Abstract
Background
Bed rest is prescribed to all patients with acute myocardial infarction (AMI), but to a variable extent. Current guidelines (American College of Cardiology/ American Heart Association) recommend at least 12 hours bed rest in patients with uncomplicated ST‐elevation myocardial infarction, however the basis for this recommendation is unclear.
Objectives
To compare the effects of short versus longer bed rest in patients with uncomplicated AMI.
Search methods
We searched the Cochrane Central Register of Controlled Trials (The Cochrane Library 2009, Issue 3), MEDLINE (January 1966 to October 2009), EMBASE (January 1988 to October 2009), PASCAL BioMed (January 1996 to August 2005), PsycINFO (January 1966 to October 2009) and BIOSIS Previews (January 1990 to October 2009). Bibliographies were checked. No language restrictions were applied.
Selection criteria
Randomised and quasi‐randomised controlled trials of short versus longer bed rest in patients with uncomplicated AMI were sought.
Data collection and analysis
Study selection was performed independently by at least two investigators according to the predefined inclusion criteria. Data were extracted by two investigators independently and in duplicate. Authors were contacted to obtain missing information.
Main results
We found 15 trials with 1487 patients assigned to a short period of bed rest (median 6 days) and 1471 patients assigned to longer bed rest (median 13 days). Generally the studies were outdated and appeared to be of moderate to poor methodological reporting quality. There was no evidence that shorter bed rest was more harmful than longer bed rest in terms of all cause mortality (RR 0.85, 95%CI 0.68 to 1.07), cardiac mortality (RR 0.81, 95%CI 0.54 to 1.19), or reinfarction (RR 1.07, 95%CI 0.79 to 1.44).
Authors' conclusions
Bed rest ranging from 2 to 12 days appears to be as safe as longer periods of bed rest. The quality of most trials is unsatisfactory. Current bed rest recommendations are not supported by the existing evidence as the optimal duration of bed rest is unknown. The lack of adequate trials is surprising, considering the large size of several studies to compare effectiveness of drugs on people with AMI.
Keywords: Humans, Bed Rest, Bed Rest/methods, Myocardial Infarction, Myocardial Infarction/therapy, Randomized Controlled Trials as Topic, Time Factors
Plain language summary
Bed rest for acute uncomplicated myocardial infarction
Bed rest is an inherent part of treatment for acute myocardial infarction (AMI). In clinical practice this intervention is prescribed in different ways and for different lengths of time. Current guidelines recommend at least 12 hours bed rest following AMI. However the basis for these recommendations is unclear. This review found 15 trials which were generally outdated and of moderate to poor methodological quality. Bed rest ranging from 2 to 12 days appears to be as safe as longer periods of bed rest. No evidence was found to support the current bed rest recommendations of not more than 12 to 24 hours. The optimal duration of bed rest after AMI remains undetermined from the available evidence.
Background
Each year, a total of about 1,100,000 people in America experience acute myocardial infarction. Accordingly, the estimated direct and indirect costs for coronary artery disease were about US$111.8 billion in 2002 (AHA 2001). Bed rest is an implicit part of the early therapy in patients with acute myocardial infarction (Allen 1999). The principle idea behind this intervention is to reduce myocardial workload, avoid further perfusion impairment of the myocardium and minimise remodelling (Wenger 1978). Most complications occur within the first 48 hours after acute myocardial infarction (Spracklen 1968). Therefore monitoring is essential for this period. As most monitoring devices are designed for recumbent patients, bed rest is often understood as a necessary condition to enable monitoring. On the other hand immobilisation in itself may adversely affect patients outcomes, e.g. by increasing the risk for thromboembolic complications (Maurere 1971), especially in patients with myocardial insufficiency (ESC 2003). Prolonged bed rest may also decrease morale or well‐being, which is an important factor for rehabilitation and return to work (Bloch 1978). In addition, prolonged bed rest may occupy beds and personnel unnecessarily, which may lead to bed shortages for acutely ill patients.
The first approach to early mobilisation was done by Levine and Lown (Levine 1952), who developed the concept of armchair mobilisation in the early 1950s. Many studies were done in the nineteen seventies to evaluate the outcome of early mobilisation and short hospital stays. Since then, hospital stays have become shorter and therapy has changed dramatically (McGovern 1996). According to ESC guidelines (ESC 2003) and ACC/AHA guidelines (ACC/AHA 2004) bed rest should be 12‐24 hours after uncomplicated acute ST‐elevation myocardial infarction, but this seems to be rather 'consensus‐based' than evidence‐based.
In contrast to the pharmacologic treatment of myocardial infarction, the influence of bed rest on outcome in patients with acute myocardial infarction has not been well examined. Resources are becoming smaller and the economic pressure is increasing. Reducing duration of bed rest and thus the length of hospital‐stay to a necessary minimum after an acute myocardial infarction could reduce costs, but must not negatively influence outcome.
Objectives
To identify the effect of bed rest on clinical outcome after uncomplicated acute myocardial infarction, to determine the optimal duration of bed rest after uncomplicated acute myocardial infarction and to identify areas of the evidence base that require more work to evaluate the optimal duration of bed rest after uncomplicated acute myocardial infarction.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials and quasi randomised trials, without language restrictions.
Types of participants
Patients with acute uncomplicated myocardial infarction, according to authors' definitions. We did not intend to make any restrictions to types of patients with regard to age, gender, race and comorbidity and to the setting. No restrictions on use of specific treatments such as fibrinolytics or early revascularisation were made.
Types of interventions
Duration of bed rest as given, transformed as feasible, most likely in hours or days. Bed rest should be defined as lying flat without permission to leave the bed for any reason.
Types of outcome measures
Primary outcome measures
Total death (total number).
Cause‐specific death (due to coronary heart disease).
Reinfarction.
Secondary outcome measures
Arrhythmia.
Thromboembolic complications.
Cardiac wall rupture/ aneurysm.
Duration of hospital stay.
Quality of life.
Search methods for identification of studies
Electronic searches
We searched the Cochrane Central Register of Controlled Trials (CENTRAL) on The Cochrane Library (2009, Issue 3), MEDLINE (January 1966 to October 2009), EMBASE (January 1988 to October 2009), PASCAL BioMed (January 1996 to October 2009), PsycINFO (January 1966 to August 2005) and BIOSIS Previews (January 1990 ‐ October 2009). See Appendix 1 and Appendix 2 for details of the search strategies.
A highly sensitive search strategy for identifying RCTs was used with MEDLINE (Dickersin 1994) and EMBASE (Lefebvre 1996).
No language restrictions were applied.
Searching other resources
References of the retrieved articles and other relevant articles or reviews were searched for relevant citations, and experts were contacted to obtain references of relevant studies.
Data collection and analysis
Study selection
The abstracts of all search hits were read independently by at least two investigators and selected according to the inclusion criteria, using an in/out form. Inconsistencies between the independent investigators were clarified by discussion between three investigators. Full text versions of all relevant articles were obtained and were read independently by at least two investigators. Irrelevant or non‐randomised studies were excluded. Inconsistencies between the independent investigators were clarified by discussion with at least three investigators.
Data extraction
Data were extracted manually onto a print‐out table based on an excel spreadsheet, by two investigators independently and in duplicate. A prototype spreadsheet for data collection was designed for this purpose. After internal approval this prototype was used in a pilot phase with five studies to evaluate its feasibility, particularly for the assessment of the presumed outcome measures. Reliability, range and consistency inspections were performed. Inconsistencies between the two observers were clarified by discussion. The sampling procedure was performed according to the QUOROM guidelines (Moher 1999).
Data analysis
Continuous data are presented as given in the papers. Proportions are reported as absolute number and percentage. Odds ratios and 95% confidence intervals were calculated to measure the effect of the intervention. We investigated clinical heterogeneity by inspection of the studies. Where clinical heterogeneity was negligible, we performed a quantitative data synthesis (meta‐analysis). Statistical heterogeneity was analysed by chi‐squared test for heterogeneity and by using the I2 statistic (Higgins 2003). Where statistical heterogeneity was unlikely we combined studies quantitatively using a fixed‐effect models (Mantel Haenszel 1959); if it had been necessary we had intended using a random‐effects model (DerSimonian 1986). To assess publication bias, funnel plot analysis (Egger 1997) was used.
