Abstract
Background
Traditionally, cavitated carious lesions and those extending into dentine have been treated by 'complete' removal of carious tissue, i.e. non‐selective removal and conventional restoration (CR). Alternative strategies for managing cavitated or dentine carious lesions remove less or none of the carious tissue and include selective carious tissue removal (or selective excavation (SE)), stepwise carious tissue removal (SW), sealing carious lesions using sealant materials, sealing using preformed metal crowns (Hall Technique, HT), and non‐restorative cavity control (NRCC).
Objectives
To determine the comparative effectiveness of interventions (CR, SE, SW, sealing of carious lesions using sealant materials or preformed metal crowns (HT), or NRCC) to treat carious lesions conventionally considered to require restorations (cavitated or micro‐cavitated lesions, or occlusal lesions that are clinically non‐cavitated but clinically/radiographically extend into dentine) in primary or permanent teeth with vital (sensitive) pulps.
Search methods
An information specialist searched four bibliographic databases to 21 July 2020 and used additional search methods to identify published, unpublished and ongoing studies.
Selection criteria
We included randomised clinical trials comparing different levels of carious tissue removal, as listed above, against each other, placebo, or no treatment. Participants had permanent or primary teeth (or both), and vital pulps (i.e. no irreversible pulpitis/pulp necrosis), and carious lesions conventionally considered to need a restoration (i.e. cavitated lesions, or non‐ or micro‐cavitated lesions radiographically extending into dentine). The primary outcome was failure, a composite measure of pulp exposure, endodontic therapy, tooth extraction, and restorative complications (including resealing of sealed lesions).
Data collection and analysis
Pairs of review authors independently screened search results, extracted data, and assessed the risk of bias in the studies and the overall certainty of the evidence using GRADE criteria. We measured treatment effects through analysing dichotomous outcomes (presence/absence of complications) and expressing them as odds ratios (OR) with 95% confidence intervals (CI). For failure in the subgroup of deep lesions, we used network meta‐analysis to assess and rank the relative effectiveness of different interventions.
Main results
We included 27 studies with 3350 participants and 4195 teeth/lesions, which were conducted in 11 countries and published between 1977 and 2020. Twenty‐four studies used a parallel‐group design and three were split‐mouth. Two studies included adults only, 20 included children/adolescents only and five included both. Ten studies evaluated permanent teeth, 16 evaluated primary teeth and one evaluated both. Three studies treated non‐cavitated lesions; 12 treated cavitated, deep lesions, and 12 treated cavitated but not deep lesions or lesions of varying depth.
Seventeen studies compared conventional treatment (CR) with a less invasive treatment: SE (8), SW (4), two HT (2), sealing with sealant materials (4) and NRCC (1). Other comparisons were: SE versus HT (2); SE versus SW (4); SE versus sealing with sealant materials (2); sealant materials versus no sealing (2).
Follow‐up times varied from no follow‐up (pulp exposure during treatment) to 120 months, the most common being 12 to 24 months.
All studies were at overall high risk of bias.
Effect of interventions
Sealing using sealants versus other interventions for non‐cavitated or cavitated but not deep lesions
There was insufficient evidence of a difference between sealing with sealants and CR (OR 5.00, 95% CI 0.51 to 49.27; 1 study, 41 teeth, permanent teeth, cavitated), sealing versus SE (OR 3.11, 95% CI 0.11 to 85.52; 2 studies, 82 primary teeth, cavitated) or sealing versus no treatment (OR 0.05, 95% CI 0.00 to 2.71; 2 studies, 103 permanent teeth, non‐cavitated), but we assessed all as very low‐certainty evidence.
HT, CR, SE, NRCC for cavitated, but not deep lesions in primary teeth
The odds of failure may be higher for CR than HT (OR 8.35, 95% CI 3.73 to 18.68; 2 studies, 249 teeth; low‐certainty evidence) and lower for HT than NRCC (OR 0.19, 95% CI 0.05 to 0.74; 1 study, 84 teeth, very low‐certainty evidence). There was insufficient evidence of a difference between SE versus HT (OR 8.94, 95% CI 0.57 to 139.67; 2 studies, 586 teeth) or CR versus NRCC (OR 1.16, 95% CI 0.50 to 2.71; 1 study, 102 teeth), both very low‐certainty evidence.
CR, SE, SW for deep lesions
The odds of failure were higher for CR than SW in permanent teeth (OR 2.06, 95% CI 1.34 to 3.17; 3 studies, 398 teeth; moderate‐certainty evidence), but not primary teeth (OR 2.43, 95% CI 0.65 to 9.12; 1 study, 63 teeth; very low‐certainty evidence).
The odds of failure may be higher for CR than SE in permanent teeth (OR 11.32, 95% CI 1.97 to 65.02; 2 studies, 179 teeth) and primary teeth (OR 4.43, 95% CI 1.04 to 18.77; 4 studies, 265 teeth), both very low‐certainty evidence. Notably, two studies compared CR versus SE in cavitated, but not deep lesions, with insufficient evidence of a difference in outcome (OR 0.62, 95% CI 0.21 to 1.88; 204 teeth; very low‐certainty evidence).
The odds of failure were higher for SW than SE in permanent teeth (OR 2.25, 95% CI 1.33 to 3.82; 3 studies, 371 teeth; moderate‐certainty evidence), but not primary teeth (OR 2.05, 95% CI 0.49 to 8.62; 2 studies, 126 teeth; very low‐certainty evidence).
For deep lesions, a network meta‐analysis showed the probability of failure to be greatest for CR compared with SE, SW and HT.
Authors' conclusions
Compared with CR, there were lower numbers of failures with HT and SE in the primary dentition, and with SE and SW in the permanent dentition. Most studies showed high risk of bias and limited precision of estimates due to small sample size and typically limited numbers of failures, resulting in assessments of low or very low certainty of evidence for most comparisons.
Keywords: Adolescent; Adult; Child; Child, Preschool; Humans; Middle Aged; Bias; Crowns; Dental Atraumatic Restorative Treatment; Dental Atraumatic Restorative Treatment/methods; Dental Caries; Dental Caries/pathology; Dental Caries/therapy; Dental Restoration Failure; Dental Restoration Failure/statistics & numerical data; Dentin; Dentition, Permanent; Network Meta-Analysis; Pit and Fissure Sealants; Pit and Fissure Sealants/therapeutic use; Randomized Controlled Trials as Topic; Tooth, Deciduous
Plain language summary
Comparing treatments for advanced tooth decay
Key messages
For decayed baby (primary) teeth, putting an off‐the‐shelf metal crown over the tooth or only partially removing decay before placing a filling may be better than the conventional treatment of removing all decay before filling.
For decayed adult (permanent) teeth, partial removal of decay before filling the tooth, or adding a second stage to this treatment where more decay is removed after several months, may be better than conventional treatment.
What is the condition?
Dental caries (tooth decay) is very common and can cause pain, eating and speaking difficulties, and self‐consciousness. Teeth are made up of three layers: enamel (hard outer layer), dentine (hard inner layer), and pulp (nerves and blood vessels). Our mouths contain bacteria, which grow in a sticky film over our teeth known as dental plaque. The bacteria live on sugar from our diet and turn it into acid that dissolves the teeth. Saliva can reverse this process, but if there is too much sugar in the diet or bacteria are not removed often enough by toothbrushing then the acids continue to erode the teeth. This can progress into the dentine, eventually causing a hole in the tooth (known as a cavitated carious lesion). If it reaches the pulp, it can cause infection.
How is the condition treated?
Dentine/cavitated carious lesions can be treated by complete removal of decayed parts of the tooth and placement of a filling. Dentists call this non‐selective carious tissue removal and conventional restoration (CR). Although effective, this risks weakening the tooth or causing problems if the pulp of the tooth is exposed. Newer alternatives involve removing less or none of the carious tissue:
1. Selective carious tissue removal (or selective excavation (SE)): decay around the edges of the cavity is fully removed, but close to the pulp, some softened dentine is left. A filling is then put in.
2. Stepwise carious tissue removal (SW): as with SE, most of the decayed parts are removed, but soft dentine is left in areas close to the pulp and the cavity is filled using materials such as composite. After a gap of several months, more of the softened dentine is removed.
3. Sealing carious lesions using sealant materials: a thin coating made from resin or glass ionomer is painted over the decayed tooth, hardens in a few minutes and makes the caries inactive by stopping bacteria reaching it.
4. Sealing using preformed metal crowns (Hall Technique, HT): a preformed metal crown (i.e. chosen from a selection of sizes to closely fit the tooth, but not moulded for the particular tooth) is pushed over the decayed tooth to seal in the carious lesion.
5. Non‐restorative cavity control (NRCC): cavities are made easier to clean, and patients helped to develop good tooth care and eating habits to reduce the risk of the decay progressing.
What did we want to find out?
We wanted to know the best way for dentists to manage decay that has extended into dentine or cavitated.
What did we do?
An information specialist searched databases to find relevant studies. We included studies known as randomised clinical trials that compared one treatment versus another treatment, fake (placebo) treatment or no treatment.
We combined study results when possible used a statistical procedure called network meta‐analysis to assess the relative effectiveness of the treatments.
We assessed whether the studies might be biased and judged the reliability of the evidence using established criteria.
What did we find?
We included 27 studies with 3350 participants (4195 teeth/lesions), mostly children. Treatment success or failure was usually evaluated at 12 to 24 months.
Sealing using sealants versus other interventions for non‐cavitated or cavitated but not deep lesions
The evidence is very uncertain, so we do not know whether sealing with sealants is better, worse or the same as conventional treatment, SE or no treatment.
HT, CR, SE, NRCC for cavitated, but not deep lesions in baby teeth
The results showed HT may be more likely to be successful than conventional treatment or NRCC.
The evidence is very uncertain for SE versus HT and CR versus NRCC.
CR, SE, SW for deep lesions
SW is probably better than conventional treatment for permanent teeth. The evidence is very uncertain for primary teeth.
SE may be better than conventional treatment for permanent teeth and possibly primary teeth (but the evidence is very uncertain for lesions that are cavitated but not deep).
SE is probably better than SW for permanent teeth. The evidence is very uncertain for primary teeth.
For deep lesions, network meta‐analysis showed failure was most likely with conventional treatment compared with SE, SW and HT.
What are the limitations of the evidence?
Most studies did not involve many people, and most people had no problems with their fillings regardless of which treatment they received. All studies were at high risk of being biased in some way. Currently, we only have low to very low certainty in most findings. This means future research could lead to different conclusions.
How up‐to‐date is this evidence?
We found studies up to 21 July 2020.
Summary of findings
Summary of findings 1. Sealing using sealant materials compared to non‐selective carious tissue removal and conventional restoration for treating cavitated or dentine carious lesions.
| Sealing using sealant materials compared to non‐selective carious tissue removal and CR for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, permanent or primary dentition Setting: secondary care/university Intervention: sealing using sealant materials Comparison: non‐selective carious tissue removal and CR | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with non‐selective carious tissue removal and CR | Risk with sealing using sealant materials | |||||
|
Failure of therapy
Follow‐up 48 months |
48 per 1000 | 200 per 1000 (25 to 711) | OR 5.00 (0.51 to 49.27) | 41 (1 RCT) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effect of sealing with sealant materials compared to CR. 1 additional parallel group study and 2 additional split‐mouth studies reported failure, but could not be included in the meta‐analysis due to the nature of the reporting of the outcome data. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CR: conventional restoration; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels due to study limitations (risk of bias) and serious imprecision (single study with low number of events, small sample size and wide confidence intervals).
Summary of findings 2. Sealing with sealant materials compared to selective carious tissue excavation for treating cavitated or dentine carious lesions.
| Sealing with sealant materials compared to SE for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary dentition Setting: secondary care/university Intervention: sealing with sealant materials Comparison: SE | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with SE | Risk with sealing with sealant materials | |||||
| Failure of therapy Follow‐up 18–24 months | 79 per 1000 | 210 per 1000 (9 to 880) | OR 3.11 (0.11 to 85.52) | 82 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effect of sealing with sealant materials compared to SE. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; SE: selective excavation; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias from lack of blinding), inconsistency (I2 = 74%) and imprecision (very low number of events, small sample size and wide confidence intervals).
Summary of findings 3. Sealing compared to no treatment for treating cavitated or dentine carious lesions.
| Sealing compared to no treatment for treating cavitated or dentine carious lesions | ||||||
|
Population: treating cavitated or dentine carious lesions, permanent dentition Setting: secondary care/university Intervention: sealing Comparison: no treatment | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with no treatment | Risk with sealing | |||||
| Failure of therapy Follow‐up 12 months | 700 per 1000 | 104 per 1000 (0 to 863) | OR 0.05 (0.00 to 2.71) | 103 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effect of sealing compared to no treatment. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for high risk of bias (blinding, incomplete outcome data and selective reporting), inconsistency (I2 = 89%) and imprecision (low number of events, small sample size and wide confidence intervals).
Summary of findings 4. Non‐selective carious tissue removal and conventional restoration compared to the Hall Technique for treating cavitated or dentine carious lesions.
| Non‐selective carious tissue removal and CR compared to HT for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary dentition Setting: primary care/practices and secondary care/university Intervention: non‐selective carious tissue removal and CR Comparison: HT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with HT | Risk with CR | |||||
| Failure of therapy Follow‐up 30–60 months | 75 per 1000 | 404 per 1000 (232 to 602) | OR 8.35 (3.73 to 18.68) | 249 (2 RCTs) | ⊕⊕⊝⊝ Lowa | HT may result in a large reduction in failure compared to non‐selective carious tissue removal and CR. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CR: conventional restoration; HT: Hall Technique; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two levels in total for high risk of bias (mainly associated with blinding) and imprecision (only two studies and wide confidence intervals).
Summary of findings 5. Selective carious tissue excavation compared to the Hall Technique for treating cavitated or dentine carious lesions.
| SE compared to HT for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary dentition Setting: secondary care/university and school setting Intervention: SE Comparison: HT | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with HT | Risk with SE | |||||
| Failure of therapy:SE vs HT – primary, cavitated but not deep Follow‐up 24 months | 90 per 1000 | 469 per 1000 (53 to 932) | OR 8.94 (0.57 to 139.67) | 586 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effect of HT compared to SE. |
| Failure of therapy:SE vs HT – primary, deep Follow‐up 24–36 months | 146 per 1000 | 250 per 1000 (89 to 531) | OR 1.95 (0.57 to 6.63) | 72 (1 RCT) | ⊕⊝⊝⊝ Very lowb | The evidence is very uncertain about the effect of HT compared to SE. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HT: Hall Technique; OR: odds ratio; RCT: randomised controlled trial; SE: selective excavation. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias due to lack of blinding of participants and outcome assessors), inconsistency (I2 = 92%) and imprecision (low number of events, small sample size and very wide confidence intervals). bDowngraded three levels for study limitations (high risk of bias due to lack of blinding of participants, incomplete reporting and selective outcome reporting), and serious imprecision (single study, low number of events, small sample size and wide confidence intervals).
Summary of findings 6. Non‐selective carious tissue removal and conventional restoration compared to non‐restorative cavity control for treating cavitated or dentine carious lesions.
| Non‐selective carious tissue removal and CR compared to NRCC for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary dentition Setting: secondary care/university Intervention: non‐selective carious tissue removal and CR Comparison: NRCC | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with NRCC | Risk with non‐selective carious tissue removal and CR | |||||
| Failure of therapy Follow‐up 30 months | 295 per 1000 | 327 per 1000 (173 to 532) | OR 1.16 (0.50 to 2.71) | 102 (1 RCT) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effect of CR compared to NRCC. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CR: conventional restoration; NRCC: non‐restorative cavity control; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias due to lack of blinding of participants), and serious imprecision (single study, low number of events and small sample size).
Summary of findings 7. The Hall Technique compared to non‐restorative cavity control for treating cavitated or dentine carious lesions.
| HT compared to NRCC for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary dentition Setting: secondary care/university Intervention: HT Comparison: NRCC | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with NRCC | Risk with HT | |||||
| Failure of therapy Follow‐up 30 months | 295 per 1000 | 74 per 1000 (21 to 237) | OR 0.19 (0.05 to 0.74) | 84 (1 RCT) | ⊕⊝⊝⊝ Very lowa | HT may result in a reduction in failure when compared to NRCC, but the evidence is very uncertain. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; HT: Hall Technique; NRCC: non‐restorative cavity control; OR: odds ratio; RCT: randomised controlled trial. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias from lack of blinding of participants and imprecision (single study, small sample size and small number of events).
Summary of findings 8. Non‐selective carious tissue removal and conventional restoration compared to stepwise carious tissue removal for treating cavitated or dentine carious lesions.
| Non‐selective carious tissue removal and CR compared to SW carious tissue removal for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary and permanent dentition Setting: secondary care/university Intervention: non‐selective carious tissue removal and CR Comparison: SW | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with non‐selective carious tissue removal and CR | Risk with SW | |||||
| Failure of therapy: CR vs SW – primary, deep Follow‐up 12 months | 258 per 1000 | 125 per 1000 (37 to 349) | OR 2.43 (0.65 to 9.12) | 63 (1 RCT) | ⊕⊝⊝⊝ Very lowa | The evidence is very uncertain about the effect of CR compared to SW in primary teeth. |
| Failure of therapy: CR vs SW – permanent, deep Follow‐up 6–60 months | 465 per 1000 | 294 per 1000 (212 to 391) | OR 2.06 (1.34 to 3.17) | 398 (3 RCTs) | ⊕⊕⊕⊝ Moderateb | In permanent teeth, SW probably results in a reduction in the number of failures compared with CR. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CR: conventional restoration; OR: odds ratio; RCT: randomised controlled trial; SW: stepwise carious tissue removal. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias for sequence generation, allocation concealment and blinding) and serious imprecision (single study, low number of events, small sample size and wide confidence intervals). bDowngraded one level for study limitations (high risk of bias prinicipally from a lack of blinding of participants and assessors).
Summary of findings 9. Non‐selective carious tissue removal and conventional restoration compared to selective carious tissue removal for treating cavitated or dentine carious lesions.
| Non‐selective carious tissue removal and CR compared to SE for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions Setting: secondary care/university Intervention: non‐selective carious tissue removal and CR Comparison: SE | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with SE | Risk with non‐selective carious tissue removal and CR | |||||
| Failure of therapy: CR vs SE – permanent, deep Follow‐up 12–18 months | 12 per 1000 | 118 per 1000 (23 to 433) | OR 11.32 (1.97 to 65.02) | 179 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | In permanent teeth, the evidence is very uncertain about the effect of CR compared to SE. |
| Failure of therapy: CR vs SE – primary, deep Follow‐up 6–36 months | 246 per 1000 | 591 per 1000 (254 to 860) | OR 4.43 (1.04 to 18.77) | 265 (4 RCTs) | ⊕⊝⊝⊝ Very lowb | In primary teeth, the evidence is very uncertain about the effect of CR compared to SE. |
| Failure of therapy: CR vs SE – primary, cavitated but not deep Follow‐up 12 months | 174 per 1000 | 115 per 1000 (42 to 284) | OR 0.62 (0.21 to 1.88) | 204 (2 RCTs) | ⊕⊝⊝⊝ Very lowc | In primary teeth with cavitated but not deep lesions, the evidence is very uncertain about the effect of CR compared to SE. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; CR: conventional restoration; OR: odds ratio; RCT: randomised controlled trial; SE: selective extraction. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias for sequence generation, allocation concealment and blinding for one study with 62% weight) and serious imprecision (small sample size, low number of events and wide confidence intervals). bDowngraded three levels for study limitations (principally for lack of blinding, imprecision and inconsistency (I2 = 66%)). cDowngraded three levels for study limitations (lack of blinding) and serious imprecision.
Summary of findings 10. Selective excavation of carious tissues compared to stepwise excavation of carious tissues for treating cavitated or dentine carious lesions.
| SE compared to SW for treating cavitated or dentine carious lesions | ||||||
| Population: treating cavitated or dentine carious lesions, primary and permanent dentition Setting: primary and secondary care/university Intervention: SE Comparison: SW | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with SW | Risk with SE | |||||
|
Failure of therapy: SW vs SE – primary, deep Follow‐up 12–24 months |
48 per 1000 | 94 per 1000 (24 to 305) | OR 2.05 (0.49 to 8.62) | 126 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | In primary teeth with deep lesions, the evidence is very uncertain about the effect of SE on SW. |
| Failure of therapy: SW vs SE – permanent, deep Follow‐up 12–60 months | 144 per 1000 | 274 per 1000 (182 to 390) | OR 2.25 (1.33 to 3.82) | 371 (3 RCTs) | ⊕⊕⊕⊝ Moderateb | In permanent teeth with deep lesions, SE probably reduces failure compared to SW. |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; OR: odds ratio; RCT: randomised controlled trial; SE: selective excavation; SW: stepwise excavation of carious tissues. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three levels for study limitations (high risk of bias across multiple domains) and serious imprecision (low number of events, small sample size and wide confidence intervals). bDowngraded one level for risk of bias.
Background
Description of the condition
Dental caries is the most prevalent disease worldwide, with billions of individuals affected by the resulting burden of pain, loss of function, impaired aesthetics and speech (Kassebaum 2015; Marcenes 2013). The oral microbiota are organised on dental hard tissues as biofilms and, under healthy conditions, these biofilms contain limited numbers of cariogenic bacteria. The condition of dental caries is caused by a shift in the composition of the oral microbiota towards increased proportions of cariogenic bacteria. When fermentable carbohydrates (i.e. sugars) are available as a substrate, the bacteria metabolise them and produce organic acids as by‐products. These acids dissolve tooth mineral. The mineral loss from the dental hard tissues (enamel and dentine) caused by these bacteria is, in its initial stages, reversible, with mineral supply from dental saliva leading to remineralisation. If the sugars are available regularly and in sufficient amount, to the cariogenic bacteria, their continued metabolism and subsequent acid production lead to a decrease in the pH within the biofilms (which is why they are termed 'acidogenic' bacteria). As these acidogenic bacteria are also 'aciduric' (i.e. acid‐tolerant) while most other bacteria are not, they increasingly dominate the biofilm. This imbalance in the biofilm results in a discrepancy in the mineral loss and gain, with a resulting net mineral loss. If this continues over time, it can lead to development of a carious lesion as the symptom of the caries disease process (Marsh 2010; Takahashi 2011). Carious lesions can range from very early mineral loss, not detectable to the naked eye, that is restricted to enamel, through to lesions that extend into dentine without any surface cavitations, to cavitated lesions, which destroy the tooth tissue and can be visible as holes in the teeth.
Description of the intervention
Traditionally, all carious lesions have been treated by removing all demineralised (affected) and bacterially contaminated (infected) dentine and replacing it using restorations (based on, for example, amalgam or composite), commonly known as a 'filling'. However, the pathophysiology of the disease process means that carious lesions can be controlled by altering the factors leading to net mineral loss. This can be achieved by reducing carbohydrate intake; removing or controlling the activity of the biofilm; sealing the tooth surface from the environment; or rebalancing demineralisation and remineralisation, for example, by applying fluoride, especially regular use of fluoride toothpaste.
For carious lesions where the tooth tissue surface has become cavitated, these options are often no longer feasible, as the biofilm is sheltered and cannot be easily removed or manipulated. In such situations, invasive (restorative) options are considered to still be required in most cases (Schwendicke 2016a). Cavities that are clinically difficult to detect (often called microcavitations) may, upon radiographic assessment, be found to penetrate the dentine. These dentinal lesions have traditionally also been considered to require a restoration (Ricketts 1995), especially when the lesion has entered the middle third of the dentine, and hence harbours large amounts of bacteria (Bakhshandeh 2018).
There are six main strategies that are the focus of this Cochrane Review and are considered suitable for treating cavitated/dentine carious lesions that would historically have been regarded as in need of a restoration. These strategies are supposed to manage cavitated lesions, microcavitated lesions, and occlusal lesions that appear clinically to be non‐cavitated but extend into dentine (seen radiographically, or clinically as grey shadowing), and are summarised in Table 11.
1. Interventions.
| Interventions | Standard practice (yes/no) | Primary/permanent teeth | Lesion depth (deep/shallow) | Tooth surface location (occlusal/smooth surface/proximal/root surface) | Tooth surface integrity (non‐cavitated/cavitated) | Surface extent (1/2/3 surfaced lesions) |
| Non‐selective carious tissue removal | Yes |
Primary and permanent teeth | Shallow and deep |
All |
Cavitated |
All |
| Selective carious tissue removal | Yes | Primary and permanent teeth | Shallow and deep | All except root surface | Cavitated | All |
| Stepwise carious tissue removal | Yes |
Primary and permanent teeth | Deep |
All except root surface |
Cavitated |
All |
| Fissure/proximal sealing | Yes |
Primary and permanent teeth | Shallow |
All except root surface |
Mainly non‐cavitated |
1 surface |
| Hall Technique | Yes |
Primary teeth | Shallow and deep |
All except root surface |
Cavitated |
All |
| Non‐restorative cavity control | Yes | Primary and permanent teeth | Shallow and deep |
All |
Cavitated |
All |
Non‐selective carious tissue removal and conventional restoration (CR). Carious dentine and enamel are removed, usually until only sound enamel and hard dentine remain. The cavity is subsequently restored (this review does not focus on the material, e.g. amalgam, composite etc. or how this restoration is performed). Especially for deep lesions, this approach carries a high risk of pulp exposure, which in turn often leads to further endodontic interventions being needed (Schwendicke 2013). In addition, CR results in more tooth structure being removed and increases the risk of weakening the tooth. Both consequences accelerate the 'restorative spiral' and limit the lifespan of the tooth.
Selective carious tissue removal (or selective excavation, SE). Carious dentine and enamel are removed, usually until only sound enamel and hard dentine remain at the cavity periphery, while centrally, dentine of different hardnesses (soft, leathery or firm) remains. The cavity is subsequently restored.
Stepwise carious tissue removal (SW). Carious dentine is removed as the first step, as described for selective removal, leaving soft dentine in the pulpo‐proximal areas. The cavity is restored, for example using glass ionomer cement or composite material, for some months. In the second step, carious tissue is now removed to firm dentine in pulpo‐proximal areas. Note that in older studies, the entire stepwise approach may have been more invasive as the second step was likely to have been more similar to the first stage with non‐selective removal (Magnusson 1977), whereas later, the procedure was recommended as being carried out less invasively.
Sealing using sealant materials such as resins and glass ionomers, placed over the carious lesion, depriving the carious biofilm of substrate. Sealants are placed without any prior tissue preparation, although some have advocated some preparation (fissurotomy, enameloplasty). We only included studies where sealants were placed without any carious tissue removal; notably, enamel may have been prepared/bevelled prior to sealing as long as no carious dentine was removed.
The Hall Technique (HT). A preformed metal crown is pushed over a carious primary molar to seal‐in the carious lesion. None of the carious tooth tissue is removed and, as previously described, the biofilm cariogenic activity is reduced by bacteria being deprived of nutrients and the lesion is arrested as the bacteria become inactive.
Non‐restorative cavity control (NRCC). The cavity shape is made cleansable, and the tooth tissue is repeatedly and frequently cleansed by the patient or carers to remove the biofilm, remineralisation therapies are targeted at the lesion (fluoride through toothbrushing or possibly silver diamine fluoride) to prevent it from progressing. Behaviour change is important to alter the habits that have led to development of the lesion (diet or plaque control, or both) and allow control of the biofilm when using NRCC.
How the intervention might work
Restoration involves the removal of demineralised carious dentine and enamel (also termed 'excavation') to allow a filling, which can be made using a variety of materials, to be placed on stable or suitably supportive tooth tissue. The process of carious tissue removal can be undertaken to various degrees or levels. All or most carious dentine can be removed with a 'non‐selective' approach using a single endpoint for removal; for example, removal until hard dentine in all parts of the cavity. Alternatively, carious dentine close to the dental pulp can be left and sealed beneath the restoration, with removal until hard dentine performed in the periphery of the cavity. This has been termed 'selective carious tissue removal'. Varying endpoints are used to guide dentine removal in different areas of the cavity (e.g. hard dentine is left peripherally, while soft or leathery or firm dentine is left centrally). A combined SW approach can also be used to treat deep carious lesions. This approach involves selective removal to soft dentine as an initial step; the cavity is then sealed for some months during which time the lesion is arrested as sealed bacteria are inactivated, dentine remineralises, becomes hardened and dried, and tertiary dentine is laid down in the pulp close to the lesion until a second selective removal to firm dentine is performed (Innes 2016). As only minimal numbers of bacteria are thought to survive long‐term below a restoration sealing, it is proposed that reduced dentine removal (resulting in increased residual dentine thickness and avoiding pulp exposure), may improve patient benefit with limited subsequent risk. However, it is currently unclear which of these strategies is most suitable for carious lesions that require restoration (Bjørndal 1997; Bjørndal 2000; Paddick 2005; Schwendicke 2016b).
The carious process is fundamentally the same for primary and permanent teeth. However, primary teeth are more vulnerable to the process as they have slightly less mineral content, the enamel and dentine layer is thinner, the dental pulps are relatively larger and the teeth are smaller. The anatomy also affects the sequelae of dental caries; dental infection tends to manifest more quickly in primary teeth. This is because the communications between the tooth and bone, where developing infection can escape from the confine of the tooth, tend to be at the top of the roots in primary teeth rather than the base of the roots as in permanent teeth. These differences mean that primary teeth tend to require relatively less disease process to experience pain and infection.
It has also been shown that, in some cases, no removal of carious tissue is needed at all; instead, carious lesions can either be sealed or otherwise controlled (Mertz‐Fairhurst 1998). Sealing places a barrier on top of the tooth surface, thereby protecting it from any further mineral loss, and isolating sealed bacteria from dietary carbohydrates, thereby inactivating them (Oong 2008). Various sealant materials are used, including resin‐based and glass ionomer products. However, as these materials can be damaged by wear and tear from chewing, sealing cavitated carious lesions with them is not usually recommended currently (Schwendicke 2016a). Instead, in primary teeth, sealing can be achieved by using preformed stainless steel crowns. This approach, the HT, has no need for local anaesthesia, tooth preparation or carious tissue removal. It is not currently clear whether sealing carious tooth tissue using sealants (primary and permanent teeth) or HT (primary teeth) results in good outcomes for teeth that have traditionally been considered required carious tissue removal and restoration (Innes 2011; Santamaria 2018).
Based on the outlined caries pathogenesis, there have been investigations into whether it might be sufficient to simply control biofilm activity in cavitated carious lesions by repeated and frequent removal of the biofilm through toothbrushing, using fluoride to remineralise, or using antimicrobials/remineralising agents such as silver diamine fluoride. However, this may not always be possible or work well where the biofilm is sheltered. Moreover, and as mentioned, the intervention must also target behaviour change to alter the factors that have led to the disease. Based on this idea, another intervention called NRCC aims to remove overhanging enamel from the cavity to allow easy access to the biofilm/lesion for cleansing and removal. The lesion can then be controlled by toothbrushing using fluoridated products, provided the patient or their carers successfully adopt and carry out this behaviour. With varying results, NRCC has, so far, been suggested for primary teeth and root surface caries only; however, it might be suitable for other carious lesions (Gruythuysen 2010; Hansen 2017; Santamaria 2018).
Why it is important to do this review
Dentists worldwide are faced daily with decisions about how best to treat carious lesions that were conventionally considered to be in need of restoration: when and how to remove carious tissue, how much tissue to remove, and even whether carious tissue should be removed at all. This creates large treatment variation among clinicians (Innes 2017; Schwendicke 2016c). One previous Cochrane Review evaluated operative interventions for managing carious lesions (Ricketts 2013). Several studies have been published since that review was undertaken and methods for synthesising relevant data have advanced. Given the prevalence of the disease, its lifelong sequelae, and the high direct and indirect costs generated (Listl 2015; Schwendicke 2013; Schwendicke 2014; Schwendicke 2015a), there is a great need to evaluate which currently available interventions are most suitable for managing cavitated/dentine carious lesions.
