Abstract
Introduction:
Conventional implants have great limitations in case of atrophic maxillary and mandibular ridges. Ultimately, patients who have severely atrophied jawbones paradoxically receive little or no treatment, as long as conventional implants are considered the device of first choice. Basal implants were developed with the goal to overcome the limitations of conventional implantology, primarily for atrophied ridges or inadequate bone with the protocol of immediate loading. However, studies regarding the rehabilitation followed by placement of screwable basal implants in atrophied ridges are limited. The purpose of the study was to conduct a prospective evaluation for the feasibility of placing strategic basal implants in clinical practice along with its merits and demerits.
Materials and Methods:
A prospective study was designed to evaluate the protocol of immediate functional loading using the technology of strategic basal implants® for fixed complete arch prostheses and segmental teeth prostheses. A minimal of 10 patients selected in the age group of 20–80 years were restored with strategic basal implants irrespective of the quality and quantity of cancellous/alveolar bone following immediate functional loading protocols.
Results:
About 157 various designs of basal implants were placed in 10 patients, out of which four failed with the survival rate of 97.5% of basal implants.
Discussion:
The new concepts laid by basal implantology eliminate all drawbacks of conventional implantology and should be used as an adjunct to improve the quality of life of our patients. The concept of strategic implantology is innovative but reliable technique for patients in need of permanent rehabilitation.
Keywords: Aggressive periodontitis, diabetes, implants, osseointegration, smoking
INTRODUCTION
Basal implantology also termed bi-cortical implantology, cortical implantology, and strategic implantology. Cortico-Basal Implantology® is a modern innovative implantology system which utilizes the basal cortical portion of the jaw bones for retention of the dental implants, which are less prone to resorption and are infection free. Basal bone is defined as the osseous tissue of the mandible and maxilla other than the alveolar processes. It acts as the basic framework of the maxilla and mandible. The basal bone is always present throughout life; it is very strong and forms the stress-bearing part of our skeleton. Utilizing the basal bone, implantologists can now place implants in regions where traditional implants would not be possible.[1]
Basal implants have unique design and are available in various types. Crestal basal implants, one among the type of basal implants, are placed flapless with no incision required. They engage the second or third cortical plates for which osseointegration is not paramount. The term “osseointegration” is called “osseoadaptation” by basal implantologist, this stems from the fact that the bone with continuous functional loads remodels and adapts over the implant surface.[2]
The present prospective study was conducted in the Department of Oral and Maxillofacial Surgery of College of Dental Sciences and Research Center, Ahmedabad, to evaluate the protocol of immediate functional loading using the technology of strategic basal implants for fixed complete arch prostheses and segment teeth prostheses along with its merits and demerits and to establish a definitive opinion about the feasibility of placing basal implants.
MATERIALS AND METHODS
A prospective study was conducted on a total of 10 patients randomly selected from the age group of 20–80 years, (See Table 1) who were restored with strategic basal implants irrespective of the quality and quantity of cancellous/alveolar bone following immediate functional loading protocols. Approvals of Institute Research Council and Ethical Committees were obtained prior to commencement of the study. The duration of the study was from October 2017 to October 2019.
Table 1.
Patient characteristics
| Observed Parameters | n (%) |
|---|---|
| Number of Patients | 10 |
| Number of implants placed | 157 |
| Number of implants in function | 153 |
| Number of implants Failed | 4 |
| Types of Rehabilitation | |
| Full mouth rehabilitation | 8 |
| Segmental rehabilitation | 2 |
| Gender | |
| Male | 5 |
| Female | 5 |
| Destructive Chronic Periodontitis | |
| Yes | 2 |
| No | 8 |
| Diabetes Mellitus | |
| Yes | 3 |
| No | 7 |
| Smoking and Tobacco Habits | |
| Yes | 4 |
| No | 6 |
A. Inclusion criteria:
Patients presented with partial or full edentulism in the upper or lower jaw
Patients having atrophied ridges [Figure 1]
Patients in whom placement of conventional implants would result in poor prognosis due to various reasons
Patients with failed bone augmentation procedures.
Figure 1.
