Abstract
SIGNIFICANCE
The use of antiobesity drugs is becoming more widespread, and the resulting adverse effects are also increasing. Visual impairments caused by weight-loss pills need a timely and accurate diagnosis and treatment. Prompt diagnosis and treatment can achieve a satisfactory prognosis.
PURPOSE
This report describes a case of a significant decline in bilateral visual acuity caused by taking diet pills and explores the possible pathogenesis.
CASE REPORT
A 32-year-old Chinese woman showed shallow anterior chambers, and intraocular pressure (IOP) was 38 mmHg bilaterally after taking Korean prescription diet pills for 6 days. The best-corrected visual acuity of both eyes was 0.03. The ultrasound biomicroscopy showed complete ciliary body detachment accompanied with angle closure. The central anterior chamber depths were 1.70 mm in the right eye and 1.61 mm in the left eye. The patient was diagnosed with ciliary body detachment with secondary elevated IOP. The patient was treated with pilocarpine, carteolol hydrochloride, brinzolamide, mannitol, and dexamethasone sodium phosphate. The patient had rewarding prognosis after treatment with discontinuation of diet pills, control of IOP, and glucocorticoids.
CONCLUSIONS
Extensive publicity and education are needed to ensure that consumers do not abuse diet pills; meanwhile, a timely diagnosis and withdrawal are crucial for a desirable prognosis. Clinicians need to consider the possibility of drug-secondary ocular diseases.
Obesity affects more than half a billion people worldwide, and economic development is one of the causes of its increasing prevalence in developing countries. It is difficult to achieve lasting weight loss by adjusting lifestyle and behavior. Therefore, the use of antiobesity drugs is becoming more widespread.1,2 The purposes of this study were to report a case of a significant decline in bilateral visual acuity caused by taking diet pills and to explore the possible pathogenesis. No identifying health information is included in this case report.
CASE REPORT
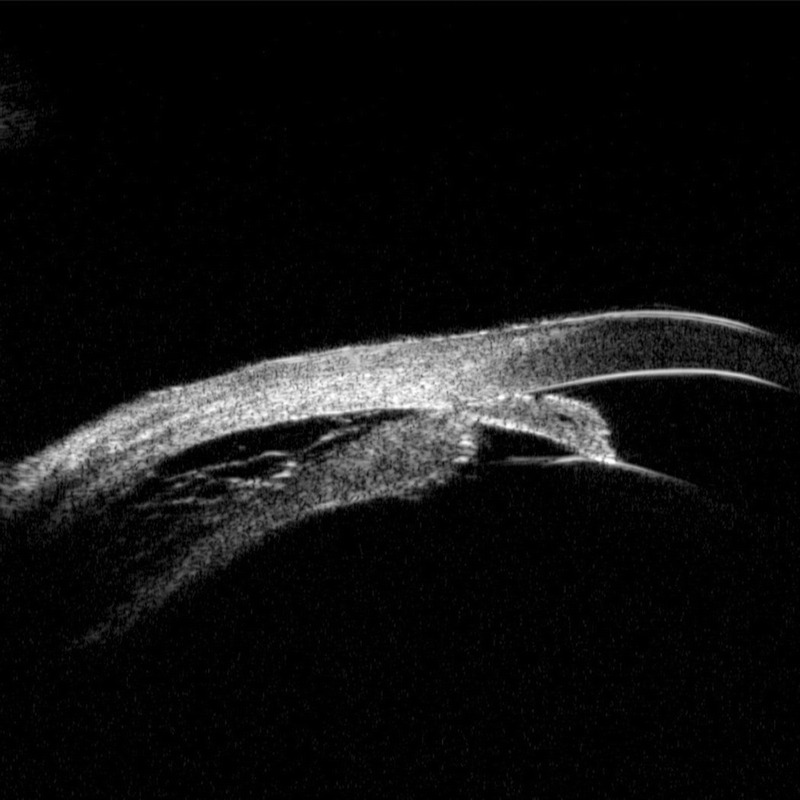
A 32-year-old Chinese woman came to our hospital presenting with sudden binocular vision loss for 3 days (Fig. 1). She had been taking diet pills (Korean), which contains acetaminophen (200 mg), psilocybin (25 mg), and chlorothiazide (237.5 mg), once a day for 6 days. She had no history of systemic disease, ocular disease, or myopia, and she denied taking any other drugs. An ophthalmologic examination showed that the best-corrected visual acuity was 0.03 