Abstract
Background
Acrylamide (AA) is a toxicant to humans, but the association between AA exposure and the risk of non-alcoholic fatty liver disease (NAFLD) remains unclear. In this study, our objective is to examine the cross-sectional association between AA exposure and the risk of NAFLD in American adults.
Methods
A total of 3234 individuals who took part in the National Health and Nutrition Examination Survey (NHANES) 2003–2006 and 2013–2016 were enrolled in the study. NAFLD was diagnosed by the U.S. Fatty Liver Index. Multivariable logistic regression models were applied to estimate the association between AA and NAFLD in the whole group and the non-smoking group.
Results
We discovered that in the whole group, serum hemoglobin adducts of AA (HbAA) were negatively associated with the prevalence of NAFLD after adjustment for various covariables (P for trend < 0.001). Compared with individuals in the lowest HbAA quartiles, the odds ratios (ORs) with 95% confidence intervals (CIs) in the highest HbAA quartiles were 0.61 (0.46–0.81) and 0.57 (0.36–0.88) in the whole group and the non-smoking group, respectively. In contrast, HbGA/HbAA showed a significantly positive correlation with the prevalence of NAFLD in both groups (P for trend < 0.001). In addition, HbGA was not significantly associated with NAFLD in the whole group or the non-smoking group.
Conclusions
HbAA is negatively associated with NAFLD whereas HbGA/HbAA is positively associated with NAFLD in adults in the U.S. Further studies are needed to clarify these relationships.
Keywords: Fatty liver disease, Acrylamide, Association, Risk
Background
Non-alcoholic fatty liver disease (NAFLD) is one of the most common chronic liver disorders, with its global prevalence estimated to be 24%, a figure expected to rise rapidly in the future [1]. NAFLD is characterized as a spectrum ranging from simple steatosis, to steatohepatitis, fibrosis, and even hepatocellular carcinoma, and it is strongly associated with metabolic syndrome [2]. Current data confirm that NAFLD is a complex disease involving multiple environmental factors and genetic predispositions [3].
Acrylamide (AA, C3H5NO), a highly reactive α, β-unsaturated carbonyl compound, is widely used in the production of its polymer, polyacrylamide, for industrial processes and gel electrophoresis in laboratories [4]. AA is generated through the Maillard reaction between asparagine and reducing sugars in low moisture-processed, carbohydrate-rich food cooked at high temperatures (above 120 °C), such as French fries and biscuits [5]. Besides food, cigarette smoking is another crucial cause of exposure, with the level of AA ranging from 0.5 to 4.2 μg per cigarette [6]. After being absorbed into the human body, AA can be metabolized by either reacting with cytochrome P-450 2E1 (CYP2E1) to form a reactive epoxy compound glycidamide (GA) or conjugating with glutathione (GSH) to form GSH conjugates [7]. Like glucose, AA and GA are also able to react with hemoglobin to form hemoglobin adducts of AA (HbAA) and GA (HbGA). Considering the lifespan of erythrocytes, these two adducts can be adopted as proper biomarkers to evaluate AA exposure within the past 4 months [8].
In 1994, AA was defined as a Group 2A carcinogenic compound by the International Agency for Research on Cancer (IARC) [9], although its carcinogenicity remains inconsistent and ambiguous across different epidemiological studies. In 2002, AA was discovered in food by Swedish scientists, which sparked research on its hazard level [10]. Similar to classic endocrine-disrupting chemicals (EDC), AA also has the potential to interfere with the endocrine system by impairing endogenous hormonal activity [11]. Previous studies showed that high AA exposure is associated with obesity-related outcomes in a population of U.S. adults [12]. Obesity has been linked with NAFLD independently of other metabolic factors [13]. It plays a key role in not only the onset of liver steatosis but also its progression [14]. Moreover, the severity of NAFLD and mortality in NAFLD patients also increase with obesity [15–17]. Besides obesity, insulin resistance has also been shown to be closely related to NAFLD [18]. Hepatic insulin action is required for lipid synthesis, glucose production and the development of hepatic steatosis during insulin resistance [19]. HbAA was shown to be associated with reduced serum insulin levels [20] and the risk of diabetes [21] in previous NHANES research. Furthermore, an in vivo study also indicated that AA disrupted glucose homeostasis in female rats possibly by impairing the physiological effects of insulin [22]. However, no epidemiological evidence has been reported to support the association between AA exposure and NAFLD.
In this study, we analyzed the associations of HbAA and HbGA with NAFLD among a nationally representative sample of American adults who were enrolled in the National Health and Nutrition Examination Survey (NHANES) 2003–2006 and 2013–2016.
Methods
Study design and population
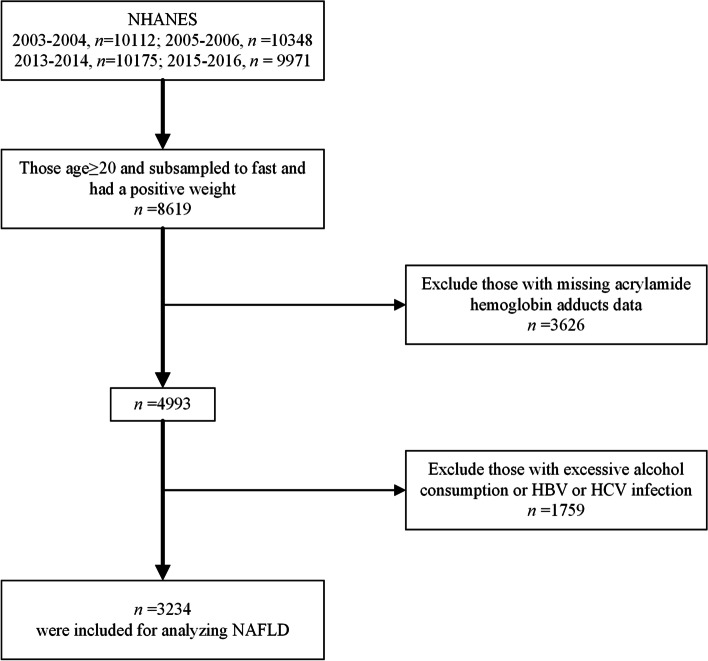
The NHANES is a series of cross-sectional surveys conducted every 2 years to continuously measure the health and nutritional status of adults and children, covering different population groups and health topics in the United States. In our study, we used the publicly available data of NHANES 2003–2006 and 2013–2016, in which HbAA and HbGA levels were tested. A total of 40,606 individuals who participated in the four survey cycles were considered in this study. Of these participants, 8619 participants aged over 20 years were subsampled to fast before attending a morning exam session, among which 4993 participants were eligible for analysis of HbAA and HbGA. We also excluded those with alcohol consumption > 2 drinks/day for men or > 1 drink/day for women, and those infected with hepatitis B virus (HBV) or hepatitis C virus (HCV) (n = 1759). Finally, 3234 participants were enrolled as the study population (Fig. 1).
Fig. 1.
Flow diagram of inclusion criteria from NHANES 2003–2006 and 2013–2016. HBV: hepatitis B virus; HCV: hepatitis C virus
Analysis of acrylamide biomarkers
The laboratory procedure for acrylamide biomarkers has been described in detail in the NHANES documentation [23]. Briefly, after the measurement of total hemoglobin, the Edman products of N-terminal HbAA and HbGA in human whole blood or erythrocytes were isolated and determined through high-performance liquid chromatography tandem mass spectrometry (HPLC/MS/MS). Final results are reported as pmol adduct per g hemoglobin (pmol/g Hb).
Definitions of NAFLD and other metabolic disorders
The ascertainment of NAFLD is based on the U.S. fatty liver index (US FLI), which was first introduced by Ruhl et al. [24]. The US FLI was established on the NHANES 1988–1994 data and calculated by using the following factors: ethnicity (non-Hispanic black, Mexican American), age (years), gamma glutamyl transferase (U/L), waist circumference (cm), fasting insulin (pmol/L), and fasting glucose (pmol/L). A US FLI ≥ 30 was selected to rule in fatty liver as suggested, and those with excessive alcohol consumption (> 2 drinks/day for men or > 1 drink/day for women) were excluded [24].
