bias in the studies included in this review, which addresses six specific domains (Higgins 2011) summarised in a specific table. For this review we assessed five of the domains (sequence generation, allocation concealment, blinding, incomplete outcome data and selective outcome reporting). Each domain has a description of what was reported. One review author (XB) completed the 'Risk of bias' judgements for each study and a second review author (SU) checked them for accuracy. Any disagreement was resolved by discussion.
Assessment of heterogeneity
This review did not include a meta‐analysis. We would have assessed heterogeneity of effect sizes by means of the Q (Chi2 statistic) using the methods of Peto and Mantel‐Haenszel. If statistical evidence had existed for homogeneity of effect sizes, the analysis would have used a fixed‐effect model. If significant heterogeneity had been present (Chi2 test with P value < 0.1 or I2 statistic value > 50%), we would have made an attempt to explain the differences based on the clinical characteristics of the included studies. We would not have combined studies that were dissimilar in terms of interventions and participants. However, if a group of studies with heterogeneous results had appeared to be similar, we would have combined the study estimates using a random‐effects model (Higgins 2002; Higgins 2003).
Data synthesis
The differences between the studies included in this review, in terms of participants' characteristics, interventions assessed and outcomes measured, only permitted a combined analysis in one of the comparisons (caffeine plus paracetamol versus placebo). For the other comparisons we presented a narrative summary.
We analysed the results for different drugs separately, except for caffeine plus paracetamol versus placebo, using Review Manager 5.1 (RevMan 2011). We performed analysis on an intention‐to‐treat (ITT) basis (i.e. all participants remained in their original trial arm, whether or not they actually received the intervention allocated).
We used dichotomous data to calculate risk ratios (RR) with 95% confidence intervals (CI). In future updates of this review, we hope to be able to calculate the numbers needed to treat for an additional beneficial outcome (NNTB) with 95% CI, as the reciprocal of the risk difference (RD) (McQuay 1998). We will use data on the proportion of participants reporting adverse events to calculate RD and numbers needed to treat for an additional harmful outcome (NNTH) with 95% CI for significant differences.
For continuous outcomes reported using the same scale, we calculated mean differences (MD) with 95% CI. In future updates of this review, we hope to be able to calculate standardised mean differences (SMD) for pooling results of continuous outcomes measured with different scales.
Subgroup analysis and investigation of heterogeneity
In future updates of this review, if sufficient data are available, we plan to carry out the following subgroup analyses:
Follow‐up time subgroup analyses
When possible, we will assess the impact of the assessed interventions at short‐term (< 24 hours), medium‐term (24 to 48 hours) or long‐term time periods (> 48 hours) for the preventive drugs.
Population subgroup analyses
Where data allow in the future, we plan to conduct separate outcome analyses to test the following null hypotheses:
there is no difference between obstetric participants and all other participants;
there is no difference between men and non‐obstetric women participants;
there is no difference between young participants (18 to 35 years old) and all other adult participants.
Sensitivity analysis
In future updates of this review, and depending on study availability, we will conduct a sensitivity analyses formulated a priori:
We will examine the effect on the primary outcome of excluding any study judged to be at a high risk of bias by two of the domains, sequence generation and allocation concealment.
If applicable we will also perform a sensitivity analysis excluding those trials with a cross‐over design.
Results
Description of studies
See the 'Characteristics of included studies', 'Characteristics of excluded studies' and 'Characteristics of ongoing studies' tables.
Results of the search
We identified 1894 references in primary electronic databases up to May 2012 from our extended search strategy for prevention and treatment with drugs for PDPH. We excluded 1768 references after a detailed reading of the title and abstract. We obtained the full‐text reports for the remainder of the studies (137 papers) to check if they strictly fulfilled all the inclusion criteria. We finally excluded 127 studies after a complete full‐text review and we contacted the study authors by email in some cases when more information was needed to decide eligibility. Ten studies completely fulfilled the inclusion criteria for this review (Abboud 1992; Al‐metwalli 2008; Devcic 1993; Doroudian 2011; Esmaoglu 2005; Flaatten 1987; Hakim 2010; Sadeghi 2012; Strelec 1994; Yousefshahi 2012).
See Figure 1.
1.

Study flow diagram.
Included studies
Included studies are described in detail in the 'Characteristics of included studies' table.
Study design
All 10 included studies (involving a total of 1611 participants) were RCTs with a parallel design. Most of them were placebo‐controlled, except Devcic 1993 and Sadeghi 2012, which used a control group without an intervention.
Setting
All included studies were single‐centre studies. Three studies were conducted in the US (Abboud 1992; Devcic 1993; Strelec 1994), three studies in Iran (Doroudian 2011; Sadeghi 2012; Yousefshahi 2012) and the remainder in Norway (Flaatten 1987), Turkey (Esmaoglu 2005), Egypt (Hakim 2010) and Saudi Arabia (Al‐metwalli 2008).
All the studies recruited the participants from hospital settings and the intervention took place while they were admitted.
Sample size
The studies included a total of 1611 participants. The smallest study had 50 participants (Al‐metwalli 2008) and the largest had 372 (Yousefshahi 2012).
Participants
The majority of participants were women (1160/1611; 72%), mostly parturients (woman in labour) (913) that required a lumbar puncture for regional anaesthesia (Abboud 1992; Al‐metwalli 2008; Devcic 1993; Hakim 2010; Sadeghi 2012; Yousefshahi 2012). There were four studies that included men (451); three with surgical patients after a spinal anaesthesia (Doroudian 2011; Esmaoglu 2005; Flaatten 1987) and one with lumbar puncture for myelography (Strelec 1994).
The median age among participants from all studies ranged from 26.1 to 48.5 years old.
Intervention
Three included studies assessed two different opioid drugs to prevent PDPH; morphine (administered into the subarachnoid space (Abboud 1992) or into the epidural space (Al‐metwalli 2008)) and fentanyl (administered into the subarachnoid space (Devcic 1993)) .
Two studies used caffeine as an intervention to prevent PDPH. Strelec 1994 compared oral caffeine 300 mg to placebo. Esmaoglu 2005 assessed oral caffeine 75 mg and 125 mg, combined with paracetamol, compared to placebo.
Two studies used intravenous dexamethasone compared to placebo to prevent PDPH (Doroudian 2011; Yousefshahi 2012).
One study compared rectal indomethacin, a non‐steroidal anti‐inflammatory drug, to placebo (Flaatten 1987). Intravenous cosyntropin, a synthetic derivative of ACTH, was compared to placebo in one study (Hakim 2010) and intravenous aminophylline, a xanthine derivative, was compared to no intervention in another study (Sadeghi 2012).
Follow‐up was short in general terms and differed between the included trials at 48 hours (Sadeghi 2012), three days (Abboud 1992; Flaatten 1987; Yousefshahi 2012) and three weeks (Devcic 1993).
Outcomes of interest
The number of participants affected by PDPH of any severity after a lumbar puncture (primary outcome) was reported in all included studies. Missing data were reported in six studies (Devcic 1993; Doroudian 2011; Flaatten 1987; Hakim 2010; Strelec 1994; Yousefshahi 2012). Adverse events related to study drugs were reported in five studies (Abboud 1992; Al‐metwalli 2008; Esmaoglu 2005; Hakim 2010; Strelec 1994).
The number of participants with severe PDPH was reported in five studies (Al‐metwalli 2008; Devcic 1993; Doroudian 2011; Esmaoglu 2005; Yousefshahi 2012).
The number of participants with any headache was detailed in two studies (Esmaoglu 2005; Yousefshahi 2012).
The number of days that participants stayed in hospital was the only outcome not reported in the included studies.
Conflict of interest
Only three studies reported any conflict of interest. Flaatten 1987 stated that Dumex‐Norway supplied the intervention drugs and placebo, Hakim 2010 stated that support was provided solely from institutional or departmental (or both) sources and Yousefshahi 2012 stated no conflict of interest.
Excluded studies
A total of 127 studies did not fulfil the inclusion criteria and were excluded.
The most frequent reasons for exclusion were that the study did not focus on PDPH (45% of studies) or describe the orthostatic component of headache (35% studies). Other less frequent reasons(20% of the excluded studies) were: was not a RCT, intervention did not aim to prevent PDPH, allocation was not randomised or did not assess an individual drug.
For a summary of the reasons for exclusion see the 'Characteristics of excluded studies' table.
Risk of bias in included studies
Risk of bias in the included studies is summarised in Figure 2 and Figure 3.
2.

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.
3.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
Sequence generation
Allocation sequence was adequately generated in three studies (Al‐metwalli 2008; Hakim 2010; Yousefshahi 2012) that reported a computer‐generated random number sequence explicitly.
The other seven included studies were described as randomised but no information was provided, so we judged them as having an unclear risk of selection bias (Abboud 1992; Devcic 1993; Doroudian 2011; Esmaoglu 2005; Flaatten 1987; Sadeghi 2012; Strelec 1994).
Allocation concealment
Two studies reported the method used to conceal the randomisation sequences (Al‐metwalli 2008; Hakim 2010) and we judged them as having a low risk of selection bias.
The other eight studies did not provide information regarding allocation concealment (Abboud 1992; Devcic 1993; Doroudian 2011; Esmaoglu 2005; Flaatten 1987; Sadeghi 2012; Strelec 1994; Yousefshahi 2012) and we judged them as having an unclear risk of selection bias.
Blinding
Blinding of participants and personnel (performance bias)
The blinding method was adequate in five of the studies (Al‐metwalli 2008; Doroudian 2011; Hakim 2010; Sadeghi 2012; Yousefshahi 2012). The rest of the studies (Abboud 1992; Devcic 1993; Esmaoglu 2005; Flaatten 1987; Strelec 1994) did not report detailed data to allow assessment of performance bias.
Blinding of outcome assessment (detection bias)
Blinding of outcome assessment was adequate in four of the included studies (Al‐metwalli 2008; Devcic 1993; Hakim 2010; Yousefshahi 2012). The six remaining studies (Abboud 1992; Doroudian 2011; Esmaoglu 2005; Flaatten 1987; Sadeghi 2012; Strelec 1994) did not report information to allow assessment of detection bias.
Incomplete outcome data
Seven studies presented results for all randomised patients or reported the number of participants lost in follow‐up with reasons explicitly stated and we judged them as having a low risk of attrition bias (Abboud 1992; Al‐metwalli 2008; Doroudian 2011; Esmaoglu 2005; Hakim 2010; Sadeghi 2012; Yousefshahi 2012).
The remainder of the studies stated explicitly the number of participants lost to follow‐up without detailed data to allow assessment of attrition bias; Devcic 1993 with six participants lost out of 194, Flaatten 1987 with three out of 250 and Strelec 1994 with two out of 60. Gender of participants lost to follow‐up in Flaatten 1987 and Strelec 1994 was not reported.
Selective reporting
Four studies presented outcomes according to objectives stated in the methods section and we judged them as having a low risk of reporting bias (Al‐metwalli 2008; Hakim 2010; Strelec 1994; Yousefshahi 2012). We judged three studies as having an unclear risk of bias because no information was provided (Abboud 1992; Esmaoglu 2005; Flaatten 1987). We judged Devcic 1993, Doroudian 2011 and Sadeghi 2012 as having a high risk as they did not report outcomes about adverse effects.
Effects of interventions
We present in this section a narrative synthesis of the results for the different outcomes of interest.
Number of participants affected by post‐dural puncture headache (PDPH) of any severity
Opioids
Opioids were assessed in three studies for this primary outcome. Epidural morphine (Al‐metwalli 2008) showed a significant risk reduction of the number of participants affected by PDPH of any severity compared to placebo (15 events in 50 participants; risk ratio (RR) 0.25; 95% confidence interval (CI) 0.08 to 0.78; Analysis 2.1).
2.1. Analysis.

Comparison 2 Epidural morphine versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
In contrast, spinal morphine and spinal fentanyl showed no differences compared to placebo in Abboud 1992 (17 events in 82 participants; RR 1.18; 95% CI 0.51 to 2.76; Analysis 1.1) or no intervention in Devcic 1993 (11 events in 194 participants; RR 1.79; 95% CI 0.54 to 5.91; Analysis 3.1) respectively, in the number of participants affected by PDPH of any severity.
1.1. Analysis.

Comparison 1 Spinal morphine versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
3.1. Analysis.

Comparison 3 Spinal fentanyl versus no intervention, Outcome 1 Number of participants affected by PDPH of any severity.
We did not undertake meta‐analysis of these three studies (Abboud 1992; Al‐metwalli 2008; Devcic 1993). The Al‐metwalli 2008 results were not combined with other studies because baseline incidence of PDPH was much higher in obstetric patients with inadvertent dural puncture during active labour than following spinal anaesthesia for caesarean section. We did not combine the results from Abboud 1992 and Devcic 1993 because opioid interventions were not dose equivalent; Devcic 1993 assessed 20 μg of fentanyl, which is dose equivalent of morphine 2 mg, which is 10 times higher than the morphine 0.2 mg used in Abboud 1992.
Intravenous cosyntropin
Intravenous cosyntropin (Hakim 2010) showed a significant risk reduction of the number of participants affected by PDPH of any severity (46 events in 95 participants; RR 0.49; 95% CI 0.31 to 0.79; Analysis 8.1) compared to placebo.
8.1. Analysis.

Comparison 8 Cosyntropin versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
Oral caffeine
Oral caffeine plus paracetamol was assessed by Esmaoglu 2005 with two different doses of caffeine, 75 mg and 125 mg, and compared to placebo. The combined analysis from these two doses of caffeine, compared to placebo, showed no significant risk reduction (42 events in 280 participants; RR 0.91; 95% CI 0.52 to 1.59; Analysis 11.1). Neither comparison showed a significant result: caffeine 75 mg versus placebo (21 events in 140 participants; RR 0.91; 95% CI 0.41 to 2.00; Analysis 4.1), caffeine 125 mg versus placebo (21 events in 140 participants; RR 0.91; 95% CI 0.41 to 2.00; Analysis 5.1) or 75 mg caffeine versus caffeine 125 mg (20 events in 140 participants; RR 1.00; 95% CI 0.44 to 2.25; Analysis 6.1). Strelec 1994 also showed no significant risk reduction (18 events in 60 participants; RR 2.00; 95% CI 0.86 to 4.63; Analysis 9.1) when comparing oral caffeine 300 mg to placebo.
11.1. Analysis.

Comparison 11 Caffeine versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
4.1. Analysis.

Comparison 4 Caffeine 75 mg versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
5.1. Analysis.

Comparison 5 Caffeine 125 mg versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
6.1. Analysis.

Comparison 6 Caffeine 75 mg versus caffeine 125 mg, Outcome 1 Number of participants affected by PDPH of any severity.
9.1. Analysis.

Comparison 9 Caffeine 300 mg versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
We did not undertake meta‐analysis of these two studies (Esmaoglu 2005; Strelec 1994) because the caffeine doses used were too different (75 mg/125 mg and 300 mg, respectively) and also because the intervention was different; caffeine plus paracetamol in Esmaoglu 2005 while Strelec 1994 used caffeine alone.
Rectal indomethacin
Rectal indomethacin (Flaatten 1987) showed no significant risk reduction when compared to placebo (51 events in 250 participants; RR 0.70; 95% CI 0.42 to 1.15; Analysis 7.1).
7.1. Analysis.

