Abstract
Background
Psoriasis is an immune‐mediated disease for which some people have a genetic predisposition. The condition manifests in inflammatory effects on either the skin or joints, or both, and it has a major impact on quality of life. Although there is currently no cure for psoriasis, various treatment strategies allow sustained control of disease signs and symptoms. Several randomised controlled trials (RCTs) have compared the efficacy of the different systemic treatments in psoriasis against placebo. However, the relative benefit of these treatments remains unclear due to the limited number of trials comparing them directly head‐to‐head, which is why we chose to conduct a network meta‐analysis.
Objectives
To compare the efficacy and safety of non‐biological systemic agents, small molecules, and biologics for people with moderate‐to‐severe psoriasis using a network meta‐analysis, and to provide a ranking of these treatments according to their efficacy and safety.
Search methods
For this living systematic review we updated our searches of the following databases monthly to September 2020: the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, and Embase. We searched two trials registers to the same date. We checked the reference lists of included studies and relevant systematic reviews for further references to eligible RCTs.
Selection criteria
Randomised controlled trials (RCTs) of systemic treatments in adults (over 18 years of age) with moderate‐to‐severe plaque psoriasis or psoriatic arthritis whose skin had been clinically diagnosed with moderate‐to‐severe psoriasis, at any stage of treatment, in comparison to placebo or another active agent. The primary outcomes of this review were: the proportion of participants who achieved clear or almost clear skin, that is, at least Psoriasis Area and Severity Index (PASI) 90 at induction phase (from 8 to 24 weeks after the randomisation), and the proportion of participants with serious adverse events (SAEs) at induction phase. We did not evaluate differences in specific adverse events.
Data collection and analysis
Several groups of two review authors independently undertook study selection, data extraction, 'Risk of bias' assessment, and analyses. We synthesised the data using pair‐wise and network meta‐analysis (NMA) to compare the treatments of interest and rank them according to their effectiveness (as measured by the PASI 90 score) and acceptability (the inverse of serious adverse events).
We assessed the certainty of the body of evidence from the NMA for the two primary outcomes and all comparisons, according to CINeMA, as either very low, low, moderate, or high. We contacted study authors when data were unclear or missing.
We used the surface under the cumulative ranking curve (SUCRA) to infer on treatment hierarchy: 0% (treatment is the worst for effectiveness or safety) to 100% (treatment is the best for effectiveness or safety).
Main results
We included 158 studies (18 new studies for the update) in our review (57,831 randomised participants, 67.2% men, mainly recruited from hospitals). The overall average age was 45 years; the overall mean PASI score at baseline was 20 (range: 9.5 to 39). Most of these studies were placebo‐controlled (58%), 30% were head‐to‐head studies, and 11% were multi‐armed studies with both an active comparator and a placebo. We have assessed a total of 20 treatments. In all, 133 trials were multicentric (two to 231 centres). All but two of the outcomes included in this review were limited to the induction phase (assessment from 8 to 24 weeks after randomisation). We assessed many studies (53/158) as being at high risk of bias; 25 were at an unclear risk, and 80 at low risk. Most studies (123/158) declared funding by a pharmaceutical company, and 22 studies did not report their source of funding.
Network meta‐analysis at class level showed that all of the interventions (non‐biological systemic agents, small molecules, and biological treatments) were significantly more effective than placebo in reaching PASI 90.
At class level, in reaching PASI 90, the biologic treatments anti‐IL17, anti‐IL12/23, anti‐IL23, and anti‐TNF alpha were significantly more effective than the small molecules and the non‐biological systemic agents.
At drug level, infliximab, ixekizumab, secukinumab, brodalumab, risankizumab and guselkumab were significantly more effective in reaching PASI 90 than ustekinumab and three anti‐TNF alpha agents: adalimumab, certolizumab, and etanercept. Ustekinumab and adalimumab were significantly more effective in reaching PASI 90 than etanercept; ustekinumab was more effective than certolizumab, and the clinical effectiveness of ustekinumab and adalimumab was similar. There was no significant difference between tofacitinib or apremilast and three non‐biological drugs: fumaric acid esters (FAEs), ciclosporin and methotrexate.
Network meta‐analysis also showed that infliximab, ixekizumab, risankizumab, bimekizumab, secukinumab, guselkumab, and brodalumab outperformed other drugs when compared to placebo in reaching PASI 90. The clinical effectiveness of these drugs was similar, except for ixekizumab which had a better chance of reaching PASI 90 compared with secukinumab, guselkumab and brodalumab. The clinical effectiveness of these seven drugs was: infliximab (versus placebo): risk ratio (RR) 50.29, 95% confidence interval (CI) 20.96 to 120.67, SUCRA = 93.6; high‐certainty evidence; ixekizumab (versus placebo): RR 32.48, 95% CI 27.13 to 38.87; SUCRA = 90.5; high‐certainty evidence; risankizumab (versus placebo): RR 28.76, 95% CI 23.96 to 34.54; SUCRA = 84.6; high‐certainty evidence; bimekizumab (versus placebo): RR 58.64, 95% CI 3.72 to 923.86; SUCRA = 81.4; high‐certainty evidence; secukinumab (versus placebo): RR 25.79, 95% CI 21.61 to 30.78; SUCRA = 76.2; high‐certainty evidence; guselkumab (versus placebo): RR 25.52, 95% CI 21.25 to 30.64; SUCRA = 75; high‐certainty evidence; and brodalumab (versus placebo): RR 23.55, 95% CI 19.48 to 28.48; SUCRA = 68.4; moderate‐certainty evidence. Conservative interpretation is warranted for the results for bimekizumab (as well as mirikizumab, tyrosine kinase 2 inhibitor, acitretin, ciclosporin, fumaric acid esters, and methotrexate), as these drugs, in the NMA, have been evaluated in few trials.
We found no significant difference between any of the interventions and the placebo for the risk of SAEs. Nevertheless, the SAE analyses were based on a very low number of events with low to moderate certainty for all the comparisons. Thus, the results have to be viewed with caution and we cannot be sure of the ranking.
For other efficacy outcomes (PASI 75 and Physician Global Assessment (PGA) 0/1) the results were similar to the results for PASI 90.
Information on quality of life was often poorly reported and was absent for several of the interventions.
Authors' conclusions
Our review shows that compared to placebo, the biologics infliximab, ixekizumab, risankizumab, bimekizumab, secukinumab, guselkumab and brodalumab were the most effective treatments for achieving PASI 90 in people with moderate‐to‐severe psoriasis on the basis of moderate‐ to high‐certainty evidence. This NMA evidence is limited to induction therapy (outcomes were measured from 8 to 24 weeks after randomisation) and is not sufficient for evaluation of longer‐term outcomes in this chronic disease. Moreover, we found low numbers of studies for some of the interventions, and the young age (mean age of 45 years) and high level of disease severity (PASI 20 at baseline) may not be typical of patients seen in daily clinical practice.
Another major concern is that short‐term trials provide scanty and sometimes poorly‐reported safety data and thus do not provide useful evidence to create a reliable risk profile of treatments. We found no significant difference in the assessed interventions and placebo in terms of SAEs, and the evidence for all the interventions was of low to moderate quality. In order to provide long‐term information on the safety of the treatments included in this review, it will also be necessary to evaluate non‐randomised studies and postmarketing reports released from regulatory agencies.
In terms of future research, randomised trials directly comparing active agents are necessary once high‐quality evidence of benefit against placebo is established, including head‐to‐head trials amongst and between non‐biological systemic agents and small molecules, and between biological agents (anti‐IL17 versus anti‐IL23, anti‐IL23 versus anti‐IL12/23, anti‐TNF alpha versus anti‐IL12/23). Future trials should also undertake systematic subgroup analyses (e.g. assessing biological‐naïve participants, baseline psoriasis severity, presence of psoriatic arthritis, etc.). Finally, outcome measure harmonisation is needed in psoriasis trials, and researchers should look at the medium‐ and long‐term benefit and safety of the interventions and the comparative safety of different agents.
Editorial note: This is a living systematic review. Living systematic reviews offer a new approach to review updating, in which the review is continually updated, incorporating relevant new evidence as it becomes available. Please refer to the Cochrane Database of Systematic Reviews for the current status of this review.
Plain language summary
Which medicines, taken by mouth or injected, work best to treat a skin condition called plaque psoriasis?
Key messages
‐ After six months of treatment, medicines called 'biologics' seem to work best to clear patches of psoriasis on the skin.
‐ Longer studies are needed to assess the benefits and potential harms of longer treatment with medicines that are injected or taken by mouth to treat psoriasis.
‐ More studies are needed that compare these types of medicines directly against each other.
What is psoriasis?
Psoriasis is an immune condition that affects the skin, and sometimes the joints. Psoriasis speeds up the production of new skin cells, which build up to form raised patches on the skin known as 'plaques'. Plaques can also be flaky, scaly, itchy, and appear red on white skin, and as darker patches on darker skin tones. Plaque psoriasis is the most common form of psoriasis.
How is psoriasis treated?
Treatments for psoriasis depend on how bad the symptoms are. Around 10% to 20% of people with moderate or severe psoriasis will need to take medicines that affect their immune system, to help control the psoriasis. These medicines are called systemic treatments, because they affect the whole body. These are usually taken by mouth (oral) or injected.
Why did we do this Cochrane Review?
There are three different types of systemic medicines to treat psoriasis:
‐ 'biologics' ‐ proteins, such as antibodies, that affect biological targets called interleukins and cytokines (parts of the immune system that affect how cells behave); ‐ small molecules ‐ organic compounds that affect immune cells; examples include apremilast and tofacitinib; and ‐ non‐biologic medicines ‐ medicines that have been in use for a long time to treat psoriasis, such as methotrexate, ciclosporin and retinoids.
We wanted to find out about the benefits and potential harms of taking systemic medicines to treat psoriasis, and to see if some medicines work better than others.
What did we do?
We searched for studies that tested systemic medicines to treat plaque psoriasis.
How up to date is this review?
We include evidence up to September 2020.
What did we find?
We found 158 studies, including 18 new studies, since our last search. The studies tested 20 different medicines, covering 57,831 people with psoriasis (average age 45 years) and lasted from 2 to 6 months. Of 132 studies that reported their source of funding, a pharmaceutical company provided funding for 123 studies and nine were funded by non‐commercial organisations or academic institutions.
Most studies compared the systemic medicine against a placebo (a 'dummy' treatment that does not contain any medicine but looks identical to the medicine being tested). They used a common measurement scale called the PASI (psoriasis area and severity index) to compare how well each medicine cleared psoriasis plaques from the skin, looking for a 90% improvement (called 'PASI 90'). Few studies reported on participants' well‐being.
We compared all the medicines with each other using a mathematical method called a network meta‐analysis.
What are the main results of our review?
All the medicines tested worked better than a placebo to treat psoriasis (measured as a 90% improvement in PASI).
Biologic medicines (that targeted interleukins 17, 23 and 12/23, and the cytokine TNF‐alpha) treated psoriasis better than the small‐molecule and non‐biologic medicines.
Compared with placebo, seven biologic medicines worked best to treat psoriasis, with little difference between them:
‐ infliximab (targets TNF‐alpha);
‐ ixekizumab, bimekizumab, secukinumab and brodalumab (target interleukin‐17); and
‐ risankizumab and guselkumab (target interleukin‐23).
We found no significant difference in the numbers of serious unwanted effects for all systemic medicines tested when compared with a placebo. However, the studies did not consistently report results about safety, such as serious unwanted effects. We therefore could not create a reliable risk profile of systemic medicines.
Limitations of the evidence
We are confident in our results for the seven biologic medicines that worked best to treat psoriasis. We are less confident in our results for serious unwanted effects, because of the low number of unwanted effects reported.
We are also less confident in the results for the non‐biologic medicines because of concerns about how some of the studies were conducted. Further research is likely to change these results.
We did not find many studies for some of the 20 medicines included in our review. Participants in the studies often had severe psoriasis at the start of the study, so our results may not be useful for people whose psoriasis is less severe. Our findings relate only to treatment with systemic medicines for up to six months at most.
Editorial note: This is a living systematic review. Living systematic reviews offer a new approach to review updating, in which the review is continually updated, incorporating relevant new evidence as it becomes available. Please refer to the Cochrane Database of Systematic Reviews for the current status of this review.
Background
Please refer to our glossary (see Table 1).
1. Glossary.
| Term | Definition |
| Antagonist | A substance that interferes with or inhibits the physiological action of another. |
| Antigen | A molecule capable of inducing an immune response |
| Anti‐TNF alpha | A pharmaceutical drug that suppresses the physiologic response to tumour necrosis factor (TNF) |
| Biological agent | Therapeutic agents consisting of immune molecules such as soluble receptors, recombinant cytokines, and monoclonal antibodies that target effector molecules or cells of the immune system |
| Biosimilar | Biological agent highly similar to another already‐approved biological medicine |
| CD6 | Cluster of differentiation (CD) 6 is a protein encoded by the CD6 gene |
| Cheilitis | An inflammation of the lips |
| Chimeric protein | A chimeric protein can be made by combining two different genes |
| Complex cyclophilin‐ciclosporin | Cyclophilins are a family of proteins that bind to ciclosporin, an immunosuppressant agent |
| Creatinine | A compound that is produced by metabolism of creatine and excreted in the urine |
| Cyclic adenosine monophosphate | It is a second messenger important in many biological processes |
| Cytokines | Small proteins produced by a broad range of cells that are important in cell signalling; they are immunomodulating agents |
| Dendritic cells | Antigen‐presenting cells of the immune system |
| Dermis | It is a layer of the skin |
| Epitope | It is a part of an antigen |
| Erythematous | Redness of the skin |
| Folic acid | B vitamin |
| Humanised antibody | Antibodies from non‐human species whose protein sequences have been modified to increase their similarity to antibody variants produced naturally in humans |
| IL‐17A | A pro‐inflammatory cytokine |
| IL‐23R | A cytokine receptor |
| Immune‐mediated | A group of diseases that are characterised by common inflammatory pathways leading to inflammation, and which may result from a dysregulation of the normal immune response |
| Immunogenicity | This is the ability of a particular substance, such as an antigen or epitope, to provoke an immune response in the body of a human or animal |
| Immunoglobulin 1 Fc | An antibody |
| Interferon (IFN)‐c | A protein released by cells, usually in response to a pathogen |
| Interleukin | A kind of cytokine |
| Janus kinase (JAK) inhibitors | A pharmaceutical drug that inhibits the activity of one or more of the Janus kinase family of enzymes |
| Keratinocytes | Epidermal cells that constitute 95% of the epidermis |
| Lymphocyte | A subtype of a white blood cell |
| Lymphoid organ | Part of the body that defends the body against invading pathogens that cause infections or the spread of tumours |
| Metalloproteinases | A protease enzyme |
| Monoclonal antibodies | Antibodies that are made by identical immune cells that are all clones of a unique parent cell |
| Murine sequence | Mouse genomic sequencing |
| Neutrophils | Type of white blood cell involved in the innate immune system |
| p40 | Subunit beta of interleukin 12 and 23 |
| Periumbilical | Around the navel |
| Pharmacological treatments | Drugs |
| Phase I | First‐in‐man studies |
| Phase II | Studies to assess how well the drug works, as well as to continue phase I safety assessments in a larger group of volunteers and participants |
| Phase III | Randomised controlled multicenter trials on large patient groups and are aimed at being the definitive assessment of how effective the drug is |
| Phase IV | Post‐marketing trials involve the safety surveillance |
| Phosphodiesterase 4 inhibitors | A pharmaceutical drug used to block the degradative action of phosphodiesterase 4 |
| Progressive multifocal leukoencephalopathy | A rare viral neurological disease characterised by progressive damage of the white matter of the brain at multiple locations |
| Receptor | A protein molecule that receives chemical signals from outside a cell |
| Small molecules | Chemically manufactured molecules (or SMOLs for short) |
| Sphingosine 1‐phosphate receptor agonists | A class of protein‐coupled receptors that are targets of the lipid signalling molecule Sphingosine‐1‐phosphate |
| T cells/CD4 T cells | A type of white blood cell that is of key importance to the immune system |
| Th1 and Tc1 cells | A type of T cell |
| Th17 and Tc17 cells | A type of T cell |
| TNF‐alpha | A protein that is part of the inflammatory response |
| Tumour necrosis factor antagonists | Class of biological agents |
| Umbilic | Navel |
| Xerosis | Dry skin |
Description of the condition
Psoriasis is an immune‐mediated disease for which a person can have genetic susceptibility, manifesting in chronic inflammatory effects on either the skin or joints, or both, with a prevalence ranging from 2.2% (USA) to 8.5% (Norway) (Boehncke 2015; Parisi 2013; Stern 2004). The causes of psoriasis are not fully understood. There appears to be interaction between environmental factors and genetic susceptibility. Genome‐wide (or whole genome) association trials found several candidate genes relating to psoriasis (Capon 2017; Elder 2010). Various environmental factors, including stress, injury, and infections, are suspected of triggering or aggravating the evolution of psoriasis. An inflammatory immune response involving dendritic cells, T cells, keratinocytes, neutrophils, and the cytokines released from immune cells initiates the pathophysiological process (Jariwala 2007; Lowes 2008; Wilson 2007; Zheng 2007).
Diagnosis is made based on clinical findings; skin biopsy is rarely used to diagnose the disease (Boehncke 2015). Several clinical types of psoriasis exist: plaque, pustular, inverse, and erythrodermic. Plaque psoriasis is the most common form, affecting 90% of people with psoriasis (Griffiths 2007). Plaque psoriasis typically appears as raised erythematous and well‐demarcated areas of inflamed skin covered with silvery‐white, scaly skin (Griffiths 2007). The location of the plaques is usually symmetrical on the elbows, knees, scalp, lower back, and the periumbilical region. For 5% to 25% of people with psoriatic rheumatic disease, their skin is also involved (Helliwell 2005; Zachariae 2003).
Severity
Chronicity characterises the natural history of plaque psoriasis; this means that severity varies over time, from minor localised patches to complete body coverage. The severity of the disease usually fluctuates around the same level for a particular person (Nijsten 2007), but for each person with this disease the evolution and duration of remission is unpredictable. The psoriasis is declared clear when there are no lesions.
More than a dozen outcome instruments are used to assess the severity of psoriasis and the efficacy of different treatments for psoriasis (Naldi 2010; Spuls 2010); the Psoriasis Area and Severity Index (PASI) score is one of these instruments (Schmitt 2005). The PASI combines the assessment of the severity of lesions and the area affected into a single score in the range of 0 (no disease) to 72 (maximal disease). Recent clinical trials evaluating biological therapies that have received secondary marketing authorisation by the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) used PASI 75, i.e. a 75% improvement in the PASI score, and more recently PASI 90, i.e. 90% improvement in the PASI score, as primary end points. PASI score has substantial limitations, such as low‐response distribution, no consensus on interpretability, and low responsiveness in mild disease (Spuls 2010). However, PASI 90 is a stringent outcome, as patients reaching PASI 90 are almost clear.
Impact and quality of life
Disease severity alone does not determine the burden of psoriasis. Multiple studies have described an impairment of the quality of life (QoL); others have focused on an evaluation of the stigma people experience; and others have studied the impact on psychosocial life (Kimball 2005).
Impairment of QoL in people with psoriasis, when measured with the 36‐item Short Form Health Survey (SF‐36) questionnaire, is higher than that of people with hypertension, diabetes, or depression (Rapp 1999).
Many tools exist to measure the QoL of people with psoriasis and other skin disorders. These measures may be categorised as psoriasis‐specific (Psoriasis Index of Quality of Life (PSORIQoL), Psoriasis Disability Index (PDI)); skin‐specific (Dermatology Life Quality Index (DLQI), Skindex (a quality‐of‐life measure for people with skin disease)); and generic QoL measures (SF‐36). However, methodological weaknesses exist in the use of QoL questionnaires, and there is poor reporting of QoL outcomes in randomised clinical trials (Le Cleach 2008). Several case‐control studies reported a higher risk of metabolic syndrome and cardiovascular comorbidities (Kremers 2007; Naldi 2005).
Description of the intervention
There is currently no cure for psoriasis, but various treatments can help to control the symptoms; thus, long‐term treatment is usually needed. In daily practice, a treatment strategy needs to be defined, and this usually involves an induction therapy, e.g. the period of time of the initial therapy intended to induce remission of the disease, and a maintenance therapy, e.g. to maintain the remission of the disease.
The therapeutic approach to psoriasis includes topical treatments as a single strategy and a first‐line therapy in the management of minor forms (Mason 2013). Nevertheless, about 20% to 30% of people with psoriasis have a moderate‐to‐severe form requiring a second‐line therapy including phototherapy and non‐biological systemic agents, such as ciclosporin, methotrexate, or acitretin. Among the systemic agents, the choice of drug is not clear. The NICE 2012 clinical guidelines in the UK proposed methotrexate as the first choice of systemic agent. Biological agents, such as the tumour necrosis factor (TNF) antagonists (infliximab, etanercept, adalimumab); the monoclonal antibody ustekinumab that targets interleukin‐12 and ‐23 (IL‐12/‐23); anti‐IL17 drugs (secukinumab or ixekizumab); and new small molecules (apremilast) are more recent systemic therapies (Boehncke 2015). Many healthcare systems have developed elaborate psoriasis treatment algorithms to address the high cost of newer therapies. Indeed, in Europe and in Canada, there are mandatory reimbursement criteria that patients must meet before being considered for these treatments, due to their high costs (Nast 2015b), such as presenting a moderate‐to‐severe psoriasis after failure, intolerance or contraindication to at least two non‐biological systemic agents (French criteria).
Non‐biological systemic treatments
The oldest oral pharmacological treatments licensed for psoriasis are ciclosporin, methotrexate, acitretin (which is the retinoid of choice for psoriasis), and fumaric acid esters (FAEs) which are licensed for psoriasis in Germany and used off‐licence in other countries (Atwan 2015).
Randomised controlled trials against placebo for both induction and maintenance therapies have demonstrated the efficacy of ciclosporin for psoriasis (Bigby 2004; Christophers 1992; Ellis 1991; Flytström 2008; Koo 1998; Heydendael 2003; Ho 1999; Mahrle 1995; Meffert 1997; Mrowietz 1995; Shupack 1997). In 2008, Saurat and colleagues conducted the only randomised trial comparing the efficacy of methotrexate versus placebo (CHAMPION 2008). Randomised trials against placebo have demonstrated the efficacy of derivatives of vitamin A, the retinoids, in the treatment of plaque psoriasis (Pettit 1979). Fumaric acid esters are an alternative therapy for people with psoriasis, even though the mechanisms of action are not completely understood (Ormerod 2004). A Cochrane Review on FAEs for psoriasis was published in 2015 (Atwan 2015).
Small molecules or target therapies affect molecules inside immune cells. Recently, small molecule drugs have been developed and show potential to treat people with psoriasis not responding to non‐biological treatments. These small molecule drugs include apremilast (Papp 2012c), tofacitinib (Bachelez 2015), and BMS‐986165 (Papp 2018). Tofacitinib and BMS‐986165 had not been approved for psoriasis at the time our analyses were done.
Biological therapies
Biological therapies use substances made from living organisms, or synthetic versions, to target the immune system. In the 20th century, the development of biological treatments expanded the therapeutic spectrum of systemic treatments for psoriasis. All of the biologics have to be given by infusion or subcutaneous injection, and all have had at least one evaluation of their effectiveness against placebo: etanercept (Leonardi 2003), infliximab (Chaudhari 2001), adalimumab (REVEAL 2008), certolizumab (Reich 2012a), ustekinumab (Lebwohl 2010), secukinumab (Reich 2015), ixekizumab (Leonardi 2012), brodalumab (Papp 2012a), bimekizumab (BE ABLE 1 2018), guselkumab (Gordon X‐PLORE 2015), mirikizumab (NCT03482011), tildrakizumab (Papp 2015), and risankizumab (NCT02672852). Bimekizumab and mirikizumab had not been approved for psoriasis at the time our analyses were done.
How the intervention might work
Dysregulation of the immune system is a critical event in psoriasis, and the evolving knowledge of the role of the immune system in the disease has had an impact on treatment development. Indeed, psoriatic plaque shows marked infiltration by activated T cells, especially CD4+ cells in the dermis. The activated T cells produce several important cytokines, namely, interferon (IFN)‐c, TNF alpha (by Th1 and Tc1 cells), IL‐17A, and IL‐23R (by Th17 and Tc17 cells) (Boehncke 2015).
Non‐biological systemic treatments
Ciclosporin
Ciclosporin is an immunosuppressive agent (a drug that reduces the efficacy of the immune system); it acts by inhibiting the initial phase of the activation of CD4+ T cells, which leads to a block on the synthesis of interleukin 2 by the complex cyclophilin‐ciclosporin, thus preventing T cell proliferation that is key to the pathogenesis of psoriasis (see above) (Ho 1996). This immunosuppression is rapid and reversible. Ciclosporin rapidly reduces the severity of the lesions (over one to three months), but the continuation of treatment is difficult after two years because of the development of adverse effects, such as elevated creatinine levels (Maza 2011). A dose of 5.0 mg/kg/day ciclosporin was significantly more effective than 2.5 mg/kg/day ciclosporin for induction of the remission of psoriasis; however, elevated creatinine was significantly more likely with 5.0 mg/kg/day ciclosporin than with 2.5 mg/kg/day ciclosporin (Christophers 1992).
Methotrexate
Methotrexate is an antimetabolite (an inhibitor of a chemical that is part of normal metabolism), which acts as an antagonist of folic acid (Montaudie 2011). Low doses of methotrexate exert anti‐inflammatory and immunomodulatory activities (Montaudie 2011). The efficacy of methotrexate cannot be assessed earlier than three months; its long‐term safety profile is good. In clinical practice, methotrexate is administered orally at 15 to 25 mg/week (Montaudie 2011).
Retinoids
Retinoids, including acitretin, are involved in the growth and differentiation of skin tissue; they bind to nuclear receptors that belong to the large family of steroid hormone receptors (Sbidian 2011). Retinoids modulate many types of proteins, including epidermal structural proteins, metalloproteinases, and cytokines (Sbidian 2011). The efficacy of retinoids is evaluated after two to three months of treatment, but skin side effects (e.g. xerosis, cheilitis) may limit the ability to increase the dose. Treatment with retinoids is best avoided in women of childbearing age because of risks to a developing foetus and the necessity of using contraception two years after discontinuation of treatment (Sbidian 2011). People receiving 50 mg/day to 75 mg/day acitretin have significantly improved psoriasis compared with those receiving 10 mg/day to 25 mg/day acitretin (Goldfarb 1988).
FAEs
Fumaric acid esters (FAEs) are chemical compounds derived from the unsaturated dicarboxylic acid (Atwan 2015). Oral preparations of FAEs in psoriasis were developed containing dimethyl fumarate (DMF) and salts of monoethyl fumarate (MEF) as main compounds (Atwan 2015). FAEs produce anti‐inflammatory effects by preventing the proliferation of T cells (Atwan 2015).
FAEs are an effective therapy in people with psoriasis (50% to 70% achieve PASI 75 improvement within four months of treatment). Tolerance is limited by gastrointestinal side effects and flushing of the skin (Atwan 2015). Several case‐series described rare adverse events, such as progressive multifocal leukoencephalopathy (Balak 2016). In clinical practice, FAEs are administered orally. People receive this after a gradual dose incrementation the equivalent of 720 mg of DMF a day.
Small molecules
Small molecule drugs modulate pro‐inflammatory cytokines and selectively inhibit signalling pathways: phosphodiesterase 4 inhibitors (apremilast), Janus kinase (JAK) inhibitors (tofacitinib), or sphingosine 1‐phosphate receptor agonists (ponesimod) (Torres 2015).
Apremilast
Apremilast belongs to the phosphodiesterase 4 (PDE4) inhibitors family (Torres 2015). By increasing cyclic adenosine monophosphate (cAMP) levels, PDE4 inhibitors reduce production of pro‐inflammatory TNF alpha and IFNγ in people with psoriasis. Apremilast has been approved for psoriasis; its efficacy seems to be higher than non‐biological systemic therapy, but no randomised controlled trials (RCTs) assessing apremilast versus methotrexate or ciclosporin have been published. However, some RCTs assessing apremilast versus methotrexate are ongoing (CTRI/2019/01/017362; CTRI/2019/07/020274). The safety of the drug should be detailed in the near future with phase 4 studies. In clinical practice, apremilast is administered orally at 30 mg twice a day (Torres 2015).
Tofacitinib
Tofacitinib is a Janus kinase (JAK) inhibitor (Torres 2015). JAK inhibitors target the Janus kinase (JAK)/signal transducer and activator of transcription (STAT) pathway, which is pivotal for the downstream signalling of inflammatory cytokines involved in psoriasis. Tofacitinib had not been approved for psoriasis at the time our analyses were done (Torres 2015).
BMS‐986165
BMS‐986165 is a potent oral tyrosine kinase 2 (TYK2) inhibitor that binds to the pseudokinase domain of the enzyme and is functionally more selective than other tyrosine kinase inhibitors. Tyrosine kinase 2 (TYK2) is an intracellular signalling enzyme which activates signal transducer and activator of transcription (STAT)–dependent gene expression and functional responses of interleukin‐12, interleukin‐23, and type I and III interferon receptors. These cytokine pathways are involved in the pathologic processes associated with psoriasis, and are distinct from responses driven by Janus kinase (JAK) 1 (JAK1), JAK1 and JAK3 in combination, JAK2, as previously described. BMS‐986165 had not been approved for psoriasis at the time our analyses were done.
Biological therapies
Biological therapies have been developed in recent years and first target and prevent T cell proliferation and then target cytokines involved in psoriasis physiopathology (e.g. anti‐TNF alpha, anti‐IL12/23, anti‐IL23, anti‐IL17).
Anti‐TNF alpha
Two monoclonal antibodies against tumour necrosis factor alpha (TNF‐α) (infliximab, adalimumab) and one recombinant TNF‐α receptor (etanercept) have been developed to inhibit TNF‐α signalling, thus preventing its inflammatory effects, and are approved for psoriasis (Gisondi 2004). A third, certolizumab, is being assessed for psoriasis in phase 3 trials.
Etanercept is a recombinant TNF‐α receptor and weakly immunogenic (provokes only a mild immune response). Its efficacy is assessed at three months. A 50 mg dose of etanercept is administered subcutaneously twice weekly for three months during the induction phase (remission of the psoriasis flare) with 50 mg administered weekly as maintenance therapy (Gisondi 2004).
Infliximab is a chimeric antibody that neutralises the action of TNF‐α. Its efficacy is evaluated after six to eight weeks of treatment. A dose of 5.0 mg/kg infliximab is given as an intravenous (IV) induction regimen at 0, 2, and 6 weeks followed by a maintenance regimen of 5.0 mg/kg every 8 weeks. The presence of a murine sequence at recognition sites can lead to the development of anti‐infliximab antibodies that may impair the therapeutic effect (Gisondi 2004).
Adalimumab is a fully humanised antibody with very low immunogenicity. Its efficacy is estimated after eight and 12 weeks of treatment. One dose of 80 mg is administered subcutaneously, followed one week later by a 40 mg subcutaneous dose, which is administered every two weeks (Mossner 2009). Those receiving TNF‐α blockers are potentially exposed to a greater risk of infection and require regular monitoring (Tubach 2009).
Certolizumab is an anti‐TNF alpha with a unique structure that does not contain an Fc (fragment crystallisable) portion as adalimumab or infliximab does, based on the human immunoglobulin G1 Fc. Certolizumab therefore does not display Fc‐mediated effects (improving solubility, increasing drug stability, and decreasing immunogenicity) (Campanati 2017). Treatment starts with a 400‐mg dose given as two injections, followed by a further 400‐mg dose two and four weeks later. After this, depending on the condition being treated, patients should continue with 200 mg or 400 mg, given as one or two injections every two or four weeks.
Anti‐IL12/23, Anti‐IL23, Anti‐IL17
Additional monoclonal antibodies have been developed against pro‐inflammatory cytokines: IL‐12, IL‐23, and IL‐17 inhibit the inflammatory pathway at a different point to the anti‐TNF alpha antibodies (Dong 2017).
Interleukin‐12 and IL‐23 share a common domain, p40, which is the target of ustekinumab (which the FDA approved in 2009) (Savage 2015). A 45 mg subcutaneous dose is administered initially (90 mg if body weight is over 100 kg), then 45 mg (or 90 mg) subcutaneously four weeks later, and thereafter 45 mg (or 90 mg) subcutaneously every 12 weeks (Savage 2015). Interleukin‐23 plays an essential role in skin inflammation in psoriasis leading to the development of agents that selectively target the IL‐23p19 subunit (Dong 2017). Drugs targeting the p19 subunit of IL‐23 are guselkumab (a fully human IgG1k monoclonal IL‐23 antagonist), tildrakizumab (a humanised IgG1k monoclonal antibody), risankizumab (high‐affinity humanised IgG1 monoclonal antibody), and mirikizumab (Dong 2017). In July 2017, the FDA approved guselkumab for psoriasis. Guselkumab is given as a 100 mg subcutaneous injection every eight weeks, following two starter doses at week 0 and week 4. More recently both tildrakizumab and risankizumab were approved. The recommended dose for tildrakizumab is one 100 mg injection, followed by a further dose after 4 weeks and then an injection every 12 weeks. The dose may be increased to 200 mg in certain patients, for example those badly affected by the disease or with bodyweight over 90 kg. The recommended dose for risankizumab is 150 mg, administered by two subcutaneous injections every 12 weeks following two initiation doses at week 0 and 4. Mirikizumab had not been approved for psoriasis at the time our analyses were done.
Interleukin‐17 inhibitors include secukinumab (a recombinant fully human anti‐IL17A IgG1k monoclonal antibody), ixekizumab (a humanised anti‐IL17 immunoglobulin G4 monoclonal antibody), brodalumab (a human IgG2 monoclonal antibody that decreases the downstream effect of IL‐17 by antagonising the IL‐17RA receptor), and bimekizumab (a humanised monoclonal IgG1 antibody that potently and selectively neutralises the biological function of both human IL‐17A and IL‐17F) (Dong 2017). The recommended dosage for secukinumab is 300 mg administered subcutaneously at weeks 0, 1, 2, 3, and 4, and then every 4 weeks thereafter. Ixekizumab is administered at 160 mg (2 x 80 mg injections) at weeks 0, 2, 4, 6, 8, 10, and 12, and then every four weeks thereafter (Dong 2017). The recommended dose for brodalumab is 210 mg given once a week for the first three weeks and then every two weeks. Bimekizumab had not been approved for psoriasis at the time our analyses were done.
Why it is important to do this review
To determine the treatment pathway in psoriasis, the efficacy and safety of each systemic treatment must be determined relative to other therapies. Several RCTs have compared against placebo the efficacy of the different systemic treatments for psoriasis. However, there are few trials comparing non‐biological systemic therapies head‐to‐head, systemic therapies against biological therapies, or biological therapies head‐to‐head. Several previous meta‐analyses or indirect comparison meta‐analyses have been published (Bansback 2009; Brimhall 2008; Gómez‐García 2017; Gospodarevskaya 2009; Lin 2012; Loveman 2009; Nast 2015a; Nelson 2008; Reich 2008; Reich 2012b; Schmitt 2008; Signorovitch 2010; Signorovitch 2015; Spuls 1997; Strober 2006; Tan 2011; Turner 2009; Woolacott 2006). However, the number of studies included in these publications was low, the searches were not exhaustive, and several trials have been published since their search dates. Also, the publications did not evaluate some systemic treatments.
A network meta‐analysis enables the best use of the direct and indirect information available to determine the relative efficacy of treatments. In other words, a network meta‐analysis will help to highlight the missing key comparisons that are needed to inform clinical practice.
Following the publication of the 2019 update of this review, we are maintaining it as a living systematic review. This means we are continually running the searches and rapidly incorporating any newly‐identified evidence into the review. We believe a living systematic review approach is appropriate for this review, for three reasons. Firstly, the review addresses an important health issue. The high prevalence of psoriasis (1% to 3% of the world population); the major impact on quality of life for many individuals; the cardiovascular comorbidities associated with significant mortality; the many therapeutic options; and the high costs of these new systemic treatments are reasons, among others, to help physicians in determining which treatment is best suited to a patient. Secondly, an important level of uncertainty remains in the existing evidence in the field of psoriasis, despite searches including the current update (up to 8 September 2020) identifying a total of 158 studies for inclusion in the review. Few head‐to‐head trials have compared systemic treatments against each other. Once the benefit of a treatment has been established against placebo using high quality of evidence, head‐to‐head trials would be helpful to provide physicians with efficacy estimates between the different biological treatments based on stronger evidence than indirect comparisons. Further head‐to‐head trials are needed to accurately rank drugs according to their risk/benefit ratio. Thirdly, we are aware of ongoing trials in this area of research that will be important to incorporate, and we expect that future research will have an impact on the conclusions. For instance, new molecules have emerged constantly (e.g. in 2017, four new biological treatments for psoriasis emerged).
The plans for this review were published as a protocol 'Systemic pharmacological treatments for chronic plaque psoriasis' (Sbidian 2015). This review is an update of 'Systemic pharmacological treatments for chronic plaque psoriasis: a network meta‐analysis' (Sbidian 2017; Sbidian 2020).
Objectives
To compare the efficacy and safety of non‐biological systemic agents (acitretin, ciclosporin, fumaric acid esters, methotrexate), small molecules (apremilast, tofacitinib, BMS‐986165), anti‐TNF alpha (etanercept, infliximab, adalimumab, certolizumab), anti‐IL12/23 (ustekinumab), anti‐IL17 (secukinumab, ixekizumab, brodalumab, bimekizumab), and anti‐IL23 (guselkumab, tildrakizumab, risankizumab, mirikizumab) for people with moderate‐to‐severe psoriasis using a network meta‐analysis, and to provide a ranking of these treatments according to their efficacy and safety.
A secondary objective is to maintain the currency of the evidence, using a living systematic review approach.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs).
Phase I trials were not eligible because participants, outcomes, dosages, and schema of administration of interventions are too different from phase II, III, and IV studies. Cross‐over trials were not eligible (because of the unpredictable evolution of psoriasis and risk of carry‐over bias). Non‐randomised studies, including follow‐up studies, were not eligible.
Types of participants
We considered trials that included adults (over 18 years of age) with moderate‐to‐severe plaque psoriasis (i.e. needed systemic treatment) or psoriatic arthritis whose skin had been clinically diagnosed with moderate‐to‐severe psoriasis and who were at any stage of treatment.
Types of interventions
We considered trials that assessed systemic treatments, irrespective of the dose and duration of treatment, compared with placebo or with an active comparator.
Systemic treatments included the following:
-
Non‐biological treatments
FAEs
Acitretin
Ciclosporin
Methotrexate
-
Small molecules
Apremilast
Tofacitinib
BMS‐986165
-
Anti‐TNF alpha
Infliximab
Etanercept
Adalimumab
Certolizumab
-
Anti‐IL12/23
Ustekinumab
Anti‐IL17
Secukinumab
Brodalumab
Ixekizumab
Bimekizumab
-
Anti‐IL23
Tildrakizumab
Guselkumab
Risankizumab
Mirikizumab
We were interested to compare both the different drugs (n = 20) and the different classes of drugs (n = 6).
Active comparators include the following:
any of the aforementioned systemic treatments; or
additional treatment not of primary interest but used for the network synthesis, such as topical treatment or phototherapy.
In multi‐arm trials, study groups assessing drugs other than those mentioned above were not eligible. In cases of multi‐dose trials, we grouped together all of the different dose groups as a single arm and performed sensitivity analysis at dose level.
In our Background section, we have referred to ongoing Cochrane Reviews that address some of the systemic treatments administered to adults with plaque psoriasis. We considered these treatments in our review, and we have liaised with each of these teams to harmonise our protocols. However, the Cochrane Review on FAEs, published in 2015, included people with all types of psoriasis and not only plaque‐type psoriasis (Atwan 2015).
In the 'Data collection and analysis > Assessment of heterogeneity' section, details on what was planned to assess the transitivity assumption for studies, participants and intervention are available.
Adaptive criteria for considering studies for this review
As a living systematic review, we are continually identifying new evidence for interventions already in the network of trials but also for novel interventions. To provide an update and a useful network of interventions for physicians, we need first to identify new interventions but also, to drop old interventions, which are no longer of interest.
To achieve these goals, we have created a research community in psoriasis, including international experts in the field who will help to provide information of new 'eligible' drugs.
Once a year, a list of all systemic drugs used for psoriasis is proposed by the scientific steering committee to the international experts’ group, including:
‐ Drugs already involved in the network
‐ Marketed drugs, identified using the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) websites (www.accessdata.fda.gov/scripts/cder/drugsatfda and www.ema.europa.eu/ema, respectively).
‐ Drugs under development, identified using the World Health Organization International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/) and ISRCTN registry (www.isrctn.com)
The international experts’ group select from this list all the systemic drugs needed for the future network. They also add relevant new interventions not proposed in the list. They provide a rationale for all proposed network changes (adding or removing interventions). The international experts' group is necessary also to determine which drugs have to be deleted from the network, with clinical practice and market authorisation being different in each country.
It is sufficient to update the interventions network once a year, as we are including phase II and III RCTs. Indeed, the timing between the phase I and the phase II/III for a promising intervention is over one year.
Types of outcome measures
Psoriasis is a chronic disease; treatments are symptomatic, often with a return to baseline after discontinuation. In the absence of an existing defined core outcome set (Spuls 2016), we chose the most relevant outcomes for patients (COMET). The Psoriasis Area and Severity Index score (PASI) 75 is the most common outcome measure used. However, confronted with a debilitating and a socially and psychologically highly visible disease, a completely 'clear or almost clear' skin is a more stringent test in the induction phase (i.e. psoriasis flare clearing phase).
Primary outcomes
The proportion of participants who achieved clear or almost clear skin, that is, at least PASI 90 at induction phase.
The proportion of participants with serious adverse events (SAEs) at induction phase. We used the definition of severe adverse events from the International Conference of Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, which includes death, life‐threatening events, initial or prolonged hospitalisation, and adverse events requiring intervention to prevent permanent impairment or damage.
Secondary outcomes
Proportion of participants who achieve PASI 75 at induction phase.
Proportion of participants who achieve a Physician Global Assessment (PGA) value of 0 or 1 at induction phase.
Quality of life measured by a specific scale. Available validated scales are the Dermatology Life Quality Index (DLQI), Skindex, Psoriasis Disability Index (PDI), or Psoriasis Symptom Inventory (PSI) at induction phase.
The proportions of participants with adverse events (AEs) at induction phase ('AE outcome' did not include SAE).
Proportion of participants who achieve PASI 75 at 52 weeks.
Proportion of participants who achieve PASI 90 at 52 weeks.
We defined the induction phase as an evaluation from 8 to 24 weeks after the randomisation. In case of multiple time points, we chose the longest one.
To avoid selection of good responders of participants entering into long‐term extension, we selected participants who have been randomised since the induction phase.
We did not include studies that had timings outside of the time ranges stated in our outcomes in our review or analyses. We did not evaluate specific adverse events, just the proportion of participants with at least one adverse event and at least one serious adverse event at induction phase.
Search methods for identification of studies
We aimed to identify all relevant RCTs, regardless of language or publication status (published, unpublished, in press, or in progress).
Electronic searches
For this living systematic review we revised our search strategies in line with advice from the Cochrane Living Evidence Network. Details of the search strategies used in the earlier published version of this review are available in Sbidian 2020.
Since September 2019 the Cochrane Skin Information Specialist has searched the following databases monthly up to 8 September 2020:
the Cochrane Central Register of Controlled Trials (CENTRAL; 2020, Issue 9) in the Cochrane Library using the strategy in Appendix 1;
MEDLINE (via Ovid) using the strategy in Appendix 2; and
Embase (via Ovid) using the strategy in Appendix 3.
Trials registers
We (SA and ES for this update) searched the following trials registers up to 25 September 2020 with the following search terms: psoriasis AND one by one, each drug name listed in Types of interventions:
World Health Organization International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/); and
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov).
Retractions and errata
We undertook a search to identify retraction statements or errata related to our included studies in MEDLINE and Embase on 11 November 2020. We retrieved no new relevant records.
Searching other resources
References from other studies
We checked the bibliographies of included studies and relevant systematic reviews for further references to relevant trials.
Unpublished literature
We contact corresponding authors of ongoing studies as we identify them, and ask them to advise us when trial results are available, or to share early or unpublished data. We also contact pharmaceutical companies to attempt to identify unpublished and ongoing trials (see Table 2).
2. Investigators contacted.
| Contact | Requested Information | Contacted | Reply | |
| Missing data | ||||
| Akcali 2014 | Prof. Akcali | Outcomes: PASI 90, PASI 75, PGA 0/1, QoL scale, AEs & SAEs | 8 and 21 November 2016 | No response |
| Al‐Hamamy 2014 | Prof. Al‐Hamamy | Outcomes: PASI 75, PGA 0/1, QoL scale, AEs and SAEs | 8 and 21 November 2016 | No response |
| Asahina 2010 | Prof. Asahina | Outcome: PASI 90 | 8 November 2016 | Asahina 2010 detailed report |
| Asahina 2016 | Prof. Asahina Pfizer | Outcomes: AEs and SAEs | 3 and 12 January 2017 | Additional data to the publication not provided |
| Asawanonda 2006 | Prof. Asawanonda | Outcomes: PASI 75, PGA 0/1, AEs and SAEs | 21 November 2016 15 December 2016 |
Asawanonda 2006 sent detailed report for PASI 75 and AEs. PGA was not collected during this study |
| Bissonnette 2015 | Prof. Bisonnette Innovaderm Recherches Inc. | Outcomes: PASI 90, PGA 0/1, AEs | 8 and 21 November 2016 | Additional data to the publication not provided |
| FEATURE 2015 | Dr Blauvelt Novartis |
Outcome: QoL scale | 8 and 21 November 2016 | Additional data to the publication not provided |
| Caproni 2009 | Prof. Fabri | Outcomes: PASI 90, PASI 75, PGA 0/1, QoL scale, AEs and SAEs | 8 and 21 November 2016 | Caproni 2009 sent detailed report for PASI 90 and SAEs. Other outcomes (PGA, QoL and AEs) not collected during this study. |
| Dogra 2013 | Prof. Dogra | Outcomes: PGA 0/1, QoL scale, AEs and SAEs | 8 and 21 November 2016 | No response |
| Dogra 2012 | Prof. Dogra | Outcomes: PGA 0/1, QoL scale, AEs and SAEs | 8 November 2016 | PGA & QoL scale not collected during this study. AEs and SAEs not provided per arm |
| Fallah Arani 2011 | Dr Fallah Arani | Outcomes: PASI 90, PGA 0/1 and QoL scale | 8 and 21 November 2016 | Outcomes not collected during this study |
| Flytström 2008 | Prof. Flytström | Outcomes: PGA 0/1 | 12 and 19 January 2017 | Additional data to the publication not provided |
| Gisondi 2008 | Prof. Gisondi | Outcomes: PASI 90, PGA 0/1, QoL scale, AEs and SAEs | 8 November 2016 | Gisondi 2008 sent detailed report for the requested outcomes except for QoL (not assessed during the study) |
| Gordon 2006 | Prof. Gordon | Outcomes: PGA0/1, AEs | 3 and 12 January 2017 | No response |
| Gottlieb 2012 | Prof. Gottlieb Abbvie |
Outcomes: PASI 90 & QoL scale | 8 November 2016 | Gottlieb 2012 sent detailed report for the requested outcomes |
| Gottlieb 2011 | Prof. Gottlieb Amgen |
Outcomes: PASI 90, PGA 0/1, QoL scale, AEs and SAEs | 8 November 2016 | Gottlieb 2011 sent detailed report for the requested outcomes |
| ACCEPT 2010 | Prof. Griffiths Janssen |
Outcome: QoL scale | 16 December 2016 | QoL was not collected during this study |
| Krueger 2016a | Pfizer | Outcomes: PASI 90, QoL scale | 3 and 12 January 2017 | No response |
| AMAGINE‐2 2015 | Prof. Lebwohl Valeant Pharmaceuticals NA LLC |
Outcomes: PASI 90 and QoL scale | 8 and 21 November 2016 | AMAGINE‐2 2015 sent detailed report for PASI 90; individual scores and median difference from baseline of QoL were not available |
| AMAGINE‐3 2015 | Prof. Lebwohl Valeant Pharmaceuticals NA LLC |
