Abstract
Background
Displaced intracapsular fractures may be treated by either reduction and internal fixation, which preserves the femoral head, or by replacement of the femoral head with an arthroplasty. This is an update of a Cochrane review first published in 2003 and previously updated in 2006.
Objectives
To compare the relative effects (benefits and harms) of any type of internal fixation versus any type of arthroplasty for intracapsular femoral fractures in adults.
Search methods
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (August 2010), The Cochrane Central Register of Controlled Trials (The Cochrane Library 2010, Issue 3), MEDLINE (1966 to August 2010), EMBASE (1988 to 2010 Week 36), and other sources.
Selection criteria
All randomised and quasi‐randomised controlled trials comparing internal fixation with arthroplasty for intracapsular hip fractures in adults.
Data collection and analysis
Both authors independently assessed trial quality and extracted data. Wherever appropriate, results were pooled.
Main results
Nineteen trials, of which two were newly included in this update, involving 3044 participants, were included. There was considerable variation in the types of implants and techniques used for both internal fixation and arthroplasty in the included trials. The risk of selection bias was low in just three trials, unclear in 13 trials and high in the three quasi‐randomised trials. Just three trials reported assessor blinding of functional outcomes.
Length of surgery, operative blood loss, need for blood transfusion and risk of deep wound infection were significantly less for internal fixation compared with arthroplasty. Fixation had a significantly higher re‐operation rate in comparison with arthroplasty (40% versus 11%; risk ratio 3.22, 95% CI 2.31 to 4.47, 19 trials). No definite differences for hospital stay, mortality, or regain of pre‐injury residential state were found. Limited information from some studies suggested pain was less and function was better for a cemented arthroplasty in comparison with fixation.
Authors' conclusions
Internal fixation is associated with less initial operative trauma but has an increased risk of re‐operation on the hip. Definite conclusions cannot be made for differences in pain and residual disability between the two groups. Future studies should concentrate on better reporting of final outcome measures and function. There is still a need for studies to define which patient groups are better served by the different treatment methods.
Plain language summary
Fracture repair compared with partial or total joint replacement for treating hip fractures located within the hip joint
Fractures of the thigh bone (femur) near the hip joint (termed intracapsular) may be treated by fixing the fracture (with screws or pins), or alternatively replacing the top of the femur at the hip joint (femoral head) with an artificial hip joint (arthroplasty).
Nineteen trials, of which two were newly included in this update, involving 3044 participants, were included in this review. Some trials had weak methods, which required a more cautious interpretation of their results. There were many different types of devices and methods used to place these devices for both treatments in the included trials.
We found that each treatment has its own specific complications. Realigning the bones and fixing the fracture (reduction and internal fixation) is a shorter operation with less blood loss. However, people having internal fixation are more likely to need another operation than those treated with joint replacement (40% versus 11%). The reason for this is mainly from a failure of the bone to heal in those cases treated with fixation. No definite differences were found between the two treatment groups in the numbers of patients who had died by various follow‐up times. People who had a replacement with an artificial hip joint that was fixed in place with cement seemed to have less residual pain and better function related to using the hip than those whose fracture was fixed. There is not enough evidence to be sure whether fixation of the bone or replacement with an artificial hip is best for treating fractures of the thigh bone near the hip joint.
Background
Description of the condition
Proximal femoral fractures or, as they are more generally termed, 'hip fractures', can be subdivided into intracapsular fractures (those occurring proximal to the attachment of the hip joint capsule to the femur) and extracapsular (those occurring distal to the hip joint capsule). Intracapsular fractures can be further subdivided into those which are displaced and those which are essentially undisplaced. Undisplaced fractures include those termed impacted, valgus or abduction fractures. Many other subdivisions and classification methods exist for intracapsular fractures but are of questionable clinical value.
A displaced intracapsular hip fracture if left untreated invariably leads to non‐union of the fracture, which results in a painful hip and inability to weight bear on that limb. Thus this type of fracture is almost always managed surgically, either by fixing the fracture using various implants and thereby retaining the femoral head, or by replacing the femoral head with a prosthesis. The displaced intracapsular fracture has frequently been termed 'the unsolved fracture', as debate continues as to whether the femoral head should be preserved by reducing and fixing the fracture or be replaced by an arthroplasty.
Description of the intervention
Internal fixation entails first reducing the fracture, generally under X‐ray control using an image intensifier. The reduced position is then held by either single or multiple screws or pins, passed across the fracture under X‐ray guidance. Numerous implants are available for fixation of the fracture, and randomised trials comparing different implants are reported in another Cochrane review (Parker 2001; last update Issue 2, 2011).
Arthroplasty for an intracapsular fracture entails replacing the femoral head, which has fractured from the femur with an artificial hip joint. The type of arthroplasty may be either a hemiarthroplasty (partial hip replacement) or a total hip replacement (THR). Hemiarthroplasty involves replacing the femoral head with a prosthesis whilst retaining the natural acetabulum and acetabular cartilage. The type of hemiarthroplasty can be broadly divided into two groups: unipolar and bipolar. The unipolar hemiarthroplasty is a solid prosthesis whilst the bipolar prosthesis is designed to allow movement to occur, not only between the acetabulum and the prosthesis, but also at a joint within the prosthesis itself. Total hip replacement involves the replacement of the acetabulum in addition to the femoral head. The acetabular component is usually made of a high‐density polyethylene and is often cemented into place. The metal femoral stems used for an arthroplasty may be either held in place with cement or inserted as a 'press fit', without cement. Randomised trials comparing different the different types of arthroplasties for hip fracture are reported in another Cochrane review (Parker 2010).
How the intervention might work
The main complication of an intracapsular fracture treated by internal fixation is the failure of the fracture to heal. This may lead to fracture displacement and this is termed 'early fracture displacement' or 'non‐union' if it occurs in the first few weeks from operation. The term 'non‐union' is also used for those fractures that fail to heal in later weeks. This generally leads to the fracture displacing with loss of position of the fixation device. An incidence of non‐union of 20% to 35% for displaced intracapsular fractures can be expected (Lu‐Yao 1994). Another major complication after internal fixation is avascular necrosis (also termed segmental collapse or femoral head necrosis). This is seen as the collapse of the femoral head and subsequent destruction of the hip joint. It occurs secondary to disruption of the blood supply to the femoral head. An incidence of 5% to 30% can be expected. Other fracture healing complications that may occur after internal fixation are backing out of the implant as the fracture heals, fracture below or around the implant and breakage of the implant.
Potential complications of arthroplasty include wound sepsis and infection around the implant, dislocation of the prosthesis, loosening of the prosthesis stem, loosening of the acetabular component (total hip replacement only), acetabular wear (hemiarthroplasty only), breakage of the implant, disassembly of the implant, fracture below or around the implant and adverse reactions to the use of cement.
Why it is important to do this review
Conducted prior to the publication of the first version of this review in 2003, a meta‐analysis (Lu‐Yao 1994) of 106 randomised trials and comparative series concluded that mortality was similar between internal fixation and arthroplasty but that re‐operation was three times more common after internal fixation. Deep infection was more common after arthroplasty. Pain was less within the first two years after arthroplasty but there was no difference in mobility between the two types of treatment. A later systematic review (Bhandari 2003) concluded that arthroplasty reduces the risk of revision surgery at a cost of increased infection rates, increased blood loss and operative times and a possible increase in early mortality rates. The previous update of our review (Parker 2006) drew similar conclusions, but also noted there remained insufficient evidence to draw definitive conclusions for pain and function. Additionally, there is continuing variation in practice in the choice of internal fixation or arthroplasty for displaced intracapsular hip fractures. Hence, an update of the review starting with an updated search for randomised trials was warranted.
Objectives
To identify and summarise the evidence from randomised controlled trials that compare femoral head preservation (by internal fixation) with femoral head replacement (by arthroplasty) after an intracapsular proximal femoral fracture. Separate comparisons were made for the different types of internal fixation and arthroplasty.
Our primary aim was to compare the relative effects (benefits and harms) of any type of internal fixation versus any type of arthroplasty. Our two secondary comparisons were of:
any type of internal fixation versus arthroplasty with a hemiarthroplasty;
any type of internal fixation versus arthroplasty with a total hip replacement.
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials comparing femoral head preservation by internal fixation with femoral head replacement using any form of arthroplasty. Quasi‐randomised trials (for example, allocation by alternation or date of birth) and trials in which the treatment allocation was inadequately concealed were considered for inclusion.
Types of participants
Skeletally mature patients with an intracapsular proximal femoral fracture.
Types of interventions
Implants used for internal fixation which preserve the femoral head versus those which replace the femoral head.
Types of outcome measures
Data for the following outcomes were sought:
a) Operative details
length of surgery (in minutes)
number of patients transfused
operative blood loss (in millilitres)
post‐operative blood transfusion (in units or as described in each study)
b) Complications related to the type of operation
For internal fixation:
non‐union of the fracture within the follow‐up period (the definition of non‐union was that used within each individual study, and this outcome included early re‐displacement of the fracture).
avascular necrosis
fracture below or around the implant
other surgical complications of fixation (as detailed in each study).
For replacement arthroplasty:
dislocation of the prosthesis
loosening of the prosthesis
acetabular wear (as defined by each study)
disassembly of the implant
fracture below or around the implant
other surgical complications (as detailed in each study).
For both methods of treatment: Re‐operations within the follow‐up period of each study were categorised as
'minor' re‐operations (removal of internal fixation device, closed surgery to reduce a dislocated prosthesis, resuture of a wound)
'moderate' re‐operations (arthroplasty after internal fixation, surgical drainage of a haematoma, open reduction of a dislocation, Girdlestone procedure or similar removal of implant and femoral head)
'major' re‐operations (conversion of a hemiarthroplasty to a total hip replacement or other revision arthroplasty, repair of a fracture around an implant)
total number of patients having any type or re‐operation from any one of the above three categories
superficial wound infection (infection of the wound in which there is no evidence that the infection extends beneath the deep fascia)
deep wound infection (infection beneath the deep fascia and invariably involving the tissues around the implant)
c) Post‐operative complications
pneumonia
thromboembolic complications (deep vein thrombosis or pulmonary embolism)
congestive cardiac failure
myocardial infarction
stroke (cerebrovascular accident)
confusional state
gastrointestinal complications (perforation or bleeding)
pressure sores
other medical complications (as detailed in each individual study)
d) Post‐operative care outcomes
days to mobilisation
length of hospital stay (in days)
economic cost (as detailed in each study)
e) Anatomical restoration
shortening (> 2 cm, or as defined in each study)
varus deformity (as defined in each study)
external rotation deformity (> 20 degrees, or as defined in each study)
loss of movement (as defined in each study)
f) Final outcome measures
mortality (within the follow‐up period of the study)
pain (persistent pain at the final follow‐up assessment)
residence at final follow‐up (return to living at home, discharge location)
mobility (use of walking aids, return of mobility)
health related quality of life measures
Search methods for identification of studies
Electronic searches
We searched the Cochrane Bone, Joint and Muscle Trauma Group Specialised Register (November 2010), the Cochrane Central Register of Controlled Trials (The Cochrane Library, 2010, Issue 3), MEDLINE (1966 to August week 5 2010) and EMBASE (1988 to 2010 Week 36). We searched the WHO International Clinical Trials Registry Platform Search Portal (to August 2010), Current Controlled Trials, (to August 2010) and the UK National Research Register (NRR) Archive (to September 2007) to identify ongoing and recently completed trials. No language or publication restrictions were applied.
In MEDLINE (Ovid online), the subject specific search strategy was combined with the sensitivity‐ and precision‐maximizing version of the Cochrane Highly Sensitive Search Strategy for identifying randomised trials (Lefebvre 2009) (seeAppendix 1). The search strategies run in The Cochrane Library (Wiley Online Library) and EMBASE (Ovid online) are also shown in Appendix 1. The MEDLINE and EMBASE search strategies published in the previous version of this review (Parker 2006) are shown in Appendix 2.
Searching other resources
We searched reference lists of articles and our own reference databases. We included the findings from handsearches of the British Volume of the Journal of Bone and Joint Surgery supplements (1996 to 2006), abstracts of the American Orthopaedic Trauma Association annual meetings (1996 to 2006) and American Academy of Orthopaedic Surgeons annual meetings (2004 to 2007). We also included handsearch results from the final programmes of SICOT (1996 and 1999) and SICOT/SIROT (2003), EFORT (2007) and the British Orthopaedic Association Congress (2000, 2001, 2002, 2003, 2005 and 2006). Up to 2007, we scrutinised weekly downloads of "Fracture" articles in new issues of Acta Orthopaedica Scandinavica (subsequently Acta Orthopaedica); American Journal of Orthopedics; Archives of Orthopaedic and Trauma Surgery; Clinical Orthopedics and Related Research; Injury; Journal of the American Academy of Orthopedic Surgeons; Journal of Arthroplasty; Journal of Bone and Joint Surgery (American and British Volumes); Journal of Orthopedic Trauma; Journal of Trauma; Orthopedics from AMEDEO.
Data collection and analysis
Selection of studies
Both review authors independently screened downloads from electronic databases and other sources for potentially eligible trials. We then independently selected trials for inclusion, usually based on full text reports. Trial authors were approached for further details of trial methods where necessary. Any disagreement was resolved by discussion.
Data extraction and management
Data for the outcomes listed above were independently extracted by both authors using a data extraction form. Any differences were resolved by discussion. Where necessary and practical, we contacted trialists for additional data and clarification.
Assessment of risk of bias in included studies
In the update of the review, three aspects of risk of bias were assessed and reported for all included studies. These were sequence generation, allocation concealment and blinding of the outcome assessors of pain and function. In this assessment, incomplete or a lack of information on sequence generation or allocation concealment was judged as 'unclear risk' of bias unless the trial was quasi‐randomised, in which case both domains were rated 'high risk'.
In addition, both authors independently assessed, without masking, each trial for 10 aspects of internal and external validity (seeTable 1). Any disagreement was resolved by discussion. Trial authors were contacted for further details of trial methodology where this was unclear.
1. Methodological quality assessment scheme.
| 1. Was there clear concealment of allocation? | Score 3 if allocation was concealed (e.g. numbered sealed opaque envelopes drawn consecutively). Score 2 if there was a possible chance of disclosure before allocation. Score 1 if the method of allocation concealment or randomisation was not stated or was unclear. Score 0 if allocation concealment was clearly not concealed such as those trials using quasi‐randomisation (e.g. even or odd date of birth). |
| 2. Were the inclusion and exclusion criteria clearly defined? | Score 1 if text states the type of fracture and which patients were included and/or excluded. Otherwise score 0. |
| 3. Were the outcomes of trial participants who withdrew or excluded after allocation described and included in an intention‐to‐treat analysis? | Score 1 if yes or text states that no withdrawals occurred, or data are presented that, by clearly showing 'participant flow', allow this to be inferred. Otherwise score 0. |
| 4. Were the treatment and control groups adequately described at entry and if so were the groups well matched or appropriate co‐variate adjustment made? | Score 1 if at least four admission details given (e.g. age, sex, mobility, function score, mental test score, fracture type) with no significant difference between groups or appropriate adjustment made. Otherwise score 0. |
| 5. Did the surgeons have prior experience of the operations they performed in the trial, prior to its commencement? | Score 1 if text states there was an introductory period or that surgeons were experienced. Otherwise score 0. |
| 6. Were the care programmes other than trial options identical? | Score 1 if text states they were or if this can be inferred. Otherwise score 0. |
| 7. Were the outcome measures clearly defined in the text with a definition of any ambiguous terms encountered? | Score 1 if yes. Otherwise score 0. |
| 8. Were the outcome assessors blind to assignment status? | Score 1 if assessors of pain and function at follow‐up were blinded to treatment outcome. Otherwise score 0. |
| 9. Was the timing of outcome measures appropriate? A minimum of 24 months active follow‐up for all surviving trial participants. | Score 1 if yes. Otherwise score 0. |
| 10. Was loss to follow‐up reported and if so were less than 5% of trial participants lost to follow‐up? | Score 1 if yes. Otherwise score 0. |
Dealing with missing data
Where the number of participants providing data for any particular outcome was reported, we used these provided data. In studies for which a number of events were reported, but the denominator was unclear, we used numbers randomised or alive at follow‐up.
Assessment of heterogeneity
Heterogeneity between comparable trials was assessed by inspection of the overlap of confidence intervals amongst included studies and tested using a standard Chi² test, with additional consideration of the I² statistic (Higgins 2003), with an I² of 50% or over representing substantial heterogeneity.
Data synthesis
For dichotomous outcomes, we reported risk ratios (RR) with 95% confidence intervals and for continuous outcomes, mean differences (MD) and 95% confidence intervals. Results of comparable groups of trials were pooled, using the Mantel‐Haenszel method for dichotomous outcomes, and inverse variance for continuous data, and the fixed‐effect model; unless heterogeneity was substantial (nominally, P < 0.10; I² > 50%), when the random‐effects model was used.
Subgroup analysis and investigation of heterogeneity
We recognised the possibility that the different types of internal fixation implants and the different types of arthroplasty (and use of bone cement) might show some differences in effectiveness or adverse effects. We have therefore presented in the analyses which studies are grouped by implant design. These enable readers to inspect the data but, where appropriate, we have explored the possibility that implant types perform differently by conducting formal tests for subgroup differences.
Results
Description of studies
Nineteen randomised controlled trials involving 3044 patients with 3048 fractures were included in the review. Two trials (Frihagen 2007; Mouzopoulos 2008) were newly included in this update as were additional reports providing long term follow‐up results for two studies (Parker 2002; Rogmark 2002). A summary of details of each of the included trials is given in the Characteristics of included studies. Twelve studies were excluded for reasons given in the Characteristics of excluded studies.
Nine (two group) studies compared fixation with a hemiarthroplasty. Jensen 1984 compared four AO screws with an uncemented Austin Moore unipolar hemiarthroplasty (posterior approach) in 102 patients. Parker 2002 compared three AO screws with an uncemented Austin Moore unipolar hemiarthroplasty (anterolateral approach) in 455 patients. Blomfeldt 2005 compared two screws with an uncemented Austin Moore hemiarthroplasty (anterolateral approach) in 60 cases. van Dortmont 2000 compared three cannulated AO/ASIF screws with a cemented Thompson unipolar hemiarthroplasty (anterior approach) in 60 patients. Puolakka 2001 compared three Ullevaal screws with a cemented Thompson hemiarthroplasty in 31 patients. van Vugt 1993 compared a Dynamic Hip Screw and two‐hole plate with a cemented Stanmore variocup bipolar hemiarthroplasty (anterolateral approach) in 43 patients. Soreide 1979 compared von Bahr screws with a Christiansen bipolar hemiarthroplasty in 104 patients. Roden 2003 compared two von Bahr screws against a Variokopf bipolar hemiarthroplasty in 100 cases. Frihagen 2007 compared two Olmed screws with a Charnley‐Hastings bipolar hemiarthroplasty in 222 patients.
Four (two group) studies compared fixation with a THR. Jonsson 1996 compared Hansson hook pins with a cemented Charnley total hip replacement and trochanteric osteotomy in 47 patients. Johansson 2002 compared two Olmed screws with a cemented Lubinus IP total hip replacement (dorsolateral approach) in 143 fractures (146 patients). Neander 1997 compared two Olmed screws with a cemented BiMetric total hip replacement (posterior approach) in 20 patients. Tidermark 2003 compared two Olmed screw with a Exeter total hip replacement in 102 cases.
Four studies compared three implants. Skinner 1989 compared a sliding compression screw plate versus an uncemented Austin Moore unipolar hemiarthroplasty (posterolateral approach) versus a Howse II total hip replacement (posterolateral approach) in 271 patients. Davison 2001 compared an Ambi sliding hip screw versus a cemented Thompson unipolar hemiarthroplasty (lateral Hardinge approach) versus a cemented Monk bipolar hemiarthroplasty (lateral Hardinge approach) in 280 patients. For the purposes of this review we have combined the two arthroplasty groups as there were no significant differences reported between them. Svenningsen 1985 compared a compression hip screw versus a nail and plate versus a Christiansen bipolar hemiarthroplasty in 169 patients. It is unclear if the prosthesis was cemented. Mouzopoulos 2008 compared a sliding hip screw fixation with a Merte hemiarthroplasty and a Plus total hip replacement in 129 patients. Again, it is unclear if the prostheses were cemented in this trial. The arthroplasty groups of Davison 2001, Mouzopoulos 2008 and Skinner 1989 have been compared in a separate review (Parker 2010).
