Abstract
Background
Accumulating evidence links paternal adiposity in the periconceptional period to offspring health outcomes. DNA methylation has been proposed as a mediating mechanism, but very few studies have explored this possibility in humans.
Methods
In the Pregnancy And Childhood Epigenetics (PACE) consortium, we conducted a meta-analysis of coordinated epigenome-wide association studies (EWAS) of paternal prenatal body mass index (BMI) (with and without adjustment for maternal BMI) in relation to DNA methylation in offspring blood at birth (13 data sets; total n = 4894) and in childhood (6 data sets; total n = 1982).
Results
We found little evidence of an association at either time point: at all CpGs, the false-discovery-rate-adjusted P-values were >0.05. In secondary sex-stratified analyses, we found just four CpGs for which there was robust evidence of an association in female offspring. To compare our findings to those of other studies, we conducted a systematic review, which identified seven studies, including five candidate gene studies showing associations between paternal BMI/obesity and offspring or sperm DNA methylation at imprinted regions. However, in our own study, we found very little evidence of enrichment for imprinted genes.
Conclusion
Our findings do not support the hypothesis that paternal BMI around the time of pregnancy is associated with offspring-blood DNA methylation, even at imprinted regions.
Keywords: Paternal, fathers, body mass index, DNA methylation, epigenetics, DOHaD, pregnancy
Key Messages
Previous small, mostly candidate gene studies have shown associations between paternal pre-pregnancy body mass index (BMI) and offspring-blood DNA methylation.
However, in our large meta-analysis of coordinated epigenome-wide association study results from a total of 19 data sets across two time points, we found little evidence to support these findings, even at imprinted regions.
This does not rule out the possibility of a paternal epigenetic effect in different tissues, at regions not covered by the 450k array, via different mechanisms or in populations with greater extremes of paternal BMI.
More research is warranted to help in understanding the size and nature of contributions of paternal adiposity to offspring epigenetics and health outcomes.
Introduction
Accumulating evidence links paternal exposures in the periconceptional period to offspring health outcomes.1–3 Results from animal studies support a causal role for ‘paternal effects’4 that are independent of maternal effects.2 Whereas prenatal maternal effects are most commonly postulated to occur via fetal intrauterine exposure, the suggested biological mechanisms underlying paternal effects3,5 include germline de novo genetic mutations6 or epigenetic changes,7 or alterations in the components or properties of semen.8
Epigenetic mechanisms that have been studied in relation to paternal exposures include DNA methylation, histone modification and microRNA expression,7 all of which can induce mitotically heritable alterations in gene expression without changes to the DNA sequence. At most loci, patterns of DNA methylation are erased shortly after fertilization to create totipotent cells. However, some loci (most notably imprinted regions) can evade erasure, thus raising the possibility of intergenerational paternal epigenetic inheritance.9,10
A large proportion of the research on paternal effects has explored dietary and metabolic exposures in relation to offspring metabolism and adiposity, sometimes including exploration of the potential mediating role of DNA methylation in sperm and offspring. Animal models of high-fat-diet-induced paternal obesity and diabetes have found associations with impaired offspring development11 and offspring metabolic phenotypes and DNA methylation in pancreatic islets.12 In humans, a recent systematic review13 found conflicting evidence on the association between paternal body mass index (BMI) and offspring birthweight, and some evidence of an association with greater offspring BMI, weight or body fat mass in childhood. A small number of studies have also found links between paternal BMI and sperm or offspring neonatal blood DNA methylation, but these have been based on candidate genes and/or had very limited sample sizes.14–20
In the Pregnancy And Childhood Epigenetics (PACE) consortium,21 we conducted meta-analyses of coordinated epigenome-wide association studies (EWAS) exploring prenatal paternal BMI in relation to genome-wide DNA methylation at birth (cord blood; 13 independent data sets across 10 cohorts) and in childhood (peripheral blood; 6 data sets across 9 cohorts). A major challenge in studies of paternal effects is the correlation between paternal and maternal phenotypes and exposures, which could be due to shared environments and/or assortative mating.22 Several studies (e.g. 23–25) including a large PACE-consortium study,26 have shown that maternal BMI is associated with a variation in offspring DNA methylation. To help disentangle any paternal effect from a maternal effect, we adjusted paternal associations for maternal BMI. We also conducted additional analyses with maternal BMI as the main exposure (unadjusted and adjusted for paternal BMI) and compared results to our primary analyses in which paternal BMI was the main exposure. Finally, we systematically reviewed the literature on associations between paternal BMI and offspring or sperm DNA methylation in humans and assessed whether our results were enriched for imprinted loci and other regions identified by previous studies.
Methods
Meta-analysis of EWASs
Participating cohorts
The EWAS meta-analysis at birth included data from 13 independent data sets from 10 cohorts in PACE (n = 4894): the Avon Longitudinal Study of Parents and Children (ALSPAC)27–29; two independent data sets from Born in Bradford (BiB)30; the Center for the Health Assessment of Mothers and Children of Salinas (CHAMACOS)31; the Generation R Study (GENR)32,33; the Genetics of Overweight Young Adults34 (GOYA; nested within the Danish National Birth Cohort); INfancia y Medio Ambiente (INMA)35; three independent data sets from the Norwegian Mother and Child Cohort Study (MoBa1, MoBa2, MoBa3)36,37; Project Viva (Viva)38; and two independent data sets generated as part of the EXPOsOMICS39 project Piccolipiù40 and RHEA.41
The EWAS meta-analysis at childhood included data from six data sets from nine PACE cohorts (n = 1982): ALSPAC, CHAMACOS, Generation R, INMA, Project Viva and the Human Early Life Exposome study (HELIX).42 HELIX is a sample containing childhood methylation data pooled from several other cohorts (BIB, EDEN,43 INMA, MoBa and RHEA). We conducted a sensitivity analysis excluding HELIX, because of concerns about potential sample overlap (albeit at a different time point) with the INMA sample.
Cohorts are summarized in Table 1 and more detailed methods for each cohort are provided in Supplementary Information File 1, available as Supplementary data at IJE online.
Table 1.
A summary of key information for participating cohorts
| Cohort | Country and ancestry | Methylation time point and array |
Paternal BMI data source |
Maternal BMI data source |
||||
|---|---|---|---|---|---|---|---|---|
| Birth | Childhood | Measured | Self-reported* | Reported by mother* | Measured* | Self-reported* | ||
| ALSPAC | UK; Northern European | 450k | 450k | ✗ | ✓ (first trimester) | ✗ | ✗ | ✓ (pre-pregnancy) |
| BIB (Asian) | UK; Pakistani | EPIC | ✗ | ✗ | ✓ (first trimester) | ✗ | ✓ (first trimester) | |
| BIB (European) | UK; Northern European | EPIC | ✗ | ✗ | ✓ (first trimester) | ✗ | ✓ (first trimester) | |
| CHAMACOS | USA; Mexican American | 450k | 450k | ✓ (around delivery) | ✗ | ✗ | Height only (first trimester) | Weight only (pre-pregnancy) |
| Generation R | The Netherlands; Northern European | 450k | 450k | ✓ (first trimester) | ✗ | ✗ | ✗ | ✓ (pre-pregnancy) |
| GOYA | Denmark; Northern European | 450k | ✗ | ✗ | ✗ | ✓ (18 months after delivery) | ✗ | ✓ (pre-pregnancy) |
| HELIX (BIB, EDEN, INMA, MoBa, RHEA) | Mixed (UK, France, Spain, Lithuania, Norway, Greece); European | ✗ | 450k | ✗ | BIB, MoBa (first trimester), EDEN (third trimester) | INMA, RHEA (first trimester) | BIB (BMI, first trimester) INMA, RHEA (height only, first trimester), EDEN (height only, second trimester) | EDEN (weight only, pre-pregnancy), INMA, RHEA (weight only, first trimester), MoBa (BMI, first trimester) |
| INMA | Spain; Southern European | 450k | 450k | ✗ | ✗ | ✓ (first trimester) | Height (first trimester) | Weight (first trimester) |
| MoBa 1 | Norway; Northern European | 450k | ✗ | ✗ | ✗ | ✓(first trimester) | ✗ | ✓ (first trimester) |
| MoBa 2 | Norway; Northern European | 450k | ✗ | ✗ | ✗ | ✓ (first trimester) | ✗ | ✓ (first trimester) |
| MoBa 3 | Norway; Northern European | 450k | ✗ | ✗ | ✗ | ✓ (first trimester) | ✗ | ✓ (first trimester) |
| Piccolipiù | Italy; Southern European | 450k | ✗ | ✗ | ✗ | ✓ (around delivery) | ✗ | ✓ (around delivery) |
| Project Viva | USA; European | 450k | 450k | ✗ | ✗ | ✓ (first trimester) | ✗ | ✓ (pre-pregnancy) |
| RHEA | Greece (Crete); Southern European | 450k | ✗ | ✗ | ✗ | ✓ (first trimester) | Height (first trimester) | Weight (first trimester) |
Time points (i.e. pre-pregnancy, first trimester, etc.) refer to the period that participants were asked to report on rather than when the questionnaire was completed.
BMI, body mass index; 450k, Illumina 450k array; EPIC, Illumina EPIC array; cohort abbreviations described in the main text.
Measurement of paternal and maternal BMIs
Paternal and maternal BMIs were calculated using either self-reported or measured height and weight of participants (Table 1). For paternal BMI, cohorts selected a time point as close to the time of pregnancy as possible. Where possible, inclusion was restricted to biological fathers, but paternity status was not ascertainable in all cohorts. For maternal BMI, cohorts used self-reported pre-pregnancy BMI or BMI measured in the early stages of pregnancy. BMI was calculated in kg/m2 and then standardized for each cohort by converting to internal Z-scores.