for both eyes. Intraocular pressure (IOP) values were 38 mmHg in the right eye and 38 mmHg in the left eye. Slit-lamp examination revealed only shallow anterior chambers bilaterally (Figs. 2A, B). The papillary reflex of both eyes was normal. No obvious abnormalities were found in the fundus (Fig. 3). Ultrasound biomicroscopy showed complete ciliary body detachment accompanied by angle closure (Figs. 4A, B). The central anterior chamber depths were 1.70 mm in the right eye and 1.61 mm in the left eye. Laboratory examinations for syphilis, HIV, and hepatitis virus were all negative. The patient was diagnosed with ciliary body detachment with secondary elevated IOP. The patient was treated with pilocarpine eye drops four times, and carteolol hydrochloride eye drops and brinzolamide eye drops twice daily oculus uterque. Mannitol (250 mL) and dexamethasone sodium phosphate (5 mg) were given by intravenous injection once daily. On the third day, the pilocarpine, carteolol hydrochloride, brinzolamide, and mannitol were withdrawn because the patient's IOP values were 12 mmHg in the right eye and 14 mmHg in the left eye. The patient's binocular visual acuity had recovered to 0.3 in the right eye and 0.5 in the left eye. On the sixth day, the patient's binocular vision had recovered to 1.0. The anterior segment photographs provided in Figs. 2C and D show the anterior chamber increase. The ultrasound biomicroscopy provided in Figs. 4C and D shows that the ciliary body detachment was resolved and the anterior chamber was deepened bilaterally. The anterior chamber depths were 2.82 mm in the right eye (1.12-mm increase) and 3.02 mm in the left eye (1.41 mm deeper than before). A B-ultrasound showed no manifest abnormality in either eye.
FIGURE 1.
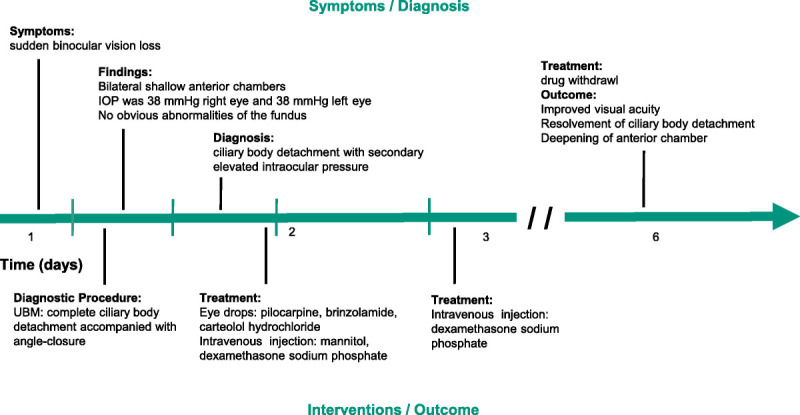
Clinical timeline: a 32-year-old Chinese woman diagnosed with ciliary body detachment with secondary elevated IOP induced by diet pills and treated with the drug after she stopped taking it. UBM = ultrasound biomicroscopy.
FIGURE 2.
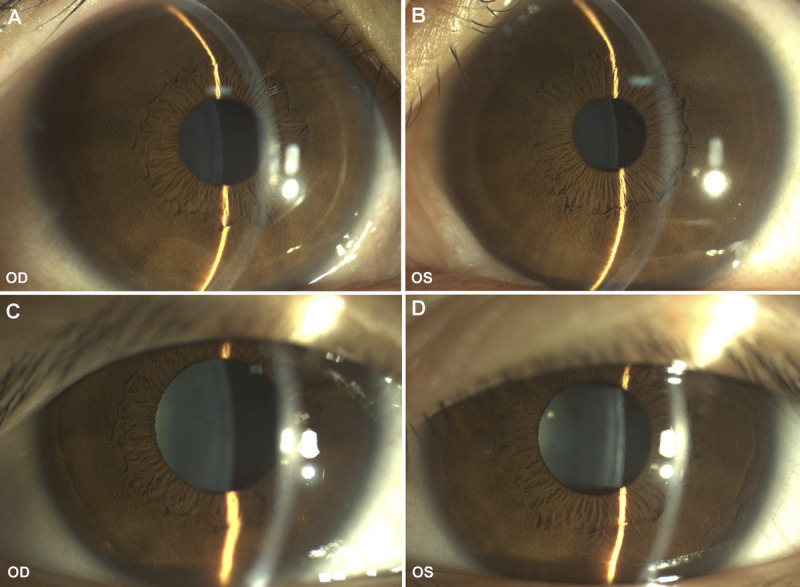
Anterior segment photographs of both eyes before and after treatment. (A) The anterior segment photograph of the right eye before treatment showed shallow peripheral anterior chamber. (B) The anterior segment photograph of the left eye before treatment showed shallow peripheral anterior chamber. (C) The peripheral anterior chamber of the right eye was deepened after treatment. (D) The peripheral anterior chamber of the left eye was deepened after treatment. OD = right eye; OS = left eye.