Objectives
To determine the comparative effectiveness of interventions (CR, SE, SW, sealing of carious lesions using sealant materials or preformed metal crowns (HT), or NRCC) to treat carious lesions conventionally considered to require restorations (cavitated or micro‐cavitated lesions, or occlusal lesions that are clinically non‐cavitated but clinically/radiographically extend into dentine) in primary or permanent teeth with vital (sensitive) pulps.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) that compared any of the interventions. We included studies that were randomised at the level of the individual or by cluster. Split‐mouth studies were also eligible for inclusion. We excluded cross‐over trials as the condition, dental caries, cannot return to baseline level following the initial intervention. In vitro studies or publications that did not report clinical outcomes were excluded.
This systematic review excluded clinical trials that did not compare different levels of carious tissue removal, and were only concerned with evaluating dental materials, or restoration techniques. Atraumatic restorative treatment (ART) trials were considered for this review but unless the extent of carious tissue removal was described or stated as selective, they were considered as non‐selective and excluded. Chemomechanical caries removal agents were considered as non‐selective caries removal strategies.
We included studies that compared the interventions described for carious lesions with each other, placebo or no treatment. If multiple records of the same study were available, we extracted data from the last time point.
Types of participants
Participants with permanent or primary teeth and vital pulps (i.e. not diagnosed as having irreversible pulpitis or pulp necrosis), and carious lesions conventionally considered in need of a restoration (i.e. cavitated lesions or, on occlusal surfaces, non‐cavitated or micro‐cavitated but radiographically extending into dentine (or clinically having a dentine shadow indicating dentine involvement)).
We used the description 'carious lesions considered to need a restoration' as we expected some, especially older, studies to not have reported on lesion depths or the state of the tooth surface integrity, but only stated that lesions required restorations. This pragmatic approach means that although these studies may not directly inform clinical practice recommendations, inclusion of their data contributed to this review.
Types of interventions
Interventions included CR, SE, SW, sealing using sealant materials or preformed metal crowns (HT) and NRCC. Note that not all interventions will have been applied in all situations where restorations might have been considered the traditional 'standard'. We acknowledge that indications for each procedure may differ according to their presentation in terms of dentition (primary/permanent), lesion depth (shallow/moderate versus deep lesions) and clinical surface integrity (non‐cavitated occlusal versus clearly and extensive cavitated proximal‐occlusal). We had planned to conduct subgroup analyses to explore the effects of the different presentations.
For lesion depths measured and recorded clinically or radiographically (or both) we distinguished between:
non‐cavitated (occlusal) lesions (usually with radiographic dentine involvement);
cavitated but shallow/moderate lesions (those that did not extend into the pulpal area or did not risk exposing the pulp during carious tissue removal, as measured subjectively, or not extending into the inner third or quarter of dentine as shown on a radiograph); and
deep lesions (those close to the pulp, risking exposure, extending into inner third or quarter of dentine).
Many trials evaluated the effect of the intervention on carious lesions of different depths. We included studies that explicitly reported outcomes for the different depths separately.
Table 11 lists the interventions and the typical types of lesion, dentition and clinical contexts for their use.
The review did not evaluate different restoration materials.
Types of outcome measures
We assessed the following outcomes and outcome measures.
Primary outcomes
-
Failure of therapy: a composite outcome, that is, complications including:
signs or symptoms of irreversible pulp inflammation or death;
endodontic therapy (pulp capping, pulp therapy or root‐canal treatment etc.);
extraction of the tooth;
restorative failure or retreatment (restoration replacement, repair, resealing of sealed lesions etc.), or both;
or a combination of the above.
Secondary outcomes
Lesion progression, if reported separately.
Subjective evaluation of the treatments by participants, regardless of the outcome measure used.
Efficiency (time needed for the intervention), costs or cost‐effectiveness (regardless of how effectiveness was defined).
Any safety issues (e.g. allergies) that were related to the interventions (adverse events).
Search methods for identification of studies
Electronic searches
Cochrane Oral Health's Information Specialist conducted systematic searches in the following databases for RCTs and controlled clinical trials. Due to the Cochrane Centralised Search project to identify all clinical trials on the database and add them to the Central Register of Controlled Trials (CENTRAL), we only searched recent months of the Embase database. See the searching page on the Cochrane Oral Health website for more information. We placed no restrictions on the language or date of publication when searching the electronic databases:
Cochrane Oral Health's Trials Register (searched 21 July 2020) (Appendix 1);
CENTRAL (2020, Issue 6) in the Cochrane Library (Appendix 2);
MEDLINE Ovid (1946 to 21 July 2020) (Appendix 3);
Embase Ovid (13 December 2017 to 21 July 2020) (Appendix 4).
We modelled subject strategies on the search strategy designed for MEDLINE Ovid. Where appropriate, we combined them with subject strategy adaptations of the highly sensitive search strategies designed by Cochrane for identifying RCTs and controlled clinical trials (as described in the Cochrane Handbook for Systematic Reviews of Interventions (Lefebvre 2020)).
Searching other resources
We searched the following trial registries for ongoing studies:
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (clinicaltrials.gov; searched 21 July 2020) (Appendix 5);
World Health Organization International Clinical Trials Registry Platform (apps.who.int/trialsearch; searched 21 July 2020) (Appendix 6).
We checked the bibliographies of included studies and any relevant systematic reviews identified for further references to relevant trials. We did not perform a separate search for adverse effects of interventions. We considered adverse effects described in the included studies only.
We checked that none of the included studies in this review were retracted due to error or fraud.
Data collection and analysis
The methodology for data collection and analysis was based on the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a), and complied with the MECIR document (Higgins 2013).
Selection of studies
Two review authors independently screened the titles and abstracts of records retrieved from the search against the inclusion criteria. The search was designed to be sensitive and include controlled clinical trials, which were filtered out early in the selection process if they were not randomised. If either review author found a record potentially eligible, we obtained and assessed the full text, again independently and in duplicate. Two review authors decided on inclusion by consensus, or in consultation with a third review author. We listed all studies excluded after full‐text assessment in the Characteristics of excluded studies table. We illustrated the study selection process in a PRISMA diagram.
Data extraction and management
Two review authors independently extracted the data from each included study using a specially designed data extraction form, which we first piloted on a small sample of studies. All review authors who performed data extraction piloted this form on the same paper(s) and we compared the content of the fields. We contacted study authors for clarification or missing outcome data where necessary and feasible. We resolved any disagreements through discussion and consulted a third review author when necessary to achieve consensus.
We extracted the following data and recorded it in the Characteristics of included studies table.
Methods: trial design, location, number of centres, recruitment period.
Study details: year of publication and year of study, inclusion/exclusion criteria, number randomised/analysed, study setting (e.g. school, practice).
Population: age, sex and number of participants; baseline caries experience.
Potentially important effect modifiers (dentition; surface location; lesion depth; surface integrity, surface extent).
Interventions: detailed description of the interventions, including number of teeth treated per participant.
Outcome data: details of the outcomes reported and outcome measures, including method of assessment and time point(s) assessed.
Other: funding sources, declarations/conflicts of interest.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias of each included study using the Cochrane risk of bias tool described in Chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b). We contacted study authors for clarification or missing information concerning sequence generation where necessary and feasible. We resolved any disagreements through discussion, consulting a third review author to achieve consensus when necessary.
We completed a risk of bias table for each included study. For each risk of bias domain, we first described what was reported to have happened in the study. This provided the rationale for our judgement of whether that domain was at low, high or unclear risk of bias.
We assessed the following domains.
Sequence generation (selection bias).
Allocation concealment (selection bias).
Blinding (performance and detection bias). Notably, blinding is not always feasible during the interventions (when obviously different operative steps are needed) or outcome examination (when different restorative materials are involved).
Incomplete outcome data (attrition bias).
Selective outcome reporting (reporting bias).
Other bias.
Measures of treatment effect
Relative treatment effects
We analysed dichotomous outcomes (presence or absence of complications indicating treatment failure) and calculated odds ratios (OR) with 95% confidence intervals (CI).
There were no continuous outcome data available for analysis.
We initially planned to calculate the effect estimates using a network meta‐analysis (NMA) wherever possible. Where the underlying assumptions of an NMA were not met or could not be assumed, we calculated the effect estimates from a standard pairwise meta‐analysis.
Relative treatment ranking
We estimated the relative ranking of the different interventions according to our primary outcome using NMA. We estimated the probability of each treatment to be ranked as the most effective, the second most effective, etc. From this information, we calculated the median rank to obtain a hierarchy of the competing interventions according to our primary outcome (these probabilities can also be used to calculate the cumulative ranking curve (SUCRA) (Chaimani 2013; Salanti 2011)).
Unit of analysis issues
Cluster‐randomised trials
Where a participant was randomised to a single intervention, and multiple lesions within a person were evaluated, we considered the person to be the cluster and the lesions clustered within an individual. We found no studies where a cluster was randomised to a single intervention, for example a dental clinic. In split‐mouth studies that randomised one or more teeth to an intervention and comparator trial arm, we considered the individual to be the cluster.
Studies with multiple treatment groups
We considered the multi‐arm studies as multiple independent two‐arm studies in pairwise meta‐analyses. We accounted for the correlation between the effect sizes from multi‐arm studies in the NMA.
Dealing with missing data
We did not need to use other statistical methods or perform any further imputation to account for missing data (Higgins 2011c).
Assessment of heterogeneity
Clinical and methodological heterogeneity within treatment comparisons
We assessed the presence of clinical heterogeneity according to dentition, lesion depth/surface integrity, within each pairwise comparison by comparing the trial and study population characteristics across all eligible trials. We had additionally planned to assess heterogeneity according to lesion location and surface extent; however, most studies did not report this information.
Measures and tests for heterogeneity
We assessed the presence of heterogeneity within each pairwise comparison using a Chi² test, where a P < 0.1 indicated statistically significant heterogeneity. We quantified heterogeneity using the I² statistic to indicate the percentage of variability that could not be attributed to random error using the following: an I² statistic of: 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; and 75% to 100% considerable heterogeneity. This is according to Section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions (Deeks 2011).
Transitivity across treatment comparisons
We assessed the assumption of transitivity by comparing the distribution of potential effect modifiers across the different pairwise comparisons of the network. We evaluated any clinical features that moderate the effects of the different interventions, including dentition and lesion depth (clinically or radiographically measured). We planned to assess surface integrity (cavitation status), but this information was rarely reported.
Assessment of statistical heterogeneity
Assumptions when estimating heterogeneity
In standard pairwise meta‐analyses, we estimated different heterogeneity variances for each pairwise comparison. In NMA, we modelled a common estimate for the heterogeneity variance across the different comparisons.
Measures and tests for heterogeneity
We based our assessment of statistical heterogeneity in the entire network on the magnitude of the heterogeneity variance parameter (Tau²) estimated from the NMA models. We estimated the between‐study standard deviation (Tau) and 95% credible interval (CrI).
Assessment of statistical inconsistency
We used the nodesplit model to check the inconsistency between direct and indirect evidence (Dias 2010). For each treatment comparison with both direct and indirect estimates, we calculated mean and CrIs (2.5% and 97.5% quantiles) for the direct, indirect and network estimates. These estimates were supplemented with a Bayesian P value for the related test of inconsistency between the direct and indirect evidence for each treatment comparison.
Assessment of reporting biases
We planned to assess publication bias according to the recommendations on testing for funnel plot asymmetry (Egger 1997), as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011a). For the NMA, we had planned to use a comparison‐adjusted funnel plot to assess network‐wide publication bias, but as all interventions compared were active and we did not identify anything that was obviously related to small‐study effects in individual trials (e.g. sponsorship status, publication date), we eventually refrained from this.
Data synthesis
Methods for direct treatment comparisons
We performed standard pairwise meta‐analyses using the random‐effects model in Review Manager Web (RevMan Web 2020).
For split‐mouth studies where the dependency of data had been considered, we pooled the data with those of parallel controlled trials using the generic inverse variance method. Where the dependency had not been considered with a split‐mouth design, we did not include these data in a meta‐analysis but reported the results of the trial narratively.
Methods for indirect and mixed comparisons
We performed a Bayesian NMA using MetaInsight, an interactive tool which used the R software package GEMTC that itself calls the Bayesian simulation analysis software JAGS (Owen 2019).
Subgroup analysis and investigation of heterogeneity
Potential sources of heterogeneity were specified a priori:
dentition;
lesion depth/surface status (non‐cavitated, cavitated but not deep, deep);
lesion location (occlusal, smooth surface, proximal, root surface); and
surface extent (one‐, two‐ or three‐surfaced lesions).
Sensitivity analysis
We planned to conduct a sensitivity analysis to investigate the effect of including studies that did not clearly specify lesion depth or surface integrity, but instead accounted for different depths and surface status by subgroup analyses. As one study used a modified placement of a stainless steel crown, not fitting the definition of the HT, we excluded that study from a sensitivity analysis to gauge the impact of including or excluding it (Chompu‐inwai 2015).
Summary of findings and assessment of the certainty of the evidence
Using GRADEpro GDT software, we generated a summary of findings tables for the main comparisons for the primary outcome. We assessed the certainty of the evidence using GRADE criteria (GRADE 2013).
Results
Description of studies
Results of the search
The initial search was carried out in June 2018 and updated several times, most recently in July 2020. We identified a further 17 articles that were related to the clinical trial protocols records. There were 7223 references in total and 4075 after deduplication. The titles were screened against the inclusion criteria and 3950 references discarded. We read the full‐texts for the remaining 141 references (102 studies) and excluded a further 94 references (75 studies) (see Excluded studies; Characteristics of excluded studies table) including one ongoing study (Vicioni‐Marques 2018). Therefore, 27 studies (47 full‐text articles) met the inclusion criteria for this review (Figure 1).
1.
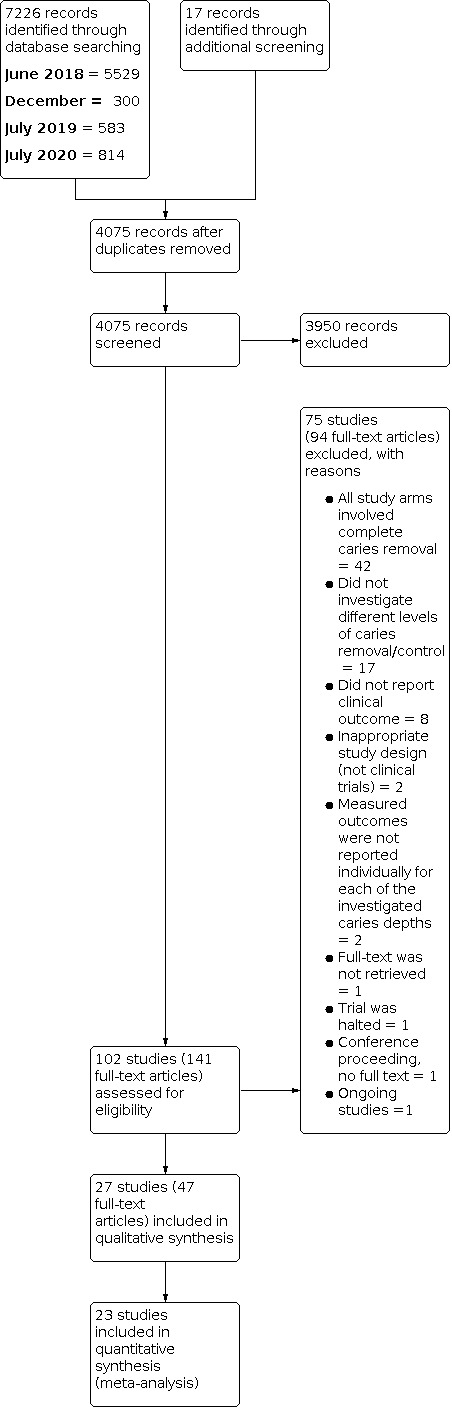
Study flow diagram.
Included studies
Trial designs and settings
The 27 included studies were published between 1977 and 2020.
The trials were conducted in 11 countries. Most trials were conducted in Brazil (13 studies). Two trials were conducted in: Germany (Elhennawy 2021; Santamaria 2018), Scotland (Foley 2004; Innes 2011), Sweden (Leksell 1996; Magnusson 1977), and Thailand (Chompu‐inwai 2015; Phonghanyudh 2012). One study was carried out in: Denmark (Bjørndal 2017), Egypt (Labib 2019), India (Khokhar 2018), New Zealand (Boyd 2021), Turkey (Orhan 2010), and the US (Mertz‐Fairhurst 1998).
All studies were published in English.
In terms of the trial design, parallel groups were the dominant trial design (24 studies), with only three studies adopting a split‐mouth approach (Borges 2012a; Innes 2011; Mertz‐Fairhurst 1998). Of the parallel‐group studies, seven had no clustering of teeth within participants (i.e. only one tooth treated per participant) (Araujo 2020; Bjørndal 2017; Hesse 2014; Khokhar 2018; Phonghanyudh 2012; Qvist 2017; Santamaria 2018); the remaining studies limited clustering, typically with only one tooth assessed per participant.
Most studies (23) were conducted within a secondary care setting, chiefly university dental clinics. One study included both primary and secondary setting (Maltz 2018). Of the remaining three trials, one was in a school setting (Araujo 2020), and two were in primary care (Boyd 2021; Innes 2011).
Participants
In total, studies recruited 3350 participants (minimum 28 in Dias 2018; maximum 521 in Qvist 2017; mean 77; median 68), with 4195 teeth/lesions treated.
The minimum age of participants was three years old, while the oldest participants were 54 years old. Two studies treated adults (Bjørndal 2017; Labib 2019). Five studies mixed adults, adolescents and children (Alves 2017; Borges 2012b; Khokhar 2018; Maltz 2018; Mertz‐Fairhurst 1998), and the remaining included adolescents and children. The mean age group for da Silveira 2012 was between 12.3 and 13.5 years with no further information on the participants' ages.
For the inclusion criteria of lesion depth into the dentine, most studies used clinical and radiographic examinations to assess this parameter (24 studies). Three studies used only clinical detection to assess the depth of the carious lesion (Araujo 2020; Magnusson 1977; Santamaria 2018). Five studies included lesions that extended into the middle third of dentine depth or beyond (Alves 2017; Borges 2012a; Borges 2012b; da Silveira 2012; Mello 2018), and one used the outer third (Phonghanyudh 2012). Four studies focused on carious lesions confined to the outer half of dentine (Boyd 2021; Dias 2018; Hesse 2014; Qvist 2017). Ten trials specified strictly including only teeth with deep carious lesions although the descriptions varied. One study only included the very deep lesion where "complete excavation" may lead to pulp exposure (Leksell 1996). Four studies used lesion extension to at least three‐quarters of the dentine depth as their inclusion criterion (Bjørndal 2017; Chompu‐inwai 2015; Franzon 2014; Orhan 2010). Two studies used the inner third of dentine or beyond (Elhennawy 2021; Labib 2019). Three studies used the inner half of dentine depth as their inclusion threshold (Khokhar 2018; Lula 2009; Maltz 2018). The remaining three clinical trials did not specify carious lesion depth, with only no signs of pulpal involvement being the inclusion criteria for lesion depth (Foley 2004; Innes 2011; Ribeiro 1999).
Ten studies included only permanent teeth (Alves 2017; Bjørndal 2017; Borges 2012b; da Silveira 2012; Khokhar 2018; Labib 2019; Leksell 1996; Maltz 2018; Mertz‐Fairhurst 1998; Qvist 2017). One study included both dentitions (Orhan 2010). The remaining 16 trials investigated the primary dentition.
The studies were eventually stratified into three groups (see below); three studies managed non‐cavitated lesions (Borges 2012a; Borges 2012b; da Silveira 2012), 12 managed cavitated, deep lesions (Bjørndal 2017; Chompu‐inwai 2015; Elhennawy 2021; Franzon 2014; Khokhar 2018; Labib 2019; Leksell 1996; Lula 2009; Magnusson 1977; Maltz 2018; Mello 2018; Orhan 2010), and the remaining 12 studies managed cavitated, but not deep lesions or lesions of varying depth (Alves 2017; Araujo 2020; Boyd 2021; Dias 2018; Foley 2004; Hesse 2014; Innes 2011; Mertz‐Fairhurst 1998; Phonghanyudh 2012; Qvist 2017; Ribeiro 1999; Santamaria 2018).
Interventions
Two studies had three trial arms that investigated different extents of caries removal (Orhan 2010; Santamaria 2018). All other studies had two trial arms included in the review. Two studies had three arms, but combined two into one (Chompu‐inwai 2015; Mertz‐Fairhurst 1998), and we excluded one arm in two studies: the ART group arm in Phonghanyudh 2012) and the Black Copper Cement arm in Foley 2004 as this material is not commonly available or used.
CR was the most commonly investigated arm with 19 comparisons in 17 studies. The most common comparison was between CR and SE, with eight studies (Foley 2004; Franzon 2014; Khokhar 2018; Lula 2009; Mello 2018; Orhan 2010; Phonghanyudh 2012; Ribeiro 1999). Four studies compared CR with SW (Bjørndal 2017; Leksell 1996; Magnusson 1977; Orhan 2010), and another two studies comparing CR with HT (Innes 2011; Santamaria 2018). Four studies compared CR and sealing with sealants (Alves 2017; Borges 2012a; Mertz‐Fairhurst 1998; Qvist 2017), and one study compared CR with NRCC (Santamaria 2018).
Two studies compared SE and HT (Araujo 2020; Boyd 2021); another study compared a modified HT versus SE (Chompu‐inwai 2015).
Four studies compared SW and SE (Elhennawy 2021; Labib 2019; Maltz 2018; Orhan 2010).
Two studies compared SE with sealing (Dias 2018; Hesse 2014). Two studies compared sealing versus no sealing (Borges 2012b; da Silveira 2012); both groups received oral hygiene instruction.
Outcomes
Primary outcomes
Most trials (23) used a binary outcome expressed with either success or failure of the procedure conducted. The four other studies used three main outcomes: success, major, and minor failure (Araujo 2020; Boyd 2021; Innes 2011; Santamaria 2018).
There were a wide variety of outcomes, many of which were composite outcomes (such as the combination of clinical and radiographic outcomes to indicate success or failure of a restoration).
Methods of outcome assessments were similar, but assessment criteria varied across the trials. Pulpal signs and symptoms and loss of vitality were the primary outcomes for 15 references (Araujo 2020; Bjørndal 2017; Boyd 2021; Chompu‐inwai 2015; Elhennawy 2021; Innes 2011; Khokhar 2018; Labib 2019; Leksell 1996; Lula 2009; Maltz 2018; Mello 2018; Orhan 2010; Phonghanyudh 2012; Santamaria 2018). This outcome was measured radiographically by recording the presence or absence of the pathogenic changes within the pulp and the areas around the tooth such as radiolucency at the radicular or apical area, or widening of the periodontal ligament. Clinically, the presence/absence of signs and symptoms related to pulp diseases such as abscess, pain or mobility.
Some studies investigated restoration survival (including survival of a sealant). Ten studies assessed the marginal integrity of the restoration (Alves 2017; Borges 2012a; Dias 2018; Elhennawy 2021; Franzon 2014; Hesse 2014; Labib 2019; Mertz‐Fairhurst 1998; Qvist 2017; Ribeiro 1999), and five studies measured retention of the restoration (Alves 2017; Foley 2004; Maltz 2018; Mertz‐Fairhurst 1998; Phonghanyudh 2012).
Four studies considered restoration survival (or restoration lost) and lesion progression (secondary caries) as minor failures (Araujo 2020; Boyd 2021; Innes 2011; Santamaria 2018).
Secondary outcomes
Trial authors mainly considered outcomes assessed at the point of treatment delivery as a secondary outcome (e.g. the time required to carry out the procedure; Araujo 2020; Dias 2018; Elhennawy 2021; Franzon 2014; Innes 2011). Four studies considered cost‐effectiveness a secondary outcome (Elhennawy 2021; Innes 2011; Labib 2019; Santamaria 2018).
Three studies measured lesion progression radiographically, or clinically by assessing cavitation (Borges 2012a; Borges 2012b; da Silveira 2012), and five studies assessed pain and sensitivity (Alves 2017; Borges 2012a; Borges 2012b; Lula 2009; Orhan 2010).
Secondary outcomes also included a range of participant‐centred outcomes. These were either reported by the participants or their carers, such as pain (Santamaria 2018), anxiety level using a visual analogue scale (Dias 2018; Elhennawy 2021), and participant acceptability to treatment through assessing their treatment comfort level (Araujo 2020). Other participant‐centred outcomes were reported by the operator such as a child's behaviour using Frankl Behaviour Rating (Santamaria 2018). Two other studies assessed treatment perceptions/preferences for all stakeholders (Innes 2011; Santamaria 2018). Araujo 2020 assessed the child's Oral Health‐related Quality of Life measure (OHRQoL)) six months after treatment.
Follow‐up times
One study had no follow‐up (where only pulp exposure at the time of treatment was carried out) (Magnusson 1977). The maximum period of follow‐up for the remaining studies varied from a minimum of four to six months (Lula 2009; Mello 2018) to 10 years (Mertz‐Fairhurst 1998). Twelve months was the most common maximum follow‐up (nine studies: Borges 2012a; Borges 2012b; da Silveira 2012; Elhennawy 2021; Labib 2019; Leksell 1996; Orhan 2010; Phonghanyudh 2012; Ribeiro 1999). Other maximum follow‐up times were: 18 months in two studies (Hesse 2014; Khokhar 2018), 24 months in five studies (Boyd 2021; Chompu‐inwai 2015; Dias 2018; Foley 2004; Franzon 2014), 30 months in one study (Santamaria 2018), 36 months in one study (Araujo 2020), 48 months in one study (Alves 2017), 60 months in three studies (Bjørndal 2017; Innes 2011; Maltz 2018), and 84 months in one study (Qvist 2017).
Excluded studies
We excluded 74 studies (94 full‐text articles) after reading the full‐text. Ten studies included one or more related publications (Straffon 1988a; Hamilton 2001; Handelman 1976; Lozano‐Chourio 2006; Mandari 2001; Martignon 2012; Motta 2013; Straffon 1988b; Taifour 2003; Valério 2016). Details of the excluded studies and the reasons for exclusion can be found in the Characteristics of excluded studies table. The main reason for exclusion for most studies (59) was that they did not compare two different levels of carious tissue removal (i.e. it was unclear if they used the same or different endpoints of tissue removal, which is one of the main discriminator between CR and SE, for instance; this mainly applied to studies involving ART); usually, studies compared different methods of carious tissue removal, different restorative techniques or different restorative materials. Eight studies did not report clinical outcomes or data relevant to the review. The inappropriate study design was another reason for excluding two reports: one was a systematic review (Hoefler 2016), and the other was a commentary (Santamaria 2014). Full‐texts could not be retrieved for one conference proceeding (Peters 2006) and one paper (Tavciovski 1966).
Ongoing studies
One study is ongoing (Vicioni‐Marques 2018; Characteristics of ongoing studies table).
Risk of bias in included studies
All studies were at high risk of bias overall as they were at high risk of bias in one or more domains. The risk of bias across and within the included studies is summed up in Figure 2 and Figure 3.
2.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Two studies were at high risk of bias for random sequence generation: one used odd or even date of birth (Magnusson 1977) and one study used "lots" and had one stage rather than a more appropriate two stage randomisation (Orhan 2010). If a two‐stage process had been used, the first step of the intervention that was common to different treatments could have been performed by the operator without them being influenced by the next part of the treatment; it is possible they may have been more cautious in deepening the cavity to avoid a pulp exposure depending on whether they were aware the patient was returning. Six studies did not give adequate information on sequence generation (Boyd 2021; Chompu‐inwai 2015; Khokhar 2018; Leksell 1996; Mello 2018; Phonghanyudh 2012; Ribeiro 1999). The other 18 studies were considered low risk of bias for random sequence generation.
Two studies were at high risk of bias for allocation concealment (Magnusson 1977; Orhan 2010), and nine studies were at unclear risk of bias. In eight, it was unclear how allocation concealment was carried out or the time that allocation was revealed (or both) were not clearly described (Boyd 2021; Franzon 2014; Hesse 2014; Leksell 1996; Mello 2018; Mertz‐Fairhurst 1998; Ribeiro 1999; Santamaria 2018), and in one study, the investigator assigned the sealed envelopes (Khokhar 2018). The remaining 16 studies were at low risk of bias for allocation concealment.
Blinding
The greatest sources of bias across all the studies were in performance bias and detection bias.
For performance bias (blinding of participants and personnel), no studies were at low risk of bias as there were different protocols for carious tissue removal to be followed or different restorations to be placed. Even when efforts were made to avoid the operator being aware of the treatments where there were two steps and the first step was common to both treatments, the operator knew during the second step what the treatment was going to be. Participants often could not be blinded because there was a difference in the appointments (e.g. some had to return for another appointment if SW was carried out) or because the restorative material was noticeably different (e.g. amalgam compared with composite or an HT crown compared to a filling). In four studies, blinding of participants and personnel was unclear (Bjørndal 2017; Hesse 2014; Khokhar 2018; Phonghanyudh 2012).
For detection bias (blinding of examiners), seven studies were at low risk of bias (Chompu‐inwai 2015; Elhennawy 2021; Franzon 2014; Khokhar 2018; Labib 2019; Maltz 2018; Phonghanyudh 2012). In 18 studies, there was a high risk of bias because the assessors could see the difference in the restorative material clinically or the extent of carious tissue removal radiographically. Two studies were at unclear risk of bias because information on blinding of examiners was not reported (Magnusson 1977; Santamaria 2018).
Incomplete outcome data
There were no concerns about attrition bias in 20 studies. Five studies were at high risk of bias due to lack of clarity over loss to follow‐up at mid‐time points (Chompu‐inwai 2015; da Silveira 2012; Dias 2018; Foley 2004; Leksell 1996), and in one study, failures were removed (Foley 2004), rather than because of a high proportion of attrition. The attrition rate was unclear because of unclear reporting in two studies (Franzon 2014; Mertz‐Fairhurst 1998).
Selective reporting
There was adequate reporting of all planned outcomes in 16 studies. Seven studies were at high risk of bias. Three of them did not fully report all outcomes (Foley 2004; Mertz‐Fairhurst 1998; Ribeiro 1999). One study excluded teeth from the analysis because they had experienced a failure (Chompu‐inwai 2015), and one study re‐treated the teeth and did not count them as failures (da Silveira 2012). One study reported only 18‐month results when the study protocol had stated that more time points would be reported (Khokhar 2018). One study reported enamel and dentine lesions' outcomes together and there was insufficient information to only include the dentine lesions that were restored (Qvist 2017).
Four studies were at unclear risk of bias as there was no study protocol available (Borges 2012a; Borges 2012b; Boyd 2021; Magnusson 1977).
Other potential sources of bias
Three studies had other forms of bias considered relevant. One study was at high risk of other bias due to the method of evaluation (Maltz 2018). Two studies were at unclear risk of other bias, one because there was inconsistency in the data presentation (Mertz‐Fairhurst 1998), and the other was poorly reported with missing information on the interventions and the depths of the initial lesions (Magnusson 1977).
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10.
We included 27 studies in this review. All studies reported the primary outcome, failure; most (23) used a binary outcome (failure); four studies reported three main outcomes (overall failure, minor failure, major failure). Seven studies included secondary outcomes including: the time required to carry out the procedure; cost‐effectiveness; patient‐centred outcomes – pain, anxiety level, participant acceptability to treatment; operator assessment of child's behaviour; treatment preferences; and OHRQoL (Araujo 2020; Dias 2018; Elhennawy 2021; Franzon 2014; Innes 2011; Labib 2019; Santamaria 2018).
As dentition and lesion depth/surface status were commonly reported and carry different clinical indications, we grouped studies with six potential subgroups according to dentition (primary versus permanent) and lesion depth plus surface status (non‐cavitated, cavitated but not deep into dentine and deep lesions). Five studies did not contribute to the meta‐analyses and are reported narratively (Table 12; Borges 2012a; Foley 2004; Magnusson 1977; Mertz‐Fairhurst 1998; Qvist 2017).
2. Included studies that did not contribute to the meta‐analyses, and reason.
| Study | Explanation for exclusion from meta‐analysis |
| Borges 2012a | Insufficient reporting to account for split mouth. |
| Foley 2004 | Data could not be extracted at individual intervention levels. Authors were contacted for previous review and gave the dataset they had, but because caries management was combined with restoration, it still was not possible. |
| Magnusson 1977 | Only pulp exposures were included numerically and no other outcome data were available. |
| Mertz‐Fairhurst 1998 | Insufficient reporting to account for split mouth. |
| Qvist 2017 | Although numbers were reported at baseline for different lesion depths, these were reported together in the results table and it was not possible to separate enamel from dentine lesions for the meta‐analysis (only cavitated or dentine lesions were of interest for this review). |
Primary outcome
Failure of therapy
Comparison 1: sealing using sealant materials compared to non‐selective carious tissue removal and conventional restoration for treating cavitated or dentine carious lesions
Two parallel RCTs (Alves 2017; Qvist 2017), and two split‐mouth RCTs (Borges 2012b; Mertz‐Fairhurst 1998) reported on failure. However, Qvist 2017 included both enamel and dentine lesions. These were separated into enamel and dentine lesions in the baseline characteristics table. While most lesions extended into dentine clinically or radiographically (hence fitting our inclusion criteria), the presentation of the results did not differentiate the outcomes for lesion depths and we could not determine which were for dentine lesions only. Hence, this study could not be included in the meta‐analysis. For all depths of lesions, 115/368 sealed and 11/153 CR lesions required re‐treatment (however, as stated, this included both the enamel and the dentine lesions). Based on the overall results, sealing using sealing materials may result in an increase of failure compared to CR, mainly due to loss of sealants. Overall, the data supporting this were limited.
The other parallel group study was included in the meta‐analysis, and reported that 4/20 sealed and 1/21 CR lesions required re‐treatment (OR 5.00, 95% CI 0.51 to 49.27) (Alves 2017). Based on this study, there was insufficient evidence of a difference between sealing and CR for cavitated lesions in the permanent dentition (Analysis 1.1; Figure 4).
1.1. Analysis.

