June 21, 2021
ABSTRACT | Understanding the social determinants of health (SDoH), social risk factors, and health-related social needs (HRSN) is critical to creating equitable health and care for all patients and communities. Health care systems need to understand their role in enacting relevant strategies, processes, and policies. One way that health care systems can explore what processes and policies work for their patients and their community is using the Plan-Do-Study-Act (PDSA) model. This discussion paper provides frameworks and approaches to using PDSA cycles to implement SDoH, social risk factors, and HRSN efforts, as a follow-up to the 2017 NAM Perspectives discussion paper Social Determinants of Health 101 for Health Care: Five Plus Five [1].
Introduction
When Social Determinants of Health 101 for Health Care: Five Plus Five [1] (SDoH 101) was published in 2017, the social determinants of health (SDoH) were emerging as an important topic in health care. Since that time, our nation has experienced the COVID-19 pandemic and its disparate impact on people of color, which has illuminated persistent health inequities and heightened the sense of urgency to reduce these disparities. To make progress towards a more just and equitable society, it is critical to address patients’ social risk factors and needs—especially in populations with disadvantages due to systemic racism or lower socioeconomic status—as well as the contextual conditions that underlie those needs.
SDoH 101 discusses five things known and five things to be learned about SDoH in health care (see Box 1); for instance, it is now known that medical care alone is insufficient to ensure better health and well-being for all Americans. This discussion paper builds on SDoH 101 and explores in more depth the five things to be learned, including the science and prioritization of interventions, the creation of partnerships, and how the assets of the community can further these partnerships. It provides several frameworks for integrating approaches to SDoH, social risk factors, and HRSN in health care, and proposes Plan-Do-Study-Act (PDSA) cycles as a quality improvement (QI) approach for health care systems.
Most of the topics outlined in SDoH 101 remain relevant in 2021, but the field has evolved to more clearly differentiate SDoH from social risk factors and HRSN. At the same time, the evidence base related to the outcomes of addressing these factors in health care is still nascent [2,36]. Given the state of the science, how can a health system responsibly use its resources to explore and fulfill its roles in addressing SDoH, social risk factors, and HRSN?
The Plan-Do-Study-Act (PDSA) cycles used by many health care systems in QI programs [52], and by research initiatives such in ASCEND (ApproacheS to Community Health Center ImplEmeNtation of Social Determinants of Health Data Collection and Action) [53], offer a helpful tool for organizations to build on current systems thinking and incorporate new aspects that are needed to address community SDoH as well as individual social risk factors and HRSN. PDSA cycles are discussed in more detail later in this paper, with additional information in Appendix A.
In employing a PDSA approach, three questions are being asked [113]:
-
1.
What are we trying to accomplish?
-
2.
How will we know that a change is an improvement?
-
3.
What changes can we make that will result in an improvement?
This paper will discuss several steps in the proposed PDSA approach, including:
Preparing to implement PDSA
-
1.
Engaging leadership
-
2.
Understanding definitions and authentic community engagement
-
3.
Selecting a framework for addressing SDoH, social risk factors, and HRSN
-
4.
Considering multiple issues when deciding about screening for social risk factors or HRSN
Employing PDSA
-
1.
Plan: Reviewing data, designing interventions, and determining how success will be measured
-
2.
Do: Implementing interventions—both at clinical and community levels—to address social risk factors or HRSN and the underlying SDoH
-
3.
Study: Studying and evaluating the results
-
4.
Act: Reflecting on the learnings with community partners before taking next steps
Preparing to Implement PDSA
When preparing to implement PDSA for community and individual approaches to address SDoH, social risk factors, and HRSN, there are several steps that will increase the likelihood of success. First, leadership involvement will help prioritize the work within the organization and can assist with removing any obstacles. Second, clarity on language and involvement of community partners from the beginning will lay a firm foundation. Third, selecting a framework for the SDoH, social risk factors, and HRSN will assist in describing and connecting the work. Finally, deciding about the role of screening for social risk factors and HRSN will set the stage for next steps in PDSA.
Engaging Leadership
When applying PDSA to SDoH, social risk factors, and HRSN, a health care system must first identify who in leadership is interested and will champion the cause, and how leaders will incorporate the organization’s connection with community health needs assessments and community benefit programs to support the PDSA cycle(s). Leaders must identify how the organization is involved with community and social partners through committees or action groups. They should ask if the organization wants to address upstream SDoH and social risk factors or HRSN identified in the clinical setting. Potential frameworks to guide this work are presented later in this discussion paper.
Box 1. Excerpts from Social Determinants of Health 101 for Health Care: Five Plus Five.
Five Things We Know about Social Determinants of Health
-
1.
As a determinant of health, medical care is insufficient for ensuring better health outcomes.
-
2.
SDoH are influenced by policies and programs and associated with better outcomes.
-
3.
New payment models are prompting interest in SDoH.
-
4.
Frameworks for integrating SDoH are emerging.
-
5.
Experiments are occurring at the local and federal levels.
Five Things to be Learned about Social Determinants of Health
-
1.
How do we prioritize SDoH for individual patients and for communities?
-
2.
How do we intervene without medicalizing SDoH?
-
3.
What (new) data are needed?
-
4.
How do we build multi-sector partnerships?
-
5.
What else, e.g., how can we focus on assets?
SOURCE: Magnan, S. 2017. Social Determinants of Health 101 for Health Care: Five Plus Five. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201710c
Leaders should also decide what new or existing structure(s) will explore and guide the PDSA cycles. They should emphasize the need for expertise in community engagement, alignment with work within and outside the organization, and evaluation. Leadership may decide to have two teams—one for a PDSA on social risk and HRSN interventions at the individual clinical level and one for policy and system changes at the community level, with cross-fertilization between the two teams to synergize efforts.
Understanding Definitions of SDoH, Social Risk Factors, HRSN, and Authentic Community Engagement
Ensuring clarity about the meanings of SDoH, social risk factors, and HRSN can help health care providers better understand what they hope to accomplish in acting to address these factors. SDoH is defined by the Centers for Disease Control and Prevention as “conditions in the places where people live, learn, work, and play (which) affect a wide range of health risks and outcomes” [3]. In its definition, the World Health Organization (see Appendix D) goes beyond the diagram included in SDoH 101 to include culture, societal values, racism, social cohesion, and social capital and other determinants. Social risk factors are “specific adverse conditions associated with poor health, such as social isolation or housing instability” [4]. Health-related social needs (HRSN) is a term developed by the Centers for Medicare & Medicaid Services (CMS) for use in their Accountable Health Communities (AHC) Screening Tool. HRSN applies to five core domains—housing instability, food insecurity, transportation problems, utility help needs, and interpersonal safety—and eight supplemental domains: financial strain, employment, family and community support, education, physical activity, substance use, mental health, and disabilities [5]. HRSN screening should incorporate patients’ perspectives on their most pressing needs. In this discussion paper, HRSN refers to social needs that include patients’ preferences and priorities for connections or next steps.
Box 2. Principles of Authentic Community Engagement.
Based on CDC principles and public health accreditation, these are principles - not requirements or a checklist.
FOSTER TRUST
Immerse yourself in the community.
Listen deeply.
Recognize different kinds of groups.
Understand the historical context of previous attempts of engagement.
Notice assets.
See different experiences.
SUPPORT COMMUNITY-LED SOLUTIONS
Work with communities.
Agree on the process.
Understand each partner’s individual and community interest.
Allocate resources.
Balance power.
Share power.
Create positive experiences of contribution.
Recognize the contributions of the community.
RECOGNIZE THAT IMPROVEMENT REQUIRES SOCIAL CHANGE
Leave the community stronger.
Stay in it for the long term.
Address racism.
Remember that self-determination is a right.
Expect tension.
Address challenges.
Welcome new accountabilities and opportunities to transform practice.
Strengthen relationships among participating groups to build power for change.
SOURCE: Adapted from Minnesota Department of Health. 2018. Principles of Authentic Community Engagement. Available at: https://www.health.state.mn.us/communities/practice/resources/phqitoolbox/docs/AuthenticPrinciplesCommEng.pdf (accessed March 20, 2021).
In clinical settings, the terms SDoH, social risk factors, and HRSN are often used interchangeably for individual adverse conditions or needs, but more clearly identifying that SDoH relate to community conditions and that social risk factors and HRSN relate to individuals will help differentiate between actions targeting individuals’ risks, needs, and preferences, and policy actions to address the conditions that underlie those risks and needs [6]. This differentiation in understanding individual social risk factors and HRSN and the underlying SDoH can be portrayed as an upstream and downstream approach, as illustrated in Figure 1.
FIGURE 1. Social Determinants and Social Needs: Moving Beyond Midstream.
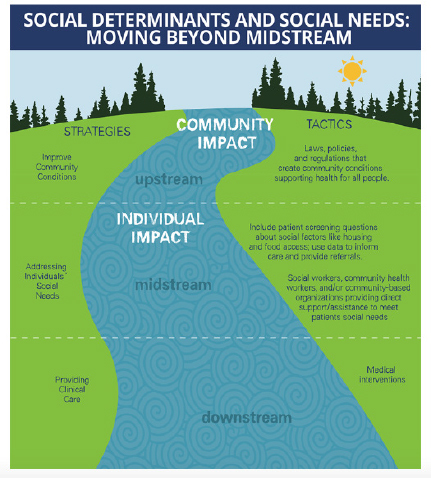
SOURCE: Castrucci, B. C. and J. Auerbach. 2019. Meeting Individual Social Needs Falls Short of Addressing Social Determinants of Health. Health Affairs Blog. Available at: https://www.healthaffairs.org/do/10.1377/hblog20190115.234942/full/ (accessed September 30, 2020). Reprinted with permission.
What is seen metaphorically downstream in clinical offices often reflects unmet social needs that stem from social risks and adverse conditions in which the patient and their family live, learn, work, pray, and play. For example, a patient may be affected by the SDoH of unaffordable neighborhood housing and a lack of livable-wage employment opportunities, which leads to the social risk of housing instability and food insecurity, which then makes chronic disease control more challenging. However, the patient may identify interpersonal safety as his or her most pressing HRSN. Ideally, a health care system is using its community benefit investments and other dollars to address upstream SDoH so that patients present with fewer downstream social risks and HRSN in clinical offices.
The stream depicted in Figure 1 is a reminder that patients live in the community that the health care system serves, and that authentic community engagement and partnership are essential to addressing SDoH, social risk factors, and HRSN. To advance authentic community engagement, the Minnesota Department of Health (MDH) suggests three guiding principles (see Box 2):
-
1.
Foster trust;
-
2.
Support community-led solutions; and
-
3.
Recognize that improvement requires social change.
Relationships between health care systems and the communities they serve must be developed over time, but health care systems must begin by listening to the community, seeing community members as partners, and working with the community to jointly create next steps. As Reverend William Barber said, “Relationships we develop with our coalition partners must be trans-formative, not transactional” [7].
Selecting a Framework for Addressing SDoH, Social Risk Factors, and HRSN
Although health care systems can begin to work anywhere in the Figure 1 stream, the greatest impact will occur with multiple strategies and tactics, especially those that utilize policy, systems, and environmental changes both inside and outside the health care system.
Although health care is delivered on an individual level, Silverstein and colleagues wrote recently: “programs that (only) address the downstream health consequences of social adversities cannot be the principal strategy” [8]. Silverstein and colleagues note that for accountable care organizations (ACOs), “The creation of financial incentives for addressing social determinants within Medicaid ACOs in particular represents an opportunity for cross-sector collaboration between health systems and other entities—such as community-based organizations or local or state government—to promote sound policy development, regulation, and advocacy” [8].
For health care, this discussion paper highlights three frameworks because they consider both community and individual approaches for the SDoH, social risk factors, and HRSN. Additional frameworks or logic models are available for exploring and evaluating outcomes of interventions [9,10].
Framework #1
The first framework, adapted from Auerbach [11], is distinguished by the “spectrum” approach—a health care system working in many different roles with partners in a community.
“The Spectrum of Health-Related Social Needs, Social Risk Factors, and Social Determinants of Health” (see Figure 2) describes approaches to addressing roles in both population health management (the patient population of a specific hospital or health system) and total population health (the health of the geographic population) [12]. Columns 1 and 2 are included in population health management; columns 3, 4 and 5 are in total population health. Auerbach argues that “working in just one box is insufficient” [13] and that health care, along with other sectors, should work to address the entire spectrum.
FIGURE 2. Framework #1: The Spectrum of Health-Related Social Needs, Social Risk Factors, and Social Determinants of Health.
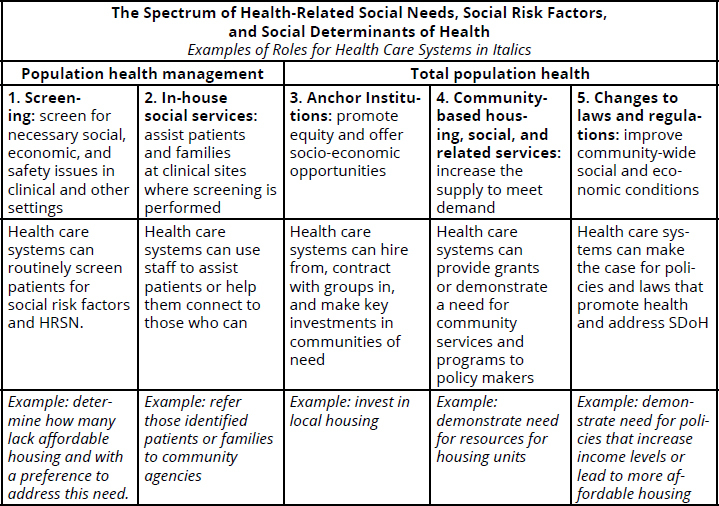
SOURCE: Adapted from Auerbach, J. 2019. Social Determinants of Health Can Only Be Addressed by a Multisector Spectrum of Activities. Journal of Public Health Management and Practice 25(6): 525-528. https://doi.org/10.1097/PHH.0000000000001088. Used with permission.