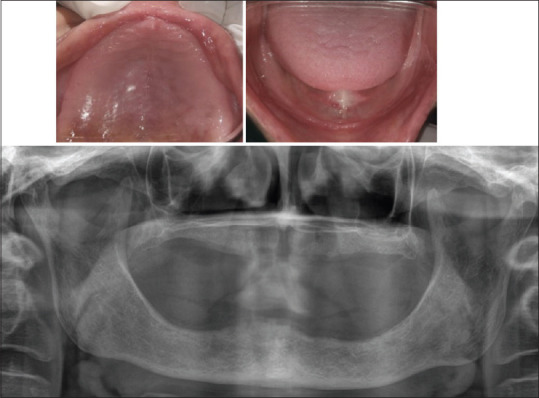
Preoperative orthopantomogram and clinical photograph
B. Exclusion criteria:
Any systemic condition which contradicts any surgical procedure
If suspected that the treatment could affect the patient's health condition like pregnancy
Any patient on IV bisphosphonate therapy
The planned implant area having persisting lesions, such as a tumour, or showed signs of chronic bone diseases which may continue even after implant placement
History of radiotherapy in the head-and-neck region for malignancies, chemotherapy for treatment of malignancy within 1 year of the procedure desired
If the patient's cooperation appeared questionable
If the patient did not give his or her informed consent to participate.
In general, on a patient, if a routine simple extraction can be done, full-mouth rehabilitation with strategic implantology can be routinely done.
The routine preoperative preparations were performed which include orthopantomogram and blood investigations; written and informed consent from the patient and patient's relative for anaesthesia, surgery, and implant placement was obtained. Intraoral periapical radiograph and cone-beam computed tomography were taken only if required. Preoperatively, all the patients were started with antibiotic prophylaxis tablet cefadroxil 500 mg BD 1 day prior to the operative day.
Intraoperative procedures included extraction, curettage, implant placement, and impression making. The procedure of implant placement was performed under local anesthetic solution 2% lignocaine with adrenaline in 1:80,000 dilution by giving infiltration and field block. Nerve blocks were completely avoided during the procedure to judge the proximity to vital anatomical structures and to avoid accidental insertion of implants at critical positions. All the procedures were done mostly flapless unless we have extraction to be done.
Usually, for completely edentulous maxillary and mandibular arches, 8-11 implants and 8 implants were placed in strategic positions, respectively (See Figure 2 and 3). The number of implants was increased based on the density of the bone. In both the jaws, the implants were placed with the primary aim of cortical anchorage at least in the second or third cortical. Even in the presence of profound periodontal involvement or periapical lesion, implants were inserted into fresh extraction sockets after extraction. None of the implants were placed with the help of surgical guides.
Figure 2.
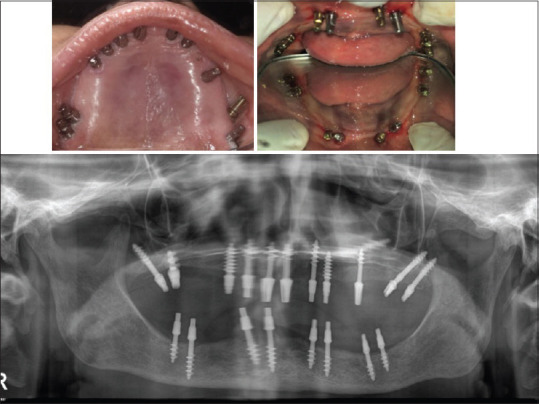
Intraoperative orthopantomogram and clinical photograph
Figure 3.
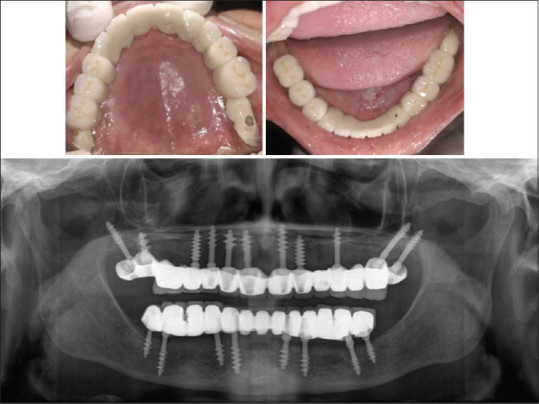
Postoperative orthopantomogram and clinical photograph
For segmental rehabilitation, an adequate number of implants were preferred and placed the same way as in completely edentulous arches. Teeth with poor prognosis were extracted and emphasis was to restore bilateral mastication with an adequate number of implants. Intraoral welding/syncrystallization of implants placed was also done in cases where enough primary stability could not be obtained.
After implant placement, impression was made by additional silicon putty and master cast was readied on the same day after recording jaw relation. Postoperatively, 2 ml dexona was injected intraorally and the patient was prescribed analgesics tablet paracetamol 500 mg + aceclofenac 100 mg BD for 3–5 days. Necessary instructions of diet and oral hygiene were given.
On the next day (2nd day) of implant placement, metal framework try-in made up of Co-Cr metal was taken up. Various adjustments regarding the height, width, and angulation were done on implants using metal cutting bur such that the metal framework snuggly fits over the implants. Teeth selection and shade selection procedure for prosthesis was also performed.