Comparison 1: Sealing versus conventional restoration (CR) (cavitated, permanent dentition), Outcome 1: Failure: sealing vs CR
4.

1.1. Failure ‐ sealing vs CR
Two additional split‐mouth studies comparing sealing versus CR reported on this outcome and confirmed the findings. These were split‐mouth RCTs on cavitated, permanent teeth (Mertz‐Fairhurst 1998), and non‐cavitated, primary teeth (Borges 2012a). Notably, Mertz‐Fairhurst 1998 performed bevelling of the enamel margin, but there was no carious tissue removal. This study reported 12/85 sealed and 8/85 CR teeth experienced failures over 10 years, whereas Borges 2012a reported 3/26 sealed and 0/26 CR teeth experienced failures after one year. Both RCTs were at high risk of bias, and neither study could be included in the meta‐analysis as they did not report results accounting for the split‐mouth study design.
We judged the certainty of evidence for this comparison to be very low, downgrading for study limitations (risk of bias), and imprecision.
Comparison 2: sealing with sealant materials compared to selective carious tissue excavation for treating cavitated or dentine carious lesions
Two RCTs reported failure for cavitated lesions in the primary dentition (Dias 2018; Hesse 2014). The pooled estimate indicated that there was insufficient evidence of a difference between sealing with sealant materials compared to selective carious tissue excavation (OR 3.11, 95% CI 0.11 to 85.52; I2 = 74%; 2 trials, 82 teeth; Analysis 2.1; Figure 5).
2.1. Analysis.

Comparison 2: Sealing versus selective excavation (SE) (cavitated, primary dentition), Outcome 1: Failure: sealing vs SE
5.

2.1 Failure ‐ sealing vs SE
We judged the certainty of evidence to be very low for this comparison, downgrading for study limitations (risk of bias), inconsistency and imprecision.
Comparison 3: sealing compared to no treatment for treating cavitated or dentine carious lesions
Two RCTs reported on failure for non‐cavitated lesions in the permanent dentition (Borges 2012b; da Silveira 2012). The evidence was very uncertain about the effect of sealing with sealant materials compared to no treatment on failure (pooled estimate OR 0.05, 95% CI 0.00 to 2.71; I2 = 89%; 2 trials, 103 teeth; Analysis 3.1; Figure 6).
3.1. Analysis.

Comparison 3: Sealing versus no treatment (non‐cavitated, permanent), Outcome 1: Failure: sealing vs no treatment
6.

3.1 Failure ‐ sealing vs no treatment
We judged the certainty of evidence to be very low for this comparison, downgrading for study limitations (risk of bias), inconsistency and imprecision.
Comparison 4: non‐selective carious tissue removal and conventional restoration compared to the Hall Technique for treating cavitated or dentine carious lesions
One split‐mouth RCT (Innes 2011) and one parallel group RCT (Santamaria 2018) reported on failure for cavitated lesions in the primary dentition. HT may result in a large reduction in failure compared to non‐selective carious tissue removal and CR (pooled estimate OR 8.35, 95% CI 3.73 to 18.68; I2 = 0%; 2 trials, 249 teeth; Analysis 4.1; Figure 7).
4.1. Analysis.

Comparison 4: Conventional restoration (CR) versus Hall Technique (HT) (cavitated, primary), Outcome 1: Failure: CR vs HT
7.

4.1 Failure ‐ CR vs HT
We judged the certainty of evidence for this comparison to be low, downgrading for study limitations (risk of bias) and imprecision.
Comparison 5: selective carious tissue excavation compared to Hall Technique for treating cavitated or dentine carious lesions
Two RCTs reported on failure for the primary dentition with cavitated but not deep lesions (Araujo 2020; Boyd 2021). The evidence about the effect of selective carious tissue excavation compared to the HT on failures was very uncertain (pooled estimate OR 8.94, 95% CI 0.57 to 139.67; I2 = 92%; 2 trials, 586 teeth; Analysis 5.1; Figure 8). We judged the certainty of evidence to be very low, downgrading for study limitations (high risk of bias), inconsistency and imprecision.
5.1. Analysis.

Comparison 5: Selective excavation (SE) versus Hall Technique (HT) (primary, cavitated; primary, deep), Outcome 1: Failure: SE vs HT
8.

5.1 Failure ‐ SE vs HT
The result was similar with primary teeth with cavitated and deep lesions (OR 1.95, 95% CI 0.57 to 6.63; 1 trial, 72 teeth; Analysis 5.1; Figure 8) (Chompu‐inwai 2015). We judged the certainty of evidence to be very low, downgrading for study limitations (high risk of bias) and serious imprecision.
Comparison 6: non‐selective carious tissue removal and conventional restoration compared to non‐restorative cavity control for treating cavitated or dentine carious lesions
One RCT reported on failure for cavitated lesions in the primary dentition (Santamaria 2018). There was insufficient evidence of a difference between CR compared to NRCC, and the evidence is very uncertain about the effect of CR for treating cavitated or dentine carious lesions (pooled estimate OR 1.16, 95% CI 0.50 to 2.71; 1 trial, 102 teeth; Analysis 6.1; Figure 9).
6.1. Analysis.

Comparison 6: Conventional restoration (CR) versus non‐restorative cavity control (NRCC) (cavitated, primary), Outcome 1: Failure: CR vs NRCC
9.

6.1 Failure ‐ CR vs NRCC
We judged the certainty of evidence for this comparison to be very low, downgrading for study limitations (high risk of bias from lack of blinding of participants) and serious imprecision.
Comparison 7: Hall Technique compared to non‐restorative cavity control for treating cavitated or dentine carious lesions
One RCT reported on failure for cavitated lesions in the primary dentition (Santamaria 2018). HT may result in a reduction in failure when compared to NRCC, but the evidence is very uncertain (OR 0.19, 95% CI 0.05 to 0.74; 1 trial, 84 teeth; Analysis 7.1; Figure 10).
7.1. Analysis.

Comparison 7: Hall Technique (HT) versus non‐restorative cavity control (NRCC) (cavitated, primary), Outcome 1: Failure: HT vs NRCC
10.

7.1 Failure ‐ HT vs NRCC
We judged the certainty of evidence for this comparison to be very low, downgrading for study limitations (high risk of bias from lack of blinding of participants) and serious imprecision.
Comparison 8: stepwise carious tissue removal compared to non‐selective carious tissue removal and conventional restoration for treating cavitated or dentine carious lesions
One RCT reported failure for deep lesions in both the primary and permanent dentition (Orhan 2010), and two for deep lesions in the permanent dentition (Bjørndal 2017; Leksell 1996).
For deep lesions in primary teeth, there was insufficient evidence of a difference in failure between SW and CR (pooled estimate OR 2.43, 95% CI 0.65 to 9.12; 1 study, 63 teeth; Analysis 8.1; Figure 11).
8.1. Analysis.

Comparison 8: Conventional restoration (CR) versus stepwise (SW) (deep, primary; deep, permanent), Outcome 1: Failure: CR vs SW
11.

8.1 Failure ‐ CR vs SW
We judged the certainty of evidence for this comparison to be very low, downgrading for study limitations (high risk of bias for sequence generation, allocation concealment and blinding) and serious imprecision.
For deep lesions in permanent teeth, SW likely results in a reduction of failure compared with conventional removal and restoration (OR 2.06, 95% CI 1.34 to 3.17; I2 = 0%; 3 studies, 398 teeth; Analysis 8.1; Figure 11).
We judged the certainty of evidence for this comparison to be moderate, downgrading for study limitations (high risk of bias, principally from lack of blinding).
Comparison 9: selective carious tissue excavation compared to non‐selective carious tissue removal and conventional restoration for treating cavitated or dentine carious lesions
Two RCTs reported the effects of the intervention in permanent teeth with deep lesions (Khokhar 2018; Orhan 2010), four studies in primary teeth with deep lesions (Franzon 2014; Lula 2009; Mello 2018; Orhan 2010), and two studies in primary teeth with cavitated but not deep lesions (Phonghanyudh 2012; Ribeiro 1999).
In permanent teeth selective carious tissue excavation may reduce the number of failures compared with CR, but the evidence is very uncertain (pooled estimate OR 11.32, 95% CI 1.97 to 65.02; I2 = 0%; 2 studies, 179 teeth; Analysis 9.1; Figure 12).
9.1. Analysis.

Comparison 9: Conventional restoration (CR) versus selective excavation (SE) (deep, permanent; deep, primary; cavitated, primary), Outcome 1: Failure: CR vs SE
12.

9.1 Failure ‐ CR vs SE
We judged the certainty of evidence to be very low, downgrading for study limitations (high risk of bias for sequence generation, allocation concealment and blinding for one study with 62% weight) and serious imprecision.
In primary teeth with deep lesions, selective carious tissue excavation may result in fewer failures compared with non‐selective carious tissue removal and CR, but the evidence is very uncertain. (pooled estimate OR 4.43, 95% CI 1.04 to 18.77; I2 = 66%; 4 studies, 265 teeth; Analysis 9.1; Figure 12).
We judged the certainty of evidence to be very low, downgrading for study limitations, inconsistency and imprecision.
In primary teeth with cavitated but not deep lesions there was insufficient evidence of a difference in failure between selective carious tissue removal and non‐selective carious tissue removal and CR (OR 0.62, 95% CI 0.21 to 1.88; I2 = 11%; 2 studies, 204 teeth; Analysis 9.1; Figure 12).
We judged the certainty of evidence to be very low, downgrading for study limitations and serious imprecision.
Comparison 10: stepwise excavation of carious tissues compared to selective excavation of carious tissues for treating cavitated or dentine carious lesions
Two RCTs reported failure in primary teeth with deep lesions (Elhennawy 2021; Orhan 2010), and three studies reported failure in permanent teeth with deep lesions (Labib 2019; Maltz 2018; Orhan 2010).
In primary teeth with deep lesions, there was insufficient evidence of a difference between SW and SE of carious tissue (pooled estimate OR 2.05, 95% CI 0.49 to 8.62; I2 = 0%; 2 studies, 126 teeth; Analysis 10.1; Figure 13). We judged the certainty of evidence to be very low, downgrading for study limitations (high risk of bias for sequence generation, allocation concealment and blinding for one study with 66% weight) and serious imprecision.
10.1. Analysis.

Comparison 10: Stepwise (SW) versus selective excavation (SE) (deep, primary; deep, permanent), Outcome 1: Failure: SW vs SE
13.