Outcomes: PASI 90 and QoL scale | 8 and 21 November 2016 | AMAGINE‐3 2015 sent detailed report for PASI 90, individual scores and median difference from baseline of QoL were not available |
| Leonardi 2012 | Prof. Leonardi | Outcomes: QoL scale and AEs | 8 and 21 November 2016 | No response |
| Mahajan 2010 | Prof. Kaur | Outcomes: PASI 90, PGA 0/1, QoL scale, AEs and SAEs | 8 and 21 November 2016 | No response |
| REVEAL 2008 | Prof. Menter | Outcome: PGA 0/1 | 8 and 21 November 2016 | No response |
| EXPRESS‐II 2007 | Prof. Menter | Outcome: PGA 0/1 | 8 and 21 November 2016 | No response |
| BRIDGE 2017 | Prof. Mrowietz | Outcome: QoL scale | 3 and 12 January 2017 | Additional data to the publication not provided |
| Ortonne 2013 | Prof. Paul Novartis |
Outcome: PASI 90 | 3 January 2017 | Additional data to the publication not provided |
| Papp 2013a | Prof. Papp | Outcome: QoL scale | 22 November 2016 13 December 2016 | Additional data to the publication not provided |
| AMAGINE‐1 2016 | Prof. Papp | Outcome: QoL scale | 22 November 2016 13 December 2016 | Additional data to the publication not provided |
| Papp 2005 | Prof. Papp | Outcome: QoL scale, AEs and SAEs | 22 November 2016 13 December 2016 | Additional data to the publication not provided |
| Papp 2012b | Prof. Papp | Outcome: QoL scale | 22 November 2016 13 December 2016 | Additional data to the publication not provided |
| Papp 2013b | Prof. Papp | Outcome: PASI 90, PGA0/1, QoL scale | 3 January 2017 | Additional data to the publication not provided |
| JUNCTURE 2015 | Prof. Paul Novartis |
Outcome: QoL scale | 15 December 2016, 2 January 2017 | Additional data to the publication not provided |
| Reich 2015 | Prof. Reich Novartis |
Outcomes: PGA 0/1 and QoL scale | 8 November 2016, 16 December 2016 | Additional data to the publication not provided |
| LIBERATE 2017 | Prof. Reich PelotonAdvantage | Outcome: QoL scale | 4 January 2017 | Additional data to the publication not provided |
| Rich 2013 | Prof. Rich | Outcome: QoL scale | 22 November 2016, 13 December 2016 | No response |
| PRESTA 2010 | Prof. Sterry | Outcomes: PASI 90 and QoL scale | 8 and 21 November 2016 | No response |
| Strober 2011 | Prof. Strober Abbvie |
Outcome: QoL scale | 8 November 2016 | Strober sent detailed report for the requested outcomes |
| CLEAR 2015 | Prof. Thaçi Novartis |
Outcome: QoL scale | 8 and 21 November 2016 | Additional data to the publication not provided |
| Torii 2010 | Prof. Torii | Outcomes: PASI 90 and PGA0/1 | 21 November 2016 | Torii sent detailed report for the requested outcomes |
| Tyring 2006 | Prof. Tyring | Outcomes: PGA 0/1 and QoL scale | 8 and 21 November 2016 | No response |
| Van Bezooijen 2016 | Dr van Bezooijen | Outcomes: PASI 90, adverse effects | 4 and 12 January 2017 | Additional data to the publication not provided |
| Van de Kerkhof 2008 | Prof. van der Kherkhof Pfizer | Outcome: AEs | 8 and 21 November 2016 | Additional data to the publication not provided |
| LOTUS 2013 | No contact | Outcome: PASI 90 | No | Authors' email not found |
| CLARITY 2018 | Prof Bagel | Outcome: QoL Scale | 24 June 2019 | Email response 01 July 2019 Dear Dr. Sbidian, It is a pleasure to e‐meet you – i am the medical director assigned to the CLARITY trial for Novartis, and I am responding on behalf of Dr. Bagel to your request of data. Thanks for your interest in the CLARITY: we published the 16w data and we are currently working on the final manuscript. The 52w manuscript will include updated PROs and clinical outcomes – unfortunately, those data are embargoed until the final manuscript is release. Once published, we’d be happy to re‐connect to see how the CLARITY data will support your meta‐analysis. Please feel free to reach out directly to me if you need any further assistance. Best regards, Elisa Muscianisi |
| ADACCESS 2018 | Prof Blauvelt | Outcome: QoL Scale | 24 June and 1st July 2019 | Email response: 2 July 2019 'Cc’ing the person who should be able to help you.' |
| EGALITY 2017 | Prof Gerdes | Outcomes: QoL Scale, AEs, SAEs | 24 June 2019 | Email response 27 June 2019 Dear Dr. Sbidian, On behalf of SANDOZ Global Medical Affairs team, I wanted to thank you for your interest to the EGALITY study and for considering it for your ongoing meta‐analysis. I’m also happy to share with you on behalf of the authors and the team who worked on the study, the requested information that you can find here attached We would highly appreciate if you can keep us informed when the meta‐analysis will be published, meanwhile, please feel free to revert back to us in case you would need any further information Thank you and have a nice afternoon Best regards Sohaib Dr. med. Sohaib HACHAICHI Global Medical Affairs Manager Immunology |
| Ikonomidis 2017 | Prof Ikonomidis | Outcomes: PASI 90, 75, PGA0/1, QoL Scale, AES, SAEs | 24 June and 1st July 2019 | No response |
| Jin 2017 | Prof Zhao | Outcomes: PASI 90, PGA0/1, QoL Scale | 24 June and 1st July 2019 | No response |
| VIP Trial 2018 | Prof Gelfand | Outcome: PASI 90 | 24 June | Email response 24 June 2019 "Yes we can do this. I propose that we have this data approved for release to you by September 30 2019" We will add the new data for the next update (living review). |
| SIGNATURE 2019 | No contact | Outcomes: PASI 90, PGA0/1, AES, SAEs | 24 June 2019 | We will contact the authors when the article is published |
| NCT02581345 | Dr Caminis | Outcome: QoL Scal | 24 June 2019 | Authors' email not found (SHIRE pharmaceutics). We will contact the authors when the article is published |
| AURIEL‐PsO 2020 | Sponsors and collaborators: Fresenius Kabi SwissBioSim GmbH Merck KGaA, Darmstadt, Germany | Outcomes: QoL Scale, AEs | 24 June 2019 | No contact; We will contact the authors when the article is published |
| NCT02850965 | Sponsors: Boehringer Ingelheim | Outcomes: PASI 90, QoL Scale, AEs | 24 June 2019 | No contact. We will contact the authors when the article is published |
| ORION 2020 | Pr Ferris | Outcome: DLQI | 24 June and 2nd July 2019 | No response |
| POLARIS 2020 | Janssen‐Cilag G.m.b.H, Germany Clinical Tria | Outcome: PGA0/1 | 24 June 2019 | No contact. We will contact the authors when the article is published |
| SustaIMM 2019 | Sponsors and collaborators: AbbVie Boehringer Ingelheim | Outcome: DLQI | 24 June 2019 | No contact. We will contact the authors when the article is published |
| Papp 2017a | Prof. Papp | Outcome: DLQI | 24 June 2019 | Email answer 24 June 2019 "I am not at liberty to release results that are not in the public domain. Regards, k" |
| BE ABLE 1 2018 | Prof. Papp | Outcome: DLQI | 24 June 2019 | Email answer 24 June 2019 "I am not at liberty to release results that are not in the public domain. Regards, k" |
| Papp 2017b | Prof. Papp | Outcome: DLQI | 24 June 2019 | Email answer 24 June 2019 "I am not at liberty to release results that are not in the public domain. Regards, k" |
| Papp 2018 | Prof. Papp | Outcome: DLQI | 24 June 2019 | Email answer 24 June 2019 "I am not at liberty to release results that are not in the public domain. Regards, k" |
| IXORA‐S 2017 | Prof. Reich | Outcome: DLQI | 24 June and 1st July 2019 | E‐mails not received (email: kreich@dermatologikum.de; kreich@jeruocon.com) |
| TRANSFIGURE 2016 | Prof. Reich | Outcomes: PGA0/1, DLQI | 24 June and 1st July 2019 | E‐mails not received (email: kreich@dermatologikum.de; kreich@jeruocon.com) |
| PRIME 2017 | Prof. Sticherling | Outcome: DLQI | 24 June and 1st July 2019 | Email answer 02 July 2019 "Dear Dr. Sbidian, thank you very much for your mail. We are currently checking the data for your table to respond in due time. Yours, Michael Sticherling" |
| CIMPACT 2018 | Prof. Lebwohl | Outcome: DLQI | 24 June and 1st July 2019 | No response |
| Lee 2016 | Outcomes: PASI 90, DLQI | 24 June and 1st July 2019 | No response | |
| NCT02672852 | Sponsors and collaborators: AbbVie Boehringer Ingelheim | Outcome: DLQI | 24 June 2019 | No contact. We will contact the authors when the article is published |
| NCT02134210 | Barbara K Finck, M.D.; Coherus Biosciences, Inc | Outcome: DLQI | 24 June 2019 | No contact. We will contact the authors when the article is published |
| Yu 2019 | Prof. Shi | Outcomes: PGA 0/1, DLQI | 12 August 2020, 8 September 2020 | No response |
| von Stebut CARIMA 2019 | Prof. von Stebut | Outcomes: PASI 90, 75, IGA 0/1, QoL Scale | 12 August 2020, 8 September 2020 | No response |
| Hodge 2017 PsOsim | Prof. Hodge | Outcomes: PASI 90, PGA 0/1, QoL Scale | 12 August 2020, 8 September 2020 | No response |
| Reich 2019 | Prof. Reich | Outcome: DLQI | 12 August 2020, 8 September 2020 | Email answer 8 September 2020: " Dear Dr. Sbidian Thank you for your interest in the mirikizumab data. The team is currently working to determine what we are allowed to share, given that this data has not been published. I have just a few questions. If we do not provide the specified information, would mirikizumab then not be included at all in the NMA? Are percentages of patients with prior phototherapy and prior topical therapy needed for the modeling? If we cannot provide mean DLQI, but we are able to provide number/% patients on prior phototherapy and topic therapy, would mirikizumab still be included in the NMA for PASI outcomes? Thank you! Bridget Charbonneau" |
| NCT02187172 Gelfand VIP‐U 2020 | Prof. Gelfand | Outcome: QoL Scale | 12 August 2020 | Email answer 17 August 2020 NCT02187172 Gelfand VIP‐U 2020 sent detailed report for the requested outcome. |
| NCT02313922 Liu 2019 | Prof. Liu | Outcome: QoL Scale | 12 August 2020 | Email answer 13 August 2020 Liu 2019 sent detailed report for the requested outcome. |
| Reich ECLIPSE 2019 | Prof. Reich | Outcomes: QoL Scale, AEs, SAEs | 12 August 2020, 8 September 2020 | Email answer 11 September 2020: "Dear Authors: I am contacting you on behalf of the ECLIPSE authors and the Janssen team. Prof. Reich has shared with us your request for additional ECLIPSE data to be included in a meta‐analysis. The authors would like to learn more about what data are being presented and what conclusions are being made in this meta‐analysis. For example, which other biologics are being compared and at what timepoints are these comparisons? ECLIPSE was not a placebo‐controlled trial and the primary endpoint was 48 weeks, which was much later than most other studies. That being said, the authors would first like to have these questions answered and to also have a better understanding of the proposed methodology and the goal of your meta‐analysis. Thank you. Best regards, Kristin M. Sharples, PhD Scientific Communications, Dermatology Medical Affairs" |
| Gottlieb IXORA‐R 2019 | Prof. Blauvelt | Outcomes: PASI 90, 75, PGA 0/1, DLQI | 12 August 2020 | Email answer 13 August 2020 Gottlieb IXORA‐R 2019 sent detailed report for the requested outcomes except for PASI 75 and DLQI (not disclosed yet). |
| NCT02748863 | Sponsors: Novartis | Outcome: DLQI | 12 August 2020 | Email answer 25 August 2020 " Le critère principal d’évaluation de l’étude repose à la fois sur le score PASI 75 et sur l’IGA mod 2011. L’Indice de Qualité de Vie (DLQI) correspond bien à un des critères d’évaluation secondaires. Les résultats de l’étude ALLURE (NCT02748863) n’ont pas encore été intégralement publiés dans la littérature scientifique. Toutefois, nous vous prions de bien vouloir trouver ci‐joints le protocole de l’étude et les premiers résultats disponibles sur le site internet clinicaltrials.gov. Ces premiers résultats incluent des données sur les caractéristiques des patients, notamment leur âge, leur sexe ainsi que leur origine ethnique. Je mets en copie de cet email la responsable médicale dermatologie de Cosentyx pour votre région, Mme Emeline Desreumaux (emeline.desreumaux@novartis.com, +33667445036), n’hésitez pas à la contacter directement pour plus d’information sur nos études cliniques. Sophie Baratin" |
| NCT03051217 | Sponsors: UCB pharma | Outcomes: AEs, SAEs | 12 August 2020, 8 September 2020 | No contact. We will contact the authors when the article is published |
| NCT03066609 | Sponsors: Novartis | Outcome: QoL Scale | 12 August 2020, 8 September 2020 | No contact. We will contact the authors when the article is published |
| NCT03055494 ObePso‐S | Sponsors: Novartis | Outcomes: PASI 75, PGA 1/0, QoL Scale, AEs, SAEs | 8 September 2020 | No contact. We will contact the authors when the article is published |
| Warren IMMerge, 2020 | Prof. Warren | Outcome: QoL Scale | 8 September 2020 | No response |
| NCT03482011 OASIS‐1 | Sponsors: Eli Lilly and Company | Outcome: DLQI | 21 October 2020 | |
| Awaiting classification studies | ||||
| Chow 2015 | Prof. Chow | outcomes: PASI 90, PASI 75, PGA 0/1, QoL scale, AEs and SAEs | 8 November 2016, 16 December 2016 | No response |
| Gurel 2015 | Prof. Gurel | Study's protocol and outcomes: PASI 90, PASI 75, PGA 0/1, QoL scale, AEs and SAEs | 17 and 24 January 2017 | Gurel 2015 sent detailed report for the requested outcomes. Finally Gurel study was classified in the included studies section. |
| Han 2007 | No contact | Outcomes: PASI 90, PASI 75, PGA 0/1, QoL scale, AEs and SAEs | No | Authors' email not found |
| Krishna 2016 | Prof. Krishna | Asking for study protocol and efficacy/safety results | 5 and 12 January 2017 11 February 2020 |
No response |
| DRKS00000716 | Prof. Jacobi | Asking for study protocol and efficacy/safety results | 12 and 19 January 2017 | No response |
| CTRI/2015/05/005830 | Prof. Shah | Asking for study protocol and efficacy/safety results | 12 and 19 January 2017 11 February 2020 |
No response |
| NCT01088165 | Prof. Holzer | Asking for study protocol and efficacy/safety results | 3 and 24 June 2019 11 February 2020 |
No response |
| NCT02655705 | Prof. Youn | Asking for study protocol and efficacy/safety results | 3 and 24 June 2019 11 February 2020 |
No response |
| CTRI /2017/09/009850 | Prof. Mease | Asking for study protocol and efficacy/safety results | 17 Ausgut 2020, 8 September 2020 | No response |
| EUCTR2010‐020168‐39‐DE | Prof. Anderson | Asking for study protocol and efficacy/safety results | 17 August 2020, 8 September 2020 | No response |
| EUCTR2015‐005279‐25‐DE | Prof. Philipp | Asking for study protocol and efficacy/safety results | 17 August 2020, 8 September 2020 | No response |
| EUCTR2017‐001615‐36‐DE | Prof. Gerdes | Asking for study protocol and efficacy/safety results | 17 August 2020, 8 September 2020 | Email answer 8 September 2020: " Dear Dr. Afach, Thank you for your request. Unfortunately the information is still confidential. BR Sascha Gerdes" |
| Ikonomidis 2019 | Prof. Ikonomidis | Asking for study protocol and efficacy/safety results | 17 August 2020, 8 September 2020 | No response |
| Makavos 2020 | Dr. Ikonomidis | Asking for study protocol and efficacy/safety results | 30 October 2020 | |
| Abstracts | ||||
| Mrowietz 2005 | Prof. Mrowietz | Study's protocol and outcomes: PASI 90, PASI 75, PGA 0/1, QoL scale, AEs and SAEs | 16 December 2016, 3 January 2017 | Additional data to the publication not provided. Finally Mrowietz study was classified in the 'Awaiting classification' section. |
| Ongoing studies | ||||
| CTRI/2016/10/007345 | Dr Piyush Agarwal, general manager Glenmark Pharmaceuticals Ltd DrPiyush.Agarwal@glenmarkpharma.com Amol.Pendse@glenmarkpharma.com |
Asking for study protocol and efficacy/safety results | 11 February 2020 | No response |
| NCT01558310a | Dr Yamauchi, Dr Patnaik, Director, Clinical Science Institute | Asking for study protocol and efficacy/safety results | 5 January 2017 | Email response: Dear Dr Sbidian,
"Thank you for your kind email, forwarded to me by Dr Paul Yamauchi, MD,PhD. Our " Study to Evaluate the Effectiveness of STELARA ™ (USTEKINUMAB) in the Treatment of Scalp Psoriasis (NCT 01558310)” completed enrolment in December 2016 and the last subject will complete in December 2017, as such we do not have the final data analysis. What is you absolute cut‐ off for publication data ? Would an interim analysis report be acceptable? Best regards, Rickie Patnaik Director, Clinical Science Institute" Will be included when published |
| EUCTR2013‐004918‐18‐NL | Prof. Spuls | Asking for study protocol and efficacy/safety results | 5 January 2017 | Email response "The study is currently ongoing and has not yet been analysed. Therefore, we are not able to provide data on efficacy or safety. We can provide you with the study protocol. Will this be helpful? Kind regards, Phyllis Spuls and Celine Busard " Will be included when published |
| NCT02701205 | Prof Hongzhong Jin | Asking for study protocol and efficacy/safety results | 3 June 2019 11 February 2020 |
Email response "This is the mail system at host mta‐8_BSR. Your message could not be delivered to one or more recipients." |
AE: adverse events; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; QoL: quality of life; SAE: serious adverse events
Once a year, we manually check additional sources (regulatory agencies and pharmaceutical company trial registries).
We searched reviews submitted to the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for drug registration (using www.accessdata.fda.gov/scripts/cder/drugsatfda and www.ema.europa.eu/ema) up to 8 September 2020.
Adverse events
We did not perform a separate search for rare or delayed adverse events of the target interventions. However, we examined data on adverse events from the included studies we identified.
Annual review of search methods for this living systematic review
Once a year we revisit our search methods, and if necessary, update the search strategies by adding or removing intervention terms. This ensures the strategies reflect any terminology changes in the topic area, or changes to search terms available in the databases we search.
Data collection and analysis
Selection of studies
We conducted the selection process through Covidence (Covidence 2019), a web tool allowing dual screening of search results based on titles and abstracts, and then full text by independent review authors. Thus, two review authors (from SA, ES, LLC for this update) independently examined each title and abstract to exclude irrelevant reports. These authors independently examined full‐text articles to determine eligibility. We contacted study authors for clarification when necessary and discussed disagreements to reach consensus. We list excluded studies and document the primary reason for exclusion.
As this is a living systematic review, we immediately screened any new citations retrieved by the monthly searches.
Data extraction and management
Two review authors (SA, ES for this update) extracted the data from published and unpublished reports independently, using a standardised form. We pilot‐tested this form (Data Extraction Form) on a set of included trials. We extracted the data to populate the 'Characteristics of included studies' tables in Review Manager 5 (RevMan) (Revman 2020).
We extracted the data from the reports of the US FDA when available, and if not from the US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov), and finally from the published reports.
Outcome data
We extracted arm‐level data from each included trial; hence, the total number of participants randomised to each intervention. For binary outcomes, we also extracted the number of participants (if available) who:
reached PASI 90, PASI 75, or PGA 0/1 during the induction phase;
reached PASI 90, PASI 75 during the maintenance phase (at week 52); and
had at least one SAE/one AE during the induction phase.
For quality of life, we extracted from each included trial the mean change score of the study‐specific scale from baseline to follow‐up.
For assessment of quality of life, we recorded all specific quality‐of‐life (QoL) scales (Dermatology Life Quality Index (DLQI), Skindex, Psoriasis Disability Index (PDI), and Psoriasis Symptom Inventory (PSI)).
Data on potential effect modifiers
We extracted baseline demographic and clinical characteristics of participants that may have acted as effect modifiers (age, sex, body weight, duration of psoriasis, severity of psoriasis at baseline, previous psoriasis treatment). Two review authors (SA, ES) checked and entered the data into the Review Manager 5 (Revman 2020) computer software. We contacted the authors of the trials to request missing data, including missing data for outcomes (see Table 2).
Assessment of risk of bias in included studies
We used Cochrane's 'Risk of bias' (RoB) tool to assess the risks of bias. Two review authors (LLC and SA for this update) independently assessed the risk of bias, and one author (ES for this update) resolved any disagreements. For each of the following domains and according to the general principles in section 8.4 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017), we judged the following 'Risk of bias' domains as 'low', 'high', or 'unclear'.
-
Selection bias (random sequence generation and allocation concealment items)
Was the allocation sequence adequately generated? We considered randomisation adequate (low risk of bias) if the allocation sequence was generated from a table of random numbers or was computer‐generated. We considered randomisation inadequate (high risk of bias) if sequences could be related to prognosis. We considered randomisation unclear if the paper stated that the trial was randomised, but did not describe the method.
Was allocation adequately concealed? We deemed allocation concealment as adequate if the report stated that it was undertaken by means of sequentially pre‐numbered sealed opaque envelopes or by a centralised system. We considered a double‐blind double‐dummy process as being at low risk of bias even if the paper did not describe the method of allocation concealment.
-
Performance and detection bias (blinding of participants,and blinding of outcome assessor items)
Was knowledge of the allocated intervention adequately prevented during the study? We evaluated the risk of bias separately for personnel and participants, outcomes assessors, and each outcome.
-
Attrition bias (incomplete outcome data item)
Were incomplete outcome data adequately addressed? We examined if there was imbalance across intervention groups in numbers or reasons for missing data, type of measure undertaken to handle missing data, and whether the analysis was carried out on an intention‐to‐treat (ITT) basis. We assessed the use of strategies to handle missing data.
-
Reporting bias (selective outcome reporting item)
Were reports of the study free of suggestion of selective outcome reporting? We evaluated if each outcome was measured, analysed, and reported. We compared outcomes specified in protocols (if available on the FDA website or ClinicalTrials.gov) and in material and methods with outcomes presented in the Results section. We considered reporting bias inadequate if one specified outcome in the protocols was lacking in the main report.
-
Other risk of bias
We did not address the 'Other risk of bias' item as we did not highlight particular circumstances leading to other risk of bias from particular trial designs, contamination between the experimental and control groups, and particular clinical settings.
Overall risk of bias
To summarise the quality of evidence and to interpret the network results, we used these six RoB criteria (random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessor, incomplete outcome data, and selective outcome reporting) in order to classify each trial.
We would classify the trial as having low risk of bias if we rated none of the domains above as high risk of bias and two or fewer as unclear risk.
We would classify the trial as having moderate risk of bias if we rated one domain as high risk of bias, one or fewer domains as unclear risk, or no domains as high risk of bias, but three or fewer were rated as unclear risk.
All other cases were assumed to pertain to high risk of bias.
Measures of treatment effect
For each pair‐wise comparison and each dichotomous outcome at each time point, we used risk ratios (RRs) with 95% confidence intervals (CIs) as a measure of treatment effect. For continuous variables (e.g. quality‐of‐life scale), we used the standardised mean difference (SMD) with a 95% CI.
For every treatment, we estimated the ranking probabilities of being at each possible rank for all outcomes. We inferred on treatment hierarchy using the surface under the cumulative ranking curve (SUCRA) (Salanti 2011). SUCRA was expressed as a percentage between 0 (when it is certain a treatment is the worst) to 100% (when it is certain a treatment is the best). The advantage of SUCRA compared to other ranking measures is that it takes into account the entire distribution of the relative effects. (For more information on SUCRA, see Chaimani 2017b; Chaimani 2017c; Veroniki 2018). It should be noted, though, that ranking measures might be of limited value in the presence of large uncertainty in the results and therefore they should always be reported along with the relative effects.
Unit of analysis issues
The primary unit of analysis was the participant. We did not consider studies with non‐standard design features that would lead to clustering (e.g. cross‐over trials).
We treated comparisons from trials with multiple intervention groups as independent two‐arm studies in the pair‐wise meta‐analyses. In this analysis, different comparisons were analysed separately and therefore no study participants were double‐counted. At the network meta‐analysis stage, we properly accounted for the within‐trial correlation.
Dealing with missing data
We extracted, when possible, both the number of randomised and analysed participants in each study arm. We contacted trial authors or sponsors by email to request missing outcome data (numbers of events and numbers of participants for important dichotomous clinical outcomes) when these were not available in study reports that were less than 10 years old (See Table 2). For the main analysis, we assumed that any participant with missing outcome data did not experience clearance (for efficacy outcomes) or did not experience AEs (for safety outcomes), whatever the group. In a sensitivity analysis, we also synthesised the data ignoring the missing participants (complete case analysis), assuming that they were missing at random (Mavridis 2014).
Assessment of heterogeneity
We undertook meta‐analyses only if we judged participants, interventions, comparisons, and outcomes to be sufficiently similar (section 10.10 of the Cochrane Handbook for Systematic Reviews of Interventions) (Deeks 2021). Potential sources of heterogeneity included participants' baseline characteristics (weight, previous systemic treatment or not, treatment doses, co‐interventions, and duration of treatment). When enough data were available, we investigated the distributions of these characteristics across studies and treatment comparisons. The latter allows assessing transitivity, i.e. whether there were important differences between the trials evaluating different comparisons other than the treatments being compared (Salanti 2014). To further reassure the plausibility of the transitivity assumption, we only included in our analyses trials not involving co‐interventions. To better reassure the plausibility of transitivity, we excluded from the main analysis trials including biological‐naïve participants, but assessing efficacy of a biological agent. Indeed, response to biologics is different depending on treatment status (systemic‐naïve or not).
In the classical meta‐analyses, we assessed statistical heterogeneity by visual inspection of the forest plots and using the Q‐test and the I2 statistic. We interpreted the I2 statistic according to the following thresholds (section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions; Deeks 2021): 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% represents considerable heterogeneity.
In the network meta‐analysis, the assessment of statistical heterogeneity in the entire network was based on the estimated heterogeneity variance parameter (τ2) estimated from the network meta‐analysis models (Jackson 2014). We also estimated the prediction intervals to assess how much the estimated heterogeneity affects the relative effects with respect to the additional uncertainly anticipated in future studies (Riley 2011). Where feasible, we would have investigated the possible sources of heterogeneity in subgroup analyses and meta‐regression.
Although we restricted the risk of important heterogeneity in our data by considering eligible only studies without co‐interventions, we investigated differences in heterogeneity across the different analyses. Specifically, we observed whether splitting the nodes of the network and analysing each drug and each dose separately reduced the heterogeneity estimate. We also ran a series of sensitivity analyses (see Sensitivity analysis), and we monitored whether heterogeneity became smaller or larger compared to the primary analysis.
Assessment of reporting biases
To assess reporting biases, we used an adaptation of the funnel plot by subtracting from each study‐specific effect size the mean of meta‐analysis of the study‐specific comparison, which we plotted against the study standard error (Chaimani 2013). We employed this 'comparison‐adjusted funnel plot' for all comparisons of an active treatment against placebo. When we detected substantial funnel plot asymmetry for the two primary outcomes, we investigated the presence of small‐study effects in the network meta‐regression (Chaimani 2012).
Data synthesis
Pairwise meta‐analysis
We conducted pair‐wise meta‐analyses to synthesise trials comparing one of the treatments against placebo or two treatments against each other. We performed pair‐wise meta‐analyses for all outcomes and comparisons, provided that at least two studies were available, using a random‐effects model.
Network meta‐analysis
We then employed network meta‐analysis (NMA) for all outcomes and comparisons, to estimate the relative effects for all possible comparisons between any pair of treatments within a frequentist framework. We provided a graphical depiction of the evidence network for all outcomes to illustrate the network geometry (Chaimani 2017a). We ran network meta‐analysis using the approach of multivariate meta‐analysis, which treats the different comparisons that appear in studies as different outcomes (White 2012).
We focused on confidence intervals as a finding of uncertainty, as confidence intervals were sufficiently narrow to rule out an important magnitude of effect.
We assessed inconsistency (i.e. the possible disagreement between the different pieces of evidence) locally and globally. Specifically, we used the loop‐specific approach (Bucher 1997) and the side‐splitting method (Dias 2010). We also fitted the design by treatment interaction model to evaluate the presence of inconsistency in the entire network (Higgins 2012).
We conducted pair‐wise meta‐analyses using Review Manager 5 (Revman 2020), and we performed all other analyses in Stata 14 using the 'network' (www.stata-journal.com/article.html?article=st0410) and 'network graphs' packages (www.stata-journal.com/article.html?article=st0411).
As this is a living systematic review, whenever we found new evidence (i.e. studies, data or information) meeting the review inclusion criteria, we extracted the data and assessed risks of bias. For trials identified as completed in clinical trial registries but without posted results or those identified only by a conference proceeding, and for missing outcome data, trained review authors contacted trialists to request complete results. Every six months, we incorporated each newly‐identified trial in the network. We performed one network for each outcome (PASI‐90, SAEs, PASI‐75, PGA, QoL and AEs). We re‐analysed the data every six months using the standard approaches outlined in this Data synthesis section, as well as the CiNeMa process. We checked the assumptions of the NMA each time we updated the analysis.
Subgroup analysis and investigation of heterogeneity
We had planned to undertake subgroup analyses and meta‐regressions to investigate potential sources of heterogeneity or inconsistency (such as weight of participants, duration of psoriasis, baseline severity, previous systemic treatments) during the induction phase, but we found no heterogeneity or inconsistency.
Sensitivity analysis
To assess the robustness of our results, we performed the following sensitivity analyses for the two primary outcomes:
running the analysis at dose‐level, considering that each different drug dose is a different intervention;
excluding trials at high risk of bias;
excluding trials with a total sample size smaller than 50 randomised participants;
analysing only the observed participants and assuming that missing participants are missing at random;
analysing only the studies with a short‐term assessment from 8 to 16 weeks (to better reassure the plausibility of the transitivity assumption);
including all trials irrespective of the previous systemic‐treatments received by the participants;
lastly, we assessed SAEs after excluding flares of psoriasis.
We undertook this analysis because it has recently been reported that after excluding cases of worsening psoriasis, the risk of occurrence of SAEs is higher in the biologic (especially for anti‐TNF agents) than in the placebo arm (Afach 2021).
Summary of findings and assessment of the certainty of the evidence
We did not include 'Summary of findings' (SoF) tables because the format of an SoF table does not allow us to present a summary of comparisons across the different drugs. The SoF tables in the last version of the review only focused on the comparisons against placebo.
We assessed the confidence of the evidence estimates from network meta‐analysis, based on the CINeMA approach which is based on the contributions of the direct comparisons to the estimation in the network meta‐analysis (CINeMA 2017; Salanti 2014). CINeMA (Confidence in Network Meta‐Analysis) is a web application that simplifies the evaluation of confidence in the findings from network meta‐analysis.
It is based on six domains: within‐study bias (referring to the impact of risk of bias in the included studies), across‐studies bias (publication or reporting bias), indirectness (relevance to the research question and transitivity), imprecision (comparing the range of treatment effects included in the 95% confidence interval with the range of equivalence), heterogeneity (predictive intervals), and incoherence (if estimates from direct and indirect evidence disagree) (Salanti 2014).
The confidence in each NMA RRAB between two given drugs A and B was evaluated for six domains. The software required some input in each domain in order to recommend whether there were 'major concerns', 'some concerns' or 'no concerns' for the particular domain.
Thus, threshold values and evaluation rules to be decided were finalised through discussions. After determining these rules, the remaining synthesis of confidence in the evidence can be automatically calculated via CINeMA web app; hence one review author finally input all the data and got the results.
Within‐trial bias: we estimated it as the weighted average of the overall risk of bias of all the trials contributing information to the estimation of RRAB.
Reporting bias: also known as 'publication bias'. We assessed publication bias by considering the comprehensive search strategy that we performed and the risk of publication bias in the specific field. The comparison‐adjusted funnel plots that test the presence of small‐study effects in the network assisted our judgement.
Indirectness: since the included studies matched the clinical question of the review, we had 'no concern' about any of the evaluated RRAB.
Imprecision: this was rated based on whether the 95% CI of RR was allowing recommendations to be made. We set the margin of equivalent effects (where none of the drugs is favoured) to between RR 0.95 and 1.05. These values were motivated by the fact that assuming 3% response rate (reaching PASI 90) for placebo, then an RRAB of 1.05 indicated a response for drug A higher than those obtained with placebo, which we considered as clinically meaningful. Then, the degree of overlap between the 95% CI of RRAB and the margin of equivalent effects suggests the judgement.
Heterogeneity: this was evaluated by monitoring the agreement between confidence intervals (CIs) and prediction intervals (PIs). CINeMA judges whether the two intervals and their overlap with the margin of equivalent effects provide similar conclusions.
Incoherence: this was evaluated by monitoring the level of disagreement between confidence intervals (CIs) of the direct and indirect RRAB and their overlap with the margin of equivalent effects.
After the judgement for all the six domains, we summarised the overall confidence in evidence for each RR between any two drugs into high, moderate, low and very low. Starting with high confidence, we downgraded by one level for each ‘major concern’ in any of the six domains; then by two‐thirds of a level down for ‘some concerns’ in ‘within‐study bias’; one‐third of a level down for each ‘some concerns’ in any of the other five domains. To obtain the final level, we rounded the number of downgrades to their nearest integer.
For each drug, we calculated the percentage of the four levels based on all comparisons including that drug, for efficacy and safety.
Results
Description of studies
Results of the search
Recent monthly Electronic searches of databases and trials registers for this living systematic review have identified an additional 1657 references for potentially eligible studies. We have also re‐examined 53 studies from the previous version of this review identified as ongoing (42 studies reported in 44 references) or awaiting classification (11 reported in 18 references). We have therefore screened a total of 1719 references for this update.
After reviewing the titles and abstracts, we discarded 1555 references. We examined the full text of the remaining 164 references. Seventeen studies (reported in 18 references) did not meet the inclusion criteria and were excluded (see Characteristics of excluded studies). Twenty‐eight trials (reported in 38 references) were identified as studies awaiting classification (see Characteristics of studies awaiting classification). We identified 29 studies (reported in 34 references) as ongoing (see Characteristics of ongoing studies). We identified 18 new included studies (reported in 34 references) for this update. We also identified 40 references which related to studies previously included in this review.
Combining the 18 new included studies with the 140 previously identified in earlier versions of this review, we have a total of 158 studies reported in 347 references.
For a further summary of our screening process, see the study flow diagram (Figure 1).
1.
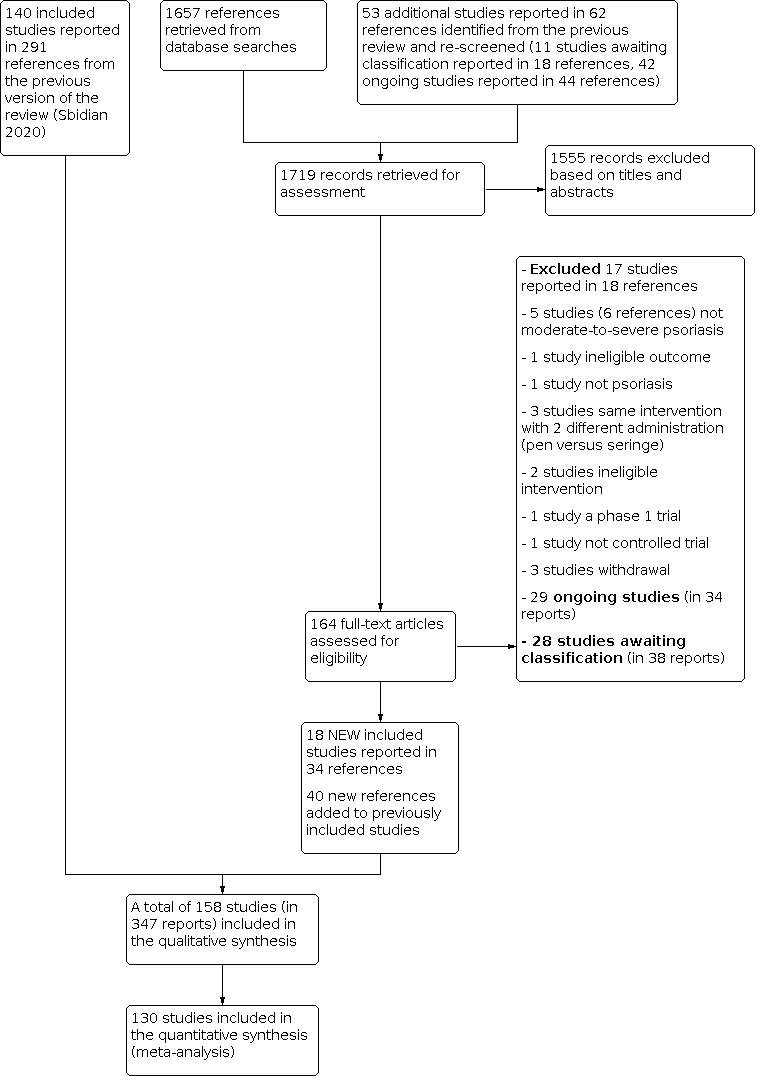
tudy flow diagram
Included studies
Trial design
All trials used a parallel‐group design. The mean sample size was 365 (range: 10 to 1881). In all, 133 trials were multicentric (2 to 231 centres) and 18 were single‐centre trials (Akcali 2014; Al‐Hamamy 2014; Asawanonda 2006; Chaudhari 2001; Chladek 2005; Dogra 2012; Dogra 2013; Dubertret 1989; Ellis 1991; VIP‐U Trial 2020; Gisondi 2008; Gurel 2015; Hunter 1963; Ikonomidis 2017; Khatri 2016; Mahajan 2010; Shehzad 2004; Van Bezooijen 2016); for seven trials, single‐centre or multicentric status was not clear (Caproni 2009; Engst 1994; Goldfarb 1988; Jin 2017; Olsen 1989; Yilmaz 2002; Yu 2019). Most of the trials recruited participants from a hospital setting, but some also from physicians' offices. The trials took place worldwide (n = 65, 42%), in Europe (n = 35, 22%), in North America (n = 28, 18%), in Asia (n = 25, 16%), or in the Middle East (n = 1, 0.7%). The location was not stated for four trials (Caproni 2009; Engst 1994; Goldfarb 1988; Olsen 1989).
In total, 78 trials out of 158 were multi‐arm; 53 multi‐arm trials assessed the same experimental drug at multiple dose levels; 14 assessed at least two different drugs; 11 assessed both the same experimental drug at multiple dose levels and different drugs. In total, eight trials assessed biosimilars versus original drugs for adalimumab (ADACCESS 2018; AURIEL‐PsO 2020; PsOsim 2017; NCT02581345; NCT02850965; Papp 2017a) and etanercept (EGALITY 2017; NCT02134210).
In total, 16 trials (Al‐Hamamy 2014; Asawanonda 2006; Bissonnette 2013; Gottlieb 2012; Gurel 2015; Lowe 1991; Mahajan 2010; NCT02313922; Ruzicka 1990; Saurat 1988; Shehzad 2004; Sommerburg 1993; Tanew 1991; Van Bezooijen 2016; Yilmaz 2002; Yu 2019) had a co‐intervention, mainly with phototherapy. Only 14 studies were carried out before the year 2000 (Dubertret 1989; Ellis 1991; Engst 1994; Goldfarb 1988; Hunter 1963; Laburte 1994; Lowe 1991; Meffert 1997; Nugteren‐Huying 1990; Olsen 1989; Ruzicka 1990; Saurat 1988; Sommerburg 1993; Tanew 1991).
Characteristics of the participants
This review includes 158 trials (18 new trials for the updated review), with a total of 57,831 randomised participants. We summarise the characteristics of the participants in the Characteristics of included studies. The participants were reported to be between 27 and 56.5 years old, with an overall mean age of 45; there were more men (38,877) than women (18,487). Age and gender were unreported for, respectively, 1643 and 467 participants (15 and 8 studies). The overall mean weight was 85.4 kg (range: 64 to 100.5 kg), and the overall mean Psoriasis Area and Severity Index (PASI) score at baseline was 20 (range: 9.5 to 39). The duration of psoriasis was 18 years (range 7 to 21.5).
Characteristics of the comparisons
Trials with two parallel arms (the different dose groups were grouped together in one 'arm')
Intervention versus placebo: 92 trials compared systemic treatments with placebo
Twenty‐two trials compared non‐biological systemic treatments versus placebo
Acitretin (n = 9) (Goldfarb 1988; Gurel 2015; Lowe 1991; Olsen 1989; Ruzicka 1990; Saurat 1988; Sommerburg 1993; Tanew 1991; Yilmaz 2002)
Fumaric acid esters (FAEs) (n = 3) (Nugteren‐Huying 1990; BRIDGE 2017; Van Bezooijen 2016)
Ciclosporin (n = 2) (Ellis 1991; Meffert 1997)
Methotrexate (n = 8) (Al‐Hamamy 2014; Asawanonda 2006; Gottlieb 2012; Hunter 1963; Mahajan 2010; NCT02313922; Shehzad 2004; METOP 2017)
Thirteen trials compared small molecule treatments versus placebo
Apremilast (n = 6) (Ohtsuki 2017; Papp 2012c; Papp 2013b; ESTEEM‐1 2015; ESTEEM‐2 2015; STYLE 2020)
Tofacitinib (n = 6) (Jin 2017; Krueger 2016a; Papp 2012b; OPT Pivotal‐1 2015; OPT Pivotal‐2 2015; Zhang 2017)
Oral tyrosine kinase 2 (TYK2) inhibitor (BMS‐986165) (n = 1) (Papp 2018)
Fifty‐seven trials compared biological treatments versus placebo
-
Anti‐TNF alpha
Etanercept (n = 8) (Bagel 2012; Gottlieb 2003a; Gottlieb 2011; Leonardi 2003; Papp 2005; Strober 2011; Tyring 2006; Van de Kerkhof 2008)
Adalimumab (n = 7) (Asahina 2010; Bissonnette 2013; Cai 2016; Elewski 2016; Gordon 2006; REVEAL 2008; VIP Trial 2018)
Infliximab (n = 6) (Chaudhari 2001; Gottlieb 2004a; EXPRESS‐II 2007; EXPRESS 2005; Torii 2010; Yang 2012)
Certolizumab (n = 4) (CIMPASI‐1 2018; CIMPASI‐2 2018; NCT03051217; Reich 2012a)
Intervention versus active comparators: 48 trials compared systemic treatments with systemic treatments
Acitretin versus acitretin (n = 1) (Dogra 2013)
Acitretin versus ciclosporin (n = 1) (Akcali 2014)
Ciclosporin versus methotrexate (n = 4) (Flytström 2008; Heydendael 2003; Piskin 2003, Sandhu 2003)
Ciclosporin versus ciclosporin (n = 3) (Dubertret 1989; Engst 1994; Laburte 1994)
Methotrexate versus methotrexate (n = 2) (Chladek 2005; Dogra 2012)
Methotrexate versus FAEs (n = 1) (Fallah Arani 2011)
Methotrexate versus infliximab (n = 1) (Barker 2011)
Acitretin versus etanercept (n = 4) (Caproni 2009; Gisondi 2008; Lee 2016; Yu 2019)
FAEs versus secukinumab (n = 1) (PRIME 2017)
FAEs versus guselkumab (n = 1) (POLARIS 2020)
FAEs versus risankizumab (n = 1) (NCT03255382)
FAEs versus Brodalumab (n = 1) (NCT03331835)
Etanercept versus etanercept (n = 5) (EGALITY 2017; NCT02134210; Ortonne 2013; PRESTA 2010; PRISTINE 2013)
Etanercept versus infliximab (n = 1) (PIECE 2016)
Etanercept versus ustekinumab (n = 1) (ACCEPT 2010)
Adalimumab versus adalimumab (n = 6) (ADACCESS 2018; AURIEL‐PsO 2020; PsOsim 2017; NCT02581345; NCT02850965; Papp 2017a)
Tofacitinib versus tofacitinib (n = 2) (Asahina 2016; Bissonnette 2015)
Secukinumab versus secukinumab (n = 2) (SCULPTURE 2015; SIGNATURE 2019)
Secukinumab versus ustekinumab (n = 2) (CLEAR 2015; CLARITY 2018)
Secukinumab versus guselkumab (n = 1) (ECLIPSE 2019)
Ixekizumab versus ixekizumab (n = 2) (Khatri 2016; IXORA‐P 2018)
Ixekizumab versus ustekinumab (n = 1) (IXORA‐S 2017)
Ixekizumab versus guselkumab (n = 1) (IXORA‐R 2020)
Risankizumab versus adalimumab (n = 1) (IMMvent 2019)
Risankizumab versus ustekinumab (n = 1) (Papp 2017b)
Risankizumab versus secukinumab (n=1) (IMMerge 2021)
Trials with three parallel arms (the different dose groups were grouped together in one 'arm')
18 trials compared systemic treatments with systemic treatments and placebo.
Methotrexate versus adalimumab versus placebo (n = 1) (CHAMPION 2008)
Etanercept versus ixekizumab versus placebo (n = 2) (UNCOVER‐2 2015; UNCOVER‐3 2015)
Etanercept versus secukinumab versus placebo (n = 1) (FIXTURE 2014)
Etanercept versus apremilast versus placebo (n = 1) (LIBERATE 2017)
Guselkumab versus adalimumab versus placebo (n = 3) (VOYAGE‐1 2016; Gordon X‐PLORE 2015; VOYAGE‐2 2017)
Brodalumab versus ustekinumab versus placebo (n = 2) (AMAGINE‐2 2015; AMAGINE‐3 2015)
Tofacitinib versus etanercept versus placebo (n = 1) (Bachelez 2015)
Certolizumab versus etanercept versus placebo (n = 1) (CIMPACT 2018)
Ustekinumab versus etanercept versus ciclosporin (n = 1) (Ikonomidis 2017)
Tildrakizumab versus etanercept versus placebo (n = 1) (ReSURFACE‐2 2017)
Risankizumab versus ustekinumab versus placebo (n = 2) (UltIMMa‐1 2018; UltIMMa‐2 2018)
Ixekizumab versus Methotrexate versus FAEs (n = 1) (Reich 2020)
Adalimumab versus secukinumab versus placebo (n = 1) (CARIMA 2019)
In total, the dataset consisted of 158 studies, which provide information on 194 direct comparisons between 36 different drug dosages, 20 different drugs, six different drug classes, and placebo. For the sensitivity analyses, the different drug doses were divided into approved dosages versus other dosages:
methotrexate, taken orally, ≥ 15 or < 15 mg a week;
ciclosporin, taken orally, ≥ 3 or < 3 mg/Kg a day;
acitretin, taken orally, ≥ 35 or < 35 mg a day;
apremilast, taken orally, 30 mg twice a day or other dosages;
tofacitinib, taken orally, 20 mg a day or other dosages;
etanercept, subcutaneous (S/C), 25 mg twice a week or etanercept 50 mg twice a week;
infliximab, intravenous, 5 mg/kg at week 0, 2, and 4 then every 6 weeks, or other dosages;
adalimumab, S/C, 80 mg at week 0, 40 mg at week 1 then 40 mg every other week or other dosages;
certolizumab, S/C, 400 mg at week 0, 2, 4 then 400 mg every other week, or other dosages;
secukinumab, S/C, 300 mg at week 0, 1, 2, 3, and 4 then every 4 weeks, or other dosages;
ixekizumab, S/C, 160 mg at week 0 then 80 mg every other week until week 12 then 80 mg monthly, or other dosages;
brodalumab, S/C, 210 mg at week 0, 1, 2, then every other week, or other dosages;
guselkumab, S/C, 100 mg at week 0 and 4 then every 8 weeks, or other dosages;
tildrakizumab, S/C, 100 mg at week 0 and 4 then every 12 weeks, or other dosages;
risankizumab, S/C, 150 mg (2 x 75 mg injections) at week 0, week 4 and every 12 weeks thereafter, or other dosages.
FAEs (taken orally), BMS‐986165 (taken orally), ustekinumab (S/C 45 mg or 90 mg according to the weight), bimekizumab (S/C) and mirikizumab (S/C) were grouped in one dosage, whatever the dosages.
For each study, we provide details of the dosage in Characteristics of included studies.
Characteristics of the outcomes
For the efficacy outcomes during induction therapy (less than 24 weeks), out of the 158 trials, 125 reported PASI 90, 114 reported on Physician Global Assessment (PGA) 0/1, 137 reported PASI 75, and 57 trials reported assessment of change in quality of life. Fifty‐eight studies used the dermatology‐specific instrument Dermatology Life Quality Index (DLQI); six studies used other specific skin instruments (Skindex and PSS). For all of these studies, the investigators provided citations to reports indicating that the tools had been previously validated. For efficacy outcomes during maintenance phase (52 weeks), 11 trials reported PASI 90 at one year (VOYAGE‐1 2016; UltIMMa‐1 2018; UltIMMa‐2 2018; IXORA‐P 2018; NCT03482011; Ohtsuki 2017; Ohtsuki 2018; JUNCTURE 2015; ECLIPSE 2019; CLEAR 2015; IMMerge 2021) and 11 reported PASI 75 at one year (VOYAGE‐1 2016; UltIMMa‐1 2018; UltIMMa‐2 2018; IXORA‐P 2018; NCT03482011; Ohtsuki 2017; Ohtsuki 2018; JUNCTURE 2015; ECLIPSE 2019; CLEAR 2015; Zhang 2017).
Out of 158 trials, 116 reported the number of participants with adverse events (different from the number of adverse events), and 131 reported the number of serious adverse events.
These outcomes were evaluated between 8 and 24 weeks: eight weeks (five studies), 10 weeks (seven studies), 12 weeks (72 studies), 13 weeks (two studies), 15 weeks (one study), 16 weeks (49 studies), 24 weeks (15 studies) and 26 weeks (two studies). Timing of assessment was unknown or not clearly defined for four studies (Engst 1994; Hunter 1963; Saurat 1988; Shehzad 2004); one study had only a timing of assessment at 52 weeks (IXORA‐P 2018).
Funding
In all, 132 studies declared a source of funding: 123 studies declared a pharmaceutical company funding, nine studies declared a unique institutional funding (Chladek 2005; PIECE 2016; Flytström 2008; Heydendael 2003; Ikonomidis 2017; VIP Trial 2018; NCT02313922; Reich 2020; Yu 2019), four studies had no funding source (Akcali 2014; Asawanonda 2006; Fallah Arani 2011; Gurel 2015), and 22 studies did not report the source of funding (Al‐Hamamy 2014; Caproni 2009; Dogra 2012; Dogra 2013; Dubertret 1989; Engst 1994; Gisondi 2008; Hunter 1963; Jin 2017; Laburte 1994; Mahajan 2010; Meffert 1997; Nugteren‐Huying 1990; Piskin 2003; Ruzicka 1990; Sandhu 2003; Saurat 1988; Shehzad 2004; Sommerburg 1993; Torii 2010; Yang 2012; Yilmaz 2002).
Excluded studies
We have excluded a total of 411 studies in 425 references throughout the course of this review.
For this update, we excluded 17 studies (reported in 18 references). The reasons for exclusion were: in five studies (six references) the participants did not present with moderate‐to‐severe psoriasis, one study had ineligible outcomes, one study did not assess psoriasis, three studies assessed the same intervention with two different administration routes (pen versus syringe), two studies had ineligible interventions, one study was a phase 1 trial, one study was not a controlled trial, and three studies were withdrawn. We detail all the reasons for exclusion in Characteristics of excluded studies and our study flow diagram at Figure 1.
We excluded seven previously included studies (total of 17 references) from the previous review because the interventions no longer meet the inclusion criteria for the review (ponesimod (Vaclavkova 2014 ‐ development of the drug for psoriasis stopped), alefacept (Ellis 2001; Jacobe 2008; Krueger 2002a; Lebwohl 2003; Yan 2011 ‐ not used anymore for psoriasis), itolizumab (Krupashankar 2014 ‐ not approved)). We excluded 166 for other reasons.
For seven studies with three arms, one arm was not included, as the intervention was not included in our search:
Saurat 1988: acitretin versus placebo versus etretinate (etretinate arm was not included);
Shehzad 2004: PUVA (psoralen and ultraviolet A) therapy versus methotrexate (methotrexate only was included);
Gottlieb 2011; Strober 2011: briakinumab versus etanercept versus placebo (briakinumab arm was not included);
Gisondi 2008: etanercept versus acitretin versus etanercept plus acitretin (etanercept plus acitretin arm was not included);
Al‐Hamamy 2014: narrowband ultraviolet B phototherapy plus methotrexate versus narrowband ultraviolet B alone and methotrexate alone (arm with methotrexate alone was not included);
VIP Trial 2018: adalimumab versus narrowband ultraviolet B phototherapy versus placebo (arm with narrowband ultraviolet B phototherapy was not included);
Lee 2016: etanercept versus acitretin versus etanercept plus acitretin (arm with etanercept plus acitretin was not included).
Thaçi 2002 compared two different dosages of ciclosporin (a fixed dosage of 200 mg/day and a dosage corresponding to 2.5 mg/kg/day), and we were unable to classify the fixed dosage group either in the ciclosporin ≥ 3 mg/kg/day group or in the ciclosporin < 3 mg/day group for the subgroup meta‐analysis.
In an earlier version of this review (Sbidian 2017), we excluded a number of studies having reviewed the full text, but without creating Characteristics of excluded studies tables (n = 203). The main reason for exclusion of these studies was that the participants did not present with moderate‐to‐severe psoriasis.
Studies awaiting classification
We classified 28 trials reported in 38 references as studies awaiting classification. More details are available in Studies awaiting classification and Table 2. Most of the awaiting studies compare a biological treatment versus another biological treatment or versus non‐biological treatment or versus placebo (n = 21). One study assessed a small molecule, and six assessed non‐biological systemic treatments.
Ongoing studies
We classified 29 trials (reported in 34 references) as ongoing studies. More details are available in Characteristics of ongoing studies and Table 2. Most of the ongoing studies compare a biological treatment versus another biological treatment or versus placebo (n = 21). Six ongoing studies assessed apremilast or oral tyrosine kinase 2 (TYK2) inhibitor, and two assessed non‐biological systemic treatments.
Risk of bias in included studies
Figure 2 and Figure 3 summarise 'Risk of bias' assessments. For overall risk of bias across studies, 80 (51%) trials were at low risk of bias. We categorised a third of the studies (53/158, 33.5%) as being at high risk of bias. We categorised the remaining 25 studies as being at unclear risk of bias. Further details of these assessments are available in the 'Risk of bias' table corresponding to each trial in the Characteristics of included studies.
2.

