Abstract
Objectives
The objective of the study is to investigate the factors associated with COVID-19 vaccination intentions and attitudes in France.
Study design
An online cross-sectional study was conducted among a representative sample of the French population between November 20th and 23rd 2020 (N = 1146).
Methods
Factors associated with the intention to get vaccinated and with COVID-19 vaccine attitudes were estimated using ordered logistic and multinomial logistic regressions, respectively. Independent variables of interest include COVID-19 and vaccine perceptions, trust, endorsement of COVID-19 conspiracy theories and time/risk preferences.
Results
Only 30.5% of our respondents would agree to get vaccinated against COVID-19 during the first semester of 2021 while 31.1% declare being unsure of their vaccination intentions. COVID-19 risk perceptions are associated with vaccination intentions and attitudes. Individual and collective benefits of the vaccine and the concerns over its safety are strongly associated with COVID-19 vaccination intentions and attitudes. Vaccine acceptors are more willing to take risks in the health domain compared with vaccine hesitant respondents which indicates that the COVID-19 vaccine is perceived as a greater health risk than the COVID-19 itself by some respondents. We also find a positive association between future preference and the willingness to get vaccinated.
Conclusion
Awareness campaigns should be conducted to enhance vaccination uptake among vaccine hesitant individuals. These campaigns could highlight the positive benefit-risk balance of the COVID-19 vaccines or the short-term benefits of vaccination and should reinsure the public on the safety of the COVID-19 vaccines.
Keywords: COVID-19, France, Vaccination, Time preference, Health belief model
Introduction
In France, the COVID-19 vaccination campaign has started in January 2021. After the vaccination of high-risk individuals, the vaccination campaign has been scaled-up to the rest of the French population from spring 2021 onward. Despite the low initial COVID-19 vaccination intentions among the French population before the launch of the vaccination campaign (only 53%1 and 39%2 of respondents from nationally representative samples of the French adult population were willing to get vaccinated in November and December 2020, respectively) and the growing vaccine hesitancy since the H1N1 influenza pandemic vaccination campaign of 2009,3, 4, 5, 6 half of the French population had received at least one dose of COVID-19 vaccine at the beginning of summer 2021. Nevertheless, the rhythm of first doses administration is currently slowing down while it is estimated that a 60%–90% level of COVID-19 vaccination uptake is needed to create herd immunity.7
Convincing vaccine hesitant populations to get vaccinated against COVID-19 is now crucial to reduce the level of circulation of the virus, to prevent the emergence of variants and to reach herd immunity. In this context, studying the factors associated with the willingness to get vaccinated against COVID-19 appears crucial to design effective awareness campaigns enhancing vaccination uptake. Previous studies have shown that COVID-19 vaccination intentions are lower among women, unemployed and less educated respondents8, 9, 10 and that they are positively associated with COVID-19 risk perceptions11 , 12 and with the perceived benefit of the vaccine.13 , 14 On the other hand, concerns over the efficacy or the safety of the vaccine were stated as reasons for not wanting to get vaccinated against COVID-19 in several studies.10 , 14, 15, 16 Lack of trust in vaccine development or testing processes and in scientific research was also found to be prevalent among vaccine hesitant respondents in the United States and Italy,16 , 17 whereas COVID-19 misinformation or endorsement of COVID-19 conspiracy theories were found to be negatively associated with vaccination intentions.18, 19, 20
In France, several studies have investigated the factors associated with COVID-19 vaccination intentions among the general population during or just after the first wave of the epidemic in spring 2020.21, 22, 23, 24, 25 These studies, conducted either in representative22, 23, 24 or non-representative21 , 25 samples of the French adult population, have found that vaccination intentions are lower among female, older (>65 years old) and low-income respondents. Respondents declaring to be ‘afraid of the new coronavirus’ or feeling ‘at risk of getting infected by the new coronavirus’ were more likely to declare they will get vaccinated if a vaccine was available in a study conducted among a non-representative sample of the French adult population.21 Being very concerned about getting infected with COVID-19 was found to be negatively correlated with COVID-19 vaccine refusal, i.e., declaring ‘probably not’ or ‘certainly not’ agreeing to get vaccinated against COVID-19 if a vaccine was available, among a representative sample of the French population.23 Vaccination history and risk factors of a severe form of COVID-19 were also shown to be significantly associated with vaccine outright refusal (never choosing to get vaccinated whatever the vaccine characteristics) and vaccine hesitancy (choosing to get vaccinated or not depending on the vaccine characteristics) in a discrete choice experiment conducted among a representative working-age population.24 COVID-19 conspiracy beliefs, measured through the level of agreement with nine items such as ‘a vaccine against the coronavirus exists, but it is kept secret by those who have it in order to increase its value’, were also found to be negatively associated with COVID-19 vaccination intentions in a study conducted among a non-representative sample of the French population in spring 2020.25 Finally, a study on COVID-19 vaccination intentions among French healthcare workers found that COVID-19 fear or perceived risk and previous flu vaccination were associated with vaccination intentions.26
Using data of an online survey conducted among a sample representative of the adult population living in France with regard to gender, age, region and socio-professional category between November 20th and 23rd 2020 (N = 1146), we study the factors associated with COVID-19 vaccination intentions and attitudes at a time the first efficacy results from phase 3 trials of COVID-19 vaccines were publicly released. Our objective is to study how COVID-19 risk perceptions, perceived efficacy and concerns over the COVID-19 vaccine, trust, endorsement of COVID-19 conspiracy theories and time and risk preferences are associated with the willingness to get vaccinated against COVID-19 during the first semester of 2021.
