Abstract
During the COVID-19 pandemic, exposure to COVID-related stimuli, has been enormous. Exposure to threat-related stimuli, can have a significant impact on people's wellbeing particularly in relation to COVID-related anxiety. The present research comprises two empirical studies. In Study 1, a newly developed Emotional Stroop Task (EST) and an Image Rating Task (IRT) were used to assess, automatic and non-automatic affective responses to COVID-related words and images during the first wave of the pandemic in the UK general population. In Study 2, the same tasks were used to evaluate the affective responses of University students during the second wave of the pandemic. Additionally, loneliness and pro-social behaviours were explored in relation COVID-related anxiety in the same population. Overall, the results showed that automatic affective responses as measured by interference effects on the EST, remained unaffected during the pandemic. However, non-automatic affective responses to COVID-related images measured by the IRT, indicated that participants rated these images as more fearful sadder and higher in anger, compared to non-COVID negative images matched for arousal and negativity and this was more evident in people with high COVID-anxiety. Trait anxiety was related to higher levels of loneliness, more prosocial behaviour and higher intentions to help others, while COVID-related anxiety mediated these effects, suggesting that for high levels of trait anxiety, participants were more likely to have helped someone in need during the pandemic when their COVID-anxiety levels were low.
Keywords: COVID-19, Anxiety, Affective responses, Loneliness, Emotional Stroop task, Image rating task, Pro-social behaviours
1. Introduction
The COVID-19 pandemic has had an unprecedented effect on everyday life and functioning, across the world (Pišot et al., 2020). Since the first trimester of 2020 increasingly more countries implemented nation-wide lockdowns and other restrictive and social distancing measures in order to protect national health systems from being overwhelmed by the increased need for medical care and treatment of COVID-19 patients (Davies et al., 2020). The pandemic has also had an unprecedented impact on mental health, manifested in increased prevalence of psychological distress, anxiety, and depressive symptoms (Vindegaard and Benros, 2020). A longitudinal study in Spain found that the prevalence of stress, anxiety, and depression symptoms were significantly increased between March and May 2020, with more than 33% of participants reporting more frequent mental health symptoms. Traumatic stress, as measured by the Impact of Event Scale (IES; Horowitz et al., 1979), was relatively stable between the two measures, but still relatively high with almost half of the participants (48.3%) self-reporting traumatic stress in response to the lockdown confinement (Planchuelo-Gómez et al., 2020). A meta-analysis of research in the general population further showed that the pooled prevalence of psychological distress and post-traumatic stress was respectively 23.8% and 24.8% (Cooke et al., 2020). Lastly, two independent meta-analyses reported that the pooled prevalence of depression symptoms was between 22% (Arora et al., 2020) and 25% in the general population (Bueno-Notivol et al., 2021). The president of the Royal College of Psychiatrists in the UK further declared that the COVID-19 pandemic poses the greatest challenge to mental health since World War II, and the World Health Organisation (2020) has recognized that affective responses to COVID-19, as well as lack of physical contact and changes in work-life balance will further exacerbate the mental health fallout of the pandemic in the coming years.
2. Affective responses to COVID-related stimuli
Since the beginning of the first wave of the COVID-19 pandemic, exposure to COVID-19 stimuli has been enormous, with images and words appearing daily on printed and online news, and in social media (Gao et al., 2020). Worldwide, people developed a new verbal vocabulary around COVID-19 (neologism or "COVID-speak"), and phrases that were previously considered emotionally neutral, were given new meaning and sentiment (e.g., sanitising, social distancing). The negative connotations of COVID-related words and images mainly associated with fear of viral exposure and death, have become part of everyday communication. However, exposure to such stimuli can cause significant deterioration to mental health as they act as signals of threat and fear (Brooks et al., 2020). Indeed, related research has indicated that more frequent exposure to COVID-19-related information in the media was significantly associated with poor mental health outcomes (Petzold et al., 2020; Xiong et al., 2020). In the anxiety literature, threat-relevant stimuli become automatized and, therefore, are attended to faster than non-threatening information (Yiend and Matthews, 2001). This attentional bias can cause the maintenance and relapse of anxiety, and lead to mental health difficulties over time.
Emotional Stroop Tasks are used to determine attentional biases to emotionally salient information by identifying interference effects to threat-related information (Williams et al., 1996). Similarly to a standard Stroop task, participants who complete the Emotional Stroop are asked to name the ink colour of words presented to them in different colours (blue, red, yellow and green). The presented words that have negative valence tend to “slow” down response times in clinical and non-clinical populations compared to neutral words (Yiend, 2010). This interference effect is taken as indication for an attentional bias suggesting a sensitivity towards environmental stimuli that are related to their concern (Williams et al., 1996; Yiend, 2010). Such hypervigilance to threatening stimuli that signal potential danger are central to many theoretical models explaining the cause of anxiety disorders (Bar-Haim et al., 2007) and depression (Epp et al., 2012; Nolen-Hoeksema et al., 1993). Moreover, attentional bias to threatening stimuli is key to maintaining and increasing the symptomatology of these disorders, by creating a vicious cycle whereby hypervigilance increases attentional biases, which, in turn, feeds into increased hypervigilance. Therefore, it is theoretically plausible that people with COVID anxiety (compared to those without COVID anxiety) will show more interference to COVID-related words compared to negative and neutral words in an Emotional Stroop task.
Image rating tasks have been widely used in understanding emotional experiences. Early theories suggested that emotional responses originate from discrete basic emotions (anger, fear, sadness, disgust, and happiness) that can be used as indicators of affective states (e.g., Tomkins, 1962; Ekman, 1992). Moreover, there are unique physiological, neural and psychological outcomes that accompany each emotion including autonomic responses and facial expressions (Colibazzi et al., 2010). Due to a number of notable limitations of discrete models of emotions (Mauss and Robinson, 2009), there has been a shift in attention to dimensional models of affect, which suggest that all emotions are a combination of at least two main dimensions: valence and arousal (e.g., Posner et al., 2005). Emotional experiences and emotional labelling are the result of a cognitive appraisal of valence and arousal both subserved by independent neural pathways (Colibazzi et al., 2010) Valence refers to the degree to which the elicited emotion is pleasant (or unpleasant) and arousal refers to the level of neurophysiological activation (responsiveness) of a person to an emotional stimulus (e.g., Kandel et al., 2000).
Investigating affective experiences and responses to COVID-19 stimuli can help in better understanding, and subsequently tackling, the mental health effects of the pandemic on the population. So far, only a handful of studies have examined affective responses and experiences to the pandemic. A Slovenian study found that more females than males self-reported greater anxiety and ruminative thinking over COVID-19, and both males and females expressed higher fear of contamination and perceived severity of COVID-19 after the first positive case was diagnosed in the country (Lep et al., 2020). A survey-based study that recorded emotional responses to the pandemic daily over 5 weeks, demonstrated that Serbian adults self-reported gradually less worry, fear of being contaminated, and anger, and that worry and fear were significantly associated with more time spent on attending to media news about the pandemic (Sadiković et al., 2020). Similarly, an experimental study showed that participants self-reported more negative emotions after they were exposed to COVID-19 pandemic information, as compared to participants who attended to non-epidemic stimuli (Wang et al., 2021; Office for National Statistics, 2020a; Office for National Statistics, 2020b).
3. The present research
So far, research on the emotional responses to COVID-related information has used self-reported measures of emotions. Also, the stimuli used to elicit emotional responses varied from general questions about feelings of fear, anger, and worry during the day (Sadiković et al., 2020), to more focused questions that addressed fear of COVID-19 contamination (e.g., Lep et al., 2020). The present research comprises two empirical studies. In Study 1, we used EST and IRT to assess, for the first time in the extant literature, automatic and non-automatic affective responses to COVID-related words and images. Study 1 was conducted in the general population in the UK during the first wave of the pandemic, between May and June 2020. According to the Office for National Statistics (report released on June 23rd 2020), by this time, there had been 43.763 deaths registered with COVID-19 as the underlying cause of death - on of the highest death tolls in Europe. Our second study was concerned with replicating the findings from Study 1 to the University student population between October and November 2020. At that time, the second wave of COVID-19 had been recorded in the UK, and the Office for National Statistics (report released on December 9th 2020) had reported significant increase in mental health symptoms, and reduced psychological well-being among University students.
For Study 1, it was hypothesized that people with COVID anxiety would show more interference on the Emotional Stroop Task, to COVID-related words, compared to neutral and negative words matched for valence and arousal, indicating greater attentional bias to COVID stimuli (Hypothesis 1). Our second hypothesis was that COVID-related images would be rated higher on negative emotions (fear, anger, sadness, and disgust), arousal and negativity, compared to neutral and negative images matched for arousal and valence (Hypothesis 2). Finally, we hypothesized that individuals with COVID anxiety would rate COVID-related images higher on negative emotions (fear, anger, sadness, and disgust), arousal and negativity, compared to those without COVID anxiety (Hypothesis 3).