Measurement of DNA methylation
Biological samples were either cord-blood samples from neonates or peripheral-blood samples from children. DNA methylation was measured using either the llumina Infinium® HumanMethylation450 (486 425 probes) or EPIC (866 553 probes) BeadChip assay (Table 1). Probes that were common to both arrays (maximum 453 008) were included in the meta-analysis. Each cohort conducted its own laboratory methods, quality control and normalization, as detailed in Supplementary Information File 1, available as Supplementary data at IJE online. All cohorts used normalized, untransformed methylation beta values on a scale of 0 to 1.
Other covariates
Questionnaire data were used to derive the following covariates, which were included in all adjusted models regardless of whether the main exposure was paternal or maternal BMI: maternal and paternal age (years); maternal smoking status during pregnancy (preferred definition: smoking throughout pregnancy/no smoking in pregnancy or quitting in the first trimester, but some cohorts used any/no smoking in pregnancy); paternal smoking status during or prior to pregnancy (any smoking in this time/no smoking in this time); maternal parity (one or more previous pregnancies/no previous pregnancies); and paternal socio-economic position (higher/lower). For the latter variable, precise definitions were cohort-specific but most cohorts used paternal educational attainment (if data on paternal socio-economic position were not available, maternal socio-economic position was used). In addition, some secondary models were stratified by the sex of the child. Cohort-specific information on covariate definitions is provided in Supplementary Information File 1, available as Supplementary data at IJE online. Some previous studies of parental BMI and offspring outcomes have elected to adjust for additional covariates such as gestational age at delivery or birthweight. We chose not to adjust for these factors because they cannot be true confounders of the association of interest (they do not influence pre-pregnancy parental BMI). They could, however, be mediators on the causal pathway and therefore adjustment for these would be over-adjustment of the potential effects of parental BMI and could also introduce collider bias.44
Systematic differences between samples (e.g. those influenced by technical batch) were addressed by generating 20 surrogate variables (SVs) using the SVA45,46 R package. The number of SVs (i.e. 20) was estimated using the ALSPAC data set and then each cohort estimated 20 SVs using their own data. Cellular heterogeneity was addressed by estimating cell-type proportions using the Houseman algorithm47 and either a cord-blood reference panel48 or a peripheral-blood reference panel,49 depending on the methylation time point.
Cohort-specific EWAS
Each cohort performed an independent EWAS according to a common, pre-specified analysis plan and R script (available on our Open Science Framework site at doi: 10.17605/OSF.IO/EBTW7). If cohorts had data for both time points, EWAS were performed separately for birth and childhood. Potential methylation outliers, thought to be introduced by a technical error or a rare single-nucleotide polymorphism (SNP), were identified and removed using the Tukey method as previously described.50
Linear-regression models, modelling offspring methylation as the outcome and parental BMI as the exposure, were applied to each CpG using the Limma R package.51 Two main models were run for both paternal and maternal BMIs: (i) a basic model in which paternal or maternal BMI associations were adjusted for estimated cell proportions, SVs for technical batch, maternal and paternal age, maternal smoking status during pregnancy, paternal smoking status during or prior to pregnancy, paternal socio-economic position and maternal parity; and (ii) a model with additional adjustment for the other parent’s BMI. In secondary analyses, the mutually adjusted models (i.e. model (ii)) were run stratified by the sex of the offspring. This is because there is some literature to support paternal effects occurring in a sex-specific manner.52,53 All probes were annotated to the human reference genome version 19, build 37.
Other cohort-specific analyses
To allow us to explore the extent to which paternal BMI is associated with offspring-blood-cell proportions (which is an important source of variation in methylation data, but also an interesting phenotype to study in its own right54), cohorts provided results (effect estimate, standard error, P-value) for linear regressions of each estimated cell type on paternal BMI. These were then meta-analysed using the R package metafor.55
Cohorts also provided the Spearman coefficient and P-value for the correlation between maternal and paternal BMIs to allow us to assess the likelihood of assortative mating as an explanation for our results.
Meta-analysis
Fixed-effects meta-analysis weighted by the inverse of the variance was performed at the University of Bristol using METAL.56 A shadow meta-analysis was also conducted independently by an author at the University of Hasselt (Rossella Alfano). All codes used to perform these analyses are provided on our Open Science Framework site at doi: 10.17605/OSF.IO/EBTW7.
The EWAS meta-analysis pipeline was as follows:
Filter probes from cohort results files to remove probes that are not common to both the EPIC and 450k array, control and QC probes, probes on SNPs, cross-hybridizing probes according to Chen et al.57 and probes on the sex chromosomes.
Perform quality checks of cohort results by plotting correlation matrices of effect estimates generated by different models, generating QQ plots and calculating Lambda values, plotting the distribution of effect estimates and producing ‘precision plots’ of 1/median standard error against the square root of the sample size for each cohort and model.
Conduct a fixed-effects meta-analysis using METAL for each model.
Adjust meta-analysis P-values for multiple testing using the false-discovery-rate (FDR) method. The threshold used to define statistical evidence of an association was an FDR-adjusted P-value <0.05.
Perform checks of meta-analysed results by plotting a correlation matrix of effect estimates generated by different models, generating QQ plots and calculating Lambda values.
Conduct a leave-one-out analysis using the R package metafor55 at sites with the smallest P-values. The leave-one-out survival criteria we specified are: when any single cohort is omitted, the meta-analysis effect estimate should be in the same direction, not attenuate substantially (arbitrarily defined as >20% change-in-estimate) and not have a confidence interval that crosses the null.
Conduct a meta-regression to explore the impact of average age at DNA-sample collection on the childhood EWAS meta-analysis results.
Conduct a sensitivity analysis at the birth time point, excluding cohorts that collected information on paternal BMI based on maternal report (GOYA, INMA, MoBa, Piccolipiù, Project Viva, RHEA) because of concern about measurement error.
Conduct a sensitivity analysis at the childhood time point excluding HELIX because of concerns about overlap between some individuals in this data set and individuals in INMA.
Perform a look-up of any CpGs identified as associated with paternal BMI in the EWAS Catalog (a repository of previously reported EWAS associations; http://www.ewascatalog.org).
Comparison of results for maternal and paternal BMIs
To assess whether paternal and maternal BMIs are associated with offspring methylation to similar extents and with similar distributions throughout the genome, we compared effect estimates for the EWAS meta-analyses with and without mutual adjustment for the other parent’s BMI. At the top 10 CpGs associated with paternal BMI with the smallest P-values, we calculated the Cochrane Q statistic to explore statistical evidence for differences between the maternal- and paternal-effect estimates.
To explore the extent to which maternal BMI might explain associations between paternal BMI and offspring methylation, we conducted Kolmogorov–Smirnov tests to assess the enrichment of our EWAS meta-analysis results for CpGs previously found to be associated with maternal BMI in the PACE consortium.26
Systematic literature review
To identify previous human studies of paternal adiposity and offspring or sperm methylation, we performed a systematic search of PubMed using the R package RISmed.58 The latest search was run in February 2020. Search terms (Supplementary Information File 2, available as Supplementary data at IJE online) were formed using intersections of terms related to paternity, methylation and adiposity. Duplicate PubMed IDs and ineligible article types (non-journal articles and reviews) were excluded. Titles/abstracts were manually screened to assess inclusion based on whether the study investigated paternal adiposity and germ-cell/offspring methylation, and whether it did so in humans. Information on study design, exposure, outcome, tissue, sample size, species and key relevant findings was manually extracted from the full text of included articles.
Testing for enrichment of candidate loci identified through the literature
To explore the enrichment of our EWAS meta-analysis results for loci identified through our literature search, we tested whether the distribution of EWAS meta-analysis P-values at these regions deviates from a null (uniform) distribution using Kolmogorov–Smirnov tests and compared the direction of the effect estimate to what has been reported previously. To identify CpG probes falling within a particular gene, we defined the location of the gene according to the GeneCards database (https://www.genecards.org) and human genome version 19, build 37.
Availability of data and code
All code used to generate our results is available on our Open Science Framework site at doi: 10.17605/OSF.IO/EBTW7. We are not able to publicly share individual-level data from participating cohorts due to issues with consent and ethics, although all summary statistics generated by meta-analysis are also available at doi: 10.17605/OSF.IO/EBTW7.
Results
EWAS meta-analysis at birth
Cohort summaries
Thirteen independent data sets were included in the EWAS meta-analyses at birth. Table 2 summarizes key characteristics of these cohorts (more details in Supplementary Information File 3, available as Supplementary data at IJE online). Around 48% of the babies were female. In all cohorts, paternal BMI had a higher mean and a lower standard deviation (SD) compared with maternal BMI. There was moderate correlation between both parents’ BMIs (r = 0.2), which might be explained by assortative mating and/or a shared environment.
Table 2.