In addition, body mass index (BMI) was calculated as weight divided by height squared (kg/m2) and used to define obesity (BMI ≥ 30.0 kg/m2) [25]. Hypertension was defined as systolic blood pressure exceeding 140 mmHg or diastolic blood pressure exceeding 90 mmHg or the use of anti-hypertensive agents [26]. Type 2 diabetes mellitus (T2DM) was defined as high fasting plasma glucose (≥ 126 mg/dL) or high glycated hemoglobin (HbA1c, ≥ 6.5%) or the use of anti-hyperglycemic agents [27]. Hyperuricemia was defined as serum uric acid levels ≥ 420 μmol/L in men and ≥ 360 μmol/L in women [28].
Covariables
We considered age (years), gender (man/woman), race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American, and other), education level (under high school, high school, and above high school), family income-to-poverty ratio (PIR), marital status (married/other), serum cotinine level, total fat intake (gm), total energy intake (kcal), albumin (g/L), LDL-cholesterol (mmol/L), total cholesterol (mmol/L), and platelet count (1000 cells/μL) as covariables. Values of total fat intake and total energy intake were obtained from 24-h dietary recall interviews.
Statistical analysis
Due to the complex, multistage sampling design used to select participants in NHANES, we constructed 8-year fasting subsample MEC weights (WTSAF2YR*1/4) for combined survey cycles (2003–2006 and 2013–2016). Surveymeans and Surveyfreq procedures were performed to describe variables in weighted forms. Continuous variables were compared by using the Surveyreg procedure, and categorical variables were compared by using the Rao–Scott χ2 test as recommended [29]. A quartile-based analysis was carried out by dividing HbAA and HbGA levels into quartiles, and the lowest one was set as the reference. Then, the Surveylogistic regression model was used to evaluate the risk factors of NAFLD. We also applied increasing degrees of adjustment to the three models. Model 1 was only adjusted for demographic and social-economic factors (age, gender, race/ethnicity, education level, family PIR, marital status, and serum cotinine level). Model 2 was adjusted for factors in model 1 plus dietary factors (total fat intake and total energy intake). Model 3 was further adjusted for biochemistry factors. The NOMCAR option was used in the estimation procedures to treat missing values as not missing completely at random. Furthermore, we conducted mediation analysis to assess whether the association between AA and NAFLD was mediated by BMI, insulin, fasting glucose or blood pressure by applying the publicly available SAS macro %mediate [30]. SAS 9.4 (SAS Institute Inc., Cary, NC) was employed for all analyses in this study. Two-sided P < 0.05 was considered to be statistically significant.
Results
From NHANES 2003–2006 and 2013–2016, a total of 3234 participants, 49.6% men and 50.4% women, were analyzed in our study. All the participants were divided into quartiles based on their HbAA levels as shown in Table 1. There were 70.0% non-Hispanic whites, 11.3% non-Hispanic blacks, 7.8% Mexican Americans, and 11.0% participants from other races. Compared with quartiles 1–3, the proportion of smokers soared to 62.2% in quartile 4, while the marriage rate decreased to 53.6%. Besides, those with higher levels of HbAA tended to be younger and have a lower BMI but higher energy intake and total fat intake. Interestingly, fasting triglyceride levels decreased monotonically in quartiles 1–3, but rose again in quartile 4, demonstrating a U-shaped curve, whereas HDL-C showed the opposite tendency. Furthermore, 30.8% of the participants had NAFLD according to their US FLI scores, and NAFLD prevalence was negatively associated with HbAA levels (P = 0.001). In subgroups, the prevalence of NAFLD grew by 2.5-fold and 4.5-fold, respectively, in the elevated alanine aminotransferase (ALT) group (ALT > 40 U/L) and the obese group (BMI ≥ 30 kg/m2). These results indicated a significant association of HbAA level with NAFLD and metabolic abnormalities.
Table 1.
Clinical characteristics of the participants in NHANES 2003–2006 according to HbAA quartiles
| Variables | Total (n = 3234) | HbAA quartiles | ||||
|---|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | P | ||
| Age, year | 49.75 ± 0.55 | 52.26 ± 0.88 | 50.94 ± 0.80 | 49.48 ± 0.75 | 46.64 ± 0.63 | < 0.001 |
| Male, % | 49.6 (1.0) | 45.4 (2.0) | 44.1 (2.2) | 47.8 (2.2) | 60.2 (1.6) | < 0.001 |
| Race/ethnicity, % | < 0.001 | |||||
| Non-Hispanic White | 70.0 (2.1) | 73.0 (2.6) | 68.9 (2.1) | 72.0 (2.8) | 70.0 (2.1) | |
| Non-Hispanic Black | 11.3 (1.2) | 10.1 (1.2) | 11.1 (1.5) | 13.6 (1.6) | 11.3 (1.2) | |
| Mexican American | 7.8 (1.0) | 8.9 (1.4) | 9.6 (1.1) | 6.4 (1.3) | 7.8 (1.0) | |
| Others | 11.0 (0.8) | 8.0 (1.2) | 10.4 (1.4) | 8.0 (1.1) | 11.0 (0.8) | |
| Smokers, % | 20.9 (1.2) | 5.4 (1.1) | 6.2 (1.4) | 7.0 (1.0) | 62.2 (2.2) | < 0.001 |
| Marriage, % | 63.9 (1.1) | 67.8 (1.7) | 67.3 (2.8) | 67.8 (2.1) | 53.6 (1.8) | < 0.001 |
| Education levels, % | < 0.001 | |||||
| Under high school | 17.1 (1.1) | 17.6 (1.5) | 14.5 (1.5) | 15.1 (1.7) | 21.0 (2.0) | |
| High school | 25.0 (1.1) | 23.4 (2.2) | 22.4 (2.2) | 23.2 (1.8) | 30.5 (1.9) | |
| Above high school | 58.0 (1.5) | 59.0 (1.8) | 63.1 (2.4) | 61.6 (2.3) | 48.6 (2.7) | |
| Family PIR | 3.07 ± 0.04 | 2.96 ± 0.06 | 3.15 ± 0.06 | 3.31 ± 0.06 | 2.86 ± 0.06 | < 0.001 |
| Body mass index, kg/m2 | 29.09 ± 0.16 | 29.61 ± 0.22 | 29.64 ± 0.30 | 28.72 ± 0.35 | 28.46 ± 0.30 | 0.036 |
| Systolic blood pressure, mmHg | 123.23 ± 0.47 | 125.15 ± 0.81 | 123.6 ± 0.85 | 122.34 ± 1.11 | 122.07 ± 0.74 | 0.059 |
| Diastolic blood pressure, mmHg | 70.08 ± 0.32 | 70.41 ± 0.90 | 69.88 ± 0.53 | 70.27 ± 0.52 | 69.81 ± 0.60 | 0.846 |