'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study
3.

'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies
Allocation
In 55 trials the method of sequence generation was not described at all, or was at best unclear. The remaining studies (n = 103) described the method used to generate the allocation sequence in sufficient detail, and we therefore judged this domain as low risk of bias for these studies. For allocation concealment, most studies (n = 93) received a judgement of low risk of bias. We considered the risk unclear for the 65 remaining trials because of the absence of reporting of the method used to guarantee concealment.
Blinding
Blinding of participants and personnel was achieved in 105 studies, whereas 43 studies were at high risk of performance bias. The remaining 10 studies were at unclear risk of performance bias. Blinding of outcome assessment was reported clearly in only 111 of the 158 included studies, whereas 26 studies were at high risk of detection bias. The risk of detection bias was unclear in the remaining 21 studies.
Incomplete outcome data
In more than two‐thirds of the trials (105/158) incomplete outcome data appeared to have been adequately addressed, and any missing outcome data were reasonably well‐balanced across intervention groups, with similar reasons for missing data across the groups. However, in 18 studies the reporting of missing outcome data was largely inadequate because of one or more of the following reasons: the high number of withdrawn participants, an imbalance between groups in the number of withdrawn participants, an imbalance in reasons for missing outcomes, or no intention‐to‐treat (ITT) analysis provided. In 35 studies, this domain was as at unclear risk of bias because the following were not reported: the number of participants, reasons for discontinuation, or missing data imputation.
Selective reporting
We considered 14 trials to be at high risk of selective outcome reporting because results for outcomes detailed in the Methods section were not reported in the Results section (Akcali 2014; Engst 1994; Hunter 1963; AMAGINE‐2 2015; AMAGINE‐3 2015; BRIDGE 2017; Nakagawa 2016; Papp 2013b; Papp 2005; LIBERATE 2017; Shehzad 2004; VIP‐U Trial 2020; PsOsim 2017; CARIMA 2019). In all, we considered 98 studies to be at low risk of bias for this domain, as outcome details in the trial register and in the Methods section were reported in the Results section. For other trials (n = 46), we considered the risk of bias as unclear, because we did not find these trials in any register.
Other potential sources of bias
As detailed in the Methods section, we did not address the 'Other risk of bias' item as we did not highlight particular circumstances leading to other risk of bias from particular trial designs, contamination between the experimental and control groups, and particular clinical settings.
Effects of interventions
Eight trials provided no usable or retrievable data and did not contribute further to the results of this review (Akcali 2014; Chladek 2005; Engst 1994; Ikonomidis 2017; Lowe 1991; Olsen 1989; Piskin 2003; Shehzad 2004; see Table 2). The main reason we could not use their data was that these studies addressed none of our outcomes.
Sixteen studies, involving 1667 participants (2.9% of the participants in this review), had a co‐intervention and did not contribute further to the results of this review, as we could not assess the specific intervention effect (Al‐Hamamy 2014; Asawanonda 2006; Bissonnette 2013; Gottlieb 2012; Gurel 2015; Lowe 1991; Mahajan 2010; NCT02313922; Ruzicka 1990; Saurat 1988; Shehzad 2004; Sommerburg 1993; Tanew 1991; Van Bezooijen 2016; Yilmaz 2002; Yu 2019).
Eight trials assessed biosimilars versus original drugs for adalimumab (ADACCESS 2018; NCT02581345; AURIEL‐PsO 2020; NCT02850965; Papp 2017a; PsOsim 2017) and etanercept (EGALITY 2017; NCT02134210). These were non‐inferiority trials, assessing the same dosage and same administration schema of biosimilar and original drug.
In total, 28 studies, involving 5209 participants, were not included in the classical or network meta‐analysis (reasons are mentioned above). The interventions of the 28 studies concerned the following:
acitretin (n = 9) (Akcali 2014; Gurel 2015; Lowe 1991; Olsen 1989; Ruzicka 1990; Saurat 1988; Sommerburg 1993; Tanew 1991; Yilmaz 2002);
methotrexate (n = 6) (Asawanonda 2006; Al‐Hamamy 2014; Chladek 2005; Gottlieb 2012; Mahajan 2010; Shehzad 2004);
ciclosporin (n = 2) (Engst 1994; Piskin 2003);
adalimumab (n = 7) (Bissonnette 2013; ADACCESS 2018; NCT02581345; AURIEL‐PsO 2020; NCT02850965; Papp 2017a; PsOsim 2017);
etanercept (n = 2) (EGALITY 2017; NCT02134210);
others (n = 2) (Van Bezooijen 2016; Ikonomidis 2017).
We included a total of 130 studies, involving 50,081 participants (86.6% participants of this review), in the classical or network meta‐analysis for at least one of the outcomes.
One study had only long‐term outcome assessments (IXORA‐P 2018).
Ten studies, involving 2132 participants (4.3% of the participants in this review) included biological‐naïve participants when assessing efficacy of a biological agent, and did not contribute further to the results of the main analysis, as we could not assume the plausibility of transitivity. Indeed, response to biologics is different depending on treatment status (systemic‐naïve or not). However, these studies were included in the sensitivity analysis (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020).
Figure 4 and Figure 5 show the network diagrams for all of the outcomes included in the review. The size of the nodes is proportional to the total number of participants allocated to each class‐level (Figure 4) and drug‐level (Figure 5) intervention, with the thickness of the lines proportional to the number of trials evaluating each direct comparison.
4.

Network plot for all the outcomes at class level
The size of the nodes is proportional to the total number of participants allocated to each intervention and the thickness of the lines proportional to the number of studies evaluating each direct comparison.
AE: adverse events; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; QoL: quality of life; SAE: serious adverse events; SAE without worsening of psoriasis correspond to SAE after exclusion of flares of psoriasis
5.

Network plot for all the outcomes at drug level
The size of the nodes is proportional to the total number of participants allocated to each intervention and the thickness of the lines proportional to the number of studies evaluating each direct comparison.
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
AE: adverse events; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; QoL: quality of life; SAE: serious adverse events; SAE without worsening of psoriasis correspond to SAE after exclusion of flares of psoriasis
Figure 6 shows the network meta‐analysis estimates of all of the outcomes for each comparison at class level.
6.

Relative effects of the class‐level intervention as estimated from the network meta‐analysis model
Outcomes were all measured at the induction phase (assessment from 8 to 24 weeks after randomisation). Drugs are reported in order of primary benefit ranking. Each cell contains the risk ratio (RR) (for dichotomous outcomes: PASI 90, serious adverse events, PASI 75, PGA 0/1, adverse events) or the standardised mean difference (SMD) (for the quality‐of‐life outcome), plus the 95% confidence interval, of the class level in the respective column versus the class level in the respective row. RRs larger than 1 for the lower triangle and smaller than 1 (or SMDs smaller than zero) for the upper triangle favour the treatment on the left. Significant results are highlighted in grey.
AE: adverse events; PASI: Psoriasis Area and Severity Index; PGA: Physician's Global Assessment; QoL: quality of life; SAE: serious adverse events; SAE without worsening of psoriasis correspond to SAE after exclusion of flares of psoriasis; AIL12/23: anti‐IL12/23; AIL17: anti‐IL17; AIL23: anti‐IL23, ATA: anti‐TNF alpha; CSA: non‐biological conventional systemic agents; PBO: placebo; SM: small molecules
Figure 7, Figure 8 and Figure 9 show the network meta‐analysis estimates of all the outcomes for each comparison at drug level.
7.

Relative effects of the intervention as estimated from the network meta‐analysis model for Psoriasis Area and Severity Index (PASI) 90 and serious adverse events (AEs)
Outcomes were all measured at the induction phase (assessment from 8 to 24 weeks after randomisation). Drugs are reported in order of primary benefit ranking. Each cell contains the risk ratio (RR) and 95% confidence interval for the two primary outcomes (PASI 90 and SAEs) of the intervention in the respective column versus the comparator in the respective row. RRs larger than 1 for the lower triangle and smaller than 1 for the upper triangle favour the treatment on the left. Certainty of evidence was assessed for each comparison using CINeMA and classified in high (highlighted in green), moderate (in blue), low (in yellow) and very‐low (in red).
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
8.

Relative effects of the intervention as estimated from the network meta‐analysis model for Psoriasis Area and Severity Index (PASI 75) and adverse events (AEs)
Outcomes were all measured at the induction phase (assessment from 8 to 24 weeks after randomisation). Drugs are reported in order of primary benefit ranking. Each cell contains the Risk Ratio (RR) and 95% confidence interval for the two secondary outcomes (PASI 75 and adverse events) of the intervention in the respective column versus the comparator in the respective row. RRs larger than 1 for the lower triangle and smaller than 1 for the upper triangle favour the treatment on the left. Significant results are are highlighted in grey.
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
9.

Relative effects of the intervention as estimated from the network meta‐analysis model for Physician's Global Assessment (PGA 0/1) and quality of life (QoL)
Outcomes were all measured at the induction phase (assessment from 8 to 24 weeks after randomisation). Drugs are reported in order of primary benefit ranking. Each cell contains the risk ratio (RR) and 95% confidence interval (PGA 0/1) or standardized mean difference (quality of life) of the intervention in the respective column versus the comparator in the respective row. RRs larger than 1 for the lower triangle and smaller than 1 (or SMDs smaller than zero) for the upper triangle favour the treatment on the left. Significant results are are highlighted in grey.
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
Figure 10, Figure 11 and Figure 12 show all of the relative effects from the network meta‐analyses against placebo with their 95% confidence and prediction intervals at class and drug level.
10.

Interval plot. Network meta‐analysis estimates of class‐level versus placebo for all the outcomes
Outcomes were all measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
AE: adverse events; CI: confidence interval; PGA: Physician Global Assessment; PrI: predictive interval; QoL: Specific quality of life scale; RR: risk ratio; SAE: serious adverse events; SAE without worsening of psoriasis correspond to SAE after exclusion of flares of psoriasis; SMD: standardised mean difference; AIL12/23: anti‐IL12/23; AIL17: anti‐IL17; AIL23: anti‐IL23, ATA: anti‐TNF alpha
11.

Interval plot. Network meta‐analysis estimates of the interventions versus placebo for the primary outcomes
CI: confidence interval; PrI: predictive interval; RR: risk ratio; SAE: serious adverse events
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
12.

Interval plot. Network meta‐analysis estimates of the interventions versus placebo for the secondary outcomes
Outcomes were all measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
AE: adverse events; CI: confidence interval; PGA: Physician Global Assessment; PrI: predictive interval; QoL: Specific quality of life scale; RR: risk ratio; SMD: standardised mean difference
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
Figure 13 shows a two‐dimensional ranking plot based on surface under the cumulative ranking curve (SUCRA) values for benefit (PASI 90) and acceptability (serious adverse events) at class and drug level. The different colours represent different groups of interventions considering their performance on both outcomes simultaneously. Interventions belonging to the same group were assumed to have a similar performance when the two primary outcomes were considered jointly (Chaimani 2013).
13.