4. Method
4.1. Participants
An initial sample of 107 participants living in the UK during the first wave of the pandemic (data collected in May-June 2020), were recruited through Prolific (www.prolific.co) and personal contacts. Six participants were rejected due missing values leaving a final sample of 101 participants all of which were financially compensated for their participation. The mean age of the participants was 29.1years (SD=9.25, Range 18-53 years), and 66 were females and 35 males. The only exclusion criteria were being ≥18 years old and not being colour blind, due to the Stroop task demands.
4.2. Measures
4.2.1. State anxiety inventory for adults - short form (STAIAD-Y1) Spielberger et al. (1968)
State anxiety was measured using the STAIAD-Y1, which asks individuals to report how they were feeling at that moment, in response to each of 10 statements on the scale from 1 (not at all) to 4 (very much so). Items are scored on a continuous scale, with higher scores indicating higher anxiety. Items 1, 3, 8 and 10 are reverse scored.
4.2.2. Coronavirus anxiety scale (CAS)
This 5-item scale was developed to identify cases of dysfunctional anxiety associated with the COVID-19 crisis (Lee, 2020). These five items assess whether someone has experienced COVID anxiety physical symptoms (such as, feeling dizzy, having trouble sleeping, feeling paralyzed, nauseous) over the past 2 weeks on a 5-point scale (0 = not at all, 4 = nearly every day over the last 2 weeks). For the purposes of subsequent analysis, we created two anxiety groups, based on their responses on the CAS. The non-anxious group (N=50) reported not having experienced any of these physical symptoms of CAS two weeks prior to data collection, while the COVID anxious group (N=51) had experienced at least one of CAS symptoms, on at least one or two days, two weeks prior to data collection.
4.2.3. Emotional Stroop task
An initial sample of 27 words deemed to be COVID-19 related were generated by the experimenters from various sources (e.g., online news, websites etc.). The selected words were matched as closely as possible to a sample of 27 neutral words selected from the ANEW database (Bradley and Lang, 1999), identical in word length and syllable count to ensure similar processing speed (Kucera and Francis, 1967).
A pilot study was carried out (n = 18) to determine the relatedness, arousal, negativity, and positivity scores of the COVID-related and neutral words using a sliding bar ranging from 0-100. A final set of 12 COVID-related words were selected on the bases of scores being higher on relatedness, arousal, negativity. These were then matched with 12 non-COVID negative words from ANEW database (Bradley and Lang, 1999) with similar word length and syllable structure. All words except ‘coronavirus’ had related matches in the ANEW database. Examples of the words are provided in the appendix A. Each of the 36 words were shown in red, blue, green and yellow font giving a total of 144 experimental trials. Words were displayed at the centre of a black screen at 10% height of the participant's display for 1500ms.
4.2.4. Image rating task
Twenty-five COVID-related images were initially selected by the experimenters from various resources (e.g., news, online websites) that commonly appeared in the media in the UK. Before commencing the main study, we run a pilot study with 18 independent participants that were not included in the main study, who were asked to rate COVID-related images on COVID relatedness, arousal and negativity using sliding bars from 0 – 100 (low to high). Their ratings were put in rank order, to determine the 12 images that were rated highest on COVID relatedness, arousal, and negativity. These final set of COVID images, were matched for arousal and valence to a set of non-COVID negative images selected from the International Affective Picture System (IAPS) and a sample of neutral images (see Itkes et al., 2017). This yielded a final sample of 36 images with 12 in each category (COVID-related, non-COVID negative and neutral images). Images were either landscape or portrait in orientation and either 528 × 400 or 530 × 700 pixels, respectively. Images were hosted on Qualtrics, each on a separate page with 6 sliding bars under each image (arousal, negativity, fear, sadness, disgust, anger). Sample of these images are presented in appendix A.
4.3. Procedure
Participants completed all tasks online using their own home computers. A single URL web link was generated, that directed participants to each part of the study and the sole requirement was to have Google Chrome browser installed in their PCs. The information form, consent form, questionnaires, image rating task, and debrief were hosted online using Qualtrics (Qualtrics, Provo, UT). The Stroop task was created using PsychoPy v2020.1 (Peirce et al., 2019), and hosted online via Pavlovia.
An introductory page contained the information sheet, explaining the nature of the study, the online consent form to be signed, spaces to provide participant I.D. and demographic information (age and gender). They were then directed to the emotional Stroop task hosted on Pavlovia. Once they completed the task, they were automatically redirected to Qualtrics to complete the image rating task. Participants could withdraw from the study at any point, in which case they were automatically redirected to a URL containing a debrief for the study. The study was approved by the University's ethics committee (Ethics approval number ER24008402).
4.3.1. COVID-19 emotional Stroop task
The Stroop task began with a dialog box for entry of the participant's identification code, followed by instructions for the task. Participants were told they would see words on the screen in either red, blue, green, or yellow ink and should identify the colour by responding with either the left, down, right, or up arrow keys, respectively. Before the first practice trial began, participants were reminded of how to answer and encouraged to respond as quickly as possible. The first practice trial block consisted of 8 trials, with 4 different words written in either red or blue ink, and a fixation cross presented before each word for 1000ms. A feedback command prompted if responses were correct or incorrect. The second practice block was identical to the first, however now words could now appear in green or yellow too for a total of 16 trials. The final practice block was identical to the second, however with the feedback prompt now removed.
Before the experimental trials, participants were reminded again of how to respond and encouraged to respond as quickly as possible. The experimental block consisted of 144 trials of 36 words randomly presented in 4 different colours (red, blue, green and yellow) for 1500ms, or until the participant had responded. When the trial ended, the word disappeared and a random inter-trial iteration jitter of 300 – 600ms preceded the beginning of the next trial to reduce task adaptation (Compton et al., 2011). Participants could withdraw at any time by pressing an ‘X’ at the top of the screen or closing their browser. To avoid issues of participants forgetting instructions, a reminder appeared after the 48th and 96th trials. On completion of the final trial, participants were instructed to press the spacebar to move onto the image rating task.
4.3.2. Image rating task
Participants were required to provide their Prolific participant I.D. before beginning the task. Participants were provided instructions and were required to use sliding bars from 0 – 100 (low to high) to report their responses to each of the images on measures of arousal, valence (negativity), fear, disgust, sadness, and anger. There was no set time limit for this task, and participants were given the option to show/hide the image while they were rating it, in case they found it distressing. A total of 36 randomly presented images (12 COVID-related, 12 neutral and 12 non-COVID negative) were presented individually, with instructions at the top of the page to remind participants of how to rate them. Specifically, participants were given the following instructions for each rating dimension:
-
Arousal - An image that is highly arousing would induce more intense emotions. 0 = calm (low arousal), 100 = intense emotion (high arousal)
Negativity - How negative the image is. 0 = neutral (not at all negative), 100 = very negative
Fear - How fearful the image makes you feel. 0 = not at all fearful, 100 = extremely fearful
Disgust - How disgusted the image makes you feel. 0 = not at all disgusted, 100 = extremely disgusted
Sadness - How sad the image makes you feel. 0 = not at all sad, 100 = extremely sad
Anger - How angry the image makes you feel. 0 = not at all angry, 100 = extremely angry
Participants used a right arrow to go to the next image. They could withdraw from the task at any point by clicking the withdraw button at the bottom of the screen. On completion of the image rating task, participants were directed to a debrief form with information about the study.
5. Results
All data were analysed in SPSS v. 26 (IBM Corp., Armonk, NT, USA). We used generalized eta squared (η 2 G) as an effect size indicator, commonly used for repeated measures designs, with the following conventions: small =.01, medium=.06 and large=.14 effect sizes (Olejnik and Algina, 2003).
No significant gender differences were observed in any study variables, except for COVID-related anxiety (CAS) were females (M=2.50, SD=3.41) reported significantly higher CAS scores than males (M=0.91, SD=1.79), t(98)=2.53, p=.013). There was also a significant difference on state anxiety between the COVID anxious (M=20.24, SD=6.64) and the non-anxious (M=16.47, SD=5.68) group t(99)=3.065, p=.003. Pearson's correlation coefficient between COVID-anxiety and state anxiety was r= .30, p=.003. Correlation coefficients between COVID-anxiety scores and outcome measures from both tasks are presented in Table 1 .
Table 1.