Comparison 7 Indomethacin versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
Intravenous dexamethasone
Intravenous dexamethasone was assessed in two studies for this primary outcome. Doroudian 2011 showed no significant risk reduction when compared to placebo (34 events in 178 participants; RR 0.79; 95% CI 0.43 to 1.45; Analysis 10.1). Yousefshahi 2012 showed a significant risk of increasing the number of participants affected by PDPH of any severity compared to placebo (39 events in 372 participants; RR 2.55; 95% CI 1.31 to 4.96; Analysis 10.1).
10.1. Analysis.

Comparison 10 Dexamethasone versus placebo, Outcome 1 Number of participants affected by PDPH of any severity.
We did not undertake a meta‐analysis of these two studies (Doroudian 2011; Yousefshahi 2012) because participants' characteristics were too different in terms of age, gender, length of gestation and spinal needle size used, and also because of statistical evidence of significant heterogeneity of effect sizes (Chi2 test with P value = 0.01 and I2 statistic value = 85%).
Intravenous aminophylline
Intravenous aminophylline (Sadeghi 2012) showed a significant risk reduction of the number of participants affected by PDPH of any severity at 24 and 48 hours after umbilical cord clamping compared to no intervention (at 24 hours: 22 events in 120 participants; RR 0.16; 95% CI 0.05 to 0.51; Analysis 12.1; at 48 hours: 17 events in 120 participants; RR 0.21; 95% CI 0.06 to 0.71; Analysis 12.1).
12.1. Analysis.

Comparison 12 Aminophylline versus no intervention, Outcome 1 Number of participants affected by PDPH of any severity.
Number of participants with severe PDPH (based on the author's definition of severity)
Opioids
Opioids were assessed in two studies for this outcome. Epidural morphine (Al‐metwalli 2008) showed no significant risk reduction compared to placebo (six events in 50 participants; RR 0.08; 95% CI 0.00 to 1.30; Analysis 2.2). Spinal fentanyl (Devcic 1993) also showed no significant risk reduction when compared to no intervention (four events in 194 participants; RR 3.06; 95% CI 0.32 to 28.93; Analysis 3.2).
2.2. Analysis.

Comparison 2 Epidural morphine versus placebo, Outcome 2 Number of participants with severe PDPH.
3.2. Analysis.

Comparison 3 Spinal fentanyl versus no intervention, Outcome 2 Number of participants with severe PDPH.
We did not undertake meta‐analysis of these two studies (Al‐metwalli 2008; Devcic 1993) because of the difference between participants' characteristics.
Oral caffeine
Data for oral caffeine doses plus paracetamol assessed in Esmaoglu 2005 were analysed in combination, caffeine 75 mg and 125 mg, showing no significant risk reduction compared to placebo (15 events in 280 participants; RR 0.88; 95% CI 0.33 to 2.35; Analysis 11.2). Individual comparisons showed no significant risk reduction in any of the reported comparisons: caffeine 75 mg compared to placebo (10 events in 140 participants; RR 1.50; 95% CI 0.44 to 5.09; Analysis 4.2), caffeine 125 mg compared to placebo (five events in 140 participants; RR 0.25; 95% CI 0.03 to 2.18; Analysis 5.2) or caffeine 75 mg compared to caffeine 125 mg (seven events in 140 participants; RR 6.00; 95% CI 0.74 to 48.55; Analysis 6.2).
11.2. Analysis.

Comparison 11 Caffeine versus placebo, Outcome 2 Number of participants with severe PDPH.
4.2. Analysis.

Comparison 4 Caffeine 75 mg versus placebo, Outcome 2 Number of participants with severe PDPH.
5.2. Analysis.

Comparison 5 Caffeine 125 mg versus placebo, Outcome 2 Number of participants with severe PDPH.
6.2. Analysis.

Comparison 6 Caffeine 75 mg versus caffeine 125 mg, Outcome 2 Number of participants with severe PDPH.
Intravenous dexamethasone
Intravenous dexamethasone was assessed in two studies. Doroudian 2011 showed no significant risk reduction compared to placebo (10 events in 178 participants; RR 0.25; 95% CI 0.05 to 1.14; Analysis 10.2). Yousefshahi 2012 could not estimate this outcome because none of the participants experienced a severe PDPH. For this reason and because of clinical differences these two studies could not be combined.
10.2. Analysis.

Comparison 10 Dexamethasone versus placebo, Outcome 2 Number of participants with severe PDPH.
Number of participants with any headache, not only those explicitly described as PDPH
Oral caffeine
A combined analysis of caffeine 75 mg with 125 mg in Esmaoglu 2005 showed no significant risk reduction compared to placebo (61 events in 280 participants; RR 0.79; 95% CI 0.51 to 1.24; Analysis 11.3). All other comparisons showed no significant risk reduction: 75 mg caffeine compared to placebo (10 events in 140 participants; RR 0.67; 95% CI 0.20 to 2.26; Analysis 4.3), 125 mg caffeine compared to placebo (nine events in 140 participants; RR 0.50; 95% CI 0.13 to 1.92; Analysis 5.3) or caffeine 75 mg compared to caffeine 125 mg (seven events in 140 participants; RR 1.33; 95% CI 0.31 to 5.74; Analysis 6.3).
11.3. Analysis.

Comparison 11 Caffeine versus placebo, Outcome 3 Number of participants with any headache.
4.3. Analysis.

Comparison 4 Caffeine 75 mg versus placebo, Outcome 3 Number of participants with any headache.
5.3. Analysis.

Comparison 5 Caffeine 125 mg versus placebo, Outcome 3 Number of participants with any headache.
6.3. Analysis.

Comparison 6 Caffeine 75 mg versus caffeine 125 mg, Outcome 3 Number of participants with any headache.
Dexamethasone
Dexamethasone was assessed in Yousefshahi 2012 and showed no significant risk reduction compared to placebo (16 events in 372 participants; RR 2.20; 95% CI 0.78 to 6.21; Analysis 10.3).
10.3. Analysis.

Comparison 10 Dexamethasone versus placebo, Outcome 3 Number of participants with any headache.
Number of days that patients stayed in hospital
None of the included studies reported this outcome.
Any possible adverse events of drugs taken to prevent PDPH
Opioids
Opioids were assessed in two studies for this outcome. Spinal morphine (Abboud 1992) showed a significant risk for increasing the number of participants affected by pruritus (28 events in 82 participants; RR 8.75; 95% CI 2.86 to 26.72; Analysis 1.2) compared to placebo, but a non‐significant result for the number of participants affected by nausea and vomiting (41 events in 82 participants; RR 0.82; 95% CI 0.53 to 1.27; Analysis 1.2).
1.2. Analysis.

Comparison 1 Spinal morphine versus placebo, Outcome 2 Number of any possible adverse effects from the drug taken to prevent PDPH.
Epidural morphine (Al‐metwalli 2008) significantly increased the number of participants affected by nausea and vomiting (15 events in 50 participants; RR 2.75; 95% CI 1.01 to 7.48; Analysis 2.3) compared to placebo. This study (Al‐metwalli 2008) showed three participants affected by pruritus, all of them in the morphine group, with a non‐significant result (three events in 50 participants; RR 7.00; 95% CI 0.38 to 128.87; Analysis 2.3).
2.3. Analysis.

Comparison 2 Epidural morphine versus placebo, Outcome 3 Number of any possible adverse effects from the drug taken to prevent PDPH.
We did not undertake meta‐analysis of these two studies (Abboud 1992; Al‐metwalli 2008) for this outcome because of the difference between participants' characteristics.
Caffeine
Oral caffeine 300 mg (Strelec 1994) showed a significant risk for increasing the number of participants affected by insomnia (11 events in 60 participants; RR 4.50; 95% CI 1.06 to 19.11; Analysis 9.2) compared to placebo. Esmaoglu 2005 reported no adverse events in either the caffeine 75 mg plus paracetamol group or in caffeine 125 mg plus paracetamol group. The study did not report this outcome in the placebo group.
9.2. Analysis.

Comparison 9 Caffeine 300 mg versus placebo, Outcome 2 Number of any possible adverse effects from the drug taken to prevent PDPH.
Intravenous cosyntropin
Intravenous cosyntropin compared to placebo (Hakim 2010) showed two participants affected by mild hypersensitivity reaction (urticaria) in the cosyntropin group, with a non‐significant result (two events in 95 participants; RR 5.10; 95% CI 0.25 to 103.57; Analysis 8.2).
8.2. Analysis.

Comparison 8 Cosyntropin versus placebo, Outcome 2 Number of any possible adverse effects from the drug taken to prevent PDPH.
Missing data (withdrawals, drop‐outs and participants lost to follow‐up)
Opioids
Spinal fentanyl (Devcic 1993) showed no significant risk of losing participants to follow‐up (six events in 194 participants; RR 2.04; 95% CI 0.38 to 10.89; Analysis 3.3) when compared to no intervention.
3.3. Analysis.

Comparison 3 Spinal fentanyl versus no intervention, Outcome 3 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up).
Rectal indomethacin
Rectal indomethacin (Flaatten 1987) showed no significant risk of losing participants to follow‐up (three events in 250 participants; RR 0.14; 95% CI 0.01 to 2.74; Analysis 7.2) when compared to placebo.
7.2. Analysis.

Comparison 7 Indomethacin versus placebo, Outcome 2 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up).
Intravenous cosyntropin
Intravenous cosyntropin (Hakim 2010) show no significant risk of losing participants to follow‐up (five events in 95 participants; RR 0.68; 95% CI 0.12 to 3.89; Analysis 8.3) when compared to placebo.
8.3. Analysis.

Comparison 8 Cosyntropin versus placebo, Outcome 3 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up).
Oral caffeine
Oral caffeine (Strelec 1994) showed no significant risk of losing participants to follow‐up when comparing 300 mg oral caffeine to placebo (two events in 60 participants; RR 0.20; 95% CI 0.01 to 4.00; Analysis 9.3).
9.3. Analysis.
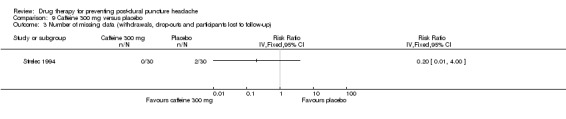
Comparison 9 Caffeine 300 mg versus placebo, Outcome 3 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up).
Intravenous dexamethasone
Intravenous dexamethasone was assessed in Yousefshahi 2012 and showed no significant risk of losing participants to follow‐up (12 events in 372 participants; RR 0.50; 95% CI 0.15 to 1.63; Analysis 10.4) compared to placebo. Doroudian 2011 could not estimate this outcome because none of the participants were lost to follow‐up.
10.4. Analysis.