Methodological quality assessment
For the quality assessment the key characteristics of study design (see below) were evaluated by two investigators independently; inconsistencies were clarified by discussion between investigators (Jüni 1999, Moher 1995). 1) Randomisation method. 2) Blinded assessment of primary outcome. 3) Intention to treat.
These key characteristics of study design were used for sensitivity analysis. Weighting studies according to the quality was not be performed (Jüni 1999).
Results
Description of studies
Results of the search
We found 532 potentially relevant articles by searching the electronic databases. Manually searching the references of the retrieved papers identified another 12 potentially eligible studies of which four papers describing three studies were included (Abraham 1975; Beckwith 1954; Hutter 1973). Twenty‐five studies were excluded because they were uncontrolled, there was no explicit statement of random allocation, because the intervention was not short versus long bed rest or because the outcome variables were physiologic measurements only (see Characteristics of excluded studies). Finally, 15 randomised and quasi‐randomised controlled trials were included with 1487 participants assigned to early mobilisation and 1471 participants assigned to a longer period of bed rest.
Included studies
The period of bed rest in the early mobilisation groups ranged between 2 and 14 days, the median was 6 days. In the longer bed rest groups, patients were confined to strict bed rest for 5 to 28 days, the median was 13 days. The regimens of early mobilisation varied, ranging from simply leaving the bed on a predefined day to detailed schedules for increasingly graded exercises. See Table 1 for details.
1. Mobilisation Schemes.
| Study | Short bed rest | Long bed rest |
| Abraham 1975 | Kept in bed for five days, allowed to use a bedside commode as soon as possible. The patients were then mobilised by sitting out of the bed: Day 6: ½ hrs twice a day Day 7: 2 hrs twice a day Day 8: all day + walk to toilet Day 9: walk around freely | Kept in bed for 12 days, allowed to use a bedside commode as soon as possible. The patients were then mobilised by sitting out of the bed: Day 13: ½ hrs twice a day Day 14: 2 hrs twice a day Day 15: all day + walk to toilet Day 16: walk around freely |
| Ahlmark 1979 | On 4th and 5th day sit up for periods of altogether 1 ½ and 3hrs Move about ward with clothes from day 6 Discharge after day 8 | Gradually mobilised after day 3 Get out of bed from day 12 Discharge after 15 days |
| Beckwith 1954 | Start sitting in chair from day 2‐5 if no pain or shock: ½ hrs 3x daily for 3 days 1 hr 3x daily for 3 days 1 ½ hrs 3x daily for 6 days Then up until day 28, bedside commode and few steps with assistance | Days 0‐14 strict bed rest, no bath, shave or feeding themselves. Days 15‐28 extend and flex feet bedside commode once daily. |
| Bloch 1974 | Start 24‐48 hrs after admission by physical therapist, depending on patients clinical course (a.m.= active mobilisation): I.a.m. of ankles and wrists; respiratory exercises II.a.m. of limbs, partial wash‐up care in bed; dangle legs on side of bed (5min) III.a.m. in bed; bedside commode; sitting 15 min. in armchair twice a day IV.a.m. against resistance; complete care in bed; 30min. in armchair twice a day V.a.m. in bed; 1 hr in armchair twice a day; 2 short walks in room VI.‐VIII. a.m. in bed; light gymnastic exercise; sitting in armchair at will; washing at the washstand; walks in corridor IX.‐X as previous + exercise with footstool XI as previous + walking down 1 flight of stairs twice a day XII‐XIV as previous + walking up 1‐3 flights of stairs twice a day | Strict bed rest for at least 3 wks, including bedpan, with nursing service for toilet and feeding; thereafter progressive mobilisation by ward nurses |
| Greco 1975 | Day 7‐8 sit in chair 1hr twice a day Day 9 sit in chair most day Day 12 walk in room 10‐15 min twice daily Day 13 walk in the yard progressively | Day 14‐15 sit in chair 1hr twice a day Day 16 sit in chair most day Day 19 walk in room 10‐15 min twice daily Day 20 walk in the yard progressively |
| Harpur 1971 | Day 0‐7 bed rest in any position, shave, feed themselves, use bedside commode; Day 0‐3 bathed in bed by nurses Day 8 sit out of bed ½ hr once a day Day 9 sit out of bed ½ hr twice a day Day 10 sit out of bed 1 hr twice a day Day 11 sit out of bed 2 hr twice a day, walk to toilet Day 12 sit out of bed 6 hrs and for meals Day 13 up all day, deep bath Day 14 up all day, climb stairs Day 14 up all day, discharge | Day 0‐14 bed rest in any position, shave, feed themselves, use bedside commode; Day 0‐3 bathed in bed by nurses Day 15 sit out of bed ½ hr once a day Day 16 sit out of bed ½ hr twice a day Day 16 sit out of bed 1 hr twice a day Day 17 sit out of bed 2 hr twice a day, walk to toilet Day 18 sit out of bed 6 hrs and for meals Day 19 up all day, deep bath Day 20 up all day, climb stairs Day 21 up all day, discharge |
| Hayes 1974 & Hayes 1976 | Sit out of bed when transferred from coronary care unit (CCU) thereafter no restriction to activities; encouraged to walk around the ward, use ordinary ward washing and toilet facilities | Day 0‐7 after transferred from CCU bed rest Sit in chair when bed was made, bedside commode Day 8‐16 allowed up, encouraged to walk around the ward |
| Hutter 1973 | Day 7‐9 dangle Day 10‐11 sit in chair Day 12‐13 walk | Day 10‐12 dangle Day 13‐16 sit in chair Day 17‐20 walk |
| Messin 1982 | From 2nd day physical training (3 stages) 5th day walking 10th day climbing stairs depending on submaximal exercise test | From 2nd day physical training (3 stages) 8th day walking 21st day climbing stairs |
| Miller 1976 | From day 0‐3 sitting and standing beside bed 30 min three times a day; used bedside commode eating while sitting at the bedside | Traditional 5 days of bed rest |
| Rowe 1989 | Day 4 walked briskly 10‐15 min twice a day with physiotherapist; over three days duration and intensity of walking increased rapidly. Day 8 climbing 1‐2 flights of stairs | Nursing staff observed patients to ensure inactivity |
| Royal Infirmary 1973 | Active leg movements from 1st day encouraged day 7 sit out of bed ½ hr day 8 sit out of bed 1 hr day 9 sit out of bed 2 hrs, stand by bed 5 min. day 10 walk once around the bed day 11 walk 25 yards day 12 walk 50 yards day 13 fully ambulant in the ward | Active leg movements from 1st day encouraged day 21 sit out of bed ½ hr day 22 sit out of bed 1 hr day 23 sit out of bed 2 hrs, stand by bed 5 min. day 24 walk once around the bed day 25 walk 25 yards day 26 walk 50 yards day 27 fully ambulant in the ward |
| Schaumann 1977 | According to WHO 1968* | Strict bed rest |
| West 1979 | From day 5: sitting out of bed for two ½ hr periods on the 5th day with subsequently increasing activity until after one week they were out of bed for 2 hrs a day and walking on the level. | From day 10: sitting out of bed for two ½ hr periods on the 10th day with subsequently increasing activity until after one week they were out of bed for 2 hrs a day and walking on the level. |
| *WHO, Regional Office for Europe. A program for the physical rehabilitation of patients with acute myocardial infarction. Kopenhagen: World Health Organisation, 1968. |
The median of the average age reported was 60 years, ranging from 52 to 67 years. The percentage of women ranged from 9% to 28%, the median being 19%. Some studies excluded people above age 70 or 75 years (Bloch 1974; Harpur 1971; Royal Infirmary 1973; West 1979). The time from acute myocardial infarction to assessment of outcome ranged from 5 days to 52 weeks (median 24 weeks). One study did not report the duration of follow up at all (Beckwith 1954). According to our protocol we used the outcome nearest to 6 months.
Most studies were published in the 1970s, the most recent study being published 1989, the oldest in 1954. Therefore, therapeutic strategies in the reported studies are not comparable to the measures employed today. The use of systemic thrombolysis was mentioned in one small study with 48 patients (Rowe 1989). The use of oral anticoagulants was described in seven studies (Abraham 1975; Beckwith 1954; Bloch 1974; Harpur 1971; Hayes 1974; Royal Infirmary 1973; West 1979), of which one described the use of aspirin (Bloch 1974).