Column 3 within Figure 2 highlights the “Anchor Institution” roles for improving equity with workplace practices and policies in hiring, purchasing, and investing. Most large health care systems would be categorized as anchor institutions in their communities, and therefore can learn much from the details in column 3. For example, members of the Cleveland Greater University Circle Initiative seek to buy locally, hire locally, live locally (e.g., invest in housing), and connect (e.g., through community partnerships and engagement) [14].
Framework #2
The second framework, outlined in the 100 Million Healthier Lives Campaign’s “Pathways to Population Health” [15], employs an individual approach (i.e., “population management”) for social risk factors and HRSN, and a community approach (i.e., “community well-being creation” or population health) for SDoH [15]. This framework includes four “portfolios” or work narratives with a guiding “equity lens” at the center (see Figure 3):
FIGURE 3. Framework #2: Pathways to Population Health.
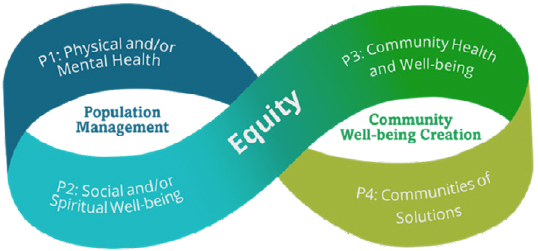
SOURCE: Institute for Healthcare Improvement. 2020. About Pathways to Population Health. Available at: http://www.ihi.org/Topics/Population-Health/Pages/Pathways-to-Population-Health.aspx (accessed September 30, 2020). Used with permission.
Population management work
P1 - Physical and/or Mental Health—e.g., create patient panels and care management, stratify for risk, integrate behavioral health, establish community partnerships
P2- Social and/or Spiritual Well-being—e.g., identify HRSN, partner with faith-based organizations for resources
Community well-being creation
P3 - Community Health and Well-being— e.g., collaboratively perform a community health needs assessment and build the systems needed for improvement
o P4 - Communities of Solutions— e.g., with others, build a long-term plan for the community (not just one project as in the portfolios above) and for health care, be an anchor institution
In addition to the pathways to population health outlined in this framework, Framework #2 provides an assessment tool (COMPASS) across eight components: Stewardship, Equity, Payment, Partnerships with People with Lived Experience, and the four Portfolios of Pathways to Population Health.
Framework #3
The third framework, presented in “Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health (Integrating Social Care),” seeks to intentionally integrate social care into a health care system’s work. It outlines five activities to strengthen how health care addresses SDoH, social risk factors, HRSN, and health disparities at the individual and community levels (see Figure 4), using transportation as an example [16]:
FIGURE 4. Framework #3: Health Care System Activities that Strengthen Social Care Integration.
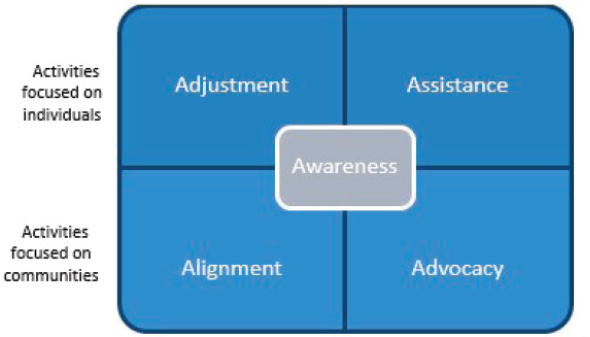
SOURCE: National Academies of Sciences, Engineering, and Medicine. 2019. Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: The National Academies Press. https://doi.org/10.17226/25467. Used with permission.
Awareness—screening: for example, for patients’ transportation needs;
Adjustment—changing care plans based on the social environment: in the transportation scenario, offering tele-health appointments whenever possible;
Assistance—providing assistance when social needs are found: for example, providing transportation vouchers;
Alignment—coordinating community resources for patients’ and families’ benefit: for example, investing in a ride-sharing program such as through a public-private partnership with the regional public transportation agency or with a private ride-share provider; and
Advocacy—advocating for policy and system changes in the community: for example, working to promote policies that expand the public transit infrastructure.
In summary, frameworks such as the three outlined above illustrate various ways in which health care systems can address SDoH, social risk factors, and HRSN in partnership with communities and patients, through both policy and system changes in the community and individual approaches with patients. (See Box 3 for two examples of community and individual approaches.)
These frameworks can be used by health care organizations and leaders to guide their thinking and actions as well as portray visually the relationships and connections of activities.
Considering Multiple Issues When Deciding about Screening for Social Risk Factors and HRSN in Clinical Settings
(Note: some literature refers to social risk factor and HRSN screening as SDoH screening)
The decision whether to screen for social risk factors or HRSN, as well as the development of clinical care work flows, is complex. Considerations include:
-
1.
Connecting the priorities and requirements of health care systems and payors;
-
2.
Understanding the perspectives of community-based organizations (CBOs);
-
3.
Selecting a tool;
-
4.
Understanding the accuracy and effectiveness of screening;
-
5.
Determining desire for assistance from patients or family members;
-
6.
Developing appropriate language; and
-
7.
Creating clinical workflows.
First, payor regulatory requirements related to screening for social risk factors or HRSN may determine a health care system’s decision. It is also important to understand the problem(s) to be solved and what the organization’s data reveal. If the organization has several locations, including across state lines, the system must decide what sites will implement screening, what populations will be screened, who will do the screening, how screening will fit into the workflow, and what will be done with the results [23]. The old adage in screening applies here—don’t screen without a plan for the results. However, some organizations will screen not just for immediate action but for a more holistic view of their patient population.
Second, health care organizations need to partner with CBOs to address social risk factors and HRSN; health and health care delivery systems should not and cannot address these factors alone. These partnerships need to develop from previous informal personal relationships, for example with grants, into formal contracts with roles and responsibilities between organizations. To respect communities and their related cultures, appropriate social sector and community resource partners should be at the table early in the process and meaningfully involved as decisions are made. When surveyed, CBOs had enthusiasm for working with health care systems, but they also said that there were competing agendas (e.g., buy vs. build) and timelines (e.g., desire for short-term outcomes vs. long-term outcomes) [24]. For example, the strict definition of homelessness that the Department of Housing and Urban Development (HUD) uses is not always consistent with the medical perspective. If medical providers refer patients whom they consider homeless but who do not meet the HUD definition, it can threaten the sustainability of the CBO.
Third, will screening be focused on one domain or multiple domains? A selected screening tool should complement current information collected on healthy behaviors, ZIP Codes, personal safety, and other domains. If an individual social risk factor tool is desired, the origins and development of the AHC tool may be a helpful place to start [25]. Recently, a social isolation risk factor screening tool has been used in three academic adult primary care clinics [26]; this has been especially relevant in the COVID-19 pandemic. Several articles and a web site (e.g., SIREN Network https://sirenetwork.ucsf.edu/tools-resources/resources/screening-tools-comparison) compare screening tools with multiple domains. In the chapter “Identifying and Addressing Patients’ Social Needs in Health Care Delivery Settings” of the Practical Playbook II, Gottlieb and Fichtenberg compare four different screening tools and their domains [27]. For practical information from a family practice perspective [28], O’Gurek and Henke discuss screening, including selection of publicly available tools and workflows. Moen and colleagues review nine tools, including a discussion of social stability. They note the interconnectedness of risk domains, especially at the upstream level. Social risks often cluster together, and multiple risks may need to be addressed at the same time to create social stability [29,30]. Although recently a poly-social risk score has been proposed, more research is needed to implement such an approach, e.g., on acquiring appropriate data sets, privacy requirements, validation, etc. [31].
A JAMA Viewpoint addresses appropriate roles for health care and clinician concerns about implementation [32]. For example, a large Kaiser Permanente study reported that the greatest barriers to implementation of universal screening are a perceived lack of time and resources to address identified issues [33]. Exploratory qualitative interviews of primary care practitioners in the San Francisco Bay area revealed that embedded processes to address unmet patient social needs “buffer” against clinician burnout [34]. Furthermore, social risk screening was acceptable to the majority of adult patients and caregivers (79%) of pediatric patients, and most (65%) supported its inclusion in the electronic medical record (EHR); this figure was even higher for patients who had received prior assistance for social needs from health care [35].
Box 3. Two Examples of Health Care Addressing a Behavioral Risk Factor and a Social Risk Factor— with Individual and Community Approaches.
The following examples illustrate how health care systems can use current and emerging evidence to address well-known behavioral health issues such as alcohol and tobacco use, as well as social risk factors such as food insecurity. Clearly, there is an interplay between such factors, but each benefit from health care systems going upstream to advocate for changes in policy and systems rather than only addressing the symptoms of the broader issues in individual patients. At the same time, downstream interventions are also critical in improving all patients’ overall health.
Example #1 – Unhealthy Substance Use
Consider how a health care provider and community members might collaborate to address alcohol and other substance use, a behavioral determinant of health and one of the AHC’s supplemental domains in its HRSN. On the clinical side, providers can screen all patients annually for unhealthy substance use by using SBIRT (screening, brief intervention, and referral to treatment) [17], which identifies people who have unhealthy substance use but do not have substance abuse disorder yet, and may benefit from brief interventions. If the provider identifies a patient with substance abuse disorder that requires additional treatment, they can refer the individual to an external specialty clinic or provider. Early and continued coordination between clinical practices and community organizations and specialty providers is critical for SBIRT to be successful [18]. For example, working with community partners, providers can assist groups supporting long-term recovery (e.g., providing space or help with virtual meetings) or support policy interventions such as alcohol pricing strategies that are part of CDC’s Health Impact in 5 Years (Hi-5) initiative [19].
Example #2 – Food Insecurity
Food insecurity is a common social risk factor and part of CMS’s HRSN screening in AHCs. An individual Hunger Vital sign screening tool [20] can be used to screen patients and families, as is done by Minnesota’s Hennepin County Medical Center in its senior and pediatric clinics. With a positive screen, patients are offered an integrated referral within the electronic medical record to a community partner food bank Second Harvest. Over 4,000 referrals occurred between January 2015 and December 2017, and Second Harvest successfully contacted 63% of the referrals and assisted 2,533 households. Staff education, training, and standardized screening were critical to success [21]. Health care systems can also refer to local agencies or community-based organizations (CBOs) that can enroll patients in evidence-based federal programs such as Supplemental Nutrition Assistance Program (SNAP) and Women, Infants, and Children (WIC) programs. Since these programs are often under-funded or funding is under attack, providers can advocate for appropriate funding, as well as use their community benefit to support local food banks, such as Second Harvest [22].
SOURCE: Developed by author.
Fourth, how accurate and effective is the screening? In a review on pediatric screening for SDoH, Sokol and colleagues conclude that the accuracy of such screening is unknown, and more research is needed to determine if subsequent interventions produce better outcomes [36]. Garg and colleagues agree that there will always be fallibility problems with screening tools. Other approaches should be considered; for example, in underserved populations, resource information sheets can help initiate conversations on social needs, focusing where patients and families desire assistance. This approach avoids the inherent problems with screening tools as well as shortens the process [37,38]. (Note: how to make these educational resources more useful is included in Appendix B – Pediatric SDoH, as well as examples of effectiveness of interventions). However, some in the pediatric community are embracing screening, even without the science that it is effective, stating that “addressing the social determinants of child health in the clinical setting is currently more of a moral imperative than it is an evidence-based practice” [39]. Going further, some pediatric researchers are asking how HRSN and/or SDoH screening should “reshape” pediatrics, and compare this issue to other upstream prevention efforts, e.g., cardiovascular risk reduction efforts, that took decades to be adopted by clinicians [40]. An article by Gottlieb et al. on the “uses and misuses” of data and the threats to validity provides an important guide to collecting or analyzing patient-, neighborhood- or ZIP Code-level HRSN data or neighborhood or ZIP Code SDoH data [41].
A fifth factor to consider in screening is the patient’s or family’s interest in assistance. A NASEM workshop focused on integrating social needs into clinical care noted: “What is clear, based on consistent findings from multiple studies, is that current screening tools identify a large number of people who are not interested in help from the health system” [16]. One study in primary care and emergency department settings found that 47% of patients with one or more social risk factors did not want assistance. Multiple factors were associated with more interest in assistance, including having more than one social risk, lower household income, and self-reported non-Hispanic Black ancestry, as well as whether participants were asked the question about desirability before being asked about social risks [42].
More remains to be learned about how people prioritize social risk factors, such as food insecurity, personal safety, and housing, as well as the conditions that foster acceptance of assistance. Do people favor mobile technology and nearby resources, as one study found? Or is the key to avoid any perception of a negative consequence [43]? In CMS’s AHC interim study results, of the patients eligible for navigation services (18% of those screened for HRSN), an average of 24% declined navigation assistance [44]. One study in community health centers reported that only 20% of the 90% who screened positive wanted assistance [45]. The reasons behind this rejection include the fallibility of screening, patients’ experiences with government and/or community organizations, and experiences based on different characteristics such as age, race, ethnicity, and immigration status [46]. DeMarchis and colleagues warn that without a better understanding of what causes some to accept assistance and others to decline it, interventions could inadvertently increase inequities. While awaiting additional research, health care systems can collaborate with patients and communities to co-create screening tools, interventions, and measurement approaches that seek to achieve equitable processes and results.