Comparison 10 Dexamethasone versus placebo, Outcome 4 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up).
We did not undertake meta‐analysis of the six RCTs included in this outcome because of the different intervention drugs assessed.
Discussion
Summary of main results
This systematic review identified three randomised controlled trials (RCTs) assessing opioids for preventing post‐dural puncture headache (PDPH): epidural morphine (Al‐metwalli 2008), spinal morphine (Abboud 1992) and spinal fentanyl (Devcic 1993). Two studies assessed oral caffeine (Esmaoglu 2005; Strelec 1994) and two studies assessed intravenous dexamethasone (Doroudian 2011; Yousefshahi 2012). Three other studies assessing different drugs for preventing PDPH were identified: rectal indomethacin (Flaatten 1987), intravenous cosyntropin (Hakim 2010) and intravenous aminophylline (Sadeghi 2012).
All the included studies reported data on the primary outcome, the number of participants affected by PDPH of any severity after a lumbar puncture. For this outcome, epidural morphine (Al‐metwalli 2008) and intravenous cosyntropin (Hakim 2010) reduced the number of participants affected by PDPH of any severity after a lumbar puncture when compared to placebo. In both RCTs participants were obstetric patients who had an inadvertent dural puncture. Also intravenous aminophylline (Sadeghi 2012) reduced the number of participants affected by PDPH of any severity after a lumbar puncture when compared to no intervention in patients undergoing elective caesarean section. Intravenous dexamethasone after caesarean section increased the risk of PDPH in Yousefshahi 2012 and showed no significant effect in adults with lower extremity surgery (Doroudian 2011). The rest of the interventions assessed for this outcome, spinal morphine (Abboud 1992) and spinal fentanyl (Devcic 1993), oral caffeine (Esmaoglu 2005; Strelec 1994) and rectal indomethacin (Flaatten 1987), did not show any relevant effect.
When assessing any possible adverse events of drugs taken to prevent PDPH, spinal morphine (Abboud 1992) increased the number of participants affected by pruritus when compared to placebo and epidural morphine (Al‐metwalli 2008) increased the number of participants affected by nausea and vomiting when compared to placebo. Also three participants in the epidural morphine group experienced pruritus. Two participants in the cosyntropin group and none in the placebo group (Hakim 2010) were affected by a mild self limiting hypersensitivity reaction (urticaria) that required no treatment. Oral caffeine 300 mg every eight hours for three days increased the number of participants affected by insomnia (Strelec 1994); however, Esmaoglu 2005 found no relevant adverse effect.
The drugs assessed in the included studies did not show any relevant effect for the rest of the outcomes of interest for this review. The number of participants with severe PDPH was similar between the interventions and their controls in five studies (Al‐metwalli 2008; Devcic 1993; Doroudian 2011; Esmaoglu 2005; Yousefshahi 2012). The number of participants with any headache, not just that explicitly described as PDPH, was reported in two studies (Esmaoglu 2005; Yousefshahi 2012) without relevant effect. Missing data (withdrawals, drop‐outs and participants lost to follow‐up) were reported in five studies (Devcic 1993; Flaatten 1987; Hakim 2010; Strelec 1994; Yousefshahi 2012), which showed no significant differences between the interventions and their controls. None of the included studies reported data showing the number of days participants stayed in hospital.
Three studies (Abboud 1992; Al‐metwalli 2008; Devcic 1993) compared opioids versus placebo but we did not undertake meta‐analysis because of the difference between participants' characteristics or because the opioid doses were not equivalent. The baseline incidence of PDPH was much higher in obstetric patients with inadvertent dural puncture during active labour than following spinal anaesthesia for caesarean section in the Al‐metwalli 2008 study. Data from Abboud 1992 and Devcic 1993 could not be combined because the opioids used were not dose equivalents. In Devcic 1993, fentanyl 20 μg was the dose equivalent of morphine 2 mg and this was different from the 0.2 mg dose of morphine that was used in Abboud 1992.
Two studies (Esmaoglu 2005; Strelec 1994) compared caffeine to placebo but we chose not to combine results because the range of caffeine doses used was too wide (75 mg, 125 mg and 300 mg) and also the intervention was different; caffeine plus paracetamol was used in Esmaoglu 2005 while Strelec 1994 used caffeine alone. The two intervention groups in Esmaoglu 2005 were analysed in combination (i.e. caffeine 75 mg and caffeine 125 mg) compared to placebo, showing no relevant effect.
Two studies (Doroudian 2011; Yousefshahi 2012) compared dexamethasone to placebo but could not be combined because participants' characteristics were too varied in terms of age, gender, length of gestation and spinal needle size used, and also because of statistical evidence of significant heterogeneity of effect sizes.
In future updates of this review, if sufficient data are available, we plan to carry out the subgroup and sensitivity analyses formulated a priori.
Overall completeness and applicability of evidence
All participants included in this review were recruited from acute care hospitals and their characteristics seemed to be similar to patients seen in usual clinical practice. The lumbar punctures were performed during hospital stay, which is the most common setting for this technique. Most of the participants in the included studies underwent lumbar puncture to administer regional anaesthesia (spinal and epidural anaesthesia), which is the most common reason for lumbar puncture. No lumbar puncture in the included studies was done for diagnostic purposes.
The opioids (morphine and fentanyl), indomethacin, aminophylline and dexamethasone, used in the included studies, are widely marketed and frequently used. Caffeine and cosyntropin are also commercialised but for more specific indications and therefore they are less widely available.
Outcomes reported from the included studies were patient‐relevant. In fact, all included studies reported on the primary effectiveness outcome, that is the number of participants affected by PDPH of any severity after a lumbar puncture. The second most reported outcome was a safety issue, that is any possible adverse events of drugs taken to prevent PDPH.
Quality of the evidence
The outlined results should be interpreted with caution owing to the diversity of drugs and doses assessed, and outcomes measured, the small sample sizes of the studies included, and the bias presented. There was a lack of data reported to allow a complete appraisal of the risk of bias; review authors' judgements about each 'Risk of bias' item were unclear in around 50% across all included studies (Figure 2). We judged three included studies (Abboud 1992; Flaatten 1987; Strelec 1994) as having an unclear risk of bias in at least five out of the six items evaluated. We judged three other included studies (Al‐metwalli 2008; Hakim 2010; Yousefshahi 2012) as having a low risk of bias in at least five out of the six items evaluated (Figure 3). We judged three studies (Devcic 1993; Doroudian 2011; Sadeghi 2012) as having a high risk of bias in only one item each.
Potential biases in the review process
This review was conducted in accordance with the previously published protocol. We are unaware of any biases in the review process. To minimise bias, the selection, assessment for inclusion eligibility, risk of bias and data extraction were done independently by more than one review author. We also contacted study authors for clarification of study data. None of the review authors have been involved in any of the included studies and none have any commercial or other conflict of interest.
Agreements and disagreements with other studies or reviews
We have found no other systematic review specifically assessing the efficacy of drugs for preventing PDPH. In one systematic review (Apfel 2010) analysing any treatment options to prevent PDPH after accidental dural puncture (e.g. prophylactic EBP, epidural morphine, intrathecal catheters, and epidural or intrathecal saline) no strong evidence was found to make a clinical recommendation but, as in this review, epidural morphine was the only drug with proven efficacy, based on a study also included in this review (Al‐metwalli 2008). One narrative review (Bezov 2010) about PDPH concluded, as we do, that caffeine was not helpful in preventing PDPH based on a study that we also included (Esmaoglu 2005).
Other Cochrane reviews (Arevalo‐Rodriguez 2011; Boonmak 2010) have investigated measures other than drugs to prevent PDPH (e.g. posture, fluids and EBP), without reaching strong recommendations. One published guideline (Verma 2011) only considers the use of smaller gauge (≥ 25 G) and pencil‐point needles for regional anaesthesia in day‐surgery patients.
Authors' conclusions
Implications for practice.
Available studies show that morphine, cosyntropin and aminophylline could be a first‐line drug therapy when trying to prevent post‐dural puncture headache (PDPH) after a lumbar puncture.
Epidural morphine and intravenous cosyntropin decreased the number of patients affected by PDPH of any severity after a lumbar puncture compared to placebo, especially in those patients with a high risk of PDPH, such as woman giving birth who have had an inadvertent dural puncture during administration of regional anaesthesia. Pruritus, nausea and vomiting due to morphine and urticaria due to cosyntropin are the adverse events reported but these are less frequent than the benefits, are not severe or life‐threatening and, if necessary, efficacious and safe drugs exist to treat them.
Aminophylline also provides the same benefit, reducing the number of participants affected by PDPH of any severity, but in this case when compared to no intervention and in patients undergoing spinal anaesthesia for elective caesarean section.
Dexamethasone increased the risk of PDPH, after spinal anaesthesia for caesarean section, when compared to placebo.
These conclusions should be interpreted with caution, owing to the lack of information to allow a complete appraisal of risk of bias and the small sample sizes of studies.
There is a lack of conclusive results for the other drugs assessed (fentanyl, caffeine, indomethacin and dexamethasone).
Implications for research.
Future research in this field should focus on the design of trials with larger samples (including the reporting of how sample size was determined) in order to provide more sound and accurate information on the effectiveness of drugs in this setting and situation.
The reporting of trials could also be improved by endorsing the CONSORT statement (Schulz 2010), which would allow a better appraisal of them for their potential inclusion into systematic reviews.
What's new
| Date | Event | Description |
|---|---|---|
| 25 July 2016 | Review declared as stable | See Published notes. |
History
Protocol first published: Issue 1, 2000 Review first published: Issue 2, 2013
| Date | Event | Description |
|---|---|---|
| 25 February 2013 | Amended | Added link to Appendix 4. |
Notes
This protocol was originally published in Issue 1, 2000 by Cathie Sudlow. The review has now been taken over by Xavier Basurto Ona and the title split into one on prevention (this present review) and another on treatment, which is being written alongside this review.
Note added July 2016:
A search in July 2015 did not identify any relevant studies likely to change the conclusions. Therefore, this review has now been stabilised following discussion with the authors and editors. If appropriate, we will update the review if new evidence likely to change the conclusions is published, or if standards change substantially which necessitate major revisions.
Acknowledgements
Xavier Basurto is a PhD student at the Pediatrics, Obstetrics and Gynecology, and Preventive Medicine Department, Universitat Autònoma de Barcelona, Barcelona, Spain. We are grateful to Caroline Struthers (former Trials Search Co‐ordinator of the Cochrane Pain, Palliative and Supportive Care Review Group) and Jane Hayes for undertaking the searches; to Marta Roqué (Iberoamerican Cochrane Center) for her help in the statistical analysis; to Richard Vanderkleyn for his help in editing the review; and to Cathie Sudlow and Charles Warlow for writing the first draft of the protocol.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 explode 'Anesthesia, Epidural' / all subheadings
#2 explode 'Anesthesia, Spinal' / all subheadings
#3 explode 'Injections, Spinal' / all subheadings
#4 explode 'Myelography' / all subheadings
#5 explode 'Spinal Puncture' / all subheadings
#6 (spine or spinal or intraspinal or dura* or intradural or epidural or lumbar* or theca* or intrathecal or subarachnoid*) near/10 (puncture* or inject* or anesth* or anaesth* or needle*)
#7 myelogra*
#8 #1 or #2 or #3 or #4 or #5 or #6 or #7
#9 explode 'Headache disorders' / all subheadings
#10 headach* or cephalgia or (head near/2 pain) or (cranial adj2 pain)
#11 #9 or #10
#12 #8 and #11
Appendix 2. MEDLINE search strategy
#1 explode 'Anesthesia, Epidural' / all subheadings
#2 explode 'Anesthesia, Spinal' / all subheadings
#3 explode 'Injections, Spinal' / all subheadings
#4 explode 'Myelography' / all subheadings
#5 explode 'Spinal Puncture' / all subheadings
#6 (spine or spinal or intraspinal or dura* or intradural or epidural or lumbar* or theca* or intrathecal or subarachnoid*) adj10 (puncture* or inject* or anesth* or anaesth* or needle*)
#7 myelogra*
#8 #1 or #2 or #3 or #4 or #5 or #6 or #7
#9 explode 'Headache disorders' / all subheadings
#10 headach* or cephalgia or (head adj2 pain) or (cranial adj2 pain)
#11 #9 or #10
#12 #8 and #11
The MEDLINE search strategy above was combined with the following highly sensitive search strategy for identifying randomised trials in MEDLINE: sensitivity‐maximising version (2008 revision); Ovid format.
Cochrane Highly Sensitive Search Strategy for identifying randomised trials
1. randomised controlled trial.pt.
2. controlled clinical trial.pt.
3. randomized.ab.
4. placebo.ab.
5. drug therapy.fs.
6. randomly.ab.
7. trial.ab.
8. groups.ab.
9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8
10. humans.sh.
11. 9 and 10
Appendix 3. EMBASE search strategy
#1 explode 'Spinal Anesthesia' / all subheadings
#2 explode 'Lumbar Puncture' / all subheadings
#3 explode 'Myelography' / all subheadings
#4 (spine or spinal or intraspinal or dura* or intradural or epidural or lumbar* or theca* or intrathecal or subarachnoid*) adj10 (puncture* or inject* or anesth* or anaesth* or needle*)
#5 myelogra*
#6 #1 or #2 or #3 or #4 or #5
#7 explode 'Headache and facial pain' / all subheadings
#8 headach* or cephalgia or (head adj2 pain) or (cranial adj2 pain)
#9 #7 or #8
The above EMBASE search strategy was combined with the following filter developed for EMBASE to identify randomised trials.
Search filter for EMBASE (Ovid format) 2008
1. random*.ti,ab.
2. factorial*.ti,ab. (5987)
3. (crossover* or cross over* or cross‐over*).ti,ab.
4. placebo*.ti,ab.
5. (doubl* adj blind*).ti,ab.
6. (singl* adj blind*).ti,ab.
7. assign*.ti,ab.
8. allocat*.ti,ab.
9. volunteer*.ti,ab.
10. CROSSOVER PROCEDURE.sh.
11. DOUBLE‐BLIND PROCEDURE.sh.
12. RANDOMIZED CONTROLLED TRIAL.sh.
13. SINGLE BLIND PROCEDURE.sh.
14. or/1‐13
15. ANIMAL/ or NONHUMAN/ or ANIMAL EXPERIMENT/
16. HUMAN/
17. 15 and 16
18. 15 not 17
19. 14 not 18
Appendix 4. CINAHL search strategy
1 anaesthesia, epidural/ or analgesia, epidural/ or “epidural analgesia administration (iowa nic)”/ or exp injections, epidural/
2 exp injections, intraspinal/
3 myelography/
4 spinal puncture/ or anaesthesia, spinal/
5 ((spine or spinal or intraspinal or dura* or intradural or epidural or lumbar* or theca* or intrathecal or subarachnoid*) and (puncture* or inject* or anesthe* or anaesthe* or needle*)).ti,ab
6 myelogra*.ti,ab
7 1 or 2 or 3 or 4 or 5 or 6
8 *headache/
9 (headach* or cephalgi* or cephalalgi*).ti,ab
10 8 or 9
11 7 and 10
12 exp clinical trials/
13 (clinical and trial*).ti
14 ((singl* or doubl* or trebl* or tripl*) and (blind* or mask*)).ti
15 (randomi?ed and control* and trial*).ti
16 random assignment/
17 (random* and allocat*).ti
18 placebo*.ti
19 placebos/
20 quantitative studies/
21 12 or 13 or 14 or 15 or 16 or 17 or 18 or 19 or 20
22 11 and 21
Data and analyses
Comparison 1. Spinal morphine versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of any possible adverse effects from the drug taken to prevent PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Pruritus | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Nausea and vomiting | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 2. Epidural morphine versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of participants with severe PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of any possible adverse effects from the drug taken to prevent PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3.1 Pruritus | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3.2 Nausea and vomiting | 1 | Risk Ratio (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 3. Spinal fentanyl versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of participants with severe PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up) | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 4. Caffeine 75 mg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of participants with severe PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of participants with any headache | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 5. Caffeine 125 mg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of participants with severe PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of participants with any headache | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 6. Caffeine 75 mg versus caffeine 125 mg.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of participants with severe PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of participants with any headache | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Number of any possible adverse effects from the drug taken to prevent PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
6.4. Analysis.