Ranking plot. Ranking plot representing simultaneously the efficacy (x axis, PASI 90) and the acceptability (y axis, serious adverse events) of all the interventions (class and drug levels) for patients with moderate‐to‐severe psoriasis. Optimal treatment should be characterised by both high efficacy and acceptability and should be in the right upper corner of this graph.
Outcomes were measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
The different colours represent different groups of interventions considering their performance on both outcomes simultaneously. Interventions belonging to the same group are assumed having a similar performance when the two primary outcomes are considered jointly
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
PASI: Psoriasis Area and Severity Index; SAE: serious adverse events; SUCRA: surface under the cumulative ranking curve
Figure 14 and Figure 15 show the ranking for all the outcomes at class and drug level, respectively.
14.

Ranking for all the outcomes at class level
AIL12/23: anti‐IL12/23; AIL17: anti‐IL17; AIL23: anti‐IL23, ATA: anti‐TNF alpha; CSA: non‐biological conventional systemic agents; PBO: placebo; SM: small molecules
AE: adverse events; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; QoL: quality of life; SAE: serious adverse events; SAE without worsening of psoriasis correspond to SAE after exclusion of flares of psoriasis
15.

Ranking for all the outcomes at drug level
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
AE: adverse events; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; QoL: quality of life; SAE: serious adverse events
Since this review does not include ‘Summary of findings' (SoF) tables, we present Figure 7 instead. Figure 7 includes all comparison results for the two main outcomes, but also absolute effects and assessment of the certainty of evidence using CiNeMa.
1. Primary outcomes
1.1 The proportion of participants who achieved clear or almost clear skin, e.g. PASI 90
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at class and drug level in Analysis 1.1; Analysis 1.2; Analysis 1.3; Analysis 1.4; Analysis 1.5; Analysis 1.6; Analysis 1.7; Analysis 1.8; Analysis 1.9; and Analysis 1.10, respectively.
1.1. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 1: Non‐biological treatments versus placebo
1.2. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 2: Non‐biological treatment 1 versus non‐biological treatment 2
1.3. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 3: Anti‐TNF alpha versus placebo
1.4. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 4: Anti‐IL12/23 versus placebo
1.5. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 5: Anti‐IL17 versus placebo
1.6. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 6: Anti‐IL23 versus placebo
1.7. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 7: Biologic versus non‐biological treatment
1.8. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 8: Biologic 1 versus biologic 2
1.9. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 9: Small molecules versus placebo
1.10. Analysis.

Comparison 1: Primary outcome ‐ PASI 90, Outcome 10: Biologic versus small molecules
In terms of reaching PASI 90, anti‐IL17 treatments (secukinumab, ixekizumab, brodalumab, and bimekizumab) were more effective than placebo (risk ratio at class level (RR) 30.68, 95% confidence interval (CI) 22.96 to 41.00). These findings were also confirmed for anti‐IL23 (guselkumab, tildrakizumab, risankizumab, and mirikizumab) (class‐level RR 20.23, 95% CI 14.76 to 27.73); anti‐IL12/23 (ustekinumab) (RR 19.77, 95% CI 13.25 to 29.52); anti‐TNF alpha (infliximab, etanercept, adalimumab, and certolizumab) (class‐level RR 13.65, 95% CI 10.71 to 17.40); and small molecules (apremilast, tofacitinib, and oral tyrosine kinase 2 (TYK2) inhibitor) (class‐level RR 7.09, 95% CI 5.05 to 9.95). Both infliximab and adalimumab were more effective than methotrexate (respectively: RR 2.86, 95% CI 2.15 to 3.80; and RR 3.73, 95% CI 2.25 to 6.19), and secukinumab was more effective than FAEs (RR 8.31, 95% CI 4.23 to 16.35). Ustekinumab, secukinumab, ixekizumab, tildrakizumab and certolizumab were more effective than etanercept. Secukinumab, ixekizumab, brodalumab, and risankizumab were more effective than ustekinumab. Guselkumab and risankizumab were more effective than adalimumab. Secukinumab and ixekizumab were more effective than guselkumab. No significant difference was observed between rizankizumab and secukinumab, or between etanercept and tofacitinib, or between etanercept and apremilast for this outcome (reaching PASI 90).
NETWORK META‐ANALYSES
The PASI 90 outcome was available in 109 trials, involving 47,230 participants (94.3% of the participants in the meta‐analysis). For two trials (Nugteren‐Huying 1990; Sandhu 2003) the number of randomised participants was not available, but we added these trials in the complete‐case sensitivity analyses. This outcome was reported in eight trials out of 99 (Asahina 2016; Bissonnette 2015; Dogra 2012; Dogra 2013; Khatri 2016; SCULPTURE 2015; SIGNATURE 2019; PRISTINE 2013), comparing different dosages of the same drug in each case. We added these trials to the sensitivity analysis at dose level. This outcome was reported in 10 trials out of 109 with biological‐naïve participants and were added to the sensitivity analysis for all trials, whatever previous treatments received by the participants (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020).
Sixty‐six trials, involving 23,721 participants, were placebo‐controlled trials; 23 studies, involving 7133 participants, were head‐to‐head comparisons; and 20 studies, involving 16,376 participants, had both a placebo and at least two active treatments arms.
PASI 90 was not reported for the remaining 21 trials including IXORA‐P 2018 (only long‐term assessment outcomes), and we were not able to obtain missing information from the trial authors (Table 2).
See Figure 4; Figure 5; Figure 6; Figure 7; Figure 10; Figure 11; Figure 14; Figure 15.
Table 3 summarises the main results of both the direct and indirect evidence and the network meta‐analysis for PASI 90. The summary relative effects from the network meta‐analysis are presented in league tables for both class‐level (Figure 6) and drug‐level (Figure 7) analyses.
3. Direct and indirect evidences and network meta‐analysis results summary table for PASI 90.
| Network meta‐analysis | Direct evidence | Indirect evidence | |||||||
| Comparisons* | RR | LCI | UCI | RR | LCI | UCI | RR | LCI | UCI |
| Adalimumab versus placebo | 17.81 | 14.82 | 21.40 | 15.16 | 11.50 | 19.96 | 20.43 | 15.85 | 26.32 |
| Apremilast versus placebo | 7.73 | 4.51 | 13.24 | 6.95 | 3.38 | 14.33 | 10.25 | 2.53 | 41.52 |
| Bimekizumab versus placebo | 58.64 | 3.72 | 923.86 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Brodalumab versus placebo | 23.55 | 19.48 | 28.48 | 26.32 | 16.77 | 41.33 | 20.11 | 10.91 | 37.07 |
| Certolizumab versus placebo | 13.42 | 9.76 | 18.44 | 19.77 | 8.29 | 47.12 | 8.10 | 2.70 | 24.32 |
| Ciclosporin versus placebo | 7.04 | 1.32 | 37.50 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Etanercept versus placebo | 10.76 | 9.03 | 12.82 | 11.52 | 8.82 | 15.03 | 9.98 | 7.53 | 13.24 |
| FAEs versus placebo | 4.36 | 2.01 | 9.46 | 4.47 | 2.01 | 9.95 | 2.93 | 0.13 | 67.39 |
| Guselkumab versus placebo | 25.52 | 21.25 | 30.64 | 28.92 | 20.59 | 40.62 | 24.12 | 19.29 | 30.16 |
| Infliximab versus placebo | 50.29 | 20.96 | 120.67 | 42.64 | 16.08 | 113.09 | 99.51 | 13.69 | 723.56 |
| Ixekizumab versus placebo | 32.48 | 27.13 | 38.87 | 30.54 | 21.37 | 43.65 | 33.20 | 26.88 | 41.01 |
| Mirikizumab versus placebo | 10.96 | 5.46 | 22.00 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Methotrexate versus placebo | 6.97 | 1.42 | 34.34 | 5.85 | 0.73 | 46.93 | 8.94 | 0.75 | 106.67 |
| Risankizumab versus placebo | 28.76 | 23.96 | 34.54 | 31.96 | 22.80 | 44.79 | 27.97 | 22.95 | 34.09 |
| Secukinumab versus placebo | 25.79 | 21.61 | 30.78 | 27.55 | 19.28 | 39.36 | 25.33 | 20.83 | 30.82 |
| Tildrakizumab versus placebo | 18.73 | 14.21 | 24.69 | 17.25 | 8.26 | 36.02 | 20.88 | 8.17 | 53.40 |
| Tofacitinib versus placebo | 8.89 | 7.09 | 11.13 | 6.94 | 4.69 | 10.27 | 14.50 | 7.39 | 28.42 |
| Tyrosine kinase 2 inhibitor versus placebo | 13.99 | 1.99 | 98.10 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Ustekinumab versus placebo | 18.46 | 15.51 | 21.98 | 17.90 | 13.65 | 23.48 | 18.73 | 15.36 | 22.83 |
| Guselkumab versus adalimumab | 1.43 | 1.32 | 1.56 | 1.45 | 1.32 | 1.59 | 1.32 | 1.04 | 1.66 |
| Risankizumab versus adalimumab | 1.62 | 1.44 | 1.81 | 1.53 | 1.33 | 1.75 | 1.83 | 1.49 | 2.25 |
| Etanercept versus apremilast | 1.39 | 0.82 | 2.38 | 1.39 | 0.71 | 2.71 | 1.40 | 0.59 | 3.31 |
| Ustekinumab versus brodalumab | 0.78 | 0.72 | 0.86 | 0.79 | 0.72 | 0.86 | 0.56 | 0.26 | .22 |
| Etanercept versus certolizumab | 0.80 | 0.61 | 1.06 | 0.83 | 0.62 | 1.11 | 0.55 | 0.22 | 1.38 |
| Methotrexate versus ciclosporin | 0.99 | 0.60 | 1.64 | 0.99 | 0.60 | 1.64 | 46.01 | 0.00 | ‐ . |
| Infliximab versus etanercept | 4.67 | 1.93 | 11.34 | 9.20 | 1.28 | 66.37 | 3.94 | 1.46 | 10.62 |
| Ixekizumab versus etanercept | 3.02 | 2.69 | 3.38 | 2.91 | 2.53 | 3.34 | 3.26 | 2.68 | 3.98 |
| Secukinumab versus etanercept | 2.40 | 2.12 | 2.72 | 2.33 | 1.86 | 2.93 | 2.43 | 2.09 | 2.82 |
| Tildrakizumab versus etanercept | 1.74 | 1.39 | 2.18 | 1.77 | 1.40 | 2.24 | 1.43 | 0.61 | 3.35 |
| Tofacitinib versus etanercept | 0.83 | 0.69 | 0.99 | 0.88 | 0.73 | 1.08 | 0.58 | 0.37 | 0.91 |
| Ustekinumab versus etanercept | 1.72 | 1.52 | 1.94 | 1.80 | 1.45 | 2.24 | 1.68 | 1.45 | 1.94 |
| Ixekizumab versus guselkumab | 1.27 | 1.17 | 1.39 | 1.29 | 1.18 | 1.42 | 1.16 | 0.93 | 1.45 |
| Methotrexate versus FAEs | 1.60 | 0.32 | 8.06 | 2.00 | 0.19 | 20.90 | 1.31 | 0.14 | 12.18 |
| Secukinumab versus risankizumab | 0.90 | 0.81 | 0.99 | 0.89 | 0.77 | 1.03 | 0.90 | 0.79 | 1.04 |
| Ustekinumab versus ixekizumab | 0.57 | 0.50 | 0.64 | 0.58 | 0.47 | 0.71 | 0.56 | 0.49 | 0.65 |
| Ustekinumab versus risankizumab | 0.64 | 0.58 | 0.71 | 0.60 | 0.52 | 0.70 | 0.67 | 0.59 | 0.77 |
| Ustekinumab versus secukinumab | 0.72 | 0.67 | 0.76 | 0.72 | 0.67 | 0.77 | 0.72 | 0.61 | 0.84 |
FAES: fumaric acid esters; LCI: low confidence interval; RR: risk ratio; UCI: upper confidence interval; vs: versus,
*The comparisons listed in this table were included in at least one direct‐evidence analysis.
All of the interventions appeared superior to placebo in terms of reaching PASI 90. At class level (Figure 6), anti‐IL17 treatment was associated with a better chance of reaching PASI 90 compared to all of the interventions: versus anti‐IL23 (RR 1.26, 95% CI 1.04 to 1.53): versus anti‐IL12/23 (RR 1.53, 95% CI 1.28 to 1.82); versus anti‐TNF alpha (RR 2.21, 95% CI 1.83 to 2.67); versus small molecules (RR 3.31, 95% CI 2.34 to 4.69); versus non‐biological systemic agents (RR 6.49, 95% CI 2.72 to 15.50). In terms of reaching PASI 90, all of the biologic interventions (anti‐IL17, anti‐IL12/23, anti‐IL23, anti‐TNF alpha) appeared significantly superior to the small molecule class of treatments and the non‐biological systemic class of treatments.
Results of comparisons between each of the drugs are available in Figure 7. There was no significant difference between infliximab, ixekizumab, bimekizumab, and risankizumab in terms of reaching PASI 90. Anti‐IL17 drugs (ixekizumab, secukinumab and brodalumab) and anti‐IL23 drugs (risankizumab and guselkumab) except tildrakizumab were significantly more likely to reach PASI 90 than ustekinumab and three anti‐TNF alpha agents: adalimumab, certolizumab and etanercept. Ustekinumab was superior to certolizumab (RR 1.38, 95% CI 1.02 to 1.86). Adalimumab and ustekinumab were superior to etanercept (RR 1.66, 95% CI 1.44 to 1.91 and RR 1.72, 95% CI 1.52 to 1.94, respectively). No significant difference was shown between tofacitinib or apremilast and two non‐biological drugs: ciclosporin and methotrexate. We assessed the certainty of evidence for each comparison using CINeMA and classified as high (highlighted in green), moderate (in blue), low (in yellow) and very low (in red) (Figure 7).
Ranking class‐level analysis (Figure 10; Figure 14; Table 4)
4. Ranking findings for all outcomes at class level.
| Class‐level interventions | SUCRA PASI 90 | Rank PASI 90 | SUCRA SAE | Rank SAE |
SUCRA SAE excluded flare of psoriasis |
Rank SAE excluded flare of psoriasis |
SUCRA PASI 75 | Rank PASI 75 | SUCRA AE | Rank AE | SUCRA PGA | Rank PGA | SUCRA QoL | Rank QoL |
| Anti‐IL17 | 99.9 | 1 | 22.6 | 7 | 24.7 | 7 | 99.5 | 1 | 24.7 | 6 | 99.9 | 1 | 73.4 | 3 |
| Anti‐IL23 | 82.9 | 2 | 77.7 | 1 | 77.2 | 1 | 81.1 | 2 | 88.3 | 2 | 81.8 | 2 | 85.5 | 1 |
| Anti‐IL12/23 | 67.2 | 3 | 43.9 | 5 | 29.2 | 6 | 69.4 | 3 | 57.5 | 3 | 68.3 | 3 | 75.8 | 2 |
| Anti‐TNF alpha | 49.8 | 4 | 51.5 | 3 | 37.4 | 5 | 50 | 4 | 52.6 | 4 | 50 | 4 | 44.5 | 5 |
| Small molecules | 32.3 | 5 | 50.4 | 4 | 72.5 | 2 | 33.3 | 5 | 5.7 | 7 | 30.5 | 5 | 20.4 | 6 |
|
Non‐biological treatments |
18 | 6 | 74.2 | 2 | 52.6 | 4 | 16.7 | 6 | 28.8 | 5 | 19.5 | 6 | 50.2 | 4 |
| Placebo | 0 | 7 | 29.7 | 6 | 56.3 | 3 | 0 | 7 | 92.4 | 1 | 0 | 7 | 0.1 | 7 |
AE: adverse events; FAEs: fumaric acid esters; PGA: Physician Global Assessment; QoL: Specific quality of life scale; SAE: serious adverse events
Anti‐IL17 class had a better chance of reaching PASI 90 using SUCRA (versus placebo: RR 30.30, 95% CI 24.43 to 37.57; SUCRA = 99.9), followed by anti‐IL23 (versus placebo: RR 23.96, 95% CI 19.35 to 29.68; SUCRA = 82.9), anti‐IL12/23 (versus placebo: RR 19.82, 95% CI 15.77 to 24.92; SUCRA = 67.2), then anti‐TNF alpha (versus placebo: RR 13.69, 95% CI 11.24 to 16.68; SUCRA = 49.8). The heterogeneity τ for this network overall was 0.05, which we considered to be low.
Ranking drug‐level analysis (Figure 11; Figure 15; Table 5)
5. Ranking findings for all outcomes at drug level.
| Drug | SUCRA PASI 90 | Rank PASI 90 | SUCRA SAE | Rank SAE |
SUCRA SAE excluded flare of psoriasis |
Rank SAE excluded flare of psoriasis |
SUCRA PASI 75 | Rank PASI 75 | SUCRA AE | Rank AE | SUCRA PGA | Rank PGA | SUCRA QoL | Rank QoL |
| Infliximab | 93.6 | 1 | 29.3 | 20 | 56.6 | 7 | 94.8 | 1 | 33.7 | 15 | 83.6 | 2 | 65.7 | 6 |
| Ixekizumab | 90.5 | 2 | 29.8 | 19 | 39.3 | 17 | 90.3 | 2 | 34.4 | 13 | 87.9 | 1 | 91.7 | 2 |
| Risankizumab | 84.6 | 3 | 68.1 | 3 | 75 | 2 | 84.2 | 3 | 71.9 | 6 | 81 | 4 | 95.3 | 1 |
| Bimekizumab | 81.4 | 4 | 83 | 2 | 83.3 | 1 | 79.8 | 4 | 4.7 | 20 | 74.2 | 6 | ‐ | ‐ |
| Secukinumab | 76.2 | 5 | 34.8 | 17 | 34.3 | 18 | 77.2 | 5 | 35.9 | 12 | 81 | 3 | 69.9 | 4 |
| Guselkumab | 75 | 6 | 44.4 | 12 | 39.5 | 16 | 73.1 | 6 | 75.3 | 5 | 61.4 | 8 | 59.2 | 7 |
| Brodalumab | 68.4 | 7 | 34.3 | 18 | 42.7 | 14 | 72.5 | 7 | 44.7 | 11 | 78.8 | 5 | 12.7 | 13 |
| Tildrakizumab | 56.5 | 8 | 52.7 | 9 | 22.4 | 19 | 58.7 | 9 | 95.2 | 1 | 46.5 | 12 | 69.5 | 5 |
| Ustekinumab | 56.1 | 9 | 46.5 | 11 | 43.7 | 13 | 60.8 | 8 | 60.6 | 8 | 57.8 | 9 | 73.5 | 3 |
| Adalimumab | 52.9 | 10 | 36.9 | 15 | 41.7 | 15 | 52.2 | 11 | 68.8 | 7 | 43.6 | 13 | 36.3 | 12 |
| Tyrosine kinase 2 inhibitor | 48.2 | 11 | 59.7 | 5 | 63.6 | 4 | 45.7 | 13 | 21.3 | 18 | 46.7 | 11 | ‐ | ‐ |
| Certolizumab | 41.4 | 12 | 58.8 | 6 | 16.2 | 20 | 49.6 | 2 | 78.2 | 3 | 52.4 | 10 | 37.5 | 11 |
| Mirikizumab | 34.1 | 3 | 62.5 | 4 | 67.1 | 3 | 55.7 | 10 | 78.2 | 4 | 67.7 | 7 | ‐ | ‐ |
| Etanercept | 33.1 | 4 | 53.7 | 8 | 48.3 | 12 | 38.9 | 14 | 53.1 | 10 | 32.3 | 15 | 42.3 | 9 |
| Ciclosporin | 26.5 | 15 | 35.4 | 16 | 51.5 | 9 | 24.2 | 16 | 22.7 | 17 | 30.1 | 16 | ‐ | ‐ |
| Methotrexate | 25.6 | 16 | 83.8 | 1 | 51.4 | 10 | 15.3 | 18 | 60.5 | 9 | 33.7 | 14 | 44.1 | 8 |
| Tofacitinib | 24.2 | 17 | 42.4 | 13 | 57.8 | 6 | 31.1 | 15 | 34 | 14 | 20.6 | 17 | 42.1 | 10 |
| Apremilast | 21.1 | 18 | 51.3 | 10 | 62 | 5 | 22 | 17 | 15.7 | 19 | 13 | 18 | 10.1 | 14 |
| FAEs | 10.4 | 19 | 55.4 | 7 | 50.9 | 11 | 9.6 | 20 | 25.6 | 16 | 7.8 | 19 | ‐ | ‐ |
| Placebo | 0.1 | 20 | 37.1 | 14 | 52.5 | 8 | 1.4 | 21 | 85.4 | 2 | 0 | 20 | 0.2 | 15 |
| Acitretine | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ | 12.8 | 19 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
AE: adverse events; FAEs: fumaric acid esters; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; QoL: specific quality of life scale; SAE: serious adverse events; SUCRA: Surface Under the Cumulative Ranking
At drug‐level, using SUCRA, infliximab had a better chance of reaching PASI 90 at drug level (versus placebo: RR 50.29, 95% CI 20.96 to 120.67; SUCRA = 93.6; high‐certainty evidence), followed by ixekizumab (versus placebo: RR 32.48, 95% CI 27.13 to 38.87; SUCRA = 90.5; high‐certainty evidence), risankizumab (versus placebo: RR 28.76, 95% CI 23.96 to 34.54; SUCRA = 84.6; high‐certainty evidence), bimekizumab (versus placebo: RR 58.64, 95% CI 3.72 to 923.86; SUCRA = 81.4; high‐certainty evidence), secukinumab (versus placebo: RR 25.79, 95% CI 21.61 to 30.78; SUCRA = 76.2; high‐certainty evidence), guselkumab (versus placebo: RR 25.52, 95% CI 21.25 to 30.64; SUCRA = 75; high‐certainty evidence), then brodalumab (versus placebo: RR 23.55, 95% CI 19.48 to 28.48; SUCRA = 68.4; moderate‐certainty evidence). The heterogeneity τ for this network overall was 0, which we considered to be low.
1.2 The proportion of participants with serious adverse events
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at class and drug level in Analysis 2.1; Analysis 2.2; Analysis 2.3; Analysis 2.4; Analysis 2.5; Analysis 2.6; Analysis 2.7; Analysis 2.8; Analysis 2.9; and Analysis 2.10, respectively.
2.1. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 1: Non‐biological treatments versus placebo
2.2. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 2: Non‐biological treatment 1 versus non‐biological treatment 2
2.3. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 3: Anti‐TNF alpha versus placebo
2.4. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 4: Anti‐IL12/23 versus placebo
2.5. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 5: Anti‐IL17 versus placebo
2.6. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 6: Anti‐IL23 versus placebo
2.7. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 7: Biologic versus non‐biological treatments
2.8. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 8: Biologic 1 versus biologic 2
2.9. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 9: Small molecules versus placebo
2.10. Analysis.

Comparison 2: Primary outcome ‐ serious adverse events (SAE), Outcome 10: Biologic versus small molecules
We found no significant differences between FAEs, etanercept, adalimumab, certolizumab, ustekinumab, secukinumab, ixekizumab, brodalumab, bimekizumab, guselkumab, tildrakizumab, risankizumab, mirikizumab, apremilast, tofacitinib, oral tyrosine kinase 2 (TYK2) inhibitor, and placebo in the number of participants with serious adverse events (SAEs). The risk of SAEs was significantly lower for participants on methotrexate compared to placebo (RR 0.16, 95% CI 0.03 to 0.88). The risk of SAEs was significantly higher for participants on infliximab compared to methotrexate (RR 2.41, 95% CI 1.04 to 5.59).
There were zero SAEs in the following trials: Fallah Arani 2011 (comparing methotrexate with FAEs); Flytström 2008 (comparing ciclosporin with methotrexate); Heydendael 2003 (comparing ciclosporin with methotrexate); Gisondi 2008; (comparing etanercept with acitretin); Bagel 2012 (comparing etanercept with placebo); Caproni 2009 (comparing etanercept with acitretin); Chaudhari 2001 (comparing inflixizimab with placebo); Jin 2017 (comparing tofacitinib with placebo); Yu 2019 (comparing etanercept with methotrexate); and Hunter 1963 (comparing methotrexate with placebo).
NETWORK META‐ANALYSES
The SAE outcome was available in 114 trials, involving 47,754 participants (95.4% of the participants in the meta‐analysis). For one trial (PRESTA 2010); the number of randomised participants was not available. We added this trial to the complete‐cases sensitivity analyses. This outcome was reported in eight trials out of 114 (Asahina 2016; Bissonnette 2015; Khatri 2016; Laburte 1994; SCULPTURE 2015; Ortonne 2013; PRISTINE 2013; PRESTA 2010), comparing different dosages of the same drug in each case. We added these studies to the sensitivity analysis at dose level. This outcome was reported in 10 trials out of 114 with biological‐naïve participants and were added to the sensitivity analysis for all trials, whatever previous treatments received by the participants (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020). Sixty‐nine trials, involving 23,337 participants, were placebo‐controlled trials; 23, involving 7885 participants, were head‐to‐head comparisons, and 22, involving 16,532 participants, had both a placebo and at least two active treatments arms.
SAEs were not reported for the 16 remaining trials, and we were not able to obtain missing information from the trial authors (Table 2).
See Figure 4; Figure 5; Figure 6; Figure 7; Figure 10; Figure 11; Figure 14; Figure 15.
Table 6 summarises the main results of both direct and indirect evidence and the network meta‐analysis for SAEs. We present the summary relative effects from the network meta‐analysis in league tables for both class‐level (Figure 6) and drug‐level (Figure 7) analyses. We found no significant difference between any of the interventions and the placebo for the risk of SAE. This result was verified after excluding flares of psoriasis as SAEs (Figure 6). We assessed the certainty of evidence for each comparison using CINeMA and classified as high (highlighted in green), moderate (in blue), low (in yellow) and very‐low (in red) (Figure 7).
6. Direct and indirect evidence and network meta‐analysis results summary table for serious adverse events.
| Network meta‐analysis | Direct evidence | Indirect evidence | |||||||
| Comparisons* | RR | LCI | UCI | RR | LCI | UCI | RR | LCI | UCI |
| Adalimumab versus placebo | 1.01 | 0.66 | 1.56 | 1.19 | 0.74 | 1.92 | 0.57 | 0.23 | 1.42 |
| Apremilast versus placebo | 0.86 | 0.49 | 1.52 | 0.86 | 0.47 | 1.56 | 1.00 | 0.04 | 26.68 |
| Bimekizumab versus placebo | 0.20 | 0.01 | 3.20 | ‐ | ‐ | ‐ | ‐ | ‐ | ‐ |
| Brodalumab versus placebo | 1.05 | 0.62 | 1.79 | 0.93 | 0.52 | 1.67 | 2.66 | 0.39 | 18.12 |
| Certolizumab versus placebo | 0.75 | 0.30 | 1.84 | 0.62 | 0.25 | 1.54 | 33.70 | 0.52 | 2180.73 |
| Ciclosporin versus placebo | 1.28 | 0.15 | 11.01 | 5.69 | 0.32 | 101.52 | 0.19 | 0.01 | 4.90 |
| Etanercept versus placebo | 0.85 | 0.58 | 1.26 | 0.72 | 0.45 | 1.14 | 1.36 | 0.63 | 2.93 |
| Fumaric ester acids versus placebo | 0.78 | 0.29 | 2.09 | 0.83 | 0.30 | 2.28 | 0.28 | 0.00 | 19.72 |
| Guselkumab versus placebo | 0.94 | 0.55 | 1.59 | 1.04 | 0.48 | 2.23 | 0.84 | 0.37 | 1.92 |
| Infliximab versus placebo | 1.16 | 0.56 | 2.39 | 1.20 | 0.56 | 2.54 | 0.78 | 0.05 | 12.25 |
| Ixekizumab versus placebo | 1.10 | 0.69 | 1.74 | 1.08 | 0.58 | 2.01 | 1.13 | 0.49 | 2.62 |
| Mirikizumab versus placebo | 0.65 | 0.17 | 2.51 | ‐ | ‐ | ‐ | ‐ | ‐ | |
| Methotrexate versus placebo | 0.33 | 0.07 | 1.59 | 0.14 | 0.02 | 0.94 | 2.22 | 0.13 | 37.63 |
| Risankizumab versus placebo | 0.71 | 0.45 | 1.13 | 0.45 | 0.23 | 0.89 | 1.04 | 0.56 | 1.95 |
| Secukinumab versus placebo | 1.03 | 0.70 | 1.52 | 1.10 | 0.67 | 1.81 | 0.93 | 0.49 | 1.77 |
| Tildrakizumab versus placebo | 0.83 | 0.37 | 1.86 | 0.99 | 0.37 | 2.60 | 0.46 | 0.06 | 3.68 |
| Tofacitinib versus placebo | 0.96 | 0.54 | 1.71 | 1.07 | 0.55 | 2.09 | 0.48 | 0.06 | |
| Ustekinumab versus placebo | 0.92 | 0.64 | 1.33 | 0.98 | 0.60 | 1.59 | 0.84 | 0.47 | |
| Guselkumab versus adalimumab | 0.93 | 0.53 | 1.63 | 0.91 | 0.44 | 1.89 | 0.95 | 0.37 | 2.43 |
| Risankizumab versus adalimumab | 0.70 | 0.40 | 1.22 | 1.12 | 0.46 | 2.75 | 0.54 | 0.27 | 1.06 |
| Etanercept versus apremilast | 0.99 | 0.51 | 1.92 | 0.68 | 0.14 | 3.40 | 1.07 | 0.52 | 2.22 |
| Ustekinumab versus brodalumab | 0.87 | 0.49 | 1.57 | 0.75 | 0.32 | 1.75 | 1.07 | 0.39 | 2.88 |
| Etanercept versus certolizumab | 1.14 | 0.43 | 3.02 | 2.28 | 0.33 | 15.76 | 0.81 | 0.23 | 2.90 |
| Methotrexate versus Ciclosporin | 0.26 | 0.03 | 2.18 | 1.02 | 0.06 | 16.18 | 0.03 | 0.00 | 0.98 |
| Infliximab versus Etanercept | 1.36 | 0.60 | 3.05 | 0.92 | 0.06 | 14.05 | 1.41 | 0.60 | 3.31 |
| Ixekizumab versus Etanercept | 1.28 | 0.77 | 2.13 | 1.03 | 0.53 | 2.03 | 1.72 | 0.78 | 3.79 |
| Secukinumab versus Etanercept | 1.21 | 0.72 | 2.03 | 1.60 | 0.47 | 5.47 | 1.13 | 0.63 | 2.03 |
| Tildrakizumab versus Etanercept | 0.97 | 0.43 | 2.18 | 0.70 | 0.26 | 1.89 | 1.94 | 0.45 | 8.28 |
| Todacitinib versus Etanercept | 1.12 | 0.60 | 2.10 | 0.87 | 0.33 | 2.30 | 1.37 | 0.59 | 3.18 |
| Ustekinumab versus Etanercept | 1.08 | 0.65 | 1.78 | 1.25 | 0.37 | 4.25 | 1.05 | 0.60 | 1.82 |
| Methotrexate versus Fumaric ester acids | 0.42 | 0.07 | 2.48 | 1.00 | 0.02 | 49.21 | 0.34 | 0.05 | 2.46 |
| Ixekizumab versus guselkumab | 1.17 | 0.67 | 2.04 | 1.20 | 0.54 | 2.64 | 1.13 | 0.49 | 2.62 |
| Ustekinumab versus Ixekizumab | 0.84 | 0.47 | 1.49 | 0.16 | 0.01 | 3.42 | 0.89 | 0.50 | 1.60 |
| Secukinumab versus Risankizumab | 1.45 | 0.86 | 2.45 | 0.67 | 0.24 | 1.84 | 1.89 | 1.05 | 3.41 |
| Ustekinumab versus Risankizumab | 1.29 | 0.80 | 2.10 | 1.82 | 0.92 | 3.60 | 0.93 | 0.47 | 1.82 |
| Ustekinumab versus secukinumab | 0.89 | 0.58 | 1.37 | 0.79 | 0.42 | 1.49 | 0.99 | 0.55 | 1.79 |
FAES: fumaric acid esters; LCI: low confidence interval; RR: risk ratio; UCI: upper confidence interval
*The comparisons listed in this table were included in at least one direct‐evidence analysis.
Ranking class‐level analysis (Figure 10; Figure 14; Table 4)
Anti‐IL23 had the highest SUCRA at class level in terms of serious adverse events (versus placebo: RR 0.78, 95% CI 0.58 to 1.06; SUCRA = 77.7), followed by non‐biological systemic treatments (versus placebo: RR 0.69, 95% CI 0.30 to 1.58; SUCRA = 74.2), anti‐TNF (versus placebo: RR 0.91, 95% CI 0.71 to 1.17; SUCRA = 51.5), and then small molecules (versus placebo: RR 0.91, 95% CI 0.62 to 1.34; SUCRA = 50.4). The heterogeneity τ for this network overall was 0, which we considered to be low.
Ranking drug‐level analysis (Figure 11; Figure 15; Table 5)
Methotrexate had the highest SUCRA at drug level in terms of serious adverse events (versus placebo: RR 0.33, 95% CI 0.07 to 1.59; SUCRA = 83.8; low‐certainty evidence), followed by bimekizumab (versus placebo: RR 0.20, 95% CI 0.01 to 3.20; SUCRA = 83; moderate‐certainty evidence), risankizumab (versus placebo: RR 0.71, 95% CI 0.45 to 1.13; SUCRA = 68.1; moderate‐certainty evidence), mirikizumab (versus placebo: RR 0.65, 95% CI 0.17 to 2.51; SUCRA = 62.5; moderate‐certainty evidence), and oral tyrosine kinase 2 inhibitor (versus placebo: RR 0.61, 95% CI 0.06 to 5.79; SUCRA = 59.7; moderate‐certainty evidence). However, no significant difference was observed between drugs and placebo. The heterogeneity τ for this network overall was 0.02, which we considered to be low. After excluding worsening of psoriasis as a SAE, ranking analysis was quite similar except for methotrexate which dropped from the 1st to the 10th rank. At the opposite end, placebo rose from the 14th to the 8th rank.
1.3 Relationship between PASI 90 and serious adverse events
See Figure 13.
These findings for both efficacy (PASI 90) and acceptability (serious adverse events) were combined together in a bivariate ranking plot, where serious adverse events were transformed into acceptability by using the inverse values of the corresponding RRs so that higher values indicate higher acceptability (due to lower SAEs): accordingly, the ideal treatment (highest performance = best efficacy + best acceptability) should appear in the upper right corner of the plot.
At class level, the highly‐effective treatment (anti‐IL17) had serious adverse events. However, the anti‐IL23 treatment group was the class with the better compromise between efficacy and acceptability.
At drug level, risankizumab and bimekizumab might be the overall best treatments, considering both outcomes jointly. This result has to be considered with caution for bimekizumab, as only one trial was available for this drug.
2. Secondary outcomes
2.1 Proportion of participants who achieve PASI 75
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at class and drug level in Analysis 3.1; Analysis 3.2; Analysis 3.3; Analysis 3.4; Analysis 3.5; Analysis 3.6; Analysis 3.7; Analysis 3.8; Analysis 3.9; and Analysis 3.10, respectively.
3.1. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 1: Non‐biological treatments versus placebo
3.2. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 2: Non‐biological treatment 1 versus non‐biological treatment 2
3.3. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 3: Anti‐TNF alpha versus placebo
3.4. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 4: Anti‐IL12/23 versus placebo
3.5. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 5: Anti‐IL17 versus placebo
3.6. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 6: Anti‐IL23 versus placebo
3.7. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 7: Biologic versus non‐biological treatments
3.8. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 8: Biologic 1 versus biologic 2
3.9. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 9: Small molecules versus placebo
3.10. Analysis.

Comparison 3: Secondary outcome ‐ PASI 75, Outcome 10: Biologic versus small molecules
NETWORK META‐ANALYSES
PASI 75 outcome was available in 119 trials, involving 48,224 participants (96.3% of the participants in this review). For one trial (PRESTA 2010), the number of randomised participants was not available. We added these trials to the complete‐case analyses. This outcome was reported in 12 trials out of 119 (Asahina 2016; Bissonnette 2015; Dogra 2012; Dogra 2013; Dubertret 1989; Khatri 2016; Laburte 1994; SCULPTURE 2015; SIGNATURE 2019; Ortonne 2013; PRISTINE 2013; PRESTA 2010), comparing different dosages of the same drug in each case. We added these trials to the sensitivity analysis at dose level. This outcome was reported in 10 trials out of 119 with biological‐naïve participants and were added to the sensitivity analysis for all trials, whatever the previous treatments received by the participants (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020). Seventy‐two trials, involving 24,502 participants, were placebo‐controlled trials; 25 trials, involving 7190 participants, were head‐to‐head comparisons; and 22 trials, involving 16,532 participants, had both a placebo and at least two active treatments arms. PASI 75 was not reported for the 11 remaining trials, and we were not able to obtain missing information from the trial authors (Table 2).
See Figure 4; Figure 5; Figure 6; Figure 8; Figure 10; Figure 12; Figure 14; Figure 15
We present the summary relative effects from the network meta‐analysis in league tables for both class‐level (Figure 6) and drug‐level (Figure 8) analyses. All of the interventions appeared superior to placebo in terms of reaching PASI 75. At class level, the anti‐IL17 class of drugs was associated with a higher chance of reaching PASI 75 compared to the other classes, except for anti‐IL23 (Figure 6). All of the interventions (anti‐IL17, anti‐IL23, anti‐IL12/23, anti‐TNF alpha) appeared significantly superior to the small molecule class and the non‐biological systemic class, and the small molecules appeared significantly superior to the non‐biological systemic agents. Results of comparisons between each of the drugs are available in Figure 8.
Ranking class‐level analysis(Figure 10; Figure 14; Table 4)
Ranking analysis performed with SUCRA strongly suggested that anti‐IL17 had a better chance of reaching PASI 75 at class level (versus placebo: RR 14.11, 95% CI 12.31 to 16.17; SUCRA = 99.9), followed by anti‐IL23 (versus placebo: RR 12.33, 95% CI 10.78 to 14.11; SUCRA = 82.9), anti‐IL12/23 (versus placebo: RR 11.52, 95% CI 10.03 to 13.24; SUCRA = 67.2), then anti‐TNF alpha (versus placebo: RR 9.01 95% CI 8.02 to 10.12; SUCRA = 49.8). The heterogeneity τ for this network overall was 0.03, which we considered to be low.
Ranking drug‐level analysis(Figure 12; Figure 15; Table 5)
Ranking analysis performed with SUCRA strongly suggested that infliximab had the higher chance of reaching PASI 75 at drug level (versus placebo: RR 18.02, 95% CI 11.92 to 27.22; SUCRA = 94.8), followed by ixekizumab (versus placebo: RR 14.54, 95% CI 12.59 to 16.79; SUCRA = 90.3), risankizumab (versus placebo: RR 13.44, 95% CI 11.87 to 15.22; SUCRA = 84.2), bimekizumab (versus placebo: RR 17.06, 95% CI 4.38 to 66.49; SUCRA = 79.8), then secukinumab (versus placebo: RR 12.71, 95% CI 11.12 to 14.52; SUCRA = 77.2). The heterogeneity τ for this network overall was 0, which we considered to be low.
2.2 Proportion of participants who achieve a Physician Global Assessment (PGA) value of 0 or 1
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at class and drug level in Analysis 4.1; Analysis 4.2; Analysis 4.3; Analysis 4.4; Analysis 4.5; Analysis 4.6; Analysis 4.7; Analysis 4.8; Analysis 4.9; and Analysis 4.10, respectively.
4.1. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 1: Non‐biological treatment versus placebo
4.2. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 2: Non‐biological treatment 1 versus non‐biological treatment 2
4.3. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 3: Anti‐TNF alpha versus placebo
4.4. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 4: Anti‐IL12/23 versus placebo
4.5. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 5: Anti‐IL17 versus placebo
4.6. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 6: Anti‐IL23 versus placebo
4.7. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 7: Biologic versus non‐biological treatments
4.8. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 8: Biologic 1 versus biologic 2
4.9. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 9: Small molecules versus placebo
4.10. Analysis.

