Abstract
Background
Kinesio Taping (KT) is one of the conservative treatments proposed for rotator cuff disease. KT is an elastic, adhesive, latex‐free taping made from cotton, without active pharmacological agents. Clinicians have adopted it in the rehabilitation treatment of painful conditions, however, there is no firm evidence on its benefits.
Objectives
To determine the benefits and harms of KT in adults with rotator cuff disease.
Search methods
We searched the Cochrane Library, MEDLINE, Embase, PEDro, CINAHL, Clinicaltrials.gov and WHO ICRTP registry to July 27 2020, unrestricted by date and language.
Selection criteria
We included randomised and quasi‐randomised controlled trials (RCTs) including adults with rotator cuff disease. Major outcomes were overall pain, function, pain on motion, active range of motion, global assessment of treatment success, quality of life, and adverse events.
Data collection and analysis
We used standard methodologic procedures expected by Cochrane.
Main results
We included 23 trials with 1054 participants. Nine studies (312 participants) assessed the effectiveness of KT versus sham therapy and fourteen studies (742 participants) assessed the effectiveness of KT versus conservative treatment. Most participants were aged between 18 and 50 years. Females comprised 52% of the sample. For the meta‐analysis, we considered the last available measurement within 30 days from the end of the intervention.
All trials were at risk of performance, selection, reporting, attrition, and other biases.
Comparison with sham taping
Due to very low‐certainty evidence, we are uncertain whether KT improves overall pain, function, pain on motion and active range of motion compared with sham taping.
Mean overall pain (0 to 10 scale, 0 no pain) was 2.96 points with sham taping and 3.03 points with KT (3 RCTs,106 participants), with an absolute difference of 0.7% worse, (95% CI 7.7% better to 9% worse) and a relative difference of 2% worse (95% CI 21% better to 24% worse) at four weeks. Mean function (0 to 100 scale, 0 better function) was 47.1 points with sham taping and 39.05 points with KT (6 RCTs, 214 participants), with an absolute improvement of 8% (95% CI 21% better to 5% worse)and a relative improvement of 15% (95% CI 40% better to 9% worse) at four weeks. Mean pain on motion (0 to 10 scale, 0 no pain) was 4.39 points with sham taping and 2.91 points with KT even though not clinically important (4 RCTs, 153 participants), with an absolute improvement of 14.8% (95% CI 22.5% better to 7.1% better) and a relative improvement of 30% (95% CI 45% better to 14% better) at four weeks. Mean active range of motion (shoulder abduction) without pain was 174.2 degrees with sham taping and 184.43 degrees with KT (2 RCTs, 68 participants), with an absolute improvement of 5.7% (95% CI 8.9% worse to 20.3% better) and a relative improvement of 6% (95% CI 10% worse to 22% better) at two weeks.
No studies reported global assessment of treatment success. Quality of life was reported by one study but data were disaggregated in subscales. No reliable estimates for adverse events (4 studies; very low‐certainty) could be provided due to the heterogeneous description of events in the sample.
Comparison with conservative treatments
Due to very low‐certainty evidence, we are uncertain if KT improves overall pain, function, pain on motion and active range of motion compared with conservative treatments. However, KT may improve quality of life (low certainty of evidence).
Mean overall pain (0 to 10 scale, 0 no pain) was 0.9 points with conservative treatment and 0.46 points with KT (5 RCTs, 266 participants), with an absolute improvement of 4.4% (95% CI 13% better to 4.6% worse) and a relative improvement of 15% (95% CI 46% better to 16% worse) at six weeks. Mean function (0 to 100 scale, 0 better function) was 46.6 points with conservative treatment and 33.47 points with KT (14 RCTs, 499 participants), with an absolute improvement of 13% (95% CI 24% better to 2% better) and a relative improvement of 18% (95% CI 32% better to 3% better) at four weeks. Mean pain on motion (0 to 10 scale, 0 no pain) was 4 points with conservative treatment and 3.94 points with KT (6 RCTs, 225 participants), with an absolute improvement of 0.6% (95% CI 7% better to 8% worse) and a relative improvement of 1% (95% CI 12% better to 10% worse) at four weeks. Mean active range of motion (shoulder abduction) without pain was 156.6 degrees with conservative treatment and 159.64 degrees with KT (3 RCTs, 143 participants), with an absolute improvement of 3% (95% CI 11% worse to 17 % better) and a relative improvement of 3% (95% CI 9% worse to 14% better) at six weeks.
Mean of quality of life (0 to 100, 100 better quality of life) was 37.94 points with conservative treatment and 56.64 points with KT (1 RCTs, 30 participants), with an absolute improvement of 18.7% (95% CI 14.48% better to 22.92% better) and a relative improvement of 53% (95% CI 41% better to 65% better) at four weeks.
No studies were found for global assessment of treatment success. No reliable estimates for adverse events (7 studies, very low certainty of evidence) could be provided due to the heterogeneous description of events in the whole sample.
Authors' conclusions
Kinesio taping for rotator cuff disease has uncertain effects in terms of self‐reported pain, function, pain on motion and active range of motion when compared to sham taping or other conservative treatments as the certainty of evidence was very low. Low‐certainty evidence shows that kinesio taping may improve quality of life when compared to conservative treatment. We downgraded the evidence for indirectness due to differences among co‐interventions, imprecision due to small number of participants across trials as well as selection bias, performance and detection bias. Evidence on adverse events was scarce and uncertain. Based upon the data in this review, the evidence for the efficacy of KT seems to demonstrate little or no benefit.
Keywords: Adolescent, Adult, Female, Humans, Male, Middle Aged, Young Adult, Glucocorticoids, Quality of Life, Rotator Cuff, Treatment Outcome
Plain language summary
Kinesio taping for rotator cuff disease
Review question
To determine the benefits and harms of kinesio taping (KT) in adults with shoulder pain such as impingement syndrome, rotator cuff disease and calcific tendinopathy.
Background
KT is one of the conservative treatments proposed for rotator cuff disease. KT is an elastic, adhesive, latex‐free taping made from cotton, without active pharmacological agents. Clinicians have adopted it in the rehabilitation treatment of painful conditions, however, there is no firm evidence on its benefits.
Study characteristics
We included 23 controlled trials with 1054 participants. Nine studies (312 participants) assessed the effectiveness of KT versus sham therapy (i.e. fake kinesio taping) and fourteen studies (742 participants) assessed the effectiveness of KT versus other conservative treatments (e.g.,conventional taping, physical therapies, exercise, glucocorticoid injection, oral medication). Most participants were aged between 18 and 50 years. Females comprised 52% of the sample.
Key results
Comparison 1. Kinesio taping versus sham therapy
Overall pain (lower scores mean less pain):
worsened by 0.7% (9% worse to 7.7% better) or 0.07 points on a zero to 10 scale
• People who had sham treatment rated their pain as 2.96 points.
• People who had kinesio taping rating their overall pain as 3.03 points.
Function (0 to 100; lower scores mean better function):
improved by 8% (5% worse to 21% better) or 8.05 points on a zero to 100 scale
• People who had sham treatment rated function as 47.10 points.
• People who had kinesio taping rated function as 39.05 points.
Pain on motion (scale 0 to 10; lower scores mean less pain):
improved by 14.8% (7.1% better to 22.5% better) or 1.48 points on a zero to 10 scale
• People who had sham treatment rated pain on motion as 4.39 points.
• People who had kinesio taping rated pain on motion as 2.91 points.
Active range of motion (AROM) (shoulder abduction) without pain (measured in degrees 0–180):
improved by 5.7% (8.9% worse to 20.3% better) or 10.23 degrees more
• Free of pain AROM was 174.2 degrees in people with sham treatment.
• Free of pain AROM was 184.43 degrees in people with kinesio taping.
Global assessment of treatment success:
no studies reported the outcome.
Quality of life:
one study reported data disaggregated in subscales.
Adverse events:
no reliable estimates for adverse events (4 studies) could be provided due to heterogeneous description of events.
Comparison 2. Kinesio taping versus conservative treatment
Overall pain (lower scores mean less pain):
improved by 4.4% (4.6% worse to 13% better) or 0.44 points on a zero to 10 scale
• People who had conservative treatment rated pain as 0.9 points.
• People who had kinesio taping rated pain as 0.46 points.
Function (0 to 100; lower scores mean better function):
improved by 13 % (2% better to 24% better) or 13.13 points on a zero to 100 scale
• People who had conservative treatment rated function as 46.6 points.
• People who had kinesio taping rated function 33.47 as points.
Pain on motion (scale 0 to 10; lower scores mean less pain):
improved by 0.6% (7% worse to 8% better) or 0.06 points on a zero to 10 scale
• People who had conservative treatment rated pain on motion as 4 points.
• People who had kinesio taping rated pain on motion as 3.94 points.
Active range of motion (AROM) (shoulder abduction) without pain (measured in degrees 0–180):
improved by 3% (11% worse to 17% better) or 3.04 degrees more on a scale 0–180°
• Free of pain AROM was 156.6 degrees in people with conservative treatment.
• Free of pain AROM was 159.64 degrees in people with kinesio taping.
Global assessment of treatment success:
no studies reported the outcome.
Quality of life (12‐item Short Form Survey‐, higher scores mean better quality):
improved by 18.7% (14.48% better to 22.92% better) or 18.7 points
• People who had conservative treatment rated quality of life as 37.94 points.
• People who had kinesio taping rated quality of life as 56.64 points.
Adverse events:
No reliable estimates for adverse events (7 studies) could be provided due to heterogeneous description of events.
Quality of evidence
Based on overall very low‐quality evidence, KT for rotator cuff disease has uncertain effects on pain, function, pain on motion and active range of motion when compared to sham taping or other conservative treatment. Low‐certainty evidence shows that kinesio taping may improve quality of life when compared to conservative treatment. Evidence on adverse events was scarce and uncertain due to low event rates, thus, we could not obtain a reliable estimate of the risk of these events from the trials in this review.
Summary of findings
Summary of findings 1. Kinesiotaping compared to sham taping for rotator cuff disease.
| Kinesio taping compared to sham taping for rotator cuff disease | ||||||
| Patient or population: rotator cuff disease Setting: outpatient Intervention: kinesio taping Comparison: sham taping | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | What happened | ||
| Without kinesio taping | With kinesio taping | Difference | ||||
| Overall pain
assessed with: numerical rating scale
Scale from: 0 (no pain) to 10 (maximum pain)
№ of participants: 106
(3 RCTs) follow‐up: end of treatment (4 weeks) |
‐ | The mean overall pain without kinesio taping was 2.96 points | The mean overall pain with kinesio taping was 3.03 points | MD 0.07 points worse (0.77 better to 0.9 worse) | ⊕⊝⊝⊝ VERY LOW 1 2 3 | We are uncertain about the effect of kinesio taping on overall pain. Absolute difference 0.7% worse (7.7% better to 9% worse) NNTB = N/A Relative percent change 2% worse (21% better to 24% worse)8 |
| Function
assessed with: DASH
Scale from: 0 (better function) to 100 (worse function)
№ of participants: 214
(6 RCTs) follow‐up: end of treatment (4 weeks) |
‐ | The mean function without kinesio taping was 47.10 points | The mean function with kinesio taping was 39.05 points | MD 8.05 points better
(4.93 worse to 21.02 better) 4 |
⊕⊝⊝⊝
VERY LOW 1 2 3 5 6 |
We are uncertain whether kinesio taping has any effect on function or not. Absolute difference 8% better (21% better to 5% worse) NNTB = N/A Relative percent change 15% better (40% better to 9% worse)8 |
| Pain on motion
assessed with: numerical rating scale
Scale from: 0 (no pain) to 10 (maximum pain)
№ of participants: 153
(4 RCTs) follow‐up: end of treatment (4 weeks) |
‐ | The mean pain on motion without kinesio taping was 4.39 points | The mean pain on motion with kinesio taping was 2.91 points | MD 1.48 points better (2.25 better to 0.71 better) | ⊕⊕⊝⊝
VERY LOW 12 3 |
Kinesio tape may have little or no effect on pain on motion but the evidence is very uncertain. Absolute difference 14.8% better (22.5% better to 7.1% better) NNTB = N/A Relative percent change 30% better (45% better to 14% better)8 |
| Active range of motion (shoulder abduction) without pain. Scale: 0 to 180 degrees
№ of participants: 68
(2 RCTs) follow‐up: end of treatment (2 weeks) |
‐ | The mean active range of motion (shoulder abduction without pain) without kinesio taping was 174.2 degrees | The mean active range of motion (shoulder abduction without pain) with kinesio taping was 184.43 degrees | MD 10.23 better (16.09 worse to 36.56 better) | ⊕⊝⊝⊝ VERY LOW 5 6 7 | We are uncertain about the effect of kinesio taping on active range of motion (shoulder abduction) without pain. Absolute difference 5.7% better (8.9% worse to 20.3% better). NNTB = N/A Relative percent change 6% better (10% worse to 22% better)8 |
| Global assessment of treatment success № of participants: (0 studies) | ‐ | Not reported | ||||
| Quality of life № of participants: (0 studies) | ‐ | ‐ | ‐ | ‐ | Not reported | |
| Adverse events № of participants: 136 (4 RCTs) | ‐ | Due to a paucity of information, data were not meta‐analysed. | Due to a paucity of information, data were not meta‐analysed. | ⊕⊝⊝⊝ VERY LOW 1 2 5 | We are uncertain whether kinesio taping results in more people reporting adverse events. | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded 1 level for serious limitations in study design due to one study being assessed as high risk of bias for selection, performance and detection bias.
2 We downgraded 1 level for serious indirectness (e.g. differences among co‐interventions). Three studies (Kang 2020; Miccinilli 2018; Simsek 2013) added a co‐intervention (exercise/general rehabilitative program) to both kinesio taping or sham taping groups. One study (Kocyigit 2016) provided exercise/NSAIDs/paracetamol as co‐interventions to both kinesio taping and sham taping groups.
3 We downgraded 1 level for serious imprecision due to number of participants fewer than 400.
4 SMD back‐translated to typical scales by multiplying the SMD by the standard deviation at baseline in the control group as reported in Simsek 2013: mean (SD) for disability (DASH): 52.69 (16.42)
5 Publication bias: missing results that could lead to non‐reporting bias
6 We downgraded 1 level for high heterogeneity (I2 > 75)
7 We downgraded 2 levels for very serious imprecision (sample size and wide confidence intervals)
8 Overall pain: relative percent change calculated using baseline mean 3.75 from Kocyigit 2016; function: relative percent change calculated using baseline mean 52.69 from Simsek 2013; pain on motion: relative percent change calculated using baseline mean 5 from Kocyigit 2016; active range of motion (shoulder abduction) without pain: relative percent change calculated using baseline mean 164.9 from Shakeri 2013
Summary of findings 2. Kinesiotaping compared to other conservative treatment for rotator cuff disease.
| Kinesio taping compared to other conservative treatment for rotator cuff disease | ||||||
| Patient or population: rotator cuff disease Setting: outpatient Intervention: kinesio taping Comparison: other conservative treatment | ||||||
| Outcomes | Relative effect (95% CI) | Anticipated absolute effects* (95% CI) | Certainty of the evidence (GRADE) | What happens | ||
| Without kinesio taping | With kinesio taping | Difference | ||||
| Overall pain
assessed with: rating scale from: 0 (no pain) to 10 (maximum pain)
№ of participants: 266
(5 RCTs) follow‐up: end of treatment (6 weeks) |
‐ | The mean overall pain without kinesio taping was 0.9 points | The mean overall pain with kinesio taping was 0.46 points | MD 0.44 points better (1.33 better to 0.46 worse) | ⊕⊝⊝⊝
VERY LOW 1 2 3 7 |
We are uncertain about the effect of kinesio taping on overall pain. Absolute difference 4.4% better (13% better to 4.6% worse) NNTB = N/A Relative percent change 15% better (46% better to 16% worse)8 |
| Function
assessed with: SPADI
scale from: 0 (better function) to 100 (worse function)
№ of participants: 499
(14 RCTs) follow‐up: end of treatment (4 weeks) |
‐ | The mean function without kinesio taping was 46.6 | The mean function with kinesio taping was 33.47 | MD 13.13 points better (1.99 better to 24.28 better)4 | ⊕⊝⊝⊝ VERY LOW 2 5 6 | We are uncertain about the effect of kinesio taping on function. Absolute difference 13% better (24% better to 2% better) NNTB = N/A Relative percent change 18% better (32% better to 3% better)8 |
| Pain on motion
assessed with: rating scale from: 0 (no pain) to 10 (maximum pain) № of participants: 225 (6 RCTs) follow‐up: end of treatment (4 weeks) |
‐ | The mean pain on motion without kinesio taping was 4 points | The mean pain on motion with kinesio taping was 3.94 points | MD 0.06 points better (0.68 better to 0.80 worse) | ⊕⊝⊝⊝ VERY LOW 2 6 7 | We are uncertain about the effect of kinesio taping on pain on motion. Absolute difference 0.6% better (7% better to 8% worse) NNTB = N/A Relative percent change = 1% better (12% better to 10% worse)8 |
| Active range of motion (shoulder abduction) without pain. Scale: 0 to 180 degrees
№ of participants: 143
(3 RCTs) follow‐up: end of treatment (6 weeks) |
‐ | The mean active range of motion (shoulder abduction without pain) without kinesio taping was 156.6 degrees | The mean active range of motion (shoulder abduction without pain) with kinesio taping was 159.64 degrees | MD 3.04 better (10.89 worse to 16.96 better) | ⊕⊝⊝⊝ VERY LOW 2 5 7 | We are uncertain about the effect of kinesio taping on active range of motion (shoulder abduction without pain) Absolute difference 3% better (11% worse to 17% better) NNTB = N/A Relative percent change 3% better (9% worse to 14% better)8 |
| Quality of life assessed with SF‐12 Health Survey scale from: 0 (worse QoL) to 100 (better QoL) № of participants: 30 (1 RCTs) follow‐up: end of treatment (4 weeks) |
‐ | The mean SF‐12 Health Survey without kinesio taping was 37.94 | The mean SF‐12 Health Survey with kinesio taping was 56.64 | MD 18.7 better (14.48 better to 22.92 better) |
⊕⊕⊝⊝ LOW 2 7 |
Kinesio taping may improve quality of life. Absolute difference 18.7% better (14.48% better to 22.92% better) NNTB = N/A Relative percent change 53% better (41% better to 65% better)8 |
| Global assessment of treatment success № of participants: (0 studies) | ‐ | No studies reported this outcome. | ||||
| Adverse events № of participants: 391 (7 RCTs) | Due to a paucity of information, data were not meta‐analysed. | Due to a paucity of information, data were not meta‐analysed. | ‐ | ⊕⊝⊝⊝ VERY LOW 2 3 6 | We are uncertain whether kinesio taping results in more people reporting adverse events | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; OR: Odds ratio; | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect Moderate certainty: we are moderately confident in the effect estimate: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different Low certainty: our confidence in the effect estimate is limited: The true effect may be substantially different from the estimate of the effect Very low certainty: we have very little confidence in the effect estimate: The true effect is likely to be substantially different from the estimate of effect | ||||||
1 We downgraded 2 levels for high heterogeneity (I2 > 90).
2 We downgraded 1 level for indirectness due to variability in control interventions.
3 We downgraded 1 level for study limitations.
4SMD back‐translated to typical scales by multiplying the SMD by the standard deviation at baseline in the control group as reported in Subasi 2016: mean (SD) for disability (SPADI): 74.8 (19.9)
5 We downgraded 1 level for high heterogeneity (I2 > 75).
6 Publication bias: missing results that could lead to non‐reporting bias
7 We downgraded 1 level for very serious imprecision (sample size).
8 Relative percent change calculation: Overall pain, calculated using baseline mean from De Oliveira 2021 = 2.9; function, calculated using baseline mean from Subasi 2016 = 74.8; pain on motion, calculated using baseline mean from Subasi 2016 = 6.8; free of pain ‐ active range of motion, calculated using baseline mean from De Oliveira 2021 = 120.5; Quality of life, calculated using baseline mean from Sikha 2017 = 35.44
Background
Description of the condition
Point prevalence of chronic shoulder pain has been variously estimated between 7% and 25%, while its incidence is around 1 per 100 per year, peaking at 2.5 per 100 per year among individuals aged 42 to 46 years (Bjelle 1989; Chard 1991). Abnormalities of the rotator cuff increase with age, from an overall prevalence of 9.7% (29 of 299) in patients aged 20 years and younger to 62% (166 of 268) in patients aged 80 years and older (Teunis 2014). It also accounts for up 10% of all referrals to physiotherapists (Peters 1994).
Shoulder disorders significantly impact on the majority of daily life activities (such as eating and dressing) and on working (Bennell 2007). In addition, shoulder pain is often associated with anxiety, depression and impaired ability to sleep, hence, affecting mood and concentration (Cho 2013).
Numerous terms are used to describe disorders of the rotator cuff (for example, subacromial impingement syndrome, rotator cuff tendinopathy or tendinitis, partial or full rotator cuff tear, calcific tendinitis and subacromial bursitis) (Schellingerhout 2008). 'Rotator cuff disease' is proposed as an umbrella term to classify disorders of the rotator cuff, whether the cause is degeneration or acute injury, to cover different anatomical locations (Buchbinder 1996; Whittle 2015), and we used this term in the review.
Rotator cuff disease, such as subacromial impingement and rotator cuff tendinopathy, is considered to be the most common causes of chronic shoulder pain (Burbank 2008). Other less frequent causes of shoulder pain include frozen shoulder, shoulder instability and shoulder joint osteoarthritis (Burbank 2008). For example, shoulder impingement accounts for 44% to 65% of shoulder complaints during general practice consultations (Van der Windt 1996), and it has an associated economic burden on healthcare systems (Virta 2012).
The occurrence of rotator cuff disorder is associated with jobs that are highly repetitive such as hairdressing (Mitchell 2005), activities that require forceful exertion or awkward postures, or have a high psychosocial job demand (Van Rijn 2010), or some sports (e.g. overhead athletes) (Ellenbecker 2010; Page 2011). The rotator cuff pain manifests in the midrange of motion (between 40° and 120°), often causing a painful arch during active abduction (Kessel 1977). Pain over the shoulder area, frequently irradiating along the ipsilateral arm, is one of the symptoms more frequently reported by patients, along with restriction in shoulder range of motion (ROM) and impeded activities of daily living (Bayam 2011). High baseline pain, disability, and previous episodes are associated with an unfavourable outcome (Littlewood 2013). It is proposed that early recognition and adequate treatment may reduce the risk of this disorder becoming a chronic condition (Kessel 1977; Khan 2013).
Conservative treatments for rotator cuff pain management include electro‐physical therapies (e.g. laser, shock wave therapy), manual mobilisation, exercise and taping (Escamilla 2014). These interventions could diminish costs related to more invasive treatments and absences from work (Ketola 2013; Khan 2013; Vas 2005).
Description of the intervention
Taping has been used for a long time to prevent and treat sports injuries as it provides protection and support to the joint or muscle or both during the movement (Williams 2012). The conventionally used tape is rigid while the recently introduced kinesio taping is an elastic, adhesive, latex‐free taping made from cotton, without active pharmacological agents and is water resistant (Kase 2003).
Kinesio taping was developed by a Japanese chiropractor, Dr Kenso Kase, in the 1970s; he described it as a natural way to relieve pain (Kase 2003). According to its inventor, kinesio taping offers several advantages over other conventional taping. Firstly, it aims to give a free range of motion in order to allow the body’s muscular system to heal itself biomechanically. Secondly, the kinesio taping can be virtually applied to any joint or musculoskeletal region, it is easy to apply, non‐allergenic and with relatively low cost (Kase 2003). At present, it is marketed by various companies under different brand names, often in a variety of colours. These qualities and aggressive marketing made kinesio taping an increasingly popular intervention amongst elite athletes who use it to try and prevent injuries (Williams 2012). Kinesio taping has also gained momentum as a potential rehabilitative intervention among the general public and health professionals in the last decade, even though sound scientific proof of its validity has been lacking.
Systematic reviews for rotator cuff disorder previously reported that the evidence related to the efficacy of conservative interventions compared with surgery was inconclusive due to low‐quality studies (Coghlan 2008; Saltychev 2015; Tashjian 2013). However high‐certainty evidence from a recent Cochrane review found that subacromial decompression surgery is not effective for shoulder pain compared with non‐surgical treatment including exercise (Karjalainen 2019). As surgery has higher costs and carries a risk of complications, conservative interventions seem to be the best option to recommend as the first choice treatment for shoulder pain (Saltychev 2015). Two recent reviews that focused on conservative interventions for rotator cuff disease concluded that the effects of manual therapy and exercise may be similar to those of glucocorticoid (steroid) injection and surgery (namely, arthroscopic subacromial decompression), but this was based on low‐quality evidence (Page 2016a). Only therapeutic ultrasound and low level laser therapy showed some benefit over placebo (Page 2016b). Kinesio taping was not included in these previous reviews.
How the intervention might work
Kinesio taping was designed to simulate the qualities of human skin, and it has roughly the same thickness as the skin (Kase 2003). Manufacturers claim that kinesio taping provides benefits by facilitating the body’s natural physiologic and healing processes with sensory stimulation and mechanical support: aiding muscle and positional stimulus through the skin, aligning fascial (connective) tissues, creating more space by lifting the soft tissues above the area of pain or inflammation, assisting drainage of lymph fluid exuding from a sore or inflamed tissue, by directing fluid toward the duct, and providing sensory stimulation and mechanical support without restricting the body’s range of motion, differently from a conventional rigid tape (Kase 2003).
These benefits are supposed to depend on the amount, as well as on the stretch direction, of the applied tape (Kase 2003). Kinesio taping can be applied producing different shapes (e.g. 'Y', 'I', 'web'), according to the shape and size of the affected muscle. Application methods differ with the therapeutic aim. When the tape is used to inhibit or restore muscle function, it is applied from its insertion to the origin to limit the muscle performance (Djordjevic 2012) or from its origin to the insertion to enhance muscle activity (e.g. forearm grip strength) (Mohammadi 2014). Conversely, when the tape is used to promote lymphatic drainage, it is applied in the fan format directing lymph fluid towards less congested parts of the lymphatic system in order to try and reduce swelling. The arms of the fan direct lymphatic flow towards the anchor facilitating drainage (e.g. to help reduce swelling after a mastectomy) (Pekyavas 2014b).
Theoretically, the mechanisms of these actions might reduce pain from rotator cuff disease. Authors have claimed that kinesio taping might: 1) improve shoulder strength, range of motion and proprioception (the sense of the relative position of body segments in relation to other body segments) (Williams 2012); 2) improve proprioceptive feedback and correct alignment during movement, to help promote the stability of the shoulder blade (Kaya 2011; Mottram 1997); 3) allow free movements of arms without pain (Host 1995); and 4) prevent acute injuries and the evolution to a chronic condition and impairments (Myers 2000). There is little evidence to support these claims.
Why it is important to do this review
Kinesio taping is one of the conservative treatments proposed for rotator cuff disease. Clinicians have adopted it in the rehabilitation treatment of painful conditions, even if firm evidence of its benefits are not yet well established.
Previous reviews focused on injury prevention in healthy subjects (Kamper 2013; Williams 2012) or considered participants with a wide spectrum of conditions relating to the musculoskeletal system focusing on different joints at the same time (Kalron 2013; Lim 2015; Montalvo 2014; Morris 2013; Mostafavifar 2012; Parreira 2014). In the latter case, data were not pooled, due to clinical heterogeneity, and the small number of retrieved studies focused on a specific condition, limiting conclusions. Recently, an increasing number of RCTs on kinesio taping use for shoulder pain have been published with conflicting findings and different attempts to synthesise the evidence have been published (Celik 2020; Dong 2015; Ghozy 2020; Saracoglu 2018). However, there has been little overlap of the included studies due to different clinical questions, aims, and publication dates. For instance, Dong 2015 presented a network meta‐analysis of all treatments for shoulder impingement syndromes; Ghozy 2020 included a wide range of diagnoses such as shoulder disability after mastectomy, hemiplegic shoulder pain or asymptomatic overhead athletes (ie. one who uses their upper arm and shoulder in an arc over head to propel a ball toward the opposing team); Saracoglu 2018 restricted the evidence to shoulder impingement syndrome; and Celik 2020 limited the included trials to pain, range of motion, and functional outcomes.
As conflicting evidence has sprung from reviews and randomised trials and there is uncertainty about the benefits of kinesio taping in people with rotator cuff disease, this review aims to address this evidence gap, given that the trials in this population have not been adequately and systematically reviewed previously.
Objectives
To determine the benefits and harms of kinesio taping in adults with shoulder pain due to rotator cuff disease.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) and quasi‐randomised controlled clinical trials (with methods of allocating participants to treatment that are not strictly random, e.g. using alternation, date of birth, or some similar method of allocation) were selected.
Types of participants
We included adults with rotator cuff disease as defined by the authors (e.g. using terminology such as subacromial impingement syndrome, rotator cuff tendonitis or tendinopathy, supraspinatus, infraspinatus or subscapularis tendonitis, subacromial bursitis, or rotator cuff tears), for any duration.
We included studies with participants with unspecified shoulder pain provided that the inclusion criteria were compatible with a diagnosis of rotator cuff disease. We also included studies of participants with mixed shoulder disorders (e.g. shoulder girdle fractures, dislocation and previous surgery, adhesive capsulitis, full thickness rotator cuff tears), if these participants were a minority of the study population (i.e. less than 20%), or if we could retrieve the data for participants with rotator cuff disease separately from the trialists.
We excluded trials that included participants with a history of significant trauma or systemic inflammatory conditions such as rheumatoid arthritis, osteoarthritis, hemiplegic shoulders, or pain in the shoulder region as part of a complex myofascial pain condition, or those with adhesive capsulitis (frozen shoulder), shoulder instability, and rotator cuff arthropathy.
Types of interventions
Experimental intervention: kinesio taping (KT) with or without standardised co‐interventions (such as supervised or home exercises), provided that co‐interventions were given equally to both experimental and control groups. We included any number of kinesio taping applications and any duration of kinesio taping applications.
We compared the experimental intervention (kinesio taping) to:
sham taping;
other conservative interventions (e.g. conventional taping, physical therapies, exercise, glucocorticoid injection, oral medication, or other interventions).
Types of outcome measures
We did not consider outcomes as part of the eligibility criteria. In fact, a recent review evaluating outcome assessment in rehabilitative interventions found considerable variation of the reporting of outcome measures in clinical trials (Gianola 2016).
Major outcomes
Overall pain (mean or mean change measured by visual analogue scale (VAS), numerical or categorical rating scale)
Function: Where trialists reported outcome data for more than one function scale, we extracted data on the scale that was highest on the following a priori defined list: (1) Shoulder Pain and Disability Index (SPADI); (2) Croft Shoulder Disability Questionnaire; (3) Constant‐Murley Score; (4) Disability of Arm Shoulder and Hand (DASH); (5) any other shoulder‐specific function scale.
Pain on motion: measured by VAS, numerical or categorical rating scale, regardless of the type of clinical evaluation e.g. on resisted movements, at the endpoint of pain‐free active shoulder ROM, with active movements, caused by a clinical diagnostic test for rotator cuff disease (e.g. empty can test of Jobe)
Active range of motion (AROM): extent of active shoulder abduction or elevation of the shoulder without pain, measured in degrees or other scales (e.g. functional target distance)
Global assessment of treatment success as defined by the trialists (e.g. proportion of participants with significant overall improvement), or measured by specific tools (e.g. Global Perceived Effect, GPE (Kamper 2010))
Quality of life as measured by generic measures (such as components of the Short Form‐36 (SF‐36)) or disease‐specific tools)
Adverse events: number of participants experiencing any adverse event (e.g. skin reactions, including severe or painful rash, itching, dermatitis, local ulceration or exfoliation, and enlarged glands)
Minor outcomes
Other measures of pain: such as, pain at night and pain at rest
Other measures of range of motion (ROM): external rotation and internal rotation measured in degrees or other scales (e.g. hand‐behind‐back distance in centimetres). If authors reported outcome data for both active and passive ROM measures, we extracted the data on active ROM only.
Muscle strength: strength of any muscle of shoulder measured by digital hand dynamometer, isokinetic peak torque, or other
Withdrawals or dropouts: proportion who withdrew from treatment due to adverse events or other reasons
The tape generally stays on for three to four days. In KT therapy, more than one application can be accepted; consequently, we considered all trials independently from the number of applications of KT and defined as 'therapeutic cycle' the time between the first application and the removal of the last KT application planned in each trial. For the meta‐analysis, we considered the last available measurement within 30 days from the end of the therapeutic cycle.
Search methods for identification of studies
Electronic searches
The following electronic databases were used to identify relevant studies published from database inception to July 27 2020:
Cochrane Central Register of Controlled Trials (CENTRAL) in The Cochrane Library;
MEDLINE via Ovid;
Embase via Ovid;
PEDro (Physiotherapy Evidence database) via http://www.pedro.org.au/;
CINAHL plus (Cumulative Index to Nursing and Allied Health Literature) via EBSCOhost.
The electronic search strategy for CENTRAL and MEDLINE is outlined in Appendix 1.
Ongoing trials and protocols of published trials were searched in the clinical trials register maintained by the US National Institutes of Health (http://clinicaltrials.gov) and the Clinical Trial Register at the International Clinical Trials Registry Platform of the World Health Organization (http://www.who.int/ictrp/en/). The reference lists of included trials and relevant review articles retrieved were reviewed to identify other potentially relevant trials. No date or language restrictions were applied.