Comparison 6 Caffeine 75 mg versus caffeine 125 mg, Outcome 4 Number of any possible adverse effects from the drug taken to prevent PDPH.
Comparison 7. Indomethacin versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up) | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 8. Cosyntropin versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of any possible adverse effects from the drug taken to prevent PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up) | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 9. Caffeine 300 mg versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Number of any possible adverse effects from the drug taken to prevent PDPH | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up) | 1 | Risk Ratio (IV, Fixed, 95% CI) | Totals not selected |
Comparison 10. Dexamethasone versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 2 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2 Number of participants with severe PDPH | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Number of participants with any headache | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Number of missing data (withdrawals, drop‐outs and participants lost to follow‐up) | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 11. Caffeine versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.52, 1.59] |
| 2 Number of participants with severe PDPH | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.33, 2.35] |
| 3 Number of participants with any headache | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.51, 1.24] |
Comparison 12. Aminophylline versus no intervention.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Number of participants affected by PDPH of any severity | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 1.1 Number of participants affected by PDPH of any severity at 24 hours | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Number of participants affected by PDPH of any severity at 48 hours | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abboud 1992.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: US (Los Angeles) Setting: hospital Study design: parallel Randomisation: not described Allocation concealment: not described Blinding: double‐blind Follow‐up period: 3 days |
|
| Participants | Randomised: 82 (intervention group: 40; control group: 42) Excluded (post‐randomisation): not described Gender (women): 82 (100%) Age (years): mean (SD): intervention group: 30.3 (6.3); control group: 29.6 (5.8) Inclusion criteria: healthy pregnant women at term, ASA I or II with no medical complications, who underwent caesarean delivery with spinal anaesthesia Exclusion criteria: not described |
|
| Interventions | Intervention group: intraspinal administration of morphine 0.2 mg in 0.2 mL solution Control group: intraspinal administration of 0.2 mL of normal saline Co‐interventions: spinal anaesthesia with 0.75% bupivacaine in 8.25% dextrose plus 0.2 mL of 1:1000 epinephrine. Hydration with 1500 mL lactated Ringer's solution |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote: "PDPH if it occurred after the patient became ambulatory, was aggravated by sitting or standing position, was relieved by lying supine, and was mostly occipital or frontal" (Page 34) Sample size calculation: quote: "Consultation with a statistician determined the sample size of the study. The statistical approach was analysed to ensure that the power of these data was adequate to decrease below the level of statistical probability that a Type II error could have been made" (Page 35) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided. Quote: "Patients were randomly assigned to receive, in a double‐blind fashion, either 0.2 mg of morphine (Group 1, n = 40) or saline (Group 2, n = 42)..." |
| Allocation concealment (selection bias) | Unclear risk | No information available |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information available |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information available |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Results presented for all 82 randomised patients |
| Selective reporting (reporting bias) | Unclear risk | No information available |
Al‐metwalli 2008.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: Saudi Arabia (Al‐Khobar) Setting: hospital Study design: parallel Randomisation: computer‐generated random number table Allocation concealment: opaque envelope labelled with the study subject number Blinding: double‐blind Follow‐up period: minimum 5 days in those without PDPH and 3 days after resolution of the headache in those with PDPH |
|
| Participants | Randomised: 50 (intervention group: 25, control group: 25) Excluded (post‐randomisation): not described Gender (women): 50 (100%) Age (years): mean (SD): intervention group 28.4 (6.0); control group 29.6 (5.4) Inclusion criteria: postpartum woman with inadvertent dural puncture during epidural analgesia in labour Exclusion criteria: temperature > 37.8 ºC, coagulopathy and delivering by caesarean section |
|
| Interventions | Intervention group: epidural morphine 3 mg in 10 mL saline and repeated the same treatment after 24 h Control group: epidural 10 mL saline and repeated the same treatment after 24 h Co‐interventions: 3 mL of lidocaine 2% with fentanyl 15 μg administered to all patients before delivery to test correct epidural placement. Next, 10 mL bupivacaine 0.25% with 50 μg of fentanyl was injected followed by a continuous infusion of bupivacaine 0.125% with 1 μg/mL of fentanyl at 10 mL/h |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote "PDPH was defined as the presence of a headache or neck ache that improved significantly or completely when the subject assumed the supine position" Sample size calculation: 24 participants calculated estimating an incidence decrease of PDPH from 75% to 35%. Significance level of 0.05 and power of 80% VRSP: 0 = no pain and 10 = worst possible pain |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomised (via a computer‐generated random number table) to treatment (morphine) group or control (saline) group" (Page 848) |
| Allocation concealment (selection bias) | Low risk | Quote: "Group assignment was determined by opening an opaque envelope labelled with the study subject number" (Page 848) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "An anaesthetist, who was blind to the study drug, injected 10 ml saline (control group) or 3 mg of morphine in 10 ml saline (morphine group)" (Page 848) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "An anaesthetist unaware of the treatment group evaluated the subjects postpartum to ascertain the presence of PDPH" (Page 848) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Results presented for all 50 randomised patients |
| Selective reporting (reporting bias) | Low risk | Results presented according to objectives stated in the introductory section |
Devcic 1993.
| Methods | Randomised, blinded, controlled trial Study type: single‐centre study Location: US (Milwaukee) Setting: hospital Study design: parallel Randomisation: not described Allocation concealment: not described Blinding: blinding of patients and outcome assessors Follow‐up period: 3 weeks |
|
| Participants | Randomised: 194 (Sprotte needle with fentanyl: 47; Sprotte needle without fentanyl: 49; Quincke needle with fentanyl: 49; Quincke needle without fentanyl: 49) Excluded (post‐randomisation): not described Gender (women): 194 (100%) Age (years): mean (SD): Sprotte needle with fentanyl: 28.2 (5.8); Sprotte needle without fentanyl: 29.5 (4.4); Quincke needle with fentanyl: 28.3 (5.6), Quincke needle without fentanyl: 28.7 (5.5) Inclusion criteria: healthy obstetric patients requiring caesarean delivery who consented to spinal anaesthesia Exclusion criteria: previously attempted or performed labour epidural analgesia or spinal anaesthesia attempted with other kind of needles |
|
| Interventions | Intervention group: subarachnoid fentanyl 20 μg through a 24‐gauge Sprotte needle or through a 25‐gauge Quincke needle Control group: subarachnoid anaesthesia without fentanyl through a 24‐gauge Sprotte needle or through a 25‐gauge Quincke needle Co‐interventions: all patients received 1000 to 1500 mL of 0.9% normal saline or Ringer's lactate solution before spinal anaesthesia and continued for 48 h Spinal anaesthesia with hyperbaric bupivacaine 0.75% to all patients. The total dose was decided by the anaesthesiologist performing the spinal anaesthesia Opioids via patient–controlled pump during the first 24 h postoperative and followed the next day by oral analgesics as needed |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote: "If the headache occurring on mobilization was aggravated by an erect position and was relieved by lying flat, it was considered to be a PDPH" (Page 223) Sample size calculation: not described PDPH severity: mild (annoying, but tolerable on ambulation, requiring oral analgesics); moderate (very annoying, very uncomfortable on ambulation, requiring bed rest, scheduled analgesia with intravenous fluids); severe (bedridden requiring EBP) Email contact |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Described as blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "All patients were evaluated daily during the first 4 postoperative days by the designated nurse, who was blinded to the type of needle and medication used... Investigators conducting telephone follow‐up were blinded to the type of needle and anaesthetic solution used" (Page 223) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 6 lost to follow‐up described (4 in fentanyl group, 2 in control group), but is unlikely that this loss may influence the outcomes |
| Selective reporting (reporting bias) | High risk | Adverse events not reported |
Doroudian 2011.
| Methods | Randomised, blinded, controlled trial Study type: single‐centre study Location: Iran (Kerman) Setting: admitted to hospital Study design: parallel Randomisation: computer‐generated random allocation Allocation concealment: not described Blinding: blinding of patients and the spinal anaesthesia staff Follow‐up period: 7 days |
|
| Participants | Randomised: 178 (intervention group: 89; control group: 89) Excluded (post‐randomisation): none Gender (women): 61 (34.3%) Age (years): mean (range): intervention group 41.7 (31 to 53); control group 40 (30 to 50) Inclusion criteria: all adults admitted to hospital for lower‐extremity surgery Exclusion criteria: hypo/hypertension, diabetes, dexamethasone intolerance or past hypersensitivity reaction, intake of any analgesic or anti‐inflammatory agent during the week prior to admission, past history of chronic headache, recent‐onset acute headache, contraindication for LP, a surgical procedure estimated to last longer than 90 minutes, current pregnancy, past/active peptic ulcer disease, active systemic fungal infection, any kind of addiction, more than 2 attempts at spinal anaesthesia, any history of cardiopulmonary disorder, long‐term admission, severe post‐spinal haemodynamic changes and strong dependency to tea or caffeine |
|
| Interventions | Intervention group: intravenous dexamethasone 8 mg (2 mL) of before spinal anaesthesia Control group: 2 mL of intravenous normal saline before spinal anaesthesia Co‐interventions: all patients received 500 mL of normal saline intravenously before intervention and spinal anaesthesia |
|
| Outcomes |
|
|
| Notes | PDPH defined as: an exclusion criteria was: quote: "long term admission which does not permit patient to resume the upright position within the first 7 days" (Page 144) and Class I intensity headache was: quote: "Patient suffers from a mild headache while sitting or walking" (Page 144) Sample size calculation: not described PDPH severity: Class I: "Patient suffers from a mild headache while sitting or walking", Class II: "Patient suffers from a moderate to severe headache while sitting or walking" and Class III: "Patient suffers from a moderate to severe headache even in supine position which impedes his/her daily activities" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization process was performed using Random Allocation Software®" (Page 143) |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "For all injections, the anesthetic staff was blind with respect to the group allocation whereas patients were also unaware regarding the content of the study injectate" (Page 144) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Results presented for all 178 randomised patients |
| Selective reporting (reporting bias) | High risk | Adverse events not reported |
Esmaoglu 2005.
| Methods | Randomised, blinded, controlled trial Study type: single‐centre study Location: Turkey (Kayseri) Setting: admitted to hospital Study design: parallel Randomisation: not described Allocation concealment: not described Blinding: outcome assessors and probably patients Follow‐up period: 7 days |
|
| Participants | Randomised: 210 (caffeine 75 group: 70; caffeine 125 group: 70; control group: 70) Excluded (post‐randomisation): not described Gender (women): 83 (39.5%) Age (years): mean (SD): caffeine 75 group: 38 (12); caffeine 125 group: 38 (11); control group: 37 (14) Inclusion criteria: patients scheduled for elective lower extremity surgery, ASA I‐II Exclusion criteria: hypertension, diabetes mellitus, caffeine consumption > 250 mg/day, intolerance to caffeine, chronic headache, contraindication to spinal anaesthesia |
|
| Interventions | Caffeine 75 group: paracetamol 500 mg + caffeine 75 mg orally Caffeine 125 group: paracetamol 500 mg + caffeine 125 mg orally Control group: placebo orally All 3 groups received intervention 1 h before the spinal anaesthesia and the same doses repeated every 6 hours for 3 days. Spinal anaesthesia with 3 mL of hyperbaric bupivacaine 0.5% Co‐interventions: all patients hydrated with at least 0.5 L of intravenous crystalloid solution before the procedure |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote: "headache was categorized as a PDPH if it was worse on sitting or standing and relieved or reduced by lying flat" (Page 59) PDPH severity: quote: "class I, mild headache when sitting or ambulating; class II, moderate to severe headache when sitting or ambulating; and class III, moderate to severe headache when supine" (Page 60) Sample size calculation: not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The interviewer was blinded as to study group assignment" (Page 59) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No explicit information but it seems that no patients were lost |
| Selective reporting (reporting bias) | Unclear risk | No information available |
Flaatten 1987.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: Norway (Bergen) Setting: admitted to hospital Study design: parallel Randomisation: not described Allocation concealment: not described Blinding: double‐blind Follow‐up period: 3 days |
|
| Participants | Randomised: 250 (intervention group: 125; control group: 125) Excluded (post‐randomisation): not described Gender (women): 85 (34%) Age (years): mean: intervention group 34.2; control group 33.0 Inclusion criteria: young (< 55 years old) hospitalised patients of either sex of ASA groups I and II, receiving spinal anaesthesia Exclusion criteria: not described |
|
| Interventions | Intervention group: indomethacin 100 mg per rectum 4 hours post operation Control group: placebo per rectum 4 hours post operation Co‐interventions: all spinal anaesthesia were performed using a 25‐G spinal needle |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote "occurred after mobilisation, aggravated by the erect or sitting position, relieved by lying flat, mostly occipital or frontal, accompanied by dizziness, vomiting, rigidity of the neck and visual disturbances" (Page 202) Sample size calculation: not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided. Quote: "following this they were randomly allocated in a double‐blind manner to receive either indomethacin 100mg or a placebo per rectum 4 hours postoperatively" (Page 202) |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Three patients were lost to follow‐up and their results are not included in the study." (Page 202). All 3 patients from placebo group, and not reasons stated. Unlikely to produce bias, but incomplete information available |