For patients in whom excessive shrinkage was expected due to inflamed tissue, hybrid prosthesis was preferred as interim prosthesis and the patient was explained about the need for replacement of prosthesis later on, whereas ceramic veneered circular bridges were preferred for most cases. On the next day of metal try-in (3rd day), either final prosthesis consisting of metal frame and veneering from either ceramics or acrylic was cemented by using glass-ionomer cement by Fuji GC after final bite adjustment.
All the prostheses given were prepared by following the concept which Dr. S. Ihde and Dr. A. Ihde had outlined. The prosthetic concept included occlusal contact on two premolars and anterior half of the first molar with equal bilateral mastication. No contact was given on anterior teeth and distal to half of the first molar [Figure 3 and 4].
Figure 4.

Facial view preoperative and postoperative
Then, the patient was regularly recalled for follow-up visits after 15 days, 3 months, 6 months, and 1 year and radiological investigation was performed at the end of 1 year.
RESULTS
A total of 10 patients with the need of partial or full-mouth rehabilitation were selected for the study. Eight cases needing full-mouth rehabilitation and two patients needing segmental rehabilitation in maxillary arch were selected for the study with five males and five females. Statistical analysis was performed using statistical software package – Statistical Package for the Social Sciences (SPSS v25). A Chi-square test was performed to compare the significance of survival of implants in respect to various designs, various cortical engaged, and in healed and extraction sockets. Statistical Package for the Social Sciences (SPSS v25)IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.
Criteria for survival and success of implant were as follows:
No pain, no detectable infection
Minimal horizontal mobility was acceptable; however, proper anchorage of the cortices was preferred
No notable bone loss visible on panoramic picture.
Criteria of possible failure were noted as follows:
The existence of discomfort or persistent pain
Vertical mobility of implant
Radiologically observable bone loss apical to the shaft of implant.
There were minimal to no complications following basal implant placement and this was a simple outpatient procedure and the patients were relieved with antibiotics and simple analgesics after the procedure.
All the implants were placed by a single operator to eliminate surgical bias. Over the course of the study, 153 implants out of 157 implants were well taken up with the survival rate of basal implants of 97.5%.
Clinically, none of the implants were tender or showed other signs of peri-implantitis at the end observation period of the study. This result can be attributed to the polished design of basal implants.
Three implants out of 84 implants placed in healed bone failed, whereas only one implant placed in extraction socket failed out of 69 implants placed in extraction sockets suggestive of the fact that basal implants can be placed in healed bone as well as extraction sockets.
Out of 10 patients, four patients were rejected by conventional implantologist and so they were considered in our study as patient demanded fixed rehabilitation, provided they satisfy the inclusion and exclusion criteria. All the patients requesting the treatment were treated following the principle of “intent to treat.”
A total of 157 implants placed in our study included 72 BECES, 59 BECES N, 15 BECES EX, and 10 KOC implants. All designs of basal implants used in our study showed an almost good survival percentage of 98.6%, 98.3%, 93.3%, and 90.9%.
It was observed that if proper anchorage from the cortical was obtained, then basal implants would survive well even in severely resorbed ridges.
In our study, 70 implants were placed immediately into the extraction socket and 87 were placed in the healed bone.
Clinically, 70 implants were placed in extraction sockets even in presence of any periodontal or periapical lesion and only a single implant failed that too due to poor anchorage obtained from the cortical.
Out of 87 implants placed in the healed bone, which obtained support even from the first alveolar cortex, 3 implants failed due to various reasons. Hence, it can be stated that the survival of screwable basal implants anchored in the second or third cortical does not depend on the presence of healed alveolar bone along the vertical shafts of the implants. The result could account for the fact that the prime requisite for success in strategic implantology is anchorage of the second or the third cortical. Our result was in accordance with the study performed by Oleg et al., who stated that the clinical success rate of the immediate functional loading concept with cortically anchored implants or implants providing corticalization of the cancellous bone (BECES/BECES N, KOC, COI) is 100%.[3]
Out of 157 implants, 95 implants were placed in maxilla and 62 implants in the mandible with a survival percentage of 96.8% for maxilla and 98.4% for the mandible. All implants placed in tubero-pterygoid, maxillary sinus floor, palate, and nasal floor survived except one each implant failing in nasal floor and maxillary sinus. Sixty-two implants were placed in mandible anchoring the inter-foramina region and lingual cortex of mandible.
From the result of our study, it can be concluded that palatal bone, tuberopterygoid region, and inter-foramina region provided excellent cortical bone with a 100% survival percentage.