| Albumin, g/L | 42.25 ± 0.10 | 42.23 ± 0.17 | 42.14 ± 0.15 | 42.34 ± 0.13 | 42.27 ± 0.15 | 0.708 |
| Alanine aminotransferase, U/L | 25.26 ± 0.54 | 24.97 ± 1.42 | 24.92 ± 0.68 | 26.37 ± 0.54 | 24.78 ± 0.48 | 0.151 |
| γ-Glutamyl transpeptidase, U/L | 25.64 ± 0.54 | 26.58 ± 1.11 | 24.73 ± 1.11 | 25.02 ± 1.06 | 26.29 ± 1.16 | 0.420 |
| Fasting triglyceride, mg/dl | 139.79 ± 2.60 | 144.28 ± 5.49 | 144.94 ± 5.71 | 124.59 ± 4.06 | 145.45 ± 6.16 | 0.008 |
| Total cholesterol, mmol/L | 5.15 ± 0.03 | 5.14 ± 0.05 | 5.19 ± 0.06 | 5.14 ± 0.04 | 5.14 ± 0.05 | 0.883 |
| HDL-C, mmol/L | 1.40 ± 0.01 | 1.39 ± 0.02 | 1.42 ± 0.02 | 1.47 ± 0.02 | 1.31 ± 0.02 | < 0.001 |
| LDL-C, mmol/L | 3.00 ± 0.02 | 2.94 ± 0.03 | 3.00 ± 0.04 | 2.99 ± 0.04 | 3.06 ± 0.04 | 0.165 |
| Platelet count, 1000 cells/μL | 259.26 ± 1.86 | 252.75 ± 2.67 | 258.53 ± 4.10 | 259.82 ± 2.46 | 265.19 ± 3.12 | 0.047 |
| Fasting blood glucose, mmol/L | 5.82 ± 0.04 | 5.98 ± 0.05 | 5.88 ± 0.08 | 5.68 ± 0.05 | 5.77 ± 0.08 | 0.002 |
| Total energy intake, kcal | 2150.57 ± 20.29 | 2001.84 ± 29.72 | 2111.09 ± 48.95 | 2165.01 ± 27.59 | 2305.21 ± 41.17 | < 0.001 |
| Total fat intake, gm | 84.14 ± 0.84 | 78.44 ± 1.42 | 82.01 ± 2.06 | 85.92 ± 1.85 | 89.45 ± 1.9 | < 0.001 |
| HbGA/HbAA | 0.95 ± 0.02 | 1.04 ± 0.05 | 0.98 ± 0.02 | 0.95 ± 0.02 | 0.82 ± 0.02 | < 0.001 |
| USFLI | 24.04 ± 0.46 | 26.61 ± 0.76 | 25.89 ± 1.03 | 21.52 ± 1.03 | 22.4 ± 0.83 | 0.002 |
| NAFLD, % | 30.8 (1.0) | 34.7 (1.8) | 34.0 (2.2) | 25.4 (1.8) | 29.5 (1.8) | 0.001 |
| Subgroup, NAFLD prevalence | ||||||
| BMI | ||||||
| < 30 kg/m2 | 13.1 (0.8) | 14.5 (1.9) | 15.5 (1.9) | 9.8 (1.1) | 13.0 (1.4) | 0.056 |
| ≥ 30 kg/m2 | 61.8 (1.7) | 65.4 (2.5) | 61.5 (3.7) | 57.4 (3.1) | 62.4 (3.7) | 0.408 |
| ALT | ||||||
| ≤ 40 U/L | 26.9 (1.0) | 29.9 (2.0) | 29.7 (2.2) | 20.7 (1.7) | 27.2 (1.8) | 0.002 |
| > 40 U/L | 69.1 (2.6) | 81.4 (5.1) | 75.0 (6.0) | 63.6 (5.6) | 56.4 (6.9) | 0.016 |
Participants were classified into quartiles according to HbAA levels: Q1, HbAA ≤ 36.10 pmol/g Hb; Q2, 36.10 < HbAA ≤ 47.60 pmol/g Hb; Q3, 47.60 < HbAA ≤ 66.50 pmol/g Hb; and Q4, HbAA > 66.50 pmol/g Hb
Continuous variables were presented as the weighted mean ± SE and compared by Survey regression models
Categorical variables were presented as weighted percent (SE) and compared by using the Rao–Scott χ2 test
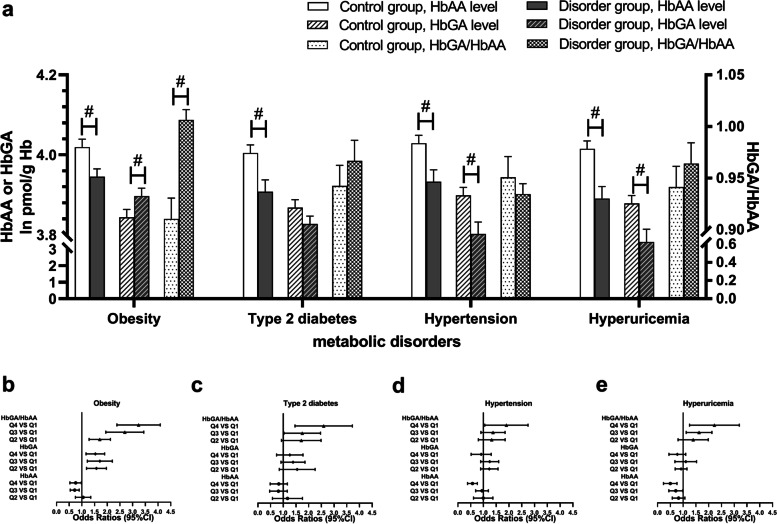
Obesity and related metabolic disorders, including type 2 diabetes, hypertension, and hyperuricemia, are all significantly associated with NAFLD as previously reported [31, 32]. Therefore, we explored the association between AA biomarkers and these metabolic disorders. As shown in Fig. 2a, HbAA concentrations were significantly lower in all disorder groups than in healthy controls. On the contrary, HbGA levels were significantly higher in the obese group but lower in hypertension and hyperuricemia groups. Correspondingly, a significantly higher ratio of HbGA and HbAA was discovered in the obese group. Further logistic regression analyses (Fig. 2b-e) revealed negative relationships between metabolic disorders and HbAA. Conversely, the HbGA/HbAA ratio showed a significantly positive relationship. These results suggested a close association between AA biomarkers and metabolic disorders.
Fig. 2.
HbAA and HbGA levels in participants with metabolic disorders. a HbAA, HbGA levels (loge transformed) and their ratio (HbGA/HbAA) in both case groups and control groups. b-e Association of AA biomarkers with the risk of metabolic disorders after adjusting for age, gender, race/ethnicity, education levels, family PIR, marital status, serum cotinine level, total fat intake, total energy intake, serum albumin, LDL-cholesterol, total cholesterol and blood platelet count. #: P < 0.01, compared by Survey regression models
We next performed complex sample logistic regression analysis with increasing degrees of adjustment to explore the associations between HbAA, HbGA, or HbGA/HbAA and NAFLD (Table 2). In a minimally adjusted model with demographic factors taken in, the estimated risk of NAFLD decreased with increasing HbAA quartiles (P for trend = 0.001). The ORs (95% CIs) of the increasing quartiles were 0.96 (0.73–1.25), 0.66 (0.52–0.85), and 0.69 (0.52–0.91) compared with the lowest quartile. Consistently, this negative association remained significant after adjustment for risk factors in model 2 [ORs (95% CIs): 0.92 (0.70–1.21), 0.65 (0.50–0.85), and 0.64 (0.48–0.84); P for trend < 0.001] and model 3 [ORs (95% CIs): 0.90 (0.68–1.19), 0.65 (0.49–0.85), and 0.61 (0.46–0.81); P for trend < 0.001]. In contrast, HbGA/HbAA showed a significantly positive correlation with the risk of NAFLD in model 1 [ORs (95% CIs): 1.69 (1.34–2.13), 2.47 (2.02–3.02), and 2.77 (2.15–3.57); P for trend < 0.001]. Similarly, this association remained significant after adjustment for risk factors in model 2 [ORs (95% CIs): 1.60 (1.25–2.04), 2.24 (1.84–2.73), and 2.72 (2.09–3.53); P for trend < 0.001] or model 3 [ORs (95% CIs): 1.68 (1.34–2.11), 2.33 (1.85–2.94), and 2.72 (2.06–3.58); P for trend < 0.001]. In addition, we did not find a significant association between HbGA and the risk of NAFLD in the adjusted models. In mediation analysis (Table 3), we found that BMI was estimated to explain 59.0% (95%CI: 42.4%–73.8%, P < 0.001) of the association between HbAA and NAFLD, while fasting glucose and insulin level could explain 20.5% (95%CI: 13.5%–29.8%, P < 0.001) and 68.8% (95%CI: 45.6%–85.2%, P < 0.001), respectively. However, no significant intermediating effect was found for blood pressure. Taken together, HbAA is negatively, whereas HbGA/HbAA is positively, associated with the risk of NAFLD. BMI and insulin mediated the relationship between AA and NAFLD.