Correlational analyses study 1.
| Stroop RT (COVID Words) | Stroop accuracy % (COVID words) | Arousal (COVID images) | Negativity (COVID images) | Fear (COVID images) | Disgust (COVID images) | Sadness (COVID images) | Anger (COVID images) | STAI State Anxiety | COVID anxiety scale | |
|---|---|---|---|---|---|---|---|---|---|---|
| Stroop RT (COVID Words) | — | |||||||||
| Stroop accuracy % (COVID words) | -0.114 | — | ||||||||
| Arousal (COVID images) | -0.198* | -0.058 | — | |||||||
| Negativity (COVID images) | -0.142 | 0.035 | 0.541*** | — | ||||||
| Fear (COVID images) | -0.093 | 0.003 | 0.320** | 0.636*** | — | |||||
| Disgust (COVID images) | -0.034 | -0.061 | 0.402*** | 0.551*** | 0.642*** | — | ||||
| Sadness (COVID images) | -0.017 | 0.014 | 0.276** | 0.554*** | 0.726*** | 0.446*** | — | |||
| Anger (COVID images) | -0.038 | -0.004 | 0.342*** | 0.512*** | 0.695*** | 0.790*** | 0.582*** | — | ||
| STAI State Anxiety | 0.025 | -0.080 | 0.103 | 0.236* | 0.359*** | 0.235* | 0.162 | 0.286** | — | |
| COVID anxiety scale | 0.129 | -0.020 | 0.100 | 0.142 | 0.407*** | 0.274** | 0.242* | 0.312** | 0.297** | — |
Note. * p < .05, ** p < .01, *** p < .001.
In addition to bivariate correlation we conducted partial correlation analysis with Variance Reduction Rate or VRR which is estimated by the formula: (zero-order correlation)2 – (partial correlation)2/(zero-order correlation)2. The VRR is an analytic method that allows us to examine how much of the variance shared between COVID-anxiety and scores in the Emotional Stroop and IRT can be attributed to state anxiety. The VRR has been widely used to assess such confounding or nuisance effects in previous research (e.g., Barkoukis et al., 2014; Chen and Spector, 1991; Lazuras et al., 2009; Lazuras et al., 2010).
In the present study we used VRR to assess the confounding effect of state anxiety on the significant associations between COVID-anxiety and IRT scores, but not between COVID-anxiety and Emotional Stroop scores, because they were non-significant. The observed zero-order correlations (r) ranged between .24 and .41 (see Table 1), and they did not change significantly after controlling for state anxiety, with observed partial correlations (r) ranging between .20 to .33. The VRR results further showed that state anxiety accounted for: 31.5% in the association between COVID-anxiety and fear ratings; 36% in the association between COVID-anxiety and disgust ratings; 27.5% in the association between COVID-anxiety and sadness ratings; and 37.1% in the association between COVID-anxiety and anger ratings.
The first hypothesis was examined using two 2 × 3 repeated measures ANCOVAs to determine differences between COVID anxious and non-anxious participants on reaction times (RTs) and accuracy (% of correct responses) to COVID, negative, and neutral words after controlling for the effects of state anxiety. There were no significant main effects or interactions for RTs and accuracy. Means and standard deviations are presented in Table 2 .
Table 2.
Descriptive statistics displaying Means and SDs for Study 1 Stroop task separated by anxiety groups.
| Groups | Covid words (RTs) | Covid words Accuracy (%) | Negative words (RTs) | Negative words Accuracy (%) | Neutral words (RTs) | Neutral words Accuracy (%) |
|---|---|---|---|---|---|---|
| Covid-Anxious | 0.73 (0.08) | 90.08 (8.67) | 0.74 (0.08) | 90.25 (9.16) | 0.73 (0.08) | 91.21 (8.30) |
| Non-anxious | 0.73 (0.08) | 91.34 (7.36) | 0.72 (0.07) | 90.44 (7.57) | 0.73 (0.06) | 90.81 (8.94) |
For the second hypothesis one-way repeated measures ANOVAs were used to calculate differences in the ratings of COVID related, negative and neutral images on arousal [F(2,200)=73.70, p<.001, η 2 G=.15], negativity [F(2,200) = 211.00, p < .001, η 2 G = .46], fear [F(2,200) = 137.01, p < .001, η 2 G = .34], disgust [F(2,200) = 220.01, p < .001, η 2 G = .49], sadness [F(2,200) = 443.00, p < .001, η 2 G = .65] and anger [F(2,200) = 129.00, p <.001, η 2 G = .36]. Post-hoc analyses using Bonferroni indicated significant differences on arousal between COVID and neutral t (200) = 10.92, p < .001, and between negative and neutral t (200) = 10.04, p <.001. There were no differences on arousal between COVID-related and negative images. Similarly, post-hoc analyses using Bonferroni corrections indicated significant differences on negativity between COVID and neutral t(200) = 16.83, p < .001, and between negative and neutral t(200) = 18.59, p < .001. There were no differences on negativity between COVID-related and negative images. Post hoc analyses for fear, disgust sadness and anger were all statistically significant and are depicted in Table 3 .
Table 3.
Post-hoc analyses using the Bonferroni correction displaying mean differences between emotional ratings for each image category.
| Within Group Comparisons |
||||
|---|---|---|---|---|
| Emotion Rating | Image Pairs | Mean Difference | SE | t |
| Fear | Covid – Negative | 9.50 | 2.16 | 4.40* |
| Covid – Neutral | 34.50 | 2.16 | 16.00* | |
| Negative – Neutral | 25.00 | 2.16 | 11.60* | |
| Disgust | Covid – Negative | - 26.07 | 1.97 | - 13.27* |
| Covid – Neutral | 14.59 | 1.97 | 7.43* | |
| Negative – Neutral | 40.66 | 1.97 | 20.69* | |
| Sadness | Covid – Negative | 20.32 | 1.95 | 10.40* |
| Covid – Neutral | 57.39 | 1.95 | 29.36* | |
| Negative – Neutral | 37.07 | 1.95 | 18.96* | |
| Anger | Covid – Negative | - 9.17 | 2.01 | - 4.55* |
| Covid – Neutral | 22.25 | 2.01 | 11.05* | |
| Negative – Neutral | 31.42 | 2.01 | 15.60* | |
Note: t-statistics marked with * denote a significance level of pBonferroni=<0.001.
To explore the third hypothesis 2 × 3 repeated measures ANCOVAs (group: COVID anxious vs non-anxious, image type: COVID, negative, neutral) with state anxiety as a covariate, were used to determine differences between COVID anxious and non-anxious on arousal, negativity, fear, disgust, sadness, and anger (DVs). Means and SDs are presented in Table 4 .
Table 4.
Means and SDs for each image type (COVID, negative and neutral), on the 4 negative emotions (fear, disgust, sadness and anger) for each anxiety group (COVID-anxious, Non-anxious).
| COVID-anxious |
Non-anxious |
||||
|---|---|---|---|---|---|
| Emotion Rating | Image Type | Mean (SD) | Emotion Rating | Image Type | Mean (SD) |
| Fear | Covid-related | 46.83 (27.79) | Fear | Covid-related | 27.24 (25.13) |
| Negative | 31.51 (21.16) | Negative | 23.45 (19.31) | ||
| Neutral | 3.55 (4.41) | Neutral | 1.35 (1.93) | ||
| Disgust | Covid-related | 20.59 (24.15) | Disgust | Covid-related | 12.30 (14.99) |
| Negative | 43.06 (21.52) | Negative | 41.91 (21.32) | ||
| Neutral | 2.55 (3.80) | Neutral | 1.09 (1.67) | ||
| Sadness | Covid-related | 65.71 (24.40) | Sadness | Covid-related | 55.90 (26.30) |
| Negative | 42.79 (14.48) | Negative | 38.13 (14.65) | ||
| Neutral | 4.20 (4.07) | Neutral | 2.56 (2.69) | ||
| Anger | Covid-related | 31.69 (25.18) | Anger | Covid-related | 17.54 (20.16) |
| Negative | 36.24 (17.33) | Negative | 31.25 (19.73) | ||
| Neutral | 3.26 (4.74) | Neutral | 1.35 (2.00) | ||
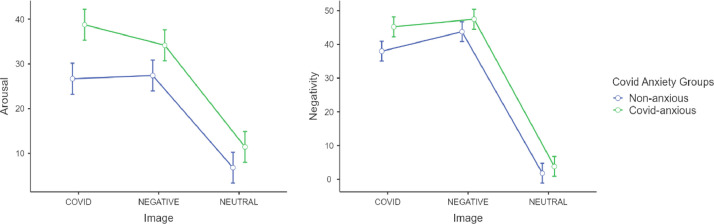
Results showed a significant main effect of image type on arousal [F(2,196) = 4.91, p < .01, η 2 G = .08], and negativity, [F(2,196) = 15.32, p < .01, η 2 G = .13] while controlling for the effects of state anxiety (p > .05). Post hoc analyses for these main effects were previously reported in the analyses for the first hypothesis. There was no significant main effect of group or a significant interaction for arousal and negativity (Fig. 1 ).
Fig. 1.
Differences on ratings of arousal and negativity between the two groups.
Note: This figure illustrates estimated marginal means for arousal and negativity (DVs) in each group (COVID-anxious, non-anxious).