A summary of the sex of the child and parental BMI for each cohort in the birth meta-analysis
| Study | N (N female, N male) | Mean paternal BMI in kg/m2 (SD) | Percentage fathers with BMI≥30 (i.e. obese) | Mean maternal BMI in kg/m2 (SD) | Percentage mothers with BMI≥30 (i.e. obese) | Spearman’s corre lation between paternal and maternal BMI (P-value) |
|---|---|---|---|---|---|---|
| ALSPAC | 531 (267, 264) | 25.0 (3.0) | 6% | 22.6 (3.3) | 4% | 0.2 (7.6×10–7) |
| Born in Bradford (British Asian) | 70 (27*, 43) | 26.6 (5.3) | 17% | 26.2 (5.8) | 21% | 0.2 (1.1×10–1) |
| Born in Bradford (White British) | 115 (59, 56) | 27.5 (4.7) | 24% | 26.7 (6.1) | 24% | 0.4 (9.1×10–4) |
| CHAMACOS | 158 (80, 78) | 28.0 (4.2) | 32% | 26.5 (4.5) | 19% | 0.1 (1.1×10–1) |
| Generation R | 947 (476, 471) | 25.2 (3.2) | 7% | 23.2 (3.9) | 6% | 0.2 (8.8×10–8) |
| GOYA | 390 (190, 200) | 25.1 (3.1) | 6% | 23.4 (3.7) | 6% | 0.1 (7.1×10–3) |
| INMA | 352 (173, 179) | 25.8 (3.5) | 13% | 23.8 (4.5) | 9% | 0.2 (4.7×10–5) |
| MoBa1 | 982 (458, 524) | 25.6 (3.1) | 8% | 24.0 (4.1) | 9% | 0.1 (6.2×10–5) |
| MoBa2 | 621 (275, 346) | 25.7 (3.1) | 8% | 24.3 (4.6) | 11% | 0.2 (2.2×10–8) |
| MoBa3 | 212 (109, 103) | 26.0 (3.1) | 9% | 24.0 (3.9) | 9% | 0.3 (2.0×10–4) |
| Piccolipiù | 98 (45, 53) | 24.9 (3.0) | 3% | 22.6 (3.9) | 8% | 0.3 (2.6×10–3) |
| Project Viva | 324 (160, 164) | 26.3 (3.6) | 13% | 24.3 (4.9) | 12% | 0.3 (1.2×10–6) |
| RHEA | 94 (45, 49) | 27.2 (4.0) | 20% | 25.1 (5.5) | 16% | 0.3 (1.1×10–2) |
| Total or meana | 4894 (2337, 2530) | 26.98 (3.2) | 10% | 23.7 (4.1) | 9% | 0.2 |
In the ‘Total’ row, the average BMI and correlation values were calculated by weighting the by the inverse variance for each cohort.* too few to be included in the sex-stratified meta-analysis.
BMI, body mass index; SD, standard deviation; cohort abbreviations described in the main text.
Quality checks
Quality checks of cohort-specific EWAS results are summarized in Supplementary Information File 4, available as Supplementary data at IJE online. Generally, no major problems were identified, but there were a small number of extreme effect estimates in some cohorts, mainly in the sex-stratified models in which the sample sizes were lower. Quality checks of the meta-analysis results (Supplementary Information File 5, available as Supplementary data at IJE online) showed that these outliers had little weighting in the meta-analysis and therefore little impact on the EWAS meta-analysis results. Therefore, these values were not excluded from the meta-analysis.
Associations between paternal BMI and offspring methylation at birth
Table 3 summarizes the results of each EWAS meta-analysis model (full results available on our Open Science Framework site at doi: 10.17605/OSF.IO/EBTW7). After FDR correction for multiple testing, we did not identify any CpG sites for which there was evidence of an association between paternal BMI and offspring DNA methylation at birth (FDR < 0.05). Effect estimates for the model with and without adjustment for maternal BMI were very similar: they correlated highly (Spearman’s r = 0.97) and the median percentage difference in effect estimates between the models was 0.23% (interquartile range: 0.1%, 0.6%), suggesting that maternal BMI was not a strong confounder. In a sensitivity analysis, excluding cohorts that defined paternal BMI based on maternal report did not increase the number of CpGs with FDR-corrected P < 0.05.
Table 3.
A summary of results of each EWAS meta-analysis model at birth
| Modela | CpGs with FDR-corrected P < 0.05 | CpGs surviving leave-one-out analysis | Meta-analysis sample size | Genomic inflation factor (λ)b | |
|---|---|---|---|---|---|
| Paternal BMI | |||||
| All offspring | 0 | n.a. | 4894 | 1.13 | |
| All offspring (additionally adjusted for maternal BMI) | 0 | n.a. | 4894 | 1.16 | |
| Female offspring (additionally adjusted for maternal BMI) | 7 | 4 (57%) | 2337 | 1.10 | |
| Male offspring (additionally adjusted for maternal BMI) | 0 | n.a. | 2530 | 1.10 | |
| Maternal BMI | |||||
| All offspring | 39 | 35 (90%) | 4894 | 1.10 | |
| All offspring (additionally adjusted for paternal BMI) | 30 | 28 (93%) | 4894 | 1.11 | |
| Female offspring (additionally adjusted for paternal BMI) | 9 | 4 (44%) | 2337 | 1.05 | |
| Male offspring (additionally adjusted for paternal BMI) | 1 | 1 (100%) | 2530 | 1.09 | |
All models adjusted for maternal and paternal age, maternal and paternal smoking, paternal education, maternal parity, estimated cell counts and 20 surrogate variables.
The genomic inflation factor (λ) estimates the extent of the bulk inflation of EWAS P-values and the excess false-positive rate. 1 = no inflation; >1 some evidence of inflation.
BMI, body mass index.
In a sex-stratified analysis adjusted for maternal BMI, we found some evidence of an association between methylation and paternal BMI at seven CpGs in female offspring only (Table 4). Three of these did not survive the leave-one-out analysis [i.e. on the omission of one cohort, the effect estimates were in different directions, changed considerably (>20%) and/or had confidence intervals that crossed the null; results in Supplementary Information File 6, available as Supplementary data at IJE online]. Of the four remaining CpGs, according to the EWAS Catalog, one (cg23487201 at APCDD1L) has previously been associated with clear cell carcinoma and pancreatic ductal adenocarcinoma and another (cg00039564 at TAX1BP1) has previously been found to be associated with rheumatoid arthritis.
Table 4.
CpGs associated with paternal BMI with FDR-adjusted P < 0.05 in female offspring only at birth (estimates are adjusted for maternal BMI)
| CpG (gene) | Estimate (95% CI) in females | P-value in females | Heterogeneity I2 in females (P-value) | Estimate (95% CI) in males | P-value in males | Estimate (95% CI) in all | P-value in all |
|---|---|---|---|---|---|---|---|
| acg03395511 (DUSP22) | 2.93 (2.55, 3.30) | 7×10–53 | 98.7 (6×10–179) | 0.39 (0.01, 0.77) | 0.04 | 0.07 (–0.21, 0.35) | 0.6 |
| acg27586797 (intergenic) | –4.90 (–5.80, –4.00) | 2×10–26 | 75.8 (1×10–5) | 1.33 (–0.03, 2.68) | 0.05 | –0.30 (–1.25, 0.65) | 0.5 |
| acg04481923 (MIR886) | 2.07 (1.42, 2.72) | 4×10–10 | 90.4 (3×10–19) | –0.08 (–0.73, 0.57) | 0.8 | –0.02 (–0.46, 0.43) | 0.9 |
| cg09452082 (intergenic) | –0.43 (–0.59, –0.26) | 4 ×10–7 | 79.3 (2×10–7) | –0.13 (–0.29, 0.04) | 0.1 | –0.18 (–0.29, –0.06) | 0.003 |
| cg23487201 (APCDD1L) | –0.17 (–0.24, –0.11) | 5 ×10–7 | 15.2 (0.3) | 0.03 (–0.03, 0.09) | 0.4 | –0.06 (–0.10, –0.01) | 0.01 |
| cg19702703 (AFAP1) | –0.45 (–0.63, –0.27) | 6 ×10–7 | 1.3 (0.4) | –0.13 (–0.30, 0.04) | 0.1 | –0.23 (–0.35, –0.11) | 0.0001 |
| cg00039564 (TAX1BP1) | –0.19 (–0.26, –0.11) | 8×10–7 | 23.4 (0.2) | 0.03 (–0.04, 0.11) | 0.4 | –0.05 (–0.10, 0.00) | 0.06 |
‘Estimate’ can be interpreted as the difference in the offspring percentage methylation per 1-standard-deviation increase in paternal BMI, after adjustment for all covariates including maternal BMI.
CpG did not survive leave-one-out analysis, indicating that the strong association was driven by a single cohort.
BMI, body mass index.
Comparison of estimates for paternal and maternal BMIs
Maternal BMI was associated with methylation at many more CpG sites than paternal BMI was (Table 3). In the main models not stratified by sex, there were 39 CpGs associated with maternal BMI before adjustment for paternal BMI and 30 after (FDR-adjusted P < 0.05); 26 overlapped. Most associations survived a leave-one-out sensitivity analysis.
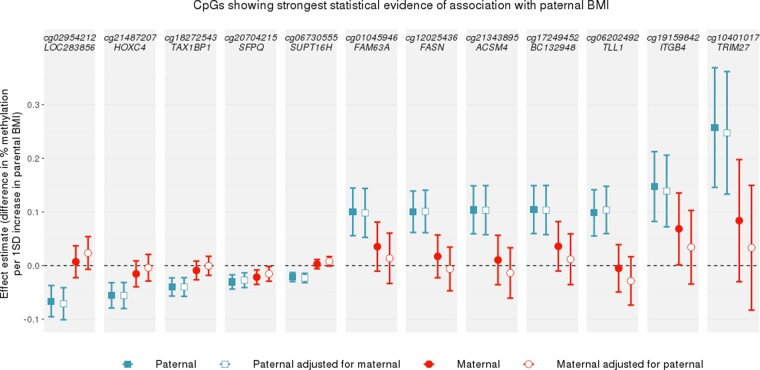
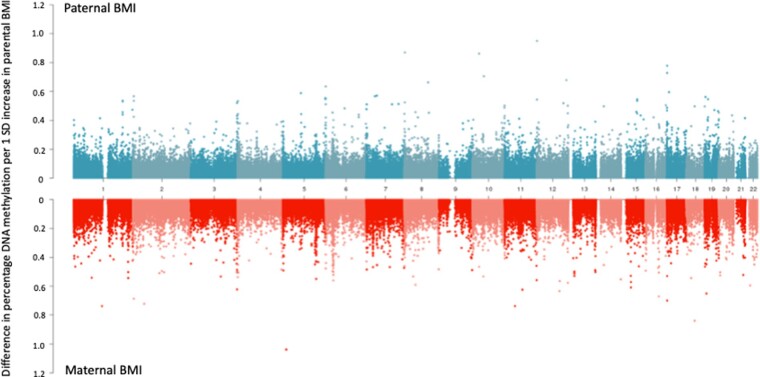
At the top CpGs associated with paternal BMI at a relaxed (but arbitrary) P-value threshold of P < 1 × 10–5, the estimated paternal effect was greater (further from the null) than the estimated maternal effect, even after adjustment for the other parent’s BMI (Figure 1). There was also strong evidence of heterogeneity between the maternal and paternal mutually adjusted estimates (all heterogeneity FDR-adjusted P-values < 0.05; I2 ranging from 86.6 to 96.4). However, apart from at the most robustly paternal BMI-associated CpG sites, this pattern (of greater paternal- than maternal-effect estimates) was not observed. In fact, throughout the genome, around half (49.6%) of the CpGs had larger absolute effect estimates for paternal BMI and the other half (50.2%) had larger absolute effect estimates for maternal BMI. Figure 2 shows that maternal-effect estimates (before adjustment for paternal BMI) were similar in size to paternal-effect estimates, and the distribution of effect estimates across the genome was similar regardless of parent. Results were very similar after mutual adjustment for the other parent’s BMI (Supplementary Information File 7, available as Supplementary data at IJE online).