Sixth, language should emphasize connections. From experienced clinicians in the field, words such as “help” may be offensive or off-putting; therefore, clinicians should avoid words such as needs, resources, help, or assistance. They should instead consider framing the approach as part of the package of care: “In addition to your health, we understand during this sensitive time that connections for essentials are important. With your permission, we’d like to support this connection” [47]. One organization, after hearing from navigator staff that clients felt stigma about accepting help, has created a social media campaign saying, “It’s OK to get help. My (navigator) family needed it, and it’s OK” [47]. Being patient- and family-centered is key; expressing empathy and understanding builds trust on these sensitive issues.
A final consideration is determining needed clinical workflows. Who will do the screening? Will it be done with the EHR, an electronic tablet, or paper? Where will the data be stored? How will it be connected to interventions? How often will screening be done? What resources are available for the screening? Interviews with staff initiating and implementing collection of data in community health centers reveal that the work is facilitated when approaches are flexible and aligned with resources and local interests [48]. There is no “one size fits all.”
It is important to note that screening for social risk factors and HRSN has some overlap with screening for adverse childhood experiences (ACEs). More clinical guidance is needed for how to address this interaction [49].
In the first 750,000 screenings of the CMS demonstration project of screening for HRSN, which have been predominantly among recipients of Medicaid (67%) and Medicare (37%) (includes dual-eligible beneficiaries), 67% reported no core HRSN while 33% reported at least one [44]. Food (67%) was the most commonly identified need, followed by housing (47%), transportation (41%), utilities such as electric, gas, oil, or water (28%), and personal safety (5%).
Only 24% of U.S. hospitals and 16% of physician practices were screening for five key HRSN as of April 2018 [50]. Practices that serve lower socio-economic populations had higher screening rates. In a commentary, Gold and Gottlieb note that from an implementation science perspective, “These findings underscore how much we still have to learn about the types of support needed to implement and sustain [social risk screening].” [51] Corroborating the need for practice structure and support, adjusted multi-variate regression models of the same data showed higher associations of screening with practices’ capacity for innovation than with overall exposure to value-based payment models, except for Medicaid accountable care organization exposure. The measured capacity for innovation included 1) a culture of innovation, e.g., encouragement of new ideas, highly publicizing successful innovations, team members openly sharing patient care challenges and failures, 2) less barriers to adopting care delivery innovations, e.g., time and incentives to implement, necessary knowledge and expertise for implementation, and 3) advanced data system capacity, e.g., communication of patients and providers via email, advanced analytics such as predicting utilization and data mining [117].
In conclusion, there are many issues for health care organizations to consider when deciding whether to screen for social risk factors and HRSN. Clinicians conducting screenings should strongly consider including a question about the desirability of being connected to services to ensure that those being screened are open to accepting connections; they should also avoid words such as help, needs, resources, and assistance. Patients and community members should be involved in the design of the system, and can help create a screening protocol and follow-up plan that pays attention to community cultures and equity. As an alternative to implementing screening, clinicians with disadvantaged populations may want to offer connections for patients across a number of domains, and let patients choose. Finally, clinicians and health care researchers have little experience in how these screening tools function in a telemedicine world; however, the COVID-19 pandemic probably foreshadows more use of virtual care. Systems must collect data to understand how to best design and redesign for improvement and equity postCOVID-19 pandemic.
Employing Plan-Do-Study-Act (PDSA)
After selecting a framework and making a decision about screening approaches and methods, health care systems can implement the Plan-Do-Study-Act (PDSA) approach (see Figure 5). This approach allows organizations to build on current systems thinking and incorporate new aspects that are needed to address community SDoH as well as individual social risk factors and HRSN.
FIGURE 5. Plan, Do, Study, Act for SDoH, Social Risk Factors, or HRSN.
SOURCE: The W. Edwards Deming Institute. Available at: https://deming.org/explore/pdsa/ (accessed April 27, 2021). Used with permission.
The PDSA cycle consists of the following steps:
P- Plan
Review the data and input from partners
Involve partners inside and outside the health care organization
Review clinical data combined with community data
Decide on interventions or the changes to be made, which can include:
Screening for social risk factors or HRSN inside the health care system with community connections
Interventions for SDoH, social risk factors, or HRSN outside and inside the health care system
Determine how the change will be measured – both in process and outcomes
D - Do
Implement the proposed changes
S - Study
Review the qualitative and quantitative results
A - Act
Reflect on the PDSA cycle and plan next steps
P - Plan
Reviewing the Data and Input from Partners
Who should be at the table to review the data for QI? For clinical issues, patients are normally the only individuals outside the health care system involved in improving the process. When implementing SDoH, social risk factors, and HRSN initiatives, as noted above, additional community partners and other sectors should be involved in the PDSA steps. Although this process requires that an organization be vulnerable and willing to share its power, shared decision-making is critical to building trust and ensuring effective action.
Data should guide the plan. The data being reviewed must expand beyond clinical information in electronic or paper records, because traditional medical records do not account for the critical SDoH, social risk factors, and HRSN outlined in the rest of this paper that deeply influence overall health. Social histories may elicit some data of interest, but there is more to be explored (see Box 4). For example, County Health Rankings and Roadmaps provide information on upstream SDoH (e.g., food environment index, childhood poverty, high school graduation rates, etc.) as well as health outcomes (e.g., premature death, poor mental health days, poor physical health days, etc.). The City Health Dashboard includes information on 37 factors that affect health in 500 U.S. cities, such as excessive housing cost, neighborhood racial/ethnic segregation, third grade reading proficiency, and lead-exposure risk. More recently, the City Health Dashboard added a COVID-19-risk index with three measures that incorporate related SDoH: CDC’s Social Vulnerability Risk, chronic conditions prevalence, and relevant age and race/ethnic demographics.
Box 4. Quantitative and Qualitative Data Sources for Planning for SDoH, Social Risk Factors, and HRSN Interventions.
Electronic health record history of social risk factors, HRSN, and/or SDoH data, if collected, including disaggregation by race, ethnicity, and geography
County Health Rankings and Roadmaps (https://www.countyhealthrankings.org)
City Health Dashboard (https://www.cityhealthdashboard.com/)
Community health needs assessments, including data on inequities
Community benefit plans
Lived experiences from patients and community members, especially disadvantaged populations
Patient surveys and/or additional community surveys
Multi-sector partner feedback
Others
SOURCE: Developed by author.
Tax-exempt hospitals must perform a community health needs assessment and demonstrate strategies to address the identified needs in their community benefit plans. How can this information, as well as other data in Box 4, help direct work inside and outside clinic walls? Who is already working in the community served by the health system to achieve shared goals? How might clinical work complement what community members seek to achieve?
Box 5 describes how one health care system has combined clinical and community data to further its work to improve not only health care but the conditions in which patients and families live.
Box 5. Combining Clinical Data with Community Data: Example.
Karen Boudreau, MD, Senior Vice-President, Enterprise Care Management and Coordination at Providence St Joseph Health is a “co-sponsor” of the organization’s SDoH and social risk factor work across five million patients in seven states, in close partnership with its community benefit work. “I think about our work on three levels: individual, population and community. We have to align and work strategies across all levels.”
Providence St Joseph Health started working on SDoH and social risk factors for various reasons in different regions: “Our organization’s mission focuses on the poor and vulnerable, and we want to increase our performance in Medicaid. But that is not sufficient…. We are looking at our clinical data combined with our publicly available block-level data. Although we are often approached by many different vendors promising all kinds of solutions, we have started with trusting and using our own data. We do want to know if patients are in an area with housing instability or low educational attainment—that tells us something about the community where our patients live and helps us think about how we approach understanding our patients’ needs.”
“For our EHR pilot, we chose two domains: the first focused on finances (i.e., food and housing insecurity) and the second on substance use, including a focus on alcohol. The impact of alcohol on lives, deaths, outcomes is massive. Most health systems don’t adequately address alcohol use, and we need to decrease its negative impact. Our organization is working on overlapping strategies in Medicaid, mental health and wellness, and housing instability—strategies braided together to ultimately improve health for our most vulnerable populations.”
“We need to develop relationships with community organizations that can help us at scale depending on what is important. For example, we don’t have as much direct control over employment beyond our own organization but are doing work to improve the environment in which our patients live through our community investments.”
Dr. Boudreau worries that health care will make addressing the SDoH and social risk factors a “transactional” process. “We as a country are way oversimplifying this; we don’t have easy answers to issues that are basically caused by poverty, systematic inequities, and racism.” But she sees the SDoH effort as a way to combine clinical data with community data to improve care for patients and to work with the community to address underlying issues to improve well-being.
SOURCE: Developed by author.
Finally, the data and community input should guide what is to be accomplished. What is a priority for patients and members of a community? When assessing a patient’s social needs and/or living conditions, what the clinician thinks is most important is often not what patients and/or community members think is most important. For example, one California public health group wanted to address tobacco in their community, but community members wanted to address safety first. The program was modified to start with what was most important to community members and build trust; after addressing safety, the residents addressed issues such as tobacco use.
Designing Interventions
The next step, after reviewing the data and deciding on the topic(s) for the intervention(s), is to review the evidence for what actions to take for the greatest impact—both for individual social needs and for policy in community SDoH. Consider the interventions cited in SDoH 101 [1] and additional background information and examples (see Appendix B). These include topics such as:
-
Background
Overall resources when considering interventions
Prevention
Interventions and what is known about cost savings
Pediatric SDoH
Employment
Poverty
Community health workers and IMPaCT
Finances and Medical-Financial Partnerships
Food insecurity and food as health care
Medical-Legal and Medical-Legal-Psychology Partnerships
Transportation
Housing
Social isolation and loneliness
Inclusion of populations in design
Since the evidence base for interventions to change SDoH, social risk factors, and HRSN is rapidly increasing and the list of interventions outlined in Appendix B is not comprehensive, an easily searchable database is SIREN (Social Interventions Research and Evaluation Network) [54]. For example, searching for “partnerships” reveals relevant articles, e.g., using a practice facilitator (quality improvement process facilitator) with Community Health Workers (CHWs) to implement community-clinical connections for small practices—although the authors state that more research is needed on the cost and ROI of these strategies [55]. A Health Affairs Blog provides examples of partnerships between aging and disability CBOs and health care systems and providers to address a full spectrum of needs, and a call for an integrated approach for social and health care services [56]. A SIREN webinar on “Data sharing & the law: overcoming health care sector barriers to sharing data on social determinants” describes Manatt Health’s efforts to address these barriers with entities, e.g., health care, housing, education, and criminal justice sectors, so that whole person care can be delivered [57]. The webinar reviews overall requirements for the health sector sharing or receiving data, considering key privacy laws and uses case analysis (e.g., housing, school health programs, prisoner re-entry, food stamps) to highlight key issues. In addition to the database, SIREN has started “Coffee and Science” thirty-minute conversations twice a month on “hot topics” in the integration of social care into health care, and a monthly “research round-up” of new publications added to the database.
One well-publicized study intervention is CMS’s AHC, with HRSN screening described previously, with subsequent navigation assistance to connect with community services, or navigation assistance and alignment of community resource capacity with the community’s service needs. Community-dwelling CMS and Medicaid beneficiaries are eligible for the study if they have one or more identified core HRSN and two self-reported emergency room (ER) visits in the 12 months before screening. The initiative is only in the third year of implementation, but initial results show:
For the eligible beneficiaries, 74% accepted navigation, but only 14% of those who completed a full year of navigation had any HRSN documented as resolved.
For the Medicare Fee-for-Service beneficiaries in the Assistance Track intervention group, there were 9% fewer ER visits than those in the control group in the first year after screening.
More on the initial results and the different approaches in this real-world experiment are described in the first evaluation report [123].
High impact policy interventions can complement individual social risk and HRSN interventions, as outlined in the following two resources:
-
1.
Health Impact in Five Years (HI-5) initiative [58]—contains proven interventions that seek to change the community or societal context (e.g. instituting physical education requirements in schools, implementing tobacco control policies and pricing strategies for alcohol products) and the SDoH (e.g., investing in early childhood education, providing financing to support affordable housing, and expanding public transportation.)
-
2.
Trust for America’s Health’s Promoting Health and Cost Control in States [59]—although at a state level, this report provides a compendium of policy changes that can impact the SDoH, such as enhancing school nutrition programs, implementing “complete streets” to promote connectedness, funding housing programs, etc. Health care organizations can work with state community partners to explore interventions that complement their clinical work on social risk factors.
Some interventions require the use of a community resource referral platform to connect patients and families to community-based organizations to address needs. A SIREN review [60] examines such platforms, including functionality, a side-by-side comparison of common platforms, issues with interoperability, and possible other approaches. The section on implementation lessons learned offers the following recommendations:
-
1.
Engage community partners from the beginning;
-
2.
Examine what already exists in the community to avoid duplication and proliferation of redundant platforms;
-
3.
Have a clear understanding of goals and needs;
-
4.
Don’t assume that if you build it they will use it; and
-
5.
Know that this work takes time.
Box 6 discusses the importance of working with community partners to develop interventions, provides an example from the field, and gives practical tips on building and sustaining these partnerships.
Evaluating the Changes
As part of the “P” in PDSA, planning for evaluation is key. The NASEM report Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health states, “Integrating social care into health care delivery holds the potential (italics added) to achieve better health outcomes….” [16] Although it is tempting to believe that something so intuitive must be effective, health care has been mistaken time and time again—which is why it is so important to plan for an evaluation for any community SDoH or individual social needs intervention. Berkowitz and Kangovi’s Milbank article is a reminder: “Health Care’s Social Movement Should Not Leave Science Behind” [63].