Methods
Design and sample
The sample is composed of 1268 French-speaking adults living in France. Respondents' recruitment was operated by an independent panellist (www.panelabs.com) over three days (November 20–23, 2020) using a quota sampling design to create a sample representative of the population living in France with regard to gender, age, region and socio-professional category. The questionnaire was hosted on Limesurvey®. Participants were presented with an information letter about the purpose of the study before being asked whether they agreed to participate. The information letter mentioned the strict anonymity of collected data and the eligibility criteria (aged more than 18 years and living in France). Given strict anonymity of collected data, the study did not need authorization of the Commission Nationale de l'Informatique et des Libertés (CNIL).
Dependent variables of interest
Respondents were asked whether they would agree to get vaccinated against COVID-19 if a vaccine were to be approved by the French national health authorities during the first semester of 2021. Intentions to get vaccinated was measured on a Likert-type scale ranging from 1 (‘I would definitely not agree’) to 5 (‘I would definitely agree’).
Participants were also asked after how much time they will be willing to get vaccinated once a COVID-19 vaccine will be available in France. Participants had to choose between the following responses: ‘as soon as possible’, ‘in less than a month’, ‘between one and three months’, ‘between three and six months’, ‘between six months and one year’, ‘between one and two years’, ‘unsure’ and ‘I would never get vaccinated’. Using respondents' answers to this question, we created a three-category vaccine attitude variable based on the continuum of vaccine hesitancy developed by the SAGE Working Group on Vaccine Hesitancy.27 Participants were categorized in the ‘vaccine acceptance’ category if they declared they would get vaccinated in less than three months, in the ‘vaccine hesitancy’ category if they declared they would get vaccinated after three months or if they declared being unsure of whether they would get vaccinated and in the ‘vaccine outright refusal’ category if they declared they would never get vaccinated.
Independent variables of interest
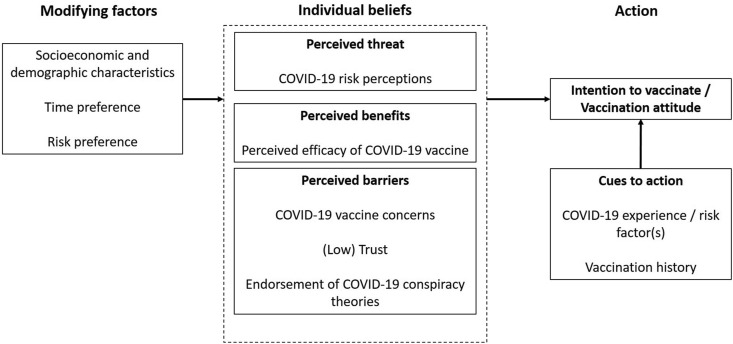
The theoretical framework based on the Health Belief Model (HBM)28 and used to investigate the factors associated with COVID-19 vaccination attitudes and intentions is presented in Fig. 1 . The HBM has been widely used in the literature to study vaccination beliefs and behaviours,29 including vaccination uptake in epidemic contexts.30, 31, 32
Fig. 1.
Theoretical framework.
The independent variables of interest were assessed by several questions with ordinal responses and factorial analyses were conducted to create scores for the different HBM constructs.
COVID-19 perceived threat
COVID-19 risk perceptions were measured using three one-item variables: the level of agreement with the assertion that ‘experts who say that COVID-19 is dangerous should be believed’ (from 1 – ‘totally disagree’ to 5 – ‘totally agree’), the perceived individual health consequences in case of infection and the perceived health impacts of the COVID-19 epidemic in France (both from 1 – ‘not serious at all’ to 5 – ‘very serious’). A risk perception score was created by averaging the answers to these three items (α = 0.67).
Perceived benefits of COVID-19 vaccination
The perceived efficacy of the COVID-19 vaccine was measured using three items. Participants were asked to rate their level of agreement with the following statements on a scale from 1 (‘totally disagree’) to 5 (‘totally agree’): ‘Getting vaccinated against COVID-19 would be a good way to protect myself against COVID-19’, ‘Getting vaccinated against COVID-19 would be important for the health of others in my community’ and ‘Vaccination against COVID-19 will help end the current pandemic’. A vaccine perceived efficacy score was created by averaging the answers to these three items (α = 0.92).