Figure 1.
A comparison of paternal and maternal body mass index (BMI)-effect estimates at CpGs with P < 1 × 10–5 in the paternal BMI epigenome-wide association study (EWAS) meta-analysis at birth. CpGs were selected if they were associated with paternal BMI with a P-value <1 × 10–5 in the model that was not adjusted for maternal BMI. Points show EWAS meta-analysis effect estimates, bars show 95% confidence intervals. Confidence intervals are not adjusted for multiple testing.
Figure 2.
A comparison of paternal and maternal body mass index (BMI) epigenome-wide association study (EWAS) effect estimates across the genome. Absolute effect estimates (y-axis) are plotted against genomic location (x-axis; numbers indicate chromosome number). Paternal BMI EWAS meta-analysis results are plotted on the top, with maternal EWAS meta-analysis results on a mirrored axis below. Models were not mutually adjusted for the other parent’s BMI (for a comparison of the mutually adjusted results, see Supporting Information File 7, available as Supplementary data at IJE online).
In a previous PACE-consortium study,26 we identified 86 cord-blood CpGs associated with maternal BMI in an EWAS meta-analysis across 19 cohorts (9 of which also contributed results to the current study). Of the 86 CpGs identified in that previous study (which had higher statistical power to detect associations), 64 were available in the current study after probe filtering. To explore the extent to which maternal BMI might be driving any association between paternal BMI and offspring methylation in the current study, we assessed the enrichment of our paternal BMI EWAS meta-analysis results for these 64 maternal BMI-associated CpGs. We found little evidence of enrichment (Kolmogorov–Smirnov P-value for inflation of EWAS P-values = 0.54 in EWASs unadjusted for maternal BMI; 0.61 in EWASs adjusted for maternal BMI), suggesting that any relationship between paternal BMI and offspring methylation was unlikely to be driven by confounding by maternal BMI, even before adjustment for maternal BMI. Conversely, the maternal BMI EWAS meta-analysis results in the current study were highly enriched for previously identified maternal BMI-associated CpGs (Kolmogorov–Smirnov P for inflation = 2.2 × 10–16 in EWASs adjusted and unadjusted for paternal BMI). This finding was as expected, given that the main exposure was the same and the samples were overlapping, but it highlights the ability of this analysis to detect strong associations with maternal BMI if they exist.
EWAS meta-analysis at childhood
Cohort summaries
Six cohorts were included in the EWAS meta-analyses at childhood. Table 5 summarizes the key characteristics of these cohorts. Around 48% of the children were female. In all cohorts, paternal BMI had a higher mean and a lower SD compared with maternal BMI.
Table 5.
A summary of sex and age of the child and parental BMI for each cohort in the childhood meta-analysis
| Study | N (N female, N male) | Mean age of children in years (SD) | Mean paternal BMI in kg/m2 (SD) | Percentage fathers with BMI≥30 (i.e. obese) | Mean maternal BMI in kg/m2 (SD) | Percentage mothers with BMI≥30 (i.e. obese) | Spearman’s correlation between paternal and maternal BMI (P-value) |
|---|---|---|---|---|---|---|---|
| ALSPAC | 570 (280, 290) | 7.5 (0.2) | 25.0 (3.1) | 7% | 22.6 (3.4) | 4% | 0.2 (5.1×10–6) |
| CHAMACOS | 108 (56, 52) | 9.2 (0.3) | 27.6 (3.4) | 27% | 27.0 (4.4) | 22% | 0.2 (2.9×10–2) |
| Generation R | 335 (174, 161) | 6.0 (0.4) | 25.0 (3.3) | 6% | 24.1 (3.9) | 6% | 0.2 (1.5×10–5) |
| HELIX | 516 (231, 285) | 8.4 (1.7) | 26.6 (3.7) | 18% | 23.9 (4.4) | 9% | 0.3 (1.1×10–10) |
| INMA | 177 (87, 90) | 4.4 (0.2) | 26.0 (3.6) | 15% | 24.6 (5.1) | 13% | 0.3 (9.6×10–5) |
| Project Viva | 276 (132, 144) | 7.8 (0.7) | 26.4 (3.7) | 15% | 24.5 (4.7) | 13% | 0.4 (4.2×10–13) |
| Totala | 1982 (960, 1022) | 6.9 (0.3) | 25.7 (3.4) | 12% | 24.3 (5.2) | 9% | 0.3 |
In the ‘Total’ row, the average BMI, age and correlation values were calculated by weighting by the inverse variance for each cohort.
BMI, body mass index.
Quality checks
Quality checks of cohort-specific EWAS results are summarized in Supplementary Information File 8, available as Supplementary data at IJE online. Meta-analysis quality checks are summarized in Supplementary Information File 9, available as Supplementary data at IJE online. We did not exclude any data following these checks.
Associations between paternal BMI and offspring methylation in childhood
Table 6 summarizes the results of each EWAS meta-analysis model (full results available on our Open Science Framework site at doi: 10.17605/OSF.IO/EBTW7). There was one CpG for which we found evidence (FDR-adjusted P < 0.05) of an association with paternal BMI [cg2720130 at GIP on chromosome 17; ß 0.4%, 95% confidence interval (CI) 0.2% to 0.5%, P = 8.8 × 10–8] and one (different) CpG with evidence of an association with maternal BMI (cg07099084 in an intergenic region on chromosome 1, ß –0.05%, 95% CI –0.03% to –0.06%, P = 1.1 × 10–7). However, neither survived mutual adjustment for the other parent’s BMI, neither was associated with parental BMI in the birth analysis and one (cg07099084) did not survive a leave-one-out analysis (Supplementary Information File 10, available as Supplementary data at IJE online). Excluding HELIX from the full meta-analysis did not change the number of associations with FDR-adjusted P < 0.05. A meta-regression also showed little evidence that the mean age of the children at methylation measurement was associated with EWAS meta-analysis effect estimates (Supplementary Information File 10, available as Supplementary data at IJE online).
Table 6.
A summary of results of each EWAS meta-analysis model at childhood
| Modela | CpGs with FDR-corrected P < 0.05 | CpGs surviving leave-one-out analysis | Meta-analysis sample size | Genomic inflation factor (λ)b | |
|---|---|---|---|---|---|
| Paternal BMI | |||||
| All offspring | 1 | 1 (100%) | 1982 | 1.03 | |
| All offspring (additionally adjusted for maternal BMI) | 0 | n.a. | 1982 | 1.00 | |
| Female offspring (additionally adjusted for maternal BMI) | 0 | n.a. | 960 | 1.00 | |
| Male offspring (additionally adjusted for maternal BMI) | 0 | n.a. | 1022 | 1.05 | |
| Maternal BMI | |||||
| All offspring | 1 | 0 (0%) | 1982 | 1.11 | |
| All offspring (additionally adjusted for paternal BMI) | 0 | n.a. | 1982 | 1.08 | |
| Female offspring (additionally adjusted for paternal BMI) | 0 | n.a. | 960 | 1.06 | |
| Male offspring (additionally adjusted for paternal BMI) | 0 | n.a. | 1022 | 1.07 | |
All models adjusted for maternal and paternal age, maternal and paternal smoking, paternal SEP, maternal parity, estimated cell counts and 20 surrogate variables.
The genomic inflation factor (λ) estimates the extent of the bulk inflation of EWAS P-values and the excess false-positive rate. 1 = no inflation; >1 some evidence of inflation.
BMI, body mass index.
Analysis of cell proportions
Paternal BMI was not associated with the proportion of any cell type in offspring blood (Supplementary Information File 11, available as Supplementary data at IJE online), except for a very small difference in the estimated proportion of nucleated red blood cells in offspring cord blood (nRBCs; 0.001 greater proportion of nRBCs per 1-SD increase in paternal BMI; 95% CI 0.0004 to 0.0017; P = 0.001) and an even smaller difference in the proportion of CD4 T-cells in childhood peripheral blood (0.0007 lower proportion of CD4 T-cells per 1-SD increase in paternal BMI; 95% CI –0.0013 to –0.0002; P = 0.007), which appeared to be largely driven by the HELIX data set and did not survive a sensitivity analysis excluding HELIX.