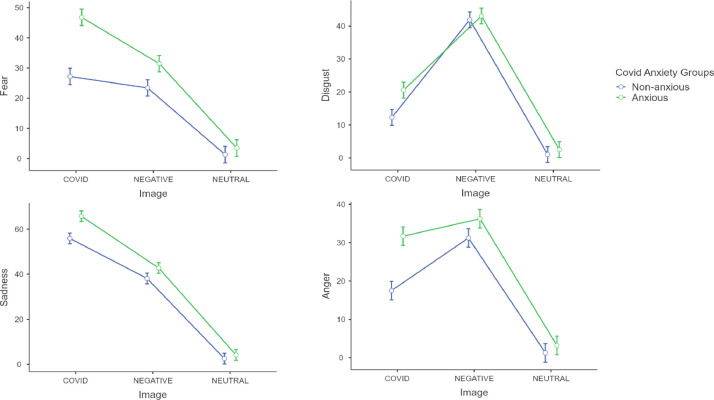
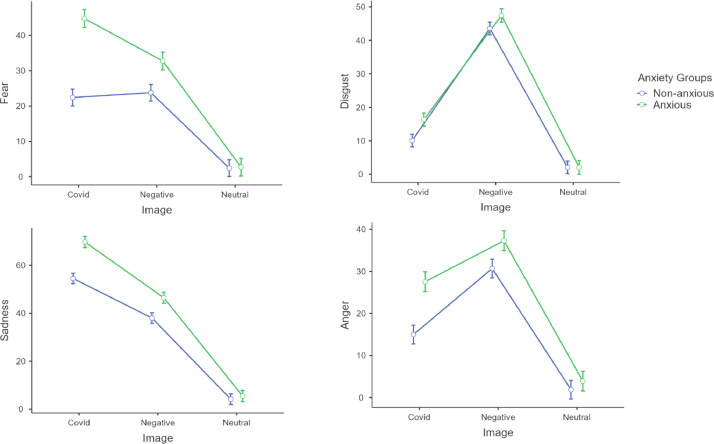
There was a significant main effect of image type on Fear [F(2,198) = 3.43, p < .05, η 2 G = .03], a significant main effect of Group [F(1,98) = 5.92, p = .01, η 2 G = .05] and a significant interaction [F(2,198) = 7.11, p< .01, η 2 G = .06]. State anxiety was a significant covariate [F(1,98) = 7.93, p < .01, η 2 G = .07]. Post hoc analyses using Bonferroni showed that COVID anxious participants rated COVID images as significantly more fearful compared to non-anxious individuals and more fearful than non-COVID negative images matched for arousal (Fig. 2 ). There was a significant main effect of image type on Disgust [F(2,198) = 15.35, p < .001, η 2 G = .13] with non-COVID negative images being rated higher on disgust compared to COVID images and neutral images in both groups (Fig. 2). State anxiety was a significant covariate [F(1,98) = 4.92, p = .02, η 2 G = .04]. Our results showed a significant main effect of image type on Sadness [F(2,198) = 35.40, p < .001, η 2 G = .26] while controlling for the effects of state anxiety (p > .05). Post hoc analyses using Bonferroni indicated that COVID images were rated significantly higher in sadness compared to non-COVID images matched for negativity in both groups (Fig. 2). Finally, there was a significant main effect of image type on Anger [F(2,198) = 11.41, p < .001, η 2 G = .10], a significant main effect of group [F(1,99) = 4.32, p < .05, η 2 G = .04] and a significant interaction [F(2,198) = 3.13, p < .05, η 2 G = .03]. State anxiety was a significant covariate [F(1,98) = 4.44, p < .05, η 2 G = .04]. Post hoc analyses indicated that COVID anxious participants rated COVID images significantly higher on anger compared to non-anxious participants (Fig. 2).
Fig. 2.
Differences on ratings of fear, disgust, sadness and anger between the two groups.
Note: This figure illustrates estimated marginal means for fear, disgust, sadness and anger (DVs) in each group (COVID-anxious, non-anxious).
6. Study 1 discussion
The findings from Study 1 were not supportive of the first hypothesis, as we did not find greater interference (attentional bias) for COVID-related words compared to neutral and negative words in COVID anxious individuals. In accordance with the second hypothesis, participants displayed higher arousal and negativity, and gave higher ratings on sadness, fear, and anger when exposed to COVID-19 images, compared to neutral images and images that have been standardized for eliciting negative affect in previous research (see Itkes et al., 2017). Finally, the third hypothesis of the study was supported with participants classified in COVID anxiety group (i.e., who had experienced anxiety over COVID two weeks prior to the study) gave higher scores on negative affect (fear and anger) to COVID-related images compared to the non-anxious group. However, in state anxiety was a significant covariate in both of these emotional ratings, suggesting that this effect may be due to ongoing levels of anxiety rather than COVID-specific anxiety. Past research has indicated that greater negative emotional reactivity, as indicated by higher scores in IAPS ratings of valence and arousal, is a risk factor for anxiety disorders (Carthy et al., 2010; Claus et al., 2020; Fox et al., 2010). In the present study we did not control for pre-existing mental health conditions, so we cannot be certain if the observed effects could be attributed to anxiety disorders. However, we did control for the potential confounding (nuisance) effect of state anxiety scores and the VRR analysis indicated that between 27.5% to 37.1% of the variance in the observed bivariate associations between COVID-anxiety and IRT scores were attributed to state anxiety levels. This suggests that a large amount of the association between COVID-anxiety and scores in the IRT can be largely explained by individual differences in COVID-related anxiety and not by general state anxiety scores. Lastly, our results indicated that participants did not differ in their affective responses to visual stimuli with respect to disgust. Although disgust serves to protect the organism from potential exposure to pathogens, such as bacteria, viruses, and/or other pathogens (Curtis et al., 2004), our findings suggest that participants evaluated COVID-related stimuli as more fearful, sad, and aggressive than disgusting.
7. Study 2
7.1. Affective responses to COVID-19 stimuli and loneliness in university students
Social distancing measures, reduced mobility, social isolation when one is experiencing flu or COVID-19 symptoms, and lack of physical contact with family, friends, and meaningful others can help in reducing the spread of COVID-19 in the community, but also contributed to increased feelings of loneliness (Killgore et al., 2020; van Tilburg et al., 2020; Shah et al., 2020) - a known risk factor for broad-based morbidity and mortality (Cacioppo and Cacioppo, 2018; Cacioppo and Hawkley, 2003). Furthermore, within the context of the COVID-19 pandemic, loneliness has been associated with higher symptoms of both depression and anxiety during the first wave of the COVID-19 pandemic in the UK (Li and Wang, 2020), and other countries (e.g., Gaeta and Brydges, 2020; Killgore et al., 2020; Palgi et al., 2020). Importantly, young adults are at higher risk for experiencing loneliness and associated mental health problems during the COVID-19 pandemic (Bu et al., 2020; Lee et al., 2020).
University students are young adults, and research has shown that the levels of loneliness, mental health problems, and suicidality were higher in this group as compared to the general population in the pre-pandemic era (Akram et al., 2020; Ibrahim et al., 2013). Data from the UK Office for National Statistics also indicated that, as of November 2020, University students in the UK reported higher anxiety scores than the general population, and more than half experienced mental health deterioration. Research in other countries has also shown that University students experienced higher levels of anxiety and stress in response to COVID-19 restriction measures (Husky et al., 2020); more sleep problems and insomnia symptoms than other social groups (Marelli et al., 2020); and that negative affect, such as fear, was significantly associated with PTSD symptoms and depression (Tang et al., 2020; Zolotov et al., 2020).
Study 2 was conducted to replicate the findings of Study 1 and further extend research on the psychological responses of University students to the COVID-19 stimuli. In the absence of interference effects to COVID-related words on the Stroop task in Study 1, we examined if prolonged exposure to COVID-related words (during the second UK lockdown) established an attentional bias, which may be linked to COVID-related anxiety and/or Trait anxiety. Therefore, Study 2 examined if University students with higher COVID anxiety showed attentional bias to COVID-related words, compared to negative words and neutral words in the Emotional Stroop Task, after controlling for the effects of Trait anxiety (Hypothesis 1). Also, we investigated if high and low COVID-anxiety groups, differentially rated the valence, arousal, and negative emotions (fear, disgust, sadness, and anger) in response to COVID-related images, after controlling for the effects of trait anxiety (Hypothesis 2).
Lastly, we further extended the findings of Study 1 in two important ways. Firstly, we examined if students with higher levels of COVID anxiety also displayed higher levels of loneliness (Hypothesis 3). This effect has been observed in the general population (e.g., Gaeta and Brydges, 2020; Killgore et al., 2020; Palgi et al., 2020) but not yet examined extensively among University students. Finally, we explored whether higher levels of COVID anxiety differentiated prosocial behaviour and willingness to engage in prosocial behaviours in University students (Hypothesis 4). Previous research has shown that prosocial behaviour (e.g., helping people in need, following social welfare norms or regulations) can be motivated both by positive affect, as well as by the experience of negative affect, such as psychological distress (Bailey et al., 2019). This type of "pressure-based" prosocial motivation (and subsequent actual prosocial behaviour) serves as a buffer that alleviates the experienced distress (Gebauer et al., 2008). In addition to its theoretical relevance, Hypothesis 4 has an applied dimension because it will show whether COVID anxiety facilitates or hampers willingness to reach out to help others in need during the pandemic, and to follow social distancing rules and other safety measures.