To know if a change indeed represents improvement, a measurement plan is required – considering measures for qualitative and quantitative changes. Interventions that have been tested previously and reported in the literature provide greater confidence of effectiveness, but this is not a guarantee; differences in population, setting and implementation can lead to different results. Look for process and outcome measures related to what change is being implemented. For example, the Children’s Hospital of Philadelphia (CHOP) community health needs assessment identified poverty as a key social risk factor. This inspired their pediatricians to work with the local Volunteer Income Tax Assistance (VITA) CBO, Campaign for Working Families (CWF), to create a medical-financial partnership (MFP) to decrease poverty in West Philadelphia. Their goal was to test a program to increase the number of tax returns for low- and moderate-income individuals for the Earned Income Tax Credit (EITC) and the Child Tax Credit (CTC). They obtained metrics of qualitative feedback from clinic leadership and the CWF. The MFP tracked number of financial returns submitted and the amount of dollars generated for the community. In two years from 337 tax returns, they have generated $700,00 returned to the community with $224,022 from the EITC and $111,874 from the CTC. Among the 22 sites of the CWF, CHOP had the second-highest rate of filing for EITC. This MFP was a proof of concept, and more work will be done to establish additional outcomes, e.g., new EITC filers [122].
With real-world quality improvement experiments, there is often no randomized-controlled data. However, it is possible to create rapid-cycle evaluation strategies or other methods for evaluation. For example, New York University (NYU) Langone Health created rapid-cycle randomized quality improvement cycles as part of their evolution to a learning health care system [64,65]. They learned that post-hospital telephone calls did not change readmissions rates or patient experience, and the targeted group for a CHW intervention did not show a decrease in acute care hospitalizations, despite intuitive beliefs that such interventions would reduce hospitalizations. Although the NYU initiative is costly, it has already paid for itself in the revenue generated—mainly by increasing clinical preventive services (e.g., a tested provider-targeted prompt which increased tobacco cessation counseling) and by stopping ineffective practices (e.g., patient-appointment reminder letters) [66]. In addition, there are other new methods such as pragmatic trials, cross-over designs, and stepped wedge designs [63]. Partnering with QI experts or evaluators in an organization or community can be helpful to determine evaluation strategies. Remember that pre- and post-observational data are often fraught with regression to the mean, especially with cost data.
Box 6. Community Partnerships and Interventions: Examples.
As health care organizations plan interventions for HRSN and SDoH, it is critical to involve community members and/or organizations. First, health care practitioners need the perspective and wisdom of the community—residents know what they need best. Second, health care organizations need to build on known assets and grow a community’s or region’s capacity to address a range of issues that impact health. Finally, we are all interconnected, and seeing clinics and hospitals as part of a spectrum better ensures that the needs of patients and families are met.
An example of creating a new partnership
When Christine Cernak, RN, Diabetes Care and Education Specialist, Senior Director, Longitudinal Care at UMass Memorial Health, began exploring HRSN and SDoH with her team, they created a community process to select a vendor who would help connect patients to needed social services. With input from the community and this new vendor partnership, UMass created Community HELP (Health and Everyday Living Programs), an online platform to connect people to needed services in Central Massachusetts [61]. The evaluation of this new process is in the early stages, but one major improvement is that it takes less than a minute to screen most patients using a modified PRAPARE (Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences) tool. The provider group has seen an increase in online searches in the ZIP Codes of practices with screening and referral, and they plan to have 75% (N=33) of UMass Memorial Medical Group primary care practices engaged in universal screening by the end of September 2021. Longitudinally, they are tracking health maintenance measures and chronic disease control as well as emergency department visits and inpatient utilization.
A resource for building or enhancing partnerships
The Practical Playbook II offers a tool for building or enhancing multi-sector partnerships [27]. It draws on specific examples from the housing, transportation, and business sectors and includes viewpoints from CBOs and practical tips, e.g., how to draft memorandums of understanding and data-sharing agreements; how to finance partnerships over the long term; and how to effectively engage elected officials in multi-sector partnerships.
A tool for assessing existing partnerships
For organizations that have existing community partnerships, the Partnership Assessment Tool for Health may be helpful in assessing progress, developing next steps, and guiding critical dialogue for the partnerships [62]. The tool covers topics such as internal and external relationships, service delivery and workflow, funding and finance, and data and outcomes. It is designed especially for health care organizations in partnership with a CBO providing human services and serving vulnerable or low-income populations.
SOURCE: Developed by author.
With an increased focus on equity, a measurement strategy to evaluate for changes in inequities or disparities should be incorporated into planning for interventions for SDoH, social risk factors, and HRSN. The Institute for Healthcare Improvement published “6 Tips for Measuring Health Equity at Your Organization” [67] and a white paper for healthcare with a chapter on “Guidance on Measuring Health Equity” [68]. Sivashanker and colleagues explore advancing equity with several different areas for measurement [69], such as an access measure of the difference between the percent of Medicaid or uninsured patients cared for by an institution and the percent of Medicaid or uninsured patients in the corresponding service area, e.g., city or region. Another measure includes referrals (e.g., social services), consultation rates, or any change in settings and whether patients are offered these services equitably. For employees, are there staff measures for equitable transitions including organizational promotions stratified by race, ethnicity, and gender or combinations thereof?
One place to start is by stratifying the processes or outcomes from the intervention(s) by demographics (e.g., race, ethnicity, gender, socioeconomic status). Sivashanker advocates for building on current quality and safety systems by adding a question, “Are there inequities here” [70]? This puts an equity lens into current everyday work, socializes equity work as the norm, and lets it grow on itself to where leaders see it as their responsibility, “dismantling racism and inequity in health care.”
D - Do
After moving through the planning phase, the team is ready for the “Do” part of PDSA. Selected clinical intervention(s) should be implemented in a rapid cycle with a few providers, a limited number of patients/community members, and important community partner(s). Small tests of proposed changes will allow for quick assessment and adaptations of the intervention before launching at a larger scale. To build success and next steps, staff, patients, and community partners should be involved in the implementation phase. If outside referral resources are part of the implementation change for social risks and needs, assess process measures linked to the desired outcomes. Also remember to communicate, communicate, and communicate while implementing change. Respecting confidentiality, patient or family stories—especially those highlighting the engagement of CBOs—may boost these efforts by showcasing the humanness and potential of this approach.
For policy and/or system changes to affect SDoH, implementation and impact require a much longer time horizon. Community partners and organizers will have experience in such work. Experienced community leaders should guide the development and implementation of policy, and the measurement of implementation milestones, e.g., implementation of school nutrition programs to complement screening for food insecurity for children and adolescents.
S - Study
In the study part of PDSA, collected process measures and/or outcome measures are reviewed. For HRSN, process measures may be the number of people screened or the number of people connected to a public health or social service agency with numbers of closed-loop referrals. An outcome measure may be the percentage of low-income children in early childhood education or home-visiting programs (process measures connected to known improved outcomes). Outcome measures require years in follow-up, but having connected process measures will ensure directionality for the best results. If a community partner helped address a policy issue, what was learned together in addressing an underlying SDoH? For example, if the focus was affordable housing, what impacts were seen in the community and in clinical care?
In working toward equity, the data selected in the planning phase should help guide how inequities or disparities should be monitored. What do community members report about how the intervention is addressing both? Have there been any unintended consequences? See Box 7 for another way to address equity.
One practical example of monitoring for equity is the Health Equity Advisory Council of the Gen-H Connect (the AHC with the Health Collaborative) in the greater Cincinnati area. As the Gen-H Connect manager Ivory Patterson notes, Council members from diverse backgrounds review the data monthly on five domains (housing instability, food insecurity, transportation problems, utility help needs, and interpersonal safety), stratified by race and ethnicity. The Council noted that food insecurity was the most commonly identified need, and more food resources were needed for African Americans in Hamilton County and for Latinx populations in Butler County. With the Council and community partners, Gen-H Connect is working to understand the food equity landscape, co-create solutions, and align food resources in the community to meet these needs [71].
Box 7. Mapping and “Seeing” Neigborhoods in the Quest for Equity - Examples.
Beck and colleagues are promoting health equity by mapping neighborhood geo-markers for use with individual patients [73]. They define geo-markers as “any ‘objective, contextual, or geographic measure’ that influences or predicts the incidence of outcome or disease.” Just as physicians look at bio-markers for diagnostic and treatment plans, clinicians can look at geo-markers to guide clinical decisions and care plans. The researchers have created a lexicon of community geo-markers (e.g., distance to pharmacy, availability of public transport, housing code violations, exposure to pollution, poverty rate, educational attainment, crime rate, etc.) with interventions (medication delivery, Medicaid rides, housing inspections, legal aid, air filtration, financial services, community health workers, resilience training, community agency referrals, etc.)
As an example, working with patients and families with asthma, Beck and colleagues developed and calculated, at a census tract level, a Pharmacy-level Asthma Medication Ratio (ratio of preventive to rescue asthma medications). They found that the higher the ratio, or the use of more corticosteroid inhalers versus beta-agonists, the less likely it is that the children in a particular geographic area will have asthma emergency room visits and hospitalizations.
They also found that children hospitalized for asthma with the highest geo-risk index (measured by census tract measures of home values, poverty, and adult educational achievement) were 80 times more likely to be re-hospitalized than children at lowest risk. Such indexes can prompt clinicians to provide additional support, such as self-management programs, home delivery of meds, and possible hospital-pharmacy partnerships to increase the use of preventive meds for asthma, referrals for home inspections, or legal advocacy. The authors concur that more research is needed to develop the policies, programs, and privacy protections such that place-based data can support the best individual interventions and the right community multi-sector partnerships to improve upstream outcomes. It is their hope that one day, “person-centered care begins the moment patients provide their address, promoting improved, equitable health outcomes.”
Alternatively, Beck and colleagues used a quality improvement approach for “hot spot” neighborhoods (i.e., neighborhoods with high rates of illness and poverty) in Cincinnati, Ohio to decrease pediatric hospitalizations [114]. The researchers specifically wanted to see the neighborhood as the entity for narrowing population health gaps between disadvantaged neighborhoods and healthier ones, “….viewing child health equity through a neighborhood lens.” Working with neighborhood partners and keeping the patient and family at the center, the researchers pursued interventions of care management, addressing social risks, transitional coordination, and actionable data for improvement. For example, they showed neighborhood-based asthma data to community members, which correlated with housing problems in a specific complex, that fueled alignment of community partners for action. The overall result was hospitalizations decreased by 20% when compared to socio-demographically similar neighborhoods.
Is there additional evidence that social risk factors and SDoH can be incorporated into electronic health records and used to inform next steps for patients and communities to improve equity? “Community Vital Signs” is envisioned as a roadmap to link aggregated population health data with patient addresses [74]. The researchers caution, however, that both individual and community data are needed - for the best interventions—with individuals and for alignment and advocacy for policy to change the community context; it is “and, not or” [75], as supported by recent research [76].
Although implementation research and financial sustainability questions remain, providing such integrated clinical and community data could help providers view their patients holistically in the quest to improve health at the patient, population, and policy levels.
Considering how to study a community partnership approach in this part of the PDSA cycle, the approach by Levi and colleagues provide useful principles and questions. They were originally designed for “accountable health communities” [72] and for use by funders and policymakers to determine “what works” and how to better structure evaluations for community partnerships and interventions. However, the principles and questions are helpful guides for how health care organizations interact with community partners. For example:
-
1.
Readiness – How have relationships among health care systems and providers, community organizations, and residents changed? How are the entities working together to achieve the desired outcome(s)?
-
2.
Common elements – How is the portfolio of interventions in HRSNs and SDoH aligned to advance the goal? How can the work be sustainable?
-
3.
Outcomes – How are measurement systems supporting the work? How are interventions regularly adjusted, both inside health care systems and in the community, including any policy interventions?
A - Act
The final part of the PDSA cycle includes spending time reflecting with community members (patients and residents) and community organizational partners before repeating the PDSA cycle for individual social risk factors and HRSN, and policy changes for SDoH. The PDSA team should revisit the question, “What changes can we make that will result in improvement?”, to consider what should be changed and what should not be changed. What was learned in this cycle? What new community partners, if any, should be at the table as the work proceeds—both as partners for implementation and partners for study and evaluation? Members of the PDSA team(s) should also decide what other principles of authentic community partnerships to enhance in the next cycle.
There are many other questions to ask at this stage. How has the selected framework for HRSN, social risk factors and SDoH been useful? What can be prioritized in the next cycle? Will there be an expansion of social risk factors or HRSN to address? Is there one that best complements what was already addressed? For example, housing and utility needs often go together. How has any policy or system change in the community been complementary to the clinical work? Here, the team should listen to staff, patients, and community residents for their priorities and insights.
Before acting again, how does this work fit with current QI initiatives in the organization and community? How has the capacity of the organization and the community to implement policy changes been strengthened? Some ideas are offered by reviewing the attributes and capacities of community-centered health care homes [77]. A group of pediatric clinicians found, for example, that one way is to expand their vision, explaining, “… we should not be content to just build a better patient-centered medical home when we also have the opportunity to partner across sectors and build patient- and family-centered health communities” [40].
Overall, the financial sustainability plan for the initiative(s) should be discussed, inviting any other partners who should be at the table for this discussion. Is the organization preparing to participate in any new payment and community models such as Community Health Access and Rural Transformation (CHART) [78] or Geographic Direct Contracting (GEO) [79] from CMS? There is hope that new payment models will prompt health care organizations to be more involved in ameliorating and addressing SDoH, social risk factors, and HRSN. However, Accountable Care Organizations (ACOs), despite motivation and new payment models, still struggle with integrating social risk factors and HRSN into health care. A qualitative study from ACO perspectives of obstacles reports that the obstacles include:
-
1.
Inadequate patient data on social needs and data on community partner capability;
-
2.
Community partnerships that are often in early stages; and
-
3.
Lack of information of how to approach investment and ROI given usual three-year cycles. [80]
Proposed policy solutions are 1) standardized data on CBOs’ services and quality, 2) opportunities for networking to facilitate partnerships locally and regionally, and 3) funding strategies that create sustainable relationships with CBOs. In addition as noted earlier, a culture for innovation, removing barriers to implementation, and advanced data system capacity may be more associated with screening for social risk factors than exposure to value-based payment models [117].