DISCUSSION
The modern basal implant has a sophisticated yet simple design, surgical protocol, and is a prosthetic friendly system. These properties have led several practitioners around the globe to include basal implantology in their practices.[4]
Basal implantology includes the application of the rules of orthopedic surgery and hence can be categorized to be an “oral division of orthopedic surgery.” Basal implantology had been developed on the basis of dental demands and application of orthopedic principles.[5]
According to Wolff's law, bone is stimulated, strengthened, and continually renewed directly by a tooth or an implant. Wolff's Law, developed by the German anatomist and surgeon Julius Wolff in the 19th century, states that bone in a healthy person or animal will adapt to the loads under which it is placed.[6] If loading on a particular bone increases, the bone will remodel itself over time to become stronger to resist that sort of loading.
Iezzi et al. performed a histological study of bone-implant interface and stated that bone response is not disturbed by stresses and strains transmitted at the interface under functional loading. Histological results could be explained by the fact that functional loading appears to stimulate bone apposition. Wolff's law states that there is a direct link between mechanical loading and bone morphology and increased stresses act as a stimulus to new bone formation, while reduced stress tends to produce a bone loss.[7]
The bone with continuous functional loads remodels and adapts over the surface of the implant, the remodeling of bone under functional loads is considered to be the fourth dimension. It should be noted that throughout these phases, the implants are under functional loads and because of which there is a continuous stimulation of the “Bone Multicellular Unit” throughout the life of the implant, this causes reparative osteogenesis leading the peri-implant bone to become dense (which increases throughout the implants life) and to adapt over the surface of the implant, thus the term “Osseoadaptation,” and this is how remodeling plays a key role and is called as the “4th Dimension.”[4]
In a case report, Stefan Ihde and Antonina Ihde evaluated the bone reaction to the polished surface and sandblasted surface in a case and evaluated it over a period of 20 years. They stated that polished vertical implant surfaces on lateral basal implants and a thin diameter at the point of mucosal penetration provide a sustainable environment for a stable (unaltered) bone level even after 20 years. If lateral basal implants with sandblasted shaft are used, crater-like bone loss is observed after a number of years.[8]
The healing of bone, i.e., osteonal remodeling, starts 3 days postoperatively. Hence, within the first 3 days, very stable bone is available. For this reason, it is recommended to equip the implant within a short period with the prosthetic splinting and to leave it in place at a minimum of 6–9 months until remodeling ceases. It should be noticed that the remodeling of the bone is not endangering the stability of implants.[9]
Gaur et al. stated that it is necessary to rigidly splint strategic implants within 3 days as the process of bone remodeling starts. They stated that it takes almost 4–6 months for bone remodeling to complete and thus achieve biological stability from mechanical stability.[10]
In 2016, S. Ihde and A. Ihde proposed the concept of “supporting polygon” to determine the position of occlusal contacts within or outside of polygon drawn up by the load transmitting part of the implants in the second or third corticals.
The aim of the treatment for work on strategic basal implants should be:
A bilateral equal and symmetrical occlusion
A bilateral equal and symmetrical mastication, with contact on first, second premolar, and the mesial half of first molar
A symmetrical function of the muscles, especially tongue
Identical angle functional masticatory de planus (AFMP) angles on both the sides.
The French and Spanish dentist Planas described in the 1980s a simple and reliable method of evaluation of the symmetry of the masticatory function. This method can be used while the patient sits in the chair, i.e., by observing the movement of the mandible to the left and the right, the angle with which the mouth opens during this movement can be detected and is termed AFMP angle.
Disengagement of the group of front teeth in occlusion and mastication
Avoiding anterior or unilateral pattern of chewing and developing lateral pattern of chewing.[11]
Complications
During the course of our study, various intraoperative, immediate postoperative, and postoperative complications were encountered.
Intraoperatively, rupture of palatine vessels while placing pterygoid implants, nasal bleeding and breakage of drill occurred while placing implants anchoring floor of the nose, breakage of drill occurred in once while drilling for pterygoid implants, however, it could be easily retrieved.
Immediately postoperatively, ecchymosis intraorally as well as extraorally could be seen, which disappeared in 1-2 weeks, reduced mouth opening after pterygoid implant placement due to injury to muscle fibers which gradually returned to normal followed by muscle relaxant.
Postoperatively, ceramic chipping off from metal framework and prosthesis loosening due to de-cementation were observed.
Overload osteolysis around a single implant due to high cuspal contact was observed in two patients. Occlusal adjustment was done. Overload osteolysis can be prevented by giving bilateral balanced, group function, mutually protected, and lingualized occlusion.