8. Methods
8.1. Participants
An initial sample of 154 University students living in the UK during the second wave of the pandemic (data collected in October-November 2020), were recruited. Twelve participants were not included in the analysis due to incomplete data sets, leaving a final sample of 142 participants all of which were participated for course credits. The mean age of the participants was 20.7 years (SD=4.76), the majority of which were females (88%). The only exclusion criteria were being ≥18 years old and not being colour blind, due to the Stroop task demands.
8.2. Measures
The measures and tasks for Study 2 were identical to Study 1, with the addition of two new scales that investigated loneliness and prosocial motivation during the COVID-19 pandemic. In this study, we also included a measure of Trait Anxiety (rather than state anxiety).
8.3. Trait anxiety inventory for adults - short form (STAIAD-Y1) Spielberger et al. (1968)
Trait Anxiety was measured using a 10-item instrument which asks individuals to report how they feel in response to each of the 10 statements on a scale of 1 (almost never) to 4 (almost always). The scale measures trait anxiety, so participants are asked to circle the appropriate number to indicate how they generally feel. Items are scored on a continuous scale, with higher scores indicating higher anxiety. Items 1, 3, 8 and 10 are reverse scored.
8.4. UCLA loneliness scale version 3 (UCLA-3)
A 20-item scale intended to determine an individual's feelings of social isolation and loneliness. Items are scored on a scale from 1 (never) to 4 (often), with higher scores indicating higher subjective loneliness (Russell, 1996). Items 1, 5, 6, 9, 10, 15, 16, 19 and 20 are reverse scored.
8.5. COVID-19 pro-social behaviour questionnaire
A 12-item checklist of pro-social behaviour during the pandemic was developed for the purposes of the present study, to investigate whether participants engaged in pro-social behaviours during the first lockdown and their willingness to engage in pro-social behaviours in the future, in the case of another national lockdown . The 12 prosocial behaviours were selected using the governmental guidelines in the UK, throughout the pandemic (Appendix 1). Participants were asked to read through the pro-social behaviour checklist and indicate, using a 5-point frequency rating scale how much they engaged in each behaviour in the first lockdown (1 = not at all, to 5 = very often); and how much they were willing to engage in pro-social behaviour in the future, should another lockdown occur, by completing a similar a 5-point Likert scale for behavioural willingness (1 = not at all willing, to 5 = very willing).
9. Results
All data were analysed in SPSS v. 26 (IBM Corp., Armonk, NT, USA). To replicate the findings from Study 1, we used the same method to determine COVID anxious and non-anxious groups. We used generalized eta squared (η 2 G) as an effect size indicator for repeated measures designs with the following conventions: small =.01, medium=.06 and large=.14 effect sizes (Olejnik and Algina, 2003). There were no significant gender differences in any of the study variables, and no significant differences in state anxiety between the COVID anxious (M=21.38, SD=7.56) and the non-anxious (M=20.33, SD=7.20). However, there was a significant difference between the COVID anxious (N=60, M=26.93, SD=5.57) and the non-anxious (N=78, M=20.95, SD=9.67) groups on Trait Anxiety t(136)=4.27, p<.001.
Person's corelation analysis showed that COVID anxiety was significant significantly associated with trait (r=.38, p<.001) but not with state anxiety scores (r=.09, p > .05). Correlation coefficient between COVID-anxiety and outcome measures from both tasks are presented in Table 5 . Like Study 1, in Study 2 we used partial correlation with Variance Reduction Rate (VRR) analysis to estimate the amount of variance attributed to trait anxiety, in the associations between COVID-anxiety and IRT scores. In Study 2, we also examined whether the association between the continuous scores of COVID-anxiety, loneliness, and prosocial behaviour could be attributed to the effects of trait anxiety. The observed zero-order correlations (r) between COVID-anxiety and IRT scores ranged between .22 and .50 (see Table 1), and they did not change significantly after controlling for state anxiety, with observed partial correlations (r) ranging between .21 to .44. The VRR results further showed that trait anxiety accounted for: 32% in the association between COVID-anxiety and negativity; 22.4% in the association between COVID-anxiety and fear ratings; 33% in the association between COVID-anxiety and sadness ratings; and 6.1% in the association between COVID-anxiety and anger ratings.
Table 5.
Correlational analyses study 2.
| Stroop RT (COVID words) | Stroop accuracy % (COVID words) | Arousal (COVID images) | Negativity (COVID images) | Fear (COVID images) | Disgust (COVID images) | Sadness (COVID images) | Anger (COVID images) | STAI State Anxiety | STAI Trait Anxiety | COVID anxiety scale | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stroop RT (COVID words) | — | ||||||||||
| Stroop accuracy % (COVID words) | -0.076 | — | |||||||||
| Arousal (COVID images) | 0.098 | 0.199* | — | ||||||||
| Negativity (COVID images) | 0.069 | 0.050 | 0.440*** | — | |||||||
| Fear (COVID images) | 0.123 | -0.120 | 0.421*** | 0.660*** | — | ||||||
| Disgust (COVID images) | 0.112 | -0.069 | 0.223** | 0.424*** | 0.372*** | — | |||||
| Sadness (COVID images) | 0.177* | 0.021 | 0.520*** | 0.706*** | 0.681*** | 0.363*** | — | ||||
| Anger (COVID images) | 0.059 | -0.052 | 0.424*** | 0.457*** | 0.529*** | 0.640*** | 0.559*** | — | |||
| STAI State Anxiety | -0.216** | -0.018 | -0.062 | -0.014 | 0.081 | -0.002 | -0.023 | 0.006 | — | ||
| STAI Trait Anxiety | 0.142 | 0.089 | 0.011 | 0.186* | 0.290*** | 0.040 | 0.217* | 0.061 | 0.129 | — | |
| COVID anxiety scale | 0.297*** | -0.161 | 0.166 | 0.285*** | 0.499*** | 0.140 | 0.317*** | 0.223** | 0.094 | 0.378*** | — |
Note. * p < .05, ** p < .01, *** p < .001
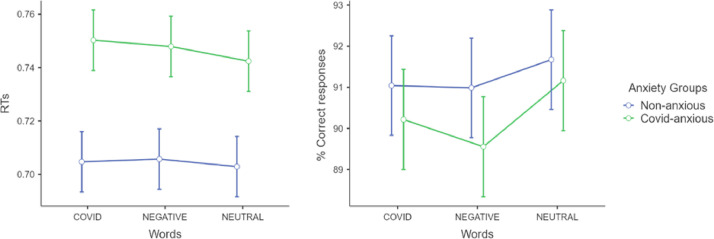
The first hypothesis was examined using two 2 × 3 repeated measures ANCOVAs to determine differences between COVID anxious and non-anxious participants on reaction times (RTs) and accuracy (% correct responses) to COVID-related, negative, and neutral words, while controlling for the effects of Trait anxiety (covariate). There was a significant main effect of group for RTs indicating that the COVID anxious group was overall slower, showing increased interference compared to the non-anxious group [F(1,140) = 4.16, p < .05, η 2 G = .034], while controlling for the effects of Trait anxiety (p > .05). Similar effects were found when the covariate was removed from the analysis [F(1,140) = 7.42, p < .001, η 2 G = .048] (Fig. 3 ). There were no significant differences between the groups for accuracy.
Fig. 3.
Differences on RTs and accuracy for the two groups on EST.
Note: This figure illustrates estimated marginal means for reaction times (RTs) and % correct responses (DVs) on the EST in each group (COVID-anxious, non-anxious).
Means and standard deviations for RTs and accuracy are presented in (Table 6 ).
Table 6.
Descriptive statistics displaying Means and SDs for Study 2 Stroop task separated by anxiety groups.
| Groups | Covid words (RTs) | Covid words Accuracy (%) | Negative words (RTs) | Negative words Accuracy (%) | Neutral words (RTs) | Neutral words Accuracy (%) |
|---|---|---|---|---|---|---|
| Covid-anxious | 0.75 (0.09) | 90.18 (9.58) | 0.75 (0.09) | 89.52 (9.35) | 0.74 (0.09) | 91.13 (8.31) |
| Non-anxious | 0.71 (0.10) | 91.01 (10.81) | 0.71 (0.10) | 90.95 (11.80 | 0.70 (0.10) | 91.64 (10.64) |
To explore the second hypothesis, 2 × 3 repeated measures ANCOVAs (group: COVID anxious vs. non-anxious, image type: COVID, negative, neutral) with trait anxiety as a covariate, were used to determine differences between COVID anxious and non-anxious on arousal, negativity, fear, disgust, sadness and anger (DVs). Means and SDs are presented in Table 7 .