10.1 Failure ‐ SW vs SE
In permanent teeth with deep lesions, SE is likely to reduce failure compared to SW (pooled estimate OR 2.25, 95% CI 1.33 to 3.82; I2 = 0%; 3 studies, 371 teeth; Analysis 10.1; Figure 13). We judged the certainty of evidence to be moderate, downgrading for study limitations (high risk of bias, principally from lack of blinding).
Network meta‐analysis on deep lesions
We planned to conduct an NMA to include all comparisons. Dentition, lesion depth/surface status, lesion location and surface extent were proposed as potential effect modifiers. The included studies reported lesion location and surface extent only infrequently. We explored the distribution of dentition and lesion depth/surface status across the pairwise contrasts for the direct comparisons, and found that the proportions of cavitated and deep categories were dissimilar across the direct contrasts, with only one study reporting the primary outcome at the non‐cavitated level. There were similar issues according to dentition where only five of the nine direct comparisons involved a mixture of primary and permanent dentition and four comparisons involved primary dentition only. Therefore, we elected to undertake the NMA for the 11 parallel group RCTs that evaluated deep lesions only, where the distribution of studies that evaluated treatment effects in the permanent or primary dentition was approximately equal (Bjørndal 2017; Chompu‐inwai 2015; Elhennawy 2021; Franzon 2014; Khokhar 2018; Labib 2019; Leksell 1996; Lula 2009; Maltz 2018; Mello 2018; Orhan 2010).
The included studies treated 1316 participants and observed 353 failures. Of these, 10 were two‐arm studies and one was a three‐arm study (which reported results for the primary and permanent dentition) (Orhan 2010). There were 16 pairwise comparisons for our NMA (4 compared SW versus CR, 5 compared SW versus SE, 6 compared SE versus CR and 1 compared SE versus a modified HT). In a sensitivity analysis, the study using a modified version of the HT was excluded (Chompu‐inwai 2015). The resulting networks are displayed in Figure 14. There was no evidence of incoherence using the node‐splitting approach for the base‐case of all studies or the sensitivity analysis of the subset of studies removing the study with a modified intervention (Chompu‐inwai 2015).
14.
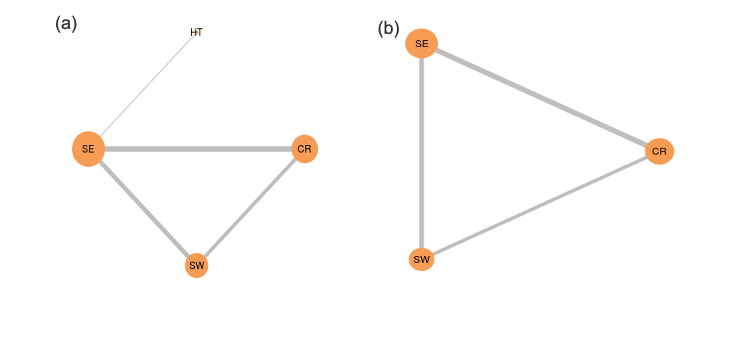
Network plot for different interventions for managing deep lesions. (a) Base‐case analysis, (b) sensitivity analysis excluding the single study using a modified Hall Technique (HT). Nodes (orange circles) and connections (grey lines) are used to display actual pairwise comparisons. The size of the node indicates the number of studies testing this strategy; thickness of the lines indicates the number of studies in which exact comparison was made.
CR: complete removal; SE: selective removal; SW: stepwise removal.
In the base‐case analysis, there is evidence of a difference in effectiveness of HT, SE and SW versus CR favouring the non‐CR interventions, while there was insufficient evidence of a difference for the remaining three pairwise comparisons. Conclusions were similar for the sensitivity analysis excluding the study that employed modified HT intervention, with evidence of a difference in effectiveness of SE or SW versus CR favouring the non‐CR interventions, with insufficient evidence of a difference for the SW versus SE comparison (Figure 15). Between‐study standard deviation (tau) was 0.96 (95% CrI 0.31 to 2.03).
15.
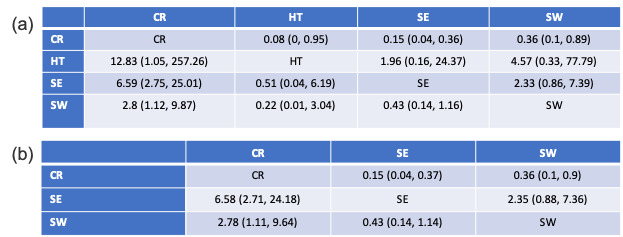
Network meta‐analysis relative effects of different interventions for treating deep lesions. (a) Base‐case analysis, (b) sensitivity analysis excluding the single study which used a modified Hall Technique (HT). Odds ratio and 95% credible intervals are shown. The odds of failure with each intervention in each row is compared against the ones in each column (e.g. in (a), CR had a 12.83 (1.05–252) times increased odds of failure compared with HT).
CR: complete removal; SE: selective removal; SW: stepwise removal.
When ranking the treatments according to failure, CR was lowest (highest risk of failure) in both the base‐case and the sensitivity analysis (the probability of CR being ranked last was 96% in the base‐case analysis and 98% in the sensitivity analysis). In the base‐case, the median rank for the modified HT was ranked first (the probability of this was 72%), followed by SE (median rank of 2) and SW (median rank of 3), while SE was ranked first (96% probability) and SW second in the sensitivity analysis. There was no evidence of statistical inconsistency at either a global or local level (comparison CR versus SE: P = 0.668; comparison CR versus SW: P = 0.667; comparison SE versus SW: P = 0.539; Appendix 7).
It should be noted that the network is relatively sparse, and that the use of the random‐effects model with a relatively small number of studies in which the number of events is small can be problematic, particularly with regards to the ranking of interventions. When a treatment effect is very uncertain and has a wide CI, it can contain very large effects and thus be ranked very highly, even though very little is known about how good the intervention is in practice. Caution against the over interpretation of ranking statistics that may not be very numerically stable in such situations is warranted.
To investigate the impact of choice of model, random versus fixed, we undertook a post hoc sensitivity analysis with analysis according to a fixed‐effect model. We observed that while the effect estimates were generally smaller than with the random‐effects model, the resultant ranking was stable and consistent with those of the random‐effects model (Appendix 8).
Secondary outcomes
Certain studies provided further outcomes beyond success, such as major or minor complications (Araujo 2020; Chompu‐inwai 2015; Innes 2011), but as these were generally in line with the results of the success reported in the same studies, we refrained from applying further meta‐analyses to them.
Lesion progression
Five studies reported progression of sealed or residual lesions (Borges 2012a; da Silveira 2012; Dias 2018; Hesse 2014; Ribeiro 1999), confirming the arrest of the majority of the sealed or residual lesions in most studies. Borges 2012a found 3/26 sealed lesions to have progressed after one year, da Silveira 2012 found 3/27 lesions after one year, Dias 2018 found 1/27 sealed and 1/21 SE lesions after two years, Hesse 2014 found 0/17 sealed and 0/17 SE lesions after 18 months and Ribeiro 1999 found 6/24 sealed after 12 months.
Subjective evaluation of the treatments by participants
We found no studies reporting subjective evaluation of the treatments by participants.
Efficiency, costs or cost‐effectiveness
With regards to cost outcomes, the available studies found HT more cost‐effective than CR or NRCC in primary teeth (Innes 2011; Santamaria 2018), or SE more cost‐effective than SW in permanent (Labib 2019) and primary teeth (Elhennawy 2021). We did not report on these in detail as the cost‐effectiveness findings were specific to the underlying setting and (for modelling studies) assumptions about pricing, etc.
Any safety issues
None of the studies reported adverse effects.
Discussion
This is a comprehensive review of interventions for treating cavitated or dentine carious lesions. It supersedes a more focused Cochrane Review on this clinical area, originally published in 2013 (Ricketts 2013). Since then, a wider number of alternatives to the conventional approach towards cavitated or dentine lesions (e.g. sealing of lesions using resin or glass ionomer sealants; sealing using the HT; or an NRCC approach) have been developed or been more widely tested in RCTs (or both). Our inclusion criteria and analytic strategy aimed at capturing these studies and reflecting on their findings.
Given that we considered such a wide range of interventions for managing lesions that traditionally received non‐selective carious tissue removal and CR, a large number of pairwise meta‐analyses were expected and conducted. We had further aimed to lever this network of studies and perform an NMA, yielding rankings and more comprehensive comparisons of interventions. Notably, and given the limitations in transitivity (i.e. homogeneity of intervention arms across the network), such NMA was only possible for one specific lesion depth (i.e. deep lesions); the results of this are discussed further below.
Summary of main results
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10.
We included 27 studies in this review and 23 studies in the meta‐analyses. We assessed the certainty of evidence for 10 comparisons, all of which provided data on our primary composite outcome of failure.
Studies were published from all over the world; the majority since 2005. Studies focused on non‐cavitated, cavitated but not deep, and deep lesions; more studies reported on the primary than the permanent dentition, while even for permanent teeth, notable conclusions emerged.
Sealing using sealant materials compared to non‐selective carious tissue removal and CR for treating cavitated or dentine carious lesions: for the outcome of failure, there was very uncertain evidence from one study for any difference between sealing using sealant materials and non‐selective carious tissue removal and CR. This study followed up participants to 48 months.
Sealing with sealant materials compared to SE for treating cavitated or dentine carious lesions: for the outcome of failure, the evidence is very uncertain about the effect of sealing with sealant materials compared to SE. These studies followed up participants to 18 and 24 months.
Sealing compared to no treatment for treating cavitated or dentine carious lesions: for the outcome of failure, there was very low certainty from two studies that suggests there may be little or no difference between the groups. These studies followed up participants for 12 months.
Non‐selective carious tissue removal and CR compared to HT for treating cavitated or dentine carious lesions: for the outcome of failure, there was low‐certainty evidence from two studies that HT may result in a large decrease in risk of failures compared with non‐selective carious tissue removal and CR. These studies followed up participants to 30 to 60 months.
SE compared to HT for treating cavitated or dentine carious lesions: for the outcome of failure, there was very low certainty from two studies that HT may result in a large decrease in risk of failure compared to SE in primary teeth with cavitated but not deep lesions. One study provided very low certainty that HT may result in a small decrease in failure compared to SE in primary teeth with deep lesions. These studies followed up participants to 24 to 36 months.
Non‐selective carious tissue removal and CR compared to NRCC for treating cavitated or dentine carious lesions: for the outcome of failure, there was very low certainty from one study that there was little or no difference between the groups for treating cavitated or dentine carious lesions. This study followed up participants for 30 months.
HT compared to NRCC for treating cavitated or dentine carious lesions: for the outcome of failure, there was very low‐certainty evidence from one study that HT may results in a slight decrease in failure compared to NRCC for treating cavitated or dentine carious lesions. This study followed up participants for 30 months.
Non‐selective carious tissue removal and CR compared to SW for treating cavitated or dentine carious lesions: for the outcome of failure, the very low‐certainty evidence from one study suggests in primary teeth SW may reduce failure compared with CR. Three studies provided moderate‐certainty evidence that in permanent teeth, SW likely results in a reduction of failure compared with CR. These studies followed up participants for 6 to 60 months.
Non‐selective carious tissue removal and CR compared to SE for treating cavitated or dentine carious lesions: for the outcome of failure in permanent teeth with deep lesions, there was very low‐certainty evidence from two studies that SE may result in a large reduction in failure compared with CR. In primary teeth with deep lesions, the very low‐certainty evidence suggests that SE may result in a reduction in failure compared with CR. In primary teeth with cavitated but not deep lesions, the very low‐certainty evidence suggests that SE may result in little to no difference in failure compared to CR. These studies followed up participants for 6 to 36 months.
SE compared to SW for treating cavitated or dentine carious lesions: for the outcome of failure in primary teeth with deep lesions, there was very low‐certainty evidence from two studies that there may be little or no difference between SE and SW. In permanent teeth with deep lesions, the moderate‐certainty evidence from three studies suggests SE probably reduces failure compared to SW. These studies followed up participants for 12 to 60 months.
We will discuss the main results along the three subgroups laid out before.
For non‐cavitated and dentine lesions and sealing, data were overall sparse and not homogeneous. Overall, it seems that sealing is a biologically grounded and applicable concept, leading to lesion arrest; however, resealing is regularly needed. This resealing, notably, requires patients' adherence to follow‐up, something which cannot be necessarily expected in high‐risk individuals (and is central to the limited performance of the NRCC approach, as detected for cavitated, but not deep lesions). Overall, data on this comparison were sparse, and only applied to cavitated or dentine lesions (i.e. those within the inclusion criteria of this review), that is, our findings do not apply to sealing of enamel or non‐cavitated lesions.
For cavitated but not deep lesions in primary teeth, there are clear indications that the HT is a suitable and efficacious treatment option, it was consistently superior to CR and to NRCC. Compared with HT, which as discussed can now be regarded as the gold standard for managing such lesions (at least when focusing on therapy success), SE also tended to come with higher risks of failure. HT seems to be especially suited for managing cavities in primary teeth, as it combines a minimal‐invasive management of carious lesions, reducing pulpal risks of exposure and complications, with a successful approach towards restoring primary teeth (where conventional direct, plastic restorations often fail after shorter periods of time, likely due to complications in moisture control and general difficulties in applicability).
For deep lesions, the evidence was strongest and transitivity (at least to some degree) given, allowing for NMA to be conducted. For permanent teeth, SW was significantly superior over CR, mainly as it avoided pulp exposures. Similarly, in permanent and primary teeth, SE was significantly superior over CR, again as it reduced pulp exposures. One study using a modified HT versus SE found no clear difference between these two comparators, and we excluded this specific study in a sensitivity analysis of our NMA. The network meta‐analytic ranking confirmed that SE and SW were clearly superior over CR; there was less certainty as to which therapy to choose from these two. The modified HT was promising for managing deep lesions, but was employed by only one study. When considering our primary outcome, failure, overall it is clear that CR should not be chosen over SE or SW for managing deep lesions, neither in primary nor permanent teeth. For choosing between SE and SW, a range of further factors may be considered; for example, there is growing evidence from both primary and modelling studies that SE is more cost‐effective than SW, mainly as it reduces initial treatment but also non‐medical and opportunity costs (Elhennawy 2021; Labib 2019; Schwendicke 2013).
Overall completeness and applicability of evidence
For non‐cavitated dentine lesions or cavitated, but not deep lesions, CR and sealing have been compared. The evidence was very limited, while its applicability can be assumed to be high, as the included comparators are already standard in general dental practice: performing a sealant for a non‐cavitated lesion is technically the same as performing such sealant for preventive reasons, for example. Given the described risk of sealant loss, the indication for sealing should be guided by clinical applicability and acceptance as well as patients' expectations and operators' experience. In case sealing is technically the more feasible and acceptable option and also in case follow‐up is likely to achieve, sealing can be recommended over the traditional restorative approach. As laid out, our meta‐analysis found very high uncertainty around any difference between sealing and CR for cavitated or dentine lesions (or both); we need to highlight that our findings do not apply to non‐cavitated or enamel lesions. Moreover, it should be highlighted that unfilled or lowly filled resins have been applied to cavitated lesions, which admittedly comes with high mechanical stress for this type of material. Alternative sealing materials may fare differently. Compared with the HT and SE/SW, the cost‐effectiveness of sealing remains unclear, while it has been shown by modelling studies that sealing instead of restorative interventions on non‐cavitated lesions has a high chance of being cost‐effective, mainly as restorative retreatments can be avoided or postponed (Schwendicke 2015b).
For cavitated, but not deep lesions in primary teeth, there is increasing data supporting HT over alternatives, while the current evidence does not permit firm conclusions as to which of these alternatives (CR, NRCC, SE) to support. Some of these alternatives have not been compared pairwise. The evidence is hence incomplete. Similarly, the applicability of the interventions in general practice varies; SE and CR are already standard in many practices, and also SW is regularly used in some countries (Schwendicke 2016c), while especially NRCC is not widely employed. HT has been tested in both primary and secondary care settings and hence should be applicable; its wider use will be dependent on acceptability and training the current and future dental workforce in employing this specific therapy. HT was also found highly cost‐effective by two studies (Innes 2011; Santamaria 2018). If HT is not available or not indicated (e.g. due to technical reasons, aesthetics etc.) for managing cavitated but not deep lesions, the decision between SE, NRCC or CR should be guided by other factors than success, as we could not identify any of these three strategies to be significantly superior over each other.
For deep lesions, and as indicated above, there are sound data for both primary and permanent teeth supporting SE and SW over CR. The applicability of these approaches will be guided to some extent by lesion depth; it has been argued that for very deep lesions (involving the inner one‐quarter of the dentine), SW should be preferred (Bjørndal 2017; ESE 2019). For deep but not very deep lesions (involving the inner one‐third or inner half of the dentine), the available data support SE over SW for both the primary and the permanent dentition (Elhennawy 2021; Labib 2019; Maltz 2018). In one study (Maltz 2018) directly comparing SW and SE with lesions extending to the inner half of dentine in permanent teeth, the authors noted a possible higher risk of failure in the SW arm related to failure of the patients to return for completion of treatment. A temporary restoration (modified zinc oxide eugenol) was used and 42 out of 147 treatments were not completed because the participant did not return for the second SW step. Of these, 26 did return and an analysis found these to have a higher rate of failure than the teeth where the second step was completed. The authors comment on this but what is not known, is whether the rate of failure was higher in those who returned (to seek further treatment) than those who did not return.
Overall, most studies had short follow‐up periods, associated with few events (failures), limited sample sizes and, as a result, low statistical power. Moreover, when assessing the total body of evidence, there is high heterogeneity in setting, specific operative approaches (e.g. the concrete endpoint of carious tissue removal in SE, SW and CR), the employed restorative strategies, dentition and age groups, which moderate the outcomes and reduce the applicability of the various interventions beyond the specific conditions they were tested in.
Quality of the evidence
The identified studies come mainly with high or unclear risk of bias. Sources of bias were mainly in allocation concealment and lack of blinding. It should be highlighted that for most interventions, blinding of operators and, in many cases, patients is not feasible. For certain comparators (e.g. involving HT or NRCC versus approaches involving plastic restorations), blinding of examiners is similarly not feasible. Overall, and building on the risk of bias, the consistency of estimates, their precision and the magnitude of differences, most comparisons showed low or very low levels of certainty in the evidence according to the grading performed. Notably, the comparisons around HT were graded higher.
Potential biases in the review process
A range of decisions taken when planning, conducting and synthesising this review may have introduced bias and require mentioning.
First, we decided to classify interventions according to the outlined categories; any type of classification comes with a loss of granularity and risks pooling slightly different therapies into one class. This was done to allow some synthesis and interpretability of the data, but impacts on the applicability; moreover, it likely explains to some degree the identified statistical heterogeneity.
Second, for some included studies, we decided to merge intervention arms (e.g. for the modified HT) (Chompu‐inwai 2015), which again means pooling interventions that were not fully, but were almost, identical. Again, this was decided to increase interpretability and reduce the number of comparators.
Third, we excluded many studies because there was no mention of different levels of carious tissue removal being compared, although there were different methods for removal employed (e.g. chemomechanical mechanical removal, ART using hand instruments etc.).
Fourth, our main outcome in this review was pooled failure, which is a notable deviation from our review protocol. We had originally planned to consider major and minor failure as primary outcomes (i.e. allowing for more granular assessment of different interventions and their sequels). The outcome failure comprises pulp exposure, pulp complications and restorative failures (major versus minor). Admittedly, and depending on the subsequent path of action taken to address these failures, they do not have the same relevance for the patient, the operator and even the payer of care (e.g. a filling repair is very different with regards to subjective impact, operative demands and costs than a tooth removal and replacement). This is especially important for sealed lesions; sealant loss was counted as failure in this review, while admittedly it can be addressed easily by resealing. The decision to switch our primary outcome was taken as only very few studies allowed a more granular assessment of outcomes, but may come with some distortions in outcomes.
Fifth, we decided to structure our analysis along lesion depths, with some inconsistencies and also limited deviations from the protocol. Notably, most interventions are applicable for more than one lesion depth. The decision for such subgrouping was made, as dentists will likely choose from a different comparator set when dealing with non‐cavitated, cavitated but not deep and deep lesions, even if there is some overlap in intervention classes. Moreover, these intervention classes are unlikely to constitute the exact same interventions when employed in different subgroups (i.e. SE will be differently conducted in deep lesions (likely leaving soft or leathery dentine in proximity to the pulp) than cavitated but not deep lesions (leaving firm dentine in more central cavity parts)).
Last, we had originally planned to conduct NMAs in all subgroups. This was not feasible given the high heterogeneity observed and the lack of transitivity identified in two of these three subgroups. In line with this, even our network meta‐analytic estimates for deep lesions should not be overinterpreted; especially rankings are misleading when resulting from limited data (as is the case in this review). Readers are encouraged to consult the pairwise estimates in addition to the ranking to gauge the uncertainty in observed effects, as these are not necessarily reflected in ranks.
Agreements and disagreements with other studies or reviews
Especially for deep lesions, our findings support recommendations laid out in consensus statements from a wide range of international groups (Schwendicke 2016a) or societies ranging from cardiology and operative dentistry (Schwendicke 2020) to endodontics (ESE 2019). In particular, there have been efforts to define the radiographic threshold as a marker for when less invasive approaches are no longer suitable and endodontic treatment should be used in permanent teeth. The inner quarter of dentine, where there is a radiodense zone between the carious lesin and dental pulp is recommended as suitable for SW but when the carious lesion is seen radiographically to have penetrated through the complete extent of the dentine (defined as extremely deep), there is a need to carry out endodontic treatment, as the risk of bacteria present and/ or invading the pulp is evident (Demant 2021). Notably, recently and building on the histological assessment of extracted teeth previously managed with SE, the risk of pulpal inflammation when conservatively managing caries lesions has been used to argue towards a more invasive approach (Ricucci 2020). While this arguments rely solely on surrogates (such as histological inflammation), this review shows that less invasive approaches such as SE, SW or HT may improve the patient‐relevant clinical outcomes. These include the less frequent occurrence of events such as pulp exposure or the need for further endodontic intervention, which have a direct, tangible and costly impact on patients and payers.
Authors' conclusions
Implications for practice.
Compared with conventional restoration (CR), the Hall Technique (HT) and selective carious tissue excavation (SE) have a lower risk of failure in the primary dentition, and SE and stepwise carious tissue removal (SW) have a lower risk of failure in the permanent dentition. Most studies showed high risk of bias and limited robustness, resulting in low‐ or very low‐certainty evidence for most comparisons.
Implications for research.
There is a need for more research investigating direct comparisons of interventions included in this review. Given the moves towards treatments that are less invasive being supported by the findings of this review, it would be helpful for future studies to focus on comparisons of those less‐invasive treatment options (SE, SE, HT and non‐restorative cavity control) in comparisons rather than against CR.
For sealing of cavitated lesions, the evidence was sparse compared to sealing of enamel lesions, where more data are available (however, the outcomes measured tended to relate to restoration loss rather than signs and symptoms for patients or long‐term outcomes). It would be relevant to assess if using different plastic sealant materials can overcome the stress involved with sealing of true cavities and hence result in lower risk of retention loss and resealing needs.
There is a lack of standardisation in outcomes and outcome measures which makes comparisons difficult. This could be addressed in future research by a core outcome set for cariology being adopted. These outcomes should reflect the view of multiple stakeholders (e.g. patients and payers) besides clinicians.
Only few studies here were set in primary care (e.g. in general dental practice), where the vast majority of carious lesion management and restorative care is carried out in most countries. Future research should consider testing interventions for managing carious lesions in the setting in which they will be used and with clinicians representative of those who will carry out the interventions in practise. In addition, translational investigations should be integrated into any intervention studies in order to increase the implementation of new evidence into practice.
Although 10 studies investigated permanent teeth, almost all were on children under 18 years old. It is likely that this is because these are logistically an easier population to recruit and retain in investigations. Future studies should consider including adults or even older adults.
Longer follow‐up times should be considered for future studies as only four studies included in the review had follow‐up data for three years or more, yet restoration longevity and pulpal outcomes are expected to exceed this.
History
Protocol first published: Issue 6, 2018
Notes
This review was based on a new protocol and search strategy that revised and updated a review first published in 2006 entitled "Complete or ultraconservative removal of decayed tissue in unfilled teeth". That review was updated in 2013 and the title changed to "Operative caries management in adults and children" to encompass all studies that remove varying amounts of caries, including those that do not remove any dentinal caries, and was withdrawn from the Cochrane Library after the new protocol for the current review was published. The new review was conducted by a new author team that retained some members of the original author team; it continued with the same intervention remit but only included studies where there was cavitation due to caries or the carious lesion extended into dentine (i.e. carious lesions confined to enamel were not included). Five studies from the previous review are included in the new review.
Acknowledgements
We thank the Cochrane Oral Health editorial team for their help in preparing this review, in particular, Professor Helen Worthington, Laura MacDonald (Managing Editor) and Anne Littlewood (Information Specialist). We also thank Cochrane Oral Health editors Dr Phil Riley, Professor Jo Dumville and Professor Ana Jeroncic; peer reviewers Professors James Bader and Chris Deery; and copy editor Anne Lawson. We thank Professor Kim Ekstrand for her comments on the protocol.
Appendices
Appendix 1. Cochrane Oral Health's Trials Register search strategy
Cochrane Oral Health's Trials Register is available via the Cochrane Register of Studies. For information on how the register is compiled, see oralhealth.cochrane.org/trials.
1 MESH DESCRIPTOR Dental Caries AND INREGISTER
2 (caries or carious) AND INREGISTER
3 ((tooth or teeth or dentin* or dental) near5 (decay* or lesion* or cavit*)) AND INREGISTER
4 #1 or #2 or #3
5 MESH DESCRIPTOR Dental Cavity Preparation AND INREGISTER
6 "carious tissue removal" AND INREGISTER
7 ((caries or carious or cavit*) near5 (stepwise or excavation or excavator*)) AND INREGISTER
8 (((caries or carious or cavit*) near5 (selective or partial or incomplete)) AND remov*) AND INREGISTER
9 (((caries or carious or cavit*) near5 (minimal or minimum)) AND invas*) AND INREGISTER
10 (dentin* near3 remov*) AND INREGISTER
11 MESH DESCRIPTOR Pit and Fissure Sealants EXPLODE ALL AND INREGISTER
12 seal* AND INREGISTER
13 MESH DESCRIPTOR Crowns EXPLODE ALL AND INREGISTER
14 crown* or "Hall technique" AND INREGISTER
15 "non‐restorative cavity control" AND INREGISTER
16 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15
17 #4 and #16
Appendix 2. Cochrane Central Register of Controlled Clinical Trials (CENTRAL) search strategy
1 MESH DESCRIPTOR Dental Caries AND CENTRAL:TARGET
2 (caries or carious) AND CENTRAL:TARGET
3 ((tooth or teeth or dentin* or dental) near5 (decay* or lesion* or cavit*)) AND CENTRAL:TARGET
4 #1 or #2 or #3
5 MESH DESCRIPTOR Dental Cavity Preparation AND CENTRAL:TARGET
6 "carious tissue removal" AND CENTRAL:TARGET
7 ((caries or carious or cavit*) near5 (stepwise or excavation or excavator*)) AND CENTRAL:TARGET
8 (((caries or carious or cavit*) near5 (selective or partial or incomplete)) AND remov*) AND CENTRAL:TARGET
9 (((caries or carious or cavit*) near5 (minimal or minimum)) AND invas*) AND CENTRAL:TARGET
10 (dentin* near3 remov*) AND CENTRAL:TARGET
11 MESH DESCRIPTOR Pit and Fissure Sealants EXPLODE ALL AND CENTRAL:TARGET
12 seal* AND CENTRAL:TARGET
13 MESH DESCRIPTOR Crowns EXPLODE ALL ANDCENTRAL:TARGET
14 crown* or "Hall technique" ANDCENTRAL:TARGET
15 "non‐restorative cavity control" ANDCENTRAL:TARGET
16 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15
17 #4 and #16
Appendix 3. MEDLINE Ovid search strategy
1. Dental caries/ 2. (caries or carious).tw. 3. ((tooth or teeth or dentin$ or dental) adj5 (decay$ or lesion$ or cavit$)).tw. 4. or/1‐3 5. Dental cavity preparation/ 6. "carious tissue removal".tw. 7. ((caries or carious or cavit$) adj5 (stepwise or excavation or excavator$)).tw. 8. ((caries or carious or cavit$) adj5 ((selective or partial or incomplete) adj2 remov$)).tw. 9. ((caries or carious or cavit$) adj5 ((minimal or minimum) adj2 invas$)).tw. 10. (dentin$ adj3 remov$).tw. 11. "Pit and fissure sealants"/ 12. seal$.tw. 13. Crowns/ 14. (crown$ or "Hall Technique").tw. 15. "non‐restorative cavity control".tw. 16. or/5‐15 17. 4 and 16
The above subject search was linked with the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials in MEDLINE (as described in Lefebvre 2020, box 3b).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. Embase Ovid search strategy
1. Dental caries/ 2. (caries or carious).tw. 3. ((tooth or teeth or dentin$ or dental) adj5 (decay$ or lesion$ or cavit$)).tw. 4. or/1‐3 5. "carious tissue removal".tw. 6. ((caries or carious or cavit$) adj5 (stepwise or excavation or excavator$)).tw. 7. ((caries or carious or cavit$) adj5 ((selective or partial or incomplete) adj2 remov$)).tw. 8. ((caries or carious or cavit$) adj5 ((minimal or minimum) adj2 invas$)).tw. 9. (dentin$ adj3 remov$).tw. 10. Fissure sealant/ 11. seal$.tw. 12. Crowns/ 13. (crown$ or "Hall Technique").tw. 14. "non‐restorative cavity control".tw. 15. Tooth crown/ 16. or/5‐15 17. 4 and 16
The above subject search was linked with the highly sensitive search strategy designed by Cochrane for identifying randomised controlled trials and controlled clinical trials in Embase (as described in Lefebvre 2020, box 3e).
Randomized controlled trial/
Controlled clinical study/
random$.ti,ab.
randomization/
intermethod comparison/
placebo.ti,ab.
(compare or compared or comparison).ti.
((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab.
(open adj label).ti,ab.
((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab.
double blind procedure/
parallel group$1.ti,ab.
(crossover or cross over).ti,ab.
((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab.
(assigned or allocated).ti,ab.
(controlled adj7 (study or design or trial)).ti,ab.
(volunteer or volunteers).ti,ab.
human experiment/
trial.ti.
or/1‐19
random$ adj sampl$ adj7 ("cross section$" or questionnaire$1 or survey$ or database$1)).ti,ab. not (comparative study/ or controlled study/ or randomi?ed controlled.ti,ab. or randomly assigned.ti,ab.)
Cross‐sectional study/ not (randomized controlled trial/ or controlled clinical study/ or controlled study/ or randomi?ed controlled.ti,ab. or control group$1.ti,ab.)
(((case adj control$) and random$) not randomi?ed controlled).ti,ab.
(Systematic review not (trial or study)).ti.
(nonrandom$ not random$).ti,ab.
"Random field$".ti,ab.
(random cluster adj3 sampl$).ti,ab.
(review.ab. and review.pt.) not trial.ti.
"we searched".ab. and (review.ti. or review.pt.)
"update review".ab.
(databases adj4 searched).ab.
(rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/
Animal experiment/ not (human experiment/ or human/)
or/21‐33
20 not 34
Appendix 5. US National Institutes of Health Ongoing Trials Register (ClinicalTrials.gov) search strategy
Expert search:
( caries OR carious OR cavity OR cavities OR "tooth decay" ) AND ( dentine OR cavitated ) AND ( stepwise OR excavation OR excavator OR selective OR partial OR minimal OR minimum OR sealant OR seal OR crown OR "Hall Technique" OR "non‐restorative cavity control" )
Appendix 6. World Health Organization International Clinical Trials Registry Platform search strategy
dentine AND stepwise OR dentine AND excavation OR dentine AND excavator OR dentine AND selective OR dentine AND partial OR dentine AND minimal OR dentine AND minimum OR dentine AND sealant OR dentine AND seal OR dentine AND crown OR dentine AND Hall Technique OR dentine AND non‐restorative cavity control
Appendix 7. Network meta‐analysis treatment ranking
Values are the probability for each treatment to be the best
Ranking table for base‐case (all studies)
| Rank 1 | Rank 2 | Rank 3 | Rank 4 | |
| CR | 0.000,05 | 0.001,62 | 0.035,51 | 0.962,81 |
| HT | 0.724,29 | 0.166,98 | 0.086,40 | 0.022,34 |
| SE | 0.259,38 | 0.711,98 | 0.028,44 | 0.000,21 |
| SW | 0.016,29 | 0.119,43 | 0.849,65 | 0.014,64 |
Ranking table with modified HT study excluded
| Rank 1 | Rank 2 | Rank 3 | |
| CR | 0.000,14 | 0.016,34 | 0.983,52 |
| SE | 0.958,83 | 0.041,01 | 0.000,16 |
| SW | 0.041,04 | 0.942,65 | 0.016,31 |
CR: complete removal; HT: Hall Technique; SE: selective removal; SW: stepwise removal.
Appendix 8. Network meta‐analysis choice of model sensitivity analysis
To investigate the impact of choice of random‐effects versus fixed‐effect model we undertook a sensitivity analysis with analysis according to a fixed‐effect model.
The results are as follows.
Treatment effects for all studies: comparison of all treatment pairs
| CR | HT | SE | SW | |
| CR | CR | 0.13 (0.03 to 0.49) | 0.25 (0.17 to 0.38) | 0.51 (0.36 to 0.73) |
| HT | 7.7 (2.02 to 29.25) | HT | 1.96 (0.55 to 6.91) | 3.96 (1.04 to 14.94) |
| SE | 3.93 (2.61 to 6.03) | 0.51 (0.14 to 1.83) | SE | 2.01 (1.35 to 3.05) |
| SW | 1.95 (1.36 to 2.8) | 0.25 (0.07 to 0.96) | 0.5 (0.33 to 0.74) | SW |
Treatment effects with studies excluded: comparison of all treatment pairs
| CR | SE | SW | |
| CR | CR | 0.26 (0.17 to 0.39) | 0.51 (0.36 to 0.73) |
| SE | 3.92 (2.59 to 5.99) | SE | 2.02 (1.35 to 3.04) |
| SW | 1.94 (1.36 to 2.78) | 0.5 (0.33 to 0.74) | SW |
CR: complete removal; HT: Hall Technique; SE: selective removal; SW: stepwise removal.
We observed that while the effect estimates were generally smaller than with the random‐effects model, the resultant rankings were stable and consistent with those of the random‐effects model.
Data and analyses
Comparison 1. Sealing versus conventional restoration (CR) (cavitated, permanent dentition).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Failure: sealing vs CR | 1 | 41 | Odds Ratio (M‐H, Random, 95% CI) | 5.00 [0.51, 49.27] |
Comparison 2. Sealing versus selective excavation (SE) (cavitated, primary dentition).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Failure: sealing vs SE | 2 | 82 | Odds Ratio (M‐H, Random, 95% CI) | 3.11 [0.11, 85.52] |
Comparison 3. Sealing versus no treatment (non‐cavitated, permanent).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Failure: sealing vs no treatment | 2 | 103 | Odds Ratio (M‐H, Random, 95% CI) | 0.05 [0.00, 2.71] |
Comparison 4. Conventional restoration (CR) versus Hall Technique (HT) (cavitated, primary).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Failure: CR vs HT | 2 | Odds Ratio (IV, Random, 95% CI) | 8.35 [3.73, 18.68] |
Comparison 5. Selective excavation (SE) versus Hall Technique (HT) (primary, cavitated; primary, deep).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Failure: SE vs HT | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1.1 Primary, cavitated but not deep | 2 | 586 | Odds Ratio (M‐H, Random, 95% CI) | 8.94 [0.57, 139.67] |
| 5.1.2 Primary, deep | 1 | 72 | Odds Ratio (M‐H, Random, 95% CI) | 1.95 [0.57, 6.63] |
Comparison 6. Conventional restoration (CR) versus non‐restorative cavity control (NRCC) (cavitated, primary).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Failure: CR vs NRCC | 1 | 102 | Odds Ratio (M‐H, Random, 95% CI) | 1.16 [0.50, 2.71] |
Comparison 7. Hall Technique (HT) versus non‐restorative cavity control (NRCC) (cavitated, primary).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Failure: HT vs NRCC | 1 | 84 | Odds Ratio (M‐H, Random, 95% CI) | 0.19 [0.05, 0.74] |
Comparison 8. Conventional restoration (CR) versus stepwise (SW) (deep, primary; deep, permanent).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Failure: CR vs SW | 3 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1.1 Primary, deep | 1 | 63 | Odds Ratio (M‐H, Random, 95% CI) | 2.43 [0.65, 9.12] |
| 8.1.2 Permanent, deep | 3 | 398 | Odds Ratio (M‐H, Random, 95% CI) | 2.06 [1.34, 3.17] |
Comparison 9. Conventional restoration (CR) versus selective excavation (SE) (deep, permanent; deep, primary; cavitated, primary).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 9.1 Failure: CR vs SE | 7 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 9.1.1 Permanent, deep | 2 | 179 | Odds Ratio (M‐H, Random, 95% CI) | 11.32 [1.97, 65.02] |
| 9.1.2 Primary, deep | 4 | 265 | Odds Ratio (M‐H, Random, 95% CI) | 4.43 [1.04, 18.77] |
| 9.1.3 Primary, cavitated but not deep | 2 | 204 | Odds Ratio (M‐H, Random, 95% CI) | 0.62 [0.21, 1.88] |
Comparison 10. Stepwise (SW) versus selective excavation (SE) (deep, primary; deep, permanent).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 10.1 Failure: SW vs SE | 4 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 10.1.1 Primary, deep | 2 | 126 | Odds Ratio (M‐H, Random, 95% CI) | 2.05 [0.49, 8.62] |
| 10.1.2 Permanent, deep | 3 | 371 | Odds Ratio (M‐H, Random, 95% CI) | 2.25 [1.33, 3.82] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alves 2017.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 12, 36 and 48 months Setting: 1 university clinic in Rio Grande do Sul, Brazil |
|
| Participants | 49 participants, 54 occlusal carious lesions in permanent molars and premolars teeth Age: 8–43 years, median age 19 years Inclusion criteria: clinical: presence of a cavitated carious lesion with no access allowing biofilm control; radiographical: carious lesions extending up to a middle third of the dentine thickness, as assessed by bitewing radiography Exclusion criteria: teeth presenting with any sign/symptom of pulp involvement |