Comparison 4: Secondary outcome ‐ PGA 0/1, Outcome 10: Biologic versus small molecules
NETWORK META‐ANALYSES
The PGA 0/1 outcome was available in 104 trials, involving 46,091 participants (92.0% of the participants in this review). For three other studies (Nugteren‐Huying 1990; Sandhu 2003; PRESTA 2010), the number of randomised participants was not available. We added these trials to the complete‐case analyses. This outcome was reported in seven trials out of 104 (Asahina 2016; Bissonnette 2015; Khatri 2016; SCULPTURE 2015; Ortonne 2013; PRISTINE 2013; PRESTA 2010), comparing different dosages of the same drug. We added these trials to the sensitivity analysis at dose level. This outcome was reported in 10 trials out of 104 with biological‐naïve participants and were added to the sensitivity analysis for all trials, whatever the previous treatments received by the participants (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020). Sixty‐three trials, involving 22,218 participants, were placebo‐controlled trials; 19 trials, involving 7341 participants, were head‐to‐head comparisons; and 22 trials, involving 16,532 participants, had both a placebo and at least two active treatments arms. PGA 0/1 was not reported for the 26 remaining trials, and we were not able to obtain missing information from the trial authors (Table 2).
See Figure 4; Figure 5; Figure 6; Figure 9; Figure 10; Figure 12; Figure 14; Figure 15.
We present the summary relative effects as estimated from the network meta‐analysis in league tables at class level (Figure 6) and drug level (Figure 9). At class level, all of the interventions appeared superior to placebo in terms of reaching PGA 0/1, and anti‐IL17 monoclonal antibodies were associated with a better chance for this outcome compared to the other drug classes (Figure 6). These differences were statistically significant. All of the interventions (anti‐IL17, anti‐IL23, anti‐IL12/23, anti‐TNF alpha) appeared significantly superior to the small molecule and the non‐biological systemic class of treatments. We found no significant difference between small molecule and non‐biological systemic agents. Results of comparisons between each of the drugs are available in Figure 9.
Ranking class‐level analysis(Figure 10; Figure 14; Table 4)
Ranking analysis performed with SUCRA strongly suggested that anti‐IL17 had a better chance of reaching PGA0/1 at class level (versus placebo: RR 15.33, 95% CI 12.93 to 18.18; SUCRA = 99.9), followed by anti‐IL23 (versus placebo: RR 12.15, 95% CI 10.32 to 14.32; SUCRA = 81.8), anti‐IL12/23 (versus placebo: RR 10.82, 95% CI 9.11 to 12.84; SUCRA = 68.3), then anti‐TNF alpha (versus placebo: RR 8.39, 95% CI 7.42 to 9.72; SUCRA = 50). The heterogeneity τ for this network overall was 0.5, which we considered to be low.
Ranking drug‐level analysis(Figure 12; Figure 15; Table 5)
Ranking analysis performed with SUCRA strongly suggested that ixekizumab had a better chance of reaching PGA0/1 at drug level (versus placebo: RR 15.38, 95% CI 12.60 to 18.77; SUCRA = 87.9), followed by infliximab (versus placebo: RR 15.34, 95% CI 9.22 to 25.54; SUCRA = 83.6), secukinumab (versus placebo: RR 14.17, 95% CI 11.44 to 17.56; SUCRA = 81), risankizumab (versus placebo: RR 14.17, 95% CI 11.71 to 17.13; SUCRA = 81), brodalumab (versus placebo: RR 13.84, 95% CI 10.49 to 18.26; SUCRA =78.8), then bimekizumab (versus placebo: RR 15.35, 95% CI 3.82 to 61.69; SUCRA = 74.2). The heterogeneity τ for this network overall was 0.03, which we considered to be low.
Focusing on efficacy outcomes (PASI 90, PASI 75, and PGA 0/1), the results were similar at class level (Figure 10; Table 4) and at drug level (Figure 11; Figure 12; Table 5).
2.3 Mean difference of quality of life measured by a specific scale
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at class and drug level in Analysis 5.1; Analysis 5.2; Analysis 5.3; Analysis 5.4; Analysis 5.5; Analysis 5.6; Analysis 5.7; Analysis 5.8; Analysis 5.9; and Analysis 5.10, respectively.
5.1. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 1: Non‐biological treatments versus placebo
5.2. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 2: Non‐biological treatment 1 versus non‐biological treatment 2
5.3. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 3: Anti‐TNF alpha versus placebo
5.4. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 4: Ustekinumab versus placebo
5.5. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 5: Anti‐IL17 versus placebo
5.6. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 6: Anti‐IL23 versus placebo
5.7. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 7: Biologic versus non‐biological treatment
5.8. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 8: Biologic 1 versus biologic 2
5.9. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 9: Small molecules versus placebo
5.10. Analysis.

Comparison 5: Secondary outcome ‐ quality of life, Outcome 10: Biologic versus small molecules
NETWORK META‐ANALYSES
The quality‐of‐life outcome was available in 68 trials, involving 30,619 participants (61.1% of the participants in this review). This outcome was also reported in seven trials (out of 68) (Asahina 2016; Bissonnette 2015; Khatri 2016; SCULPTURE 2015; SIGNATURE 2019; Ortonne 2013; PRISTINE 2013), comparing different dosages of the same drug. We added these trials to the sensitivity analyses at dose level. This outcome was reported in 10 trials out of 68 with biological‐naïve participants and were added to the sensitivity analysis for all trials, whatever the previous treatments received by the participants (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020). The quality‐of‐life outcome was not reported for the 62 remaining trials, and we were not able to obtain missing information from the trial authors (Table 2). Forty‐one trials, involving 16,663 participants, were placebo‐controlled trials; 13, involving 3986 participants, were head‐to‐head comparisons; and 14, involving 9970 participants, had both a placebo and at least two active treatments arms.
See Figure 4; Figure 5; Figure 6; Figure 9; Figure 10; Figure 12; Figure 14; Figure 15.
We present the summary relative effects from the network meta‐analysis in league tables for both class‐level (Figure 6) and drug‐level (Figure 9) analyses. All classes of treatments appeared superior to placebo in terms of showing significant improvement on a quality‐of‐life scale. Anti‐IL23, anti‐IL12/23, anti‐IL17 and anti‐TNF agents were associated with a higher chance of improving quality of life compared to small molecules (Figure 6). These differences were statistically significant for all of the classes. No significant difference was shown between the different biological agents except for anti‐IL23 and anti‐TNF alpha (anti‐IL23 was more favourable than anti‐TNF alpha). There were no significant differences between the small molecules and the non‐biological agents. Results of comparisons between each of the drugs are available in Figure 9.
Ranking class‐level analysis(Figure 10; Figure 14Table 4)
Ranking analysis performed with SUCRA strongly suggested that anti‐IL23 had a better chance of improving quality of life at class level (versus placebo: standardised mean difference (SMD) −1.41, 95% confidence interval (CI) −1.64 to −1.17; SUCRA = 85.5), followed by anti‐IL12/23 (versus placebo: SMD −1.33, 95% CI −1.61 to −1.06; SUCRA = 75.8), and anti‐IL17 (versus placebo: SMD −1.31, 95% CI −1.61 to −1.01; SUCRA = 73.4). The heterogeneity τ for this network overall was 0.13, which we considered to be low.
Ranking drug‐level analysis(Figure 12; Figure 15Table 5)
Ranking analysis for quality of life performed with SUCRA strongly suggested that risankizumab was the best treatment at drug level (versus placebo: SMD −1.77, 95% CI −2.14 to −1.40; SUCRA = 95.3), followed by ixekizumab (versus placebo: SMD −1.67, 95% CI −1.97 to −1.38; SUCRA = 91.7), ustekinumab (versus placebo: SMD −1.39, 95% CI −1.61 to −1.17; SUCRA = 73.5), secukinumab (versus placebo: SMD −1.41, 95% CI −2.11 to −0.70; SUCRA = 69.9), then tildrakizumab (versus placebo: SMD −1.35, 95% CI −1.67 to −1.03; SUCRA = 69.5). The heterogeneity τ for this network overall was 0.07, which we considered to be low. Moreover, five interventions (acitretin, ciclosporin, oral tyrosine kinase 2 inhibitor, bimekizumab and mirikizumab) were not included in the ranking at drug level, due to no available data.
In total, information on quality of life was poorly reported and lacking for almost half of the population included in the NMA, so has to be considered with caution.
2.4 The proportions of participants with adverse events
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at class and drug level in Analysis 6.1; Analysis 6.2; Analysis 6.3; Analysis 6.4; Analysis 6.5; Analysis 6.6; Analysis 6.7; Analysis 6.8; Analysis 6.9; and Analysis 6.10 respectively.
6.1. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 1: Non‐biological treatments versus placebo
6.2. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 2: Non‐biological treatment 1 versus non‐biological treatment 2
6.3. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 3: Anti‐TNF alpha versus placebo
6.4. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 4: Ustekinumab versus placebo
6.5. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 5: Anti‐IL17 versus placebo
6.6. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 6: Anti‐IL23 versus placebo
6.7. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 7: Biologic versus non‐biological treatments
6.8. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 8: Biologic 1 versus biologic 2
6.9. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 9: Small molecules versus placebo
6.10. Analysis.

Comparison 6: Secondary outcome ‐ adverse events, Outcome 10: Biologic versus small molecules
NETWORK META‐ANALYSES
Adverse events (AEs) outcome was available in 105 trials, involving 45,677 participants (91.2% of the participants in this review). AEs were not reported for the 25 remaining trials, and we were not able to obtain missing information from the trial authors (Table 2). This outcome was also reported in six trials (Asahina 2016; Bissonnette 2015; Khatri 2016; SCULPTURE 2015; Ortonne 2013; PRISTINE 2013), comparing different dosages of the same drug, and were added to the sensitivity analyses at dose level. This outcome was reported in 10 trials out of 105 with biological‐naïve participants and were added to the sensitivity analysis for all trials, whatever the previous treatments received by the participants (Barker 2011; Caproni 2009; Gisondi 2008; Lee 2016; NCT03255382; NCT03331835; Reich 2020; CHAMPION 2008; PRIME 2017; POLARIS 2020). Sixty‐three trials, involving 22,325 participants, were placebo‐controlled trials; 20, involving 6820 participants, were head‐to‐head comparisons; and 22, involving 16,532 participants, had both a placebo and at least two active treatments arms.
See Figure 4; Figure 5; Figure 6; Figure 8; Figure 10; Figure 12; Figure 14; Figure 15
We present the summary relative effects from the network meta‐analysis in league tables for both class‐level (Figure 6) and drug‐level (Figure 8) analyses. At class level, all of the classes of treatments had a more significant risk of AEs compared to placebo, except anti‐IL23. Significant associations were found: anti‐IL17 had a higher risk of AEs compared with anti‐IL23 and anti‐IL12/23; anti‐IL23 also had a lower risk of AEs compared with anti‐TNF and small molecules (Figure 6). Results of comparisons between each of the drugs are available in Figure 8.
Ranking class‐level analysis(Figure 10; Figure 14Table 4)
Placebo had the highest SUCRA (SUCRA 92.4) at class‐level for all adverse events, followed by anti‐IL23 (versus placebo: RR 1.01, 95% CI 0.95 to 1.07; SUCRA = 88.3), anti‐IL12/23 (versus placebo: RR 1.07, 95% CI 1.01 to 1.14; SUCRA = 57.5), then anti‐TNF agents (versus placebo: RR 1.08, 95% CI 1.03 to 1.13; SUCRA = 52.6). The heterogeneity τ for this network overall was 0.01, which we considered to be low.
Ranking drug‐level analysis(Figure 12; Figure 15; Table 5)
Tildrakizumab had the highest SUCRA at drug‐level for all adverse events (versus placebo: RR 0.93, 95% CI 0.82 to 1.04; SUCRA = 95.2), followed by placebo (SUCRA = 85.4), certolizumab (versus placebo: RR 1.01, 95% CI 0.89 to 1.15; SUCRA = 78.2), then mirikizumab (versus placebo: RR 0.99, 95% CI 0.81 to 1.22; SUCRA = 78.2). The heterogeneity τ for this network overall was 0, which we considered to be low.
2.5. Proportion of participants who achieve PASI 90 at 52 weeks
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at drug level in Analysis 7.1; Analysis 7.2; and Analysis 7.3.
7.1. Analysis.

Comparison 7: Secondary outcome ‐ PASI 90 at 52 weeks, Outcome 1: Biologic 1 versus biologic 2
7.2. Analysis.

Comparison 7: Secondary outcome ‐ PASI 90 at 52 weeks, Outcome 2: Small molecule 1 versus small molecule 2
7.3. Analysis.

Comparison 7: Secondary outcome ‐ PASI 90 at 52 weeks, Outcome 3: Biologic versus placebo
Eight head‐to‐head comparisons compared two different biologics; three compared two different dosages of secukinumab, guselkumab, and apremilast respectively; and one compared a biologic with placebo. We produced one meta‐analysis for the comparison risankizumab versus ustekinumab. For reaching PASI 90 at 52 weeks, risankizumab was more effective than ustekinumab (RR 1.73, 95% CI 1.46 to 2.05). Secukinumab was more effective than ustekinumab to reach PASI 90 at 52 weeks (RR 1.23, 95% CI 1.15 to 1.31); guselkumab was more effective than adalimumab to reach PASI 90 at 52 weeks (RR 1.59, 95% CI 1.40 to 1.81); ixekizumab every other week was more effective than ixekizumab every four weeks to reach PASI 90 at 52 weeks (RR 1.06, 95% CI 1.01 to 1.11); guselkumab was more effective than secukinumab to reach PASI 90 at 52 weeks (RR 0.83, 95% CI 0.78 to 0.89); risankizumab was more effective than secukinumab to reach PASI 90 at 52 weeks (RR 1.52, 95% CI 1.31 to 1.76); and ixekizumab was more effective than ustekinumab to reach PASI 90 at 52 weeks (RR 1.30, 95% CI 1.11 to 1.52; 1 study).
2.6. Proportion of participants who achieve PASI 75 at 52 weeks
DIRECT EVIDENCE
We report treatment estimates for pair‐wise meta‐analyses at drug level in Analysis 8.1; and Analysis 8.2.
8.1. Analysis.

Comparison 8: Secondary outcome ‐ PASI 75 at 52 weeks, Outcome 1: Biologic 1 versus biologic 2
8.2. Analysis.

Comparison 8: Secondary outcome ‐ PASI 75 at 52 weeks, Outcome 2: Small molecules 1 versus small molecules 2
Eight head‐to‐head comparisons compared two different biologics; four compared two different dosages of secukinumab, guselkumab, apremilast and tofacitinib respectively. We produced one meta‐analysis for the comparison risankizumab versus ustekinumab. For reaching PASI 75 at 52 weeks, risankizumab was more effective than ustekinumab (RR 1.26, 95% CI 1.12 to 1.41). Secukinumab was more effective than ustekinumab to reach PASI 75 at 52 weeks (RR 1.13, 95%CI 1.04 to 1.22); guselkumab was more effective than adalimumab to reach PASI 75 at 52 weeks (RR 1.40, 95% CI 1.28 to 1.54); ixekizumab every other week was more effective than ixekizumab every four weeks to reach PASI 75 at 52 weeks (RR 1.14, 95% CI 1.07 to 1.22); secukinumab was more effective than guselkumab to reach PASI 75 at 52 weeks (RR 1.14, 95% CI 1.08 to 1.21); risankizumab was more effective than secukinumab to reach PASI 75 at 52 weeks (RR 1.28, 95% CI 1.14 to 1.44); and ixekizumab was more effective than ustekinumab to reach PASI 75 at 52 weeks (RR 1.16, 95% CI 1.05 to 1.29).
We did not conduct network meta‐analyses, given the low number of studies for this outcome.
3. Assessment of heterogeneity and inconsistency
We did not identify important heterogeneity either in direct meta‐analyses or in network meta‐analysis. The common outcome‐specified network heterogeneity and the prediction intervals suggested the presence of low heterogeneity for all outcomes. We investigated differences in heterogeneity between class‐ and drug‐level analysis, and we also investigated differences in heterogeneity between primary and sensitivity analyses for the primary outcomes (see: 4. subgroup and sensitivity analyses). The results were very similar.
The distribution of some participant characteristics (age, sex ratio, weight, severity of psoriasis) did not give an indication of important differences in these characteristics across comparisons (see Figure 16; Figure 17).
16.

Distributions of age (on the left, mean age in years in the y axis) and PASI score at baseline (on the right, mean PASI in the y axis) ratio of participants across comparisons (x axis)
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
17.

Distributions of sex (on the left, percentage of males in the y axis) and weight (on the right, mean weight in kilograms in the y axis) of participants across comparisons (x axis)
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
At drug‐level analysis, the global test for inconsistency was not significant for any of the outcomes. We detail results of a global test for inconsistency at drug level in Figure 18 and Figure 19 for PASI 90 and SAEs, respectively. The loop‐specific and side‐splitting approaches did not indicate inconsistency for the two primary outcomes (Figure 20; Figure 21). There are a handful of loops and comparisons with statistically significant inconsistency for secondary outcomes (PASI 75 and adverse events), but it does not exceed the expected level of inconsistency that has been suggested by empirical evidence (Veroniki 2013), which is about 10% of the total number of loops.
18.

Side‐splitting approach and design‐by‐treatment interaction model for inconsistency for Psoriasis Area and Severity Index (PASI) 90
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
19.

Side‐splitting approach and design‐by‐treatment interaction model for inconsistency for serious adverse events (SAEs)
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
20.

Inconsistency plots for all the outcomes at class level
Inconsistency factor (IF) is calculated as the risk ratio (RR)/standardised mean difference (SMD) for direct evidence over the RR/SMD for indirect evidence in the loop with its 95% confidence interval (CI). IF value close to 0 indicates the absence of evidence for disagreement between direct and indirect evidence.
AIL12/23: anti‐IL12/23; AIL17: anti‐IL17; AIL23: anti‐IL23, ATA: anti‐TNF alpha; CSA: non‐biological conventional systemic agents; PBO: placebo; SM: small molecules
21.

Inconsistency plots for all the outcomes at drug level
Inconsistency factor (IF) is calculated as the risk ratio (RR)/standardised mean difference (SMD) for direct evidence over the RR/SMD for indirect evidence in the loop with its 95% confidence interval (CI). IF value close to 0 indicates the absence of evidence for disagreement between direct and indirect
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
4. Subgroup and sensitivity analyses
As we found no heterogeneity, we did not perform subgroup analyses. From a clinical point of view, it could nevertheless be interesting to have specific efficacy/safety data depending on participants' comorbidities or psoriasis characteristics. However, we did not have enough data for any of the aforementioned characteristics, and were therefore unable to run subgroup analyses and meta‐regressions to investigate their potential effects on the results.
Results of the sensitivity analyses involving the following were similar to those of the main analysis for the two primary outcomes:
excluding studies with fewer than 50 participants (Figure 22) (the heterogeneity τ for this subgroup network was 0 and 0.02 for PASI 90 and SAEs respectively, which we considered to be low);
completers (Figure 23) (the heterogeneity τ for this subgroup network was 0 and 0.02 for PASI 90 and SAEs respectively, which we considered to be low);
analyses at dose level splitting approved dosages versus other dosages for each drug (Figure 24) (the heterogeneity τ for this subgroup network was 0 for PASI 90 and SAEs, which we considered to be low);
excluding studies at high risk of bias (Figure 25) (the heterogeneity τ for this subgroup network was 0 for PASI 90 and 0.03 for SAEs, which we considered to be low);
analysing only the studies with a short‐term assessment from 8 to 16 weeks (Figure 26): the heterogeneity τ for this subgroup network was 0 for PASI 90 and 0.02 for SAEs, which we considered to be low.
analysing including trials with systemic‐treatment‐naïve participants (Figure 27): the heterogeneity τ for this subgroup network was 0 for PASI 90 and SAEs, which we considered to be low.
22.

Sensitivity analyses ‐ Interval plot. Network meta‐analysis results for primary outcomes (PASI 90 and serious adverse events, left and right forest plot respectively) for trials with at least 50 participants.
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
CI: confidence interval; PASI: Psoriasis Area and Severity Index; RR: risk ratio
23.

Sensitivity analyses ‐ Interval plot. Network meta‐analysis results for primary outcomes (PASI 90 and serious adverse events, left and right forest plot respectively) for the completers.
Outcomes were measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
CI: confidence interval; PASI: Psoriasis Area and Severity Index; RR: risk ratio
24.
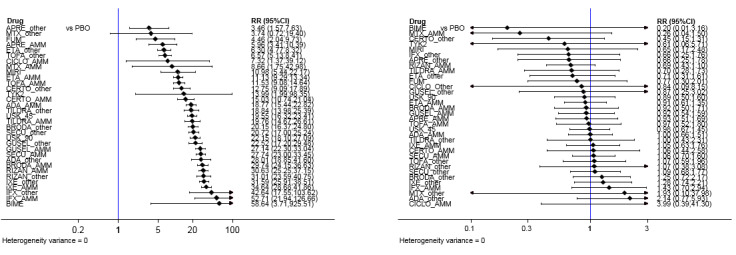
Sensitivity analyses ‐ Interval plot. Network meta‐analysis results for primary outcomes (PASI 90 and serious adverse events, left and right forest plot respectively) for all the interventions depending on the doses: approved dosages versus other dosages
Outcomes were measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
MTX_AMM/Other: methotrexate ≥ 15 mg per week/ < 15 mg per week; CICLO_AMM/Other: ciclosporin ≥ 3 mg/kg/day/<3 mg/kg/day; ACI_AMM/Other: acitretin ≥ 35 mg per day/<35 mg per day; FUM: fumaric acid esters all dosages; APRE_AMM/Other: apremilast 30 mg twice daily/other dosages; TOFA_AMM/Other: tofacitinib 20 mg per day/Other dosages; ETA_AMM/Other: etanercept 50 mg twice a week/Other dosage; IFX_AMM/Other: infliximab 5 mg/kg week 0, 2, 4 every 6 weeks/Other dosages; ADA_AMM/Other: adalimumab 80 mg Week 0, 40 mg Week 1 then 40 mg every other week/Other dosages; CERTO_AMM/Other: certolizumab 400 mg at week 0,2,4 then 400 mg every other week or other dosages/Other dosages; USK 45/90: ustekinumab 45/90 mg; SECU_AMM/Other: secukinumab 300 mg at week 0, 1, 2, 3, and 4 then every 4 weeks or other dosages/other dosages; IXE_AMM/Other: ixekizumab 160 mg at Week then 80 mg every other weeks until week 12 then 80 mg monthly or other dosages; TILDRA_AMM/Other: tildrakizumab 100 mg at week 0 and 4 then every 12 weeks/Other dosages; GUSEL 100: guselkumab 100 mg per injection; BRODA_AMM/Other: brodalumab 210 mg at week 0, 1, 2 then every other weeks/other dosages; RISAN_AMM/Other: risankizumab, S/C, 150 mg (two 75 mg injections) at Week 0, Week 4 and every 12 weeks thereafter/other dosages; TYK2 (Oral Tyrosine kinase 2 inhibitor), MIRI (mirikizumab) and BIME (bimekizumab) (S/C) were grouped in one dosage whatever the dosages.
CI: confidence interval; PASI: Psoriasis Area and Severity Index; RR: risk ratio; AMM: 'approved dosage'
25.

Sensitivity analyses ‐ Interval plot. Network meta‐analysis results for primary outcomes (PASI 90 and serious adverse events, left and right forest plot respectively) for all the interventions excluding studies at high risk of bias.
Outcomes were measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
CI: confidence interval; PASI: Psoriasis Area and Severity Index; RR: risk ratio
26.

Sensitivity analyses ‐ Interval plot. Network meta‐analysis results for primary outcomes (PASI 90 and serious adverse events, left and right forest plot respectively) for all the interventions including studies with a short‐term assessment from 8 to 16 weeks.
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
CI: confidence interval; PASI: Psoriasis Area and Severity Index; RR: risk ratio
27.

Sensitivity analyses ‐ Interval plot. Network meta‐analysis results for primary outcomes (PASI 90 and serious adverse events, left and right forest plot respectively) for all the interventions including studies with systemic treatment‐naive participants.
Outcomes were measured at the induction phase (assessment from 8 to 24 weeks after randomisation).
ACI: acitretin; ADA: adalimumab; APRE: apremilast; BIME: bimekizumab; BRODA: brodalumab; CERTO: certolizumab; CICLO: ciclosporin; ETA: etanercept; FUM: fumaric acid; IFX: infliximab; IXE: ixekizumab; GUSEL: guselkumab; MIRI: mirikizumab; MTX: methotrexate; PBO: placebo; RISAN: risankizumab; SECU: secukinumab; TILDRA: tildrakizumab; TOFA: tofacitinib; TYK2: Oral Tyrosine kinase 2 inhibitor; USK: ustekinumab
CI: confidence interval; PASI: Psoriasis Area and Severity Index; RR: risk ratio
5. Reporting bias
The comparison‐adjusted funnel plots generally appeared symmetrical, and only the graph for quality of life presented some evidence of small‐study effects which might be caused by selective outcome reporting (Figure 28). As the funnel plots were symmetrical, we did not consider running meta‐regression.
28.