Table 2.
Association of AA exposure with the risk of NAFLD in whole group (n = 3234)
| HbAA | HbGA | HbGA/HbAA | ||||
|---|---|---|---|---|---|---|
| OR (95%CI) | Ptrend | OR (95%CI) | Ptrend | OR (95%CI) | Ptrend | |
| Model 1 | 0.001 | 0.145 | < 0.001 | |||
| Q1 (reference) | ||||||
| Q2 | 0.96 (0.73–1.25) | 1.24 (0.88–1.74) | 1.69 (1.34–2.13) | |||
| Q3 | 0.66 (0.52–0.85) | 1.27 (0.95–1.70) | 2.47 (2.02–3.02) | |||
| Q4 | 0.69 (0.52–0.91) | 1.28 (0.98–1.67) | 2.77 (2.15–3.57) | |||
| Model 2 | < 0.001 | 0.262 | < 0.001 | |||
| Q1 (reference) | ||||||
| Q2 | 0.92 (0.70–1.21) | 1.25 (0.89–1.76) | 1.60 (1.25–2.04) | |||
| Q3 | 0.65 (0.50–0.85) | 1.22 (0.88–1.70) | 2.24 (1.84–2.73) | |||
| Q4 | 0.64 (0.48–0.84) | 1.24 (0.93–1.64) | 2.72 (2.09–3.53) | |||
| Model 3 | < 0.001 | 0.998 | < 0.001 | |||
| Q1 (reference) | ||||||
| Q2 | 0.90 (0.68–1.19) | 1.07 (0.76–1.49) | 1.68 (1.34–2.11) | |||
| Q3 | 0.65 (0.49–0.85) | 1.10 (0.79–1.53) | 2.33 (1.85–2.94) | |||
| Q4 | 0.61 (0.46–0.81) | 1.15 (0.85–1.55) | 2.72 (2.06–3.58) | |||
Quartiles of HbAA: Q1, HbAA ≤ 36.10 pmol/g Hb; Q2, 36.10 < HbAA ≤ 47.60 pmol/g Hb; Q3, 47.60 < HbAA ≤ 66.50 pmol/g Hb; and Q4, HbAA > 66.50 pmol/g Hb
Quartiles of HbGA: Q1, HbGA ≤ 32.30 pmol/g Hb; Q2, 32.30 < HbGA ≤ 44.90 pmol/g Hb; Q3, 44.90 < HbGA ≤ 65.00 pmol/g Hb; and Q4, HbGA > 65.00 pmol/g Hb
Quartiles of HbGA/HbAA: Q1, ≤ 0.732; Q2, 0.732 < HbGA/HbAA ≤ 0.895; Q3, 0.895 < HbGA/HbAA ≤ 1.091; and Q4, HbGA/HbAA > 1.091
Model 1 was adjusted for demographic factors (age, gender, race/ethnicity, education levels, family PIR, marital status, and serum cotinine level)
Model 2 was adjusted for model 1 plus total fat intake and total energy intake
Model 3 was further adjusted for model 2 plus biochemistry factors (serum albumin, LDL-cholesterol, total cholesterol and blood platelet count)
Table 3.
Results of mediation analysis between HbAA and NAFLD
| Mediator | Proportion (%) of effect due to mediation (95% CI) | P value |
|---|---|---|
| Body fat index | 59.0% (42.4%–73.8%) | < 0.001 |
| Fasting glucose | 20.5% (13.5%–29.8%) | < 0.001 |
| Fasting insulin | 68.8% (45.6%–85.2%) | < 0.001 |
| Blood pressurea | 2.3% (0.2%–24.8%) | 0.226 |
aBlood pressure was denoted as mean arterial pressure
The results of subgroup analyses are shown in Table 4. There was no particular subgroup that showed the strongest negative association between HbAA and NAFLD in socio-economic factors. However, liver function (evaluated by ALT) was detected as a significant modifier for the association (P for interaction < 0.001). Stronger negative associations of HbAA with NAFLD were detected among people who had elevated ALT levels [ORQ4vsQ1: 0.74 (0.54–1.01) for ALT ≤ 40 U/L and 0.32 (0.11–0.93) for ALT > 40 U/L].
Table 4.
Odds ratios for associations between HbAA and NAFLD in subgroups
| Subgroups | HbAA quartile (pmol/g Hb)a | Ptrend | Pinteraction | ||
|---|---|---|---|---|---|
| Q2 (36.10 < HbAA ≤ 47.60) | Q3 (47.60 < HbAA ≤ 66.50) | Q4 (HbAA > 66.50) | |||
| Age | 0.130 | ||||
| ≤ 50 years | 0.93 (0.56–1.55) | 0.80 (0.51–1.26) | 0.66 (0.41–1.06) | 0.032 | |
| > 50 years | 0.87 (0.66–1.13) | 0.51 (0.37–0.70) | 0.51 (0.34–0.78) | 0.001 | |
| Gender | 0.717 | ||||
| Male | 0.95 (0.68–1.31) | 0.75 (0.48–1.16) | 0.64 (0.36–1.11) | 0.102 | |
| Female | 0.86 (0.60–1.23) | 0.55 (0.39–0.75) | 0.60 (0.36–1.01) | 0.003 | |
| Race | 0.006 | ||||
| Non-Hispanic white | 0.82 (0.56–1.19) | 0.56 (0.41–0.78) | 0.51 (0.37–0.72) | < 0.001 | |
| Non-Hispanic black | 1.03 (0.40–2.65) | 1.06 (0.46–2.41) | 0.58 (0.28–1.18) | 0.228 | |
| Mexican American | 0.77 (0.40–1.51) | 0.46 (0.26–0.83) | 0.69 (0.31–1.56) | 0.115 | |
| Education levels | 0.895 | ||||
| Under high school | 1.57 (0.76–3.24) | 0.63 (0.34–1.16) | 0.80 (0.52–1.21) | 0.017 | |
| High school | 0.95 (0.55–1.62) | 0.66 (0.39–1.11) | 0.63 (0.30–1.34) | 0.131 | |
| Above high school | 0.76 (0.49–1.19) | 0.64 (0.42–0.98) | 0.53 (0.35–0.78) | 0.005 | |
| Married | 0.887 | ||||
| No | 1.00 (0.67–1.47) | 0.59 (0.36–0.98) | 0.65 (0.45–0.92) | 0.007 | |
| Yes | 0.87 (0.63–1.22) | 0.67 (0.49–0.90) | 0.60 (0.42–0.88) | 0.006 | |
| ALT | < 0.001 | ||||
| ≤ 40 U/L | 0.96 (0.69–1.34) | 0.62 (0.45–0.86) | 0.74 (0.54–1.01) | 0.006 | |
| > 40 U/L | 0.45 (0.16–1.28) | 0.36 (0.19–0.66) | 0.32 (0.11–0.93) | 0.014 | |
aORs were compared to quartile1 (HbAA ≤ 36.10 pmol/g Hb), adjusted for full model
It has been reported that dietary intake and smoking are generally two important non-occupational sources of AA. To exclude the confounding influence of smoking and to focus on dietary factors, we confined the analysis to the non-smoker group (serum cotinine level ≤ 10 ng/ml) [33]. Similar to the whole group, a negative association between HbAA and NAFLD and a positive association between HbGA/HbAA and NAFLD were found in model 1 and model 2 (Table 5). After adjustment for covariables in model 3, the significant associations remained in the HbAA and HbGA/HbAA groups [ORs (95% CIs): 0.79 (0.63–0.99), 0.72 (0.52–0.99), and 0.57 (0.36–0.88), P for trend = 0.014; 1.77 (1.26–2.49), 2.54 (1.71–3.75), and 3.31 (2.18–5.03), P for trend < 0.001, respectively]. However, we did not observe a significant association between HbGA and NAFLD in the non-smoker group in model 3. To conclude, AA biomarkers remained related to NAFLD in the non-smoker group.