The key for the long-term survival is proper case selection, atraumatic extraction, achieving primary stability and anchorage from second or third cortical, rigid prosthesis fabrication with occlusion concept outlined by Dr Ihde, achieving equal bilateral mastication and lingualized occlusion, maintaining good oral hygiene, and routine follow-up at regular intervals.
Shahed et al. stated that basal implants may lead to submucosal infection. This may result in infected vertical parts if the implants are submerged below the mucosal level over time, eliminating the necessary gateway for suppuration as the area of penetration is closed with scar tissue. Any inflammation of this type will spread just like a submucosal abscess and is treated in the same way.[12]
CONCLUSION
Within the limits of the study, the following conclusion can be summarized:
The cumulative survival rate of basal implants was 97.5%
As basal implants obtained support from cortical bone, it aids its application in patients with diabetes, smoking, and aggressive periodontitis with a better prognosis
Basal implants survive equally well in the extraction socket. No statistically significant difference was seen in survival when basal implants are placed in healed bone and extraction sockets
There was no statistically significant difference in survival of various designs of basal implants (BECES, BECES N, BECES EX, and KOC)
The survival of individual implant depends equally on fixation of cortical and prosthesis which helps in rigid fixation. Tubero-pterygoid junction, palatal bone, and interforaminal bone provide good cortical anchorage for implant placement
As the patient is given prosthesis with occlusal loading within 72 h, the protocols of strategic basal implantology were easily accepted by patients.
The concept of strategic implantology is an innovative but reliable technique for patients in need of permanent rehabilitation. Basal implants are an excellent alternative to risky bone augmentations and they allow immediate loading under most circumstances. They make dental implant treatments available, safe, and affordable even for smokers and patients with controlled diabetes and chronic destructive periodontitis. Hence, it can be stated that basal implantology provides the operator with the necessary tool to enhance the quality of life for patients in need of fixed rehabilitation. The most important change to be made in our minds is that almost all patients can carry fixed prostheses with satisfactory results. Moreover, the concepts laid by basal implantology eliminate all drawbacks of conventional implantology and should be used as an adjunct to improve the quality of life of our patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Yadav RS, Sangur R, Mahajan T, Rajanikant AV, Singh N, Singh R. An alternative to conventional dental implants: Basal implants. Rama Univ J Dent Sci. 2015;2:22–8. [Google Scholar]
- 2.Gupta A, Madan B, Bakshi M, Garg M. Full mouth rehabilitation with immediate loading basal implants. Int J Prev Clin Dent Res. 2017;4:159–61. [Google Scholar]
- 3.Oleg D, Alexander L, Konstantinovic Vitomir S, Olga S, Damir S, Biljana M. Immediate-functional loading concept with one-piece implants (Beces/Beces N/Kos/Boi) in the mandible and maxilla – A multi-center retrospective clinical study. J Evol Med Dent Sci. 2019;8:306–15. [Google Scholar]
- 4.Gupta AD, Verma A, Dubey T, Thakur S. Basal osseointegrated implants: Classification and review. Int J Contemp Med Res. 2017;4:2329–35. [Google Scholar]
- 5.Ihde S, Ihde A. Immediate Loading. Munich: Internat. Implant Foundation Publ; 2012. [Google Scholar]
- 6.Frost HM. Wolff's Law and bone's structural adaptations to mechanical usage: An overview for clinicians. Angle Orthod. 1994;64:175–88. doi: 10.1043/0003-3219(1994)064<0175:WLABSA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Iezzi G, Pecora G, Scarano A, Perrotti V, Piattelli A. Immediately loaded screw implant retrieved after a 12-year loading period: A histologic and histomorphometric case report. J Osseointegration. 2009;2009:54–9. [Google Scholar]
- 8.Ihde S, Ihde A. Considerations regarding dental implant surfaces, bone reaction and “Peri-implantitis”. Ann Maxillofac Surg. 2018;8:365–8. doi: 10.4103/ams.ams_224_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ihde S, Ihde A. Introduction into the Work with the Strategic Implant Foundation Publishing. 2015 [Google Scholar]
- 10.Gaur V, Doshi A, Ihde S, Fernandes G. Immediate loading of edentulous mandibular arch with screw retained final prosthesis on strategic implants® with single piece multi unit abutment heads: A case report. BAOJ Dent. 2018;4:042. [Google Scholar]
- 11.Ihde S, Ihde A. Cookbook Mastication. Munich: Internat. Implant Foundation; 2015. [Google Scholar]
- 12.Shahed SS, Nagaral SC, Mujawar AM. Basal implants: A breakthrough for atrophic ridges: Review. J Appl Dent Med Sci. 2018;4:53. [Google Scholar]