Two studies used a variety of implants. Rogmark 2002, in a multicentre trial, compared Hansson hook‐pins or Olmed screws versus replacement arthroplasty (hemiarthroplasty or total hip replacement, using a variety of implants) in 409 patients. STARS 2006 was a multicentre trial comparing internal fixation, cemented bipolar hemiarthroplasty and cemented total hip replacement in a total of 298 patients. The method of surgery and type of implant used for each of the three surgical groups was at the discretion of the participating surgeons.
The information given on inclusion and exclusion criteria and characteristics of trial participants varied, making it difficult to assess how homogenous, or otherwise, the patient groups were across the studies. The lower limit of the age ranges of participants in the included studies varied from 60 to 75. Two studies, Davison 2001 and van Vugt 1993, had an upper limit of 79 and 80 years respectively but the remaining studies had no upper age limit. Where defined, the mental function of trial participants varied between studies. Five studies (Davison 2001; Mouzopoulos 2008; Roden 2003; STARS 2006; Tidermark 2003) specifically excluded patients with a low mental‐health score, while Blomfeldt 2005 and van Dortmont 2000 only included patients with dementia.
Risk of bias in included studies
The risk of bias assessments for sequence generation, allocation concealment and blinding for individual trials are shown in Figure 1 and an overall summary is given in Figure 2. The majority of judgements for sequence generation and allocation concealment were 'unclear', which reflected in part the poor reporting of the methods of randomisation in these trials. Only three trials (Frihagen 2007; Rogmark 2002; STARS 2006) were judged at low risk for selection bias reflecting adequate allocation concealment. The three quasi‐randomised trials (Mouzopoulos 2008; Skinner 1989; Soreide 1979) were considered at high risk of bias resulting from both inadequate sequence generation and lack of allocation concealment. Further details of the randomisation methods reported in the 19 trials are given below. Just three trials (Davison 2001; Frihagen 2007; Mouzopoulos 2008) were considered at low risk of assessor blinding for functional outcome assessment.
1.
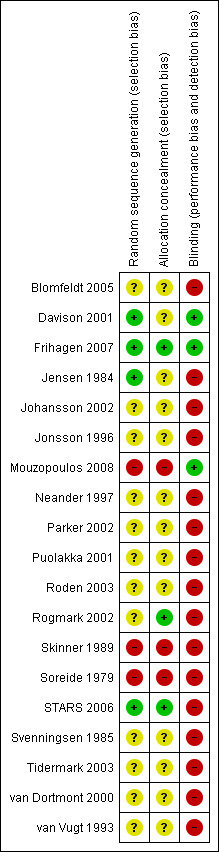
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
2.
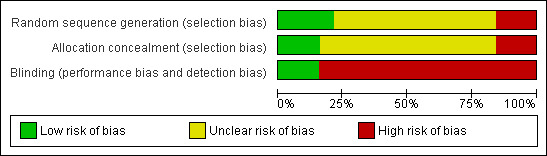
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
As assessed using the tool described in Table 1, the methodological quality of the included studies varied greatly. The assessment of the different studies is detailed in Table 2. In general the older trials have inferior trial methodology compared with the more recently designed trials, although this may in part be due to better trial reporting and there are exceptions. The improvement is most noticeable with the use of more secure methods of randomisation, better reporting of inclusion and exclusion criteria and clearer reporting of outcomes with less loss to follow‐up of patients.
2. Methodological quality assessment results (see Table 1 for criteria).
| Study ID | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 |
| Soreide 1979 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| Jensen 1984 | 2 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 |
| Svenningsen 1985 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 |
| Skinner 1989 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 |
| van Vugt 1993 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 |
| Jonsson 1996 | 2 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 |
| Neander 1997 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| van Dortmont 2000 | 2 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 |
| Davison 2001 | 2 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 0 |
| Puolakka 2001 | 2 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 1 |
| Johansson 2002 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 |
| Parker 2002 | 2 | 1 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 |
| Rogmark 2002 | 3 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 1 |
| Roden 2003 | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| Tidermark 2003 | 2 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| Blomfeldt 2005 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 |
| STARS 2006 | 3 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 |
| Frihagen 2007 | 3 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| Mouzopoulos 2008 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 1 | 0 |
STARS 2006 used a computer telephone randomisation service. Frihagen 2007, Johansson 2002 and Rogmark 2002 used sequentially numbered sealed envelopes, Jensen 1984 and van Dortmont 2000 used random numbers in sealed opaque envelopes, while Blomfeldt 2005, Jonsson 1996, Parker 2002, Puolakka 2001 and Tidermark 2003 used sealed envelopes. Davison 2001 stated only that they used computer generation of random numbers. Neander 1997, Soreide 1979, Svenningsen 1985 and van Vugt 1993 gave no information about their method of randomisation. Three trials (Mouzopoulos 2008; Soreide 1979; Skinner 1989) were quasi‐randomised. Allocation was by alternation in Mouzopoulos 2008, patient's date of birth in Soreide 1979 and by the day of week in Skinner 1989.
Five trials (Blomfeldt 2005; Frihagen 2007; Parker 2002; STARS 2006; van Dortmont 2000) reported results on an intention‐to‐treat basis. Randomised patients were excluded from the analysis in the following eight trials (Davison 2001; Johansson 2002; Jonsson 1996; Mouzopoulos 2008; Rogmark 2002; Skinner 1989; Soreide 1979; Tidermark 2003) for reasons given in the Characteristics of included studies.
Effects of interventions
Where available the results have been presented in the analyses. As previously noted, and reflecting current practice, the included trials used a wide selection of implants for both fixation and replacement arthroplasty, making direct comparisons between trials difficult. As the 19 included studies employed a large variety of implants it was not possible to present the results in a simple format. Analyses 1.1 to 1.45 test our primary hypothesis by pooling data to compare a policy of internal fixation with a policy of arthroplasty. These analyses contain subgroups for internal fixation versus hemiarthroplasty, internal fixation versus total hip arthroplasty, and internal fixation versus any hip arthroplasty. These results need to be viewed with caution because of the range of implants used and the heterogeneity of study participants. Analyses 2.1 to 2.18 present pooled data for internal fixation versus hemiarthroplasty, with subgroup analysis of different individual comparisons. Analyses 3.1 to 3.15 present pooled data for internal fixation versus total hip arthroplasty, with subgroup analysis of different individual comparisons. The results for Skinner 1989 and STARS 2006, each of which had three treatment groups, are presented separately in the analyses for hemiarthroplasty (Analysis 2) and total hip replacement (Analysis 3). This does not apply for Rogmark 2002 because the different types of arthroplasty were all in one treatment group of this trial.
Operative details
Length of surgery
Thirteen trials recorded this outcome and all reported a significantly shorter operative time for fixation. Seven trials gave the means with standard deviations and are shown in the analyses (seeAnalysis 1.1; Analysis 2.1; Analysis 3.1). The data for all three analyses have not been pooled given the clearly visible and highly significant heterogeneity reflecting large variations in the length of operations. This is consistent with the large variety of surgical methods employed in these seven trials and may also reflect different definitions of this outcome. The reported times may not include the time needed for reduction of the fracture for internal fixation and relate only to the duration of the surgical procedure.
1.1. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 1 Length of surgery ( in minutes).
2.1. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 1 Length of surgery (in minutes).
3.1. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 1 Length of surgery (in minutes).
Results from the other five studies were as follows: Jensen 1984 reported mean times of 67 minutes for fixation with four AO screws versus 91 minutes with uncemented Austin Moore hemiarthroplasty. The time for internal fixation did not include the reduction time. van Vugt 1993 reported mean times of 66 minutes for fixation with a dynamic hip screw versus 80 minutes for a Stanmore bipolar hemiarthroplasty. Soreide 1979 reported mean times of 38 minutes for fixation with von Bahr screws versus 86 minutes for Christiansen bipolar hemiarthroplasty. The time for internal fixation did not include the reduction time. Svenningsen 1985 reported mean times of 42 minutes for fixation with a compression screw versus 39 minutes for fixation with a McLaughlin nail plate versus 79 minutes for a Christiansen bipolar hemiarthroplasty. Lastly, Rogmark 2002 reported mean times of 27 minutes for fixation with Hansson hook‐pins or Olmed screws versus 80 minutes for various arthroplasties.
Operative blood loss
Eight studies reported on operative blood loss and all favoured fixation. Seven gave the means with standard deviations and are therefore presented in the analyses (seeAnalysis 1.2; Analysis 2.2; Analysis 3.2). The data for these analyses have not been pooled given the highly significant heterogeneity. As shown in Analysis 1.2, fixation was associated with a lower operative blood loss, with mean differences ranging between 149 ml (Parker 2002) and 550 ml (Tidermark 2003). van Vugt 1993 reported perioperative blood loss for all the 21 patients in the dynamic hip screw group as less than 500 ml (median 200 ml). For the 22 patients in the Stanmore bipolar group, 18 had a blood loss of less than 500 ml, three had a blood loss of 500 ml to 1000 ml and one had a blood loss greater than 1000 ml (median 400 ml).
1.2. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 2 Operative blood loss (in millilitres).
2.2. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 2 Operative blood loss (in millilitres).
3.2. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 2 Operative blood loss (in millilitres).
Post‐operative blood transfusion
Six studies reported the number of patients transfused following fixation compared with arthroplasty (seeAnalysis 1.3). Transfusion was required less frequently in the internal fixation group, with the exception of the STARS 2006 trial. Mean units of blood transfused reported in two studies was reduced for the fixation group (seeAnalysis 1.4). In addition, Svenningsen 1985 found lower mean units of blood transfused in the two fixation groups (0.3 units for the compression screw and McLaughlin nail plate groups) compared with 1.4 units for the Christiansen bipolar hemiarthroplasty group.
1.3. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 3 Number of patients transfused.
1.4. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 4 Mean units blood transfused.
Complications related to type of operation
Because the complications following fixation and replacement arthroplasty are different and specific to the type of surgery it is not possible to make direct comparisons between the two groups.
Non‐union of fracture following internal fixation
This included, what is also termed in some reports, early displacement, redisplacement, early dislocation of the fracture and pseudarthrosis. For the 15 trials that reported this outcome it occurred in 314/1064 (29.5%) of patients treated by internal fixation (seeAnalysis 1.5).
1.5. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 5 Non‐union of fracture within follow‐up period (includes early displacement).
Avascular necrosis following internal fixation
This also includes those cases termed late segmental collapse and femoral head necrosis. For the 12 trials reporting this outcome, avascular necrosis was reported in 100/999 (10%) of patients (seeAnalysis 1.6).
1.6. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 6 Avascular necrosis.
Dislocation of prosthesis after arthroplasty
Results from the trials that reported the number of patients with dislocation are summarised in Analysis 1.7, with results presented separately for hemiarthroplasty and total hip replacement (THR). For hemiarthroplasty, there were 35/887 (3.9%) patients with dislocations and for THR, 44/333 (13.2%). A number of patients with dislocations had recurrent dislocations, particularly for those with THR. However, reporting of recurrent dislocations was variable. Skinner 1989 stated that five of the 18 patients with a dislocated THR had recurrent dislocations. Rogmark 2002 reported 15 patients with dislocations, of which seven had recurrent dislocations and six of the 12 patients with dislocation in Johansson 2002 were recurrent. Tidermark 2003 had only one case of dislocation which was recurrent and required revision.
1.7. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 7 Dislocation of prosthesis.
Loosening of arthroplasty
The six trials that reported this outcome found that loosening of the prosthesis occurred in 21/632 (3.3%) of patients (seeAnalysis 1.8).
1.8. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 8 Loosening of prosthesis.
Acetabular wear
This outcome applies only to hemiarthroplasty. For this review we have included acetabular protrusion and erosion. The five trials reporting this outcome recorded its occurrence in 10/519 (1.9%) of patients (see Analysis 1.9).
1.9. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 9 Acetabular wear (as defined by each study).
Fracture below or around the implant
This outcome occurs after both internal fixation and arthroplasty but was only reported in five studies. The incidence was 8/576 (1.4%) after internal fixation and 18/552 (3.3%) after arthroplasty (seeAnalysis 1.10).
1.10. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 10 Fracture below/around implant.
Re‐operations
Results in the analyses are presented as number of patients having a secondary operation classified as 'minor', 'moderate,' or 'major', as described in Types of outcome measures. The total number of re‐operations is the number of patients who had any type of re‐operation for the hip fracture. Pooled results for 'moderate' re‐operations significantly favoured arthroplasty (seeAnalysis 1.12: RR 9.35, 95% CI 5.79 to 15.07). Pooled results for 'major' re‐operations significantly favoured internal fixation (seeAnalysis 1.13: RR 0.41, 95% CI 0.19 to 0.87). Pooled results for number of patients having any type of secondary operation (seeAnalysis 1.14) were statistically significant in favour of arthroplasty (RR 3.22, 95% CI 2.31 to 4.47). This finding applied for both hemiarthroplasty (RR 3.13, 95% CI 1.95 to 5.03) and THR (RR 3.43; 95% CI 1.45 to 8.10).
1.12. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 12 Re‐operations moderate (e.g. fixation to arthroplasty, drainage, girdlestone).
1.13. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 13 Re‐operations major (e.g. revision arthroplasty, hemiarthroplasty to THR).
1.14. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 14 Total re‐operation rate (within follow‐up period of study).
Superficial wound infection
Pooled data from 14 trials (seeAnalysis 1.15) showed no difference for this outcome for fixation versus arthroplasty (RR 0.85, 95% CI 0.53 to 1.38).
1.15. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 15 Superficial wound infection.
Deep wound infection
Analysis of pooled data for 15 trials (seeAnalysis 1.16) showed a reduced risk of infection with fixation in comparison with arthroplasty (RR 0.53, 95% CI 0.30 to 0.93).
1.16. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 16 Deep wound infection.
Post‐operative complications
Where reported, data have been pooled for the complications of pneumonia, thromboembolic complications, congestive cardiac failure, myocardial infarction, stroke (cerebrovascular accident), confusional states, gastrointestinal complications and pressure sores (seeAnalysis 1.17; Analysis 1.18; Analysis 1.19; Analysis 1.20; Analysis 1.21; Analysis 1.22; Analysis 1.23; Analysis 1.24; Analysis 1.25; and Analysis 1.26). None of these complications showed any statistically significant difference between treatment methods. Pooled results for all complications which includes data on all complications available from individual studies, in addition to those outcomes listed above showed a lower risk of medical complications after fixation compared with replacement arthroplasty (seeAnalysis 1.27, RR 0.73, 95% CI 0.58 to 0.92).
1.17. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 17 Pneumonia.
1.18. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 18 Deep vein thrombosis.
1.19. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 19 Pulmonary embolism.
1.20. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 20 Thromboembolic complications combined.
1.21. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 21 Congestive cardiac failure/heart failure.
1.22. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 22 Myocardial infarction.
1.23. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 23 Stroke (cerebrovascular accident).
1.24. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 24 Confusional state.
1.25. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 25 Gastrointestinal complications.
1.26. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 26 Pressure sores.
1.27. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 27 Total medical complications (as defined in each study).
Post‐operative care outcomes
Length of hospital stay
Hospital stay data (means and standard deviations) were reported in five studies (Frihagen 2007; Mouzopoulos 2008; Parker 2002; STARS 2006; van Dortmont 2000) (seeAnalysis 1.28). Only the study of Mouzopoulos 2008 reported notable differences with a reduced stay for those treated by arthroplasty, whilst the remaining studies found no statistically significant differences between treatment methods. Jonsson 1996 reported no statistically significant difference in the median stay in hospital: 12 days after fixation versus 15 days after THR. Rogmark 2002 reported a mean acute hospital stay of 10 days after fixation and 12 days after arthroplasty: the difference between the two groups was reported as being statistically significant (P < 0.001). However, a high proportion of these patients were transferred to rehabilitation facilities and the time spent in these units was not reported. Svenningsen 1985 reported a mean stay of 17 days after screw plate fixation, 18 days after nail plate fixation and 18 days after arthroplasty. van Vugt 1993 reported a mean hospital stay of 32 days after fixation versus 30 days after arthroplasty, a difference that was reported as not being statistically significant. Roden 2003 reported a mean hospital stay of 15 days in both groups. Johansson 2002 reported, with incomplete data, that there was no significant difference in hospital stay between groups (27 versus 25 days).
1.28. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 28 Length of hospital stay (in days).
Economic cost
Parker 2002 compared patients treated with three AO screws with those with an uncemented Austin Moore hemiarthroplasty and found that the mean cost was higher for fixation. The mean cost of treatment was GBP 4758 (EUR 7137) for internal fixation and GBP 4350 (EUR 6525) for hemiarthroplasty. This included the cost of any readmission and additional surgery related to the hip fracture.
Johansson 2002 reported a mean cost of SEK 117,838 (EUR 13100) for internal fixation versus SEK 115,315 (EUR 12700) for total hip replacement, a difference that was reported as not being statistically significant.
Soreide 1979 compared von Bahr screws with a Christiansen bipolar hemiarthroplasty and found that initial hospital stay for hemiarthroplasty was 2.4 times more expensive but with the more expensive follow‐up and more frequent readmission rate for fixation, this was reduced to 1.6 times overall.
Rogmark 2002 reported costs for a subgroup of 68 patients in a separate report. The mean two‐year cost for the 36 cases treated by fixation was USD 21,000 compared with a mean cost of USD 15,000 after arthroplasty.
The STARS 2006 study gave an average cost of GBP 14,882 for those treated by internal fixation, of GBP 13,863 for hemiarthroplasty and of GBP 12,253 for total hip replacement.
Anatomical restoration
Shortening
Parker 2002 measured limb length discrepancy at one year after surgery. They reported a mean shortening of 8.8 millimetres in 95 patients treated with three AO screws and a mean of 3.6 millimetres in 86 patients after Austin Moore hemiarthroplasty. This difference was reported as being statistically significant (P = 0.004). No other studies reported on this outcome.
Loss of flexion
Parker 2002 reported a mean loss of flexion of 8.8 degrees in 95 patients treated with three AO screws and a mean of 9.2 degrees in 86 patients after Austin Moore hemiarthroplasty at one year after surgery. The difference was not statistically significant (reported P = 0.83). Tidermark 2003 used a movement score which showed no statistically significant difference at four months but favoured arthroplasty at one and two years (P < 0.01 and P < 0.05). Mouzopoulos 2008 reported, without presenting data, that there was no statistically significant difference in the range of passive movements between groups, but that hip flexion and rotation seemed to be better after arthroplasty.
Final outcome measures
Mortality
There was no statistically significant difference between fixation and arthroplasty for mortality at any of the reported time periods up to 10 years from surgery (seeAnalysis 1.29, 30 days: RR 0.76, 95% CI 0.46 to 1.24, 4 trials; Analysis 1.30, 3 to 6 months: RR 0.87; 95% CI 0.70 to 1.08, 15 trials; Analysis 1.31, 12 months: RR 0.95, 95% CI 0.81 to 1.11, 14 trials; Analysis 1.32, 24 to 48 months: RR 0.97; 95% CI 0.87 to 1.09, 15 trials; Analysis 1.33, 10 years: RR 0.98, 95% CI 0.92 to 1.05, 2 trials). There was a tendency to a lower mortality for internal fixation in comparison with hemiarthroplasty in the first six months after surgery but the difference was not statistically significant (seeAnalysis 1.29 and Analysis 1.30).
1.29. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 29 Mortality 30 days.
1.30. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 30 Mortality up to 3 to 6 months.
1.31. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 31 Mortality up to 12 months.
1.32. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 32 Mortality up to 24 to 48 months.
1.33. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 33 Mortality 10 years.
Davison 2001 reported mortality at six months as percentages: 5% after fixation; 7% after a cemented Thompson and 10% after a cemented Monk bipolar. (Figures for one year were 8%, 11% and 12% respectively. Those for two years were 12%, 20% and 17%; and for three years: 19%, 28% and 22%. The mean survival times of the three groups were stated to be 79 months, 61 months and 68 months respectively, a difference that was stated to be statistically significant). Skinner 1989 (178 cases) also presented mortality as percentages. Results at two months were 12% after internal fixation, 15% after hemiarthroplasty and 10% after THR. At one year, these figures were 25%, 27% and 23% respectively. None of the differences at the two follow‐up times were reported as being statistically significant. Parker 2002 reported a trend to a lower mortality for fixation amongst those aged 90 years and over, although the results were not statistically significant.
