Abstract
Background
Numerous different implants with screws, pins and side plates have been used for the internal fixation of intracapsular hip fractures.
Objectives
To determine from randomised trials which implant is superior for the internal fixation of intracapsular proximal femoral fractures.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (13 September 2010), the Cochrane Central Register of Controlled Trials (The Cochrane Library 2010, Issue 3), MEDLINE (1950 to August week 5, 2010), EMBASE (1980 to 2010 Week 36), and other sources.
Selection criteria
Randomised and quasi‐randomised trials comparing different implants for the internal fixation of intracapsular hip fractures in adults.
Data collection and analysis
Two review authors independently assessed trial quality, by use of an 11 item scale, risk of bias relating to sequence generation and allocation concealment, and extracted data. Additional information was sought from trialists. After grouping by implant type, comparable groups of trials were subgrouped and where appropriate, data were pooled using the fixed‐effect model or, where there was significant heterogeneity, the random‐effects model.
Main results
There are now 30 studies involving 6334 participants (6339 fractures) included in this review, which was published in 2011. There was considerable variation in the quality of trial methodology and generally inadequate reporting of methods and trial findings. Allocation concealment was confirmed in one trial only. The main outcome measures reported were fracture healing complications, re‐operations and mortality. The reporting of functional outcomes was particularly poor.
Few trials tested the same comparison. Most of the results for the 25 separate comparisons, frequently tested within one trial only, showed no statistically significant differences between the two implants under test. It was noted that the more rare findings of favourable results were often for implants developed within the same institutions as the trial. There was a consistent finding of less avascular necrosis with the sliding hip screw in comparison with five different types of cancellous screws but there was no significant difference found for re‐operations. Additionally, the sliding hip screw was found to take longer to insert and to have an increased operative blood loss compared with multiple screws or pins.
Authors' conclusions
No clear conclusions can be made on the choice of implant for internal fixation of intracapsular fractures from the available evidence within randomised trials.
Plain language summary
Different implants used to fix certain types of hip fractures
Many different types of implants are used to fix fractures of the hip, which are close to the hip joint (intracapsular fractures). Implants are used to stabilise the bone during healing thereby reducing the chance of the bones slipping out of line. They consist of either screws or pins and may have an additional side plate attached, which is fixed to the bone.
This review of randomised controlled trials included 30 studies involving more than 6000 participants. Most of the trials were poorly reported and had flaws in their methods that could have affected their results. Few trials tested the same comparison. Most of the results for the 25 separate comparisons, frequently tested within one trial only, failed to show that one implant was better than the other under comparison. There was a consistent finding of one serious complication (avascular necrosis) with the sliding hip screw in comparison with five different types of cancellous screws. However, this was not reflected in a decrease in re‐operations for this group. Additionally, the sliding hip screw was found to take longer to insert and to have an increased operative blood loss compared with multiple screws or pins.
This review found no evidence from trials undertaken so far that there were any major differences between different implants in patient survival or complications related to the operation.
Background
Proximal femoral fractures or, as they are more generally termed, 'hip fractures', can be subdivided into intracapsular fractures (those occurring proximal to the attachment of the hip joint capsule to the femur) and extracapsular (those occurring distal to the hip joint capsule). Intracapsular fractures can be further subdivided into those which are displaced and those which are essentially undisplaced. Undisplaced fractures include those termed impacted or adduction fractures. Many other subdivisions and classification methods exist for intracapsular fractures but these have not been shown to be of reliable clinical usefulness (Parker 1993).
Intracapsular hip fractures are generally managed surgically, either by fixing the fracture using various implants and thereby retaining the femoral head, or by replacing the femoral head with a prosthesis. The latter option is not considered in this review. The rationale for operative treatment of intracapsular fractures is to reduce the risk of the fracture displacing, for undisplaced fractures, and to maintain fracture reduction for displaced fractures. Surgery entails passing single or multiple screws or pins across the fracture site. For displaced fractures the fracture must first be reduced, which may be achieved either by an open or closed reduction.
Numerous implants have been developed over time for the internal fixation of the fracture. Tronzo identified over 100 in 1974 (Tronzo 1974). These implants are inserted under X‐ray guidance using either an open or percutaneous procedure. Implants may be divided into those which are smooth (pins) and those which are threaded (screws). The type of threads used on screws may vary from narrow to wide and deep. In addition, the proportion of the screw which is threaded may vary from the tip only to the entire length. The number of pins or screws inserted across the fracture can vary from one to in excess of 10, depending on the size of the implant used. Screws or pins may also be connected to a side plate which is then fixed with screws to the side of the femur. Another variation on implant design is a small metal 'tongue' which is pushed out of the tip of a nail into the subchondral bone of the femur.
Examples of single nails are the Smith‐Petersen nail, Thornton nail and Rydell four‐flanged nail. Examples of a single nail with a side plate are the Holt, Jewett nail plate, Massie nail, McLaughlin nail plate, Pugh nail and Thornton nail plate. Of these implants, the Massie and Pugh nails have the capacity for sliding at the nail/plate junction, allowing for collapse at the fracture site. Examples of a single screw with a side plate are the sliding hip screw (SHS) and equivalent models such as the Ambi, Dynamic, or Richards' screws. These implants all have the capacity for sliding at the screw/plate junction.
Examples of implants with a 'tongue', which can be extruded from its tip, are the Rydell four‐flanged nail and Hansson pins. Examples of implants that are normally used in pairs are Garden screws, Hansson pins, Richards' screws, Tronzo (VLF) screws, Uppsala/Olmed screws, von Bahr screws, and Ullevaal screws. Examples of implants for which three are normally inserted are AO screws, Gouffon screws, Hessel pins, Mecron screws, Nystrom nails, Ullevaal screws and Scand screws.
The main fracture healing complication after internal fixation of an intracapsular fracture is the failure of the fracture to heal. This may lead to fracture displacement and is termed either 'early fracture displacement' or 'non‐union' if it occurs in the first few weeks after operation. The term 'non‐union' is also used for those fractures which fail to heal in later weeks. This normally results in the fracture displacing with loss of position of the fixation device. For this review the term non‐union refers to both those fractures which show early displacement plus those which later fail to heal. An incidence of non‐union of five to ten per cent can be expected following an undisplaced intracapsular fracture; this rises to about 20 to 40 per cent for displaced intracapsular fractures (Lu‐Yao 1994; Parker 1993).
The other main fracture healing complication is avascular necrosis (also termed segmental collapse or femoral head necrosis). This is seen as collapse of the femoral head and subsequent destruction of the hip joint. It occurs secondary to disruption of the blood supply to the femoral head. An incidence of 16 per cent for displaced intracapsular fractures has been reported (Lu‐Yao 1994).
Other fracture healing complications that may occur are backing out of the implant as the fracture collapses, fracture below or around the implant and breakage of the implant.
Objectives
To identify and summarise the evidence from randomised controlled trials of the effects of different implants for the internal fixation of intracapsular proximal femoral fractures.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials comparing alternative implants. Quasi‐randomised trials (for example, allocation by alternation or date of birth) and trials in which the treatment allocation was inadequately concealed were considered for inclusion. No language restriction was applied.
Types of participants
Skeletally mature patients with an intracapsular proximal femoral fracture.
Types of interventions
Implants used for internal fixation of an intracapsular proximal femoral fracture.
Types of outcome measures
The principal outcome measure was the non‐union rate which includes early displacement of the fracture. Data for the following outcomes were sought:
a) Operative details
length of surgery (in minutes)
operative blood loss (in millilitres)
number of patients transfused
post‐operative blood transfusion (in units)
radiographic screening time (in seconds)
b) Fracture fixation complications
non‐union of the fracture within the follow‐up period (the definition of non‐union will be that used within each individual study and this outcome will include early re‐displacement of the fracture).
avascular necrosis
fracture below the implant
other surgical complications of fixation (as detailed in each study)
total fracture fixation complications (sum of the four above outcomes)
re‐operation (within the follow‐up period of the study).
superficial wound infection (infection of the wound in which there is no evidence that the infection extends beneath the deep fascia to the site of the implant)
deep wound infection (infection around the implant)
wound haematoma
c) Post‐operative complications
pneumonia
thromboembolic complications (deep vein thrombosis or pulmonary embolism)
any medical complications (as detailed in each individual study)
length of hospital stay (in days)
d) Anatomical restoration
shortening (as defined in each study)
varus deformity (as defined in each study)
external rotation deformity (> 20 degrees)
e) Final outcome measures
mortality (within the follow‐up period of the study)
pain (persistent pain at the final follow‐up assessment)
residence at final follow‐up (return to living at home, discharge location)
mobility (use of walking aids, return of mobility)
regain of activities of daily living
health related quality of life measures
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (13 September 2010), the Cochrane Central Register of Controlled Trials (2010, Issue 3), MEDLINE (1950 to August week 5 2010) and EMBASE (1980 to 2010 Week 36). We searched the WHO International Clinical Trials Registry Platform Search Portal, Current Controlled Trials, and the UK National Research Register (NRR) Archive (all to April 2009) to identify ongoing and recently completed trials. No language or publication restrictions were applied.
The generic search strategies for hip fracture trials run in The Cochrane Library (Wiley Online Library) and MEDLINE (2002 onwards) are shown in Appendix 1. This MEDLINE search was combined with the sensitivity‐ and precision‐maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomized trials (Lefebvre 2009). The general search strategy for hip fracture trials in EMBASE (2002 onwards) is also shown in Appendix 1.
Searching other resources
We searched reference lists of articles and our own reference databases. We included the findings from handsearches of the British Volume of the Journal of Bone and Joint Surgery supplements (1996 to 2006), abstracts of the American Orthopaedic Trauma Association annual meetings (1996 to 2006) and American Academy of Orthopaedic Surgeons annual meetings (2004 to 2007). We also included handsearch results from the final programmes of SICOT (1996 and 1999) and SICOT/SIROT (2003), EFORT (2007) and the British Orthopaedic Association Congress (2000, 2001, 2002, 2003, 2005 and 2006). Up to 2007, we scrutinised weekly downloads of "Fracture" articles in new issues of Acta Orthopaedica Scandinavica (subsequently Acta Orthopaedica); American Journal of Orthopedics; Archives of Orthopaedic and Trauma Surgery; Clinical Orthopedics and Related Research; Injury; Journal of the American Academy of Orthopedic Surgeons; Journal of Arthroplasty; Journal of Bone and Joint Surgery (American and British Volumes); Journal of Orthopedic Trauma; Journal of Trauma; Orthopedics from AMEDEO.
Data collection and analysis
Selection of studies
Study selection was performed by one author.
Data extraction and management
Data for the outcomes listed above were independently extracted by both review authors using a data extraction form. Any differences were resolved by discussion.
Assessment of risk of bias in included studies
In the update of the review (2011), two aspects of risk of bias were assessed by one author (MJP) and reported. These were sequence generation and allocation concealment. In this assessment, incomplete or a lack of information on sequence generation or allocation concealment was judged as 'unclear' risk of bias unless the trial was quasi‐randomised, in which case both were rated 'no'.
We also independently assessed 11 aspects of methodological quality using a slightly modified scheme to that used in former versions of the review (seeTable 1). There was no masking of the study names or authors. Any differences were resolved by discussion.
1. Methodological quality assessment scheme.
| Items | Scores |
| 1. Was there an adequate method of sequence generation? | Score 1 if adequate method such as table of random numbers, shuffled envelopes, coin tossing. Score 0 if inadequate such as date of birth, patient registration number. |
| 2. Was there clear concealment of allocation? | Score 1 if adequate such as central allocation, sequentially numbered opaque envelopes drawn consecutively. Otherwise score 0. |
| 3. Were the outcome assessors blind to assignment status? | Score 1 if assessors of pain and function at follow‐up were blinded to treatment outcome. Otherwise score 0. |
| 4. Were the inclusion and exclusion criteria clearly defined? | Score 1 if text states type of fracture and which patients were included and/or excluded. Otherwise score 0. |
| 5. Were the outcomes of patients who withdrew or excluded after randomisation described and included in an intention‐to‐treat analysis? | Score 1 if yes or text states that no withdrawals occurred of patients after randomisation or if they were included separately and results included in the group to which they were allocated. Otherwise score 0. |
| 6. Were the treatment and control groups adequately described at entry and if so were the groups well matched, or appropriate covariate adjustment made? | Score 1 if at least four admission details given (e.g. age, sex, mobility, function score, mental test score, fracture type) with either no important difference between groups or appropriate adjustment made. Otherwise score 0. |
| 7. Were less that 5% of patients lost to follow‐up. | Score 1 if yes. Otherwise score 0. |
| 8. Was the timing of outcome measures appropriate? | A minimum of 12 months follow‐up for all surviving patients. Score 1 if yes. Otherwise score 0. |
| 9. Were the outcome measures clearly defined in the text with a definition of any ambiguous terms encountered? | Score 1 if yes. Otherwise score 0. |
| 10. Were the surgeons experienced at both operations prior to commencement of the trial? | Score 1 if text states there was an introductory period or that all surgeons were experienced in both operations. Otherwise score 0. |
| 11. Were the care programmes other than trial options identical? | Score 1 if text states they were or if this can be inferred. Otherwise score 0. |
Measures of treatment effect
Risk ratios and 95% confidence limits were calculated for dichotomous outcomes, and mean differences and 95% confidence limits calculated for continuous outcomes.
Assessment of heterogeneity
Heterogeneity between comparable trials was assessed by visual inspection of the overlap of confidence intervals amongst included studies and tested using a standard Chi² test.
Data synthesis
Where appropriate, results of comparable groups of trials were pooled using the fixed‐effect model. Where there was substantial heterogeneity, the results of the random‐effects model were checked and presented.
Sensitivity analysis
We planned but did not undertake sensitivity analyses to investigate the effects of including trials which at risk of bias from lack of allocation concealment.
Results
Description of studies
Thirty studies were included and details of these are given in the Characteristics of included studies. The included studies involve a total of 6334 patients (6339 fractures). Alho 1998 involved three hospitals with different randomisation of implants within each centre. Results for each centre in this study are therefore considered separately under three headings (Alho 1998(a); Alho 1998(b); Alho 1998(c)).
The majority of studies included both undisplaced and displaced fractures. Kuokkanen 1991 included only undisplaced fractures while Alho 1998 (Alho 1998(a); Alho 1998(b); Alho 1998(c)), Benterud 1997, Christie 1988, Frandsen 1981, Madsen 1987 and Paus 1986 included only displaced fractures. Dalen 1985 did not state the number of displaced fractures.
The types of implant studied differed considerably. Few studies compared the same implants. Details of comparisons can be found in the Characteristics of included studies, and are summarised under each comparison in Effects of interventions.
Four studies (Ingwersen 1992;Jukkala‐Partio 2000;Poulsen 1995;Sernbo 1986) were excluded for the reasons listed in the Characteristics of excluded studies.
The authors of this report would be pleased to receive any additional information from any of the included studies which may then be included in updates of this review.
Risk of bias in included studies
The risk of bias assessments for sequence generation and allocation concealment for individual trials are shown in Figure 1 and an overall summary is given in Figure 2. The majority of judgements were 'unclear', which reflected in part the poor reporting of the methods of randomisation in these trials. Sequence generation was considered adequate in six trials. Only Lykke 2003 was judged as having adequate concealment of allocation. Four quasi‐randomised trials (Harper 1992, Nordkild 1985, Stromquist 1988; Stromqvist 1984) were considered at high risk of bias resulting from both inadequate sequence generation and lack of allocation concealment. Details of the randomisation methods reported in the 30 trials are given below.
1.