Finally, organizations should communicate and celebrate internally and externally what has been accomplished and learned. Credit should be given to community partners who have been involved, highlighting stories of the benefits to the community and community residents as well as the health care system.
Conclusion
With the engagement of community partners, health care organizations can take next steps to change the delivery of care and the context for their patients’ health and well-being. Leadership perspectives and involvement are key to the success of such initiatives. Health care leaders can begin by selecting a framework for the organization for upstream SDoH and downstream social risk factors and HRSNs. Such a framework can guide their internal thinking and their interactions with CBOs and community entities. The next step is to consider the multiple factors related to screening some or all patients for selected social risk factors and HRSN. With community partners, health care organizations should use the Plan-Do-Study-Act (PDSA) cycle to explore the data and determine what is to be accomplished, starting with the greatest needs identified from the data and the community perspective—including both the individual social risk factors and HRSN and the community conditions where people live, work, play, pray, and learn. They should then review what is known about evidence-based interventions, e.g., by consulting the SIREN network and determining what interventions clinically and in the community can address prioritized HRSN, social risk factors, and SDoH. It is important to pay close attention to where policy, system, and environmental changes will provide the greatest impact inside the clinical walls and outside in the community; collaborate with QI experts and evaluators to know that change represents an improvement; and listen carefully to communities that have suffered the greatest disparities and inequities - particularly where they see community assets and needed partnerships.
New payment models will likely spur providers’ interest in addressing SDoH, social risk factors, and HRSN, but much needs to be learned about the needed culture and infrastructure for innovation and implementation. The COVID-19 pandemic, as well as the urgent, recent calls for racial and social justice, should continue to increase new approaches for health and well-being. The convergence of these three factors, combined with visionary leaders in health care and the community, provides an opportunity to advance better health, better health care, and lower costs. To succeed, organizations must create learning health systems and form authentic community partnerships, and must also be humble as relationships and science evolve. For health care systems, using the approach described in SDOH 201 can guide steps along the way, both upstream and downstream.
APPENDIX A– More Details on PDSA
Plan-Do-Study-Act
https://www.health.state.mn.us/communities/practice/resources/phqitoolbox/pdsa.html
Part of a public health toolbox but with many helpful tools applicable to health care and communities.
The ABCs of PDCA
http://www.phf.org/resourcestools/Documents/ABCs_of_PDCA.pdf
Includes more details on each of the phases.
Institute for Health Care Improvement
http://www.ihi.org/resources/Pages/Tools/PlanDoStudyActWorksheet.aspx
http://www.ihi.org/resources/Pages/HowtoImprove/ScienceofImprovementTestingMultipleChanges.aspx
This is a simplified PDSA worksheet that may be familiar to health care organizations; it will need to be adapted to include the community partnership involvement important to addressing HRSN and SDoH.
APPENDIX B – Interventions Referenced in Social Determinants of Health 201 for Health Care
This is not an exhaustive list but provides a starting point, in addition to SDOH 101 for Health Care [1].
Overall resources when considering interventions
A review by Beck et al. [81] titled “Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care” and the Fichtenberg et al. article [82] on key research questions are good places to start when considering interventions to pursue.
Two National Academies of Sciences, Engineering, and Medicine (NASEM) workshops (in addition to the report Integrating Social Care into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health [16]) highlight the interest in this topic:
-
1.
Investing in Interventions That Address Non-Medical, Health-Related Social Needs: Proceedings of a Workshop [83]. This workshop summary includes current science on housing, food security, and multi-social needs interventions as well as a discussion on ROI.
-
2.
Models for Population Health Improvement by Health Care Systems and Partners: Tensions and Promise on the Path Upstream: A Workshop [84].
The “Take Action” section of the County-Based Rankings and Roadmaps [85] provides guidance on evidence-based policy and program interventions, steps to turn data into action, and discussion of how to engage community partners. Additional resources can be found in Appendix C.
Prevention
Although there often is a rush to new ideas, the “bread and butter” responsibility of health care should not be forgotten, especially efforts to decrease disparities in the delivery of traditional clinical prevention. As social risk factors and HRSN are addressed, the interventions in the “Three Buckets of Prevention” (traditional clinical prevention, innovative clinical prevention, and community-wide prevention) [86] are reminders about the importance of seeing patients as community residents and addressing a full spectrum of individual and community interventions with partners. The approaches are very consistent with the downstream and upstream analogies of HRSN, social risk factors, and SDoH.
Interventions and cost savings
An article by Maciosek and colleagues [87] highlights that societal, “cost-saving” clinical preventive services are childhood immunization series, brief prevention counseling to youth on tobacco use, tobacco use screening and brief counseling in adults, alcohol misuse screening and brief intervention in adults, and aspirin chemo-prevention for those at higher risk of cardiovascular disease. It is sobering to note that many population health management interventions on targeted populations have not, or have not yet, shown cost savings [88].
Recently, a “social-return-on-investment” (SROI) analysis was completed of Bon Secours Hospital’s affordable housing initiative in Baltimore, Maryland. Although the analysis did not include the start-up costs, the “Housing for Health” program generated a potential $1.30 to $1.92 in social value for every dollar of annual operating expenses. Such SROI can incorporate the unique, multi-dimensional returns of individual, social and community outcomes difficult to measure in traditional economic analyses. Longer-term analyses could include the initial investment [116].
The Commonwealth Fund published a return-on-investment (ROI) calculator that includes a summary of evidence on interventions for health-related social needs for high-need or complex adults (“Interventions to Address the Social Determinants of Health”) [89]. The categories examined include transportation, nutrition, housing, home modifications, counseling, and care management. As always with results, care should be taken to consider regression to the mean, costs of the intervention not included in cost savings, and results that overstate the science.
Pediatric SDoH
A randomized controlled trial (RCT) cluster study “Well Child Care, Evaluation, Community Resources, Advocacy, Referral, Education” (WE CARE), focused on mothers of young children, specifically mentions screening for desirability for assistance and providing referrals when assistance is desired, with additional follow-up phone calls. At 12 months, in comparison to the control, WE CARE mothers were more likely to be enrolled in a community resource and be employed, their children were more likely to be in child care, their families were more likely to be receiving fuel assistance, and they were less likely to be in a homeless shelter [39]. A RCT by Pantell and colleagues in urgent and primary care clinics of two safety-net hospitals in northern California showed decreased hospitalizations after caregivers with children who identified with social risks were assigned to volunteer navigators who connected families to community resources (versus being given a non-personalized handout with community social resources). There was no change in emergency room use [118].
It is not clear what the place and intensity of support should be for connecting patients to resources. For example, pediatric providers referred more caregivers to a navigator in-person (45%) vs the same navigator remotely (29%), but there was no difference between in-person and remote navigator in subsequent patient contacts with the navigator or enrollment in resources for unmet social needs [119]. In contrast to a previous study [120], Gottlieb and colleagues in a pediatric urgent care clinic population found that assigning caregivers a longitudinal navigator for social services did not decrease social risk factors or improve child health more than the provision of updated, curated, and personalized information on community resources [121]. For example, the study used two techniques which increase the usefulness of resource materials: highlighting information most relevant to the top three priorities identified by the caregiver and providing contact names (when available) at the relevant community resources. The authors note this study adds to what is known about “the dose” and possible scalability of interventions to address social risk factors in clinical settings but concludes that more research is needed to determine effectiveness.
Employment
As one of the SDoH, employment is a key to health and well-being. Pinto and colleagues [90] review the literature on addressing employment within healthcare, with most articles focusing on patients with mental illness.
They identify five components of successful programs:
-
1.
A multi-disciplinary team including employment specialist(s);
-
2.
A package of comprehensive services;
-
3.
Individually tailored approaches;
-
4.
A holistic view of the patient/potential employee; and
-
5.
Ongoing relationships with prospective employers.
Although such an array of services is not practical for most health care organizations, referral processes to community resources are doable.
Poverty
Although there are not many well-designed clinical studies about health care interventions to address poverty, pediatric care groups can be organized to address families living in poverty, including (1) individual, proven approaches such as home visitation, (2) use of resources with track records of success, such as Reach Out and Read, and (3) practice level political advocacy [91,92].
Finances and Medical-Financial Partnerships
Concerning finances, a Canadian primary care study in collaboration with a financial literacy organization is testing an online patient tool to increase access to financial benefits [93]. For Medical-Financial Partnerships (MFP), a review describes three different models (on-site full scope financial services, on-site targeted scope financial services, and off-site financial service referral). These models may or may not be linked to screening for HRSN or SDOH, but all work to decrease the financial stress of low-income families [94]. The most successful MFPs in health care have clinical, financial, and administrative champions; on-site facilities; access to volunteers in addition to paid staff; and funding support, often from grants, donations, or, in one case, hospital community benefit dollars.
Food Insecurity and Food as Health Care
On food insecurity, a systematic review of the US literature of health care-based interventions reveals a common theme—an increase in process measures (e.g., referrals to food resources and resource use) with few available health outcomes measures [46]. The authors reviewed 23 studies that met inclusion criteria and concluded that “the low number and low quality of studies limit inferences about their effectiveness.” Some organizations are actively screening and intervening for food insecurity, but published outcome results are not available. Of note, a recent non-health care based RCT with people who screened positive for diabetes at food banks found that clients given self-management support and diabetes-appropriate food showed an increase in food security and an increase in intake of fruit and vegetables in the intervention group but no significant change in self-management or glycemic control (HbA1c) [96]. However, one intervention with complex patients with high health care utilization referred by a clinician for medically tailored meals (10 per week) through one Massachusetts community service agency appears to decrease health care use and costs [97]. This matched cohort study extends previous research to this broader population with clinical, nutritional, and socio-economic risk. However, before this expensive model is generalized, more research is needed, especially in matching different patient needs to appropriate cost-effective interventions (e.g., SNAP, food pantries, senior centers with meal provisions, Meals on Wheels, etc.).
A study in Colorado compared seven CBOs and three health care clinics enrolling food insecure clients in SNAP. Given equal amounts of money and a five-part care cascade from screening to enrollment, the CBOs assisted more individuals (55%) than the health care organizations (22%) along the care cascade. A familiar theme emerged: only 35% of individuals who were food insecure participated in the care cascade and enrolled in SNAP. Those more likely were adults 40 years or older, rural residents, and American Indians/Alaska Natives [98].
Medical-Legal and Medical-Legal-Psychology Partnerships
Medical-legal partnerships can help providers consider SDoH, social risks, and HRSN that may not be intuitive such as cash assistance, housing conditions, utilities shut-off, legal status, educational assistance for children, and family protection needs such as guardianship. There are many different forms of these partnerships, as outlined in a paper by Regenstein and colleagues [99], but they all start with a willingness to explore a different community partnership, e.g., with a non-profit legal aid organization. Although the research on health outcomes from these partnerships is nascent, there is interest in how these partnerships can decrease disparities [99]. County Health Rankings has an overview of the current evidence for MLP [95].
One such partnership at Cincinnati Children’s Hospital was highlighted in SDoH 101 [1] and is now called the Cincinnati Child Health-Law Partnership (Child HeLP). Subsequently, the practitioners are testing a medical-legal-psychology (MLPP) model with embedded clinical psychologists providing consultation for behavioral and mental health services including prevention and short-term therapy. For the first year, the MLPP received approximately 6% of all Child HeLP referrals (N=74) with 50% for educational issues such as special education, behavioral supports, and disciplinary problems in schools. Although the clinicians early experience is limited, they see a benefit in this integrated approach for at-risk youth and families to understand and address the trauma and adversities in a more equitable approach [115].
Transportation
A systematic review on non-emergency medical transportation (NEMT) services [100] found that very few studies (N=8) on effectiveness met the criteria for inclusion, despite how commonly transportation interventions are used. Even of the eight, most studies are not peer-reviewed RCTs and do not contain health outcomes. Of the three RCTs, one rideshare study showed no decrease in no-show rates, and two other studies showed decreases in no-show rates. Interestingly, in these three studies, only 3-30% of the patients used the offered transportation services—another reminder to inquire about the desirability of assistance. The authors concur with others that the offer of NEMT may be primarily a psychosocial intervention that conveys concern and urgency for the well-being of patients. Several studies were excluded from the systematic review because the effect of transportation from other social interventions could not be examined; however, some of those studies [101] show a benefit on health outcomes. This is another reminder of the clustering of social risks and the need to address risks holistically to achieve the greatest possible acceptance and impact. Nevertheless, it is difficult to isolate the individual contribution of NEMT services. In addition, few studies have matched transportation use patterns with patient preferences (e.g., older patients use public transportation less than younger patients), and few have studied new modes of electronically facilitated rideshares in primary care [102].
Community Health Workers and IMPaCT
To address social risks more holistically, the standardized IMPaCT (Individualized Management for Patient-centered Targets) model uses community health workers (CHWs) who focus on upstream issues that transcend diseases. Patients with two or more chronic diseases in high poverty neighborhoods set a health goal with their physician, and the CHWs provide “tailored coaching, social support, advocacy, and navigation,” but no specific disease interventions or education. One study by Kangovi et al. in an academic medical center showed a reduction in hospitalizations at one year of 28% with some improved clinical indicators and with improved self-rated mental health and quality of care [103]. A subsequent generalization study confirmed improved self-rated quality of care and a decrease in hospital days and lower rates of re-hospitalizations over the control arm, [104] with an estimated return on investment within a fiscal year to an average Medicaid payer of $2.47 for every one dollar invested [105]. Another benefit of the IMPaCT-style approach is the attention to upstream social and behavioral factors that may help lay the foundation for interventions at the population or community level.