Two studies reported on long term mortality at 10 years (Parker 2002; Rogmark 2002). Both studies found no statistically significant difference between groups (seeAnalysis 1.33).
Pain at follow‐up
For several trials (Davison 2001; Jensen 1984; Soreide 1979; Svenningsen 1985; van Vugt 1993), pain was incorporated into a composite score of overall function and thus it was not possible to comment on residual pain in these studies. van Dortmont 2000 did not report pain, as it was considered unreliable in patients with senile dementia (personal correspondence).
Only five trials gave the number of patients with residual pain at one year (seeAnalysis 1.34). These studies showed significant heterogeneity. Pooling of data showed a tendency to less pain with fixation for the two studies which compared an internal fixation with uncemented hemiarthroplasty (RR 0.81; 95% CI 0.62 to 1.05). For the two studies that compared internal fixation against a cemented THR, the results tended to favour arthroplasty (RR 3.08; 95% CI 0.90 to 10.56). Drawing on our findings of a trend to lower pain after cemented arthroplasty when compared with an uncemented arthroplasty (Parker 2010), we note that the two studies in the hemiarthroplasty group (Blomfeldt 2005; Parker 2002) used an uncemented arthroplasty. The other three trials used cemented arthroplasty. The use of cemented arthroplasty may thus be an important consideration for this outcome (seeAnalysis 1.35, test for subgroup differences: Chi² = 4.62, df = 1 (P = 0.03), I² = 78.3%). These findings were supported by those studies which used a pain score (Frihagen 2007; Parker 2002; Tidermark 2003) (seeAnalysis 1.36 and Analysis 1.37).
1.34. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 34 Residual pain at 1 year.
1.35. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 35 Residual pain at 1 year (subgrouped by cemented versus uncemented).
1.36. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 36 Mean pain score at 1 to 2 years.
1.37. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 37 Mean pain score at 1 to 2 years (subgrouped by cemented versus uncemented).
Further examination of pain outcomes taking into account of whether the arthroplasty was cemented or uncemented generally adds support to this finding.
Additional results from the studies that involved an uncemented arthroplasty were from Blomfeldt 2005, Blomfeldt 2005 and Skinner 1989. Blomfeldt 2005 also reported that pain scores were reduced for arthroplasty at four months but by the one‐ and two‐year assessments there were no statistically significant differences between the two groups. Parker 2002 also reported no statistically significant difference between groups in mean pain scores (2.40 versus 2.22, P = 0.91). Skinner 1989 reported that, at one year, 12% of those treated by internal fixation had significant residual pain as opposed to 27% treated by uncemented hemiarthroplasty, whilst none of those treated by cemented THR complained of residual pain.
For those studies involving a cemented arthroplasty, Roden 2003 reported that at four months the consumption of analgesia was less in the arthroplasty group (21/44 versus 6/44, P < 0.001). This study stated without providing patient numbers that at five years after surgery there was no statistically significant difference between groups. STARS 2006 reported statistically significant reduced pain score for those treated by hemiarthroplasty at four and 12 months, but not at two years when no statistically significant difference was apparent (P values reported as 0.07, 0.005 and 0.22). For the STARS 2006 study of fixation versus THR, there were also statistically significantly reduced pain scores at four months but not at one or two years for those treated with THR (reported P values = 0.05, 0.10 and 0.24). STARS 2006 also found a reduced number of patients with moderate to severe residual pain at 12 months in the cemented arthroplasty group (seeAnalysis 1.34, RR 1.30, 95% CI 1.05 to 1.61). Tidermark 2003 reported that pain scores at four months, one and two years were statistically significantly better for those treated by arthroplasty. Frihagen 2007 reported less pain for those treated with a hemiarthroplasty at four months (P = 0.01) but by 12 and 24 months the difference was not statistically significant.
Rogmark 2002 used cemented and uncemented arthroplasty. This study reported significantly more hip pain on walking in the fixation group at four (61% versus 34%, reported P < 0.001) and 12 months (43% versus 25%, P = 0.002) but not at 24 months follow‐up (32% versus 25%, reported P = not significant).
Two studies reported on long term pain at up to 15 years from surgery (Parker 2002; Rogmark 2002). Both studies found no statistically significant difference between groups.
Failure to return to same residence
The failure to return to the same residence in the long term (as opposed to transfer for further rehabilitation), was only reported in two studies, both using hemiarthroplasty (Jensen 1984; Parker 2002). Pooled results (Analysis 1.39) showed no difference between groups (RR 0.84, 95% CI 0.54 to 1.33).
1.39. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 39 Failure to return to same residence at final follow‐up.
Failure to regain mobility
Similar to pain, mobility results were often incorporated in composite functional scores. The actual numbers who regained their former mobility were only available from six studies. Analysis 1.40, which presents the results from these studies, showed no statistically significant difference between fixation and arthoplasty in the long term recovery of mobility (RR 1.02, 95% CI 0.74 to 1.39). In this analysis, we assumed that failure to return to preoperative mobility has meant a deterioration rather than an improvement. There is substantial heterogeneity in the results from the studies, which is likely to also reflect the variation in the definition of this outcome.
1.40. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 40 Failure to regain mobility.
Jonsson 1996 stated without data that more patients in the fixation group required walking aids at one year than in the THR group (P = 0.06). STARS 2006 reported on walking at four, 12 and 24 months using a composite score. This was reported to be significantly better for hemiarthroplasty at four months (P = 0.04), but not at 12 and 24 months (P value 0.25 and 0.12). For the comparison of fixation versus THR, the reported results favoured THR at all three time intervals (P = 0.001, 0.04 and 0.03). Tidermark 2003 used a walking score, which showed statistically significant better score for those treated by arthroplasty at four months (P < 0.001), one year (P < 0.01) and two years (P < 0.05).
Rogmark 2002 reported percentages of those with reduced walking ability, inability to walk up stairs and need for walking frame at four, 12, and 24 months. Walking ability was better following arthroplasty, although this difference was only just statistically significant at 24 months (P = 0.05). The numbers unable to climb stairs or in need of major walking aids at 12 months were not statistically significantly different between groups, although at four months both of these outcomes favoured arthroplasty (reported P values < 0.001). Mouzopoulos 2008 stated without data that the walking speed was faster for those treated with arthroplasty compared with those treated by internal fixation (P value reported as < 0.05).
Two studies reported on long term regain of mobility up to 15 years after surgery (Parker 2002; Rogmark 2002) with both studies found no statistically significant difference between groups.
Hip and other composite scores
See hip scores: Analysis 1.41, Analysis 1.42, Analysis 1.43; EQ‐5D: Analysis 1.44; and Barthel index score: Analysis 1.45
1.41. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 41 Harris hip score (at 1 year).
1.42. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 42 Hip rating questionnaire at 1 year.
1.43. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 43 Hip scores (at 1 year).
1.44. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 44 Mean Eq‐5d score (at 1 year).
1.45. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 45 Barthel index score of below 95 at 1 year.
For the comparison between internal fixation and hemiarthroplasty the following studies reported no difference between methods:
Davison 2001 reported no significant difference in the Harris Hip Scores or Barthel Index at one, two, three, four and five years. Svenningsen 1985 used their own composite hip assessment score for 101 patients and found no significant differences in scores between treatment methods. van Vugt 1993 also used their own score for 39 patients at three months, two years (33 patients) and three years (31 patients). 'Moderate or poor' outcomes were reported for these times for fixation versus arthroplasty of 8/20 versus 6/19, 2/17 versus 5/16 and 0/16 versus 6/15 patients. van Dortmont 2000 used an activities of daily living score for 31 patients at one year from injury. Mean scores were 7.2 after fixation and 7.9 after arthroplasty, which was stated as being not significant. Parker 2002 also used a composite activities of daily living (ADL) score for 190 patients assessed at one year. There was no statistically significant difference (P = 0.65) between the two groups. Blomfeldt 2005 reported no statistically significant difference in an activities of daily living score at four months and one and two years. Mouzopoulos 2008 using the Barthel index and Harris hip score reported no statistically significant difference between groups at one and four year follow‐up. This statement is contradicted for the Harris hip score at one year in Analysis 1.41.
The following studies reported better results after fixation compared with hemiarthroplasty:
Jensen 1984 reported better scores in the fixation group using the Stichfield classification (P = 0.006). Blomfeldt 2005 reported no difference in HRQOL (health related quality of life) scores at four months and one year, but improved for the internal fixation group at two years (P < 0.01).
The following studies reported better results after hemiarthroplasty compared with fixation:
Soreide 1979 assessed 67 patients at 12 months after surgery using the Stichfield classification and reported that more patients in the internal fixation group were classified only as fair or poor (P = 0.025). STARS 2006 used a composite score of pain, walking and function, which showed better results at four months and one year but not at two years (P = 0.004, P = 0.01, P = 0.14). The EuroQol (EQ‐5D) utility score showed no statistically difference between groups at four months, one and two years (P = 0.10, P = 0.15, P = 0.93). Frihagen 2007 using the Harris hip score reported significantly better scores for the hemiarthroplasty group at 4 months (P = 0.003) and 12 months (P = 0.01) but not at 24 months (P = 0.26). For the Barthel index, there was no difference at four months (P = 0.66) but a difference in favour of hemiarthroplasty at 12 and 24 months (P = 0.02). The results for the EQ‐5D index score also favoured hemiarthroplasty (P = 0.06 at 4 months, 0.07 at 12 months and 0.03 at 24 months).
For studies which compared internal fixation with total hip arthroplasty, all studies reported better results after arthroplasty:
Johansson 2002 reported that Harris Hip Scores were better in the arthroplasty group at three months (P = 0.001), one year (P = 0.006) and two years (P = 0.05). Neander 1997 used the Harris Hip Score at 18 months. The arthroplasty group had better results, with a mean score of 98 against 83 for the fixation group (P < 0.05). Skinner 1989 in a long term follow‐up assessed patients at a mean of 13 years after surgery using the Harris Hip Score and reported a 'trend' in favour of THR. The number of patients assessed was not stated. Tidermark 2003 used a HRQOL and ADL score. HRQOL scores were better for arthroplasty at 4 months (P < 0.005) and one and two years (P < 0.05). The ADL scores showed no statistically significant difference at 4, 12, 24 and 48 months. STARS 2006 used a composite score of pain, walking and function, which showed better results at four months and one year but not at two years (P = 0.001, P = 0.04, P = 0.11). The EuroQol (EQ‐5D) utility score showed a tendency for better results for the arthroplasty group after four months, one and two years (P = 0.02, P = 0.04, P = 0.07). Mouzopoulos 2008 using the Barthel index and Harris hip score reported a statistically significant difference between groups in favour of those treated by using a total hip arthroplasty.
Patient satisfaction
Only Davison 2001 reported on patient satisfaction, which was lowest in the internal fixation group.
Discussion
Some caution is needed when considering the results of this review because of the wide range of implants used both for fixation and replacement arthroplasty. It is likely that this variety of usage will continue in clinical practice. Recently published updates of Cochrane reviews (Parker 2010; Parker 2001 ‐ updated in 2011) have found insufficient evidence to recommend one implant over another, for either procedure. There was, however, some evidence to suggest that a cemented prosthetic replacement was associated with less risk of failure to regain mobility and less post‐operative pain than an uncemented prosthesis. More research was recommended. This may have implications for this review as those studies that used an uncemented implant may be less relevant (Blomfeldt 2005; Jensen 1984; Parker 2002; Skinner 1989).
Regarding operative details, it is clear that, compared with replacement arthroplasty, internal fixation is associated with a shorter length of surgery, and lower operative blood loss and need for transfusion.
The orthopaedic complications and resultant surgery following reduction and fixation are different to those after replacement arthroplasty. This makes it difficult to decide which treatment has a greater implication in terms of re‐operations, for the patient, surgeon and hospital resources. In addition some re‐operations are of a greater consequence than others. We subdivided re‐operations into three categories: minor, moderate and major. We accept that this division is somewhat arbitrary, but consider it is important to differentiate between a more minor surgical procedure, such as removal of an internal fixation implant which is a short operation, sometimes done as a day case procedure and under local anaesthesia, and the more extensive operations such as a revision arthroplasty.
The analyses only document the number of patients requiring secondary operations in each category. A number of these patients would have more than one secondary operation. This may occur in patients who had a removal of an internal fixation device and an arthroplasty at a later date. In addition dislocation of an arthroplasty may have occurred more than once in some patients, particularly for those with a THR. The number of times that recurrent dislocation occurred was often not reported. This meant that we were not able to present results for the total number of re‐operations for the different treatment methods. Also, the re‐operation rates given in the tables are only for those re‐operations that occurred within the follow‐up period and as documented in the individual studies. The number and nature of later surgical procedures in some studies were poorly documented. As the follow‐up period of most of the studies was one to three years the overall re‐operation rate is lower than would occur in clinical practice. This may be particularly relevant for the long‐term revision rate of the arthroplasties, which was not well documented.
The analyses for the outcome of re‐operation indicate that internal fixation is associated with an increased risk of re‐operation when compared with arthroplasty (40% versus 11%). Most re‐operations after internal fixation were accounted for by the occurrence of fracture non‐union and avascular necrosis, with surgical treatment of this by insertion of an arthroplasty. 'Major' re‐operations which were all either revision arthroplasty or surgical treatment of a fracture around an implant were more common after arthroplasty.
As would be expected for a more extensive surgical operation, arthroplasty was associated with an increased risk of deep wound infection around the implant.
For the postoperative complications of pneumonia, thromboembolic complications, cardiac failure, myocardial infarction, stroke (cerebrovascular accident) and pressure sores there was no difference in incidence between treatment methods. While there was a tendency for a lower total complication rate after internal fixation, this outcome was not present for all studies and it would be inappropriate to make definite conclusions from this.
Although pooling of data was generally not possible for the outcome of hospital stay, there appeared to be no major differences in hospital stay between treatment methods.
There was very poor reporting of the outcome measures of shortening of the limb, rotational deformity or loss of movement of the affected hip. Further studies are required to report on this outcome before any definite conclusions may be made. In particular, it may be useful to explore the correlation between anatomical and functional outcomes, to assess how much the loss of a certain degree of range of movement is clinically important from a functional point of view.
Pooling of data for mortality showed there was essentially no difference between fixation and arthroplasty. There was however a trend to a lower early mortality for those treated by internal fixation in the studies of Frihagen 2007, Jensen 1984 and Parker 2002. It is unfortunate that the data for the study of Davison 2001 cannot be included in the analysis as this study reported without usable data, a reduced mortality after internal fixation. All studies indicated that any differences in mortality that were found early were no longer present at one year and thereafter. The majority of studies did not undertake an intention‐to‐treat analysis. This may bias the outcome of mortality in favour of arthroplasty. For example, Rogmark 2002, states that 10 patients were excluded after randomisation (generally to the arthroplasty group) as they were considered unfit for arthroplasty. The outcomes for these patients should have been included within the group to which they were randomised, but were in fact excluded from the analysis. This means that potentially sicker patients were removed from the arthroplasty group.
The important final outcome measure of pain was poorly reported or not even mentioned in many studies. This makes the formation of definite conclusions on the degree of pain experienced from the two procedures impossible. There was some indication, consistent with the findings of Parker 2010, that pain was less after a cemented arthroplasty but not an uncemented arthroplasty. Again this would need confirmation.
The outcomes of failure to regain mobility and failure to return to former residential status were poorly reported and it was not possible to determine if any notable differences existed between the treatment methods.
Composite scores were used by many of the studies in assessing outcome. A number of different outcomes were used to make up these scores and included pain, movement and function ability. The variety of scores used and variable reporting of results means that such scores have limited value in summarising results within a systematic review. The results as presented suggest similar scores were achieved for the comparisons of fixation with an uncemented hemiarthroplasty, but for those studies comparing fixation with THR results, scores appeared to be better after arthroplasty.
In this review, the age range of included participants is wide notwithstanding that several trials set lower age limits (between 60 and 75 years). Some studies have only looked at patients able to pass a cognitive assessment, while others have included those with cognitive impairment including two studies that only included these patients. These factors (age and mental function) alone, in clinical practice, often influence choice of surgery. Even if there was an easy way to group trials by age of participants, this would be somewhat of an arbitrary decision and potentially subject to biases. For the 'younger' patients (age range 50 to 70), the long term outcomes of residual pain and revision are more relevant, whilst for the older patients (age over 70 years), the outcome of mortality may be more relevant. Because of the limited studies to date with their varying entry requirements and different treatment methods at present we have not been able to analyse the studies grouped for age of mental status.
Agreements and disagreements with other studies or reviews
Two previous meta‐analyses on this topic have reported similar conclusions to this study (Bhandari 2003; Rogmark 2006). These both reported the increased re‐operation rate associated with internal fixation and the absence of major differences in functional outcomes and mortality between treatment methods.
Authors' conclusions
Implications for practice.
Both internal fixation and arthroplasty have their own inherent surgical complications. Internal fixation is associated with less surgical trauma for the primary operation but fracture healing complications and secondary surgical operations are more prevalent. There appears to be no difference in the mortality at one year or more between procedures. For the survivors, pain and function appear to be better after a cemented arthroplasty.
Implications for research.
Further well‐conducted randomised controlled trials are required on this topic. Such trials should use implants and surgical techniques that reflect current practice and the best evidence available. They should have appropriate methodology with full reporting of final outcome measures and an adequate length of follow‐up. Studies should also be undertaken to see which particular groups of patients would be better treated by either internal fixation or arthroplasty. These groups may be the frail elderly, those with specific medical conditions that may affect recovery or fracture healing, or the 'younger' patient with a longer life expectancy.
Feedback
Included trials: change of setting
Summary
Jan Tidermark: I am the senior author of two of the included trials (Tidermark 2003 and Blomfeldt 2005). The setting of the studies is not correctly presented in the review. The correct address for both studies is: Karolinska Institutet at Stockholm Söder Hospital, Sweden.
Reply
Many thanks for bringing this to our attention. This has now been amended in the review.
Contributors
Lindsey Shaw (Review Group Co‐ordinator) and Martyn Parker (contact author).
What's new
| Date | Event | Description |
|---|---|---|
| 12 September 2011 | New search has been performed | For the second update, the main changes were as follows: 1. The search for trials was updated to August 2010. 2. Risk of bias was assessed for sequence generation, allocation concealment and blinding of outcome assessors. 3. There were two newly included trials (Frihagen 2007 and Mouzopoulos 2008). 4. Extra reference to the study of Rogmark 2002 added. 5. Extra references and data for two studies added after publication of long term follow‐up results for two studies (Parker 2002; Rogmark 2002). 6.Two newly identified studies (Pathi 1989; Shafee 2007) were excluded. 7. There were no changes to the conclusions of the review. |
History
Protocol first published: Issue 3, 1999 Review first published: Issue 2, 2003
| Date | Event | Description |
|---|---|---|
| 9 September 2008 | Amended | Converted to new review format. |
| 11 August 2006 | New citation required and conclusions have changed | For the first update of the review, published Issue 4, 2006, the following changes were made:
1. search updated to December 2005;
2. newly identified studies of Blomfeldt 2005, Roden 2003 and STARS 2005 included;
3. Tidermark 2003 moved from ongoing to included;
4. additional 46 cases added to study of Johansson 2000, now renamed Johansson 2002, and an extra reference added;
5. new study, El‐Abed 2005, was excluded;
6. extra references added for Parker 2000, and name changed to Parker 2002;
7. extra references added for Rogmark 2002.
In light of the new evidence, some changes were made to the conclusions of the review. For details of previous updates see 'Published Notes'. |
Notes
In Issue 2, 2001 the lead reviewer on the protocol of this review changed to Ms Moyra Masson. The previous lead reviewer, Dr Martyn Parker, remained a co‐reviewer. Some of the outcomes sought were further defined, the proposed statistical analysis changed from Peto odds ratios to relative risks and the methodological quality assessment tool was modified (Item 9).
Acknowledgements
We thank Joanne Elliott for updating the search strategy and searches, and Lindsey Elstub, Helen Handoll and Rajan Madhok for their help with various aspects of this update. For acknowledgements for former versions, see Appendix 3.