Table 7.
Means and SDs for each image type (COVID, negative and neutral), on the 4 negative emotions (fear, disgust, sadness and anger) for each anxiety group (COVID-anxious, Non-anxious).
| COVID-anxious |
Non-anxious |
||||
|---|---|---|---|---|---|
| Emotion Rating | Image Type | Mean (SD) | Emotion Rating | Image Type | Mean (SD) |
| Fear | Covid-related | 45.45 (28.12) | Fear | Covid-related | 23.10 (24.70) |
| Negative | 33.43 (22.66) | Negative | 24.45 (21.52) | ||
| Neutral | 3.40 (5.01) | Neutral | 3.10 (7.33) | ||
| Disgust | Covid-related | 16.55 (16.75) | Disgust | Covid-related | 10.29 (15.43) |
| Negative | 47.65 (21.16) | Negative | 43.78 (23.05) | ||
| Neutral | 2.24 (3.71) | Neutral | 2.26 (4.32) | ||
| Sadness | Covid-related | 70.27 (22.67) | Sadness | Covid-related | 55.06 (28.33) |
| Negative | 47.02 (16.92) | Negative | 38.57 (16.43) | ||
| Neutral | 6.04 (9.27) | Neutral | 4.74 (11.13) | ||
| Anger | Covid-related | 28.02 (28.15) | Anger | Covid-related | 15.42 (21.21) |
| Negative | 37.75 (20.12) | Negative | 31.14 (20.49) | ||
| Neutral | 4.35 (10.54) | Neutral | 2.33 (4.28) | ||
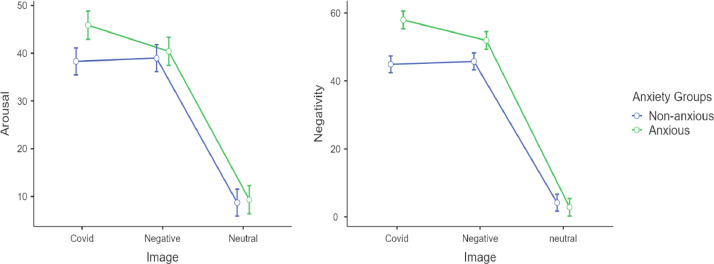
Results showed a significant main effect of image type on arousal [F(2,272) = 16.27, p < .001, η 2 G = .10] with COVID-related images and non-COVID negative images being rated as significantly more arousing than neutral images after controlling for the effects trait anxiety (p<.05). There were no differences in arousal between the COVID-related and non-COVID negative images (Fig. 4 ).
Fig. 4.
Differences on ratings of arousal and negativity between the two groups.
Note: This figure illustrates estimated marginal means for arousal and negativity (DVs) in each group (COVID-anxious, non-anxious).
Similarly, there was a significant main effect of image type on negativity, [F(2,270) = 21.01, p < .001, η 2 G = .13] and a significant interaction [F(2,270) = 3.51, p < .05, η 2 G = .02] after controlling for the effects of trait anxiety (p>.05). Planned post-hoc comparisons using Bonferroni indicated that there were no significant differences on negativity between COVID-related and non-COVID negative images, but both were significantly less negative than neutral. In relation to Fear, the results showed that there was a significant a significant main effect of image type [F(2,270) = 5.809, p < .05, η 2 G = .04], a significant main effect of group [F(1,135) = 10.74, p <.01, η 2 G = .07], and a significant interaction [F(2,270) = 10.26, p < .001, η 2 G = .07] after controlling for the effect of trait anxiety (p>.05). Follow-up comparisons indicated that COVID anxious individuals exhibited significantly higher fear for COVID-related images compared to non-COVID negative images matched for arousal and negativity an effect that was not observed in the non-anxious group. There was a significant main effect of image type on disgust ratings [F(2,270) = 36.01, p < .001, η 2 G = .21], with non-COVID negative images being rated as more disgusting compared to COVID-related images and neutral images by both groups.
We also found a significant main effect of image type on Sadness [F(2,270) = 30.92, p < .001, η 2 G = .19], a significant main effect of group [F(1,135) = 7.44, p < .01, η 2 G = .05], and a significant interaction (Huynh-Feldt correction was applied) [F(1.58, 213.11) = 3.78, p = .034, η 2 G = .03] after controlling for the effects of trat anxiety (p>.05). Post-hoc comparisons indicated that both groups rated COVID-related images as sadder than non-COVID negative images and neutral images, but the COVID anxious group showed higher ratings compared to the non-anxious group.
Finally, there was a significant main effect of image type on Anger [F(2,270) = 7.84, p < .001, η 2 G = .06], a significant main effect of group [F(1,135) = 6.59, p < .05, η 2 G = .05], and a significant interaction [F(2,270) = 4.09, p < .05, η 2 G = .03] after controlling for the effects of trait anxiety (p>.05). Planned comparisons indicated that COVID-anxious individuals rated COVID-related images higher in anger than non-anxious individuals but lower than non-COVID negative images a pattern that was similar in both groups (Fig. 5 ).
Fig. 5.
Differences on ratings of fear, disgust, sadness and anger between the two groups.
Note: This figure illustrates estimated marginal means for fear, disgust, sadness and anger (DVs) in each group (COVID-anxious, non-anxious).
To examine Hypotheses 3 and 4 we conducted moderated regression analyses to assess whether COVID-anxiety scores are associated with self-reported loneliness (Model 1), self-reported past prosocial behaviour (Model 2) and willingness to engage in prosocial behaviour in the future (Model 3), and whether this association was moderated by levels of trait anxiety. For this reason, and following the recommendations of Cohen et al. (2013) the scores in COVID-anxiety and trait anxiety were standardised and their interaction term (COVID-anxiety × trait anxiety) was computed. Each moderated regression model was completed in two steps, and the first step included the main effects of the COVID and trait anxiety, and the second step included their interaction term. Unstandardized beta weights (B) and 95% confidence intervals (CIs) were used. The analyses indicated that the multivariate association of COVID-anxiety with the three outcome variables (i.e., loneliness, past prosocial behaviour, and willingness to engage in prosocial behaviour in the future) was non-significant, and only trait anxiety was significantly associated with all three outcomes (Model 1: R 2 = 73.1%, F = 121.47, p < .001, B trait anxiety = .865, p < .001; Model 2: R 2 = 22.7%, F = 13.08, p < .001, B trait anxiety = .357, p < .001; Model 3: R 2 = 49.2%, F = 45.18, p < .001, B trait anxiety = .670, p < .001). Only in Model 2, the association between trait anxiety and self-reported past prosocial behaviour was significantly moderated by the levels of COVID anxiety (B COVID-anxiety × trait anxiety = -.264, p = .025), suggesting that for high levels of trait anxiety, participants were more likely to have helped someone in need during the pandemic when their COVID-anxiety levels were low.
10. Study 2 discussion
The aim of Study 2 was to replicate and extend the findings of Study 1 to a population of University students, in the UK during the second lockdown. To do so, University students completed the same Emotional Stroop Task (EST) and an Image Rating Task as in Study 1, and also completed a loneliness questionnaire, and a measure assessing past pro-social behaviour during the first national lockdown, and willingness to engage in pro-social behaviour in the future, in the prospect of another lockdown. Overall, Study 2 results replicated the findings of Study 1 and largely supported the respective hypotheses.
Specifically, COVID-anxious participants reported significantly higher levels of negativity, fear, sadness and anger when exposed to COVID-related images, compared to non-anxious participants. The VRR analysis also showed that the associations between the continuous scores of COVID anxiety and IRT scores remained statistically significant, after controlling for trait anxiety scores, suggesting a small nuisance effect of trait anxiety. Moreover, fear and sadness were particularly prevalent in COVID-anxious participants, when rating COVID-related images compared to non-COVID negative images matched for arousal and negativity. Also, in accordance with the findings in Study 1, our results indicated that both anxious and non-anxious participants rated COVID-related images as less disgusting than non-COVID negative images. A possible explanation for this finding is that COVID-related images did not contain elements of core disgust (such as bodily fluids) that evoke disgust responses (e.g., Olatunji et al., 2008), while some of the non-COVID negative images involved core disgust elements (e.g., rats). The results of Study 2 also demonstrated that COVID-anxious participants were generally slower than non-anxious individuals on the Emotional Stroop Task without, however, showing any particular interference for COVID-related words, compared to non-COVID negative and neutral words, and this was not influenced by scores on trait anxiety.