Perceived barriers to COVID-19 vaccination
COVID-19 vaccine concerns were measured using two items. Participants were asked how much they worried about the side-effects and the rapidity of development of the new COVID-19 vaccine on a scale from 1 (‘not worried at all’) to 5 (‘very worried’). A vaccine concern score was created by averaging the answers to these two items (α = 0.81).
On a scale from 1 (‘totally disagree’) to 5 (‘totally agree’), respondents were asked whether they agreed with three assertions stating that they trust the government, the pharmaceutical industry and science to fight the COVID-19 epidemic and to limit its negative effects and with one assertion stating that they trust official information regarding the number of COVID-19 infections, hospitalizations and deaths in France. The answers to these four questions were averaged to create a trust score (α = 0.78).
To measure the tendency to endorse COVID-19 conspiracy theories, respondents were asked to rate their level of agreement (from 1 – ‘totally disagree’ to 5 – ‘totally agree’) with following three statements chosen based on previous literature.20 , 21
-
1.
COVID-19 was created in a laboratory to reduce the world's population.
-
2.
A vaccine against COVID-19 is available for a long time, but it is being kept secret by the pharmaceutical industry to increase its value.
-
3.
The COVID-19 pandemic is part of a global effort to impose compulsory vaccination.
A mean COVID-19 conspiracy score was calculated by averaging the responses to these three questions (α = 0.84).
Cues to action
We collected information on experience of COVID-19 symptoms (with or without medical confirmation), experience of close contact(s) with COVID-19 cases, risk factors for a severe form of COVID-19 and vaccination history (frequency of uptake of recommended vaccines and uptake of seasonal flu vaccination over the past three years).
Modifying factors
Respondents' risk preference was measured by a single question asking them to rate their willingness to take risk in the health domain on a scale from 0 (‘extremely careful’) to 10 (‘extremely adventurous’). The French-validated 7-item short version of the Consideration of Future Consequences Scale33 was used as a measure of future preference (α = 0.71).
Individual control factors include socio-economic and demographic characteristics (gender, age, region, matrimonial status, education level, whether the respondent works as a health professional, income and size of the residency city, and perceived health status.
Data analysis
A total of 1146 observations were available after quality checks (see Appendix A for details on quality checks performed and participants discarded). The final sample was slightly reweighted to match French official census statistics for gender, age, region, education level and size of residency city. Factors associated with the intention to get vaccinated were estimated using an ordered logistic model. Factors associated with the vaccine attitude categorization (‘vaccine acceptance’, ‘vaccine hesitancy’ and ‘vaccine outright refusal’) were estimated using multinomial logistic regressions using the ‘vaccine acceptance’ category as the base outcome. All regression analyses were run using Stata®, version 15.
Results
Table 1 presents the summary statistics for the dependent and independent variables used in regression analyses. Among our respondents, 30.5% declare they would probably or definitely agree to get vaccinated against COVID-19 if a vaccine were to be approved in France during the first semester of 2021, whereas 31.1% declare being unsure whether they would be willing to get vaccinated. Regarding the COVID-19 vaccine attitude, 25% of respondents are classified in the ‘vaccine acceptance’ category, 60.6% in the ‘vaccine hesitancy’ category and 14.4% in the ‘vaccine outright refusal’ category.
Table 1.
Descriptive statistics.
| Characteristic | Mean (SD) [Min; Max] | N (%) |
|---|---|---|
| Gender | ||
| Female | 637 (55.6%) | |
| Male | 509 (44.4%) | |
| Age | ||
| 20-24 | 79 (6.9%) | |
| 25-34 | 175 (15.3%) | |
| 35-44 | 206 (18.0%) | |
| 45-54 | 198 (17.3%) | |
| 55-64 | 195 (17.0%) | |
| >65 | 293 (25.6%) | |
| Region | ||
| Auvergne-Rhône-Alpes | 161 (14.0%) | |
| Bourgogne-Franche-Comté | 50 (4.4%) | |
| Bretagne | 60 (5.2%) | |
| Centre-Val de Loire | 41 (3.6%) | |
| Grand Est | 88 (7.7%) | |
| Hauts-de-France | 118 (10.3%) | |
| Île-de-France | 231 (20.2%) | |
| Normandie | 37 (3.2%) | |
| Nouvelle-Aquitaine | 92 (8.0%) | |
| Occitanie | 93 (8.1%) | |