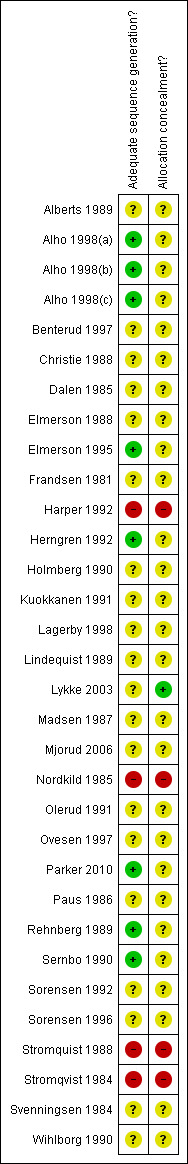
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
2.
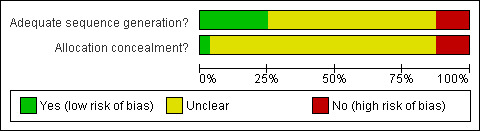
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Lagerby 1998 used closed sealed envelopes drawn in a sequential order. Elmerson 1988 randomised patients from a table of randomised numbers at the time of surgery. Alho 1998 (Alho 1998(a); Alho 1998(b); Alho 1998(c)) used random numbers within closed envelopes. Herngren 1992 and Elmerson 1995 also used a 'random numbers table'. Rehnberg 1989 also used random numbers but also matched for age, sex and type of residence. Wihlborg 1990 used sealed envelopes opened on the day of the operation. Lykke 2003 used sealed opaque numbered envelopes. Mjorud 2006 used sealed numbered envelopes. Paus 1986 used 'coded envelopes' and Sernbo 1990 used a random number generator to randomise the patient in the operating theatre. Parker 2010 used the toss of a coin.
Both Stromquist 1988 and Stromqvist 1984 used open randomisation with odd and even dates of birth. Nordkild 1985 stated they used 'odd and even numbers'. Harper 1992 used the even or odd medical record number.
Alberts 1989, Benterud 1997, Christie 1988, Dalen 1985, Frandsen 1981, Kuokkanen 1991, Lindequist 1989, Madsen 1987, Olerud 1991, Ovesen 1997, Svenningsen 1984, Sorensen 1992, and Sorensen 1996 did not give the method of randomisation. Holmberg 1990 stated that patients were randomised in the operating theatre but did not specify the method used.
The methodological assessment scores for the included studies are shown in Appendix 2.
Effects of interventions
For all the included studies the outcomes measures of non‐union, avascular necrosis, total fracture healing complications, re‐operations (for arthroplasty or implant removal), mortality and length of surgery are shown in the analysis tables. Data are not available from all included trials on all outcomes. Where significant results are reported in trials, these are also reported here.
Thornton nail versus three Scand pins
Dalen 1985 compared a single Thornton nail with three Scand pins in 94 patients. The limited results presented in the analyses indicate a tendency to a lower failure rate with the Scand pins (Analysis 1.1, Analysis 1.2). Intracapsular pressures were measured for 21 of the cases and showed no difference in intra‐operative intra‐articular pressures.
1.1. Analysis.
Comparison 1 Thornton nail versus three Scand pins, Outcome 1 All fracture healing complications.
1.2. Analysis.
Comparison 1 Thornton nail versus three Scand pins, Outcome 2 Re‐operations.
Thornton nail versus sliding nail plate
Frandsen 1981 compared a single Thornton nail with a sliding nail plate in 383 patients. Results indicate a lower risk of non‐union (Analysis 2.1) for those fractures treated with a sliding nail plate but no statistically significant difference in avascular necrosis (Analysis 2.2) or people with either complication (Analysis 2.3).
2.1. Analysis.
Comparison 2 Thornton nail versus sliding nail plate, Outcome 1 Non‐union.
2.2. Analysis.
Comparison 2 Thornton nail versus sliding nail plate, Outcome 2 Avascular necrosis.
2.3. Analysis.
Comparison 2 Thornton nail versus sliding nail plate, Outcome 3 All fracture healing complications.
Sliding compression screw implant versus McLaughlin nail plate
Svenningsen 1984 compared a sliding compression screw plate implant with a McLaughlin nail plate in 255 patients. Results indicate a tendency towards an increased non‐union rate for those treated with the McLaughlin nail plate (Analysis 3.1). There were no statistically significant differences between the two groups for avascular necrosis (Analysis 3.2), all fracture healing complications (Analysis 3.3), re‐operations (Analysis 3.4), infection (Analysis 3.5) or mortality (Analysis 3.6). Length of surgery was a mean of 43 minutes for the compression screw implant and 38 minutes for the McLaughlin nail plate (P < 0.001). Hospital stay and fall in haemoglobin were reported as showing no significant difference between groups.
3.1. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 1 Non‐union.
3.2. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 2 Avascular necrosis.
3.3. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 3 All fracture healing complications.
3.4. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 4 Re‐operations ‐ implant removal.
3.5. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 5 Superficial wound infection.
3.6. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 6 Deep wound infection.
Sliding hip screw (SHS) versus sliding nail plate
Nordkild 1985 compared the SHS with the sliding nail plate in 49 patients. Results indicate no difference in the incidence of fracture healing complications (Analysis 4.1, Analysis 4.2) or re‐operations (arthroplasty) (Analysis 4.3) but an increased number of patients having residual pain in the nail plate group (Analysis 4.4). Other outcomes reported were range of hip movements and walking aids used which showed no significant difference between groups. Bone scintigraphy was performed in a subgroup of 35 patients and showed no statistically significant difference between groups.
4.1. Analysis.
Comparison 4 Sliding hip screw versus sliding nail plate, Outcome 1 Non‐union.
4.2. Analysis.
Comparison 4 Sliding hip screw versus sliding nail plate, Outcome 2 Avascular necrosis.
4.3. Analysis.
Comparison 4 Sliding hip screw versus sliding nail plate, Outcome 3 Re‐operations ‐ arthroplasty.
4.4. Analysis.
Comparison 4 Sliding hip screw versus sliding nail plate, Outcome 4 Pain at follow‐up.
SHS versus double divergent pins
One study of 127 patients compared these implants (Christie 1988). The results for 15 patients were not given as they had either died early within the follow‐up period or had been lost to follow‐up. The data for non‐union, avascular necrosis, re‐operations (all for revision to arthroplasty) and use of walking aids at follow‐up are given in the analyses. These results indicate a trend to a lower risk of non‐union (Analysis 5.1) and fewer re‐operations (Analysis 5.4) for those fractures fixed with the double divergent pins but no difference in the other outcomes.
5.1. Analysis.
Comparison 5 Sliding hip screw versus double divergent pins, Outcome 1 Non‐union.
5.4. Analysis.
Comparison 5 Sliding hip screw versus double divergent pins, Outcome 4 Re‐operations.
SHS versus different types of cancellous bone screws
Eight studies compared the SHS with different types of cancellous bone screws (Benterud 1997; Harper 1992; Kuokkanen 1991; Madsen 1987; Ovesen 1997; Paus 1986; Sorensen 1992; Sorensen 1996). The results for the individual comparisons are described separately below but presented together in the analyses: Non‐union (Analysis 6.1), avascular necrosis (Analysis 6.2), fracture healing complications (Analysis 6.3), re‐operations ‐ arthroplasty (Analysis 6.4), re‐operations ‐ implant removal (Analysis 6.5), deep wound infection (Analysis 6.6), mortality (Analysis 6.7), and pain at follow‐up (Analysis 6.8).
6.1. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 1 Non‐union.
6.2. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 2 Avascular necrosis.
6.3. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 3 All fracture healing complications.
6.4. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 4 Re‐operations ‐ arthroplasty.
6.5. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 5 Re‐operations ‐ implant removal.
6.6. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 6 Deep wound infection.
6.7. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 7 Mortality.
6.8. Analysis.
Comparison 6 Sliding hip screw versus cancellous screws, Outcome 8 Pain at follow‐up.
SHS versus Uppsala/ Olmed screws
Benterud 1997 reported a study of 225 patients and found no difference in the incidence of fracture healing complications. Sorensen 1996 reported a study as a conference abstract for 101 patients and found no difference in the total incidence of fracture healing complications. Ovesen 1997 also reported a similar study only as a conference abstract for 316 fractures. The incidence of fracture healing complications for those who attended follow‐up was reported as 31 per cent for the SHS and 25 per cent for Uppsala screws. The difference between these groups was reported as being not statistically significant. Re‐operations for arthroplasty were required in 33/108 (30.6%) of SHS cases and 31/117 (26.5%) of the Uppsala group.
Benterud 1997 also reported that two patients in the SHS group developed wound infection requiring debridement. These were classified as deep wound infections in the analyses. Benterud 1997 found no difference between the two groups in mortality nor in pain at follow‐up. Ovesen 1997 reported 'no difference' in mortality between groups at three, 12 and 24 months. The average hospital stay was 18 days in the SHS group and 15 days in the Uppsala screws group.
Benterud 1997 reported a significantly reduced median anaesthetic time for Olmed screws of 74 minutes versus 100 minutes for the SHS. Median operative times were 29 versus 55 minutes respectively. Ovesen 1997 reported median operative times of 25 minutes for Uppsala screws and 45 minutes for the SHS . Median operative blood loss was 10 ml for Uppsala screws and 100 ml for the SHS ‐ this was reported as being statistically significant.
SHS versus two von Bahr screws
One study (Paus 1986) compared the SHS with two von Bahr screws in 131 patients. Results indicate no significant difference in any of the outcomes other than an increased number of patients treated with von Bahr screws who had implant removal (Analysis 6.5). Length of surgery was also reported as showing a significant increase for the SHS (52 versus 41 minutes, P < 0.05).
SHS versus Gouffon screws
Sorensen 1992 compared the SHS with Gouffon screws in 73 patients. The trial was stopped earlier than planned because of the higher fixation failure rate in the Gouffon screw group. Results in the analyses shows a reduced fracture healing complications rate for the SHS (RR 0.52, 95% CI 0.31 to 0.87) but a higher mortality for SHS compared to the Gouffon screws (RR 2.53, 95% CI 1.09 to 5.86).
SHS versus three cancellous screws
Kuokkanen 1991 compared the SHS with three cannulated Mercon screws in 33 patients. Results for non‐union, avascular necrosis, re‐operations, deep wound infection and mortality are shown in the analyses with no significant difference for the different implants. In addition, there was one case of screw penetration into the acetabulum for the cancellous screw group. It was also reported there was no difference in the length of surgery between groups (61 minutes in each group). Mean operative blood loss was 200 ml for the cancellous screws and 245 ml for the SHS. The surviving patients were assessed by the Harris Hip Score (Harris 1969) ‐ the results were stated to be 'somewhat better' for the SHS group (3/14 fair or poor for the SHS versus 6/15 for cancellous screws).
Harper 1992 compared the SHS (Ambi screw) with three cancellous screws in 209 patients. Only limited outcomes were reported. The number of cases requiring arthroplasty for fracture healing complications was 9/102 in the SHS group and 11/107 in the cancellous screw group. In addition there were two cases of fracture below the cancellous screws. There was no difference in mortality between groups.
SHS versus four cancellous screws
Madsen 1987 compared the SHS with four cancellous AO screws in 103 patients. Results for non‐union of the fracture were presented using an actuarial survival analysis from which it was not possible to determine the number of patients who had died, been lost to follow‐up or developed non‐union. The paper reported a two‐year cumulated union rate of 64 per cent for the SHS and 84 per cent for the parallel screw group, a difference that was reported as being statistically significant (P < 0.05). Results for avascular necrosis, re‐operations and deep wound infection given in the analyses show no significant differences.
Madsen 1987 also reported on length of surgery which was a mean of 130 minutes for the SHS and 108 minutes for the parallel screws. Figures for the mean operative blood loss were 350 ml versus 200 ml for the cases of SHS and parallel screws who had a general anaesthetic and 200 ml versus 150 ml for those who had a regional anaesthetic. All these differences between groups were significantly in favour of the cancellous screws. Bone scintigraphy was also measured in 87 cases in Madsen 1987. The number of femoral heads with an impaired uptake was 14/40 for the SHS and 5/47 for the cancellous screws, a difference that was reported to be statistically significant.
Two von Bahr screws versus Hessel pins
Lindequist 1989 compared von Bahr screws with Hessel pins for 150 patients. All the results of this study are presented in the analyses (Analysis 7.1 to Analysis 7.8) and indicate a reduction in fracture healing complications (RR 0.58, 95% CI 0.40 to 0.83, Analysis 7.3) and re‐operations (RR 0.47, 95% CI 0.28 to 0.79, Analysis 7.4; RR 0.26, 95% CI 0.10 to 0.66, Analysis 7.5) for the von Bahr screws.
7.1. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 1 Non‐union.
7.8. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 8 Mortality ‐ 2 years.
7.3. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 3 All fracture healing complications.
7.4. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 4 Re‐operations ‐ arthroplasty.
7.5. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 5 Re‐operations ‐ implant removal.
Two von Bahr screws versus Gouffon screws
Lindequist 1989 compared von Bahr screws with Gouffon screws in 169 patients. All the results of this study are presented in the analyses (Analysis 8.1 to Analysis 8.8) and indicate no significant difference in the incidence of fracture healing complications but a reduction in re‐operations for implant removal (Analysis 8.5) for the von Bahr screws.
8.1. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 1 Non‐union.
8.8. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 8 Mortality ‐ 2 years.
8.5. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 5 Re‐operations ‐ implant removal.
Two von Bahr screws versus two Uppsala screws
One study of 222 patients compared these two implants (Rehnberg 1989). Results indicate a higher risk of non‐union and fracture healing complications for the von Bahr screws (RR 3.18, 95% CI 1.70 to 5.94, Analysis 9.1; RR 2.17, 95% CI 1.32 to 3.55, Analysis 9.3). In addition to the complications shown in the analyses there were two cases of screw penetration in the Uppsala group and one in the von Bahr group. Other outcomes reported were for mortality Analysis 9.6), mean length of surgery and mean operative blood loss for which there was no significant difference between groups. Pain was assessed at four and 12 months and reported to be significantly reduced for those treated with Uppsala screws (P < 0.001 at 4 months, P < 0.01 at 12 months). Use of walking aids was reported to be significantly more common (P < 0.01) after von Bahr screws at four months, but no significant difference was noted at 12 months. There was no significant difference in the change in residential status between groups for four and 12 months.
9.1. Analysis.
Comparison 9 Two von Bahr screws versus two Uppsala screws, Outcome 1 Non‐union.
9.3. Analysis.
Comparison 9 Two von Bahr screws versus two Uppsala screws, Outcome 3 All fracture healing complications.
9.6. Analysis.
Comparison 9 Two von Bahr screws versus two Uppsala screws, Outcome 6 Mortality ‐ 12 months.
Three Richard screws versus two Uppsala screws
Lagerby 1998 studied 268 fractures in 266 patients. Results for non‐union (Analysis 10.1), avascular necrosis (Analysis 10.2), fracture healing complications (Analysis 10.3) and pain at follow‐up (Analysis 10.4) show no significant difference between the two implants. Re‐operations, mortality and use of walking aids were reported as showing 'no difference' between groups.
10.1. Analysis.
Comparison 10 Three Richards screws versus two Uppsala screws, Outcome 1 Non‐union.
10.2. Analysis.
Comparison 10 Three Richards screws versus two Uppsala screws, Outcome 2 Avascular necrosis.
10.3. Analysis.
Comparison 10 Three Richards screws versus two Uppsala screws, Outcome 3 All fracture healing complications.
10.4. Analysis.
Comparison 10 Three Richards screws versus two Uppsala screws, Outcome 4 Pain (moderate/severe) at one year.
Three Ullevaal screws versus two Olmed screws
Alho 1998(a) and Alho 1998(c) compared three Ullevaal screws with two Olmed screws in 358 patients. The limited results as presented in the analyses show a lower re‐operation rate for conversion to arthroplasty for those patients treated at Ullevaal hospital (Alho 1998(c); RR 0.42, 95% CI 0.22 to 0.83, Analysis 11.1). No difference in this re‐operation rate was seen at the other centre (Alho 1998(a)). There was no difference between the two interventions in the implant removal rate (Analysis 11.2). Three patients in the Ullevaal screw group and one in the Olmed screw group suffered fracture below the screws, necessitating revision fixation (Analysis 11.3). No other outcomes were reported.