Housing
For housing, an RCT by Sadowski et al. [106] for homeless patients with medical illnesses describes the multifaceted intervention of housing and case management that decreased hospitalizations and emergency room visits. Most importantly, there was a community-wide collaboration of providers, social workers, and advocacy groups who tailored the housing and case management interventions to the needs of the patients. However, it should be noted that these homeless patients were higher utilizers of the health care system at baseline; therefore, the intervention may not show the same effect on homeless patients with different characteristics. The NASEM report Permanent Supportive Housing: Evaluating the Evidence for Improving Health Outcomes Among People Experiencing Chronic Homelessness [107] concludes that there is not substantial published evidence (outside of HIV/AIDS patients) that permanent supportive housing increases health outcomes or decreases costs, but makes numerous recommendations to improve the state of the science. One study to watch is “Housing Prescriptions as Health Care” [108], which also takes a multi-faceted approach for medically complex families. Early results are promising, with the researchers initially concluding that changes in the housing and public sector are needed (e.g., increasing affordable housing and rental assistance) before housing can be seen as a health care intervention. This study, however, also raises the issue of the “medicalization” of a social, population issue [109]—i.e., when are these interventions best initiated at a public policy population level, versus through individual health care?
Social Isolation and Loneliness
Social isolation and loneliness are increasingly recognized as a risk factors for poor health, especially for older adults. In 2020, the NASEM published a consensus study titled Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System [110]. As the science of evidence-based interventions develops, health care should address underlying medical conditions e.g., hearing impairment, poor vision, and limited mobility that can exacerbate social isolation and loneliness. Routine medical practices such as discharge planning and care coordination should work with social services and community organizations to address individuals’ needs. As in other efforts to address social risk factors, the relationships between the health care system, CBOs and resources should be strengthened. The NASEM report also recommends that the U.S. Department of Health and Human Services should establish a central center for evidence, resources, training, and best practices on social isolation and loneliness, given the public health impact of these factors.
Inclusion of Populations in Design
The term “inclusion health” is used to describe a service, research, and policy approach for the most “marginalized and excluded populations,” for example people who have experienced homelessness, drug use, incarceration, and sex work. Luchenski and colleagues [111] review the current evidence for addressing the morbidity and inequities in these populations, who often have upstream histories of ACEs, poverty, and overall “deprivation.” Although a framework for addressing social exclusion and inequities is still being developed, Luchenski and colleagues advocate for practitioners to include these populations in designing interventions to decrease the barriers in obtaining and utilizing health and social services. Although there are effective interventions for physical and mental health illnesses as well as addiction, less is known about how to create inclusion health for the whole person that encompasses factors such as legal aid, housing, employment, and education. A preventive agenda is needed to go further upstream to address the root causes of ACEs, poverty, and the mis-aligned environment that produces and reinforces exclusion and inequities. Luchenski et al.’s article specifically discusses:
-
1.
Engagement objectives that the authors used to co-create their work with marginalized populations;
-
2.
The population’s definition of “inclusion health;”
-
3.
Their prioritized interventions (e.g., housing is number one); and
-
4.
A listing of effective interventions obtained from the systematic literature review.
This inclusion work is a tangible “nothing about us without us” (often known for its use in disability movements) [112] to addressing inequities in this complex population.
APPENDIX C - Additional Resources for SDoH, Social Risks, and HRSN
SIREN Network (Social Interventions Research and Evaluation Network)
(https://sirenetwork.ucsf.edu/)
A research network dedicated to “improve health and health equity by advancing high quality research on health care sector strategies to improve social conditions.” SIREN includes a searchable evidence and resource library as well as monthly “research round-ups” and recent “Coffee and Science” conversations.
Centers for Disease Control and Prevention (CDC) Social Determinants of Health
(https://www.cdc.gov/socialdeterminants/index.htm)
General information, CDC research on SDoH, CDC programs affecting SDoH, sources for data on SDoH, policy resources to support SDoH, tools for putting SDoH into action and CDC’s commitment to addressing racism.
Agency for Healthcare Research and Quality (AHRQ) Social Determinants of Health
(https://www.ahrq.gov/sdoh/index.html)
General information, SDoH & health systems research, SDoH & practice improvement, SDoH data and analytics, and SDoH resources.
Robert Wood Johnson Foundation Focus Areas
(https://www.rwjf.org/en/our-focus-areas/topics/social-determinants-of-health.html)
General information, work on healthy communities, County Health Rankings and Roadmaps, examples from RWJF Culture of Health Prize.
RAND Corporation
Social Determinants of Health
(https://www.rand.org/topics/social-determinants-of-health.html)
Research articles and commentaries on SDoH.
The Urban Institute
(https://www.urban.org/policy-centers/cross-center-initiatives/social-determinants-health/about)
SDoH information about the Urban Institute’s Policies for Action national research program of the Robert Wood Johnson Foundation, strategies to advance well-being in cities, and efforts to partner with and convene change-makers.
APPENDIX D - Final Form of the World Health Organization’s Commission on Social Determinants of Health Conceptual Framework
Figure A. Final form of the CSDH conceptual framework.
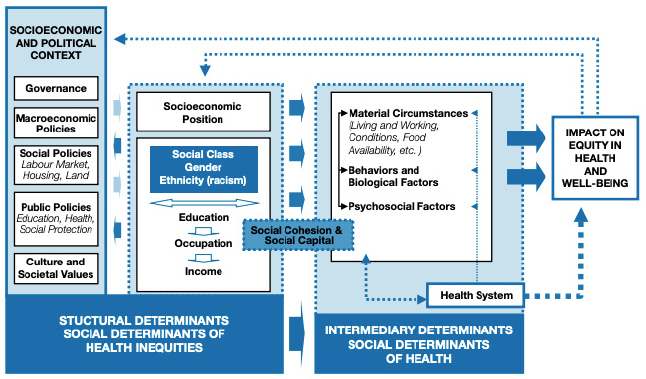
SOURCE: Solar, O., and A. Irwin. 2010. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). World Health Organization. Available at: https://www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf (accessed December 14, 2020.) Used with permission.
Acknowledgments
The author acknowledges and appreciates content contributions from John Auerbach and Alina Baciu, discussions on social risk factors and HRSN at Epic’s SDoH sub-committee of its Population Health Steering Board, editorial assistance from Amy LaFrance at HealthPartners Institute, and professional and technical assistance from Mary B. Wittenbreer and Jennifer L. Feeken at Regions Hospital Medical Library.
This paper also benefited from the thoughtful input of Jeffrey Levi, The George Washington University; Connie Hwang, Alliance of Community Health Plans; Rachel Gold, Kaiser Permanente Center for Health Research; and Kalpana Ramiah, Essential Hospitals Institute.
Funding Statement
The views expressed in this paper are those of the author and not necessarily of the author’s organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies.
Footnotes
Conflict-of-Interest Disclosures: Sanne Magnan discloses that she is a non-paid member of Epic’s Population Health Steering Board (2016-2020) and chair of its SDoH sub-committee (2018-2020)
The concept of this paper was presented at the annual American College of Physicians’ Internal Medicine meeting in Philadelphia, PA, April 2019.
References
- 1.Magnan S. NAM Perspectives. National Academy of Medicine; Washington, DC: 2017. Social Determinants of Health 101 for Health Care: Five Plus Five. Discussion Paper. [DOI] [Google Scholar]
- 2.Gottlieb LM, Wing H, Adler NE. A Systematic Review of Interventions on Patients’ Social and Economic Needs. American Journal of Preventive Medicine. 2017;53(5):719–729. doi: 10.1016/j.amepre.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Social Determinants of Health: Know What Affects Health. 2020. [February 20, 2021]. https://www.cdc.gov/socialdeterminants/index.htm. [Google Scholar]
- 4.Alderwick H, Gottlieb LM. The Milbank Quarterly. June (Volume 97) 2019. [February 25, 2021]. Meanings and Misunderstandings: A Social Determinants of Health Lexicon for Health Care Systems. https://www.milbank.org/quarterly/articles/meanings-and-misunderstandings-a-social-determinants-of-health-lexicon-for-health-care-systems/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Medicare and Medicaid Services. The Accountable Health Communities Health-Related Social Needs Screening Tool. 2020. [February 20, 2021]. https://innovation.cms.gov/Files/worksheets/ahcm-screen-ingtool.pdf. [Google Scholar]
- 6.Green K, Zook M. Health Affairs Blog. 2019. When Talking About Social Determinants, Precision Matters. [DOI] [Google Scholar]
- 7.Minnesota Department of Health. Principles of Authentic Community Engagement. 2018. [March 20, 2021]. https://www.health.state.mn.us/communities/practice/resources/phqitoolbox/docs/AuthenticPrinciplesCommEng.pdf. [Google Scholar]
- 8.Silverstein M, Hsu HE, Bell A. Addressing Social Determinants to Improve Population Health: The Balance Between Clinical Care and Public Health. JAMA. 2019;322(24):2379–2380. doi: 10.1001/jama.2019.18055. [DOI] [PubMed] [Google Scholar]
- 9.Gurewich D, Garg A, Kressin NR. Addressing Social Determinants of Health Within Healthcare Delivery Systems: A Framework to Ground and Inform Health Outcomes. Journal of General Internal Medicine. 2020;35:1571–1575. doi: 10.1007/s11606-020-05720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coughlin SS, Mann P, Vernon M, Young L, Ayyala D, Sams R, Hatzigeorgiou C. A logic framework for evaluating social determinants of health interventions in primary care. Journal of Hospital Management and Health Policy. 2019;3:23. doi: 10.21037/jhmhp.2019.09.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Auerbach J. Social Determinants of Health Can Only Be Addressed by a Multisector Spectrum of Activities. Journal of Public Health Management and Practice. 2019;25(6):525–528. doi: 10.1097/PHH.0000000000001088. [DOI] [PubMed] [Google Scholar]
- 12.Jacobson DM, Teutsch S. An Environmental Scan of Integrated Approaches for Defining and Measuring Total Population Health by the Clinical Care System, the Government Public Health System and Stakeholder Organizations. [February 20, 2021]. n.d. https://www.improvingpopulationhealth.org/PopHealthPhaseIICommissionedPaper.pdf. [Google Scholar]
- 13.Auerbach J. 2018. [March 20, 2021]. Maryland Population Health Forum Presentation. https://pophealth.health.maryland.gov/Documents/9.%20Lunch%20Session_John%20Auerbach%20Slides.pdf. [Google Scholar]
- 14.National Academies of Sciences, Engineering, and Medicine. Communities in Action, Pathways to Health Equity: Anchor Institutions. 2018. [March 20, 2021]. https://www.nap.edu/resource/24624/anchor-institutions/ [Google Scholar]
- 15.Saha S, Loehrer S, Cleary-Fishman M, Johnson K, Chenard R, Gunderson G, Goldberg R, Little J, Resnick J, Cutts T, Barnett K. Pathways to Population Health: An Invitation to Health Care Change Agents. 2017. [February 20, 2021]. http://www.ihi.org/Topics/Population-Health/Documents/Pathway-stoPopulationHealth_Framework.pdf. [Google Scholar]
- 16.National Academies of Sciences, Engineering, and Medicine. Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. Washington, DC: The National Academies Press; 2019. [DOI] [PubMed] [Google Scholar]
- 17.Massachusetts Department of Public Health Bureau of Substance Abuse Services. SBIRT: A Step-by-Step Guide. 2012. [February 20, 2021]. https://www.masbirt.org/sites/www.masbirt.org/files/documents/toolkit.pdf. [Google Scholar]
- 18.Hargraves D, White C, Frederick R, Cinibulk M, Peters M, Young A, Elder N. Implementing SBIRT (Screening, Brief Intervention and Referral to Treatment) in Primary Care: Lessons Learned from a Multi-practice Evaluation Portfolio. Public Health Reviews. 2017;38:31. doi: 10.1186/s40985-017-0077-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. Pricing Strategies for Alcohol Products. 2020. [February 20, 2021]. https://www.cdc.gov/policy/hst/hi5/alcoholpricing/index.html. [Google Scholar]
- 20.Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, Cook JT, Ettinger de Cuba SA, Casey PH, Chilton M, Cutts DB, Meyers AF, Frank DA. Development and Validity of a 2-Item Screen to Identify Families at Risk for Food Insecurity. [March 20, 2021];Pediatrics. 2010 126(1):e26–e32. doi: 10.1542/peds.2009-3146. https://pediatrics.aappublications.org/content/126/1/e26. [DOI] [PubMed] [Google Scholar]