| Pays de la Loire | 79 (6.9%) | |
| Provence-Alpes-Côte d'Azur | 96 (8.4%) | |
| Size of residency city | ||
| Less than 10,000 inhabitants | 544 (47.5%) | |
| 10,000 inhabitants or more | 602 (52.5%) | |
| Matrimonial status | ||
| Single | 202 (17.6%) | |
| Civil union or married | 502 (43.8%) | |
| In a relationship | 287 (25.0%) | |
| Divorced or separated | 133 (11.6%) | |
| Widow or widower | 22 (1.9%) | |
| Education | ||
| < A level | 280 (24.4%) | |
| A level | 277 (24.2%) | |
| Two-year university diploma | 241 (21.0%) | |
| >Two-year university diploma | 348 (30.4%) | |
| Monthly income | ||
| <1000 euros | 86 (7.5%) | |
| 1000–2000 euros | 393 (34.3%) | |
| 2000–4000 euros | 443 (38.7%) | |
| >4000 euros | 123 (10.7%) | |
| Not applicable or not wishing to answer | 101 (8.8%) | |
| Health worker | ||
| No | 1073 (93.6%) | |
| Yes | 73 (6.4%) | |
| Perceived health | ||
| Poor or very poor | 101 (8.8%) | |
| Fair | 406 (35.4%) | |
| Good | 465 (40.6%) | |
| Very good | 174 (15.2%) | |
| Risk factors for a severe form of COVID-19 | ||
| No risk factor | 699 (61.0%) | |
| 65 years old or more | 293 (25.6%) | |
| Other risk factors (chronic diseases, pregnant) | 154 (13.4%) | |
| COVID-19 symptoms | ||
| No symptoms | 960 (83.8%) | |
| Symptoms without medical confirmation | 131 (11.4%) | |
| Symptoms with medical confirmation | 55 (4.8%) | |
| COVID-19 close contact | ||
| No | 1046 (91.3%) | |
| At least once | 100 (8.7%) | |
| Flu vaccination | ||
| No | 728 (63.5%) | |
| At least once in the past three years | 418 (36.5%) | |
| Recommended vaccine | ||
| Never | 94 (8.2%) | |
| Hardly | 130 (11.3%) | |
| Sometimes | 226 (19.7%) | |
| Often | 296 (25.8%) | |
| Always | 400 (34.9%) | |
| COVID-19 vaccination intentions | ||
| I would not agree at all | 241 (21.0%) | |
| I probably would not agree | 200 (17.5%) | |
| I would agree or maybe not | 356 (31.1%) | |
| I would probably agree | 197 (17.2%) | |
| I would definitely agree | 152 (13.3%) | |
| COVID-19 vaccine attitude | ||
| Vaccine acceptance | 287 (25.0%) | |
| Vaccine hesitancy | 694 (60.6%) | |
| Vaccine outright refusal | 165 (14.4%) | |
| COVID-19 risk perception score | 3.59 (0.73) [1; 5] | |
| COVID-19 vaccine concern score | 3.91 (0.98) [1; 5] | |
| COVID-19 vaccine efficacy score | 3.37 (1.10) [1; 5] | |
| Trust score | 3.08 (0.90) [1; 5] | |
| COVID-19 conspiracy score | 2.31 (1.11) [1; 5] | |
| Health risk propensity | 3.38 (2.64) [0; 10] | |
| Consideration of Future Consequences scale | 3.33 (0.66) [1; 5] | |
| Observations | 1146 | 1146 |
Table 2 presents the regression analysis results for vaccination intentions and attitudes. Full regression results are available in Table S1 of Appendix B.
Table 2.
Results of regression analyses.
| Vaccination intentions |
Vaccine attitude (Ref: Vaccine acceptance) |
||
|---|---|---|---|
| Vaccine hesitancy | Vaccine outright refusal | ||
| Male | 1.471∗ | 0.606∗ | 0.595 |
| (Ref: Female) |
[1.091, 1.984] |
[0.374, 0.982] |
[0.281, 1.258] |
| Perceived health (Ref: Poor or very poor) | |||
| Fair | 1.516 | 0.717 | 0.576 |
| [0.816, 2.819] | [0.294, 1.748] | [0.129, 2.568] | |
| Good | 1.274 | 1.096 | 2.881 |
| [0.676, 2.401] | [0.418, 2.872] | [0.637, 13.035] | |
| Very good | 0.923 | 1.290 | 7.205∗ |
| [0.464, 1.835] | [0.421, 3.949] | [1.447, 35.876] | |
| COVID-19 risk factors (Ref: none) | |||
| 65 years old and more | 1.569 | 1.123 | 0.370 |
| [0.759, 3.245] | [0.359, 3.515] | [0.074, 1.854] | |
| Other risk factors (chronic disease, pregnant) | 1.817∗ | 0.812 | 0.650 |
| [1.085, 3.042] | [0.401, 1.645] | [0.211, 2.003] | |
| Flu vaccination (Ref: Not in the past 3 years) | |||
| At least once in the past 3 years | 2.004∗∗∗ | 0.406∗∗ | 0.209∗∗ |
| [1.406, 2.857] | [0.236, 0.698] | [0.073, 0.597] | |
| Recommended vaccines (Ref: Never) | |||
| Rarely | 1.637 | 0.262 | 0.0654∗∗ |
| [0.857, 3.127] | [0.051, 1.352] | [0.010, 0.413] | |
| Sometimes | 1.915∗ | 0.276 | 0.0485∗∗∗ |
| [1.023, 3.584] | [0.068, 1.116] | [0.009, 0.268] | |
| Often | 3.194∗∗∗ | 0.201∗ | 0.0248∗∗∗ |
| [1.805, 5.653] | [0.054, 0.753] | [0.005, 0.125] | |
| Always | 3.734∗∗∗ | 0.141∗∗ | 0.0157∗∗∗ |
| [2.003, 6.959] | [0.038, 0.528] | [0.003, 0.085] | |
| COVID-19 risk perception score | 1.342∗ | 0.537∗∗ | 0.589 |
| [1.001, 1.799] | [0.353, 0.818] | [0.320, 1.084] | |
| COVID-19 vaccine concern score | 0.343∗∗∗ | 3.668∗∗∗ | 5.632∗∗∗ |
| [0.280, 0.420] | [2.741, 4.908] | [3.216, 9.863] | |
| COVID-19 vaccine efficacy score | 4.848∗∗∗ | 0.307∗∗∗ | 0.0485∗∗∗ |