|
| Interventions | 2 treatment arms Treatments were performed by 20 dental students from the Federal University of Rio Grande do Sul (34 teeth) and by 1 experience dentist (20 teeth), who supervised all the procedures at chair side. This researcher accompanied each clinical step, to ensure the standardisation of the clinical procedures, including clinical and radiographic diagnosis, rubber dam installation, caries removal and application of the restoration/sealing technique. Prior to tooth random assignment, all teeth were cleaned, local anaesthesia applied and under rubber dam isolated. Standardisation also included the follow‐up assessment at 1 year and then after 3–4 years. Group 1 (28 teeth): sealant placed directly over the carious lesion: acid etching with 37% phosphoric acid gel for 30 seconds; cavity washing and drying; application of the sealant material (Fluroshield, Caulk/Dentsply, Rio de Janeiro, Brazil) on the occlusal lesion, with an explorer; light‐curing for 20 seconds; removal of the rubber dam; and occlusal adjustments when necessary. Group 2 (26 teeth): CR treatment: removal of all carious dentine using a slowly rotating, sterile, round steel bur, according to the clinical hardness criteria; acid etching with 37% phosphoric acid gel for 30 seconds in enamel and for 15 seconds in dentine; cavity washing and drying; application of the bonding agent (Excite Adhesive, Ivoclar Vivadent, São Paulo, Brazil) on the enamel and dentine cavity walls; light‐curing for 20 seconds; restoration with a resin composite (Tetric Ceram Ivoclar‐VivaDent, São Paulo, Brazil); removal of the rubber dam and occlusal adjustments when necessary. |
|
| Outcomes |
Primary outcome Combination of clinical and radiographic parameters (bitewing radiographs): retention or integrity of sealant (complete retention, partial retention or lost retention) or restoration (optimal, acceptable or unacceptable), lack of caries progression and absence of pain/sensitivity. Need for repair/replacement of restoration Secondary outcome Secondary caries in the sealant/restoration margins |
|
| Notes | Funding: University, National Coordination of Post‐Graduate Education (CAPES), Ivoclar/Vivadent (Sao Paulo, Brazil), and Caulk/Dentsply (Rio de Janeiro, Brazil). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequence automatically generated at random. |
| Allocation concealment (selection bias) | Low risk | Concealed randomisation, sequentially numbered using sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of dentist not possible. Dentist were aware of different procedures. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Follow‐up assessment performed by the same operator who performed and knew the distribution of treatments in the 2 arms. Quotes: "Treatments were performed by 20 dental students … and by one researcher (FCMSG), who supervised all the procedures;" "The teeth were assessed clinically and radiographically after 1 year (FCMSG and BM)." "...sealants were classified as complete retention, partial retention or lost retention, whereas restorations were classified as optimal, acceptable or unacceptable." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised teeth included in analysis. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Araujo 2020.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 36 months. Clinical outcomes related to restoration survival evaluated at 1, 6, 12, 18, 24, 30 and 36 months Setting: intervention and assessments carried out in Schools in rural Brazil Children treated during school hours in empty classrooms, lying on a school table with a mattress. Operators were positioned at end of table sitting on a chair high enough to access the child's mouth and used a light attached in their forehead to enable visualisation of the child's mouth. |
|
| Participants | Unit of randomisation: participant 131 children (ART = 65; HT = 66), 1 tooth per child Age: 5–10 years (mean age 8.1 SD 1.2 years) Inclusion criteria: aged 5–10 years; ≥ 1 cavitated occluso‐proximal carious lesion in a primary molar with no signs or symptoms of pulp involvement; generally co‐operative behaviours that could be managed by the operators in the school setting; no known medical conditions |
|
| Interventions | 2 treatment arms Treated by 3 trained operators who treated 44, 44 and 43 participants each, in both arms. Both treatments were carried out according to standard protocols. Group 1 (65 children): SE (ART) cavities prepared using hand instruments and restored using the encapsulated high‐viscosity GIC EQUIA Forte (GC Corp, Leuven, BE). Group 2 (66 children): HT: no carious tissue removal, or tooth preparation/reduction to facilitate the crown fitting or crown trimming. An orthodontic separator was placed between the teeth when there was a tight proximal contact point between the tooth to be fitted with crown and the adjacent tooth. PMCs (3M ESPE, St Paul, NM, USA) were cemented using encapsulated GIC Fuji I (GC Corp., Leuven, BE). |
|
| Outcomes | Outcomes criteria were according to Innes 2007. Primary outcome
Secondary outcomes
|
|
| Notes | A post‐hoc analysis was carried out to investigate exfoliation of teeth treated. Teeth treated with HT exfoliated earlier than those with ART (P = 0.007). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The children were assigned using random allocation." |
| Allocation concealment (selection bias) | Low risk | Quote: "with the aid of a randomisation list." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Both children and dentists had to know which treatment was being applied as 1 was a silver‐coloured crown and the other was a white‐filling material. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcome assessors could not be blinded as 1 treatment was a silver‐coloured crown and the other was a white‐filling material. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Matched study protocol and deviation was explained and was due to poor response rate ("less than 50%") for a questionnaire so the results were not considered to be likely to represent the whole group. |
| Selective reporting (reporting bias) | Low risk | All outcomes were reported. |
| Other bias | Low risk | No other biases detected. |
Bjørndal 2017.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 60 months. February 2005 to April 2007 Setting: 2 Danish centres (the Dental Schools at the University of Copenhagen and Aarhus University) and 4 Swedish centres (Karolinska Institute, Stockholm; Faculty of Odontology, Malmö; Uppsala Public Dental Service and Gothenburg Public Dental Service) |
|
| Participants | 314 teeth Age (range): 25.3–38.0 years, median age 29 years; group 1: 29.0 (25.3–38.0) years; group 1: 29.0 (26.0–37.8) years Gender: 56% women Inclusion criteria: aged ≥ 18 years; primary caries lesion radiographically involving ≥ 75% of the dentin; and the presence of a well‐defined radiodense zone between the caries lesion and the pulp; in patients who reported pain, the pain was provoked and confirmed by stimulation with cold or compressed air (pretreatment pain) Exclusion criteria: prolonged unbearable pain or pain disturbing night sleep (or both); no response to cold and electrical pulp testing; attachment loss > 5 mm; apical radiolucency; pregnancy; any systemic disease preventing enrolment; lack of informed consent |
|
| Interventions | 2 treatment arms Group 1 (143 participants, 156 teeth): SW excavation; the first excavation included removal of the superficial necrotic and demineralised dentin with complete excavation of the peripheral demineralised dentin, avoiding excavation close to the pulp; when a temporary restoration could be properly placed, no further excavation was carried out, leaving soft, wet and discoloured dentin centrally on the pulpal wall. After 8–12 weeks, the cavity was re‐entered and the final excavation was carried out leaving only central yellowish or greyish hard dentin (equal to the hardness of sound dentin, as judged by gentle probing). Group 2 (149 participants, 158 teeth): direct complete excavation completed during the first visit. Criteria for evaluating the remaining dentin were identical to those used at the second visit in the SW group. |
|
| Outcomes |
Primary outcome Success/failure: failure including pulp exposure; pulp vitality with apical radiolucency; no pulp vitality with apical radiolucency; unbearable pain; after 12 months number of teeth failed |
|
| Notes | Sample size calculation showed that 134 participants were needed in each group to detect a 20% difference in the success rate between SW and CR at a 2‐sided alpha level of 5% (type I error) and 90% power (type II error of 10 %), when expecting 50% in the direct complete excavation group to retain pulp vitality without apical radiolucency after 1 year. Funding: KerrHawe, 3M ESPE, LM‐instruments, Dentsply, DeTrey Dentsply, and Gedr. Brasseler are acknowledged for providing the products. This trial was supported by the Danish Agency for Science Technology and Innovation, and the Danish Regions. Declarations/conflicts of interest: none stated. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were centrally randomised to either direct pulp capping vs partial pulpotomy using a similar randomisation procedure as the one described for the excavation trial but only stratifying for pain (yes or no). |
| Allocation concealment (selection bias) | Low risk | The allocation sequences for SW vs CR (1:1) were computer generated, stratified for pain (yes or no), age (18–49 years or ≥ 50 years), and centre in blocks of 6. The block size was unknown to the investigators. Concealed allocation was achieved through central telephone randomisation (Copenhagen Trial Unit). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Patients were unaware of the treatment assignment, and all were seen in at least two treatment visits." Operators could not be blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The outcome assessor could not be blinded for the primary outcome of pulp exposure as this was assessed during treatment, by the operator. For measurements of failure though assessors may have been blinded – similar restorative materials. Quote: "Two blinded observers independently examined the radiographs. Success/failure outcomes: clinical assessment – no comment about blinded outcome assessment. Radiographic assessment – blinded. Pulp exposure assessment – not blinded as operator (who was not blinded to intervention) made judgement. Inter‐examiner agreement in the determination of success or failure was judged as good (Kappa = 0.67)." Patient remained blind as both groups had 2 appointments with removal of restoration. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dropouts were 7%. No clear explanation of cause, but low risk of bias due to the small numbers involved. |
| Selective reporting (reporting bias) | Low risk | Study protocol was available and outcomes reported in prespecified way. |
| Other bias | Low risk | No other biases detected. |
Borges 2012a.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 12 months Setting: 1 university in Brazil |
|
| Participants | 30 children Age: 5–9 years Inclusion criteria: presence of 2 primary molars with non‐cavitated dentine lesions radiographically located between the enamel dentine junction and the middle 1/3rd of dentine Exclusion criteria: presence of restorations and white spot lesions or cavitations on other tooth surfaces; teeth with reported sensitivity to any type of stimulus |
|
| Interventions | 2 treatment arms Group 1 (30 teeth): sealant: oral hygiene instructions for daily tooth brushing and the use of dental floss; prophylaxis with pumice and water; rubber dam placement; prophylaxis with a Robinson brush containing pumice and water; acid etching with 37% phosphoric acid for 30 seconds, washing with an air‐water spray, and drying; applying a fluoride‐releasing, resin‐based sealant Fluorshield (Caulk/Dentsply, Milford, DE, USA) with a dental probe (SS White Duflex); light curing for 20 seconds with a light‐curing device (Coltolux LED (Coltene Whaledent, Altstätten, Switzerland)); occlusion check. Group 2 (30 teeth): CR: oral hygiene instructions for daily tooth brushing and the use of dental floss; anaesthesia; rubber dam isolation; cavity preparation with a diamond bur number 1012 (KG Sorensen, Barueri, São Paulo, Brazil) mounted in a high‐speed handpiece (Dabi Atlante, Ribeirao Preto, SP, Brazil); excavation of carious tissue using a dentin excavator; finishing of the cavity with a number 329 carbide bur (KG Sorensen); acid etching of enamel and dentine for 15 seconds and drying with sterile cotton; application of 2 coats of a single‐component etch‐and‐rinse adhesive system (Stae, SDI, Victoria, Australia), application of light curing to solvent for 10 seconds (Coltolux LED (Coltene Whaledent, Altstätten, Switzerland)); restoration with increments of composite resin (Ice A2 shade, SDI, Victoria, Australia) and light cuing. |
|
| Outcomes |
Primary outcomes Clinical efficacy (cavitation, marginal integrity of sealant or restoration) after 12 month; number of teeth failed Secondary outcomes Radiographic efficacy (dimension change of radiolucent area between baseline and interval (group 1); presence of secondary caries (group 2)) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a random sampling method which assigned a number to each eligible tooth that was put into a sealed opaque envelope. The numbers were randomly selected by an examiner to allocate the teeth to each group (experimental or control). |
| Allocation concealment (selection bias) | Low risk | Used a random sampling method which assigned a number to each eligible tooth that was put into a sealed opaque envelope. The numbers were randomly selected by an examiner to allocate the teeth to each group (experimental or control). |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants/operators. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Only radiographic assessment blinded (a single calibrated and blinded examiner performed this evaluation). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition balanced between groups. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available – insufficient information to permit judgement of low or high risk of bias. |
| Other bias | Low risk | No other biases detected. |
Borges 2012b.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 12 months Setting: 1 university in Brazil |
|
| Participants | 35 participants Age: 12–19 years Caries experience: not reported (participants at high risk of caries) Inclusion criteria: presence of visually non‐cavitated lesions between the enamel dentine junction and the middle 1/3rd of dentine Exclusion criteria: presence of restorations and white spot lesions or cavitations on other tooth surfaces; teeth with reported sensitivity to any type of stimulus |
|
| Interventions | 2 treatment arms Group 1 (30 teeth): oral hygiene instructions for daily tooth brushing and the use of dental floss; prophylaxis with pumice and water; rubber dam placement; prophylaxis with a Robinson brush containing pumice and water; acid etching with 37% phosphoric acid for 30 seconds, washing with an air‐water spray, and drying; applying a fluoride‐releasing, resin‐based sealant Fluorshield (Caulk/Dentsply, Milford, DE, USA) with a dental probe (SS White Duflex); light curing for 20 seconds with a light‐curing device (Optilight LD MAX; Gnatus Equipamentos Medico‐Odontologicos Ltda); occlusion check. Group 2 (30 teeth): oral hygiene instructions for daily tooth brushing and the use of dental floss; prophylaxis with pumice and water (no treatment). |
|
| Outcomes |
Primary outcome Radiographic and clinical (cavitation, tooth sensitivity) caries progression at 12 months |
|
| Notes | Borges 2012a reported 24‐ and 36‐month results – but only for the experimental group. All lesions from the control group were excluded (mainly as they had been restored as caries progression occurred). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Each eligible tooth was assigned a number; these numbers were noted on individual pieces of paper, which were subsequently put into a sealed opaque envelope. An external examiner withdrew 1 paper at a time and allocated 30 teeth to each group. |
| Allocation concealment (selection bias) | Low risk | Each eligible tooth was assigned a number; these numbers were noted on individual pieces of paper, which were subsequently put into a sealed opaque envelope. An external examiner withdrew 1 paper at a time and allocated 30 teeth to each group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants or operators. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | No blinding of assessor. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition balanced between groups. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available – insufficient information to permit judgement of low or high risk of bias. |
| Other bias | Low risk | No other biases detected. |
Boyd 2021.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 1 and 2 years Setting: primary care in Whanganui, New Zealand |
|
| Participants | Unit of randomisation: teeth 295 children, 570 carious primary teeth analysed for both arms Age: 3–8 years Inclusion criteria: children aged 3–8 years attending for their next dental examination from 37 schools and preschools; no medical history; radiograph: ≥ 1 radiographically detectable proximal carious lesion in the primary molars, with healthy pulp and with a score of P3 or P4 in the following radiographic scoring system: P0, no radiolucency; P1, radiolucency in outer half of enamel; P2, radiolucency in inner half of enamel; P3, radiolucency < 0.5 mm into dentine; P4, radiolucency > 0.5 mm into dentine but confined to dentine's outer half; teeth had to have more than half the root structure remaining. If a child had > 1 tooth affected by a proximal lesion, > 1 tooth was included Exclusion criteria: unable to have radiographs taken; no carious lesions present or into dentine at the P3 or P4 level; medically compromised; no parental consent or did not assent to participation in the study |
|
| Interventions | 2 treatment arms Group 1 (149 children, 273 teeth): HT: procedure conducted in line with Innes 2011. Separating elastics were provided for dental therapists to use prior to the HT when needed. An SSC was placed without any carious tissue removal or tooth preparation. Group 2 (146 children, 297 teeth): SE: included tooth preparation with SE, which included SSC, amalgam, composite or glass ionomer cement restorations. |
|
| Outcomes | Success or failure based on clinical and radiographic measures combined at 1‐ and 2‐year follow‐up to give composite outcomes of success, minor failure or major failure as defined by Innes 2007.
|
|
| Notes | There was clustering of multiple teeth per participant. Participant follow‐up rate at 12 months was 95% and at 24 months was 91%. Study funded by a grant from Cure Kids New Zealand, and stainless‐steel crowns and cement were provided by 3M. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No information and no prepublished protocol to check. No data in the trial registration. Quote: "with children randomized to intervention with either the HT or NHT upon recruitment to the study." |
| Allocation concealment (selection bias) | Unclear risk | No information and no prepublished protocol to check. No data in the trial registration. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Unable to blind participants or personnel because of types of intervention – visibly different. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Unable to blind outcome assessor because of types of intervention – visibly different. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All teeth in trial accounted for. |
| Selective reporting (reporting bias) | Unclear risk | No published protocol. |
| Other bias | Low risk | No other biases detected. |
Chompu‐inwai 2015.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 24 months, recruitment period not reported Setting: Faculty of Dentistry, Chiang Mai University, Chiang Mai, Thailand |
|
| Participants | 42 participants, 109 lesions on occlusal or proximal (or both) surfaces of primary molars Age: group 1: 41–113 months; mean 70.0, SD 14.6 months; group 2: 46–137 months; mean 71.2, SD 20.7 months; group 3: 37–119 months; mean 65.8, SD 18.4 months Gender: 50% female – group breakdown not provided Inclusion criteria: deep dentine caries involving occlusal or proximal (or both) surfaces of primary molars and a risk of pulp exposure if completely excavated; absence of clinical symptoms or presence only of pain provoked with stimulation, such as complaints of impaction of food when eating, and no signs of irreversible pulpitis, such as spontaneous pain; absence of clinical swelling or pus exudates/fistula of soft or periodontal tissues; absence of abnormal tooth mobility; absence of pain on percussion; and restorable tooth. Radiographic inclusion criteria: extension of dental caries ≥ 3/4 of the entire dentin thickness, with a thin radiopaque dentin layer between the radiolucent caries lesion and the dental pulp; no superimposition of dental caries on the dental pulp; absence of widened PDL space; absence of radiolucency in the furcation area; absence of radiolucency in the periapical regions; absence of pathological internal or external (or both) root resorption; and absence of calcification or pulp canal obliteration (or both) |
|
| Interventions | 3 treatment arms (we combined groups 2 and 3) Group 1 (43 teeth): CR (non‐selective) (IPT group); first step was standardised SSC preparation, as detailed by McDonald 2011. Next, the soft demineralised dentin around the lateral walls of the carious lesion was removed at depth of 1 mm made by a low‐speed round tungsten carbide bur 1 mm in diameter (Jota AG, Ruethi, Switzerland) to create a sound dentin surface that could provide maximum bonding with the subsequent use of base or luting cement. Then, each tooth was treated according to the previous random allocation. In the IPT group, the additional soft demineralised dentin was repeatedly removed until the remaining soft carious dentin was close to the pulp and any further removal of caries, as judged by the operator, would have resulted in pulp exposure. Group 2 (33 teeth): SE; (MCRB/L group), no additional caries removal was performed following crown preparation. The remaining caries and the rest of the cavity were covered with RMGI base material (Vitrebond), which was mixed and light cured according to the manufacturer's instructions. Group 3 (33 teeth): MCRL group; the tooth was treated exactly as in the MCRB/L group, except for no base was placed. Next, an SSC (3M ESPE, St Paul, NM, USA) was immediately tried on each prepared tooth and marginal adaptation was achieved, as described byMcDonald 2011. |
|
| Outcomes |
Primary outcome Clinical and radiographic failures after 7, 14 and 24 months At follow‐up appointments, the SSC must have been in good condition with no defects, such as perforation or marginal defects; otherwise, the treated tooth was excluded. The criteria used to determine clinical success were absence of: postoperative pain, swelling, abscess formation, pathological mobility and pain on percussion. A parallel periapical follow‐up radiograph was made after the clinical examination. The criteria used to determine the radiographic success were absence of: widened PDL; periapical or furcation radiolucency (or both); and pathological internal or external root resorption (or both) that was not compatible with expected resorption due to the exfoliation process. Pulp canal obliteration was not considered a failure in this study. |
|
| Notes | There is some ambiguity over how much caries was removed in groups. Funding: The Research Fund for Postgraduate and Undergraduate Students of the Faculty of Dentistry and The Research Fund of the Graduate School, Chiang Mai University, Chiang Mai, Thailand. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | An online statistical computing program was used to generate the block randomisation, with a block size of 3. All 32 blocks of 3 were put into the box. Comment: 109 teeth were stated as being randomised but the groups were uneven (43/33/33) suggestive of non‐random allocation. |
| Allocation concealment (selection bias) | Low risk | Prior to the beginning of the treatment, an assistant cast a concealed lot out of a box. Then, the allocation of treatment was immediately disclosed to the operator but not to the participants (both child and parent). If the treated tooth was later excluded for any reasons, the excluded lot was put back into the box to equal the number of each treatment group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | 1 standardised postgraduate student in paediatric dentistry performed all the treatments under the supervision of 1 instructor. Quote: "The allocation of treatment was immediately disclosed to the operator but not to the participants (both child and parent)." Operator could not be blinded. Difference between caries removal in each arm minimal so operator could be influenced by preference for 1 arm or another. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | For the follow‐up evaluations, only 1 member of the research team had access to treatment records and radiographs. 2 evaluators, both blinded to the treatment groups and not involved in treating the teeth or supervising the treatment, independently evaluated the treated teeth clinically. 2 evaluators were calibrated with the instructor using the first set of radiographs. Then they independently evaluated the second set of radiographs twice, 2 weeks apart. This resulted in Cohen's kappa values of 0.76 and 0.86 for intraexaminer reliabilities and 0.88 for interexaminer reliability. Quote: "two evaluators, completely blinded to the treatment groups and not involved in treating the teeth or supervising the treatment, independently evaluated the teeth clinically." and "Two evaluators were calibrated, then they independently evaluated the second set of radiographs twice, two weeks apart." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Teeth were excluded from this study if accidental pulp exposure occurred or if the soft caries was unintentionally completely removed, based on the operator's judgement, using the visual and tactile senses. Also, authors excluded a number of teeth from analysis that seemed to be due to failure but did not count as failure because it was not recorded. |
| Selective reporting (reporting bias) | High risk | Not reported why some teeth were excluded. |
| Other bias | Low risk | No other biases detected. |
da Silveira 2012.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 4‐monthly intervals over 1 year Duration of study: 12 months Setting: 1 University in Brazil |
|
| Participants | 38 participants, 51 permanent molars Age (mean): group 1: 13.04 year; group 2: 12.53 years Caries experience: not reported (moderate‐to‐high risk of caries according to Thompson 2005 criteria) Inclusion criteria: clinical: teeth with non‐cavitated caries lesions by visual examination; radiographs: (using bitewings) caries depth between the enamel‐dentine junction and middle one‐third of dentine; the presence of restorations and white spot lesions or cavitations on other tooth surfaces. Participants should not have a medical condition or be taking antibiotics during the period of 2 months prior to the study Exclusion criteria: presence of restorations and white spot lesions or cavitations on other tooth surfaces; symptoms of teeth sensitivity to any type of stimulus |
|
| Interventions | 2 treatment arms Group 1 (27 teeth): sealant: oral hygiene instructions for daily tooth brushing and the use of dental floss; prophylaxis with pumice and water; rubber dam isolation; pumice and water prophylaxis with a Robinson brush (Microdont, São Paulo, SP, Brazil); sealing of pits and fissures with a conventional glass ionomer cement (Vidrion R, SSWhite, Juiz de Fora, MG, Brazil); protection of the sealant with a light polymerised adhesive (Scotchbond, Multipurpose Plus, 3M ESPE, St Paul, MN, USA). Group 2 (24 teeth): no sealant: oral hygiene instructions for daily tooth brushing and the use of dental floss; prophylaxis with pumice and water; no treatment. |
|
| Outcomes |
Primary outcome Clinical efficacy/sensitivity of cavitation after 12 months Secondary outcome Radiographic efficacy (increase of radiolucent area between baseline and interval) |
|
| Notes | In the experimental group, the lost sealant was replaced – teeth with sealant loss were not assigned as failure. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Used a random sampling method in which a number was assigned to each eligible tooth and then put into a sealed opaque envelope. Envelopes were randomly selected by an examiner who allocated the teeth to each group. |
| Allocation concealment (selection bias) | Low risk | Used a random sampling method in which a number was assigned to each eligible tooth and then put into a sealed opaque envelope. Envelopes were randomly selected by an examiner who allocated the teeth to each group. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants/operators. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Only radiographic assessment blinded (a single calibrated and blinded examiner performed this evaluation). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | There are 10 teeth that were lost during the follow‐up albeit it was stated otherwise "All the teeth examined at baseline could be evaluated after 1‐year follow‐up." Teeth with sealant loss were re‐treated and have not been assigned as a failure. |
| Selective reporting (reporting bias) | High risk | There is an unexplained inconsistency in the number of teeth between Table 2 and Table 3 and 4. |
| Other bias | Low risk | No other biases detected. |
Dias 2018.
| Study characteristics | ||
| Methods | RCT, parallel groups Stratified by caries risk Duration of study: interim study with follow‐up after 24 months. Recall examinations performed with 3‐, 6‐, 12‐ and 24‐month intervals Setting: Paediatric Dental Unit of the University of Rio de Janeiro (Brazil) |
|
| Participants | Randomisation unit: teeth 28 children, 57 primary molars with occlusal caries in outer half dentine Age: 3–8 years; mean 6.79, SD 1.81 years Caries experience: ≥ 1 primary molar with caries into outer half dentine. Measured using dmft/DMFT; but also caries risk was measured using the cariogram. Baseline dmft/DMFT 5.56, SD 2.51; 54.4% of teeth had visible plaque Inclusion criteria: good health; occlusal cavitated caries lesion, limited to 1.5 mm in diameter and extending up to the outer half of dentine confirmed by a radiograph. When ≥ 1 tooth per child fulfilled the inclusion criteria, all received the same treatment) Exclusion criteria: the presence of cavities or restorations in other surfaces of target tooth; children with caries lesions in other teeth than the primary molars or with signs and symptoms of pulpal or periradicular pathology, including pain in any tooth; or if children were unable to co‐operate during clinical appointments |
|
| Interventions | 2 treatment arms Group 1 (14 children, 29 teeth analysed): sealing caries with a flowable resin: cleaning of occlusal surface with pumice, local anaesthesia, rubber dam, 37% phosphoric acid for 15 seconds, rinsing and drying, application of adhesive system following manufacturer's instructions and light‐curing for 15 seconds, resin applied and cured for 20 seconds, occlusion checked and adjusted if necessary. Group 2 (14 children, 28 teeth analysed): PCR followed by restoration with a composite restoration and flowable resin. Protocol: cleaning of occlusal surface with pumice; local anaesthesia; rubber dam; cavity opened with high‐speed diamond bur and caries lesion completely removed at the enamel‐dentin junction, dentin caries partially removed with hand instruments until dentin started to become "firm and leathery"; 37% phosphoric acid for 15 seconds; rinsing and drying; application of adhesive system following manufacturer instructions and light curing for 15 seconds; restoration with resin until cavity was filled and cured in increments each for 20 seconds; occlusion checked and adjusted if necessary. |
|
| Outcomes |
Primary outcomes Clinical success measured by USPHS criteria and radiographic evidence of caries progression Radiographic lesion progression Secondary outcomes Child anxiety using Facial Image Scale performed immediately before and directly after treatment, and presented to the children by the examiner (child pointed to the image) Registered time between time tooth was isolated with rubber dam, to the time the rubber dam was removed (in minutes) at time of treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Children were randomised (quote) "by a block design using a coin tossing system." First, they were stratified in 2 clusters paired by caries risk, then each cluster was allocated to a group by tossing a coin. |
| Allocation concealment (selection bias) | Low risk | Children were randomised (quote) "with allocation concealment (through sequentially numbered, white, sealed envelopes)" distributed by a third investigator not involved with the clinical assessment or data analysis. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not described for participants. Treatments are different so at baseline operator could not have been blinded. However, evaluation of restoration success and radiographic change was done by blinded evaluators. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Clinical outcome (quote) "conducted by an experienced examiner who was blinded to the treatment." Radiographic analysis performed by 2 trained and calibrated examiners who were blinded in relation to study groups. However, timing and anxiety performed by the clinician during treatment, and as treatments were different, the clinician could not have been blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Few children missing, and, at 24 months, 13 participants in group 1 and 12 patients in group 2 were equal, but at 3 month is higher in control group and unclear why. |
| Selective reporting (reporting bias) | Low risk | All data outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Elhennawy 2021.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 12 months Setting: Charité – Universitätsmedizin Berlin, Center for Dental and Craniofacial Sciences, Germany |
|
| Participants | 74 children, 74 primary teeth Age: 3–9 years; group 1: mean 6.3, SD 1.5 years; group 2: mean 6.3, SD 1.9 years Gender (boys/girls): group 1: 21/37 (57%/43%); group 2: 14/37 (38%/62%) Caries risk (low/middle/high): group 1: 2/12/23; group 2: 2/13/22 Inclusion criteria: children aged 3–9 years with minimum 1 vital, clinically and radiographically non‐symptomatic, retainable, deeply carious primary molar with a carious lesion involving either only the occlusal or the occlusal and 1 proximal (mesial or distal) surface (i.e. a 1‐ or 2‐surfaced lesion). The lesion was required to radiographically extend into the inner third of the dentine (D3) and show signs of activity, e.g. plaque retention, papillary bleeding, softness of the surface, etc. Parental consent was required from each patient. In addition, participant's co‐operation for treatment under no or only local anaesthesia was expected Exclusion criteria: people with systemic diseases or disabilities, known allergies to the restoration material used as well as teeth which were expected to exfoliate within the next 18 month |
|
| Interventions | 2 treatment arms Group 1 (37 participants, 37 teeth): SE; first treatment visit was performed identically for SE and SW to the extent of SE to leathery dentin. After 6 months (T2), follow‐up examination was performed before the allocation was revealed to the operator. Thus, the initial examination was blinded to both participants and examiner. In the SE group, no further treatment was applied. Group 2 (37 participants, 37 teeth): SW; first treatment visit was performed identically for both groups, following the rules of SE to leathery dentin. After 6 months, the second removal step was performed after removing the restoration until only firm dentin remained in proximity to the pulp. A new restoration was then provided adhesively as described. |
|
| Outcomes |
Primary outcome Absence of endodontic or restorative complications (success), after 12 month; number of teeth failed Secondary outcomes Participant's subjective assessment of the treatment, measured using a Visual Analogue Scale (for SW, assessments were performed after each step, and means used) Total cost and opportunity costs |
|
| Notes | Quote: "sample size calculation was planned for our primary outcome parameter, success, which is defined as not experiencing endodontic or restorative complications. Based on an existing trial on permanent teeth, we anticipated a hazard ratio of 1.3 [18] of SW compared with SE, with α=0.05 and 1‐β=0.9. Originally, we also allowed for substantial drop‐out and subgroup analyses in our sample size estimation, with 192 patients eventually to be included. This planned sample size was not realizable since a multi‐centre trial was not conducted due to limited funding, and recruitment was eventually terminated after 15 month. With the recruited 74 patients, we have to acknowledge that our trial might be under‐powered to detect the originally assumed differences in our primary outcome, which is why we regard it as a pilot trial." Declarations/conflicts of interest: none stated. Funding: funded by Forschungsgemeinschaft Dental e.V. (FGD), Deutsche Gesellschaft für Zahn‐, Mund‐ und Kieferheilkunde (DGZMK), Deutsche Gesellschaft für Restaurative und Regenerative Zahnerhaltung (DGR²Z), GC and Heraeus Kulzer GmbH. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequence generation for treatment allocations performed via random number tables after T0 (a simple random number chain was used, no block randomisation performed). |
| Allocation concealment (selection bias) | Low risk | Allocation concealment performed via sealed opaque envelopes; and allocation only revealed at T2 (i.e. after 6 months) after the re‐examination of the molar. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Operator blinding during the second removal step and subsequent blinding of participants was not possible, but participants were informed not to reveal treatment allocation to the examiner during follow‐up examinations. Quote: "Also, clinical follow‐up examinations were performed by a dentist who was blinded to the allocation and had not been involved in the treatment … patients were informed not to reveal treatment allocation to the examiner during follow‐up examinations." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | As described, both the first removal step and the first re‐examination performed blinded. Also, clinical follow‐up examinations performed by a dentist who was blinded to the allocation and had not been involved in the treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low number of dropouts. |
| Selective reporting (reporting bias) | Low risk | Reported as per protocol. |
| Other bias | Low risk | No other biases detected. |
Foley 2004.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 24 months Setting: 1 University in Scotland, UK |
|
| Participants | 44 children, 79 primary teeth Age: range 3.7–9.5 years, mean 6.8 years Caries experience: any caries depth, as long as lesions having reached the pulp of the tooth Inclusion criteria: children requiring ≥ 1 pair of restorations in their primary molar teeth; teeth had to be in different quadrants and had to be clinically and radiographically asymptomatic Exclusion criteria: previously restored cavities |
|
| Interventions | 3 treatment arms (we did not include data from group 1 as Black Copper Cement is not commonly available or used) Group 1 (36 teeth): participants given option for local anaesthesia; isolation with cotton wool rolls and saliva ejector; instrumentation of cavitated lesions limited to gaining access to caries, removal of gross soft caries only and the preparation of a cavity, sufficient to allow an adequate bulk of restorative material to be placed (i.e. ≥ 3 mm); for non‐cavitated lesions, access to the carious dentine was made using a small, round, high‐speed diamond bur to penetrate through the enamel layer, followed by minimal use of the slow speed handpiece to make the cavity retentive; no other instrumentation was undertaken (i.e. PCR); for occlusal cavities, the cavity was lined with a thin mix of Black Copper Cement and restored with a conventional GIC (Chemfil Superior); covering of the restoration with petroleum jelly. Group 2 (43 teeth): caries treatment as described for group 1. Restoration with a conventional GIC (Chemfil Superior); covering of the restoration with petroleum jelly. Group 3 (41 teeth): participants given option for local anaesthesia; isolation with cotton wool rolls and saliva ejector; conventional preparation (i.e. removal of all carious dentine); restoration of the operator's choice, usually either a conventional glass ionomer cement or an amalgam restoration (where an amalgam restoration was placed, the cavity was also made mechanically retentive). |
|
| Outcomes | Clinical or radiographic failure (or both) after 24 month | |
| Notes | Inconsistency in reporting of failed teeth: 7 + 7 + 10 failed teeth did not equal overall 31 failed teeth; some teeth with restoration failure had been excluded from analysis. Funding: Tattersall Scholarship, University of Dundee and the Carnegie Trust for the Universities of Scotland. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Molar pairs were randomly assigned using computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Sealed opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants/operators. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Only radiographic assessment blinded. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Teeth with restoration failures were excluded from study. (6 molars were withdrawn from the trial due to restoration failure and abscess formation.) |