Finally, participants with higher levels of trait anxiety, but not COVID-anxiety, also tended to report higher levels of loneliness, more engagement in prosocial behaviour during the first lockdown, and stronger willingness to help others should a need a rise in the future. Nevertheless, COVID-anxiety moderated this latter association, so that higher levels of trait anxiety were associated more strongly with willingness to be prosocial, when COVID-anxiety levels were low. This effect is in line with previous research on pressure-based prosocial behaviour and suggests that people may be willing to help others to alleviate their general anxiety levels, only to the extend their COVID-related anxiety is kept at low levels.
11. General discussion
The world is currently faced with a global pandemic that has an unprecedented effect on mental health outcomes, and on risk factors that contribute to poor mental health, such as loneliness. Consuming more news and information about COVID plays a role in this process (Petzold et al., 2020; Xiong et al., 2020). The present research examined, for the first time in the extant literature, emotional responses to COVID-related stimuli by using methods designed to capture both automatic and controlled responses, such as Emotional Stroop Task (EST) and Image Rating Tasks (IRT) respectively. Study 1 findings indicated that, compared to negative and neutral pictures, COVID-related pictures elicited significantly higher levels of arousal, negativity, fear, sadness, and anger. Furthermore, our findings from both studies showed that there were no differences between COVID-anxious and non-anxious people on automatic affective responses to COVID-related words in the Stroop Task, compared to negative and neutral words (i.e., no interference effect). On the other hand, both studies showed that, compared to non-anxious participants, those in the COVID-anxious group rated COVID-related images higher, than non-COVID negative images, in fear and anger. Taken together, these results imply that there may be a dissociation between automatic and controlled processes in affective responses to COVID-related stimuli. This dissociation could not be easily attributed to stimulus type (e.g., words vs images, because previous research has indicated that amygdala responses to emotionally salient negative stimuli were independent of stimulus type (Kensinger and Schacter, 2006). However, this dissociation could be explained by that the EST is designed to capture attentional biases to emotionally salient threatening stimuli that involve more automatic processes, whereas the IRT involves higher-order evaluative processes.
Certain limitations should be mentioned. First of all, we did not control for previous experiences with COVID (e.g., having been contaminated, or having been severely affected by COVID). It is possible that having experienced adverse COVID-related outcomes could have influenced the results, especially with regards to more automatic responses to COVID stimuli. Secondly, we did not control for pre-existing anxiety or mood disorders that may have confounded the observed effects. However, we controlled for the effects of general anxiety levels (state and trait) and, via VRR analysis, we identified the amount of variance (or nuisance effect) attributed to either state or trait anxiety in each study. The present study also had several important strengths. First of all, we developed novel COVID-specific tasks that can be readily used by future research on the emotional impact of COVID in the general population, or in clinical populations (e.g., COVID survivors, long COVID patients, people with mental health difficulties). Secondly, our research advances the extant literature on the affective responses to COVID, which is scarce and largely based on self-reported measures. Thirdly, and related to the measurement methodology we used, our study allowed for the distinction between controlled (IRT) and automatic (EST) affective responses to COVID-related stimuli. Lastly, our research indicated that higher trait anxiety was associated with greater loneliness and more willingness to engage in prosocial behaviour. In the case of previous prosocial behaviour, the association with trait anxiety was moderated by levels of COVID-related anxiety (Study 2).
Funding
The study was internally funded by Sheffield Hallam University (departmental funding) and the funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
CRediT authorship contribution statement
Antonia Ypsilanti: Conceptualization, Data curation, Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing. Emma Mullings: Conceptualization, Data curation, Formal analysis, Writing – review & editing. Oliver Hawkins: Methodology, Project administration, Software, Supervision, Validation, Visualization. Lambros Lazuras: Formal analysis, Funding acquisition, Writing – original draft, Writing – review & editing.
Declaration of Competing Interest
The authors do not have any conflict of interest to declare.
Acknowledgement
We would like to thank Dr David Reynolds for facilitating data collection from the UG Psychology students for study 2.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.08.031.
Appendix. Supplementary materials
References
- Akram U., Ypsilanti A., Gardani M., Irvine K., Allen S., Akram A., ..., Lazuras L. Prevalence and psychiatric correlates of suicidal ideation in UK university students. J. Affect. Disord. 2020;272:191–197. doi: 10.1016/j.jad.2020.03.185. [DOI] [PubMed] [Google Scholar]
- Arora T., Grey I., Östlundh L., Lam K.B.H., Omar O.M., Arnone D. The prevalence of psychological consequences of COVID-19: A systematic review and meta-analysis of observational studies. J. Health Psychol. 2020 doi: 10.1177/1359105320966639. [DOI] [PubMed] [Google Scholar]
- Barkoukis V., Lazuras L., Tsorbatzoudis H. Beliefs about the causes of success in sports and susceptibility for doping use in adolescent athletes. J. Sports Sci. 2014;32(3):212–219. doi: 10.1080/02640414.2013.819521. [DOI] [PubMed] [Google Scholar]
- Bailey T., Totsika V., Hastings R.P., Hatton C., Emerson E. Developmental trajectories of behaviour problems and prosocial behaviours of children with intellectual disabilities in a population-based cohort. J. Child Psychol. Psychiatry. 2019;60(11):1210–1218. doi: 10.1111/jcpp.13080. [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y., Lamy D., Pergamin L., Bakermans-Kranenburg M.J., Van Ijzendoorn M.H. Threat-related attentional bias in anxious and nonanxious individuals: a meta-analytic study. Psychol. Bull. 2007;133(1):1. doi: 10.1037/0033-2909.133.1.1. [DOI] [PubMed] [Google Scholar]
- Bradley M.M., Lang P.J. Vol. 30. University of Florida; 1999. Affective Norms for ENGLISH Words (ANEW): Instruction Manual and Affective Ratings; pp. 25–36. (Affective Norms for ENGLISH Words (ANEW): Instruction Manual and Affective Ratings). Technical report C-1, the center for research in psychophysiology. [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet North Am. Ed. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu, F., Steptoe, A., & Fancourt, D. (2020). Loneliness during lockdown: trajectories and predictors during the COVID-19 pandemic in 35,712 adults in the UK. medRxiv, doi:10.1101/2020.05.29.20116657. [DOI] [PMC free article] [PubMed]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021;21(1) doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Cacioppo S. The growing problem of loneliness. Lancet North Am. Ed. 2018;391(10119):426. doi: 10.1016/S0140-6736(18)30142-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C. Social isolation and health, with an emphasis on underlying mechanisms. Perspect. Biol. Med. 2003;46(3):S39–S52. [PubMed] [Google Scholar]
- Carthy T., Horesh N., Apter A., Edge M.D., Gross J.J. Emotional reactivity and cognitive regulation in anxious children. Behav. Res. Ther. 2010;48(5):384–393. doi: 10.1016/j.brat.2009.12.013. [DOI] [PubMed] [Google Scholar]
- Chen P.Y., Spector P.E. Negative affectivity as the underlying cause of correlations between stressors and strains. J. Health Psychol. 1991;76(3):398. doi: 10.1037/0021-9010.76.3.398. [DOI] [PubMed] [Google Scholar]
- Clauss K., Bardeen J.R., Thomas K., Benfer N. The interactive effect of emotional reactivity and maladaptive metacognitive beliefs on anxiety. Cognit. Emot. 2020;34(2):393–401. doi: 10.1080/02699931.2019.1625752. [DOI] [PubMed] [Google Scholar]
- Cohen J., Cohen P., West S.G., Aiken L.S. Routledge; New Jersey: 2013. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences. [Google Scholar]
- Colibazzi T., Posner J., Wang Z., Gorman D., Gerber A., Yu S., Peterson B.S. Neural systems subserving valence and arousal during the experience of induced emotions. Emotion. 2010;10(3):377–389. doi: 10.1037/a0018484. [DOI] [PubMed] [Google Scholar]
- Compton R.J., Arnstein D., Freedman G., Dainer-Best J., Liss A. Cognitive control in the intertrial interval: evidence from EEG alpha power. Psychophysiology. 2011;48(5):583–590. doi: 10.1111/j.1469-8986.2010.01124.x. [DOI] [PubMed] [Google Scholar]
- Cooke J.E., Eirich R., Racine N., Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatry Res. 2020;292:3–5. doi: 10.1016/j.psychres.2020.113347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis V., Aunger R., Rabie T. Evidence that disgust evolved to protect from risk of disease. Proc. R. Soc. Lond. B Biol. Sci. 2004;271:131–133. doi: 10.1098/rsbl.2003.0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies N.G., Kucharski A.J., Eggo R.M., Gimma A., Edmunds W.J., Jombart T., ..., Liu Y. Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health. 2020;5(7):e375–e385. doi: 10.1016/S2468-2667(20)30133-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekman P. An argument for basic emotions. Cognit. Emot. 1992;6(3-4):169–200. [Google Scholar]