| [3.612, 6.506] | [0.192, 0.492] | [0.026, 0.091] | |
| Trust score | 1.344∗ | 0.866 | 0.704 |
| [1.067, 1.693] | [0.622, 1.205] | [0.414, 1.195] | |
| COVID-19 conspiracy score | 1.101 | 0.864 | 1.070 |
| [0.944, 1.284] | [0.680, 1.098] | [0.748, 1.531] | |
| Health risk propensity | 1.022 | 0.890∗ | 0.978 |
| [0.968, 1.080] | [0.809, 0.979] | [0.845, 1.132] | |
| Consideration of Future Consequences Scale | 1.267∗ | 1.239 | 0.946 |
| [1.012, 1.588] | [0.841, 1.826] | [0.502, 1.783] | |
| Observations | 1146 | 1146 | 1146 |
| Pseudo R-squared | 0.377 | 0.509 | 0.509 |
Results are presented as odd ratios with 95% confidence interval in brackets. An odd ratio between 0 and 1 indicates a negative association. An odd ratio greater than 1 indicates a positive association.
∗P < 0.05, ∗∗P < 0.01, ∗∗∗P < 0.001.
Male and respondents with COVID-19 risk factors other than age report a higher willingness to get vaccinated. Previous vaccination history is strongly associated with the intention to get vaccinated against COVID-19. The COVID-19 risk perception score is positively and significantly associated with vaccination intentions. The vaccine perceived efficacy score is strongly and positively associated with the willingness to get vaccinated, whereas the vaccine concern score is strongly and negatively associated with COVID-19 vaccination intentions. We find a positive and significant association between the trust score and the willingness to get vaccinated. Future preference is significantly associated with COVID-19 vaccination intentions.
Women are more often vaccine hesitant compared to men. Respondents who got vaccinated against seasonal flu at least once in the last three years and those who more often get vaccinated when recommended are less likely to belong to the ‘vaccine hesitancy’ or ‘vaccine outright refusal’ categories. Respondents who consider their health as very good are more likely to belong to the ‘vaccine outright refusal’ category. The COVID-19 risk perception score is lower among vaccine hesitant respondents than among vaccine acceptors. Respondents in the ‘vaccine hesitancy’ or ‘vaccine outright refusal’ categories tend to have a higher vaccine concern score and a lower vaccine efficacy score than vaccine acceptors. Finally, we find that respondents in the ‘vaccine acceptance’ category declare being more willing to take risks in the health domain compared to vaccine hesitant respondents.
Discussion
Only 30.5% of our respondents would probably or definitely agree to get vaccinated against COVID-19, whereas 31.1% declare being unsure whether they would be willing to get vaccinated. In line with studies available for France,21, 22, 23 we find that women have lower COVID-19 vaccination intentions which is problematic as they are overrepresented among caregivers of dependent elderly in France.34 Moreover, given the key role played by women in childhood vaccinations, COVID-19 vaccine hesitancy among women is of worry at the time COVID-19 vaccination is opening to children under 18 in France. Among respondents at risk of a severe form of COVID-19, vaccination intentions are higher for pregnant women and for respondents with chronic diseases but not for respondents older than 65 years. Respondents who frequently get vaccinated also express higher intentions to get vaccinated against COVID-19 and are less likely to be vaccine hesitant. However, the pool of people getting vaccinated against COVID-19 needs to be extended far beyond at-risk individuals and those usually in favour of vaccination to create herd immunity in France.
Similar to Detoc et al.21 or Ward et al.,23 we find higher vaccination intentions and lower COVID-19 vaccine hesitancy among respondents with elevated COVID-19 risk perception. Moreover, the perceived individual and collective benefits of the vaccine and the concerns over its safety are strongly associated with COVID-19 vaccination intentions. The magnitude and level of significance of the associations between the intention and lower COVID-19 vaccine hesitancy vaccine perceptions and COVID-19 vaccination intentions/attitudes are higher than those observed for COVID-19 risk perceptions. This seems to indicate that vaccine perceptions play a greater role in the willingness to get vaccinated than COVID-19 risk perceptions. Similar to results obtained in the United States16 or Italy,17 we also find that distrust in the government, the pharmaceutical industry or science for the management of the COVID-19 epidemic is associated with lower vaccination intentions.