FIGURE 3.
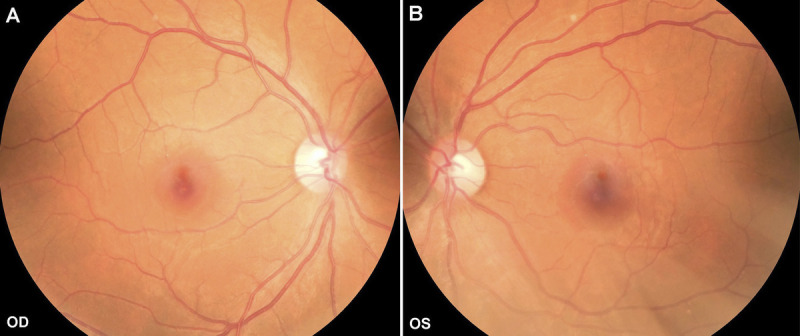
Fundus photographs of both eyes at first visit. (A) The fundus photograph of the right eye showed relatively normal fundus. (B) The fundus photograph of the left eye showed relatively normal fundus. OD = right eye; OS = left eye.
FIGURE 4.
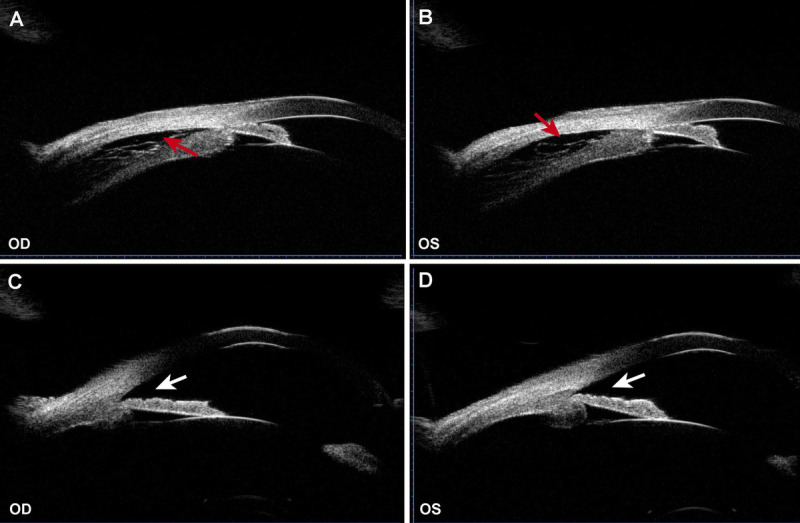
The UBM examination of both eyes before and after treatment. (A) The UBM of the right eye before treatment revealed ciliary body detachment (red arrow) accompanied with angle closure (white arrow). (B) The UBM of the left eye before treatment revealed ciliary body detachment (red arrow) accompanied with angle closure (white arrow). (C) The ciliary body detachment of the right eye was resolved with angle opening (white arrow) after treatment. (D) The ciliary body detachment of the left eye was resolved with angle opening (white arrow) after treatment. OD = right eye; OS = left eye; UBM = ultrasound biomicroscopy.
DISCUSSION
The patient's maximum IOP was 38 mmHg and quickly recovered to normal after treatment. The patient's condition needed to be differentially diagnosed from primary acute angle-closure glaucoma. She had no family history but did have a prominent medicine history, and she was a young woman, an age when primary acute angle-closure glaucoma is rare. Ciliary body detachment was another distinctly important sign, which we believed to be the primary cause of her vision loss.