Appendices
Appendix 1. Search strategies
The Cochrane Library (Wiley Online Library)
#1 MeSH descriptor Hip Fractures explode all trees 927 #2 ((hip* or femur* or femoral* or intracapsular* or subcapital or transcervical) NEAR/4 fracture*):ti,ab,kw 1952 #3 (#1 OR #2) 1952 #4 (pin or pins or pinned or pinning or nail* or screw* or plate* or arthroplast* or fix* or prosthes*):ti,ab,kw 29319 #5 MeSH descriptor Internal Fixators, this term only 98 #6 MeSH descriptor Bone Screws, this term only 394 #7 MeSH descriptor Fracture Fixation, Internal explode all trees 652 #8 MeSH descriptor Bone Plates, this term only 212 #9 MeSH descriptor Bone Nails, this term only 250 #10 MeSH descriptor Arthroplasty, this term only 139 #11 MeSH descriptor Arthroplasty, Replacement, Hip, this term only 1172 #12 (#4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11) 29319 #13 (#3 AND #12) 745 #14 (extracapsular or trochanteric or subtrochanteric or pertrochanteric or intertrochanteric):ti 389 #15 (intracapsular or subcapital or transcervical):ti 225 #16 (#14 AND NOT #15) 379 #17 (#13 AND NOT #16) 499 #18 (SR‐MUSKINJ) 6748 #19 (#17 AND NOT #18) 145 (Restrict by product: Clinical Trials )
Lines #18 and #19 were included to filter out all records already present in the Bone, Joint and Muscle Trauma Group's Specialised Register.
MEDLINE (OVID online)
1 exp Hip Fractures/ (14794) 2 ((hip$ or femur$ or femoral$ or intracapsular$ or subcapital or transcervical) adj4 fracture$).tw. (20570) 3 or/1‐2 (24920) 4 (pin$1 or nail$ or screw$1 or plate$1 or arthroplast$ or fix$ or prosthes$).tw. (385604) 5 Internal Fixators/ or Bone Screws/ or Fracture Fixation, Internal/ or Bone Plates/ or Bone Nails/ (40241) 6 Arthroplasty/ or Arthroplasty, Replacement, Hip/ (17548) 7 or/4‐6 (404588) 8 and/3,7 (10370) 9 (extracapsular or trochanteric or subtrochanteric or pertrochanteric or intertrochanteric).ti. (3536) 10 (intracapsular or subcapital or transcervical).ti. (1753) 11 9 not 10 (3458) 12 8 not 11 (9105) 13 Randomized controlled trial.pt. (298721) 14 Controlled clinical trial.pt. (82422) 15 randomized.ab. (205154) 16 placebo.ab. (121719) 17 Clinical trials as topic/ (150826) 18 randomly.ab. (149185) 19 trial.ti. (88477) 20 13 or 14 or 15 or 16 or 17 or 18 or 19 (692318) 21 exp Animals/ not Humans/ (3531211) 22 20 not 21 (640356) 23 12 and 22 (461) 24 (2003$ or 2004$ or 2005$ or 2006$ or 2007$ or 2008$ or 2009$ or 2010$).ed. (5627549) 25 23 and 24 (209)
EMBASE (OVID online)
1 exp hip fracture/ (20636) 2 ((hip$ or femur$ or femoral or intracapsular$ or subcapital or transcervical) adj4 fracture$).tw. (23792) 3 or/1‐2 (31432) 4 (pin$1 or nail$ or screw$1 or plate$1 or arthroplast$ or fix$ or prosthes$).tw. (434374) 5 bone nail/ or bone plate/ or bone screw/ or ender nail/ or external fixator/ or fixation device/ or interlocking nail/ or internal fixator/ or osteosynthesis material/ (26043) 6 exp fracture fixation/ (52878) 7 arthroplasty/ or hip arthroplasty/ (18137) 8 or/4‐7 (465804) 9 and/3,8 (13255) 10 (extracapsular or trochanteric or subtrochanteric or pertrochanteric or intertrochanteric).ti. (4058) 11 (intracapsular or subcapital or transcervical).ti. (1907) 12 10 not 11 (3967) 13 9 not 12 (11698) 14 Randomized controlled trial/ (280313) 15 Clinical trial/ (804967) 16 Controlled clinical trial/ (161695) 17 Randomization/ (52313) 18 Single blind procedure/ (13269) 19 Double blind procedure/ (98937) 20 Prospective study/ (154609) 21 ((clinical or controlled or comparative or prospective$ or randomi#ed) adj3 (trial or study)).tw. (508940) 22 (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. (126704) 23 ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. (126329) 24 ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. (150805) 25 RCT.tw. (5874) 26 or/14‐25 (1373779) 27 Case Study/ or Abstract Report/ or Letter/ (762331) 28 26 not 27 (1345199) 29 13 and 28 (1397) 30 (2003$ or 2004$ or 2005$ or 2006$ or 2007$ or 2008$ or 2009$ or 2010$).em. (6429705) 31 29 and 30 (758)
Appendix 2. Previous search strategies
MEDLINE (OVID online) (1966 to December 2005)
1. exp Hip Fractures/ 2. ((hip$ or femur$ or femoral$ or trochant$ or pertrochant$ or intertrochant$ or subtrochant$ or intracapsular$ or extracapsular$) adj4 fracture$).tw. 3. or/1‐2 4. (pin$1 or nail$ or screw$1 or plate$1 or arthroplast$ or fix$ or prosthes$).tw. 5. Internal Fixators/ or Bone Screws/ or Fracture Fixation, Internal/ or Bone Plates/ or Bone Nails/ 6. Arthroplasty/ or Arthroplasty, Replacement, Hip/ 7. or/4‐6 8. and/3,7 9. randomized controlled trial.pt. 10. controlled clinical trial.pt. 11. Randomized Controlled Trials/ 12. Random Allocation/ 13. Double Blind Method/ 14. Single Blind Method/ 15. or/9‐14 16. exp Animals/ not Humans/ 17. 15 not 16 18. clinical trial.pt. 19. exp Clinical Trials as topic/ 20. (clinic$ adj25 trial$).tw. 21. ((singl$ or doubl$ or trebl$ or tripl$) adj25 (blind$ or mask$)).tw. 22. Placebos/ 23. placebo$.tw. 24. random$.tw. 25. Research Design/ 26. or/18‐25 27. 26 not 16 28. 27 not 17 29. Comparative Study.pt. 30. Evaluation Studies.pt. 31. Follow Up Studies/ 32. Prospective Studies/ 33. (control$ or prospectiv$ or volunteer$).tw. 34. or/29‐33 35. 34 not 16 36. 35 not (17 or 28) 37. 17 or 28 or 36 38. and/8,37
EMBASE (OVID online) (1988 to December 2005)
1. exp Hip Fracture/ 2. ((hip$ or femur$ or femoral$ or trochant$ or pertrochant$ or subtrochant$ or intracapsular$ or extracapsular$) adj4 fracture$).tw. 3. or/1‐2 4. (pin$ or nail$ or screw$ or plate$ or arthroplast$ or hemiarthroplast$ or fix$ or prosthes$).tw. 5. bone nail/ or bone plate/ or bone screw/ or ender nail/ or external fixator/ or interlocking nail/ or osteosynthesis material/ 6. exp fracture fixation/ 7. arthroplasty/ or hip arthroplasty/ 8. or/4‐7 9. and/3,8 10. exp Randomized Controlled trial/ 11. exp Double Blind Procedure/ 12. exp Single Blind Procedure/ 13. exp Crossover Procedure/ 14. Controlled Study/ 15. or/10‐14 16. ((clinical or controlled or comparative or placebo or prospective$ or randomi#ed) adj3 (trial or study)).tw. 17. (random$ adj7 (allocat$ or allot$ or assign$ or basis$ or divid$ or order$)).tw. 18. ((singl$ or doubl$ or trebl$ or tripl$) adj7 (blind$ or mask$)).tw. 19. (cross?over$ or (cross adj1 over$)).tw. 20. ((allocat$ or allot$ or assign$ or divid$) adj3 (condition$ or experiment$ or intervention$ or treatment$ or therap$ or control$ or group$)).tw. 21. or/16‐20 22. or/15,21 23. limit 22 to human 24. and/9,23
Appendix 3. Former acknowledgements and contributions of authors statements
Acknowledgements (issue 4, 2006)
Moyra Masson was the lead and Stephanie Schoelzel (formerly Fleischer) was co‐author for the first version of this review. We thank Moyra Masson for her further help with reviewing the trials for the first update. We are indebted to Prof William Gillespie and Dr Helen Handoll for their help. We would also like to thank the following for useful comments from editorial review: Prof William Gillespie, Prof James Hutchison, Prof Rajan Madhok, Prof Gordon Murray, A/Prof Peter Herbison, Dr Janet Wale and Prof Marc Swiontkowski and Mr Garnet Tregonning.
Moyra Masson's work on the first version of the review was supported by the Scottish Home and Health Department, UK.
Contributions of authors (issue 4, 2006)
Martyn Parker initiated and designed the review, read all the studies, extracted data and checked all text and results. Moyra Masson was lead author for the first edition of this review. In this capacity, she read all the studies, extracted and entered data, compiled the first drafts and checked all text and results. For the first version of the review, Stephanie Fleischer (now Schoelzel) read the majority of the studies and extracted data. For the first update of the review, Kurinchiselvum Gurusamy read all the new studies, extracted data and checked the data. Kurinchiselvum Gurusamy also checked the text and presentation of the results. Martyn Parker is the guarantor of this review.
Data and analyses
Comparison 1. Internal fixation versus arthroplasty (all types).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Length of surgery ( in minutes) | 8 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 Fixation versus hemiarthroplasty | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Fixation versus total hip replacement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Internal fixation versus replacement arthroplasty (various) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Operative blood loss (in millilitres) | 7 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 Fixation versus hemiarthroplasty | 6 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Fixation versus total hip replacement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of patients transfused | 6 | 1231 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.09, 0.64] |
| 3.1 Fixation versus hemiarthroplasty | 4 | 831 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.11, 0.53] |
| 3.2 Fixation versus total hip replacement | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 0.07 [0.02, 0.22] |
| 3.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.71, 1.63] |
| 4 Mean units blood transfused | 2 | 547 | Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.10, ‐0.04] |
| 4.1 Fixation versus hemiarthroplasty | 2 | 547 | Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.10, ‐0.04] |
| 5 Non‐union of fracture within follow‐up period (includes early displacement) | 15 | 2178 | Risk Ratio (M‐H, Fixed, 95% CI) | 27.94 [15.65, 49.86] |
| 5.1 Fixation versus hemiarthroplasty | 10 | 1454 | Risk Ratio (M‐H, Fixed, 95% CI) | 24.24 [12.68, 46.36] |
| 5.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 22.59 [5.52, 92.50] |
| 5.3 Internal fixation versus replacement arthroplasty (various) | 1 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 110.67 [6.89, 1776.91] |
| 6 Avascular necrosis | 12 | 2051 | Risk Ratio (M‐H, Fixed, 95% CI) | 19.22 [8.16, 45.27] |
| 6.1 Fixation versus hemiarthroplasty | 9 | 1394 | Risk Ratio (M‐H, Fixed, 95% CI) | 13.06 [4.82, 35.42] |
| 6.2 Fixation versus total hip replacement | 2 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 20.66 [2.83, 150.74] |
| 6.3 Internal fixation versus replacement arthroplasty (various) | 1 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 61.09 [3.77, 989.69] |
| 7 Dislocation of prosthesis | 15 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1 Fixation versus hemiarthroplasty | 10 | 1806 | Risk Ratio (M‐H, Random, 95% CI) | 0.27 [0.06, 1.16] |
| 7.2 Fixation versus total hip replacement | 6 | 806 | Risk Ratio (M‐H, Random, 95% CI) | 0.08 [0.02, 0.25] |
| 7.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.40, 4.07] |
| 8 Loosening of prosthesis | 6 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 8.1 Fixation versus hemiarthroplasty | 6 | 1185 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.22 [0.08, 0.61] |
| 8.2 Internal fixation versus total hip replacement | 1 | 320 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.00, 1.97] |
| 9 Acetabular wear (as defined by each study) | 5 | 940 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.05, 0.90] |
| 9.1 Fixation versus hemiarthroplasty | 5 | 940 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.05, 0.90] |
| 10 Fracture below/around implant | 5 | 1128 | Risk Ratio (M‐H, Random, 95% CI) | 0.40 [0.09, 1.67] |
| 10.1 Fixation versus hemiarthroplasty | 3 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.05, 4.56] |
| 10.2 Fixation versus total hip replacement | 1 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.01, 7.40] |
| 10.3 Internal fixation versus replacement arthroplasty (various) | 1 | 409 | Risk Ratio (M‐H, Random, 95% CI) | 0.18 [0.02, 1.50] |
| 11 Re‐operations minor (e.g. removal of fixation, dislocation of arthroplasty) | 17 | 2618 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.69, 2.68] |
| 11.1 Fixation versus hemiarthroplasty | 11 | 1623 | Risk Ratio (M‐H, Random, 95% CI) | 2.36 [1.05, 5.30] |
| 11.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.16, 4.70] |
| 11.3 Internal fixation versus replacement arthroplasty (various) | 2 | 680 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.00, 22.30] |
| 12 Re‐operations moderate (e.g. fixation to arthroplasty, drainage, girdlestone) | 17 | 2618 | Risk Ratio (M‐H, Random, 95% CI) | 9.35 [5.79, 15.07] |
| 12.1 Fixation versus hemiarthroplasty | 11 | 1623 | Risk Ratio (M‐H, Random, 95% CI) | 7.56 [4.88, 11.72] |
| 12.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 17.96 [4.31, 74.91] |
| 12.3 Internal fixation versus replacement arthroplasty (various) | 2 | 680 | Risk Ratio (M‐H, Random, 95% CI) | 45.28 [3.31, 619.46] |
| 13 Re‐operations major (e.g. revision arthroplasty, hemiarthroplasty to THR) | 17 | 2618 | Risk Ratio (M‐H, Random, 95% CI) | 0.41 [0.19, 0.87] |
| 13.1 Fixation versus hemiarthroplasty | 11 | 1623 | Risk Ratio (M‐H, Random, 95% CI) | 0.47 [0.16, 1.41] |
| 13.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 0.24 [0.03, 2.12] |
| 13.3 Internal fixation versus replacement arthroplasty (various) | 2 | 680 | Risk Ratio (M‐H, Random, 95% CI) | 0.19 [0.01, 4.21] |
| 14 Total re‐operation rate (within follow‐up period of study) | 19 | 3045 | Risk Ratio (M‐H, Random, 95% CI) | 3.22 [2.31, 4.47] |
| 14.1 Fixation versus hemiarthroplasty | 11 | 1623 | Risk Ratio (M‐H, Random, 95% CI) | 3.13 [1.95, 5.03] |
| 14.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 3.43 [1.45, 8.10] |
| 14.3 Internal fixation versus replacement arthroplasty (various) | 4 | 1107 | Risk Ratio (M‐H, Random, 95% CI) | 3.26 [1.65, 6.43] |
| 15 Superficial wound infection | 14 | 1986 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.53, 1.38] |
| 15.1 Fixation versus hemiarthroplasty | 9 | 1373 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.86 [0.46, 1.58] |
| 15.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.13, 1.50] |
| 15.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [0.50, 4.62] |
| 16 Deep wound infection | 15 | 2825 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.30, 0.93] |
| 16.1 Fixation versus hemiarthroplasty | 10 | 1592 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.24, 0.91] |
| 16.2 Fixation versus total hip replacement | 2 | 248 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.62 [0.11, 63.28] |
| 16.3 Internal fixation versus replacement arthroplasty (various) | 3 | 985 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.59 [0.17, 2.07] |
| 17 Pneumonia | 5 | 1003 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.51, 1.40] |
| 17.1 Fixation versus hemiarthroplasty | 4 | 857 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.56, 1.61] |
| 17.2 Fixation versus total hip replacement | 1 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.01, 2.37] |
| 18 Deep vein thrombosis | 9 | 1558 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.50, 1.96] |
| 18.1 Fixation versus hemiarthroplasty | 4 | 945 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.50, 3.96] |
| 18.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.08, 1.52] |
| 18.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.53 [0.39, 5.98] |
| 19 Pulmonary embolism | 9 | 1558 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.30 [0.59, 2.86] |
| 19.1 Fixation versus hemiarthroplasty | 4 | 945 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.89 [0.58, 6.15] |
| 19.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.92 [0.37, 10.12] |
| 19.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.51 [0.10, 2.48] |
| 20 Thromboembolic complications combined | 13 | 2174 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.13 [0.70, 1.83] |
| 20.1 Fixation versus hemiarthroplasty | 7 | 1152 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.67, 2.68] |
| 20.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.22, 2.06] |
| 20.3 Internal fixation versus replacement arthroplasty (various) | 2 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.52, 2.72] |
| 21 Congestive cardiac failure/heart failure | 4 | 1057 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.45, 1.70] |
| 21.1 Fixation versus hemiarthroplasty | 1 | 455 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.33, 3.09] |
| 21.2 Fixation versus total hip replacement | 2 | 193 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.91 [0.16, 5.04] |
| 21.3 Internal fixation versus replacement arthroplasty (various) | 1 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.79 [0.31, 2.00] |
| 22 Myocardial infarction | 6 | 1068 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.58 [0.22, 1.51] |
| 22.1 Fixation versus hemiarthroplasty | 1 | 455 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.07 [0.24, 104.94] |
| 22.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.47 [0.12, 1.82] |
| 22.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.08] |
| 23 Stroke (cerebrovascular accident) | 9 | 1645 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.43, 1.69] |
| 23.1 Fixation versus hemiarthroplasty | 4 | 725 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.23, 3.09] |
| 23.2 Fixation versus total hip replacement | 3 | 213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.20, 4.50] |
| 23.3 Internal fixation versus replacement arthroplasty (various) | 2 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.32, 2.11] |
| 24 Confusional state | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 24.1 Fixation versus hemiarthroplasty | 2 | 675 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.55, 1.39] |
| 25 Gastrointestinal complications | 3 | 703 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.54 [0.23, 1.30] |
| 25.1 Hemiarthroplasty | 2 | 557 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.28, 2.13] |
| 25.2 Total hip replacement | 1 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.02, 1.46] |
| 26 Pressure sores | 7 | 1380 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.11 [0.55, 2.23] |
| 26.1 Fixation versus hemiarthroplasty | 4 | 819 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.47, 2.66] |
| 26.2 Fixation versus total hip replacement | 2 | 152 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.25, 8.31] |
| 26.3 Internal fixation versus replacement arthroplasty (various) | 1 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.18, 4.33] |
| 27 Total medical complications (as defined in each study) | 13 | 2173 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.58, 0.92] |
| 27.1 Fixation versus hemiarthroplasty | 7 | 1151 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.51, 1.02] |
| 27.2 Fixation versus total hip replacement | 4 | 315 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.36, 1.06] |
| 27.3 Internal fixation versus replacement arthroplasty (various) | 2 | 707 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.51, 1.22] |
| 28 Length of hospital stay (in days) | 5 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 28.1 Fixation versus hemiarthroplasty | 4 | 821 | Mean Difference (IV, Random, 95% CI) | 1.12 [‐3.07, 5.31] |
| 28.2 Fixation versus total hip replacement | 1 | 75 | Mean Difference (IV, Random, 95% CI) | 4.70 [2.51, 6.89] |
| 28.3 Internal fixation versus replacement arthroplasty (various) | 1 | 298 | Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐2.43, 1.07] |
| 29 Mortality 30 days | 4 | 780 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.46, 1.24] |
| 29.1 Fixation versus hemiarthroplasty | 4 | 780 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.46, 1.24] |
| 30 Mortality up to 3 to 6 months | 15 | 2320 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.70, 1.08] |
| 30.1 Fixation versus hemiarthroplasty | 10 | 1345 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.66, 1.07] |
| 30.2 Fixation versus total hip replacement | 3 | 268 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.52 [0.89, 7.14] |
| 30.3 Internal fixation versus replacement arthroplasty (various) | 2 | 707 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.34, 1.27] |
| 31 Mortality up to 12 months | 14 | 2317 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.81, 1.11] |
| 31.1 Fixation versus hemiarthroplasty | 8 | 1213 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.78, 1.13] |
| 31.2 Fixation versus total hip replacement | 3 | 268 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.68, 2.05] |
| 31.3 Internal fixation versus replacement arthroplasty (various) | 3 | 836 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.89 [0.61, 1.30] |
| 32 Mortality up to 24 to 48 months | 15 | 2335 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.87, 1.09] |
| 32.1 Fixation versus hemiarthroplasty | 9 | 1204 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.84, 1.10] |
| 32.2 Fixation versus total hip replacement | 3 | 295 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.04 [0.71, 1.53] |
| 32.3 Internal fixation versus replacement arthroplasty (various) | 3 | 836 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.74, 1.29] |
| 33 Mortality 10 years | 2 | 864 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.92, 1.05] |
| 33.1 Fixation versus hemiarthroplasty | 1 | 455 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.90, 1.03] |
| 33.2 Internal fixation versus replacement arthroplasty (various) | 1 | 409 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.01 [0.90, 1.13] |
| 34 Residual pain at 1 year | 5 | 750 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.79, 1.94] |
| 34.1 Fixation versus hemiarthroplasty | 2 | 366 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.62, 1.05] |
| 34.2 Fixation versus total hip replacement | 2 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 3.08 [0.90, 10.56] |
| 34.3 Internal fixation versus replacement arthroplasty (various) | 1 | 256 | Risk Ratio (M‐H, Random, 95% CI) | 1.3 [1.05, 1.61] |
| 35 Residual pain at 1 year (subgrouped by cemented versus uncemented) | 5 | 750 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.79, 1.94] |
| 35.1 Fixation versus cemented (hemi)arthroplasty | 3 | 384 | Risk Ratio (M‐H, Random, 95% CI) | 1.96 [0.91, 4.23] |
| 35.2 Fixation versus uncemented (hemi)arthroplasty | 2 | 366 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.62, 1.05] |
| 36 Mean pain score at 1 to 2 years | 3 | 521 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.68, 0.26] |
| 36.1 Internal fixation versus hemiarthroplasty | 2 | 437 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.02 [‐0.43, 0.39] |
| 36.2 Internal fixation versus replacement arthroplasty (various types) | 1 | 84 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.06, ‐0.19] |
| 37 Mean pain score at 1 to 2 years (subgrouped by cemented versus uncemented) | 3 | 521 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.68, 0.26] |
| 37.1 Internal fixation versus cemented (hemi)arthroplasty | 2 | 197 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.78, ‐0.07] |
| 37.2 Internal fixation versus uncemented (hemi)arthroplasty | 1 | 324 | Std. Mean Difference (IV, Random, 95% CI) | 0.17 [‐0.05, 0.38] |
| 38 Pain at 2 to 3 years | 2 | 322 | Risk Ratio (M‐H, Random, 95% CI) | 3.49 [0.11, 115.59] |
| 38.1 Fixation versus total hip replacement | 2 | 322 | Risk Ratio (M‐H, Random, 95% CI) | 3.49 [0.11, 115.59] |
| 39 Failure to return to same residence at final follow‐up | 2 | 372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.33] |
| 39.1 Fixation versus hemiarthroplasty | 2 | 372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.33] |
| 40 Failure to regain mobility | 6 | 593 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.74, 1.39] |
| 40.1 Fixation versus hemiarthroplasty | 6 | 593 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.74, 1.39] |
| 41 Harris hip score (at 1 year) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 41.1 Fixation versus hemiarthroplasty | 2 | 223 | Mean Difference (IV, Fixed, 95% CI) | ‐6.61 [‐9.73, ‐3.49] |
| 41.2 Fixation versus total hip replacement | 1 | 65 | Mean Difference (IV, Fixed, 95% CI) | ‐10.30 [‐12.78, ‐7.82] |
| 42 Hip rating questionnaire at 1 year | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 42.1 Fixation versus hemiarthroplasty | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 42.2 Fixation versus total hip replacement | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 43 Hip scores (at 1 year) | 3 | Std. Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 43.1 Fixation versus hemiarthroplasty | 3 | 374 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.38 [‐0.58, ‐0.17] |
| 43.2 Fixation versus total hip replacement | 2 | 168 | Std. Mean Difference (IV, Fixed, 95% CI) | ‐0.77 [‐1.10, ‐0.45] |
| 44 Mean Eq‐5d score (at 1 year) | 2 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 44.1 Fixation versus hemiarthroplasty | 2 | 341 | Mean Difference (IV, Fixed, 95% CI) | ‐0.07 [‐0.14, ‐0.00] |
| 44.2 Fixation versus total hip replacement | 1 | 130 | Mean Difference (IV, Fixed, 95% CI) | ‐0.12 [‐0.33, 0.09] |
| 45 Barthel index score of below 95 at 1 year | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 45.1 Fixation versus hemiarthroplasty | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
1.11. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 11 Re‐operations minor (e.g. removal of fixation, dislocation of arthroplasty).