Our results are in line with previous studies using the HBM to investigate vaccination intentions. Indeed, a meta-analysis of studies using the HBM found that risk likelihood, susceptibility, and severity significantly predicted vaccination behaviours35 while we also find that the perceived threat is significantly associated with COVID-19 vaccination intentions. Moreover, the strong associations we find between the perceived efficacy/concerns regarding the COVID-19 vaccines and vaccination intentions/attitudes are consistent with a recent scooping review which highlighted that of the four main HBM constructs, perceived barriers and perceived benefits were the strongest predictors of health-related behavioural changes.36 More specifically, as found for COVID-19 vaccination intentions and attitudes in this study, previous literature on vaccination behaviours during epidemic contexts, such as H1N1 or influenza, highlighted the importance of the perceived barriers31 , 37 and perceived benefits38 , 39 of the vaccine on vaccination uptake. Very recently, and in concordance with our results, other studies investigating COVID-19 vaccination intentions using the HBM theoretical framework also emphasized the importance of perceived severity, perceived vaccine benefits and perceived barriers to vaccination on vaccination acceptance.30 , 40 , 41
Taken together, our results on the HBM variables suggest that targeted communication campaigns should be launched to enhance trust in the newly developed vaccines and to increase vaccination uptake among vaccine hesitant populations. Convincing vaccine hesitant populations to get vaccinated against COVID-19 is indeed crucial to reduce the level of circulation of the virus and to prevent the emergence of variants against which the currently available vaccines might be less effective. Given the observed concern over the rapidity of development, these campaigns could explain how the rapid progresses on the COVID-19 vaccines were made possible by unprecedented research efforts and financing (including government financing), by previous scientific knowledge on coronaviruses and on vaccine development for other pathogens and by the rapid genetic sequencing of this new coronavirus that allowed the subsequent development of messenger RNA vaccines. Public health authorities should also explain that, while accelerated trial procedures allowed for a rapid assessment of COVID-19 vaccines by health technology agencies, safety and efficacy routine checks were performed as scrupulously as done for any other drugs or vaccines seeking market authorisation.
The positive association we find between the propensity to take risk in the health domain and the willingness to get vaccinated quickly (i.e., in less than three months) is worrisome as it indicates that the COVID-19 vaccine is perceived by some respondents as a greater health risk than the COVID-19 itself. Then, it appears important for information campaigns to underline the positive benefit-risk balance of the COVID-19 vaccines by stressing out the risks associated with a COVID-19 infection and how much these risks can be reduced thanks to vaccination. Such information campaigns will enhance vaccination uptake among both individuals with a low COVID-19 risk perception and those currently perceiving the COVID-19 vaccine as a greater health risk than the COVID-19 itself.
As previously found for flu vaccination42, 43, 44 or H1N1 influenza vaccination38 our regression results also point to a positive association between future preference and COVID-19 vaccination intentions. This indicates that respondents who are more present-oriented are less likely to get vaccinated against COVID-19. To heighten vaccination uptake among present-oriented individuals, information campaigns could stress out the short-term benefits of the COVID-19 vaccination, for example by highlighting how COVID-19 vaccination will allow travelling across Europe and attending large gatherings or events. Reducing the sort-term opportunity cost of the COVID-19 vaccination, for example by offering vaccines at the workplace or at the location of summer holidays, could also enhance vaccination uptake among present-oriented individuals.
Our study is not without limitation. First, the cross-sectional design used in this study does not allow the identification of causal effects. Second, our results regarding the intentions to get vaccinated are not directly comparable to those of previous studies2 , 23 as we included a neutral response modality (‘I would maybe agree to get vaccinated or maybe not’) to this question, whereas previous studies did not. Further studies, preferably using longitudinal designs, should be conducted to study the factors associated with COVID-19 vaccination intentions in France.
Carefully designing targeted vaccination awareness campaigns appears crucial for public decision-makers to enhance vaccination uptake among vaccine hesitant individuals to reach herd immunity in France. These campaigns could stress out the positive benefit-risk balance of the COVID-19 vaccines, reinsure the public on the safety of the vaccine and highlight the short-term benefits of the vaccination.
Author statements
Ethical approval
Given strict anonymity of collected data, the study did not need authorization of the Commission Nationale de l'Informatique et des Libertés (CNIL).
Funding
This research benefited from a funding from the research unit of the authors, Montpellier Recherche en Economie, for data collection. The funding source had no role in study design, data analysis, interpretation of data, nor in the writing of the manuscript or in the decision to submit the article for publication.
Competing interests
None declared.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2021.07.035.