Searching other resources
The reference lists of included articles was searched to ascertain if any relevant trials were not identified by the electronic searches. Kinesio taping manufacturers were contacted to identify additional unpublished trials.
Data collection and analysis
Selection of studies
Two review authors (SG, GC) independently selected the citations identified in the literature search on the basis of title and abstract, discarding those not meeting the inclusion criteria. All potentially relevant articles were retrieved for an assessment of the full text. The assessment of eligibility was conducted independently by two review authors. If any doubt arose that a study met the inclusion criteria, a consensus meeting was held to resolve disagreements concerning the inclusion of RCTs, and another review author (AA) would be consulted if disagreements persisted. We documented excluded studies in the ‘Characteristics of excluded studies’ table and provided an individual reason for exclusion.
Data extraction and management
We used a data collection form for study characteristics and outcome data, which was piloted on at least one eligible RCT. Two review authors (VI, EF) independently extracted study characteristics from included studies. We extracted for each study the following characteristics:
Methods: design, start date and total duration, setting and withdrawals from the study
Participants: number, mean or median age with a dispersion measure, sex, shoulder pathology and systemic conditions
Interventions: kinesio taping application methods (characteristics, direction related to function, stretch, shape and size of the strips, target muscle, number and duration of applications, provider), comparisons, concomitant therapies and/or medications
Outcomes: list of relevant outcomes assessed, definitions used, values of means and standard deviations at baseline and at all time points and/or change from baseline measures for continuous outcomes, and frequencies for categorical outcomes
Characteristics of the design of the trial as outlined below in the Assessment of risk of bias in included studies section
Notes: funding and notable declarations of conflict of interest of trial authors
Two review authors (VI, EF) independently extracted all outcome measure data from the included studies. We resolved disagreements by consensus or by involving a third person (SG). Two review authors (SG,GC) transferred data into Review Manager (Review Manager 2014). We double‐checked that data were entered correctly by comparing the data presented in the systematic review with the study reports. We noted in the 'Characteristics of included studies' table if outcome data were not reported in a usable way.
A priori decision rules to assist in selecting which data to extract in the event of multiple outcome reporting were the following:
Where authors reported outcomes for more than one pain at movement score, we extracted data on the scale highest on the following list: (1) visual analogue or rating scale; (2) any other pain score;
According to the recent systematic review about the quality of measurement properties per questionnaire (Huang 2015), where authors reported outcomes for more than one disability scale, we extracted data on the scale that was highest on the following list: (1) the Western Ontario Rotator Cuff Index (WORC) (Kirkley 2003); (2) Shoulder Pain and Disability Index (SPADI) (Roach 1991); (3) the Simple Shoulder Test (SST) (Godfrey 2007); (4) Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire (Hudak 1996); (5) Constant Score (Constant 1987); (6) any other function scale;
Physiotherapy studies have small sample sizes and use patient‐reported outcomes, such as pain, that have high between‐subject variability. Consequently, imbalances between groups are possible at baseline, even with adequate randomisation. Moreover, the effects are often very small in this field. Consequently, differences between groups are difficult to detect. For these reasons, if a study reported both change and its SD, and final value and its SD, we used change from baseline values rather than final values (Banerjee 2008). If studies reported only final values and SD, we used the available measures.
Assessment of risk of bias in included studies
Two review authors (SG, GC) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). We resolved any disagreement by discussion or by involving another author (AA). We assessed the risk of bias according to the following domains:
Random sequence generation (selection bias)
Allocation concealment (selection bias)
Blinding of participants (performance bias)
Blinding of care providers (performance bias)
Blinding of outcome assessment for self‐reported outcomes such as pain, function, global assessment, quality of life (detection bias)
Blinding of outcome assessment ‐ assessor‐reported outcomes (detection bias)
Incomplete outcome data for each treatment group (attrition bias)
Selective outcome reporting (reporting bias)
Other bias: group similarity at baseline (selection bias); unequal use of co‐intervention
We graded each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for our judgement in the risk of bias table. We summarised the risk of bias judgements across different studies for each of the domains listed. The two review authors (SG, GC) resolved discrepancies in judgement by discussion and asked a third review author (AA) to make the final judgment if they could not reach a consensus.
In physiotherapy trials which mainly use self‐reported measures, blinding of participants (as the outcome assessor) is crucial for patient‐reported outcomes due to their self‐reported nature. However, blinding of participants was not always possible to achieve as participants were aware if they received a given treatment (e.g. kinesio taping or physical exercises), unless they received a sham therapy (e.g. kinesio taping compared to sham kinesio taping). Nevertheless, we described and reported the methods to blind participants and outcome assessors ‐ i.e. see domain 4 and 5 in the list above. If blinding of participants was adequate, we judged studies to be at low risk of detection bias for self‐reported outcomes (pain, function, quality of life, treatment success, adverse events); if blinding of the outcome assessor was adequate, we judged studies to be at low risk of detection bias for assessor‐reported outcomes (i.e. range of motion, strength measurements). If no description was given, we contacted the study authors for more information and, if we did not receive a response, we assigned a judgement of unclear risk of bias. If blinding was not present or was not possible because of the nature of intervention, we judged the study to be at high risk of bias because it was possible that the lack of blinding might have influenced the results.
Analogously, we considered the impact of missing data for the following major outcomes (overall pain and function). Where information on risk of bias related to unpublished data or correspondence with a trialist, we noted this in the risk of bias table.
We presented the figures generated by the risk of bias tool to provide summary assessments of the risk of bias.
Measures of treatment effect
For the major and minor outcomes, we assessed the treatment effects using the risk ratio (RR) for dichotomised outcomes and the mean difference (MD) for continuous outcomes with their corresponding 95% confidence intervals (CIs). However, when different scales were used to measure the same conceptual outcome (e.g. pain, disability), standardised mean differences (SMDs) were calculated. SMDs were back‐translated to a typical scale (e.g. 0 to 10 for pain) by multiplying the SMD by a typical among‐person standard deviation (e.g. the standard deviation of the control group at baseline from the most representative trial) (Schunemann 2017b).
If some scales increase with disease severity whilst others decrease, it is essential to multiply the mean values from one set of studies by –1 (or alternatively to subtract the mean from the maximum possible value for the scale) to ensure that all the scales point in the same direction.
For pain, a negative effect size indicated that kinesio taping was more beneficial than the comparison therapy, meaning that participants had better pain relief. For the other outcomes such as ROM, a positive effect size indicated that kinesio taping was more beneficial than the comparison therapy, meaning that participants had a greater ROM.
In the 'Effects of interventions' results section and the 'comments' column of the 'Summary of findings' tables, we provided the absolute per cent difference, the relative per cent change from baseline, and the number needed to treat for an additional beneficial outcome (NNTB) and number needed to treat for an additional harmful outcome (NNTH) (the NNTB or NNTH were provided only when the outcome showed a statistically significant difference).
For dichotomous outcomes, NNTB or NNTH were calculated from the control group event rate and the relative risk using the Visual Rx NNT calculator (Cates 2008). The NNTB or NNTH for continuous measures were calculated using the Wells calculator (available at the CMSG Editorial office).
For dichotomous outcomes, the absolute per cent change was calculated from the difference in the risks between the intervention and control group using GRADEpro (GRADEpro GDT 2015) and expressed as a percentage. For continuous outcomes, the absolute benefit was calculated as the improvement in the intervention group minus the improvement in the control group, in the original units, expressed as a percentage.
The relative per cent change for dichotomous data was calculated as the risk ratio ‐ 1 and expressed as a percentage. For continuous outcomes, the relative difference in the change from baseline was calculated as the absolute benefit divided by the baseline mean of the control group, expressed as a percentage.
Unit of analysis issues
The unit of randomisation and analysis in the included trials was the individual participant. Exceptionally, people may present with bilateral shoulder pain, which may be randomised to a single treatment for each shoulder. Therefore, a trial including people with bilateral shoulder pain may present results for shoulders rather than individuals, a potential unit of analysis issue. We still included such studies as if people with bilateral shoulder pain were included and a sensitivity analysis was undertaken.
For studies containing more than two intervention groups, making multiple pairwise comparisons between all possible pairs of intervention groups possible, in order to overcome a unit of analysis error, we used the following strategy: we split the ‘shared’ group into two or more groups with smaller sample size, and included two or more (reasonably independent) comparisons.
Dealing with missing data
a) Individuals missing from the reported results of primary studies
For included studies, we noted any discrepancy between the number randomised and the number analysed in each treatment group, reporting the percentage of loss to follow‐up in each group and reasons for attrition. Where data were missing, we contacted the corresponding authors of included studies by written correspondence (e.g. emailing or writing to corresponding author(s)) to retrieve any available unreported data. If information on missing individuals was not provided, we performed available case analysis, commenting on the possible impact of missing data on the results. If more than 10 studies were included, we explored the impact of including studies with missing individual data on the conclusion of the meta‐analysis by performing a sensitivity analysis.
b) Missing summary data for an outcome
If a study did not provide usable summary measures for an outcome, it was included in the review but excluded from the meta‐analysis. Implications of its absence were discussed. For studies that reported a mean difference but no standard deviation (SD), the latter was computed from other statistics ‐ such as standard errors, confidence intervals, t‐value or P values – whenever possible. If standard deviations could not be calculated, and random missingness could be assumed, they were imputed (Deeks 2020). For each outcome, we imputed missing SDs as the pooled SD from all other trials in the same meta‐analysis by treatment group. This is, both for fixed‐ and random‐effects models, an easy method of analysis and it is less biased than excluding studies with missing standard deviations (Furukawa 2006). If the proportion of trials missing variability data for a particular outcome was high (> 30%), we conducted analyses using only available data, and implications were discussed in the text.
Assessment of heterogeneity
Clinical and methodological heterogeneity were assessed in terms of participants, interventions, outcomes and study characteristics for the included studies. This was conducted by observing the data extraction tables.
Statistical heterogeneity was evaluated using forest plots, the I² statistics and the estimate of the between‐study variance (τ²) (Higgins 2003; Higgins 2009). The interpretation of an I² value of 0% to 40% might 'not be important'; 30% to 60% may represent 'moderate' heterogeneity; 50% to 90% may represent 'substantial' heterogeneity; and 75% to 100% may represent 'considerable' heterogeneity (Deeks 2020).
Assessment of reporting biases
We used funnel plots to explore the likelihood of reporting biases when at least 10 studies were included in the meta‐analysis. First, we assessed funnel plot asymmetry visually, integrating visual inspection with the use of formal tests for funnel plot asymmetry. For continuous outcomes, we used the test proposed by Egger (Egger 1997), and for dichotomous outcomes, we used the test proposed by Harbord (Harbord 2006). If asymmetry was suggested by visual assessment or detected by tests, we discussed possible explanations (such as publication bias, poor methodological quality, true heterogeneity, artefact or chance) and considered implications for the review findings (Sterne 2017).
We considered the possibility of small‐study bias on review findings. In the presence of small‐sample bias, the random‐effects estimate of the intervention is more beneficial than the fixed‐effect estimate (Sterne 2017).
We assessed the risk of bias due to selective outcome reporting by comparing outcomes the trial investigators intended to measure with outcomes reported in trial reports. We reviewed protocols or clinical trial registries to determine intended outcomes. Otherwise, we compared outcomes reported in the ‘Results’ section to those described in the ‘Methods’ section.
We also examined studies to verify if they had been analysed on an intention‐to‐treat (ITT), per‐protocol or available case basis.
Data synthesis
We undertook meta‐analyses only where this was meaningful, i.e. if the treatments and comparators, participants and the underlying clinical question were similar enough for pooling to make sense (low clinical and methodological heterogeneity). We used either a fixed‐effect or random‐effects model on the basis of careful consideration of the extent of statistical heterogeneity and whether it could be explained by available features, including the size of the studies. If high heterogeneity (I² > 75%) was detected and could not be reduced by accounting for methodological or clinical features among trials, the results were not combined but presented as a narrative synthesis.
If dichotomous outcomes, such as side effects, were very rare and at least one study had no events, we performed the meta‐analysis using a generalised linear mixed model, allowing the inclusion of studies with no events (Stijnen 2010). If continuous outcomes had a highly skewed distribution, we considered transformation before pooling. If we pooled studies using the SMD, the Hedges’ bias‐correction was used by default to adjust for small‐sample bias (Hedges 1981). We used 95% CIs throughout.
We analysed the data using Review Manager 5.3 (Review Manager 2014). Where necessary, we performed meta‐regression or other analyses using the software R (R software) and the package metaphor (Viechtbauer 2010) (which are not supported in Revman).
Subgroup analysis and investigation of heterogeneity
Subgroup analyses were planned for the following subgroups only if sufficient studies were retrieved in the data collection process, as it is unlikely that the investigation of heterogeneity produced useful findings unless a substantial number of studies were identified.
1. Number of applications of kinesio taping: one versus two or more applications:
In kinesio taping therapy, consecutive applications can be performed (Kase 2003), therefore, we tried to understand if applying the kinesio taping more than once (i.e. prolonging the KT treatment for more than three to four days) was more beneficial, similar to using high dose for medicines.
2. Target population: 'overhead' people (e.g. athletes, workers) versus general population:
Individuals who are at risk of developing impingement syndrome include athletes (e.g. baseball players), assembly‐line workers, warehouse workers, and others who perform repetitive work with the arms raised above shoulder height. In those individuals, the shoulder pain may be more severe than in the general population. In fact, athletes and overhead workers have a different pattern of scapular kinematics than the general population (Timmons 2012).
We restricted subgroup analysis to pain and function outcomes. We conducted a statistical test for heterogeneity across subgroup results and computed an I2 statistic. We used the random‐effects models to analyse the variation in the mean effects in the different subgroups using meta‐regression techniques if the number of studies in the meta‐analysis were adequate. Acknowledging that subgroup comparisons are observational, we used caution in the interpretation of subgroup analyses.
Sensitivity analysis
We planned to carry out the following sensitivity analysis: studies with missing data for participants excluded to allow investigation of their impact on the results of the meta‐analysis.
We conducted sensitivity analysis to investigate the effects of risks of bias. We assessed the effect of including studies with unclear or high risk of the following biases on subjective outcomes (pain, function, quality of life, treatment success) by:
removing studies with lack of or unclear random sequence generation or adequate allocation concealment to assess the potential effect of selection bias;
removing studies with lack of or unclear participant blinding to assess the potential effect of performance and detection bias.
Summary of findings and assessment of the certainty of the evidence
Where there were sufficient data, we created summary of findings tables in GRADEpro (GRADEpro GDT 2015) using the following outcomes:
Active range of motion (AROM): extent of active shoulder abduction/elevation of the shoulder without pain, measured in degrees or other scales (e.g. functional target distance);
Overall pain (mean or mean change measured by visual analogue scale (VAS), numerical or categorical rating scale);
Function. Where trialists reported outcome data for more than one function scale, we extracted data on the scale that was highest on the following a priori defined list: (1) Shoulder Pain and Disability Index (SPADI); (2) Croft Shoulder Disability Questionnaire; (3) Constant‐Murley Score; (4) any other shoulder‐specific function scale;
Pain on motion measured by VAS, numerical or categorical rating scale, regardless of the type of clinical evaluation e.g. on resisted movements, at the endpoint of pain‐free active shoulder ROM, with active movements, caused by a clinical diagnostic test for Shoulder Impingement Syndrome (SIS) (e.g. empty can test of Jobe);
Global assessment of treatment success as defined by the trialists (e.g. proportion of participants with significant overall improvement), or measured by specific tools (e.g. Global Perceived Effect, GPE (Kamper 2010));
Quality of life as measured by generic measures (such as components of the Short Form‐36 (SF‐36)) or disease‐specific tools);
Number of participants experiencing any adverse events (e.g. skin reactions, including severe or painful rash, itching, dermatitis, local ulceration or exfoliation, and enlarged glands).
We used the following minimal important difference (MID) values when interpreting the importance of differences between the groups:
Active range of motion (AROM): absolute improvement of 10%;
Overall pain (visual analogue scale (VAS) or numeric rating scale (NRS); 0 to 10): 1.5 points (Hao 2019);
Function (DASH score; 0 to 100) 10.2 points (Hao 2019), or (SPADI score; 0 to 100) 13 points (Dabija 2019; Roy 2009);
Pain on motion (visual analogue scale (VAS) or numeric rating scale (NRS); 0 to 10): 2.1 points (Hao 2019);
Global assessment of treatment success: absolute improvement of 10%;
Quality of life (scale; 0 to 100) 10 points or absolute improvement of 10%.
The tables included the main comparisons described in the Types of interventions as follows:
kinesio taping use versus sham taping
kinesio taping use versus other interventions (e.g. exercise)
SOF tables presented treatment effects within 30 days from the end of the therapeutic cycle.
Regardless of whether available homogeneous data were sufficient to allow review authors to quantitatively summarise the data, we assessed the overall quality of the evidence for each outcome. To accomplish this, we used the five GRADE considerations (study limitations, consistency of effect, imprecision, indirectness, and publication bias), as recommended in the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2020) and in the Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (GRADEpro GDT 2015; Schünemann 2013). For each outcome, the quality starts at high when high‐quality RCTs provide results; quality is reduced by one or two levels when each of the quality considerations above are not met:
High‐quality evidence:
Consistent findings have been noted among at least 75% of RCTs with no limitations on study design; with consistent, direct and precise data; and with no known or suspected publication biases. Further research is unlikely to change the estimate or our confidence in the results.
Moderate‐quality evidence:
One of the domains is not met. Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate.
Low‐quality evidence:
Two of the domains are not met. Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.
Very low‐quality evidence:
Three of the domains are not met. We are very uncertain about the results.
No evidence:
No RCTs were identified that addressed this outcome.
Results
Description of studies
Results of the search
Overall, we identified 1991 articles in MEDLINE (944), Embase (236), CINAHL (367), Central (368), Pedro (43), WHO ICTRP and Clinicaltrials.gov (33); after duplicates were removed, we identified 1789 records. Four reviewers in pairs (SG, CG, VI, EF) independently reviewed abstracts and retrieved 68 full‐text articles, which they read in full. Two additional trials are awaiting classification. We also found six related publications of included studies and seven duplicates. One study was not retrieved. Overall, eight ongoing clinical trials and 21 studies were excluded with reasons outlined in Excluded studies. Therefore, we finally included a total of 23 studies. A flow diagram of the study selection is presented (see Figure 1).
1.
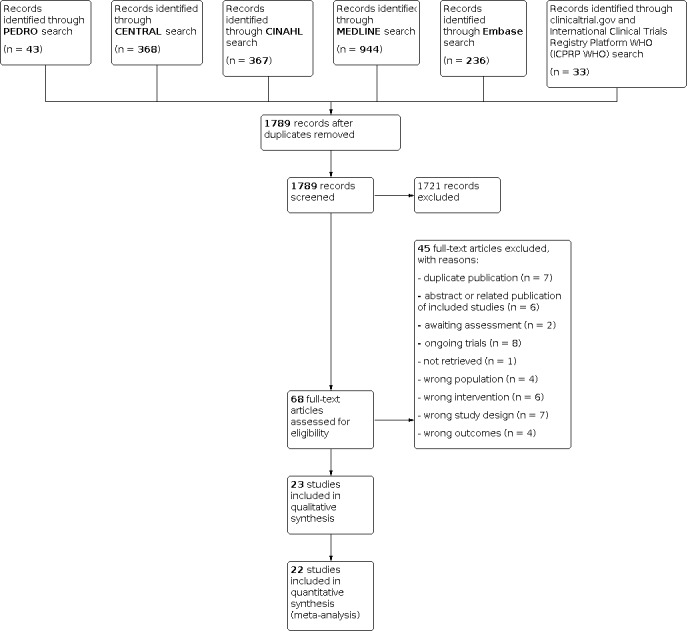
Study flow diagram
Included studies
In total, 23 studies (with 1054 participants) were included in the review. A full description of the characteristics of the included studies is provided in the Characteristics of included studies table.
We contacted the corresponding authors of seven trials for additional information on including outcome data (De Oliveira 2021; Devereaux 2016; Gandhi 2016; Kaya 2011; Miccinilli 2018; Miller 2009; Thelen 2008). We received responses and useful data from two of the authors (De Oliveira 2021; Miccinilli 2018). One author (Gandhi 2016) answered our request but did not have useful data for quantitative analysis.
Participants
A total of 1054 participants were enrolled in the 23 trials. There were more women (N = 464, 52%) than men (N = 421, 48%). Three trials did not report gender (Hsu 2009; Kaya 2011; Pekyavas 2016). The mean/median age of the patients ranged from a minimum of 20 years (Gandhi 2016; Thelen 2008) to a maximum of 62.5 years (Miccinilli 2018), with the majority between 18 and 50 years. Percentages of patients’ withdrawals or dropouts ranged from a minimum of 0% (Gandhi 2016; Sikha 2017; Shakeri 2013) to a maximum of 30.6% (Jena Etnoyer‐Slaski 2016), with a mean attrition value of 8%.
Sixteen trials considered patients with a diagnosis of impingement (Devereaux 2016; Gandhi 2016; Gençbay 2019; Hsu 2009; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2011; Kaya 2014; Keenan 2017; Kocyigit 2016; Miller 2009; Mohamed 2019; Pekyavas 2016; Shakeri 2013; Sikha 2017; Simsek 2013), two trials included patients with a rotator cuff disease diagnosis (De Oliveira 2021; Miccinilli 2018) and three trials considered both impingement and rotator cuff disease diagnoses (Goksu 2016; Kul 2018; Thelen 2008). Three trials (13%) included patients with other shoulder disorders (Frassanito 2018; Jena Etnoyer‐Slaski 2016; Kang 2020).
The main reported inclusion criteria were as follows:
Pain characteristics:
pain onset prior to 150° of active shoulder elevation in any plane (Goksu 2016; Kaya 2011; Kang 2020; Sikha 2017; Thelen 2008);
pain interfering with the patient’s daily routine (Gençbay 2019; Frassanito 2018; Kang 2020; Kaya 2011; Miller 2009; Sikha 2017; Simsek 2013; Thelen 2008);
specific intervals on Visual Analogic Scale: a score of at least 5 out of 10 (Pekyavas 2016); a score between 2 ‐7 (Kocyigit 2016).
Pain temporal criteria:
pain on the day of testing (Keenan 2017);
shoulder pain that had continued for more than one week during the last six months prior to the study (Hsu 2009; Shakeri 2013);
pain lasting for one month or longer (Gençbay 2019; Simsek 2013; Subasi 2016);
pain which had been ongoing for 1‐3 months (subacute) (Devereaux 2016; Goksu 2016);
pain for a minimum of two weeks (Frassanito 2018; Keenan 2017);
pain of more than six‐weeks duration (Miller 2009).
Positivity at radiological examination (Devereaux 2016; Frassanito 2018; Goksu 2016; Kul 2018; Miccinilli 2018; Subasi 2016).
-
Manual tests positivity
Painful arc during active shoulder elevation (De Oliveira 2021; Devereaux 2016; Gençbay 2019; Hsu 2009; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Shakeri 2013; Subasi 2016);
Hawkins test (De Oliveira 2021; Devereaux 2016; Goksu 2016; Hsu 2009; Kang 2020; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Miccinilli 2018; Miller 2009; Shakeri 2013; Sikha 2017; Simsek 2013; Subasi 2016; Thelen 2008);
Neer test (De Oliveira 2021; Frassanito 2018; Gençbay 2019; Hsu 2009; Kang 2020; Keenan 2017; Kocyigit 2016; Kul 2018; Miccinilli 2018; Shakeri 2013; Sikha 2017; Simsek 2013; Subasi 2016);
Yocum test (Frassanito 2018; Shakeri 2013);
Empty can test Jobe (De Oliveira 2021; Frassanito 2018; Goksu 2016; Hsu 2009; Kang 2020; Kaya 2011; Kocyigit 2016; Miccinilli 2018; Sikha 2017; Shakeri 2013; Subasi 2016; Thelen 2008);
Full can test Jobe (Frassanito 2018);
External rotation resistant test (De Oliveira 2021; Kang 2020; Kaya 2014; Miccinilli 2018);
Drop sign (Kul 2018).
Intervention and comparisons
Nine studies, with a total of 312 participants, focused on the efficacy of kinesio taping versus sham taping (Hsu 2009; Kang 2020; Keenan 2017; Kocyigit 2016; Jena Etnoyer‐Slaski 2016; Miccinilli 2018; Shakeri 2013; Simsek 2013; Thelen 2008). In particular, five trials investigated the effect of kinesio taping alone versus sham therapy (Hsu 2009; Keenan 2017; Jena Etnoyer‐Slaski 2016; Kocyigit 2016 Shakeri 2013; Thelen 2008), while four studies investigated the effect of kinesio taping with a co‐intervention (general rehabilitative program/exercise) versus sham taping with the same co‐intervention, three provided a general rehabilitative program/exercise (Miccinilli 2018; Kang 2020; Simsek 2013) and one assessed exercise plus paracetamol/NSAIDs (Kocyigit 2016).
Fourteen studies, with a total of 742 participants, focused on the efficacy of kinesio taping versus a conservative treatment. Among these, seven studies assessed the effect of kinesio taping with a co‐intervention versus a conservative treatment alone (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Miller 2009; Pekyavas 2016; Sikha 2017). In particular, one study assessed the effect of kinesio taping with exercise versus exercise alone (Devereaux 2016); one study assessed the effect of kinesio taping combined with myofascial release therapy versus myofascial release therapy alone (Gandhi 2016); three studies assessed the effect of kinesio taping combined with a routine physiotherapy/rehabilitative program versus a routine physiotherapy/rehabilitative program alone (De Oliveira 2021; Miller 2009; Sikha 2017); one study assessed the effect of kinesio taping combined with exercise versus exercise alone (Pekyavas 2016); and, one study assessed the effect of kinesio taping combined with extracorporeal shock wave therapy versus extracorporeal shock wave therapy alone (Frassanito 2018). The remaining seven studies assessed the effect of kinesio taping with a co‐intervention versus a conservative treatment with the same co‐intervention as the experimental group (Gençbay 2019; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Mohamed 2019; Subasi 2016). In particular, one study assessed the effect of kinesio taping combined with a home exercise program versus subacromial injections (betamethasone (sodium phosphate and acetate) (1 cc) plus prilocaine (4 cc)) combined with the same home exercise program (Subasi 2016); one study investigated the effect of kinesio taping combined with a home exercise program versus subacromial steroid injections (corticosteroid injection of triamcinolone acetonide and bupivacaine) with a home exercise program (Goksu 2016); two studies assessed the effect of kinesio taping combined with exercise versus manual therapy with exercise (Kaya 2014; Mohamed 2019); two studies assessed the effect of kinesio taping combined with a home exercise program versus physical therapy modalities with the home exercise program (Kaya 2011; Kul 2018); and one study assessed the effect of kinesio taping combined with extracorporeal shock wave therapy versus exercise and extracorporeal shock wave therapy (Gençbay 2019).
Overall, we included nine studies in the kinesio taping versus sham taping comparison and fourteen studies in the kinesio taping versus conservative intervention comparison.
The included studies addressed the following comparisons:
KT vs sham taping. In this comparison, we included studies that explicitly used sham taping in the control group (with or without a co‐intervention in the experimental and control group).
KT vs other conservative interventions (e.g. conventional taping, physical therapies, exercise, glucocorticoid injection, oral medication, or other interventions). In this group, we included studies that compared KT with or without a co‐intervention vs conservative treatment with or without a co‐intervention.
See Table 3 for the composition of experimental and control groups in the included studies.
1. Composition of experimental and control groups of included studies.
| Comparison 1. Kinesio taping versus sham taping | ||||
| Experimental group | Control group | |||
| Author | Experimental | Co‐intervention | Control | Co‐intervention |
| Thelen 2008 | Kinesio taping | None | Sham taping | None |
| Hsu 2009 | Kinesio taping | None | Sham taping | None |
| Keenan 2017 | Kinesio taping | None | Sham taping | None |
| Kocyigit 2016 | Kinesio taping | Exercise/paracetamol/NSAIDs | Sham taping | Exercise/paracetamol/NSAIDs |
| Simsek 2013 | Kinesio taping | Exercise | Sham taping | Exercise |
| Miccinilli 2018 | Kinesio taping | Rehabilitative protocol | Sham taping | Rehabilitative protocol |
| Jena Etnoyer‐Slaski 2016 | Kinesio taping | None | Sham taping | None |
| Shakeri 2013 | Kinesio taping | None | Sham taping | None |
| Kang 2020 | Kinesio taping | Exercise | Sham taping | Exercise |
| Comparison 2. Kinesio taping versus conservative treatment | ||||
| Experimental group | Control group | |||
| Author | Experimental | Co‐intervention | Control | Co‐intervention |
| Devereaux 2016 | Kinesio taping | Exercise | Exercise | None |
| Frassanito 2018 | Kinesio taping | Extracorporeal Shock Wave Therapy (ESWT) | Extracorporeal Shock Wave Therapy (ESWT) | None |
| Gandhi 2016 | Kinesio taping | Myofascial release therapy | Myofascial release therapy | None |
| Goksu 2016 | Kinesio taping | Home exercise program | Steroid injection ((1 cc triamcinolone acetonide ‐ 40 mg) and 4 cc bupivacaine) | Home exercise program |
| Kaya 2014 | Kinesio taping | Exercise | Manual therapy | Exercise |
| Kaya 2011 | Kinesio taping | Home exercise program (HEP) | Physical therapy modalities | Home exercise program (HEP) |
| Kul 2018 | Kinesio taping | Home exercise program (HEP) | Physical therapies modalities | Home exercise program (HEP) |
| Miller 2009 | kinesio taping | Routine physiotherapy | Routine physiotherapy | None |
| Pekyavas 2016 | Group a: Kinesio taping | Exercise | Exercise | None |
| Pekyavas 2016 | Group b: Kinesio taping | Exercise, manual therapy | ||
| Pekyavas 2016 | Group c: Kinesio taping | Exercise, manual therapy, high‐intensity laser therapy | ||
| Subasi 2016 | Kinesio taping | Home exercise program (HEP) | Injection (betamethasone (sodium phosphate and acetate) (1 cc) plus prilocaine (4 cc)) | Home exercise program (HEP) |
| De Oliveira 2021 | Kinesio taping | Rehabilitative program | Rehabilitative program | None |
| Gençbay 2019 | Kinesio taping | Exercise | Extracorporeal Shock Wave Therapy (ESWT) | Exercise |
| Mohamed 2019 | Kinesio taping | Supervised exercise | Manual therapy | Supervised exercise |
| Sikha 2017 | Kinesio taping | Conventional therapy | Conventional therapy | None |
Taping technique
Seventeen studies adhered to specific taping techniques (See Table 4 and Table 5):
2. Kinesio taping intervention characteristics in included studies.
| Study | Taping Technique | Size | Target muscle | N° applications | Duration of treatment | Provider |
| De Oliveira 2021 | Kase | 5 cm Elastic Kinesio® Tex Classic | 1) Supraspinatus 2) Deltoid 3) Trapezius | 10 | 3 dd | Certified PT |
| Devereaux 2016 | Spider | Not reported | Not reported | 4 | 3‐5 dd | Registered physiotherapist who had received training in the application technique of the tape |
| Frassanito 2018 | Alternative technique | Not reported | 1) Deltoid 2) Supraspinatus | 3 | 3 dd | Not reported |
| Gandhi 2016 | Alternative technique | Not reported | 1) Deltoid | 18 | 2 dd | Not reported |
| Gençbay 2019 | Kase | Kinesio Tex | 1) Supraspinatus 2) Deltoid 3) Glenohumeral articulation | 6 | 3/4 dd | Not reported |
| Goksu 2016 | Kase | Standard 5 cm beige Kinesio Tex tape | 1) Supraspinatus 2) Deltoid 3) Coracoid process | 3 | 3 dd | Physician (PB) |
| Hsu 2009 | Kase | 5 cm x 28 cm piece of Kinesio tape | Lower trapezius | 1 | Immediate | Not reported |
| Jena Etnoyer‐Slaski 2016 | Alternative technique | Not reported | Supraspinatus and infraspinatus | Not reported | Not reported | Clinician |
| Kang 2020 | Alternative technique | Not specified | 1) Trapezius 2) Trapezius 3) Glenohumeral articulation | 8 | 2/3 dd | Not reported |
| Kaya 2011 | Kase | Standard 2 in (5 cm) | All techniques were identified according to the tissue that was in need of help. | 6 | 4‐5 dd | The secondary author (GB) applied the taping |
| Kaya 2014 | Kase | Not reported | 1) supraspinatus 2) deltoids 3) teres minor | 3 | 3 dd | The first author applied the taping. |
| Keenan 2017 | Kase | 2 inch | 1) Supraspinatus 2) Deltoid 3) Coracoid process | 1 | Immediate | The first author applied the taping. |
| Kocyigit 2016 | Alternative technique | Not reported | 1) Deltoid 2) Deltoid 3) ACJ articulation | 3 | 4 dd | Not reported |
| Kul 2018 | Kase | Not reported | 1) Deltoid 2) Supraspinatus | 3 | 5 dd | Not reported |
| Miccinilli 2018 | Kase | Not reported | 1) Deltoid 2) Glenohumeral articulation 3) Rhomboid | 6 | 2 dd | Physiotherapist |
| Miller 2009 | Scapular taping | An initial tape layer comprised a 50 mm hypoallergenic polyacrylate adhesive non‐woven bandage over which was laid a 38 mm premium non‐elastic zinc oxide adhesive tape. | 1) Deltoid 2) Lower trapezius | 6 | 2 dd | Education sessions were provided to treating physiotherapists to attain agreement on range of acceptable treatment options. |
| Mohamed 2019 | Kase | Not specified | 1) Supraspinatus 2) Deltoid 3) Glenohumeral articulation | 12 | 3/4 dd | Not reported |
| Pekyavas 2016 | Kase | Not reported | 1) Deltoid 2) Supraspinatus 3) Glenohumeral articulation | 5 | 3 dd | Not reported |
| Shakeri 2013 | Kase | Standard 2 in (5 cm) beige Kinesio TexTM tape | 1) Supraspinatus 2) Deltoid 3) Glenohumeral articulation 4) Lower trapezius | 2 | 2/3 dd | Clinician |
| Sikha 2017 | Kase | Not specified | 1) Supraspinatus 2) Deltoid 3) Glenohumeral articulation | Not reported | Not reported | Not reported |
| Simsek 2013 | Kase | 5 cm | 1) Deltoid 2) Supraspinatus | 4 | 3 dd | Certified Physiotherapist |
| Subasi 2016 | Kase | 5 cm Elastic Kinesio® Tex Gold tapes | 1) Supraspinatus 2) Deltoid 3) Glenohumeral articulation | 3 | 5 dd | Kinesio tapes were applied by the same physiotherapist. |
| Thelen 2008 | Kase | 2 in (5 cm) | 1) Supraspinatus 2) Deltoid 3) Glenohumeral articulation | 2 | 6 d | Certified KT practitioner |
3. TIDieR checklist.
| 1) Is it clear where the intervention was delivered? | 2) Is it clear who received the intervention? | 3) Is it clear who delivered the intervention? | 4) Is it clear the schedule of the intervention? | 5) Is it clear the intensity of the intervention? | 6) Is the procedure (including the sequencing of the technique) of the intervention sufficiently clear? | 7) Are the physical or informational materials used adequately described? | |
| First author | yes/no | Yes/no/not stated | Yes/no/not stated | Yes/no/not stated | Yes/no/not stated | Yes/no/not stated | Yes/no/not stated |
| De Oliveira 2021 | yes | yes | yes | yes | yes | yes | yes |
| Devereaux 2016 | not stated | yes | yes | yes | yes | yes | yes |
| Frassanito 2018 | yes | yes | not stated | yes | yes | yes | yes |
| Gandhi 2016 | not stated | yes | not stated | no | no | no | no |
| Gençbay 2019 | yes | yes | not stated | yes | yes | yes | yes |
| Goksu 2016 | not stated | yes | yes | no | no | yes | yes |
| Hsu 2009 | not stated | yes | not stated | yes | no | yes | yes |
| Jena Etnoyer‐Slaski 2016 | yes | yes | no | not stated | not stated | no | no |
| Kang 2020 | yes | yes | not stated | yes | yes | yes | yes |
| Kaya 2014 | yes | yes | yes | yes | yes | yes | yes |
| Kaya 2011 | not stated | yes | yes | no | no | yes | no |
| Keenan 2017 | no | yes | yes | no | no | yes | yes |
| Kocyigit 2016 | not stated | yes | yes | yes | yes | yes | not stated |
| Kul 2018 | no | yes | not stated | yes | not stated | not stated | not stated |
| Miccinilli 2018 | yes | yes | yes | no | yes | no | not stated |
| Miller 2009 | yes | yes | yes | yes | yes | not stated | yes |
| Mohamed 2019 | yes | yes | not stated | yes | yes | yes | yes |
| Pekyavas 2016 | yes | yes | yes | no | not stated | yes | not stated |
| Shakeri 2013 | no | yes | not stated | no | no | yes | yes |
| Sikha 2017 | yes | yes | not stated | not stated | yes | yes | yes |
| Simsek 2013 | not stated | yes | yes | yes | yes | no | yes |
| Subasi 2016 | yes | yes | yes | yes | yes | yes | yes |
| Thelen 2008 | yes | yes | yes | yes | yes | yes | yes |
In sixteen studies, with a total of 731 participants, application was consistent with the protocol for rotator cuff tendonitis/impingement suggested by Kase and colleagues (De Oliveira 2021; Gençbay 2019; Goksu 2016; Hsu 2009; Kaya 2011; Kaya 2014; Keenan 2017; Kul 2018; Miccinilli 2018; Mohamed 2019; Pekyavas 2016; Shakeri 2013; Sikha 2017; Simsek 2013; Subasi 2016; Thelen 2008);
One study, with 100 participants, followed the SpiderTech taping technique (Devereaux 2016).