Funnel plot for network meta‐analysis of all the outcomes
AE: adverse event; lnRR: Mean effect size; PASI: Psoriasis Area and Severity Index; QoL: Specific quality of life scale; RR: Risk ratio; SAE: serious adverse events; SAE without worsening of psoriasis correspond to SAE after exclusion of flares of psoriasis; SMD: standardised mean difference
6. Grading of the evidence
We present results of evaluation of certainty of evidence for the primary efficacy and safety outcomes in Table 7; Table 8 and Figure 7; Figure 29; Figure 30.
7. Study Bias distribution for PASI 90 using CINeMA.
| Comparison | Number of studies | Within‐study bias | Reporting bias | Indirectness | Imprecision | Heterogeneity | Incoherence | Confidence rating |
| ADA:GUSEL | 3 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:PBO | 8 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:RISAN | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| APRE:ETA | 1 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:PBO | 5 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| BIME:PBO | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| BRODA:PBO | 5 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BRODA:USK | 2 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CERTO:ETA | 1 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:PBO | 5 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CICLO:MTX | 2 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:IFX | 1 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| ETA:IXE | 2 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:PBO | 14 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:SECU | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:TILDRA | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:TOFA | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:USK | 1 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:MTX | 1 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:PBO | 1 | Major concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| GUSEL:IXE | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| GUSEL:PBO | 5 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IFX:PBO | 5 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IXE:PBO | 4 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IXE:USK | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| MIRI:PBO | 2 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| MTX:PBO | 2 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| PBO:RISAN | 4 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| PBO:SECU | 13 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| PBO:TILDRA | 3 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| PBO:TOFA | 5 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| PBO:TYK2 | 1 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| PBO:USK | 10 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| RISAN:SECU | 1 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| RISAN:USK | 3 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| SECU:USK | 2 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:APRE | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:BIME | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:BRODA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:CERTO | 0 | No concerns | Undetected | No concerns | Some concerns | No concerns | No concerns | High |
| ADA:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ADA:ETA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:FAEs | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| ADA:IFX | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:IXE | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ADA:SECU | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:TOFA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ADA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:BIME | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:BRODA | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| APRE:CERTO | 0 | Some concerns | Undetected | No concerns | Some concerns | Some concerns | No concerns | Low |
| APRE:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:GUSEL | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| APRE:IFX | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| APRE:IXE | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| APRE:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:RISAN | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| APRE:SECU | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| APRE:TILDRA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| APRE:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:USK | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BIME:BRODA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:CERTO | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BIME:ETA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BIME:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BIME:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:CERTO | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BRODA:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:ETA | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BRODA:FAEs | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BRODA:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:IFX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:IXE | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| BRODA:MIRI | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| BRODA:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:RISAN | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BRODA:SECU | 0 | Some concerns | Undetected | No concerns | Some concerns | No concerns | No concerns | Moderate |
| BRODA:TILDRA | 0 | No concerns | Undetected | No concerns | Some concerns | No concerns | No concerns | High |
| BRODA:TOFA | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| BRODA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:FAEs | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CERTO:GUSEL | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| CERTO:IFX | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CERTO:IXE | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| CERTO:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:RISAN | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CERTO:SECU | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CERTO:TILDRA | 0 | No concerns | Undetected | No concerns | Some concerns | No concerns | No concerns | High |
| CERTO:TOFA | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CERTO:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:USK | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CICLO:ETA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:FAEs | 0 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:GUSEL | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:IFX | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CICLO:IXE | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:MIRI | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:PBO | 0 | Major concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| CICLO:RISAN | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:SECU | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:TILDRA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:TYK2 | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:USK | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:FAEs | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| ETA:GUSEL | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:RISAN | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| ETA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| FAEs:GUSEL | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:IFX | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:IXE | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:MIRI | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:RISAN | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:SECU | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:TILDRA | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| FAEs:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:TYK2 | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:USK | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| GUSEL:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:MIRI | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| GUSEL:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| GUSEL:RISAN | 0 | No concerns | Undetected | No concerns | Some concerns | No concerns | No concerns | High |
| GUSEL:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:TILDRA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| GUSEL:TOFA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| GUSEL:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:USK | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IFX:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:MIRI | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IFX:MTX | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| IFX:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:TILDRA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IFX:TOFA | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| IFX:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:USK | 0 | Some concerns | Undetected | No concerns | No concerns | No concerns | No concerns | Moderate |
| IXE:MIRI | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IXE:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| IXE:RISAN | 0 | No concerns | Undetected | No concerns | Some concerns | No concerns | No concerns | High |
| IXE:SECU | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IXE:TILDRA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IXE:TOFA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| IXE:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MIRI:RISAN | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| MIRI:SECU | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| MIRI:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MTX:RISAN | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:SECU | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:TILDRA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:TYK2 | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:USK | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| RISAN:TILDRA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| RISAN:TOFA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| RISAN:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| SECU:TILDRA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| SECU:TOFA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| SECU:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TILDRA:TOFA | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| TILDRA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TILDRA:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TOFA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TOFA:USK | 0 | No concerns | Undetected | No concerns | No concerns | No concerns | No concerns | High |
| TYK2:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
8. Study bias distribution for serious adverse events using CINeMA.
| Comparison | Number of studies | Within‐study bias | Reporting bias | Indirectness | Imprecision | Heterogeneity | Incoherence | Confidence rating |
| ADA:GUSEL | 3 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:PBO | 9 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:RISAN | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:ETA | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:PBO | 7 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:PBO | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:PBO | 5 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:USK | 2 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:ETA | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:PBO | 4 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:MTX | 2 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:PBO | 1 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:IFX | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:IXE | 2 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:PBO | 13 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:SECU | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:TILDRA | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:TOFA | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:USK | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| FAEs:MTX | 1 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:PBO | 1 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| GUSEL:IXE | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:PBO | 5 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:PBO | 6 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:PBO | 4 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:USK | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:PBO | 2 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MTX:PBO | 2 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| PBO:RISAN | 4 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| PBO:SECU | 12 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| PBO:TILDRA | 3 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| PBO:TOFA | 7 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| PBO:TYK2 | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| PBO:USK | 11 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| RISAN:SECU | 1 | No concerns | Undetected | No concerns | Major concerns | No concerns | Major concerns | Low |
| RISAN:USK | 3 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| SECU:USK | 2 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:APRE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:BIME | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:BRODA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:CERTO | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ADA:ETA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ADA:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ADA:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ADA:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:BIME | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:BRODA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:CERTO | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| APRE:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| APRE:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:BRODA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:CERTO | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BIME:ETA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BIME:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BIME:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BIME:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:CERTO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:ETA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:IFX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:RISAN | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:SECU | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| BRODA:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| BRODA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:CICLO | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CERTO:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CERTO:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| CICLO:ETA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:FAEs | 0 | Major concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:GUSEL | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:IFX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:IXE | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:MIRI | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:RISAN | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:SECU | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:TILDRA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:TYK2 | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| CICLO:USK | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:FAEs | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:GUSEL | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| ETA:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| ETA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| FAEs:GUSEL | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:IFX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:IXE | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:MIRI | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:RISAN | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:SECU | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:TILDRA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:TYK2 | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| FAEs:USK | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| GUSEL:IFX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| GUSEL:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| GUSEL:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:IXE | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| IFX:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IFX:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:MIRI | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:MTX | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| IXE:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:MTX | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MIRI:RISAN | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:SECU | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MIRI:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MTX:RISAN | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:SECU | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| MTX:TOFA | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:TYK2 | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| MTX:USK | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| RISAN:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| RISAN:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| RISAN:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| SECU:TILDRA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| SECU:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| SECU:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TILDRA:TOFA | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TILDRA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TILDRA:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TOFA:TYK2 | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
| TOFA:USK | 0 | Some concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Low |
| TYK2:USK | 0 | No concerns | Undetected | No concerns | Major concerns | No concerns | No concerns | Moderate |
29.
Certainty of evidence per drug for PASI 90 using CINeMA
Each drug is presented as a bar, which indicates the composition of the 4‐level confidence of evidence from all comparisons including that drug. Green: high confidence; blue: moderate confidence; yellow: low confidence; red: very low confidence.
30.
Certainty of evidence per drug for Serious Adverse Events using CINeMA
Each drug is presented as a bar, which indicates the composition of the 4‐level confidence of evidence from all comparisons including that drug. Green: high confidence; blue: moderate confidence; yellow: low confidence; red: very low confidence.
Table 7 and Table 8 represent for PASI 90 and SAEs respectively, the evaluation of concerns (no concern, some concerns or major concerns) for each domain assessed (within‐study bias, reporting bias, indirectness, imprecision, heterogeneity and incoherence). We detected no reporting bias, and there were no concerns that indirectness was present for any comparison for PASI 90 or SAEs. After the judgement for all the six domains, our overall confidence in the evidence for each comparisons is rated high, moderate, low and very low, as described in the Methods section. Results of overall confidence in evidence are available in Table 7, Table 8 and Figure 7.
Figure 29 and Figure 30 represent by drug the overall percentage of comparisons including that drug assessed as high, moderate, low and very‐low certainty of evidence. For PASI 90, the overall certainty of the evidence was moderate to high. None of the comparisons were assessed as very low. For methotrexate and ciclosporin certainty of evidence was low for more than 80% of comparisons including these treatments. For bimekizumab, brodalumab, certolizumab, FAEs, infliximab, and oral tyrosine kinase 2 inhibitor, certainty of evidence was moderate for most comparisons. For all other drugs, the certainty of evidence was high for most comparisons. Reasons for downgrading to moderate or low certainty were within‐study bias or imprecision, or both. For SAEs, the overall certainty of evidence was low to moderate. None of the comparisons were assessed as very low. For tofacitinib, methotrexate, FAEs, brodalumumab and ciclosporin, the certainty of evidence was low. The certainty of evidence was moderate for all other treatments. Reasons for downgrading to moderate or low certainty were within‐study bias or imprecision, or both.
Discussion
Summary of main results
Our review and meta‐analysis compares all systemic pharmacological drugs and systemic drugs undergoing phase II/III trials used for moderate‐to‐severe psoriasis in 2020.
This updated review included 158 studies, involving 57,831 randomised adult participants, which assessed most outcomes during the induction phase (from 8 to 24 weeks after randomisation). Participants in the included studies were young, with a mean age of 45 years, and had moderate‐to‐severe psoriasis with an overall mean PASI score at baseline of 20. Ninety‐two trials compared systemic treatment against placebo, 48 were head‐to‐head trials, and 18 had both an active comparator and a placebo. Sixteen trials had a co‐intervention, mainly phototherapy. Eight trials assessed biosimilars versus original drugs for adalimumab or etanercept. Finally, 123 studies declared pharmaceutical company funding, and 22 studies did not report the source of funding.
We included 130 studies (without co‐intervention and without trials in biosimilar development), involving 50,081 participants (87% of the participants in this review), in the classical or network meta‐analysis (NMA). Non‐biological systemic agents, the oldest class‐level treatment (acitretin, ciclosporin, fumaric acid esters (FAEs), methotrexate); anti‐TNF alpha treatments (etanercept, infliximab, adalimumab, certolizumab); an anti‐IL12/23 treatment (ustekinumab); anti‐IL17 treatments (secukinumab, ixekizumab, brodalumab); and anti‐IL23 (guselkumab, tildrakizumab, risankizumab) have all been approved for psoriasis, except for bimekizumab and mirikizumab. Apart from apremilast, small molecule drugs (tofacitinib, tyrosine kinase 2 inhibitor (BMS‐986165)), had not been approved for psoriasis at the time we conducted our analyses.
The following results are based on network meta‐analysis.
All of the assessed interventions appeared superior to placebo in terms of reaching Psoriasis Area and Severity Index (PASI) 90.
At class level, network meta‐analysis showed that the biologics anti‐IL17, anti‐IL23, anti‐IL12/23, and anti‐TNF alpha outperformed the small molecules and the non‐biological agents to reach PASI 90.
For reaching PASI 90, the most effective drugs when compared to placebo were (in SUCRA (surface under the cumulative ranking curve) rank order): infliximab (high‐certainty evidence), ixekizumab (high‐certainty evidence), risankizumab (high‐certainty evidence), bimekizumab (high‐certainty evidence), secukinumab (high‐certainty evidence), guselkumab (high‐certainty evidence), and brodalumab (moderate‐certainty evidence); see Figure 7. The clinical effectiveness of these drugs was similar when compared against each other, except for ixekizumab which had a better chance of reaching PASI 90 compared with secukinumab, guselkumab and brodalumab.
At drug level, infliximab, ixekizumab, secukinumab, brodalumab, risankizumab and guselkumab were significantly more effective in reaching PASI 90 than ustekinumab and three anti‐TNF alpha agents: adalimumab, certolizumab, and etanercept. Ustekinumab and adalimumab were significantly more effective in reaching PASI 90 than etanercept; ustekinumab more effective than certolizumab, and the clinical effectiveness for ustekinumab and adalimumab was similar. Only one trial assessed the efficacy of bimekizumab in this network, so the results for bimekizumab have to be interpreted with caution, as well as those for mirikizumab (two trials including a phase 2), tyrosine kinase 2 inhibitor, acitretin, ciclosporin, fumaric acid esters, and methotrexate. There was no significant difference between tofacitinib or apremilast and three non‐biological drugs: FAES, ciclosporin and methotrexate. The results were similar to PASI 90 for the other efficacy outcomes (PASI 75 and PGA 0/1).
We found no significant difference between any of the interventions and the placebo for the risk of serious adverse events (SAEs). Methotrexate (low‐certainty evidence), bimekizumab (moderate‐certainty evidence), risankizumab (moderate‐certainty evidence), mirikizumab (moderate‐certainty evidence) and oral tyrosine kinase 2 inhibitor (moderate‐certainty evidence) had the highest SUCRA at drug level for all the SAEs (see Figure 7).
There was often poor reporting of information about quality of life, and these data were absent for several of the interventions.
Finally, considering both efficacy (PASI 90 outcome) and acceptability (SAE outcome), highly‐effective treatments also had more SAEs than the other treatments, and risankizumab and bimekizumab appeared to be the better compromise between efficacy and acceptability, bearing in mind the limitations that affect interpretation of the SAE results, such as the very low number of events on which they were based.
Overall completeness and applicability of evidence
We were able to draw some conclusions on the effectiveness (and ranking) of the systemic treatment options for moderate‐to‐severe chronic plaque psoriasis during the induction phase. Long‐term efficacy and safety data are lacking. Specific details are listed below.
Participants
Participants in the included studies had a mean age of 45 years and had moderate‐to‐severe psoriasis, with an overall mean PASI score at baseline of 20 (range: 9.5 to 39) and a duration of psoriasis of 18 years (range 7 to 21.5). This young age and the high level of disease severity may not be typical of patients seen in daily clinical practice, or those who need a first‐line systemic treatment.
In addition, participants selected for randomised controlled trials (RCTs) generally have few major comorbidities. Almost all studies including one biological arm excluded patients with a history of infectious diseases or malignancies and signs of severe renal, cardiac, hepatic, demyelinating, or other disorders. This may impact the generalisability of these results for clinical practice. However, some participant characteristics (such as being overweight, imbalanced sex ratio in favour of men, presence of metabolic syndrome) were reflective of a moderate‐to‐severe psoriasis population, comparable to literature data (Wolkenstein 2009).
Interventions
Evidence on 20 active treatments included in this review was derived from 158 trials (searched for up to September 2020). We included all interventions, irrespective of the dose. Thus, we increased the number of available RCTs for each intervention and had more power to assess SAEs and adverse events (AEs). The number of studies included in the NMA was still low for the following interventions: bimekizumab, mirikizumab, tyrosine kinase 2 inhibitor, acitretin, ciclosporin, fumaric acid esters, and methotrexate, meaning we must be cautious about the conclusions drawn for these drugs. The results from the sensitivity analysis using a standard dose for each intervention was similar for PASI 90 (and SAEs) compared to the main analyses, giving us confidence in the results of the main analysis.
For drugs just approved or not yet approved for psoriasis, ongoing studies are still investigating bimekizumab, mirikizumab, brodalumab, and BMS‐986165 (Characteristics of ongoing studies).
Comparisons
Most studies included in the review were only placebo‐controlled (around 60%). Once the benefit of a treatment has been established against placebo using high‐quality evidence, only head‐to‐head trials would be helpful to provide physicians with efficacy estimates between the different biologics, based on stronger evidence than indirect comparisons.
Outcomes
Many of the trials included in this review provide evidence for the proportion of participants who reached PASI 90, PASI 75, or Physician Global Assessment (PGA) 0/1 or who experienced SAEs or AEs. We chose PASI 90 as the main efficacy outcome. The differences in PASI 90 rates must be balanced against the differences in quality‐of‐life improvements that are observed. Results for both outcomes cannot be correlated. On the other hand, patient‐reported outcome (PRO) data were scanty and poorly reported in our review. Moreover, the heterogeneity of the scales used for QOL in psoriasis trials required using the standardised mean difference (SMD) in the network. SMD shows the difference in standard deviations of the outcome, and from a clinical point of view, the interpretation of the results is difficult. It has been suggested that values 0.2, 0.5 and 0.8 might indicate small, moderate and large magnitude of the effect size (Cohen 1988). So, from a clinical point of view, the interpretation of the results was difficult: a significant result for PRO between two drugs did not mean that the result was clinically useful for the patients. Results for SAEs have to be interpreted cautiously, because RCTs do not last long enough and are not powered to be able to detect rare and severe adverse events. The results of our sensitivity analysis assessing SAEs without psoriasis flares did not differ from those of the primary outcome. We did not summarise individual SAE types or classes of SAE in this review, in part because classification differed across different data sources. This was the subject of a separate detailed assessment of types of SAE, adverse events leading to discontinuation of trial medication, and system‐organ class adverse events (Afach 2021).
Timing
All of the trials included in the NMAs assessed the efficacy of the different treatments during the induction treatment phase (from 8 to 24 weeks). Assessment of longer‐term outcomes may also be relevant for this chronic disease. The trials were designed to detect differences in the severity of psoriasis in response to therapy over short periods of treatment, and are often underpowered and of insufficient duration to detect rare or long‐term adverse events. It is therefore of interest to conduct studies taking into account the induction of remission but also the long‐term management (long‐term remission) and the long‐term safety of the drug. In order to provide long‐term information on the safety of the treatments included in this review, it will be necessary also to evaluate non‐randomised studies and postmarketing reports released from regulatory agencies.
Quality of the evidence
Overall, our confidence in the treatment estimates for PASI 90 is high or moderate for comparisons involving anti‐IL17 , anti‐IL12/23 , anti‐IL23, or anti‐TNF alpha agents, and small molecules. We judged our confidence in treatment estimates for PASI 90 as low for the comparisons involving non‐biological systemic agents; we downgraded the certainty of the evidence for risk of bias and then for imprecision. We judged our confidence in the treatment estimates for SAEs to be low certainty for one‐third of the treatment estimates, and moderate for the others; we downgraded the certainty of the evidence for imprecision and risk of bias.
Risk of bias
The risks of bias in the included studies appear to be globally low (Figure 2; Figure 3). However, some limitations should be discussed.
There was variation in how well the studies took measures to blind investigators and participants: a third of trials in this review were rated at high or unclear risk of performance bias (53 out of 158). This is an important point to highlight, as the outcomes used for assessing efficacy were subjective. However, the proportion of trials at high risk of blinding used in the network meta‐analyses decreased to 22% (28 out of 130).
The reporting of missing outcome data was largely inadequate in a few studies. Since we chose a likely scenario that any participant with missing outcome data did not experience clearance for the overall analyses, we minimised the risk of overestimating efficacy due to how we reported missing data.
Finally, we rated a few trials at high risk of selective outcome reporting. However, we chose a stringent definition of studies at high risk of selective outcome reporting: we considered reporting bias inadequate if one specified outcome in protocols was lacking in the main report. A large proportion of included trials did not report the patient‐reported outcomes in the main report but only in slicing publications (see Included studies). We extracted outcomes of interest both in main and slicing publications, but this disadvantaged trials that did not report all of the specified outcomes in the main report.
Indirect comparison and network meta‐analyses as standard pair‐wise meta‐analyses provide 'observational' evidence, since the treatments being compared have not been randomised across studies. However, we considered carefully the assumption underpinning the validity of indirect comparisons, to assure a sufficiently coherent evidence base (Cipriani 2013). The limitations of this review are reflected by CINeMA evaluations.
Heterogeneity (i.e. variation in effect modifiers within comparisons) and inconsistency (imbalance in effect modifiers between comparisons)
We found no evidence of heterogeneity either in direct comparisons or in the entire networks. At drug‐level analysis, the global test for inconsistency was not significant for any of the outcomes.
Imprecision
The number of studies included in the NMA was low for the following interventions (one or two studies for each interventions): bimekizumab, mirikizumab, tyrosine kinase 2 inhibitor, acitretin, ciclosporin, fumaric acid esters, and methotrexate, meaning we must be cautious about the conclusions drawn for these drugs. Indeed, it has been shown that treatment effect estimates differed according to trial sample size, with stronger effect estimates seen in small to moderately‐sized trials than in the largest trials (Dechartres 2013). Moreover, treatment effects in randomised controlled phase II trials were better than those in matched phase III trials (Liang 2019).
Indirectness or transitivity assumption
We did not find any evidence that important variables, such as age, sex, weight, and duration and severity of psoriasis, varied across comparisons (see Characteristics of included studies and Figure 16; Figure 17). However, the lack of data did not allow us to check the distributions of previous treatments across comparisons, so transitivity cannot properly be assessed statistically.
Several participant characteristics have changed in newer trials, such as participants' exclusion criteria. However, most of the included trials were conducted after 2000, minimising the variability across trial participant characteristics. The location of the trial could also create some differences between participants, as the response to treatment could be related to genetic background (Chiu 2014). To further confirm the plausibility of the transitivity assumption, we only included in our analyses trials not involving co‐interventions and not selecting participants on their previous systemic treatments, and performed several sensitivity analyses (see Quality of the evidence: Heterogeneity).
Publication bias
We assessed publication bias, considering the comprehensive search strategy we performed and the risk of publication bias in the specific field. The comparison‐adjusted funnel plot for all placebo‐controlled trials for all the outcomes did not indicate any evident risk of publication bias for the two primary outcomes (Figure 28).
Potential biases in the review process
We performed an extensive search for relevant trials. However, we did not contact pharmaceutical companies who do not have publicly available trials databases to enquiry whether they had conducted any additional relevant trials. We consider the probability that we have missed an eligible trial is low, considering our wide search, and this view is supported by the absence of small‐study effects (testing by the comparison‐adjusted funnel plots). However, the fact that 28 studies are awaiting classification and have not yet been incorporated may be a potential source of bias.
We conducted study selection, data extraction, and 'Risk of bias' assessments in duplicate and independently, and we reached consensus by discussing any discrepancies. Some published trial reports did not provide enough details to extract outcomes and adequately assess risks of bias, especially those performed before 2000 (i.e. before the International Committee of Medical Journal Editors issued the requirement of trial registration for publication). However, we contacted the authors of the trials to request missing data, but we cannot avoid some biased assessment in the review process due to incomplete reporting of trial details or results, or both.
We had some departures from the protocol plans (see Differences between protocol and review), especially excluding from the NMA analysis trials selecting participants on their previous systemic treatments.
Thus, we added one new sensitivity analysis including all trials, irrespective of the previous systemic treatments.
We only used CINeMA to assess our confidence in the results.
Agreements and disagreements with other studies or reviews
We searched in MEDLINE Ovid (from 1946) using the strategy "Psoriasis" AND "Network Meta‐analysis" for already‐published network meta‐analyses, identifying 71 references.
We compared our findings with the six most recent network meta‐analyses (Armstrong 2020; Geng 2018; Gómez‐García 2017; Jabbar‐Lopez 2017; Loos 2018; Xu 2019). Gómez‐García 2017 included 27 trials involving 10,629 participants, assessing three anti‐TNF alpha agents (infliximab, etanercept, and adalimumab), one anti‐IL12/23 agent (ustekinumab), and one anti‐IL17 agent (secukinumab). Jabbar‐Lopez 2017 included 41 trials, involving 20,561 participants, assessing the same drugs as Gómez‐García 2017, plus ixekizumab (another anti‐IL17 agent) and methotrexate. Loos 2018 included 34 trials, involving 22,892 participants, assessing biologic treatments (infliximab, adalimumab, etanercept, ustekinumab, secukinumab, ixekizumab and brodalumab) and apremilast. Armstrong 2020 included 60 trials (the number of participants is unknown) assessing biologic treatments (infliximab, adalimumab, etanercept, certolizumab, ustekinumab, secukinumab, ixekizumab, brodalumab, risankizumab, guselkumab, and tildrakizumab), apremilast and FAEs. As Geng 2018 and Xu 2019 included systemic treatments withdrawn from the market (briakinumab and efalizumab), we did not investigate these two reviews in detail.
Compared to previous reviews, we included more interventions and consequently more trials (n = 158) and participants (n = 57,831). Regarding the overlapping period between the different NMAs, we also included more trials than the other meta‐analyses. Indeed, we performed a larger search in terms of the number of databases used, including trials registers and other resources (unpublished literature), irrespective of the date or language limitations.
Gómez‐García 2017 presented both PASI 75 and PASI 90 results. Jabbar‐Lopez 2017 chose a composite outcome: PASI 90 or Physician Global Assessment (PGA) 1. We chose PASI 90 as our primary efficacy outcome, because complete clearance seems the less subjective outcome and the most relevant for patient expectations in short‐term assessment (induction phase). The composite outcome used by Jabbar‐Lopez 2017 did not reflect complete or almost complete clearance. Indeed, PGA 1 is highly correlated with PASI 75 and not with PASI 90, which could lead to a classification bias (Robinson 2012). Loos 2018 and Armstrong 2020 presented PASI 50, 75, and 90 results.
Jabbar‐Lopez 2017 and Armstrong 2020 presented their results using the number needed to treat for an additional beneficial outcome (NNTB). Although NNTB is an easily understandable and very useful measure for patients and clinicians, it can be misleading in a network meta‐analysis, since it requires the assumption of a common average control group risk applying to all studies. This is a rather strong assumption, particularly in networks involving head‐to‐head studies without a control group, as here.
Infliximab was also the most effective drug in Gómez‐García 2017, without significant difference between infliximab and secukinumab. Infliximab was ranked in third place after ixekizumab and secukinumab in Jabbar‐Lopez 2017, without a significant difference between infliximab and secukinumab. Infliximab was ranked in third place after ixekizumab and brodalumab in Loos 2018, without a significant difference between these three drugs and secukinumab (4th rank). Risankizumab, ixekizumab, brodalumab, guselkumab, secukinumab and infliximab were the best treatment options in Armstrong 2020. Our findings were close to these results, but differed in the ranking. One hypothesis is that time of evaluation range choice (from 10 to 16 weeks in Armstrong 2020 and from 8 to 24 weeks in our study) failed to include more Infliximab trials in Armstrong 2020. Our review also includes new agents (bimekizumab and mirikizumab for biologics).
Among the previous network meta‐analyses, Loos 2018 did not assess inconsistency, and two reported significant global and local inconsistency for PASI 75 (Gómez‐García 2017; Jabbar‐Lopez 2017).
Authors' conclusions
Implications for practice.
In terms of achieving PASI 90 with induction therapy (evaluation from 8 to 24 weeks after the randomisation), we found the following results, based on network meta‐analysis.
At class level, all of the assessed interventions (non‐biological systemic agents, small molecules, and biological treatments) showed significant superiority compared with placebo;
At class level, the biologic treatments anti‐IL17, anti‐IL12/23, anti‐IL23, and anti‐TNF alpha showed significant superiority compared with small molecules and non‐biological systemic agents;
At drug level, infliximab, ixekizumab, secukinumab, brodalumab, risankizumab and guselkumab were significantly more effective in reaching PASI 90 than ustekinumab and three anti‐TNF alpha agents: adalimumab, certolizumab, and etanercept. Ustekinumab and adalimumab were significantly more effective in reaching PASI 90 than etanercept; ustekinumab was more effective than certolizumab, and the clinical effectiveness for ustekinumab and adalimumab was similar.
When compared with placebo, the following biological agents are the most effective treatments (in SUCRA rank order) for reaching PASI 90: infliximab (high‐certainty evidence), ixekizumab (high‐certainty evidence), risankizumab (high‐certainty evidence), bimekizumab (high‐certainty evidence), secukinumab (high‐certainty evidence), guselkumab (high‐certainty evidence), and brodalumab (moderate‐certainty evidence). The clinical effectiveness of these seven drugs was similar when compared against each other, except for ixekizumab, which had a better chance of reaching PASI 90 compared with secukinumab, guselkumab and brodalumab.
There was no significant difference between tofacitinib or apremilast and three non‐biological drugs: fumaric acid esters (FAEs), ciclosporin and methotrexate.
For the other efficacy outcomes (PASI 75 and PGA0/1), the results were similar to the results for PASI 90.
For serious adverse events, there was no significant difference between any of the assessed interventions and placebo. Nonetheless, analyses of SAE events were based on a very low number of events with low‐to‐moderate certainty for all the comparisons. The findings therefore have to be viewed with caution. Considering both efficacy (PASI 90 outcome) and acceptability (SAE outcome), highly‐effective treatments also had more SAEs than the other treatments: risankizumab and bimekizumab appeared to be the better compromise between efficacy and acceptability.
Information on quality of life was not well reported and was absent for several of the interventions.
Conservative interpretation is warranted for the results for bimekizumab, mirikizumab, tyrosine kinase 2 inhibitor, acitretin, ciclosporin, fumaric acid esters, and methotrexate, as these drugs in the NMA have only been evaluated in few trials.
The evidence is limited to a selected trial population (participants were young (mean age of 45 years), had a high level of disease severity (with an overall mean score of PASI 20 at baseline, and were long‐time sufferers), and had few major comorbidities), and the NMA evidence was limited to the induction treatment phase (all results were measured from 8 to 24 weeks after randomisation), which is not relevant enough for a chronic disease, which would require long‐term treatment.
Our main results (i.e. superiority of efficacy of the biologic treatments anti‐IL17, anti‐IL12/23, anti‐IL23, and anti‐TNF alpha compared with small molecules and the non‐biological systemic agents) do not reflect the 'real life' management of patients in Europe or Canada, as an example. Currently, biological treatments may be positioned as third‐line therapies by regulatory bodies, with mandatory reimbursement criteria that patients must meet before being considered for these treatments (moderate‐to‐severe disease after failure, intolerance or contraindication to non‐biological systemic agents). Recently, the same restrictions were applied to apremilast. Such decisions were based on the lack of long‐term safety knowledge but also taking into account economic consideration. In this review, we found insufficient evidence to evaluate long‐term safety, and we did not address economic considerations, so the question of the choice of first‐line treatment for moderate‐to‐severe psoriasis is still debated.
The first choice in non‐biological systemic agents is still in question, as the limited number of trials assessing non‐biological systemic agents did not allow us to draw robust conclusions; this is also true for some small‐molecule treatments and biological treatments.
Implications for research.
From a clinical point of view, we need drugs that can be administered long‐term to provide continuous effective control, because continued remission after successful treatment is as important as successful induction of remission. Moreover, treatment should be easy to use, well accepted by patients, have minimal drug‐to‐drug interactions, and should have minimal monitoring requirements, because convenience is also an important issue when dealing with chronic diseases that require prolonged treatments. Finally, the cost of the drug should be affordable by most patients and by any national health service.
Specific questions and issues in the management of psoriasis still remain unmet:
Which non‐biological systemic agents have the best benefit/risk balance?
Which patients are candidates for small molecule treatment?
Which treatments work for subgroups of patients (age, psoriasis severity, previous treatment, psoriatic arthritis, race and ethnicity)?
Which treatments offer the best combination of safety and efficacy in patients with major comorbidities (e.g. hepatitis B/C, latent tuberculosis, HIV, and renal, cardiac, and hepatic impairment) as well as pregnancy?
Adjustment of therapy for patients with stable low disease activity;
Add‐on therapy or switching for patients who failed with a systemic treatment;
Long‐term safety data for all the treatments.
1. Future trials need to ensure the following.
Participants: enough information about participants is needed to enable systematic subgroup analyses for biological‐naïve patients (or non‐biological systemic‐agent‐naïve); future trials also need to provide an adequate description of data on other important potential effect modifiers such as previous systemic treatments, whether participants are overweight/obese, the duration of a participant's psoriasis, baseline psoriasis severity (efficacy differences could be expected for patients with PASI at 10 and patients with PASI at 40); race and ethnicity, and presence of psoriatic arthritis.
Interventions: high‐quality trials assessing the efficacy of non‐biological systemic agents are still needed.
Comparators: once the benefit of a treatment has been established against placebo, only head‐to‐head trials would be helpful to provide physicians with efficacy estimates between the different biologics, with stronger evidence than indirect comparisons. Head‐to‐head comparisons are lacking between the non‐biological systemic agents and small molecules and against each other. More head‐to‐head comparisons between biological agents are also needed (anti‐IL17 versus anti‐IL23, anti‐IL23 versus anti‐IL12/23, anti‐TNF alpha versus anti‐IL12/23).