Table 5.
Association of AA exposure with risk of NAFLD in non-smokers (n = 2620)
| HbAA | HbGA | HbGA/HbAA | ||||
|---|---|---|---|---|---|---|
| OR (95%CI) | Ptrend | OR (95%CI) | Ptrend | OR (95%CI) | Ptrend | |
| Model 1 | 0.006 | 0.111 | < 0.001 | |||
| Q1 (reference) | ||||||
| Q2 | 0.80 (0.64–1.00) | 0.93 (0.74–1.15) | 1.86 (1.38–2.50) | |||
| Q3 | 0.78 (0.58–1.05) | 1.12 (0.93–1.34) | 2.63 (1.93–3.59) | |||
| Q4 | 0.57 (0.40–0.82) | 1.20 (0.88–1.64) | 3.42 (2.40–4.87) | |||
| Model 2 | 0.004 | 0.205 | < 0.001 | |||
| Q1 (reference) | ||||||
| Q2 | 0.79 (0.62–1.00) | 0.93 (0.74–1.18) | 1.85 (1.34–2.56) | |||
| Q3 | 0.72 (0.52–0.99) | 1.08 (0.87–1.34) | 2.61 (1.85–3.68) | |||
| Q4 | 0.54 (0.36–0.81) | 1.18 (0.84–1.65) | 3.64 (2.44–5.44) | |||
| Model 3 | 0.014 | 0.325 | < 0.001 | |||
| Q1 (reference) | ||||||
| Q2 | 0.79 (0.63–0.99) | 0.79 (0.60–1.04) | 1.77 (1.26–2.49) | |||
| Q3 | 0.72 (0.52–0.99) | 0.95 (0.76–1.18) | 2.54 (1.71–3.75) | |||
| Q4 | 0.57 (0.36–0.88) | 1.08 (0.80–1.45) | 3.31 (2.18–5.03) | |||
Quartiles of HbAA: Q1, ≤ 35.00 pmol/g Hb; Q2, 35.00 < HbAA ≤ 44.20 pmol/g Hb; Q3, 44.20 < HbAA ≤ 55.60 pmol/g Hb; and Q4, > 55.60 pmol/g Hb
Quartiles of HbGA: Q1, ≤ 30.30 pmol/g Hb; Q2, 30.30 < HbGA ≤ 41.00 pmol/g Hb; Q3, 41.00 < HbGA ≤ 55.50 pmol/g Hb; and Q4, > 55.50 pmol/g Hb
Quartiles of HbGA/HbAA: Q1, ≤ 0.768; Q2, 0.768 < HbGA/HbAA ≤ 0.926; Q3, 0.926 < HbGA/HbAA ≤ 1.118; and Q4, > 1.118
Model 1 was adjusted for demographic factors (age, gender, race/ethnicity, education levels, family PIR, and marital status)
Model 2 was adjusted for model 1 plus total fat intake and total energy intake
Model 3 was further adjusted for model 2 plus biochemistry factors (serum albumin, LDL-cholesterol, total cholesterol and blood platelet count)
Discussion
To the best of our knowledge, this is the first study to focus on the association between acrylamide hemoglobin adducts and NAFLD in a representative sample of American adults. The overall prevalence of NAFLD was 30.8%, which is consistent with the prevalence of NAFLD in the U.S. adult population [1]. In this study, we found a negative correlation of serum HbAA levels with NAFLD as well as with metabolic disorders. We also found that the HbAA level remained negatively associated with the risk of NAFLD, yet the HbGA/HbAA level was positively associated with the risk of NAFLD, in the whole group after adjustment for socio-demographic factors, lifestyle factors, and risk factors. Besides, our results showed that HbGA was not significantly associated with the risk of NALFD in the adjusted models.
The neurotoxicity, genotoxicity, and reproductive toxicity of AA have been well demonstrated by previous studies [34–36]. The effects of AA are mediated by the formation of genotoxic metabolites, oxidative stress, affected propagation of neural signals, and interrupted endocrine hormones [37]. In recent years, evidence on its hepatotoxicity has been reported, for the liver is the main site of AA biotransformation. Sun et al. reported that when rats were intraperitoneally injected with 40 mg/kg AA for four weeks, the levels of serum ALT and AST were markedly higher in the treated group than in the normal control group [38]. Additionally, AA (20 mg/kg) increased the levels of liver oxidative stress markers, including protein carbonyl content, nitric oxide, and lipid peroxides, but markedly decreased the activity of liver antioxidants, including superoxide dismutase (SOD) and glutathione peroxidase (GSH-Px). The imbalance between antioxidants and oxidative stress caused the increase of inflammatory markers such as NF-κB, TNF-α, and IL-1β [39, 40]. Furthermore, these stress factors might induce a rapid decline in hepatocyte mitochondrial membrane potential as well as an increase in the activity of caspase-3, the final mediator of apoptosis [41].
However, the results mentioned above were based on AA doses far higher than those the general population is exposed to in daily life. The median HbAA level in our study was 50.6 pmol/g Hb, equivalent to a total uptake of 2 µg/kg body weight/day according to the pharmacokinetics parameters proposed by Calleman [42]. In terms of exposure via food, U.S. Food and Drug Administration (FDA) investigators estimated that the mean and 90th percentile of daily dietary AA exposure of the U.S. population were 0.44 and 0.95 µg/kg body weight [43]. In contrast, it was reported by the Joint Expert Committee on Food Additives (JECFA) that the no observed adverse effect level (NOAEL) of AA for a non-carcinogenic end-point was 0.2 mg/kg body weight/day. According to the above standard, Liu et al. did not discover any toxic effect on rat livers from the metabolic perspective after chronic exposure to AA at NOAEL for 16 weeks [44]. Moreover, in October 2000, the National Toxicology Program (NTP) organized an independent and open peer review and proposed a concept of “low-dose effects,” which referred to the biological changes that occur in the range of human exposures or at doses lower than those typically used in the standard testing paradigm for evaluating reproductive and developmental toxicity [45]. Therefore, whether long-term, low-dose exposure to AA has negative effects on human health needs further investigation.
In recent years, a consensus-driven term “metabolic-associated fatty liver disease” (MAFLD) has been proposed to refine the scope of NAFLD [46]. This updated nomenclature better reflects the underlying metabolic dysfunction that primarily drives this disease [47]. Accordingly, there are some cross-sectional studies utilizing the NHANES database to investigate the relationships between AA and metabolic dysfunction. HbAA was found to be inversely associated with obesity and android fat mass with statistical significance [12, 48]. In addition, Lin et al. [20] reported that increased HbAA was associated with decreased levels of blood insulin and the insulin resistance status in adults. Similarly, we also discovered a negative association between HbAA and the prevalence of metabolic disorders. Since the elements above are common comorbidities of NAFLD, it is reasonable that HbAA was negatively associated with NAFLD in our findings. Indeed, AA has been considered as a potential endocrine-disrupting chemical (EDC) related to various metabolic abnormalities [11]. However, rather than a traditional threshold model or a linear non-threshold model, EDCs may show a U-shaped dose–response curve, commonly called hormesis [49], which means it exhibits a change in the sign of its first derivative [50]. As mentioned above, people’s normal daily exposure to AA is far lower than the NOAEL, and may be located at the decreasing interval of the curves [51]. Grünwald et al. [52] reported that compared with the control group fed flour only, beetles fed flour enriched with 5% charred toast (providing AA) survived significantly longer. This increased stress resistance might result from the activation of arylhydrocarbon receptor (AHR) and nuclear factor erythroid 2-related factor 2 (NRF-2). Nevertheless, the underlying mechanisms need further elucidation.