Application target
Muscles/structures targeted by taping procedures (See Table 5):
Deltoid in seventeen studies (De Oliveira 2021; Devereaux 2016; Gandhi 2016; Gençbay 2019; Hsu 2009; Jena Etnoyer‐Slaski 2016; Kaya 2011; Kaya 2014; Kul 2018; Miccinilli 2018; Miller 2009; Mohamed 2019; Pekyavas 2016; Shakeri 2013; Sikha 2017; Simsek 2013; Thelen 2008);
Supraspinatus in sixteen studies (De Oliveira 2021; Gandhi 2016; Gençbay 2019; Hsu 2009; Jena Etnoyer‐Slaski 2016; Kaya 2011; Kaya 2014; Kocyigit 2016; Kul 2018; Miccinilli 2018; Mohamed 2019; Shakeri 2013; Sikha 2017; Simsek 2013; Subasi 2016; Thelen 2008);
Glenohumeral articulation in nine studies (Gençbay 2019; Hsu 2009; Kang 2020; Kaya 2014; Kocyigit 2016; Kul 2018; Mohamed 2019; Sikha 2017; Thelen 2008);
Lower trapezius in five studies (Devereaux 2016; Frassanito 2018; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2014);
Coracoid process in two studies (Gandhi 2016; Simsek 2013);
Rhomboid in one study (Kocyigit 2016);
Teres minor in one study (Kaya 2011);
Infraspinatus in one study (Subasi 2016);
Acromioclavicular joint articulation in one study (Pekyavas 2016);
In one study, taping procedures were defined according to the participant's need (Goksu 2016).
Intervention provider
Thirteen studies, with a total of 649 participants, reported taping procedures provided by a clinician (De Oliveira 2021; Devereaux 2016; Goksu 2016; Jena Etnoyer‐Slaski 2016; Kaya 2011; Kaya 2014; Keenan 2017; Miccinilli 2018; Miller 2009; Shakeri 2013; Simsek 2013; Subasi 2016; Thelen 2008), six studies specified that taping procedures were provided by the same clinician (Goksu 2016; Kaya 2011; Kaya 2014; Keenan 2017; Miccinilli 2018; Subasi 2016) and five specified that taping procedures were provide by a certified/trained physiotherapist (De Oliveira 2021; Devereaux 2016; Miller 2009; Simsek 2013; Thelen 2008) (See Table 5).
Number of applications
The number of applications varied considerably across studies, ranging from one (Keenan 2017) to 18 applications (Gandhi 2016), with the majority between three and six applications (See Table 5).
Application duration
The duration of each tape application ranged from immediate removal (Hsu 2009; Keenan 2017) to six days (Thelen 2008), with the majority between three and five days of duration (See Table 5).
Outcomes
All studies considered pretreatment and post‐treatment outcome measures. In particular, outcomes were assessed at the following follow‐up: post‐treatment at three days (Shakeri 2013; Thelen 2008), five days (Simsek 2013), six days (Thelen 2008), 12 days (Kocyigit 2016; Simsek 2013), 15 days (Kul 2018; Miccinilli 2018; Pekyavas 2016), one week (Frassanito 2018; Goksu 2016; Jena Etnoyer‐Slaski 2016; Kaya 2011; Shakeri 2013), two weeks (Devereaux 2016; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2011; Miller 2009), three weeks (De Oliveira 2021; Gençbay 2019; Jena Etnoyer‐Slaski 2016), four weeks (Frassanito 2018; Goksu 2016; Jena Etnoyer‐Slaski 2016; Kang 2020; Kocyigit 2016; Kul 2018; Subasi 2016; Sikha 2017), six weeks (De Oliveira 2021; Gandhi 2016; Kaya 2014; Miller 2009; Mohamed 2019), twelve weeks (Frassanito 2018; Gençbay 2019; Subasi 2016;) and six months (De Oliveira 2021).
Major outcomes
-
Overall pain:
VAS: three studies (Frassanito 2018; Kang 2020; Mohamed 2019);
NRS: two studies (Gandhi 2016; Jena Etnoyer‐Slaski 2016);
Brief Pain Inventory (BPI): one study (De Oliveira 2021);
Pain subscore SPADI: two studies (Pekyavas 2016; Subasi 2016);
Percentage of improved patients: one study (Gençbay 2019).
-
Function:
SPADI: seven studies (Gandhi 2016; Goksu 2016; Miller 2009; Mohamed 2019; Pekyavas 2016; Subasi 2016; Thelen 2008);
Constant Score: five studies (Devereaux 2016; Kocyigit 2016; Kul 2018; Miccinilli 2018; Simsek 2013);
DASH: six studies (De Oliveira 2021; Frassanito 2018; Gençbay 2019; Kaya 2011; Kaya 2014; Simsek 2013);
WORC: two studies (De Oliveira 2021; Kul 2018);
SST: one study (Devereaux 2016);
Short Form Self‐Regulation Questionnaire (SSRQ): one study (Frassanito 2018);
Oxford Shoulder Score (OSS: one study (Frassanito 2018);
American Shoulder and Elbow Surgeons (ASES‐100): one study (Kul 2018));
Self‐reported flexi‐level scale of shoulder function (FLEX‐SF): one study (Kang 2020);
Penn Shoulder Score (PSS): two studies (Jena Etnoyer‐Slaski 2016; Sikha 2017).
-
Pain on motion:
VAS: nine studies (Goksu 2016; Kaya 2011; Kaya 2014; Kocyigit 2016; Kul 2018; Miller 2009; Shakeri 2013; Simsek 2013; Subasi 2016);
NRS: two studies (Devereaux 2016; Miccinilli 2018).
-
Active range of motion (free of pain):
Conventional goniometer: five studies (Goksu 2016; Shakeri 2013; Simsek 2013; Sikha 2017; Thelen 2008);
Digital inclinometer: one study (De Oliveira 2021).
-
Global assessment of treatment success:
Global rating of change: one study (De Oliveira 2021).
-
Quality of life:
SF‐12: one study (Sikha 2017);
Nottingham Health Profile (NHP): one study (Kocyigit 2016).
Adverse events: ten studies (Devereaux 2016; Frassanito 2018; Goksu 2016; Hsu 2009; Jena Etnoyer‐Slaski 2016; Kaya 2011; Kocyigit 2016; Kul 2018; Miller 2009; Thelen 2008).
Minor outcomes
-
Pain at night:
VAS: five studies (Kaya 2011; Kaya 2014; Kocyigit 2016; Kul 2018; Simsek 2013).
-
Pain at rest:
VAS: five studies (Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Simsek 2013);
Numerical Pain rating score (NPRS): two studies (Devereaux 2016; Miccinilli 2018).
-
Muscle strength:
Medical Research Council (MRC) Scale for Muscle Strength: one study (Miccinilli 2018);
Isokinetic dynamometry: one study (Keenan 2017);
Hand dynamometer: one study (Simsek 2013).
Withdrawals or dropouts: proportion who withdrew from treatment due to adverse events or other reasons. Seventeen studies reported data regarding withdrawal or dropouts (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Goksu 2016; Hsu 2009; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2011; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Miccinilli 2018; Miller 2009; Shakeri 2013; Thelen 2008).
Funding and conflict of interest
Two (9%) trials were rated as having high risk of bias because of potential conflict of interest in study funding (Devereaux 2016; Jena Etnoyer‐Slaski 2016) and five (22%) studies did not report any funding or conflict of interest, being rated as unclear risk of bias (De Oliveira 2021; Gençbay 2019; Goksu 2016; Miccinilli 2018; Pekyavas 2016; Shakeri 2013; Sikha 2017).
Excluded studies
Overall, eight ongoing clinical trials and 21 studies were excluded for various reasons (see Characteristics of excluded studies): the intervention was ineligible (n = 6), the clinical condition and/or population were ineligible (n = 4), the outcome of interest was not measured (n = 4), or wrong study design (n = 2). We have listed the excluded full‐text articles (excluding the conference proceedings) in the table of Characteristics of excluded studies.
Risk of bias in included studies
A summary of the risk of bias in included trials is presented in Figure 2 and Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
The methods of sequence generation and allocation concealment were respectively rated as being at low risk of bias in six (26%) trials (De Oliveira 2021; Devereaux 2016; Kaya 2014; Miller 2009; Pekyavas 2016; Thelen 2008) and in eight (35%) trials (De Oliveira 2021; Frassanito 2018; Gandhi 2016; Goksu 2016; Kang 2020; Miccinilli 2018; Miller 2009; Thelen 2008). Only three (16%) trials used appropriate methods to both generate and conceal the allocation sequence (De Oliveira 2021; Miller 2009; Thelen 2008), and so were rated at low risk of allocation bias for both these methods. We rated only one (5%) trial at high risk of allocation bias because the allocator was aware of the randomisation scheme (Kaya 2011) and two trials were rated at high risk of random sequence generation bias because sequences were not generated randomly (Kaya 2011; Keenan 2017).
Group similarity at baseline was rated as being at low risk of bias in 14 (74%) trials (Devereaux 2016; Frassanito 2018; Goksu 2016; Hsu 2009; Kaya 2011; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Miccinilli 2018; Pekyavas 2016; Simsek 2013; Subasi 2016; Thelen 2008).
One (5%) study was rated as being at high risk of selection bias, because of discrepancies at baseline between groups (Miller 2009). We rated four (21%) trials at unclear risk of selection bias due to lack of data (De Oliveira 2021; Gandhi 2016; Jena Etnoyer‐Slaski 2016; Shakeri 2013).
Blinding
Blinding
In KT studies, blinding of participants and care providers from treatment allocation was rare due to the nature of the intervention.
Performance bias
Blinding of personnel was rated as being at high risk in all except six studies (26%) in which the risk was unclear (Gençbay 2019; Kul 2018; Mohamed 2019; Sikha 2017; Simsek 2013; Subasi 2016). We rated blinding of participants (performance bias) as being at low risk for five (22%) studies (Hsu 2009; Keenan 2017; Kocyigit 2016; Shakeri 2013; Thelen 2008); unclear risk for eight (35%) studies (De Oliveira 2021; Gençbay 2019; Kul 2018; Miccinilli 2018; Mohamed 2019; Sikha 2017; Simsek 2013; Subasi 2016); and high risk for ten (43%) studies (Devereaux 2016; Frassanito 2018; Gandhi 2016; Goksu 2016; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2011; Kaya 2014; Miller 2009; Pekyavas 2016). Overall, we rated risk of performance bias as high (Figure 2).
Detection bias
For detection bias, we assessed self‐reported and assessor‐reported outcomes separately. Not all trials used a combination of both kinds of outcomes. While completing the risk of bias tool, we were unable to insert 'not applicable' or to leave the section blank (indicating that the outcome was not measured), thus, in such cases, we specified the rating as 'low risk' and inserted the comment 'no objective outcome planned and assessed'.
For self‐reported outcomes, we rated 10 (43%) studies as being at high risk of bias (Devereaux 2016; Frassanito 2018; Gandhi 2016; Goksu 2016; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2011; Kaya 2014; Miller 2009; Pekyavas 2016).
For assessor‐reported outcomes, 19 (83%) studies reported appropriate outcome measurements and were therefore rated as being at low risk of bias (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Hsu 2009; Jena Etnoyer‐Slaski 2016; Kang 2020; Kaya 2011; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Miccinilli 2018; Miller 2009; Pekyavas 2016; Shakeri 2013; Simsek 2013; Subasi 2016; Thelen 2008).
We rated five additional studies as being at low risk for this domain, however, these should actually be rated as 'not applicable' because the outcome was not planned and assessed (Devereaux 2016; Frassanito 2018; Gandhi 2016; Kaya 2011; Kaya 2014). One study did not report the methods for measuring the objective outcome and the risk of bias was rated as unclear (Goksu 2016). Overall, we rated detection bias to be at low risk (Figure 2).
Incomplete outcome data
Fifteen (65%) trials either had no dropouts, losses to follow‐up or exclusions, or had a small amount of attrition that was deemed unlikely to bias the results (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Goksu 2016; Hsu 2009; Kang 2020; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Miccinilli 2018; Pekyavas 2016; Shakeri 2013; Sikha 2017; Thelen 2008). In three (13%) trials, there was differential dropout across groups, with reasons that appeared to be related to the treatments received, and thus we rated these trials as being at high risk of attrition bias (Jena Etnoyer‐Slaski 2016; Kaya 2011; Miller 2009). In the remaining five (22%) trials, there was no information for judgement so the risk of attrition bias was unclear (Gandhi 2016; Gençbay 2019; Mohamed 2019; Simsek 2013; Subasi 2016).
Selective reporting
We rated only one (4%) trial at low risk of selective reporting bias because all outcomes specified in the trial registry entry or the trial protocol were fully reported in the trial publication (Jena Etnoyer‐Slaski 2016). We rated four (17%) trials at high risk of selective reporting bias because data for at least one outcome that was listed in the trial registry entry or the methods section of the publication were not reported in the results section at all (De Oliveira 2021; Kang 2020; Miccinilli 2018; Subasi 2016). We rated the remaining 18 (78%) trials at unclear risk of selective reporting bias because even if outcome data were completely reported for all outcomes specified in the methods section of the publication, none of these trials was registered in a trials registry or had an available trial protocol (Devereaux 2016; Frassanito 2018; Gandhi 2016; Gençbay 2019; Goksu 2016; Hsu 2009; Kaya 2011; Kaya 2014; Keenan 2017; Kocyigit 2016; Kul 2018; Miller 2009; Mohamed 2019; Pekyavas 2016; Shakeri 2013; Sikha 2017; Simsek 2013; Thelen 2008).
Overall, publication bias was detected for function, Figure 4. However, we found several RCTs without outcome data available for performing meta‐analyses, thus, in the GRADE assessment, we graded this lack of information as selective publication and selective non‐reporting (Page 2018a).
4.

Funnel plot of comparison 10: kinesio taping versus other conservative treatment, outcome: 10.2 function
Other potential sources of bias
Unequal use of co‐intervention
Overall, no unequal use of co‐interventions was detected among the included trials. Only one trial ( Pekyavas 2016) assessed the effect of kinesio taping in a multi‐arm trial with more than one co‐intervention compared to exercise alone.
Effects of interventions
Kinesio taping versus sham taping within 30 days from the end of treatment
We used the final values rather than change from baseline values for major and minor outcomes.
Major outcomes
Three studies provided data for overall pain (Jena Etnoyer‐Slaski 2016; Kang 2020; Kocyigit 2016), six studies for function (Jena Etnoyer‐Slaski 2016; Kang 2020; Kocyigit 2016; Miccinilli 2018; Shakeri 2013; Simsek 2013), four studies for pain on motion (Kocyigit 2016; Miccinilli 2018; Shakeri 2013; Simsek 2013), and three studies for active range of motion (Shakeri 2013; Simsek 2013; Thelen 2008). No studies reported data for global assessment of treatment success and quality of life. Four studies provided data for adverse events (Hsu 2009; Jena Etnoyer‐Slaski 2016; Kocyigit 2016; Thelen 2008).
Overall pain
Three studies provided data for overall pain (Jena Etnoyer‐Slaski 2016; Kang 2020; Kocyigit 2016) including a total of 106 participants. Results showed no statistically significant reduction of overall pain in the kinesio taping group compared to sham taping (mean difference (MD) 0.07, 95% confidence interval (CI) (0.77 better to 0.9 worse), absolute difference (0.7% worse, 7.7% better to 9% worse), and relative percent change (2% worse, 21% better to 24% worse, Analysis 1.1). Assuming a minimal clinically important difference of 1.5 points, this finding was not clinically relevant. Heterogeneity analysis demonstrated substantial heterogeneity (Tau² = 0.29; Chi² = 4.27, df = 2 (P = 0.12); I² = 53%). Very low‐certainty evidence downgraded for bias, imprecision and indirectness showed that we are uncertain if kinesio taping reduced overall pain at four weeks compared with sham taping.
1.1. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 1: Overall pain
Function
Seven studies reported function (Jena Etnoyer‐Slaski 2016; Kang 2020; Kocyigit 2016; Miccinilli 2018; Shakeri 2013; Simsek 2013; Thelen 2008) with six reporting useful data, including a total of 214 participants. Results showed a statistically significant reduction of disability in the kinesio taping group compared to sham taping (SMD ‐0.49 [‐1.28, 0.30], absolute difference (8% better, 21% better to 5% worse), and relative percentage change (15% better, 40% better to 9% worse), Analysis 1.2). Assuming a minimal clinically important difference of 10.2 points, this finding (MD ‐8.05, 95% CI (4.93 worse to 21.02 better)) is not clinically relevant. Heterogeneity analysis demonstrated substantial evidence of heterogeneity (Tau² = 0.84; Chi² = 37.16, df = 5 (P = 0.00001); I² = 87%). Very low‐certainty evidence downgraded for bias, imprecision, inconsistency and indirectness shows that we are uncertain whether KT improves function compared to sham taping at four weeks.
1.2. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 2: Function
Pain on motion
Four studies reported useful data for pain on motion (Kocyigit 2016; Miccinilli 2018; Shakeri 2013; Simsek 2013), including a total of 153 participants. Results showed a statistically significant reduction of pain on motion in the kinesio taping group compared to sham taping (MD ‐1.48, 95% CI (2.25 better to 0.71 better), Analysis 1.3)) absolute difference (14.8% better, 22.5% better to 7.1% better), and relative percent change (30% better, 45% better to 14% better). Assuming a minimal clinically important difference of 2.1 points, this improvement could not be considered clinically important. Heterogeneity analysis demonstrated no heterogeneity (Chi² = 1.47, df = 3 (P = 0.69); I² = 0%). Very low‐certainty evidence downgraded for bias, imprecision and indirectness at four weeks suggests we are uncertain whether KT reduces pain on motion when compared with sham taping.
1.3. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 3: Pain on motion
Active range of motion (AROM) ‐ without pain (shoulder abduction and flexion)
Three studies reported active range of motion – free of pain (Shakeri 2013; Simsek 2013; Thelen 2008). Among these, two trials (Shakeri 2013; Simsek 2013) provided useful information for active range of motion (shoulder flexion and shoulder abduction) without pain for a total of 68 participants. Results showed no statistically significant improvements in active range of motion for shoulder abduction (mean difference (MD) 10.23, 95% CI (16.09 worse to 36.56 better; I² = 90%), Analysis 1.4), absolute difference (5.7% better, 8.9% worse to 20.3% better), and relative percent change (6% better, 10% worse to 22% better). Assuming that an improvement of 10% is clinically important, this finding could not be considered clinically relevant. There was a statistically significant worsening with KT in the active range of motion for shoulder flexion without pain (MD ‐4.12, 95% CI ‐6.10 to ‐2.13; I² = 0%); but this also did not reach the level of a clinically important difference. Considering active range of motion without pain for shoulder abduction as a proxy for the outcome, very low‐certainty evidence downgraded for publication bias, inconsistency and imprecision at two weeks showed that we are uncertain about the effect of KT when compared with sham taping for AROM without pain.
1.4. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 4: AROM without pain (shoulder abduction and flexion)
Global assessment of treatment success
No studies were found for global assessment of treatment success.
Quality of life
One study (Kocyigit 2016) reported data for quality of life using the Nottingham Health Profile Assessment (NHP). Data were available but divided into six subscales: (1) sleep; (2) mobility; (3) energy; (4) pain; (5) emotional reactions; and (6) social isolation. None of the subscale items was indicated as a proxy of the overall quality assessment, thus, no data were included in the summary of findings table.
Adverse events
Four studies reported data for adverse events (Hsu 2009; Jena Etnoyer‐Slaski 2016; Kocyigit 2016; Thelen 2008). Overall, three adverse events were reported by two studies: two events of mild non‐pruritic rash in Thelen 2008 (referring group was not specified) and one event of pruritic rash in the sham control group in Kocyigit 2016. Two studies reported no adverse events (Hsu 2009; Jena Etnoyer‐Slaski 2016). Five studies did not collect data on adverse events (Kang 2020; Keenan 2017; Miccinilli 2018; Shakeri 2013; Simsek 2013). Due to a paucity of information, data were not meta‐analysed. We are uncertain about the adverse events of kinesio taping compared to sham taping (very low‐certainty evidence).
Minor outcomes
Two studies reported the effect of kinesio taping on the minor outcomes of overall pain at rest (Miccinilli 2018; Simsek 2013), three studies reported pain at night (Kocyigit 2016; Shakeri 2013; Simsek 2013), and muscle strength was measured in three studies (Keenan 2017; Miccinilli 2018; Simsek 2013). Six studies provided data for all‐cause withdrawals or dropouts (Hsu 2009; Keenan 2017; Kocyigit 2016; Miccinilli 2018; Shakeri 2013; Thelen 2008).
Other measures of pain: such as, pain at night and pain at rest
Two studies (including 78 participants) reported data on pain at rest (Miccinilli 2018; Simsek 2013). Kinesio taping did not change pain at rest compared to sham taping (MD ‐0.72, 95% CI ‐1.69 to 0.25; Analysis 1.5), with no evidence of heterogeneity (Chi² = 0.65, df = 1 (P = 0.42); I² = 0%). Three studies with 113 participants reported data on pain at night (Kocyigit 2016; Shakeri 2013; Simsek 2013). Results showed a statistically significant reduction of pain at night with kinesio taping compared to sham (MD ‐1.59, 95% IC ‐2.69 to ‐0.50; Analysis 1.6). Heterogeneity analysis demonstrated no heterogeneity (Chi² = 1.12, df = 2 (P = 0.57); I² = 0%).
1.5. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 5: Pain at rest
1.6. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 6: Pain at night
Other measures of range of motion (ROM): external rotation and internal rotation
One trial including 38 participants (Simsek 2013) reported data on active range of motion without pain for shoulder internal rotation and shoulder external rotation. Results showed a statistically insignificant effect of kinesio taping compared to sham taping in improving active range of motion for shoulder internal rotation (MD ‐0.70, 95% CI ‐6.81 to 5.41) and shoulder external rotation (MD ‐2.20, 95% CI ‐13.45 to 9.05) (Analysis 1.7).
1.7. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 7: AROM without pain (shoulder external and internal rotation)
Muscle strength
Muscle strength was measured in three studies (Keenan 2017; Miccinilli 2018; Simsek 2013). Shoulder flexion, shoulder extension and shoulder abduction were reported by two studies (Miccinilli 2018; Simsek 2013). Shoulder adduction was reported by only 40 participants (Miccinilli 2018). Shoulder internal and external rotation were analysed by three studies (Keenan 2017; Miccinilli 2018; Simsek 2013) with 98 participants. Kinesio taping compared to sham taping seemed to be effective in improving shoulder flexion (SMD 0.66, 95% CI 0.20 to 1.11; I² = 0%), shoulder extension (SMD 0.60, 95% CI 0.15 to 1.06; I² = 0%), and shoulder abduction (SMD 0.57, 95% CI 0.11 to 1.02; I² = 0%). There was no effect of kinesio taping compared to sham taping for shoulder adduction (SMD 0.60, 95% CI ‐0.04 to 1.24; I² = 0%); shoulder external rotation (SMD 0.27, 95% CI ‐0.55 to 1.09; I² =74%) and shoulder internal rotation (SMD 0.27, 95% CI ‐0.40 to 0.95; I² = 62%) (Analysis 1.8).
1.8. Analysis.

Comparison 1: Kinesiotaping versus sham taping, Outcome 8: Muscle strength
Withdrawals or dropouts: proportion who withdrew from treatment due to adverse events or other reasons
Eight studies reported data regarding withdrawals or dropouts (Hsu 2009; Jena Etnoyer‐Slaski 2016; Kang 2020; Keenan 2017; Kocyigit 2016; Miccinilli 2018; Shakeri 2013; Thelen 2008). One study did not report data on withdrawals (Simsek 2013). Two studies did not have withdrawals or dropouts (Hsu 2009; Shakeri 2013). Five studies reported a median percentage of withdrawals or dropouts of 9.8% with a range (min‐max) from 3.3% (Keenan 2017) to 30.6% (Jena Etnoyer‐Slaski 2016).
Kinesio taping versus conservative treatments within 30 days from the end of treatment
We used the final values rather than change from baseline values for major and minor outcomes.
Major outcomes
Six studies provided data for overall pain (De Oliveira 2021; Frassanito 2018; Gandhi 2016; Gençbay 2019; Mohamed 2019; Pekyavas 2016), fourteen studies for function (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Gençbay 2019; Goksu 2016; Kaya 2011; Kaya 2014; Kang 2020; Kul 2018; Miller 2009; Pekyavas 2016; Sikha 2017; Subasi 2016), six studies for pain on motion (Devereaux 2016; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Subasi 2016), and three studies for active range of motion – free of pain (De Oliveira 2021; Goksu 2016; Sikha 2017). One study reported data for quality of life (Sikha 2017). No studies reported data for global assessment of treatment success.
Seven studies provided clear data for adverse events (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Goksu 2016; Kaya 2011; Kul 2018; Miller 2009), and nine studies provided data for all‐cause withdrawals or dropouts (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Miller 2009).
Overall pain
Six studies reported overall pain, with five studies including a total of 266 participants providing data for overall pain (De Oliveira 2021; Frassanito 2018; Mohamed 2019; Pekyavas 2016; Subasi 2016). Results showed a statistically insignificant reduction of overall pain in the kinesio taping group compared to the group receiving other conservative treatments (MD ‐0.44, 95% CI 1.33 better to 0.46 worse), absolute difference (4% better, 13% better to 4.6% worse), and relative percentage change (15% better, 46% better to 16% worse) (Analysis 2.1). Assuming a minimal clinically important difference of 1.5 points, this finding was not clinically relevant. Heterogeneity analysis demonstrated substantial heterogeneity (Tau² = 1.38; Chi² = 118.92, df = 6 (P < 0.00001); I² = 95%). Very low‐certainty evidence downgraded for bias, inconsistency and indirectness indicates we are uncertain whether kinesio taping (with or without co‐intervention) improves overall pain when compared with other conservative treatments at six weeks.
2.1. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 1: Overall pain
Function
Fourteen studies with 499 participants reported function (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Gençbay 2019; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Miller 2009; Mohamed 2019; Pekyavas 2016; Sikha 2017; Subasi 2016), but four did not provide useful data (Devereaux 2016; Gandhi 2016; Kaya 2011; Miller 2009). Results showed a statistically significant reduction of disability in the kinesio taping group compared to conservative treatments (SMD ‐0.66, 95% CI ‐1.22 to ‐0.10), absolute difference (13% better, 24% better to 2% better), and relative percentage change (18% better, 32% better to 3% better) (Analysis 2.2). Assuming a minimal clinically important difference of 13 points, this benefit (MD ‐13.13, 95% CI 1.99 better to 24.28 better) includes a clinically important improvement. Heterogeneity analysis demonstrated substantial heterogeneity (Tau² = 0.94; Chi² = 98.87, df = 11 (P < 0.001); I² = 89%). Very low‐certainty evidence, downgraded for publication bias (Figure 4), inconsistency and indirectness at four weeks, indicates that, when compared with other conservative treatments, kinesio taping (with or without a co‐intervention) has uncertain effects on function.
2.2. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 2: Function
Pain on motion
Six studies including a total of 225 participants reported pain on motion (Devereaux 2016; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Subasi 2016). Two studies did not provide useful data (Devereaux 2016; Kaya 2011). Results showed a statistically insignificant reduction of pain on motion in the kinesio taping group compared to other conservative treatments (MD 0.06, 95% CI 0.68 better to 0.80 worse), absolute difference (0.6% better, 7% better to 8% worse), and relative percentage change (1% better, 12% better to 10% worse) (Analysis 2.3). Assuming a minimal clinically important difference of 2.1 points, this finding did not include a clinically important benefit. Heterogeneity analysis demonstrated moderate heterogeneity (Chi² = 5.75, df = 3 (P = 0.12); I² = 48%). Very low‐certainty evidence, downgraded for imprecision, bias and indirectness at four weeks, shows that we are uncertain about the effects of kinesio taping (with or without a co‐intervention) on pain on motion when compared with other conservative treatments.
2.3. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 3: Pain on motion
Active range of motion (AROM) ‐ without pain (shoulder abduction and flexion)
Three studies including 143 participants reported active range of motion without pain data on shoulder flexion and shoulder abduction (De Oliveira 2021; Goksu 2016; Sikha 2017). Results showed a not statistically significant improvement of range of motion with KT compared to other conservative treatments for shoulder abduction (MD 3.04, 95% CI 10.89 worse to 16.96 better), absolute difference (3% better, 11% worse to 17% better), and relative percent change (3% better, 9% worse to 14% better) (Analysis 2.4).Heterogeneity analysis demonstrated substantial heterogeneity (Chi² = 15.54, df = 2 (P = 0.0004); I² = 87%) and shoulder flexion (MD 4.43, 95% CI ‐8.37 to 17.24; heterogeneity: Chi² = 15.39, df = 2 (P = 0.0005); I² = 87%). Considering active range of shoulder abduction without pain as proxy for the outcome, very low‐certainty evidence, downgraded for inconsistency, imprecision and indirectness at six weeks, indicates that we are uncertain about the effects of kinesio taping (with or without a co‐intervention) on AROM without pain when compared with other conservative treatments.