The currently available drugs approved for weight management by the U.S. Food and Drug Administration are orlistat, lorcaserin, phentermine/topiramate, liraglutide, and naltrexone/bupropion, all of which have different mechanisms. Orlistat, by inhibiting the lipase in the gastrointestinal tract, prevents the decomposition of the fat in food into free fatty acids and thus inhibits the use and absorption of fat.3 Lorcaserin is a highly selective 5-hydroxytryptamine 2C receptor agonist that may influence eating through promoting satiety, reducing the incentive motivational value of food, and improving impulse control4; it may be more effective in obesity associated with emotional eating. Phentermine/topiramate is a fixed-dose, controlled-release, combination product whose mechanisms in weight loss are still under investigation. Phentermine works to suppress appetite by strengthening the neurotransmission of norepinephrine and dopamine.5 The mechanism of action of topiramate in obesity treatment may be through augmenting the activity of γ-aminobutyrate and inhibiting aminomethyl phosphoric acid/kainite excitatory glutamate receptors or carbonic anhydrase.6 Liraglutide is a glucagon-like peptide 1 analog that lowers body weight through decreased calorie intake; it has an anorectic effect through activation of glucagon-like peptide 1 receptors in certain areas in the brain.7 Naltrexone and bupropion have a synergistic effect on food intake. When combined, they act on hypothalamic brain regions to regulate appetite and energy expenditure.8 Among these drugs, only topiramate has been reported to have an association with angle-closure glaucoma.9
On the official Web site for Korean New Drugs, we found that the main ingredient of one of the company's diet pills is paracetamol, which contains acetaminophen (200 mg). The other two ingredients are psilocybin and chlorothiazide, which were detected by a biological company using mass spectrographic analysis. Both acetaminophen and chlorothizide have been reported to be significantly associated with the development of acute angle-closure glaucoma in both eyes.10–12
Psilocybin is one of the most widely used psychedelics in human studies because of its relative safety, moderately long active duration, and good absorption in subjects.13,14 The foremost visual effects of psilocybin are enhanced color saturation, pattern recognition, and visual acuity (at lower doses) and vision distortions and perspective distortion hallucinations (at higher doses).13 No complication of the detachment of the ciliary body caused by psilocybin has ever been reported.
In the latest literature, Zeng et al.12 reported a 39-year-old man who presented with transient myopia with uveal effusion and high IOP induced by excessive use of nonprescription cold and flu medication. They concluded that the acetaminophen in the medication was responsible for the ciliary body detachment by affecting choroidal leakage caused by the cholinergic nerve pathway.12 Because our patient did not take acetaminophen in excess, we speculate that acetaminophen might have had only a secondary effect on ciliary body detachment and not have been a major factor.
Another important ingredient in the diet pills taken by our patient is chlorothiazide, which is also considered to be a significant factor in ciliary body detachment. Chlorothiazide belongs to the class of sulfonamide diuretics, which can stimulate the synthesis of prostaglandins.15 Prostaglandins are recognized to be the mediators of inflammation, which can cause an increase in vasodilation and permeability; we speculate that these processes can eventually lead to ciliary body edema, exudation, and detachment. Ciliochoroidal effusion leads to relaxation of the ciliary zone and the forward rotation of the ciliary body and, in turn, displaces the iris forward to close the anterior chamber angle.10,15,16 Finally, the anterior chamber becomes shallower, and acute angle closure may occur. Although chlorothiazide has been reported to be associated with glaucoma, it has not been reported in weight-loss drugs. The widespread use of diet pills requires vigilance against this adverse effect.
Treatment principles include the discontinuation of diet pills and control of IOP. Glucocorticoid is helpful to relieve the ciliary body edema, which has a satisfactory prognosis.
CONCLUSIONS
Diet pills are widely used and can cause eye adverse effects. Diet pills contain various ingredients, including chlorothiazide, acetaminophen, and topiramate, which have a strong association with ciliary body detachment, which can lead to grave damage to visual acuity. The mechanism of ciliary body detachment may originate from choroidal effusion induced by the medicine through the synthesis of prostaglandins, which can cause an increase in vasodilation and permeability. Extensive publicity and education are needed to ensure that consumers do not abuse diet pills; meanwhile, a timely diagnosis and withdrawal are crucial for a desirable prognosis. Because of the widespread use of diet pills, clinicians need to consider the possibility of drug-secondary ocular diseases.