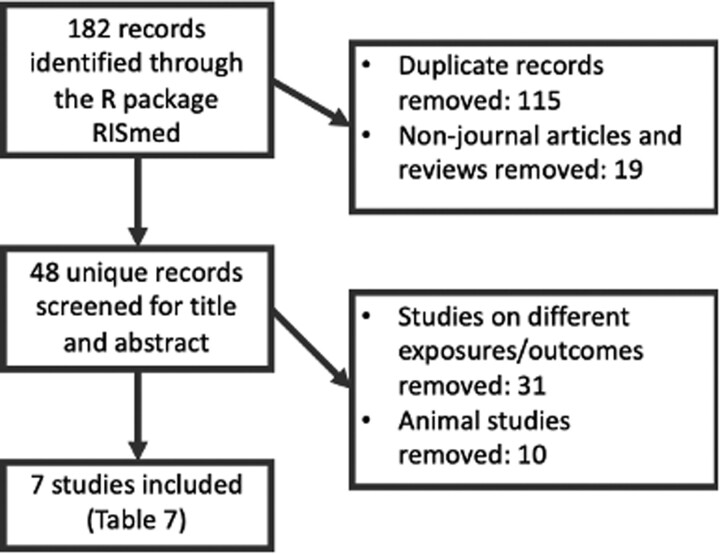
Systematic literature review
Figure 3 summarizes the workflow and Table 7 outlines the seven included studies resulting from a systematic literature review of human studies of paternal adiposity and offspring or gamete methylation. There were five studies of imprinted regions and two untargeted array-based studies. Four studies investigated DNA methylation in offspring cord blood, two in paternal sperm and one in both.
Figure 3.
The systematic-review process used to identify human studies of paternal adiposity and offspring or germ-cell methylation
Table 7.
Summary of identified studies of paternal adiposity and sperm or offspring DNA methylation. In all studies of offspring methylation, the estimated effect of paternal BMI/obesity was adjusted for maternal BMI/obesity
| Study (country) | Exposure | Outcome | Sample size | Studied regions | Key findings |
|---|---|---|---|---|---|
| Noor et al.20 (USA) | Paternal BMI | Offspring DNA methylation at birth (cord blood), age 3 and age 7 (peripheral blood) | 429 | Untargeted (Illumina 450k array) | Paternal BMI was associated with cord-blood DNA methylation at nine CpGs with an FDR-adjusted P-value <0.05. Three of these persisted at age 3 and one of those also persisted at age 7. When stratified by maternal BMI, no CpGs were associated with paternal BMI in the subset with maternal BMI <25, but 18 CpGs were identified in the subset with maternal BMI≥25. None persisted at later time points |
| Potabattula et al.19 (Germany) | Paternal BMI | Sperm DNA methylation and cord-blood DNA methylation | 294 (sperm) and 113 (cord blood) | Imprinted genes: MEST/PEG1, SNRPN/PEG4, NNAT/PEG5, SGCE/PEG10, H19-IG, IGF2, MEG3-IG, and one obesity-related gene: HIF3A | Paternal BMI was positively associated with MEG3 methylation in sperm and in male (but not female) offspring. There were some other small magnitude associations in sex-stratified analyses |
| Potabattula et al.17 (Germany) | Paternal BMI | Cord-blood DNA methylation | 46 | Six imprinted genes: H19, IGF2, MEST, PEG3, MEG3, NNAT | Paternal BMI was positively associated with methylation of the paternal MEST allele |
| Soubry et al.16 (USA) | Paternal overweight or obesity | Sperm DNA methylation | 67 (23 overweight or obese) | 12 imprinted genes: MEG3, MEG3-IG, IGF2, H19, GRB10, NDN, NNAT, PLAGL1, SGCE/PEG10, SNRPN, PEG1/MEST, PEG3 | Paternal overweight/obesity was associated with lower sperm methylation at MEG3, NDN, SNRPN and SGCE/PEG10 and higher methylation at MEG3-IG, H19, IGF2 compared with controls. There was little evidence of association at GRB10, NNAT, PLAGL1, PEG1/MEST, PEG3 |
| Donkin et al.18 (Denmark) | Paternal obesity | Sperm DNA methylation | 23 (10 obese) | Untargeted (RRBS) | There were 9081 unique genes differentially methylated in the sperm of lean compared with obese men with an FDR-adjusted P < 0.1 (7059 with FDR-adjusted P < 0.05) |
| Soubry et al.15 (USA) | Paternal obesity and paternal BMI | Cord-blood DNA methylation | 63 (16 obese) | Seven imprinted genes: MEG3, MEST, NNAT, PEG3, PLAGL1, SGCE, PEG10 | Paternal obesity was associated with lower offspring methylation at MEST, NNAT, PEG3. Paternal BMI was positively correlated with methylation at SGCE/PEG10 |
| Soubry et al.14 (USA) | Paternal obesity | Cord-blood DNA methylation | 70 (16 obese) | Two imprinted genes: H19, IGF2 | Paternal obesity was associated with lower methylation at IGF2 compared with controls, but there was no difference at H19 |
BMI, body mass index; RRBS, reduced representation bisulphite sequencing.
Comparison to the literature
Imprinted regions identified in studies by Soubry et al. and Potabattula et al
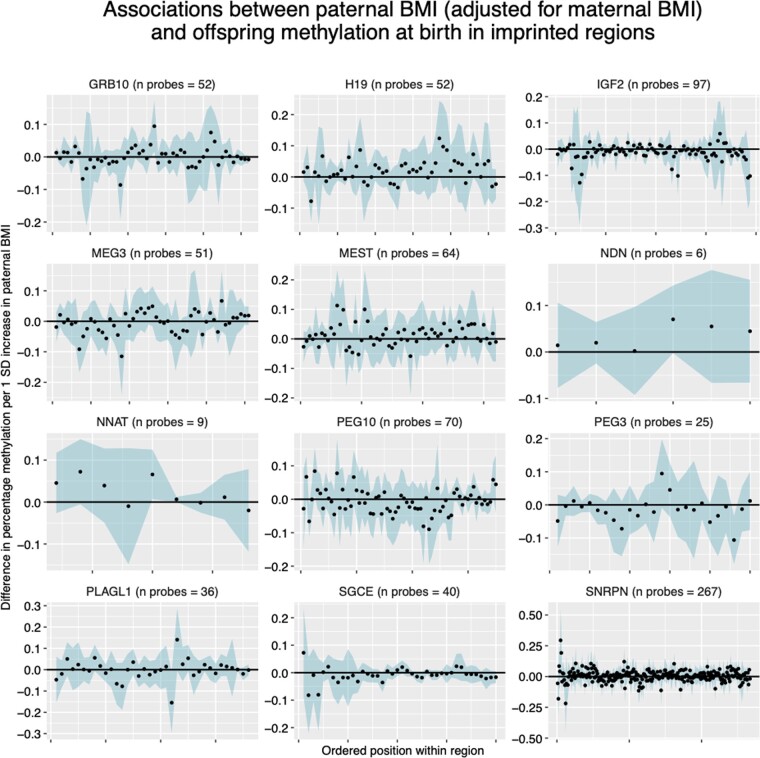
At paternally imprinted regions identified in the literature review, EWAS meta-analysis effect estimates for the association between paternal BMI and cord-blood methylation (adjusted for maternal BMI) were small with no clear trend in direction (Figure 4). Findings were similar for the EWAS model unadjusted for maternal BMI (Supplementary Information File 12, available as Supplementary data at IJE online).
Figure 4.
Paternal body mass index (BMI)-effect estimates at CpGs within imprinted regions. Each panel shows a different imprinted gene, with CpGs arranged in order on the x-axis. The blue ribbon shows the 95% confidence intervals. All results are adjusted for maternal BMI.
Regions identified by Donkin et al
Donkin et al.18 reported 9081 genes differentially methylated between sperm samples from lean and obese men (with FDR-adjusted P < 0.1). Of these, we could only map to 511 CpGs at the same genomic positions in our cord-blood EWAS meta-analysis results, because Donkin et al. measured methylation using reduced representation bisulphite sequencing (RRBS) with a higher coverage of the genome than the 450k array. In our paternal BMI EWAS meta-analysis at birth (adjusted for maternal BMI), we found the same direction of effect at only roughly half of these genes (252/511) and only 17 of these had a P-value < 0.05, with none surviving FDR correction for multiple testing at either 511 or 252 sites. QQ plots and a Kolmogorov–Smirnov test suggested that our EWAS P-values at these 252 sites were not smaller than would be expected by chance (Supplementary Information File 12, available as Supplementary data at IJE online; Kolmogorov–Smirnov P = 0.27). Findings were similar when using the EWAS meta-analysis P-values from the paternal BMI model that was not adjusted for maternal BMI (Supplementary Information File 12, available as Supplementary data at IJE online).
CpGs identified by Noor et al
In Project Viva (a cohort that also contributed results to our meta-analysis), Noor et al. identified nine CpGs for which cord-blood methylation was associated with periconceptional paternal BMI after adjustment for maternal BMI.20 In our results at birth, we found the same direction of estimated effect at seven out of nine CpGs. Only one of these had a P-value < 0.05 but this association also survived FDR correction for multiple testing at nine sites (cg04763273 mapping to TFAP2C; –0.41% difference in methylation per 1-SD increase in paternal BMI; 95% CI –0.67 to –0.15; P = 0.002). According to our leave-one-out-analysis criteria, this CpG ‘survived’ after omission of Project Viva, but it did not survive after omission of Generation R. A Kolmogorov–Smirnov test suggested that our EWAS P-values at the nine CpGs identified by Noor et al. were not smaller than would be expected by chance (Kolmogorov–Smirnov P = 0.21). Noor et al. also identified 18 CpGs for which cord-blood methylation was associated with paternal BMI when the analysis was restricted to a subset of offspring of mothers with a BMI > 25. In our (unstratified) results at birth, we found the same direction of estimated effect at only 9 of these 18 CpGs, only 1 had a P-value < 0.05 (cg04763273) and a Kolmogorov–Smirnov test suggested that our EWAS P-values were not smaller than would be expected by chance (Kolmogorov–Smirnov P = 0.54).