1.38. Analysis.
Comparison 1 Internal fixation versus arthroplasty (all types), Outcome 38 Pain at 2 to 3 years.
Comparison 2. Internal fixation versus hemiarthroplasty.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Length of surgery (in minutes) | 6 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Screws versus Thompson | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Screws versus Moore | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.3 Screws or SHS versus bipolar hemiarthroplasty | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Operative blood loss (in millilitres) | 5 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Screws versus Thompson | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.2 Screws versus Moore | 2 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2.3 Screws or SHS versus bipolar hemiarthroplasty | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of patients transfused | 5 | 1060 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.39 [0.29, 0.53] |
| 3.1 Screws versus Moore | 2 | 507 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.12 [0.06, 0.26] |
| 3.2 Screws v Christiansen bipolar | 1 | 104 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.45] |
| 3.3 Screws or SHS versus bipolar hemiarthroplasty | 2 | 449 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.56, 1.14] |
| 4 Re‐operations minor ( eg fixation‐ removal of metalwork, dislocation of hemiarthroplasty) | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.1 Screws versus Thompson | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 0.31 [0.01, 7.15] |
| 4.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 5.39 [0.23, 126.75] |
| 4.3 SHS versus Moore | 1 | 182 | Risk Ratio (M‐H, Random, 95% CI) | 0.04 [0.00, 0.67] |
| 4.4 SHS versus Stanmore bipolar | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.5 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.04, 31.12] |
| 4.6 SHS versus Thompson or Monk bipolar | 1 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 4.02 [0.75, 21.56] |
| 4.7 2 von Bahr screws versus Variokopf bipolar hemiarthroplasty | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.35, 3.26] |
| 4.8 2 Olmed screws versus bipolar hemiarthroplasty | 1 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 2.80 [1.31, 5.98] |
| 5 Re‐operations moderate (eg fixation to hemiarthroplasty or total hip replacement, drainage, girdlestone) | 12 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 5.1 Screws versus Thompson | 2 | 91 | Risk Ratio (M‐H, Random, 95% CI) | 6.12 [1.13, 33.22] |
| 5.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Random, 95% CI) | 8.15 [2.46, 26.98] |
| 5.3 SHS versus Moore | 1 | 182 | Risk Ratio (M‐H, Random, 95% CI) | 10.00 [3.16, 31.60] |
| 5.4 SHS versus Stanmore bipolar | 1 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 3.14 [0.71, 13.87] |
| 5.5 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Random, 95% CI) | 3.72 [1.28, 10.76] |
| 5.6 SHS versus Thompson or Monk bipolar | 1 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 17.43 [5.41, 56.09] |
| 5.7 2 von Bahr screws versus Variokopf bipolar hemiarthroplasty | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 7.39 [2.38, 22.91] |
| 5.8 2 Olmed screws versus bipolar hemiarthroplasty | 1 | 219 | Risk Ratio (M‐H, Random, 95% CI) | 8.37 [3.45, 20.32] |
| 6 Re‐operations major (eg revision hemiarthroplasty or conversion to total hip replacement) | 12 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Screws versus Thompson | 2 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.32, 1.60] |
| 6.3 SHS versus Moore | 1 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.42] |
| 6.4 SHS versus Stanmore bipolar | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.10 [0.01, 1.62] |
| 6.5 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.01, 0.52] |
| 6.6 SHS versus Thompson or Monk bipolar | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.07, 6.36] |
| 6.7 2 von Bahr screws versus Variokopf bipolar hemiarthroplasty | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.30 [0.01, 7.10] |
| 6.8 2 Olmed screws versus bipolar hemiarthroplasty | 1 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.76 [0.48, 160.76] |
| 7 Total re‐operation rate (within follow‐up period of study) | 14 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Screws versus Thompson | 2 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.15 [1.22, 21.68] |
| 7.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.82 [3.85, 8.79] |
| 7.3 SHS versus Moore | 1 | 182 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.36 [0.85, 2.18] |
| 7.4 SHS versus Stanmore bipolar | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.90 [0.36, 2.23] |
| 7.5 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.72, 2.47] |
| 7.6 SHS versus Thompson or Monk bipolar | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.04 [3.34, 14.83] |
| 7.7 SHS versus hemiarthroplasty (unknown type) | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.4 [0.92, 6.23] |
| 7.8 Screws or SHS versus bipolar hemiarthroplasty | 1 | 229 | Risk Ratio (M‐H, Fixed, 95% CI) | 7.21 [3.21, 16.22] |
| 7.9 2 von Bahr screws versus Variokopf bipolar hemiarthroplasty | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.93 [1.91, 8.07] |
| 7.10 2 Olmed screws versus bipolar hemiarthroplasty | 1 | 219 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.16 [2.28, 7.58] |
| 8 Superficial wound infection | 9 | 1502 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.87 [0.50, 1.53] |
| 8.1 Screws versus Thompson | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.09 [0.00, 1.48] |
| 8.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.45 [0.56, 3.77] |
| 8.3 SHS versus Stanmore bipolar | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.21 [0.01, 4.11] |
| 8.4 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.11, 2.13] |
| 8.5 SHS versus Thompson or Monk bipolar | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.0 [0.25, 145.88] |
| 8.6 Screws or SHS versus bipolar hemiarthroplasty | 1 | 229 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.41 [0.41, 4.87] |
| 9 Deep wound infection | 11 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 Screws versus Thompson | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.17 [0.04, 0.75] |
| 9.3 SHS versus Moore | 1 | 198 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.15 [0.01, 2.79] |
| 9.4 SHS versus Stanmore bipolar | 1 | 43 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 9.5 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.35 [0.08, 1.66] |
| 9.6 SHS versus Thompson or Monk bipolar | 1 | 280 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.03, 16.21] |
| 9.7 Screws or SHS versus bipolar hemiarthroplasty | 2 | 448 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.23 [0.48, 3.11] |
| 10 Length of hospital stay (in days) | 5 | 1036 | Mean Difference (IV, Random, 95% CI) | 0.79 [‐2.13, 3.72] |
| 10.1 Screws versus Thompson | 1 | 60 | Mean Difference (IV, Random, 95% CI) | 4.5 [‐11.20, 20.20] |
| 10.2 Screws versus Moore | 1 | 455 | Mean Difference (IV, Random, 95% CI) | 0.30 [‐5.20, 5.80] |
| 10.3 Screws or SHS versus bipolar hemiarthroplasty | 2 | 449 | Mean Difference (IV, Random, 95% CI) | ‐0.80 [‐2.60, 1.00] |
| 10.4 SHS versus hemiarthroplasty (unknown type) | 1 | 72 | Mean Difference (IV, Random, 95% CI) | 3.90 [2.45, 5.35] |
| 11 Mortality at 30 days | 4 | 780 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.46, 1.24] |
| 11.1 SHS or screws versus bipolar hemiarthroplasty | 4 | 780 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.76 [0.46, 1.24] |
| 12 Mortality up to 3 to 6 months | 10 | 1474 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.64, 1.03] |
| 12.1 Screws versus Thompson | 2 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.52, 2.00] |
| 12.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.77 [0.56, 1.08] |
| 12.3 SHS versus Stanmore bipolar | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.25 [0.03, 2.05] |
| 12.4 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.12 [0.61, 2.08] |
| 12.5 Screws or SHS versus bipolar hemiarthroplasty | 2 | 451 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.41, 1.23] |
| 13 Mortality up to 12 months | 10 | 1528 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.78, 1.11] |
| 13.1 Screws versus Thompson | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.34 [0.85, 2.11] |
| 13.2 Screws versus Moore | 3 | 617 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.73, 1.21] |
| 13.3 SHS versus Stanmore bipolar | 1 | 41 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.09, 1.92] |
| 13.4 Screws, SHS or nail & plate versus Christiansen bipolar | 2 | 273 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.60, 1.54] |
| 13.5 Screws or SHS versus bipolar hemiarthroplasty | 2 | 451 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.82 [0.55, 1.24] |
| 13.6 SHS versus hemiarthroplasty (unknown type) | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.27, 2.53] |
| 14 Mortality 24 to 48 months | 11 | 1519 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.95 [0.84, 1.08] |
| 14.1 Screws versus Thompson | 2 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.91, 1.49] |
| 14.2 Screws versus Moore | 3 | 580 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.73, 1.06] |
| 14.3 2 von Bahr screws versus Variokopf bipolar hemiarthroplasty | 1 | 100 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.55 [0.48, 4.97] |
| 14.4 SHS versus Stanmore bipolar | 1 | 42 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.30, 2.31] |
| 14.5 SHS or nail & plate versus Christiansen bipolar | 1 | 169 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.67, 1.56] |
| 14.6 Screws or SHS versus bipolar hemiarthroplasty | 2 | 451 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.97 [0.71, 1.32] |
| 14.7 SHS versus hemiarthroplasty (unknown type) | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.43, 1.67] |
| 15 Mortality 10 years | 1 | 455 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.90, 1.03] |
| 15.1 Screws versus Moore | 1 | 455 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.90, 1.03] |
| 16 Pain at one year | 3 | 561 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.98 [0.82, 1.18] |
| 16.1 Screws versus Thompson | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Screws versus Moore | 2 | 366 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.62, 1.04] |
| 16.3 Screws or SHS versus bipolar hemiarthroplasty | 1 | 195 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.26 [0.99, 1.61] |
| 17 Failure to return to same residence at final follow‐up | 2 | 372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.33] |
| 17.1 Screws versus Moore | 2 | 372 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.84 [0.54, 1.33] |
| 18 Failure to regain mobility | 6 | 593 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.86, 1.15] |
| 18.1 Screws versus Thompson | 1 | 24 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.87 [0.53, 6.57] |
| 18.2 Screws versus Moore | 3 | 419 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.88 [0.75, 1.04] |
| 18.3 2 von Bahr screws versus Variokopf bipolar hemiarthroplasty | 1 | 84 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.95 [1.15, 3.30] |
| 18.4 Screws v Christiansen bipolar | 1 | 66 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.69, 1.43] |
2.3. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 3 Number of patients transfused.
2.4. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 4 Re‐operations minor ( eg fixation‐ removal of metalwork, dislocation of hemiarthroplasty).
2.5. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 5 Re‐operations moderate (eg fixation to hemiarthroplasty or total hip replacement, drainage, girdlestone).
2.6. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 6 Re‐operations major (eg revision hemiarthroplasty or conversion to total hip replacement).
2.7. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 7 Total re‐operation rate (within follow‐up period of study).
2.8. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 8 Superficial wound infection.
2.9. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 9 Deep wound infection.
2.10. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 10 Length of hospital stay (in days).
2.11. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 11 Mortality at 30 days.
2.12. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 12 Mortality up to 3 to 6 months.
2.13. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 13 Mortality up to 12 months.
2.14. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 14 Mortality 24 to 48 months.
2.15. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 15 Mortality 10 years.
2.16. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 16 Pain at one year.
2.17. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 17 Failure to return to same residence at final follow‐up.
2.18. Analysis.
Comparison 2 Internal fixation versus hemiarthroplasty, Outcome 18 Failure to regain mobility.
Comparison 3. Internal fixation versus Total Hip Replacement.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Length of surgery (in minutes) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 1.1 2 Olmed screws verus Exeter THR | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 Screws or SHS versus THR (various) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Operative blood loss (in millilitres) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2.1 2 Olmed screws verus Exeter THR | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Number of patients transfused | 2 | 240 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.20, 0.50] |
| 3.1 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.07 [0.02, 0.22] |
| 3.2 Screws or SHS versus THR (various) | 1 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.74 [0.43, 1.26] |
| 4 Re‐operations minor (Fixation removal of metalwork, dislocation of THR) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Hansson pin versus Charnley | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.80] |
| 4.2 2 Olmed screws versus Lubinus or BiMetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.52 [0.23, 1.14] |
| 4.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 9.25 [1.23, 69.60] |
| 4.4 SHS versus Howse II | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.03 [0.00, 0.43] |
| 5 Re‐operations moderate (Fixation to hemiarthroplasty or THR, drainage, girdlestone) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5.1 Hansson pin versus Charnley | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 14.4 [0.87, 238.56] |
| 5.2 2 Olmed screws versus Lubinus or BiMetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 27.16 [3.66, 201.50] |
| 5.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 34.26 [2.12, 553.64] |
| 5.4 SHS versus Howse II | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 59.67 [3.70, 961.20] |
| 6 Re‐operations major (revision THR) | 5 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 6.1 Hannson pin versus Charnley | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.48] |
| 6.2 2 Olmed screws versus Lubinus or BiMetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.76] |
| 6.4 SHS versus Howse II | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.08 [0.00, 1.32] |
| 7 Total re‐operation rate (within follow‐up period of study) | 7 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Hansson pin versus Charnley | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.35 [0.78, 14.50] |
| 7.2 2 Olmed screws versus Lubinus or Bimetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.32 [1.36, 3.94] |
| 7.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 11.56 [2.89, 46.25] |
| 7.4 SHS versus Howse II | 1 | 180 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.47 [0.90, 2.38] |
| 7.5 Screws or SHS versus THR (various) | 1 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 4.5 [1.98, 10.21] |
| 7.6 SHS versus THR (unknown type) | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 12.0 [1.63, 88.29] |
| 8 Superficial wound infection | 4 | 315 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.43 [0.13, 1.50] |
| 8.1 Hansson pin versus Charnley | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.32 [0.01, 7.48] |
| 8.2 2 Olmed screws versus Lubinus or BiMetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.66 [0.14, 3.15] |
| 8.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.19 [0.01, 3.76] |
| 9 Deep wound infection | 3 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 9.1 SHS versus Howse II | 1 | 178 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.16 [0.01, 3.36] |
| 9.2 2 Olmed screws versus Lubinus or BiMetric | 1 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.62 [0.11, 63.28] |
| 9.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Hospital stay (days) | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 10.1 Screws or SHS versus THR (various) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 10.2 SHS versus THR (unknown type) | 1 | Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Mortality up to 2 to 4 months | 4 | 406 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.21 [0.91, 5.40] |
| 11.1 2 Olmed screws versus Lubinus or BiMetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.03 [0.65, 6.29] |
| 11.2 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 6.48 [0.34, 122.37] |
| 11.3 Screws or SHS versus THR (various) | 1 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.26, 8.70] |
| 12 Mortality at 12 to 18 months | 4 | 390 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.03 [0.64, 1.64] |
| 12.1 2 Olmed screws versus Lubinus or BiMetric | 2 | 166 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.99 [0.55, 1.76] |
| 12.2 Screws or SHS versus THR (various) | 1 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.44, 5.08] |
| 12.3 SHS versus THR (unknown type) | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.27, 2.53] |
| 13 Mortality at 24 months | 4 | 433 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.18 [0.79, 1.75] |
| 13.1 Hansson pin versus Charnley | 1 | 47 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.64 [0.12, 3.48] |
| 13.2 2 Olmed screws versus Lubinus or BiMetric | 1 | 146 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.61, 1.66] |
| 13.3 2 Olmed screws verus Exeter THR | 1 | 102 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [0.68, 5.03] |
| 13.4 Screws or SHS versus THR (various) | 1 | 138 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.5 [0.56, 3.99] |
| 14 Mortality at 4 years | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Totals not selected | |
| 14.1 SHS versus THR (unknown type) | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Pain at 1 year | 2 | 157 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.40 [1.02, 1.90] |
| 15.1 Hansson pin versus Charnley | 1 | 35 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.91 [0.80, 4.55] |
| 15.2 Screws or SHS versus THR (various) | 1 | 122 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.31 [0.94, 1.82] |
3.3. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 3 Number of patients transfused.
3.4. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 4 Re‐operations minor (Fixation removal of metalwork, dislocation of THR).
3.5. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 5 Re‐operations moderate (Fixation to hemiarthroplasty or THR, drainage, girdlestone).
3.6. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 6 Re‐operations major (revision THR).
3.7. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 7 Total re‐operation rate (within follow‐up period of study).
3.8. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 8 Superficial wound infection.
3.9. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 9 Deep wound infection.