| Selective reporting (reporting bias) | Unclear risk | No information available |
Hakim 2010.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: Egypt (Cairo) Setting: admitted to hospital Study design: parallel Randomisation: computer‐generated random number list Allocation concealment: yes Blinding: blinding of patients, hospital health personnel and outcome assessors Follow‐up period: 14 days |
|
| Participants | Randomised: 95 (intervention group: 47; control group: 48) Excluded (post randomisation): 5 (intervention group: 2; control group: 3) Gender (women): 95 (100%) Age (years): mean (SD): intervention group: 31.3 (4.8); control group: 29.7 (4.9) Inclusion criteria: parturients who had epidural analgesia for normal vaginal delivery and who suffered an inadvertent dural tap Exclusion criteria: contraindication to steroid or ACTH therapy (e.g. hypertension or diabetes mellitus), pre‐eclampsia, or contraindication to EBP (e.g. fever or leukocytosis) |
|
| Interventions | Intervention group: cosyntropin 1 mg (Cortrosy®, Amphastar Pharmaceuticals Inc) in 1 mL solution, intravenously over 5 min Control group: 1 mL of normal saline intravenously Co‐interventions: epidural analgesia: test with 3 mL of 2% lidocaine with 1:200,000 epinephrine. Loading dose of 8 to 15 mL of bupivacaine 0.125% plus fentanyl 50 μg. Continuous infusion of bupivacaine 0.125% with fentanyl 2 μg/mL at 8 to 15 mL/h. Patients with accidental dural puncture were encouraged to ambulate and to drink plenty of fluids, with prescription of stool softeners |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote: "PDPH if they developed headache within 5 days after dural puncture, which worsened within 15 min of sitting or standing, and improved within 15 min after lying, with at least one of the following criteria: neck stiffness, tinnitus, hypacusia, photophobia, or nausea" (Page 414) Sample size calculation: estimated 44 patients in each group for detecting at least a 30% difference between the groups the incidence of PDPH, a beta error of 0.2, 2‐tailed alfa‐error of 0.05 and degree of freedom of 1 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Patients were randomly assigned to one of two groups using a computer‐generated random number list. The list was created using the GraphPad StatMate version 1.01i software" (Page 414) |
| Allocation concealment (selection bias) | Low risk | Quote: "The list... was accessible to anaesthesiologist attending to patients in labor through the computer database" (Page 414) |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Injections were prepared by assistants not participating in the study, and both the patients and those involved in the study were blinded as to the patients' group" (Page 414) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Nurses and anaesthesiologists involved in headache assessment were blinded as to the patients' group" (Page 414) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Flowchart showing incidence of accidental dural puncture, patient recruitment and randomisation, incidence of PDPH and need for EBP and repeat EBP" (Page 415) |
| Selective reporting (reporting bias) | Low risk | Results presented according to objectives stated in the introductory section |
Sadeghi 2012.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: Iran (Shiraz) Setting: admitted to hospital Study design: parallel Randomisation: not described Allocation concealment: not described Blinding: double‐blind (patient and researcher) Follow‐up period: 48 hours after elective caesarean section |
|
| Participants | Randomised: 120 (intervention group: 60; control group: 60) Excluded (post‐randomisation): not described Gender (women): 120 (100%) Age (years): mean (SD): intervention group 26.11 (4.4); control group 26.35 (5.3) Inclusion criteria: patients undergoing elective caesarean section Exclusion criteria: headache, psychiatric problems, back pain, pre‐eclampsia, coagulation disorders, convulsion background, spinal anaesthesia history and those who used any kinds of opiates |
|
| Interventions | Intervention group: after the child birth and umbilical cord clamping, aminophylline 1 mg/kg intravenously Control group: no intervention Co‐interventions: 2 mL lidocaine 1% used for skin anaesthesia. A combination of 55 mg lidocaine 5% (dose and concentration as cited in the publication) and meperidine 5 mg were used for spinal anaesthesia. Needle nº 23 used for the spinal anaesthesia. In case of hypotension in both groups, ephedrine 5 mg intravenously. In both groups, the patients rested 24 h after the operation and then started walking |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote "Post dural puncture headache (PDPH) is a kind of headache that worsens by standing up and dwindles with recumbency" (Page 13) Sample size calculation: not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were randomly divided into two groups with an accidental allocation" (Page 14) |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "double‐blind randomised study (patient and researcher)" (Page 14) Quote: "data collection performed by a trained nurse that did not know anything about the intervention, the other stages of the study were performed by the doctors who knew the whole project and it may cause bias in the study" (Page 15) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "data collection performed by a trained nurse that did not know anything about the intervention, the other stages of the study were performed by the doctors who knew the whole project and it may cause bias in the study" (Page 15) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No explicit information but it seems that no patients were lost |
| Selective reporting (reporting bias) | High risk | Adverse events not reported |
Strelec 1994.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: US (Pittsburgh) Setting: hospital Study design: parallel Randomisation: not described Allocation concealment: not described Blinding: described as double‐blind Follow‐up period: 4 days |
|
| Participants | Randomised: 60 (intervention group: 30; control group: 30) Excluded (post randomisation): 2 (intervention group: 0; control group: 2) Gender (women): 18 (31%) Age (years): mean (SD): intervention group: 40.2 (13.3); control group: 48.5 (13) Inclusion criteria: participants who have had a lumbar myelography Exclusion criteria: not described |
|
| Interventions | Intervention group: oral anhydrous caffeine capsules, 300 mg every 8 hours for 3 days Control group: placebo capsules every 8 hours for 3 days Co‐interventions: all other caffeinated substances were forbidden |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote: "PDPH criteria included postural headache, associated N/V, photophobia and neck stiffness" (Page 79) Sample size calculation: not described |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information provided |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | No information provided |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No information provided |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 2 lost. No information provided about the reasons or the moment, but unlikely this is a cause of bias |
| Selective reporting (reporting bias) | Low risk | Results presented according to objectives stated in the introductory section |
Yousefshahi 2012.
| Methods | Randomised, double‐blind, controlled trial Study type: single‐centre study Location: Iran (Tehran) Setting: admitted to hospital Study design: parallel Randomisation: computer‐generated random number list Allocation concealment: not described Blinding: described as double‐blind Follow‐up period: 3 days |
|
| Participants | Randomised: 372 (intervention group: 186; control group: 186) Excluded (post randomisation): 12 (intervention group: 4; control group: 8) Gender (women): 372 (100%) Age (years): mean: intervention group: 28.5; control group: 28.9 Inclusion criteria: parturient after spinal anaesthesia for caesarean section Exclusion criteria: patients ASA class higher than II, sensitive to local anaesthetics, anticoagulant therapy, pre‐eclampsia or skin infection at the site of needle insertion |
|
| Interventions | Intervention group: intravenous dexamethasone 8 mg (2 mL) after clamping the umbilical cord Control group: 2 mL of intravenous normal saline after clamping the umbilical cord Co‐interventions: all patients received 500 mL of normal saline or Ringer's solution intravenously before spinal anaesthesia. Ondansetron, metoclopramide and H2‐blockers as needed |
|
| Outcomes |
|
|
| Notes | PDPH defined as: quote: "PDPH was defined as a headache located in the occipital and/or frontal areas which was worsened by standing or sitting, and alleviates by lying down" (Page 2) Sample size calculation: quote: "The study was designed to achieve 80 % power to detect a 15 % difference in the population, in which the prevalence of the condition was 8.9 % based on previous studies. The level of statistical significance was reported to be 5 %" (Page 3) Email contact with Fardin Yousefshahi MD on April 2012 for clarification about missing data |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were divided into two groups based on a computer random number generator" (Page 2) |
| Allocation concealment (selection bias) | Unclear risk | No information provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Each patient received a specific row number for grouping into the dexamethasone or placebo group, corresponding to a computerized randomization system; grouping was not reflected in the patient’s data sheet" (Page 2) |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Trained nurses, who were unaware of the objectives of the study, asked the patients about any occurrence of headache every 24 h for 72 h. The patients complaining of possible PDPH were then visited by an anesthesiologist, similarly unaware of the study objectives, to rule out other causes of headache" (Page 2) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: "Twelve patients were excluded from the study due to missing data" (Page 2). 4 patients from the intervention group and 8 from the control group |
| Selective reporting (reporting bias) | Low risk | Results presented according to objectives stated in the introductory section |
ACTH: adrenocorticotropic hormone; ASA: American Society of Anesthesiologists; EBP: epidural blood patch; LP: lumbar puncture; PDPH: post‐dural puncture headache; SD: standard deviation; VRSP: Verbal Rating Score for Pain.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ackerman 2004 | No individual drug assessed |
| Altunkaya 2005 | The study did not focus on PDPH |
| Aziz 1968 | The orthostatic component of headache not described |
| Balestrieri 2003 | The study was not a RCT (letter) |
| Beilin 2003 | The orthostatic component of headache not described |
| Breebaart 2003 | The study did not focus on PDPH |
| Caldwell 1994 | The orthostatic component of headache not described |
| Camann 1992 | The orthostatic component of headache not described |
| Camann 1993 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Campbell 1995 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Cesur 2009 | The study was not a RCT (retrospective observational study) |
| Chalmers 1988 | The study did not focus on PDPH Intervention was not aimed at preventing PDPH |
| Chilvers 1997 | Intervention was not aimed at preventing PDPH |
| Cho 2008 | The study did not focus on PDPH |
| Clarke 2009 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Colonna‐Romano 1989 | No individual drug assessed |
| Cowan 1980 | The orthostatic component of headache not described |
| D'Angelo 1994 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Danelli 2004 | The study did not focus on PDPH |
| Dayioglu 2009 | The orthostatic component of headache not described |
| De Pietri 2006 | The orthostatic component of headache not described |
| Delfino 2001 | The orthostatic component of headache not described |
| Dijkstra 2008 | The orthostatic component of headache not described Intervention was not aimed to prevent PDPH |
| Dilli 2008 | The study did not focus on PDPH |
| Dominguez‐Hervella 1993 | The orthostatic component of headache not described |
| Edström 1986 | The orthostatic component of headache not described |
| Elkhodair 2010 | The study was not a RCT (Critically Appraised Topics) |
| Fogarty 1993 | The study did not focus on PDPH |
| Fogarty 1995 | The study did not focus on PDPH |
| Frey 1998 | The orthostatic component of headache not described |
| Frizelle 1997 | The orthostatic component of headache not described |
| Fu 2008 | The study did not focus on PDPH |
| Fujii 1998 | The study did not focus on PDPH |
| Förster 2006 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Gangopadhyay 2010 | The orthostatic component of headache not described |
| Ganzi 1995 | No individual drug assessed |
| Garg 2010 | The study did not focus on PDPH |
| Gielen 1986 | The study did not focus on PDPH |
| Ginsberg 1996 | The study did not focus on PDPH |
| Girgin 2008 | The study did not focus on PDPH |
| Gogarten 2004 | The study did not focus on PDPH |
| Gurbet 2008 | The study did not focus on PDPH |
| Hansen 1979 | The orthostatic component of headache not described |
| Hansen 1980 | The study was not a RCT (letter) |
| Harsten 1997 | The orthostatic component of headache not described |
| Hein 2010 | The orthostatic component of headache not described |
| Hendriks 2009 | The orthostatic component of headache not described |
| Ilioff 1990 | The orthostatic component of headache not described |
| Imbelloni 2003 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Imbelloni 2009 | Intervention was not aimed at preventing PDPH |
| Imbelloni 2010 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Jacobsohn 2005 | The orthostatic component of headache not described |
| Kallio 2004 | The study did not focus on PDPH |
| Kallio 2005 | The study did not focus on PDPH |
| Kaukinen 1981 | Allocation was not randomised |
| Kouri 2004 | The study did not focus on PDPH |
| Lanz 1982 | The study did not focus on PDPH |
| Lauretti 1999 | The study did not focus on PDPH |
| Lauretti 1999b | The study did not focus on PDPH |
| Lauretti 2000 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Lauretti 2000b | The study did not focus on PDPH |
| Lee 2005 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Lewis 1992 | The study did not focus on PDPH |
| Lierz 2004 | The study did not focus on PDPH |
| Luck 2008 | The study did not focus on PDPH |
| López‐Soriano 2002 | The orthostatic component of headache not described |
| Manaa 2005 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Martlew 2009 | The study was not a RCT (letter) |
| Massou 2008 | The study was not a RCT (letter) |
| Meininger 2003 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Michalek‐Sauberer 2008 | The orthostatic component of headache not described |
| Morrison 1994 | The study did not focus on PDPH |
| Mosavy 1975 | Allocation was not randomised |
| Murto 1999 | The orthostatic component of headache not described |
| Møller 1984 | The orthostatic component of headache not described |
| Neilson 2008 | The study did not focus on PDPH |
| Ogun 2003 | The study did not focus on PDPH |
| Paech 1993 | The orthostatic component of headache not described |