2.4. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 4: AROM without pain (shoulder abduction and flexion)
Global assessment of treatment success
No studies were found for global assessment of treatment success.
Quality of life
One study including 30 participants reported useful data for quality of life using the SF‐12 Health Survey (Sikha 2017). Results showed a statistically significant improvement of quality of life with kinesio taping compared to conservative treatment (MD 18.70, 95% CI 14.48 better to 22.92 better, absolute difference (18.7% better, 14.48% better to 22.92% better) (Analysis 2.5), and relative percent change (53% better, 41% better to 65% better). Assuming an improvement of 10% as clinically important, this finding includes a clinically important benefit for KT (heterogeneity not applicable). Low‐certainty evidence, downgraded for indirectness and imprecision at four weeks, indicates that kinesio taping (with or without a co‐intervention) may improve quality of life when compared with other conservative treatments but the evidence is limited.
2.5. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 5: Quality of life
Adverse events
Seven studies reported adverse events (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Goksu 2016; Kaya 2011; Kul 2018; Miller 2009).Overall, five adverse events were reported by three studies: one event of skin redness after the application of kinesio taping in the experimental group (Frassanito 2018), two events of local irritation in kinesio taping groups (Goksu 2016), and two events of adverse reaction to tape in the kinesio taping group (Miller 2009). Four studies reported no adverse events (De Oliveira 2021; Devereaux 2016; Kaya 2011; Kul 2018). Seven studies did not collect data on adverse events (Gandhi 2016; Gençbay 2019; Kaya 2014; Mohamed 2019; Pekyavas 2016; Sikha 2017; Subasi 2016). Due to a paucity of information, data were not meta‐analysed. We are uncertain about the adverse events of kinesio taping compared with conservative treatments (very low‐certainty evidence).
Minor outcomes
Five studies reported the efficacy of kinesio taping on minor outcomes of pain at rest (Devereaux 2016; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018), and three studies reported on pain at night (Kaya 2011; Kaya 2014; Kul 2018). No studies reported muscle strength as an outcome.
Other measures of pain: such as, pain at night and pain at rest
Five studies including 155 participants reported pain at rest (Devereaux 2016; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018). Two studies (Devereaux 2016; Kaya 2011) did not provide useful data. Results showed a statistically insignificant increase in pain at rest with kinesio taping (with or without a co‐intervention) compared to other conservative treatments (MD 0.17, 95% CI ‐0.24 to 0.58; Chi² = 2.83, df = 2 (P = 0.24); I² = 29%; Analysis 2.6).
2.6. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 6: Pain at rest
Three studies including 94 participants reported pain at night (Kaya 2011; Kaya 2014; Kul 2018) with one study (Kaya 2011) not reporting useful data. Results showed a statistically significant reduction in pain at night with kinesio taping (with or without a co‐intervention) compared to other conservative treatments (MD ‐0.57, 95% CI ‐3.07 to 1.93; Chi² = 7.94, df = 1 (P = 0.005); I² = 87%; Analysis 2.7).
2.7. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 7: Pain at night
Other measures of range of motion (ROM): external rotation and internal rotation
One study including 61 participants (Goksu 2016) provided data for shoulder internal rotation (MD ‐0.70, 95% CI ‐3.28, 1.88). Two studies including 91 participants (Goksu 2016; Sikha 2017) provided data for shoulder external rotation (MD 3.37, 95 CI ‐5.25 to 11.99). Results showed no effect of kinesio taping (with or without a co‐intervention) on active range of motion for these outcomes (Analysis 2.8).
2.8. Analysis.

Comparison 2: Kinesiotaping versus other conservative treatment, Outcome 8: AROM without pain (shoulder external and internal rotation)
Muscle strength
No studies reported muscle strength as an outcome.
Withdrawals or dropouts: proportion who withdrew from treatment due to adverse events or other reasons
Nine studies provided data for withdrawals or dropouts (De Oliveira 2021; Devereaux 2016; Frassanito 2018; Gandhi 2016; Goksu 2016; Kaya 2011; Kaya 2014; Kul 2018; Miller 2009). Two studies did not report data on the outcome (Gençbay 2019; Pekyavas 2016). Three studies did not have any withdrawals or dropouts (Kul 2018; Mohamed 2019; Sikha 2017). Eight studies reported a median percentage of withdrawals or dropouts of 9.2% with a range (min‐max) from 5.3% (Gandhi 2016) to 19% (Devereaux 2016).
Subgroup analysis
Two studies performed one application of KT(Hsu 2009; Keenan 2017). Due to a limited number of studies reporting these characteristics on pain and function for our comparisons of interest, we did not perform subgroup analysis for the number of applications of kinesio taping (one versus two or more applications). All other included studies performed two or more applications.
Two studies included athletes (Goksu 2016; Hsu 2009). Due to a limited number of studies reporting these characteristics on pain and function for our comparison of interest, we did not perform subgroup analysis for the target population ('overhead' people such as athletes versus the general population). All other included studies investigated the general population.
Sensitivity analysis
No sensitivity analysis was performed to investigate the effectiveness of kinesio taping versus sham taping or other conservative treatments since all trials were at high or unclear risk of random sequence generation or adequate allocation concealment and blinding of participants.
Discussion
Summary of main results
This systematic review summarised the results of 23 controlled trials including 1054 participants on the effectiveness and safety of KT for rotator cuff disease. The KT applications were reported at the end of treatment (two to six weeks). The findings were as follows:
Kinesio taping versus sham taping within 30 days from the end of treatment
In term of efficacy, nine studies involving 312 participants compared KT versus sham taping. Overall, due to very low certainty of evidence, we are uncertain if KT improves overall pain, function, pain on motion and pain free‐AROM. In terms of adverse events, the quality of evidence is very uncertain about the safety of KT for rotator cuff disease: four studies reported a low rate of adverse effects for the overall implementation of interventions without a specific rate for groups (median 2%, IQR 1‐4%).
Kinesio taping versus other conservative treatment at the end of the intervention
Fourteen studies involving 742 participants compared KT (with or without a co‐intervention) versus other conservative treatment. Overall, due to very low certainty of evidence, we are uncertain if KT improves overall pain, function, pain on motion and pain free‐AROM compared to conservative treatment. With low certainty of evidence, KT (with or without a co‐intervention) may improve quality of life with statistically and clinically relevant effects compared to conservative treatment. In terms of adverse events, the quality of evidence was very low, hence, we are uncertain about the safety of KT for rotator cuff disease: seven studies reported a low rate of adverse effects for the overall implementation of interventions without a specific rate for groups (median 1%, IQR 0‐3%; very low certainty of evidence).
Kinesio taping (with or without a co‐intervention) compared to conservative treatments seems to offer little benefit for overall pain, function and pain on movement. Assuming that standard care (a general rehabilitative program) or another conservative treatment might improve outcomes such as function (e.g. ultrasound Page 2016b), it may not be surprising that kinesio taping did not provide any additional benefit.
Overall completeness and applicability of evidence
Inconsistent reporting of major outcomes across trials was found and reported in Table 6. Overall, 91% of trials reported overall pain, function and pain on motion, out of which 35%, 70% and 35% of trials, respectively, reported complete data. Partial reporting of function data from one trial precluded its inclusion in the analyses contributing to waste of research efforts. Other major outcomes were reported by a lower proportion of trials. Only one study measured global assessment of treatment success but no outcome data were reported. Two trials reported only minor outcomes.
4. Outcome Reporting Bias In Trials (ORBIT) matrix.
| Major outcomes | |||||||
| Study ID | Overall Pain | Function | Pain on motion | Active range of motion | Global assessment of treatment success | Quality of life | Adverse events |
| De Oliveira 2021 | Full | Full | Not measured | Full | Measured | Not measured | Partial |
| Devereaux 2016 | ? | Partial | Partial | ? | ? | ? | Partial |
| Frassanito 2018 | Full | Full | ? | ? | ? | ? | Partial |
| Gandhi 2016 | ? | Partial | ? | ? | ? | ? | ? |
| Gençbay 2019 | Partial | Full | ? | ? | ? | ? | ? |
| Goksu 2016 | ? | Full | Full | Full | ? | ? | Partial |
| Hsu 2009 | ? | ? | ? | ? | ? | ? | Partial |
| Jena Etnoyer‐Slaski 2016 | Full | Full | Not measured | Not measured | Not measured | Not measured | Partial |
| Kang 2020 | Full | Full | Not measured | Not measured | Not measured | Not measured | Not measured |
| Kaya 2011 | ? | Partial | Partial | ? | ? | ? | Partial |
| Kaya 2014 | ? | Full | Full | ? | ? | ? | Partial |
| Keenan 2017 | ? | ? | ? | ? | ? | ? | ? |
| Kocyigit 2016 | Full | Full | Full | ? | ? | Partial | ? |
| Kul 2018 | ? | Full | Full | ? | ? | ? | Partial |
| Miccinilli 2018 | ? | Full | Full | ? | ? | ? | ? |
| Miller 2009 | ? | Partial | ? | ? | ? | ? | Partial |
| Mohamed 2019 | Full | Full | ? | ? | ? | ? | ? |
| Pekyavas 2016 | Full | Full | ? | ? | ? | ? | ? |
| Shakeri 2013 | ? | Full | Full | Full | ? | ? | ? |
| Sikha 2017 | ? | Full | ? | Full | ? | Full | ? |
| Simsek 2013 | ? | Full | Full | Full | ? | ? | ? |
| Subasi 2016 | Full | Full | Full | ? | ? | ? | ? |
| Thelen 2008 | ? | Partial | ? | Partial | ? | ? | Partial |
‘Full': sufficient data for inclusion in a meta‐analysis was reported (e.g. mean, standard deviation and sample size per group for continuous outcomes).
'Partial': insufficient data for inclusion in a meta‐analysis was reported (e.g. means only, with no measures of variance).
'Measured': outcome was measured but no outcome data was reported.
'Not measured': outcome was not measured by the trialists.
'?': unclear whether the outcome was measured or not (as a trial protocol was unavailable).
Sample sizes were small and the pooled samples were still less than the 400 participants criterion, hence, the evidence was downgraded to low. Therefore, we recommend caution in generalising the results of this review to the wider population of individuals with shoulder pain for rotator cuff disease.
The TIDIER Checklist showed a completeness of the intervention description on kinesio taping even though we found an overall variability in the application modality (Table 5). The target application varied, comprising different muscles, however, the most frequent muscle targets were deltoid and supraspinatus. Overall, the interventions were provided by clinicians and in a minority of cases (5 out of 19) involved certified/trained physiotherapists. Finally, the required number of applications ranged from three to six applications with a few ranging from one to 18 applications.
In the comparison of KT versus other conservative treatment at the end of the intervention, some studies reported serious differences among co‐interventions that could weaken applicability. These co‐interventions varied by including exercises, manual therapy and physical therapy modalities; each of these might impact differently on shoulder impingement syndrome outcomes (Steuri 2017), thus obfuscating the isolated beneficial effect of kinesio taping. However, co‐interventions were equally distributed between experimental (kinesio taping) and control group in half of the trials in the kinesio taping group versus conservative interventions while, in the remaining, the co‐intervention was only applied to the experimental group assessing the effect of KT as additional treatment.
Quality of the evidence
Kinesio taping versus sham taping within 30 days from the end of treatment
The quality of the evidence was very low for pain: we downgraded the evidence for serious limitations in study design due to one study being assessed as high risk of bias for selection, performance and detection bias, serious indirectness due to differences among co‐interventions in the included studies and for serious imprecision since the optimal information size was not met (participants fewer than 400).
Function was judged as very low certainty of evidence for serious limitations in study design for the above reasons, serious indirectness due to differences among co‐interventions in the included studies, serious inconsistency andfor serious imprecision since the optimal information size was not met (participants fewer than 400) and publication bias (missing results that could lead to non‐reporting bias).
Pain on motion was affected by serious indirectness due to differences among co‐interventions in the included studies as well as by serious study design limitations and imprecision of the estimates since the optimal information size was not met (participants fewer than 400) and the 95% confidence intervals included the threshold of benefit and harm; hence, the certainty of the evidence was very low. The outcome of active range of motion (shoulder abduction without pain) was judged as very low‐quality evidence due to publication bias, serious inconsistency due to high heterogeneity (I2 > 75) and very serious imprecision with small sample size and very wide 95% confidence intervals including the threshold of benefits.
Overall, all major outcomes were mostly downgraded for concerns about imprecision, indirectness and study design limitation due to unclear selection bias, and high risk of both detection and performance bias. The latter bias can be mainly avoided by double‐blinding. This was impossible to implement in the comparison of kinesio taping versus other conservative treatment because participants in the experimental and control groups would be aware of their status. On the contrary, in the KT versus sham kinesio taping comparison, the blinding of participants was possible and all investigating studies reported the procedure involving the blinding of participants.
Kinesio taping versus other conservative treatments within 30 days from the end of treatment
The quality of the evidence was very low for pain; we downgraded it for very serious inconsistency (substantial heterogeneity (I2 > 90)), serious indirectness due to variability in the control interventions, and for serious study design limitations due to high risk of bias for selection, performance and detection bias.
Function was judged as having very low certainty of evidence for serious indirectness due to variability in the control interventions, serious inconsistency for high heterogeneity (I2 > 75) and publication bias.
Pain on motion was affected by serious indirectness due to variability in the control interventions, serious imprecision due to the optimal information size not being met (participants fewer than 400) and publication bias; hence, the certainty of the evidence was very low. Quality of life was downgraded to low‐certainty evidence for indirectness due to variability in the control interventions and serious imprecision (optimal information size not being reached as participants were fewer than 400). AROM shoulder abduction without pain was judged as very low‐quality evidence, downgraded for serious indirectness due to variability in the control interventions, serious inconsistency for high heterogeneity (I2 > 75) and for serious imprecision since the optimal information size was not met (participants fewer than 400).
Potential biases in the review process
To the best of our knowledge, we identified all relevant trials meeting our inclusion/exclusion criteria through searching all major databases without language restrictions. None of the review authors has been involved with the conduct of any of the included trials.
We updated searches up to July 2020 and utilised multiple databases even if we did not undertake a search for grey literature on MedrXiv or BiorXIv for pre‐prints. However, since the majority of the evidence we included had 'negative' findings, we believe that identification and inclusion of unpublished studies with non‐significant results is unlikely to have changed our conclusions. By searching clinical trial registries (e.g. ClinicalTrials.gov), we enhanced the opportunity to identify unpublished trials and selective reporting of outcomes. In fact, we retrieved two trials with preliminary results which are not yet published (De Oliveira 2021; Jena Etnoyer‐Slaski 2016) and which were not included in the more recent systematic reviews. Therefore, we think it is very unlikely that we missed relevant trials that would change the conclusions of our review.
We contacted primary authors for clarification and additional information where indicated, although responses were not always obtained. Furthermore, reported data in some studies could not be used due to missing data or errors in standard deviations.
We used a standardised procedure to determine the selection, inclusion and assessment of studies in this review and review authors were trained in data extraction. According to the protocol, to prevent selective inclusion of results (Page 2013), we used predefined decision rules to select data from trials when multiple measurement scales, time points and analyses were reported. We documented the study characteristics and intervention in sufficient detail to avoid inconsistent application in study selection and data extraction.
Two members of our multidisciplinary team are clinicians who frequently use kinesio taping and one author has also experienced the intervention as a consumer (i.e. one team member had shoulder impingement) and brought the perspective of lived experience during the protocol and review process.
We used intention‐to‐treat data preferentially.
Agreements and disagreements with other studies or reviews
In 2015, one network meta‐analysis, focusing on all interventions for shoulder impingement syndrome, found that KT with exercise was superior to exercise alone in improving function measured with the Constant–Murley score but no superiority was found for pain score (Dong 2015). On the contrary, our results did not find a beneficial effect of kinesio taping versus conservative treatments. However, the contribution to the evidence in Dong and colleagues' review for kinesio taping comes from only one study (Simsek 2013), limiting the interpretation of evidence compared to our overall cohort including 14 trials which compared KT to conservative treatment and nine trials which compared KT to sham treatment.
We found one previous review focusing on any type of taping methods (both rigid and elastic KT) for subacromial impingement syndrome on pain (at rest, at night, on movement), range of motion, and muscle strength (Saracoglu 2018). The search for the Saracoglu 2018 review generated three RCTs and one controlled trial (135 participants) published between 2009 and 2013. These four studies were assessed for methodological quality using the PEDro scale, rather than the Cochrane risk of bias tool as in our review, which led to one study being assessed as being at low quality because of study design limitations. Saracoglu 2018 did not perform meta‐analysis even if any kind of taping (rigid or elastic) was used with physiotherapy interventions (e.g. exercise, electrotherapy, and manual therapy), being an optional modality. Thus, their results did not differentiate between rigid and elastic tape, limiting the implications for practice.
Ghozy 2020 conducted a systematic review assessing the efficacy of KT on shoulder pain and function. Nevertheless, their PICO included a wide range of diagnoses such as shoulder disability after mastectomy, hemiplegic shoulder pain or asymptomatic overhead athletes. Results were not subgrouped and any interpretation was not relevant to our clinical question.
Another recent systematic review including 16 trials conducted by Celik 2020, examined the effect of KT for shoulder disorders. The methodological quality was investigated using the PEDro scale. In agreement with our review, although they reported positive effects in some studies, there was no firm evidence of any benefit of KT on shoulder disorders.
Authors' conclusions
Implications for practice.
Based on very low‐certainty evidence, this systematic review suggests that KT for rotator cuff disease has uncertain effects in terms of self‐reported pain, function, pain on motion and active range of motion when compared to sham taping or other conservative treatment. Low‐certainty evidence shows that kinesio taping may improve quality of life when compared to conservative treatment.
Evidence on adverse events was scarce and uncertain due to low event rates, thus, we could not obtain a reliable estimate of the risk of these events from the trials in this review.
Overall, our review might not support the use of kinesio taping in clinical practice as a treatment for rotator cuff diseases due to uncertainty in the evidence surrounding its benefit and harms; moreover, we did not consider the costs of KT and the preferences of providers and recipients in using KT. We are uncertain about the effect of kinesio taping on function and pain on motion when compared to sham KT. We are uncertain about the effects of kinesio taping combined with a co‐intervention (as, for example, exercise, manual therapy or physical therapy modalities) on pain, range of motion and function. Kinesio taping combined with a co‐intervention may improve quality of life compared to conservative treatment.
KT has uncertain effects, even though it is widely used, due to its practicality and safety despite additional costs.
Implications for research.
Although KT is widely used, due to its practicality and safety, direct scientific evidence on its efficacy and harms is lacking. We identified several research gaps that have implications for future research. So far, KT has not demonstrated a beneficial effect due to imprecision (fewer than 400 participants/optimal information size not reached), inconsistency, study design limitations and indirectness in the co‐interventions. Among trials with non‐statistically significant findings, a recent publication found that 60% of studies were not able to include the planned sample, resulting in imprecision of effects (low‐certainty evidence) (Gianola 2019).
In addition, when these studies were combined, we did not reach the optimal information size, which is one of the reasons for downgrading the certainty of the evidence (Turner 2013).
Randomised controlled trials are the best study design to assess the efficacy of an intervention, however, when planning future studies, authors should intend to reach an adequate sample size, use proper statistical analysis, and clearly report outcome data to improve the quality of conduct and reporting of the studies.
We identified heterogeneity in the reporting of domains and measurement instruments (Page 2018). Trials on interventions such as KT for rotator cuff disease should be designed with a core outcome set in order to standardise efficacy outcome and outcome measurements across studies (Gagnier 2017). The selection of appropriate outcomes or domains is crucial when designing clinical trials, to appreciate the effects of different interventions, pool results, and make valid comparisons among trials.
Analogously, trials should clearly describe all details for delivering KT such as the provider, the target muscles, and especially the modality of application, schedule and duration in order to better assess the right implementation and usage of kinesio taping. We observed that the Kase modality has been the most commonly used method for applying KT for shoulder pain, however, other modalities have been used with different muscle targets, so it would be helpful to investigate if the type of modality or muscle target might influence KT effects for patients in a multi‐arm trial. Moreover, since pain may persist for a long time in this population (few studies in our review included populations having pain for more than three months), it would be interesting to assess if co‐variables and exposures (e.g. pain knowledge, psychological variables) might influence the process of chronicisation and change in pain severity and so affect treatment results (Mills 2019; Sullivan 2016).
Concordantly, clinicians should consider these limitations when using KT for their patients.
History
Protocol first published: Issue 7, 2017
Acknowledgements
Linda Li for contributions to earlier work on the update in study design.
Appendices
Appendix 1. Search strategies for CENTRAL and MEDLINE
Search strategy for CENTRAL:
MeSH descriptor: [Shoulder Pain] explode all trees
MeSH descriptor: [Shoulder Impingement Syndrome] explode all trees
MeSH descriptor: [Rotator Cuff ] explode all trees
MeSH descriptor: [Bursitis] explode all trees
((shoulder* in All Text or rotator* in All Text) and (bursitis in All Text or impinge* in All Text or tendonitis in All Text or tendonitis in All Text or tendinopathy in All Text or pain* in All Text))
“rotator cuff ” in All Text
#1 or #2 or #3 or #4 or #5 or #6
tap* in All Text
kinesio* in All Text
#8 or #9
#7 and #10
Search strategy for MEDLINE (Ovid):
shoulder pain/
shoulder impingement syndrome/
rotator cuff/
exp bursitis/
((shoulder$ or rotator cuff ) adj5 (bursitis or or impinge$ or tendinitis or tendonitis or tendinopathy or pain$)).mp.
rotator cuff.mp.
or/1‐6
(tap$ or kinesiotap$ or kinesio$)
randomized controlled trial.pt.
controlled clinical trial.pt.
randomized.ab.
placebo.ab.
drug therapy.fs.
randomly.ab.
trial.ab.
groups.ab.
1 or 2 or 3 or 4 or 5 or 6 or 7 or 8
exp animals/ not humans.sh.
9 not 10
7 and 8 and 19
Data and analyses
Comparison 1. Kinesiotaping versus sham taping.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Overall pain | 3 | 106 | Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.77, 0.90] |
| 1.2 Function | 6 | 214 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.28, 0.30] |
| 1.3 Pain on motion | 4 | 153 | Mean Difference (IV, Random, 95% CI) | ‐1.48 [‐2.25, ‐0.71] |
| 1.4 AROM without pain (shoulder abduction and flexion) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.4.1 Shoulder abduction | 2 | 68 | Mean Difference (IV, Random, 95% CI) | 10.23 [‐16.09, 36.56] |
| 1.4.2 Shoulder flexion | 2 | 68 | Mean Difference (IV, Random, 95% CI) | ‐4.12 [‐6.10, ‐2.13] |
| 1.5 Pain at rest | 2 | 78 | Mean Difference (IV, Random, 95% CI) | ‐0.72 [‐1.69, 0.25] |
| 1.6 Pain at night | 3 | 113 | Mean Difference (IV, Random, 95% CI) | ‐1.59 [‐2.69, ‐0.50] |
| 1.7 AROM without pain (shoulder external and internal rotation) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 1.7.1 Shoulder external rotation | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐2.20 [‐13.45, 9.05] |
| 1.7.2 Shoulder internal rotation | 1 | 38 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐6.81, 5.41] |
| 1.8 Muscle strength | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.8.1 Shoulder flexion | 2 | 78 | Std. Mean Difference (IV, Random, 95% CI) | 0.66 [0.20, 1.11] |
| 1.8.2 Shoulder extension | 2 | 78 | Std. Mean Difference (IV, Random, 95% CI) | 0.60 [0.15, 1.06] |
| 1.8.3 Shoulder abduction | 2 | 78 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [0.11, 1.02] |
| 1.8.4 Shoulder adduction | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.60 [‐0.04, 1.24] |
| 1.8.5 Shoulder external rotation | 3 | 98 | Std. Mean Difference (IV, Random, 95% CI) | 0.27 [‐0.55, 1.09] |
| 1.8.6 Shoulder internal rotation | 3 | 98 | Std. Mean Difference (IV, Random, 95% CI) | 0.27 [‐0.40, 0.95] |
Comparison 2. Kinesiotaping versus other conservative treatment.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Overall pain | 5 | 266 | Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐1.33, 0.46] |
| 2.2 Function | 10 | 499 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.22, ‐0.10] |
| 2.3 Pain on motion | 4 | 225 | Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.80, 0.68] |
| 2.4 AROM without pain (shoulder abduction and flexion) | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.4.1 Shoulder abduction | 3 | 143 | Mean Difference (IV, Random, 95% CI) | 3.04 [‐10.89, 16.96] |
| 2.4.2 Shoulder flexion | 3 | 143 | Mean Difference (IV, Random, 95% CI) | 4.43 [‐8.37, 17.24] |
| 2.5 Quality of life | 1 | 30 | Mean Difference (IV, Fixed, 95% CI) | 18.70 [14.48, 22.92] |
| 2.6 Pain at rest | 3 | 155 | Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.24, 0.58] |
| 2.7 Pain at night | 2 | 94 | Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐3.07, 1.93] |
| 2.8 AROM without pain (shoulder external and internal rotation) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.8.1 Shoulder external rotation | 2 | 91 | Mean Difference (IV, Random, 95% CI) | 3.37 [‐5.25, 11.99] |
| 2.8.2 Shoulder internal rotation | 1 | 61 | Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐3.28, 1.88] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
De Oliveira 2021.
| Study characteristics | ||
| Methods | Study design: a single‐blind, parallel‐group RCT Setting: center for Interdisciplinary Research in Rehabilitation and Social Integration Research (CIRRIS) Québec City, Quebec, Canada Timing: between November 2016 and November 2017 Interventions: standardised rehabilitation program plus kinesio taping application versus the same standardised rehabilitation program Sample size: fifty‐two participants were recruited. An a priori sample size was calculated using a superiority trial design based on changes reported by the DASH scores for individuals with rotator cuff tendinopathy. According to sample size calculation, 22 participants per group were required. Considering a possible loss to follow‐up of 15%, 26 participants per group were recruited. Analysis: intention‐to‐treat and per‐protocol analyses were conducted. | |
| Participants | Criteria for defining the condition being treated: have one positive sign in each of the three following categories: painful arc of movement (flexion, and/or abduction); neer or Kennedy‐Hawkins impingement signs; pain during resisted external rotation, abduction, or empty can test
Inclusion criteria: be aged 18‐65 years
Exclusion criteria: presence of an open wound compromising kinesio taping application; previous shoulder surgery; allergy or intolerance to kinesio taping; adhesive capsulitis (passive shoulder ROM < 50%); history of glenohumeral dislocation (< 12 months) or fracture to the shoulder girdle; shoulder pain reproduced by cervical movements or cervicobrachialgia; clinical sign of full‐thickness RC tears (positive lag signs).
Baseline characteristics:
Intervention: kinesio taping (KT)
Number randomised: 26
Number included in analyses: 26
Age: 30.9 ± 9.0 years
Sex: M 15 (57.7%); F 11 (42.3%)
Diagnosis: rotator cuff tendinopathy
Dominant shoulder affected: 18 (69.2%) Mean (SD) pain (Back Pain Index): 2.9 (1.6) Mean (SD) function (DASH 0‐100): 28.1 (11.8) Mean (SD) function (WORC index 0‐100): 60.5 (19.2) Comparator: rehabilitation program Number randomised: 26 Number included in analyses: 26 Age: 29.4 ± 7.5 years Sex: M 15 (57.7%); F 11 (42.3%) Diagnosis: rotator cuff tendinopathy Dominant shoulder affected: 17 (65.4%) Mean (SD) pain (Back Pain Index): 2.9 (1.5) Mean (SD) function (DASH 0‐10): 27.8 (10.0) Mean (SD) function (WORC index 0‐100): 56.2 (18.3) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Intervention: KT
Tape: kinesio tape 2 in (5 cm); taping method: kase protocol; target: deltoid, supraspinatus, trapezius; number of applications: 10; single application duration: 3 dd; provider: certified PT. Rehabilitation program: twice weekly during the first four weeks, then once weekly for the last two weeks. Co‐intervention: standardised rehabilitation program Control: rehabilitation program A standardised rehabilitation program, consisting of 10 physiotherapy sessions of 30‐45 minutes duration, was provided twice weekly during the first four weeks, then once weekly. The intervention included patient education, manual therapy, stretching and strengthening exercises. |
|
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | This work was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior and the Fundação de Amparo à Pesquisa de Minas Gerais. FCLO receives a doctoral scholarship from the Brazilian Government through the Science without Borders programme in association with the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – CAPES. J‐S Rand FD are supported by salary awards from the Fonds de Recherche Québec‐Santé (FRQS) and the Canadian Institutes of Health Research (CIHR). No conflict of interest. Trial registration: NCT02881021 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "an independent researcher conducted randomization stratified by sex using a block design". |
| Allocation concealment (selection bias) | Low risk | "sequentially numbered sealed opaque" |
| Blinding of participants (performance bias) | Unclear risk | Discrepancy between trial registration (single‐blind (outcomes assessor)), protocol ("single blind participants)", and full publication ("participants were unaware of the treatment provided to other participants..") were presented. |
| Blinding of personnel (performance bias) | High risk | "single blind (participants or assessors)" |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Low risk | To assess blinding effectiveness, the evaluators answered some questions to test their blinding. In the results section, authors confirmed the effectiveness of the blinding of assessors. However, for self‐reported outcomes, the participant was the assessor. Thus, in the full publication, we noted: "participants were unaware of the treatment provided to other participants..". ‐ but the participant was the assessor for self‐reported outcomes. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | To assess blinding effectiveness, the evaluators answered some questions to test their blinding. In the results section, authors confirmed the effectiveness of the blinding of assessors. Thus, there were appropriate measurements for assessor‐reported outcomes (i.e. ROM). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up |
| Selective reporting (reporting bias) | High risk | Missing outcome data ‐ discrepancy from published protocol |
| Unequal use of co‐intervention | Low risk | KT + other conservative treatment versus the same conservative treatment |
Devereaux 2016.
| Study characteristics | ||
| Methods | Study design: prospective, single‐centre, assessor‐blind parallel‐group randomised control trial with 3 groups Setting: an orthopaedic clinic at an academic‐community teaching hospital Timing: October 2009 to June 2012 Interventions: group 1 received precut kinesiology tape (PCT) and exercise, group 2 received a nonsteroidal anti‐inflammatory drug (NSAID) and exercise, and group 3 received exercise only. Sample size: one hundred patients were randomised. Eighty‐one patients completed the study. A minimum of 26 participants per treatment group (total, n = 78) were needed to obtain power of 80% and an alpha of 0.05. This calculation was based on a difference in pain intensity levels of 2 points on the NPRS, which has been shown to be the minimal clinically important difference (MCID), and an SD of 2.5. Analysis: intention‐to‐treat analysis planned and executed. Generalised linear models were fit to assess within‐group and between‐group differences in the pain scores from pre to post‐intervention. These analyses were carried out using both a multiple imputation algorithm to account for missing data and complete case dataset. | |
| Participants | Criteria for defining the condition being treated: primary complaint of anterolateral shoulder pain; a painful arc (60‐120°); a positive Hawkins–Kennedy test indicating SAI; imaging consistent with impingement (e.g. bony abnormalities of the coracoacromial arch, inflammation of the bursa, or rotator cuff tendons)
Restriction on duration of symptoms: subacute onset of pain (< 12 months) Inclusion criteria: minimum 18 years of age Exclusion criteria: previous history of shoulder surgery on the affected side; previous history of therapeutic kinesiology taping of the shoulder; medical contraindication to NSAIDs; frozen shoulder; labral tears; soft‐tissue imaging documenting high‐grade or partial‐thickness rotator cuff tears; instability; glenohumeral arthritis; traumatic shoulder pathology (e.g. fractures); signs and symptoms because of referred pain (e.g. cervical); chronic pain (> 12 months); and previous history of contact dermatitis Baseline characteristics: Intervention: PCT (pre‐cut kinesiology taping) + exercise Number of participants at enrolment: 33 Number randomised: 33 Number included in analyses: 33 (6 lost to follow‐up) Age: 50.0 ± 11.9 years Sex: M 22 (66.7%); F 11 (33.3%) Diagnosis: Sub‐acromial impingement Mean (SD) pain (NPRS 0‐10): 6.5 (2.3) Mean (SD) function (Constant score): 54.7 (11.9) Mean (SD) function (SST): 6.5 (2.5) Intervention 2: NSAID + exercise Number of participants at enrolment: 29 Number randomised: 29 Number included in analyses: 29 (4 lost to follow‐up) Age: 44.0 ± 10.5 years Sex: M 21 (72.4%); F 8 (27.6%) Diagnosis: Sub‐acromial impingement Mean (SD) pain (NPRS 0‐10): 6.3 (2.5) Mean (SD) function (Constant score): 58.2 (18.6) Mean (SD) function (SST): 6.7 (2.7) Comparator: Exercise Number of participants at enrolment: 38 Number randomised: 38 Number included in analyses: 38 (9 lost to follow‐up) Age: 50.0 ± 13.3 years Sex: M 18 (47.3%); F 20 (52.7%) Diagnosis: Sub‐acromial impingement Mean (SD) pain (NPRS 0‐10): 6.3 (2.6) Mean (SD) function (Constant score): 54.5 (18.3) Mean (SD) function (SST): 6.1 (3.1) Pretreatment group differences: treatment groups were similar at baseline with no significant difference in demographics or baseline characteristics. |
|
| Interventions | Experimental: PCT
Tape: precut Shoulder Spider; taping method: precut Shoulder Spider; target: not reported; number of applications: 4; single application duration: 3‐5 dd; provider: trained physiotherapist. Co‐intervention: exercise programs consisting of 3 phases: phase 1 (proximal kinetic chain); phase 2 (scapulothoracic); phase 3 (glenohumeral) home exercise program Control: NSAIDs 2‐week supply (28 pills) of Naprosyn enteric‐coated, 500 mg, 1 pill, twice daily with meals. Co‐intervention: Exercise programs consisting of 3 phases: phase 1 (proximal kinetic chain); phase 2 (scapulothoracic); phase 3 (glenohumeral) home exercise program |
|
| Outcomes | Outcomes
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: supported by an unrestricted research grant from Nucap Medical Inc. A. Elmaraghy has received consultancy fees from Arthrex. Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "The treating physiotherapist randomly assigned participants to a treatment group using a computer‐generated random number table". |
| Allocation concealment (selection bias) | Unclear risk | "Each participant was randomly assigned to one of the 3 groups". Insufficient information for judgement |
| Blinding of participants (performance bias) | High risk | "Study participants were also not blinded to the allocation process". |
| Blinding of personnel (performance bias) | High risk | "The physiotherapist involved in the clinical treatment component of the study was not blinded to the assignment of treatment groups". |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "This study was a prospective, single‐center, assessor blind parallel‐group randomized control trial. To avoid bias, the physiotherapist was not involved in measurement of pretreatment and post‐treatment outcomes or data analysis". However, "Study participants were also not blinded to the allocation process". |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | No objective outcome planned and assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "One of the weaknesses of our study was the overall dropout rate of 19%, which is relatively high but similar to other randomized studies on kinesiology tape". Percentage dropout < 20% |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with other conservative treatment versus the same conservative treatment |
Frassanito 2018.