CYP2E1 plays a crucial role in AA metabolism, and scientists have identified a complex interplay between CYP2E1 and NAFLD [7]. On the one hand, liver CYP2E1 level is inducible, and can be upregulated by high levels of fatty acids, low levels of adiponectin, and the status of insulin resistance [53, 54], which all pathophysiologically characterize NAFLD. Thus, NAFLD patients are likely to have increased CYP2E1 expression and activity [55]. On the other hand, this association can go both ways, that is, higher CYP2E1 activity could also favor liver injury. For example, enhanced enzymatic activity of CYP2E1 promoted reactive oxidative stress (ROS) production, resulting in oxidative stress and hepatic steatosis in mice and LO2 cells [56]. In addition, ROS induced mitochondrial dysfunction, a major risk factor in the development of NAFLD, through post-translational protein modifications and mitochondrial DNA damage [57, 58]. O’Shea et al. observed that two pharmacokinetic parameters, mean oral clearance and apparent volume of distribution of chlorzoxazone (mediated primarily by CYP2E1), were about 50% greater in the obese group, consistent with the induction of CYP2E1. Accordingly, such individuals may be at an increased risk of CYP2E1-mediated toxicities and adverse effects [59]. Correspondingly, we found in this study that HbGA/HbAA, which reflects the extent of AA biotransformation, was positively associated with NAFLD in the fully adjusted model. Previous studies reported that the metabolic conversion rate of AA to GA was saturated at low doses because of the saturated activity of CYP2E1 enzyme [60, 61]. This indicated that HbGA/HbAA correlated negatively to HbAA, so the inverse association between HbAA and NAFLD in this study could be a reflection of CYP2E1 activity without AA itself playing a causative role. Ghanayem et al. reported that AA-induced genotoxicity was absent in CYP2E1-null mice [62]. As a result, CYP2E1 is considered to be responsible for AA-related hepatotoxicity.
In addition to CYP2E1, other possible enzymes responsible for AA degradation include microbial amidases, which catalyze the hydrolysis of AA to ammonia and acrylic acid [63]. Amidases also play an important role in cell proliferation. It is noteworthy that some native microbes in the intestines, such as Escherichia coli and Enterococcus faecalis, may present this potential [64]. There is mounting evidence that the gut and the liver have multiple interactions with each other, and disturbance of the gut–liver axis is linked to NAFLD via complicated mechanisms [65]. Despite a lack of studies that focused on how AA impacts gut microbiota, we believe that it will be a novel research direction.
In subgroup analyses, we revealed a stronger reverse association between HbAA and NAFLD in the elevated ALT (> 40U/L) group. Assay of the serum ALT level has become a primary screening method for liver injury [66]. According to the “multiple hit” hypothesis, NAFLD is a complex disease with multiple insults acting together [67]. Therefore, we may keep an eye on the AA level of people with liver dysfunction so as to avoid an extra hit by AA.
Although we used a large-scale, quality-controlled database to draw conclusions, there exist some limitations in our study. First, owing to the cross-sectional nature of this study, it was not possible to infer directly which factor came first. In this study, we discovered a negative association between HbAA and NAFLD. However, it seems more reasonable that this association is a reflection of the CYP2E1 activity, that is, HbGA/HbAA, rather than an indication that AA is responsible for the development of NAFLD. Regretfully, we did not acquire the information about the expression or polymorphisms of CYP2E1 in the current study population. Furthermore, French fries and processed cereal-grain-based foods were discovered to be the greatest contributors to dietary AA intake, while fresh vegetables and fruits were just the opposite [43]. As restricting high-carbohydrate foods and consuming more vegetables and fruits are recommended for NAFLD patients [68], another possible explanation for the negative association is that people with NAFLD might have followed dietary advice to restrict the consumption of foods containing AA. Second, NAFLD was determined by socio-demographical data and blood biomarker values, in which misclassification bias might be inevitable. In addition, to avoid overcorrection, we had to exclude overweight and diabetes classifications from the regression models, although it would be of interest to assess whether these conditions mediated the association between AA and NAFLD. Third, AA Hb biomarkers can only reflect the exposure level within 120 days, which is not long enough to estimate the cumulative effect of AA exposure across several years [8]. Therefore, further long-term cohort studies should be employed to elucidate these relationships.
Conclusion
In conclusion, we reported that HbAA was negatively and HbGA/HbAA was positively associated with NAFLD in the U.S. population, independently of traditional NAFLD risk factors. Further studies are needed to clarify the relationships between them.
Acknowledgements
We thank members of the National Center for Health Statistics (NCHS) of the Centers for Disease Control (CDC) and Prevention and the participants who enrolled in the National Health and Nutrition Examination Survey.
Abbreviations
- AA
Acrylamide
- ALT
Alanine aminotransferase
- BMDL10
Benchmark dose lower confidence limit
- BMI
Body mass index
- CI
Confidence interval
- EDC
Endocrine-disrupting chemical
- EFSA
European food safety authority
- FDA
Food and Drug Administration
- GA
Glycidamide
- GGT
Gamma glutamyl transferase
- GSH
Glutathione
- Hb
Hemoglobin
- HbA1c
Glycated hemoglobin
- HbAA
Hemoglobin adducts of acrylamide
- HbGA
Hemoglobin adducts of glycidamide
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HDL-C
High density lipoprotein cholesterol
- HPLC/MS/MS
High-performance liquid chromatography tandem mass spectrometry
- JECFA
Joint Expert Committee on Food Additives
- LDL-C
Low density lipoprotein cholesterol
- MOE
Margin of exposure
- NAFLD
Non-alcoholic fatty liver disease
- NHANES
National Health and Nutrition Examination Survey
- NOAEL
No observed adverse effect level
- NTP
National Toxicology Program
- OR
Odds ratio
- PIR
Income-to-poverty ratio
- ROS
Reactive oxidative stress
- SOD
Superoxide dismutase
- T2DM
Type 2 diabetes mellitus
- TG
Triglyceride
- US FLI
U.S. fatty liver index
Authors’ contributions
ZL: Conceptualization, Formal analysis, Software, Writing—Original Draft. JW: Formal analysis, Software. SC: Data Curation. CX: Project administration, Funding acquisition, and Supervision. YZ: Conceptualization, Supervision. The author(s) read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China, grant number 81722009 and 81770573.
Availability of data and materials
The datasets analyzed during the current study are available in the NHANES repository, https://wwwn.cdc.gov/nchs/nhanes/default.aspx.
Declarations
Ethics approval and consent to participate
NHANES was approved by NCHS Research Ethics Review Board. More details on https://www.cdc.gov/nchs/nhanes/irba98.htm.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Zhening Liu, Email: liuzn@zju.edu.cn.
Jinghua Wang, Email: jinghuajing614@163.com.
Shenghui Chen, Email: chensheng0805@163.com.
Chengfu Xu, Email: xiaofu@zju.edu.cn.
Yu Zhang, Email: y_zhang@zju.edu.cn.