11.1. Analysis.
Comparison 11 Three Ullevaal screws versus two Uppsala/Olmed screws, Outcome 1 Re‐operations ‐ arthroplasty.
11.2. Analysis.
Comparison 11 Three Ullevaal screws versus two Uppsala/Olmed screws, Outcome 2 Re‐operations ‐ implant removal.
11.3. Analysis.
Comparison 11 Three Ullevaal screws versus two Uppsala/Olmed screws, Outcome 3 Fracture below screws (requiring re‐operation).
Three Ullevaal screws versus two Tronzo screws
Alho 1998(b) compared three Ullevaal screws with two Tronzo screws in 249 patients. The limited results, as presented in the analyses, indicate no difference in the number of patients needing conversion to arthroplasty (Analysis 12.1), but a tendency to a lower removal of the implant for the Tronzo screws, although the result did not reach statistical significance (RR 2.05, 95% CI 0.90 to 4.66, Analysis 12.2). One patient in the Ullevaal screw group suffered fracture below the screws, necessitating revision fixation (Analysis 12.3). No other outcomes were reported.
12.1. Analysis.
Comparison 12 Three Ullevaal screws versus two Tronzo screws, Outcome 1 Re‐operations ‐ arthroplasty.
12.2. Analysis.
Comparison 12 Three Ullevaal screws versus two Tronzo screws, Outcome 2 Re‐operations ‐ implant removal.
12.3. Analysis.
Comparison 12 Three Ullevaal screws versus two Tronzo screws, Outcome 3 Fracture below screws (requiring re‐operation).
Three screws of any type versus two screws of any type
Exploratory analysis was undertaken to combine all studies which compared three screws with two screws (Alho 1998(a); Alho 1998(b); Alho 1998(c); Lagerby 1998). Results as indicated in the analyses (Analysis 13.1 to Analysis 13.8) show no significant difference between three or two screws except for re‐operation for arthroplasty. For this outcome there was a significant reduction for the three screws (32/302 versus 52/305: RR 0.64, 95% CI 0.43 to 0.97, Analysis 13.4). However, when those cases of non‐union in Lagerby 1998 are considered as well, the difference in major fracture healing complications between three and two screws becomes statistically insignificant (Analysis 13.7).
13.1. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 1 Non‐union.
13.8. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 8 Pain (moderate/severe) at one year.
13.4. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 4 Re‐operations ‐ arthroplasty.
13.7. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 7 Re‐operation for arthroplasty or non‐union.
Three short threaded AO screws versus three long threaded AO screws
Parker 2010 compared three AO screws with 16 mm of threads with three AO screws of 32 mm threads in 432 patients. Results as presented in the analyses showed no statistically significant differences in the occurrence of fracture healing complications (Analysis 14.1, Analysis 14.2, Analysis 14.3), re‐operations (Analysis 14.4, Analysis 14.5), mortality (Analysis 14.6), residual pain (Analysis 14.7) or change in residential status (Analysis 14.8) between the two methods of fixation. In addition there was no difference between groups for the regain of mobility and mean pain scores at one year from injury.
14.1. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 1 Non‐union.
14.2. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 2 Avascular necrosis.
14.3. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 3 Fracture below screws.
14.4. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 4 Re‐operations ‐ all types.
14.5. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 5 Re‐operations ‐ implant removal.
14.6. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 6 Mortality ‐ one year.
14.7. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 7 Pain at one year follow‐up.
14.8. Analysis.
Comparison 14 Three short thread AO screws versus three long threaded AO screws, Outcome 8 Failure to return to same residential status at one year (survivors).
Three Scand screws versus three Nystrom nails
Alberts 1989 compared three Nystrom nails with three Scand screws in 133 patients. Results as presented in the analyses showed no difference for fracture healing complications (Analysis 15.1, Analysis 15.2, Analysis 15.3), infection (Analysis 15.4, Analysis 15.5) and mortality (Analysis 15.6, Analysis 15.7). Extrusion of the implant was more common with the Nystrom nails. Mean length of surgery was 18 minutes for the Nystrom nails and 30 minutes for the Scand screws (P value reported as < 0.001).
15.1. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 1 Non‐union.
15.2. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 2 Avascular necrosis.
15.3. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 3 All fracture healing complications.
15.4. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 4 Superficial wound infection.
15.5. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 5 Deep wound infection.
15.6. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 6 Mortality ‐ one year.
15.7. Analysis.
Comparison 15 Three Scand screws versus three Nystrom nails, Outcome 7 Mortality ‐ two years.
Three Gouffon screws with a Rydell four‐flanged nail
Two studies compared these two implants. Elmerson 1988 reported a study of 223 patients and Wihlborg 1990 a study of 200 patients. Results as presented in the analyses showed no difference between the two implants for the outcome measures of non‐union (Analysis 16.1), avascular necrosis (Analysis 16.2), fracture healing complications (Analysis 16.3), re‐operations (for arthroplasty) (Analysis 16.4), infection (Analysis 16.5, Analysis 16.6) or mortality (Analysis 16.7, Analysis 16.8).
16.1. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 1 Non‐union.
16.2. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 2 Avascular necrosis.
16.3. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 3 All fracture healing complications.
16.4. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 4 Re‐operations.
16.5. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 5 Superficial wound infection.
16.6. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 6 Deep wound infection.
16.7. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 7 Mortality ‐ one year.
16.8. Analysis.
Comparison 16 Three Gouffon screws versus Rydell four‐flanged nail, Outcome 8 Mortality ‐ two years.
Elmerson 1988 also indicated that the mean length of surgery was 38 minutes for Gouffon screws and 28 minutes for the Rydell nail, a difference that was reported to be statistically significant (P < 0.001).
Two Hansson pins versus a Rydell four‐flanged nail
Three studies compared these implants: Holmberg 1990 reported a study of 220 patients; Sernbo 1990 of 410 patients and Stromqvist 1984 of 152 patients. The outcomes measures, where reported, for non‐union (Analysis 17.1), avascular necrosis (Analysis 17.2), fracture healing complications (Analysis 17.3), re‐operations (Analysis 17.4, Analysis 17.5) and mortality at two years (Analysis 17.6) are shown in the analyses. Results indicated no significant difference in outcomes between the two implants for any of the outcomes listed above; the random‐effects model was used for the first five analyses because of clearly significant heterogeneity.
17.1. Analysis.
Comparison 17 Two Hansson pins versus Rydell four‐flanged nail, Outcome 1 Non‐union.
17.2. Analysis.
Comparison 17 Two Hansson pins versus Rydell four‐flanged nail, Outcome 2 Avascular necrosis.
17.3. Analysis.
Comparison 17 Two Hansson pins versus Rydell four‐flanged nail, Outcome 3 All fracture healing complications.
17.4. Analysis.
Comparison 17 Two Hansson pins versus Rydell four‐flanged nail, Outcome 4 Re‐operations ‐ arthroplasty.
17.5. Analysis.
Comparison 17 Two Hansson pins versus Rydell four‐flanged nail, Outcome 5 Re‐operations ‐ implant removal.
17.6. Analysis.
Comparison 17 Two Hansson pins versus Rydell four‐flanged nail, Outcome 6 Mortality ‐ 2 years.
Holmberg 1990 reported that a similar number of patients in each group (27/110 and 26/110) failed to return to the same residential status. Sernbo 1990 also gave figures for the mean length of surgery, radiographic screening time, length of hospital stay and numbers going back to the same residential state. There was no significant difference between groups for any of these outcomes. Stromqvist 1984 reported no cases of deep wound infection in either group and also presented the results of bone scintimetric evaluation for 138 of the patients. This indicated a statistically significant reduction of uptake of isotope for those fractures treated with the four‐flanged nail.
Two Hansson pins versus Sliding Hip Screw (SHS)
Both Elmerson 1995 (222 patients) and Sorensen 1996 (99 patients) found no difference in the incidence of fracture healing complications (Analysis 18.1, Analysis 18.2, Analysis 18.3), or re‐operations (Analysis 18.4). Mortality was reported in Elmerson 1995 with no difference between implants (Analysis 18.5). Elmerson 1995 also reported on the length of surgery, which was significantly lower for the Hansson pins (24 versus 34 minutes, Analysis 18.6).
18.1. Analysis.
Comparison 18 Two Hansson pins versus sliding hip screw, Outcome 1 Non‐union.
18.2. Analysis.
Comparison 18 Two Hansson pins versus sliding hip screw, Outcome 2 Avascular necrosis.
18.3. Analysis.
Comparison 18 Two Hansson pins versus sliding hip screw, Outcome 3 All fracture healing complications.
18.4. Analysis.
Comparison 18 Two Hansson pins versus sliding hip screw, Outcome 4 Re‐operations ‐ arthroplasty.
18.5. Analysis.
Comparison 18 Two Hansson pins versus sliding hip screw, Outcome 5 Mortality ‐ 2 years.
18.6. Analysis.
Comparison 18 Two Hansson pins versus sliding hip screw, Outcome 6 Length of surgery.
Two Hansson hook pins versus cancellous screws
Six studies compared two Hansson hook pins with different types of cancellous bone screws (Herngren 1992; Lykke 2003; Mjorud 2006; Olerud 1991; Sorensen 1996; Stromquist 1988). The results for the individual comparisons are described separately below but presented together in the analyses: Non‐union (Analysis 19.1), avascular necrosis (Analysis 19.2), fracture healing complications (Analysis 19.3), re‐operations ‐ arthroplasty (Analysis 19.4), re‐operations ‐ arthroplasty or need for arthroplasty (Analysis 19.5), re‐operations ‐ implant removal (Analysis 19.6), re‐operations ‐ type not specified (Analysis 19.7), deep wound infection (Analysis 19.8), superficial wound infection (Analysis 19.9), and mortality (Analysis 19.10).
19.1. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 1 Non‐union.
19.2. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 2 Avascular necrosis.
19.3. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 3 All fracture healing complications.
19.4. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 4 Re‐operations ‐ arthroplasty.
19.5. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 5 Re‐operation ‐ arthroplasty or need for arthroplasty.
19.6. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 6 Re‐operations ‐ implant removal.
19.7. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 7 Re‐operations ‐ type not specified.
19.8. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 8 Deep wound infection.
19.9. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 9 Superficial wound infection.
19.10. Analysis.
Comparison 19 Two Hansson pins versus cancellous screws, Outcome 10 Mortality.
Two Hansson pins versus two Uppsala screws
Three studies compared these implants: Herngren 1992 (179 patients, 180 fractures), Olerud 1991 (115 patients) and Sorensen 1996 (100 patients). Pooled results using the random‐effects model for non‐union, avascular necrosis and all fracture healing complications show no significant differences between the two implants. Notably, Olerud 1991 reported a significant reduction in the incidence of non‐union for those treated with the Uppsala screws (RR 3.79, 95% CI 1.51 to 9.53), while the two trials (Herngren 1992; Sorensen 1996) found no difference between implants for the incidence of fracture healing complications. Herngren 1992 also reported three cases of trochanteric fracture of the same hip in those treated with the Hansson pins and one case with Uppsala screws. Pooled data for mortality from two trials showed trend to lower mortality in the Hansson pin group.
Length of surgery reported by Herngren 1992 was a mean of 33 minutes for the Hansson pins and 38 minutes for the Uppsala screws.
Olerud 1991 also reported, without figures, that at the four and 12 month follow‐up there was a statistically significant increased incidence of pain (P = 0.0007 at 4 months, P = 0.007 at 12 months), failure to regain residential status (P = 0.028 at 4 months, P = 0.03 at 12 months) and reduction in mobility (P = 0.008 at 4 months, P = 0.097 at 12 months) for those treated by the Hansson pins.
Herngren 1992 noted there was local discomfort to lateral protrusion of the implant in six out of 96 Uppsala screw cases but in no patients of the Hansson group.
Two Hansson hook pins versus two AO screws
Stromquist 1988 studied 110 cases. Follow‐up of patients was for only four months and the trial methodology was poor. Non‐union and avascular rates were not given but re‐operations within the follow‐up period were stated as fewer for the Hansson pins. However, it was reported that more patients in the Hansson pin group were scheduled for arthroplasty, such that the difference between groups for those who had re‐operations and needed re‐operation was not significantly different (Analysis 19.5). Mortality and bone scintimetry results showed no significant difference between the two implants.
Two Hansson hook pins versus three AO screws
Mjorud 2006 studied 199 cases. Follow‐up of patients was for two years. Outcomes reported and detailed in the analyses were fracture healing complications and re‐operations. None of these outcomes showed any difference between groups. Mean length of surgery was 36 minutes for the Hansson pins and 40 minutes for the AO screws, a difference that was reported as not statistically significant. Mortality reported at up to two years from surgery showed no difference between groups. Other outcomes reported which also showed no statistically significant difference between groups were inability to walk at discharge and later walking ability.
Two Hansson hook pins versus three Ullevaal screws
Lykke 2003 compared two Hansson pins with three Ullevaal screws in 278 fractures. Results as indicated in the analyses show no significant difference in non‐union, fracture healing complications, re‐operations, wound infections or mortality between treatment groups. There appeared, however, a potential trend to a lower rate of avascular necrosis in the Hansson pin group. In addition the study reported there was no differences in the degree of residual pain at follow‐up between groups (31% versus 23%), mean or median length of hospital stay (12 versus 10 days, 8 versus 8 days), or proportion of patients discharged to rehabilitation homes (47% versus 49%). The complication of deep vein thrombosis was similar between groups (one in each) as was that from pneumonia (one in the Hansson pin group versus three in the Ullevaal group). Fracture healing complications were more common in those cases in which drill penetration into the hip joint occurred during surgery. Drill penetration was more common in the Ullevaal screw group (7 versus 16 cases).
Discussion
Thirty studies using a wide variety of orthopaedic implants were identified and included within the analysis. The methodology of the studies varied considerably and most trials scored poorly, although in some of these cases the low score may reflect a poor reporting of trial methods rather than poor trial methodology. Additionally, risk of bias assessment relating to sequence generation and allocation concealment found only six trials were at low risk of bias for the first item and only one trial at low risk of bias for the second. The main outcome measures reported were fracture healing complications, re‐operations and mortality. The reporting of functional outcomes was poor and only documented in a small number of studies. The few significant differences observed after multiple analyses may have arisen by chance. Taken in conjunction with the generally low methodological quality of the studies as reported, caution needs to be adopted in drawing any definite conclusions. Most of the reported trials enrolled less than 300 participants. Thus, they were likely to be underpowered to provide evidence of significant difference between devices unless these differences had been expected to be large. Biologically or mechanically plausible differences between devices compared, and thus the hypotheses apparently being tested in the trials, were often unclear.
A significant potential for bias within the studies may have occurred in those centres which were evaluating an implant that was developed in their own institution, or by one of the authors of the study. The studies concerned were for Hansson pins (Stromqvist 1984), Uppsala screws (Olerud 1991; Rehnberg 1989), sliding compression screw plate (Svenningsen 1984) and Ullevaal screws (Alho 1998(c)). All these reported better outcomes for their own implants. The problems are highlighted in Alho 1998 who recommends that evaluation of implants by centres with a particular interest or expertise in one of the implants, is strongly prone to biases even within the context of a randomised trial. The cause for these biases is difficult to explain.
The conclusions for the different implants are summarised in the following.
Double divergent pins; fixed (static) nail plate; sliding compression screw plate; Hessel pins and Nystrom nails
For all these implants, only one randomised trial was found evaluating each implant (Alberts 1989: Nystrom nails; Christie 1988: double divergent pins; Lindequist 1989: Hessel pins; Svenningsen 1984: fixed nail plate and sliding compression screw plate). None of these studies showed a clear difference between the implants under investigation. Therefore, no conclusions can be made for the use of these implants from the randomised trials undertaken to date.