Outcomes: outcome measure harmonisation is needed for psoriasis, as has been done for eczema by the COMET (Core Outcome Measures in Effectiveness Trials) Initiative.
Timingassessment strategy: all of the trials included in this review were limited to the induction phase (from 8 to 24 weeks). Long‐term efficacy data are critical for chronic diseases. Placebo‐controlled long‐term trials would not be ethical, due to the suffering it would entail for the people in the placebo group. However, long‐term studies comparing different drugs would be ethical and informative. Such long‐term trials could also assess the adjustment of therapy for patients with stable cleared psoriasis.
2. New trial designs are needed, such as pragmatic trials that permit dose adjustment once in remission, switching, and additional treatments (i.e. adding two or more systemic treatments) as in normal clinical practice. All of this unmet medical need evidence would improve the management of the condition.
3. Finally, evidence‐based decision‐making and management of chronic plaque psoriasis require both efficacy AND safety data. As we already know, the limitations of network meta‐analysis and of randomised clinical trials (included in these meta‐analyses) mean we cannot reliably interpret the significance of rare events, given their current design. These studies are designed to detect differences in the severity of psoriasis in response to therapy over short periods of treatment, and are often underpowered and of insufficient duration to detect rare or long‐term adverse events. One way to counter this is to include observational cohort studies/registries in a network observational meta‐analysis.
What's new
| Date | Event | Description |
|---|---|---|
| 10 December 2021 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 8 September 2020 are included in the current update (published April 2021, 158 included studies). In addition, the team continues with the monthly screening (last search date 5 October 2021) and have found a further 18 new studies and 31 ongoing studies that will be included in a forthcoming update. |
History
Protocol first published: Issue 2, 2015 Review first published: Issue 12, 2017
| Date | Event | Description |
|---|---|---|
| 28 May 2021 | Amended | There was a mistake in Figure 24 (PASI 90), which we have now rectified. |
| 13 April 2021 | New search has been performed | In this update, we have fully incorporated a further 18 new included studies and 13 new ongoing studies from searches up to 8 September 2020, which have been incorporated in an updated network meta‐analysis. This update includes a new biological agent in the network: mirikizumab. |
| 13 April 2021 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 8 September 2020 are included in the current update (published April 2021, 158 included studies). In addition, the team continues with the monthly screening (last search date 17 March 2021) and have found a further 8 new studies and 15 ongoing studies that will be included in a future update. |
| 13 April 2021 | New citation required and conclusions have changed | This update includes more interventions, including a new anti‐IL23. Network meta‐analysis showed that infliximab, ixekizumab, risankizumab, bimekizumab, secukinumab, guselkumab, and brodalumab outperformed other drugs when compared to placebo in reaching PASI 90. The clinical effectiveness of these drugs was similar, except for ixekizumab which had a better chance of reaching PASI 90 compared with secukinumab, guselkumab and brodalumab. |
| 8 March 2021 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020, 140 included studies). In addition, the team have found a further 18 new included studies and 13 new ongoing studies from searches up to 8 September 2020, to be published in an updated network meta‐analysis. In further searches (up to 20 January 2021) for a future update, the team have found 3 new studies to be included and 14 ongoing studies. |
| 27 January 2021 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020, 140 included studies). In addition, the team have found a further 18 new included studies and 13 new ongoing studies from searches up to 8 September 2020, to be published in an updated network meta‐analysis. In further searches (up to 14 December 2020) for a future update, the team have found 1 new study to be included and 13 ongoing studies. |
| 13 October 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 8 September 2020) and has found a further 15 new studies and 13 new ongoing studies that will be included in the next update which is underway. |
| 3 September 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 22 July 2020) and has found a further 15 new studies and 12 new ongoing studies that will be included in the next update which is underway. |
| 20 July 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 24 June 2020) and has found a further 14 new studies and 12 new ongoing studies that will be included in the next update which is underway. |
| 6 July 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 27 May 2020) and has found a further 14 new studies and 12 new ongoing studies that will be included in the next update which is underway. |
| 17 April 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 10 March 2020) and has found a further 14 new studies and 11 new ongoing studies that will be included in the next update which is underway. |
| 4 March 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 12 February 2020) and has found a further 14 new studies and 7 new ongoing studies that will be included in the next update which is underway. |
| 12 February 2020 | Amended | This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 31 January 2019 are included in the current update (published January 2020). In addition, the team continues with the monthly screening (last search date 15 January 2020) and has found a further 13 new studies and 7 new ongoing studies that will be included in the next update which is underway. |
| 2 January 2020 | New search has been performed | This update included 31 new studies with 11,867 additional participants. We updated the review in line with the MECIR standards. |
| 2 January 2020 | New citation required and conclusions have changed | This update included studies of more interventions, assessing new anti‐IL17 and anti‐IL23 agents. |
Notes
This is a Living Systematic Review. Searches are run and screened monthly. Search results up to 8 September 2020 are included in the current update (published April 2021, 158 included studies). In addition, the team continues with the monthly screening (last search date 5 October 2021) and have found a further 18 new studies and 31 ongoing studies that will be included in a forthcoming update.
Acknowledgements
The Cochrane Skin editorial base wishes to thank Robert Dellavalle, who was the Cochrane Dermatology Editor for this review; a referee from Cochrane's Methods Support Unit who does not want to be acknowledged in the review; the clinical referees, Brandon Adler and Alex G Ortega Loayza; and Kate Cahill who copy‐edited this review.
We would like to thank Dr Ibrahim Yaylali from Cochrane Oral Health for his translation of Gurel 2015 from Turkish into English.
We would like to thank Professors Rintaro Mori and Erika Ota from St Luke's International University, Graduate School of Nursing Science, Tokyo, Japan, for their translation of Rinsho Iyaku 1991 from Japanese into English.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Skin, and was also supported by the Complex Reviews Support Unit, also funded by the National Institute for Health Research (project number 14/178/29).
Department of Health Disclaimer
The views and opinions expressed herein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, the Complex Reviews Support Unit, NIHR, NHS, or the Department of Health.
Appendices
Appendix 1. Cochrane Central Register of Controlled Trials (CENTRAL) via the Cochrane Library, search strategy
#1 MeSH descriptor: [Psoriasis] this term only #2 psoria*:ti,ab,kw #3 (palmoplantar* next pustulosis):ti,ab,kw #4 pustulosis palmaris et plantaris:ti,ab,kw #5 (pustulosis and palms and soles):ti,ab,kw #6 #1 or #2 or #3 or #4 or #5 #7 MeSH descriptor: [Methotrexate] explode all trees #8 MeSH descriptor: [Fumarates] explode all trees #9 MeSH descriptor: [Etretinate] explode all trees #10 MeSH descriptor: [Acitretin] explode all trees #11 MeSH descriptor: [Isotretinoin] explode all trees #12 MeSH descriptor: [Retinoids] explode all trees #13 MeSH descriptor: [Antibodies, Monoclonal] explode all trees #14 MeSH descriptor: [Interleukin‐12] explode all trees #15 MeSH descriptor: [Interleukin‐23] explode all trees #16 MeSH descriptor: [Interleukin‐12 Subunit p40] explode all trees #17 MeSH descriptor: [Tumor Necrosis Factors] explode all trees #18 MeSH descriptor: [Tumor Necrosis Factor‐alpha] explode all trees #19 MeSH descriptor: [Receptors, Tumor Necrosis Factor, Type II] explode all trees #20 MeSH descriptor: [Receptors, Tumor Necrosis Factor] explode all trees #21 MeSH descriptor: [Receptors, Tumor Necrosis Factor, Type I] explode all trees #22 MeSH descriptor: [TNF‐Related Apoptosis‐Inducing Ligand] explode all trees #23 MeSH descriptor: [Antibodies, Monoclonal] explode all trees #24 MeSH descriptor: [Immunoglobulin Fab Fragments] explode all trees #25 MeSH descriptor: [Phototherapy] explode all trees #26 MeSH descriptor: [Ultraviolet Therapy] explode all trees #27 MeSH descriptor: [PUVA Therapy] explode all trees #28 MeSH descriptor: [Photochemotherapy] explode all trees #29 MeSH descriptor: [Cyclosporine] explode all trees #30 (methotrexate* or amethopterin or mtx or mexate or fumar* or dimethylfumarate or fae or dmf or fumaderm or acitretin or tegison or soriatane or neotigason or ((oral or orally or systemic) and retinoid*) or isotretinoin or accutane or etretin* or ustekinumab or stelara or secukinumab or "CNTO 1275" or "cdp571" or etanercept* or enbrel or adalimumab* or "d2e7" or humira or golimumab or simponi or briakinumab or "ABT‐874" or "psoralen uva" or ciclosporin or cyclosporine or cyclosporine or brodalumab or ixekizumab or phototherap* or ultraviolet or PUVA or photochemotherap* or photodynamic or "light therap*" or photoradiation or "broad band uvb" or "broad band ultraviolet b" or "narrow band uvb" or "narrow band ultraviolet b" or BBUVB or NBUVB or BB‐UVB or NB‐UVB or infliximab* or (monoclonal next antibod*) or remicade or interleukin* or "anti tumour necrosis factor" or "anti tumor necrosis factor" or ("tumour necrosis factor" next antibod*) or ("tumor necrosis factor" next antibod*) or "tnf antibod*" or ("tnf alpha" next antibod*) or "anti tnf" or ("immunoglobulin fab" next fragment*) or "p40 subunit" or "tumor necrosis factor*" or tnf or ("antitumor necrosis" next factor*) or ("antitumour necrosis" next factor*) or ampremilast or guselkumab or tofacitinib or certolizumab or tildrakizumab or BMS‐986165 or bimekizumab or rizankizumab or risankizumab or mirikizumab):ti,ab,kw #31 {or #7‐#30} #32 #6 and #31
Searches were date limited by the date a record was added to the database.
Appendix 2. MEDLINE (Ovid) search strategy
1. exp Psoriasis/ or psoria$.ti,ab. 2. palmoplantar$ pustulosis.ti,ab. 3. pustulosis palmaris et plantaris.ti,ab. 4. (pustulosis and palms and soles).ti,ab. 5. 1 or 2 or 3 or 4 6. exp Methotrexate/ 7. methotrexate$.mp. 8. amethopterin.mp. 9. mtx.ti,ab. 10. mexate.mp. 11. exp Fumarates/ 12. (fumar$ and esters).mp. 13. dimethylfumarate.mp. 14. fae.ti,ab. 15. dmf.ti,ab. 16. fumarate$1.mp. 17. fumaderm.mp. 18. Etretinate/ 19. Acitretin/ 20. Tegison.mp. 21. (Soriatane or Neotigason).mp. 22. ((oral or orally or systemic) and retinoid$).ti,ab. 23. Isotretinoin/ 24. Accutane.mp. 25. isotretinoin.ti,ab. 26. etretin$.mp. 27. acitretin.mp. 28. Retinoids/ 29. Ustekinumab.mp. 30. stelara.mp. 31. secukinumab.mp. 32. apremilast.mp. 33. guselkumab.mp. 34. tofacitinib.mp. 35. BMS‐986165.mp. 36. Ri?ankizumab.mp. 37. CNTO 1275.mp. 38. exp antibodies, monoclonal/ 39. monoclonal antibod$.mp. 40. exp Interleukin‐23/ or exp Interleukin‐12/ 41. exp Interleukin‐12 Subunit p40/ or p40 subunit.mp. 42. exp Tumor Necrosis Factors/ or exp Tumor Necrosis Factor‐alpha/ or exp Receptors, Tumor Necrosis Factor, Type II/ or exp Receptors, Tumor Necrosis Factor/ or exp Receptors, Tumor Necrosis Factor, Type I/ or exp TNF‐Related Apoptosis‐Inducing Ligand/ 43. (anti tumour necrosis factor or anti tumor necrosis factor).mp. 44. (tumor necrosis factor‐alpha or tumour necrosis factor‐alpha).mp. 45. anti tnf.mp. 46. (tnf antibod$ or tnf alpha antibod$).mp. 47. (tumour necrosis factor antibod$ or tumor necrosis factor antibod$).mp. 48. (antitumor necrosis factor or antitumour necrosis factor).mp. 49. exp Immunoglobulin Fab Fragments/ 50. (infliximab$ or monoclonal antibody cA2 or remicade).mp. 51. cdp571.mp. 52. (etanercept$ or enbrel).mp. 53. (adalimumab$ or d2e7 or humira).mp. 54. (golimumab or simponi).mp. 55. (Briakinumab or ABT‐874).mp. 56. exp Phototherapy/ 57. exp Ultraviolet Therapy/ 58. exp PUVA Therapy/ 59. exp Photochemotherapy/ 60. photodynamic therap$.mp. 61. phototherap$.mp. 62. photochemotherap$.mp. 63. puva.mp. 64. ultraviolet.mp. 65. light therap$.mp. 66. photoradiation therap$.mp. 67. BBUVB.mp. 68. NBUVB.mp. 69. BB‐UVB.mp. 70. NB‐UVB.mp. 71. broad band uvb.mp. 72. broad band ultraviolet b.mp. 73. narrow band uvb.mp. 74. narrow band ultraviolet b.mp. 75. psoralen ultraviolet a.mp. 76. psoralen uva.mp. 77. Cyclosporine/ 78. (Ciclosporin or cyclosporine or cyclosporin).mp. 79. Bimekizumab.mp. 80. brodalumab.mp. 81. ixekizumab.mp. 82. certolizumab.mp. 83. tildrakizumab.mp. 84. mirikizumab.mp. 85. or/6‐84 86. randomized controlled trial.pt. 87. controlled clinical trial.pt. 88. randomized.ab. 89. placebo.ab. 90. clinical trials as topic.sh. 91. randomly.ab. 92. trial.ti. 93. 86 or 87 or 88 or 89 or 90 or 91 or 92 94. exp animals/ not humans.sh. 95. 93 not 94 96. 5 and 85 and 95
[Lines 86‐95: Cochrane Highly Sensitive Search Strategy for identifying randomized trials in MEDLINE: sensitivity‐ and precision‐maximizing version (2008 revision); Ovid format, from section 3.6.1 in Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M‐I, Noel‐Storr A, Rader T, Shokraneh F, Thomas J, Wieland LS. Technical Supplement to Chapter 4: Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, Welch VA (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 6. Cochrane, 2019. Available from: www.training.cochrane.org/handbook]
We time limited results from this database using two different methods: Results were limited by the Create Date (date when the record was added to the database). Results were also limited by the Entry Date (the date processing of the record was completed). Using two date‐limiting fields and combining the results is recommended by the Cochrane Living Evidence Network. See example search syntax below showing limiting with the Create Date (dt) and the Entry Date (ed):
96. 5 and 85 and 95
97. limit 96 to dt=20181031‐20190416
98. limit 96 to ed=20181031‐20190416
99. 97 or 98
Searches are run monthly with an overlap of three months to ensure no records are missed.
Appendix 3. Embase (Ovid) search strategy
1. exp PSORIASIS/ 2. psoria$.mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] 3. palmoplantar$ pustulosis.mp. 4. pustulosis palmaris et plantaris.mp. 5. (pustulosis and palms and soles).mp. [mp=title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword, floating subheading word, candidate term word] 6. 1 or 2 or 3 or 4 or 5 7. methotrexate/ 8. methotrexate$.ti,ab. 9. amethopterin.ti,ab. 10. mtx.ti,ab. 11. mexate.ti,ab. 12. fumaric acid derivative/ 13. (fumar$ and esters).ti,ab. 14. dimethylfumarate.ti,ab. 15. fae.ti,ab. 16. dmf.ti,ab. 17. fumarate$1.ti,ab. 18. fumaderm.ti,ab. 19. etretinate/ 20. acitretin.ti,ab. 21. tegison.ti,ab. 22. (Soriatane or Neotigason).ti,ab. 23. ((oral or orally or systemic) and retinoid$).ti,ab. 24. isotretinoin/ 25. isotretinoin.ti,ab. 26. Accutane.ti,ab. 27. etretin$.ti,ab. 28. retinoid/ 29. ustekinumab.ti,ab. 30. ustekinumab/ 31. stelara.ti,ab. 32. secukinumab/ 33. secukinumab.ti,ab. 34. ampremilast.ti,ab. 35. guselkumab/ 36. guselkumab.ti,ab. 37. tofacitinib/ 38. tofacitinib.ti,ab. 39. "CNTO 1275".ti,ab. 40. monoclonal antibod$.ti,ab. 41. exp monoclonal antibody/ 42. interleukin 23/ 43. interleukin 12/ 44. interleukin 12p40/ 45. p40 subunit.ti,ab. 46. exp tumor necrosis factor/ 47. tumor necrosis factor alpha/ 48. tumor necrosis factor receptor 2/ 49. tumor necrosis factor receptor/ 50. tumor necrosis factor related apoptosis inducing ligand/ 51. (anti tumour necrosis factor or anti tumor necrosis factor).ti,ab. 52. (tumor necrosis factor‐alpha or tumour necrosis factor‐alpha).ti,ab. 53. anti tnf.ti,ab. 54. (tnf antibod$ or tnf alpha antibod$).ti,ab. 55. (tumour necrosis factor antibod$ or tumor necrosis factor antibod$).ti,ab. 56. (antitumor necrosis factor or antitumour necrosis factor).ti,ab. 57. "immunoglobulin F(ab) fragment"/ 58. (infliximab$ or monoclonal antibody cA2 or remicade).ti,ab. 59. cdp571.ti,ab. 60. (etanercept$ or enbrel).ti,ab. 61. (adalimumab$ or d2e7 or humira).ti,ab. 62. (golimumab or simponi).ti,ab. 63. (Briakinumab or ABT‐874).ti,ab. 64. exp phototherapy/ 65. PUVA/ 66. photochemotherapy/ 67. photodynamic therap$.ti,ab. 68. phototherap$.ti,ab. 69. photochemotherap$.ti,ab. 70. puva.ti,ab. 71. ultraviolet.ti,ab. 72. light therap$.ti,ab. 73. photoradiation therap$.ti,ab. 74. BBUVB.ti,ab. 75. NBUVB.ti,ab. 76. BB‐UVB.ti,ab. 77. NB‐UVB.ti,ab. 78. broad band uvb.ti,ab. 79. broad band ultraviolet b.ti,ab. 80. narrow band uvb.ti,ab. 81. narrow band ultraviolet b.ti,ab. 82. psoralen ultraviolet a.ti,ab. 83. psoralen uva.ti,ab. 84. cyclosporin/ 85. (Ciclosporin or cyclosporine or cyclosporin).ti,ab. 86. brodalumab.ti,ab. 87. ixekizumab.ti,ab. 88. ixekizumab/ 89. brodalumab/ 90. certolizumab.mp. 91. tildrakizumab.mp. 92. BMS‐986165.ti,ab. 93. bimekizumab/ 94. Bimekizumab.ti,ab. 95. risankizumab/ 96. Ri?ankizumab.ti,ab. 97. mirikizumab/ 98. Mirikizumab.ti,ab. 99. or/7‐98 100. crossover procedure.sh. 101. double‐blind procedure.sh. 102. single‐blind procedure.sh. 103. (crossover$ or cross over$).tw. 104. placebo$.tw. 105. (doubl$ adj blind$).tw. 106. allocat$.tw. 107. trial.ti. 108. randomized controlled trial.sh. 109. random$.tw. 110. or/100‐109 111. exp animal/ or exp invertebrate/ or animal experiment/ or animal model/ or animal tissue/ or animal cell/ or nonhuman/ 112. human/ or normal human/ 113. 111 and 112 114. 111 not 113 115. 110 not 114 116. 6 and 99 and 115
[Lines 100‐115: Based on terms suggested for identifying RCTs in Embase (section 3.6.2) in Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M‐I, Noel‐Storr A, Rader T, Shokraneh F, Thomas J, Wieland LS. Technical Supplement to Chapter 4: Searching for and selecting studies. In: Higgins JPT, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, Welch VA (eds). Cochrane Handbook for Systematic Reviews of Interventions Version 6. Cochrane, 2019. Available from: www.training.cochrane.org/handbook]
We time limited results from this database by the Date Delivered field (date the citation XML file is created for delivery to Ovid and has a state=’new’). The Date Delivered field is recommended for date limiting in Embase in the Cochrane Information Specialists’ Handbook, section 6.6 Updating searches. See example search syntax below (dd=date delivered):
116. 6 and 99 and 115
117. limit 116 to dd=20181031‐20190416
Searches are run monthly with an overlap of three months to ensure no records are missed.
Appendix 4. Living systematic review protocol
Living systematic reviews (LSRs) and living network meta‐analyses (Living NMAs) offer a new approach to review updating in which the review is continually updated, incorporating relevant new evidence as it becomes available (Elliott 2017).
The methods outlined below are specific to maintaining this review as a living systematic review on the Cochrane Library. They will be used immediately upon publication of this update. Core review methods, such as the criteria for considering studies in the review and assessment of risk of bias, are unchanged. As such, below we outline only those areas of the Methods for which additional activities or rules apply.
Six methodological steps will be repeated at regular intervals to update the NMA over time: adaptive search for treatments and trials, screening of reports and selection of trials, data extraction, assessment of risk of bias, update of the network of trials and synthesis, and finally dissemination.
1. Adaptive search for treatments and trials
(1) As a living systematic review, we aim to identify all relevant RCTs, regardless of language or publication status (published, unpublished, in press, or in progress).
Bibliographic databasesThe Cochrane Skin Information Specialist (ED) will search the following databases every month:
We will limit the Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library. Searches of this database by the date a record was added to the database.
MEDLINE via Ovid. We will limit Results sets from this database using two different methods: Results will first be limited by the Create Date (date when the record was added to the database). Results will also be limited by the Entry Date (the date processing of the record was completed). Using two date‐limiting fields and combining the results is recommended by the Living Systematic Review Methods Group. See example search syntax below showing limiting with the Create Date (dt) and the Entry Date (ed):
96. 5 and 85 and 95
97. limit 96 to dt=20181031‐20190416
98. limit 96 to ed=20181031‐20190416
99. 97 or 98
Embase via Ovid. We will limit results from this database by the Date Delivered field (date the citation XML file is created for delivery to Ovid and has a state=’new’). The Date Delivered field is recommended for date limiting in Embase in the Cochrane Information Specialists’ Handbook, section 6.6 Updating searches. See example search syntax below (dd=date delivered):
116. 6 and 99 and 115
117. limit 116 to dd=20181031‐20190416
Note that different limit options are proposed for MEDLINE and Embase, because their record fields are different.
For all date‐limiting of bibliographic databases described above, we will apply an overlap of three months with previous searches. This approach is recommended by the Living Systematic Review Methods Group and aims to minimise the risk of missing relevant trials.
The search strategies for these three databases are displayed in Appendix 2 (MEDLINE) and Appendix 3 (Embase). The CENTRAL strategy has been slightly amended and is shown below:
#1 MeSH descriptor: [Psoriasis] this term only #2 psoria*:ti,ab,kw #3 (palmoplantar* next pustulosis):ti,ab,kw #4 pustulosis palmaris et plantaris:ti,ab,kw #5 (pustulosis and palms and soles):ti,ab,kw #6 #1 or #2 or #3 or #4 or #5 #7 MeSH descriptor: [Methotrexate] explode all trees #8 MeSH descriptor: [Fumarates] explode all trees #9 MeSH descriptor: [Etretinate] explode all trees #10 MeSH descriptor: [Acitretin] explode all trees #11 MeSH descriptor: [Isotretinoin] explode all trees #12 MeSH descriptor: [Retinoids] explode all trees #13 MeSH descriptor: [Antibodies, Monoclonal] explode all trees #14 MeSH descriptor: [Interleukin‐12] explode all trees #15 MeSH descriptor: [Interleukin‐23] explode all trees #16 MeSH descriptor: [Interleukin‐12 Subunit p40] explode all trees #17 MeSH descriptor: [Tumor Necrosis Factors] explode all trees #18 MeSH descriptor: [Tumor Necrosis Factor‐alpha] explode all trees #19 MeSH descriptor: [Receptors, Tumor Necrosis Factor, Type II] explode all trees #20 MeSH descriptor: [Receptors, Tumor Necrosis Factor] explode all trees #21 MeSH descriptor: [Receptors, Tumor Necrosis Factor, Type I] explode all trees #22 MeSH descriptor: [TNF‐Related Apoptosis‐Inducing Ligand] explode all trees #23 MeSH descriptor: [Antibodies, Monoclonal] explode all trees #24 MeSH descriptor: [Immunoglobulin Fab Fragments] explode all trees #25 MeSH descriptor: [Phototherapy] explode all trees #26 MeSH descriptor: [Ultraviolet Therapy] explode all trees #27 MeSH descriptor: [PUVA Therapy] explode all trees #28 MeSH descriptor: [Photochemotherapy] explode all trees #29 MeSH descriptor: [Cyclosporine] explode all trees #30 (methotrexate* or amethopterin or mtx or mexate or fumar* or dimethylfumarate or fae or dmf or fumaderm or acitretin or tegison or soriatane or neotigason or ((oral or orally or systemic) and retinoid*) or isotretinoin or accutane or etretin* or ustekinumab or stelara or secukinumab or "CNTO 1275" or "cdp571" or etanercept* or enbrel or adalimumab* or "d2e7" or humira or golimumab or simponi or briakinumab or "ABT‐874" or "psoralen uva" or ciclosporin or cyclosporine or cyclosporine or brodalumab or ixekizumab or phototherap* or ultraviolet or PUVA or photochemotherap* or photodynamic or "light therap*" or photoradiation or "broad band uvb" or "broad band ultraviolet b" or "narrow band uvb" or "narrow band ultraviolet b" or BBUVB or NBUVB or BB‐UVB or NB‐UVB or infliximab* or (monoclonal next antibod*) or remicade or interleukin* or "anti tumour necrosis factor" or "anti tumor necrosis factor" or ("tumour necrosis factor" next antibod*) or ("tumor necrosis factor" next antibod*) or "tnf antibod*" or ("tnf alpha" next antibod*) or "anti tnf" or ("immunoglobulin fab" next fragment*) or "p40 subunit" or "tumor necrosis factor*" or tnf or ("antitumor necrosis" next factor*) or ("antitumour necrosis" next factor*) or ampremilast or guselkumab or tofacitinib or certolizumab or tildrakizumab or BMS‐986165 or bimekizumab or rizankizumab or risankizumab or mirikizumab):ti,ab,kw #31 {or #7‐#30} #32 #6 and #31
Deduplication and preparation the results for primary screening will be performed by the Cochrane Skin Information Specialist (ED)
Trials registers We will search records of RCTs from ClinicalTrials.gov and the WHO’s International Clinical Trials Registry Platform (ICTRP) through CENTRAL, which now includes trial records from these resources. Records are added to CENTRAL on a monthly basis (see relevant sections of ‘How CENTRAL is created’). CENTRAL therefore has a short lag period behind the individual registries.
Unpublished literature
We will search reviews submitted to the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for drug registration (using www.accessdata.fda.gov/scripts/cder/drugsatfda and www.ema.europa.eu/ema) yearly.
Review of search methods We will review search methods and strategies approximately yearly, ensuring they reflect any terminology changes in the topic area or in the databases searched. We will also revisit yearly our serach methods, and if necessary update the search strategies by adding or removing intervention terms.
(2) As a living systematic review, we aim to continually identify new evidence for interventions already in the network of trials but also for novel interventions. Indeed, for the 2019 review update, we identified several new interventions in the ongoing trials section that were not part of the initial network (e.g. risankizumab). To provide an update and useful network of interventions for physicians, we need first to identify new interventions but also, to drop old interventions, which are no longer of interest.
To achieve these goals:
(1) We will create a research community in psoriasis, including international experts in the field who will help to provide information of new 'eligible' drugs.
Once a year, a list of all systemic drugs used for psoriasis will be proposed by the scientific steering committee to the international experts’ group, including:
Drugs already involved in the network
Marketed drugs, which will be identified using the U.S. FDA and the EMA websites (www.accessdata.fda.gov/scripts/cder/drugsatfda and www.ema.europa.eu/ema, respectively).
Drugs under development, which will be identified using the World Health Organization International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/) and ISRCTN registry (www.isrctn.com).
The international experts’ group will select from this list all the systemic drugs needed for the future network. They will also add new interventions not proposed in the list. They will provide a rationale for all proposed network changes (adding or removing interventions). The international experts’ group is necessary also to determine which drugs have to be deleted from the network, with clinical practice and market authorisation being different in each country.
It will be sufficient to update the interventions network once a year, as we will include phase II and III RCTs. Indeed, the timing between the phase I and the phase II/III for a promising intervention is over one year.
(2) At the same time, we will search the different data sources described for the initial NMA with the latest updated search strategy. The Cochrane Skin Group will perform the electronic search.
2.1. Every month, we will re‐run the search from the date of the last iteration to the following one (covering a 1‐month interval), on an automated basis, for electronic searches, trial registries and conference proceedings. We will use a script file (html extraction by automated http requests) to automatically and simultaneously search multiple sources every month. We will manually screen the reference lists of any newly‐included studies and identified systematic reviews.
2.2. Every year, two authors (ES, LLC) will check other sources (regulatory agencies and industry trial registries) on a manual basis. We will also update the search strategy by adding or removing interventions. We will also review search methods and strategies approximately yearly, to ensure they reflect any terminology changes in the topic area, or in the databases.
As additional steps to inform the living systematic review, one author (ES) contacts corresponding authors of ongoing studies as they are identified and asks them to advise when results are available, or to share early or unpublished data.
2 Screening of reports and selection of trials
We will immediately screen any new citations retrieved by the monthly searches. We will pay attention to duplicate studies, i.e. the same trial reported in several articles. We will consider using Cochrane’s Screen4Me workflow to help assess the search results, depending on the volume of search results we identify in the first few months. Screen4Me comprises three components: known assessments – a service that matches records in the search results to records that have already been screened in Cochrane Crowd and been labelled as 'an RCT' or as 'Not an RCT'; the RCTclassifier – a machine learning model that distinguishes RCTs from non‐RCTs; and if appropriate, CochraneCrowd (crowd.cochrane.org) – Cochrane’s citizen science platform where the Crowd help to identify and describe health evidence.
Selection process will then be done through Covidence (Covidence 2019), a web tool allowing a double selection on title, abstract and then full text by independent reviewers.
3 Data synthesis
Whenever we find new evidence (i.e. studies, data or information) meeting the review inclusion criteria, we will extract the data and assess risks of bias. For trials identified as completed in clinical trial registries but without posted results or those identified only by a conference proceeding, and for missing outcome data, trained reviewers will contact trialists to request complete results.
Every three months, we will incorporate each newly‐identified trial in the network. We will perform one network for each outcome (PASI‐90, SAEs, PASI‐75, PGA, QoL and AEs). We will re‐analyse the data every three months using the standard approaches outlined in the Data synthesis section as well as the GRADE process.
4 Dissemination
The general principle is that an update is published on the Cochrane Library with an open access each time new findings that impact on review conclusions have been identified.
We will present the results with sufficient information so that the live cumulative NMA becomes a useful tool to help medical decision‐making, taking into account the safety and efficacy of all systemic treatments for chronic plaque psoriasis. The live cumulative NMA will also provide evidence for future guidelines (and updates) on moderate‐to‐severe psoriasis treatment in France but also in Europe (European Dermatology Guidelines) and world‐wide.
We will present :
Network graphs for each outcome and at each iteration how the networks of evidence evolves over time
Treatment effects in forest plots, league tables and reporting of treatment rankings
Assessments of NMA assumptions and risks of bias for each included trial, to allow readers to assess their level of confidence in the results
Characteristics and results of included trials, to allow for an evaluation of clinical diversity and transitivity.
We will make publicly available in open access to ensure a transparent process:
The protocol (and its amendments)
Statistical programmes
The screening and selection elements (flow diagram, list of included trials, list of excluded trials with reasons for exclusion)
Data and analyses
Comparison 1. Primary outcome ‐ PASI 90.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Non‐biological treatments versus placebo | 4 | 1022 | Risk Ratio (M‐H, Random, 95% CI) | 2.82 [1.02, 7.78] |
| 1.1.1 Methotrexate versus placebo | 3 | 318 | Risk Ratio (M‐H, Random, 95% CI) | 2.06 [0.53, 7.97] |
| 1.1.2 Fumaric acid esters versus placebo | 1 | 704 | Risk Ratio (M‐H, Random, 95% CI) | 4.47 [2.01, 9.95] |
| 1.2 Non‐biological treatment 1 versus non‐biological treatment 2 | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.2.1 Ciclosporin versus methotrexate | 2 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.47, 2.98] |
| 1.2.2 Methotrexate versus fumaric acid esters | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 3.82 [1.65, 8.85] |
| 1.3 Anti‐TNF alpha versus placebo | 32 | 11869 | Risk Ratio (M‐H, Random, 95% CI) | 13.65 [10.71, 17.40] |
| 1.3.1 Etanercept versus placebo | 14 | 5650 | Risk Ratio (M‐H, Random, 95% CI) | 11.68 [8.14, 16.75] |
| 1.3.2 Adalimumab versus placebo | 9 | 3421 | Risk Ratio (M‐H, Random, 95% CI) | 13.13 [8.01, 21.53] |
| 1.3.3 Certolizumab versus placebo | 5 | 1153 | Risk Ratio (M‐H, Random, 95% CI) | 19.77 [8.29, 47.12] |
| 1.3.4 Infliximab versus placebo | 5 | 1645 | Risk Ratio (M‐H, Random, 95% CI) | 27.71 [12.52, 61.30] |
| 1.4 Anti‐IL12/23 versus placebo | 10 | 4274 | Risk Ratio (M‐H, Random, 95% CI) | 19.77 [13.25, 29.52] |
| 1.4.1 Ustekinumab versus placebo | 10 | 4274 | Risk Ratio (M‐H, Random, 95% CI) | 19.77 [13.25, 29.52] |
| 1.5 Anti‐IL17 versus placebo | 22 | 11462 | Risk Ratio (M‐H, Random, 95% CI) | 30.68 [22.96, 41.00] |
| 1.5.1 Secukinumab versus placebo | 12 | 3835 | Risk Ratio (M‐H, Random, 95% CI) | 31.46 [19.46, 50.86] |
| 1.5.2 Ixekizumab versus placebo | 4 | 3268 | Risk Ratio (M‐H, Random, 95% CI) | 53.85 [15.34, 189.07] |
| 1.5.3 Brodalumab versus placebo | 5 | 4109 | Risk Ratio (M‐H, Random, 95% CI) | 26.33 [16.77, 41.33] |
| 1.5.4 Bimekizumab versus placebo | 1 | 250 | Risk Ratio (M‐H, Random, 95% CI) | 58.64 [3.72, 923.86] |
| 1.6 Anti‐IL23 versus placebo | 14 | 5881 | Risk Ratio (M‐H, Random, 95% CI) | 20.23 [14.76, 27.73] |
| 1.6.1 Guselkumab versus placebo | 5 | 1767 | Risk Ratio (M‐H, Random, 95% CI) | 27.79 [16.23, 47.60] |
| 1.6.2 Tildrakizumab versus placebo | 3 | 1903 | Risk Ratio (M‐H, Random, 95% CI) | 17.26 [8.27, 36.05] |
| 1.6.3 Risankizumab versus placebo | 4 | 1476 | Risk Ratio (M‐H, Random, 95% CI) | 24.00 [13.04, 44.18] |
| 1.6.4 Mirikizumab versus placebo | 2 | 735 | Risk Ratio (M‐H, Random, 95% CI) | 14.29 [3.30, 61.98] |
| 1.7 Biologic versus non‐biological treatment | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.7.1 Etanercept versus acitretin | 2 | 102 | Risk Ratio (M‐H, Random, 95% CI) | 4.56 [0.81, 25.79] |
| 1.7.2 Infliximab versus methotrexate | 1 | 868 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [2.15, 3.80] |
| 1.7.3 Adalimumab versus methotrexate | 1 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 3.73 [2.25, 6.19] |
| 1.7.4 Secukinumab versus fumaric acid esters | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 8.31 [4.23, 16.35] |
| 1.7.5 Ixekizumab versus fumaric acid esters | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 8.60 [3.69, 20.04] |
| 1.7.6 Ixekizumab versus methotrexate | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 2.05 [1.43, 2.94] |
| 1.7.7 Guselkumab versus fumaric ester acids | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 6.02 [3.13, 11.60] |
| 1.7.8 Risankizumab versus fumaric ester acids | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 8.33 [3.87, 17.95] |
| 1.7.9 Brodalumab versus fumaric acid esters | 1 | 210 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [2.04, 4.42] |
| 1.8 Biologic 1 versus biologic 2 | 22 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.8.1 Ustekinumab versus etanercept | 1 | 903 | Risk Ratio (M‐H, Random, 95% CI) | 1.80 [1.45, 2.24] |
| 1.8.2 Secukinumab versus etanercept | 1 | 980 | Risk Ratio (M‐H, Random, 95% CI) | 2.32 [1.85, 2.92] |
| 1.8.3 Inliximab versus etanercept | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 9.20 [1.28, 66.37] |
| 1.8.4 Ixekizumab versus etanercept | 2 | 2209 | Risk Ratio (M‐H, Random, 95% CI) | 2.98 [2.24, 3.98] |
| 1.8.5 Tildrakizumab versus etanercept | 1 | 934 | Risk Ratio (M‐H, Random, 95% CI) | 1.76 [1.39, 2.23] |
| 1.8.6 Certolizumab versus etanercept | 1 | 502 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.90, 1.61] |
| 1.8.7 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.30, 1.50] |
| 1.8.8 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.41, 2.12] |
| 1.8.9 Brodalumab versus ustekinumab | 2 | 3088 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.16, 1.39] |
| 1.8.10 Risankizumab versus ustekinumab | 3 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [1.43, 1.93] |
| 1.8.11 Guselkumab versus adalimumab | 3 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [1.26, 1.62] |
| 1.8.12 Risankizumab versus adalimumab | 1 | 605 | Risk Ratio (M‐H, Random, 95% CI) | 1.53 [1.33, 1.75] |
| 1.8.13 Secukinumab versus guselkumab | 1 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.02, 1.19] |
| 1.8.14 Ixekizumab versus guselkumab | 1 | 1027 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.18, 1.42] |
| 1.8.15 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.97, 1.30] |
| 1.9 Small molecules versus placebo | 11 | 5388 | Risk Ratio (M‐H, Random, 95% CI) | 7.09 [5.05, 9.95] |
| 1.9.1 Apremilast versus placebo | 5 | 2029 | Risk Ratio (M‐H, Random, 95% CI) | 6.94 [3.37, 14.30] |
| 1.9.2 Tofacitinib versus placebo | 5 | 3092 | Risk Ratio (M‐H, Random, 95% CI) | 7.81 [4.54, 13.46] |
| 1.9.3 TYK2 versus placebo | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 13.99 [1.99, 98.10] |
| 1.10 Biologic versus small molecules | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.10.1 Etanercept versus tofacitinib | 1 | 998 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.93, 1.38] |
| 1.10.2 Etanercept versus apremilast | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.72, 2.78] |
Comparison 2. Primary outcome ‐ serious adverse events (SAE).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Non‐biological treatments versus placebo | 4 | 1023 | Risk Ratio (M‐H, Random, 95% CI) | 0.39 [0.09, 1.70] |
| 2.1.1 Methotrexate versus placebo | 3 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 0.16 [0.03, 0.88] |
| 2.1.2 Fumaric acid esters versus placebo | 1 | 704 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.31, 2.21] |
| 2.2 Non‐biological treatment 1 versus non‐biological treatment 2 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.2.1 Methotrexate versus fumaric ester acids | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.10] |
| 2.3 Anti‐TNF alpha versus placebo | 32 | 10454 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.77, 1.49] |
| 2.3.1 Etanercept versus placebo | 13 | 4265 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.53, 1.60] |
| 2.3.2 Adalimumab versus placebo | 10 | 3485 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.72, 1.84] |
| 2.3.3 Certolizumab versus placebo | 4 | 1026 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.19, 7.50] |
| 2.3.4 Infliximab versus placebo | 6 | 1678 | Risk Ratio (M‐H, Random, 95% CI) | 1.99 [0.82, 4.78] |
| 2.4 Anti‐IL12/23 versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.59, 1.54] |
| 2.4.1 Ustekinumab versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.59, 1.54] |
| 2.5 Anti‐IL17 versus placebo | 21 | 10987 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.72, 1.36] |
| 2.5.1 Secukinumab versus placebo | 11 | 3360 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.59, 1.66] |
| 2.5.2 Ixekizumab versus placebo | 4 | 3268 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.63, 2.13] |
| 2.5.3 Brodalumab versus placebo | 5 | 4109 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.52, 1.61] |
| 2.5.4 Bimekizumab versus placebo | 1 | 250 | Risk Ratio (M‐H, Random, 95% CI) | 0.20 [0.01, 3.16] |
| 2.6 Anti‐IL23 versus placebo | 14 | 5882 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.50, 1.16] |
| 2.6.1 Guselkumab versus placebo | 5 | 1767 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.50, 2.28] |
| 2.6.2 Tildrakizumab versus placebo | 3 | 1904 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.37, 2.77] |
| 2.6.3 Risankizumab versus placebo | 4 | 1476 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.24, 2.10] |
| 2.6.4 Mirikizumab versus placebo | 2 | 735 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.17, 2.48] |
| 2.7 Biologic versus non‐biological treatments | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.7.1 Etanercept versus acitretin | 3 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.30 [0.01, 7.02] |
| 2.7.2 Infliximab versus methotrexate | 1 | 868 | Risk Ratio (M‐H, Random, 95% CI) | 2.41 [1.04, 5.59] |
| 2.7.3 Adalimumab versus methotrexate | 1 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 2.04 [0.19, 22.14] |
| 2.7.4 Secukinumab versus fumaric acid esters | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.53 [0.16, 1.75] |
| 2.7.5 Ixekizumab versus fumaric ester acids | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.10] |
| 2.7.6 Ixekizumab versus methotrexate | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.06, 15.58] |
| 2.7.7 Guselkumab versus fumaric ester acids | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [0.26, 8.51] |
| 2.7.8 Risankizumab versus fumaric ester acids | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.50 [0.05, 5.37] |
| 2.7.9 Brodalumab versus fumaric acid esters | 1 | 300 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.32, 28.52] |
| 2.8 Biologic 1 versus biologic 2 | 21 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.8.1 Ustekinumab versus etanercept | 1 | 903 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.38, 4.11] |
| 2.8.2 Secukinumab versus etanercept | 1 | 980 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.41, 2.82] |
| 2.8.3 Infliximab versus etanercept | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.06, 13.87] |
| 2.8.4 Ixekizumab versus etanercept | 2 | 2209 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.55, 2.06] |
| 2.8.5 Tildrakizumab versus etanercept | 1 | 934 | Risk Ratio (M‐H, Random, 95% CI) | 0.72 [0.28, 1.87] |
| 2.8.6 Certolizumab versus etanercept | 1 | 502 | Risk Ratio (M‐H, Random, 95% CI) | 2.56 [0.30, 21.74] |
| 2.8.7 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.70, 2.30] |
| 2.8.8 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 6.09 [0.30, 125.89] |
| 2.8.9 Brodalumab versus ustekinumab | 2 | 3088 | Risk Ratio (M‐H, Random, 95% CI) | 1.51 [0.64, 3.56] |
| 2.8.10 Risankizumab versus ustekinumab | 3 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.24, 1.32] |
| 2.8.11 Guselkumab versus adalimumab | 3 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.45, 1.84] |
| 2.8.12 Risankizumab versus adalimumab | 1 | 605 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.46, 2.72] |
| 2.8.13 Ixekizumab versus guselkumab | 1 | 1027 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.58, 2.47] |
| 2.8.14 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.54, 4.09] |
| 2.9 Small molecules versus placebo | 15 | 5982 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.61, 1.43] |
| 2.9.1 Apremilast versus placebo | 7 | 2593 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.48, 1.52] |
| 2.9.2 Tofacitinib versus placebo | 7 | 3122 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.57, 2.11] |
| 2.9.3 TYK2 versus placebo | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 0.61 [0.06, 5.71] |
| 2.10 Biologic versus small molecules | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 2.10.1 Etanercept versus tofacitinib | 1 | 998 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.46, 2.89] |
| 2.10.2 Etanercept versus apremilast | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 0.33 [0.04, 3.14] |
Comparison 3. Secondary outcome ‐ PASI 75.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Non‐biological treatments versus placebo | 4 | 1025 | Risk Ratio (M‐H, Random, 95% CI) | 2.42 [1.74, 3.35] |
| 3.1.1 Methotrexate versus placebo | 2 | 283 | Risk Ratio (M‐H, Random, 95% CI) | 2.36 [1.19, 4.68] |
| 3.1.2 Fumaric acid esters versus placebo | 1 | 704 | Risk Ratio (M‐H, Random, 95% CI) | 2.56 [1.68, 3.89] |
| 3.1.3 Acitretin versus placebo | 1 | 38 | Risk Ratio (M‐H, Random, 95% CI) | 1.85 [0.23, 14.80] |
| 3.2 Non‐biological treatment 1 versus non‐biological treatment 2 | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.2.1 Ciclosporin versus methotrexate | 2 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.84, 2.23] |
| 3.2.2 Methotrexate versus fumaric acid esters | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 2.30 [0.74, 7.19] |
| 3.3 Anti‐TNF alpha versus placebo | 35 | 12078 | Risk Ratio (M‐H, Random, 95% CI) | 9.21 [7.78, 10.91] |
| 3.3.1 Etanercept versus placebo | 15 | 5762 | Risk Ratio (M‐H, Random, 95% CI) | 8.56 [7.07, 10.36] |
| 3.3.2 Adalimumab versus placebo | 10 | 3485 | Risk Ratio (M‐H, Random, 95% CI) | 8.25 [6.03, 11.29] |
| 3.3.3 Certolizumab versus placebo | 5 | 1153 | Risk Ratio (M‐H, Random, 95% CI) | 9.55 [6.13, 14.88] |
| 3.3.4 Infliximab versus placebo | 6 | 1678 | Risk Ratio (M‐H, Random, 95% CI) | 18.87 [8.53, 41.75] |
| 3.4 Anti‐IL12/23 versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 11.52 [8.75, 15.17] |
| 3.4.1 Ustekinumab versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 11.52 [8.75, 15.17] |
| 3.5 Anti‐IL17 versus placebo | 21 | 11380 | Risk Ratio (M‐H, Random, 95% CI) | 15.52 [12.41, 19.42] |
| 3.5.1 Secukinumab versus placebo | 11 | 3753 | Risk Ratio (M‐H, Random, 95% CI) | 16.78 [12.20, 23.08] |
| 3.5.2 Ixekizumab versus placebo | 4 | 3268 | Risk Ratio (M‐H, Random, 95% CI) | 17.44 [10.45, 29.10] |
| 3.5.3 Brodalumab versus placebo | 5 | 4109 | Risk Ratio (M‐H, Random, 95% CI) | 12.80 [8.46, 19.36] |
| 3.5.4 Bimekizumab versus placebo | 1 | 250 | Risk Ratio (M‐H, Random, 95% CI) | 17.06 [4.41, 66.09] |
| 3.6 Anti‐IL23 versus placebo | 14 | 5882 | Risk Ratio (M‐H, Random, 95% CI) | 11.60 [9.56, 14.06] |
| 3.6.1 Guselkumab versus placebo | 5 | 1767 | Risk Ratio (M‐H, Random, 95% CI) | 12.65 [9.24, 17.31] |
| 3.6.2 Tildrakizumab versus placebo | 3 | 1904 | Risk Ratio (M‐H, Random, 95% CI) | 11.24 [7.33, 17.23] |
| 3.6.3 Risankizumab versus placebo | 4 | 1476 | Risk Ratio (M‐H, Random, 95% CI) | 11.36 [7.95, 16.21] |
| 3.6.4 Mirikizumab versus placebo | 2 | 735 | Risk Ratio (M‐H, Random, 95% CI) | 9.87 [5.74, 16.98] |
| 3.7 Biologic versus non‐biological treatments | 10 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.7.1 Etanercept versus acitretin | 3 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 1.98 [1.26, 3.12] |
| 3.7.2 Infliximab versus methotrexate | 1 | 868 | Risk Ratio (M‐H, Random, 95% CI) | 1.86 [1.58, 2.19] |
| 3.7.3 Adalimumab versus methotrexate | 1 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 2.25 [1.72, 2.94] |
| 3.7.4 Secukinumab versus fumaric acid esters | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 3.30 [2.36, 4.62] |
| 3.7.5 Ixekizumab versus fumaric ester acids | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 4.08 [2.46, 6.77] |
| 3.7.6 Ixekizumab versus methotrexate | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.06, 1.56] |
| 3.7.7 Guselkumab versus fumaric acid esters | 1 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 3.26 [2.13, 4.99] |
| 3.7.8 Risankizumab versus fumaric acid esters | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 2.95 [2.06, 4.23] |
| 3.7.9 Brodalumab versus fumaric acid esters | 1 | 210 | Risk Ratio (M‐H, Random, 95% CI) | 2.12 [1.64, 2.76] |
| 3.8 Biologic 1 versus biologic 2 | 21 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.8.1 Ustekinumab versus etanercept | 1 | 903 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.13, 1.40] |
| 3.8.2 Secukinumab versus etanercept | 1 | 980 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [1.44, 1.88] |
| 3.8.3 Infliximab versus etanercept | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 2.07 [1.12, 3.81] |
| 3.8.4 Ixekizumab versus etanercept | 2 | 2209 | Risk Ratio (M‐H, Random, 95% CI) | 1.79 [1.43, 2.24] |
| 3.8.5 Tildrakizumab versus etanercept | 1 | 934 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.16, 1.50] |