Discussion
Summary and interpretation of findings
In coordinated EWAS meta-analysis using a total of 19 data sets, at a genome-wide level of significance (FDR-adjusted P < 0.05), we found little evidence of an association between prenatal paternal BMI and offspring-blood DNA methylation at birth or in childhood. In secondary sex-stratified analyses, we found robust associations between paternal BMI and cord-blood methylation at just four CpGs in female offspring only. There was little evidence of residual confounding by maternal BMI, and paternal BMI was not strongly associated with estimated cell heterogeneity at either time point. At the top CpGs most strongly associated with paternal BMI, estimates of the effect of paternal BMI on methylation were larger than estimates of the effect of maternal BMI, suggesting some evidence of paternal-specific association at these top CpGs (although not passing our P-value threshold). However, more associations with maternal BMI than paternal BMI surpassed our P-value threshold (FDR-adjusted P < 0.05) and, across the whole genome, estimates of the effect of paternal BMI were similar in magnitude to those of maternal BMI.
The lack of statistical support for paternal associations may reflect limited power and we cannot discount an impact of paternal BMI on offspring DNA methylation without studies in populations with greater variability in paternal BMI and/or larger sample sizes. Although we note that we found associations with maternal BMI using exactly the same samples, if any true effect of paternal BMI is weaker than the maternal effect, power could still be an issue. Furthermore, we cannot rule out an impact on DNA methylation measured in different tissues and/or at regions not covered by the 450k array.
Comparison to the literature
Our largely null findings are in contrast to some previous findings. In a systematic review, we identified seven studies that have previously reported associations between paternal BMI and sperm or offspring methylation in humans. Five of these (three from one study and group14–16 and two from another17,19) were candidate gene studies that found associations between paternal obesity or higher BMI and sperm or offspring-cord-blood methylation at imprinted regions (all after adjustment for maternal BMI or obesity). There is a strong biological rationale for studying imprinted regions in the context of paternal exposures, because methylation marks at imprinted regions appear to survive the wave of demethylation that occurs following fertilization and therefore have the potential to pass on epigenetic information from the gametes to the offspring.10,59 However, where studies of imprinted genes have considered the same loci, the directions of the estimated effects have been discordant between studies. For example, Potabattula et al.17 found a positive correlation between paternal BMI and cord-blood methylation at MEST but Soubry et al.14 found that the cord blood of the offspring of obese fathers was lower than that of controls, indicating an inverse correlation with BMI. There are also paradoxical findings at SGCE/PEG10 and IGF2 between studies of sperm16 and cord blood14 but, if methylation differences in sperm are transmitted to offspring, we would expect the same direction of estimated effects in these tissues. In our EWAS meta-analysis of paternal BMI, we found little evidence of enrichment for imprinted genes. Effect estimates at individual CpGs within imprinted regions were small and the direction of effect varied within most genes (Figure 4). Therefore, we found little evidence to support the findings of these candidate gene studies, despite having a much larger sample size and statistical power. However, it should be noted that the Illumina BeadChip array does not provide full coverage of imprinted regions, so further, more detailed analysis of these regions may be justified.
One small study (total n = 23; 10 obese) by Donkin et al.18 used an untargeted genome-wide approach that identified >9000 CpGs throughout the genome differentially methylated in the sperm of obese vs lean men. Only 511 of these CpGs were available in our meta-analysis but we found little evidence of an association at these. The difference in findings of the two studies could reflect a number of factors, including differences in the studied tissue (sperm vs offspring blood), technology (RRBS vs 450k), definition of the phenotype (i.e. obese/lean vs BMI over the whole range) or study sample (e.g. all the obese men in Donkin et al. were glucose-intolerant).
Finally, in our meta-analysis, we replicated the direction of effect at seven out of nine CpGs identified in Noor et al.’s study of periconceptional paternal BMI and cord-blood DNA methylation in Project Viva.20 One of these CpGs (cg04763273 near TFAP2C) appeared to be robustly associated with paternal BMI, but we found limited evidence to support their other findings. Our study designs were similar in that we used the same Illumina array, exposure definition, offspring tissue and time point, and even had some sample overlap (Project Viva contributed results to our meta-analysis). However, there were some differences in the model and our sample size was >11 times larger and therefore more robust for identifying false positives.
Strengths
Analyses were conducted according to a pre-specified, harmonized analysis plan, which is publicly available to aid reproducibility. All the code used to conduct these analyses and all the resulting EWAS meta-analysis summary statistics are publicly available on our Open Science Framework site at doi: 10.17605/OSF.IO/EBTW7. This means that new studies with relevant data could undertake identical analyses and meta-analyse with our results to produce more precise estimates.
Our study uses a sample size of 4894, which is >11-fold larger than all the independent studies identified in our systematic review (Table 7), the largest of which has a sample size of 429. It draws together rich data from multiple birth cohorts internationally and this richness allowed us to adjust for important potential confounders. We also attempted to adjust for systematic variation in the DNA-methylation data by generating and adjusting for SVs, which is an approach that has been shown to reduce the risk of false positives.45 In a further attempt to ensure the robustness of our results, we conducted sensitivity analyses (leave-one-out at top sites, excluding cohorts with only maternal-reported paternal BMI, excluding HELIX from the genome-wide meta-analysis, and meta-regression of age).
Our rich data enabled us to conduct a series of novel analyses. First, we explored associations between paternal prenatal BMI and offspring DNA methylation at childhood, which allows exploration of the persistence of associations from birth and/or the effect of paternal BMI postnatally (which we would expect to be correlated with prenatal paternal BMI). Second, we explored associations between paternal BMI and cellular heterogeneity, which is an important source of variation in methylation data, but also an interesting phenotype to study in its own right.54 Third, we have previously shown that maternal BMI is associated with offspring methylation, which may reflect a causal intrauterine effect at some CpGs.26 Therefore, to help us tease apart paternal from maternal effects, we compared paternal models adjusted and unadjusted for maternal BMI and we also studied maternal BMI as the main exposure. A particular advantage here was that we included the same samples in both analyses and adjusted for the same covariates, so the sample sizes were the same and the main exposure (paternal or maternal BMI) was the only difference between models. We calculated the correlation between maternal and paternal BMI in each cohort, which provided modest support for assortative mating, but, by comparing paternal- and maternal-effect estimates and assessing the enrichment of our paternal results for the CpGs that we previously identified as associated with maternal BMI,26 we were able to infer that maternal BMI was not an important confounder driving associations between paternal BMI and offspring methylation.
Limitations
There are a number of limitations that should be considered when interpreting our results. First, the 450k array covers only 1.7% of CpGs on the genome, so regions (including imprinted regions) that might be differentially methylated in association with paternal BMI might be missed. Second, BMI could be a poor measure of paternal adiposity in our sample, partly due to general issues with the use of BMI as a measure of adiposity60,61 (perhaps particularly in men) and partly due to measurement error introduced by self- or partner report. One study showed that lean mass explained more variability in men’s BMI than body fat did, whereas the opposite was seen in women.60 Measurement error might be higher for paternal BMI than maternal BMI because few cohorts had direct measurements and, in some instances, BMI was reported for the father by the mother, introducing additional measurement error to the questionnaire-reported variable (however, we found similar results in our EWAS meta-analysis when we excluded cohorts that used maternal report to define paternal BMI). More variation in offspring methylation might be captured by another measure such as fat-mass percentage or a measure of ‘lipotoxicity’61 but these data were not available. Third, offspring blood might not be the most suitable tissue to study and effects might be seen in other tissues such as adipose (given previous evidence of associations between paternal and offspring adiposity) but, again, we were limited by data availability. Fourth, the range of paternal BMI in our study sample could be insufficient to show an effect. As with associations between maternal BMI and offspring adiposity,62 there might be a J- or U-shaped relationship between paternal BMI and offspring outcomes, whereby strong associations are only seen at the extremes of the distribution. We anticipated that we would not have enough power to dichotomize into (extreme) obese and lean groups, so we were limited to only studying paternal BMI across the whole range as a continuous variable. Indeed, in our birth analysis, only 10% of fathers across all cohorts were obese (Table 2; Supplementary Information File 3, available as Supplementary data at IJE online), which is the same as a recent estimate of the worldwide prevalence of obesity in men, but much lower than the estimated prevalence of obesity in adults living in Europe (23%) and America (28%),63 where most of our sample reside. This relatively low occurrence of paternal obesity (and therefore variability in BMI) in our sample may partly explain why we did not find stronger evidence of an association with our outcome. Finally, paternal data, including paternal BMI, from birth-cohort studies are potentially more at risk of bias than maternal data. Lower prioritization and greater difficulties in recruiting fathers can introduce a higher degree of missing data for fathers compared with that for mothers. If paternal participation is related to BMI, this could create a selection bias in our sample. Additionally, non-paternity (i.e. partners not being genetically related to their offspring) might also introduce bias if it is related to paternal BMI. Both of these issues could bias paternal estimates towards the null and therefore could be a plausible non-biological reason for our observation of more FDR < 0.05 associations between offspring methylation and maternal than paternal BMI.
Suggestions for further research
Fathers are a potential long-overlooked target for public-health advice and interventions to improve child health, as well as the health of the fathers themselves and their partners.3 Paternal effects on offspring health have been observed, so there is a logical motivation to further investigate the potential underlying molecular mechanisms. As mentioned above, in studies of the effect of paternal adiposity, this work could focus on extreme ends of the BMI distribution and/or other more informative measures of adiposity such as fat-mass index, waist circumference or measures of lipotoxicity.61 Evidence from animal studies suggests that other epigenetic mechanisms such as long non-coding RNAs or tRNAs could be more likely intergenerational carriers of paternal information than DNA methylation and it would be useful to extend these investigations to humans.