Single Thornton nail
This implant was found to have been evaluated in two randomised studies; one against three cancellous screws (Dalen 1985) and another against a sliding nail plate (Frandsen 1981). Both studies reported a tendency to a lower risk of fracture healing complications with the comparison implant. While there are limited data on the use of this implant, its use cannot be recommended given the tendency to inferior results in both comparisons.
Sliding nail plate
This implant has been evaluated in two randomised studies, one against a single Thornton nail (Frandsen 1981), where a lower rate of non‐union was found for the nail plate, and the other against an SHS (Nordkild 1985), where more patients had residual pain in the nail plate group. However, the small number of patients evaluated within these two trials means that no definite conclusions can be made regarding the use of a sliding nail plate.
Rydell four‐flanged nail
This implant was found to have been evaluated in five randomised studies, two comparing against Gouffon pins (Elmerson 1988;Wihlborg 1990) and three studies comparing against Hansson pins (Holmberg 1990;Sernbo 1990;Stromqvist 1984). No difference for the incidence of fracture healing complications or mortality between groups was found. As exception was found for Stromqvist 1984, where the results favoured the Hansson pin but, as stated already, this trial is potentially biased given the implant had been developed in the same institution.
Hansson hook (LIH) pins
This implant has been evaluated in 10 randomised trials. Bias may have occurred in these studies, possibly due to greater experience with one of the implants under investigation. A strong trend to improved outcomes with the Hansson pins was found in the study from Lund, Sweden (Stromqvist 1984), where the pins were developed by one of the paper's authors. The study from Uppsala, Sweden (Holmberg 1990) was from a unit where the Rydell nail was the implant used before the start of the study. This study showed a tendency to lower complications with the Rydell nail. A study from Uppsala (Olerud 1991) compared Hansson pins with Uppsala screws and found better outcomes with the latter group. The difference in results between studies may therefore be due to familiarity or special expertise with the use of one of the implants under investigation.
Three studies compared Hansson pins with the Rydell nail (Holmberg 1990; Sernbo 1990; Stromqvist 1984). Although, as described above, Stromqvist 1984 showed better outcomes after the Hansson pins, overall there were no notable differences between implants. Three studies compared Hansson pins with Uppsala screws (Herngren 1992; Olerud 1991;Sorensen 1996), two with two AO screws (Mjorud 2006; Stromquist 1988), one with Ullevaal screws (Lykke 2003) and two with the SHS (Elmerson 1995; Sorensen 1996). Overall there were no notable differences in fracture healing complications between implants.
Sliding hip screw (SHS)
This implant has been evaluated more extensively within 11 randomised studies. Christie 1988 compared the SHS with double divergent pins. There was a tendency to lower fracture healing complications after double divergent pins, but due to the low numbers of patients reported, no definite conclusions can be made about the comparison of these two implants. Nordkild 1985 compared the SHS with the sliding nail plate. Results indicated no difference in the incidence of fracture healing complications, but more patients had residual pain in the nail plate group. Two studies compared the SHS with Hansson pins (Elmerson 1995; Sorensen 1996). Neither study found any significant difference in the incidence of fracture healing complications.
Eight studies compared the SHS with different types of cancellous bone screws (Benterud 1997; Harper 1992; Kuokkanen 1991; Madsen 1987; Ovesen 1997; Paus 1986; Sorensen 1992; Sorensen 1996). Summation of results showed an increased incidence of avascular necrosis and also a tendency to a higher fixation failure rate with the cancellous screws, although the overall re‐operation rate for fixation failure did not differ between implants. Those studies that reported on operative blood loss and operative time noted an increase for the SHS. The findings of a significantly higher mortality in the SHS group of Sorensen 1992 were not found in the other five trials providing data for this outcome.
Multiple screws
Implants consisting of multiple screws were the most prevalent type of implant studied. Eighteen studies compared a multiple parallel screw technique against an alternative type of implant. As summarised above, for those studies that compared multiple screws against the SHS (Benterud 1997; Harper 1992; Kuokkanen 1991; Madsen 1987; Ovesen 1997; Paus 1986; Sorensen 1992; Sorensen 1996), there was no overall difference in the number of fracture healing complications between implants aside from an increased incidence of avascular necrosis for the screws, but some studies noted that the SHS fixation took longer and had an increased blood loss. For those studies, which compared parallel screws with another type of implant, no study demonstrated notable differences for these comparisons. These studies were those comparing Gouffon screws with the Rydell nail (Elmerson 1988; Wihlborg 1990), Uppsala/Olmed screws with Hansson pins (Olerud 1991; Sorensen 1996; Herngren 1992), AO screws with Hansson pins (Mjorud 2006; Stromquist 1988), Ullevaal screws with Hansson pins (Lykke 2003), Scand hip pins with the Thornton nail (Dalen 1985), Scand hip pins with Nystrom nails (Alberts 1989) and von Bahr screws with Hessel pins (Lindequist 1989).
A further five studies compared different screw types (Alho 1998 (Alho 1998(a); Alho 1998(b); Alho 1998(c)); Lagerby 1998; Lindequist 1989; Rehnberg 1989; Parker 2010). For these studies it was not possible to make any notable conclusions between the different screw types affecting the incidence of fracture healing complications. This included those studies which compared two versus three screws.
Authors' conclusions
Implications for practice.
There is insufficient evidence from randomised controlled trials to determine the best implant for internal fixation of intracapsular fractures.
Implications for research.
Further studies are required to determine the choice of implant for internal fixation of intracapsular fractures. Future studies should be adequately powered to detect any clinically important difference between implant types; in the light of the evidence from this review, they may require recruiting thousands rather than hundreds of participants, and to be multi‐centre in order to increase generalisability and avoid biases which may have arisen in the past from single centre studies. These trials should have appropriate methodology with a minimum of one year follow‐up of cases and always report the results in full, even if the difference between implants is not significant. The current ongoing multi‐centre FAITH trial (FAITH) does address these issues and is comparing the two most commonly used implants of the SHS and multiple screws.
What's new
| Date | Event | Description |
|---|---|---|
| 18 January 2011 | New search has been performed | For this update, published in Issue 2, 2011, the following amendments were made: 1. Title changed from 'Internal fixation implants for intracapsular proximal femoral fractures in adults' to 'Internal fixation implants for intracapsular hip fractures in adults' 2. New studies of Mjorud 2006 and Parker 2010 included. 3. Ongoing study of FAITH added. 4. Risk of bias assessment implemented for sequence generation and allocation concealment. 5. Additional reference to studies of Stromqvist 1984 and Sernbo 1990 added. There were no changes to the conclusions of the review. |
History
Protocol first published: Issue 2, 1999 Review first published: Issue 4, 2001
| Date | Event | Description |
|---|---|---|
| 27 June 2008 | Amended | Converted to new review format. |
| 27 August 2003 | New search has been performed | For the first update in Issue 4, 2003 the following changes were made: 1. New study of Lykke 2003 included. 2. Sernbo 1986 and Jukkala‐Partio 2000 added to excluded studies. 3. Extra reference to studies of Olerud 1991 and Sorensen 1992 added. There were no changes to the conclusions of the review. |
Acknowledgements
Glyn Stockton was co‐author for the first edition of this review. Helen Handoll independently extracted data and checked the study of Parker 2010. We are indebted to Prof William Gillespie, Leeann Morton and Dr Helen Handoll for their help. We would also like to thank the following for useful comments from editorial review: Prof Rajan Madhok, Prof Gordon Murray, Prof Marc Swiontkowski, Dr Janet Wale, Peter Herbison, Prof James Hutchison, Dr Dicky Lam and Dr Jean‐Claude Theis.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (Wiley Online Library)
#1 MeSH descriptor Hip Fractures explode all trees (927) #2 ((hip* or femur* or femoral* or intracapsular* or subcapital or transcervical) NEAR/4 fracture*):ti,ab,kw (1952) #3 (#1 OR #2) (1952) #4 (pin or pins or pinned or pinning or nail* or screw* or plate* or arthroplast* or fix* or prosthes*):ti,ab,kw (29319) #5 MeSH descriptor Internal Fixators, this term only (98) #6 MeSH descriptor Bone Screws, this term only (394) #7 MeSH descriptor Fracture Fixation, Internal explode all trees (652) #8 MeSH descriptor Bone Plates, this term only (212) #9 MeSH descriptor Bone Nails, this term only (250) #10 MeSH descriptor Arthroplasty, this term only (139) #11 MeSH descriptor Arthroplasty, Replacement, Hip, this term only (1172) #12 (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) (29319) #13 (#3 AND #12) (745) #14 (extracapsular or trochanteric or subtrochanteric or pertrochanteric or intertrochanteric):ti (389) #15 (intracapsular or subcapital or transcervical):ti (225) #16 (#14 AND NOT #15) (379) #17 (#13 AND NOT #16) (499)
MEDLINE (Ovid Web)
1 exp Hip Fractures/ (14794) 2 ((hip$ or femur$ or femoral$ or intracapsular$ or subcapital or transcervical) adj4 fracture$).tw. (20570) 3 or/1‐2 (24920) 4 (pin$1 or nail$ or screw$1 or plate$1 or arthroplast$ or fix$ or prosthes$).tw. (385604) 5 Internal Fixators/ or Bone Screws/ or Fracture Fixation, Internal/ or Bone Plates/ or Bone Nails/ (40241) 6 Arthroplasty/ or Arthroplasty, Replacement, Hip/ (17548) 7 or/4‐6 (404588) 8 and/3,7 (10370) 9 (extracapsular or trochanteric or subtrochanteric or pertrochanteric or intertrochanteric).ti. (3536) 10 (intracapsular or subcapital or transcervical).ti. (1753) 11 9 not 10 (3458) 12 8 not 11 (9105) 13 Randomized Controlled Trial.pt. (298721) 14 Controlled Clinical Trial.pt. (82422) 15 randomized.ab. (205154) 16 placebo.ab. (121719) 17 Clinical Trials as Topic.sh. (150826) 18 randomly.ab. (149185) 19 trial.ti. (88477) 20 13 or 14 or 15 or 16 or 17 or 18 or 19 (692318) 21 exp Animals/ not Humans/ (3531211) 22 20 not 21 (640356) 23 12 and 22 (461)
EMBASE (Ovid Web)
1 exp Hip Fracture/ (20636) 2 ((hip$ or femur$ or femoral or intracapsular$ or subcapital or transcervical) adj4 fracture$).tw. (23792) 3 or/1‐2 (31432) 4 (pin$1 or nail$ or screw$1 or plate$1 or arthroplast$ or fix$ or prosthes$).tw. (434374) 5 Bone Nail/ or Bone Plate/ or Bone Screw/ or Ender Nail/ or External Fixator/ or Fixation Device/ or Interlocking Nail/ or Internal Fixator/ or Osteosynthesis Material/ (26043) 6 exp Fracture Fixation/ (52878) 7 Arthroplasty/ or Hip Arthroplasty/ (18137) 8 or/4‐7 (465804) 9 and/3,8 (13255) 10 (extracapsular or trochanteric or subtrochanteric or pertrochanteric or intertrochanteric).ti. (4058) 11 (intracapsular or subcapital or transcervical).ti. (1907) 12 10 not 11 (3967) 13 9 not 12 (11698) 14 Randomized Controlled Trial/ (280313) 15 Clinical Trial/ (804967) 16 Controlled Clinical Trial/ (161695) 17 Randomization/ (52313) 18 Single Blind Procedure/ (13269) 19 Double Blind Procedure/ (98937) 20 Prospective Study/ (154609) 21 ((clinical or controlled or comparative or prospective$ or randomi#ed) adj3 (trial or study)).tw. (508940) 22 (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. (126704) 23 ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. (126329) 24 ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. (150805) 25 RCT.tw. (5874) 26 or/14‐25 (1373779) 27 Case Study/ or Abstract Report/ or Letter/ (762331) 28 26 not 27 (1345199) 29 13 and 28 (1397)
Appendix 2. Methodological quality assessment results
| Study ID | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 |
| Thornton nail versus three Scand pins | |||||||||||
| Dalen 1985 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Thornton nail versus sliding nail plate | |||||||||||
| Frandsen 1981 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 |
| Sliding compression screw plate versus McLaughlin nail plate | |||||||||||
| Svenningsen 1984 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 |
| Sliding hip screw versus sliding nail plate | |||||||||||
| Nordkild 1985 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 0 | 1 |
| Sliding hip screw versus double divergent pins | |||||||||||
| Christie 1988 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 |
| Sliding hip screw versus two von Bahr screws | |||||||||||
| Paus 1986 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 |
| Sliding hip screw versus Gouffon screws | |||||||||||
| Sorensen 1992 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| Sliding hip screw versus cancellous screws | |||||||||||
| Harper 1992 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 |
| Madsen 1987 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 |
| Kuokkanen 1991 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 |
| Sliding hip screw versus Hansson pins versus Uppsala screws | |||||||||||
| Sorensen 1996 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Sliding hip screw versus two Uppsala or Olmed screws | |||||||||||
| Benterud 1997 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
| Ovesen 1997 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Sliding hip screw versus two Hansson pins | |||||||||||
| Elmerson 1995 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 |
| Three Gouffon pins versus a Rydell four flanged nail | |||||||||||
| Elmerson 1988 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 |
| Wihlborg 1990 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Two Hansson pins versus a Rydell four flanged nail | |||||||||||
| Holmberg 1990 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Sernbo 1990 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 0 |
| Stromqvist 1984 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 |
| Two Hansson pins versus two Uppsala screws | |||||||||||
| Herngren 1992 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Olerud 1991 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 |
| Two Hansson hook pins versus three Ullevaal screws | |||||||||||
| Lykke 2003 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 |
| Two Hansson hook pins versus two AO screws | |||||||||||
| Stromquist 1988 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 |
| Two Hansson hook pins versus three AO screws | |||||||||||
| Mjorud 2006 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 1 |
| Three Richard screws versus two Uppsala screws | |||||||||||
| Lagerby 1998 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 |
| Two von Bahr screws versus two Uppsala screws | |||||||||||
| Rehnberg 1989 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 |
| Three Ullevaal screws versus two Olmed screws | |||||||||||
| Alho 1998(a) | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 |
| Three Ullevaal screws versus two Tronzo screws | |||||||||||
| Alho 1998(b) | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 |
| Three Ullevaal screws versus two Olmed screws | |||||||||||
| Alho 1998(c) | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 |
| Three Nystrom nails versus three Scand screws | |||||||||||
| Alberts 1989 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 0 |
| von Bahr screws versus Hessel pins versus Gouffon screws | |||||||||||
| Lindequist 1989 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 1 |
| Three short thread AO screws versus three long threaded AO screws | |||||||||||
| Parker 2010 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
Data and analyses
Comparison 1. Thornton nail versus three Scand pins.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Re‐operations | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 2. Thornton nail versus sliding nail plate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 3. Sliding compression screw plate versus fixed nail plate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Superficial wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Deep wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Mortality ‐ 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
3.7. Analysis.
Comparison 3 Sliding compression screw plate versus fixed nail plate, Outcome 7 Mortality ‐ 1 year.
Comparison 4. Sliding hip screw versus sliding nail plate.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Re‐operations ‐ arthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Pain at follow‐up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 5. Sliding hip screw versus double divergent pins.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Use of walking aids at follow‐up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
5.2. Analysis.
Comparison 5 Sliding hip screw versus double divergent pins, Outcome 2 Avascular necrosis.
5.3. Analysis.
Comparison 5 Sliding hip screw versus double divergent pins, Outcome 3 All fracture healing complications.
5.5. Analysis.
Comparison 5 Sliding hip screw versus double divergent pins, Outcome 5 Use of walking aids at follow‐up.