Risk of bias in included studies
Overall the quality of reporting did not meet current standards (see Characteristics of included studies). Five studies explicitly used proper randomisation methods (Bloch 1974; Hutter 1973; Royal Infirmary 1973; Schaumann 1977; West 1979), four used the word random in the methods section but gave no detail of how the sequence was generated (Ahlmark 1979; Greco 1976; Messin 1982; Rowe 1989), and the remaining studies used quasi‐randomisation methods (Abraham 1975; Beckwith 1954; Harpur 1971; Hayes 1974; Hayes 1976; Miller 1976). Only one paper reported explicitly that the outcome was assessed in a blinded fashion (Hutter 1973) and only one study stated explicitly that the analysis was according to the intention‐to‐treat principle (Hutter 1973). In the remaining studies it was unclear whether patients were excluded and how this was handled.
Effects of interventions
We found 15 trials including 1487 patients assigned to early mobilisation and 1471 patients assigned to a longer period of bed rest.
In several studies only limited information on age, gender or details on diagnosis was given to help in clearly assessing the degree of clinical heterogeneity. There was some degree of variability in the durations of bed rest and modes of mobilisation. In summary we assumed, however, that studies were essentially comparable. Therefore we attempted formal meta‐analysis. This was supported by the low statistical heterogeneity generally found in the analyses.
Primary outcome
Thirteen papers reported on mortality (Analysis 1.1) and three papers reported on cardiac death (Analysis 1.2). There was no evidence that duration of bed rest was associated with all cause or cardiac death after uncomplicated myocardial infarction (RR 0.85, 95%CI 0.68 to 1.07, and RR 0.81, 95%CI 0.54 to 1.19, respectively). Eleven papers reported on reinfarction (Analysis 2.1). There was no association between the rate of reinfarction and the duration of bed rest (RR 1.07, 95%CI 0.79 to 1.44).
1.1. Analysis.
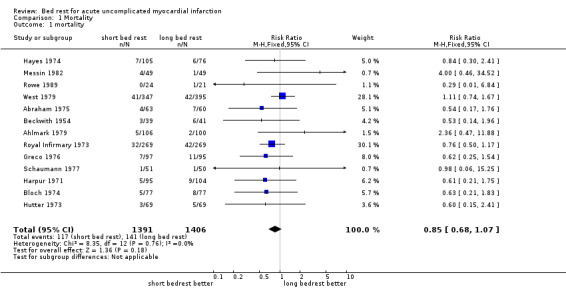
Comparison 1 Mortality, Outcome 1 mortality.
1.2. Analysis.
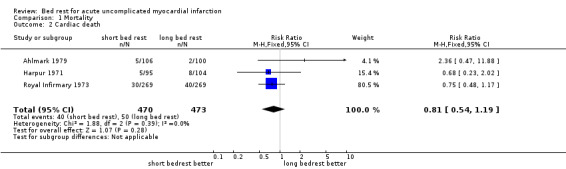
Comparison 1 Mortality, Outcome 2 Cardiac death.
2.1. Analysis.
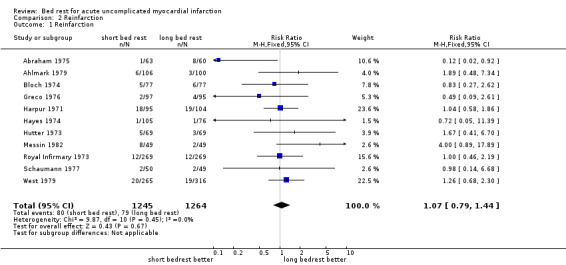
Comparison 2 Reinfarction, Outcome 1 Reinfarction.
Secondary outcomes
Arrhythmia was reported in seven studies (Analysis 3.1). There was no difference in arrhythmia rates between short and long bed rest.
3.1. Analysis.
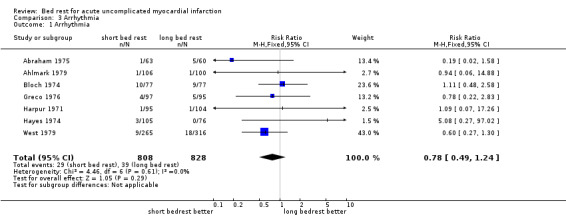
Comparison 3 Arrhythmia, Outcome 1 Arrhythmia.
Thromboembolic complications were reported in six studies (Analysis 4.1). Some researchers took great pains to measure the presence of thrombosis, including fibrinogen scans and venography. The rate of such an event was somewhat lower in patients with shorter duration of bed rest, but this was not statistically significant.
4.1. Analysis.
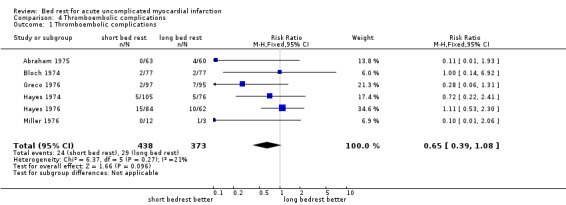
Comparison 4 Thromboembolic complications, Outcome 1 Thromboembolic complications.
Cardiac wall rupture/aneurysm were reported in one study only (Analysis 5.1). In 199 patients seven such events were observed, there was no significant difference between the groups.
5.1. Analysis.
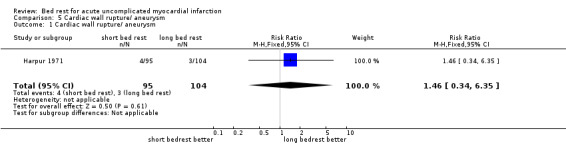
Comparison 5 Cardiac wall rupture/ aneurysm, Outcome 1 Cardiac wall rupture/ aneurysm.
Duration of hospital stay was not reported as an outcome in most studies but was rather a predefined item of the protocol. Duration of hospital stay has therefore been reported (Analysis 6.1), but data were not combined.
6.1. Analysis.
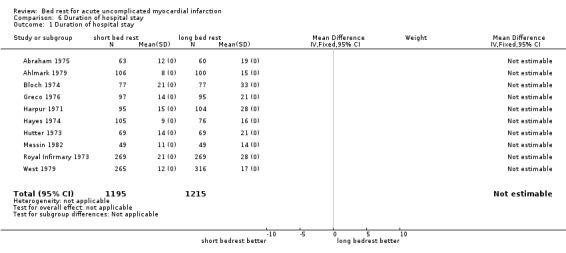
Comparison 6 Duration of hospital stay, Outcome 1 Duration of hospital stay.
None of the studies reported on quality of life.
Publication bias
Publication bias cannot be excluded completely when looking at the funnel plot with mortality as the end point (Figure 1). It seems not very likely when looking at reinfarction as the endpoint (Figure 2). The 11 studies looking at reinfarction also assessed mortality.
1.
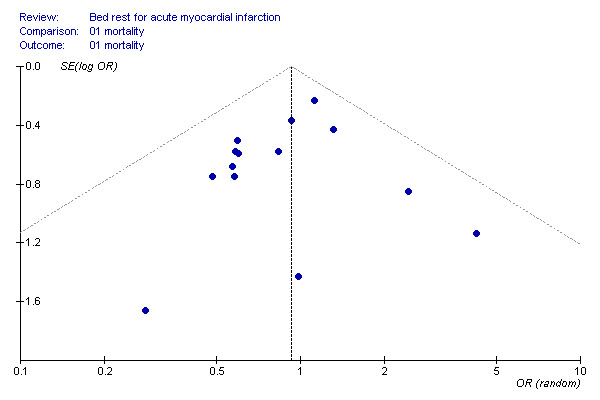
funnel plot 1.
outcome is all‐cause mortality
2.