3.10. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 10 Hospital stay (days).
3.11. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 11 Mortality up to 2 to 4 months.
3.12. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 12 Mortality at 12 to 18 months.
3.13. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 13 Mortality at 24 months.
3.14. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 14 Mortality at 4 years.
3.15. Analysis.
Comparison 3 Internal fixation versus Total Hip Replacement, Outcome 15 Pain at 1 year.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Blomfeldt 2005.
| Methods | Randomisation by: sealed envelopes technique | |
| Participants | One hospital, Karolinska Institute at Stockholm Söder Hospital, Sweden. 60 patients. Characteristics of participants: Mean age: 84 years. Male: 6 (10%) Loss to follow‐up: 1 (2%) Inclusions: short portable mental status questionnaire of less than 3/10 or a diagnosis of dementia, displaced fracture of the femoral neck, aged 70 years plus, able to walk independently Exclusions: pathological fractures, fracture more than 24 hours from occurrence, rheumatoid arthritis, osteoarthritis | |
| Interventions | 1. Reduction and fixation with two cannulated screws versus 2. Uncemented Moore unipolar hemiarthroplasty inserted via an anterolateral modified Hardinge approach | |
| Outcomes | Follow‐up for 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: length of surgery in minutes, operative blood loss, number of patients transfused (b) Complications related to type of operation: For internal fixation: fixation failure, early redisplacement, non‐union, avascular necrosis, fracture around implant For replacement arthroplasty: fracture around implant, dislocation Re‐operations Wound healing: superficial, infection, deep sepsis (c) Postoperative complications: none (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 4, 12, 24 months Pain at 4, 12, 24 months; Activities of daily living score; Health related quality of life questionnaire; Walking ability (Charnley score); Movement of the hip (Charnley score); Failure to regain mobility (g) Economic cost: none | |
| Notes | Additional information supplied by trialists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | 'sealed envelopes technique' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | not mentioned |
Davison 2001.
| Methods | Randomisation by: computer generation of random numbers. | |
| Participants | General hospital, Leicester, UK. From 1 January 1991 to 31 January 1996 280 patients. Characteristics of participants: Median age: in each group 73, 76, 75 (range 69 to 79). Male: 67 (24%) Loss to follow‐up: 50 (17.9%) Inclusions: Displaced intracapsular fracture of the proximal femur, Aged 65 to 79 Exclusions: Abbreviated mental test score < 5/13, uncontrolled Parkinson's disease, pathological fracture, disseminated malignancy, Paget's disease, rheumatoid arthritis, long‐term steroids | |
| Interventions | 1. Reduction and fixation with 'Ambi' compression hip screw (AHS) and 2 hole plate versus: 2. Cemented Thompson unipolar hemiarthroplasty (Hardinge approach) versus 3. Cemented Monk bipolar hemiarthroplasty (Hardinge approach) | |
| Outcomes | Follow‐up for 5 years at 6/52, 1/12, 24/12, 36/12, 48/12, 60/12. Actual minimum 2 years OUTCOMES COLLECTED BY TRIAL (a) Operative details: none (b) Complications related to type of operation: For internal fixation: non‐union, migration and cut‐out of screw, avascular necrosis and collapse, degeneration of joint For replacement arthroplasty: acetabular erosion, loosening and subsidence (c) Postoperative complications: none (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 6, 12, 18, 24, 30, 36 months and time to death Time to revision Harris hip score Subjective function and satisfaction Functional outcome from home assessment Barthel index (for activities of daily living) Time to preinjury state and satisfaction with outcome (g) Economic cost: none | |
| Notes | Discrepancy with abstract 1997 which mentions 282 patients. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'computer generation of random numbers' |
| Allocation concealment (selection bias) | Unclear risk | 'computer generation of random numbers' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | Low risk | Home assessment of patients by observer blinded to type of operative treatment |
Frihagen 2007.
| Methods | Randomisation by: sealed opaque numbered envelopes. | |
| Participants | One university hospital, Oslo, Norway From September 2002 to March 2004 222 fractures in 221 patients Mean age: 83 years (range not stated). Male: 57 (26%) Loss to follow‐up: 1 (0.5%) Inclusions: age 60 years and above, displaced fracture of the femoral neck, previously ambulant Exclusions: pathological fractures, fracture more than 96 hours from occurrence, previous hip pathology, unfit for either procedure, living outside the hospital area | |
| Interventions | 1. Reduction and fixation with two Olmed screws versus 2. Cemented Charnley‐Hastings bipolar hemiarthroplasty | |
| Outcomes | Follow‐up for 48 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: length of surgery in minutes, operative blood loss, number of patients transfused (b) Complications related to type of operation: For internal fixation: fixation failure, early redisplacement, non‐union, avascular necrosis, fracture around implant For replacement arthroplasty: fracture around implant, dislocation, loosening of the implant Re‐operations Wound healing: superficial, infection, deep sepsis (c) Postoperative complications: deep vein thrombosis pulmonary embolism pressure sores confusion wound infections (d) Postoperative care outcomes: length of hospital stay (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 1, 4, 12 and 24 months Pain (visual analogue scale) at 4 months, 1 and 2 years Harris hip score at 4 months, 1 and 2 years Eq 5d score at 4 months, 1 and 2 years Barthel index score at 4 months, 1 and 2 years (g) Economic cost: none | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'envelopes sealed and mixed before they were numbered' |
| Allocation concealment (selection bias) | Low risk | 'opaque envelopes' which were sealed and mixed before being numbered |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | Low risk | The physiotherapist undertaking the follow‐up assessments was blinded to the treatment group |
Jensen 1984.
| Methods | Randomisation by: random numbers using sealed opaque envelopes. | |
| Participants | One hospital, Ashrus, Denmark. From 2 January 1975 to 31 August 1978 102 patients Characteristics of participants: Median age: in each group 80.5 and 70 years. Male: 32 (31%) Reported that the fixation group included more patients with a poor prognosis. Loss to follow‐up: 2 (2%) Inclusions: Fresh and non‐pathological fractures of the femoral neck, displaced to stage III or IV Garden, aged 70 years plus Exclusions: pathological fractures (by inference) | |
| Interventions | 1. Reduction and fixation with 4 AO screws versus 2. Uncemented Moore unipolar hemiarthroplasty inserted via a posterior approach | |
| Outcomes | Follow‐up for 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: length of surgery in minutes (b) Complications related to type of operation: For internal fixation: fixation failure, early redisplacement, non‐union, avascular necrosis For replacement arthroplasty: prosthesis loosening, settling, acetabular protrusion, periarticular calcification (grade 3), allergy to metal For both methods of treatment:per or subtrochanteric fracture, femoral shaft fracture Re‐operations Wound healing: superficial, infection, deep sepsis, haematoma (c) Postoperative complications: Deep vein thrombosis, Pulmonary embolism Medical complications: cardiopulmonary, neurological, gastrointestinal, urinary retention, pressure sore (d) Postoperative care outcomes: Mean time to weight‐bearing (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 1, 6, 12, 24 months Need for walking aids Social function Stitchfield's hip assessment (incorporates pain, range of movement, ability to walk) (g) Economic cost: none | |
| Notes | Additional information from Dr Jensen | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | random numbers using sealed opaque envelopes. |
| Allocation concealment (selection bias) | Unclear risk | random numbers using sealed opaque envelopes |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding |
Johansson 2002.
| Methods | Randomisation by: sequentially numbered sealed envelopes. Only those patients allocated to THR were consented to the study | |
| Participants | One orthopaedic hospital, Linkoping, Sweden. From September 1994 to May 1998 143 patients. Characteristics of participants: Mean age: 84 (range 75 to 101) Male: 34 (24%) Loss to follow‐up: 15 (10%) Inclusions: displaced and acute femoral neck fracture, aged 75 and over, dementia not an exclusion, ambulatory before trauma Exclusions: contraindications to major surgery, malignancy of significance, signs of rheumatic joint disease, anaesthetically unfit for total hip arthroplasty | |
| Interventions | 1. Reduction and fixation with 2 parallel Olmed screws versus 2. Total hip replacement, Lubinus IP (cemented, dorsolateral approach) | |
| Outcomes | Follow‐up for 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: none (b) Complications related to type of operation: For internal fixation: redisplacement, non‐union, avascular necrosis, intolerable hip pain, local pain from screws For replacement arthroplasty: stiff hip, dislocations For both methods of treatment: re‐operations, superficial infection, deep wound infection (c) Postoperative complications: Deep vein thrombosis Pneumonia Medical complications, Gastrointestinal bleed, heart failure Cerebrovascular accident ‐Myocardial infarction Hospital stay (d) Postoperative care outcomes: none (e) Anatomical restoration:none (f) Final outcome measures: Mortality at 3, 12, 24 months Harris hip score after surgery, at 3/12, 1 and 2 years (g) Economic costs: Cost is Swedish Korona | |
| Notes | 146 fractures in 143 patients. 5 further cases were allocated to THR but refused to participate and excluded and a further 11 were excluded after randomisation. Additional publication looking at heterotopic ossification. Appears to use same patients as main study although there is a discrepancy in the dates patients were included between the two papers. Additional information supplied by Dr Johansson. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated how the envelopes were prepared. |
| Allocation concealment (selection bias) | Unclear risk | Numbered sequentially sealed envelopes were used and then only those allocated to THR were consented to the study. It remains unclear if for those allocated to THR any patients refused and were then excluded. |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding |
Jonsson 1996.
| Methods | Randomisation by: sealed envelope. | |
| Participants | One hospital, Malmo, Sweden. 1990s 47 patients. Characteristics of participants: Median age fixation 79, arthroplasty 80 (range 67 to 89) Male: 11 (23%) Loss to follow‐up: 2 (4%) Inclusions: cervical hip fracture, Garden III or IV; fully ambulatory and living in own homes before the fracture Exclusions: fracture > 48 hours old at time of admission, considered by anaesthetist not to be healthy enough to with stand strain of a hip replacement | |
| Interventions | 1. Reduction and fixation with Hansson hook pins versus 2. Total hip replacement, Charnley (trochanteric osteotomy) | |
| Outcomes | Follow‐up for 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: none (b) Complications related to type of operation: For internal fixation: non‐union, late segmental collapse For replacement arthroplasty: dislocation For both methods of treatment: superficial infection (c) Postoperative complications: Confusion Deep vein thrombosis Pulmonary embolism Bedsore Urinary tract infection Myocardial infarction Heart failure (d) Postoperative care outcomes: Length of hospital stay (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 24 months Social, walking, pain (g) Economic cost: none | |
| Notes | Pilot study. 50 randomised. 3 excluded after randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'sealed envelope' |
| Allocation concealment (selection bias) | Unclear risk | 'sealed envelope' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding |
Mouzopoulos 2008.
| Methods | Method of randomisation: alternation | |
| Participants | Orthopaedic unit in Athens, Greece From April 1999 to April 2002 129 patients with a displaced intracapsular fracture. Mean age: 74 years (range not stated) Percentage male: 31 (28% of 109) Follow‐up: mean 48 months Loss to follow‐up: 2 (4%) lost but in addition, 8 excluded because of previous hip fracture and 18 patients who had revision surgery were not followed‐up for the functional assessments. Inclusions: age over 70 years, good cognitive function, moderately dependent, displaced intracapsular fracture Exclusions: Pagets disease, history of cancer, rheumatoid arthritis |
|
| Interventions | 1. Internal fixation with a Sliding Hip Screw
versus: 2. Merte hemiarthroplasty versus 3. De Puy total hip replacement. It was not stated if the prostheses were cemented in place |
|
| Outcomes | Follow‐up for 48 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: none (b) Complications related to type of operation Re‐operations (1 and 4 years) (c) Postoperative complications: none (d) Postoperative care outcomes: Length of hospital stay (e) Anatomical restoration: none (f) Final outcome measures: Mortality (1 and 4 years) Barthel score (1 and 4 years) Harris hip score (1 and 4 years) Range of movement Walking speed (g) Economic cost: none | |
| Notes | Eight patients who had had a previous hip fracture and 18 patients who had a revision operation were excluded from the follow‐up assessments. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 'these 129 participants were randomly divided, by two orthopaedic surgeons, into three groups according to the type of surgical operation there were to undergo, following this order: hemi‐arthroplasty, total arthroplasty, internal fixation, etc" |
| Allocation concealment (selection bias) | High risk | alternation: as above |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | Low risk | Assessors of function were blinded to the type of surgery |
Neander 1997.
| Methods | Randomisation by: closed envelopes. | |
| Participants | One hospital, Stockholm, Sweden. From February 1990 to October 1990 20 patients. Loss to follow‐up: none Characteristics of participants: Mean age: 86 (range 79 to 94) Male: 5 (25%) Inclusions: fresh displaced femoral neck fracture, stage III‐IV; aged over 65, admitted from own homes Exclusions: history of previous disabilities of the legs, hormonal therapy or other medications or suffered from illnesses known to affect the bone metabolism | |
| Interventions | 1. Reduction and fixation with 2 parallel Olmed screws versus 2.Total hip replacement, BiMetric (cemented, posterior approach) | |
| Outcomes | Follow‐up for 18 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: none (b) Complications related to type of operation: Infection Re‐operations (c) Postoperative complications: Pulmonary embolism Myocardial infarction Cerebral infarction (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 18 months Bone mineral density Harris hip score (g) Economic cost: none | |
| Notes | Four patients not included in bone mineral density analysis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | no mentioned |
| Allocation concealment (selection bias) | Unclear risk | closed envelopes |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding |
Parker 2002.
| Methods | Randomisation by: sealed opaque identical envelopes containing the instructions about the type of operation. | |
| Participants | One hospital, Peterborough, UK. From July 1991 to February 2001 455 patients. Characteristics of participants: Mean age 82 years (range 71 to 103) Male: 91 (20%) Loss to follow‐up: none at one year. Two in the long term follow‐up report. Inclusions: displaced cervical hip fracture (defined as clear displacement of the fracture on both anteroposterior and lateral radiograms), aged > 70 years Exclusions: rheumatoid arthritis, chronic renal failure, significant arthritis of hip, patient unfit for either surgical procedure, delay > 48 hours fracture to surgery, Paget's disease, metabolic bone disease | |
| Interventions | 1. Reduction and fixation with 3 AO screws versus 2. Uncemented Austin Moore unipolar hemiarthroplasty (anterolateral approach) | |
| Outcomes | Follow‐up for minimum 1 year for all survivors for initial report. Subsequent long‐term follow‐up report with mean follow‐up of survivors of 10.6 years (range 9‐15 years) OUTCOMES COLLECTED BY TRIAL (a) Operative details: Length of surgery in minutes Operative blood loss in ml Units blood transfused Operative blood pressure fall (b) Complications related to type of operation For internal fixation: non‐union, avascular necrosis For replacement arthroplasty: dislocation, loosening of prosthesis For both methods: Fracture below/around implant Re‐operations Superficial wound infection Deep wound infection (c) Postoperative complications: Deep vein thrombosis Pulmonary embolism Congestive cardiac failure Confusion post‐op Pressure sores Urinary retention Gastrointestinal bleeding Gastric aspiration Renal failure Clostridia diarrhoea Amputation leg (d) Postoperative care outcomes Length hospital stay/orthopaedic ward only, total stay, stay inclusive of readmission time Mean dose morphine post‐op Mean number co‐proxamol (e) Anatomical restoration: Shortening Loss of flexion (f) Final outcome measures: Mortality for minimum follow‐up of 9 years Pain scores (Charnley) (up to 9 to 15 years) Residence (up to 9 to 15 years) ‐Reduction in mobility (up to 9‐15 years) ‐Walking aids (up to 9‐15 years) ‐Activities of daily living score (g) Economic cost: Mean cost including readmissions and additional surgery | |
| Notes | One year results published as for the principle reference. Subsequent report with long‐term follow up of the patients. Additional data supplied by MJ Parker. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | envelopes containing the operative instructions were not independently prepared |
| Allocation concealment (selection bias) | Unclear risk | sealed opaque identical envelopes |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | All outcomes recorded by lead trialists |
Puolakka 2001.
| Methods | Randomisation by: sealed envelopes. | |
| Participants | one centre, Tampere, Finland From February 1994 31 patients Characteristics of participants: Mean age 81 yr fixation, 82 years arthroplasty (range 77 to 90) 5 (16%) male Loss to follow‐up: none Inclusions: femoral neck fracture, Garden 3‐4; aged > 75 years Exclusions: unable to walk independently (without other person's help), rheumatoid arthritis | |
| Interventions | 1. Reduction and fixation with 3 Ulleval screws versus 2. Cemented Thompson unipolar hemiarthroplasty (posterior approach) | |
| Outcomes | Follow‐up for 2 years at 6 weeks, 3, 12, 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details Mean length of surgery in minutes Mean operative blood loss in ml (b) Complications related to type of operation Internal fixation/pseudarthrosis, osteonecrosis, failed osteosynthesis Replacement arthroplasty/evaluation of stem position and cementing For both methods: Re‐operation, wound infection (c) Postoperative complications Immediate systemic complications (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures Mortality 3 and 24 months (g) Economic cost | |
| Notes | Study terminated early due to high complication rate in fixation group. One patient randomised to receive internal fixation was excluded from the study as acceptable reduction of the fracture could not be achieved and this patient was treated with an arthroplasty. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | 'sealed envelopes' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding of assessors of pain and function |
Roden 2003.
| Methods | Randomisation by: sealed envelopes. | |
| Participants | One hospital, Sundsvall County Hospital, Sweden. From February 1992 to September 1994 100 patients. Characteristics of participants: Mean age 81 years (range 70 to 96) Male: 29 (29%) Loss to follow‐up: not stated Inclusions: displaced cervical hip fracture, aged > 70 years Exclusions: senile dementia, immobility, unable to consent, refusal, delay > 12 hours fracture to surgery, 'medical findings' | |
| Interventions | 1. Reduction and fixation with 2 von Bahr screws versus 2. Cemented Variokopf bipolar hemiarthroplasty (posterior approach) | |
| Outcomes | Follow‐up for minimum 5 years all survivors OUTCOMES COLLECTED BY TRIAL (a) Operative details: Length of surgery in minutes Operative blood loss in ml Units blood transfused (b) Complications related to type of operation For internal fixation: non‐union, avascular necrosis For replacement arthroplasty: dislocation For both methods: Re‐operation Superficial wound infection Deep wound infection (c) Postoperative complications: not clearly stated (d) Postoperative care outcomes Length hospital stay /orthopaedic ward only Number discharged home directly (e) Anatomical restoration: no outcomes (f) Final outcome measures: Mortality at 2 and 5 years Pain at 4 months and 5 years (g) Economic cost: none given | |
| Notes | Extra information supplied by trialists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not stated |
| Allocation concealment (selection bias) | Unclear risk | 'sealed envelopes' opened in the operating room |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding of assessors of pain and function |
Rogmark 2002.
| Methods | Randomisation by: sealed, opaque numbered envelopes drawn sequentially. | |
| Participants | Multicentre: 12 centres in Sweden From 1995 to 1997 409 patients Characteristics of participants: Mean age male, 80.7 years Mean age female, 81.8 years Male: 85 (21%) Loss to follow‐up at 2 years: 41/450 were drop‐outs (10 planned surgery stopped due to medical reasons, 8 lost to follow‐up, 7 not meeting criteria, 13 withdrawals, 3 died before surgery). 409 included in analysis. Inclusions: cervical hip fracture, graded 3‐4; independent, mentally alert Exclusions: mentally confused, bedridden or institution dwelling, rheumatoid arthritis, fracture > 2 days | |
| Interventions | 1. Reduction and fixation with Hansson hook‐pins or Olmed screws versus 2. Replacement arthroplasty, various types, choice of surgeon and included cemented and uncemented types. | |
| Outcomes | Follow‐up for 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: Time admission to surgery. Length of surgery in minutes (b) Complications related to type of operation For internal fixation: non‐union or early redisplacement, avascular necrosis, pain. For replacement arthroplasty: dislocation, diaphyseal fracture. For both methods: Re‐operation Deep infection Failure (c) Postoperative complications: stroke, pulmonary or cardiac insufficiency, pressure sores, venous thromboembolic complication (d) Postoperative care outcomes Length of hospital stay. (e) Anatomical restoration: None (f) Final outcome measures: Mortality, perioperative and at 4, 12 and 24 months Functional outcome (walking ability and pain) Pain Mobility (g) Economic cost: for a subgroup of 68 cases | |
| Notes | Twenty‐six patients did not attend 2 year control (failure status reported at 1 year) Additional information supplied by the trialists Cost information was reported in a paper in 2003 for a subgroup of 68 cases. Subsequent report of this study with a long‐term follow‐up of included patients (Leonardsson 2010) presents the outcomes of mortality, surgical complications, re‐operations, hip pain and mobility. Mean follow up was 123/124 months with 4 patients lost to follow‐up. The number of dislocations was reported as 15 in the original report but 12 in the later report with two of these dislocations occurring after the initial report was made. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | not clearly stated |
| Allocation concealment (selection bias) | Low risk | 'sealed numbered opaque envelopes' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | no mention of blinding of assessors of pain and function |
Skinner 1989.