- Epp A.M., Dobson K.S., Dozois D.J., Frewen P.A. A systematic meta-analysis of the Stroop task in depression. Clin. Psychol. Rev. 2012;32(4):316–328. doi: 10.1016/j.cpr.2012.02.005. [DOI] [PubMed] [Google Scholar]
- Fox E., Cahill S., Zougkou K. Preconscious processing biases predict emotional reactivity to stress. Biol. Psychiatry. 2010;67(4):371–377. doi: 10.1016/j.biopsych.2009.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaeta L., Brydges C.R. Coronavirus-related anxiety, social isolation, and loneliness in older adults in northern California during the stay-at-home order. J. Aging Soc. Policy. 2020;00(00):1–12. doi: 10.1080/08959420.2020.1824541. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., ..., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15(4) doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebauer J.E., Riketta M., Broemer P., Maio G.R. Pleasure and pressure based prosocial motivation: divergent relations to subjective well-being. J. Res. Personal. 2008;42(2):399–420. doi: 10.1016/j.jrp.2007.07.002. [DOI] [Google Scholar]
- Horowitz M.J., Wilner N., Alvarez W. Impact of event scale (IES): a measure of subjective distress. Psychosom. Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Husky M.M., Kovess-Masfety V., Swendsen J.D. Stress and anxiety among university students in france during covid-19 mandatory confinement. Compr. Psychiatry. 2020;102 doi: 10.1016/j.comppsych.2020.152191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibrahim A.K., Kelly S.J., Adams C.E., Glazebrook C. A systematic review of studies of depression prevalence in university students. J. Psychiatr. Res. 2013;47(3):391–400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- Itkes O., Kimchi R., Haj-Ali H., Shapiro A., Kron A. Dissociating affective and semantic valence. J. Exp. Psychol. 2017;146(7):924. doi: 10.1037/xge0000291. [DOI] [PubMed] [Google Scholar]
- Kandel E.R., Schwartz J.H., Jessell T.M., Siegelbaum S., Hudspeth A.J., Mack S., editors. Vol. 4. McGraw Hill; New York: 2000. pp. 1227–1246. (Principles of Neural Science, Principles of Neural Science). [Google Scholar]
- Killgore W.D.S., Cloonan S.A., Taylor E.C., Dailey N.S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kensinger E.A., Schacter D.L. Processing emotional pictures and words: effects of valence and arousal. Cognit. Affect. Behav. Neurosci. 2006;6(2):110–126. doi: 10.3758/cabn.6.2.110. [DOI] [PubMed] [Google Scholar]
- Kučera H., Francis W.N. University Press of New England; 1967. Computational Analysis of Present-Day American English. [Google Scholar]
- Lazuras L., Rodafinos A., Matsiggos G., Stamatoulakis A. Perceived occupational stress, affective, and physical well-being among telecommunication employees in Greece. Soc. Sci. Med. 2009;68(6):1075–1081. doi: 10.1016/j.socscimed.2008.12.020. [DOI] [PubMed] [Google Scholar]
- Lazuras L., Barkoukis V., Rodafinos A., Tzorbatzoudis H. Predictors of doping intentions in elite-level athletes: a social cognition approach. J. Sport Exerc. Psychol. 2010;32(5):694–710. doi: 10.1123/jsep.32.5.694. [DOI] [PubMed] [Google Scholar]
- Lee C.M., Cadigan J.M., Rhew I.C. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. J. Adolesc. Health. 2020;67(5):714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44(7):393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Lep Ž, Babnik K., Hacin Beyazoglu K. Emotional responses and self-protective behavior within days of the COVID-19 outbreak: the promoting role of information credibility. Front. Psychol. 2020;11:1–8. doi: 10.3389/fpsyg.2020.01846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L.Z., Wang S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marelli S., Castelnuovo A., Somma A., Castronovo V., Mombelli S., Bottoni D., ..., Ferini-Strambi L. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J. Neurol. 2020;268(1):8–15. doi: 10.1007/s00415-020-10056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauss I.B., Robinson M.D. Measures of emotion: a review. Cognit. Emot. 2009;23(2):209–237. doi: 10.1080/02699930802204677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office for National Statistics. (2020a, December 9). Deaths involving COVID-19, England and Wales: deaths occurring in May 2020. Retrieved from https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19englandandwales/deathsoccurringinmay2020.
- Office for National Statistics. (2020b, June 23). Coronavirus and higher education students: England, 20 November to 25 November 2020.Retrieved from https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandhighereducationstudents/england20novemberto25november2020.
- Nolen-Hoeksema S., Morrow J., Fredrickson B.L. Response styles and the duration of episodes of depressed mood. J. Abnorm. Psychol. 1993;102(1):20–28. doi: 10.1037/0021-843X.102.1.20. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Haidt J., McKay D., David B. Core, animal reminder, and contamination disgust: three kinds of disgust with distinct personality, behavioral, physiological, and clinical correlates. J. Res. Personal. 2008;42(5):1243–1259. [Google Scholar]
- Olejnik S., Algina J. Generalized eta and omega squared statistics: measures of effect size for some common research designs. Psychol. Methods. 2003;8(4):434–447. doi: 10.1037/1082-989X.8.4.434. [DOI] [PubMed] [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y.…Hoffman Y. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirce J., Gray J.R., Simpson S., MacAskill M., Höchenberger R., Sogo H., ..., Lindeløv J.K. PsychoPy2: experiments in behavior made easy. Behav. Res. Methods. 2019;51(1):195–203. doi: 10.3758/s13428-018-01193-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petzold M.B., Bendau A., Plag J., Pyrkosch L., Mascarell Maricic L., Betzler F., ..., Ströhle A. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020;10(9):1–10. doi: 10.1002/brb3.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pišot S., Milovanović I., Šimunič B., Gentile A., Bosnar K., Prot F., ..., Drid P. Maintaining everyday life praxis in the time of COVID-19 pandemic measures (ELP-COVID-19 survey) Eur. J. Public Health. 2020;30(6):1181–1186. doi: 10.1093/eurpub/ckaa157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Planchuelo-Gómez Á, Odriozola-González P., Irurtia M.J., de Luis-García R. Longitudinal evaluation of the psychological impact of the COVID-19 crisis in Spain. J. Affect. Disord. 2020;277:842–849. doi: 10.1016/j.jad.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner J., Russell J.A., Peterson B.S. The circumplex model of affect: An integrative approach to affective neuroscience, cognitive development, and psychopathology. Dev. Psychopathol. 2005;17(3):715–734. doi: 10.1017/S0954579405050340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D.W. UCLA loneliness scale (version 3): reliability, validity, and factor structure. J. Pers. Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Sadiković S., Branovački B., Oljača M., Mitrović D., Pajić D., Smederevac S. Daily monitoring of emotional responses to the coronavirus pandemic in Serbia: a citizen science approach. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.02133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S.G.S., Nogueras D., van Woerden H.C., Kiparoglou V. The COVID-19 pandemic: a pandemic of lockdown loneliness and the role of digital technology. J. Med. Internet Res. 2020;22(11):1–7. doi: 10.2196/22287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spielberger C.D., Gorsuch R.L., Lushene R.E. Consulting Psychologists Press; 1968. State-trait anxiety inventory (STAI): test manual for form X. [Google Scholar]
- Tang W., Hu T., Hu B., Jin C., Wang G., Xie C., ..., Xu J. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomkins S. Springer Publishing; 1962. Affect Imagery Consciousness: Volume I: the Positive Affects. [Google Scholar]
- van Tilburg T.G., Steinmetz S., Stolte E., van der Roest H., de Vries D.H. Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J. Gerontol. 2020:1–7. doi: 10.1093/geronb/gbaa111. XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Wang Z., Liu X., Yang X., Zheng M., Bai X. The impacts of a COVID-19 epidemic focus and general belief in a just world on individual emotions. Personal. Indiv. Differ. 2021;168 doi: 10.1016/j.paid.2020.110349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J.M., Mathews A., MacLeod C. The emotional Stroop task and psychopathology. Psychol. Bull. 1996;122(1):3–24. doi: 10.1037/0033-2909.120.1.3. [DOI] [PubMed] [Google Scholar]
- World health organisation (2020). COVID-19 disrupting mental health services in most countries, WHO survey.Retrieved from https://www.who.int/news/item/05-10-2020-covid-19-disrupting-mental-health-services-in-most-countries-who-survey.
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., ..., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yiend J., Mathews A. Anxiety and attention to threatening pictures. Q. J. Exp. Psychol. Sect. A. 2001;54(3):665–681. doi: 10.1080/713755991. [DOI] [PubMed] [Google Scholar]
- Yiend J. The effects of emotion on attention: a review of attentional processing of emotional information. Cognit. Emot. 2010;24(1):3–47. [Google Scholar]
- Zolotov Y., Reznik A., Bender S., Isralowitz R. COVID-19 fear, mental health, and substance use among Israeli university students. Int. J. Mental Health Addict. 2020 doi: 10.1007/s11469-020-00351-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.