| Palahniuk 1979 | Allocation was not randomised No individual drug assessed |
| Pan 2001 | The study did not focus on PDPH |
| Patra 2005 | The study did not focus on PDPH |
| Phero 1987 | The orthostatic component of headache not described |
| Plaja 2000 | The study did not focus on PDPH |
| Prusinski 1974 | Allocation was not randomised |
| Radpay 2003 | The study did not focus on PDPH |
| Reinhart 1985 | The study did not focus on PDPH |
| Rivera‐Ordonez 2005 | The study did not focus on PDPH |
| Roux 1983 | The orthostatic component of headache not described |
| Rucci 1985 | The study did not focus on PDPH |
| Ryan 1983 | The study did not focus on PDPH |
| Sakaguchi 2000 | The study did not focus on PDPH |
| Sangarlangkarn 1987 | The orthostatic component of headache not described |
| Sanli 2005 | Intervention was not aimed at preventing PDPH |
| Santos 1986 | The study was not a RCT (no control group) The orthostatic component of headache not described |
| Sawhney 2004 | The study did not focus on PDPH |
| Sengupta 1989 | No individual drug assessed |
| Seyhan 2005 | The study was not a RCT (no control group) |
| Shah 2003 | The study did not focus on PDPH |
| Singh 2006 | The study did not focus on PDPH |
| Smith 2004 | The study did not focus on PDPH |
| Soni 2001 | The study did not focus on PDPH |
| Sudarshan 1995 | The study did not focus on PDPH |
| Tekin 2007 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Thomas 2006 | The study did not focus on PDPH |
| Trivedi 1993 | Epidural saline infusion was not used as a pharmacological agent |
| Tsen 2001 | The orthostatic component of headache not described |
| Tucker 2004 | The study did not focus on PDPH |
| Tuncer 2005 | The study did not focus on PDPH |
| Turan 2006 | The study did not focus on PDPH |
| Turker 2003 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Unlugenc 2006 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Unlugenc 2009 | The orthostatic component of headache not described Intervention was not aimed at preventing PDPH |
| Usubiaga 1967 | Allocation was not randomised No individual drug assessed |
| Vaghadia 1997 | Intervention was not aimed at preventing PDPH |
| Vale 1995 | The study did not focus on PDPH |
| Vichitvejpaisal 1992 | Intervention was not aimed at preventing PDPH |
| Viscusi 2005 | The study did not focus on PDPH |
| Waxler 2004 | The study did not focus on PDPH |
| Wells 2004 | The study did not focus on PDPH |
| Whiteside 2003 | Intervention was not aimed at preventing PDPH |
| Widerlöv 1979 | The orthostatic component of headache not described |
| Wilder‐Smith 1998 | The study did not focus on PDPH |
| Wood 1993 | The study did not focus on PDPH |
| Yanagidate 2004 | The study did not focus on PDPH |
| Yeh 2000 | The study did not focus on PDPH |
| Yücel 1999 | The orthostatic component of headache not described |
| Zackova 2000 | The study did not focus on PDPH |
PDPH: post‐dural puncture headache; RCT: randomised controlled trial
Differences between protocol and review
Types of participants: “The use of a standardized diagnostic criteria for PDPH was not required, but it should at least be described as orthostatic headache which worsens on standing and improved by lying down.” The “it should at least be” has been added to emphasise the need to include only those studies that have used an orthostatic headache criteria to include participants.
PaPaS Review Group Specialised Register electronic search eliminated.
CINAHL search strategy included.
Background has been adapted with a previous published Cochrane review on treatment drugs for PDPH (Basurto 2011).
Contributions of authors
Conceiving the review (guarantor): Xavier Basurto (XB).
Screening search results: XB, Sonia Uriona (SU).
Screening retrieved papers against inclusion criteria: XB, SU, Laura Martínez (LM), Ivan Solà (IS), Xavier Bonfill Cosp (XBC).
Appraising quality of papers: XB, LM, SU.
Extracting data from papers: XB, LM, SU.
Data management for the review: XB, LM.
Entering data into Review Manager (RevMan 5.1): XB, LM.
Interpretation of data: XB, LM, IS, XBC.
Statistical analysis: XB, LM, IS.
Writing the review: XB, LM, SU, IS.
Comment and editing of review drafts: XB, LM, SU, IS, XBC.
Responsible for reading and checking review before submission: XB, LM, IS, XBC.
Responsible for initiating and running the update of this review: XB.
Sources of support
Internal sources
Iberoamerican Cochrane Centre, Spain.
CIBER de Epidemiología y Salud Pública (CIBERESP), Spain.
External sources
Agencia de Calidad del Sistema Nacional de Salud, Ministerio de Salud y Consumo, Spain.
Declarations of interest
None known.
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Abboud 1992 {published data only}
- Abboud TK, Zhu J, Reyes A. Effect of subarachnoid morphine on the incidence of spinal headache. Regional Anesthesia 1992;17(1):34‐6. [PubMed] [Google Scholar]
Al‐metwalli 2008 {published data only}
- Al‐metwalli RR. Epidural morphine injections for prevention of post dural puncture headache. Anaesthesia 2008;63(8):847‐50. [DOI] [PubMed] [Google Scholar]
Devcic 1993 {published data only}
- Devcic A, Sprung J, Patel S, Kettler R, Maitra‐D'Cruze A. PDPH in obstetric anesthesia: comparison of 24‐gauge Sprotte and 25‐gauge Quincke needles and effect of subarachnoid administration of fentanyl. Regional Anesthesia 1993;18(4):222‐5. [PubMed] [Google Scholar]
Doroudian 2011 {published data only}
- Doroudian MR, Norouzi M, Esmailie M, Tanhaeivash R. Dexamethasone in preventing post‐dural puncture headache: a randomized, double‐blind, placebo‐controlled trial. Acta Neurologica Belgica 2011;62:143‐6. [PubMed] [Google Scholar]
Esmaoglu 2005 {published data only}
- Esmaoglu A, Akpinar H, Uğur F. Oral multidose caffeine‐paracetamol combination is not effective for the prophylaxis of postdural puncture headache. Journal of Clinical Anesthesia 2005;17(1):58‐61. [DOI] [PubMed] [Google Scholar]
Flaatten 1987 {published data only}
- Flaatten H, Rodt S, Rosland J, Vamnes J. Postoperative headache in young patients after spinal anaesthesia. Anaesthesia 1987;42(2):202‐5. [DOI] [PubMed] [Google Scholar]
Hakim 2010 {published data only}
- Hakim SM. Cosyntropin for prophylaxis against postdural puncture headache after accidental dural puncture. Anesthesiology 2010;113(2):413‐20. [DOI] [PubMed] [Google Scholar]
Sadeghi 2012 {published data only}
- Sadeghi SE, Abdollahifard G, Nasabi NA, Mehrabi M, Safarpour AR. Effectiveness of single dose intravenous aminophylline administration on prevention of post dural puncture headache in patients who received spinal anesthesia for elective cesarean section. World Journal of Medical Sciences 2012;7(1):13‐6. [Google Scholar]
Strelec 1994 {published data only}
- Strelec S, Prylinski J, Sakert T, Royal M. The efficacy of multi‐dose oral caffeine in prevention of post‐dural puncture headache. Regional Anesthesia 1994;19(2S):79. [Google Scholar]
Yousefshahi 2012 {published data only}
- Yousefshahi F, Dahmardeh AR, Khajavi M, Najafi A, Khashayar P, Barkhordari K. Effect of dexamethasone on the frequency of postdural puncture headache after spinal anesthesia for cesarean section: a double‐blind randomized clinical trial. Acta Neurologica Belgica 2012 Apr 20 [Epub ahead of print]. [DOI] [PubMed]
References to studies excluded from this review
Ackerman 2004 {published data only}
- Ackerman WE, Juneja MM, Kaczorowski DM. Prophylactic epidural blood patch for the prevention of postdural puncture headache in the parturient. Anesthesiology Review 1990;17(2):45‐9. [Google Scholar]
Altunkaya 2005 {published data only}
- Altunkaya H, Ozer Y, Demirel CB, Ozkocak I, Keser S, Bayar A. Preoperative multimodal administration of morphine in arthroscopic surgery. Archives of Orthopaedic and Trauma Surgery 2005;125(9):609‐13. [DOI] [PubMed] [Google Scholar]
Aziz 1968 {published data only}
- Aziz H, Pearce J, Miller E. Vasopressin in prevention of lumbar puncture headache. British Medical Journal 1968;4(5632):677‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Balestrieri 2003 {published data only}
- Balestrieri PJ. The incidence of postdural puncture headache and combined spinal‐epidural: some thoughts. International Journal of Obstetric Anesthesia 2003;12(4):305‐6. [DOI] [PubMed] [Google Scholar]
Beilin 2003 {published data only}
- Beilin Y, Zahn J, Abramovitz S, Bernstein H, Hossain S, Bodian C. Subarachnoid small‐dose bupivacaine versus lidocaine for cervical cerclage. Anesthesia and Analgesia 2003;97(1):56‐61. [DOI] [PubMed] [Google Scholar]
Breebaart 2003 {published data only}
- Breebaart MB, Vercauteren MP, Hoffmann VL, Adriaensen HA. Urinary bladder scanning after day‐case arthroscopy under spinal anaesthesia: comparison between lidocaine, ropivacaine, and levobupivacaine. British Journal of Anaesthesia 2003;3:309‐13. [DOI] [PubMed] [Google Scholar]
Caldwell 1994 {published data only}
- Caldwell LE, Rosen MA, Shnider SM. Subarachnoid morphine and fentanyl for labor analgesia. Efficacy and adverse effects. Regional Anesthesia 1994;19(1):2‐8. [PubMed] [Google Scholar]
Camann 1992 {published data only}
- Camann WR, Denney RA, Holby ED, Datta S. A comparison of intrathecal, epidural, and intravenous sufentanil for labor analgesia. Anesthesiology 1992;77(5):884‐7. [DOI] [PubMed] [Google Scholar]
Camann 1993 {published data only}
- Camann WR, Minzter BH, Denney RA, Datta S. Intrathecal sufentanil for labor analgesia. Effects of added epinephrine. Anesthesiology 1993;78(5):870‐4. [DOI] [PubMed] [Google Scholar]
Campbell 1995 {published data only}
- Campbell DC, Camann WR, Datta S. The addition of bupivacaine to intrathecal sufentanil for labor analgesia. Anesthesia and Analgesia 1995;81(2):305‐9. [DOI] [PubMed] [Google Scholar]
Cesur 2009 {published data only}
- Cesur M, Alici HA, Erdem AF, Silbir F, Celik M. Decreased incidence of headache after unintentional dural puncture in patients with cesarean delivery administered with postoperative epidural analgesia. Journal of Anesthesia 2009;23(1):31‐5. [DOI] [PubMed] [Google Scholar]
Chalmers 1988 {published data only}
- Chalmers PC, Lang CM, Harte FA, Greenhouse BB. Double‐blind comparison of intravenous nalbuphine and placebo in the amelioration of side‐effects of epidural narcotics. Pain Clinic 1988;2(1):49‐56. [Google Scholar]
Chilvers 1997 {published data only}
- Chilvers CR, Vaghadia H, Mitchell GW, Merrick PM. Small‐dose hypobaric lidocaine‐fentanyl spinal anesthesia for short duration outpatient laparoscopy. II. Optimal fentanyl dose. Anesthesia and Analgesia 1997;84(1):65‐70. [DOI] [PubMed] [Google Scholar]
Cho 2008 {published data only}
- Cho JE, Kim JY, Kim JE, Chun DH, Jun NH, Kil HK. Epidural sufentanil provides better analgesia from 24 h after surgery compared with epidural fentanyl in children. Acta Anaesthesiologica Scandinavica 2008;52(10):1360‐3. [DOI] [PubMed] [Google Scholar]
Clarke 2009 {published data only}
- Clarke H, Pereira S, Kennedy D, Gilron I, Katz J, Gollish J, et al. Gabapentin decreases morphine consumption and improves functional recovery following total knee arthroplasty. Pain Research and Management 2009;14(3):217‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Colonna‐Romano 1989 {published data only}
- Colonna‐Romano P, Shapiro BE. Unintentional dural puncture and prophylactic epidural blood patch in obstetrics. Anesthesia and Analgesia 1989;69:522‐3. [PubMed] [Google Scholar]
Cowan 1980 {published data only}
- Cowan JM, Durward WF, Harrington H, Johnston JH, Donovan B. DDAVP in the prevention of headache after lumbar puncture. British Medical Journal 1980;280(6209):224. [DOI] [PMC free article] [PubMed] [Google Scholar]
D'Angelo 1994 {published data only}
- D'Angelo R, Anderson MT, Philip J, Eisenach JC. Intrathecal sufentanil compared to epidural bupivacaine for labor analgesia. Anesthesiology 1994;80(6):1209‐15. [DOI] [PubMed] [Google Scholar]
Danelli 2004 {published data only}
- Danelli G, Fanelli G, Berti M, Cornini A, Lacava L, Nuzzi M, et al. Spinal ropivacaine or bupivacaine for cesarean delivery: a prospective, randomized, double‐blind comparison. Regional Anesthesia and Pain Medicine 2004;29(3):221‐6. [DOI] [PubMed] [Google Scholar]
Dayioglu 2009 {published data only}
- Dayioglu H, Baykara ZN, Salbes A, Solak M, Toker K. Effects of adding magnesium to bupivacaine and fentanyl for spinal anesthesia in knee arthroscopy. Journal of Anesthesia 2009;23(1):19‐25. [DOI] [PubMed] [Google Scholar]
Delfino 2001 {published data only}
- Delfino J, Do Vale NB. Spinal anesthesia with 0.5% isobaric ropivacaine or levobupivacaine for lower limb surgeries. Revista Brasileira de Anestesiologia 2001;51(2):91‐7. [Google Scholar]
De Pietri 2006 {published data only}
- Pietri L, Siniscalchi A, Reggiani A, Masetti M, Begliomini B, Gazzi M, et al. The use of intrathecal morphine for postoperative pain relief after liver resection: a comparison with epidural analgesia. Anesthesia and Analgesia 2006;102(4):1157‐63. [DOI] [PubMed] [Google Scholar]
Dijkstra 2008 {published data only}
- Dijkstra T, Reesink JA, Verdouw BC, Pol WS, Feberwee T, Vulto AG. Spinal anaesthesia with articaine 5% vs bupivacaine 0.5% for day‐case lower limb surgery: a double‐blind randomized clinical trial. British Journal of Anaesthesia 2008;100(1):104‐8. [DOI] [PubMed] [Google Scholar]
Dilli 2008 {published data only}
- Dilli D, Dallar Y, Sorgui NH. Intravenous ketamine plus midazolam vs. intravenous ketamine for sedation in lumbar puncture: a randomized controlled trial. Indian Pediatrics 2008;45(11):899‐904. [PubMed] [Google Scholar]
Dominguez‐Hervella 1993 {published data only}
- Domínguez‐Hervella FD, Rey MS, Guede GR, Martín V, Martínez J, Castro A. Combined subarachnoid and epidural block with a single injection, with a modified Tuohy needle and used in hip surgery. Revista Española de Anestesiología y Reanimación 1993;40(5):279‐83. [PubMed] [Google Scholar]
Edström 1986 {published data only}
- Edström HH, Blitt CD, Draper EM, Manny BT, Hameroff SR. Hypotension in spinal anesthesia: a comparison of tetracaine and bupivacaine. Regional Anesthesia and Pain Medicine 1986;11:139‐42. [Google Scholar]
Elkhodair 2010 {published data only}
- Elkhodair S. Towards evidence based emergency medicine: best BETs from the Manchester Royal Infirmary. Bet 1. Caffeine in the prophylaxis of postlumbar puncture headache. Emergency Medicine Journal 2010;27(6):476‐7. [DOI] [PubMed] [Google Scholar]
Fogarty 1993 {published data only}
- Fogarty DJ, Carabine UA, Milligan KR. Comparison of the analgesic effects of intrathecal clonidine and intrathecal morphine after spinal anaesthesia in patients undergoing total hip replacement. British Journal of Anaesthesia 1993;71(5):661‐4. [DOI] [PubMed] [Google Scholar]
Fogarty 1995 {published data only}
- Fogarty DJ, O'Hanlon JJ, Milligan KR. Intramuscular ketorolac following total hip replacement with spinal anaesthesia and intrathecal morphine. Acta Anaesthesiologica Scandinavica 1995;39(2):191‐4. [DOI] [PubMed] [Google Scholar]
Förster 2006 {published data only}
- Förster JG, Rosenberg PH, Niemi TT. Continuous spinal microcatheter (28 gauge) technique for arterial bypass surgery of the lower extremities and comparison of ropivacaine with or without morphine for postoperative analgesia. British Journal of Anaesthesia 1996;97(3):393–400. [DOI] [PubMed] [Google Scholar]
Frey 1998 {published data only}
- Frey K, Holman S, Mikat‐Stevens M, Vazquez J, White L, Pedicini E, et al. The recovery profile of hyperbaric spinal anesthesia with lidocaine, tetracaine, and bupivacaine. Regional Anesthesia and Pain Medicine 1998;23(2):159‐63. [DOI] [PubMed] [Google Scholar]
Frizelle 1997 {published data only}
- Frizelle HP, Duranteau J, Samii K. A comparison of propofol with a propofol‐ketamine combination for sedation during spinal anesthesia. Anesthesia and Analgesia 1997;84(6):1318‐22. [DOI] [PubMed] [Google Scholar]