References
- 1.Younossi Z, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20. doi: 10.1038/nrgastro.2017.109. [DOI] [PubMed] [Google Scholar]
- 2.Marchesini G, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003;37(4):917–923. doi: 10.1053/jhep.2003.50161. [DOI] [PubMed] [Google Scholar]
- 3.Kallwitz ER, et al. Prevalence of suspected nonalcoholic fatty liver disease in Hispanic/Latino individuals differs by heritage. Clin Gastroenterol Hepatol. 2015;13(3):569–576. doi: 10.1016/j.cgh.2014.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bergmark E. Hemoglobin adducts of acrylamide and acrylonitrile in laboratory workers, smokers and nonsmokers. Chem Res Toxicol. 1997;10(1):78–84. doi: 10.1021/tx960113p. [DOI] [PubMed] [Google Scholar]
- 5.Mottram DS, Wedzicha BL, Dodson AT. Acrylamide is formed in the Maillard reaction. Nature. 2002;419(6906):448–449. doi: 10.1038/419448a. [DOI] [PubMed] [Google Scholar]
- 6.Moldoveanu SC, Gerardi AR. Acrylamide analysis in tobacco, alternative tobacco products, and cigarette smoke. J Chromatogr Sci. 2011;49(3):234–242. doi: 10.1093/chrsci/49.3.234. [DOI] [Google Scholar]
- 7.Li D, et al. Metabolism of acrylamide: interindividual and interspecies differences as well as the application as biomarkers. Curr Drug Metab. 2016;17(4):317–326. doi: 10.2174/1389200216666151015115007. [DOI] [PubMed] [Google Scholar]
- 8.Bergmark E, et al. Determination of hemoglobin adducts in humans occupationally exposed to acrylamide. Toxicol Appl Pharmacol. 1993;120(1):45–54. doi: 10.1006/taap.1993.1085. [DOI] [PubMed] [Google Scholar]
- 9.IARC . Monographs on the evaluation for carcinogenic risk of chemicals to humans. 1994. Some industrial chemicals; pp. 435–453. [PMC free article] [PubMed] [Google Scholar]
- 10.Stadler RH, et al. Food chemistry: acrylamide from Maillard reaction products. Nature. 2002;419(6906):449–450. doi: 10.1038/419449a. [DOI] [PubMed] [Google Scholar]
- 11.Matoso V, et al. Acrylamide: a review about its toxic effects in the light of Developmental Origin of Health and Disease (DOHaD) concept. Food Chem. 2019;283:422–430. doi: 10.1016/j.foodchem.2019.01.054. [DOI] [PubMed] [Google Scholar]
- 12.Huang M, et al. Association of acrylamide hemoglobin biomarkers with obesity, abdominal obesity and overweight in general US population: NHANES 2003–2006. Sci Total Environ. 2018;631–632:589–596. doi: 10.1016/j.scitotenv.2018.02.338. [DOI] [PubMed] [Google Scholar]
- 13.Li L, et al. Obesity is an independent risk factor for non-alcoholic fatty liver disease: evidence from a meta-analysis of 21 cohort studies. Obes Rev. 2016;17(6):510–519. doi: 10.1111/obr.12407. [DOI] [PubMed] [Google Scholar]
- 14.Polyzos SA, Kountouras J, Mantzoros CS. Obesity and nonalcoholic fatty liver disease: from pathophysiology to therapeutics. Metabolism. 2019;92:82–97. doi: 10.1016/j.metabol.2018.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Leung JC-F, et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology. 2017;65(1):54–64. doi: 10.1002/hep.28697. [DOI] [PubMed] [Google Scholar]
- 16.Berzigotti A, et al. Obesity is an independent risk factor for clinical decompensation in patients with cirrhosis. Hepatology. 2011;54(2):555–561. doi: 10.1002/hep.24418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ioannou GN, et al. Is obesity a risk factor for cirrhosis-related death or hospitalization? A population-based cohort study. Gastroenterology. 2003;125(4):1053–1059. doi: 10.1016/S0016-5085(03)01200-9. [DOI] [PubMed] [Google Scholar]
- 18.Mantovani A, et al. Nonalcoholic fatty liver disease and risk of incident type 2 diabetes: a meta-analysis. Diabetes Care. 2018;41(2):372–382. doi: 10.2337/dc17-1902. [DOI] [PubMed] [Google Scholar]
- 19.Titchenell PM, Lazar MA, Birnbaum MJ. Unraveling the regulation of hepatic metabolism by insulin. Trends Endocrinol Metab. 2017;28(7):497–505. doi: 10.1016/j.tem.2017.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lin CY, et al. Association among acrylamide, blood insulin, and insulin resistance in adults. Diabetes Care. 2009;32(12):2206–2211. doi: 10.2337/dc09-0309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yin G, et al. Association of acrylamide and glycidamide haemoglobin adduct levels with diabetes mellitus in the general population. Environ Pollut. 2021;277:116816. doi: 10.1016/j.envpol.2021.116816. [DOI] [PubMed] [Google Scholar]
- 22.Yue Z, et al. Effect of acrylamide on glucose homeostasis in female rats and its mechanisms. Food Chem Toxicol. 2020;135:110894. doi: 10.1016/j.fct.2019.110894. [DOI] [PubMed] [Google Scholar]
- 23.2003–2004 data documentation, codebook, and frequencies acrylamide & glycidamide. Available from: https://wwwn.cdc.gov/Nchs/Nhanes/2003-2004/L06AGE_C.htm#Description_of_Laboratory_Methodology. Accessed 25 Jan 2020.
- 24.Ruhl CE, Everhart JE. Fatty liver indices in the multiethnic United States national health and nutrition examination survey. Aliment Pharmacol Ther. 2015;41(1):65–76. doi: 10.1111/apt.13012. [DOI] [PubMed] [Google Scholar]
- 25.Yanovski SZ, Yanovski JA. Obesity prevalence in the United States — up, down, or sideways? N Engl J Med. 2011;364(11):987–989. doi: 10.1056/NEJMp1009229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chobanian AV, et al. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 27.American Diabetes Association 2. Classification and diagnosis of diabetes. Diabetes Care. 2016;39(Suppl 1):S13–22. doi: 10.2337/dc16-S005. [DOI] [PubMed] [Google Scholar]
- 28.Bardin T, Richette P. Definition of hyperuricemia and gouty conditions. Curr Opin Rheumatol. 2014;26(2):186–191. doi: 10.1097/BOR.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 29.NHANES tutorials - module 7 - hypothesis testing. Available from: https://wwwn.cdc.gov/nchs/nhanes/tutorials/Module7.aspx. Accessed 26 Jan 2020.
- 30.%mediate | Donna Spiegelman | Harvard T.H. Chan School of Public Health. Available from: https://www.hsph.harvard.edu/donna-spiegelman/software/mediate/. Accessed 25 Apr 2021.