| Study characteristics | ||
| Methods | Study design: parallel‐group, 1:1 allocation ratio, single‐centre, randomised, superiority trial Setting: rehabilitation Institute outpatients. The study was carried out at the Scientific Institute of Montescano, Istituti Clinici Scientifici Maugeri, Italy. Timing: from July 2013 to January 2016 Interventions: in the experimental group, patients underwent three sessions (once a week for 3 weeks) of ESWT with kinesio taping applied at the end of each session. Controls underwent three sessions of ESWT only. Sample size: forty‐two patients with rotator cuff calcific tendinopathy. Sample size computation was based on the outcome measure DASH. The estimated sample size was 15 patients per group. Analysis: per‐protocol analysis was conducted. | |
| Participants | Criteria for defining the condition being treated: signs of rotator cuff calcific tendinopathy on imaging (musculoskeletal ultrasound, standard radiography, magnetic resonance) and positivity to specific tests of functionality (Jobe, Lift‐off, Patte, Palm up, Yocum, Neer)
Restriction on duration of symptoms: pain and shoulder range of motion limitation in activities of daily living (ADL) for at least 2 weeks
Inclusion criteria:
age > 18 years, the absence of cognitive impairment and impaired consciousness which could prevent the subject from expressing free and informed consent
Exclusion criteria:
treatment with intra‐articular infiltration therapy (corticosteroids or corticosteroids/anaesthetic) and/or physical therapy to the affected shoulder within 4 weeks prior to the study, ongoing cortisone or non‐steroidal anti‐inflammatory (NSAID) therapy, partial or complete tear of the tendons of the rotator cuff on imaging, severe glenohumeral and/or acromioclavicular osteoarthritis, surgery for direct shoulder injury, concomitant cervical symptoms consistent with radiculopathy, outcomes of neurological diseases involving the shoulder, dermatological diseases, damaged skin (scars, infections, or ulcerations not fully healed) involving the affected shoulder, blood coagulation diseases or anticoagulant therapy, decompensated diabetes, tumours, bone infections, pregnancy, presence of a pacemaker, rheumatoid arthritis or other connective tissue diseases, and allergy to adhesive tape
Baseline characteristics:
Intervention: extracorporeal Shock Wave Therapy (ESWT) + Kinesio Taping (KT)
Number randomised: 24
Number included in analyses: 21 (3 lost to follow‐up)
Age: 54.1 ± 10.3 years
Sex: M 7 (33%); F 14 (66%)
Diagnosis: calcific tendinopathy of the rotator cuff
Dominant shoulder affected: 13 (62%) Mean (SD) pain (VAS 0‐10): 6.6 (1.5) Mean (SD) function (DASH): 33.6 (12.1) Comparator: ESWT Number randomised: 26 Number included in analyses: 21 (5 lost to follow‐up) Age: 48.7 ± 11.9 years Sex: M 9 (43%); F 12 (57%) Diagnosis: calcific tendinopathy of the rotator cuff Dominant shoulder affected: 11 (52%) Mean (SD) pain (VAS 0‐10): 6.7 (1.1) Mean (SD) function (DASH): 31.1 (8.9) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Experimental: KT
Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus; number of applications: 3; single application duration: 3 dd; provider: not reported; Co‐intervention: extracorporeal shock wave therapy Control: ESWT Delivered at 4 Hz, with 1800 pulses, and energy flux density ranging from 0.07 to 0.15 mJ/mm2; patient in sitting position and the affected arm extended alongside the body and rotated max 15° internally and externally |
|
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | No source of findings declared. The authors certified that there was no conflict of interest with any financial organisation regarding the material discussed in the manuscript. Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "a computer‐generated list of random numbers obtained with the Matlab random numbers generator" |
| Allocation concealment (selection bias) | Low risk | "The sequence was concealed until assignment and the personnel enrolling participants did not know in advance which treatment the patient was assigned". |
| Blinding of participants (performance bias) | High risk | Nature of delivered intervention |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | No information for judgement. However, blinding of participants not possible because of nature of delivered intervention |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | No objective outcome planned and assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with other conservative treatment versus the same conservative treatment |
Gandhi 2016.
| Study characteristics | ||
| Methods | Study design: single‐centre, quasi‐experimental pilot study Setting: not reported Timing: the study was conducted for a period of 6 weeks. Interventions: control group received myofascial release therapy for the shoulder whereas the experimental group received myofascial release therapy with shoulder taping. The treatment was given on alternative days. Sample size: 38 collegiate basketball players were recruited for the study. Sample size was not calculated. Analysis: not reported | |
| Participants | Criteria for defining the condition being treated: clinical diagnosis of subacromial impingement syndrome, positive shoulder impingement test
Restriction on duration of symptoms – if yes, participants specified this
Inclusion criteria: male basketball players, age group 18‐22 years
Exclusion criteria: history of previous injury around shoulder, severe labrum or capsule tear, patient with radiating pain, severe pain around the shoulder, allergic to tape and skin infections
Baseline characteristics:
Overall cohort of participants:
Number of participants at enrolment: NR
Number randomised: 38
Number included in analyses: 38
Age: 20 ± 2 years
Sex: M 38 (100%)
Diagnosis: subacromial impingement syndrome
Intervention: myofascial release therapy + Kinesio Taping (KT)
Mean (SD) pain (NPRS 0‐10): 6.39 (not reported) Mean (SD) function (SPADI): 79.4 (not reported) Intervention: myofascial release therapy Mean (SD) pain (NPRS 0‐10): 6.47 (not reported) Mean (SD) function (SPADI): 79.4 (not reported Pretreatment group differences: not reported |
|
| Interventions | Experimental: kinesio taping [KT]
Tape: not specified; taping method: not specified; target: deltoid; number of applications: 18; single application duration: 2 dd; provider: not reported Co‐intervention: myofascial release therapy (stretch of pectoralis minor and pectoralis major, and anterior part of deltoid) Control group: myofascial release therapy (stretch of pectoralis minor and pectoralis major, and anterior part of deltoid) |
|
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | The authors did not reported any source of funding. The authors declared any conflict of interest. Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "players were divided into two groups with equal number of participants". "Block randomization process was used" Insufficient information for judgement |
| Allocation concealment (selection bias) | Low risk | "Block randomization process was used and randomly done 1 or 2 labeled envelopes to determine their groups allocation, the subjects done 1 of remaining 2 envelopes to and the process was repeated". |
| Blinding of participants (performance bias) | High risk | Nature of delivered intervention |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | No information for judgement. However, blinding of participants not possible because of the nature of the delivered intervention |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | No objective outcome planned and assessed |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data regarding loss to follow‐up. Insufficient information for judgement |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with other conservative treatment versus the same conservative treatment |
Gençbay 2019.
| Study characteristics | ||
| Methods | Study design: single‐centre Setting: outpatient clinic of Physical Medicine and Rehabilitation at Bakirkoy Sadi Konuk Training and Research Hospital Timing: the study was conducted for a period of 3 weeks. Interventions: group 1 received Extracorporeal Shockwave Therapy (ESWT group), and group 2 received kinesio taping therapy (KT group). KT was applied twice a week and each patient received a total of 6 KT therapies in total. Co‐interventions: cold pack therapy was applied for 30 minutes on affected shoulder skin with its fabric cover until the end of the treatment. An exercise program (including a range of motion exercises, Codman's pendulum exercises and finger ladder exercises) was also given to all patients. The patients did the exercises in 2 sets, 10 repetitions and 5 seconds rest between sets at the clinic and two times (with 12 hours interval) at home. Sample size: fifty‐one patients (41 women and 10 men). Sample size was not calculated. Analysis: not reported |
|
| Participants | Diagnosed by physical examination, diagnostic tests including shoulder pain between 60‐120° with shoulder elevation (positive painful arch test), positive NEER test, painful internal and external rotation, and pain in daily living activities
Restriction on duration of symptoms: shoulder pain which had been ongoing for at least one month
Inclusion criteria: aged 25‐70 years, presented with shoulder pain which had been ongoing for at least one month
Exclusion criteria: not stated
Baseline characteristics:
Overall cohort of participants:
Number of participants at enrolment: not reported
Number randomised: not reported
Number included in analyses: 51
Age: between 26 and 69 years (mean age: 47.47 ± 10.12 years)
Sex: M 41 (19.6%)
Diagnosis: subacromial impingement syndrome
Intervention: kinesio Taping (KT)
Mean (SD) pain (VAS 0‐10): 4.09 (0.78) Mean (SD) function (DASH): 47.34 (17.09) Control: ESWT Mean (SD) pain (VAS 0‐10): 4.21 (0.79) Mean (SD) function (DASH): 44.03 (14.49) Pretreatment group differences: not reported, only age and sex were reported |
|
| Interventions | Experimental: kinesio taping Tape: precut Kinesio Tex; taping method: not reported; target: deltoid; number of applications: 6; single application duration: 3‐5 dd; provider: not reported, co‐interventions: cold pack therapy for 30 minutes until the end of the treatment. An exercise program (including a range of motion exercises, Codman's pendulum exercises and finger ladder exercises): 2 sets of exercise, 10 repetitions and 5 seconds rest between sets at the clinic and two times (with 12 hours interval) at home Control: ESWT Extracorporeal Shockwave Therapy: (STORZ Medical Masterpuls MP100‐SWISS brand) was set at a frequency of 12‐15 Hz, 2‐3 bars and 2500 pulses. Co‐interventions: cold pack therapy for 30 minutes until the end of the treatment. An exercise program (including a range of motion exercises, Codman's pendulum exercises and finger ladder exercises): 2 sets of exercise, 10 repetitions and 5 seconds rest between sets at the clinic and two times (with 12 hours interval) at home |
|
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | The authors did not reported any source of funding. The authors declared any conflict of interest. Trial registration: not reported Adverse events: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly divided into two groups". Insufficient information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "The patients were randomly divided into two groups". Insufficient information for judgement |
| Blinding of participants (performance bias) | Unclear risk | Authors did not provide information regarding blinding. No information for judgement |
| Blinding of personnel (performance bias) | Unclear risk | Authors did not provide information regarding blinding. No information for judgement |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | Authors did not provide information regarding blinding. No information for judgement |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Unclear risk | Authors did not provide information regarding blinding. No information for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No data regarding loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Goksu 2016.
| Study characteristics | ||
| Methods | Study design: single‐centre, randomised control trial Setting: not reported. Timing: From 2012 to 2013 Interventions: a single subacromial corticosteroid and local anaesthetic injection versus kinesio taping performed three times in intervals of 3 days Sample size: sixty‐one patients (48 females and 13 males; mean age: 43.04 ± 6.31 years) with SIS were enrolled into the study. Power analyses demonstrated a need for at least 30 participants per group given an SD of 20 mm VAS, a difference in pain intensity between groups of 20 mm on the VAS, at a level of 0.05 with power set at 60%. Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: pain before 150 in any plane of range of motion, positive Jobe or Hawkins test, pain in daily living activities, detection of rotator cuff tendinopathy/subacromial impingement syndrome on magnetic resonance imaging (MRI)
Restriction on duration of symptoms: presented with shoulder pain which had been ongoing for one to three months
Inclusion criteria: aged 20‐50 years
Exclusion criteria: previous fracture in the shoulder girdle complex, glenohumeral dislocation/subluxation, acromioclavicular sprain or separation, adhesive capsulitis, diabetes mellitus, use of anticoagulants, history of steroid injection therapy for shoulder, total rupture in the rotator cuff tendons on MRI, history of neck and shoulder surgery, or radicular neck pain within previous 3 months, patients taking regular systemic NSAIDs or steroids, pregnant or breastfeeding mothers and malignancy
Baseline characteristics: Intervention: Kinesio Taping (KT) Number randomised: 34 Number included in analyses: 30 (4 lost to follow‐up) Age: 42.63 ± 6.88 years Sex: M 5; F 25 Diagnosis: rotator cuff tendinopathy/subacromial impingement syndrome Dominant shoulder affected: 21 Duration of symptoms: 2.33 ± 0.78 months Mean (SD) pain (VAS 0‐100): 33 (11.18) Mean (SD) function (SPADI): 43.94 (13.39) Control: subacromial injection Number randomised: 33 participants Number included in analyses: 31 participants (2 lost to follow‐up) Age: 43.45 ± 6.39 Sex: M 8; F 23 Diagnosis: rotator cuff tendinopathy/subacromial impingement syndrome Dominant shoulder affected: 20 participants Duration of symptoms: 2.37 ± 0.81 months Mean (SD) pain (VAS 0‐10): 36.77 (13) Mean (SD) function (SPADI): 44.93 (13.48) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Experimental: KT
Tape: kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus, coracoid process; number of applications: 3; single application duration: 3 dd; provider: physician. Co‐interventions: home exercise program comprising pendulum exercises and pain‐limited active ROM exercises of shoulder elevation, depression, flexion, abduction, rotations, and strengthening exercises. 10 repetitions in 1 set daily, 30 s rest periods between sets of different types of exercises; 7 sessions with 24 h between sessions Control: subacromial injection Subacromial corticosteroid injection (1 cc triamcinolone acetonide ‐ 40 mg) and 4 cc bupivacaine combination with a 22‐G injector using posterior subacromial approach Co‐interventions: home exercise program comprising pendulum exercises and pain‐limited active ROM exercises of shoulder elevation, depression, flexion, abduction, rotations, and strengthening exercises. 10 repetitions in 1 set daily, 30 s rest periods between sets of different types of exercises; 7 sessions with 24 h between sessions |
|
| Outcomes | All evaluations were performed before treatment, and at the first and fourth weeks after therapies.
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | The authors did not reported any source of funding. The authors declared any conflict of interest. Trial registration: not reported Data analysis: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly allocated to receive either single local subacromial corticosteroid/LA injection or KT therapy". "Casual randomization using sealed numbered envelopes without strata or blocks was performed by an administrative assistant". Insufficient information for judgement regarding random sequence generation |
| Allocation concealment (selection bias) | Low risk | "Casual randomization using sealed numbered envelopes without strata or blocks was performed by an administrative assistant". p.485 |
| Blinding of participants (performance bias) | High risk | Nature of delivered intervention |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "The same physician blinded to randomization evaluated all the patients before treatment, and on the first and fourth week of the treatments (FT)". However, blinding of participants was not possible because of the nature of the delivered intervention. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Unclear risk | No information for judgement on methods used in the ROM measurement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Hsu 2009.
| Study characteristics | ||
| Methods | Study design: a cross‐over, pretest/post‐test repeated measures design was used. Setting: not reported Timing: not reported Interventions: an elastic taping (Kinesio TexTM) versus a placebo taping (3 MMicropore tape) over the lower trapezius muscle Sample size: seventeen baseball players with shoulder impingement were recruited and completed the tests. Power analyses demonstrated a need for at least 30 participants per group given an SD of 20 mm VAS, a difference in pain intensity between groups of 20 mm on the VAS, at a level of 0.05 with power set at 60%. Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: subjects were included if they showed a positive sign in two or more shoulder impingement screening items, and in at least one of the specific subacromial impingement tests. The shoulder impingement screening items were: (1) a history of proximal anterior or lateral shoulder pain persisting for more than 1 week during the last six months; (2) painful arc with active shoulder elevation; (3) tenderness to palpation of rotator cuff tendons; (4) pain with resisted isometric shoulder abduction; (5) positive Jobe’s test (empty can test). Specific subacromial impingement tests used in this study were the Neer sign and Hawkins sign.
Restriction on duration of symptoms: more than 1 week during the last six months
Inclusion criteria: baseball players
Exclusion criteria: (1) a history of dislocation or traumatic injuries on the tested shoulder complex; (2) a history of shoulder surgery within the last 6 months; (3) reproduction of symptoms in the cervical screening examination (active and passive range of motion, and overpressure); (4) failure to complete two testing sessions
Baseline characteristics:
Overall cohort of participants:
Number randomised: 17
Number included in analyses: 17
Age: 23 ± 2.8 years
Sex: NR
Diagnosis: shoulder impingement
Duration of symptoms: from 0 to 24 months (median = 2 months) Intervention: kinesio Taping Mean (SD) pain not measured Mean (SD) function not measured Comparator: sham taping Mean (SD) pain not measured Mean (SD) function not measured Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Intervention: kinesio Taping
Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: lower trapezius; number of applications: 1; single application duration: immediate; provider: not reported Control: sham taping The placebo tape was a same‐sized Y‐shaped 3 M Micropore tape (3 M, St. Paul, USA), applied over the same position without any stretch force. |
|
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: this study was sponsored by China Medical University (CMU94‐038) and Taipei City Hospital. Conflict of interest: not reported Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "All subjects received both types of taping with the order of taping randomly assigned as the elastic taping first or the placebo taping first". No information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "All subjects received both types of taping with the order of taping randomly assigned as the elastic taping first or the placebo taping first". No information for judgement |
| Blinding of participants (performance bias) | Low risk | "the placebo tape was same sized..." |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Low risk | Participants were blinded to the interventions. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate outcome measurements for ROM, muscle strength, EMG. "the lower trapezius muscle strength was tested by a blinded examiner." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing data |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | No co‐interventions |
Jena Etnoyer‐Slaski 2016.
| Study characteristics | ||
| Methods | Study design: single‐centre randomised control trial; open‐label Setting: outpatients who reported to the Sport and Spine Rehab, Rockville, Maryland, United States, 20878 Timing: not reported Interventions: increasing tension TheraBand Kinesiology Tape (TB‐KT) vs no tension TB‐KT Sample size: a convenience sample size of 36 patients was recruited. Analysis: per‐protocol analysis executed | |
| Participants | Criteria for defining the condition being treated: diagnosis of shoulder pain tested within the first 2 to 3 therapy visits
Inclusion criteria: 18‐64 years old
Exclusion criteria: corticosteroid treatment within the last two weeks; post‐surgical cases; and pregnancy
Baseline characteristics:
Overall cohort of participants if reported:
Number of participants at enrolment: 36
Number randomised: 36
Number included in analyses: 25
Age (mean and range): 39.81 (18 to 64) years
Sex: M 18; F 18
Diagnosis: Shoulder pain
Intervention: increasing Tension Taping (ITT)
Number randomised: 16
Number included in analyses: 13 (3 lost to follow‐up)
Age: 42.38 (18 to 63) years
Sex: M 9; F 7
Mean (SD) pain (NPRS 0‐10): 5.46 (0.76) Mean (SD) function (PENN Shoulder Score): 53.53 (6.24) Control: control Tension Taping (CTT) Number randomised: 20 Number included in analyses: 12 (8 lost to follow‐up) Age: 37.75 (19 to 64) years Sex: M 9; F 11 Mean (SD) pain (NPRS 0‐10): 5.12 (0.734) Mean (SD) function (PENN Shoulder Score): 52.09 (5.99) Pretreatment group differences: not reported |
|
| Interventions | Intervention: ITT
Tape: not reported; taping method: not specified; target: supraspinatus, infraspinatus; number of applications: not reported; single application duration: not reported; provider: clinician
Over the course of the 4 weeks of care, the tension of the intervention group’s tape systemically increased based on the following timelines:
week 1: 0% tension
week 2: 25% tension
week 3: 50% tension
week 4: 75% tension
Intervention: CTT
Over the course of the 4 weeks of care, the tension of the control group’s tape remained at 0% tension. No co‐intervention used |
|
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: not reported Trial registration: NCT02686437 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Allocation: Randomized; Intervention Model: Parallel Assignment; Masking: None (Open Label); Primary Purpose: Treatment". Insufficient information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "Allocation: Randomized; Intervention Model: Parallel Assignment; Masking: None (Open Label); Primary Purpose: Treatment". Insufficient information for judgement |
| Blinding of participants (performance bias) | High risk | "None (Open Label)" |
| Blinding of personnel (performance bias) | High risk | "None (Open Label)" |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "None (Open Label)" |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Adverse events reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Unbalanced and high dropout rate (n = 3/16; n = 8/20) |
| Selective reporting (reporting bias) | Low risk | Published protocol without changes in outcome details |
| Unequal use of co‐intervention | Low risk | No co‐interventions |
Kang 2020.
| Study characteristics | ||
| Methods | Study design: single‐blinded randomised controlled trial Setting: an outpatient rehabilitation clinic in a university hospital Timing: the study was conducted for a period of 4 weeks. Interventions: kinesiology taping with and without tension. Both groups also performed strengthening and stretching exercises 3 times per week for 4 weeks. Sample size: the sample size assessment was reported. A sample size of 18 subjects per group can provide 80% power to detect an effect size of 0.85 between 2 groups of shoulder angles at an alpha level of 0.05 with a two‐tailed test using G‐power. Thirty‐six subjects aged 20‐75 years were recruited from University Hospital. Analysis: not reported |
|
| Participants | The inclusion criterion for subjects with SIS was positive results on at least 3 of 5 tests: Neer's test, Hawkin's test, Empty can test, pain or weakness with resisted external rotation test, and tenderness in the tendon of rotator cuff. The criterion for RSP was acromial distance of 2.6 cm, which was measured as the distance from the table to the border of the lateral‐posterior acromion when subjects were in supine position with the shoulder in neutral position. Each patient had been diagnosed with impingement symptoms by a physician or orthopaedic surgeon. Exclusion criteria: patients with shoulder pain onset due to trauma, a history of shoulder fracture or dislocation, cervical radiculopathy, degenerative joint disease of the shoulder, or surgical interventions on the shoulder. Thirty‐six round shoulder subjects with impingement syndrome participated in this study, and 34 completed the 4‐week follow‐up (2 subjects were lost to follow‐up). Baseline characteristics: Intervention: kinesiology taping/exercise group Number randomised: 36 Number included in analyses: 18 Age: 50 ± 13 years Sex: F 14/18 Mean (SD) pain (VAS 0‐10): 4.7 (1.7) Mean (SD) function not measured Control intervention: Placebo taping/exercise group Number randomised: 36 Number included in analyses: 34 (2 lost) Age: 45 ± 9 years Sex: F 10/16 Mean (SD) pain (VAS 0‐10): 5.1 (1.5) Mean (SD) function not measured Diagnosis: subacromial impingement syndrome (SIS) and round shoulder position (RSP) Duration of symptoms: not stated Pretreatment group differences: reported |
|
| Interventions | Intervention: kinesiology taping [KT] Tape: not reported (size not specified); taping method: alternative technique; target: trapezius, glenohumeral articulation; number of applications: 8; single application duration: 2‐3 dd; provider: not reported Co‐intervention: exercise group Control: sham taping Co‐intervention: exercise group |
|
| Outcomes | Overall Pain: Visual Analogue Scale 0‐10 cm Function: Self‐reported flexi‐level scale of shoulder function (FLEX‐SF) Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: not reported Trial registration: NCT03413488 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A randomized clinical trial with a blinded assessor was conducted.The patient took a form (with a letter a (n = 18) or b (n = 18)) indicating allocation to either group from a closed envelope; only the therapist had direct access to the randomization list". Insufficient information for judgement |
| Allocation concealment (selection bias) | Low risk | "A randomized clinical trial with a blinded assessor was conducted.The patient took a form (with a letter a (n= 18) or b (n= 18)) indicating allocation to either group from a closed envelope; only the therapist had direct access to the randomization list". |
| Blinding of participants (performance bias) | High risk | This study was a single‐blinded randomised controlled trial. |
| Blinding of personnel (performance bias) | High risk | This study was a single‐blinded randomised controlled trial. |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "A randomized clinical trial with a blinded assessor was conducted. Outcomes were assessed before intervention and at 2 and 4 weeks during the intervention period. The investigator was blinded to the results, and a recorder noted the outcomes". Participants were not blinded. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | "A randomized clinical trial with a blinded assessor was conducted. Outcomes were assessed before intervention and at 2 and 4 weeks during the intervention period. The investigator was blinded to the results, and a recorder noted the outcomes". |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. No information for intention‐to‐treat |
| Selective reporting (reporting bias) | High risk | ClinicalTrials.gov Identifier: NCT03413488. Published protocol with changes in outcome details in the publication: introduction of shoulder angle (SA) and missing outcomes (length of the pectoralis minor, acromial distance, posterior and anterior shoulder tightness, distance of scapular medial border) |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus sham taping with the same co‐intervention |
Kaya 2011.
| Study characteristics | ||
| Methods | Study design: quasi‐RCT Setting: not reported Timing: September 2006 to December 2008 Interventions: therapeutic KT plus home exercise program (HEP) versus physical therapy modalities (ultrasound, transcutaneous electrical nerve stimulation (TENS), exercise, and hot pack) plus the same HEP Sample size: 55 patients were enrolled in the study. The minimum sample size required for 80% statistical power and 5% significance level was 22 for each group. Estimated power for 55 subjects was calculated as 90.7%. Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: pain before 150° of active shoulder elevation in any plane, positive empty can test indicating the possible supraspinatus involvement, positive Hawkins–Kennedy test indicating possible external impingement, subjective complaint of difficulty performing activities of daily living.
Restriction on duration of symptoms: shoulder pain which lasted more than 6 months
Inclusion criteria: age of 18‐70 years
Exclusion criteria: intra‐articular steroid injection, shoulder girdle fracture, glenohumeral dislocation/subluxation, acromioclavicular sprain, concomitant cervical symptoms consistent with radiculopathy, history of a shoulder surgery within the previous 12 weeks
Baseline characteristics:
Intervention: kinesio Taping (KT)
Number randomised: 30
Number included in analyses: 30
Age: 56.2 ± 7.2 years
Sex: ND
Diagnosis: subacromial impingement syndrome
Duration of symptoms: 6.3 ± 4.3 months
Mean (SD) pain (VAS 0‐100): 42 (29.5) Mean (SD) function (DASH): 58.6 (16.5) Comparator: physical therapy (PT) Number randomised: 30 Number included in analyses: 25 (5 lost to follow‐up) Age: 59.5 ± 7.9 years Sex: ND Diagnosis: subacromial impingement syndrome Duration of symptoms: 7.2 ± 4.9 months Mean (SD) pain (VAS 0‐100): 54 (28.3) Mean (SD) function (DASH): 56.6 (17.8) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Intervention: KT
Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus, teres minor; number of applications: 3; single application duration: 3 dd; provider: the same physician. Co‐intervention: home exercise program
HEP consisted of isometric exercises, range of motion, strengthening (serratus anterior, trapezius, and external rotation) and stretching (posterior shoulder and pectoralis minor), and relaxation of the trapezius twice a day.
Control: PT
A daily program of physical therapy modalities (ultrasound, transcutaneous electrical nerve stimulation (TENS), exercise, and hot pack). Intermittent ultrasound of 1 MHz and 1 W/cm2 for 5 min was used daily. TENS and hot pack were applied 20 min a day. Co‐intervention: Home Exercise Program HEP consisted of isometric exercises, range of motion, strengthening (serratus anterior, trapezius, and external rotation) and stretching (posterior shoulder and pectoralis minor), and relaxation of the trapezius twice a day. |
|
| Outcomes | All measures were obtained at baseline, and at first (except for the DASH) and second weeks of the treatment
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: not reported Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "Subjects were assigned to two groups according to their date of admittance". "The lack of randomization and sequential allocation of patients are also other factors that weaken the power of this study". |
| Allocation concealment (selection bias) | High risk | "The lack of randomization and sequential allocation of patients are also other factors that weaken the power of this study". |
| Blinding of participants (performance bias) | High risk | Nature of delivered intervention |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "KT was performed by the first author, and the assessments were carried out by the first and second authors". Participants were not blinded due to the nature of delivered interventions. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | No objective outcome planned and assessed |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "The possible existence of a drop out bias which may lead to over‐ or underestimation of our results" |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Kaya 2014.
| Study characteristics | ||
| Methods | Study design: randomised clinical trial Setting: outpatient physical therapy unit Timing: not reported Interventions: KT with exercise versus manual therapy with exercise Sample size: fifty‐four patients diagnosed as having subacromial impingement syndrome were included. Power analyses demonstrated a need for at least 26 participants per group given an SD of 25 mm VAS, difference in pain intensity between groups of 20 mm on the VAS, an α level of.05, with power set at 80% Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: the combination of the Hawkins‐Kennedy impingement sign, the painful arc sign, and the infraspinatus muscle test was used to diagnose SIS.
Exclusion criteria: cervical spine involvement; presence of a glenohumeral joint adhesive capsulitis, or instability; a history of previous shoulder surgery; having another physiotherapy treatment of this disorder in the past 6 weeks; or steroid injection into or around the shoulder in the past 2 months. The patients with recurrent complaints or long history of complaint over a year were also excluded. Furthermore, MRI scans were assessed to confirm if there were any massive rotator cuff or labral tears to exclude from the study.
Baseline characteristics:
Intervention: Kinesio Taping
Number randomised: 30
Number included in analyses: 28 (2 lost to follow‐up)
Age: 50.85 ± 5.17 years
Sex: M 11; F 17
Diagnosis: subacromial impingement syndrome
Duration of symptoms: 6–26 weeks
Mean (SD) pain (VAS 0‐10): 2.89 (3.10) Mean (SD) function (DASH): 65.01 (16.38) Comparator: Manual Therapy Number randomised: 30 Number included in analyses: 26 (4 lost to follow‐up) Age: 47.15 ± 9.44 years Sex: M 10; F 16 Diagnosis: subacromial impingement syndrome Duration of symptoms: 6–28 weeks Mean (SD) pain (VAS 0‐10): 3.11 (3.03) Mean (SD) function (DASH): 64.97 (18.39) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Intervention: Kinesio Taping Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: according to patient’s need; number of applications: 6; single application duration: 4‐5 dd; provider: the same clinician. Co‐intervention: Exercise Therapy The exercise therapy included 3 phases: phase 1: strengthening of the rotator cuff; phase 2: shoulder elevation exercises; phase 3: push‐up on wall and push‐up plus with Thera‐Band. To move onto another phase, the subject was required to perform the exercises in the previous phase for 2 weeks without an increase in symptoms. Control: Manual therapy The MT group received a combination of manual therapies by the therapist. General mobilisation, neuromuscular facilitation techniques, glenohumeral joint mobilisation, soft tissue massage and joint mobilisation of the neck, thoracic region, and elbow areas by physical therapist experienced in manual therapy. Co‐intervention: Exercise Therapy The exercise therapy included 3 phases: phase 1: strengthening of the rotator cuff; phase 2: shoulder elevation exercises; phase 3: push‐up on wall and push‐up plus with Thera‐Band. To move onto another phase, the subject was required to perform the exercises in the previous phase for 2 weeks without an increase in symptoms. | |
| Outcomes | Assessments were applied at the baseline and after completing 6 weeks of related interventions
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: none Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Randomization was designed according to the random case sample in SPSS program (SPSS, Chicago, IL). The SPSS software randomly assigned participants to one of the groups". |
| Allocation concealment (selection bias) | Unclear risk | "were randomly allocated to 2 study groups: kinesio taping with exercise (n = 28) or manual therapy with exercise (n = 26)". Insufficient information for judgement |
| Blinding of participants (performance bias) | High risk | Nature of delivered intervention |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | Participants not blinded due to the nature of delivered intervention |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | No objective outcome planned and assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. "The subset of per‐protocol analysis is an 'as‐treated' analysis in which only participants adherent to the intervention were included from all randomized participants by using baseline‐post intervention analysis". |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Keenan 2017.
| Study characteristics | ||
| Methods | Study design: placebo‐controlled quasi‐experimental study Setting: research laboratory Timing: not reported Interventions: kinesio tape versus placebo taping Sample size: 30 subjects participated in the study. Sample size for a repeated measures ANOVA of within‐between factors was calculated a priori using an α = 0.05, power of at least 80%, moderate effect size (0.30), moderate correlation among repeated measures (0.60), and three groups with two testing sessions per subject. 27 subjects per group were required for this study (9 healthy controls, 9 SIS taped with KT, 9 SIS taped with Coverroll®). Based on potential attrition of 10%, total sample size was increased to 30 (10 per group). Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: positivity at each of these three tests: Neer’s Test, Hawkins‐Kennedy Test, and Painful Arc Test
Restriction on duration of symptoms: localised shoulder pain for a minimum of two weeks
Inclusion criteria: presence on the day of testing with clinical signs of SAIS
Exclusion criteria: healthy subjects had no current shoulder pathology, neuromuscular disease, and peripheral neuropathy; previous history of shoulder complex fracture, surgery, or injection; and previous history of cervical spine or brachial plexus injury. Subjects with SAIS were free from neuromuscular disease and peripheral neuropathy as well as having no previous history of shoulder complex fracture/surgery, cervical spine injury, or brachial plexus injury.