There is also huge scope to study the effects of other paternal characteristics, some of which might be related to BMI, such as chronic inflammation, circulating levels or dietary intake of nutrients and nutritional supplements (especially those that influence one carbon metabolism, such as folate) and health behaviours like smoking and alcohol consumption. Studies of paternal effects are increasingly appearing in the literature (although still lagging far behind studies of maternal effects).3,64 Indeed, studies of paternal effects on a wide range of phenotypes are underway in many of the PACE-consortium cohorts that contributed to this paper [e.g. see the Exploring Prenatal Influences on Childhood Health study, which is a multicohort study of effects of maternal and paternal prenatal health behaviours on childhood health over multiple domains].
Conclusion
In this large EWAS meta-analysis, we found little evidence of an association between paternal pre-pregnancy BMI and offspring DNA methylation in blood, including at imprinted genes. However, this does not rule out the possibility of a paternal epigenetic effect in different tissues or via different mechanisms. More research is warranted to gain a greater understanding of the size and nature of contributions of paternal adiposity to offspring outcomes more broadly.
Supplementary data
Supplementary data are available at IJE online.
Full list of authors:
Gemma C Sharp,1* Rossella Alfano,2,3 Akram Ghantous,4 Jose Urquiza,5,6 Sheryl L Rifas-Shiman,7 Christian M Page,8,9 Jianping Jin,10 Silvia Fernández-Barrés,5,6,11 Gillian Santorelli,12 Gwen Tindula,13 Paul Yousefi,1 Leanne Kupers,1 Carlos Ruiz-Arenas,5,6,11 Vincent WV Jaddoe,14,15 Dawn DeMeo,16,17 Serena Fossati,5,6,11 John Wright,12 Karen Huen,18 Maja Popovic,19 Ellen A Nohr,20,21 George Davey Smith,1 Johanna Lepeule,22 Andrea Baccarelli,23 Maria C Magnus,8 Wenche Nystad,24 Maribel Casas,5,6,11 Emily Oken,7 Siri E Håberg,8 Marina Vafeiadi,25 Theano Roumeliotaki,25 Martine Vrijheid,5,10,11 Monica C Munthe-Kaas,26,27 Brenda Eskenazi,28 Luca Ronfani,29 Nina Holland,13 Leda Chatzi,30 Helle Margrete Meltzer,27 Zdenko Herceg,4 Michelle Plusquin,2,3 Mariona Bustamante,5,6,11 Marie-France Hivert,6,7 Deborah A Lawlor,1,32 Thorkild IA Sørensen,1,33,34 Stephanie J London,35 Janine F Felix14,15 and Caroline L Relton1
1MRC Integrative Epidemiology Unit, Population Health Sciences, Bristol Medical School, University of Bristol, UK, 2Centre for Environmental Sciences, Hasselt University, Diepenbeek, Belgium, 3MRC Centre for Environment and Health School of Public Health Imperial College London, London, UK, 4Epigenetics Group, International Agency for Research on Cancer, Lyon, France, 5ISGlobal, Barcelona, Spain, 6Universitat Pompeu Fabra (UPF), Barcelona, Spain, 7Department of Population Medicine, Harvard Medical School, Harvard Pilgrim Health Care Institute, Boston, MA, USA, 8Centre for Fertility and Health, Norwegian Institute of Public Health, Norway, 9Oslo Centre for Biostatistics and Epidemiology, Oslo University Hospital, Oslo, Norway, 10Westat, Inc, Durham, NC, USA, 11CIBER Epidemiología y Salud Pública (CIBERESP), Madrid, Spain, 12Bradford Institute for Health Research, Bradford, UK, 13Children’s Environmental Health Laboratory, Division of Environmental Health Sciences, School of Public Health, University of California, Berkeley, CA, USA, 14Generation R Study Group, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 15Department of Pediatrics, Erasmus MC, University Medical Center Rotterdam, Rotterdam, The Netherlands, 16Division of Network Medicine, Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA, 17Division of Pulmonary and Critical Care Medicine, Department of Medicine, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA, 18Children’s Environmental Health Laboratory, Division of Environmental Health Sciences, School of Public Health, University of California, Berkeley, CA, USA, 19Cancer Epidemiology Unit, Department of Medical Sciences, University of Turin, Turin, Italy, 20Institute of Clinical Research, University of Southern Denmark, Odense, Denmark, 21Centre of Women's, Family and Child health, University of South-Eastern Norway, Kongsberg, Norway, 22Univ. Grenoble Alpes, Inserm, CNRS, Team of Environmental Epidemiology Applied to Reproduction and Respiratory Health, France, 23Laboratory of Precision Environmental Biosciences, Columbia University Mailman School of Public Health, New York, NY, USA, 24Department of Chronic Diseases and Ageing, Division of Mental and Physical Health, Norwegian Institute of Public Health, Oslo, Norway, 25Department of Social Medicine, Faculty of Medicine, University of Crete, Heraklion, Greece, 26Pediatric Department of Hematology and Oncology, Oslo University Hospital, Norway, 27Division of Infectious Diseases and Environmental Health, Norwegian Institute of Public Health, Norway, 28Center for Environmental Research and Children's Health (CERCH), School of Public Health, University of California, Berkeley, CA, USA, 29Clinical Epidemiology and Public Health Research Unit, Institute for Maternal and Child Health, IRCCS Burlo Garofolo, Italy, 30Department of Preventive Medicine, University of Southern California, Los Angeles, CA, USA, 31Diabetes Unit, Massachusetts General Hospital, Boston, MA, USA, 32National Institute for Health Research Bristol Biomedical Research Centre, Bristol, UK, 33Novo Nordisk Foundation Center for Basic Metabolic Research, Faculty of Medical and Health Sciences, University of Copenhagen, Copenhagen, Denmark, 34Department of Public Health, Section of Epidemiology, Faculty of Medical and Health Sciences, University of Copenhagen, Copenhagen, Denmark and 35Department of Health and Human Services, Research Triangle Park, National Institute of Environmental Health Sciences, National Institutes of Health, NC, USA
Funding
Funding for each cohort and research group are listed in Supplementary Information File 1, available as Supplementary data at IJE online.
Conflict of interest
None declared.
Supplementary Material
Acknowledgements
Acknowledgements for each cohort and research group are listed in Supplementary Information File 1, available as Supplementary data at IJE online. Appropriate ethics approval has been obtained for all participating cohorts and is detailed in Supplementary Information File S1, available as Supplementary data at IJE online. All summary statistics generated by meta-analysis are available at doi: 10.17605/OSF.IO/EBTW7.
References
- 1.Braun JM, Messerlian C, Hauser R.. Fathers matter: why it’s time to consider the impact of paternal environmental exposures on children’s health. Curr Epidemiol Rep 2017;4:46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleming TP, Watkins AJ, Velazquez MA. et al. Origins of lifetime health around the time of conception: causes and consequences. Lancet 2018;391:1842–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharp GC, Lawlor DA.. Paternal impact on the life-course development of obesity and type 2 diabetes in the offspring. Diabetologia 2019;62:1802–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Crean AJ, Bonduriansky R.. What is a paternal effect? Trends Ecol Evol 2014;29:554–59. [DOI] [PubMed] [Google Scholar]
- 5.Rando OJ.Daddy issues: paternal effects on phenotype. Cell 2012;151:702–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Acuna-Hidalgo R, Veltman JA, Hoischen A.. New insights into the generation and role of de novo mutations in health and disease. Genome Biol 2016;17:241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Day J, Savani S, Krempley BD, Nguyen M, Kitlinska JB.. Influence of paternal preconception exposures on their offspring: through epigenetics to phenotype. Am J Stem Cells 2016;5:11–18. [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar M, Kumar K, Jain S, Hassan T, Dada R.. Novel insights into the genetic and epigenetic paternal contribution to the human embryo. Clinics (Sao Paulo) 2013;68:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hammoud SS, Nix DA, Zhang H, Purwar J, Carrell DT, Cairns BR.. Distinctive chromatin in human sperm packages genes for embryo development. Nature 2009;460:473–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seisenberger S, Peat JR, Hore TA, Santos F, Dean W, Reik W.. Reprogramming DNA methylation in the mammalian life cycle: building and breaking epigenetic barriers. Philos Trans R Soc B Biol Sci 2013;368:20110330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitchell M, Bakos HW, Lane M.. Paternal diet-induced obesity impairs embryo development and implantation in the mouse. Fertil Steril 2011;95:1349–53. [DOI] [PubMed] [Google Scholar]
- 12.Ng S-F, Lin RCY, Laybutt DR, Barres R, Owens JA, Morris MJ.. Chronic high-fat diet in fathers programs β-cell dysfunction in female rat offspring. Nature 2010;467:963–66. [DOI] [PubMed] [Google Scholar]
- 13.Oldereid NB, Wennerholm U-B, Pinborg A. et al. The effect of paternal factors on perinatal and paediatric outcomes: a systematic review and meta-analysis. Hum Reprod Update 2018;24:320–89. [DOI] [PubMed] [Google Scholar]
- 14.Soubry A, Schildkraut JM, Murtha A. et al. Paternal obesity is associated with IGF2 hypomethylation in newborns: results from a Newborn Epigenetics Study (NEST) cohort. BMC Med 2013;11:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soubry A, Murphy SK, Wang F. et al. Newborns of obese parents have altered DNA methylation patterns at imprinted genes. Int J Obes 2015;39:650–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soubry A, Guo L, Huang Z. et al. Obesity-related DNA methylation at imprinted genes in human sperm: results from the TIEGER study. Clin Epigenet 2016;8:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Potabattula R, Dittrich M, Böck J. et al. Allele-specific methylation of imprinted genes in fetal cord blood is influenced by cis-acting genetic variants and parental factors. Epigenomics 2018;10:1315–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Donkin I, Versteyhe S, Ingerslev LR. et al. Obesity and bariatric surgery drive epigenetic variation of spermatozoa in humans. Cell Metab 2016;23:369–78. [DOI] [PubMed] [Google Scholar]
- 19.Potabattula R, Dittrich M, Schorsch M. et al. Male obesity effects on sperm and next-generation cord blood DNA methylation. PLoS One 2019;14:e0218615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noor N, Cardenas A, Rifas-Shiman S. et al. Association of periconception paternal body mass index with persistent changes in DNA methylation of offspring in childhood. JAMA Netw Open 2019;2:e1916777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Felix JF, Joubert BR, Baccarelli AA. et al. Cohort profile: pregnancy and childhood epigenetics (PACE) consortium. Int J Epidemiol 2018;47:22–23u. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lawlor DA, Mishra GD.. Family Matters: Designing, Analysing and Understanding Family Based Studies in Life Course Epidemiology. Oxford University Press, New York, 2009.