| Selective reporting (reporting bias) | High risk | Not all relevant outcomes clearly presented (e.g. exact number of failed teeth). No information on outcome measure for clinical assessment of restorations. |
| Other bias | Low risk | No other biases detected. |
Franzon 2014.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 24 months. Clinical and radiographic outcomes assessed at 3, 6, 12, 18 and 24 months after treatment Setting: Department of Paediatric Dentistry, School of Dentistry from Federal University of Rio Grande do Sul (UFRGS, Porto Alegre, Brazil) |
|
| Participants | 51 children, 120 deep carious lesions in dentine Age: 3–8 years; mean 67, SD 16 months Caries experience: ≥ 1 molar with acute deep carious lesion in the inner quarter of dentine and involving 1 (occlusal) or 2 surfaces (occlusal‐proximal) Inclusion criteria: radiographic: lesion extended to the inner quarter of dentine and involving 1 (occlusal) or 2 surfaces (occlusal‐proximal); no medical history radiographic inclusion criteria were: absence of sensitivity or spontaneous pain (or both); swelling, fistula and mobility incompatible with the root resorption stage; absence of periapical or interradicular radiolucency or other radiographic signs indicative of pulp necrosis Exclusion criteria: impossible to perform the restorative procedures |
|
| Interventions | 2 treatment arms Group 1 (54 teeth analysed): total caries removal: under local anaesthesia and rubber dam isolation, dentinal carious lesions were accessed when necessary with a round diamond bur (1011/1012) operated at high speed under water‐cooling. Decayed dentine was removed completely from the lateral walls of cavities using round burs at low speed. After total caries removal, the absence of caries was confirmed after removal of all softened dentine using a blunt‐tipped probe. Each cavity was then cleaned, washed and dried. Calcium hydroxide cement was applied to the pulpal wall, followed by 37% phosphoric acid etching of enamel for 15 seconds and dentine for 7 seconds. The cavity was then flushed with air/water spray and dried with sterilised cotton pellets while retaining tissue moisture. Cavities then restored with composite resin after hybridisation with an adhesive system. The rubber dam was then removed and occlusion was tested and adjusted. Group 2 (66 teeth analysed): PCR: under local anaesthesia and rubber dam isolation, dentinal carious lesions were accessed when necessary with a round diamond bur (1011/1012) operated at high speed under water‐cooling. Decayed dentine was removed completely from the later walls of cavities using round burs at low speed. PCR was performed using visual and tactile clinical criteria. Excavation was stopped when hardened, dried dentine with a leathery consistency was achieved. Each cavity was then cleaned, washed and dried. Calcium hydroxide cement was applied to the pulpal wall, followed by 37% phosphoric acid etching of enamel for 15 seconds and dentine for 7 seconds. The cavity was then flushed with air/water spray and dried with sterilised cotton pellets while retaining tissue moisture. Cavities then restored with composite resin after hybridisation with an adhesive system. The rubber dam was then removed and occlusion was tested and adjusted. Complete removal in the peripheral area; central removal of soft dentine. |
|
| Outcomes |
Primary outcomes Restoration failure of class I and II restorations (primary outcome) was characterised by a blinded, trained and calibrated operator using a modified USPHS at 3, 6, 12, 18 and 24 months Discolouration: absent (Alpha/Bravo) or present (Charlie/Delta); marginal integrity: present (Alpha/Bravo) or absent with exposed dentine (Charlie/Delta); anatomical shape: suitable boundary and continuity (Alpha/Bravo) or lack of sufficient to expose dentine or liner materials (Charlie/Delta) restorative material; adjacent carious lesion: absent (Alpha) or present (Charlie). The Alpha and Bravo scores were recorded as a clinical success Secondary outcomes Interval 24 months; children, carer and provider preference/acceptability Time to perform the treatment |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The choice of the experimental groups to which the teeth belong was taken by lot, with the aid of a coin, after anaesthesia and rubber dam isolation. |
| Allocation concealment (selection bias) | Unclear risk | Concealment not mentioned. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of the operators was not possible, because they knew the type of decayed dentine excavation. Participants and the clinical examiner were blinded about the type of treatment that each tooth received (the same restorative material was used). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Calibrated, blinded operator evaluated restoration survival by clinical examination. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Three boys, comprising four teeth, did not return for any of the follow‐up examinations and were excluded from the analyses." Comment: 2 teeth from each group, unclear why. |
| Selective reporting (reporting bias) | Low risk | All data outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Hesse 2014.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up duration of the study: 18 months. The outcome assessed after 6, 12 and 18 months assessments Setting: School of Dentistry of University of São Paulo, Brazil |
|
| Participants | 36 children, 36 primary teeth Age: 4–9 years, mean 7 years Gender: 16 (44.4%) girls; 20 (55.6%) boys Caries experience: above average (mean 6.0) according to age‐related dmft values for Brazilians Inclusion criteria: assessed radiographically and clinically: clinically: only children with good general health, and at ≥ 1 primary molar with occlusal active caries lesion, not previously restored, classified as ICDAS score 5, with an opening < 3 mm diameter in the enamel, measured with a millimetre probe, and no pain history; radiographically: lesion extended into dentine, but no more than halfway through |
|
| Interventions | 2 treatment arms Group 1 (17 participants, 17 teeth): pit and fissure resin‐based sealant application, without removing caries tissue. Teeth sealed according to following protocol: occlusal surface cleaned with pumice; local anaesthesia applied; rubber dam applied; 37% phosphoric acid placed on occlusal surface for 15 seconds; surface rinsed and dried; adhesive system (Adper Single Bond 2, 3M ESPE, Saint Paul, NM, USA) applied, following the manufacturer's instructions and light cured for 20 seconds; resin‐based sealant (Fluroshield, Dentsply, Rio de Janeiro, Brazil) applied and light cured for 20 seconds; occlusion checked and adjusted when necessary. Group 2 (19 participants, 19 teeth): SE; teeth restored according to the following protocol: occlusal surface cleaned with pumice; local anaesthesia applied; rubber dam applied; cavity opened in enamel with a diamond bur in high speed, carious tissue completely removed in the enamel/dentin junction and partially removed with hand instruments until the dentine started to become firm and leathery in pulpal areas; 37% phosphoric acid applied in the cavity for 15 seconds; surface rinsed and dried; adhesive system (Adper Single Bond 2, 3M ESPE, Saint Paul, NM, USA) applied, following the manufacturer's instructions and light cured for 20 seconds; restoration with composite resin (Z250, 3M ESPE, Saint Paul, NM, USA), using the incremental technique until cavity was filled and light cured of each increment for 20 seconds; occlusion checked and adjusted when necessary. |
|
| Outcomes |
Primary outcomes Radiographic assessment: caries progression (absence/present) Clinical: partial loss and total loss (failure) or total retention (success) The marginal integrity of sealants and restorations were assessed clinically by 1 examiner trained by a "golden standard" evaluator regarding the evaluation criteria. To calculate the intraexaminer concordance, 15 participants involved in the research were re‐evaluated with an interval of 2 weeks (kappa = 1.00). The scores for clinical assessment were: partial loss and total loss (failure) or total retention (success). When integrity failures were found during the follow‐up visits, the reapplication of the sealant or restoration‐repair was done; however, the related tooth was considered as a failure in the subsequent clinical analysis. The evaluation criteria for the clinical assessment at the follow‐ups were the same for both groups. Secondary outcome Lesion progression status after 6 months |
|
| Notes | Sample size: sample power was calculated (using an α error of 5%) and resulted in 0.9. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Participants were randomly allocated into 2 groups with the use of a list of random numbers generated by computer. |
| Allocation concealment (selection bias) | Unclear risk | No information provided on allocation concealment or timing. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | All treatments were performed by 1 trained operator and helped by a dental assistant. The operator was a final‐year undergraduate dental student who was previously trained to perform both techniques used in this study. A training week was included to give the operator the opportunity to familiarise herself with the sealants application and restorative technique prior to the start of the operative phase. Dentist would know intervention. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Clinically – no mention of blinding but similar restorative procedures so may have been blinded. The examiners assessed the radiographs through paired evaluations comparing 2 by 2, blinded regarding chronological. Outcomes were clinical in nature – not participant reported. Not possible to blind outcome assessment. Quote: "The examiners assessed the radiographs through paired evaluations comparing two by two, blinded regarding chronological order of the radiographs and without the aid of any magnification loops." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Low number of dropouts. |
| Selective reporting (reporting bias) | Low risk | Reported as per methods. |
| Other bias | Low risk | No other biases detected. |
Innes 2011.
| Study characteristics | ||
| Methods | 2011 (phase 1): split‐mouth, RCT; 2015 (phase 2): retrospective observation of RCT participants; parallel groups (recruited and treated July 2001 to January 2004) Follow‐up: 1, 2, 5 years and to exfoliation Setting: 17 general dental practices in Scotland (UK), recruiting 10 participants each |
|
| Participants | 132 children, 264 teeth Age: 3–10 years; mean 6.8, SD 1.6 years ("Two children were three years of age and six children were 10 years of age. In the inclusion criteria, the lower age of four years was originally chosen because it was felt that children any younger would not tolerate radiographic examination. This decision was not based on clinical rationale relating to the treatments. It was, therefore, decided to include these patients. With the patients over nine years of age, the recruiting GDPs anticipated that the teeth were still likely to be present after two years. As the study was a split mouth design, inclusion of these teeth would not bias either for or against the intervention or control and they were, therefore, also included in the analyses.") Inclusion criteria: aged 4–9 years, with no significant health problem, and presenting for routine dental care to their general dental practice. Matched (clinically and radiographically) caries lesions (for tooth type, arch and extent of caries) on primary molars. |
|
| Interventions | Teeth in pairs were analysed (264 teeth in study), from 132 participants 2 treatment arms Group 1 (132 participants, 132 teeth allocated, 128 treated): HT and sealing using performed metal crowns. No caries removal (only food could be removed from the cavity), tooth preparation or anaesthesia. Correct size of the crown was selected, filled with glass ionomer luting cement, seated with digital pressure and child asked to bite hard to fully seat the crown. Excess cement removed and child continued biting until cement had set Group 2 (132 participants, 132 teeth allocated, 128 treated): non‐selective caries removal from the periphery of the cavity, and as far as possible in the base without causing pulpal exposure; and placement of a restoration of choice based on usual care (including local anaesthesia if usually used) |
|
| Outcomes |
Primary outcome Major failures (irreversible pulpitis, loss of vitality, abscess or unrestorable tooth) Secondary outcomes Minor failures (reversible pulpitis, restoration loss/wear/fracture or secondary caries) Preferences for each treatment (child, parent, dentist) Time taken to explain and complete treatment Cost |
|
| Notes | Schwendicke 2019 (see under Innes 2011) represents an analysis of Innes 2011, regarding cost‐effectiveness. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation for treatment allocation and order (blocked at every 10th generation), by telephoning to a central administrator. |
| Allocation concealment (selection bias) | Low risk | Not described from original trial on retrospective paper, but from author, it was performed by calling to a central location by telephone, so likely concealed. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not described for participants in retrospective paper, even though PMC were used for Hall crown and only 1 participant in control group, so patients probably were not blinded either. Clinicians could not have been blinded as treatment are different. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | For retrospective data collection, blinded as data collected based on participants study number and no other identifier as to group allocation. For study not blinding of examiners possible. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reason for missing data provided in CONSORT diagram of 2011 and 2007 paper (split‐mouth design). |
| Selective reporting (reporting bias) | Low risk | All data outcomes for retrospective data reported. |
| Other bias | Low risk | No other biases detected. |
Khokhar 2018.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 18 month Setting: University Clinic; Postgraduate Department of Conservative Dentistry and Endodontics of PGIDS (Post Graduate Institute of Dental Sciences), Rohtak, India |
|
| Participants | 143 permanent teeth Age: range 14–54 years, mean 25.19 years Inclusion criteria: mature permanent mandibular molars having deep carious lesions involving half or more of the dentine detected by radiographic examination, confirmed as vital teeth using the electric pulp test, and the cold test and the absence of apical radiolucency Exclusion criteria: signs and symptoms of irreversible pulpitis, swelling, fistula and mobility |
|
| Interventions | 2 treatment arms All procedures were performed under local anaesthesia and rubber dam isolation. Group 1 (70 teeth): SE: carious tissue from the lateral walls and dentino‐enamel junction was removed completely using low‐speed metal burs or hand excavator, or both. Superficial necrotic dentin was removed from the pulpal and axial wall using low‐speed round bur. A layer of soft, wet carious dentin was left adjacent to pulpal wall and cavity was cleaned with distilled water and gently dried with air and moist cotton pellet. Group 2 (73 teeth): non‐selective caries removal: carious tissue from the lateral walls and dentino‐enamel junction was removed completely using low‐speed metal burs or hand excavator, or both. A caries‐detector dye (Kurary, Tokyo, Japan) was applied to dentine for 10 seconds, followed by washing. This procedure was repeated until the dentine was no longer stained. In all cavities RMGIC (Fuji Lining LC; GC, Tokyo, Japan) was applied to the pulpal wall after conditioning, followed by etching with 37% phosphoric acid for 15 seconds, and restored with composite resin (Tetric N‐Ceram; Ivoclar Vivadent), using the incremental technique and each increment was polymerised for 40 seconds. The rubber dam was then removed and occlusion was checked. In cases of pulp exposure direct pulp capping, pulpotomy and root canal treatment was performed. |
|
| Outcomes |
Primary outcome After 18 month, success was defined as positive response to cold and electric pulp test, absence of signs and symptoms of irreversible pulpitis (spontaneous pain, fistula and swelling) and absence of periapical alterations (radiolucency at furcal or periapical region) (combined outcome). Digital radiographs were taken with standardised exposure parameters (70 kvp, 3.5 mAs, and 0.2 seconds) by a single operator according to a standardised procedure by placement of film holders (XCP‐DS Carestream) in paralleling technique. All radiographs were obtained by the same digital imaging system (Kodak RVG 5200; Carestream Dental). |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Randomization was developed to eliminate any bias on the part of the investigators and to equalize the number of patients between the two treatment groups." Comment: it was never clarified how the randomisation was performed. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Using an equal proportion randomization allocation ratio, one of the investigators (M. J.) created envelopes containing concealed assignment codes that were assigned sequentially to eligible patients." Comment: 1 of the investigators assigned the envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Using an equal proportion randomization allocation ratio, one of the investigators (M. J.) created envelopes containing concealed assignment codes that were assigned sequentially to eligible patients." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Two blinded examiners assessed the clinical and radiographic outcomes of test and control treatments at 1, 3, 6, 12, and 18 month after treatment." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | There was loss of 7 participants (3 SE and 4 CR), which we considered a very small proportion of teeth lost to follow‐up. |
| Selective reporting (reporting bias) | High risk | Quote: "Outcomes of test and control treatments at 1, 3, 6, 12, and 18 month after treatment." Comment: authors reported only 18‐month outcomes. |
| Other bias | Low risk | No other biases detected. |
Labib 2019.
| Study characteristics | ||
| Methods | Randomised clinical trial, parallel groups Follow‐up: 12 months Setting: Misr International University in Cairo, Egypt |
|
| Participants | 115 participants, 132 permanent teeth Age: 18–47 years; mean 29.25, SD 6.8 years Inclusion criteria: men and women (aged 18–50 years), able to tolerate necessary restorative procedures, willing to sign the informed consent, accepted the follow‐up period, posterior permanent tooth with occlusal/occlusal/proximal deep carious lesion, radiographically (bitewing radiograph) extending to the inner 1/3 of dentine (D3) with a radio‐opaque layer between the carious lesion and the pulp chamber. Sensible teeth according to cold pulp test Exclusion criteria: allergy to any of the restorative materials, people undergoing orthodontic treatment with fixed appliances, pregnant women, people with debilitating systemic diseases, teeth with previous restorations, spontaneous pain or prolonged pain (> 15 seconds) after sensitivity test (cold test), which would indicate irreversible pulpitis, negative sensibility tests, periapical radiolucencies and sensitivity to axial or lateral percussion; mobile teeth, indicating periodontal disease or trauma; external or internal resorption |
|
| Interventions | 2 treatment arms Both arms followed the same baseline treatment protocol: under rubber dam isolation and local anaesthesia, carious tissue removal to hard dentine performed peripherally, while soft dentine close to pulp (pulpal floor/axial wall) was left and restored with glass ionomer material. Group 1 (66 teeth): SE: at a second appointment, the glass ionomer was cut back pulpally or axially (or both), to act as a base leaving a sufficient bulk of 2 mm for the final restoration. For proximal preparations, a sectional matrix system (Palodent Plus, Dentsply) was used. Selective etching of enamel was performed using 35% phosphoric acid gel (Scotchbond Universal Etchant, 3M ESPE, St Paul, NM, USA) for 15 seconds, rinsed for 15 seconds with water, gently air dried with water‐free/oil‐free air for 5 seconds and excess moisture blot‐dried using absorbent tissue. A single layer of universal adhesive (Single Bond Universal, 3M ESPE, St Paul, NM, USA) was applied to the entire cavity preparation using an applicator brush, rubbed in for 10 seconds, air dried for 5 seconds and light‐cured for 20 seconds as described above. The overlaying resin composite (Filtek Z350 XT, 3M ESPE, St Paul, NM, USA) was applied in 2‐mm thick increments, which were light‐cured for 20 seconds as described. The restoration was contoured and finished while polishing was achieved using 1‐step polishing system (Dimanto, Voco, Germany). Group 2 (66 teeth): SW: at a second appointment, re‐entry for the carious lesion was performed by total removal of the glass ionomer and the residual carious lesion until firm dentine remained. The cavity was partially filled again with the highly viscous glass ionomer to serve as a base. The final composite resin restoration was provided using the same restorative procedures as described for group 1. |
|
| Outcomes |
Primary outcome Treatment success: absence of endodontic/restorative (pulp necrosis, irreversible pulpitis, postoperative pain, need of tooth extraction) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | The randomisation unit was the tooth. Sequence generation performed using Microsoft Excel (Microsoft, Washington, USA) by an independent contributor. Block randomisation was performed with 1:1 allocation ratio using random block sizes of 34, 30, 30, 30 and 8. Randomisation sequence and block sizes were concealed from the primary investigator and other operators. |
| Allocation concealment (selection bias) | Low risk | Quote: "The randomisation unit was the tooth. Sequence generation was performed using Microsoft Excel (Microsoft, Washington, USA) by an independent contributor. Block randomisation was performed with 1:1 allocation ratio using random block sizes of 34, 30, 30, 30 and 8. Randomisation sequence and block sizes were concealed from the primary investigator and other operators. Participants who came back for their second visit (T2) with vital teeth and showing no signs of failure had each tooth allocated remotely via phone prior to further treatment (n = 113)." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The restorative procedure used 2 steps for all groups; in the first visit, a glass ionomer restoration was placed; in the second step, this was either only cut back to serve as a liner for a composite resin restoration (in SE) or completely removed to allow the second excavation step (SW), followed by reapplication of a glass ionomer base and a resin composite restoration. This was done to prevent operator bias during the first visit and to keep the participant blinded to trial design. However, there was still potential for bias at the second stage as the operator knew whether they were removing all glass ionomer base (for SW) or only partial (for SE). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quotes: "Randomisation sequence and block sizes were concealed from the primary investigator and other operators." "Assessment of clinical and radiographic criteria for success was performed by two blinded, calibrated outcome assessors for each tooth. In addition, the following data were collected by a dentist who had not been involved in the treatment at all visits, including possible re‐treatment visits in case failures occurred: (1) Materials used. (2) Travel times for the patients. (3) The time needed for each visit. Data collection used standardised forms for each visit." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 8% censoring per annum was within pre‐established margins. Similar numbers lost to follow‐up, 7 to 8 T2 and 12 to 14 at T3. Methodologically consistent, but could not rule out that lost to follow‐up was not related to the treatment provided in violation of independent censoring. In contrast, the accounting of the extraction as a failure instead of censoring is a satisfactory management of this risk. |
| Selective reporting (reporting bias) | Low risk | Quote: "Reporting of this trial follows the Consolidated Standards of Reporting Trials (CONSORT) guidelines to ensure transparent and complete reporting." All expected outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Leksell 1996.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 12 months Setting: Department of Pedodontics, Eastman Institute or at the District Dental Clinics in Rinkeby and Tensta, County of Stockholm; 3 secondary care centres |
|
| Participants | 116 children, 127 permanent teeth Age: 6–16 years Gender: not reported Inclusion criteria: permanent posterior teeth were selected if the radiographs revealed carious lesions to such a depth that pulp exposure could be expected if non‐selective was chosen |
|
| Interventions | 2 treatment arms In all teeth, the first clinical procedure comprised opening of the cavity with high‐speed equipment including removal of carious enamel. The bulk of carious dentine was then removed with a sharp excavator supplemented by drilling with round burs at low speed. Group 1 (57 teeth): SW; in 57 teeth, randomly selected for SW, the remaining innermost layer of carious dentine was covered with calcium hydroxide. At the second appointment, the excavation was continued with excavators or round burs (or both) until hard dentin was reached or a pulp exposure occurred. A caries‐free cavity bottom was defined as no softening of the remaining dentine when examining the cavity floor with a blunt explorer. Group 2 (70 teeth): non‐selective caries removal defined as no softening of the remaining dentine when examining the cavity floor with a blunt explorer. |
|
| Outcomes |
Primary outcome Pulp exposure, symptoms of pulpal disease after 12 month |
|
| Notes | Funding: not reported. Declarations/conflicts of interest: none. Sample size: not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomly selected for either SW or direct complete excavation. Comment: no detail on randomisation – uneven numbers in each arm of trial suggest problem with randomisation. |
| Allocation concealment (selection bias) | Unclear risk | No indication of when operator was informed of treatment group or how concealment was maintained. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding not possible – different number of appointments, operator knew caries removal technique. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not possible – the outcome assessor could not be blinded for the primary outcome of pulp exposure as this was assessed during treatment by the operator. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 12 month was the minimal follow‐up. 80 teeth fulfilled this requirement, 40 treated by SW and 40 by CR. 6 participants in the SW group did not return for subsequent appointments. By eliminating teeth with pulpal exposures the study design introduced a source of potential bias. |
| Selective reporting (reporting bias) | Low risk | Published report includes expected outcomes. |
| Other bias | Low risk | No other biases detected. |
Lula 2009.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 6 month, recruitment period June to August 2007 Setting: Paediatric Dentistry Clinic of UFMA, Brazil |
|
| Participants | 30 children, 36 primary teeth Age: 5–8 years Gender: not reported Inclusion criteria: patient healthy and with ≥ 1 carious primary molar; primary molar presenting pulp vitality, without previous restoration and with no radiographic signs suggestive of pulp or periapical abnormalities (or both); carious lesion active carious lesion in the inner half of dentine, with the buccal‐lingual opening measuring ≥ 2 mm and involving the occlusal or occluso‐proximal surface |
|
| Interventions | 2 treatment arms Group 1 (18 teeth): SE; after access to the lesion had been gained the whole of the carious tissue involving the lateral walls and dentino‐enamel junction was removed, whereas only superficial necrotic dentine was removed from the pulpal and axial walls using low‐speed round burs. Group 2 (18 teeth): non‐selective caries removal: the teeth of the participants were anaesthetised, isolated with a rubber dam and then submitted to the technique of caries removal as previously defined by the random sequence. In the control group, the cavity was accessed with a number 329 carbide bur at high rotation and carious tissue was completely removed with smooth spherical burs at low rotation, with the size of the bur being compatible with that of the lesion. To reduce examiner subjectivity, a caries detector dye was applied to dentin for 10 seconds, followed by washing. This procedure was repeated until the dentine was no longer stained. |
|
| Outcomes |
Primary outcome Pulp exposure, signs or symptoms of pulpal disease, microflora levels following complete caries removal and PCR – subsequent levels 3–6 month later, radiographic signs of caries progression |
|
| Notes | Declarations/conflicts of interest: none. Sample size: not reported. Funding: Conselho Nacional de Desenvolvimento Cientifico e Tecnologico/Edital Universal and Fundacao de Amparo A Pesquisa do Estado do Maranhao. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "… the sample was randomized using a sequence of random numbers generated in an electronic spreadsheet by a person who did not belong to the research group." |
| Allocation concealment (selection bias) | Low risk | Quote: "… this information was passed on to the examiner (E.C.O.L) only at the time of treatment." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | All teeth were protected with calcium hydroxide cement, etched with 37% phosphoric acid for 15 seconds, and restored with an adhesive system and resin composite and within 3–6 months of treatment, the teeth were submitted to clinical and radiographic examination to determine signs and symptoms of pulp vitality. Comment: all teeth were restored with the same materials and all teeth were re‐entered; therefore, it is likely the participants were blinded regarding their treatment. Operator blinding not possible as they knew caries removal technique. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not possible – the outcome assessor could not be blinded for the primary outcome of pulp exposure as this was assessed during treatment, by the operator. Within 3‐6 months of treatment, the teeth were submitted to clinical and radiographic examination to determine signs and symptoms of pulp vitality. Next the restorative materials were removed in the 2 groups and a new dentine sample was collected. Comment: although efforts were made to maintain blinding of the outcome assessor by restoring each group with the same materials and carrying out the same review protocol, overall there was a high risk of bias that was introduced during pulp exposure assessment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 2 participants excluded from partial removal group due to exfoliation of tooth and loss of contact with participants. 2 participants excluded from complete removal group due to necrosis and loss of restoration. Reasons for dropouts different and related to treatment in complete removal group. |
| Selective reporting (reporting bias) | Low risk | Published report includes expected outcomes. |
| Other bias | Low risk | No other biases detected. |
Magnusson 1977.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: in 1 group, no follow‐up; in the other (SW), follow‐up associated with this treatment (6 weeks) Setting: 1 university in Sweden |
|
| Participants | 62 children, 110 molars Age: 5–10 years Inclusion criteria: primary molars with deep carious lesions Exclusion criteria: signs of pulpitis (i.e. episodes of persistent or shooting pain, tooth that were tender to percussion), radiographic signs of pathological periradicular or internal pulp changes |
|
| Interventions | 2 treatment arms Group 1 (62 participants, 55 teeth): excavation until all softened dentine had been removed; no information on final restoration measures and material. Group 2 (62 participants, 55 teeth): excavation until a thin layer of soft dentine remained on the pulpal cavity floor; washing of the cavity with a microbiocidal solution; covering of remaining carious tissue with calcium hydroxide; bonding of the dressing with a thin layer of cement; sealing of the cavity with zinc‐oxide‐eugenol cement; reopening after 4–6 weeks; removing of all softened tissue; no information on final restoration measures and material; in 9 cases a second period of 4 weeks of calcium‐hydroxide dressing was considered necessary. |
|
| Outcomes |
Primary outcome Pulp exposure and pulpal complications between treatment steps (only for SW group) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | If the child was born on an odd day of the month, the molar was excavated step by step; if born on an even day of the month, immediate complete removal of softened carious dentine. |
| Allocation concealment (selection bias) | High risk | Due to predictable nature. No concrete method for allocation concealment reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding of participants/operators. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No blinding of assessor reported. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | No attrition occurred. |
| Selective reporting (reporting bias) | Unclear risk | No study protocol available – insufficient information to permit judgement of low or high risk of bias. Incomplete description of the intervention, i.e. on how complete excavation was defined. |
| Other bias | Unclear risk | Missing information on the depth of lesions in the included teeth. |
Maltz 2018.
| Study characteristics | ||
| Methods | RCT, parallel groups Follow‐up: 18 months, 3 years, 5 years Setting: primary care (Public Health Services) or secondary care (Brazilian Federal Universities) |
|
| Participants | Children, 233 teeth Age: mean 17.17 years, median 14 years, minimum 6 years Caries experience: DMFT 7.9, SD 5.7 Inclusion criteria: deep caries lesion (> 1/2 dentine on radiographic examination) permanent molars; positive response to thermic test; no pain or sensitivity to percussion and absence of periapical pathologies Exclusion criteria: cuspal loss or caries beneath the gingival margin |
|
| Interventions | 2 treatment arms Group 1 (153 teeth): SE: after local anaesthesia and rubber dam isolation, the lesion was accessed with a diamond bur. Then, complete excavation from cavity walls was performed with dentine excavators or low‐speed burs, according to the hardness‐tactile criteria (hardness to probe). SE of carious dentine (only disorganised dentine was removed) on the pulp wall was performed by manual instruments. The cavity was washed with distilled water and dried with sterile filter paper. The teeth were randomised, and those allocated to the test group (SE) received reconstruction of the surrounding walls and pulp lining with glass‐ionomer cement (Vitro Fil, DFL, Rio de Janeiro, Brazil). Teeth were then filled with composite resin (Tetric EvoCeram, Ivoclar/Vivadent, Liechtenstein) or amalgam (GS‐80, SDI, Bayswater, WA, Australia). Group 2 (146 teeth): SW: initial treatment as described. Teeth allocated to the control group (SW) received indirect pulp capping with calcium hydroxide cement (Dycal, Caulk/Dentsply, Rio de Janeiro, Brazil) and temporary filling with a modified zinc oxide eugenol cement (IRM, Caulc/Dentsply, Rio de Janeiro, Brazil). The cavity was reopened after a median time of 90 days, the remaining decayed dentine was removed, and the teeth were restored. |
|
| Outcomes |
Primary outcome Pulp vitality, evaluated by: a positive response to cold test, absence of spontaneous pain, negative sensitivity to percussion, absence of periapical lesion (radiographic examination), restoration quality |
|
| Notes | Funding: CAPES, CNPq (40.3420/04‐0), FAPERGS (04/1531‐8), Ivoclar/Vivadent (Schaan, Liechtenstein), DFL (Rio de Janeiro, Brazil), SDI (Bayswater WA, Australia), and Hu‐Friedy (Chicago, IL, USA). Study authors note that the SW treatment was not fully completed in all participants and an intention‐to‐treat analysis was used: "failure of patients to attend the second appointment compromised the therapy performance in our study. Out of the 114 SW treatments evaluated, 26 have not completed the treatment thus increasing substantially the risk for failure." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Teeth were randomly assigned for test or control groups. Quote: "A number corresponding to each treatment group was printed on pieces of paper and kept in dark flasks. A paper was selected from the flask by a person other than the operator, and the treatment indicated was executed (test/control)." |
| Allocation concealment (selection bias) | Low risk | The operator was blinded to the allocation sequence and only knew treatment arm after caries excavation. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of dentist not possible. Dentist were aware of different number of appointments required in the 2 arms. Authors noted the risk of bias. Quote: "Blinding of patients was not possible due to the different number of appointments in each treatment." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Final examination (5 years) performed by an external examiner, who did not know treatment allocation, in addition (quote): "The patients files were coded, therefore the examiner were not aware of which group the patients pertained." |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Although 70 teeth were missing from final follow‐up, these were evenly split between groups. The authors report that "no significant difference was found regarding demographic and clinical variables. The only variable that differed between lost and followed individuals was the region, with a higher proportion of patients lost to follow‐up in the Midwest region. This fact has been addressed by the adjusted analysis..." |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | High risk | The use of Weibull as a parametric test to study survival is a methodological error. Note that if the data fit with this fully parametric test, it is because the observations are very reduced in number and frequency. As a result, the test does not reflect the ACTUAL risk of failure of the treatment studied, but that settled arbitrarily for the authors. |
Mello 2018.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 4–6 months (mean 5 months) Setting: secondary care (University), Brazil |
|
| Participants | 44 children, 62 primary teeth Age: 5–9 years Inclusion criteria: deep carious primary molars (> 2/3 into dentine); without sensitivity or spontaneous pain (or both) or pulp exposure, tooth mobility, fistula or abscess, pulp or root pathologies observed on radiograph; or root resorption of > 2/3 on radiograph; and tooth with restorative possibility Exclusion criteria: children with systemic diseases, allergy to latex or local anaesthetic |
|
| Interventions | 2 treatment arms Group 1 (24 teeth): SE: infected dentin was removed, while the affected dentin was maintained on the pulpal wall. Group 2 (38 teeth): non‐selective caries removal: both infected and affected dentin removed. |
|
| Outcomes |
Primary outcome Signs or symptoms of pulpal disease: pain, clinical or radiological loss of vitality, mobility, root resorption, etc. Clinically/radiographically success/failure after 6 months Secondary outcome Pulp exposure during excavation |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Authors did not report method of random allocation to treatment groups. |
| Allocation concealment (selection bias) | Unclear risk | Allocation concealment not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Single operator performed both treatments. Blinding of dentist not possible due to differences in techniques. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not possible for the outcome of pulp exposure as the operator assessed it during treatment. Clinical and radiological examination blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All teeth included in analysis. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Mertz‐Fairhurst 1998.
| Study characteristics | ||
| Methods | RCT, split‐mouth design Duration of study: 24 months. Follow‐up: 10 years; assessment intervals 6 months, and 1, 2, 3, 4, 5, 6, 9 and 10 years Setting: School of Dentistry, Medical College of Georgia, Augusta, GA, US; treatment performed by faculty members |
|
| Participants | 123 participants, 156 pairs of molar or premolar teeth (312 teeth) Age: 8–52 years; median 23 years Inclusion criteria: each person must have had at least 1 pair of Class I lesions in premolars or permanent molars, and the carious lesions must have been clinically and radiographically (outer half of dentine) obvious |
|
| Interventions | 3 treatment arms (we combined groups 1 and 2) Group 1 (79 teeth): CR: unsealed amalgam AGU: rubber dam when possible. It was prepared using the traditional principles for Class I cavity form in which the preparation was extended into non‐carious fissures to prevent future caries activity (extension for prevention). Complete removal of soft demineralised dentine and chalky white demineralised enamel. Amalgam placement. Group 2 (77 teeth): CR: sealed amalgam restoration: rubber dam when possible. Removed all soft demineralised dentine only in the localised area of the carious lesion, but the preparation was not extended into unaffected fissures and grooves. If 2 separate occlusal lesions were present, they were not combined into a single larger amalgam restoration. Instead, 2 small localised cavity preparations were made, except when the distance between the 2 cavity preparations would be < 0.5 mm. After the amalgam was placed, the operator applied sealant over the restoration and all pits and fissures of the tooth. Group 3 (156 teeth): caries sealing using composite (CompS/C): rubber dam when possible. The only preparation for the CompS/C restorations consisted of placing a 45‐ to 60‐degree bevel in the enamel surrounding the frank cavitated lesion. This occlusally divergent bevel had to be ≥ 1 mm wide and placed in sound enamel. The operator removed all the crumbly, opaque demineralised enamel with a bur until they reached translucent sound enamel. They did not remove undermined enamel or caries below the bevel. After restoration and a final shaping of the occlusal anatomy with rotary instruments, the operator etched all the occlusal, buccal and lingual pits and fissures for 60 seconds, washed the etchant thoroughly and applied a chemically cured sealant. The sealant, which was applied with an applicator supplied in the sealant kit, was placed over the entire restoration and adjacent etched enamel as well as over all the pits and fissures of the tooth. |