Comparison 6. Sliding hip screw versus cancellous screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 4 | 462 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.57, 1.57] |
| 1.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.89, 2.03] |
| 1.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.55, 1.76] |
| 1.3 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.28, 1.05] |
| 1.4 Sliding hip screw versus three cancellous screws | 1 | 33 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Avascular necrosis | 5 | 565 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.62 [0.38, 1.01] |
| 2.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.38, 1.65] |
| 2.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.23, 1.53] |
| 2.3 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.13, 1.66] |
| 2.4 Sliding hip screw versus three cancellous screws | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.66] |
| 2.5 Sliding hip screw versus four cancellous screws | 1 | 103 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.61 [0.15, 2.43] |
| 3 All fracture healing complications | 6 | 772 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.70, 1.05] |
| 3.1 Sliding hip screw versus two Uppsala/Olmed screws | 2 | 326 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.07 [0.81, 1.40] |
| 3.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.30] |
| 3.3 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.31, 0.87] |
| 3.4 Sliding hip screw versus three cancellous screws | 2 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.28, 1.27] |
| 4 Re‐operations ‐ arthroplasty | 5 | 565 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.74, 1.33] |
| 4.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.15 [0.76, 1.75] |
| 4.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.53, 1.85] |
| 4.3 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.60 [0.32, 1.12] |
| 4.4 Sliding hip screw versus three cancellous screws | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.66] |
| 4.5 Sliding hip screw versus four cancellous screws | 1 | 103 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.38 [0.65, 8.70] |
| 5 Re‐operations ‐ implant removal | 5 | 565 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.30, 2.45] |
| 5.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Random, 95% CI) | 2.17 [0.56, 8.45] |
| 5.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.04, 0.86] |
| 5.3 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.05, 5.73] |
| 5.4 Sliding hip screw versus three cancellous screws | 1 | 33 | Risk Ratio (M‐H, Random, 95% CI) | 3.29 [0.80, 13.57] |
| 5.5 Sliding hip screw versus four cancellous screws | 1 | 103 | Risk Ratio (M‐H, Random, 95% CI) | 0.51 [0.16, 1.59] |
| 6 Deep wound infection | 4 | 492 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.66 [0.63, 11.25] |
| 6.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.41 [0.26, 111.49] |
| 6.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.97 [0.18, 21.20] |
| 6.3 Sliding hip screw versus three cancellous screws | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.4 Sliding hip screw versus four cancellous screws | 1 | 103 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.04 [0.19, 21.80] |
| 7 Mortality | 5 | 671 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.83, 1.89] |
| 7.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.49, 2.40] |
| 7.2 Sliding hip screw versus two von Bahr screws | 1 | 131 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.55 [0.19, 1.55] |
| 7.3 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.53 [1.09, 5.86] |
| 7.4 Sliding hip screw versus three cancellous screws | 2 | 242 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.61, 2.95] |
| 8 Pain at follow‐up | 2 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.58, 1.12] |
| 8.1 Sliding hip screw versus two Uppsala/Olmed screws | 1 | 225 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.55, 1.62] |
| 8.2 Sliding hip screw versus three Gouffon screws | 1 | 73 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.70 [0.48, 1.01] |
Comparison 7. von Bahr screws versus Hessel pins.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations ‐ arthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Superficial wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Deep wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Mortality ‐ 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
7.2. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 2 Avascular necrosis.
7.6. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 6 Superficial wound infection.
7.7. Analysis.
Comparison 7 von Bahr screws versus Hessel pins, Outcome 7 Deep wound infection.
Comparison 8. von Bahr screws versus Gouffon screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations ‐ arthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Superficial wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Deep wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Mortality ‐ 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
8.2. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 2 Avascular necrosis.
8.3. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 3 All fracture healing complications.
8.4. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 4 Re‐operations ‐ arthroplasty.
8.6. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 6 Superficial wound infection.
8.7. Analysis.
Comparison 8 von Bahr screws versus Gouffon screws, Outcome 7 Deep wound infection.
Comparison 9. Two von Bahr screws versus two Uppsala screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations ‐ arthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Mortality ‐ 12 months | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
9.2. Analysis.
Comparison 9 Two von Bahr screws versus two Uppsala screws, Outcome 2 Avascular necrosis.
9.4. Analysis.
Comparison 9 Two von Bahr screws versus two Uppsala screws, Outcome 4 Re‐operations ‐ arthroplasty.
9.5. Analysis.
Comparison 9 Two von Bahr screws versus two Uppsala screws, Outcome 5 Re‐operations ‐ implant removal.
Comparison 10. Three Richards screws versus two Uppsala screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Pain (moderate/severe) at one year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 11. Three Ullevaal screws versus two Uppsala/Olmed screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Re‐operations ‐ arthroplasty | 2 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.30, 0.95] |
| 2 Re‐operations ‐ implant removal | 2 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.52, 1.70] |
| 3 Fracture below screws (requiring re‐operation) | 2 | 358 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.19 [0.33, 14.53] |
Comparison 12. Three Ullevaal screws versus two Tronzo screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Re‐operations ‐ arthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Fracture below screws (requiring re‐operation) | 1 | Peto Odds Ratio (Peto, Fixed, 95% CI) | Totals not selected |
Comparison 13. Three screws (any type) versus two screws (any type).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations ‐ arthroplasty | 3 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.43, 0.97] |
| 5 Re‐operations ‐ implant removal | 3 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.78, 2.02] |
| 6 Fracture below screws (requiring re‐operation) | 3 | 607 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.45 [0.48, 12.38] |
| 7 Re‐operation for arthroplasty or non‐union | 4 | 875 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.62, 1.17] |
| 8 Pain (moderate/severe) at one year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
13.2. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 2 Avascular necrosis.
13.3. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 3 All fracture healing complications.
13.5. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 5 Re‐operations ‐ implant removal.
13.6. Analysis.
Comparison 13 Three screws (any type) versus two screws (any type), Outcome 6 Fracture below screws (requiring re‐operation).
Comparison 14. Three short thread AO screws versus three long threaded AO screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 Fracture below screws | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Re‐operations ‐ all types | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Mortality ‐ one year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Pain at one year follow‐up | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 8 Failure to return to same residential status at one year (survivors) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 15. Three Scand screws versus three Nystrom nails.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 4 Superficial wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Deep wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Mortality ‐ one year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Mortality ‐ two years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected |
Comparison 16. Three Gouffon screws versus Rydell four‐flanged nail.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.92 [0.65, 1.30] |
| 2 Avascular necrosis | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.09 [0.57, 2.08] |
| 3 All fracture healing complications | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.73, 1.27] |
| 4 Re‐operations | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.74, 1.71] |
| 5 Superficial wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Deep wound infection | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 7 Mortality ‐ one year | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.66, 1.94] |
| 8 Mortality ‐ two years | 2 | 423 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.60, 1.28] |
Comparison 17. Two Hansson pins versus Rydell four‐flanged nail.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 3 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.54, 1.58] |
| 2 Avascular necrosis | 3 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 0.59 [0.28, 1.24] |
| 3 All fracture healing complications | 3 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.48, 1.23] |
| 4 Re‐operations ‐ arthroplasty | 3 | 782 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.43, 1.61] |
| 5 Re‐operations ‐ implant removal | 2 | 630 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.51, 1.96] |
| 6 Mortality ‐ 2 years | 2 | 372 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.81, 1.48] |
Comparison 18. Two Hansson pins versus sliding hip screw.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 2 Avascular necrosis | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 3 All fracture healing complications | 2 | 321 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.70, 1.25] |
| 4 Re‐operations ‐ arthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 5 Mortality ‐ 2 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6 Length of surgery | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Comparison 19. Two Hansson pins versus cancellous screws.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Non‐union | 4 | 772 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.73, 2.13] |
| 1.1 Two Hansson pins versus two Uppsala screws | 2 | 295 | Risk Ratio (M‐H, Random, 95% CI) | 2.04 [0.66, 6.24] |
| 1.2 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.40, 1.53] |
| 1.3 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.61, 1.49] |
| 2 Avascular necrosis | 4 | 772 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.43, 2.05] |
| 2.1 Two Hansson pins versus two Uppsala screws | 2 | 295 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.69, 3.21] |
| 2.2 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.36, 4.66] |
| 2.3 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.21, 1.08] |
| 3 All fracture healing complications | 5 | 872 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.77, 1.67] |
| 3.1 Two Hansson pins versus two Uppsala screws | 3 | 395 | Risk Ratio (M‐H, Random, 95% CI) | 1.50 [0.79, 2.84] |
| 3.2 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.56, 1.59] |
| 3.3 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.55, 1.13] |
| 4 Re‐operations ‐ arthroplasty | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.52, 1.04] |
| 4.1 Two Hansson pins versus two cancellous AO | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.02, 1.25] |
| 4.2 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.43, 1.34] |
| 4.3 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.53, 1.31] |
| 5 Re‐operation ‐ arthroplasty or need for arthroplasty | 3 | 587 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.58, 1.12] |
| 5.1 Two Hansson pins versus two cancellous AO | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.29, 2.22] |
| 5.2 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.43, 1.34] |
| 5.3 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.53, 1.31] |
| 6 Re‐operations ‐ implant removal | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 6.1 Two Hansson pins versus three AO screws | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Re‐operations ‐ type not specified | 2 | 379 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.73, 1.51] |
| 7.1 Two Hansson pins versus two Uppsala screws | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.76, 2.33] |
| 7.2 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.54, 1.42] |
| 8 Deep wound infection | 2 | 458 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.13, 4.45] |
| 8.1 Two Hansson pins versus two Uppsala screws | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.13, 4.45] |
| 8.2 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Superficial wound infection | 1 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [0.16, 19.43] |
| 9.1 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.78 [0.16, 19.43] |
| 10 Mortality | 5 | 882 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.68, 1.06] |
| 10.1 Two Hansson pins versus two Uppsala screws | 2 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.63 [0.38, 1.04] |
| 10.2 Two Hansson pins versus two cancellous AO | 1 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.29, 3.03] |
| 10.3 Two Hansson pins versus three AO screws | 1 | 199 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.57, 1.33] |
| 10.4 Two Hansson pins versus three Ullevaal screws | 1 | 278 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.70, 1.35] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alberts 1989.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 0 Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Stockholm, Sweden 133 patients with an intracapsular fracture. 65% of fractures were displaced Mean age: 77 years (range 39 to 99) % male: 30% | |
| Interventions | Three Nystrom nails versus three Scand screws. Nystrom nails are 6.5 mm smooth pins Scand pins are 6.5 mm cancellous threaded screws | |
| Outcomes | Length of surgery Non‐union Avascular necrosis Screw penetration Breakage of implant Superficial wound infection Deep wound infection Mortality (one and two years) | |
| Notes | The results for 15 patients entered in the study were not given as they had either 'early death' or were lost to follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Alho 1998(a).
| Methods | Method of randomisation: "random numbers in closed envelopes" Number lost to follow‐up: 6/607 (1%) ‐ this is the total number for the three studies of Alho Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Rogaland Central Hospital, Norway (one of three centres in a multicentre study) 191 patients with an intracapsular fracture. % of fractures displaced: 100% Mean age: Median 79 years (range 54 to 97) % male: 22% | |
| Interventions | Two Olmed screws versus three Ullevaal screws Olmed screws are the same as Uppsala screws with a 6 mm shank and 8 mm threads Ullevaal screws are 7 mm shank and 7 mm cancellous threaded screws |
|
| Outcomes | Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Fracture below the screws | |
| Notes | One of three centres in a multicentre study. Results for the three centres are presented separately and there was a significant difference in the characteristics of patients and re‐operations between centres as detailed in Alho 1998. Patients at Ullevaal hospital were older, those at Rogaland were more likely to live in residential accommodation and more re‐operations were undertaken at Rogaland hospital | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "Random numbers" |
| Allocation concealment? | Unclear risk | "Closed envelopes" |
Alho 1998(b).
| Methods | Method of randomisation: "random numbers in closed envelopes" Number lost to follow‐up: 6/607(1%) ‐ this is the total number for the three studies of Alho Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Akeershus, Norway (one of three centres in a multicentre study) 249 patients with an intracapsular fracture. % of fractures displaced: 100% Mean age: median 78 years (range 54 to 96) % male: 18% | |
| Interventions | Three Ullevaal screws versus two Tronzo screws Tronzo (VLF) screws are cancellous screws with a sliding capacity to allow for collapse at the fracture site; Ullevaal screws are 7 mm shank and 7 mm cancellous threaded screws |
|
| Outcomes | Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Fracture below the screws | |
| Notes | One of three centres in a multicentre study. Results for the three centres are presented separately and there was a significant difference in the characteristics of patients and re‐operations between centres as detailed in Alho 1998. Patients at Ullevaal hospital were older, those at Rogaland were more likely to live in residential accommodation and more re‐operations were undertaken at Rogaland hospital. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "Random numbers" |
| Allocation concealment? | Unclear risk | "Closed envelopes" |
Alho 1998(c).
| Methods | Method of randomisation: "random numbers in closed envelopes" Number lost to follow‐up: 6/607(1%) ‐ this is the total number for the three studies of Alho Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Ullevaal Hospital, Norway (one of three centres in a multicentre study) 167 patients with an intracapsular fracture. % of fractures displaced: 100% Mean age: median 81 years (range 56 to 97) % male: 22% | |
| Interventions | Two Olmed screws versus three Ullevaal screws Olmed screws are the same as Uppsala screws with a 6 mm shank and 8 mm threads; Ullevaal screws are 7 mm shank and 7 mm cancellous threaded screws |
|
| Outcomes | Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Fracture below the screws | |
| Notes | One of three centres in a multicentre study. Results for the three centres are presented separately and there was a significant difference in the characteristics of patients and re‐operations between centres as detailed in Alho 1998. Patients at Ullevaal hospital were older, those at Rogaland were more likely to live in residential accommodation and more re‐operations were undertaken at Rogaland hospital | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "Random numbers" |
| Allocation concealment? | Unclear risk | "Closed envelopes" |
Benterud 1997.
| Methods | Method of randomisation: not stated Number lost to follow‐up: not stated Length of follow‐up: median 39 months (range 22 to 51) | |
| Participants | Orthopaedic unit in Ullevaal, Norway 225 patients with an intracapsular fracture. % of fractures displaced: 100% (all displaced) Mean age: median 81 years (range 63 to 97) % male: 21% | |
| Interventions | Sliding hip screws supplemented with a parallel cancellous screw versus two Olmed screws Olmed screws are the same as Uppsala screws with a 6 mm shank and 8 mm threads |
|
| Outcomes | Length of surgery Operative blood loss Non‐union Avascular necrosis Re‐operations Wound infection Mortality (three months) | |
| Notes | The results for 1 patient who received the wrong implant were not included | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Christie 1988.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 8 (6.3%) Length of follow‐up: mean 33 months | |
| Participants | Orthopaedic unit in Edinburgh, Scotland, UK 127 patients with a displaced intracapsular fractureAll fractures were displaced Mean age: 69 years (range 26 to 80) % male: not stated | |
| Interventions | Sliding hip screw fixation or double divergent pins | |
| Outcomes | Non‐union Avascular necrosis Re‐operation rate Use of walking aids | |
| Notes | The results for 15 patients entered in the study were not given as they had either 'early death' or were lost to follow‐up. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Dalen 1985.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 9 (8.7%) Length of follow‐up: mean 12.6 months | |
| Participants | Orthopaedic unit in Danderyd, Sweden 94 patients with an intracapsular fracture. % of fractures displaced: not stated Mean age: 79 years (range 68 to 90) % male: 24% | |
| Interventions | Thornton nail versus three Scand pins The Thornton nail is a flanged trifin cannulated nail Scand pins are 6.5 mm cancellous threaded screws |
|
| Outcomes | Non‐union Re‐operation Intra‐articular pressure | |
| Notes | The results for 9 patients were not given because of 'technical failure of abnormalities of the opposite hip.' The report of Jacobsson relates to the intraarticular pressures for 21 of the patients | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Elmerson 1988.