- 31.Younossi ZM, et al. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. doi: 10.1002/hep.28431. [DOI] [PubMed] [Google Scholar]
- 32.Dietrich P, Hellerbrand C. Non-alcoholic fatty liver disease, obesity and the metabolic syndrome. Best Pract Res Clin Gastroenterol. 2014;28(4):637–653. doi: 10.1016/j.bpg.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 33.Vesper HW, et al. Among 10 sociodemographic and lifestyle variables, smoking is strongly associated with biomarkers of acrylamide exposure in a representative sample of the U.S. population. J Nutr. 2013;143(6):995S–1000S. doi: 10.3945/jn.112.173013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tyl RW, Friedman MA. Effects of acrylamide on rodent reproductive performance. Reprod Toxicol. 2003;17(1):1–13. doi: 10.1016/S0890-6238(02)00078-3. [DOI] [PubMed] [Google Scholar]
- 35.Carere A. Genotoxicity and carcinogenicity of acrylamide: a critical review. Ann Ist Super Sanita. 2006;42(2):144–155. [PubMed] [Google Scholar]
- 36.Erkekoglu P, Baydar T. Acrylamide neurotoxicity. Nutr Neurosci. 2014;17(2):49–57. doi: 10.1179/1476830513Y.0000000065. [DOI] [PubMed] [Google Scholar]
- 37.Semla M, et al. Acrylamide: a common food toxin related to physiological functions and health. Physiol Res. 2017;66:205–217. doi: 10.33549/physiolres.933381. [DOI] [PubMed] [Google Scholar]
- 38.Sun R, et al. Protective effect of curcumin on acrylamide-induced hepatic and renal impairment in rats: involvement of CYP2E1. Nat Prod Commun. 2020;15(3):1–9. [Google Scholar]
- 39.Karimi MY, et al. Ellagic acid prevents oxidative stress, inflammation, and histopathological alterations in acrylamide-induced hepatotoxicity in wistar rats. J Diet Suppl. 2020;17(6):651–62. [DOI] [PubMed]
- 40.Acaroz U, et al. The ameliorative effects of boron against acrylamide-induced oxidative stress, inflammatory response, and metabolic changes in rats. Food Chem Toxicol. 2018;118:745–752. doi: 10.1016/j.fct.2018.06.029. [DOI] [PubMed] [Google Scholar]
- 41.Seydi E, et al. Involvement of mitochondrial-mediated caspase-3 activation and lysosomal labilization in acrylamide-induced liver toxicity. Toxicol Environ Chem. 2015;97(5):563–575. doi: 10.1080/02772248.2015.1047671. [DOI] [Google Scholar]
- 42.Calleman CJ. The metabolism and pharmacokinetics of acrylamide: implications for mechanisms of toxicity and human risk estimation. Drug Metab Rev. 1996;28(4):527–590. doi: 10.3109/03602539608994018. [DOI] [PubMed] [Google Scholar]
- 43.Abt E, et al. Acrylamide levels and dietary exposure from foods in the United States, an update based on 2011–2015 data. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2019;36(10):1475–1490. doi: 10.1080/19440049.2019.1637548. [DOI] [PubMed] [Google Scholar]
- 44.Liu Y, et al. Metabonomics analysis of liver in rats administered with chronic low-dose acrylamide. Xenobiotica. 2020;50(8):894–905. [DOI] [PubMed]
- 45.Melnick R, et al. Summary of the National Toxicology Program’s report of the endocrine disruptors low-dose peer review. Environ Health Perspect. 2002;110(4):427–431. doi: 10.1289/ehp.02110427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eslam M, et al. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology. 2020;158(7):1999–2014. doi: 10.1053/j.gastro.2019.11.312. [DOI] [PubMed] [Google Scholar]
- 47.The Lancet, G. H Redefining non-alcoholic fatty liver disease: what’s in a name? Lancet Gastroenterol Hepatol. 2020;5(5):419. doi: 10.1016/S2468-1253(20)30091-1. [DOI] [PubMed] [Google Scholar]
- 48.Chu PL, et al. Negative association between acrylamide exposure and body composition in adults: NHANES, 2003–2004. Nutr Diabetes. 2017;7(3):e246. doi: 10.1038/nutd.2016.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Calabrese EJ, Baldwin LA. Toxicology rethinks its central belief. Nature. 2003;421(6924):691–692. doi: 10.1038/421691a. [DOI] [PubMed] [Google Scholar]
- 50.Kohn M, Melnick R. Biochemical origins of the non-monotonic receptor-mediated dose-response. J Mol Endocrinol. 2002;29:113–123. doi: 10.1677/jme.0.0290113. [DOI] [PubMed] [Google Scholar]
- 51.Calabrese EJ, Baldwin LA. The hormetic dose-response model is more common than the threshold model in toxicology. Toxicol Sci. 2003;71(2):246–250. doi: 10.1093/toxsci/71.2.246. [DOI] [PubMed] [Google Scholar]
- 52.Grünwald S, Niedermeier J, Wenzel U. Hormesis is induced in the red flour beetle Tribolium castaneum through ingestion of charred toast. Eur J Nutr. 2015;54(4):535–541. doi: 10.1007/s00394-014-0734-8. [DOI] [PubMed] [Google Scholar]
- 53.Anthérieu S, et al. Induction of vesicular steatosis by amiodarone and tetracycline is associated with up-regulation of lipogenic genes in heparg cells. Hepatology. 2011;53(6):1895–1905. doi: 10.1002/hep.24290. [DOI] [PubMed] [Google Scholar]
- 54.Aubert J, et al. Increased expression of cytochrome P450 2E1 in nonalcoholic fatty liver disease: mechanisms and pathophysiological role. Clin Res Hepatol Gastroenterol. 2011;35(10):630–637. doi: 10.1016/j.clinre.2011.04.015. [DOI] [PubMed] [Google Scholar]
- 55.Leung TM, Nieto N. CYP2E1 and oxidant stress in alcoholic and non-alcoholic fatty liver disease. J Hepatol. 2013;58(2):395–398. doi: 10.1016/j.jhep.2012.08.018. [DOI] [PubMed] [Google Scholar]
- 56.Ma L, et al. Involvement of CYP2E1-ROS-CD36/DGAT2 axis in the pathogenesis of VPA-induced hepatic steatosis in vivo and in vitro. Toxicology. 2020;445:152585. doi: 10.1016/j.tox.2020.152585. [DOI] [PubMed] [Google Scholar]
- 57.Begriche K, et al. Drug-induced toxicity on mitochondria and lipid metabolism: mechanistic diversity and deleterious consequences for the liver. J Hepatol. 2011;54(4):773–794. doi: 10.1016/j.jhep.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 58.Mohamed AA, et al. Role of CYP2E1 in mitochondrial dysfunction and hepatic injury by alcohol and non-alcoholic substances. Curr Mol Pharmacol. 2017;10(3):207–225. doi: 10.2174/1874467208666150817111114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.O’Shea D, et al. Effect of fasting and obesity in humans on the 6-hydroxylation of chlorzoxazone: a putative probe of CYP2E1 activity. Clin Pharmacol Ther. 1994;56(4):359–367. doi: 10.1038/clpt.1994.150. [DOI] [PubMed] [Google Scholar]
- 60.Calleman CJ, et al. A nonlinear dosimetric model for hemoglobin adduct formation by the neurotoxic agent acrylamide and its genotoxic metabolite glycidamide. Environ Health Perspect. 1993;99:221–223. doi: 10.1289/ehp.9399221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vikstrom AC, et al. In vivo doses of acrylamide and glycidamide in humans after intake of acrylamide-rich food. Toxicol Sci. 2011;119(1):41–49. doi: 10.1093/toxsci/kfq323. [DOI] [PubMed] [Google Scholar]
- 62.Ghanayem BI, et al. Absence of acrylamide-induced genotoxicity in CYP2E1-null mice: evidence consistent with a glycidamide-mediated effect. Mutat Res. 2005;578(1–2):284–297. doi: 10.1016/j.mrfmmm.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 63.Nawaz M, et al. Purification and characterization of an amidase from an acrylamide-degrading Rhodococcus sp. Appl Environ Microbiol. 1994;60:3343–3348. doi: 10.1128/aem.60.9.3343-3348.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Duda-Chodak A, et al. A review of the interactions between acrylamide, microorganisms and food components. Food Funct. 2016;7(3):1282–1295. doi: 10.1039/C5FO01294E. [DOI] [PubMed] [Google Scholar]
- 65.Leung C, et al. The role of the gut microbiota in NAFLD. Nat Rev Gastroenterol Hepatol. 2016;13(7):412–425. doi: 10.1038/nrgastro.2016.85. [DOI] [PubMed] [Google Scholar]
- 66.Senior JR. Alanine aminotransferase: a clinical and regulatory tool for detecting liver injury-past, present, and future. Clin Pharmacol Ther. 2012;92(3):332–339. doi: 10.1038/clpt.2012.108. [DOI] [PubMed] [Google Scholar]
- 67.Buzzetti E, Pinzani M, Tsochatzis EA. The multiple-hit pathogenesis of non-alcoholic fatty liver disease (NAFLD) Metabolism. 2016;65(8):1038–1048. doi: 10.1016/j.metabol.2015.12.012. [DOI] [PubMed] [Google Scholar]
- 68.Moore MP, et al. A fad too far? Dietary strategies for the prevention and treatment of NAFLD. Obesity (Silver Spring) 2020;28(10):1843–1852. doi: 10.1002/oby.22964. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available in the NHANES repository, https://wwwn.cdc.gov/nchs/nhanes/default.aspx.