|
| Outcomes | Restorations clinically failed or marginal integrity failure; restoration integrity. | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Treatment assignment was statistically randomised for each study tooth using a randomisation list prepared by a statistician. |
| Allocation concealment (selection bias) | Unclear risk | No information on how allocation concealment was carried out. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Not possible to blind operators as treatments were different. Unclear about participants. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Double‐blind examiners for radiographic examinations. Other not described, but difficult to blind different materials. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Reasons for attrition not always clear. |
| Selective reporting (reporting bias) | High risk | Unclear whether all outcomes were fully reported. |
| Other bias | Unclear risk | Data were not presented in same manner throughout, so unclear in places. |
Orhan 2010.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 12 months Setting: secondary care (university) in Turkey |
|
| Participants | 123 children, 154 primary second or permanent first molars Age: 4–15 years Inclusion criteria: deep dentine carious lesions assessed clinical and radiographic (≥ 3/4); absence of fistula, swelling in periodontal tissues, and abnormal tooth mobility; absence of clinical symptoms of irreversible pulpitis; absence of radiolucencies at the inter‐radicular or periapical pathologies; pulp sensitivity confirmed by a cold stimulation tester or electric pulp tester, or both |
|
| Interventions | After the administration of anaesthetics and the rubber dam isolation, the first clinical step in all teeth comprised the opening of the cavity and the removal of undermined enamel using high‐speed equipment with copious air/water spray and diamond burs (KG Sorensen, Zenith Dental ApS, Agerskov, Denmark). Caries at the lateral walls of the cavity and at the enamel‐dentine junction was completely removed with excavators or tungsten carbide round burs at low speed, or both. Subsequently, the central cariogenic biomasses and superficial part of the necrotic and demineralised dentine were removed as follows. 3 treatment arms Group 1 (50 teeth: 31 primary, 19 permanent): SE: after eliminating the superficial part of the necrotic dentine, excavation continued until the operator thought pulp exposure would occur with further excavation; thus, a layer of soft carious dentine was left on the cavity floor adjacent to the pulp wall. The remaining innermost layer of carious dentine was covered with calcium hydroxide (Dycal, Caulk/Dentsply, Dentsply, Milford, DE, USA). The cavity was then restored with a layer of glass ionomer, followed by compomer (Dyract Extra, Dentsply, DeTrey GmbH, Konstanz, Germany) for primary molars and composite resin (Grandio Voco, 27457, Cuxhaven, Germany) for permanent molars. Group 2 (49 teeth: 32 primary, 17 permanent): 2‐step caries removal: in this group, the same treatment protocols were carried out as in the previous group. Following the application of calcium hydroxide, however, cavities were sealed using reinforced zinc oxide eugenol cement (IRM, LD Caulk Division, Dentsply) for a 3‐month period. Teeth were followed every month, and the integrity of the temporary restoration was checked. After this 3‐month interval, the clinical and radiographic examinations were repeated. In the clinical examination procedure, history of pain, sensitivity to percussion and palpation, mobility, and absence or existences of fistula or oedema were recorded. The pulp sensitivity was evaluated again using a cold stimulation tester and electric pulp tester. After the rubber dam application, the temporary filling and the remaining carious dentin were removed with excavators and slowly rotating burs. Restoration as with group 1. Group 3 (55 teeth: 31 primary, 24 permanent): non‐selective caries removal: similar to group 1, while all carious dentine was removed using excavators and slowly rotating burs until hard dentin was reached or pulp exposure occurred. A caries‐free cavity was defined as one without softening in the remaining dentine upon the examination of the cavity floor with a blunt probe using moderate pressure. |
|
| Outcomes |
Primary outcome Signs or symptoms of pulpal disease: pain, clinical or radiological loss of vitality, mobility, root resorption, etc. after 12 months Secondary outcome Pulp exposure during excavation Bacteriological growth from dentine samples |
|
| Notes | Funding: The Scientific and Technological Research Council of Turkey (project no. SBAG‐AYD‐459; 104S068). | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Quote: "Teeth were randomly assigned for the treatment groups as: 1‐visit IPT; 2‐visit IPT; and DCE. For the random selection, lots were drawn by the investigator who was blinded to the treatments." |
| Allocation concealment (selection bias) | High risk | Quote: "In the 2‐visit IPT group, the operator knew there would be a second visit and wanted to reduce the pulp exposure risk; thus, she might have been more cautious while deepening the cavity during the first excavation. The randomization, however, should have been performed in 2 steps. In the first step, only DCE and IPT groups should be constituted. Then, if IPT is chosen from the first draw of lots, a new draw of lots should be made after the first excavation to decide whether it will be a 1‐ or 2‐visit procedure. If this methodology was used, there might be pulp exposures in the initial excavation of 2‐visit IPT (likewise in 1‐visit IPT)." |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Participants/dentist were aware of different number of appointments required in the 3 arms. Blinding not possible due to differences in techniques. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not possible for the outcome of pulp exposure as the operator assessed it during treatment. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised teeth included in analysis. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Phonghanyudh 2012.
| Study characteristics | ||
| Methods | RCT, parallel groups Duration of study: 12 months Setting: 2 dental hospitals in Thailand |
|
| Participants | 276 children, 276 primary teeth Age: 6–11 years Caries experience: participants with high‐risk caries (dmft > 5); ≥ 1 primary molar with caries into dentine without pulpal involvement Inclusion criteria: asymptomatic primary molars with dentinal caries (no pain, no tooth mobility, no gingival swelling); radiographically dentine caries involved ≥ 1/3 dentin; being restorable with fillings |
|
| Interventions | 3 treatment arms (we did not include group 2, the ART arm) Group 1 (92 participants, 92 teeth): partial, SE: soft carious tissues at enamel dentine junction completely removed, without further removal of carious dentin, restoration with glass ionomer cement. Group 2 (92 participants, 92 teeth): ART, non‐selective caries removal: all soft carious dentin removed and restoration with glass ionomer cement. Group 3 (92 participants, 92 teeth): non‐selective caries removal, restoration with glass ionomer cement. |
|
| Outcomes |
Primary outcome Pulpal symptoms/loss of vitality; restoration failure (loss of restoration or > 0.5 mm marginal defect or wear) after 12 months Secondary outcome Pulp exposure during excavation |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "The study was carried out in Saraburi and Suphanburi provinces, which were randomly selected from 10 provinces near Bangkok. Using multi‐stage cluster sampling, 6 primary schools were sampled with 450 schoolchildren." Comment: block randomisation not sufficiently explained. Quote: "The children were randomly allocated to the 3 study groups by children picking the ball with a group number inside, without replacement." |
| Allocation concealment (selection bias) | Low risk | Lottery method. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding of dentist not possible due to differences in techniques. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Clinical and radiological examination blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised teeth included in analysis. |
| Selective reporting (reporting bias) | Low risk | All expected outcomes reported. |
| Other bias | Low risk | No other biases detected. |
Qvist 2017.
| Study characteristics | ||
| Methods | RCT, parallel group Duration of study: 84 months Setting: 9 dental hospitals in Copenhagen |
|
| Participants | 521 children, 521 permanent teeth Age: 6–17 years, mean 11.9, SD 2.2 years ≥ 1 permanent molar with caries limited to half of the dentin without pulpal involvement Inclusion criteria: ≥ 1 occlusal lesion requiring restorative treatment clinically or radiographically assessed; radiographic depth of lesion limited to half of the dentine Exclusion criteria: the occlusal lesion had communication with an approximal caries lesion or occlusal/approximal restoration; tooth was hypomineralised; serious chronic diseases that affect caries experience and activity |
|
| Interventions | 2 treatment arms Group 1 (368 participants, 368 teeth): sealing over caries. Group 2 (153 participants, 153 teeth): composite resin restorations; extent of caries excavation not reported. |
|
| Outcomes |
Primary outcome Survival of fissure sealant until replaced by a restoration and longevity of sealants and restorations until retreatment Secondary outcome Caries progression beneath sealing or restoration |
|
| Notes | Funding: University of Copenhagen; 3M ESPE, Danish Employees Dentists Organization, Ivoclar Vivadent, Stiftelsen Patentmedelsfonden för Odontologisk Profylaxforskning and VOCO for donation of materials and/ or financial support for presentations. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Allocation sequence described in detail. Central randomisation at University of Copenhagen, sequentially numbered, sealed envelopes. |
| Allocation concealment (selection bias) | Low risk | Central randomisation at University of Copenhagen, sequentially numbered, sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Blinding was not possible." Blinding not possible – operator knew caries removal technique. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not confirmed, all teeth were restored with different materials, which probably looked different in the treatment arms. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised teeth were included in analyses. |
| Selective reporting (reporting bias) | High risk | Although all expected outcomes were reported, and the lesions were grouped into those limited to enamel and those extending into dentine in the baseline characteristics table, the results tables presented data for enamel and dentine lesions together and there was insufficient information to extract the data based on lesion extent and only include the dentine lesions that were restored. |
| Other bias | Low risk | No other biases detected. |
Ribeiro 1999.
| Study characteristics | ||
| Methods | RCT, parallel‐group Follow‐up: 24 hours, and 3, 6, 9, and 12 months Setting: secondary care (University) in Brazil |
|
| Participants | 38 children, 48 primary molars Age: 7–11 years Inclusion criteria: ≥ 1 primary molar with caries into dentine without pulpal involvement, due to exfoliate in approximately 1 year; no radiographic signs of pulp pathology; physiological root resorption initiated or expected within 1 year |
|
| Interventions | 2 treatment arms Group 1 (24 teeth): SE: complete removal of carious tissue from the dentino‐enamel; soft carious dentine was intentionally left in the cavity junction, carious tissue from the pulpal/axial walls was left. Resin composite restoration (Scotchbond Multi‐Purpose, 3M, Seefeld; Z100, 3M). Group 2 (24 teeth): non‐selective caries removal: caries detecting solution was used. All identified irreversibly infected dentin was removed with a number 2 low‐speed round bur. Resin composite restoration (Scotchbond Multi‐Purpose, 3M, Seefeld; Z100, 3M). |
|
| Outcomes |
Primary outcome Restoration success measured clinically Retention: modification of the criteria introduced by Houpt 1994 was used as follows: score 0, no loss of the restoration; 1, partial loss of the restoration or 2 total loss of the restoration. Marginal integrity: marginal adaptation was evaluated directly by visual inspection ≥ 1 year after the restorations had been placed. Clinical findings (sign or symptoms, or both) of pulpal injury or any other problem with the restoration (or both). Pain or discomfort reported by the participants or their parents was also recorded on this form. If a restoration had to be removed, it was considered a failure. Caries progression: radiographically (periapical radiographs) progression of the radiolucent area in the experimental group (group 2). Histological using SEM: caries progression. |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomisation method not explained. The teeth were randomly assigned to 1 of 2 clinical procedures. |
| Allocation concealment (selection bias) | Unclear risk | No information about when operator was informed of treatment arm. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | No blinding; operator knew differences in the techniques. |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Blinding not confirmed, although all teeth were restored with the same materials. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised teeth included in analysis. |
| Selective reporting (reporting bias) | High risk | Participants were given forms to report on discomfort and perceptions of treatment but this was not reported on. |
| Other bias | Low risk | No other biases detected. |
Santamaria 2018.
| Study characteristics | ||
| Methods | RCT, parallel group Duration of study: 2.5 years Setting: Department for Preventive and Paediatric Dentistry of Greifswald University, Germany |
|
| Participants | 169 children Age: 3–8 years; mean 5.6, SD 1.5 years Caries experience: d3mft, 5.96 HT, 5.58 NRCC, 5.34 CR Inclusion criteria: children aged 3–8 years, a primary molar with an occluso‐proximal, surface caries lesion at the dentine level (ICDAS score 3–5), no clinical or radiographic signs or symptoms of pulpal or periradicular pathology, no systemic diseases that required special considerations for dental treatment and willingness to participate. Only 1 tooth per child was included in the study. |
|
| Interventions | 3 treatment arms Group 1 (52 participants, 52 teeth): HT: no local anaesthesia, no caries removal, use of SSC cemented with luting cement. If the contact points were tight, orthodontic separator elastics were inserted and left in place for 2–3 days before placement of the crown at the next appointment. For HT, the participants underwent routine dental check‐ups twice per year. Group 2 (52 participants, 52 teeth): NRCT: the lesions were opened using a high‐speed bur removing the overhanging enamel to make the cavity accessible for plaque removal. The residual biofilm on the cavity was cleaned using a rotary bristle brush, and 22,600‐ppm fluoride varnish (Duraphat, GABA, Lörrach, Germany) was applied. Site‐specific toothbrushing instructions were given to parents/children using a bucco‐lingual technique and this was followed up with reinforcement of diet and oral hygiene instruction. For the NRCT arm, children were asked to attend every 3 months to monitor the lesion status and to reinforce dietary and oral hygiene advice to assist the caries arrest process, including Duraphat application on clinically active carious lesions. Group 3 (65 participants, 65 teeth): CR: non‐selective caries removal and compomer restorations. Local anaesthesia was used when needed. A high‐speed handpiece was used to gain access to the lesion; peripheral caries was removed with a slow handpiece and an excavator to cleave away the carious dentine from the pulpal wall. A matrix band and a porta‐matrix (Henry Schein Inc, Melville, NY, USA) or a T‐Band (Pulpdent, Watertown, MA, USA), and a wedge (Interdental Wedge, Kerr, Bioggio, Switzerland) were used to restore the cavities. All cavities were restored with Compomer (Dyract, Dentsply, Konstanz, Germany). For the CR arm, the participants underwent routine dental check‐ups twice per year. |
|
| Outcomes |
Primary outcome Failures (minor and major) at 2.5 years; minor failure (reversible pulpitis, caries progression, or secondary caries), major failure (irreversible pulpitis, abscess, unrestorable tooth) Secondary outcome Survival at 2.5 years without any minor and major failure event Gingival and Plaque Index at 1 year, Plaque Index: 0 = no plaque, 1 = thin visible plaque, 2 = thick visible plaque. Gingival Index: 0 = no swelling, 1 = mild swelling, 2 = moderate‐to‐severe gingival swelling. Child's behaviour during the operative session was assessed by the dentists using the Frankl Behavior Rating Scale. This 4‐point scale ranges from definitely negative behaviour, when the child refuses the treatment, cry, etc. definitely positive behaviour, when the child is completely co‐operative. Pain: 5‐point scale includes 5 faces of children representing from very light to very intense pain. Children were asked to select the face that represents how he/she felt during treatment. Treatment perceptions and opinions: 5‐point Likert scales were used to assess parent's perceptions of their child's behaviour, comfort during treatment and satisfaction with treatment undertaken and dentist's ease of treatment provision/material, participant's discomfort and the relative time for the procedure. Parents were also asked whether they would choose the same treatment option again, and dentists were asked which treatment option, out with the study, they would have chosen for that tooth. Parent's perception of child behaviour and comfort |
|
| Notes | Schwendicke 2018 (see under Santamaria 2014) represents an analysis of Santamaria 2017, regarding cost‐effectiveness. Funding: Department for Preventive and Paediatric Dentistry of Greifswald University, Germany. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | A computer‐generated random number list with allocation concealment was used to assign children to 1 of 3 arms: HT, NRCT and CR. |
| Allocation concealment (selection bias) | Unclear risk | A computer‐generated random number list with allocation concealment was used to assign children to 1 of 3 arms: HT, NRCT and CR. Method not described in detail. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Personnel and participants could not be blinded as treatments were different. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not mentioned. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Reasons for attrition explained in CONSORT table; associated with moving away or failed to return. Dropout analyses showed no statistically significant differences between dropout cases and participants for mean age (P = 0.90), gender distribution (P = 0.49), d3mft values (P = 0.74), ICDAS score (P = 0.91), type of treated tooth (first or second primary molar, P = 0.32), or type of treatment (P = 0.93). In 5 cases (HT = 3; CR = 2), parents/children who did not attend recalls were reached by telephone. |
| Selective reporting (reporting bias) | Low risk | All data outcomes reported. |
| Other bias | Low risk | No other biases detected. |
ART: atraumatic restorative treatment; CR: conventional restoration; DCE: dental continuing education; dmft: decayed, missed, filled teeth primary teeth; DMFT: decayed, missed, filled teeth permanent teeth; HT: Hall Technique; ICDAS: International Caries Detection and Assessment System; IPT: indirect pulp therapy; MCRL: minimal caries removal with only resin‐modified glass ionomer luting cement; MCRB/L: minimal caries removal with both resin‐modified glass ionomer base material and luting cement; NRCC: non‐restorative cavity control; NRCT: non‐restorative caries treatment; OHRQoL: Oral Health‐related Quality of Life; OVD: occlusal vertical dimension; PCR: partial caries removal; PDL: periodontal ligament; PMC: preformed metal crown; RCT: randomised controlled trial; RMGI: resin‐modified glass ionomer; RMGIC: resin‐modified glass ionomer cement; SD: standard deviation; SE: selective excavation; SEM: scanning electron microscope; SSC: stainless steel crown; SW: stepwise caries removal; USPHS: United States Public Health Service.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ali 2018 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Alkilzy 2011 | The measured outcomes were not reported individually for each of the investigated caries depths (ICDAS: D1–D3). |
| Alkilzy 2018 | Not comparing 2 different levels of caries removal/control. |
| Allen 2005 | Not comparing 2 different levels of caries removal/control. |
| Ammari 2014 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Anauate‐Netto 2017 | Not comparing 2 different levels of caries removal. |
| Anusavice 1987 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal, which aimed to completely remove carious tissue. |
| Arrow 2015 | Not comparing 2 different levels of caries removal/control. |
| Aswathi 2017 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal, which aimed to completely remove carious tissue. Did not report clinical outcomes. |
| Azrak 2004 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Bakhshandeh 2015 | Not comparing 2 different levels of caries removal/control. All minimal preparation. |
| Balciuniene 2005 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Barata 2008 | Compared complete caries removal in both groups. |
| Bergmann 2005 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Bianchi 1989 | Compared complete caries removal in both groups. |
| Bohari 2012 | Compared complete caries removal in both groups. |
| Braga 2009 | Not comparing 2 different levels of caries removal/control. All minimal preparation. |
| Bressani 2013 | Compared complete caries removal in both groups. |
| Calderari 1989 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Cavel 1988 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal which aimed to completely remove carious tissue. |
| Chomyszyn‐Gajewska 2006 | Compared complete caries removal in both groups. |
| de Almeida 2013 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal which aimed to completely remove carious tissue. Did not report clinical outcomes. |
| Dülgergil 2005 | Not comparing 2 methods of caries removal/control. |
| Ekstrand 2010 | Not comparing 2 methods of caries removal/control. |
| El‐Tekeya 2012 | Did not report clinical outcomes. |
| Flório 2001 | Enamel caries only. Compared fissure sealants with fluoride application, no caries removal/control. |
| Foley 2003 | Did not report clinical outcomes. |
| Fure 2000 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Gibson 1980 | The measured outcomes were not reported individually for each of the investigated caries depths. |
| Giza 2007 | Compared complete caries removal for both groups. |
| Goyal 2015 | Compared complete caries removal for both groups. |
| Hamilton 2001 | Complete caries removal using air abrasion. |
| Handelman 1976 | Not comparing 2 different levels of caries removal/control. |
| Hassan 2016 | Did not report clinical outcomes. |
| Heinrich 1988 | No clinical outcomes. Only histological. |
| Hoefler 2016 | Not a clinical trial. A systematic review. |
| Hosein 2008 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Kakaboura 2003 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Kalf‐Scholte 2003 | Compared complete caries removal for all groups. |
| Kavvadia 2004 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Kirzioglu 2007 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Kochhar 2011 | Compared complete caries removal for all groups. |
| Kotb 2009 | Compared complete caries removal for all groups. |
| Lager 2003 | Did not report clinical outcomes. |
| Lakshmi 2018 | Not comparing 2 different levels of caries removal/control. |
| Lozano‐Chourio 2006 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Maguire 2020 | For trial arms, "conventional management of decay, with best‐practice prevention" could be considered as complete carious tissue removal from the protocol, "biological management of decay, with best‐practice prevention" equivalent to sealing in strategies as this arm included fissure sealing over carious lesions and the Hall Technique and "best‐practice prevention alone" also involved no caries removal. However, each arm involved a variety of techniques and there was no information on the extent of the carious lesions prior to each treatment. Randomisation was carried out at 'person' level rather than 'tooth' level and there were no tooth specific data either for results of interventions as all outcomes were expressed as per person. Tooth data were clustered and it was not possible to discern which teeth had received which individual type of treatment and what the outcome was for individual treatment items. |
| Malmström 2003 | Complete caries removal using air abrasion. |
| Maltz 2012 | Did not report clinical outcomes. |
| Mandari 2001 | Compared complete caries removal for all groups. |
| Maragakis 2001 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Martignon 2012 | Not comparing 2 different levels of caries removal/control. |
| Matsumoto 2013 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Carisolv) which aimed to completely remove carious tissue. |
| Moreira 2017 | Not comparing 2 different levels of caries removal/control. |
| Motta 2013 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Papacarie) which aimed to completely remove carious tissue. |
| Muñoz‐Sandoval 2019 | Not comparing 2 different levels of caries removal/control. |
| Nadanovsky 2001 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal which aimed to completely remove carious tissue. |
| Pandit 2007 | Compared complete caries removal for all groups. |
| Peric 2009 | Compared complete caries removal for all groups. |
| Peters 2006 | Conference proceeding. Abstract only – no full text available. |
| Rios Caro 2012 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal (Papacarie) which aimed to completely remove carious tissue. |
| Ruff 2018 | Not comparing 2 different levels of caries removal/control. |
| Santamaria 2014 | Not a clinical trial. A commentary. |
| Sarmadi 2018 | Compared complete caries removal for all groups. |
| Straffon 1988a | Not comparing 2 different levels of caries removal/levels. |
| Straffon 1988b | Not comparing 2 different levels of caries removal/control. |
| Taifour 2003 | Compared complete caries removal for all groups. |
| Tavciovski 1966 | Full‐text was not retrievable. |
| Thompson 2015 | It was stated that the trial was halted. |
| Valério 2016 | Compared complete caries removal for all groups. |
| Wang 2007 | Compared complete caries removal for all groups. |
| Welbury 1990 | Compared complete caries removal for all groups. |
| Zakirulla 2012 | Not reporting clinical outcomes. |
| Zinck 1988 | Both complete caries removal. Compared complete caries removal with chemomechanical caries removal which aimed to completely remove carious tissue. |
ICDAS: International Caries Detection and Assessment System.
Characteristics of ongoing studies [ordered by study ID]
Vicioni‐Marques 2018.
| Study name | Comparison of three restorative protocols in teeth with molar‐incisor hipomineralization (MIH): a randomized controlled clinical study |
| Methods | Randomised clinical trial |
| Participants | Children aged 6–10 years ≥ 1 permanent first molar with occlusal surface with severe MIH grade (with posteruptive enamel fracture and dentin exposure), it may not be reported hypersensitivity in the selected tooth. |
| Interventions | 3 experimental arms Group 1: temporary restoration with glass ionomer (Equia Forte; GC Corporation, Tokyo, Japan) for 30 days + restoration in composite resin (Filtek Resin Z350 XT; 3M Corporate Headquarters, St Paul, USA) Group 2: restoration with composite resin (Filtek Resin Z350 XT) Group 3: composite resin restoration (Filtek Resin Z350 XT) + application of diode laser |
| Outcomes | Primary outcomes
Secondary outcomes
|
| Starting date | 2018 |
| Contact information | Fernanda Vicioni Marques, PhD student. Tel: +55 16 999936791. E‐mail: fernanda.vicioni.marques@usp.br. |
| Notes |
MIH: molar‐incisor hypomineralisation.
Differences between protocol and review
The differences between the protocol and review largely pertain to subgroup and network meta‐analysis.
The most relevant difference is the change in primary outcome: we had originally planned to exclude minor complications, which also is a composite measure including, for example, restoration loss treated by re‐restoration, or partial restoration failure treated by repair (Innes 2011). Given that most studies did not report complications in such degree of granularity, our primary outcome was changed to failure. Notably, failure pools a range of outcomes with different importance to different stakeholders; this should be considered when interpreting our findings, but was the common denominator allowing useful synthesis.
Moreover, a range of subgroup and stratified analyses had been planned; given the availability of data, not all of them were and could be conducted, as outlined in the Methods section.
Last, we had planned network meta‐analyses for all subgroups and lesion depths, that is, indications. Given limited comparability across studies, we refrained from this for most indications and only performed network meta‐analysis for interventions on deep lesions.
If multiple records of the same study were available, we extracted data from the last time point. We had originally planned to extract data from all time points.
Further smaller deviations are noted in the Methods section.
Contributions of authors
Protocol
FS and NI conceived, designed and wrote the review.
TW wrote the Methods section of the protocol.
MF, LB, JEC, TL, CL, GG, RMS and DR revised the protocol.
Review
FS and NI selected studies.
FS, NI, TL, MF, LB, JGR, GG, CL, AM, DR and RMS extracted data.
FS, NI and TW analysed data.
FS, NI and TL wrote the review.
All authors read, revised and agreed to the manuscript.
Sources of support
Internal sources
The University of Manchester, Manchester Academic Health Sciences Centre (MAHSC) and National Institute for Health Research (NIHR) Manchester Biomedical Research Centre, UK
External sources
-
National Institute for Health Research (NIHR), UK
This project was supported by the NIHR, via Cochrane Infrastructure funding to Cochrane Oral Health. The views and opinions expressed herein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, the NIHR, the National Health Service or the Department of Health.
-
Cochrane Oral Health Global Alliance, Other
The production of Cochrane Oral Health reviews has been supported financially by our Global Alliance since 2011 (oralhealth.cochrane.org/partnerships-alliances). Contributors over recent years have been the American Association of Public Health Dentistry, USA; AS‐Akademie, Germany; the British Association for the Study of Community Dentistry, UK; the British Society of Paediatric Dentistry, UK; the Canadian Dental Hygienists Association, Canada; the Centre for Dental Education and Research at All India Institute of Medical Sciences, India; the National Center for Dental Hygiene Research & Practice, USA; New York University College of Dentistry, USA; and NHS Education for Scotland, UK; Swiss Society of Endodontology, Switzerland.
Declarations of interest
FS: none.
TW: none. I am Statistical Editor with Cochrane Oral Health.
TL: none. I am an Editor with Cochrane Oral Health.
WA: none.
LB: none.
JEC: none. I am a Co‐ordinating Editor with Cochrane Oral Health.
MF: in the last 36 months, I have received grant support from the National Institutes for Health (NIH), the Delta Dental Foundation, DentaQUest, Colgate; have served as a grant reviewer for NIH; have consulted for 3M, DentaQuest; served as part of the National Scientific Advisory Committee for Delta Dental Foundation; and been a member of the Council for Scientific Affairs of the American Dental Association.
JGR: none.
GG: none.
CL: none.
AM: none.
DR: none.
MR: none.
RMS: none.
NPI: none.
New
References
References to studies included in this review
Alves 2017 {published data only}
- Alves LS, Giongo FC, Mua B, Martins VB, Barbachan E Silva B, Qvist V, et al. A randomized clinical trial on the sealing of occlusal carious lesions: 3–4-year results. Brazilian Oral Research 2017;31:E44. [DOI: 10.1590/1807-3107BOR-2017.vol31.0044] [PMID: ] [DOI] [PubMed] [Google Scholar]
Araujo 2020 {published data only}
- Araujo MP, Innes NP, Bonifacio CC, Hesse D, Olegario IC, Mendes FM, et al. Atraumatic restorative treatment compared to the Hall Technique for occluso-proximal carious lesions in primary molars; 36-month follow-up of a randomised control trial in a school setting. BMC Oral Health 2020;20(1):318. [DOI: 10.21203/rs.3.rs-31623/v2] [WEB: www.researchsquare.com/article/rs-31623/v2] [DOI] [PMC free article] [PubMed]
- Hesse D, Araujo MP, Olegário IC, Innes N, Raggio DP, Bonifácio CC. Atraumatic restorative treatment compared to the Hall Technique for occluso-proximal cavities in primary molars: study protocol for a randomized controlled trial. Trials 2016;17(169):1-13. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjørndal 2017 {published data only}
- Bjørndal L, Fransson H, Bruun G, Markvart M, Kjældgaard M, Näsman P, et al. Randomized clinical trials on deep carious lesions: 5-year follow-up. Journal of Dental Research 2017;96(7):747-53. [DOI: 10.1177/0022034517702620] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Bjørndal L, Reit C, Bruun G, Markvart M, Kjaeldgaard M, Näsman P, et al. Treatment of deep caries lesions in adults: randomized clinical trials comparing stepwise vs. direct complete excavation, and direct pulp capping vs. partial pulpotomy. European Journal of Oral Sciences 2010;118(3):290-7. [DOI: 10.1111/j.1600-0722.2010.00731.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Borges 2012a {published data only}
- Borges BC, De Souza Bezerra Araújo RF, Dantas RF, De Araújo Lucena A, De Assunção Pinheiro IV. Efficacy of a non-drilling approach to manage non-cavitated dentin occlusal caries in primary molars: a 12-month randomized controlled clinical trial. International Journal of Paediatric Dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children 2012;22(1):44-51. [DOI: 10.1111/j.1365-263X.2011.01156.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Borges 2012b {published data only}
- Borges BC, Campos GB, da Silveira AD, Lima KC, Pinheiro IV. Efficacy of a pit and fissure sealant in arresting dentin non-cavitated caries: a 1-year follow-up, randomized, single-blind, controlled clinical trial. American Journal of Dentistry 2010;23(6):311-6. [PMID: ] [PubMed] [Google Scholar]
- Borges BC, Souza Borges J, Braz R, Montes MA, Assunção Pinheiro IV. Arrest of non-cavitated dentinal occlusal caries by sealing pits and fissures: a 36-month, randomised controlled clinical trial. International Dental Journal 2012;62(5):251-5. [DOI: 10.1111/j.1875-595X.2012.00117.x] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Boyd 2021 {published data only}
- Boyd DH, Thomson WM, Leon de la Barra S, Fuge KN, den Heever R, Butler BM, et al. A primary care randomized controlled trial of Hall and conventional restorative techniques. JDR Clinical & Translational Research 2021;6(2):205-12. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chompu‐inwai 2015 {published data only}
- Chompu-inwai P, Boonsongsawat K, Sastraruji T, Sophasri T, Mankaen S, Nondon S, et al. Three incomplete caries removal techniques compared over two years in primary molars with asymptomatic deep caries or reversible pulpitis. Pediatric Dentistry 2015;37(5):41-8. [PMID: ] [PubMed] [Google Scholar]
da Silveira 2012 {published data only}
- da Silveira AD, Borges BC, Almeida Varela H, Lima KC, Pinheiro IV. Progression of non-cavitated lesions in dentin through a nonsurgical approach: a preliminary 12-month clinical observation. European Journal of Dentistry 2012;6(1):34-42. [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Dias 2018 {published data only}
- Dias KR, Andrade CB, Wait TT, Chamon R, Ammari MM, Soviero VM, et al. Efficacy of sealing occlusal caries with a flowable composite in primary molars: a 2-year randomized controlled clinical trial. Journal of Dentistry 2018;74:49-55. [DOI: 10.1016/j.jdent.2018.05.014] [PMID: ] [DOI] [PubMed] [Google Scholar]
Elhennawy 2021 {published data only}
- Elhennawy K, Finke C, Paris S, Reda R, Jost-Brinkmann PG, Schwendicke F. Selective vs stepwise removal of deep carious lesions in primary molars: 24 months follow-up from a randomized controlled trial. Clinical Oral Investigations 2021;25(2):645-52. [DOI: 10.1007/s00784-020-03536-6] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhennawy K, Finke C, Paris S, Reda S, Jost-Brinkmann PG, Schwendicke F. Selective vs stepwise removal of deep carious lesions in primary molars: 12-months results of a randomized controlled pilot trial. Journal of Dentistry 2018;77:72-7. [DOI: 10.1016/j.jdent.2018.07.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
Foley 2004 {published data only}
- Foley J, Evans D, Blackwell A. Partial caries removal and cariostatic materials in carious primary molar teeth: a randomised controlled clinical trial. British Dental Journal 2004;197(11):697-701; discussion 689. [DOI: 10.1038/sj.bdj.4811865] [PMID: ] [DOI] [PubMed] [Google Scholar]
Franzon 2014 {published data only}
- Franzon R, Guimarães LF, Magalhães CE, Haas AN, Araujo FB. Outcomes of one-step incomplete and complete excavation in primary teeth: a 24-month randomized controlled trial. Caries Research 2014;48(5):376-83. [DOI: 10.1159/000357628] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Franzon R, Opdam NJ, Guimarães LF, Demarco FF, Casagrande L, Haas AN, et al. Randomized controlled clinical trial of the 24-months survival of composite resin restorations after one-step incomplete and complete excavation on primary teeth. Journal of Dentistry 2015;43(10):1235-41. [DOI: 10.1016/j.jdent.2015.07.011] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Liberman J, Franzon R, Guimarães LF, Casagrande L, Haas AN, Araujo FB. Survival of composite restorations after selective or total caries removal in primary teeth and predictors of failures: a 36-months randomized controlled trial. Journal of Dentistry 2020;93:103268. [DOI] [PubMed] [Google Scholar]
Hesse 2014 {published data only}
- Hesse D, Bonifácio CC, Mendes FM, Braga MM, Imparato JC, Raggio DP. Sealing versus partial caries removal in primary molars: a randomized clinical trial. BMC Oral Health 2014;14:58. [DOI: 10.1186/1472-6831-14-58] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Innes 2011 {published data only}
- Innes N, Stewart M, Souster G, Evans D. The Hall Technique; retrospective case-note follow-up of 5-year RCT. British Dental Journal 2015;219(8):395-400. [DOI: 10.1038/sj.bdj.2015.816] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Innes NP, Evans DJ, Stirrups DR. Sealing caries in primary molars: Hall Technique RCT 5-year results. In: International Association of Dental Research (IADR); 2010 July 14-17; Barcelona, Spain. 2010.
- Innes NP, Evans DJ, Stirrups DR. Sealing caries in primary molars: randomized control trial, 5-year results. Journal of Dental Research 2011;90(12):1405-10. [DOI: 10.1177/0022034511422064] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Innes NP, Evans DJ, Stirrups DR. The Hall Technique; a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice: acceptability of the technique and outcomes at 23 months. BMC Oral Health 2007;7:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwendicke F, Krois J, Robertson M, Splieth C, Santamaria R, Innes N. Cost-effectiveness of the Hall Technique in a randomized trial. Journal of Dental Research 2019;98(1):61-7. [DOI: 10.1177/0022034518799742] [PMID: ] [DOI] [PubMed] [Google Scholar]
Khokhar 2018 {published data only}
- Khokhar M, Tewari S. Outcomes of partial and complete caries excavation in permanent teeth: a 18 month clinical study. Contemporary Clinical Dentistry 2018;9(3):468-473. [DOI: 10.4103/ccd.ccd_344_18] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Labib 2019 {published data only}
- Labib ME, Hassanein OE, Moussa M, Yassen A, Schwendicke F. Selective versus stepwise removal of deep carious lesions in permanent teeth: a randomised controlled trial from Egypt – an interim analysis. BMJ Open 2019;9(9):e030957. [DOI: 10.1136/bmjopen-2019-030957] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leksell 1996 {published data only}
- Leksell E, Ridell K, Cvek M, Mejàre I. Pulp exposure after stepwise versus direct complete excavation of deep carious lesions in young posterior permanent teeth. Endodontics & Dental Traumatology 1996;12(4):192-6. [DOI: 10.1111/j.1600-9657.1996.tb00513.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lula 2009 {published data only}
- Lula EC, Monteiro-Neto V, Alves CM, Ribeiro CC. Microbiological analysis after complete or partial removal of carious dentin in primary teeth: a randomized clinical trial. Caries Research 2009;43(5):354-8. [DOI: 10.1159/000231572] [PMID: ] [DOI] [PubMed] [Google Scholar]
Magnusson 1977 {published data only}
- Magnusson BO, Sundell SO. Stepwise excavation of deep carious lesions in primary molars. Journal of the International Association of Dentistry for Children 1977;8(2):36-40. [PMID: ] [PubMed] [Google Scholar]
Maltz 2018 {published data only}
- Jardim JJ, Mestrinho HD, Koppe B, Paula LM, Alves LS, Yamaguti PM, et al. Restorations after selective caries removal: 5-year randomized trial. Journal of Dentistry 2020;99:10341. [DOI] [PubMed] [Google Scholar]