| Methods | Method of randomisation: "by the surgical nurse at the time of surgery according to a table of random numbers" Number lost to follow‐up: 9(4%) Length of follow‐up: 24 months |
|
| Participants | Orthopaedic unit in Gothenburg, Sweden 223 patients with an intracapsular fracture. 74% of fractures were displaced Mean age: 77 years (range 18 to 98) % male: 30% | |
| Interventions | Three Gouffon screws versus Rydell nail Gouffon screws are 6.5 mm cancellous screws Rydell nail is a four flanged nail with a hook extruded at its tip | |
| Outcomes | Length of surgery Non‐union Avascular necrosis Superficial wound infection Deep wound infection Mortality (one and two years) | |
| Notes | The results for 20 patients entered in the study were not given as they had died within three months of fracture. No fracture healing complications were reported in this group. In 16 cases the fracture was not reducible and these were excluded as treated by a prosthesis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "by the surgical nurse at the time of surgery according to a table of random numbers" |
| Allocation concealment? | Unclear risk | "by the surgical nurse at the time of surgery according to a table of random numbers" |
Elmerson 1995.
| Methods | Method of randomisation: "random number table" Number lost to follow‐up: 3 (1.2%) Length of follow‐up: mean 24 months | |
| Participants | Orthopaedic unit in Sahlgren Hospital, Gothenburg, Sweden 222 patients with an intracapsular fracture. 55% of fractures were displaced Mean age: 77 years (range 50 to 94) % male: 31% | |
| Interventions | Sliding hip screw versus two Hansson hook pins (LIH pins) Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip |
|
| Outcomes | Length of surgery Non‐union Avascular necrosis Re‐operations for arthroplasty Mortality (two years) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "random number table" |
| Allocation concealment? | Unclear risk | not stated |
Frandsen 1981.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 21 (5.4%) Length of follow‐up: median 25 and 32 months (range median 24 to 65 months) | |
| Participants | Orthopaedic unit in Odense, Denmark 383 patients with an intracapsular fracture. 100% of fractures were displaced Median age: 78 years (range 22 to 96) % male: 22% | |
| Interventions | Thornton nail versus sliding nail plate The Thornton nail is a flanged trifin cannulated nail The sliding nail plate is similar to a sliding hip screw but has flanges instead of a lag screw. The nail is connected to the plate with a bolt |
|
| Outcomes | Non‐union Avascular necrosis | |
| Notes | The 1979 paper was a preliminary result of the study.
The Thornton nail plate fixation was referred to in the paper as Smith‐Petersen osteosynthesis. Study involved displaced fractures only |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Harper 1992.
| Methods | Method of randomisation: by even or odd numbers of patient record Number lost to follow‐up: not stated Length of follow‐up: 18 months | |
| Participants | Orthopaedic unit in Leicester, England 209 patients with an intracapsular fracture. 83% of fractures were displaced Mean age: 72 years (range 25 to 93) % male: 26% | |
| Interventions | Sliding hip screw (Ambi hip screw) versus three parallel cannulated cancellous screws (Richards Medical) | |
| Outcomes | Fracture healing complications Mortality ‐ 1 year | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | "the last digit of the patients accident and emergency number" |
| Allocation concealment? | High risk | "the last digit of the patients accident and emergency number" |
Herngren 1992.
| Methods | Method of randomisation: by "sequence of random numbers" Number lost to follow‐up: 5 (2.8%) Length of follow‐up: 12 months | |
| Participants | Orthopaedic unit in Ostersund, Sweden 180 fractures in 179 patients with an intracapsular fracture. 72% of fractures were displaced Mean age: 78 years (range 28 to 97) % male: 37% | |
| Interventions | Two Uppsala screws versus two Hansson pins Uppsala screws are 8 mm cancellous screws with a 6mm shank Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip |
|
| Outcomes | Length of surgery Non‐union Avascular necrosis Later trochanteric fracture Re‐operations Local discomfort Deep wound infection Mortality (one year) | |
| Notes | One fracture could not be reduced and was excluded as treated by a prosthesis. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "Sequence of random numbers" |
| Allocation concealment? | Unclear risk | "Sequence of random numbers" |
Holmberg 1990.
| Methods | Method of randomisation: "in the operating theatre". Exact method not stated Number lost to follow‐up: 5 (2.3%) Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Uppsala, Sweden 220 patients with an intracapsular fracture. 65% of fractures were displaced Mean age: 79 years (range 40 to 98) % male: 25% | |
| Interventions | Rydell four flanged nail versus two Hansson hook pins (LIH pins) Rydell nail is a four flanged nail with a hook extruded at its tip Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip | |
| Outcomes | Non‐union Avascular necrosis Re‐operations for arthoplasty Re‐operations for implant removal Mortality at 2 years Failure to return home | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "in the operating theatre". Exact method not stated |
| Allocation concealment? | Unclear risk | "in the operating theatre". Exact method not stated |
Kuokkanen 1991.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 0 Length of follow‐up: mean 24 months (range 17 to 35 months) | |
| Participants | Orthopaedic unit in Helsinki, Finland 33 patients with an intracapsular fracture. % of fractures displaced: none (all undisplaced) Mean age: 66 years (range 21 to 84) % male: not stated | |
| Interventions | Sliding hip screw versus three cannulated cancellous screws (Mercon) Mercon screws are 6.5 mm cancellous threaded screws | |
| Outcomes | Non‐union Avascular necrosis Screw penetration Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Deep wound infection Length of surgery Operative blood loss Mortality Harris hip score | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Lagerby 1998.
| Methods | Method of randomisation: "in block of four using a closed envelope system. The envelopes were drawn in sequential order" Number lost to follow‐up: 28 (10.4%) Length of follow‐up: 12 months | |
| Participants | Orthopaedic unit in Vasteras, Sweden 268 fractures in 266 patients with an intracapsular fracture. 72% of fractures were displaced Mean age: 80 years (range 31 to 99) % male: 33% | |
| Interventions | Three Richards screws versus two Uppsala screws Richards screws are 4.8 mm shaft and 6.86 mm thread diameter Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip | |
| Outcomes | Non‐union Avascular necrosis Screw penetration Re‐operations ‐ arthroplasty Mortality Pain Use of walking aids | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "in block of four using a closed envelope system. The envelopes were drawn in sequential order" |
| Allocation concealment? | Unclear risk | "in block of four using a closed envelope system. The envelopes were drawn in sequential order" |
Lindequist 1989.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 6 (2.7%) Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Galve, Sweden 220 patients with an intracapsular fracture. 80% of fractures were displaced Mean age: 77 years (range 32 to 97) % male: 29% | |
| Interventions | Gouffon pins versus von Bahr screws versus Hessel pins Number of screws/pins used not stated Gouffon pins are 6.5 mm cancellous screws von Bahr screws are 7 mm cancellous screws with a 5.5 mm shank Hessel pins are 6.5 mm diameter smooth pins | |
| Outcomes | Non‐union Avascular necrosis Superficial wound infection Deep wound infection Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Mortality (two years) | |
| Notes | The study was in two parts. Firstly von Bahr screws versus Hessel pins and then von Bahr screws versus Gouffon screws. Results of von Bahr screws for the two parts were presented together. The paper reported that there was no difference in the failure rate for the screws between the first and second parts | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Lykke 2003.
| Methods | Method of randomisation: "numbered sealed opaque envelopes in blocks of 50" Number lost to follow‐up: not stated Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Oslo, Norway 278 intracapsular fracture. 72% of fractures were displaced Mean age: 82 years (range 27 to 101) % male: 18% | |
| Interventions | Two Hansson hook‐pins versus three Ullevaal hip screws Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip Ullevaal screws are 7 mm shank and 7 mm cancellous threaded screws | |
| Outcomes | Non‐union and early fracture displacement Avascular necrosis Re‐operations ‐ arthroplasty Superficial wound sepsis Deep wound sepsis Wound haematoma Deep vein thrombosis Pneumonia Mortality ‐ up to two years Pain Return to the same residential status Length of hospital stay (mean or median) Drill penetration of the femoral head | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "numbered sealed opaque envelopes in blocks of 50" |
| Allocation concealment? | Low risk | "numbered sealed opaque envelopes in blocks of 50" |
Madsen 1987.
| Methods | Method of randomisation: not stated Number lost to follow‐up: not stated Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Esbjerg, Denmark 103 patients with an intracapsular fracture. 100% of fractures were displaced Mean age: 74 years (range 25 to 92) % male: 24% | |
| Interventions | Sliding hip screw versus four AO cancellous screws AO screws are have 6.5 mm cancellous threads | |
| Outcomes | Length of surgery Operative blood loss Non‐union and early fracture displacement Avascular necrosis Re‐operations ‐ arthroplasty Re‐operations ‐ removal Deep wound infection Bone scintigraphy | |
| Notes | The 1986 paper related solely to the results of bone scintigraphy for 87 of the patients One patient died after randomisation and before surgery | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Mjorud 2006.
| Methods | Method of randomisation: "in blocks of 50 with sealed numbered envelopes" Number lost to follow‐up: not stated Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Lund, Sweden 199 patients with an intracapsular fracture. 65% of fractures were displaced Mean age: 81 years (range 28 to 101) % male: 24% | |
| Interventions | Two Hansson hook pins versus three titanium AO cancellous screws | |
| Outcomes | Length of surgery Poor implant positioning Drill penetration at surgery Non‐union and early fracture displacement Avascular necrosis Re‐operations ‐ arthroplasty Re‐operations ‐ removal Re‐operations ‐ Girdlestone excision arthroplasty Length of hospital stay Mortality Walking ability | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "in blocks of 50 with sealed numbered envelopes" |
| Allocation concealment? | Unclear risk | "in blocks of 50 with sealed numbered envelopes" |
Nordkild 1985.
| Methods | Method of randomisation: "odd and even numbers" Number lost to follow‐up: 0 Length of follow‐up: median 40 months (range 1 to 64) | |
| Participants | Orthopaedic unit in Copenhagen, Denmark 49 patients with an intracapsular fracture 78% of fractures were displaced Mean age: 62 years (range 32 to 86) % male: 33% | |
| Interventions | Sliding hip screw versus sliding nail plate The sliding nail plate has a trifin tip and sliding can occur between this and the outer barrel similar to a sliding hip screw. The barrel is attached to a short plate using a locking bolt. | |
| Outcomes | Non‐union Avascular necrosis Re‐operations Pain Range of movement of the hip Use of walking aids Bone scintigraphy | |
| Notes | A significant difference in mean ages was noted between groups, with those allocated to the nail plate group being younger (P < 0.025) The 1987 paper was for 35 of the patients who had bone scintigraphy performed at 6 weeks, 3, 6 and 12 months | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | "odd and even numbers were used" |
| Allocation concealment? | High risk | "Odd and even number were used" |
Olerud 1991.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 0 Length of follow‐up: 12 months | |
| Participants | Orthopaedic unit in Uppsala, Sweden 115 patients with an intracapsular fracture 71% of fractures were displaced Mean age: 80 years (range not stated) % male: 16% | |
| Interventions | Two Hansson pins versus two Uppsala screws Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip Uppsala screws are 8 mm cancellous screws with a 6 mm shank | |
| Outcomes | Non‐union Avascular necrosis Mortality (one year) Pain Mobility Failure to return to same residence | |
| Notes | Study conducted in the institution were one of the methods of internal fixation was originated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Ovesen 1997.
| Methods | Method of randomisation: not stated Number lost to follow‐up: not stated Length of follow‐up: mean 24 months | |
| Participants | Orthopaedic unit in Odense, Denmark 316 fractures in 314 patients with an intracapsular fracture. 80% of fractures were displaced Mean age: not stated (range not stated) % male: not stated | |
| Interventions | Two Uppsala screws versus sliding hip screw Uppsala screws are 8 mm cancellous screws with a 6 mm shank | |
| Outcomes | Fracture healing complications Length of surgery Operative blood loss Re‐operations ‐ arthroplasty Length of hospital stay Mortality | |
| Notes | Reported only as a conference abstract | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Parker 2010.
| Methods | Method of randomisation: "single toss of a coin" Number lost to follow‐up: 2 Length of follow‐up: 12 months | |
| Participants | Orthopaedic unit in Peterborough, UK 432 patients with an intracapsular fracture. 44% of fractures were displaced Mean age: 77 years (range 29 to 99) % male: 23% | |
| Interventions | Three 16 mm threaded 6.5 mm cannulated cancellous AO screws versus three 32 mm threaded 6.5 mm cannulated cancellous AO screws | |
| Outcomes | Non‐union Avascular necrosis Fracture below the implant Re‐operations Pain at follow‐up Failure to return to same residence Failure to regain mobility Mortality | |
| Notes | Additional methodological and results provided by Martyn Parker in response to letter from Helen Handoll | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Randomised by "by the single toss of a coin, heads to 6.5 mm cancellous screws with short threads (16 mm) and tails to long threads (32 mm)" |
| Allocation concealment? | Unclear risk | Coin toss was done on the ward by surgeon (information from lead investigator) |
Paus 1986.
| Methods | Method of randomisation: "coded envelopes" Number lost to follow‐up: 0 Length of follow‐up: mean 28 months (range 13 to 41) | |
| Participants | Orthopaedic unit in Aker 131 patients with an intracapsular fracture. 100% of fractures were displaced Mean age: 69 years (all patients aged less than 80 years. Range not stated) % male: 18% | |
| Interventions | Two von Bahr screws versus two sliding hip screws von Bahr screws are 7 mm cancellous screws with a 5.5 mm shank | |
| Outcomes | Non‐union Avascular necrosis Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Deep wound infection Length of surgery Mortality (during follow‐up) | |
| Notes | Study restricted to patients aged less than 80 years | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | "after the x‐ray examinations by selecting a previously coded envelope containing direction of type of operation" |
| Allocation concealment? | Unclear risk | "after the x‐ray examinations by selecting a previously coded envelope containing direction of type of operation" |
Rehnberg 1989.
| Methods | Method of randomisation: "a table of random numbers and they were also matched with respect to age, fracture type and living conditions" Number lost to follow‐up: 0 Length of follow‐up: 12 months | |
| Participants | Orthopaedic unit in Uppsala, Sweden 222 patients with an intracapsular fracture. 77% of fractures were displaced Mean age: 80 years (range 55 to 98) % male: 25% | |
| Interventions | Two von Bahr screws versus two Uppsala screws von Bahr screws are 7 mm cancellous screws with a 5.5 mm shank Uppsala screws are 8 mm cancellous screws with a 6 mm shank | |
| Outcomes | Non‐union Avascular necrosis Screw penetration Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Length of surgery Operative blood loss Mortality (one year) Pain Use of walking aids Failure to return to same residence | |
| Notes | Study conducted in the institution were one of the methods of internal fixation was originated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "a table of random numbers and they were also matched with respect to age, fracture type and living conditions" |
| Allocation concealment? | Unclear risk | "a table of random numbers and they were also matched with respect to age, fracture type and living conditions" |
Sernbo 1990.