Appendix A. Supplementary data
The following is/are the Supplementary data to this article:
References
- 1.Santé Publique France . 2020. COVID-19 Point épidémiologique hebdomadaire du 03 décembre 2020.https://www.santepubliquefrance.fr/maladies-et-traumatismes/maladies-et-infections-respiratoires/infection-a-coronavirus/documents/bulletin-national/covid-19-point-epidemiologique-du-3-decembre-2020 [Google Scholar]
- 2.Ifop. Balises d’opinion #119 Questions d’actualité : regards sur la police/Intention de se faire vacciner contre la Covid-19. 2 https://www.ifop.com/wp-content/uploads/2020/12/117000-Rapport-CN-SR-N119.pdf.
- 3.Bone A., Guthmann J.P., Nicolau J., Lévy-Bruhl D. Population and risk group uptake of H1N1 influenza vaccine in mainland France 2009-2010: results of a national vaccination campaign. Vaccine. 2010 Nov 29;28(51):8157–8161. doi: 10.1016/j.vaccine.2010.09.096. [DOI] [PubMed] [Google Scholar]
- 4.Bocquier A., Fressard L., Galtier F., Verger P. Influenza vaccine coverage trends among targeted groups from 2006 to 2015, in France: Aurélie Bocquier. Eur J Public Health. 2017;27(suppl_3) doi: 10.1093/eurpub/ckx187.115. ckx187.15-ckx.15. [DOI] [Google Scholar]
- 5.Rey D., Fressard L., Cortaredona S., Bocquier A., Gautier A., Peretti-Watel P., et al. Vaccine hesitancy in the French population in 2016, and its association with vaccine uptake and perceived vaccine risk-benefit balance. Euro Surveill. 2018 Apr;23(17) doi: 10.2807/1560-7917.ES.2018.23.17.17-00816. 17-00816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Verger P., Fressard L., Collange F., Gautier A., Jestin C., Launay O., et al. Vaccine hesitancy among general practitioners and its determinants during controversies: a national cross-sectional survey in France. EBioMedicine. 2015 Jun 23;2(8):891–897. doi: 10.1016/j.ebiom.2015.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson R.M., Vegvari C., Truscott J., Collyer B.S. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020 Nov 21;396(10263):1614–1616. doi: 10.1016/S0140-6736(20)32318-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Malik A.A., McFadden S.M., Elharake J., Omer S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020 Sep;26:100495. doi: 10.1016/j.eclinm.2020.100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rhodes A., Hoq M., Measey M.A., Danchin M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2020 Sep 14;S1473-S3099(20):30724–30726. doi: 10.1016/S1473-3099(20)30724-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paul E., Steptoe A., Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communication. Lancet Reg Health Eur. 2021 doi: 10.1016/j.lanepe.2020.100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dror A.A., Eisenbach N., Taiber S., Morozov N.G., Mizrachi M., Zigron A., et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020 Aug;35(8):775–779. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams L., Gallant A.J., Rasmussen S., Brown Nicholls L.A., Cogan N., et al. Towards intervention development to increase the uptake of COVID-19 vaccination among those at high risk: outlining evidence-based and theoretically informed future intervention content. Br J Health Psychol. 2020 Nov;25(4):1039–1054. doi: 10.1111/bjhp.12468. [DOI] [PubMed] [Google Scholar]
- 13.Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020 Sep 29;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sherman S.M., Smith L.E., Sim J., Amlôt R., Cutts M., Dasch H., et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2020 Nov 26:1–10. doi: 10.1080/21645515.2020.1846397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020 Sep;21(7):977–982. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fisher K.A., Bloomstone S.J., Walder J., Crawford S., Fouayzi H., Mazor K.M. Attitudes toward a potential SARS-CoV-2 vaccine : a survey of U.S. Adults. Ann Intern Med. 2020 Dec 15;173(12):964–973. doi: 10.7326/M20-3569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. Eur J Epidemiol. 2020 Aug;35(8):785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romer D., Jamieson K.H. Conspiracy theories as barriers to controlling the spread of COVID-19 in the U.S. Soc Sci Med. 2020 Oct;263:113356. doi: 10.1016/j.socscimed.2020.113356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Earnshaw V.A., Eaton L.A., Kalichman S.C., Brousseau N.M., Hill E.C., Fox A.B. COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl Behav Med. 2020 Oct 8;10(4):850–856. doi: 10.1093/tbm/.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruiz J.B., Bell R.A. Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021 Feb 12;39(7):1080–1086. doi: 10.1016/j.vaccine.2021.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Detoc M., Bruel S., Frappe P., Tardy B., Botelho-Nevers E., Gagneux-Brunon A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine. 2020 Oct 21;38(45):7002–7006. doi: 10.1016/j.vaccine.2020.09.