Fu 2008 {published data only}
- Fu RQ, Tian YK, Fang WR. Combined spinal and epidural anaesthesia with chloroprocaine for hysterectomy. Clinical and Experimental Pharmacology & Physiology 2008;35(1):60‐3. [DOI] [PubMed] [Google Scholar]
Fujii 1998 {published data only}
- Fujii Y, Tanaka H, Toyooka H. Prevention of nausea and vomiting with granisetron, droperidol and metoclopramide during and after spinal anaesthesia for caesarean section: a randomized, double‐blind, placebo‐controlled trial. Acta Anaesthesiologica Scandinavica 1998;42(8):921‐5. [DOI] [PubMed] [Google Scholar]
Gangopadhyay 2010 {published data only}
- Gangopadhyay S, Gupta K, Acharjee S, Nayak SK, Dawn S, Piplai G. Ketamine, tramadol and pethidine in prophylaxis of shivering during spinal anaesthesia. Journal of Anaesthesiology Clinical Pharmacology 2010;26(1):59‐63. [Google Scholar]
Ganzi 1995 {published data only}
- Ganzi F, Ganzi L, Sabo D, Mandell G, Ramanathan S, Patel R. Incidence of spinal headache after spinal anesthesia: a prospective randomized study. Anesthesia and Analgesia 1995;80:S143. [Google Scholar]
Garg 2010 {published data only}
- Garg A, Ahmed F, Khandelwal M, Chawla V, Verma AP. The effect of transdermal nitroglycerine on intrathecal fentanyl with bupivacaine for postoperative analgesia following gynaecological surgery. Anaesthesia and Intensive Care 2010;38(2):285‐90. [DOI] [PubMed] [Google Scholar]
Gielen 1986 {published data only}
- Gielen M, Huho J, DeGrood PM, Edström HH. A double‐blind evaluation of hyperbaric solutions of bupivacaine 0.5% and lidocaine 5% in spinal anesthesia. Regional Anesthesia 1986;11:176‐81. [Google Scholar]
Ginsberg 1996 {published data only}
- Ginsberg L, Caine SE, Valentine AR. Corticosteroids and the prevention of adverse reactions to myelography. British Journal of Neurosurgery 1996;10(3):285‐7. [DOI] [PubMed] [Google Scholar]
Girgin 2008 {published data only}
- Girgin NK, Gurbet A, Turker G, Bulut T, Demir S, Kilic N, et al. The combination of low‐dose levobupivacaine and fentanyl for spinal anaesthesia in ambulatory inguinal herniorrhaphy. Journal of International Medical Research 2008;36(6):1287‐92. [DOI] [PubMed] [Google Scholar]
Gogarten 2004 {published data only}
- Gogarten W, Velde M, Soetens F, Aken H, Brodner G, Gramke HF, et al. A multicentre trial comparing different concentrations of ropivacaine plus sufentanil with bupivacaine plus sufentanil for patient‐controlled epidural analgesia in labour. European Journal of Anaesthesiology 2004;21(1):38‐45. [DOI] [PubMed] [Google Scholar]
Gurbet 2008 {published data only}
- Gurbet A, Turker G, Girgin NK, Aksu H, Bahtiyar NH. Combination of ultra‐low dose bupivacaine and fentanyl for spinal anaesthesia in out‐patient anorectal surgery. Journal of International Medical Research 2008;365:964‐70. [DOI] [PubMed] [Google Scholar]
Hansen 1979 {published data only}
- Hansen PE, Hansen JH. DDAVP, a synthetic analogue of vasopressin, in prevention of headache after lumbar puncture and lumbar pneumoencephalography. Acta Neurologica Scandinavica 1979;60(3):183‐8. [DOI] [PubMed] [Google Scholar]
Hansen 1980 {published data only}
- Hansen PE, Hansen JH. Desmopressin (DDAVP) in lumbar puncture. British Medical Journal 1980;280(6223):1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harsten 1997 {published data only}
- Harsten A, Gillberg L, Håkansson L, Olsson M. Intrathecal sufentanil compared with epidural bupivacaine analgesia in labour. European Journal of Anaesthesiology 1997;14(6):642‐5. [DOI] [PubMed] [Google Scholar]
Hein 2010 {published data only}
- Hein A, Rosblad P, Norman M, Ryniak S, Tingaker B, Jakobsson J, et al. Addition of low‐dose morphine to intrathecal bupivacaine/sufentanil labour analgesia: a randomised controlled study. International Journal of Obstetric Anesthesia 2010;19(4):384‐9. [DOI] [PubMed] [Google Scholar]
Hendriks 2009 {published data only}
- Hendriks MP, Weert CJM, Snoeck MMJ, Hu HP, Pluim MAL, Gielen MJM. Plain articaine or prilocaine for spinal anaesthesia in day‐case knee arthroscopy: a double‐blind randomized trial. British Journal of Anaesthesia 2009;102(2):259‐63. [DOI] [PubMed] [Google Scholar]
Ilioff 1990 {published data only}
- Ilioff G, Strelec SR, Rothfus W, Teeple E. Does prophylactic intramuscular caffeine sodium benzoate decrease incidence of post dural puncture headache. Regional Anesthesia 1990;15(1S):65. [Google Scholar]
Imbelloni 2003 {published data only}
- Imbelloni LE, Vieira EM, Rocha A, Gouveia MA, Cordeiro JA. Spinal anesthesia for cesarean section with 0.5% isobaric bupivacaine plus fentanyl and morphine. Prospective study with different volumes. Revista Brasileira de Anestesiologia 2003;53(3):322‐30. [PubMed] [Google Scholar]
Imbelloni 2009 {published data only}
- Imbelloni LE, Gouveia MA, Vieira EM, Cordeiro JA. A randomised, double‐blind comparison of three different volumes of hypobaric intrathecal bupivacaine for orthopaedic surgery. Anaesthesia and Intensive Care 2009;37(2):242‐7. [DOI] [PubMed] [Google Scholar]
Imbelloni 2010 {published data only}
- Imbelloni LE, Gouveia MA, Cordeiro JA. Hypobaric 0.15% bupivacaine versus hypobaric 0.6% lidocaine for posterior spinal anesthesia in outpatient anorectal surgery. Revista Brasileira de Anestesiologia 2010;60(2):113‐20. [DOI] [PubMed] [Google Scholar]
Jacobsohn 2005 {published data only}
- Jacobsohn E, Lee TWR, Amadeo RJ, Syslak PH, Debrouwere RG, Bell D, et al. Low‐dose intrathecal morphine does not delay early extubation after cardiac surgery. Canadian Journal of Anesthesia 2005;52(8):848‐57. [DOI] [PubMed] [Google Scholar]
Kallio 2004 {published data only}
- Kallio H, Snall EVT, Kero MP, Rosenberg PH. A comparison of intrathecal plain solutions containing ropivacaine 20 or 15 mg versus bupivacaine 10 mg. Anesthesia and Analgesia 2004;99(3):713‐7. [DOI] [PubMed] [Google Scholar]
Kallio 2005 {published data only}
- Kallio H, Snall EVT, Suvanto SJ, Tuomas CA, Iivonen MK, Pokki JP, et al. Spinal hyperbaric ropivacaine‐fentanyl for day‐surgery. Regional Anesthesia and Pain Medicine 2005;30(1):48‐54. [DOI] [PubMed] [Google Scholar]
Kaukinen 1981 {published data only}
- Kaukinen S, Kaukinen L, Kannisto K, Kataja M. The prevention of headache following spinal anaesthesia. Annales Chirurgiae et Gynaecologiae 1981;70(3):107‐11. [PubMed] [Google Scholar]
Kouri 2004 {published data only}
- Kouri ME, Kopacz DJ. Spinal 2‐chloroprocaine: a comparison with lidocaine in volunteers. Anesthesia and Analgesia 2004;98(1):75‐80. [DOI] [PubMed] [Google Scholar]
Lanz 1982 {published data only}
- Lanz, E, Theiss D, Riess W, Sommer U. Epidural morphine for postoperative analgesia: a double‐blind study. Anesthesia and Analgesia 1982;61(3):236‐40. [PubMed] [Google Scholar]
Lauretti 1999 {published data only}
- Lauretti GR, Oliveira R, Reis MP, Mattos AL, Pereira NL. Transdermal nitroglycerine enhances spinal sufentanil postoperative analgesia following orthopedic surgery. Anesthesiology 1999;90(3):734‐9. [DOI] [PubMed] [Google Scholar]
Lauretti 1999b {published data only}
- Lauretti GR, Oliveira R, Julião MCC, Reis MP, Paccola CAJ. Postoperative analgesia by intra‐articular and epidural neostigmine following knee surgery. Regional Anesthesia and Pain Medicine 1999;24(3):17. [Google Scholar]
Lauretti 2000 {published data only}
- Lauretti GR, Oliveira R, Perez MV, Paccola CAJ. Postoperative analgesia by intraarticular and epidural neostigmine following knee surgery. Journal of Clinical Anesthesia 2000;12(6):444‐8. [DOI] [PubMed] [Google Scholar]
Lauretti 2000b {published data only}
- Lauretti GR, Oliveira AP, Julião MC, Reis MP, Pereira NL. Transdermal nitroglycerine enhances spinal neostigmine postoperative analgesia following gynecological surgery. Anesthesiology 2000;93(4):943‐6. [DOI] [PubMed] [Google Scholar]
Lee 2005 {published data only}
- Lee YY, Ngan Kee WD, Muchhal K, Chan CK. Randomized double‐blind comparison of ropivacaine‐fentanyl and bupivacaine‐fentanyl for spinal anaesthesia for urological surgery. Acta Anaesthesiologica Scandinavica 2005;49(10):1477‐82. [DOI] [PubMed] [Google Scholar]
Lewis 1992 {published data only}
- Lewis RP, Spiers SP, McLaren IM, Hunt PC, Smith HS. Pethidine as a spinal anaesthetic agent ‐ a comparison with plain bupivacaine in patients undergoing transurethral resection of the prostate. European Journal of Anaesthesiology 1992;9(2):105‐9. [PubMed] [Google Scholar]
Lierz 2004 {published data only}
- Lierz P, Gustorff B, Markow G, Felleiter P. Comparison between bupivacaine 0.125% and ropivacaine 0.2% for epidural administration to outpatients with chronic low back pain. European Journal of Anaesthesiology 2004;21:32‐7. [DOI] [PubMed] [Google Scholar]
López‐Soriano 2002 {published data only}
- López‐Soriano F, Lajarín B, Rivas F, Verdú JM, López‐Robles J. Hyperbaric subarachnoid ropivacaine in ambulatory surgery: comparative study with hyperbaric bupivacaine. Revista Española de Anestesiología y Reanimación 2002;49:71‐5. [PubMed] [Google Scholar]
Luck 2008 {published data only}
- Luck JF, Fettes PDW, Wildsmith JAW. Spinal anaesthesia for elective surgery: a comparison of hyperbaric solutions of racemic bupivacaine, levobupivacaine, and ropivacaine. British Journal of Anaesthesia 2008;101(5):705‐10. [DOI] [PubMed] [Google Scholar]
Manaa 2005 {published data only}
- Manaa EM, El‐Faroug O. Comparative study between intrathecal low‐dose bupivacaine versus lidocaine for anorectal surgery. Egyptian Journal of Anaesthesia 2005;21:75‐8. [Google Scholar]
Martlew 2009 {published data only}
- Martlew RA. Spinal opioids and the prevention of postdural puncture headache. Anaesthesia 2009;64:97. [DOI] [PubMed] [Google Scholar]
Massou 2008 {published data only}
- Massou S, Drissi M, Hatim G, Ibat D, Drissi Kamili N, Atmani M. Does propofol have effect on postdural puncture headache?. Annales Francaises d Anesthesie et de Reanimation 2008;27(10):861‐2. [DOI] [PubMed] [Google Scholar]
Meininger 2003 {published data only}
- Meininger D, Byhahn C, Kessler P, Nordmeyer J, Alparslan Y, Hall BA, et al. Intrathecal fentanyl, sufentanil, or placebo combined with hyperbaric mepivacaine 2% for parturients undergoing elective cesarean delivery. Anesthesia and Analgesia 2003;96:852–8. [DOI] [PubMed] [Google Scholar]
Michalek‐Sauberer 2008 {published data only}
- Michalek‐Sauberer A, Kozek‐Langenecker SA, Heinzl H, Deusch E, Chiari A. Median effective local anesthetic doses of plain bupivacaine and ropivacaine for spinal anesthesia administered via a spinal catheter for brachytherapy of the lower abdomen. Regional Anesthesia and Pain Medicine 2008;33(1):4‐9. [DOI] [PubMed] [Google Scholar]
Morrison 1994 {published data only}
- Morrison LM, Emanuelsson BM, McClure JH, Pollok AJ, McKeown DW, Brockway M, et al. Efficacy and kinetics of extradural ropivacaine: comparison with bupivacaine. British Journal of Anaesthesia 1994;72(2):164‐9. [DOI] [PubMed] [Google Scholar]
Mosavy 1975 {published data only}
- Mosavy SH, Shafei M. Prevention of headache consequent upon dural puncture in obstetric patient. Anaesthesia 1975;30(6):807‐9. [DOI] [PubMed] [Google Scholar]
Murto 1999 {published data only}
- Murto K, Lui ACP, Cicutti N. Adding low dose meperidine to spinal lidocaine prolongs postoperative analgesia. Canadian Journal of Anaesthesia 1999;46(4):327‐34. [DOI] [PubMed] [Google Scholar]
Møller 1984 {published data only}
- Møller IW, Fernandes A, Edström HH. Subarachnoid anaesthesia with 0.5% bupivacaine: effects of density. British Journal of Anaesthesia 1984;56(11):1191‐5. [DOI] [PubMed] [Google Scholar]
Neilson 2008 {published data only}
- Neilson G, Lennox P, Vaghadia H. Selective spinal anesthesia: a comparison of 2‐chloroprocaine with lidocaine for ambulatory TUPR surgery. Canadian Journal of Anaesthesia 2008;55(S1):4752021‐2. [Google Scholar]
Ogun 2003 {published data only}
- Ogun CO, Kirgiz EN, Duman A, Okesli S, Akyurek C. Comparison of intrathecal isobaric bupivacaine‐morphine and ropivacaine‐morphine for Caesarean delivery. British Journal of Anaesthesia 2003;90(5):659‐64. [DOI] [PubMed] [Google Scholar]
Paech 1993 {published data only}
- Paech MJ. The influence of adrenaline on postoperative analgesia after subarachnoid morphine. Anaesthesia and Intensive Care 1993;21(1):79‐84. [DOI] [PubMed] [Google Scholar]
Palahniuk 1979 {published data only}
- Palahniuk R, Cumming M. Prophylactic blood patch does not prevent post lumbar puncture headache. Canadian Journal of Anesthesia 1979;26(2):132‐3. [DOI] [PubMed] [Google Scholar]
Pan 2001 {published data only}
- Pan PH, Moore CH. Comparing the efficacy of prophylactic metoclopramide, ondansetron, and placebo in cesarean section patients given epidural anesthesia. Journal of Clinical Anesthesia 2001;13(6):430‐5. [DOI] [PubMed] [Google Scholar]
Patra 2005 {published data only}
- Patra P, Kapoor MC, Nair TGM. Spinal anaesthesia with low dose bupivacaine and fentanyl for endoscopic urological surgeries. Journal of Anaesthesiology Clinical Pharmacology 2005;21(2):147‐54. [Google Scholar]
Phero 1987 {published data only}
- Phero JC, Bridenbaugh PO, Edström HH, Hagenouw RR, Knarr D, Mukkada TA, et al. Hypotension in spinal anesthesia: a comparison of isobaric tetracaine with epinephrine and isobaric bupivacaine without epinephrine. Anesthesia and Analgesia 1987;66(6):549‐52. [PubMed] [Google Scholar]
Plaja 2000 {published data only}
- Plaja I, Arxer A, Metje M, Santiveri X, Villalonga A, Fernandez MA, et al. Comparison of 5% prilocaine and 2% mepivacaine in spinal anesthesia for transurethral resection. Revista Espanola de Anestesiologia y Reanimacion 2000;47(5):194‐7. [PubMed] [Google Scholar]
Prusinski 1974 {published data only}
- Prusinski A, Klimek A. Sandomigran in the prevention of headaches following lumbar puncture. Neurologia i Neurochirurgia Polska 1974;8(4):565‐8. [PubMed] [Google Scholar]
Radpay 2003 {published data only}
- Radpay B, Karimi‐Zandi S, Dabir S, Parsa T. Comparison between epidural morphine versus morphine + fentanyl in lung resection surgery. Archives of Iranian Medicine 2003;6(2):81‐5. [Google Scholar]
Reinhart 1985 {published data only}
- Reinhart K, Dallinger‐Stiller G, Dennhardt R, Heinemeyer G, Eyrich K. Comparison of midazolam, diazepam and placebo i.m. as premedication for regional anaesthesia. A randomized double‐blind study. British Journal of Anaesthesiology 1985;57(3):294‐9. [DOI] [PubMed] [Google Scholar]
Rivera‐Ordonez 2005 {published data only}
- Rivera‐Ordonez A, Rivera‐Flores J. Postoperative epidural analgesia: ketamine plus bupivacaine vs bupivacaine alone in hip and femur surgery. Revista Mexicana de Anestesiologia 2005;28(1):14‐9. [Google Scholar]
Roux 1983 {published data only}
- Roux FX, Mallet A, Meresse S. Prevention of cephalalgia following rachiocentesis. A controlled double blind trial of intravenous tiapride. Semaine des Hopitaux 1983;59(5):319‐21. [PubMed] [Google Scholar]
Rucci 1985 {published data only}
- Rucci FS, Cardamone M, Migliori P. Fentanyl and bupivacaine mixtures for extradural blockade. British Journal of Anaesthesia 1985;57(3):275‐84. [DOI] [PubMed] [Google Scholar]
Ryan 1983 {published data only}
- Ryan DW, Pridie AK, Copeland PF. Plain bupivacaine 0.5%: a preliminary evaluation as a spinal anaesthetic agent. Annals of the Royal College of Surgeons of England 1983;65(1):40‐3. [PMC free article] [PubMed] [Google Scholar]
Sakaguchi 2000 {published data only}
- Sakaguchi Y, Sakura S, Shinzawa M, Saito Y. Does adrenaline improve epidural bupivacaine and fentanyl analgesia after abdominal surgery?. Anaesthesia and Intensive Care 2000;28(5):522‐6. [DOI] [PubMed] [Google Scholar]
Sangarlangkarn 1987 {published data only}
- Sangarlangkarn S, Klaewtanong V, Jonglerttrakool P, Khankaew V. Meperidine as a spinal anesthetic agent: a comparison with lidocaine‐glucose. Anesthesia and Analgesia 1987;66(3):235‐40. [PubMed] [Google Scholar]
Sanli 2005 {published data only}