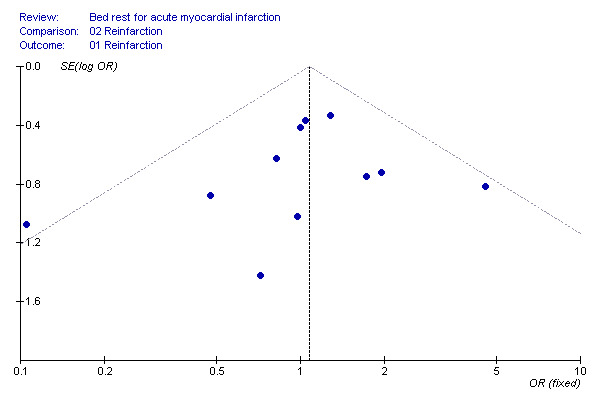
funnel plot 2.
outcome is reinfarction
Sensitivity analysis
Sensitivity analysis to investigate the influence of trial quality on the effect of bed rest on all cause mortality yielded comparable figures: in studies reporting allocation concealment with levels A and B showed virtually the same effect as those studies with level C or D reporting (RR 0.78, 95%CI 0.56 to 1.09; and RR 0.92, 95%CI 0.66 to 1.28; respectively, Analysis 7.1 ). There was only one study reporting blinding of the outcome assessor and intention‐to‐treat analysis. This study (Hutter 1973) showed a more pronounced beneficial effect of short bed rest on mortality than the summary effect of the other studies (RR 0.60, 95%CI 0.15 to 2.41, and RR 0.85, 95%CI 0.68 to 1.07, respectively). The qualitatively best study (Hutter 1973) compared 9 with 12 days of bed rest. This is a fairly outdated comparison.
7.1. Analysis.
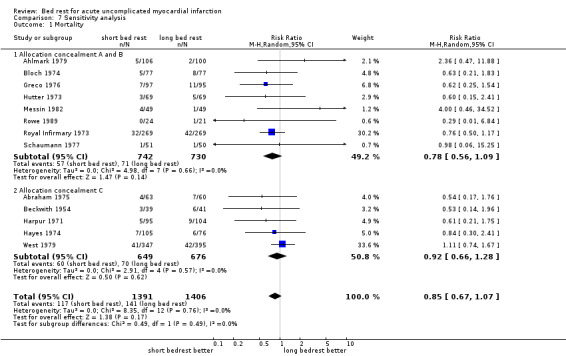
Comparison 7 Sensitivity analysis, Outcome 1 Mortality.
Discussion
All studies investigating bed rest in acute myocardial infarction are very old and for most studies the quality of reporting is generally poor. Taking this into account, we are not able to make any inferences about the effects on clinical outcomes of contemporary much shorter durations of bed rest, nor did we find any evidence to support current policies. In the era of comparatively long durations of bed‐rest, there was no evidence to support longer durations over shorter durations of bed rest. It has to be emphasised that we could not find evidence for the 12‐hour bed rest as proposed by leading cardiology associations.
Potential biases and heterogeneity
It is not possible to exclude publication bias given the limited number of trials available, although it does not seem very likely. Whether a quantitative synthesis of the data is a useful exercise may be debatable: (1) the quality of reporting was in general very low and; (2) there was clinical heterogeneity, in particular concerning variable durations of bed rest in both groups. We believe however, that quantitatively combining the findings is an elegant means to summarise that shorter bed rest has no or little adverse effects, compared to longer bed rest. Of note most studies had a very small sample size, the largest containing only 742 patients.
Internal and external validity
The quality of reporting was in general not satisfactory, in particular when applying rigorous standards (Begg 1996). It is, however, impossible to say how much the quality of reporting is associated with the internal validity of these studies, because most of these studies were performed long before any reporting standards were established. It is known that studies of very low quality show an effect away from unity (Schulz 1995), but this seems not to be a problem here. We did our best to rule out any kind of publication bias and addressed heterogeneity. Thus we believe that the internal and external validity of our review is as good as could be achieved with reliance on the published reports of the trials.
Comparison with already existing meta‐analyses
To the best of our knowledge there is only one other meta‐analysis addressing a similar question besides a paper published version of this review (Herkner 2003). The study by Allen et al (Allen 1999) addressed bed rest in general as a poorly evaluated, but frequently prescribed, therapy for a wide range of diseases. The study included bed rest for the treatment of acute myocardial infarction, spontaneous labour, pulmonary tuberculosis but also after interventions like lumbar puncture. They concluded that there is no evidence that bed rest as a therapy has beneficial effects. However, there are some technical and methodological shortcomings. The authors searched only MEDLINE and the Cochrane Controlled Trial Register and found only five articles. Consequently it is possible that this review was subject to publication bias, or at least may not have given the full picture. We identified an additional 11 trials, two published in other languages than English. All but one showed no difference in outcome between the groups. Further a probably non‐randomised study (Lamers 1973) was included in the systematic review by Allen et al. Because of its methodological strengths and comprehensiveness we believe that our review further strengthens the findings of Allen et al (Allen 1999).
Authors' conclusions
Implications for practice.
Given the limitations of the evidence, most of which is from old trials and of little relevance to contemporary clinical practice, it is not possible to make a definitive judgement on whether shorter or longer durations of bed rest are safer. Current practice has moved to markedly shorter durations of bed rest, with the most recent ACC/AHA (ACC/AHA 2004) and ESC (ESC 2003) guidelines recommending durations of no more than 12 to 24 hours bed rest. However, such advice is not based on any randomised evidence and the optimal duration of bed rest will remain unknown without further trials. It is likely that a certain minimum time in bed will always be required and that practical requirements in management of coronary care beds will determine how long this is.
Implications for research.
For a frequent and dangerous disease this lack of adequate trials is quite surprising in the light of tremendously large studies to compare effectiveness of drugs (GUSTO III) for acute myocardial infarction. In the early 1980s Cochrane suggested, based on an emerging evidence, mobilising patients with uncomplicated acute myocardial infarction on the second day (Cochrane 1981). It took several years to implement this in clinical practice. Twenty years later guidelines and practice have changed accordingly. The evidence, however, has not really improved.
The next step, however, should be a survey to evaluate the patients' subjective preferences for bed rest after uncomplicated ST‐elevation myocardial infarction. Based on that, strategies for bed rest other than strictly time‐based schedules, like patient‐determined bed rest may be of interest.
With increased use of telemetric monitoring (using wireless monitoring technologies), bed‐rest is no longer mandatory for monitoring purposes. Telemonitoring would provide an opportunity to compare much shorter durations of bed‐rest (< 12 hours) with longer durations (e.g. 2 days) in people with uncomplicated myocardial infarction. These trials should include assessing the effect on quality of life, because we know almost nothing about influences on this important outcome.
What's new
| Date | Event | Description |
|---|---|---|
| 5 December 2012 | Review declared as stable | This review is no longer being updated as the last included study was published in 1989. So it has become a historical review. |
History
Protocol first published: Issue 4, 2002 Review first published: Issue 2, 2007
| Date | Event | Description |
|---|---|---|
| 12 October 2009 | New search has been performed | The search was updated in October 2009, minor changes were made to the search strategy. No new studies were identified for inclusion. The conclusions are unchanged. |
| 8 September 2008 | Amended | Converted to new review format. |
| 5 February 2007 | New citation required and conclusions have changed | Substantive amendment |
Notes
The last study included in this review comes from 1989, most studies were performed in the 1970's, and so represents a historical review. Should the subject become salient again it is unlikely that the contemporary stuidies would compare with those in this review. Almost all components of AMI therapy have dramatically changed, and the issues involved today do not compare to the issues at the time when the studies from my review were published ‐ femoral access issues and mobilisation might serve as one example amongst many others.
Acknowledgements
Eva Lüftenegger, MA, who helped us to translate the French articles and Dimitri Schaminer, who helped to translate the Russian articles. We are indebted to Jana Thoennissen, MD, who helped us very much with the protocol and attributed to an earlier version of this review. Margaret Burke, TSC Cochrane Heart Group, re‐run the search from 2005‐2009 for the update review.