- 21.Hager KA, Lofthus DK, Balan B, Cutts D. Electronic Medical Record–Based Referrals to Community Nutritional Assistance for Food-Insecure Patients. Annals of Family Medicine. 2020;18(3):278. doi: 10.1370/afm.2530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hartline-Grafton H, Hassink SG. Food Insecurity and Health: Practices and Policies to Address Food Insecurity among Children. Academic Pediatrics. 2020 doi: 10.1016/j.acap.2020.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.American Association of Family Physicians. Three things to consider before you start screening for social determinants of health. 2019. [February 20, 2021]. https://www.aafp.org/journals/fpm/blogs/inpractice/entry/social_needs_screening.html. [Google Scholar]
- 24.Byhoff E, Taylor 2019 LA. Massachusetts Community-Based Organization Perspectives on Medicaid Redesign. [March 20, 2021];American Journal Preventive Medicine. 57(6S1):S74–S81. doi: 10.1016/j.amepre.2019.07.017. https://www.ajpmonline.org/article/S07493797(19)30325-3/fulltext. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Billioux A, Verlander K, Anthony S, Alley D. NAM Perspectives. National Academy of Medicine; Washington, DC: 2017. Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. Discussion Paper. [DOI] [Google Scholar]
- 26.Tung EL, De Marchis EH, Gottlieb LM, Lindau ST, Pantell MS. Journal of General Internal Medicine. 2021. Patient Experiences with Screening and Assistance for Social Isolation in Primary Care Settings. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Michener L, Castrucci BC, Bradley DW, Hunter EL, Thomas CW, Patterson C, Corcoran E. The Practical Playbook II: Building Multisector Partnerships That Work. Duke University Medical Center; Durham, NC: 2019. [Google Scholar]
- 28.O’Gurek DT, Henke C. A Practical Approach to Screening for Social Determinants of Health. [February 20, 2021];Family Practice Management. 2018 25(3):7–12. https://pubmed.ncbi.nlm.nih.gov/29989777/ [PubMed] [Google Scholar]
- 29.Moen M, Storr C, German D, Friedmann E, Johantgen M. A Review of Tools to Screen for Social Determinants of Health in the United States: A Practice Brief. Population Health Management. 2020;23(6):422–429. doi: 10.1089/pop.2019.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Reviews. 2018;39:19. doi: 10.1186/s40985-018-0094-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Figueroa JF, Frakt AB, Jha AK. Addressing Social Determinants of Health: Time for a Polysocial Risk Score. JAMA. 2020;323(16):1553–1554. doi: 10.1001/jama.2020.2436. [DOI] [PubMed] [Google Scholar]
- 32.Davidson KW, McGinn T. Screening for Social Determinants of Health: The Known and Unknown. JAMA. 2019;322(11):1037–1038. doi: 10.1001/jama.2019.10915. [DOI] [PubMed] [Google Scholar]
- 33.Schickedanz A, Hamity C, Rogers A, Sharp AL, Jackson A. Clinician Experiences and Attitudes Regarding Screening for Social Determinants of Health in a Large Integrated Health System. Medical Care. 2019;57(6, 2):S197–S201. doi: 10.1097/MLR.0000000000001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kung A, Cheung T, Knox M, Willard-Grace R, Halpern J, Olayiwola JN, Gottlieb L. Capacity to Address Social Needs Affects Primary Care Clinician Burnout. Annals of Family Medicine. 2019;17(6):487–494. doi: 10.1370/afm.2470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Marchis EH, Hessler D, Fichtenberg C, Adler N, Byhoff E, Cohen AJ, Doran KM, Ettinger de Cuba S, Fleegler EW, Lewis CC, Lindau ST, Tung EL, Huebschmann AG, Prather AA, Raven M, Gavin N, Jepson S, Johnson W, Ochoa E, Jr, Olson AL, Sandel M, Sheward RS, Gottlieb LM. Part I: A Quantitative Study of Social Risk Screening Acceptability in Patients and Caregivers. [March 20, 2021];American Journal of Preventive Medicine. 2019 57(6S1):S25–S37. doi: 10.1016/j.amepre.2019.07.010. https://www.sciencedirect.com/science/article/pii/S0749379719303186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sokol R, Austin A, Chandler C, Byrum E, Bousquette J, Lancaster C, Doss G, Dotson A, Urbaeva V, Singichetti B, Brevard K, Wright ST, Lanier P, Shanahan M. Screening Children for Social Determinants of Health: A Systematic Review. Pediatrics. 2019;144(4):e20191622. doi: 10.1542/peds.2019-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garg A, Sheldrick RC, Dworkin PH. The Inherent Fallibility of Validated Screening Tools for Social Determinants of Health. Academic Pediatrics. 2018;18(2):123–124. doi: 10.1016/j.acap.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 38.Hassan A, Scherer EA, Pikcilingis A, Krull E, McNickles L, Marmon G, Woods ER, Fleegler EW. Improving Social Determinants of Health Effectiveness of a Web-Based Intervention. [March 20, 2021];American Journal of Preventive Medicine. 2015 49(6):822–831. doi: 10.1016/j.amepre.2015.04.023. https://pubmed.ncbi.nlm.nih.gov/26215831/ [DOI] [PubMed] [Google Scholar]
- 39.Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics. 2015;135(2):e296–e304. doi: 10.1542/peds.2014-2888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schickedanz A, Gottlieb L, Szilagyi P. Will Social Determinants Reshape Pediatrics? Upstream Clinical Prevention Efforts Past, Present, and Future. Academic Pediatrics. 2019;19(8):858–859. doi: 10.1016/j.acap.2019.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gottlieb LM, Francis DE, Beck AF. Uses and Misuses of Patient- and Neighborhood-level Social Determinants of Health Data. The Permanente Journal. 2018;22:18–078. doi: 10.7812/TPP/18-078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De Marchis EH, Hessler D, Fichtenberg C, Fleegler EW, Huebschmann AG, Clark CR, Cohen AJ, Byhoff E, Ommerborn MJ, Adler N, Gottlieb LM. Assessment of Social Risk Factors and Interest in Receiving Health Care-Based Social Assistance Among Adult Patients and Adult Caregivers of Pediatric Patients. JAMA Network Open. 2020;3(10):e2021201. doi: 10.1001/jamanetworkopen.2020.21201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cullen D, Attridge M, Fein JA. Food for Thought: A Qualitative Evaluation of Caregiver Preferences for Food Insecurity Screening and Resource Referral. [March 20, 2021];Academic Pediatrics. 2020 20(8):1157–1162. doi: 10.1016/j.acap.2020.04.006. https://pubmed.ncbi.nlm.nih.gov/32302758/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Medicare and Medicaid Solutions. Accountable Health Communities Model. [March 20, 2021]. n.d. https://innovation.cms.gov/media/document/ahc-fact-sheet-2020-prelim-findings. [Google Scholar]
- 45.Gold R, Bunce A, Cowburn S, Dambrun K, Dearing M, Middendorf M, Mossman N, Hollombe C, Mahr P, Melgar G, Davis J, Gottlieb L, Cottrell E. Adoption of Social Determinants of Health EHR Tools by Community Health Centers. Annals of Family Medicine. 2018;16(5):399–407. doi: 10.1370/afm.2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.De Marchis EH, Torres JM, Benesch T, Fichtenberg C, Allen IE, Whitaker EM, Gottlieb LM. Interventions Addressing Food Insecurity in Health Care Settings: A Systematic Review. Annals of Family Medicine. 2019;17(5):436–447. doi: 10.1370/afm.2412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Obermeyer J, Haley A. Personal Communication. Jan 25, 2021. [Google Scholar]
- 48.Gruβ I, Bunce A, Davis J, Dambrun K, Cottrell E, Gold R. Initiating and Implementing Social Determinants of Health Data Collection in Community Health Centers. Population Health Management. 2021;24(1) doi: 10.1089/pop.2019.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jones CM, Merrick MT, Houry DE. Identifying and Preventing Adverse Childhood Experiences: Implications for Clinical Practice. JAMA. 2019;323(1):25–26. doi: 10.1001/jama.2019.18499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of Screening for Food Insecurity, Housing Instability, Utility Needs, Transportation Needs, and Interpersonal Violence by US Physician Practices and Hospitals. JAMA Network Open. 2019;2(9):e1911514. doi: 10.1001/jamanetworkopen.2019.11514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gold R, Gottlieb L. National Data on Social Risk Screening Underscore the Need for Implementation Research. JAMA Network Open. 2019;2(9):e1911513. doi: 10.1001/jamanetworkopen.2019.11513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Berwick DM. Developing and testing changes in delivery of care. Annals of Internal Medicine. 1998;128(8):651–656. doi: 10.7326/00034819-128-8-199804150-00009. [DOI] [PubMed] [Google Scholar]
- 53.The ASCEND Project. Guide to Social Determinants of Health Screening and Referral-Making Using the EHR. [March 20, 2021]. n.d. https://cdr.lib.unc.edu/downloads/5m60qv06g?locale=en. [Google Scholar]
- 54.SIREN. Home. [March 20, 2021]. n.d. https://siren.network/ [Google Scholar]
- 55.Islam N, Rogers ES, Schoenthaler A, Thorpe LE, Shelley D. A Cross-Cutting Workforce Solution for Implementing Community–Clinical Linkage Models. American Journal of Public Health. 2020;110(S2):S191–S193. doi: 10.2105/AJPH.2020.305692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Robertson L, Chernof BA. Health Affairs Blog. 2020. [February 22, 2021]. Addressing Social Determinants: Scaling Up Partnerships with Community-Based Organization Networks. https://www.healthaffairs.org/do/10.1377/hblog20200221.672385/full/ [Google Scholar]
- 57.Mann C, Dworkowitz A. SIREN. 2020. [January 31, 2021]. Data Sharing and the Law: Overcoming Health Care Sector Barriers to Sharing Data on Social Determinants. https://www.youtube.com/watch?v=ebeMb2xOEBA&feature=youtu.be. [Google Scholar]
- 58.Centers for Disease Control and Prevention. Health Impact in 5 Years. 2018. [February 20, 2021]. https://www.cdc.gov/policy/hst/hi5/index.html. [Google Scholar]
- 59.Trust for America’s Health. Promoting Health and Cost Control in States: How States Can Improve Community Health & Well-being Through Policy Change. 2019. [March 20, 2021]. https://www.tfah.org/wp-content/uploads/2019/02/2019-PHACCS-Report_FINAL.pdf. [Google Scholar]
- 60.Cartier Y, Fichtenberg C, Gottlieb L. Community Resource Referral Platforms: A Guide for Health Care Organizations. San Francisco, CA: SIREN; 2019. [December 14, 2020]. https://sirenetwork-ucsf.edu/tools-resources/resources/community-resource-referral-platforms-a-guide-forhealth-care-organizations. [Google Scholar]
- 61.CommunityHELP. Home. [March 20, 2021]. n.d. https://www.communityhelp.net/ [Google Scholar]
- 62.Center for Health Care Strategies, Inc. Partnership Assessment Tool for Health. 2017. [February 20, 2021]. https://www.chcs.org/resource/partnershipassessment-tool-health/ [Google Scholar]
- 63.Berkowitz SA, Kangovi S. Milbank Quarterly Opinion. 2020. Health Care’s Social Movement Should Not Leave Science Behind. [DOI] [Google Scholar]
- 64.Horwitz LI, Kuznetsova M, Jones SA. Creating a Learning Health System through Rapid-Cycle, Randomized Testing. New England Journal of Medicine. 2019;381(12):1175–1179. doi: 10.1056/NEJMsb1900856. https://www.nejm.org/doi/10.1056/NEJMsb1900856. [DOI] [PubMed] [Google Scholar]
- 65.Institute of Medicine. Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press; 2013. [DOI] [PubMed] [Google Scholar]
- 65.Horwitz L. Personal communication. Jan 29, 2021. [Google Scholar]
- 67.Institute for Healthcare Improvement. 6 Tips for Measuring Health Equity at Your Organization. 2017. [February 20, 2021]. http://www.ihi.org/communities/blogs/6-tips-for-measuring-health-equity-at-your-organization. [Google Scholar]
- 68.Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J. IHI White Paper. Cambridge, Massachusetts: Institute for Healthcare Improvement; 2016. [February 28, 2021]. Achieving Health Equity: A Guide for Health Care Organizations. http://www.ihi.org/resources/Pages/IHIWhitePapers/Achieving-Health-Equity.aspx. [Google Scholar]
- 69.Sivashanker K, Duong T, Resnick A, Eappen S. NEJM Catalyst. 2020. Health Care Equity: From Fragmentation to Transformation. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0414. [Google Scholar]
- 70.Sivashanker K, Mohta NS. NEJM Catalyst. 2020. Dismantling Racism and Inequity in Health Care: The Critical Interplay Between Equity, Quality and Safety. https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0598. [Google Scholar]
- 71.Patterson I. Personal communication. Feb 4, 2021. [Google Scholar]
- 72.Levi J, Fukuzawa DD, Sim S, Simpson P, Standish M, Wang Kong C, Weiss AF. Health Affairs Blog. 2018. Developing a Common Framework for Assessing Accountable Communities for Health. https://www.healthaffairs.org/do/10.1377/hblog20181023.892541/full/ [Google Scholar]
- 73.Beck AF, Sandel MT, Ryan PH, Kahn RS. Mapping Neighborhood Health Geomarkers to Clinical Care Decisions to Promote Equity in Child Health. Health Affairs (Millwood) 2017;36(6):999–1005. doi: 10.1377/hlthaff.2016.1425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bazemore AW, Cottrell EK, Gold R, Hughes LS, Phillips RL, Angier H, Burdick TE, Carrozza MA, DeVoe JE. “Community vital signs”: incorporating geocoded social determinants into electronic records to promote patient and population health. Journal of the American Medical Informatics Association. 2016;23(2):407–412. doi: 10.1093/jamia/ocv088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cottrell EK, Gold R. Personal communication. Jan 9, 2020. [Google Scholar]
- 76.Cottrell EK, Hendricks M, Dambrun K, Cowburn S, Pantell M, Gold R, Gottlieb LM. Comparison of Community-Level and Patient-Level Social Risk Data in a Network of Community Health Centers. JAMA Network Open. 2020;3(10):e2016852. doi: 10.1001/jamanetworkopen.2020.16852. PMID: 33119102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cantor J, Cohen L, Mikkelsen L, Paňares R, Srikantharajah J, Valdovinos E. Community-Centered Health Homes: Bridging the gap between health services and community prevention. 2011. [February 20, 2021]. https://www.preventioninstitute.org/publications/community-centered-health-homes-bridging-the-gap-between-health-services-and-community-prevention. [Google Scholar]