Baseline characteristics:
Intervention: Kinesio Taping
Number randomised: 10
Number included in analyses: 10
Age: 24.91 ± 5.14 years
Sex: M 5; F 5
Diagnosis: subacromial impingement syndrome
Mean (SD) pain not measured Mean (SD) function (SPADI): 32.77 (13.93) Control: sham Taping Number randomised: 10 Number included in analyses: 10 Age: 23.78 ± 3.17 years Sex: M 8; F 2 Diagnosis: subacromial impingement syndrome Mean (SD) pain not measured Mean (SD) function (SPADI): 25.31 (17.15) Control 2: Kinesio Tape on healthy subjects Number randomised: 10 Number included in analyses: 10 Age: 25.78 ± 3.78 years Sex: M 3; F 7 Diagnosis: none Mean (SD) pain not measured (healthy subjects) Mean (SD) disability not measured (healthy subjects) Pretreatment group differences: Statistical differences in gender composition between groups |
|
| Interventions | Intervention: KT
Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus, coracoid process; number of applications: 1; single application duration: immediate; provider: the same clinician Control: ST Sham taping procedures followed Kase protocol, using Cover‐Roll tape. |
|
| Outcomes | Measures pre/post‐treatment:
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: Freddie H. Fu, MD Graduate Research Award and the University of Pittsburgh School of Health and Rehabilitation Sciences Research Development Fund Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | "SAIS subjects were alternatively allotted at the time of enrolment". |
| Allocation concealment (selection bias) | Unclear risk | "SAIS subjects were alternatively allotted at the time of enrolment". Insufficient information for judgement |
| Blinding of participants (performance bias) | Low risk | "Subjects were blinded as to which tape they received". |
| Blinding of personnel (performance bias) | High risk | Nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Low risk | No information for judgement. However, "Subjects were blinded as to which tape they received". |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. muscle strength) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. No intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | No co‐interventions |
Kocyigit 2016.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blind, placebo‐controlled trial Setting: outpatient clinic Timing: not reported Interventions: KT versus sham taping Sample size: 45 patients were randomised; 41 completed the study. Type I error (α) was set at 0.05 and power of the test was selected as 0.80 and the calculated sample size appropriate to test the hypothesis and have confidence was 41. The number of patients to ensure that final sample size was achieved was calculated to be 46 when the proportion of attrition was 10%. Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: Neer’s impingement sign; Hawkins’ test; painful arc test; and the Jobe test applied to all participants by the same physiatrist at baseline. The patients with positive results for at least three of these tests were diagnosed with SIS.
Inclusion criteria: mild–moderate shoulder pain (VAS between 20 and 70 mm); age between 18–70 years; no previous application of KTs
Exclusion criteria: history of previous shoulder fracture/surgery in last 6 months; previous or concurrent diagnosis of rotator cuff tear; glenohumeral joint/ACJ osteoarthritis; cervical disc herniation accompanied by radicular symptoms; inflammatory joint disease; history of electrotherapy or injection for the shoulder in the last 3 months
Baseline characteristics:
Overall cohort of participants:
Number of participants at enrolment: 55
Number randomised: 45
Number included in analyses: 41
Age (mean and SD, or range): 45 ± 15 years (range 20–65 years)
Diagnosis: subacromial impingement syndrome
Duration of symptoms: 38 ± 46 weeks (range 4–204 weeks)
Intervention: Kinesio Taping (KT)
Number randomised: 22
Number included in analyses: 21 (1 lost to follow‐up)
Age: 50.6 ± 10.1 (range 23–65 years)
Sex: M 6; F 15 Mean (SD) pain (VAS 0‐100): 48.14 (22.12) Mean (SD) function (Constant score): 54.6 (6.3) Control: sham Taping (ST) Number randomised: 23 Number included in analyses: 20 (3 lost to follow‐up) Age: 49.2 ± 8.8 (range 26–65 years) Sex: M 7; F 13 Mean (SD) pain (VAS 0‐100): 50 (21.7) Mean (SD) function (Constant scoreI): 50.5 (5.1) Pretreatment group differences: No between‐group differences were observed. |
|
| Interventions | Intervention: KT Tape: not reported; taping method: not specified; target: deltoid, ACJ articulation; number of applications: 3; single application duration: 4 dd; provider: not reported Control: ST The control group received sham taping (5 centimetres beta fix surgical hypoallergenic flexible tape) identical to the KT group. No force was applied to the tape during application, the tape merely being overlaid on the skin. Co‐interventions: An exercise program consisting of Codman pendulum exercises 10 repetitions/3 sets/day was prescribed to all patients. Use of nonsteroidal anti‐inflammatory drugs was restricted, and the participants were allowed to take paracetamol 500 mg tablets per day when they experienced pain interfering with functional activities. | |
| Outcomes | Assessments were executed at baseline, at the end of the taping period (12th day), and at one month post‐intervention
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "We used the numbered envelopes method for randomisation of patients into two groups". |
| Allocation concealment (selection bias) | Unclear risk | "We used the numbered envelopes method for randomisation of patients into two groups". Insufficient information for judgement |
| Blinding of participants (performance bias) | Low risk | "The control group received sham taping identical to the KT group". "We do believe that blinding of the subjects was appropriate". |
| Blinding of personnel (performance bias) | High risk | High for nature of delivered intervention |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Low risk | "The control group received sham taping identical to the KT group". " We do believe that blinding of the subjects was appropriate". |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcome (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. Per‐protocol analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus sham taping with the same co‐intervention |
Kul 2018.
| Study characteristics | ||
| Methods | Study design: single‐centre two‐arm randomised controlled trial Setting: not reported Timing: between June 2014 and June 2015 Interventions: kinesio taping plus home exercise program (HEP) versus physical therapy and HEP Sample size: 40 patients were randomly divided into two study groups. Analysis: not reported | |
| Participants | Criteria for defining the condition being treated: patients clinically (Neer, Hawkins, painful arc, drop arm, Yergason, supraspinatus, and active ROM tests were performed for clinical diagnosis) and radiologically (diagnosed by a radiologist on magnetic resonance imaging) diagnosed with SIS (who had supraspinatus tendinitis or partial supraspinatus rupture) were included in the study.
Inclusion criteria: aged between 18 and 70 years; able to comply with the treatment protocol
Exclusion criteria: history of conservative PT in the shoulder area within the last 6 months, local steroid injection to the shoulder area within the last 3 months, chronic steroid use, adhesive capsulitis, presence of bicipital tendinitis, total rupture in the supraspinatus or other rotator cuff muscles, and rotator cuff tendinitis, and with a history of shoulder joint surgery, systemic inflammatory disease that can affect the shoulder area, cervical radiculopathy, metabolic bone disease, and diabetes mellitus
Baseline characteristics:
Intervention: Kinesio Taping (KT)
Number randomised: 20
Number included in analyses: 20
Age: 49.6 ± 10.1 years
Sex: M 3; F 17
Diagnosis: subacromial impingement syndrome
Duration of symptoms: 18.5 ± 19.4 months
Mean (SD) pain (VAS 0‐10): 4 (0) Mean (SD) function (WORC): 1288.5 (293) Control: Physical Therapy (PT) Number randomised: 20 Number included in analyses: 20 Age: 54.8 ± 8.2 years Sex: M 7; F 13 Diagnosis: subacromial impingement syndrome Duration of symptoms: 12.6 ± 11 months Mean (SD) pain (VAS 0‐10): 3.65 (1.8) Mean (SD) function (WORC): 1246.5 (253.5) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Intervention: KT Tape: not reported; taping method: Kase protocol; target: deltoid, supraspinatus; number of applications: 3; single application duration: 5 dd; provider: not reported. Co‐interventions: Home Exercise Program consisting of ROM, Codman, and stretching (posterior capsule) and strengthening (isometric) exercises. Patients were asked to follow the exercise routine 3 times a day and to repeat each exercise 10 times. Control: PT PT group patients were asked to follow a daily program that consisted of applying a Hot‐Pack for 20 min, transcutaneous electrical nerve stimulation (TENS) for 30 min, and ultrasound (US) with settings of 1 MHz and 1 W/cm2 for 10 min in a continuous mode on the painful shoulder and in a circular style. Co‐interventions: Home Exercise Program consisting of ROM, Codman, and stretching (posterior capsule) and strengthening (isometric) exercises. Patients were asked to follow the exercise routine 3 times a day and to repeat each exercise 10 times. | |
| Outcomes | For each outcome, patients were assessed based on the pretreatment (T1), post‐treatment (T2), and end‐of‐study (T3: post‐treatment 1‐month follow‐up)
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | The authors declared that this study had received no financial support. Conflict of interest: none Trial registration: NA |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Patients were numbered according to their order of admission and were randomly assigned into one of the two groups until the number of the group is equal". Insufficient information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "Patients were numbered according to their order of admission and were randomly assigned into one of the two groups until the number of the group is equal". Insufficient information for judgement |
| Blinding of participants (performance bias) | Unclear risk | "KT and assessments were performed by the same person". Authors did not provide information for judgement regarding blinding. |
| Blinding of personnel (performance bias) | Unclear risk | "KT and assessments were performed by the same person". Authors did not provide information for judgement regarding blinding. |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | "KT and assessments were performed by the same person". Authors did not provide information for judgement regarding blinding. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All patients complied with the treatment protocol. |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Miccinilli 2018.
| Study characteristics | ||
| Methods | Study design: monocentric prospective double‐blind randomised controlled trial Setting: outpatients who report to the Department of Physical and Rehabilitation Medicine of Campus Bio‐Medico, University of Rome Timing: between September 2016 and December 2017 Interventions: KT application plus standardised rehabilitative protocol of exercises versus sham KT application plus the same standardised rehabilitative protocol of exercises Sample size: 42 patients were randomised; 40 participants completed the study. Power calculation was not reported. Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: radiologic diagnosis of rotator cuff tendinopathy (RoCT) with evidence of pathognomonic signs at musculoskeletal echography or magnetic resonance; clinical positivity to at least one of the specific shoulder tests for RoCT shoulder pain
Exclusion criteria: total tendon lesion; previous fracture or shoulder dislocation; presence of skin lesions contraindicating the application of KT; coexisting elbow, forearm, wrist, hand and fingers pathologies; history of neoplasm; cognitive impairment (MMSE < 24); diabetes mellitus; statin use; diagnosis of anxiety‐depressive syndrome
Baseline characteristics:
Intervention: Kinesio Taping (KT)
Number randomised: 21
Number included in analyses: 21
Age: 61 ± 12 years
Sex: M 9; F 12
Diagnosis: rotator cuff tendinopathy
Median (IQR) pain (NRS 0‐10): 3 (1‐3) Median (IQR) function (Constant score): 44 (40‐53) Control: Sham Taping (ST) Number randomised: 21 Number included in analyses: 19 Age: 64 ± 10 years Sex: M 9; F 10 Diagnosis: rotator cuff tendinopathy Median (IQR) pain (NRS 0‐10): 2 (1‐3.5) Median (IQR) function (Constant score): 42 (38‐51.5) Pretreatment group differences: no between‐group differences were observed. |
|
| Interventions | Intervention: KT Tape: not reported; taping method: Kase protocol; target: deltoid, glenohumeral articulation, rhomboid; number of applications: 6; single application duration: 2 dd; provider: physiotherapist Co‐interventions: 10 sessions of rehabilitative treatment, from Monday to Friday for two consecutive weeks, consisting of:
Control: ST Decompressive deltoid‐like application, functional‐like application and a rhomboid‐like application. Taping was positioned without tensioning, with limb in neutral position, without joint involvement (exclusion of the humeral head for the deltoid‐like application, exclusion of the vertebral column for the rhomboid‐like application) Co‐interventions: 10 sessions of rehabilitative treatment, from Monday to Friday for two consecutive weeks, consisting of:
|
|
| Outcomes | Measures pre/post‐treatment:
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: not reported Trial registration: not reported Adverse events: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "subjects were randomly assigned to two groups by another examiner using the envelope system (1:1)". Insufficient information for judgement |
| Allocation concealment (selection bias) | Low risk | "subjects were randomly assigned to two groups by another examiner using the envelope system (1:1)". Insufficient information for judgement |
| Blinding of participants (performance bias) | Unclear risk | "The examiner was blind to real/sham taping treatment. However, the blinding of participants was unclear". |
| Blinding of personnel (performance bias) | High risk | "Even if the physiotherapist involved in rehabilitative treatment was blind to the type of taping application, the application of KT can be recognized for shaping application". |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | "The examiner was blind to real/sham taping treatment. However, the blinding of participants was unclear". |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | The examiner was blind to real/sham taping treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up. No information for intention‐to‐treat analysis |
| Selective reporting (reporting bias) | High risk | No protocol published; discrepancy between Methods and Results sections in outcomes declared |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus sham taping with the same co‐intervention |
Miller 2009.
| Study characteristics | ||
| Methods | Study design: pilot single‐blind, randomised controlled trial Setting: outpatients who report to the Royal Newcastle Hospital, New South Wales, Australia Timing: not reported Interventions: scapular taping plus physical therapy versus physical therapy Sample size: twenty‐two people were recruited. Power calculations were not reported. Analysis: intention‐to‐treat analysis executed | |
| Participants | Criteria for defining the condition being treated: unilateral shoulder pain and positivity at shoulder impingement test described by Hawkins and Kennedy
Restriction on duration of symptoms: pain of more than six weeks duration
Inclusion criteria: people aged between 18 and 70 years. Written and verbal competence in the English language
Exclusion criteria: cervical spine involvement in the disorder defined by active neck movement reproducing pain in the shoulder region; presence of a glenohumeral joint adhesive capsulitis as identified by a loss of passive shoulder motion into external rotation; history of previous shoulder surgery; physiotherapy treatment for this disorder in the past four weeks; steroid injection into or around the shoulder in the past two months; demonstrable neurological deficits; poor or fragile skin condition; report of past skin reaction associated with the use of adhesive tape
Baseline characteristics:
Intervention: Kinesio Taping (KT)
Number randomised: 10
Number included in analyses: 6 (4 lost to follow‐up)
Age (median (interquartile range)): 62 (51–67)
Sex: M 3; F 7
Diagnosis: subacromial impingement syndrome
Duration of symptoms (median (interquartile range)): 16 (7–26) weeks Median (IQR) pain (SPADI pain): 54.6 (43.6‐69.1) Median (IQR) function (SPADI): 47.7 (39.4‐62.8) Control: Physical therapy (PT) Number randomised: 12 Number included in analyses: 11 (1 lost to follow‐up) Age (median (interquartile range)): 54.5 (45.5–62.5) Sex: M 7; F 5 Diagnosis: subacromial impingement syndrome Duration of symptoms (median (interquartile range)): 17 (12–65) weeks Median (IQR) pain (SPADI pain): 60 (32.7‐67.3) Median (IQR) function (SPADI): 54.4 (27.2‐65.1) Pretreatment group differences: at baseline, the control group had a significantly lower median age and a greater number of male participants than the taped group. |
|
| Interventions | Intervention: KT Tape: 50 mm hypoallergenic polyacrylate adhesive bandage over which was laid a 38 mm premium non‐elastic zinc oxide adhesive tape; taping method: scapular taping; target: deltoid, lower trapezius; number of applications: 6; single application duration: 2 dd; provider: trained physiotherapists. Co‐intervention: routine physiotherapy treatment as indicated in an individual assessment of the participants' condition by their treating physiotherapist Control: Physical Therapy Routine physiotherapy treatment as indicated in an individual assessment of the participants' condition by their treating physiotherapist | |
| Outcomes | Measurement occurred prior to randomisation at baseline and then at 2 weeks and 6 weeks following the commencement of treatment.
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Financial support from the Division of Allied Health, Hunter Area Health Service, Australia Conflict of interest: not reported Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomisation list was created using a random number table. |
| Allocation concealment (selection bias) | Low risk | Sequentially numbered sealed opaque envelopes |
| Blinding of participants (performance bias) | High risk | "A randomized, single‐blind clinical trial design was used..All participants were then assessed by a blinded research assistant using standard physiotherapy measures.." |
| Blinding of personnel (performance bias) | High risk | "All participants were then assessed by a blinded research assistant using standard physiotherapy measures". |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "All participants were then assessed by a blinded research assistant using standard physiotherapy measures". However, participants were not blinded. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "One further limitation arose as a consequence of the differential rate of loss to follow‐up. Ideally, this pilot study should have been analyzed using an intention to treat analysis whereby all participants’ data would be included in the final analysis". |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Unequal use of co‐intervention | Low risk | KT with other conservative treatment versus the same conservative treatment |
Mohamed 2019.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial
Setting: King Fahd Specialist Hospital and King Khalid Hospital in Tabuk, Saudi Arabia
Timing: the study was conducted for a period of 6 weeks.
Interventions: group 1 received KT with supervised exercise; group 2 received manual therapy + supervised exercise.
Sample size: the sample size assessment was reported: power of 80%, α = 0.05 to detect a difference of 20%, in the application of KT and MT with SET. Analysis: not reported |
|
| Participants | The inclusion criteria were: pain in the shoulder with no history of major trauma, limited active and passive range of motion in the shoulder and no previous physical therapy treatment taken within the previous year. Exclusion criteria were: shoulder instability, degenerative changes in the shoulder, post‐traumatic stiffness, frozen shoulder, acromioclavicular joint disorders, upper extremity and cervical spine disorders, glenohumeral subluxation, steroid injection in the shoulder over a two‐month period and dislocation. Baseline characteristics: Intervention: Kinesio Taping (KT) + supervised exercise Number randomised: 16 Number included in analyses: not reported Age (average): 44 years Sex: M 100% Diagnosis: subacromial impingement syndrome Duration of symptoms: 44% of patients had the symptoms for three to six months, Mean (SD) pain (NPRS): 5.69 (1.58) Mean (SD) function (SPADI): 35.62 (5.74) Control: manual therapy + supervised exercise Number randomised: 16 Number included in analyses: not reported Age (average): 47 years Sex: M 100% Diagnosis: subacromial impingement syndrome Duration of symptoms: 50% of patients in the MT group had the symptoms for one to three months. Mean (SD) pain (NPRS): 6.56 (1.5) Mean (SD) function (SPADI): 46.87 (8.10) Pretreatment group differences: baseline characteristics were reported but no statistics such as P values were reported; however, the authors declared: "There were no statistically significant differences between the two groups in pre‐treatment evaluation; which indicates that the patients in both groups were identical". |
|
| Interventions | Intervention: Kinesio Taping (KT) Two types of kinesio taping procedure followed in the application of SIS: 1. Muscle Inhibition Technique: KT was applied with 10‐15% tension in the deltoid and supraspinatus muscle, from insertion to origin. 2. Glenohumeral (GH) joint mechanical correction: KT was applied from the anterior to the posterior part of the GH joint with 50–75 % tension. The tape was applied to the subjects for two sessions per week for six weeks. The participants were instructed to remove KT before the subsequent application. Tape: not reported (size not specified); taping method: alternative technique; target: trapezius, glenohumeral articulation; number of applications: 8; single application duration: 2‐3 dd; provider: not reported Co‐intervention: Supervised exercise therapy, self‐correction and stabilisation exercises for the scapula, shoulder depression during movements such as flexion, abduction and external rotation, rotator cuff muscle exercises, and pain‐free ROM exercises Control: Manual Therapy (MT) MT techniques were applied to the joints and related soft tissues at varying speeds and amplitudes, by using passive accessory movements (PAM). Graded mobilisation techniques I‐IV were used in this study. Co‐intervention: supervised exercise therapy, self‐correction and stabilisation exercises for the scapula, shoulder depression during movements such as flexion, abduction and external rotation, rotator cuff muscle exercises, and pain‐free ROM exercises |
|
| Outcomes | Overall pain: numerical pain rating scale (NPRS) 0 ‐ 10 cm Active range of motion ‐ free of pain: flexion, abduction, external rotation with goniometer Function: SPADI Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | The study was supported by grants from the Deanship of Scientific Research, University of Tabuk, Ministry of Higher Education, Kingdom of Saudi Arabia. Conflict of interest: not reported Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "A randomised controlled trial with a total number of thirty‐two subjects participated in the study". Insufficient information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "A randomised controlled trial with a total number of thirty‐two subjects participated in the study". Insufficient information for judgement |
| Blinding of participants (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of personnel (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Unclear risk | Poor reporting prevented any judgement. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Poor reporting prevented any judgement. |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Pekyavas 2016.
| Study characteristics | ||
| Methods | Study design: randomised controlled trial Setting: not reported Timing: not reported Interventions: four groups: 1. exercise (EX); 2. Kinesio Tape (KT) + EX; 3. Manual Therapy + KT + EX; 4. MT + KT + high‐intensity laser therapy (HILT) + EX Sample size: seventy‐five patients were recruited for the study. The power analysis indicated that 15 participants for each group were needed with 80% power and a 5% type 1 error. Analysis: per‐protocol analysis was executed. | |
| Participants | Criteria for defining the condition being treated: shoulder pain (5/10 points from visual analogue scale) and diagnosis of SAIS by a physical medicine and rehabilitation doctor
Restriction on duration of symptoms: symptoms for at least 3 months prior to admission
Exclusion criteria: soft tissue or bone problems affecting the shoulder; acute inflammation affecting the shoulder region; neurologic problems; scoliosis; systematic rheumatic problems; undergone orthopaedic problems or surgery affecting neck; obese (BMI > 30 kg/m2)
Baseline characteristics:
Overall cohort of participants:
Number of participants at enrolment: 75
Number randomised: 70
Number included in analyses: 70
Age (mean and SD): 47.1 ± 13.8 years
Diagnosis: subacromial impingement syndrome
Control: Exercise (EX)
Number randomised: 15
Number included in analyses: 15
Age: 40.6 ± 11.7 years
Mean (SD) pain (SPADI pain): 67.20 (11.48) Mean (SD) function (SPADI): 44.73 (17.17) Intervention: Kinesio Taping (KT) + exercise (EX) Number randomised: 20 Number included in analyses: 20 Age: 49.4 ± 12.6 years Mean (SD) pain (SPADI pain): 55.80 (21.16) Mean (SD) function (SPADI): 72.65 (30.13) Intervention: (KT) + (EX) + Manual Therapy (MT) Number randomised: 16 Number included in analyses: 16 Age: 45.4 ± 15.5 years Mean (SD) pain (SPADI pain): 74.43 (5.25) Mean (SD) function (SPADI): 111 (16.92) Intervention: (KT) + (EX) + (MT) + High‐Intensity Laser Therapy [HILT] Number randomised: 19 Number included in analyses: 19 Age: 51.1 ± 14.3 years Mean (SD) pain (SPADI pain): 76.42 (4.88) Mean (SD) function (SPADI): 114.89 (11.94) Pretreatment group differences: no statistically significant differences were observed between the groups at baseline. |
|
| Interventions | Intervention: KT
Tape: not reported; taping method: Kase protocol; target: deltoid, supraspinatus, glenohumeral articulation; number of applications: 5; single application duration: 3 dd; provider: not reported. Co‐intervention: Home Exercise Program: All the patients were instructed to perform the active ROM, stretching, and strengthening exercise program including rotator cuff muscles, rhomboids, levator scapulae, and serratus anterior with a Thera‐Band at home at least seven times a week for 10–15 min. The exercises were taught by a physiotherapist, and all the patients did the exercises every day during the 3 weeks without fail.
Intervention: MT
Manual treatment consisted of deep friction massage on the supraspinatus muscle, radial nerve stretching, scapular mobilisation, glenohumeral joint mobilisation, and proprioceptive neuromuscular facilitation techniques. Co‐intervention: Home Exercise Program and kinesio taping
Intervention: HILT
HILT group received HILT with a neodymium‐yttrium aluminium garnet laser having a pulsating waveform produced by an HIRO® 3.0 device reaching very high power peaks (3 kW) with an Nd:YAG pulsed source (wavelength 1064 nm). The total dose of energy administered was approximately 2050 J. The total time taken to apply all the three stages of HILT was approximately 30 min. Co‐intervention: Home Exercise Program, kinesio taping and manual therapy Intervention: Home Exercise Program All the patients were instructed to perform the active ROM, stretching, and strengthening exercise program including rotator cuff muscles, rhomboids, levator scapulae, and serratus anterior with a Thera‐Band at home at least seven times a week for 10–15 min. The exercises were taught by a physiotherapist, and all the patients did the exercises every day during the 3 weeks without fail. |
|
| Outcomes | Outcomes were assessed before and at the end of the treatment (15th day).
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "online random allocation software program" |
| Allocation concealment (selection bias) | Unclear risk | "online random allocation software program". It was not clear how and who performed the allocation. |
| Blinding of participants (performance bias) | High risk | "All patients were assessed by an experienced physiotherapist, and the treatments were performed by another experienced physiotherapist in order to provide a single blind structure of the study". |
| Blinding of personnel (performance bias) | High risk | "All patients were assessed by an experienced physiotherapist, and the treatments were performed by another experienced physiotherapist in order to provide a single blind structure of the study". |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | High risk | "All patients were assessed by an experienced physiotherapist, and the treatments were performed by another experienced physiotherapist in order to provide a single blind structure of the study". However, participants were not blinded. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcome (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Completed flow chart; no dropouts |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Unequal use of co‐intervention | High risk | Multi‐arm trial with KT in combination with other conservative treatment versus conservative treatment |
Shakeri 2013.
| Study characteristics | ||
| Methods | Study design: randomised, double‐blinded, placebo‐controlled study Setting: outpatients Timing: not reported Interventions: standardised therapeutic KT versus standardised placebo KT Sample size: a total of 30 patients with SIS participated in this study. Power analysis was used to determine the sample size for the study. Type I error (α) was set at 0.05 and the power of the test was 0.80. Considering this, the calculated sample size showed that 15 subjects in each group was appropriate to test the hypothesis and have confidence in the results. Analysis: not reported | |
| Participants | Criteria for defining the condition being treated: positivity in two or more shoulder impingement screening items (history of proximal anterior or lateral shoulder pain; painful arc sign during active shoulder elevation; tenderness to rotator cuff tendon palpation; pain with resisted isometric shoulder abduction; positive Jobe’s test), and positivity in at least one of the specific subacromial impingement tests (Neer sign, the Hawkins sign, the Yocum test)
Restriction on duration of symptoms: continued for more than one week during the last six months prior to study
Exclusion criteria: history of dislocation, fracture, or traumatic injuries within the shoulder complex; history of shoulder surgery within the last six months; reproduction of symptoms during the cervical screening examination; failure to complete testing sessions; complete rupture of rotator cuff muscles with acute inflammation
Baseline characteristics:
Intervention: Kinesio Taping (KT)
Number randomised: 15
Number included in analyses: 15
Age: 46.53 ± 13.31 years
Diagnosis: shoulder impingement syndrome
Duration of symptoms: 7.63 ± 7.43 months
Mean (SD) pain (VAS 0‐10): 5.86 (1.8) Mean (SD) function (DASH): 40.95 (16.05) Control: Sham Taping (ST) Number randomised: 15 Number included in analyses: 15 Age: 46.6 ± 14.24 years Diagnosis: shoulder impingement syndrome Duration of symptoms: 9.33 ± 10.48 months Mean (SD) pain (VAS 0‐10): 5.53 (1.55) Mean (SD) function (DASH): 37.18 (13.37) Pretreatment group differences: Not reported |
|
| Interventions | Intervention: KT
Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus, glenohumeral articulation, lower trapezius; number of applications: 2; single application duration: 2‐3 dd; provider: clinician
Control: ST
The patients in the control group received a standardised, placebo KT. No co‐intervention used |
|
| Outcomes | All the measures were obtained at baseline, immediately after taping, after 3 days of wearing the tape (on the fourth day), and finally at one week after wearing the KT:
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: not reported Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Block randomisation was used to keep the numbers in each group very close". |
| Allocation concealment (selection bias) | Unclear risk | "Block randomisation was used to keep the numbers in each group very close". |
| Blinding of participants (performance bias) | Low risk | "The participants were unaware whether they were in the experimental or control group of the study". Double‐blinded, Placebo‐controlled design |
| Blinding of personnel (performance bias) | High risk | "Two investigators were involved in this study. One performed the taping in both groups, and the second, who was unaware of the group assignment, performed the measurements before and after KT". Double‐blinded, placebo‐controlled design |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Low risk | "Two investigators were involved in this study. One performed the taping in both groups, and the second, who was unaware of the group assignment, performed the measurements before and after KT". Double‐blinded, placebo‐controlled design. In addition, "the participants were unaware whether they were in the experimental or control group of the study". |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No missing outcome data |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | No co‐interventions |
Sikha 2017.
| Study characteristics | ||
| Methods | Study design: study sampled with random allocation Setting: NIOH, Kolkata Timing: not reported Interventions: only conventional therapy (n = 15) verus both kinesio taping and conventional therapy (n = 15) Sample size: not reported Analysis: not reported | |
| Participants | Inclusion criteria: subjects having a history of proximal anterior/lateral shoulder pain; pain beginning prior to 150 degrees of active shoulder elevation in any plane and if two or more of the specific impingement tests were found positive (Empty can test or Jobe test, Hawkins‐kennedy test, Neer’s sign); subjects with complaint of having difficulty in performing the activities of daily living Exclusion criteria: shoulder girdle fracture, glenohumeral dislocation/subluxation, cervical spine symptoms verified by Spurling’s test, history of shoulder surgery in the past 12 weeks. osteoarthritis of glenohumeral joint and clinically verified rheumatoid arthritis Restriction on duration of symptoms: not reported Baseline characteristics: Intervention: Kinesio Taping (KT) + conventional therapy Number randomised: 15 Number included in analyses: 15 Age: 44.33 (7.22) years Sex: M 9; F 6 Diagnosis: subacromial impingement syndrome Mean (SD) pain not measured Mean (SD) function (Penn Shoulder score): 32.24 (2.51) Control: only conventional therapy Number randomised: 15 Number included in analyses: 15 Age: 43.40 (7.55) years Sex: M 9; F 6 Diagnosis: subacromial impingement syndrome Mean (SD) pain not measured Mean (SD) function (Penn Shoulder score): 32.64 (4.45) Pretreatment group differences: description of both groups which were homogenous |
|
| Interventions | Intervention: kinesio taping and conventional therapy. Dosage of intervention 5 days in a week for 4 weeks (that included 15 minutes in application of KT followed by 30 minutes rest; subsequently 40 minutes engagement in activity). Tape: Kase (size not specified); taping method: Kase protocol; target: deltoid, supraspinatus, glenohumeral articulation; number of applications: not reported; duration: not reported; provider: not reported Co‐intervention: conventional exercise protocol/standard exercise protocol, adapted from the exercise given by American Association of Orthopaedic Surgeon (AAOS). Intervention of 40 min, 5 days in a week for 4 weeks in conjunction with occupational therapy remedial activities: Shoulder wheel, Finger ladder, Wall mounted overhead sanding unit, Rope and pulley, Arm ergometer Control: conventional exercise protocol/standard exercise protocol, adapted from the exercise given by American Association of Orthopaedic Surgeon (AAOS). Intervention of 40 min, 5 days in a week for 4 weeks in conjunction with occupational therapy remedial activities: Shoulder wheel, Finger ladder, Wall mounted overhead sanding unit, Rope and pulley, Arm ergometer |
|
| Outcomes | Active range of motion ‐ free of pain: flexion abduction and external rotation Function: Penn Shoulder Score (including pain, satisfaction and function) Quality of life: Health‐related quality of life: SF‐12 Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: not reported Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The participants in this study were [a] sample of convenience with random allocation comprised of total 30 subjects in two groups". Insufficient information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "The participants in this study were [a] sample of convenience with random allocation comprised of total 30 subjects in two groups". Insufficient information for judgement |
| Blinding of participants (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of personnel (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | "The subjects (between age of 18 to 65 years) included in this study were referred from main assessment clinic of NIOH, Kolkata". Insufficient information for judgement |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Unclear risk | "The subjects (between age of 18 to 65 years) included in this study were referred from main assessment clinic of NIOH, Kolkata". Insufficient information for judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | "There was no drop out during the study". No information for intention‐to‐treat analysis |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | KT with other conservative treatment versus the same conservative treatment |
Simsek 2013.
| Study characteristics | ||
| Methods | Study design: a randomised, double‐blind, controlled clinical trial Setting: not reported Timing: not reported Interventions: therapeutic kinesio taping and exercise therapy versus sham kinesio taping and exercise therapy Sample size: thirty‐eight (25 female, 13 male) patients with SIS were randomly divided into therapeutic KT (n = 19) and sham KT (n = 19) groups. A minimum of 17 patients per group was necessary for 80% statistical power. Analysis: intention‐to‐treat analysis executed | |
| Participants | Criteria for defining the condition being treated: pain interfering with the patient’s daily routine and positivity at Neer and Hawkin’s impingement tests
Restriction on duration of symptoms: pain lasting for one month or longer
Inclusion criteria: patients between the ages of 18 and 70
Exclusion criteria: calcific tendinitis and degenerative arthritis in plain roentgenograms, pathological findings in addition to subacromial effusion in MR images, a history of shoulder, waist and chest surgery, fracture or dislocation of the affected shoulder, cervical problems accompanied by radicular symptoms, inflammatory joint disease, and physiotherapy for the shoulder within last three months Baseline characteristics: Overall cohort of participants: Number of participants at enrolment: 38 Number randomised: 38 Number included in analyses: 38 Age: 51 years, range: 18 to 69 years Sex: M 13; F 25 Diagnosis: subacromial impingement syndrome Intervention: Kinesio Taping (KT) Number randomised: 19 Number included in analyses: 19 Age: 48 years Sex: M 8; F 11 Dominant shoulder affected: 52% Duration of symptoms: 10.37 ± 8.26 months Mean (SD) pain (VAS 0‐10): 2.74 (2.73) Mean (SD) function (DASH): 46.15 (19.83) Control: Sham Taping (ST) Number randomised: 19 Number included in analyses: 19 Age: 53 years Sex: M 5; F 14 Dominant shoulder affected: 63% Duration of symptoms: 10.37 ± 6.65 months Mean (SD) pain (VAS 0‐10): 3.21 (2.92) Mean (SD) function (DASH): 52.69 (16.42) Pretreatment group differences: shoulder flexion strength, active ROM in flexion, painless ROM during internal rotation |
|
| Interventions | Interventions:
Tape: kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus; number of applications: 4; single application duration: 3 dd; provider: certified physiotherapist. Co‐intervention: patients were given exercises defined by Hughston and Riivald. All exercises were begun with 5 repeats and increased to 15 repeats, as tolerated. Training was performed once a day, for 5 days a week under supervision of a physiotherapist and lasted two weeks. Patients were asked to repeat the exercises as one set during weekdays and two sets on weekends at home. Control: sham kinesio tape Co‐intervention: patients were given exercises defined by Hughston and Riivald. All exercises were begun with 5 repeats and increased to 15 repeats, as tolerated. Training was performed once a day, for 5 days a week under supervision of a physiotherapist and lasted two weeks. Patients were asked to repeat the exercises as one set during weekdays and two sets on weekends at home. |
|
| Outcomes | All assessments were performed before the treatment and on the 5th and 12th days:
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: Scientific Research Project Fund of Cumhuriyet University Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Thirty‐eight (25 female, 13 male) patients with SIS were randomly divided into therapeutic KT (n = 19) and sham KT (n = 19) groups". No information for judgement |
| Allocation concealment (selection bias) | Unclear risk | "Thirty‐eight (25 female, 13 male) patients with SIS were randomly divided into therapeutic KT (n = 19) and sham KT (n = 19) groups". No information for judgement |
| Blinding of participants (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of personnel (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | "Assessments were performed before the treatment and on the 5th and 12th days by a researcher blinded to the information about the patient and the group". However, no information for blinding of participants was present. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. ROM and muscle strength). "Assessments were performed before the treatment and on the 5th and 12th days by a researcher blinded to the information about the patient and the group". |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | It was not clear whether participants were lost to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | No protocol published |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus sham taping with the same co‐intervention |
Subasi 2016.
| Study characteristics | ||
| Methods | Study design: single‐centre RCT Setting: outpatients who reported to the Physical Medicine & Rehabilitation Department of Antalya Training and Research Hospital Timing: not reported Interventions: kinesiological taping versus subacromial injection therapy Sample size: 70 patients were recruited for the study. Analysis: intention‐to‐treat analysis planned and executed; or ITT planned, but per‐protocol executed; not reported | |
| Participants | Criteria for defining the condition being treated: the patients with one or more positive results for specific tests such as Neer’s, Hawkins, painful arc, supraspinatus and 0° abduction, or supraspinatus lesion revealed by radiological imaging were diagnosed as SIS.