Appendices
Appendix 1. Search Strategies 2009
CENTRAL on The Cochrane Library
#1 MeSH descriptor myocardial infarction explode all trees #2 MeSH descriptor acute coronary syndrome this term only #3 myocardial next infarct* in All Text #4 heart next infarct* in All Text #5 coronary next syndrome* in All Text #6 heart next attack* in All Text #7 coronary next thrombosis in All Text #8 (#1 or #2 or #3 or #4 or #5 or #6 or #7) #9 MeSH descriptor early ambulation this term only #10 MeSH descriptor Bed Rest this term only #11 bedrest in All Text #12 bed next rest in All Text #13 (confined in All Text near/3 bed in All Text) #14 bedbound in All Text #15 (early in All Text near/3 ambulat* in All Text) #16 (early in All Text near/3 activi* in All Text) #17 (early in All Text near/3 mobili* in All Text) #18 immobili* in All Text #19 (#9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18) #20 (#8 and #19)
MEDLINE on Ovid
1 exp Myocardial Infarction/ 2 exp Myocardial Ischemia/ 3 ami.tw. 4 mi.tw. 5 myocardial infarct$.tw. 6 acute heart infarction.tw. 7 coronary thrombos$.tw. 8 myomala$.tw. 9 acute coronary syndrome$.tw. 10 heart attack$.tw. 11 myocardial isch$.tw. 12 post‐infarction.tw. 13 or/1‐12 14 Early Ambulation/ 15 Bed Rest/ 16 bed rest.tw. 17 bed‐rest.tw. 18 bedrest.tw. 19 confined to bed.tw. 20 bedbound.tw. 21 (early adj3 ambulat$).tw. 22 (early adj3 discharge$).tw. 23 (early adj3 activit$).tw. 24 (early adj3 mobili$).tw. 25 immobili$.tw. 26 recumb$.tw. 27 or/14‐26 28 13 and 27 29 randomized controlled trial.pt. 30 controlled clinical trial.pt. 31 Randomized controlled trials/ 32 random allocation/ 33 double blind method/ 34 single‐blind method/ 35 or/29‐34 36 exp animal/ not humans/ 37 35 not 36 38 clinical trial.pt. 39 exp Clinical Trials as Topic/ 40 (clin$ adj25 trial$).ti,ab. 41 ((singl$ or doubl$ or trebl$ or tripl$) adj (blind$ or mask$)).ti,ab. 42 placebos/ 43 placebo$.ti,ab. 44 random$.ti,ab. 45 research design/ 46 or/38‐45 47 46 not 36 48 37 or 47 49 28 and 48
EMBASE on Ovid <to 2009 Week 40>
1 exp Heart Infarction/ 2 ami.tw. 3 mi.tw. 4 myocardial infarct$.tw. 5 acute heart infarction.tw. 6 coronary thrombos$.tw. 7 myomala$.tw. 8 acute coronary syndrome$.tw. 9 heart attack$.tw. 10 myocardial isch$.tw. 11 post‐infarction.tw. 12 or/1‐11 13 Bed Rest/ 14 bed rest.tw. 15 bed‐rest.tw. 16 bedrest.tw. 17 confined to bed.tw. 18 bedbound.tw. 19 (early adj3 ambulat$).tw. 20 (early adj3 discharge$).tw. 21 (early adj3 activit$).tw. 22 (early adj3 mobili$).tw. 23 immobili$.tw. 24 recumb$.tw. 25 or/13‐24 26 12 and 25 27 controlled clinical trial/ 28 random$.tw. 29 randomized controlled trial/ 30 follow‐up.tw. 31 double blind procedure/ 32 placebo$.tw. 33 placebo/ 34 factorial$.ti,ab. 35 (crossover$ or cross‐over$).ti,ab. 36 (double$ adj blind$).ti,ab. 37 (singl$ adj blind$).ti,ab. 38 assign$.ti,ab. 39 allocat$.ti,ab. 40 volunteer$.ti,ab. 41 Crossover Procedure/ 42 Single Blind Procedure/ 43 or/27‐42 44 (exp animals/ or nonhuman/) not human/ 45 43 not 44 46 45 and 26
PsycINFO on Ovid <1987 to October Week 1 2009>
1 Myocardial Infarctions/ 2 coronary thromboses/ 3 ami.tw. 4 mi.tw. 5 myocardial infarct$.tw. 6 heart infarction.tw. 7 coronary thrombos$.tw. 8 myomala$.tw. 9 coronary syndrome$.tw. 10 heart attack$.tw. 11 post‐infarction.tw. 12 or/1‐11 13 bed rest.tw. 14 bed‐rest.tw. 15 bedrest.tw. 16 confined to bed.tw. 17 bedbound.tw. 18 (early adj3 ambulat$).tw. 19 (early adj3 discharge$).tw. 20 (early adj3 activit$).tw. 21 (early adj3 mobili$).tw. 22 immobili$.tw. 23 or/13‐22 24 23 and 12 25 limit 24 to yr="2005 ‐ 2009" 26 limit 25 to human (5)
BIOSIS on ISI Web of Knowledge
#5 and #6 Databases=PREVIEWS Timespan=2005‐2009 # 6 >TA=human Databases=PREVIEWS Timespan=2005‐2009 # 5 #1 and #2 and #4 Databases=PREVIEWS Timespan=2005‐2009 # 4 TS=(randomi* or trial or control* or groups or blind*) Databases=PREVIEWS Timespan=2005‐2009 # 3 #1 and #2 Databases=PREVIEWS Timespan=2005‐2009 # 2 TS=(myocardial infarct* or heart infarct* or coronary thrombosis or coronary syndrome or heart attack or post‐infarction or AMI) Databases=PREVIEWS Timespan=2005‐2009 # 1 TS=(bedrest or bed rest or early mobili* or immobili* or early ambulation) Databases=PREVIEWS Timespan=2005‐2009
Appendix 2. Search Strategies 2005
CENTRAL
#1 MI or AMI #2 MYOCARDIAL INFARCT* #3 ACUTE HEART INFARCTION #4 CORONARY THROMBOS* #5 MYOMALA* #6 ACUTE CORONARY SYNDROM* #7 HEART ATTACK* #8 MYOCARDIAL ISCH* #9 (((((((#1 or #2) or #3) or #4) or #5) or #6) or #7) or #8) #10 EARLY‐AMBULATION*:ME #11 BED REST #12 BEDREST #13 BED‐REST #14 (CONFINED near BED) #15 BEDBOUND #16 (EARLY near AMBULAT*) #17 (EARLY near ACTIVIT*) #18 (EARLY near DISCHARGE) #19 (EARLY near MOBILI*) #20 IMMOBILI* #21 ((((((((((#10 or #11) or #12) or #13) or #14) or #15) or #16) or #17) or #18) or #19) or #20) #22 (#9 and #21)
MEDLINE (SIlver Platter)
1 exp Myocardial Infarction/ (MeSH) 2 exp Myocardial Ischemia/ (MeSH) 3 ami 4 mi 5 myocardial infarct* 6 acute heart infarction 7 coronary thrombos* 8 myomala* 9 acute coronary syndrome* 10 heart attack* 11 myocardial isch* 12 post‐infarction 13 or/ 1‐12 14 Early Ambulation/ (MeSH) 15 Bed Rest/ (MeSH) 16 bed rest 17 bed‐rest 18 bedrest 19 confined to bed 20 bedbound 21 (early near ambulat*) 22 (early near discharge*) 23 (early activit*) 24 (early near mobili*) 25 immobili* 26 recumb* 27 or/ 14‐26 28 13 and 27
EMBASE (Silver Platter)
1 exp Heart Infarction/ (Thesaurus) 2 ami 3 mi 4 myocardial infarct* 5 acute heart infarction 6 coronary thrombos* 7 myomala* 8 acute coronary syndrome* 9 heart attack* 10 myocardial isch* 11 post‐infarction 12 or/1‐11 13 Bed Rest/ (Thesaurus) 14 bed rest 15 bed‐rest 16 bedrest 17 confined to bed 18 bedbound 19 (early near ambulat*) 20 (early near discharge*) 21 (early activit*) 22 (early near mobili*) 23 immobili* 24 recumb* 25 or/13‐24 26 12 and 25
PsycINFO (Silver Platter)
1 Coronary thromboses (Thesaurus) 2 Myocardial infarctions (Thesaurus) 3 AMI 4 MI 5 Post‐infarction 6 Myocardial infarct* 7 Acute heart infarction* 8 Coronary thrombos* 9 Myomala* 10 Acute coronary syndro* 11 Heart attack 12 Myocardial isch* 13 (#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13) 14 bed‐rest 15 bed rest 16 bedrest 17 early near ambulat* 18 confined to bed 19 bedbound 20 early activity 21 early near discharge* 22 early near mobili* 23 immobili* 24 recumb* 25 (#14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24) 26 (#13 and #25) No RCT filter used.