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.COCONEL Group A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis. 2020 Jul;20(7):769–770. doi: 10.1016/S1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ward J.K., Alleaume C., Peretti-Watel P., COCONEL Group The French public's attitudes to a future COVID-19 vaccine: the politicization of a public health issue. Soc Sci Med. 2020 Nov;265:113414. doi: 10.1016/j.socscimed.2020.113414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schwarzinger M., Watson V., Arwidson P., Alla F., Luchini S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021;6(4):e210–e221. doi: 10.1016/S2468-2667(21)00012-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bertin P., Nera K., Delouvée S. Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front Psychol. 2020 Sep 18;11:565128. doi: 10.3389/fpsyg.2020.565128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gagneux-Brunon A., Detoc M., Bruel S., Tardy B., Rozaire O., Frappe P., et al. Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J Hosp Infect. 2021 Feb;108:168–173. doi: 10.1016/j.jhin.2020.11.020. Epub 2020 Nov 28. PMID: 33259883; PMCID: PMC7699157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MacDonald N.E. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 28.Rosenstock I.M. Why people use health services. Milbank Mem Fund Q. 1966 Jul;44(3):94–127. doi: 10.1111/j.1468-0009.2005.00425.x. Suppl. [DOI] [PubMed] [Google Scholar]
- 29.Janz N.K., Becker M.H. The health belief model: a decade later. Health Educ Q. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 30.Lin Y., Hu Z., Zhao Q., Alias H., Danaee M., Wong L.P. In: Marques E.T.A., editor. vol. 14. 2020. Understanding COVID-19 vaccine demand and hesitancy: a nationwide online survey in China. (PLoS Negl Trop Dis). (12) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Santos A.J., Kislaya I., Machado A., Nunes B. Beliefs and attitudes towards the influenza vaccine in high-risk individuals. Epidemiol Infect. 2017;145(9):1786–1796. doi: 10.1017/S0950268817000814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mercadante A.R., Law A.V. Will they, or Won't they? Examining patients' vaccine intention for flu and COVID-19 using the Health Belief Model. Res Soc Adm Pharm. 2021 doi: 10.1016/j.sapharm.2020.12.012. Published online December 2020:S1551741120312407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Demarque C., Apostolidis T., Chagnard A., Dany L. Adaptation et validation française de l’échelle de perspective temporelle «Consideration of future consequences» (CFC) Bull Psychol. 2010:351–360. doi: 10.3917/bupsy.509.0351. [DOI] [Google Scholar]
- 34.Besnard X., Brune M., Couvert N., Roy D. 2019. Les proches aidants des seniors et leur ressenti sur l’aide apportée. Résultats des enquêtes «CARE» auprès des aidants (2015-2016. [Google Scholar]
- 35.Brewer N.T., Chapman G.B., Gibbons F.X., Gerrard M., McCaul K.D., Weinstein N.D. Meta-analysis of the relationship between risk perception and health behavior: the example of vaccination. Health Psychol. 2007;26(2):136–145. doi: 10.1037/0278-6133.26.2.136. [DOI] [PubMed] [Google Scholar]
- 36.Sulat J.S., Prabandari Y.S., Sanusi R., Hapsari E.D., Santoso B. The validity of health belief model variables in predicting behavioral change: a scoping review. Health Edu. 2018;118(6):499–512. doi: 10.1108/HE-05-2018-0027. [DOI] [Google Scholar]
- 37.Scherr C.L., Jensen J.D., Christy K. Dispositional pandemic worry and the health belief model: promoting vaccination during pandemic events. J Public Health. 2016;27 doi: 10.1093/pubmed/fdw101. Published online September. jphm;fdw101v2. [DOI] [PubMed] [Google Scholar]
- 38.Nan X., Kim J. Predicting H1N1 vaccine uptake and H1N1-related health beliefs: the role of individual difference in consideration of future consequences. J Health Commun. 2014;19(3):376–388. doi: 10.1080/10810730.2013.821552. [DOI] [PubMed] [Google Scholar]
- 39.Alhalaseh L., Fayoumi H., Khalil B. The Health Belief Model in predicting healthcare workers' intention for influenza vaccine uptake in Jordan. Vaccine. 2020;38(46):7372–7378. doi: 10.1016/j.vaccine.2020.09.002. [DOI] [PubMed] [Google Scholar]
- 40.Wong MC, Wong EL, Huang J, Cheung AW, Law K, Chong MK, et al. Acceptance of the COVID-19 vaccine based on the health belief model: a population-based survey in Hong Kong. Vaccine. 2021;39(7):1148–1156. doi: 10.1016/j.vaccine.2020.12.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wong L.P., Alias H., Wong P.-F., Lee H.Y., AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccine Immunother. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chapman G.B., Coups E.J. Time preferences and preventive health behavior: acceptance of the influenza vaccine. Med Decis Making. 1999 Jul-Sep;19(3):307–314. doi: 10.1177/0272989X9901900309. [DOI] [PubMed] [Google Scholar]
- 43.Tsutsui Y., Benzion U., Shahrabani S., Din G.Y. A policy to promote influenza vaccination: a behavioral economic approach. Health Pol. 2010 Oct;97(2–3):238–249. doi: 10.1016/j.healthpol.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 44.Nuscheler R., Roeder K. To vaccinate or to procrastinate? That is the prevention question. Health Econ. 2016 Dec;25(12):1560–1581. doi: 10.1002/hec.3268. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.