Restriction on duration of symptoms: shoulder pain which had been ongoing for over a month
Exclusion criteria: other disorders causing shoulder pain
Baseline characteristics:
Intervention: Kinesio Taping (KT)
Number randomised: 35
Number included in analyses: 35
Age: 53.46 ± 10.7 years
Sex: M 15; F 20
Diagnosis: subacromial impingement syndrome
Duration of symptoms: 2.9 ± 1.5 months
Mean (SD) pain (VAS 0‐10): 6.60 (1.6) Mean (SD) function (SPADI): 76.9 (18.9) Control: Subacromial injection Number randomised: 35 Number included in analyses: 35 Age: 54.29 ± 10.4 years Sex: M 8; F 27 Diagnosis: subacromial impingement syndrome Duration of symptoms: 2.7 ± 1.3 months Mean (SD) pain (VAS 0‐10): 6.8 (1.5) Mean (SD) function (SPADI): 74.8 (19.9) Pretreatment group differences: in the baseline assessment, no significant differences were detected between the groups. |
|
| Interventions | Intervention: KT
Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus, glenohumeral articulation; number of applications: 3; single application duration: 5 dd; provider: the same physiotherapist. Co‐intervention: Home Exercise Program: A 3‐month exercise program was prescribed for both groups including stretching and strength exercises. Stretching exercises were prescribed for 7 days per week over 3 months. The exercises were performed as a home‐based program and described by the same physiotherapist. All patients were given an illustrated leaflet containing descriptions of the recommended exercises. Control: subacromial injection Betamethasone (sodium phosphate and acetate) (1 cc) plus prilocaine (4 cc) was injected into the subacromial space in the group 1 patients, by the same physiatrist. The posterior approach was preferred and was performed at 1 cm medial and inferior to the posterior corner of the acromion. Co‐intervention: Home Exercise Program, a 3‐month exercise program was prescribed for both groups including stretching and strength exercises. Stretching exercises were prescribed for 7 days per week over 3 months. The exercises were performed as a home‐based program and described by the same physiotherapist. All patients were given an illustrated leaflet containing descriptions of the recommended exercises. |
|
| Outcomes | All patients were assessed at baseline and at 1 and 3 months post‐intervention
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: none Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The patients were randomly assigned into two groups using the numbered envelopes method". |
| Allocation concealment (selection bias) | Unclear risk | "The patients were randomly assigned into two groups using the numbered envelopes method". |
| Blinding of participants (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of personnel (performance bias) | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Unclear risk | Poor reporting prevented any judgement. |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | No flow chart was reported and no information for judgement |
| Selective reporting (reporting bias) | High risk | No protocol was published; passive ROM was planned but not reported in the Results section. |
| Unequal use of co‐intervention | Low risk | KT with co‐intervention versus conservative treatment with the same co‐intervention |
Thelen 2008.
| Study characteristics | ||
| Methods | Study design: prospective, randomised, double‐blinded, clinical trial using a repeated‐measures design Setting: the Cadet Physical Therapy Clinic at the United States Military Academy or Keller Army Community Hospital at West Point, NY Timing: September 2006 to September 2007 Interventions: 2 groups: therapeutic KT group or sham KT group Sample size: forty‐two subjects clinically diagnosed with rotator cuff tendonitis/impingement were recruited. A priori power analysis demonstrated the need for at least 26 subjects per group, given a standard deviation of 25 mm (VAS), a difference in pain intensity between groups of 20 mm on the VAS, an alpha level of.05, and with power set at 80%. Analysis: to account for the missing data, the authors performed an intention‐to‐treat analysis utilising the last‐observation‐carried‐forward (LOCF) model. This technique involves using the last recorded value for each outcome measure and applying it to the remaining missing value(s). | |
| Participants | Criteria for defining the condition being treated: pain onset prior to 150° of active shoulder elevation in any plane, positive Empty can test indicating possible supraspinatus involvement, positive Hawkins‐Kennedy test indicating possible external impingement, subjective complaint of difficulty performing activities of daily living
Restriction on duration of symptoms: shoulder pain not longer than 6 months
Inclusion criteria: being 18 to 50 years of age
Exclusion criteria: shoulder girdle fracture, glenohumeral dislocation/subluxation, acromioclavicular sprain, concomitant cervical spine symptoms, a history of shoulder surgery within the previous 12 weeks
Baseline characteristics:
Intervention: Kinesio Tape ‐ KT
Number of participants at enrolment: 21
Number randomised: 21
Number included in analyses: 21 (3 lost to follow‐up)
Age: 21.3 ± 1.7 years
Sex: M 19; F 2
Diagnosis: Shoulder pain
Duration of symptoms (d): 19 (5‐35)
Mean (SD) pain (VAS 0‐100): 44.1 (20.1) Mean (SD) function (SPADI): 37.4 (15.2) Comparator: Sham Tape ‐ ST Number of participants at enrolment: 21 Number randomised: 21 Number included in analyses: 21 (4 lost to follow‐up) Age: 19.8 ± 1.5 years Sex: M 17; F 4 Diagnosis: Shoulder pain Duration of symptoms (d): 8 (5‐30) Mean (SD) pain (VAS 0‐100): 43.9 (21.7) Mean (SD) function (SPADI): 34 (13.9) Pretreatment group differences: no meaningful differences existed between groups at baseline. |
|
| Interventions | Intervention: Kinesio Taping Tape: Kinesio tape 2 in (5 cm); taping method: Kase protocol; target: deltoid, supraspinatus, glenohumeral articulation; number of applications: 2; single application duration: 6 dd; provider: certified clinician Control: Sham Taping In this study, authors used an alternative sham taping application. The sham group sites were selected because they were the most common locations of perceived pain by patients with rotator cuff tendonitis or impingement. | |
| Outcomes |
Outcomes used in this review The following outcomes were considered at the end of treatments:
|
|
| Notes | Funding: none Conflict of interest: none Trial registration: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Subjects were assigned to 1 of 2 groups using a random‐number generator and allocation was concealed". |
| Allocation concealment (selection bias) | Low risk | "Subjects were assigned to 1 of 2 groups using a random‐number generator and allocation was concealed". |
| Blinding of participants (performance bias) | Low risk | "Although the taping applications looked different, they were well concealed under short‐sleeve clothing. Therefore, we do not believe that blinding of the subjects was compromised". |
| Blinding of personnel (performance bias) | High risk | "Prospective, randomised, double‐blinded, clinical trial" |
| Blinding of outcome assessment (detection bias) self‐reported outcomes | Low risk | "To avoid bias, the second author, who was blinded to the group assignment, measured outcomes". In addition, "although the taping applications looked different, they were well concealed under short‐sleeve clothing. Therefore, we do not believe that blinding of the subjects was compromised". |
| Blinding of outcome assessment (detection bias) assessor‐reported outcomes | Low risk | Appropriate measurements for assessor‐reported outcomes (i.e. active ROM) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No high percentage and unbalanced loss to follow‐up |
| Selective reporting (reporting bias) | Unclear risk | No published protocol |
| Unequal use of co‐intervention | Low risk | No co‐interventions |
AAOS:American Academy of Orthopaedic Surgeons (AAOS) ACJ:Acromioclavicular Joint (ACJ) ADL:Activities of daily living ANOVA:Analysis of variance ASES‐100:American Shoulder and Elbow Surgeons (ASES) Shoulder Score BMI:Body Mass Index BPI:Brief Pain Inventory C‐M: Constant–Murley scale
cm: centimeter
CTT: control Tension Taping DASH:Disability of the Arm, Shoulder and Hand dd:days EMG: Electromyography ESWT:Extracorporeal Shock Wave Therapy EX:exercise FLEX‐SF:Self‐reported flexi‐level scale of shoulder function GH:Glenohumeral joint HEP:Home Exercise Program HILT:High‐intensity laser therapy KT: Kinesio Taping IQR: Interquartile range ITT:increasing Tension Taping
ITT: Intention‐to‐treat analysis
LOCF: Last‐observation‐carried‐forward MCID:Minimal clinically important difference MMSE:Mini‐Mental State Examinafion MRC:Medical Research Council scale MRI:Magnetic resonance imaging MT:Manual Therapy NA:Not available NR:Not reported NEER:Neer's Test NHP:Nottingham Health Profile NPRS:Numeric pain rating scales NSAID:Nonsteroidal anti‐inflammatory drug OSS:Oxford Shoulder Score PAM: Passive accessory movements PCT:Precut kinesiology tape PENN:PENN Shoulder Score PT:Physical therapy RC:Rotator cuff RCT:Randomized controlled trial RoCT:rotator cuff tendinopathy ROM:Range of Motion RSP:Round shoulder position SAI:: subacromial impingement SAIS:subacromial impingement syndrome SD:Standard Deviation SET:Supervised exercise therapy SF‐12:12‐item Short Form Survey SIS:Shoulder Impingement Syndrome SPADI:Shoulder Pain Disability Index SSRQ:Subjective Shoulder Rating Questionnaire SST:Simple Shoulder Test ST:Sham Taping T(0)(1)(2)(3):Time point TB‐KT:TheraBand Kinesiology Tape TENS:transcutaneous electrical nerve stimulation TTDPM:Threshold to detect passive motion US:Ultrasound VAS:Visual Analogue Scale WBS:Wong‐Baker Face Rating Scale WORC:Western Ontario Rotator Cuff inde
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aguilera Eguía 2014 | Wrong study design |
| Akbaba 2017 | Wrong intervention |
| Apeldoorn 2017 | Wrong intervention |
| Desjardins‐Charbonneau 2015 | Wrong study design |
| Djordjevic 2012 | Outcome of interest was not measured. |
| Dong 2015 | Wrong study design |
| Elliot 2003 | Wrong study design |
| Fong 2019 | Outcome of interest was not measured. |
| Kalter 2011 | Wrong intervention |
| Karakaş 2015 | Wrong population |
| Kim 2014 | Wrong study design |
| Lambers Heerspink 2015 | Wrong population |
| Leong 2017 | Outcome of interest was not measured. |
| Leong 2019 | Outcome of interest was not measured. |
| Ozer 2017 | Wrong population |
| Parreira 2014 | Wrong study design |
| Pekyavas 2014 | Wrong study design |
| Polimeni 2003 | Wrong intervention |
| Reynard 2018 | Wrong population |
| Shih 2018 | Wrong intervention |
| Teys 2013 | Wrong intervention |
Characteristics of studies awaiting classification [ordered by study ID]
Saorín‐Morote 2016.
| Methods | Study design: double‐blind randomised controlled trial |
| Participants | Sixty patients (56.7% women; mean = 50.1 years; SD = 15.28), diagnosed with painful shoulder syndrome |
| Interventions | Intervention: Manual therapy with thoracic analytic mobilisation, kinesio taping® (group 2: n = 30), and a home exercise program Control: Manual therapy with thoracic analytic mobilisation, McConnell Taping (group 1: n = 30) or kinesio taping® (group 2: n = 30), and a home exercise program Rehabilitation program duration: The treatment lasted until the symptoms disappeared or stabilizaton of symptoms, with a mean of 4.2 sessions (SD = 2.22). |
| Outcomes | Outcomes were assessed after the first session, at the end of treatment, and three months later. Outcomes: ‐ Pain assessed by Visual Analogue Scale (VAS) |
| Notes | Available only as a conference abstract |
Yildiz 2017.
| Methods | Study design: randomised controlled trial |
| Participants | 54 patients with impingement syndrome aged 18 to 65 years |
| Interventions | Intervention: shoulder kinesio taping application in addition to TENS, hot pack and ultrasound Control: transcutaneous electrical nerve stimulation (TENS), hot pack and ultrasound Rehabilitation program: ten sessions |
| Outcomes | Outcomes were assessed before and after treatment. Outcomes: ‐ Pain: Visual analog scale (night pain, rest pain, pain with motion and general pain) ‐ Shoulder ROM (goniometer measurements) ‐ Function: Shoulder Disability Questionnaire and Disabilities of the Arm Shoulder and Hand |
| Notes | Available only as a conference abstract |
ROM: Range of motion TENS: TransCutaneous Electrical Nerve Stimulation VAS: Visual Analogue Scale
Characteristics of ongoing studies [ordered by study ID]
ACTRN12611000359932.
| Study name | In patients with impingement shoulder syndrome, is the Mulligan method and kinesio taping effective in improving shoulder range of motion? |
| Methods | Target sample size: 20 Recruitment status: Completed Study type: Interventional Study design: Purpose: Treatment Allocation: Randomised controlled trial Masking: Blinded (masking used) |
| Participants | Impingement shoulder syndrome |
| Interventions | Intervention: Mulligan method (or Mobilisation With Movement treatment or MWM treatment, which are all terms for the same procedure) and kinesio taping were done on the same group (intervention group); Control intervention: exercises that are usual or standard program for impingement shoulder syndrome. Specific exercises are as follows: pendular exercises, active pain‐limited shoulder exercises of shoulder elevation, depression, flexion, abduction, rotations; static strenghtening exercises for rotator cuff and scapular stabilizers' muscles; 10 repetitions in one set daily per type of exercise, 30 sec rest between sets;10 sessions with 24 hours between sets. |
| Outcomes | 1. pain‐free active shoulder abduction was assessed using universal goniometer and expressed in degrees [before treatment, on the 5th day and on the 10th day of the treatment]. 2. pain‐free active shoulder flexion was assessed using universal goniometer and expressed in degrees [before treatment, on the 5th day and on the 10th day of the treatment]. |
| Starting date | 07/04/2011 |
| Contact information | Address: Bulevar Zorana Djindjica 115, 11000 Belgrade Serbia and Montenegro Telephone: +381658542279 Email: odordev@EUnet.rs |
| Notes | https://anzctr.org.au/ACTRN12611000359932.aspx |
CTRI/2013/07/003847.
| Study name | To compare the effectiveness of rigid tape and kinesio tape in reducing pain and improving shoulder function in patient diagnosed with rotator cuff injury |
| Methods | Target sample size: 40 Recruitment status: Not yet recruiting Study type: Interventional Study design: Randomized, parallel‐group, multiple arm trial Method of generating randomisation sequence: permuted block randomisation Fixed method of allocation concealment: sequentially numbered, sealed, opaque envelopes Blinding and masking: participants blinded Phase: Phase 3 |
| Participants | Patients who are diagnosed to have rotator cuff injury |
| Interventions | Intervention: kinesio tape for 1 week Control Intervention: rigid tape for 1 week |
| Outcomes | 1. Disabilities of the Arm, Shoulder and Hand 2. Pain ‐ Visual Analogue Scale Time point: baseline data before intervention and follow‐up data after one week |
| Starting date | 29‐07‐2013 |
| Contact information | Name: Nirav Bhavsar Designation: Lecturer Affiliation: Fr Muller Medical College Address: Dept of Physiotherapy, Father Muller Charitable Institutions, Father Muller Road, Kankanady, Mangalore, Karnataka, India Dakshina Kannada, Karnataka, 575 002, India Phone: 7259712493 Email: pt_nirav@yahoo.co.in |
| Notes | http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=6694 |
CTRI/2018/09/015780.
| Study name | Efficacy of kinesio taping on shoulder proprioception in patients with subacromial impingement syndrome |
| Methods | Target sample size: 34 Recruitment status: Completed Study type: Interventional Study design: Randomised, parallel‐group, placebo‐controlled trial Method of generating randomisation sequence: Computer‐generated randomisation Method of allocation concealment: an open list of random numbers Blinding and masking: investigator blinded Phase: Phase 1 |
| Participants | Shoulder pain with positive Hawkins Kennedy test, Neers impingement classification of 2 and 3 |
| Interventions | Intervention: kinesio taping Control intervention: sham taping |
| Outcomes | 1. Shoulder proprioception 2. Strength 3. DASH questionnaire time point: Before and after the intervention |
| Starting date | 15‐10‐2018 |
| Contact information | Name: Apoorva Laxmi Address: Ramaiah Medical College and Hospitals, Department of Physiotherapy, Matikere, MSRIT post, MS Ramai Nagar, Bengaluru, Karnataka ‐ 560054, Karnataka, India Telephone: 9008025432 Email: pshobha76@gmail.com Affiliation: Ramaiah Medical College |
| Notes | http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=27270 |
CTRI/2020/05/024970.
| Study name | Effect Of therapeutic kinesio‐taping In patients with shoulder impingement syndrome: a randomized controlled trial |
| Methods | Target sample size: 20 Recruitment status: Not yet recruiting Study type: Interventional Study design: Randomised, parallel‐group, placebo‐controlled trial Method of generating randomisation sequence: Computer‐generated randomisation Method of allocation concealment: sequentially numbered, sealed, opaque envelopes Blinding and masking: participants blinded |
| Participants | Patients who had been medically diagnosed with shoulder impingement syndrome or following clinical criteria of impingement in unilateral shoulder. Clinical criteria include ‐ onset of pain prior to 150‐degree of shoulder elevation (flexion & abduction) and painful medial rotation, positive empty can test that defines involvement of supraspinatus muscle and positive Hawkins‐Kennedy test/Neerâs sign indicating impingement syndrome |
| Interventions | Intervention: Kinesio taping along with ultrasound therapy: kinesio taping for supraspinatus, deltoid muscle and joint correction technique for 3 days along with ultrasound therapy for 8 minutes with intensity 1.5 w/cm2 Control Intervention: Placebo kinesio taping and ultrasound therapy: placebo kinesio taping with no tension 1 over the acromioclavicular joint and 1 on the distal deltoid for 3 days with ultrasound therapy for 8 minutes with intensity 1.5 w/cm2 |
| Outcomes | 1. Numerical pain rating scale (NPRS) 2. Acromio‐humeral distance using ultrasonography 3. Range of motion using goniometer 4. Shoulder pain and disability index (SPADI) Time point: Baseline, immediately post‐treatment, 3 days after intervention |
| Starting date | 01‐05‐2020 |
| Contact information | Name: Dr Surendra Wani Address: Oppo. Govt. Milk Dairy, M.I.D.C., 414111 Ahmadnagar, MAHARASHTRA India Telephone: 9960473324 Email: wanisuren@gmail.com Affiliation: D.V.V.P.Fs College of Physiotherapy |
| Notes | http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=42577 |
IRCT20180406039203N1.
| Study name | Evaluation and comparison of two therapeutic physiotherapy protocols of high power or low power lasers combined with kinesio taping on shoulder function and musculoskeletal sonography parameters in patients with subacromial impingement syndrome |
| Methods | Target sample size: 37 Recruitment status: completed Study type: interventional Study design: randomisation: randomised Blinding: single‐blinded, placebo used Assignment: parallel‐group Purpose: treatment Other design features: precise assessment of changes before and after treatment with ultrasound Randomisation description: simple and individual randomisation will be done through sealed envelopes Blinding description: individuals participating in the study are blind to what kind of laser they receive or are in the control group |
| Participants | Subacromial impingement syndrome, impingement syndrome of right shoulder Stage I, II in Neer classification The presence of tendonitis and inflammation in the MRI that is being examined by a doctor Painful arch 40‐120 of shoulder abduction Positive Yocum, Neer and Hawkins‐Kennedy tests Weakness or pain in resistance external rotation, internal rotation and abduction |
| Interventions | Intervention: A high power laser with a power of 4 watts for 9 minutes will be used on a subacromial space of 10 centimetres in area, and the total energy received will be 2050 joules per square centimetre. Treatment will be performed three times a week for seven sessions. Control intervention: A low power laser with a power of 200 MW for 16 minutes will be used on a subacromial space of 10 cm2. The total energy received will be 200 joules per square centimetre. |
| Outcomes | 1. Pain 2. Range of motion (ROM) |
| Starting date | 2018‐06‐03 |
| Contact information | Name: Zohre Zaki Address: Jala Ale Ahmad Street, Tarbiat Modares University, 14115‐111, Tehran, Islamic Republic of Iran Telephone: +98 21 8288 0000 Email: zaki_zohre@yahoo.com Affiliation: Tarbiat Modares University |
| Notes | http://en.irct.ir/trial/30534 |
NCT02290730.
| Study name | Effect of kinesio taping on muscle strength in lower trapezius |
| Methods | Target sample size: 49 Recruitment Status: Completed Study Type: Interventional (clinical trial) Actual enrolment: 49 participants Allocation: Randomised Intervention Model: Parallel‐group assignment Masking: Single (outcomes assessor) |
| Participants | Shoulder problems |
| Interventions | Intervention: kinesio tape on lower trapezius Control intervention: no intervention |
| Outcomes | 1. Maximal isometric muscle strength monitored by a hand‐held dynamometer 2. Time of break force 3. Self‐reported strength 4. Effort scale |
| Starting date | 14‐11‐2014 |
| Contact information | Grethe Myklebust, Phd, PT, Norwegian School of Sport Sciences |
| Notes | https://clinicaltrials.gov/ct2/history/NCT02290730 |
NCT04242381.
| Study name | Short term effect of kinesiotaping in patients with shoulder impingement syndrome |
| Methods | Target sample size: 75 Recruitment status: Completed Study type: Interventional (clinical trial) Actual Enrolment: 75 participants Allocation: Randomised Intervention model: Parallel‐group assignment Intervention Model Description: Randomised sham‐controlled study Masking: Single (investigator) Masking Description: All participants were assessed by the same clinician (FB) at baseline and at two weeks after completing the interventions by a visual analog scale (VAS), range of motion (ROM) and Disabilities of the Arm, Shoulder and Hand Questionnaire (DASH). KT and sham KT applications were made by the same clinician (NM). For ultrasonographic (US) measurements, the participants were sent to a clinician (DGK) who was blinded to the group allocation. |
| Participants | Patients with shoulder impingement with at least three positive results in the Hawkins‐Kennedy, Neer, empty can, drop‐arm, and lift‐off tests |
| Interventions | Intervention 1: kinesio taping (KT) Intervention 2: exercise (EX) Control intervention: sham kinesiotaping (sham KT) |
| Outcomes | 1. Pain level 2. Functional status 3. Joint range of motion measurements 4. Ultrasonography Time frame: 4 weeks |
| Starting date | 1‐01‐2016 |
| Contact information | Fatih Bagcier, Principal Investigator, Kars State Hospital |
| Notes | https://clinicaltrials.gov/ct2/show/NCT04242381 |
RBR‐65qh7j.
| Study name | Kinesio tape in the injuries of the rotating sleeve: clinical test randomizado double blind |
| Methods | Target sample size: 60 Recruitment status: recruiting Study type: Intervention Study design: Clinical trial of a randomised, parallel‐group, double‐blind, 3‐arm treatment |
| Participants | Rotator cuff lesion grades I and II in the Neer classification; both sexes; age from 18 to 70 years; have signed the informed consent form; subacromial pain for at least three months; two of the three positive impact tests (Jobe, Hawkins and Neer) |
| Interventions | Intervention: exercise group with 20 subjects. There will be a program of 7 eccentric exercises for the symptomatic shoulder. The group will perform the exercises three times a week for 45 minutes each session for four weeks, totaling 12 sessions. Control intervention: kinesio tape with 20 subjects, and 3 bandages applied on the symptomatic shoulder in each subject |
| Outcomes | 1. Active and passive movements of flexion, abduction, extension, internal and external rotation 2. Assessment of muscle strength 3. Functional evaluation and quality of life: functional and quality of life questionnaires from the modified UCLA, Constant‐Murley scale and the Shoulder Pain and Disability Index (SPADI) 4. Pain: Analog visual pain scale |
| Starting date | 11/06/2019 |
| Contact information | Name: Rodrigo Boff Daitx Address: Rua Universitária, 1900 95560‐000, Torres, Brazil Telephone: +55‐51‐992123616 Email: rodrigo.roseta@hotmail.com |
| Notes | http://www.ensaiosclinicos.gov.br/rg/RBR‐65qh7j/ |
DASH: Disability of the Arm, Shoulder and Hand
EX: Exercise
KT: Kinesio taping
MRI: Magnetic resonance Imaging
MW: Megawatt
NPRS: Numeric pain rating scales
ROM: Range of motion
SPADI: Shoulder Pain Disability Index
UCLA: University of California at Los Angeles
US: Ultrasound
VAS: Visual Analogue Scale
Differences between protocol and review
The outcome measures section stated that outcomes were not considered as part of the eligibility criteria, however, some studies have been excluded because the ‘outcome of interest' was not measured.
Analyses were perfomed with random effetcs model since we assumed a general heterogeneity among combined studies related to kinesio taping application, delivery modalities and presence of co‐interventions, moreover in the presence of small heterogeneity random and fixed effects model give similar results (Nikolakopoulou 2014).
We pooled studies even when heterogeneity was > 75% since we downgraded the quality of the evidence in the presence of substantial heterogeneity.
We assessed clinical relevance in the interpretation of the effects, as required by the GRADE approach.
Contributions of authors
SG conceived and coordinated the project, wrote the manuscript, carried out the search, conducted screenings, extracted data and completed the risk of bias assessment;
VI and EF extracted data and complete the tables including the Tidier Checklist;
AA wrote the protocol, resolved doubts of disagreement in data extraction and risk of bias assessment and provided input for writing the discussion;
LL revised the manuscript and provided input for writing the discussion;
LM and MGV conceived the project and provided statistical advice and input for writing the discussion;
GC wrote the manuscript and carried out the search, conducted screenings, extracted data, completed the risk of bias assessment, and is the guarantor of the review;
All authors approved the manuscript.