PASCAL Biomed and BIOSIS
1 AMI 2 MI 3 Myocardial infarct* 4 Acute heart infarction 5 Coronary thrombos* 6 Myomala* 7 Acute coronary syndro* 8 Heart attack 9 Myocardial isch* 10 Post‐infarction 11 (#1 OR #2 OR #3 OR #4 OR #5 OR#6 OR #7 OR #8 OR #8 OR#9 OR #10) 12 bed rest 13 bedrest 14 bed‐rest 15 confined to bed 16 bedbound 17 early ambulation 18 early activity 19 early discharge 20 early mobili* 21 immobili* 22 recumb* 23 (#12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22) 24 PLACEBO* 25 randomi* 26 trial* 27 control* 28 compar* 29 blind* 30 clinic* 31 study 32 (#24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31) 33 #11 AND #23 AND #32
Data and analyses
Comparison 1. Mortality.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 mortality | 13 | 2797 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.68, 1.07] |
| 2 Cardiac death | 3 | 943 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.54, 1.19] |
Comparison 2. Reinfarction.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Reinfarction | 11 | 2509 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.79, 1.44] |
Comparison 3. Arrhythmia.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Arrhythmia | 7 | 1636 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.49, 1.24] |
Comparison 4. Thromboembolic complications.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Thromboembolic complications | 6 | 811 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.65 [0.39, 1.08] |
Comparison 5. Cardiac wall rupture/ aneurysm.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Cardiac wall rupture/ aneurysm | 1 | 199 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.46 [0.34, 6.35] |
Comparison 6. Duration of hospital stay.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Duration of hospital stay | 10 | 2410 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
Comparison 7. Sensitivity analysis.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Mortality | 13 | 2797 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.67, 1.07] |
| 1.1 Allocation concealment A and B | 8 | 1472 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.56, 1.09] |
| 1.2 Allocation concealment C | 5 | 1325 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.66, 1.28] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Abraham 1975.
| Methods | Allocation: admission rotation Blinding: not stated Intention‐to treat: not stated | |
| Participants | 61 vs 62 years of age, 25 vs 26% female, community hospital | |
| Interventions | 5 days vs 12 days | |
| Outcomes | 52 weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Ahlmark 1979.
| Methods | Allocation:random Blinding: not stated Intention‐to treat: no | |
| Participants | 61 vs 62 years of age, 24 vs 18% female, community hospital | |
| Interventions | 6 days vs 12 days | |
| Outcomes | 3 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Beckwith 1954.
| Methods | Allocation:alternate patients Blinding: not stated Intention‐to treat: not stated | |
| Participants | 65 vs 65 years old, university hospital | |
| Interventions | 2‐5 days vs 28 days | |
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Bloch 1974.
| Methods | Allocation: random table Blinding: not stated Intention‐to treat: not stated | |
| Participants | 58 vs 58 years of age, 17 vs 16% female, university hospital | |
| Interventions | 8 days vs 21 days | |
| Outcomes | After hospital discharge | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Greco 1976.
| Methods | Allocation:random Blinding: not stated Intention‐to treat: not stated | |
| Participants | 58 vs 58 years of age, 7 vs 10% female, community hospital | |
| Interventions | 6 days vs 13 days | |
| Outcomes | 2.7 years | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Harpur 1971.
| Methods | Allocation: hospital rotation Blinding: not stated Intention‐to treat: not stated | |
| Participants | 60 vs 60 years of age, 13 vs 14% female, university hospital | |
| Interventions | 7 days vs 21 days | |
| Outcomes | 8 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Hayes 1974.
| Methods | Allocation: ward rotation Blinding: not stated Intention‐to treat: not stated | |
| Participants | 56 vs 56 years of age, 13 vs 18% female, community hospital | |
| Interventions | 2 days vs 9 days | |
| Outcomes | 6 weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Hayes 1976.
| Methods | Allocation: ward rotation Blinding: not stated Intention‐to treat: not stated | |
| Participants | 56 vs 55 years of age, 12 vs 15% female, community hospital | |
| Interventions | 2 days vs 9 days | |
| Outcomes | 12 days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Hutter 1973.
| Methods | Allocation: stratified randomisation Blinding: yes Intention‐to treat: yes | |
| Participants | 60 vs 60 years of age, 25 vs 28% female, university hospital | |
| Interventions | 9 days vs 12 days | |
| Outcomes | 24 weeks | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Messin 1982.
| Methods | Allocation: random Blinding: not stated Intention‐to treat: not stated | |
| Participants | 55 vs 55 years of age, no female, university hospital | |
| Interventions | 4 days vs 7 days | |
| Outcomes | 2 years | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Miller 1976.
| Methods | Allocation: every 3rd patient Blinding: not stated Intention‐to treat: not stated | |
| Participants | 54 vs 54 years of age, university hospital | |
| Interventions | 1‐3 days vs 5 days | |
| Outcomes | 9 days | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
Rowe 1989.
| Methods | Allocation: random Blinding: unclear Intention‐to treat: unclear | |
| Participants | 55 vs 57 years of age, 7 vs 10% female, community hospital | |
| Interventions | 4 days vs 7 days | |
| Outcomes | 3 months | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Royal Infirmary 1973.
| Methods | Allocation: balanced randomisation Blinding: not stated Intention‐to treat: not stated | |
| Participants | 54 vs 52 years of age, 18 vs 26% female, community hospital | |
| Interventions | 6 days vs 20 days | |
| Outcomes | 1 year | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Unclear risk | B ‐ Unclear |
Schaumann 1977.
| Methods | Allocation: random; sealed envelope Blinding: not stated Intention‐to treat: not stated | |
| Participants | 65 vs 65 years old, 31 vs 20% female, university hospital | |
| Interventions | 6 days vs 20 days | |
| Outcomes | In hospital | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | Low risk | A ‐ Adequate |
West 1979.
| Methods | Allocation: open random list Blinding: not stated Intention‐to treat: not stated | |
| Participants | 60 vs 60 years of age, 18 vs 20% female, multicentre | |
| Interventions | 4 days vs 9 days | |
| Outcomes | 1 year | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment (selection bias) | High risk | C ‐ Inadequate |
vs: versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Armstrong 1999 | Other invervention than length of bed rest, only abstract available |
| Bloch 1973 | Other invervention than length of bed rest |
| Chaturvedi 1974 | Other invervention than length of bed rest |
| Costanza 1981 | Other invervention than length of bed rest |
| DeBusk 1982 | Other invervention than length of bed rest |
| Fareeduddin 1969 | Did not report any of the predefined endpoints, only physiologic measurements |
| Gelson 1976 | Other invervention than length of bed rest |
| Gembitskii 1983 | A controlled study but not explicitly stated that random allocation was used |
| Haviar 1968 | Other invervention than length of bed rest |
| Hill 1978 | Other invervention than length of bed rest |
| Krasemann 1979 | Other invervention than length of bed rest |
| Lamers 1973 | A controlled study but not explicitly stated that random allocation was used |
| Lau 1980 | Other invervention than length of bed rest |
| Mather 1976 | Other invervention than length of bed rest |
| McNeer 1978 | Other invervention than length of bed rest |
| Newby 1996 | Other invervention than length of bed rest |
| Newby 2000 | Other invervention than length of bed rest |
| Pfisterer 1977 | Other invervention than length of bed rest |
| Rechnitzer 1972 | Other invervention than length of bed rest |
| Senaratne 1999 | Other invervention than length of bed rest |
| Simon 1974 | Other invervention than length of bed rest |
| Stegaru 1974 | Before and after design study |
| Stegaru 1976 | None of the predefined endpoints reported, physiologic measurements only |
| van der Vlugt 2000 | Other invervention than length of bed rest |
| Zdichynec 1977 | A controlled study but not explicitly stated that random allocation was used |
Differences between protocol and review
The search in 2009 did not include PASCAL Biomed as we did not have access to this database.
Contributions of authors
The main responsibilities were as follows: Development of the protocol: HH and MM Searching the literature: HH, CH and JA Data extraction: JA and CH Writing and reviewing and approving the manuscript: HH, MM, CH and JA
HH acts as the guarantor of the manuscript
Sources of support
Internal sources
Medical University of Vienna, Austria.