| Methods | Randomisation by: day of week unclear due to reporting of results in percentages. | |
| Participants | One hospital, Kent, UK. From December 1984 to December 1986 271 patients Characteristics of participants: Mean age: 79.7 years Male: 27 (10%) Loss to follow‐up: not clear. Inclusions: displaced subcapital femoral neck fracture (Garden III and IV, Aged 65 and over, patients with compromised mental state included Exclusions: old fractures, pathological fractures, doubt regarding grading of fracture, rheumatoid arthritis | |
| Interventions | 1. Reduction and fixation with Richard's compression screw plate versus: 2. Uncemented Austin Moore unipolar hemiarthroplasty (posterolateral approach) versus 3.Total hip replacement, cemented Howse II (posterolateral approach) | |
| Outcomes | Follow‐up for 13 years OUTCOMES COLLECTED BY TRIAL (a) Operative details: none (b) Complications related to type of operation: For internal fixation: non‐union, failure of fixation, femoral head collapse or avascular necrosis For replacement arthroplasty: acetabular erosion, loosening, heterotopic ossification, dislocation For both methods: revision rate, deep infection (c) Postoperative complications: Pulmonary embolism Myocardial infarction perioperative death Peroneal nerve palsy Iatrogenic femoral fracture (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 2 months, 1 and 13 years. 13 year survival analysis Pain and mobility (Sikorski and Barrington) Functional results by questionnaire Harris hip score at 13 years (g) Economic cost: none | |
| Notes | 290 patients randomised; 19 patients excluded after randomisation (patients not traceable, missing medical records, wrong randomisation or patients unfit to be assessed) 1 year results published in Injury 1989 for 278 patients. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 'randomly allocated according to one of the following three methods of treatment according to the day of the week on which they were admitted' |
| Allocation concealment (selection bias) | High risk | 'randomly allocated according to one of the following three methods of treatment according to the day of the week on which they were admitted' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
Soreide 1979.
| Methods | Randomisation by: date of birth. | |
| Participants | One hospital, Bergen, Norway. From 1 October 1974 to 30 September 1976 104 patients Characteristics of participants: Mean age: fixation 77.9 , arthroplasty 78.3 years. Male: 21 (20%) Loss to follow‐up: 7 (6.7%) Inclusions: acute femoral neck fracture (Garden II‐IV), aged over 67 Exclusions: by implication pathological fractures, metastatic carcinoma | |
| Interventions | ‐Reduction and fixation with von Bahr screws versus ‐Bipolar hemiarthroplasty, Christiansen | |
| Outcomes | Follow‐up for 12 months Mean: fixation 14.7 months, arthroplasty 14.5 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: Length of surgery Transfusion (b) Complications related to type of operation: For internal fixation: mechanical failure, necrosis of femoral head For replacement arthroplasty: postoperative luxation, delerin luxation For both methods: re‐operation, superficial infection, haematoma (c) Postoperative complications: Deep vein thrombosis and Pulmonary embolism combined Cardiopulmonary Neurological Drug exanthema Urinary retention (d) Postoperative care outcomes Length of necessary hospital stay Days to mobilisation (e) Anatomical restoration: Range of movement (f) Final outcome measures: Mortality at 1, 6, 12 months Walking ability and aids used Stitchfield's hip assessment (pain, movement, capacity for walking) (g) Economic cost: Includes initial stay and stay inclusive of re‐operations | |
| Notes | Fractures include Garden II‐IV. Discrepancy in numbers originally randomised 121 or 123. 17 excluded after randomisation. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | 'randomized into two groups according to their date of birth' |
| Allocation concealment (selection bias) | High risk | 'randomized into two groups according to their date of birth' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
STARS 2006.
| Methods | Randomisation by: computer telephone randomisation service. | |
| Participants | 11 hospitals in Scotland, UK 298 patients Characteristics of participants: Mean age: 75 years Male: 66 (22%) Loss to follow‐up: 2 (0.7%) Inclusions: mobile, mental test score equal to or more than 7/10, aged 60 and above, no serious concomitant disease, displaced intracapsular fracture Exclusions: those not satisfying the above criteria | |
| Interventions | 1. Reduction and fixation with cancellous screws or sliding hip screw versus: 2. Cemented bipolar hemiarthroplasty versus 3. Cemented total hip replacement (surgical approach for arthroplasty was that preferred by the surgeon) | |
| Outcomes | Follow‐up for 24 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: length of surgery in minutes, number transfused (b) Complications related to type of operation: For internal fixation: fixation failure, early redisplacement, non‐union, avascular necrosis For replacement arthroplasty: dislocation Re‐operations Wound healing: superficial infection, deep sepsis (c) Postoperative complications: Deep vein thrombosis Pulmonary embolism Cerebrovascular accident Septicaemia Other medical complications (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 4, 12, 24 months Pain at 4, 12, 24 months Walking score at 4, 12, 24 months Function score at 4, 12, 24 months EQ5D score at 4, 12, 24 months (g) Economic cost: estimated cost for the three trial procedures | |
| Notes | Additional information supplied by trialists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 'centralized fully automated computer‐based telephone service' |
| Allocation concealment (selection bias) | Low risk | 'centralized fully automated computer‐based telephone service' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
Svenningsen 1985.
| Methods | Randomisation by: method not stated. | |
| Participants | One hospital, Trondheim, Norway. From October 1977 to January 1980 169 patients. Characteristics of participants: Mean age in each group 79 both fixations 83 arthroplasty (range 70 to 93) Male: 42 (24.9%) Loss to follow‐up: 7 (4.1%) Inclusions: displaced femoral neck fracture (Garden III‐IV), aged over 70 Exclusions: not reported | |
| Interventions | 1. Reduction and fixation with compression screw versus 2. McLaughlin nail plate versus 3. Bipolar hemiarthroplasty, Christiansen (lateral approach) | |
| Outcomes | Follow‐up for 36 months. OUTCOMES COLLECTED BY TRIAL (a) Operative details: Duration of operation Number of blood transfusions (b) Complications related to type of operation: For both methods: re‐operations, superficial infection (c) Postoperative complications: Deep vein thrombosis Pulmonary embolism Pneumonia Cerebrovascular accident (d) Postoperative care outcomes: Mortality at 6, 12, 36 months Bed bound time (e) Anatomical restoration: none (f) Final outcome measures: Clinical results adapted from Love (pain and mobility) (g) Economic cost: none | |
| Notes | Translation obtained for main points of article. Previous publication in Acta Orthop Scand 1984 reports better results in SHS group compared to nail‐plate in undisplaced and displaced fractures. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
Tidermark 2003.
| Methods | Randomisation by: sealed envelopes. | |
| Participants | One hospital, Karolinska Institute at Stockholm Söder Hospital, Sweden. 102 patients. (8 further patients were randomised but excluded: Six in the arthroplasty group were excluded as two patients had aortic valve stenosis, one patient had urinary tract infection, two patients changed their mind, and one had rheumatoid arthritis. For the internal fixation group, one had rheumatoid arthritis and one changed their mind) Characteristics of participants: Mean age: 79/81 years (range 70 to 96) Male: 20 (20%) Loss to follow‐up: 3 (3%) Inclusions: age 70 years and above, short portable mental status questionnaire of more than 2/10, displaced fracture of the femoral neck, not living in an institution, able to walk independently or with aids Exclusions: pathological fractures, fracture more than 24 hours from occurrence, rheumatoid arthritis, osteoarthritis | |
| Interventions | 1. Reduction and fixation with two cannulated screws versus 2. Exeter's modular stem cemented total hip replacement via an anterolateral approach | |
| Outcomes | Follow‐up for 48 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: length of surgery in minutes, operative blood loss, number of patients transfused (b) Complications related to type of operation: For internal fixation: fixation failure, early redisplacement, non‐union, avascular necrosis, fracture around implant For replacement arthroplasty: fracture around implant, dislocation Re‐operations Wound healing: superficial, infection, deep sepsis (c) Postoperative complications: deep vein thrombosis pulmonary embolism pressure sores myocardial infarction (d) Postoperative care outcomes: none (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 4, 12, 24, 48 months Pain at 4, 12, 24, 48 months Activities of daily living score Health related quality of life questionnaire Walking ability (Charnley score) Movement of the hip (Charnley score) Failure to regain mobility (g) Economic cost: none | |
| Notes | Additional information provided by trialists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | 'sealed envelope technique' |
| Allocation concealment (selection bias) | Unclear risk | 'sealed envelope technique' |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
van Dortmont 2000.
| Methods | Randomisation by: method not stated. | |
| Participants | One hospital, Rotterdam, Netherlands. From April 1991 to January 1995 60 patients. Characteristics of participants: Mean age 84 (range 71 to 96) Male: 8 (13.3%) Loss to follow‐up: none reported. Inclusions: displaced intracapsular femoral neck fracture (Garden III‐IV), aged over 70, diagnosis of 'senile dementia' before admission Exclusions: not mentioned | |
| Interventions | 1. Reduction and fixation with 3 AO/ASIF screws versus 2. Unipolar Thompson hemiarthroplasty (cemented, anterior approach) | |
| Outcomes | Follow‐up for 24 months Mean 16.5 months. OUTCOMES COLLECTED BY TRIAL (a) Operative details: Number days admission to surgery Length of surgery Operative blood loss (b) Complications related to type of operation: For internal fixation: adequacy of reduction Early and later secondary displacement, non‐union For both methods: Re‐operations, deep sepsis, superficial infection, haematoma, dehiscence (c) Postoperative complications: none (d) Postoperative care outcomes: (e) Anatomical restoration: none (f) Final outcome measures Mortality at 30 days, 4 and 12 months Ability to walk independently at 4 and 12 months Activities of daily living at 4 months (g) Economic cost: none | |
| Notes | Study specifically for patients with senile dementia Confidence intervals for continuous outcomes supplied by the trialists | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
van Vugt 1993.
| Methods | Randomisation by: method not stated. | |
| Participants | One hospital, Leyenburg, The Hague, Netherlands. From 1 October 1985 to 1 November 1987 43 patients Characteristics of participants: Mean age: Fixation 75.3, arthroplasty 76 (range 71 to 80) Male: 18 (42%) Loss to follow‐up: 3 (7%) Inclusions: intracapsular fracture (Garden III‐IV), aged 71 to 80, good degree of independence according to Broos Exclusions: none stated | |
| Interventions | 1. Reduction and fixation with dynamic hip screw versus 2. Bipolar hemiarthroplasty, Stanmore variocup (anterolateral approach) | |
| Outcomes | Follow‐up for 36 months OUTCOMES COLLECTED BY TRIAL (a) Operative details: Preoperative delay Operation time Perioperative blood loss (b) Complications related to type of operation: For internal fixation: delayed or non‐union, femoral head necrosis For replacement arthroplasty: loosening of prosthetic stem, acetabular protrusion, periarticular calcifications For both methods: Superficial and deep wound infection, haematoma, secondary intervention (c) Postoperative complications: Thromboembolic disease cardiovascular Pulmonary infection cerebrovascular accident psychiatric disease urinary tract infection pressure sore (d) Post‐operative care outcomes: Admission time (e) Anatomical restoration: none (f) Final outcome measures: Mortality at 1, 3, 6, 12, 24, 36 months Clinical effects of secondary intervention, loss of degree of independence, pain, and hip mobility (Shepherd) (g) Economic cost: none | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not stated |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding (performance bias and detection bias) Were the assessors of pain and function at follow‐up blinded to the treatment allocation | High risk | No mention of blinding of assessors of pain and function |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bray 1988 | This study involved 34 patients, aged over 50 years, who were allocated to fixation with Knowles or Neufeld pins or replacement with a cemented bipolar hemiarthroplasty (type not specified). Follow‐up of patients averaged 19 months. Minimal data reported. Patients receiving hemiarthroplasties had statistically significantly longer anaesthetic and surgery time and greater blood loss. For length of hospital stay, average pain grade and average mobility grade there was no statistical difference between the two groups. The trial was excluded due to inadequate randomisation. Patients were allocated according to day of week and surgeon preference. Surgeon A elected on all even nights to use internal fixation, surgeon B on all odd nights to use hemiarthroplasty. In addition to the low numbers recruited five were lost to follow‐up. |
| El‐Abed 2005 | This study was reported as a randomised comparison of 60 patients with an intracapsular fracture treated with a sliding hip screw and 62 patients treated with a hemiarthroplasty. The choice of treatment was by the preference of the attending surgeon on the day of admission. This study was excluded as it was considered as an inappropriate method of randomisation. (Additional information supplied by the trialists.) |
| Hunter 1969 | Retrospective survey of 186 patients treated with internal fixation (Smith Petersen pin or pin and plate) or primary prosthesis (Judet or Moore). The author concluded that there was a lower morbidity and mortality rate following fixation. Excluded as not randomised. |
| Hunter 1974 | Retrospective review of 200 patients treated with internal fixation (Thornton nail‐plate, Ken nail or Knowles pins) or prosthetic replacement (Thompson or Moore) . The author concluded that internal fixation gave lower morbidity, mortality and better results than prosthetic replacement. Excluded as not randomised. |
| Neander 2000 | This was a randomised trial of 100 patients allocated to fixation with Olmed screws or replacement with a cemented BiMetric total hip replacement. Follow‐up was for 48 months. The authors concluded that there was an unacceptably high complication and re‐operation rate in the osteosynthesis group. Patients with total hip arthroplasty had fewer complications and a better clinical outcome after four years. This trial was excluded due to inadequate randomisation procedure. The first 20 patients were randomised with closed envelopes but the last 80 were allocated according to the day of week they were admitted (Monday to Thursday total hip replacement, Friday to Sunday reduction and fixation). The 17 year follow‐up of the trial was registered in 2011. |
| Parker 1992 | This was a comparative study of 200 patients, 94 treated by internal fixation with two Garden screws and 104 with a hemiarthroplasty. Treatment was determined by the preference of the on call consultant, with some using internal fixation and the others arthroplasty. Results showed no significant difference in mortality. Internal fixation had a shorter hospital stay and a higher re‐admission and re‐operation rate. The study was excluded as it was not a randomised study. |
| Pathi 1989 | This paper was described in the text as a ‘randomized trial of surgical treatment’. Of the 45 included patients, 10 patients were subsequently excluded because of loss to follow‐up. For the remaining 35 patients, 5 were treated with internal fixation with Smith‐Peterson nailing, 10 by internal fixation with Garden screws, 7 with a Thompson hemiarthroplasty and 13 with an Austin Moore hemiarthroplasty. There was limited description of patient characteristics, treatment methods and trial methodology. The only outcomes reported clearly were wound sepsis requiring antibiotics for two patients in the fixation group and five in the arthroplasty group. Nine cases of failure of surgical treatment were reported in the fixation group but it was unclear what constituted failure of treatment. Five wound haematomas and transient sciatic nerve paralysis were reported in the arthroplasty group. Re‐operations were not reported. Regain of mobility was reported at one year but the numbers were unclear. The study was excluded because of the inadequate trial methodology and reporting of the results. |
| Riley 1978 | This study was only reported as an abstract. The study involved 151 patients allocated to Garden cross screw fixation or Austin Moore or Thompson prostheses. The author considered that prosthetic replacement gave significantly better results. The study was excluded as it provided no adequate data. |
| Rodriguez 1987 | This was a comparative study of 301 patients following fixation with 3 AO screws or replacement with a cemented Thompson hemiarthroplasty. The authors reported a lower incidence of immediate postoperative mortality and infection in the fixation group. Excluded as not randomised. |
| Shafee 2007 | This was described in the abstract of the paper as a prospective study of 50 patients who were treated with either an Austin Moore hemiarthroplasty or internal fixation with a sliding hip screws, Moor’s pins or cancellous screws. The full text of the article was not obtainable. The study was excluded because of lack of information and it was unlikely that it was a randomised trial. |
| Sikorski 1981 | This was a randomised study of 218 patients. Patients were allocated to three arms ‐ fixation with Garden screws, a cemented Thompson using an anterior approach or to a cemented Thompson using a posterior approach. Patients in the fixation arm whose fractures were irreducible in theatre were then randomised to an anterior or posterior Thompson. These were then analysed as a fourth group with no details of which surgical approach they received. Interpreting results was confusing. Follow‐up of patients was for 24 months or until revision. Operative mortality in the irreducible group was reported as unacceptable. The authors concluded that the anterior hemiarthroplasty was the safest treatment . This study was excluded due to its poor methodological quality. The comparison between anterior and posterior approach is being considered in a separate Cochrane review. |
| Stewart 1984 | Retrospective study comparing internal fixation with Pugh's nail and plate with a Thompson hemiarthroplasty in 100 patients. The authors found results comparable at one year but failure rate was higher following internal fixation. Excluded because the study was not randomised. |
Differences between protocol and review
Risk of bias assessment was carried out on three items: sequence generation, allocation concealment and blinding.
Contributions of authors
Martyn Parker initiated and designed the review, read all the studies, extracted data and checked all text and results. For this and first update of the review, Kurinchiselvum Gurusamy read all the new studies, extracted data and checked the data. Kurinchiselvum Gurusamy also checked the text and presentation of the results. Martyn Parker is the guarantor of this review.
Sources of support
Internal sources
Peterborough and Stamford Hospitals NHS Trust, UK.
External sources
No sources of support supplied
Declarations of interest
Martyn Parker has received and may continue to receive financial payment from manufacturing companies of orthopaedic implants for attending meeting organised by these companies and for advising on the design and use of hip fracture implants. Kurinchi Gurusamy has no connection with any manufacturing company. Martyn Parker was the lead investigator in one of the included trials, assessment of eligibility of this trial and the subsequent quality assessment was done independently by the other review author.
New search for studies and content updated (no change to conclusions)
References
References to studies included in this review
Blomfeldt 2005 {published data only}
- Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. Journal of Bone and Joint Surgery ‐ British Volume 2005;87(4):523‐9. [DOI] [PubMed] [Google Scholar]
- Errata in ‐ Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. Journal of Bone & Joint Surgery ‐ British Volume 2005;87(8):1166. [DOI] [PubMed] [Google Scholar]
- Tidermark J, Blomfeldt R, Ponzer S, Tornkvist H. Internal fixation versus hemiarthroplasty for displaced femoral neck fractures in elderly patients with severe cognitive impairment: a randomized controlled trial [Abstract]. Orthopaedic Trauma Association Annual Meeting; 2004 Oct 8‐10; Hollywood, Florida. 2004. http://www.hwbf.org/ota/am/ota04/otapa/OTA041056.htm (accessed 24 Jan 2004).
Davison 2001 {published data only}
- Calder SJ, Anderson GH, Gregg PJ. Bipolar hemiarthroplasty for displaced intracapsular hip fractures: a randomised prospective trial [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1995;77 Suppl 2:214. [PubMed] [Google Scholar]
- Calder SJ, Anderson GH, Harper WM, Gregg PJ. The place of bipolar hemiarthroplasty in displaced intracapsular hip fracture [Abstract]. Journal of Bone and Joint Surgery. British Volume 1995;77 Suppl 1:6. [Google Scholar]
- Calder SJ, Anderson GH, Harper WM, Gregg PJ. The use of bipolar hemi‐arthroplasty in intracapsular hip fracture ‐ a prospective randomised trial [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1995;77 Suppl 1:103. [Google Scholar]
- Calder SJ, Anderson GH, Harper WM, Gregg PJ. The use of the Nottingham Health Profile in a randomised trial of treatment of displaced intracapsular hip fractures [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1994;76 Suppl 2 & 3:150. [Google Scholar]
- Calder SJ, Anderson GH, Harper WM, Jagger C, Gregg PJ. A subjective health indicator for follow‐up. A randomised trial after treatment of displaced intracapsular hip fractures. Journal of Bone and Joint Surgery ‐ British Volume 1995;77(3):494‐6. [PubMed] [Google Scholar]
- Davison J, Harper WM, Gregg PJ. Which treatment for the displaced fractures of the femoral neck? A prospective randomised comparison of three surgical procedures [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1997;79 Suppl 2:243‐4. [Google Scholar]
- Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ. Treatment for displaced intracapsular fracture of the proximal femur: a prospective, randomised trial in patients aged 65 to 79 years. Journal of Bone and Joint Surgery ‐ British Volume 2001;83(2):206‐12. [DOI] [PubMed] [Google Scholar]
- Davison JNS, Harper WM, Gregg PJ. Treatment for displaced intracapsular fracture of the proximal femur. A prospective randomised trial in patients aged from 65 to 79 years [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1999;81 Suppl 2:232. [DOI] [PubMed] [Google Scholar]
Frihagen 2007 {published data only}
- Frihagen F, Nordsletten L, Madsen JE. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 2007;335(7632):1251‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jensen 1984 {published and unpublished data}
- Jensen J. Personal communication September 10 2001.