- 23.Sharp GC, Lawlor DA, Richmond RC. et al. Maternal pre-pregnancy BMI and gestational weight gain, offspring DNA methylation and later offspring adiposity: findings from the Avon Longitudinal Study of Parents and Children. Int J Epidemiol 2015;44:1288–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gemma C, Sookoian S, Alvariñas J. et al. Maternal pregestational BMI is associated with methylation of the PPARGC1A promoter in newborns. Obesity (Silver Spring) 2009;17:1032–39. [DOI] [PubMed] [Google Scholar]
- 25.Morales E, Groom A, Lawlor DA, Relton CL.. DNA methylation signatures in cord blood associated with maternal gestational weight gain: results from the ALSPAC cohort. BMC Res Notes 2014;7:278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharp GC, Salas LA, Monnereau C. et al. Maternal BMI at the start of pregnancy and offspring epigenome-wide DNA methylation: findings from the Pregnancy And Childhood Epigenetics (PACE) consortium. Hum Mol Genet 2017;26:4067–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fraser A, Macdonald-Wallis C, Tilling K. et al. Cohort profile: the Avon Longitudinal Study of Parents and Children: ALSPAC mothers cohort. Int J Epidemiol 2013;42:97–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boyd A, Golding J, Macleod J. et al. Cohort profile: the ‘children of the 90s’: the index offspring of the Avon Longitudinal Study of Parents and Children. Int J Epidemiol 2013;42:111–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Relton CL, Gaunt T, McArdle W. et al. Data resource profile: accessible resource for integrated epigenomic studies (ARIES). Int J Epidemiol 2015;44:1181–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright J, Small N, Raynor P; on behalf of the Born in Bradford Scientific Collaborators Group et al. Cohort Profile: The Born in Bradford multi-ethnic family cohort study. Int J Epidemiol 2013;42:978–91. [DOI] [PubMed] [Google Scholar]
- 31.Eskenazi B, Bradman A, Gladstone E. A, Jaramillo S, Birch K, Holland N.. CHAMACOS, a longitudinal birth cohort study: lessons from the fields. J Child Heal 2003;1:3–27. [Google Scholar]
- 32.Jaddoe VV, Mackenbach JP, Moll HA. et al. The generation R study: design and cohort profile. Eur J Epidemiol 2006;21:475–84. [DOI] [PubMed] [Google Scholar]
- 33.Kooijman MN, Kruithof CJ, Duijn C. V. et al. The generation R study: design and cohort update 2017. Eur J Epidemiol 2016;31:1243–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paternoster L, Evans DM, Nohr EA. et al. Genome-wide population-based association study of extremely overweight young adults—the GOYA study. PLoS One 2011;6:e24303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guxens M, Ballester F, Espada M. et al. Cohort profile: the INMA—INfancia y medio ambiente—(environment and childhood) project. Int J Epidemiol 2012;41:930–40. [DOI] [PubMed] [Google Scholar]
- 36.Magnus P, Irgens LM, Haug K. et al. Cohort profile: the Norwegian mother and child cohort study (MoBa). Int J Epidemiol 2006;35:1146–50. [DOI] [PubMed] [Google Scholar]
- 37.Magnus P, Birke C, Vejrup K. et al. Cohort Profile Update: The Norwegian Mother and Child Cohort Study (MoBa). Int J Epidemiol 2016;45:382–88. [DOI] [PubMed] [Google Scholar]
- 38.Oken E, Baccarelli AA, Gold DR. et al. Cohort profile: project viva. Int J Epidemiol 2015;44:37–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vineis P, Chadeau-Hyam M, Gmuender H. et al. The exposome in practice: design of the EXPOsOMICS project. Int J Hyg Environ Health 2017;220:142–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Farchi S, Forastiere F, Vecchi Brumatti L. et al. Piccolipiù, a multicenter birth cohort in Italy: protocol of the study. BMC Pediatr 2014;14:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chatzi L, Leventakou V, Vafeiadi M. et al. Cohort profile: the mother-child cohort in Crete, Greece (RHEA study). Int J Epidemiol 2017;46:1392–93k. [DOI] [PubMed] [Google Scholar]
- 42.Maitre L, Bont J. D, Casas M. et al. Human Early Life Exposome (HELIX) study: a European population-based exposome cohort. BMJ Open 2019;8:e021311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Heude B, Forhan A, Slama R. et al. Cohort Profile: The EDEN mother-child cohort on the prenatal and early postnatal determinants of child health and development. Int J Epidemiol 2016;45:353–63. [DOI] [PubMed] [Google Scholar]
- 44.Wilcox AJ, Weinberg CR, Basso O.. On the pitfalls of adjusting for gestational age at birth. Am J Epidemiol 2011;174:1062–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leek JT, Storey JD.. Capturing heterogeneity in gene expression studies by surrogate variable analysis. PLoS Genet 2007;3:e161–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Leek JT, Johnson WE, Parker HS, Jaffe AE, Storey JD.. The SVA package for removing batch effects and other unwanted variation in high-throughput experiments. Bioinformatics 2012;28:882–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Houseman EA, Accomando WP, Koestler DC. et al. DNA methylation arrays as surrogate measures of cell mixture distribution. BMC Bioinformatics 2012;13:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bakulski KM, Feinberg JI, Andrews SV. et al. DNA methylation of cord blood cell types: applications for mixed cell birth studies. Epigenetics 2016;11:354–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reinius LE, Acevedo N, Joerink M. et al. Differential DNA methylation in purified human blood cells: implications for cell lineage and studies on disease susceptibility. PLoS One 2012;7:e41361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sharp GC, Arathimos R, Reese SE; The Cohorts for Heart and Aging Research in Genomic Epidemiology plus (CHARGE +) methylation alcohol working group et al. Maternal alcohol consumption and offspring DNA methylation: findings from six general population-based birth cohorts. Epigenomics 2018;10:27–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.GK Smyth. Limma: linear models for microarray data. In: Gentleman R, Carey V, Huber W, Irizarry RA, Dudoit S (eds). Bioinforma Comput Biol Solut Using R Bioconductor. New York: Springer, 2005, pp. 397–420. [Google Scholar]
- 52.Suderman M, Simpkin A, Sharp GC. et al. Sex-associated autosomal DNA methylation differences are wide-spread and stable throughout childhood. bioRxiv 118265. [Google Scholar]
- 53.Perez-Pastor EM, Metcalf BS, Hosking J, Jeffery AN, Voss LD, Wilkin TJ.. Assortative weight gain in mother–daughter and father–son pairs: an emerging source of childhood obesity. Longitudinal study of trios (EarlyBird 43). Int J Obes 2009;33:727–35. [DOI] [PubMed] [Google Scholar]
- 54.Chen Y-P, Xiao X-M, Li J, Reichetzeder C, Wang Z-N, Hocher B.. Paternal body mass index (BMI) is associated with offspring intrauterine growth in a gender dependent manner. PLoS One 2012;7:e36329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lappalainen T, Greally JM.. Associating cellular epigenetic models with human phenotypes. Nat Rev Genet 2017;18:441–51. [DOI] [PubMed] [Google Scholar]
- 56.Viechtbauer W.Conducting meta-analyses in R with the metafor package. J Stat Softw 2010;36:1–48. [Google Scholar]
- 57.Willer CJ, Li Y, Abecasis GR.. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 2010;26:2190–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen Y, Lemire M, Choufani S. et al. Discovery of cross-reactive probes and polymorphic CpGs in the Illumina Infinium HumanMethylation450 microarray. Epigenetics 2013;8:203–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kovalchik S, RISmed: Download content from NCBI Databases. 2017.
- 60.Tang W, Ho S.. Epigenetic reprogramming and imprinting in origins of disease. Rev Endocr Metab Disord 2007;8:173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Romero-Corral A, Somers VK, Sierra-Johnson J. et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int J Obes 2008;32:959–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sørensen TIA, Virtue S, Vidal-Puig A.. Obesity as a clinical and public health problem: Is there a need for a new definition based on lipotoxicity effects? Biochim Biophys Acta 2010;1801:400–04. [DOI] [PubMed] [Google Scholar]
- 63.Lawlor DA, Relton C, Sattar N, Nelson SM.. Maternal adiposity—a determinant of perinatal and offspring outcomes? Nat Rev Endocrinol 2014;8:679–88. [DOI] [PubMed] [Google Scholar]
- 64.Chooi YC, Ding C, Magkos F.. The epidemiology of obesity. Metabolism 2019;92:6–10. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.