External sources
No sources of support supplied
Declarations of interest
None known
Stable (no update expected for reasons given in 'What's new')
References
References to studies included in this review
Abraham 1975 {published data only}
- Abraham AS, Sever Y, Weinstein M, Dollberg M, Menczel J. Value of early ambulation in patients with and without complications after acute myocardial infarction. New England Journal of Medicine 1975;292:719‐22. [DOI] [PubMed] [Google Scholar]
Ahlmark 1979 {published data only}
- Ahlmark G, Ahlberg G, Saetre H, Haglund I, Korsgren M. A controlled study of early discharge after uncomplicated myocardial infarction. Acta Medica Scandinavica 1979;206:87‐91. [DOI] [PubMed] [Google Scholar]
Beckwith 1954 {published data only}
- Beckwith JR, Kernodle DT, LeHew AE, Wood JE. The management of myocardial infarction with particular reference to the chair treatment. Annals of Internal Medicine 1954;41:1189‐95. [DOI] [PubMed] [Google Scholar]
Bloch 1974 {published data only}
- Bloch A, Maeder JP, Haissly JC, Felix J, Blackburn H. Early mobilization after myocardial infarction. A controlled study. American Journal of Cardiology 1974;34:152‐7. [DOI] [PubMed] [Google Scholar]
Greco 1976 {published data only}
- Greco R, Musto B, Boccalatte A, Marsico F. Early mobilization in myocardial infarct [Mobilizzazione precoce nell'infarto del miocardio.]. Bollettino della Societa Italiana di Cardiologia 1976;21:161‐8. [PubMed] [Google Scholar]
Harpur 1971 {published data only}
- Harpur JE, Conner WT, Hamilton M, Kellett RJ, Galbraith HJ, Murray JJ, et al. Controlled trial of early mobilisation and discharge from hospital in uncomplicated myocardial infarction. Lancet 1971;2:1331‐4. [DOI] [PubMed] [Google Scholar]
Hayes 1974 {published data only}
- Hayes MJ, Morris GK, Hampton JR. Comparison of mobilization after two and nine days in uncomplicated myocardial infarction. British Medical Journal 1974;2:10‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hayes 1976 {published data only}
- Hayes MJ, Morris GK, Hampton JR. Lack of effect of bed rest and cigarette smoking on development of deep venous thrombosis after myocardial infarction. British Heart Journal 1976;38:981‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hutter 1973 {published data only}
- Baughman KL, Hutter AM, DeSanctis RW, Kallman CH. Early discharge following acute myocardial infarction. Archives of Internal Medicine 1982;142:875‐78. [PubMed] [Google Scholar]
- Hutter AM, Sidel VW, Shine KI, DeSanctis RW. Early hospital discharge after myocardial infarction. New England Journal of Medicine 1973;288:1141‐4. [DOI] [PubMed] [Google Scholar]
Messin 1982 {published data only}
- Messin R, Demaret B. Accelerated versus classical early mobilization after myocardial infarction. Advances in Cardiology 1982;31:152‐5. [DOI] [PubMed] [Google Scholar]
Miller 1976 {published data only}
- Miller RR, Lies JE, Carretta RF, Wampold DB, DeNardo GL, Kraus JF, et al. Prevention of lower extremity venous thrombosis by early mobilization. Confirmation in patients with acute myocardial infarction by 125I‐fibrinogen uptake and venography. Annals of Internal Medicine 1976;84:700‐3. [DOI] [PubMed] [Google Scholar]
Rowe 1989 {published data only}
- Rowe MH, Jelinek MV, Liddell N, Hugens M. Effect of rapid mobilization on ejection fractions and ventricular volumes after acute myocardial infarction. American Journal of Cardiology 1989;63:1037‐41. [DOI] [PubMed] [Google Scholar]
Royal Infirmary 1973 {published data only}
- Medical Division, Royal Infirmary, Glasgow. Early mobilisation after uncomplicated myocardial infarction. Prospective study of 538 patients. Lancet 1973;2(7825):346‐9. [PubMed] [Google Scholar]
Schaumann 1977 {published data only}
- Schaumann HJ, Stegaru B, Neuss H, Scheurlen H. A controlled clinical study of early mobilisation of patients with myocardial infarction [Eine kontrollierte klinische Studie uber die Fruhmobilisation von Infarktpatienten. Teil 1: Die klinische Behandlungsphase]. Medizinische Klinik 1977;72:465‐70. [PubMed] [Google Scholar]
West 1979 {published data only}
- West RR, Henderson AH. Long term survival of patients mobilised early after acute myocardial infarction. British Heart Journal 1985;53:243‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West RR, Henderson AH. Randomised multicentre trial of early mobilisation after uncomplicated myocardial infarction. British Heart Journal 1979;42:381‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Armstrong 1999 {published data only}
- Armstrong PW, Fu Y, Chang CW, Kaul P, Granger CB, Ohman EM. Increased early discharge does not compromise mortality: Insights from GUSTO I and GUSTO III. Circulation 1999;100(18):I‐499. [Google Scholar]
Bloch 1973 {published data only}
- Bloch A, Maeder JF, Maeder JP. Early mobilization in the acute phase of myocardial infarct [Mobilisation précoce à la phase aiguë de l'infarctus du myocarde]. Schweizerische Medizinische Wochenschrift 1973;103:1817‐1818. [PubMed] [Google Scholar]
Chaturvedi 1974 {published data only}
- Chaturvedi NC, Walsh MJ, Evans A, Munro P, Boyle DM, Barber JM. Selection of patients for early discharge after acute myocardial infarction. British Heart Journal 1974;36:533‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Costanza 1981 {published data only}
- Costanza G, Centamore GM, Chiaranda G, Dammino MG, Caro R, Ferrante A, et al. Early ambulation in acute myocardial infarct as the 1st phase of cardiological rehabilitation [La mobilizzazione precoce nell'infarto miocardico acuto come prima fase della riabilitazione cardiologica]. Bollettino della Societa Italiana di Cardiologia 1981;26(12):2293‐6. [PubMed] [Google Scholar]
DeBusk 1982 {published data only}
- DeBusk, R. Physical Conditioning following Myocardial Infarction. Advances in Cardiology 1982;31:156‐161. [DOI] [PubMed] [Google Scholar]
Fareeduddin 1969 {published data only}
- Fareeduddin K, Abelmann WH. Impaired orhtostatic tolerance after bed rest in patients with myocardial infarction. New England Journal of Medicine 1969;280(7):345‐50. [DOI] [PubMed] [Google Scholar]
Gelson 1976 {published data only}
- Gelson AD, Carson PH, Tucker HH, Phillips R, Clarke M, Oakley GD. Course of patients discharged early after myocardial infarction. British Medical Journal 1976;1(6025):1555‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gembitskii 1983 {published data only}
- Gembitskii EV, Koniaev BV, Karacharov AT, Lindo GV, Virs EA. Various aspects of rehabilitation of patients with myocardial infarct at the hospital stage [Nekotorye aspekty reabilitatsii bol'nykh infarktom miokarda na gospital'nom etape]. Kardiologiia 1983;23(9):72‐5. [PubMed] [Google Scholar]
Haviar 1968 {published data only}
- Haviar V, Mayer R. Is a prolonged bedrest in the treatment of myocardial infarct necessary? [Ist eine langwierige Bettruhe bei der Behandlung des Herzinfarktes notwendig?]. Verhandlungen der Deutschen Gesellschaft fur Kreislaufforschung 1968;34:367‐71. [PubMed] [Google Scholar]
Hill 1978 {published data only}
- Hill JD, Hampton JR, Mitchell JRA. A randomised trial of home‐versus‐hospital management for patients with suspected myocardial infarction. Lancet 1978;1(8069):837‐41. [DOI] [PubMed] [Google Scholar]
Krasemann 1979 {published data only}
- Krasemann EO, Jungmann H. Return to work after myocardial infarction. Cardiology 1979;64(3):190‐6. [DOI] [PubMed] [Google Scholar]
Lamers 1973 {published data only}
- Lamers HJ, Drost WS, Kroon BJ, Es LA, Meilink‐Hoedemaker LJ, Birkenhager WH. Early mobilization after myocardial infarction: a controlled study. British Medical Journal 1973;1(5848):257‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lau 1980 {published data only}
- Lau YK, Smith J, Morrison SL, Chamberlain DA. Policy for early discharge after acute myocardial infarction. British Medical Journal 1980;280(6230):1489‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mather 1976 {published data only}