- 78.Centers for Medicare and Medicaid Services. CHART Model. 2021. [March 20, 2021]. https://innovation.cms.gov/innovation-models/chart-model. [Google Scholar]
- 79.Centers for Medicare and Medicaid Services. Geographic Direct Contracting Model. 2021. [March 20, 2021]. https://innovation.cms.gov/innovation-models/geographic-direct-contracting-model. [Google Scholar]
- 80.Murray GF, Rodriguez HP, Lewis VA. Upstream with a Small Paddle: How ACOs Are Working Against the Current to Meet Patients’ Social Needs. Health Affairs (Millwood) 2020;39(2):199–206. doi: 10.1377/hlthaff.2019.01266. https://www.healthaffairs.org/doi/10.1377/hlthaff.2019.01266. [DOI] [PubMed] [Google Scholar]
- 81.Beck AF, Cohen AJ, Colvin JD, Fichtenberg CM, Fleegler EW, Garg A, Gottlieb LM, Pantell MS, Sandel MT, Schickedanz A, Kahn RS. Perspectives from the Society for Pediatric Research: interventions targeting social needs in pediatric clinical care. Pediatric Research. 2018;84:10–21. doi: 10.1038/s41390-018-0012-1. [DOI] [PubMed] [Google Scholar]
- 82.Fichtenberg CM, Alley DE, Mistry KB. Improving Social Needs Intervention Research: Key Questions for Advancing the Field. American Journal of Preventive Medicine. 2019;57(6S1):S47–S54. doi: 10.1016/j.amepre.2019.07.018. [DOI] [PubMed] [Google Scholar]
- 83.National Academies of Sciences, Engineering, and Medicine. Investing in Interventions That Address Non-medical, Health-related Social Needs: Proceedings of a Workshop. Washington, DC: The National Academies Press; 2019. [DOI] [PubMed] [Google Scholar]
- 84.National Academies of Science, Engineering and Medicine. Models for Population Health Improvement by Health Care Systems and Partners - Tensions and Promise on the Path Upstream: Proceedings of a Workshop. Washington, DC: The National Academies Press In press; 2020. [PubMed] [Google Scholar]
- 85.County Health Rankings & Roadmaps. Take Action to Improve Health. 2021. [February 20, 2021]. https://www.countyhealthrankings.org/take-action-to-improve-health. [Google Scholar]
- 86.Auerbach J. The Three Buckets of Prevention. Journal of Public Health Management and Practice. 2016;22(3):215–218. doi: 10.1097/PHH.0000000000000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Maciosek MV, LaFrance AB, Dehmer SP, McGree DA, Flottemesch TJ, Xu Z, Solberg LI. Updated Priorities Among Effective Clinical Preventive Services. Annals of Family Medicine. 2017;15(1):14–22. doi: 10.1370/afm.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jha AK. Population Health Management: Saving Lives and Saving Money? JAMA. 2019;322(5):390–391. doi: 10.1001/jama.2019.10568. [DOI] [PubMed] [Google Scholar]
- 89.The Commonwealth Fund. Welcome to the Return on Investment (ROI) Calculator for Partnerships to Address the Social Determinants of Health. 2020. [February 20, 2021]. https://www.commonwealthfund.org/roi-calculator. [Google Scholar]
- 90.Pinto AD, Hassen N, Craig-Neil A. Employment Interventions in Health Settings: A Systematic Review and Synthesis. Annals of Family Medicine. 2018;16(5):447–460. doi: 10.1370/afm.2286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Beck AF, Tschudy MM, Coker TR, Mistry KB, Cox JE, Gitterman BA, Chamberlain LJ, Grace AM, Hole MK, Klass PE, Lobach KS, Ma CT, Navsaria D, Northrip KD, Sadof MD, Shah AN, Fierman AH. Determinants of Health and Pediatric Primary Care Practices. Pediatrics. 2016;137(3):e20153673. doi: 10.1542/peds.2015-3673. https://pubmed.ncbi.nlm.nih.gov/26933205/ [DOI] [PubMed] [Google Scholar]
- 92.Fierman AH, Beck AF, Chung EK, Tschudy MM, Coker TR, Mistry KB, Siegel B, Chamberlain LJ, Conroy K, Federico SG, Flanagan PJ, Garg A, Gitterman BA, Grace AM, Gross RS, Hole MK, Klass P, Kraft C, Kuo A, Lewis G, Lobach KS, Long D, Ma CT, Messito M, Navsaria D, Northrip KR, Osman C, Sadof MD, Schickedanz AB, Cox J. Redesigning Health Care Practices to Address Childhood Poverty. Academic Pediatrics. 2016;16(3):S136–S146. doi: 10.1016/j.acap.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 93.Aery A, Rucchetto A, Singer A, Halas G, Bloch G, Goel R, Raza D, Upshur REG, Bellaire J, Katz A, Pinto AD. Implementation and impact of an online tool used in primary care to improve access to financial benefits for patients: a study protocol. BMJ Open. 2017;7(10):e015947. doi: 10.1136/bmjopen-2017-015947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bell ON, Hole MK, Johnson K, Marcil LE, Solomon BS, Schickedanz A. Medical-Financial Partnerships: Cross-Sector Collaborations Between Medical and Financial Services to Improve Health. Academic Pediatrics. 2020;20(2):166–174. doi: 10.1016/j.acap.2019.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.County Health Rankings & Roadmaps. Medical-legal partnerships. 2021. [February 20, 2021]. https://www.countyhealthrankings.org/take-action-to-improve-health/what-works-for-health/strategies/medical-legal-partnerships. [Google Scholar]
- 96.Seligman HK, Smith M, Rosenmoss S, Marshall MB, Waxman E. Comprehensive Diabetes Self-Management Support from Food Banks: A Randomized Controlled Trial. American Journal of Public Health. 2018;108(9):1227–1234. doi: 10.2105/AJPH.2018.304528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Berkowitz SA, Terranova J, Randall L, Cranston K, Waters DB, Hsu J. Association Between Receipt of a Medically Tailored Meal Program and Health Care Use. JAMA Internal Medicine. 2019;179(6):786–793. doi: 10.1001/jamainternmed.2019.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kelly C, Maytag A, Allen M, Ross C. Journal of Public Health Management and Practice. 2020. Results of an Initiative Supporting Community-Based Organizations and Health Care Clinics to Assist Individuals With Enrolling in SNAP. [DOI] [PubMed] [Google Scholar]
- 99.Regenstein M, Trott J, Williamson A, Theiss J. Addressing Social Determinants Of Health Through Medical-Legal Partnerships. Health Affairs (Millwood) 2018;37(3):378–385. doi: 10.1377/hlthaff.2017.1264. https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.1264. [DOI] [PubMed] [Google Scholar]
- 100.Solomon EM, Wing H, Steiner JF, Gottlieb LM. Impact of transportation interventions on health care outcomes: A systematic review. Medical Care. 2020;58(4):384–391. doi: 10.1097/MLR.0000000000001292. [DOI] [PubMed] [Google Scholar]
- 101.Starbird LE, DiMaina C, Sun C, Han H. A Systematic Review of Interventions to Minimize Transportation Barriers Among People with Chronic Diseases. Journal of Community Health. 2019;44:400–411. doi: 10.1007/s10900-0180572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Powers B, Rinefort S, Jain SH. Health Affairs Blog. 2018. [May 10, 2021]. Shifting Non-Emergency Medical Transportation to Lyft Improves Patient Experience and Lowers Costs. https://www.healthaffairs.org/do/10.1377/hblog20180907.685440/full/ [Google Scholar]
- 103.Kangovi S, Mitra N, Grande D, Huo H, Smith RA, Long JA. Community Health Worker Support for Disadvantaged Patients with Multiple Chronic Diseases: A Randomized Clinical Trial. American Journal of Public Health. 2017;107(10):1660–1667. doi: 10.2105/AJPH.2017.303985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kangovi S, Mitra N, Norton L, Harte R, Zhao X, Carter T, Grande D, Long JA. Effect of Community Health Worker Support on Clinical Outcomes of Low-Income Patients Across Primary Care Facilities: A Randomized Clinical Trial. JAMA Internal Medicine. 2018;178(12):1635–1643. doi: 10.1001/jamainternmed.2018.4630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kangovi S, Mitra N, Grande D, Long JA, Asch DA. Evidence-Based Community Health Worker Program Addresses Unmet Social Needs and Generates Positive Return on Investment. Health Affairs (Millwood) 2020;39(2):207–213. doi: 10.1377/hlthaff.2019.00981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a Housing and Case Management Program on Emergency Department Visits and Hospitalizations Among Chronically Ill Homeless Adults: A Randomized Trial. JAMA. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 107.National Academies of Sciences, Engineering, and Medicine. Permanent Supportive Housing: Evaluating the Evidence for Improving Health Outcomes Among People Experiencing Chronic Homelessness. Washington, DC: The National Academies Press; 2018. [DOI] [PubMed] [Google Scholar]
- 108.Bovell-Ammon A, Mansilla C, Poblacion A, Rateau L, Heeren T, Cook JT, Zhang T, de Cuba SE, Sandel MT. Housing Intervention for Medically Complex Families Associated with Improved Family Health: Pilot Randomized Trial. Health Affairs (Millwood) 2020;39(4):613–621. doi: 10.1377/hlthaff.2019.01569. [DOI] [PubMed] [Google Scholar]
- 109.Lantz PM. The Medicalization of Population Health: Who Will Stay Upstream? The Milbank Quarterly. 2018;97(1):36–39. doi: 10.1111/14680009.12363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.National Academies of Sciences, Engineering, and Medicine. Social isolation and loneliness in older adults: Opportunities for the health care system. Washington, DC: The National Academies Press; 2020. [DOI] [PubMed] [Google Scholar]
- 111.Luchenski S, Maguire N, Aldridge RW, Hayward A, Story A, Perri P, Withers J, Clint S, Fitzpatrick S, Hewett N. What works in inclusion health: overview of effective interventions for marginalised and excluded populations. Lancet. 2018;391(10117):266–280. doi: 10.1016/S0140-6736(17)31959-1. [DOI] [PubMed] [Google Scholar]
- 112.YNPN Twin Cities. “Nothing About Us Without Us” … including the use of this slogan. [February 20, 2021]. n.d. http://www.ynpntwincities.org/_nothing_about_us_without_us_including_the_use_of_this_slogan. [Google Scholar]
- 113.Berwick DM, Nolan TW. Physicians as Leaders in Improving Health Care: A New Series in Annals of Internal Medicine. Annals of Internal Medicine. 1998;128(4):289–292. doi: 10.7326/00034819-128-4-199802150-00008. [DOI] [PubMed] [Google Scholar]
- 114.Beck AF, Anderson KL, Rich K, Taylor SC, Iyer SB, Kotagal UR, Kahn RS. Cooling the Hot Spots Where Child Hospitalization Rates Are High: A Neighborhood Approach to Population Health. Health Affairs (Millwood) 2019;38(9):1433–1441. doi: 10.1377/hlthaff.2018.05496. [DOI] [PubMed] [Google Scholar]
- 115.Lawton R, Whitehead M, Henize A, Fink E, Salamon M, Kahn R, Beck AF, Klein M. Medical-Legal-Psychology Partnerships - Innovation in Addressing Social Determinants of Health in Pediatric Primary Care. Academic Pediatrics. 2020;20(7):902–904. doi: 10.1016/j.acap.2020.06.011. [DOI] [PubMed] [Google Scholar]
- 116.Drabo EF, Eckel G, Ross SL, Brozic M, Carlton CG, Warren TY, Kleb G, Laird A, Pollack Porter KM, Pollack CE. A Social-Return-On-Investment Analysis of Bon Secours Hospital’s ‘Housing For Health’ Affordable Housing Program. Health Affairs (Millwood) 2021;40(3):513–520. doi: 10.1377/hlthaff.2020.00998. https://doi. org/10.1377/hlthaff.2020.00998. [DOI] [PubMed] [Google Scholar]
- 117.Brewster AL, Fraze TK, Gottlieb LM, Frehn J, Murray GF, Lewis VA. The Role of Value-Based Payment in Promoting Innovation to Address Social Risks: A Cross-Sectional Study of Social Risk Screening by US Physicians. Milbank Quarterly. 2020;98(4):1114–1133. doi: 10.1111/14680009.12480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Pantell MS, Hessler D, Long D, Alqassari M, Schudel C, Laves E, Velazquez DE, Amaya A, Sweeney P, Burns A, Harrison FL, Adler NE, Gottlieb LM. Effects of In-Person Navigation to Address Family Social Needs on Child Health Care Utilization – A Randomized Clinical Trial. JAMA Ne-work Open. 2020;3(6):e206445. doi: 10.1001/jamanetworkopen.2020.6445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Messmer E, Brochier A, Joseph M, Tripodis Y, Garg A. Impact of an On-Site Versus Remote Patient Navigator on Pediatricians’ Referrals and Families’ Receipt of Resources for Unmet Social Needs. Journal of Primary Care & Community Health. 2020;11:1–6. doi: 10.1177/2150132720924252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gottlieb LM, Hessler D, Long D, Laves E, Burns AR, Amaya A, Sweeney P, Schudel C, Adler NE. Effects of social needs screening and in-person service navigation on child health: A randomized clinical trial. Journal of the American Medical Association Pediatrics. 2016;170(11):e162521. doi: 10.1001/jamapediatrics.2016.2521. [DOI] [PubMed] [Google Scholar]
- 121.Gottlieb LM, Adler NE, Wing H, Velazquez D, Keeton V, Romero A, Hernandez M, Vera AM, Caceres EU, Arevalo C, Herrera P, Suarez MB, Hessler D. Effects of In-Person Assistance vs Personalized Written Resources about Social Services on Household Social Risks and Child and Caregiver Health – A Randomized Clinical Trial. JAMA Network Open. 2020;3(3):e200701. doi: 10.1001/jamanetworkopen.2020.0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Dalembert G, Fiks AG, O’Neill G, Rosin R, Jenssen BP. Impacting Poverty with Medical Financial Partnerships Focused on Tax Incentives. NEJM Catalyst Innovations in Care Delivery. 2021;2(4) doi: 10.1056/CAT.20.0594. [DOI] [Google Scholar]
- 123.RTI International. Accountable Health Communities (AHC) Model Evaluation – First Evaluation Report. 2020. [May 26, 2021]. https://innovation.cms.gov/data-and-reports/2020/ahc-first-eval-rpt. [Google Scholar]