| Methods | Method of randomisation: "in the operating theatre by a random number generator" Number lost to follow‐up: 1 (0.2%) Length of follow‐up: mean 24 months | |
| Participants | Orthopaedic unit in Malmo, Sweden 410 patients with an intracapsular fracture. 75% of fractures were displaced Mean age: 77 years (range not stated) % male: 25% | |
| Interventions | Rydell four flanged nail versus two Hansson hook pins (LIH pins) Rydell nail is a four flanged nail with a hook extruded at its tip Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip | |
| Outcomes | Length of surgery Radiographic screening time Operative blood loss Non‐union Avascular necrosis Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Length of hospital stay Failure to return home | |
| Notes | Figures for number of complications and re‐operations were inferred from table of figures which gave percentages | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | "in the operating theatre by a random number generator" |
| Allocation concealment? | Unclear risk | "in the operating theatre by a random number generator" |
Sorensen 1992.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 1 (1.4%) Length of follow‐up: mean 36 months | |
| Participants | Orthopaedic unit in Hellerup, Denmark 73 patients with an intracapsular fracture. 86% of fractures were displaced Mean age: 77 years (range 52 to 94) % male: 25% | |
| Interventions | Sliding hip screw versus three Gouffon screws Gouffon pins are 6.5 mm cancellous screws | |
| Outcomes | Non‐union Avascular necrosis Re‐operations ‐ arthroplasty Re‐operations ‐ implant removal Mortality (three years) | |
| Notes | Trial was discontinued early due to higher failure rate in the Gouffon screw group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Sorensen 1996.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 14 (9.3%) Length of follow‐up: mean 12 months | |
| Participants | Orthopaedic unit in Gentofte, Denmark 150 patients with an intracapsular fracture. 67% of fractures were displaced Mean age: 80 years (range 47 to 94) % male: 25% | |
| Interventions | Sliding hip screw versus two Hansson hook pins (LIH pins) versus two Uppsala screws Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip Uppsala screws are 8 mm cancellous screws with a 6 mm shank | |
| Outcomes | Total radiographic complications (penetration, early loosening, non‐union, avascular necrosis) | |
| Notes | Reported as a conference abstract only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Not stated |
| Allocation concealment? | Unclear risk | Not stated |
Stromquist 1988.
| Methods | Method of randomisation: even or odd date of birth Number lost to follow‐up: 3 (3.6%) Length of follow‐up: 4 months | |
| Participants | Orthopaedic unit in Helsingborg, Sweden 110 patients with an intracapsular fracture. 64% of fractures were displaced Mean age: 77 years (range 32 to 92) % male: 25% | |
| Interventions | Two AO screws versus two Hansson hook pins AO screws are have 6.5 mm cancellous threads Hansson hook pins (LIH) are 6.5 mm diameter smooth pins with a hook which is extruded at its tip | |
| Outcomes | Re‐operation Need for re‐operation ‐ arthroplasty Mortality (4 months) Bone scintimetry | |
| Notes | Study translated from article in French courtesy of Celine Froidevaux | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | Even or odd date of birth |
| Allocation concealment? | High risk | Even or odd date of birth |
Stromqvist 1984.
| Methods | Method of randomisation: even or odd date of birth Number lost to follow‐up: 0 Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Lund, Sweden 152 patients with an intracapsular fracture. 72% of fractures were displaced Mean age: 78 years (range 52 to 95) % male: not stated | |
| Interventions | Rydell four flanged nail versus two Hansson hook pins (LIH pins) Rydell nail is a four flanged nail with a hook extruded at its tip Hansson hook pins are 6.5 mm diameter smooth pins with a hook which is extruded at its tip | |
| Outcomes | Non‐union Avascular necrosis Re‐operations Deep wound infection Mortality at two years Bone scintimetry | |
| Notes | Lars Hansson, one of the paper's co‐authors, was the inventor of the Hansson pin The 1983 paper related to the results of post‐operative bone scintimetric evaluation for 134 of the patients |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | High risk | “AO screws were inserted if they were born on an even day, and with hook pins if they were born on an odd day” |
| Allocation concealment? | High risk | “AO screws were inserted if they were born on an even day, and with hook pins if they were born on an odd day” |
Svenningsen 1984.
| Methods | Method of randomisation: not stated Number lost to follow‐up: 7 (2.7%) Length of follow‐up: mean 36 months | |
| Participants | Orthopaedic unit in Trondheim, Norway 255 patients with an intracapsular fracture. 69% of fractures were displaced Mean age: 71 years (range not stated) % male: 25% | |
| Interventions | Sliding compression screw plate versus McLaughlin nail plate The compression screw plate was similar to a short one hole plate sliding hip screw with an additional screw proximally and a compression device incorporated into the plate barrel The nail plate used was a Thornton trifin nail connected to a side plate by a locking bolt |
|
| Outcomes | Non‐union Avascular necrosis Re‐operations ‐ implant removal Superficial wound infection Deep wound infection Length of surgery Fall in haemoglobin Mortality Length of hospital stay | |
| Notes | The trial also has a prosthesis group. Results for this part of the study are included within the Cochrane review of internal fixation versus arthroplasty for intracapsular fractures. Subgroup of patients aged over 70 years reported in addition in the paper of Svenningsen 1985 | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | not stated |
| Allocation concealment? | Unclear risk | not stated |
Wihlborg 1990.
| Methods | Method of randomisation: "sealed envelopes" Number lost to follow‐up: 0 Length of follow‐up: 24 months | |
| Participants | Orthopaedic unit in Ljungby, Sweden 200 patients with an intracapsular fracture. 83% of fractures were displaced Mean age: 77 years (range 46 to 100) % male: 29% | |
| Interventions | Three Gouffon pins versus Rydell four flanged nail Gouffon pins are 6.5 mm cancellous screws The Rydell nail is a four flanged nail with a hook extruded at its tip |
|
| Outcomes | Non‐union Avascular necrosis Re‐operations Mortality (one and two years) | |
| Notes | Once randomised, patients were allocated to a surgeon who was familiar with the implant to which the patient had been allocated to receive | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | “randomized cards indicating the group of surgeons to which the patient was to be allocated were kept in sealed envelopes that were opened on the day of the operation” |
| Allocation concealment? | Unclear risk | “randomized cards indicating the group of surgeons to which the patient was to be allocated were kept in sealed envelopes that were opened on the day of the operation” |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ingwersen 1992 | This prospective randomised trial was reported only as a conference abstract. The study compared 100 patients treated with either two Olmed screws or two Richards screws. Twenty‐six patients were subsequently excluded for the operation being the wrong indication (9), died (12) or lost to follow‐up (5). Follow‐up was for only three months (range two to six months). No loss of fixation was reported in the undisplaced fractures. For the displaced fracture 're‐dislocation' was reported in 14/29 of the Olmed screws and 23/31 of the Richard screws. The study was excluded as there was only a limited follow‐up and inadequate reporting of results. |
| Jukkala‐Partio 2000 | This was a comparative study of 40 patients in which their intracapsular fracture was fixed with metallic screws and 40 patients who had their fracture fixed with three bioabsorbable screws. For undisplaced fracture non‐union occurred in 5/29 and 8/29 for the bioabsorbable screws versus the metal screws. For displaced fractures non‐union occurred in 6/11 cases for both groups. Walking ability and range of movement were reported to be better after the bioabsorbable fixation. The study was excluded as there was no randomisation of patients. |
| Poulsen 1995 | This is a retrospective review of 182 patients treated at one centre where one department treated the patients by sliding screw plate and the other department used the sliding hip screw. It was excluded, as it was not a randomised controlled trial. |
| Sernbo 1986 | This randomised trial reported only as a conference abstract involved 300 patients with an intracapsular fracture randomised to either the Rydell nail or three cannulated screws. After one and two years there was 'no significant difference' in the mortality, walking capacity or social rehabilitation between the two groups. Complications of displacement, avascular necrosis and pseudarthrosis occurred in 36% of the Rydell group and 30% of the cannulated screw group, with re‐operations in 20% of the Rydell group and 16% of the screw group. The study was excluded as because there was inadequate reporting of results within the conference abstract and no mention of the number of patients in each group. |
Characteristics of ongoing studies [ordered by study ID]
FAITH.
| Trial name or title | Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH): a multi‐centre randomised trial comparing sliding hip screws and cancellous screws on revision surgery rates and quality of life in the treatment of femoral neck fractures |
| Methods | A multi‐centre randomised trial |
| Participants | Patients with an intracapsular fracture that is to be treated by internal fixation |
| Interventions | Comparing sliding hip screws and cancellous screws |
| Outcomes | Primary outcome measures: Revision surgery Secondary outcome measures: Function, quality of life, complications, including mortality, avascular necrosis, nonunion, implant breakage or failure, implant removal after fracture healing to minimize pain, and infection. |
| Starting date | March 2009 |
| Contact information | Julie Agel, MA 612‐273‐8052 (agelx001@umn.edu) |
| Notes | Predicted end date March 2013 |
Differences between protocol and review
In the update of the review (2011), two aspects of risk of bias were assessed and reported: sequence generation and allocation concealment. We also modified our former scheme for assessment methodological quality, mainly adding in an item for sequence generation.
Contributions of authors
Martyn Parker initiated and designed the review, read all studies, extracted data and compiled the first drafts. Kurinchi Gurusamy checked data from the newly studies identified for the first and second update. Martyn Parker is the guarantor of the review.
Sources of support
Internal sources
Scottish Home and Health Department, UK.
External sources
No sources of support supplied
Declarations of interest
Martyn Parker was the lead author of one of the studies included in this review (Parker 2010). The assessment of this study was undertaken by Kurinchi Gurusamy and Helen Handoll. Martyn Parker has received and may continue to receive financial payment from manufacturing companies of orthopaedic implants used for the internal fixation of hip fractures and for attending meeting organised by these companies and for advising on the design and use of hip fracture implants. Kurinchi Gurusamy has no connection with any manufacturing company.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Alberts 1989 {published data only}
- Alberts KA, Jaerveus J, Zyto K. Nail versus screw fixation of femoral neck fractures. A 2‐year radiological and clinical prospective study. Annales Chirurgiae et Gynaecologiae 1989;78:298‐303. [PubMed] [Google Scholar]
Alho 1998(a) {published data only}
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Biases in a randomized comparison of three types of screw fixation in displaced femoral neck fractures. Acta Orthopaedica Scandinavica 1998;69(5):463‐8. [DOI] [PubMed] [Google Scholar]
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Problems in orthopedic multicenter studies ‐ screw fixation of displaced femoral neck fracture [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1998;282:11. [DOI] [PubMed] [Google Scholar]
- Austdal S, Benterud JG, Blikra G, Kuokkanen H, Lindequist S, Lerud P, et al. Osteosynthesis of displaced femoral neck fractures with multiple screws ‐ a randomised multicenter study [abstract]. Journal of Bone and Joint Surgery. British Volume 1993;75 Suppl 2:199. [Google Scholar]
- Benterud J, Alho A. Multiple screw fixation for displaced femoral neck fractures ‐ a multicentre study [abstract]. Journal of Bone and Joint Surgery. British Volume 1995;77 Suppl 2:214. [Google Scholar]
- Benterud JG, Blikra G, Lerud P, Raugstad TS, Austdal S, Lindequist S, et al. Multicentre randomized study on osteosynthesis of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1994;260:32‐3. [Google Scholar]
- Benterud JG, Blikra G, Lerud P, Raugstad TS, Austdal S, Lindequist S, et al. Multicentric randomized study on screw osteosynthesis of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1992;248:85. [Google Scholar]
Alho 1998(b) {published data only}
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Biases in a randomized comparison of three types of screw fixation in displaced femoral neck fractures. Acta Orthopaedica Scandinavica 1998;69(5):463‐8. [DOI] [PubMed] [Google Scholar]
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Problems in orthopedic multicenter studies ‐ screw fixation of displaced femoral neck fracture [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1998;282:11. [DOI] [PubMed] [Google Scholar]
- Austdal S, Benterud JG, Blikra G, Kuokkanen H, Lindequist S, Lerud P, et al. Osteosynthesis of displaced femoral neck fractures with multiple screws ‐ a randomised multicenter study [abstract]. Journal of Bone and Joint Surgery. British Volume 1993;75 Suppl 2:199. [Google Scholar]
- Benterud J, Alho A. Multiple screw fixation for displaced femoral neck fractures ‐ a multicentre study [abstract]. Journal of Bone and Joint Surgery. British Volume 1995;77 Suppl 2:214. [Google Scholar]
- Benterud JG, Blikra G, Lerud P, Raugstad TS, Austdal S, Lindequist S, et al. Multicentre randomized study on osteosynthesis of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1994;260:32‐3. [Google Scholar]
- Benterud JG, Blikra G, Lerud P, Raugstad TS, Austdal S, Lindequist S, et al. Multicentric randomized study on screw osteosynthesis of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1992;248:85. [Google Scholar]
Alho 1998(c) {published data only}
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Biases in a randomized comparison of three types of screw fixation in displaced femoral neck fractures. Acta Orthopaedica Scandinavica 1998;69(5):463‐8. [DOI] [PubMed] [Google Scholar]
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Problems in orthopedic multicenter studies ‐ screw fixation of displaced femoral neck fracture [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1998;282:11. [DOI] [PubMed] [Google Scholar]
- Austdal S, Benterud JG, Blikra G, Kuokkanen H, Lindequist S, Lerud P, Raugstad TS, Alho A. Osteosynthesis of displaced femoral neck fractures with multiple screws ‐ a randomised multicenter study [abstract]. Journal of Bone and Joint Surgery. British Volume 1993;75 Suppl 2:199. [Google Scholar]
- Benterud J, Alho A. Multiple screw fixation for displaced femoral neck fractures ‐ a multicentre study [abstract]. Journal of Bone and Joint Surgery. British Volume 1995;77 Suppl 2:214. [Google Scholar]
- Benterud JG, Blikra G, Lerud P, Raugstad TS, Austdal S, Lindequist S, et al. Multicentre randomized study on osteosynthesis of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1994;260:32‐3. [Google Scholar]
- Benterud JG, Blikra G, Lerud P, Raugstad TS, Austdal S, Lindequist S, et al. Multicentric randomized study on screw osteosynthesis of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1992;248:85. [Google Scholar]
Benterud 1997 {published data only}
- Alho A, Benterud JG, Ronningen H, Hoiseth A. Prediction of disturbed healing in femoral neck fracture: radiographic analysis of 149 cases. Acta Orthopaedica Scandinavica 1992;63(6):639‐44. [DOI] [PubMed] [Google Scholar]
- Benterud JG, Alho A. Displaced femoral neck fracture treated with HCS or Olmed screws ‐ 225 randomized patients followed for 3 years [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1994;256:18. [Google Scholar]
- Benterud JG, Husby T, Nordsletten L, Alho A. Fixation of displaced femoral neck fractures with a sliding screw plate and a cancellous screw or two Olmed screws ‐ A prospective, randomized study of 225 elderly patients with a 3‐year follow‐up. Annales Chirurgiae et Gynaecologiae 1997;86(4):338‐42. [PubMed] [Google Scholar]
Christie 1988 {published data only}
- Christie J, Howie CR, Armour PC. Fixation of displaced subcapital femoral fractures. Compression screw fixation versus double divergent pins. Journal of Bone and Joint Surgery. British Volume 1988;70(2):199‐201. [DOI] [PubMed] [Google Scholar]
- Howie CR, Christie J, Watson H. A prospective randomised trial of compression screw fixation versus double divergent pin fixation for displaced subcapital fracture of the femur [abstract]. Journal of Bone and Joint Surgery. British Volume 1987;69(3):490. [Google Scholar]
Dalen 1985 {published data only}
- Dalen N, Jacobsson B. Factors influencing the incidence of reoperation after femoral neck fractures. International Orthopaedics 1985;9:235‐7. [DOI] [PubMed] [Google Scholar]
- Jacobsson B, Dalen N, Jonsson B, Ackerholm P. Intraarticular pressure during operation of cervical hip fractures. Acta Orthopaedica Scandinavica 1988;59(1):16‐8. [DOI] [PubMed] [Google Scholar]
Elmerson 1988 {published data only}
- Elmerson S, Gunnar BJ, Andersson J, Irstam L, Zetterberg C. Internal fixation of femoral neck fracture. No difference between the Rydell four‐flanged nail and Gouffon's pins. Acta Orthopaedica Scandinavica 1988;59(4):372‐6. [DOI] [PubMed] [Google Scholar]
Elmerson 1995 {published data only}
- Elmerson S, Sjostedt A, Zetterberg C. Fixation of femoral neck fracture. A randomized 2‐year follow‐up study of hook pins and sliding screw plate in 222 patients. Acta Orthopaedica Scandinavica 1995;66(6):507‐10. [DOI] [PubMed] [Google Scholar]
Frandsen 1981 {published data only}
- Frandsen PA. Osteosynthesis of displaced fractures of the femoral neck. A comparison between Smith‐Petersen Osteosynthesis and sliding‐nail‐plate osteosynthesis ‐ a radiological study. Acta Orthopaedica Scandinavica 1979;50(4):443‐9. [DOI] [PubMed] [Google Scholar]
- Frandsen PA, Andersen Jr PE. Treatment of displaced fractures of the femoral neck. Smith‐Petersen osteosynthesis versus sliding‐nail‐plate osteosynthesis. Acta Orthopaedica Scandinavica 1981;52(5):547‐52. [DOI] [PubMed] [Google Scholar]
Harper 1992 {published data only}
- Harper WM. A prospective randomised trial comparing multiple parallel cannulated screws with a sliding hip screw and plate. In 'Treatment of intracapsular proximal femoral fractures'. Thesis. Leicester: University of Leicester, 1994:158‐86.