- Jensen J, Rasmussen TB, Christensen S, Holm‐Moller S, Lauritzen J. Internal fixation or prosthetic replacement in fresh femoral neck fractures [Abstract]. Acta Orthopaedica Scandinavica 1984;55:712. [Google Scholar]
- Jensen J, Rasmussen TB, Christensen S, Holm‐Moller S, Lauritzen J. Internal fixation or prosthetic replacement in fresh femoral neck fractures. A randomized clinical trial using cancellous bone screws (AO‐ASIF) or Austin Moore prosthesis. Unpublished report 1982.
Johansson 2002 {published data only}
- Bachrach‐Lindstrom M, Johansson T, Unosson M, Ek AC, Wahlstrom O. Nutritional status and functional capacity after femoral neck fractures: a prospective randomised one‐year follow‐up study. Aging ‐ Clinical & Experimental Research 2000;12(5):366‐74. [DOI] [PubMed] [Google Scholar]
- Johansson T. Displaced femoral neck fractures; a prospective randomized study of clinical outcome, nutrition and costs [dissertation]. Linkoping: Linkoping University, 2002. [Google Scholar]
- Johansson T, Bachrach‐Lindstrom M, Aspenberg P, Jonsson D, Wahlstrom O. The total costs of a displaced femoral neck fracture: Comparison of internal fixation and total hip replacement ‐ A randomised study of 146 hips. International Orthopaedics 2006;30(1):1‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson T, Bachrach‐Lindstrom M, Jonsson D, Aspenbert P, Wahlstrom O. Displaced femoral neck fractures: replace! sometimes fix. Journal of Bone and Joint Surgery ‐ British Volume 2004;86 Suppl 3:261. [Google Scholar]
- Johansson T, Jacobsson SA, Ivarsson I, Knutsson A, Wahlstrom O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthopaedica Scandinavica 2000;71(6):597‐602. [DOI] [PubMed] [Google Scholar]
- Johansson T, Risto O, Knutsson A. Heterotopic ossification following internal fixation or arthroplasty for displaced femoral neck fractures: A prospective randomized study. International Orthopaedics 2001;25(4):223‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jonsson 1996 {published data only}
- Jonsson B, Sernbo I, Carlsson A, Fredin H, Johnell O. Social function after cervical hip fracture. A comparison of hook‐pins and total hip replacement in 47 patients. Acta Orthopaedica Scandinavica 1996;67(5):431‐4. [DOI] [PubMed] [Google Scholar]
Mouzopoulos 2008 {published data only}
- Mouzopoulos G, Stamatakos M, Arabatzi H, Vasiliadis G, Batanis G, Tsembeli A, et al. The four year functional result after a displaced subcapital hip fracture treated with three different surgical options. International Orthopaedics 2008;32(3):367‐73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Neander 1997 {published data only}
- Neander G, Adolphson P, Sivers K, Dahlborn M, Dalen N. Bone and muscle mass after femoral neck fracture. A controlled quantitative computed tomography study of osteosynthesis versus primary total hip arthroplasty. Archives of Orthopaedic and Trauma Surgery 1997;116(8):470‐4. [DOI] [PubMed] [Google Scholar]
Parker 2002 {published and unpublished data}
- Parker MJ. Internal fixation or arthroplasty for displaced intracapsular fracture in the elderly ‐ a randomised trial [Abstract]. Acta Orthopaedica Scandinavica 1998;69 Suppl 280:31. [DOI] [PubMed] [Google Scholar]
- Parker MJ, Khan RJ, Crawford J, Pryor GA. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly. A randomised trial of 455 patients. Journal of Bone and Joint Surgery ‐ British Volume 2002;84(8):1150‐5. [DOI] [PubMed] [Google Scholar]
- Parker MJ, Khan RJK, Crawford J, Pryor GA. Hemiarthroplasty or internal fixation for displaced intracapsular femoral neck fractures in the elderly: A prospective randomised controlled trial [abstract]. Journal of Bone and Joint Surgery ‐ British Volume 2004;86 (SUPP III):338. [Google Scholar]
- Parker MJ, Pryor G, Gurusamy K. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures: a long‐term follow‐up of a randomised trial. Injury 2010;41(4):370‐3. [DOI] [PubMed] [Google Scholar]
- Parker MJ, Pryor GA. Internal fixation or arthroplasty for displaced cervical hip fractures in the elderly: a randomised controlled trial of 208 patients. Acta Orthopaedica Scandinavica 2000;71(5):440‐6. [DOI] [PubMed] [Google Scholar]
Puolakka 2001 {published data only}
- Puolakka TJS, Laine H‐J, Tarvainen T, Aho H. Thompson hemiarthroplasty is superior to Ullevaal screws in treating displaced femoral neck fractures in patients over 75 years. A prospective randomized study with two‐year follow‐up. Annales Chirurgiae et Gynaecologiae 2001;90(3):225‐8. [PubMed] [Google Scholar]
Roden 2003 {published data only}
- Roden M, Ellene B, Fredin H. Treatment of displaced femoral neck fracture ‐ internal fixation versus bipolar endoprosthesis ‐ a preliminary report of a prospective randomized study [Abstract]. Acta Orthopaedica Scandinavica 1996;67 Suppl 270:33. [Google Scholar]
- Roden M, Schon M, Fredin H. Treatment of displaced femoral neck fractures: a randomised minimum 5‐year follow‐up study of screws and bipolar hemiarthroplasty in 100 patients. Acta Orthopedica Scandinavica 2003;74(1):42‐4. [DOI] [PubMed] [Google Scholar]
Rogmark 2002 {published and unpublished data}
- Leonardsson O, Akesson K, Carlsson A, Rogmark C, Sernbo I. Nail or arthroplasty? 10‐year results of a randomised study of 450 patients. Journal of Bone and Joint Surgery ‐ British Volume 2010;92 (SUPP IV):552. [DOI] [PubMed] [Google Scholar]
- Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long‐term follow‐up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. Journal of Bone and Joint Surgery ‐ British Volume 2010;92(3):406‐12. [DOI] [PubMed] [Google Scholar]
- Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur; functional outcome for 450 patients at two years. Journal of Bone and Joint Surgery ‐ British Volume 2002;84(2):183‐8. [DOI] [PubMed] [Google Scholar]
- Rogmark C, Carlsson A, Johnell O, Sernbo I. Costs of internal fixation and arthroplasty for displaced femoral neck fractures: A randomized study of 68 patients. Acta Orthopaedica Scandinavica 2003;74(3):293‐8. [DOI] [PubMed] [Google Scholar]
- Rogmark C, Carlsson A, Johnell O, Sernbo I, Kreder HJ. Arthroplasty led to fewer failures and more complications than did internal fixation for displaced fractures of the femoral neck. Journal of Bone & Joint Surgery ‐ American Volume 2002;84(11):2108. [DOI] [PubMed] [Google Scholar]
- Rogmark C, Johnell O, Sernbo I. Nail or arthroplasty ‐ a randomised study of displaced, cervical hip fractures [Abstract]. Acta Orthopaedica Scandinavica 1998;69 Suppl:280:30. [Google Scholar]
- Rogmark C, Sernbo I, Johnell O. Nail or arthroplasty: a randomised study of displaced femoral neck fractures: 2 year results [abstract]. American Academy of Orthopaedic Surgeons 68th Annual Meeting; 2001 Feb 27‐Mar 4; San Francisco (CA). http://www.aaos.org/wordhtml/anmt2001/sciprog/052.htm (accessed 23 Mar 2001).
- Roeck N. A prospective, randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur [Letter]. Journal of Bone and Joint Surgery ‐ British Volume 2003;85(3):464‐5. [PubMed] [Google Scholar]
Skinner 1989 {published data only}
- Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of the femur ‐ 13 year results of a prospective randomised study. Injury 2000;31(10):793‐7. [DOI] [PubMed] [Google Scholar]
- Ravikumar KJ, Marsh G, Jairaj P. Internal fixation vs hemiarthroplasty vs total hip replacement for displaced subcapital fractures of the femur‐13 year results of a prospective randomised study. Journal of Bone and Joint Surgery ‐ British Volume 1998;80 Suppl 1:50‐1. [Google Scholar]
- Skinner P, Ellery J, Riley D, Beaumont A. Displaced subcapital fractures of the femur: which operation? [Abstract]. Journal of Bone and Joint Surgery. British Volume 1988;70(4):677. [Google Scholar]
- Skinner P, Riley D, Ellery J, Beaumont A, Coumine R, Shafighian B. Displaced subcapital fractures of the femur: a prospective randomized comparison of internal fixation, hemiarthroplasty and total hip replacement. Injury 1989;20(5):291‐3. [DOI] [PubMed] [Google Scholar]
Soreide 1979 {published data only}
- Raugstad TS, Soreide O, Molster A. Screw fixation versus primary prosthetic replacement in acute displaced femoral neck fractures [Abstract]. Acta Orthopaedica Scandinavica 1978;49:636. [Google Scholar]
- Soreide O, Alho A, Rietti D. Internal fixation versus endoprosthesis in the treatment of femoral neck fractures in the elderly. A prospective analysis of comparative costs and the consumption of hospital resources. Acta Orthopaedica Scandinavica 1980;51:827‐31. [DOI] [PubMed] [Google Scholar]
- Soreide O, Molster A, Raugstad TS. Internal fixation or primary prosthetic replacement for treatment of acute femoral neck fractures in the elderly: A prospective randomized study [Abstract]. Acta Orthopaedica Scandinavica 1979;50:805‐6. [Google Scholar]
- Soreide O, Molster A, Raugstad TS. Internal fixation versus primary prosthetic replacement in acute femoral neck fractures: a prospective, randomized clinical study. British Journal of Surgery 1979;66(1):56‐60. [DOI] [PubMed] [Google Scholar]
- Soreide O, Rietti D, Alho A. Internal fixation versus primary prosthetic replacement in acute femoral neck fractures. Cost effectiveness analysis [Abstract]. Acta Orthopaedica Scandinavica 1979;50:806. [Google Scholar]
STARS 2006 {published data only}
- Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technology Assessment (Winchester, England) 2005;9(41):iii‐iv, ix‐x, 1‐65. [http://www.ncchta.org/execsumm/summ941.htm] [DOI] [PubMed] [Google Scholar]
- Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomised comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty; treatment of displaced intracapsular hip fractures in healthy older people. Journal of Bone and Joint Surgery ‐ American Volume 2006;88(2):249‐60. [DOI] [PubMed] [Google Scholar]
- Keating JF, Masson MA, Forbes JF, Scott NW, Grant A. Randomized trial of reduction and fixation versus bipolar hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures in the fit older patient. Orthopaedic Trauma Association Annual Meeting 2002. http://www.hwbf.org/ota/am/ota02/otapa/OTA02641.htm. (accessed 25 Nov 2002).
Svenningsen 1985 {published data only}
- Svenningsen S, Benum P, Nesse O, Furset OI. Dislocated femoral neck fractures in the elderly. A comparison of 3 methods of treatment [Larhalsbrudd hos eldre‐en sammenligning av tre behandlingsmetoder]. Nordisk Medicin 1985;100:256‐9. [PubMed] [Google Scholar]
- Svenningsen S, Benum P, Nesse O, Furset OI. Femoral neck fractures in the elderly. A comparison of 3 therapeutic methods [Larhalsbrudd hos eldre. En sammenligning av tre behandlingsmetoder]. Tidsskrift for den Norske Laegeforening 1985;105(7):492‐5. [PubMed] [Google Scholar]
Tidermark 2003 {published data only}
- Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. Journal of Bone and Joint Surgery ‐ American Volume 2005;87(8):1680‐8. [DOI] [PubMed] [Google Scholar]
- Kamath S. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly [Comment. Letter]. Journal of Bone and Joint Surgery ‐ British Volume 2004;86(1):148‐9. [PubMed] [Google Scholar]
- Tidermark J. Quality of life after femoral neck fractures. Acta Orthopaedica Scandinavica 2003;74 Suppl 309:1‐42. [PubMed] [Google Scholar]
- Tidermark J, Bergstrom G, Svensson O, Tornkvist H, Ponzer S. Responsiveness of the EuroQol (EQ 5‐D) and the SF‐36 in elderly patients with displaced femoral neck fractures. Quality of Life Research 2003;12(8):1069‐79. [DOI] [PubMed] [Google Scholar]
- Tidermark J, Ponzer S, Svensson O, Soderqvist A. Tornkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. Journal of Bone and Joint Surgery ‐ British Voume 2003;85(3):380‐8. [DOI] [PubMed] [Google Scholar]
- Tidermark J, Ponzer S, Svensson O, Tornkvist. Internal fixation vs. primary total hip arthroplasty for displaced femoral neck fractures: A prospective randomised study [Abstract]. Journal of Orthopaedic Trauma 2000;14(2):134‐5. [Google Scholar]
van Dortmont 2000 {published data only}
- Dortmont LM, Douw CM, Breukelen AM, Laurens DR, Mulder PG, Wereldsma JC, et al. Cannulated screws versus hemiarthroplasty for displaced intracapsular femoral neck fractures in demented patients. Annales Chirurgiae et Gynaecologiae 2000;89(2):132‐7. [PubMed] [Google Scholar]
- Dortmont LMC. Personal communication September 9 2001.
van Vugt 1993 {published data only}
- Vugt AB, Oosterwijk WM, Goris RJ. Osteosynthesis versus endoprosthesis in the treatment of unstable intracapsular hip fractures in the elderly. A randomised clinical trial. Archives of Orthopaedic and Trauma Surgery 1993;113(1):39‐45. [DOI] [PubMed] [Google Scholar]
- Vugt AB. Oosterwijk WM. Goris RJ. Predictive value of early scintimetry in intracapsular hip fractures. A prospective study with regard to femoral head necrosis, delayed union and non‐union. Archives of Orthopaedic & Trauma Surgery 1993;113(1):33‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bray 1988 {published data only}
- Bray TJ, Smith Hoefer E, Hooper A, Timmerman L. The displaced femoral neck fracture. Internal fixation versus bipolar endoprosthesis. Results of a prospective, randomized comparison. Clinical Orthopaedics and Related Research 1988;(230):127‐40. [PubMed] [Google Scholar]
- Kirschenbaum IH. The displaced femoral neck fracture: internal fixation versus bipolar endoprosthesis. Results of a prospective, randomized comparison [letter]. Clinical Orthopaedics and Related Research 1989;(240):311‐2. [PubMed] [Google Scholar]
El‐Abed 2005 {published data only}
- El‐Abed K, McGuinness A, Brunner J, Dallovedova P, O'Connor P, Kennedy JG. Comparison of outcomes following uncemented hemiarthroplasty and dynamic hip screw in the treatment of displaced subcapital hip fractures in patients aged greater than 70 years. Acta Orthopaedica Belgica 2005;71(1):48‐54. [PubMed] [Google Scholar]
Hunter 1969 {published data only}
- Hunter G A. A comparison of the use of internal fixation and prosthetic replacement for fresh fractures of the neck of the femur. British Journal of Surgery 1969;56(3):229‐32. [DOI] [PubMed] [Google Scholar]
Hunter 1974 {published data only}
- Hunter GA. A further comparison of the use of internal fixation and prosthetic replacement for fresh fractures of the neck of the femur. British Journal of Surgery 1974;61(5):382‐4. [DOI] [PubMed] [Google Scholar]
Neander 2000 {published and unpublished data}
- Neander G. Reduction and fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures. Results after four years of a prospective randomised study in 100 patients. Displaced femoral neck fractures. Studies on osteosynthesis and total hip arthroplasty. Stockholm: Division of Orthopaedics, Karolinska Institutet, Danderyds Hospital, 2000:1‐21. [ISBN 91 ‐628‐4167 ‐X] [Google Scholar]
- Sköldenberg O. Total hip arthroplasty compared to internal fixation for displaced intracapsular fractures of the femoral neck. ClinicalTrials.gov register. http://clinicaltrials.gov/show/NCT01344772 (accessed 28/08/11) 2011. [NCT01344772]
Parker 1992 {published data only}
- Parker MJ. Internal fixation or arthroplasty for displaced subcapital fractures in the elderly?. Injury 1992;23(8):521‐4. [DOI] [PubMed] [Google Scholar]
Pathi 1989 {published data only}
- Pathi KM, Murthy BS. Hemiarthroplasty versus internal fixation for displaced sub‐capital fracture neck femur. Indian Journal of Orthopedics 1989;23(2):149‐51. [Google Scholar]
Riley 1978 {published data only}
- Riley TBH. Knobs or screws? ‐ a prospective trial of prosthetic replacement against internal fixation of subcapital fractures [Abstract]. Journal of Bone and Joint Surgery ‐ British Volume 1978;60(1):136. [Google Scholar]
Rodriguez 1987 {published data only}
- Rodriguez J, Herrara A, Canales V, Serrano S. Epidemiologic factors, morbidity and mortality after femoral neck fractures in the elderly. A comparative study: internal fixation vs. hemiarthroplasty. Acta Orthopaedica Belgica 1987;53(4):472‐9. [PubMed] [Google Scholar]
Shafee 2007 {published data only}
- Shafee M, Tariq MA, Chisti MK. Intracapsular fracture neck of femur. Medical Forum Monthly 2007;18(3):6‐10. [Google Scholar]
Sikorski 1981 {published data only}
- Sikorski JM, Barrington R. Internal fixation versus hemiarthroplasty for the displaced subcapital fracture of the femur. Journal of Bone and Joint Surgery ‐ British Volume 1981;63(3):357‐61. [DOI] [PubMed] [Google Scholar]
Stewart 1984 {published data only}
- Stewart HD. Pugh's nail fixation versus Thompson's prosthesis for displaced subcapital fractures of the femur. Injury 1984;15(4):227‐31. [DOI] [PubMed] [Google Scholar]
Additional references
Bhandari 2003
- Bhandari M, Devereaux PJ, Swiontkowski MF, Tornetta P 3rd, Obremskey W, Koval KJ, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta‐analysis. Journal of Bone and Joint Surgery ‐ American Volume 2003;85(9):1673‐81. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lefebvre 2009
- Lefebvre C, Manheimer E, Glanville J. 6.4.11 Search filters. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.2 (updated September 2009). The Cochrane Collaboration, 2009. Available from www.cochrane‐handbook.org.
Lu‐Yao 1994
- Lu‐Yao GL, Keller RB, Littenberg B, Wennberg JE. Outcomes after displaced fractures of the femoral neck. A meta‐analysis of one hundred and six published reports. Journal of Bone and Joint Surgery ‐ American Volume 1994;76(1):15‐25. [DOI] [PubMed] [Google Scholar]
Parker 2001
- Parker MJ, Stockton G, Gurusamy KS. Internal fixation implants for intracapsular proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 2001, Issue 4. [DOI: 10.1002/14651858.CD001467] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2010
- Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 2010, Issue 6. [DOI: 10.1002/14651858.CD001706.pub4] [DOI] [PubMed] [Google Scholar]
Rogmark 2006
- Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta‐analysis of 14 randomized studies with 2,289 patients. Acta Orthopaedica 2006;77(3):359‐67. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Masson 2002
- Masson M, Parker MJ, Fleischer S. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 2003, Issue 2. [DOI: 10.1002/14651858.CD001708] [DOI] [PubMed] [Google Scholar]
Parker 2006
- Parker MJ, Gurusamy KS. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD001708.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