Footnotes
Funding/Support: None of the authors have reported funding/support.
Conflict of Interest Disclosure: None of the authors have reported a financial conflict of interest.
Author Contributions: Conceptualization: YL, YT; Data Curation: XG, FY; Writing – Original Draft: YL; Writing – Review & Editing: FY.
Contributor Information
Yanzhen Li, Email: lyz18940889319@sina.com.
Yuan Tao, Email: taoyuanchn@163.com.
Xiaofang Gao, Email: 2273760872@qq.com.
REFERENCES
- 1.Fox A, Feng W, Asal V. What Is Driving Global Obesity Trends? Globalization or “Modernization”? Global Health 2019;15:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pilitsi E, Farr OM, Polyzos SA. Pharmacotherapy of Obesity: Available Medications and Drugs under Investigation. Metabolism 2019;92:170–92. [DOI] [PubMed] [Google Scholar]
- 3.Lucas KH, Kaplan-Machlis B. Orlistat—A Novel Weight Loss Therapy. Ann Pharmacother 2001;35:314–28. [DOI] [PubMed] [Google Scholar]
- 4.Higgins GA, Fletcher PJ, Shanahan WR. Lorcaserin: A Review of Its Preclinical and Clinical Pharmacology and Therapeutic Potential. Pharmacol Ther 2020;205:107417. [DOI] [PubMed] [Google Scholar]
- 5.Smith SM, Meyer M, Trinkley KE. Phentermine/Topiramate for the Treatment of Obesity. Ann Pharmacother 2013;47:340–9. [DOI] [PubMed] [Google Scholar]
- 6.Garvey WT. Phentermine and Topiramate Extended-release: A New Treatment for Obesity and Its Role in a Complications-centric Approach to Obesity Medical Management. Expert Opin Drug Saf 2013;12:741–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Secher A Jelsing J Baquero AF, et al. The Arcuate Nucleus Mediates GLP-1 Receptor Agonist Liraglutide-dependent Weight Loss. J Clin Invest 2014;124:4473–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Billes SK, SInnayab P, Cowley MA. Naltrexone/Bupropion for Obesity: An Investigational Combination Pharmacotherapy for Weight Loss. Pharmacol Res 2014;84:1–11. [DOI] [PubMed] [Google Scholar]
- 9.Symes RJ, Etminan M, Mikelberg FS. Risk of Angle-closure Glaucoma with Bupropion and Topiramate. JAMA Ophthalmol 2015;133:1187–9. [DOI] [PubMed] [Google Scholar]
- 10.Murphy RM Bakir B O'Brien C, et al. Drug-induced Bilateral Secondary Angle-closure Glaucoma: A Literature Synthesis. J Glaucoma 2016;25:e99–105. [DOI] [PubMed] [Google Scholar]
- 11.Subak-Sharpe I Low S Nolan W, et al. Pharmacological and Environmental Factors in Primary Angle-closure Glaucoma. Br Med Bull 2010;93:125–43. [DOI] [PubMed] [Google Scholar]
- 12.Zeng R Li YP Chen CL, et al. Non-prescription Cold and Flu Medication–induced Transient Myopia with Uveal Effusion: Case Report. BMC Ophthalmol 2019;19:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Geiger HA, Wurst MG, Daniels RN. Dark Classics in Chemical Neuroscience: Psilocybin. ACS Chem Neurosci 2018;9:2438–47. [DOI] [PubMed] [Google Scholar]
- 14.Meikle SE Liknaitzky P Rossell SL, et al. Psilocybin-assisted Therapy for Depression: How Do We Advance the Field? Aust N Z J Psychiatry 2020;54:225–31. [DOI] [PubMed] [Google Scholar]
- 15.Roh YR, Woo SJ, Park KH. Acute-onset Bilateral Myopia and Ciliochoroidal Effusion Induced by Hydrochlorothiazide. Korean J Ophthalmol 2011;25:214–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rhee DJ, Goldberg MJ, Parrish RK. Bilateral Angle-closure Glaucoma and Ciliary Body Swelling from Topiramate. Arch Ophthalmol 2001;119:1721–3. [PubMed] [Google Scholar]