- Harper WM, Gregg PJ. The treatment of intracapsular proximal femoral fractures: a randomized prospective trial [abstract]. Journal of Bone and Joint Surgery. British Volume 1992;74 Suppl 3:282. [Google Scholar]
Herngren 1992 {published data only}
- Herngren B, Mork‐Petersen F, Bauer M. Uppsala screws or Hansson pins for internal fixation of femoral neck fractures? A prospective study of 180 cases. Acta Orthopaedica Scandinavica 1992;63(1):41‐6. [DOI] [PubMed] [Google Scholar]
Holmberg 1990 {published data only}
- Holmberg S, Mattsson P, Dahlborn M, Ersmark H. Fixation of 220 femoral neck fractures. A prospective comparison of the Rydell nail and the LIH hook pins. Acta Orthopaedica Scandinavica 1990;61(2):154‐7. [DOI] [PubMed] [Google Scholar]
Kuokkanen 1991 {published data only}
- Kuokkanen H, Korkala O, Antti‐Poika I, Tolonen J, Lehtimaki MY, Silvennoinen T. Three cancellous bone screws versus a screw‐angle plate in the treatment of Garden I and II fractures of the femoral neck. Acta Orthopaedica Belgica 1991;57:53‐7. [PubMed] [Google Scholar]
Lagerby 1998 {published data only}
- Lagerby M, Asplund S, Ringqvist I. Cannulated screws for fixation of femoral neck fractures: No difference between Uppsala screws and Richards screws in a randomized prospective study of 268 cases. Acta Orthopaedica Scandinavica 1998;69(4):387‐91. [DOI] [PubMed] [Google Scholar]
Lindequist 1989 {published data only}
- Lindequist S, Malmqvist B, Ullmark G. Fixation of femoral neck fracture. Prospective comparison of von Bahr screws, Gouffon screws and Hessel pins [published erratum appears in Acta Orthopaedica Scandinavica 1989 Aug;60(4):507‐508]. Acta Orthopaedica Scandinavica 1989;60(3):293‐8. [DOI] [PubMed] [Google Scholar]
Lykke 2003 {published data only}
- Lykke N, Lerud PJ, Stromsoe K, Thorngren K‐G. Fixation of fracture of the femoral neck: a prospective, randomised trial of three Ullevaal hip screws versus two Hansson hook‐pins. Journal of Bone Joint Surgery. British Volume 2003;85:426‐30. [DOI] [PubMed] [Google Scholar]
Madsen 1987 {published data only}
- Linde F, Andersen E, Hvass I, Madsen F, Pallesen R. Avascular femoral head necrosis following fracture fixation. Injury 1986;17:159‐63. [DOI] [PubMed] [Google Scholar]
- Madsen F, Linde F, Andersen E, Birke H, Hvass I, Poulsen TD. Fixation of displaced femoral neck fractures. A comparison between sliding screw plate and four cancellous bone screws. Acta Orthopaedica Scandinavica 1987;58:212‐6. [DOI] [PubMed] [Google Scholar]
- Madsen F, Linde F, Andersen E, Birke H, Hvass I, Poulsen TD. Sliding screw plate versus four ASIF cancellous bone screws in the treatment of displaced femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica 1986;57:598‐9. [DOI] [PubMed] [Google Scholar]
Mjorud 2006 {published data only}
- Mjorud J, Skaro O, Solhaug JH, Thorngren K‐G. A randomised study in all cervical hip fractures. Osteosynthesis with Hansson hook‐pins versus AO‐screws in 199 consecutive patients followed for two years. Injury 2006;37(8):768‐77. [DOI] [PubMed] [Google Scholar]
Nordkild 1985 {published data only}
- Nordkild P, Sonne‐Holm S, Jensen JS. Femoral neck fracture: sliding screw plate versus sliding nail plate ‐a randomized trial. Injury 1985;16:449‐54. [DOI] [PubMed] [Google Scholar]
- Sonne‐Holm S, Nordkild P, Dyrbye M, Jensen JS. The predictive value of bone scintigraphy after internal fixation of femoral neck fractures. Injury 1987;18:33‐5. [DOI] [PubMed] [Google Scholar]
- Sonne‐Holm S, Nordkild P, Dyrbye M, Jensen JS. The predictive value of bone scintigraphy after internal fixation of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica 1986;57:181. [Google Scholar]
Olerud 1991 {published data only}
- Hellqvist E, Olerud C, Rehnberg L. Hansson pins vs Uppsala screws in treating femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1990;61(237):56. [Google Scholar]
- Olerud C, Rehnberg L. Femoral neck fractures: Swedish experience. In: Marti RK, Dunki Jacobs PB editor(s). Proximal femoral fractures: operative techniques and complications. Vol. 1, London: Medical Press, 1993:219‐40. [Google Scholar]
- Olerud C, Rehnberg L, Hellquist E. Internal fixation of femoral neck fractures. Two methods compared. Journal of Bone and Joint Surgery. British Volume 1991;73:16‐9. [DOI] [PubMed] [Google Scholar]
Ovesen 1997 {published data only}
- Ovesen O, Poulsen TD, Andersen I. Uppsala screws versus dynamic hip screw for internal fixation of femoral neck fractures [abstract]. Journal of Bone and Joint Surgery. British Volume 1997;79 Suppl 2:244. [Google Scholar]
- Ovesen O, Poulsen TD, Andersen I, Jensen PE, Damholt UW. Uppsala screws versus dynamic hip screw for internal fixation of femoral neck fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1997;274:40. [Google Scholar]
Parker 2010 {published data only}
- Parker MJ. personal communication October 29 2010.
- Parker MJ, Ali SM. Short versus long thread cannulated cancellous screws for intracapsular hip fractures: a randomised trial of 432 patients. Injury 2010;41(4):382‐4. [DOI] [PubMed] [Google Scholar]
Paus 1986 {published data only}
- Paus A, Gjengedal E, Hareide A, Jorgensen JJ. Dislocated fractures of the femoral neck treated with von Bahr screws or hip compression screw. Results of a prospective, randomized study. Journal of the Oslo City Hospitals 1986;36:55‐61. [PubMed] [Google Scholar]
Rehnberg 1989 {published data only}
- Olerud C, Rehnberg L. Femoral neck fractures: Swedish experience. In: Marti Rk, Dunki Jacobs PB editor(s). Proximal femoral fractures: operative techniques and complications. Vol. 1, London: Medical Press, 1993:207‐19. [Google Scholar]
- Rehnberg L, Olerud C. A new method for osteosynthesis prevents early complications in cervical hip fractures [Ny osteosyntesmetod minskar de tidiga komplikationerna vid cervikala hoftfrakturer]. Lakartidningen 1988;85:3820‐1. [MEDLINE: ] [PubMed] [Google Scholar]
- Rehnberg L, Olerud C. Femoral neck fractures: A prospective randomized comparison of von Bahr and Uppsala screws [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1990;237:55. [Google Scholar]
- Rehnberg L, Olerud C. Fixation of femoral neck fractures. Comparison of the Uppsala and von Bahr screws. Acta Orthopaedica Scandinavica 1989;60:579‐84. [DOI] [PubMed] [Google Scholar]
Sernbo 1990 {published data only}
- Sernbo I, Holmquist H, Redlund‐Johnell I, Johnell O. Radiographic prediction of failure after fixation of cervical hip fracture. Acta Orthopaedica Scandinavica 1994;65(3):295‐8. [DOI] [PubMed] [Google Scholar]
- Sernbo I, Johnell O, Baath L, Nilsson JA. Internal fixation of 410 cervical hip fractures. A randomized comparison of a single nail versus two hook‐pins. Acta Orthopaedica Scandinavica 1990;61(5):411‐4. [DOI] [PubMed] [Google Scholar]
Sorensen 1992 {published data only}
- Sorensen JL, Varmarken JE, Bomler J. Internal fixation of femoral neck fractures. Dynamic Hip and Gouffon screws compared in 73 patients. Acta Orthopaedica Scandinavica 1992;63(3):288‐92. [DOI] [PubMed] [Google Scholar]
- Varmarken JE, Sorensen JL, Bomler J. Internal fixation of femoral neck fractures; a randomised comparison of Dynamic Hip Screw and Gouffon Pins [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1992;63(247):35‐6. [DOI] [PubMed] [Google Scholar]
Sorensen 1996 {published data only}
- Sorensen AI, Scavenius M, Aagaard H, Ronnebech J, Torholm C. Dynamic hip screw versus Hook‐pins versus Uppsala screws in treatment of fracture of the cervical neck [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1996;267:30. [Google Scholar]
Stromquist 1988 {published data only}
- Roos H, Hansson LI, Ohlin P, Stromquist B. Screws or hook pins in femoral neck fracture fixation? [abstract]. Acta Orthopaedica Scandinavica 1986;57:250. [Google Scholar]
- Stromquist B, Roos H, Hansson LI, Ohlin P. Fixation of fractures of the femoral neck using screws or hook‐pins. Radionuclide study and short‐term results [Fixation des fractures du col femoral par vissage ou "broches en crochet". Etude scintimetrique et resultats a court terme. Fixation des fractures du col femoral par vissage ou "broches en crochet". Etude scintimetrique et resultats a court terme.]. Revue de Chirurgie Orthopedique et Reparatrice de L'appareil Moteur 1988;74:609‐13. [MEDLINE: ] [PubMed] [Google Scholar]
Stromqvist 1984 {published data only}
- Stromqvist B. Femoral head vitality after intracapsular hip fracture. 490 cases studied by intravital tetracycline labelling and Tc‐MDP radionuclide imaging. Acta Orthopaedica Scandinavica 1983;54(Suppl 200):17. [PubMed] [Google Scholar]
- Stromqvist B, Hansson LI, Nilsson LT, Thorngren K‐G. Two‐year follow‐up of femoral neck fractures with special reference to type of osteosynthesis. Acta Orthopaedica Scandinavica 1984;55:712‐3. [DOI] [PubMed] [Google Scholar]
- Stromqvist B, Hansson LI, Nilsson LT, Thorngren KG. Two‐year follow‐up of femoral neck fractures. Comparison of osteosynthesis methods. Acta Orthopaedica Scandinavica 1984;55:521‐5. [DOI] [PubMed] [Google Scholar]
- Stromqvist B, Hansson LI, Palmer J, Ceder L, Thorngren KG. Scintimetric evaluation of nailed femoral neck fractures with special reference to type of osteosynthesis. Acta Orthopaedica Scandinavica 1983;54:340‐7. [DOI] [PubMed] [Google Scholar]
Svenningsen 1984 {published data only}
- Benum P, Nesse O, Svenningsen S. Fracture of the neck of the femur. A randomized prospective study [abstract]. Acta Orthopaedica Scandinavica 1980;51:371. [Google Scholar]
- Svenningsen S, Benum P, Nesse O, Furset OI. Femoral neck fractures in the elderly ‐ a comparison of 3 treatment methods [Larhalsbrudd hos eldre‐‐en sammenligning av tre behandlingsmetoder]. Nordisk Medicin 1985;100:256‐9. [MEDLINE: ] [PubMed] [Google Scholar]
- Svenningsen S, Benum P, Nesse O, Furset OI. Femoral neck fractures in the elderly. A comparison of 3 therapeutic methods [Larhalsbrudd hos eldre. En sammenligning av tre behandlingsmetoder]. Tidsskr for den Norske Laegeforening 1985;105(7):492‐5. [MEDLINE: ] [PubMed] [Google Scholar]
- Svenningsen S, Benum P, Nesse O, Furset OI. Internal fixation of femoral neck fractures. Compression screw compared with nail plate fixation. Acta Orthopaedica Scandinavica 1984;55:423‐9. [DOI] [PubMed] [Google Scholar]
Wihlborg 1990 {published data only}
- Wihlborg O. Fixation of femoral neck fractures. A four‐flanged nail versus threaded pins in 200 cases. Acta Orthopaedica Scandinavica 1990;61(5):415‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ingwersen 1992 {published data only}
- Ingwersen J, Skoglund A, Syversen S. Early loss of fixation of cervical hip fractures [abstract]. Acta Orthopaedica Scandinavica. Supplementum 1992;247:6‐7. [Google Scholar]
Jukkala‐Partio 2000 {published data only}
- Jukkala‐Partio K, Partio EK, Helevirta P, Pohjonen T, Tormala P, Rokkanen P. Treatment of subcapital femoral neck fractures with bioabsorbable or metallic screw fixation. Annals Chirurgiae et Gynaecologiae 2000;89:45‐52. [PubMed] [Google Scholar]
Poulsen 1995 {published data only}
- Poulsen TD, Ovesen O, Andersen I. Percutaneous osteosynthesis with two screws in treating femoral neck fractures. Orthopedics 1995;18(7):661‐4. [DOI] [PubMed] [Google Scholar]
Sernbo 1986 {published data only}
- Sernbo I, Edwards P, Johnell O, Baath L. Cannulated screws versus spring loaded single nail in cervical hip fractures: A prospective randomized trial [abstract]. Acta Orthopaedica Scandinavica 1986;57:598. [Google Scholar]
References to ongoing studies
FAITH {unpublished data only}
- Bhandari M. Fixation using Alternative Implants for the Treatment of Hip fractures (FAITH): a multi‐centre randomised trial comparing sliding hip screws and cancellous screws on revision surgery rates and quality of life in the treatment of femoral neck fractures. http://apps.who.int/trialsearch/Trial.aspx?TrialID=ISRCTN25524122 (accessed 18 January 2011). [DOI] [PMC free article] [PubMed]
Additional references
Alho 1998
- Alho A, Austdal S, Benterud JG, Blikra G, Lerud P, Raugstad TS. Biases in a randomized comparison of three types of screw fixation in displaced femoral neck fractures. Acta Orthopaedica Scandinavica 1998;69(5):463‐8. [DOI] [PubMed] [Google Scholar]
Harris 1969
- Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mould arthroplasty. An end‐result study using a new method of result evaluation. Journal of Bone and Joint Surgery. American Volume 1969;51‐A(4):737‐55. [PubMed] [Google Scholar]
Lefebvre 2009
- Lefebvre C, Manheimer E, Glanville J. Chapter 6.4.11 Search filters. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 (updated September 2009). The Cochrane Collaboration, 2009. Available from www.cochrane‐handbook.org.
Lu‐Yao 1994
- Lu‐Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcome after displaced fracture of the femoral neck: a meta‐analysis of one hundred and six published reports. Journal of Bone and Joint Surgery. American Volume 1994;76‐A:15‐25. [DOI] [PubMed] [Google Scholar]
Parker 1993
- Parker MJ, Pryor GA. Hip fracture management. Oxford: Blackwell Scientific Publications, 1993. [Google Scholar]
Tronzo 1974
- Tronzo RG. Hip nails for all occasions. The Orthopedic Clinics of North America 1974;5:479‐91. [PubMed] [Google Scholar]