Sources of support
Internal sources
-
IRCCS Galeazzi Orthopaedic Institute, Unit of Clinical Epidemiology, Milan, Italy
Ricerca Corrente ‐ Italian Ministry of Health
External sources
No sources of support provided
Declarations of interest
Andreano Anita: none known
Castellini Greta: none known
Gianola Silvia: none known
Fascio Edoardo: none known
Iannicelli Valerio: none known
Moja Lorenzo: none known
Linda C Li: none known
Valsecchi Maria Grazia: none known
New
References
References to studies included in this review
De Oliveira 2021 {published and unpublished data}
- Oliveira FCL, Fontenay BP, Bouyer LJ, Desmeules F, Roy JS. Effects of kinesiotaping added to a rehabilitation programme for patients with rotator cuff tendinopathy: protocol for a single-blind, randomised controlled trial addressing symptoms, functional limitations and underlying deficits. BMJ Open 2017;7(9):e017951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveira FCL, Pairot de Fontenay B, Bouyer LJ, Desmeules F, Roy JS. Effects of kinesiotaping on symptoms, functional limitations and underlying deficits of individuals with Rotator cuff tendinopathy: a single-blind, randomized controlled trial. Clinical Journal of Sport Medicine 2018;28(3):e45. [Google Scholar]
- Oliveira FCL, Pairot de Fontenay B, Bouyer LJ, Desmeules F, Roy JS. Kinesiotaping for the rehabilitation of rotator cuff-related shoulder pain: a randomized clinical trial. Sports Health 2021;13(2):161-72. [DOI: 10.1177/1941738120944254] [DOI] [PMC free article] [PubMed] [Google Scholar]
Devereaux 2016 {published data only}
- Devereaux M, Velanoski KQ, Pennings A, Elmaraghy A. Short-term effectiveness of precut kinesiology tape versus an NSAID as adjuvant treatment to exercise for subacromial impingement: a randomized controlled trial. Clinical Journal of Sport Medicine 2016;26(1):24-32. [DOI] [PubMed] [Google Scholar]
Frassanito 2018 {published data only}
- Frassanito P, Cavalieri C, Maestri R, Felicetti G. Effectiveness of extracorporeal shock wave therapy and kinesio taping in calcific tendinopathy of the shoulder: a randomized controlled trial. European Journal of Physical and Rehabilitation Medicine 2018;54(3):333-40. [DOI] [PubMed] [Google Scholar]
Gandhi 2016 {published data only}
- Gandhi VM AB, Kumar RKP. Effectiveness of Myofascial Release Therapy with Shoulder Taping on Subacromial Impingement Syndrome in Collegiate Basket Ball Players - A Quasi experimental Pilot study. Bangladesh Journal of Medical Science 2016;15(3):347-51. [Google Scholar]
Gençbay 2019 {published data only}
- Gençbay MB, Işıksaçan N, Koşer M, Kasapoğlu P, Akbaş O, Pekediş K. The effectiveness of extracorporeal shock wave and kinesio tape treatments in shoulder impingement syndrome. Nobel Medicus 2019;15(1):56-62. [Google Scholar]
Goksu 2016 {published data only}
- Goksu H, Tuncay F, Borman P. The comparative efficacy of kinesio taping and local injection therapy in patients with subacromial impingement syndrome. Acta Orthopaedica et Traumatologica Turcica 2016;50(5):483-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hsu 2009 {published data only}
- Hsu YH, Chen WY, Lin HC, Wang WT, Shih YF. The effects of taping on scapular kinematics and muscle performance in baseball players with shoulder impingement syndrome. Journal of Electromyography and Kinesiology 2009;19(6):1092-9. [DOI] [PubMed] [Google Scholar]
Jena Etnoyer‐Slaski 2016 {published and unpublished data}
- Etnoyer-Slaski J. Tension of THERABAND® kinesiology tape on shoulder pain (ShoulderTBKT). https://clinicaltrials.gov/ct2/show/NCT02686437 First posted: February 19, 2016. [CLINICALTRIAL.GOV: NCT02686437]
Kang 2020 {published data only}
- Kang FJ, Chiu YC, Wu SC, Wang TG, Yang JL, Lin JJ. Kinesiology taping with exercise does not provide additional improvement in round shoulder subjects with impingement syndrome: a single-blinded randomized controlled trial. Physical Therapy in Sport. 2019;40:99-106. [DOI] [PubMed] [Google Scholar]
Kaya 2011 {published data only}
- Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clinical Rheumatology 2011;30(2):201-7. [DOI] [PubMed] [Google Scholar]
Kaya 2014 {published data only}
- Kaya DO, Baltaci G, Toprak U, Atay AO. The clinical and sonographic effects of kinesiotaping and exercise in comparison with manual therapy and exercise for patients with subacromial impingement syndrome: a preliminary trial. Journal of Manipulative and Physiological Therapeutics 2014;37(6):422-32. [DOI] [PubMed] [Google Scholar]
Keenan 2017 {published data only}
- Keenan KA, Akins JS, Varnell M, Abt J, Lovalekar M, Lephart S, et al. Kinesiology taping does not alter shoulder strength, shoulder proprioception, or scapular kinematics in healthy, physically active subjects and subjects with subacromial impingement syndrome. Physical Therapy in Sport 2017;24:60-6. [DOI] [PubMed] [Google Scholar]
Kocyigit 2016 {published data only}
- Kocyigit F, Acar M, Turkmen MB, Kose T, Guldane N, Kuyucu E. Kinesio taping or just taping in shoulder subacromial impingement syndrome? A randomized, double-blind, placebo-controlled trial.. Physiotherapy Theory and Practice 2016;32(7):501-8. [DOI] [PubMed] [Google Scholar]
Kul 2018 {published data only}
- Kul A, Ugur M. Comparison of the efficacy of conventional physical therapy modalities and kinesio taping treatments in shoulder impingement syndrome. Eurasian Journal of Medicine 2018;51(2):139-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
Miccinilli 2018 {published data only}
- Miccinilli S, Bravi M, Morrone M, Santacaterina F, Stellato L, Bressi F, et al. A triple application of kinesio taping supports rehabilitation program for rotator cuff tendinopathy: a randomized controlled trial. Journal of Orthopedics, Traumatology and Rehabilitation 2018;20(6):499-505. [PubMed] [Google Scholar]
Miller 2009 {published data only}
- Miller P, Osmotherly P. Does scapula taping facilitate recovery for shoulder impingement symptoms? A pilot randomized controlled trial. Journal of Manual and Manipulative Therapy 2009;17(1):E6-E13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohamed 2019 {published data only}
- Mohamed SHP, Alatawi SF. Comparison of kinesio taping and manual therapy with supervised exercise therapy for the treatment of shoulder impingement syndrome.. International Journal of Physiotherapy 2019;6(5):177-85. [Google Scholar]
Pekyavas 2016 {published data only}
- Pekyavas NO, Baltaci G. Short-term effects of high-intensity laser therapy, manual therapy, and kinesio taping in patients with subacromial impingement syndrome. Lasers in Medical Sciences 2016;31(6):1133-41. [DOI] [PubMed] [Google Scholar]
Shakeri 2013 {published data only}
- Shakeri H, Keshavarz R, Arab AM, Ebrahimi I. Clinical effectiveness of kinesiological taping on pain and pain-free shoulder range of motion in patients with shoulder impingement syndrome: a randomized, double blinded, placebo-controlled trial. International Journal of Sports Physical Therapy 2013;8(6):800-10. [PMC free article] [PubMed] [Google Scholar]
Sikha 2017 {published data only}
- Sikha S, Jeetendra M, Pankaj B. Effect of kinesio taping on motion, pain with functional performance and subsequent quality of life in subject with subacromial impingement syndrome. International Journal of Medical Research and Health Sciences 2017;6:71-8. [Google Scholar]
Simsek 2013 {published data only}
- Simsek HH, Balki S, Keklik SS, Ozturk H, Elden H. Does kinesio taping in addition to exercise therapy improve the outcomes in subacromial impingement syndrome? A randomized, double-blind, controlled clinical trial. Acta Orthopaedica et Traumatologica Turcica 2013;47(2):104-10. [DOI] [PubMed] [Google Scholar]
Subasi 2016 {published data only}
- Subasi V, Cakir T, Arica Z, Sarier RN, Filiz MB, Dogan SK, et al. Comparison of efficacy of kinesiological taping and subacromial injection therapy in subacromial impingement syndrome. Clinical Rheumatology 2016;35(3):741-6. [DOI] [PubMed] [Google Scholar]
Thelen 2008 {published data only}
- Thelen MD, Dauber JA, Stoneman PD. The clinical efficacy of kinesio tape for shoulder pain: a randomized, double-blinded, clinical trial. Journal of Orthopaedic & Sports Physical Therapy 2008;38(7):389-95. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Aguilera Eguía 2014 {published data only}
- Aguilera Eguía RA, Zafra Santos EO, Araya Quintanill FA , Gómez Carreño LE , Soto Aliaga JX , Vargas Varga A, et al. Using the taping in the clinical management of patients with sub-acromial impingement: a systematic review [Uso del taping en el manejo clínico de sujetos con pinzamiento sub-acromial: revisión sistemática]. Revista de la Sociedad Española del Dolor Jan/Feb 2014;21(1):39-49. [Google Scholar]
Akbaba 2017 {published data only}
- Akbaba YA, Mutlu EK, Altun S, Gümüşoğlu G, Çelik D. The effects of kinesio tape application with different verbal input given to with patients with rotator cuff tear. Orthopaedic Journal of Sports Medicine 2017;5:suppl2. [Google Scholar]
Apeldoorn 2017 {published data only}
- Apeldoorn AT, Kamper SJ, Kalter J, Knol DL, Tulder MW, Ostelo RW. Rigid shoulder taping with physiotherapy in patients with subacromial pain syndrome: a randomized controlled trial. Journal of Rehabilitation Medicine. 2017;49(4):347-53. [DOI] [PubMed] [Google Scholar]
Desjardins‐Charbonneau 2015 {published data only}
- Desjardins-Charbonneau A, Roy JS, Dionne CE, Desmeules F. The efficacy of taping for rotator cuff tendinopathy: a systematic review and meta-analysis. International Journal of Sports Physical Therapy 2015;10(4):420-33. [PMC free article] [PubMed] [Google Scholar]
Djordjevic 2012 {published data only}
- Djordjevic OC, Vukicevic D, Katunac L, Jovic S. Mobilization with movement and kinesiotaping compared with a supervised exercise program for painful shoulder: results of a clinical trial. Journal of Manipulative and Physiological Therapeutics 2012;35(6):454-63. [DOI] [PubMed] [Google Scholar]
Dong 2015 {published data only}
- Dong W, Goost H, Lin XB, Burger C, Paul C, Wang ZL, et al. Treatments for shoulder impingement syndrome: a PRISMA systematic review and network meta-analysis. Medicine (Baltimore) 2015;10:e510. [DOI] [PMC free article] [PubMed] [Google Scholar]
Elliot 2003 {published data only}
- Elliot D, Harris G, Triffitt PD. A pilot study to determine whether taping improves the outcome of physiotherapy treatment for shoulder impingement. In: Chartered Society of Physiotherapy Annual Congress & Exhibition: Defining Practice, Friday, October 17 to Sunday, October 19 2003, International Convention Centre, Birmingham; 51-51. 2003.
Fong 2019 {published data only}
- Fong SM, Ng LK, Ma WW, Wang HK, Bae YH, Yam TT, et al. Effects of kinesiology taping on shoulder girdle muscle activity and sports performance during badminton forehand overhead strokes in amateur badminton players with shoulder impingement syndrome. Journal of Sports Medicine and Physical Fitness 2019;59(6):994-1000. [DOI] [PubMed] [Google Scholar]
Kalter 2011 {published data only}
- Kalter J, Apeldoorn AT, Ostelo RW, Henschke N, Knol DL, Tulder MW. Taping patients with clinical signs of subacromial impingement syndrome: the design of a randomized controlled trial. BMC Musculoskeletal Disorder 2011;12:188. [DOI] [PMC free article] [PubMed] [Google Scholar]
Karakaş 2015 {published data only}
- Karakaş. Effects of kinesiologic taping or pneumatic compression application on pain and functionality in upper extremity musculoskeletal problems. Fizyoterapi Rehabilitasyon 2015;26(2):S17-S18. [Google Scholar]
Kim 2014 {published data only}
- Kim SY, Kang MH, Kim ER, Oh JS. Kinesio Taping improves shoulder internal rotation and the external/internal rotator strength ratio in patients with rotator cuff tendinitis. Isokinetics and Exercise Science 2014;22(3):259-263. [Google Scholar]
Lambers Heerspink 2015 {published data only}
- Lambers Heerspink FO, Raay JJ, Koorevaar RC, Eerden PJ, Westerbeek RE, 't Riet E, et al. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. Journal of Shoulder and Elbow Surgery 2015;24(8):1274-81. [DOI] [PubMed] [Google Scholar]
Leong 2017 {published data only}
- Leong HT, Ng GY, Fu SN. Effects of scapular taping on the activity onset of scapular muscles and the scapular kinematics in volleyball players with rotator cuff tendinopathy. Journal of Science and Medicine in Sport 2017;20(6):555-60. [DOI] [PubMed] [Google Scholar]
Leong 2019 {published data only}
- Leong HT, Fu SN. The Effects of Rigid Scapular Taping on the Subacromial Space in Athletes With and Without Rotator Cuff Tendinopathy: A Randomized Controlled Study. Journal of Sport Rehabilitation 2019;28(3):250-55. [DOI] [PubMed] [Google Scholar]
Ozer 2017 {published data only}
- Özer ST, Gülpınar D, Yeşilyaprak SS. The effects of shoulder and scapular region rigid taping and kinesio taping on scapular dyskinesis and pectoralis minor shortness in overhead athletes. Orthopaedic Journal of Sports Medicine 2017;5:suppl2. [Google Scholar]
Parreira 2014 {published data only}
- Parreira Pdo C, Costa Lda C, Hespanhol LC Jr, Lopes AD, Costa LO. Current evidence does not support the use of Kinesio Taping in clinical practice: a systematic review. Journal of Physiotherapy 2014;60(1):31-9. [DOI] [PubMed] [Google Scholar]
Pekyavas 2014 {published data only}
- Pekyavas NO, Ergun N. Effects of different exercise and kinesiotaping application on pain, flexibility, strength and range of motion in patients with subacromial impingement syndrome [ Subakromiyal sikisma sendromunda farkli egzersiz ve kinezyobant uygulamalarinin atri, esneklik, Kuwet ve eklem hareket acikltina etkisi]. Fizyoterapi Rehabilitasyon 2014;25(1):S31. [Google Scholar]
Polimeni 2003 {published data only}
- Polimeni V, Panuccio A, Furfari P, Crupi D, Barreca G, Forgione G, et al . Preliminary study on the efficacy of various rehabilitation therapies for shoulder pain. Europa Medicophysica 2003;39(1):59-63. [Google Scholar]
Reynard 2018 {published data only}
- Reynard F, Vuistiner P, Leger B, Konzelmann M. Immediate and short-term effects of kinesiotaping on muscular activity, mobility, strength and pain after rotator cuff surgery: a crossover clinical trial. BMC Musculoskeletel Disorder 2018;19(1):305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shih 2018 {published data only}
- Shih YF, Lee YF, Chen WY. Effects of kinesiology taping on scapular reposition accuracy, kinematics, and muscle activity in athletes with shoulder impingement syndrome: a randomized controlled study. Journal of Sport Rehabilitation 2018;27(6):560-69. [DOI] [PubMed] [Google Scholar]
Teys 2013 {published data only}
- Teys P, Bisset L, Collins N, Coombes B, Vicenzino B. One-week time course of the effects of Mulligan's mobilisation with movement and taping in painful shoulders. Manual Therapy 2013;18(5):372-77. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Saorín‐Morote 2016 {published data only}
- Saorin‐Morote D, Gomez‐Conesa A, Velandrino‐Nicolas A. Combined treatment of manual therapy, taping and home exercises in patients with painful shoulder syndrome. Manual Therapy 2016;25:e64-5. [Google Scholar]
Yildiz 2017 {published data only}
- Yildiz A, Buyuktepe Y. HPR the effects of kinesio taping on pain, joint range of motion, muscle strength and disability in impingement syndrome. Annals of the Rheumatic Diseases 2017;76:1476-7. [Google Scholar]
References to ongoing studies
ACTRN12611000359932 {published data only}
- ACTRN12611000359932. The Mulligan method and kinesio taping - initial effects on recovery of painful shoulder in patients with impingement shoulder syndrome, is the Mulligan method and kinesio taping effective in improving shoulder range of motion? https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12611000359932. [ANZCTR: ACTRN12611000359932]
CTRI/2013/07/003847 {published data only}
- CTRI/2013/07/003847. Use of various types of tape in reducing shoulder pain and improve function. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=6694. [CTRI: CTRI/2013/07/003847]
CTRI/2018/09/015780 {published data only}
- CTRI/2018/09/015780. Effect of elastic tape on joint position sense of shoulder joint in patients with impingement of muscles in the shoulder. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=27270. [CTRI: CTRI/2018/09/015780]
CTRI/2020/05/024970 {published data only}
- CTRI/2020/05/024970. Taping In patients with shoulder impingement syndrome. http://www.ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=42577. [CTRI: CTRI/2020/05/024970]
IRCT20180406039203N1 {published data only}
- IRCT20180406039203N1. Evaluation and comparison of two therapeutic physiotherapy protocols of high power or low power lasers combined with kinesio taping on shoulder function and musculoskeletal sonography parameters in patients with subacromial impingement syndrome. https://en.irct.ir/trial/30534. [IRCT: IRCT20180406039203N1]
NCT02290730 {published data only}
- NCT02290730. Effect of kinesio taping on muscle strength in lower trapezius. https://clinicaltrials.gov/ct2/show/NCT02290730. [CLINICALTRIALS.GOV: NCT02290730]
NCT04242381 {published data only}
- NCT04242381. Short term effect of kinesiotaping in patients with shoulder impingement syndrome. https://clinicaltrials.gov/ct2/show/NCT04242381. [CLINICALTRIAL.GOV: NCT04242381]
RBR‐65qh7j {published data only}
- RBR-65qh7j. Effect of elastic tape on shoulder tendinitis. https://ensaiosclinicos.gov.br/rg/RBR-65qh7j/. [REBEC: RBR-65qh7j]
Additional references
Banerjee 2008
- Banerjee S, Wells GA, Chen L. Caveats in the meta-analyses of continuous data: a simulation study. Ottawa: Canadian Agency for Drugs and Technologies in Health, 2008. [Google Scholar]
Bayam 2011
- Bayam L, Ahmad MA, Naqui SZ, Chouhan A, Funk L. Pain mapping for common shoulder disorders. American Journal of Orthopedics 2011;40(7):353-8. [PubMed] [Google Scholar]
Bennell 2007
- Bennell K, Coburn S, Wee E, Green S, Harris A, Forbes A, et al. Efficacy and cost-effectiveness of a physiotherapy program for chronic rotator cuff pathology: a protocol for a randomised, double-blind, placebo-controlled trial. BMC Musculoskeletal Disorders 2007;8:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjelle 1989
- Bjelle A. Epidemiology of shoulder problems. Bailliere's Clinical Rheumatology 1989;3(3):437-51. [DOI] [PubMed] [Google Scholar]
Buchbinder 1996
- Buchbinder R, Goel V, Bombardier C, Hogg-Johnson S. Classification systems of soft tissue disorders of the neck and upper limb: do they satisfy methodological guidelines? Journal of Clinical Epidemiology 1996;49(2):141-9. [DOI] [PubMed] [Google Scholar]
Burbank 2008
- Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: part I. Evaluation and diagnosis. American Family Physician 2008;77:453-60. [PubMed] [Google Scholar]
Cates 2008 [Computer program]
- Visual Rx. Version 3. Dr. Christopher Cates, 2008. www.nntonline.net.
Celik 2020
- Celik D, Karaborklu Argut S, Coban O, Eren I. The clinical efficacy of kinesio taping in shoulder disorders: a systematic review and meta analysis. Clinical Rehabilitation 2020;34(6):723-40. [DOI] [PubMed] [Google Scholar]
Chard 1991
- Chard MD, Hazleman R, Hazleman BL, King RH, Reiss BB. Shoulder disorders in the elderly: a community survey. Arthritis and Rheumatism 1991;34(6):766-9. [DOI] [PubMed] [Google Scholar]
Cho 2013
- Cho CH, Jung SW, Park JY, Song KS, Yu KI. Is shoulder pain for three months or longer correlated with depression, anxiety, and sleep disturbance? Journal of Shoulder and Elbow Surgery 2013;22(2):222-8. [DOI] [PubMed] [Google Scholar]
Coghlan 2008
- Coghlan JA, Buchbinder R, Green S, Johnston RV, Bell SN. Surgery for rotator cuff disease. Cochrane Database of Systematic Reviews 2008, Issue 1. Art. No: CD005619. [DOI: 10.1002/14651858.CD005619.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Constant 1987
- Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clinical Orthopaedics and Related Research 1987;214:160-4. [PubMed] [Google Scholar]
Dabija 2019
- Dabija DI, Jain NB. Minimal clinically important difference of shoulder outcome measures and diagnoses: a systematic review. American Journal of Physical Medicine & Rehabilitation 2019;98(8):671-6. [DOI: 10.1097/PHM.0000000000001169] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2020
- Deeks JJ, Higgins JPT, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Djordjevic 2012
- Djordjevic OC, Vukicevic D, Katunac L, Jovic S. Mobilization with movement and kinesiotaping compared with a supervised exercise program for painful shoulder: results of a clinical trial. Journal of Manipulative and Physiological Therapeutics 2012;35:454‐63. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellenbecker 2010
- Ellenbecker TS, Cools A. Rehabilitation of shoulder impingement syndrome and rotator cuff injuries: an evidence-based review. British Journal of Sports Medicine 2010;44(5):319-27. [DOI] [PubMed] [Google Scholar]
Escamilla 2014
- Escamilla RF, Hooks TR, Wilk KE. Optimal management of shoulder impingement syndrome. Open Access Journal of Sports Medicine 2014;5:13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Furukawa 2006
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta-analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59(1):7-10. [DOI] [PubMed] [Google Scholar]
Gagnier 2017
- Gagnier JJ, Page MJ, Huang H, Verhagen AP, Buchbinder R. Creation of a core outcome set for clinical trials of people with shoulder pain: a study protocol. Trials 2017;18:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghozy 2020
- Ghozy S, Dung NM, Morra ME, Morsy S, Elsayed GG, Tran L, et al. Efficacy of kinesio taping in treatment of shoulder pain and disability: a systematic review and meta-analysis of randomised controlled trials. Physiotherapy 2020;107:176-88. [DOI] [PubMed] [Google Scholar]
Gianola 2016
- Gianola S, Frigerio P, Agostini M, Bolotta R, Castellini G, Corbetta D, et al. Completeness of outcomes description reported in low-back pain rehabilitation interventions: a survey of 185 randomized trials. Physiotherapy Canada 2016;68(3):267-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gianola 2019
- Gianola S, Castellini G, Corbetta D, Moja L. Rehabilitation interventions in randomized controlled trials for low back pain: proof of statistical significance often is not relevant. Health and Quality of Life Outcomes 2019;17(1):127. [PMID: ] [PMID: PMID: 31331343] [PMID: doi: 10.1186/s12955-019-1196-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Godfrey 2007
- Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the simple shoulder test: psychometric properties by age and injury type. Journal of Shoulder and Elbow Surgery 2007;16(3):260-7. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- GRADEpro. Version accessed prior to 1 July 2021. Hamilton (ON): GRADE Working Group, McMaster University (developed by EvidencePrime, Inc.), 2015. Available from www.gradepro.org.
Hao 2019
- Hao Q, Devji T, Zeraatkar D, Wang Y, Qasim A, Siemieniuk RAC, et al. Minimal important differences for improvement in shoulder condition patient-reported outcomes: a systematic review to inform a BMJ Rapid Recommendation. BMJ Open 2019;9(2):e028777. [DOI] [PMC free article] [PubMed] [Google Scholar]
Harbord 2006
- Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Statistics in Medicine 2006;25(20):3443-57. [DOI] [PubMed] [Google Scholar]
Hedges 1981
- Hedges L. Distribution theory for Glass' estimator of effect size and related estimators. Journal of Educational Statistics 1981;6(2):107–28. [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. British Medical Journal 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2009
- Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. Journal of the Royal Statistical Society 2009;172(1):137-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JPT, Altman DG, Sterne JAC (editors). Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors), Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from training.cochrane.org/handbook/archive/v5.2.
Host 1995
- Host HH. Scapular taping in the treatment of anterior shoulder impingement. Physical Therapy 1995;75(9):803-12. [DOI] [PubMed] [Google Scholar]
Huang 2015
- Huang H, Grant JA, Miller BS, Mirza FM, Gagnier JJ. A systematic review of the psychometric properties of patient-reported outcome instruments for use In patients with rotator cuff disease. American Journal of Sports Medicine 2015;43(10):2572-82. [DOI] [PubMed] [Google Scholar]
Hudak 1996
- Hudak PL, Amadio PC, Bombardier C, Beaton D, Cole D, Davis A, et al. Development of an upper extremity outcome measure: the Dash (Disabilities of the Arm, Shoulder and Hand). American Journal of Industrial Medicine 1996;29:602-8, Erratum in: American Journal of Industrial Medicine 1996; 30(3): 602-8. [DOI] [PubMed] [Google Scholar]
Kalron 2013
- Kalron A, Bar-Sela S. A systematic review of the effectiveness of kinesio taping - fact or fashion? European Journal of Physical and Rehabilitation Medicine 2013;49(5):699-709. [PubMed] [Google Scholar]
Kamper 2010
- Kamper SJ, Ostelo RW, Knol DL, Maher CG, De Vet HC, Hancock MJ. Global perceived effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. Journal of Clinical Epidemiology 2010;63(7):760-6 e1. [DOI] [PubMed] [Google Scholar]
Kamper 2013
- Kamper SJ, Henschke N. Kinesio taping for sports injuries. British Journal of Sports Medicine 2013;47(17):1128-9. [DOI] [PubMed] [Google Scholar]
Karjalainen 2019
- Karjalainen TV, Jain NB, Heikkinen J, Johnston RV, Page CM, Buchbinder R. Surgery for rotator cuff tears. Cochrane Database of Systematic Reviews 2019, Issue 12. Art. No: CD013502. [DOI: 10.1002/14651858.CD013502] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kase 2003
- Kase K, Wallis J, Kase T. Clinical Therapeutic Applications Of The Kinesio Taping Method. Tokyo (Japan): Kinesio Taping Association, Ken Ikai Co Ltd, 2003. [Google Scholar]
Kaya 2011
- Kaya E, Zinnuroglu M, Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clinical Rheumatology 2011;30(2):201-7. [DOI] [PubMed] [Google Scholar]
Kessel 1977
- Kessel L, Watson M. The painful arc syndrome. Clinical classification as a guide to management. Journal of Bone and Joint Surgery 1977;59:166-72. [DOI] [PubMed] [Google Scholar]
Ketola 2013
- Ketola S, Lehtinen J, Rousi T, Nissinen M, Huhtala H, Konttinen YT, et al. No evidence of long-term benefits of arthroscopic acromioplasty in the treatment of shoulder impingement syndrome: five-year results of a randomised controlled trial. Bone & Joint Research 2013;2(7):132-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khan 2013
- Khan Y, Nagy MT, Malal J, Waseem M. The painful shoulder: shoulder impingement syndrome. Open Orthopaedics Journal 2013;7:347-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirkley 2003
- Kirkley A, Alvarez C, Griffin S. The development and evaluation of a disease-specific quality-of-life questionnaire for disorders of the rotator cuff: the Western Ontario Rotator Cuff Index. Clinical Journal of Sport Medicine 2003;13(2):84-92. [DOI] [PubMed] [Google Scholar]
Lim 2015
- Lim EC, Tay MG. Kinesio taping in musculoskeletal pain and disability that lasts for more than 4 weeks: is it time to peel off the tape and throw it out with the sweat? A systematic review with meta-analysis focused on pain and also methods of tape application. British Journal of Sports Medicine 2015;49(24):1558-66. [DOI] [PubMed] [Google Scholar]
Littlewood 2013
- Littlewood C, May S, Walters S. Epidemiology of rotator cuff tendinopathy: a systematic review. Shoulder & Elbow 2013;5(4):256–65. [Google Scholar]
Mills 2019
- Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. British Journal of Anesthesia 2019;123(2):e273-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2005
- Mitchell C, Adebajo A, Hay E, Carr A. Shoulder pain: diagnosis and management in primary care. British Medical Journal 2005;331(7525):1124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mohammadi 2014
- Mohammadi HK, Kalantari KK, Naeimi SS, Pouretezad M, Shokri E, Tafazoli M, et al. Immediate and delayed effects of forearm kinesio taping on grip strength. Iranian Red Crescent Medical Journal 2014;16(8):e19797. [DOI] [PMC free article] [PubMed] [Google Scholar]
Montalvo 2014
- Montalvo AM, Cara EL, Myer GD. Effect of kinesiology taping on pain in individuals with musculoskeletal injuries: systematic review and meta-analysis. Physician and Sports Medicine 2014;42(2):48-57. [DOI] [PubMed] [Google Scholar]
Morris 2013
- Morris D, Jones D, Ryan H, Ryan CG. The clinical effects of Kinesio(R) Tex taping: a systematic review. Physiotherapy Theory and Practice 2013;29(4):259-70. [DOI] [PubMed] [Google Scholar]
Mostafavifar 2012
- Mostafavifar M, Wertz J, Borchers J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. Physician and Sports Medicine 2012;40(4):33-40. [DOI] [PubMed] [Google Scholar]
Mottram 1997
- Mottram SL. Dynamic stability of the scapula. Manual Therapy 1997;2(3):123-31. [DOI] [PubMed] [Google Scholar]
Myers 2000
- Myers JB, Lephart SM. The role of the sensorimotor system in the athletic shoulder. Journal of Athletic Training 2000;35(3):351-63. [PMC free article] [PubMed] [Google Scholar]
Nikolakopoulou 2014
- Nikolakopoulou A, Mavridis D, Salanti G. How to interpret meta-analysis models: fixed effect and random effects meta-analyses. . Evidence-Based Mental Health 2014 ;17(2):64. [DOI: 10.1136/eb-2014-101794] [DOI] [PubMed] [Google Scholar]
Page 2011
- Page P. Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. International Journal of Sports Physical Therapy 2011;6(1):51-8. [PMC free article] [PubMed] [Google Scholar]
Page 2013
- Page MJ, McKenzie JE, Forbes A. Many scenarios exist for selective inclusion and reporting of results in randomized trials and systematic reviews. Journal of Clinical Epidemiology 2013;66(5):524-37. [DOI] [PubMed] [Google Scholar]
Page 2016a
- Page MJ, Green S, McBain B, Surace SJ, Deitch J, Lyttle N, et al. Manual therapy and exercise for rotator cuff disease. Cochrane Database of Systematic Reviews 2016, Issue 6. Art. No: CD012224. [DOI: 10.1002/14651858.CD012224] [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2016b
- Page MJ, Green S, Mrocki MA, Surace SJ, Deitch J, McBain B, et al. Electrotherapy modalities for rotator cuff disease. Cochrane Database of Systematic Reviews 2016, Issue 6. Art. No: CD012225. [DOI: 10.1002/14651858.CD012225] [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2018
- Page MJ, Huang H, Verhagen AP, Gagnier JJ, Buchbinder R. Outcome reporting in randomized trials for shoulder disorders: literature review to inform the development of a core outcome set. Arthritis Care and Research (Hoboken) 2018;70(2):252-9. [DOI] [PubMed] [Google Scholar]
Page 2018a
- Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ Open 2018;8:e019703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pekyavas 2014b
- Pekyavas NO, Tunay VB, Akbayrak T, Kaya S, Karatas M. Complex decongestive therapy and taping for patients with postmastectomy lymphedema: a randomized controlled study. European Journal of Oncology Nursing 2014;18:585-90. [DOI] [PubMed] [Google Scholar]
Peters 1994
- Peters D, Davies P, Pietroni P. Musculoskeletal clinic in general practice: study of one year's referrals. British Journal of General Practice 1994;44(378):25-9. [PMC free article] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Roach 1991
- Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care and Research 1991;4(4):143-9. [PubMed] [Google Scholar]
Roy 2009
- Roy JS, MacDermid JC, Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires.. Arthritis & Rheumatology 2009;61(5):623-32. [DOI: 10.1002/art.24396] [DOI] [PubMed] [Google Scholar]
R software [Computer program]
- A Language and Environment for Statistical Computing. R Core Team. Vienna (Austria): R Foundation for Statistical Computing, 2013. www.R-project.org/.
Saltychev 2015
- Saltychev M, Aarimaa V, Virolainen P, Laimi K. Conservative treatment or surgery for shoulder impingement: systematic review and meta-analysis. Disability and Rehabilitation 2015;37(1):1-8. [DOI] [PubMed] [Google Scholar]
Saracoglu 2018
- Saracoglu I, Emuk Y, Taspinar F. Does taping in addition to physiotherapy improve the outcomes in subacromial impingement syndrome? A systematic review. Physiotherapy Theory and Practice 2018;34(4):1-13. [DOI] [PubMed] [Google Scholar]
Schellingerhout 2008
- Schellingerhout JM, Verhagen AP, Thomas S, Koes BW. Lack of uniformity in diagnostic labeling of shoulder pain: time for a different approach. Manual Therapy 2008;13:478-83. [DOI] [PubMed] [Google Scholar]
Schünemann 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editors. GRADE handbook for grading quality of evidence and strength of recommendations using the GRADE approach (updated October 2013). The GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Schunemann 2017b
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, et al (editors). Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017). Cochrane, 2017. Available from training.cochrane.org/handbook/archive/v5.2.
Sterne 2017
- Sterne JAC, Egger M, Moher D, Boutron I (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Churchill R, Chandler J, Cumpston MS (editors). Cochrane Handbook for Systematic Reviews of Interventions, Version 5.2.0 (updated June 2017), Cochrane, 2017. Available from training.cochrane.org/handbook/archive/v5.2.
Steuri 2017
- Steuri R, Sattelmayer M, Elsig S, Kolly C, Tal A, Taeymans J, et al. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: a systematic review and meta-analysis of RCTs. British Journal of Sports Medicine 2017;51(8):1340-7. [DOI: 10.1136/bjsports-2016-096515] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stijnen 2010
- Stijnen T, Hamza TH, Ozdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Statistics in Medicine 2010;29(29):3046-67. [DOI] [PubMed] [Google Scholar]
Sullivan 2016
- Sullivan MJL. Controlling for “confounders” in psychosocial pain research. Pain 2016;157(4):775-6. [DOI] [PubMed] [Google Scholar]
Tashjian 2013
- Tashjian RZ. Is there evidence in favour of surgical interventions for the subacromial impingement syndrome? Clinical Journal of Sport Medicine 2013;23(5):406-7. [DOI] [PubMed] [Google Scholar]
Teunis 2014
- Teunis T, Lubberts B, Reilly BT. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. Journal of Shoulder and Elbow Surgery 2014;23(12):1913-21. [DOI] [PubMed] [Google Scholar]
Timmons 2012
- Timmons MK, Thigpen CA, Seitz AL, Karduna AR, Arnold BL, Michener LA. Scapular kinematics and subacromial-impingement syndrome: a meta-analysis. Journal of Sport Rehabilitation 2012;21(4):354-70. [DOI] [PubMed] [Google Scholar]
Turner 2013
- Turner RM, Bird SM, Higgins JP. The impact of study size on meta-analyses: examination of underpowered studies in Cochrane reviews. PLOS One 2013;8(3):e59202. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van der Windt 1996
- Van der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. British Journal of General Practice 1996;46(410):519-23. [PMC free article] [PubMed] [Google Scholar]
Van Rijn 2010
- Van Rijn RM, Huisstede BM, Koes BW, Burdorf A. Associations between work-related factors and specific disorders of the shoulder - a systematic review of the literature. Scandinavian Journal of Work, Environment & Health 2010;36(3):189-201. [DOI] [PubMed] [Google Scholar]
Vas 2005
- Vas J, Perea-Milla E, Mendez C, Galante AH, Madrazo F, Medina I, et al. Acupuncture and rehabilitation of the painful shoulder: study protocol of an ongoing multicentre randomised controlled clinical trial. BMC Complementary and Alternative Medicine 2005;5:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Viechtbauer 2010
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software 2010;36:1-48. [Google Scholar]
Virta 2012
- Virta L, Joranger P, Brox JI, Eriksson R. Costs of shoulder pain and resource use in primary health care: a cost-of-illness study in Sweden. BMC Musculoskeletal Disorders 2012;13:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Whittle 2015
- Whittle S, Buchbinder R. Rotator cuff disease. Annals of Internal Medicine 2015;162(1):ITC1-ITC15. [DOI: 10.7326/AITC201501060] [DOI] [PubMed] [Google Scholar]
Williams 2012
- Williams S, Whatman C, Hume PA, Sheerin K. Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Medicine 2012;42(2):153-64. [DOI] [PubMed] [Google Scholar]