- Sanli S, Yegin A, Kayacan N, Yilmaz M, Coskunfirat N, Karsli B. Effects of hyperbaric spinal ropivacaine for caesarean section: with or without fentanyl. European Journal of Anaesthesiology 2005;22(6):457‐61. [DOI] [PubMed] [Google Scholar]
Santos 1986 {published data only}
- Santos DJ, Barett T, Lachica R, Coyle D. Efficacy of epidural saline patch in preventing post‐dural puncture headache. Regional Anesthesia 1986;11(1):42‐3. [Google Scholar]
Sawhney 2004 {published data only}
- Sawhney S, Gupta RC, Shukla RN, Chakravorty S, Kulkarni SN. Post‐operative analgesia with epidural ketamine and morphine. Journal of Anaesthesiology Clinical Pharmacology 2004;20(4):401‐5. [Google Scholar]
Sengupta 1989 {published data only}
- Sengupta P, Bagley G, Lim M. Prevention of postdural puncture headache after spinal anaesthesia for extracorporeal shockwave lithotripsy. An assessment of prophylactic epidural blood patching. Anaesthesia 1989;44(1):54‐6. [DOI] [PubMed] [Google Scholar]
Seyhan 2005 {published data only}
- Seyhan TO, Baskan I, Karadeniz M, Senturk M. Epidural saline infusion for prophylaxis of postdural puncture headache a preliminary report. Regional Anesthesia and Pain Medicine 2005;30(5S1):75. [Google Scholar]
Shah 2003 {published data only}
- Shah FR, Halbe AR, Panchal ID, Goodchild CS. Improvement in postoperative pain relief by the addition of midazolam to an intrathecal injection of buprenorphine and bupivacaine. European Journal of Anaesthesiology 2003;20(11):904‐10. [DOI] [PubMed] [Google Scholar]
Singh 2006 {published data only}
- Singh V, Gupta LK, Singh GP. Comparison among intrathecal fentanyl and butorphanol in combination with bupivacaine for lower limb surgeries. Journal of Anaesthesiology Clinical Pharmacology 2006;22(4):371‐5. [Google Scholar]
Smith 2004 {published data only}
- Smith KN, Kopacz DJ, McDonald SB. Spinal 2 ‐ chloroprocaine: a dose‐ranging study and the effect of added epinephrine. Anesthesia and Analgesia 2004;98(1):81‐8. [DOI] [PubMed] [Google Scholar]
Soni 2001 {published data only}
- Soni AK, Miller CG, Pratt SD, Hess PE, Oriol NE, Sarna MC. Low dose intrathecal ropivacaine with or without sufentanil provides effective analgesia and does not impair motor strength during labour: a pilot study. Canadian Journal of Anaesthesia 2001;48(7):677‐80. [DOI] [PubMed] [Google Scholar]
Sudarshan 1995 {published data only}
- Sudarshan G, Browne BL, Matthews JNS, Conacher ID. Intrathecal fentanyl for post‐thoracotomy pain. British Journal of Anaesthesia 1995;75(1):19‐22. [DOI] [PubMed] [Google Scholar]
Tekin 2007 {published data only}
- Tekin M, Kati I, Tomak Y, Kisli E. Effect of dexmedetomidine IV on the duration of spinal anesthesia with prilocaine: a double‐blind, prospective study in adult surgical patients. Current Therapeutic Research ‐ Clinical and Experimental 2007;68(5):313‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2006 {published data only}
- Thomas S, Beevi S. Epidural dexamethasone reduces postoperative pain and analgesic requirements. Canadian Journal of Anesthesia 2006;53(9):899‐905. [DOI] [PubMed] [Google Scholar]
Trivedi 1993 {published data only}
- Trivedi NS, Eddi D, Shevde, K. Headache prevention following accidental dural puncture in obstetric patients. Journal of Clinical Anesthesia 1993;5(1):42‐5. [DOI] [PubMed] [Google Scholar]
Tsen 2001 {published data only}
- Tsen LC, Schultz R, Martin R, Datta S, Bader AM. Intrathecal low‐dose bupivacaine versus lidocaine for in vitro fertilization procedures. Regional Anesthesia and Pain Medicine 2001;26(1):52‐6. [DOI] [PubMed] [Google Scholar]
Tucker 2004 {published data only}
- Tucker AP, Mezzatesta J, Nadeson R, Goodchild CS. Intrathecal midazolam II: combination with intrathecal fentanyl for labor pain. Anesthesia and Analgesia 2004;98(6):1521‐7. [DOI] [PubMed] [Google Scholar]
Tuncer 2005 {published data only}
- Tuncer S, Bariskaner H, Reisli R, Sarkilar G, Cicekci F, Otelcioglu S. Effect of gabapentin on postoperative pain: a randomized, placebo‐controlled clinical study. The Pain Clinic 2005;17(1):95‐9. [Google Scholar]
Turan 2006 {published data only}
- Turan A, Kaya G, Karamanlioglu B, Pamukcu Z, Apfel CC. Effect of oral gabapentin on postoperative epidural analgesia. British Journal of Anaesthesia 2006;96(2):242‐6. [DOI] [PubMed] [Google Scholar]
Turker 2003 {published data only}
- Turker G, Uckunkaya N, Yilmazlar A, Demirag B, Tokat O. Effects of adding epinephrine plus fentanyl to low‐dose lidocaine for spinal anesthesia in outpatient knee arthroscopy. Acta Anaesthesiologica Scandinavica 2003;47(8):986‐92. [DOI] [PubMed] [Google Scholar]
Unlugenc 2006 {published data only}
- Unlugenc H, Ozalevli M, Gunes Y, Olguner S, Evruke C, Ozcengiz D, et al. A double‐blind comparison of intrathecal S(+) ketamine and fentanyl combined with bupivacaine 0.5% for Caesarean delivery. European Journal of Anaesthesiology 2006;23(12):1018‐24. [DOI] [PubMed] [Google Scholar]
Unlugenc 2009 {published data only}
- Unlugenc H, Ozalevli M, Gunduz M, Gunasti S, Urunsak I F, Guler T, et al. Comparison of intrathecal magnesium, fentanyl, or placebo combined with bupivacaine 0.5% for parturients undergoing elective cesarean delivery. Acta Anaesthesiologica Scandinavica 2009;53(3):346‐53. [DOI] [PubMed] [Google Scholar]
Usubiaga 1967 {published data only}
- Usubiaga JE, Usubiaga LE, Brea LM, Goyena R. Effect of saline injections on epidural and subarachnoid space pressures and relation to postspinal anesthesia headache. Anesthesia and Analgesia 1967;46(3):293‐6. [PubMed] [Google Scholar]
Vaghadia 1997 {published data only}
- Vaghadia H, McLeod DH, Mitchell GW, Merrick PM, Chilvers CR. Small‐dose hypobaric lidocaine‐fentanyl spinal anesthesia for short duration outpatient laparoscopy. I. A randomized comparison with conventional dose hyperbaric lidocaine. Anesthesia and Analgesia 1997;84(1):59‐64. [DOI] [PubMed] [Google Scholar]
Vale 1995 {published data only}
- Vale NB, Silva Neto JD, Magalhães Filho EB, Nascimento W, Pereira F, França A. Spinal anesthesia with 0.5% bupivacaine and 2% lidocaine without glucose in a fixed dose ‐ efficacy/toxicity in the morning and in the afternoon. Revista Brasileira De Anestesiologia 1995;45(5):301‐7. [Google Scholar]
Vichitvejpaisal 1992 {published data only}
- Vichitvejpaisal P, Svastdi‐Xuto O, Udompunturux S. A comparative study of isobaric and hyperbaric solution of bupivacaine for spinal anaesthesia in caesarean section. Journal of the Medical Association of Thailand 1992;75(5):278‐82. [PubMed] [Google Scholar]
Viscusi 2005 {published data only}
- Viscusi ER, Martin G, Hartrick CT, Singla N, Manvelian G. Forty‐eight hours of postoperative pain relief after total hip arthroplasty with a novel, extended‐release epidural morphine formulation. Anesthesiology 2005;102(5):1014‐22. [DOI] [PubMed] [Google Scholar]
Waxler 2004 {published data only}
- Waxler B, Mondragon SA, Patel SN, Nedumgottil K. Intrathecal lidocaine and sufentanil shorten post‐operative recovery after outpatient rectal surgery. Canadian Journal of Anesthesia 2004;51(7):680‐4. [DOI] [PubMed] [Google Scholar]
Wells 2004 {published data only}
- Wells J, Paech MJ, Evans SF. Intrathecal fentanyl‐induced pruritus during labour: the effect of prophylactic ondansetron. International Journal of Obstetric Anesthesia 2004;13(1):35‐9. [DOI] [PubMed] [Google Scholar]
Whiteside 2003 {published data only}
- Whiteside JB, Burke D, Wildsmith JAW. Comparison of ropivacaine 0.5% (in glucose 5%) with bupivacaine 0.5% (in glucose 8%) for spinal anaesthesia for elective surgery. British Journal of Anaesthesia 2003;90(3):304‐8. [DOI] [PubMed] [Google Scholar]
Widerlöv 1979 {published data only}
- Widerlöv E, Lindström L. D.D.A.V.P. and headache after lumbar puncture. Lancet 1979;1(8115):548. [DOI] [PubMed] [Google Scholar]
Wilder‐Smith 1998 {published data only}
- Wilder‐Smith CH, Wilder‐Smith OHG, Farschtschian M, Naji P. Preoperative adjuvant epidural tramadol: the effect of different doses on postoperative analgesia and pain processing. Acta Anaesthesiologica Scandinavica 1998;42(3):299‐305. [DOI] [PubMed] [Google Scholar]
Wood 1993 {published data only}
- Wood MB, Rubin AP. A comparison of epidural 1% ropivacaine and 0.75% bupivacaine for lower abdominal gynecologic surgery. Anesthesia and Analgesia 1993;76(6):1274‐8. [DOI] [PubMed] [Google Scholar]
Yanagidate 2004 {published data only}
- Yanagidate F, Dohi S. Epidural oxycodone or morphine following gynaecological surgery. British Journal of Anaesthesia 2004;93(3):362‐7. [DOI] [PubMed] [Google Scholar]
Yeh 2000 {published data only}
- Yeh HM, Chen LK, Lin CJ, Chan WH, Chen YP, Lin CS, et al. Prophylactic intravenous ondansetron reduces the incidence of intrathecal morphine‐induced pruritus in patients undergoing cesarean delivery. Anesthesia and Analgesia 2000;91(1):172‐5. [DOI] [PubMed] [Google Scholar]
Yücel 1999 {published data only}
- Yücel A, Ozyalçin S, Talu GK, Yücel EC, Erdine S. Intravenous administration of caffeine sodium benzoate for postdural puncture headache. Regional Anesthesia and Pain Medicine 1999;24(1):51‐4. [PubMed] [Google Scholar]
Zackova 2000 {published data only}
- Zackova M, Manfredini P, Strali W, Baravelli A, Furnari G, Accorsi A. Comparison of 0.125% bupivacaine and 0.2% ropivacaine in obstetric analgesia. Minerva Anestesiologica 2000;66(9):643‐8. [PubMed] [Google Scholar]
Additional references
Ahmed 2006
- Ahmed SV, Jayawarna C, Jude E. Post lumbar puncture headache: diagnosis and management. Postgraduate Medicine 2006;82(973):713–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Angle 2005
- Angle P, Tang SL, Thompson D, Szalai JP. Expectant management of postdural puncture headache increases hospital length of stay and emergency room visits. Canadian Journal of Anaesthesia 2005;52(4):397–402. [DOI] [PubMed] [Google Scholar]
Apfel 2010
- Apfel CC, Saxena A, Cakmakkaya OS, Gaiser R, George E, Radke O. Prevention of postdural puncture headache after accidental dural puncture: a quantitative systematic review. British Journal of Anaesthesia 2010;105(3):255‐63. [DOI] [PubMed] [Google Scholar]
Arevalo‐Rodriguez 2011
- Arevalo‐Rodriguez I, Ciapponi A, Munoz L, Roqué i Figuls M, Bonfill Cosp X. Posture and fluids for preventing post‐dural puncture headache. Cochrane Database of Systematic Reviews 2011, Issue 7. [DOI: 10.1002/14651858.CD009199] [DOI] [Google Scholar]
Banks 2001
- Banks S, Paech M, Gurrin L. An audit of epidural blood patch after accidental dural puncture with a Tuohy needle in obstetric patients. International Journal of Obstetric Anesthesia 2001;10(3):172‐6. [DOI] [PubMed] [Google Scholar]
Basurto 2011
- Basurto Ona X, Martínez García L, Solà I, Bonfill Cosp X. Drug therapy for treating post‐dural puncture headache. Cochrane Database of Systematic Reviews 2011, Issue 8. [DOI: 10.1002/14651858.CD007887.pub2] [DOI] [PubMed] [Google Scholar]
Baumgarten 1987
- Baumgarten RK. Should caffeine become the first‐line treatment for postdural puncture headache?. Anesthesia and Analgesia 1987;66(9):913–4. [PubMed] [Google Scholar]
Berger 1998
- Berger CW, Crosby ET, Grodecki W. North American survey of the management of dural puncture occurring during labour epidural analgesia. Canadian Journal of Anesthesia 1998;45(2):110‐4. [DOI] [PubMed] [Google Scholar]
Bezov 2010
- Bezov D, Ashina S, Lipton R. Post‐dural puncture headache: part II ‐ prevention, management, and prognosis. Headache 2010;50(9):1482‐98. [DOI] [PubMed] [Google Scholar]
Boonmak 2010
- Boonmak P, Boonmak S. Epidural blood patching for preventing and treating post‐dural puncture headache. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD001791.pub2] [DOI] [PubMed] [Google Scholar]
Choi 2003
- Choi PT, Galinski SE, Takeuchi L, Lucas S, Tamayo C, Jadad AR. PDPH is a common complication of neuraxial blockade in parturients: a meta‐analysis of obstetrical studies. Canadian Journal of Anaesthesia 2003;50(5):460‐9. [DOI] [PubMed] [Google Scholar]
Clark 1996
- Clark JW, Solomon GD, Senanayake PD, Gallagher C. Substance P concentration and history of headache in relation to postlumbar puncture headache: towards prevention. Journal of Neurology, Neurosurgery and Psychiatry 1996;60(6):681–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Davignon 2002
- Davignon KR, Dennehy K. Update on postdural puncture headache. International Anesthesiology Clinics 2002;40(4):89–102. [DOI] [PubMed] [Google Scholar]
Denny 1987
- Denny N, Masters R, Pearson D, Read J, Sihota M, Selander D. Postdural puncture headache after continuous spinal anesthesia. Anesthesia and Analgesia 1987;66(8):791–4. [PubMed] [Google Scholar]
Grande 2005
- Grande PO. Mechanisms behind postspinal headache and brain stem compression following lumbar dural puncture ‐ a physiological approach. Acta Anaesthesiologica Scandinavica 2005;49(5):619–26. [DOI] [PubMed] [Google Scholar]
Hafer 1997
- Hafer J, Rupp D, Wollbrück M, Engel J, Hempelmann G. The effect of needle type and immobilization on postspinal headache. Anaesthetist 1997;46(10):860‐6. [DOI] [PubMed] [Google Scholar]
Harrington 2004
- Harrington BE. Postdural puncture headache and the development of the epidural blood patch. Regional Anesthesia and Pain Medicine 2004;29(2):136–63. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta‐analysis. Statistics in Medicine 2002;21:1539‐58. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. Available from www.cochrane‐handbook.org..
International Headache Society 2004
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia 2004;24(Suppl 1):9–160. [DOI] [PubMed] [Google Scholar]
Kuczkowski 2006
- Kuczkowski KM. The treatment and prevention of post‐dural puncture headache. Acta Anaesthesiologica Belgica 2006;57(1):55–6. [PubMed] [Google Scholar]
Lavi 2006
- Lavi R, Yarnitsky D, Rowe JM, Weissman A, Segal D, Avivi I. Standard vs atraumatic Whitacre needle for diagnostic lumbar puncture: a randomized trial. Neurology 2006;67(8):1492–4. [DOI] [PubMed] [Google Scholar]
Lybecker 1995
- Lybecker H, Djernes M, Schmidt JF. Postdural puncture headache (PDPH): onset, duration, severity, and associated symptoms. An analysis of 75 consecutive patients with PDPH. Acta Anaesthesiologica Scandinavica 1995;39(5):605‐12. [DOI] [PubMed] [Google Scholar]
McQuay 1998
- McQuay HJ, Moore RA. An Evidence‐Based Resource for Pain Relief. Oxford: Oxford University Press, 1998. [Google Scholar]
Morewood 1993
- Morewood GH. A rational approach to the cause, prevention and treatment of postdural puncture headache. Canadian Medical Association Journal 1993;149(8):1087‐93. [PUBMED: 8221447] [PMC free article] [PubMed] [Google Scholar]
Newman 2010
- Newman MJ, Cyna AM, Middleton P. Epidural catheter replacement and intrathecal catheter techniques for preventing post‐dural puncture headache following an inadvertent dural puncture in labour. Cochrane Database of Systematic Reviews 2010, Issue 1. [DOI: 10.1002/14651858.CD008266] [DOI] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Schulz 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Annals of Internal Medicine 2010;152:726–32. [DOI] [PubMed] [Google Scholar]
Thew 2008
- Thew M, Paech MJ. Management of postdural puncture headache in the obstetric patient. Current Opinion in Anesthesiology 2008;21(3):288–92. [DOI] [PubMed] [Google Scholar]
Turnbull 2003
- Turnbull DK, Shepherd DB. Post‐dural puncture headache: pathogenesis, prevention and treatment. British Journal of Anaesthesia 2003;91(5):718‐29. [DOI: 10.1093/bja/aeg231] [DOI] [PubMed] [Google Scholar]
Vallejo 2000
- Vallejo MC, Mandell GL, Sabo DP, Ramanathan S. Postdural puncture headache: a randomized comparison of five spinal needles in obstetric patients. Anesthesia and Analgesia 2000;91(4):916‐20. [DOI] [PubMed] [Google Scholar]
Verma 2011
- Verma R, Alladi R, Jackson I, Johnston I, Kumar C, Page R, et al. Day case and short stay surgery: 2. Anaesthesia 2011;66(5):417‐34. [DOI] [PubMed] [Google Scholar]