- Mather HG, Morgan DC, Pearson NG, Read KL, Shaw DB, Steed GR, et al. Myocardial infarction: a comparison between home and hospital care for patients. British Medical Journal 1976;1(6015):925‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
McNeer 1978 {published data only}
- McNeer JF, Wagner GS, Ginsburg PB, Wallace AG, McCants CB, Conley MJ, et al. Hospital discharge one week after acute myocardial infarction. New England Journal of Medicine 1978;298(5):229‐32. [DOI] [PubMed] [Google Scholar]
Newby 1996 {published data only}
- Newby LK, Califf RM, Guerci A, Weaver WD, Col J, Horgan JH, et al. Early discharge in the thrombolytic era: an analysis of criteria for uncomplicated infarction from the Global Utilization of Streptokinase and t‐PA for Occluded Coronary Arteries (GUSTO) trial. Journal of the American College of Cardiology 1996;27(3):625‐32. [DOI] [PubMed] [Google Scholar]
Newby 2000 {published data only}
- Newby LK, Eisenstein EL, Califf RM, Thompson TD, Nelson CL, Peterson ED, et al. Cost effectiveness of early discharge after uncomplicated acute myocardial infarction. New England Journal of Medicine 2000;342(11):749‐55. [DOI] [PubMed] [Google Scholar]
Pfisterer 1977 {published data only}
- Pfisterer M, Schweizer W, Burkart F. Early mobilisation after myocardial infarction. A prospective and controlled study [Fruh‐Mobilisation nach Myokardinfarkt ‐ eine prospektive, kontrollierte Studie]. Zeitschrift fur Kardiologie 1977;66(1):15‐8. [PubMed] [Google Scholar]
Rechnitzer 1972 {published data only}
- Rechnitzer PA, Pickard HA, Paivio AU, Yuhasz MS, Cunningham D. Long‐term follow‐up study of survival and recurrence rates following myocardial infarction in exercising and control subjects. Circulation 1972;45(4):853‐7. [DOI] [PubMed] [Google Scholar]
Senaratne 1999 {published data only}
- Senaratne MP, Irwin ME, Shaben S, Griffiths J, Nagendran J, Kasza L, et al. Feasibility of direct discharge from the coronary/intermediate care unit after acute myocardial infarction. Journal of the American College of Cardiology 1999;33(4):1040‐6. [DOI] [PubMed] [Google Scholar]
Simon 1974 {published data only}
- Simon H, Huszar S, Fricke G, Kikis D. Frühmobilisation und Rehabilitation von Infarktpatienten. Therapiewoche 1974;14:1492‐7. [Google Scholar]
Stegaru 1974 {published data only}
- Stegaru B, Schaumann HJ, Kollmeier W. Hemodynamic and metabolic studies in patients with recent myocardial infarct prior to and following early mobilization [Hämodynamische und metabolische Unersuchungen bei Patienten mit frischem Herzinfarkt vor und nach Frühmobilisation]. Verhandlungen der Deutschen Gesellschaft fur Innere Medizin 1974;80:1051‐4. [PubMed] [Google Scholar]
Stegaru 1976 {published data only}
- Stegaru B, Schaumann HJ, Kollmeier W, Neuss H. Early mobilization after myocardial infarction. Hemodynamic and metabolic studies [Fruhmobilisation nach Herzinfarkt. Hamodynamische und metabolische Untersuchugen]. Medizinische Klinik 1976;71(14):573‐9. [PubMed] [Google Scholar]
van der Vlugt 2000 {published data only}
- Vlugt MJ, Boersma H, Leenders CM, Pop GA, Veerhoek MJ, Simoons ML, et al. Prospective study of early discharge after acute myocardial infarction (SHORT). European Heart Journal 2000;21(12):992‐9. [DOI] [PubMed] [Google Scholar]
Zdichynec 1977 {published data only}
- Zdichynec B. Experiences with the early mobilisation of elderly patients with myocardial infarction [Erfahrungen mit der Fruhmobilisation des Herzinfarktes im hohen Alter]. Rehabilitation (Stuttgart) 1977;16(3):157‐61. [PubMed] [Google Scholar]
Additional references
ACC/AHA 2004
- Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, et al. ACC/AHA Guidelines for the Management of Patients With ST‐Elevation Myocardial Infarction. Circulation 2004;110:e82‐292. [PubMed] [Google Scholar]
AHA 2001
- American Heart Association. 2002 Heart and Stroke Statistical Update. Dallas, Texas: American Heart Association, 2001. [Google Scholar]
Allen 1999
- Allen, C, Glasziou P, Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet 1999;354:1229‐33. [DOI] [PubMed] [Google Scholar]
Begg 1996
- Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, et al. Improving the quality of reporting of randomized controlled trials. JAMA 1996;276:637‐9. [DOI] [PubMed] [Google Scholar]
Bloch 1978
- Bloch A, Meader JP. [Mobilisation précoce après infarctus du myocarde]. Schweizerische Zeitschrift für Sportmedizin 1978;26(1):27‐36. [PubMed] [Google Scholar]
Cochrane 1981
- Cochrane AL. Acute myocardial infarction: place of treatment and length of stay. Herz 1981;6:112‐5. [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta‐analysis in clinical trials. Controlled Clinical Trials 1986;7:177‐88. [DOI] [PubMed] [Google Scholar]
Dickersin 1994
- Dickersin K, Scherer R, Lefebvre C. Identifying relevant studies for systematic reviews. British Medical Journal 1994;309:1286‐91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Smith GD, Schneider M, Minder C. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315:629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
ESC 2003
- Werf F, Ardissino D, Betriu A, Cokkinos DV, Falk E, Fox KA, et al. Management of acute myocardial infarction in patients presenting with ST‐segment elevation. The Task Force on the Management of Acute Myocardial Infarction of the European Society of Cardiology. European Heart Journal 2003;24:28‐66. [DOI] [PubMed] [Google Scholar]
GUSTO III
- The GUSTO III Investigators. A comparison of reteplase with alteplase for acute myocardial infarction. New England Journal of Medicine 1997;337:1118‐23. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐560. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jüni 1999
- Jüni P, Witschi A, Bloch R, Egger M. The hazards of scoring the quality of clinical trials for meta analysis. JAMA 1999;282:1054‐60. [DOI] [PubMed] [Google Scholar]
Lefebvre 1996
- Lefebvre C, McDonald S. Development of a sensitive search strategy for reports of randomised controlled trials in EMBASE. Paper presented at the Fourth International Cochrane Colloquium 20 ‐24 Oct ; Adelaide, Australia 1996.
Levine 1952
- Levine SA, Lown B. "Armchair" treatment of acute coronary thrombosis. JAMA 1952;148:1365. [DOI] [PubMed] [Google Scholar]
Mantel Haenszel 1959
- Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. Journal of the National Cancer Institute 1959;22:719‐748. [PubMed] [Google Scholar]
Maurere 1971
- Maurere BJ, Wray R, Shillingford JP. Frequency of venous thrombosis after myocardial infarction. Lancet 1971;2(7739):1385‐87. [DOI] [PubMed] [Google Scholar]
McGovern 1996
- McGovern PG, Pankow JS, Shahar E, Doliszny KM, Folsom AR, Blackburn H, et al. Recent trends in acute coronary heart disease‐‐mortality, morbidity, medical care, and risk factors. The Minnesota Heart Survey Investigators. New England Journal of Medicine 1996;334:884‐90. [DOI] [PubMed] [Google Scholar]
Moher 1995
- Moher D, Jadad AR, Nichol G, Penman M, Tugwell P, Walsh S. Assessing the Quality of randomized controlledf trials: an annotated bibliography of scales and checklists. Controlled Clinical Trials 1995;16:62‐73. [DOI] [PubMed] [Google Scholar]
Moher 1999
- Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reporting of reports of meta‐analyses of randomised controlled trials: the QUOROM statement. Lancet 1999;34:1896‐1900. [DOI] [PubMed] [Google Scholar]
Schulz 1995
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
Spracklen 1968
- Spracklen FH, Besterman EM, Everest MS, Litchfield JW, Petrie M. Late ventricular dysrhythmias after myocardial infarction. British Medical Journal 1968;4(5627):364‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wenger 1978
- Wenger NK. The physiologic basis for early ambulation after myocardial infarction. Cardiovascular Clinics 1978;9(3):107‐15. [PubMed] [Google Scholar]
References to other published versions of this review
Herkner 2003
- Herkner H, Thoennissen J, Nikfadjam M, Laggner AN, Müllner M. Short versus prolonged bed rest after uncomplicated acute myocardial infarction: a systematic review and meta‐analysis. J Clin Epidemiol 2003;56:775‐81. [DOI] [PubMed] [Google Scholar]