- Maltz M, Garcia R, Jardim JJ, Paula LM, Yamaguti PM, Moura MS, et al. Randomized trial of partial vs. stepwise caries removal: 3-year follow-up. Journal of Dental Research 2012;91(11):1026-31. [DOI] [PubMed] [Google Scholar]
- Maltz M, Jardim JJ, Mestrinho HD, Yamaguti PM, Podestá K, Moura MS, et al. Partial removal of carious dentine: a multicenter randomized controlled trial and 18-month follow-up results. Caries Research 2013;47(2):103-9. [DOI: 10.1159/000344013] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Maltz M, Koppe B, Jardim JJ, Alves LS, Paula LM, Yamaguti PM, et al. Partial caries removal in deep caries lesions: a 5-year multicenter randomized controlled trial. Clinical Oral Investigations 2018;22(3):1337-43. [DOI] [PubMed] [Google Scholar]
Mello 2018 {published data only}
- Mello B, Stafuzza CT, Vitor L, Rios D, Silva T, Machado M, et al. Evaluation of dentin-pulp complex response after conservative clinical procedures in primary teeth. International Journal of Clinical Pediatric Dentistry 2018;11(3):188-92. [DOI: 10.5005/jp-journals-10005-1509] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mertz‐Fairhurst 1998 {published data only}
- Mertz-Fairhurst EJ, Adair SM, Sams DR, Curtis JW Jr, Ergle JW, Hawkins KI, et al. Cariostatic and ultraconservative sealed restorations: nine-year results among children and adults. ASDC Journal of Dentistry for Children 1995;62(2):97-107. [PMID: ] [PubMed] [Google Scholar]
- Mertz-Fairhurst EJ, Call-Smith KM, Shuster GS, Williams JE, Davis QB, Smith CD, et al. Clinical performance of sealed composite restorations placed over caries compared with sealed and unsealed amalgam restorations. Journal of the American Dental Association (1939) 1987;115(5):689-94. [DOI: 10.14219/jada.archive.1987.0288] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mertz-Fairhurst EJ, Curtis JW Jr, Ergle JW, Rueggeberg FA, Adair SM. Ultraconservative and cariostatic sealed restorations: results at year 10. Journal of the American Dental Association (1939) 1998;129(1):55-66. [DOI: 10.14219/jada.archive.1998.0022] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mertz-Fairhurst EJ, Smith CD, Williams JE, Sherrer JD, Mackert JR Jr, Richards EE, et al. Cariostatic and ultraconservative sealed restorations: six-year results. Quintessence International 1992;23(12):827-38. [PMID: ] [PubMed] [Google Scholar]
- Mertz-Fairhurst EJ, Williams JE, Schuster GS, Smith CD, Pierce KL, Mackert JR Jr, et al. Ultraconservative sealed restorations: three-year results. Journal of Public Health Dentistry 1991;51(4):239-50. [DOI: 10.1111/j.1752-7325.1991.tb02222.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Orhan 2010 {published data only}
- Orhan AI, Oz FT, Orhan K. Pulp exposure occurrence and outcomes after 1- or 2-visit indirect pulp therapy vs complete caries removal in primary and permanent molars. Pediatric Dentistry 2010;32(4):347-55. [PMID: ] [PubMed] [Google Scholar]
Phonghanyudh 2012 {published data only}
- Phonghanyudh A, Phantumvanit P, Songpaisan Y, Petersen PE. Clinical evaluation of three caries removal approaches in primary teeth: a randomised controlled trial. Community Dental Health 2012;29(2):173-8. [PMID: ] [PubMed] [Google Scholar]
Qvist 2017 {published data only}
- Qvist V, Borum MK, Møller KD, Andersen TR, Blanche P, Bakhshandeh A. Sealing occlusal dentin caries in permanent molars: 7-year results of a randomized controlled trial. JDR Clinical and Translational Research 2017;2(1):73-86. [DOI: 10.1177/2380084416680191] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ribeiro 1999 {published data only}
- Ribeiro CC, Baratieri LN, Perdigão J, Baratieri NM, Ritter AV. A clinical, radiographic, and scanning electron microscopic evaluation of adhesive restorations on carious dentin in primary teeth. Quintessence International 1999;30(9):591-9. [PMID: ] [PubMed] [Google Scholar]
Santamaria 2018 {published data only}
- NCT01797458. Randomised control trial on three different approaches to managing class 2 cavities in primary teeth. clinicaltrials.gov/ct2/show/NCT01797458 (first received 22 February 2013). [CLINICALTRIALS.GOV IDENTIFIER: NCT01797458]
- Santamaría RM, Innes NP, Machiulskiene V, Schmoeckel J, Alkilzy M, Splieth CH. Alternative caries management options for primary molars: 2.5-year outcomes of a randomised clinical trial. Caries Research 2018;51(6):605-14. [DOI: 10.1159/000477855] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Santamaria RM, Innes NP, Machiulskiene V, Evans DJ, Alkilzy M, Splieth CH. Acceptability of different caries management methods for primary molars in a RCT. International Journal of Paediatric Dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children 2015;25(1):9-17. [DOI: 10.1111/ipd.12097] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Santamaria RM, Innes NP, Machiulskiene V, Evans DJ, Splieth CH. Caries management strategies for primary molars: 1-yr randomized control trial results. Journal of Dental Research 2014;93(11):1062-9. [DOI: 10.1177/0022034514550717] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwendicke F, Krois J, Splieth CH, Innes N, Robertson M, Schmoeckel J, et al. Cost-effectiveness of managing cavitated primary molar caries lesions: a randomized trial in Germany. Journal of Dentistry 2018;78:40-5. [DOI: 10.1016/j.jdent.2018.05.022] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ali 2018 {published data only}
- Ali AH, Koller G, Foschi F, Andiappan M, Bruce KD, Banerjee A, et al. Self-limiting versus conventional caries removal: a randomized clinical trial. Journal of Dental Research 2018;97(11):1207-13. [DOI: 10.1177/0022034518769255] [DOI] [PubMed] [Google Scholar]
Alkilzy 2011 {published data only}
- Alkilzy M, Berndt C, Splieth CH. Sealing proximal surfaces with polyurethane tape: three-year evaluation. Clinical Oral Investigations 2011;15(6):879-84. [DOI: 10.1007/s00784-010-0457-z] [DOI] [PubMed] [Google Scholar]
Alkilzy 2018 {published data only}
- Alkilzy M, Tarabaih A, Santamaria RM, Splieth CH. Self-assembling peptide P11-4 and fluoride for regenerating enamel. Journal of Dental Research 2018;97(2):148-54. [DOI: 10.1177/0022034517730531] [DOI] [PMC free article] [PubMed] [Google Scholar]
Allen 2005 {published data only}
- Allen KL, Salgado TL, Janal MN, Thompson VP. Removing carious dentin using a polymer instrument without anesthesia versus a carbide bur with anesthesia. Journal of the American Dental Association 2005;136(5):643-51. [DOI: 10.14219/jada.archive.2005.0237] [DOI] [PubMed] [Google Scholar]
Ammari 2014 {published data only}
- Ammari MM, Moliterno LF, Hirata R Jr, Séllos MC, Soviero VM, Coutinho Filho WP. Efficacy of chemomechanical caries removal in reducing cariogenic microbiota: a randomized clinical trial. Brazilian Oral Research 2014;28:1-6. [DOI: 10.1590/1807-3107bor-2014.vol28.0031] [DOI] [PubMed] [Google Scholar]
Anauate‐Netto 2017 {published data only}
- Anauate-Netto C, Neto LB, Amore R, DI Hipólito V, D'Alpino PH. Caries progression in non-cavitated fissures after infiltrant application: a 3-year follow-up of a randomized controlled clinical trial. Journal of Applied Oral Science 2017;25(4):442-54. [DOI: 10.1590/1678-7757-2016-0633] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anusavice 1987 {published data only}
- Anusavice KJ, Kincheloe JE. Comparison of pain associated with mechanical and chemomechanical removal of caries. Journal of Dental Research 1987;66(11):1680-3. [DOI: 10.1177/00220345870660111501] [DOI] [PubMed] [Google Scholar]
Arrow 2015 {published data only}
- Arrow P, Klobas E. Minimum intervention dentistry approach to managing early childhood caries: a randomized control trial. Community Dentistry and Oral Epidemiology 2015;3(6):511-20. [DOI: 10.1111/cdoe.12176] [PMID: ] [DOI] [PubMed] [Google Scholar]
Aswathi 2017 {published data only}
- Aswathi KK, Rani SP, Athimuthu A, Prasanna P, Patil P, Deepali KJ. Comparison of efficacy of caries removal using polymer bur and chemomechanical caries removal agent: a clinical and microbiological assessment – an in vivo study. Journal of Indian Society Pedodontics and Preventive Dentistry 2017;35(1):6. [DOI: 10.4103/0970-4388.199232] [DOI] [PubMed] [Google Scholar]
Azrak 2004 {published data only}
- Azrak B, Callaway A, Grundheber A, Stender E, Willershausen B. Comparison of the efficacy of chemomechanical caries removal (Carisolv‘) with that of conventional excavation in reducing the cariogenic flora. International Journal of Paediatric Dentistry 2004;14(3):182-91. [DOI] [PubMed] [Google Scholar]
Bakhshandeh 2015 {published data only}
- Bakhshandeh A, Ekstrand K. Infiltration and sealing versus fluoride treatment of occlusal caries lesions in primary molar teeth. 2–3 years results. International Journal of Paediatric Dentistry 2015;25(1):43-50. [DOI] [PubMed] [Google Scholar]
Balciuniene 2005 {published data only}
- Balciuniene I, Sabalaite R, Juskiene I. Chemomechanical caries removal for children. Stomatologija 2005;7(2):40-4. [PubMed] [Google Scholar]
Barata 2008 {published data only}
- Barata TJ, Bresciani E, Mattos MC, Lauris JR, Ericson D, Navarro MF. Comparison of two minimally invasive methods on the longevity of glass ionomer cement restorations: short-term results of a pilot study. Journal of Applied Oral Science 2008;16(2):155-60. [DOI: 10.1590/s1678-77572008000200014] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bergmann 2005 {published data only}
- Bergmann J, Leitão J, Kultje C, Bergmann D, Clode MJ. Removing dentine caries in deciduous teeth with Carisolv: a randomised, controlled, prospective study with six-month follow-up, comparing chemomechanical treatment with drilling. Oral Health Preventive Dentistry 2005;3(2):105-11. [PubMed] [Google Scholar]
Bianchi 1989 {published data only}
- Bianchi S, Ciuffreda M, Poggio C, Piacentini C, Paroli R. The Caridex system for removal of dental caries. Clinical trial [Sistema Caridex per la rimozione della caries. Sperimentazione clinica]. Dental Cadmos 1989;57(12):46-52. [PubMed] [Google Scholar]
Bohari 2012 {published data only}
- Bohari MR, Chunawalla YK, Ahmed BM. Clinical evaluation of caries removal in primary teeth using conventional chemomechanical and laser technique: an in vivo study. Journal of Contemporary Dental Practice 2012;13(1):40-7. [DOI: 10.5005/jp-journals-10024-1093] [DOI] [PubMed] [Google Scholar]
Braga 2009 {published data only}
- Braga MM, Mendes FM, De Benedetto MS, Imparato JC. Effect of silver diamine fluoride on incipient caries lesions in erupting permanent first molars: a pilot study. Journal of Dentistry for Children (Chicago, Ill.) 2009;76(1):28-33. [PubMed] [Google Scholar]
Bressani 2013 {published data only}
- Bressani AE, Mariath AA, Haas AN, Garcia-Godoy F, Araujo FB. Incomplete caries removal and indirect pulp capping in primary molars: a randomized controlled trial. American Journal of Dentistry 2013;26(4):196-200. [PubMed] [Google Scholar]
Calderari 1989 {published data only}
- Calderari G, Bruno E, Di Gianvittorio A, Gagliani M, Re S. Clinical investigation of the Caridex system [Sperimentazione clinica del Sistema Caridex]. Attualita Dentale 1989;5(26-27):6-16. [PubMed] [Google Scholar]
Cavel 1988 {published data only}
- Cavel WT, Kelsey WP 3rd, Barkmeier WW, Blankenau RJ. Clinical evaluation of chemomechanical removal of cervical caries. General Dentistry 1988;36(5):405-8. [PubMed] [Google Scholar]
Chomyszyn‐Gajewska 2006 {published data only}
- Chomyszyn-Gajewska M, Kwapinska H, Zarzecka J. Pain perception in children during caries removal with the Vector system: a pilot study. European Archives of Paediatric Dentistry 2006;7(1):38-41. [DOI: 10.1007/BF03320813 Full-text links] [DOI] [PubMed] [Google Scholar]
de Almeida 2013 {published data only}
- Almeida SM, Franca FM, Florio FM, Ambrosano GM, Basting RT. Analysis of total microbiota in dentin after mechanical or papain-based chemomechanical caries removal. General Dentistry 2013;6(4):59-63. [PubMed] [Google Scholar]
Dülgergil 2005 {published data only}
- Dülgergil CT, Ercan E, Yildirim I. A combined application of ART-fluoride varnish for immigrant junior field-workers: 12-months follow-up field trial in rural Anatolia. Oral Health and Preventive Dentistry 2005;3(2):97-104. [PubMed] [Google Scholar]
Ekstrand 2010 {published data only}
- Ekstrand KR, Bakhshandeh A, Martignon S. Treatment of proximal superficial caries lesions on primary molar teeth with resin infiltration and fluoride varnish versus fluoride varnish only: efficacy after 1 year. Caries Research 2010;44(1):41-6. [DOI: 10.1159/000275573] [DOI] [PubMed] [Google Scholar]
El‐Tekeya 2012 {published data only}
- El-Tekeya M, El-Habashy L, Mokhles N, El-Kimary E. Effectiveness of 2 chemomechanical caries removal methods on residual bacteria in dentin of primary teeth. Paediatric Dentistry 2012;34(4):325-30. [PubMed] [Google Scholar]
Flório 2001 {published data only}
- Flório FM, Pereira AC, Meneghim Mde C, Ramacciato JC. Evaluation of non-invasive treatment applied to occlusal surfaces. ASDC Journal of American Society of Dentistry for Children 2001;68(5-6):326-31. [PubMed] [Google Scholar]
Foley 2003 {published data only}
- Foley J, Blackwell A. In vivo cariostatic effect of black copper cement on carious dentine. Caries Research 2003;37(4):254-60. [DOI: 10.1159/000070867] [DOI] [PubMed] [Google Scholar]
Fure 2000 {published data only}
- Fure S, Lingström P, Birkhed D. Evaluation of Carisolv™ for the chemo-mechanical removal of primary root caries in vivo. Caries Research 2000;34(3):275-80. [DOI: 10.1159/000016602] [DOI] [PubMed] [Google Scholar]
Gibson 1980 {published data only}
- Gibson GB, Richardson AS. Sticky fissure management. 30-month report. Journal of Canadian Dental Association 1980;46(4):255-8. [PubMed] [Google Scholar]
Giza 2007 {published data only}
- Giza S. Comparative studies of carious defects filling using the classical method and dental drill, and using the Carisolv chemomechanical method and the YAG: Er CTL-1601 laser [Badanie Porównawcze Opracowywania Ubytków Próchnicowych Metodą Klasyczną Przy Użyciu Wiertarki Stomatologicznej, Metodą Chemo-Mechaniczną Preparatem Carisolv Oraz Laserem Yag:Er Ctl-1601]. Annales Academiae Medicae Stetinensis 2007;53(3):88-99. [PubMed] [Google Scholar]
Goyal 2015 {published data only}
- Goyal PA, Kumari R, Kannan VP, Madhu S. Efficacy and tolerance of papain gel with conventional drilling method: a clinico-microbiological study. Journal Clinical Paediatric Dentistry 2015;39(2):109-12. [DOI: 10.17796/jcpd.39.2.n25754863557k727] [DOI] [PubMed] [Google Scholar]
Hamilton 2001 {published data only}
- Hamilton JC, Dennison JB, Stoffers KW, Gregory WA, Welch KB. Early treatment of incipient carious lesions: a two-year clinical evaluation. Journal of the American Dental Association 2002;133(12):1643-51. [DOI: 10.14219/jada.archive.2002.0114] [DOI] [PubMed] [Google Scholar]
- Hamilton JC, Dennison JB, Stoffers KW, Welch KB. A clinical evaluation of air-abrasion treatment of questionable carious lesions: a 12-month report. Journal of the American Dental Association 2001;132(6):762-9. [DOI: 10.14219/jada.archive.2001.0273] [DOI] [PubMed] [Google Scholar]
Handelman 1976 {published data only}
- Handelman SL, Leverett DH, Espeland M, Curzon J. Retention of sealants over carious and sound tooth surfaces. Community Dentistry Oral Epidemiology 1987;15(1):1-5. [DOI: 10.1111/j.1600-0528.1987.tb00470.x] [DOI] [PubMed] [Google Scholar]
- Handelman SL, Leverett DH, Espeland MA, Curzon JA. Clinical radiographic evaluation of sealed carious and sound tooth surfaces. Journal of the American Dental Association 1986;113(5):751-4. [DOI: 10.14219/jada.archive.1986.0269] [DOI] [PubMed] [Google Scholar]
- Handelman SL, Leverett DH, Solomon ES, Brenner CM. Use of adhesive sealants over occlusal carious lesions: radiographic evaluation. Community Dentistry Oral Epidemiology 1981;9(6):256-9. [DOI: 10.1111/j.1600-0528.1981.tb00341.x] [DOI] [PubMed] [Google Scholar]
- Handelman SL, Washburn F, Wopperer P. Two-year report of sealant effect on bacteria in dental caries. Journal of the American Dental Association 1976;93(5):967-70. [DOI: 10.14219/jada.archive.1976.0007] [DOI] [PubMed] [Google Scholar]
- Leverett DH, Handelman S, Brenner C, Iker H. Cost analysis of sealants: prevention and treatment of carious lesions. Journal of Dental Research 1983;80:225. [DOI] [PubMed] [Google Scholar]
- Leverett DH, Handelman SL, Brenner CM, Iker HP. Cost-effectiveness of sealants as an alternative to conventional restorations. Journal of Dental Research 1978;57:360. [Google Scholar]
- Leverett DH, Handelman SL, Brenner CM, Iker HP. Use of sealants in the prevention and early treatment of carious lesions: cost analysis. Journal of the American Dental Association 1983;106(1):39-42. [DOI: 10.14219/jada.archive.1983.0024] [DOI] [PubMed] [Google Scholar]
Hassan 2016 {published data only}
- Hassan AF, Yadav G, Tripathi AM, Mehrotra M, Saha S, Garg N. A comparative evaluation of the efficacy of different caries excavation techniques in reducing the cariogenic flora: an in vivo study. International Journal Clinical Paediatric Dentistry 2016;9(3):214. [DOI: 10.5005/jp-journals-10005-1366] [DOI] [PMC free article] [PubMed] [Google Scholar]
Heinrich 1988 {published data only}
- Heinrich R, Kneist S. Antimicrobial effect of calcium hydroxide [Antimikrobielle Wirkung von Kalziumhydroxid]. Stomatologie der DDR 1988;38(10):693-8. [PMID: ] [PubMed] [Google Scholar]
Hoefler 2016 {published data only}
- Hoefler V, Nagaoka H, Miller CS. Long-term survival and vitality outcomes of permanent teeth following deep caries treatment with step-wise and partial-caries-removal: a systematic review. Journal of Dentistry 2016;54:25-32. [DOI: 10.1016/j.jdent.2016.09.009] [DOI] [PubMed] [Google Scholar]
Hosein 2008 {published data only}
- Hosein T, Hasan A. Efficacy of chemo-mechanical caries removal with Carisolv. Journal of College of Physicians and Surgeons Pakistan 2008;18(4):222-5. [PubMed] [Google Scholar]
Kakaboura 2003 {published data only}
- Kakaboura A, Masouras C, Staikou O, Vougiouklakis G. A comparative clinical study on the Carisolv caries removal method. Quintessence International 2003;34(4):269-71. [PubMed] [Google Scholar]
Kalf‐Scholte 2003 {published data only}
- Kalf-Scholte SM, Amerongen WE, Smith AJ, Haastrecht HJ. Atraumatic restorative treatment (ART): a three-year clinical study in Malawi – comparison of conventional amalgam and ART restorations. Journal Public Health Dentistry 2003;63(2):99-103. [DOI: 10.1111/j.1752-7325.2003.tb03482.x] [DOI] [PubMed] [Google Scholar]
Kavvadia 2004 {published data only}
- Kavvadia K, Karagianni V, Polychronopoulou A, Papagiannouli L. Primary teeth caries removal using the Carisolv chemomechanical method: a clinical trial. Pediatric Dentistry 2004;26(1):23-8. [PubMed] [Google Scholar]
Kirzioglu 2007 {published data only}
- Kirzioglu Z, Gurbuz T, Yilmaz Y. Clinical evaluation of chemomechanical and mechanical caries removal: status of the restorations at 3, 6, 9 and 12 months. Clinical Oral Investigation 2007;11(1):69. [DOI: 10.1007/s00784-006-0072-1] [DOI] [PubMed] [Google Scholar]
Kochhar 2011 {published data only}
- Kochhar GK, Srivastava N, Pandit IK, Gugnani N, Gupta M. An evaluation of different caries removal techniques in primary teeth: a comparative clinical study. Journal of Clinical Paediatric Dentistry 2011;36(1):5-9. [DOI: 10.17796/jcpd.36.1.u2421l4j68847215] [DOI] [PubMed] [Google Scholar]
Kotb 2009 {published data only}
- Kotb RM, Abdella AA, El Kateb MA, Ahmed AM. Clinical evaluation of Papacarie in primary teeth. Journal of Clinical Paediatric Dentistry 2009;34(2):117-23. [DOI: 10.17796/jcpd.34.2.f312p36g18463716] [DOI] [PubMed] [Google Scholar]
Lager 2003 {published data only}
- Lager A, Thornqvist E, Ericson D. Cultivatable bacteria in dentine after caries excavation using rose-bur or Carisolv. Caries Research 2003;37(3):206-11. [DOI: 10.1159/000070446] [DOI] [PubMed] [Google Scholar]
Lakshmi 2018 {published data only}
- Lakshmi MS, Srilatha KT, Nandlal B, Deshmukh S. Clinical evaluation of preventive effect of fissure sealants on initial carious lesion of permanent mandibular molars pretreated with and without fluoride varnish by fluorescence camera. International Journal of Clinical Paediatric Dentistry 2018;11(2):89-93. [DOI: 10.5005/jp-journals-10005-1491] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lozano‐Chourio 2006 {published data only}
- Lozano-Chourio MA, Zambrano O, González H, Quero M. Clinical randomized controlled trial of chemomechanical caries removal (Carisolv™). International Journal of Paediatric Dentistry 2006;16(3):161-7. [DOI: 10.1111/j.1365-263X.2006.00719.x] [DOI] [PubMed] [Google Scholar]
- Lozano-Chourio MA, Zambrano O, Rivera L, Aguilera LA. Ultraconservative caries removal: microbiological evaluation, and identification with PCR. IADR General Session; 2009 Apr 1-4; Miami, FL 2009:682.
Maguire 2020 {published data only}
- Maguire A, Clarkson JE, Douglas GV, Ryan V, Homer T, Marshman Z, et al. Best-practice prevention alone or with conventional or biological caries management for 3- to 7-year-olds: the FiCTION three-arm RCT. Health Technology Assessment 2020;24(1):1-174. [DOI: 10.3310/hta24010] [DOI] [PMC free article] [PubMed] [Google Scholar]
Malmström 2003 {published data only}
- Malmström HS, Chaves Y, Moss ME. Patient preference: conventional rotary handpieces or air abrasion for cavity preparation. Operative Dentistry 2003;28(6):667-71. [PubMed] [Google Scholar]
Maltz 2012 {published data only}
- Maltz M, Henz SL, Oliveira EF, Jardim JJ. Conventional caries removal and sealed caries in permanent teeth: a microbiological evaluation. Journal of Dentistry 2012;40(9):776-82. [DOI: 10.1016/j.jdent.2012.05.011] [DOI] [PubMed] [Google Scholar]
Mandari 2001 {published data only}
- Mandari GJ, Frencken JE, van't Hof MA. Six-year success rates of occlusal amalgam and glass-ionomer restorations placed using three minimal intervention approaches. Caries Research 2001;37(4):246-53. [DOI] [PubMed] [Google Scholar]
- Mandari GJ, Truin GJ, van't Hof MA, Frencken JE. Effectiveness of three minimal intervention approaches for managing dental caries: survival of restorations after 2 years. Caries Research 2001;35(2):90-4. [DOI: 10.1159/000047438] [DOI] [PubMed] [Google Scholar]
Maragakis 2001 {published data only}
- Maragakis GM, Hahn P, Hellwig E. Clinical evaluation of chemomechanical caries removal in primary molars and its acceptance by patients. Caries Research 2001;35(3):205-10. [DOI: 10.1159/000047457] [DOI] [PubMed] [Google Scholar]
Martignon 2012 {published data only}
- Martignon S, Ekstrand KR, Ellwood R. Efficacy of sealing proximal early active lesions: an 18-month clinical study evaluated by conventional and subtraction radiography. Caries Research 2006;40(5):382-8. [DOI: 10.1159/000094282] [DOI] [PubMed] [Google Scholar]
- Martignon S, Ekstrand KR, Gomez J, Lara JS, Cortes A. Infiltrating/sealing proximal caries lesions: a 3-year randomized clinical trial. Journal of Dental Research 2012;91(3):288-92. [DOI: 10.1177/0022034511435328] [DOI] [PubMed] [Google Scholar]
- Martignon S, Tellez M, Santamaría RM, Gomez J. Sealing distal proximal caries lesions in first primary molars: efficacy after 2.5 years. Caries Reseach 2010;44(6):562-70. [DOI: 10.1159/000321986] [DOI] [PubMed] [Google Scholar]
Matsumoto 2013 {published data only}
- Matsumoto SF, Motta LJ, Alfaya TA, Guedes CC, Fernandes KP, Bussadori SK. Assessment of chemomechanical removal of carious lesions using Papacarie Duo™: randomized longitudinal clinical trial. Indian Journal of Dental Research 2013;24(4):488-92. [DOI: 10.4103/0970-9290.118393] [DOI] [PubMed] [Google Scholar]
Moreira 2017 {published data only}
- Moreira KM, Kantovitz KR, Aguiar JP, Borges AF, Pascon FM, Puppin-Rontani RM. Impact of the intermediary layer on sealant retention: a randomized 24-month clinical trial. Clinical Oral Investigation 2017;21(5):1435-43. [DOI: 10.1007/s00784-016-1890-4] [DOI] [PubMed] [Google Scholar]
Motta 2013 {published data only}
- Motta LJ, Bussadori SK, Campanelli AP, da Silva AL, Alfaya TA, Godoy CH, et al. Pain during removal of carious lesions in children: a randomized controlled clinical trial. International Journal of Dentistry 2013;2013:896381. [DOI: 10.1155/2013/896381] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta LJ, Bussadori SK, Campanelli AP, Silva AL, Alfaya TA, Godoy CH, et al. Efficacy of Papacarie(®) in reduction of residual bacteria in deciduous teeth: a randomized, controlled clinical trial. Clinics (Sao Paulo). Clinics (Sao Paulo, Brazil) 2014;69(5):319-22. [DOI: 10.6061/clinics/2014(05)04] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motta LJ, Bussadori SK, Campanelli AP, Silva AL, Alfaya TA, Godoy CH, et al. Randomized controlled clinical trial of long-term chemo-mechanical caries removal using Papacarie™ gel. Journal Applied Oral Science 2014;22(4):307-13. [DOI: 10.1590/1678-775720130488] [DOI] [PMC free article] [PubMed] [Google Scholar]
Muñoz‐Sandoval 2019 {published data only}
- Muñoz-Sandoval C, Gambetta-Tessini K, Giacaman RA. Microcavitated (ICDAS 3) carious lesion arrest with resin or glass ionomer sealants in first permanent molars: a randomized controlled trial. Journal of Dentistry 2019;88:103163. [DOI: 10.1016/j.jdent.2019.07.001] [DOI] [PubMed] [Google Scholar]
Nadanovsky 2001 {published data only}
- Nadanovsky P, Cohen Carneiro F, Souza de Mello F. Removal of caries using only hand instruments: a comparison of mechanical and chemo-mechanical methods. Caries Research 2001;35(5):384-9. [DOI: 10.1159/000047478] [DOI] [PubMed] [Google Scholar]
Pandit 2007 {published data only}
- Pandit IK, Srivastava N, Gugnani N, Gupta M, Verma L. Various methods of caries removal in children: a comparative clinical study. Indian Society of Pedodontic and Preventive Dentistry 2007;25(2):93. [DOI: 10.4103/0970-4388.33456] [DOI] [PubMed] [Google Scholar]
Peric 2009 {published data only}
- Peric T, Markovic D, Petrovic B. Clinical evaluation of a chemomechanical method for caries removal in children and adolescents. Acta Odontologica Scandinavica 2009;67(5):277-83. [DOI: 10.1080/00016350902976779] [DOI] [PubMed] [Google Scholar]
Peters 2006 {published data only}
- Peters MC, Flamenbaum MH, Eboda NN, Feigal RJ, Inglehart MR. Chemomechanical caries removal in children: efficacy and efficiency. Journal of the American Dental Association 2006;137(12):1658-66. [DOI: 10.14219/jada.archive.2006.0111] [DOI] [PubMed] [Google Scholar]
Rios Caro 2012 {published data only}
- Rios Caro T, Aguirre A, Saavedra JH, Alfaya T, Frana C, Fernandes K, et al. Effectiveness of carious removal with chemomechanical system versus traditional method. General Session of the International Association for Dental Research; 2012 Jun 20-23; Iguaçu Falls, Brazil.
Ruff 2018 {published data only}
- Ruff RR, Niederman R. Silver diamine fluoride versus therapeutic sealants for the arrest and prevention of dental caries in low-income minority children: study protocol for a cluster randomized controlled trial. Trials 2018;19(1):523. [DOI: 10.1186/s13063-018-2891-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Santamaria 2014 {published data only}
- Santamaria R, Innes N. Trial shows partial caries removal is an effective technique in primary molars. Evidence Based Dentistry 2014;15(3):81-2. [DOI: 10.1038/sj.ebd.6401044] [DOI] [PubMed] [Google Scholar]
Sarmadi 2018 {published data only}
- Sarmadi R, Andersson EV, Lingström P, Gabre P. A randomized controlled trial comparing Er:YAG laser and rotary bur in the excavation of caries – patients' experiences and the quality of composite restoration. Open Dentistry Journal 2018;12:443-54. [DOI: 10.2174/1874210601812010443] [DOI] [PMC free article] [PubMed] [Google Scholar]
Straffon 1988a {published data only}
- Dennison JB, Straffon LH. Clinical evaluation comparing sealant and amalgam – 4 year report. Journal of Dental Research 1981;520:843. [DOI] [PubMed] [Google Scholar]
- Straffon LH, Dennison JB. Clinical evaluation comparing sealant and amalgam after 7 years: final report. Journal of the American Dental Association 1988;117(6):751-5. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
Straffon 1988b {published data only}
- Dennison JB, Straffon LH. Clinical evaluation comparing sealant and amalgam – 4 year report. Journal of Dental Research 1981;60:520. [DOI] [PubMed] [Google Scholar]
- Straffon LH, Dennison JB. Clinical evaluation comparing sealant and amalgam after 7 years: final report. Journal of the American Dental Association 1988;117(6):751-5. [DOI: 10.14219/jada.archive.1988.0107] [DOI] [PubMed] [Google Scholar]
Taifour 2003 {published data only}
- Taifour D, Frencken JE, Beiruti N, van't Hof MA, Truin GJ, Palenstein Helderman WH. Comparison between restorations in the permanent dentition produced by hand and rotary instrumentation – survival after 3 years. Community Dentistry and Oral Epidemiology 2003;31(2):122-8. [DOI: 10.1034/j.1600-0528.2003.00027.x] [DOI] [PubMed] [Google Scholar]
- Taifour D, Frencken JE, Beiruti N, van't Hof MA, Truin GJ. Effectiveness of glass-ionomer (ART) and amalgam restorations in the deciduous dentition: results after 3 years. Caries Research 2002;36(6):437-44. [DOI: 10.1159/000066531] [DOI] [PubMed] [Google Scholar]
Tavciovski 1966 {published data only}
- Tavciovski I, Cvetković N. Our results in the treatment of deep caries [Nasi rezultati vo lekuvanjeto na caries profunda]. God Zb Med Fak Skopje 1966;13:231-5. [PubMed] [Google Scholar]
Thompson 2015 {published data only}
- Thompson V, Craig RG, Curro FA, Green WS, Ship JA. Alternative Treatment of Deep Carious Lesions Based on Biological Evidences. clinicaltrials.gov/ct2/show/NCT00973089 (first received 9 September 2009). [CLINICALTRIALS IDENTIFICATION NUMBER: NCT00973089]
Valério 2016 {published data only}
- Valério RA, Borsatto MC, Serra MC, Polizeli SA, Nemezio MA, Galo R, et al. Caries removal in deciduous teeth using an Er:YAG laser: a randomized split-mouth clinical trial. Clinical Oral Investigations 2016;20(1):65-73. [DOI: 10.1007/s00784-015-1470-z] [DOI] [PubMed] [Google Scholar]
- Valerio RA, Polizeli SA, Serra MC, Borsatto MC, Corona SA. Partial caries removal with Er: YAG laser. A pilot study. In: IADR/AADR/CADR General Session; 2013 Mar 20-23; Seattle, WA. Seattle (WA). Alexandria (VA): International Association for Dental Research, 2013.
Wang 2007 {published data only}
- Wang J, Wang HM. Effects of three caries removal methods on children's dental fear evaluated by physiological measure. Shanghai Kou Qiang Yi Xue 2007;16(2):149-52. [PubMed] [Google Scholar]
Welbury 1990 {published data only}
- Welbury RR, Walls AW, Murray JJ, McCabe JF. The management of occlusal caries in permanent molars. A 5-year clinical trial comparing a minimal composite with an amalgam restoration. British Dental Journal 1990;169(11):361-6. [DOI: 10.1038/sj.bdj.4807385] [DOI] [PubMed] [Google Scholar]
Zakirulla 2012 {published data only}
- Zakirulla M, Uloopi KS, Subba Reddy VV. In vivo comparison of reduction in bacterial count after caries excavation with 3 different techniques. Journal of Dentistry for Children (Chicago, Ill.) 2012;78(1):31-5. [PubMed] [Google Scholar]
Zinck 1988 {published data only}
- Zinck JH, McInnes-Ledoux P, Capdeboscq C, Weinberg R. Chemomechanical caries removal—a clinical evaluation. Journal of Oral Rehabilitation 1988;15(1):23-33. [DOI: 10.1111/j.1365-2842.1988.tb00143.x] [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Vicioni‐Marques 2018 {published data only}
- Vicioni-Marques F, Carvalho FK. Comparison of three restorative protocols in teeth with molar-incisor hipomineralization (MIH): a randomized controlled clinical study, University of Sao Paulo. clinicaltrials.gov/ct2/show/NCT03760497 (first received 30 November 2018). [CLINICALTRIALS.GOV IDENTIFIER (NCT NUMBER): NCT03760497]
Additional references
Bakhshandeh 2018
- Bakhshandeh A, Floriano I, Braga MM, Thorlacius KA, Ekstrand KR. Relationship between depth of approximal caries lesions and presence of bacteria in the dentine in primary and permanent posterior teeth: a radiographic examination with microbiological evaluation. Acta Odontologica Scandinavica 2018;76(7):509-14. [DOI: 10.1080/00016357.2018.1444201] [DOI] [PubMed]
Bjørndal 1997
- Bjørndal L, Larsen T, Thylstrup A. A clinical and microbiological study of deep carious lesions during stepwise excavation using long treatment intervals. Caries Research 1997;31(6):411-7. [DOI] [PubMed] [Google Scholar]
Bjørndal 2000
- Bjørndal L, Larsen T. Changes in the cultivable flora in deep carious lesions following a stepwise excavation procedure. Caries Research 2000;34(6):502-8. [DOI] [PubMed] [Google Scholar]
Chaimani 2013
- Chaimani A, Higgins JP, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PloS One 2013;8(10):e76654. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JP, Altman DG. Chapter 9: Analysing data and undertaking meta-analyses. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. training.cochrane.org/handbook/archive/v5.1/.
Demant 2021
- Demant S, Dabelsteen S, Bjørndal LI. A macroscopic and histological analysis of radiographically well-defined deep and extremely deep carious lesions: carious lesion characteristics as indicators of the level of bacterial penetration and pulp response [A macroscopic and histological analysis of radiographically well-defined deep and extremely deep carious lesions: carious lesion characteristics as indicators of the level of bacterial penetration and pulp response]. International Endodontic Journal 2021;54(3):319-330. [DOI: 10.1111/iej.13424] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dias 2010
- Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Statistics in Medicine 2010;29:932-44. [DOI] [PubMed] [Google Scholar]
Egger 1997
- Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315(7109):629-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
ESE 2019
- Duncan HF, Galler KM, Tomson PL, Simon S, El-Karim I, Kundzina R, et al. European Society of Endodontology position statement: management of deep caries and the exposed pulp. International Endodontic Journal 2019;52(7):923-34. [DOI] [PubMed] [Google Scholar]
GRADE 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
GRADEpro GDT [Computer program]
- GRADEpro GDT. Version accessed 31 May 2018. Hamilton (ON): McMaster University (developed by Evidence Prime), 2015. Available at gradepro.org.
Gruythuysen 2010
- Gruythuysen R. Non-restorative cavity treatment: managing rather than masking caries activity. Nederlands Tijdschrift voor Tandheelkunde 2010;117(3):173-80. [DOI] [PubMed] [Google Scholar]
Hansen 2017
- Hansen NV, Nyvad B. Non-operative control of cavitated approximal caries lesions in primary molars: a prospective evaluation of cases. Journal of Oral Rehabilitation 2017;44(7):537-44. [DOI: 10.1111/joor.12508] [DOI] [PubMed] [Google Scholar]
Higgins 2011a
- Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from training.cochrane.org/handbook/archive/v5.1/.
Higgins 2011b
- Higgins JP, Green S. Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. training.cochrane.org/handbook/archive/v5.1/.
Higgins 2011c
- Higgins JP, Green S. Chapter 7: Selecting studies and collecting data. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. training.cochrane.org/handbook/archive/v5.1/.
Higgins 2013
- Higgins JP, Lasserson T, Chandler J, Tovey D, Churchill R. Standards for the conduct and reporting of new Cochrane intervention reviews, reporting of protocols and the planning, conduct and reporting of updates. community.cochrane.org/mecir-manual (accessed 30 May 2018).
Houpt 1994
- Houpt M, Fuks A, Eidelman E . The preventive (composite resin/sealant) restoration: nine-year results. Quintessence International 1994;25:155-59. [PubMed] [Google Scholar]
Innes 2007
- Innes NP, Evans DJ, Stirrups DR. The Hall Technique; a randomized controlled clinical trial of a novel method of managing carious primary molars in general dental practice: acceptability of the technique and outcomes at 23 months. BMC Oral Health 2007;7 (18). [DOI: 10.1186/1472-6831-7-18] [DOI] [PMC free article] [PubMed] [Google Scholar]
Innes 2016
- Innes NP, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on terminology. Advances in Dental Research 2016;28(2):49-57. [DOI] [PubMed] [Google Scholar]
Innes 2017
- Innes NP, Schwendicke F. Restorative thresholds for carious lesions: systematic review and meta-analysis. Journal of Dental Research 2017;96(5):501-8. [DOI] [PubMed] [Google Scholar]
Kassebaum 2015
- Kassebaum NJ, Bernabé E, Dahiya M, Bhandari B, Murray CJ, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. Journal of Dental Research 2015;94(5):650-8. [DOI] [PubMed] [Google Scholar]
Lefebvre 2020
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical Supplement to Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions, Version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Listl 2015
- Listl S, Galloway J, Mossey PA, Marcenes W. Global economic impact of dental diseases. Journal of Dental Research 2015;94(10):1355-61. [DOI] [PubMed] [Google Scholar]
Marcenes 2013
- Marcenes W, Kassebaum NJ, Bernabé E, Flaxman A, Naghavi M, Lopez A, et al. Global burden of oral conditions in 1990-2010: a systematic analysis. Journal of Dental Research 2013;92(7):592-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Marsh 2010
- Marsh PD. Microbiology of dental plaque biofilms and their role in oral health and caries. Dental Clinics of North America 2010;54(3):441-54. [DOI] [PubMed] [Google Scholar]
McDonald 2011
- McDonald RE, Avery DR, Dean JA. Restorative dentistry. In: McDonald RE, Avery DR, Dean JA, eds. Dentistry for the Child and Adolescent. 9th edition. St Louis, Mo: CV MosbyInc, 2011:322-42. [Google Scholar]
Oong 2008
- Oong EM, Griffin SO, Kohn WG, Gooch BF, Caufield PW. The effect of dental sealants on bacteria levels in caries lesions: a review of the evidence. Journal of the American Dental Association 2008;139(3):271-8. [DOI] [PubMed] [Google Scholar]
Owen 2019
- Owen RK, Bradbury N, Xin Y, Cooper N, Sutton A. MetaInsight: An interactive web-based tool for analyzing, interrogating, and visualizing network meta-analyses using R-shiny and netmeta. Research Synthesis Methods 2019;10:569-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Paddick 2005
- Paddick JS, Brailsford SR, Kidd EA, Beighton D. Phenotypic and genotypic selection of microbiota surviving under dental restorations. Applied Environmental Microbiology 2005;71(5):2467-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2020 [Computer program]
- Review Manager Web (RevMan Web). Version 3.2.1. The Cochrane Collaboration, 2020. Available at revman.cochrane.org.
Ricketts 1995
- Ricketts DN, Kidd EA, Beighton D. Operative and microbiological validation of visual, radiographic and electronic diagnosis of occlusal caries in non-cavitated teeth judged to be in need of operative care. British Journal of Dentistry 1995;179(6):214-20. [DOI] [PubMed] [Google Scholar]
Ricketts 2013
- Ricketts D, Lamont T, Innes NP, Kidd E, Clarkson JE. Operative caries management in adults and children. Cochrane Database of Systematic Reviews 2013, Issue 3. Art. No: CD003808. [DOI: 10.1002/14651858.CD003808.pub3] [DOI] [PubMed] [Google Scholar]
Ricucci 2020
- Ricucci D, Siqueira JF Jr, Rôças IN, Lipski M, Shiban A, Tay FR. Pulp and dentine responses to selective caries excavation: a histological and histobacteriological human study. Journal of Dentistry 2020;100:103430. [DOI] [PubMed] [Google Scholar]
Salanti 2011
- Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. Journal of Clinical Epidemiology 2011;64(2):163-71. [DOI] [PubMed] [Google Scholar]
Schwendicke 2013
- Schwendicke F, Stolpe M, Meyer-Lueckel H, Paris S, Dörfer CE. Cost-effectiveness of one- and two-step incomplete and complete excavations. Journal of Dental Research 2013;92(10):880-7. [DOI] [PubMed] [Google Scholar]
Schwendicke 2014
- Schwendicke F, Paris S, Stolpe M. Cost-effectiveness of caries excavations in different risk groups – a micro-simulation study. BMC Oral Health 2014;14:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwendicke 2015a
- Schwendicke F, Stolpe M, Innes N. Conventional treatment, Hall Technique or immediate pulpotomy for carious primary molars: a cost-effectiveness analysis. International Endodontic Journal 2015;49(9):817-26. [DOI: 10.1111/iej.12537] [DOI] [PubMed] [Google Scholar]
Schwendicke 2015b
- Schwendicke F, Stolpe M, Meyer-Lueckel H, Paris S. Detecting and treating occlusal caries lesions: a cost-effectiveness analysis. Journal of Dental Research 2015;94(2):272-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwendicke 2016a
- Schwendicke F, Frencken JE, Bjørndal L, Maltz M, Manton DJ, Ricketts D, et al. Managing carious lesions: consensus recommendations on carious tissue removal. Advances in Dental Research 2016;28(2):58-67. [DOI] [PubMed] [Google Scholar]
Schwendicke 2016b
- Schwendicke F, Diederich C, Paris S. Restoration gaps needed to exceed a threshold size to impede sealed lesion arrest in vitro. Journal of Dentistry 2016;48:77-80. [DOI] [PubMed] [Google Scholar]
Schwendicke 2016c
- Schwendicke F, Göstemeyer G. Understanding dentists' management of deep carious lesions in permanent teeth: a systematic review and meta-analysis. Implementation Science 2016;11(1):142. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schwendicke 2020
- Schwendicke F, Splieth CH, Bottenberg P, Breschi L, Campus G, Doméjean S, et al. How to intervene in the caries process in adults: proximal and secondary caries? An EFCD-ORCA-DGZ expert Delphi consensus statement. Clinical Oral Investigations 2020;24(9):3315-21. [DOI] [PubMed] [Google Scholar]
Takahashi 2011
- Takahashi N, Nyvad B. The role of bacteria in the caries process: ecological perspectives. Journal of Dental Research 2011;90(3):294-303. [DOI] [PubMed] [Google Scholar]
Thompson 2005
- Thompson VP, Kaim JM. Nonsurgical treatment of incipient and hidden caries. Dental Clinics of North America 2005;49:905-21. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Schwendicke 2018
- Schwendicke F, Walsh T, Fontana M, Bjørndal L, Clarkson JE, Lamont T, Levey C, Gostemeyer G, Santamaria RM, Ricketts D, Innes NPT. Interventions for treating cavitated or dentine carious lesions. Cochrane Database of Systematic Reviews 2018, Issue 6. Art. No: CD013039. [DOI: 10.1002/14651858.CD013039] [DOI] [PMC free article] [PubMed] [Google Scholar]