| 3.8.6 Certolizumab versus etanercept | 1 | 502 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [1.01, 1.40] |
| 3.8.7 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.10, 1.19] |
| 3.8.8 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.09, 1.41] |
| 3.8.9 Brodalumab versus ustekinumab | 2 | 3088 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.04, 1.17] |
| 3.8.10 Risankizumab versus ustekinumab | 3 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.13, 1.33] |
| 3.8.11 Guselkumab versus adalimumab | 3 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.14, 1.32] |
| 3.8.12 Risankizumab versus adalimumab | 1 | 605 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.17, 1.37] |
| 3.8.13 Secukinumab versus guselkumab | 1 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.99, 1.07] |
| 3.8.14 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.05, 1.26] |
| 3.9 Small molecules versus placebo | 14 | 5679 | Risk Ratio (M‐H, Random, 95% CI) | 4.96 [3.77, 6.51] |
| 3.9.1 Apremilast versus placebo | 6 | 2290 | Risk Ratio (M‐H, Random, 95% CI) | 3.86 [2.59, 5.74] |
| 3.9.2 Tofacitinib versus placebo | 7 | 3122 | Risk Ratio (M‐H, Random, 95% CI) | 6.14 [4.31, 8.73] |
| 3.9.3 TYK2 versus placebo | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 7.77 [2.59, 23.36] |
| 3.10 Biologic versus small molecules | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.10.1 Etanercept versus tofacitinib | 1 | 998 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.02, 1.28] |
| 3.10.2 Etanercept versus apremilast | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.86, 1.71] |
Comparison 4. Secondary outcome ‐ PGA 0/1.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Non‐biological treatment versus placebo | 4 | 1023 | Risk Ratio (M‐H, Random, 95% CI) | 2.87 [1.97, 4.18] |
| 4.1.1 Methotrexate versus placebo | 3 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 3.19 [1.66, 6.16] |
| 4.1.2 Fumaric acid esters versus placebo | 1 | 704 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [1.72, 4.32] |
| 4.2 Non‐biological treatment 1 versus non‐biological treatment 2 | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.2.1 Ciclosporin versus methotrexate | 1 | 88 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.47, 1.46] |
| 4.2.2 Methotrexate versus fumaric acid esters | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 3.86 [1.84, 8.09] |
| 4.3 Anti‐TNF alpha versus placebo | 29 | 10194 | Risk Ratio (M‐H, Random, 95% CI) | 8.89 [7.36, 10.74] |
| 4.3.1 Etanercept versus placebo | 13 | 5030 | Risk Ratio (M‐H, Random, 95% CI) | 8.11 [6.35, 10.37] |
| 4.3.2 Adalimumab versus placebo | 9 | 3337 | Risk Ratio (M‐H, Random, 95% CI) | 7.89 [6.13, 10.16] |
| 4.3.3 Certolizumab versus placebo | 5 | 1266 | Risk Ratio (M‐H, Random, 95% CI) | 27.86 [12.17, 63.79] |
| 4.3.4 Infliximab versus placebo | 3 | 561 | Risk Ratio (M‐H, Random, 95% CI) | 13.11 [6.69, 25.69] |
| 4.4 Anti‐IL12/23 versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 10.69 [7.63, 14.98] |
| 4.4.1 Ustekinumab versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 10.69 [7.63, 14.98] |
| 4.5 Anti‐IL17 versus placebo | 19 | 11082 | Risk Ratio (M‐H, Random, 95% CI) | 19.01 [14.65, 24.67] |
| 4.5.1 Secukinumab versus placebo | 9 | 3455 | Risk Ratio (M‐H, Random, 95% CI) | 21.03 [11.53, 38.33] |
| 4.5.2 Ixekizumab versus placebo | 4 | 3268 | Risk Ratio (M‐H, Random, 95% CI) | 17.46 [9.87, 30.90] |
| 4.5.3 Brodalumab versus placebo | 5 | 4109 | Risk Ratio (M‐H, Random, 95% CI) | 18.78 [13.29, 26.55] |
| 4.5.4 Bimekizumab versus placebo | 1 | 250 | Risk Ratio (M‐H, Random, 95% CI) | 15.35 [3.96, 59.49] |
| 4.6 Anti‐IL23 versus placebo | 14 | 5882 | Risk Ratio (M‐H, Random, 95% CI) | 11.01 [9.06, 13.38] |
| 4.6.1 Guselkumab versus placebo | 5 | 1767 | Risk Ratio (M‐H, Random, 95% CI) | 10.87 [8.11, 14.57] |
| 4.6.2 Tildrakizumab versus placebo | 3 | 1904 | Risk Ratio (M‐H, Random, 95% CI) | 10.26 [6.62, 15.91] |
| 4.6.3 Risankizumab versus placebo | 4 | 1476 | Risk Ratio (M‐H, Random, 95% CI) | 11.50 [7.95, 16.66] |
| 4.6.4 Mirikizumab versus placebo | 2 | 735 | Risk Ratio (M‐H, Random, 95% CI) | 12.26 [5.88, 25.56] |
| 4.7 Biologic versus non‐biological treatments | 8 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.7.1 Infliximab versus methotrexate | 1 | 868 | Risk Ratio (M‐H, Random, 95% CI) | 1.99 [1.67, 2.37] |
| 4.7.2 Adalimumab versus methotrexate | 1 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 2.44 [1.79, 3.32] |
| 4.7.3 Secukinumab versus fumaric acid esters | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 6.16 [3.59, 10.57] |
| 4.7.4 Etanercept versus acitretin | 2 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 4.98 [1.15, 21.49] |
| 4.7.5 Ixekizumab versus fumaric acid esters | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 6.43 [3.19, 12.96] |
| 4.7.6 Ixekizumab versus methotrexate | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [1.24, 2.23] |
| 4.7.7 Risankizumab versus fumaric acid esters | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 2.43 [1.75, 3.38] |
| 4.7.8 Brodalumab versus fumaric acid esters | 1 | 210 | Risk Ratio (M‐H, Random, 95% CI) | 3.24 [2.15, 4.87] |
| 4.8 Biologic 1 versus biologic 2 | 21 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.8.1 Ustekinumab versus etanercept | 1 | 903 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.24, 1.58] |
| 4.8.2 Secukinumab versus etanercept | 1 | 980 | Risk Ratio (M‐H, Random, 95% CI) | 2.09 [1.73, 2.53] |
| 4.8.3 Infliximab versus etanercept | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [1.30, 4.81] |
| 4.8.4 Ixekizumab versus etanercept | 2 | 2209 | Risk Ratio (M‐H, Random, 95% CI) | 2.01 [1.74, 2.31] |
| 4.8.5 Tildrakizumab versus etanercept | 1 | 934 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.05, 1.37] |
| 4.8.6 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.19, 1.38] |
| 4.8.7 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [1.24, 1.68] |
| 4.8.8 Brodalumab versus ustekinumab | 2 | 3088 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.07, 1.27] |
| 4.8.9 Risankizumab versus ustekinumab | 3 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.23, 1.52] |
| 4.8.10 Guselkumab versus adalimumab | 3 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.19, 1.34] |
| 4.8.11 Risankizumab versus adalimumab | 1 | 605 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [1.25, 1.54] |
| 4.8.12 Secukinumab versus guselkumab | 1 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.95, 1.05] |
| 4.8.13 Ixekizumab versus guselkumab | 1 | 1027 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [1.21, 1.46] |
| 4.8.14 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.10, 1.37] |
| 4.9 Small molecules versus placebo | 13 | 5704 | Risk Ratio (M‐H, Random, 95% CI) | 3.92 [3.17, 4.84] |
| 4.9.1 Apremilast versus placebo | 6 | 2333 | Risk Ratio (M‐H, Random, 95% CI) | 3.52 [2.40, 5.16] |
| 4.9.2 Tofacitinib versus placebo | 6 | 3104 | Risk Ratio (M‐H, Random, 95% CI) | 4.17 [3.37, 5.17] |
| 4.9.3 TYK2 versus placebo | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 8.24 [2.74, 24.76] |
| 4.10 Biologic versus small molecules | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 4.10.1 Etanercept versus tofacitinib | 1 | 998 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.04, 1.27] |
| 4.10.2 Etanercept versus apremilast | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [0.78, 2.27] |
Comparison 5. Secondary outcome ‐ quality of life.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Non‐biological treatments versus placebo | 2 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.40, 0.06] |
| 5.1.1 Methotrexate versus placebo | 2 | 283 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.40, 0.06] |
| 5.2 Non‐biological treatment 1 versus non‐biological treatment 2 | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.2.1 Methotrexate versus fumaric acid esters | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | ‐7.44 [‐9.47, ‐5.41] |
| 5.3 Anti‐TNF alpha versus placebo | 25 | 8534 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.19, ‐0.97] |
| 5.3.1 Etanercept versus placebo | 8 | 3246 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.11 [‐1.34, ‐0.88] |
| 5.3.2 Adalimumab versus placebo | 9 | 3055 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.98 [‐1.11, ‐0.85] |
| 5.3.3 Certolizumab versus placebo | 3 | 588 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.00 [‐1.26, ‐0.74] |
| 5.3.4 Infliximab versus placebo | 5 | 1645 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.29 [‐1.48, ‐1.10] |
| 5.4 Ustekinumab versus placebo | 9 | 3359 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.35 [‐1.54, ‐1.16] |
| 5.5 Anti‐IL17 versus placebo | 6 | 3566 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐1.80, ‐1.13] |
| 5.5.1 Ixekizumab versus placebo | 3 | 3126 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.76 [‐2.09, ‐1.43] |
| 5.5.2 Brodalumab versus placebo | 2 | 349 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.44, ‐0.47] |
| 5.5.3 Secukinumab versus placebo | 1 | 91 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.41 [‐1.87, ‐0.94] |
| 5.6 Anti‐IL23 versus placebo | 8 | 4146 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.46 [‐1.62, ‐1.30] |
| 5.6.1 Guselkumab versus placebo | 3 | 1444 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐1.54, ‐1.18] |
| 5.6.2 Tildrakizumab versus placebo | 3 | 1904 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.36 [‐1.48, ‐1.23] |
| 5.6.3 Risankizumab versus placebo | 2 | 798 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.82 [‐2.04, ‐1.60] |
| 5.7 Biologic versus non‐biological treatment | 5 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.7.1 Adalimumab versus methotrexate | 1 | 218 | Mean Difference (IV, Fixed, 95% CI) | ‐3.40 [‐5.75, ‐1.05] |
| 5.7.2 Ixekizumab versus fumaric acid esters | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | ‐7.71 [‐9.74, ‐5.68] |
| 5.7.3 Ixekizumab versus methotrexate | 1 | 108 | Mean Difference (IV, Fixed, 95% CI) | ‐0.27 [‐2.31, 1.77] |
| 5.7.4 Guselkumab versus fumaric acid esters | 1 | 119 | Mean Difference (IV, Fixed, 95% CI) | ‐5.80 [‐8.06, ‐3.54] |
| 5.7.5 Risankizumab versus fumaric acid esters | 1 | 120 | Mean Difference (IV, Fixed, 95% CI) | ‐7.60 [‐9.97, ‐5.23] |
| 5.7.6 Brodalumab versus fumaric acid esters | 1 | 210 | Mean Difference (IV, Fixed, 95% CI) | ‐2.57 [‐4.27, ‐0.87] |
| 5.8 Biologic 1 versus biologic 2 | 8 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 5.8.1 Ixekizumab versus etanercept | 2 | 2209 | Mean Difference (IV, Fixed, 95% CI) | ‐1.99 [‐2.39, ‐1.59] |
| 5.8.2 Guselkumab versus adalimumab | 2 | 1407 | Mean Difference (IV, Fixed, 95% CI) | ‐1.73 [‐2.50, ‐0.97] |
| 5.8.3 Risankizumab versus ustekinumab | 2 | 799 | Mean Difference (IV, Fixed, 95% CI) | ‐1.00 [‐1.50, ‐0.50] |
| 5.8.4 Tildrakizumab versus etanercept | 1 | 932 | Mean Difference (IV, Fixed, 95% CI) | ‐1.40 [‐2.20, ‐0.60] |
| 5.8.5 Infliximab versus etanercept | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | ‐1.60 [‐2.93, ‐0.27] |
| 5.9 Small molecules versus placebo | 9 | 5061 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐0.99, ‐0.60] |
| 5.9.1 Apremilast versus placebo | 5 | 2166 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐0.70, ‐0.47] |
| 5.9.2 Tofacitinib versus placebo | 4 | 2895 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.23, ‐0.93] |
| 5.10 Biologic versus small molecules | 1 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.10.1 Etanercept versus tofacitinib | 1 | 998 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.19, 0.07] |
Comparison 6. Secondary outcome ‐ adverse events.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 6.1 Non‐biological treatments versus placebo | 4 | 1023 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.78, 1.50] |
| 6.1.1 Methotrexate versus placebo | 3 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.81, 1.10] |
| 6.1.2 Fumaric acid esters versus placebo | 1 | 704 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.22, 1.62] |
| 6.2 Non‐biological treatment 1 versus non‐biological treatment 2 | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.2.1 Ciclosporin versus methotrexate | 2 | 172 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.90, 1.34] |
| 6.2.2 Methotrexate versus fumaric acid esters | 2 | 168 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.90, 1.24] |
| 6.3 Anti‐TNF alpha versus placebo | 27 | 9856 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [1.02, 1.10] |
| 6.3.1 Etanercept versus placebo | 11 | 4225 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [1.00, 1.16] |
| 6.3.2 Adalimumab versus placebo | 9 | 3338 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.99, 1.12] |
| 6.3.3 Certolizumab versus placebo | 4 | 1026 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.86, 1.09] |
| 6.3.4 Infliximab versus placebo | 4 | 1267 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.93, 1.36] |
| 6.4 Ustekinumab versus placebo | 11 | 4596 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [1.01, 1.13] |
| 6.5 Anti‐IL17 versus placebo | 21 | 11333 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.11, 1.30] |
| 6.5.1 Secukinumab versus placebo | 11 | 3706 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.06, 1.36] |
| 6.5.2 Ixekizumab versus placebo | 4 | 3268 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.07, 1.45] |
| 6.5.3 Brodalumab versus placebo | 5 | 4109 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.00, 1.32] |
| 6.5.4 Bimekizumab versus placebo | 1 | 250 | Risk Ratio (M‐H, Random, 95% CI) | 1.70 [1.11, 2.58] |
| 6.6 Anti‐IL23 versus placebo | 14 | 5882 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.87, 1.00] |
| 6.6.1 Guselkumab versus placebo | 5 | 1767 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.90, 1.11] |
| 6.6.2 Tildrakizumab versus placebo | 3 | 1904 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.72, 1.02] |
| 6.6.3 Risankizumab versus placebo | 4 | 1476 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.77, 1.07] |
| 6.6.4 Mirikizumab versus placebo | 2 | 735 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.83, 1.19] |
| 6.7 Biologic versus non‐biological treatments | 9 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.7.1 Infliximab versus methotrexate | 1 | 868 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.97, 1.20] |
| 6.7.2 Adalimumab versus methotrexate | 1 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.78, 1.05] |
| 6.7.3 Secukinumab versus fumaric acid esters | 1 | 202 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.71, 0.94] |
| 6.7.4 Etanercept versus acitretin | 2 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.72, 1.96] |
| 6.7.5 Ixekizumab versus fumaric acid esters | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.74, 1.21] |
| 6.7.6 Ixekizumab versus methotrexate | 1 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.76, 1.25] |
| 6.7.7 Guselkumab versus fumaric acid esters | 1 | 119 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.65, 0.89] |
| 6.7.8 Risankizumab versus fumaric acid esters | 1 | 120 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.70, 0.99] |
| 6.7.9 Brodalumab versus fumaric acid esters | 1 | 210 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.62, 0.87] |
| 6.8 Biologic 1 versus biologic 2 | 21 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.8.1 Ustekinumab versus etanercept | 1 | 903 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.89, 1.06] |
| 6.8.2 Secukinumab versus etanercept | 1 | 980 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.89, 1.12] |
| 6.8.3 Ixekizumab versus etanercept | 2 | 2209 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.97, 1.15] |
| 6.8.4 Infliximab versus etanercept | 1 | 48 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.86, 1.08] |
| 6.8.5 Tildrakizumab versus etanercept | 1 | 934 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.65, 0.86] |
| 6.8.6 Certolizumab versus etanercept | 1 | 502 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.86, 1.28] |
| 6.8.7 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.98, 1.16] |
| 6.8.8 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.93, 1.13] |
| 6.8.9 Brodalumab versus ustekinumab | 2 | 3088 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.93, 1.09] |
| 6.8.10 Risankizumab versus ustekinumab | 3 | 965 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.85, 1.11] |
| 6.8.11 Guselkumab versus adalimumab | 3 | 1658 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.89, 1.09] |
| 6.8.12 Risankizumab versus adalimumab | 1 | 605 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.82, 1.43] |
| 6.8.13 Ixekizumab versus guselkumab | 1 | 1027 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.92, 1.15] |
| 6.8.14 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.87, 1.15] |
| 6.9 Small molecules versus placebo | 14 | 5785 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [1.14, 1.38] |
| 6.9.1 Apremilast versus placebo | 7 | 2593 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.13, 1.36] |
| 6.9.2 Tofacitinib versus placebo | 6 | 2925 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.01, 1.63] |
| 6.9.3 TYK2 versus placebo | 1 | 267 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [0.97, 1.77] |
| 6.10 Biologic versus small molecules | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 6.10.1 Etanercept versus tofacitinib | 1 | 998 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.89, 1.12] |
| 6.10.2 Etanercept versus apremilast | 1 | 166 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.03, 1.69] |
Comparison 7. Secondary outcome ‐ PASI 90 at 52 weeks.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 7.1 Biologic 1 versus biologic 2 | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.1.1 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.15, 1.31] |
| 7.1.2 Secukinumab 150 versus secukinumab 300 | 1 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.61, 1.13] |
| 7.1.3 Guselkumab versus adalimumab | 1 | 663 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [1.40, 1.81] |
| 7.1.4 Risankizumab versus ustekinumab | 2 | 799 | Risk Ratio (M‐H, Random, 95% CI) | 1.73 [1.46, 2.05] |
| 7.1.5 Guselkumab 100 versus guselkumab 50 | 1 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.85, 1.25] |
| 7.1.6 Ixekizumab Q2W versus Ixekizumab Q4W | 1 | 1227 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [1.01, 1.11] |
| 7.1.7 Secukinumab versus guselkumab | 1 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 0.83 [0.78, 0.89] |
| 7.1.8 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.31, 1.76] |
| 7.1.9 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.11, 1.52] |
| 7.2 Small molecule 1 versus small molecule 2 | 1 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 7.2.1 Apremilast 30mg versus apremilast other | 1 | 170 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.84, 1.86] |
| 7.3 Biologic versus placebo | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.58, 1.12] |
| 7.3.1 Secukinumab versus placebo | 1 | 82 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.58, 1.12] |
Comparison 8. Secondary outcome ‐ PASI 75 at 52 weeks.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 8.1 Biologic 1 versus biologic 2 | 11 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.1.1 Secukinumab versus ustekinumab | 2 | 1778 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [1.04, 1.22] |
| 8.1.2 Secukinumab 150 versus secukinumab 300 | 1 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.70, 1.06] |
| 8.1.3 Guselkumab versus adalimumab | 1 | 663 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [1.28, 1.54] |
| 8.1.4 Risankizumab versus ustekinumab | 2 | 799 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.12, 1.41] |
| 8.1.5 Guselkumab 100 versus guselkumab 50 | 1 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.88, 1.09] |
| 8.1.6 Ixekizumab Q2W versus ixekizumab Q4W | 1 | 1227 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.07, 1.22] |
| 8.1.7 Secukinumab versus guselkumab | 1 | 1048 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [1.08, 1.21] |
| 8.1.8 Risankizumab versus secukinumab | 1 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.14, 1.44] |
| 8.1.9 Ixekizumab versus ustekinumab | 1 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.05, 1.29] |
| 8.2 Small molecules 1 versus small molecules 2 | 2 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 8.2.1 Tofacitinib 10 mg versus tofacitinib 20 mg | 1 | 178 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.63, 0.95] |
| 8.2.2 Apremilast 30 versus apremilast other | 1 | 170 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.46, 2.78] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
ACCEPT 2010.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: 26 March 2007 ‐ 15 January 2009 Location: 67 centres in Manchester, UK |
|
| Participants |
Randomised: 903 participants (mean age 45 years, 613 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab (n = 209), SC, 45 mg, weeks 0 ‐ 4, 4 weeks Control intervention B. Ustekinumab (n = 347), SC, 90 mg, weeks 0 ‐ 4, 4 weeks C. Etanercept (n = 347), SC, 50 mg x 2/weeks, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding, Quote (p 127): "Supported by Centocor Research and Development." Declarations of interest (p 127) "Dr. Griffiths reports receiving consulting and lecture fees from Abbott, Janssen‐Cilag, Merck Serono, Novartis, Schering‐Plough, and Wyeth and grant support from Merck Serono; Dr. Strober, receiving consulting and lecture fees from Centocor, Johnson & Johnson, Amgen, and Abbott Laboratories and grant support from Amgen and Abbott Laboratories; Dr. van de Kerkhof, receiving consulting fees from Schering‐Plough, Celgene, Centocor, Almirall, UCB, Wyeth, Pfizer, Soffinova, Abbott, Actelion, Galderma, Novartis, Janssen‐Cilag, and Leo Pharma; Dr. Ho, receiving advisory‐board and lecture fees from Schering, Abbott, Janssen‐Ortho, Pfizer, Amgen, and Wyeth and grant support from Centocor, Abbott, Amgen, and Wyeth; Dr. Menter, receiving advisory‐board, consulting, and lecture fees from Abbott, Amgen, Astellas, Biogen Idec, Celgene, Centocor, Genentech, Warner Chilcott, and Wyeth; Drs. Yeilding, Guzzo, Xia, and Dooley and Ms. Li, being employees of Johnson & Johnson and having equity and holding stock options in Johnson & Johnson; Dr. Zhou, being an employee of Johnson & Johnson, having equity and holding stock options in Johnson & Johnson, and having equity in Wyeth; Dr. Fidelus‐Gort, being a former employee of Johnson & Johnson and having equity and holding stock options in Johnson & Johnson; and Dr. Goldstein, receiving consulting fees from Centocor. No other potential conflict of interest relevant to this article was reported." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 119): “We randomly assigned...” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 119): “We randomly assigned...” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 119): “Patients were aware of their treatment assignment”, ... “All study personnel, except those who dispensed or administered a study agent remained unaware of the treatment assignments" Comment: high risk for participants and unclear risk for personnel (no description of means used to avoid communication between participants and personnel and very difficult to avoid) |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 119): “All study personnel, except those who dispensed or administered a study agent remained unaware of the treatment assignments" Comment: no description of the method used to assess the primary outcome |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 903 participants underwent randomisation, 903 were analysed Comment: methods for dealing with missing data not specified |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00454584). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
ADACCESS 2018.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: December 2013 and March 2015 Location: 73 study centres in Bulgaria, France, Slovakia and the USA Phase 3 |
|
| Participants |
Randomised: 465 participants (mean age 46 years, 184 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. GP2017, n = 231 Control intervention B. ref‐ADMB (Humira; AbbVie Ltd, Maidenhead, UK; AbbVie Inc., North Chicago, IL, U.S.A), n = 234 sourced from Europe or the USA, an initial dose of 80 mg subcutaneous, then followed by 40 mg every other week, starting 1 week after the initial dose until week 15 |
|
| Outcomes |
Assessment at week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 623): "The study was funded by Hexal AG, a Sandoz company. The funder had a role in the study design, data collection, data analysis and manuscript preparation" Confict of interest Quote (p 623): "A. Blauvelt has served as a scientific adviser and clinical study investigator for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Dermira Inc., Eli Lilly and Company, Janssen, Merck Sharp & Dohme, Novartis, Sandoz, UCB Pharma and Valeant; and as a paid speaker for Eli Lilly and Company and Janssen. J.P.L. has served as a clinical study investigator for Sandoz and has received a grant from University Hospital Nice. J.F.F. has served as a clinical study investigator for and has received research grants from Sandoz. J.M.W.served as a clinical study investigator for and has received research grants from Sandoz, and has received research grants and honoraria from Novartis. D.G. has served as a clinical study investigator for Sandoz. E.S., J.J.L. and A. Balfour are employees of Hexal AG (a Novartis Division). C.L.L. has served as a consultant or advisory board member for AbbVie, Amgen, Boehringer Ingelheim, Dermira, Eli Lilly and Company, Janssen, LEO Pharma, Pfizer, Sandoz, VCB and Vitae; as an investigator for Actavis, AbbVie, Amgen, Boehringer Ingelheim, Celgene, Coherus, Cellceutix, Corrona, Dermira, Eli Lilly and Company, Galderma, Glenmark, Janssen, LEO Pharma, Merck, Novartis, Novella, Pfizer, Sandoz, Sienna, Stiefel and Wyeth; and as a participant in speaker bureaus for AbbVie, Celgene, Eli Lilly and Company and Novartis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 624): "This was a randomized, multicentre phase III confirmatory study consisting of four periods...Randomization was stratified by prior systemic therapy, region and body weight, and was performed centrally" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 624): "This was a randomized, multicentre phase III confirmatory study consisting of four periods...Randomization was stratified by prior systemic therapy, region and body weight, and was performed centrally" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 624): “The study was double blinded; patients, investigator staff and the people performing the study assessments remained blinded to the identity of the given treatments until week 51.” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 624): “The study was double blinded; patients, investigator staff and the people performing the study assessments remained blinded to the identity of the given treatments until week 51.” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 465 Management of missing data: Quote (supplemental appendix): "No imputation of missing values was performed." Non‐inferiority trial: Quote (p 626): "In line with guidance from the U.S. Food and Drug Administration (FDA), efficacy analyses were conducted using the per protocol analysis set. The per protocol set is considered conservative, as protocol violators who could bias study results towards equivalence are excluded. Supportive analyses were performed using the full analysis set." Table 1: Both per protocol and full‐set analyses Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02016105) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results posted on ClinicalTrials.gov |
Akcali 2014.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: January 2008 ‐ January 2009 Location: Gaziantep, Turkey (1 centre) |
|
| Participants |
Randomised: 55 participants (mean age 39 years, 33 male) Inclusion criteria
Exclusion criteria None Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 25), orally, 0.3 ‐ 0.5 mg/kg/d Control intervention B. Cyclosporin (n = 21), orally, 3 mg/kg/d |
|
| Outcomes | Assessment at 8 weeks Primary outcome of the trial
Outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1121): "No specific grant" Declarations of interest: Quote (p 1121): "The authors declare that there are no conflicts of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p1119): "Patients were stratified into one of two groups via a computer‐generated randomisation schedule" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not stated that it was a blinded trial. Acitretin has visible side effects (muco cutaneous dryness) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: no independent assessor. Not stated that it was a blind trial. Acitretin has visible side effects. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 55, analysed 46 Management of missing data: not stated |
| Selective reporting (reporting bias) | High risk | Comment: no primary or secondary outcomes stated. No protocol available |
Al‐Hamamy 2014.
| Study characteristics | ||
| Methods | RCT, active‐placebo controlled, open‐label trial Date of study: February 2010 ‐ October 2011 Location: Baghdad, Iraq (1 centre) |
|
| Participants |
Randomised: 120 participants (mean age 41 years, 41 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
No more statements regarding time and reasons of follow‐up |
|
| Interventions |
Intervention A. Methotrexate + NBUVB (n = 38), 20 mg/week + 45 mJ/cm2, 3 times/week Control intervention B. NBUVB (n = 38), 45 mJ/cm2, 3 times/week C. Methotrexate (n = 37), 20 mg/week |
|
| Outcomes | Assessment at 6 months Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (page 1531): "three groups randomly...” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: No description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not stated that it was a blind trial, probably not blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: no independent assessor. Not stated that it was a blind trial, probably not blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 120, analysed 113 Management of missing data: not stated |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol available. The outcomes mentioned in the methods section appeared to have been reported |
AMAGINE‐1 2016.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: 29 August 2012 ‐ 12 March 2014 Location: 73 centres worldwide (Europe, USA and Canada) |
|
| Participants |
Randomised: 661 participants (mean age 46 years, 484 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Brodalumab (n = 222), SC, 210 mg every 2 weeks Control intervention B. Brodalumab (n = 219), SC, 140 mg every 2 weeks C. Placebo (n = 220) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1): "This study was funded by Amgen Inc. & AstraZeneca/MedImmune." Declarations of interest (pp 13‐14): "K.A.P. has served as a consultant, investigator and/or speaker for AbbVie, Amgen Inc., Astellas Pharma, Bayer AG, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Forward Pharma, Galderma, Janssen Biotech Inc., LEO Pharma, Merck, Novartis, Pfizer, Roche and UCB Pharma. K.R. has served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis, including AbbVie, Amgen Inc., Biogen‐Idec, Celgene, Centocor, Covagen, Forward Pharma, GSK, Janssen‐Cilag, LEO Pharma, Lilly, Medac, MSD, Novartis, Pfizer, Takeda and Vertex. C.P. has served as a consultant and investigator for Amgen Inc., AbbVie, Boehringer, Janssen‐Cilag, LEO Pharma, Lilly, Novartis and Pfizer. A.B. has served as a consultant and investigator for AbbVie, Amgen Inc., Anacor, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Genentech, Janssen, Merck, Novartis, Pfizer, Regeneron and Sandoz." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (pp 2 and 3): "Patients were randomized... IP supply was controlled by interactive voice response system and box numbers were assigned at each visit" Comment: no description of the method used to guarantee the random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote (pp 2 and 3): "Patients were randomized...IP supply was controlled by interactive voice response system and box numbers were assigned at each visit". Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "Randomizations remained blinded to all patients and investigators... Throughout the study, patients received placebo as needed to maintain the blind until it was broken." Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "Randomizations remained blinded to all patients and investigators... Throughout the study, patients received placebo as needed to maintain the blind until it was broken." Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 661, 661 analysed Management of missing data: quote (pp 4‐5): "The full analysis set included all randomised patients... Mutiple imputations for missing data" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01708590; AMAGINE‐1). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. |
AMAGINE‐2 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: August 2012 ‐ September 2014 Location: 142 centres worldwide |
|
| Participants |
Randomised: 1831 participants (mean age 45 years, 1258 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Brodalumab (n = 610), SC, 140 mg (2 injections week 0, 1 injection eow) Control intervention B. Brodalumab (n = 612), SC, 210 mg (2 injections week 0, 1 injection eow) C. Ustekinumab (n = 300), SC, 45/90 mg (week 0, week 4 and every 12 weeks) D. Placebo (n = 309), orally (same drug administration) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1319) “Amgen funded both studies. ... and Amgen conducted the data analyses. All the authors interpreted the data” Declarations of interest (p 1327): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Dr. Lebwohl reports grant support from Amgen, AbbVie, Janssen Biotech, UCB Pharma, Pfizer, Celgene, Eli Lilly, and Novartis outside the submitted work. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol): “The randomisation lists will be generated by Amgen using a permuted block design within each strata...via an interactive voice response system” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (protocol): “The randomisation lists will be generated by Amgen using a permuted block design within each strata...via an interactive voice response system” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol, cf 6. Treatment procedure): “This is a double dummy procedure...” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol, cf 6. Treatment procedure): “This is a double dummy procedure...” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1831, analysed 1831 Dealing with missing data Quote (protocol and p 1321) "...with missing data imputed as indicating no response" Comment: well described |
| Selective reporting (reporting bias) | High risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT0178603) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except for participant‐reported outcome |
AMAGINE‐3 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: September 2012 ‐ August 2014 Location: 142 centres worldwide (no sites that were included in the AMAGINE‐2 study) |
|
| Participants |
Randomised: 1881 participants (mean age 45 years, 1288 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Brodalumab (n = 629), SC, 140 mg (2 injections week 0, 1 injection eow) Control intervention B. Brodalumab (n = 624), SC, 210 mg (2 injections week 0, 1 injection eow) C. Ustekinumab (n = 313), SC, 45/90 mg (week 0, week 4 and every 12 weeks) D. Placebo (n = 315), orally (same drug administration) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1319) “Amgen funded both studies. ... and Amgen conducted the data analyses. All the authors interpreted the data” Declarations of interest (p 1327): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Dr. Lebwohl reports grant support from Amgen, AbbVie, Janssen Biotech, UCB Pharma, Pfizer, Celgene, Eli Lilly, and Novartis outside the submitted work. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol): “The randomisation lists will be generated by Amgen using a permuted block design within each strata..." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (protocol): “The randomisation lists will be generated by Amgen using a permuted block design within each strata...via an interactive voice response system” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol, cf 6. Treatment procedure): “This is a double dummy procedure...” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol, cf 6. Treatment procedure): "This is a double dummy procedure...” |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1881, analysed 1881 Dealing with missing data Quote (protocol and p 1321) "...with missing data imputed as indicating no response" Comment: well described |
| Selective reporting (reporting bias) | High risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01708629) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except for participant‐reported outcome |
Asahina 2010.
| Study characteristics | ||
| Methods | RCT, active, placebo‐controlled, double‐blind Date of study: September 2005 ‐ December 2006 Location: 42 centres in Japan |
|
| Participants |
Randomised: 169 participants (mean age 45 years, 143 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab (n = 38), 40 mg, SC, eow B. Adalimumab (n = 43), 40 mg, SC, 2 injections, week 0, 1 injection eow (week 2) C. Adalimumab (n = 41), 80 mg, SC, eow Control D. Placebo (n = 46), 0.8 mL, SC, eow |
|
| Outcomes | Assessment at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: support by Abbott (Quote p 309) Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 301): "Patients were randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 301): "Adalimumab 40mg/0.8mL and Placebo 0.8 mL were supplied two‐vial cartons (Adalimumab+Adalimumab, Adalimumab+placebo, Placebo+Placebo)" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Comment: no specific description of the method used to guarantee blinding of outcome assessment but considering that this was a placebo‐controlled trial with no known systematic AEs we considered the risk as low |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 169, analysed 169 Management of missing data: Quote (p 302): "Patients without evaluation at week 16 were considered non‐responders for the primary analysis" Comment: the report provided sufficient detail about the management of missing data to permit a clear judgement |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol available. The outcomes mentioned in the Methods section appeared to have been reported |
Asahina 2016.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind Date of study: March 2012 ‐ January 2014 Location: 16 centres in Japan |
|
| Participants |
Randomised: 95 participants, 94 treated (mean age 49 years, 78 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 43), orally, 5 mg twice daily Control intervention B. Tofacitinib (n = 44), orally, 10 mg twice daily |
|
| Outcomes | Assessment at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 878): "This study was sponsored by Pfizer Inc. Medical writing support under the guidance of the authors was provided by Kate Silverthorne, Ph.D., at Complete Medical Communications and was funded by Pfizer Inc" Declarations of interest: Quote (p 878): "A. A., A. I., S. I., H. S. and M. O. have received consultancy fees from Pfizer Inc. Y. S., Y. T., S. T. and M. N. are employees of Pfizer Japan Inc. T. E. has nothing to disclose." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 870): "Patients were randomized 1:1 to tofacitinib 5 or 10 mg b.i.d. using a computer‐generated randomization schedule". Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 870): "patients were registered by the investigator in a central randomized management system" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 870): "Tofacitinib was supplied as 5 mg tablets with a corresponding matching placebo. Patients and study staff were unable to determine from the packaging which treatment group the patient was assigned to. Patients, investigators, study teams, the contract research organization and the sponsor remained blinded throughout the study period " Comment: the report provided sufficient detail about the measures used to blind study participants and personnel from knowledge of which intervention a participant received, to permit a clear judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 870): "Tofacitinib was supplied as 5 mg tablets with a corresponding matching placebo. Patients and study staff were unable to determine from the packaging which treatment group the patient was assigned to. Patients, investigators, study teams, the contract research organization and the sponsor remained blinded throughout the study period " Comment: the report provided sufficient detail about the measures used to blind study participants and personnel from knowledge of which intervention a participant received, to permit a clear judgement |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned n = 95, 94 received at least 1 dose of study drug, 87 had moderate‐severe psoriasis (study population) and 12 had psoriatic arthritis Management of missing data: Quote (p 871): "The full analysis set included all randomized patients who received one or more dose of study drug...Missing values were treated as non‐responders (non‐responder imputation)." Table 2: 87 analysed participants Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01519089) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Asawanonda 2006.
| Study characteristics | ||
| Methods | RCT, active placebo‐controlled, double‐blind Date of study: not reported Location: Bangkok, Thailand, Asia |
|
| Participants |
Randomised: 24 participants (mean age 40 years (methotrexate) 48 years (placebo), 15 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 11), 15 mg/week, orally Control B. Placebo (n = 13), orally Co‐intervention: phototherapy UVB |
|
| Outcomes | Assessment at 24 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: (quote p 1013) no funding source Declarations of interest: (quote p 1013) "None identified" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1014): "randomized by way of randomization cards" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1014): "to receive either MTX or placebo, which were identical in appearance" Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1015): "PASI scores were given by a investigator blinded to the treatment assignment" Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 24, analysed 24 Management of missing data: Comment: no more precision regarding methods for dealing with missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol available. The outcomes mentioned in the Methods section appeared to have been reported. |
AURIEL‐PsO 2020.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind trial Date of study: February 2016 ‐ December 2017 Location: world‐wide |
|
| Participants |
Randomised: 443 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Biosimilar group (9), Humira group (19)
|
|
| Interventions |
Intervention A. Biological: MSB11022, S/C, Biosimilar adalimumab week 0: 80 mg, week 1: 40 mg, then 40 mg EOW, n = 222 Control Intervention B. Biological: adalimumab (Humira) week 0: 80mg, week 1: 40 mg, then 40 mg EOW, n = 221 |
|
| Outcomes |
At 16 weeks Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov): EMD Serono Research and Development Institute, Inc. Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (ClinicalTrials.gov): "Allocation: randomized" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Double (Participant, Investigator)" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Double (Participant, Investigator)" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: not stated Results posted on ClinicalTrials.gov: Per protocol analyses (non‐inferiority trial) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02660580) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Bachelez 2015.
| Study characteristics | ||
| Methods | RCT, active placebo‐controlled, double‐blind Date of study: 29 November 2010 ‐ 13 September 2012 Location: 122 worldwide excluding the USA and Canada |
|
| Participants |
Randomised: 1106 participants (mean age 46 years, 458 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 330), orally, 5 mg twice daily Control intervention B. Tofacitinib (n = 332) orally, 10 mg twice daily C. Etanercept (n = 336) SC, 50 mg twice weekly D. Placebo (n = 108) |
|
| Outcomes | Assessment at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 555): "This study was designed and funded by Pfizer Inc. Study investigators gathered the data, which were maintained in a database by Pfizer." Declarations of interest: Quote (p 560): "HB has provided consultancy services for AbbVie, Amgen, Boehringer, Celgene, Janssen, Leo Pharma, Lilly, Novartis, MSD, Pfizer, and Sandoz. He has also acted as an adviser for AbbVie, Amgen, Boehringer, Celgene, Janssen, Leo Pharma, Lilly, Novartis, Pfizer, and Sandoz; has served on speaker’s bureaus for AbbVie, Amgen, Celgene, Janssen, Leo Pharma, Lilly, Novartis, and Pfizer; and has received a research grant from Pfizer. PCMvdK has provided consultancy services for Celgene, Centocor, Almirall, Amgen, Pfizer, Philips, Abbott, Ely Lilly, Galderma, Novartis, JanssenCilag, Leo Pharma, Sandoz, and Mitsubishi. He has also done clinical trials for Basilea, Pfizer, Ely Lilly, Amgen, AbbVie, Philips Lighting, JanssenCilag, and Leo Pharma. RS has served on speaker’s bureaus for Pfizer, Schülke and Mayr, Lohmann & Rauscher, Meda Pharmaceuticals, Menarini Pharmaceuticals, Stockhausen, and Smith & Nephew; has had consulting agreements with Pfizer, Novartis, Lohmann & Rauscher, Urgo, Chemomedica, Schülke & Mayr, and Pantec Biotechnologies; and has received research and educational grants from Stockhausen, 3M‐Woundcare, Smith & Nephew, Lohmann & Rauscher, Enjo Commercials, Urgo, Chemomedica, and Schülke & Mayr. FV has been a principal investigator, member of a scientific advisory board, or speaker for AbbVie, Janssen, Eli Lilly, Merck, Novartis, and Pfizer. SC has been a consultant and/or speaker for Pfizer, AbbVie, Novartis, Merck, and Janssen‐Cilag. JPa, JPr, PG, HT, MT, HV, and RW are employees of Pfizer Inc. AK, J‐HL, and VY declare no competing interests." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 553): "A computer‐generated randomization schedule was used to assign patients to the treatment groups". Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (pp 553‐4): "The study site contacted an interactive voice response system or web‐based interactive response system..." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 553): "For this randomised, double‐blind, double‐dummy, placebo‐controlled, parallel‐group phase 3 study" Comment: the report provided sufficient detail about the measures used to blind study participants and personnel from knowledge of which intervention a participant received, to permit a clear judgement |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 553): "Double Blind (Subject, Caregiver, Investigator, Outcomes Assessor), Patients and study personnel were masked to treatment assignment: the study drug packaging was labelled.... " Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1106, 1101 received at least 1 dose of study drug Management of missing data: Quote (p 554): "The primary analysis population for efficacy was the full analysis set, which was defined as all patients who received at least one dose of study drug... We judged patients with missing values for all binary endpoints to be non‐responders in efficacy assessments" Table 2: 1101 analysed participants Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01241591). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. |
Bagel 2012.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: North America |
|
| Participants |
Randomised: 124 participants (median age 39 years (etanercept) and 42 years (placebo), 69 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 62), SC, 50 mg, twice a week Control intervention B. Placebo (n = 62), SC, twice a week |
|
| Outcomes | Assessment at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: Amgen Inc Declarations of interest (Quote p 86): "Dr Bagel receives a salary as founder of the Psoriasis Treatment Center of Central New Jersey. He has received speaker honoraria from Leo Pharma, Galderma, Centocor, Abbott, and Amgen. He has also been compensated as a consultant for Galderma and has served as an investigator for Centocor, Abbott, and Amgen. Dr Lynde has received research grants and honoraria from Amgen, Abbott, Merck, Ortho Biotech, Leo Pharma, and Galderma, for whom he has served as an advisory board member, consultant, and speaker. He has also served as an investigator for Amgen, Abbott, Merck, Ortho Biotech, and Leo Pharma. Dr Tyring has received a research grant and honoraria from Amgen, for whom he has served as a consultant, investigator, and speaker. He has also served as an investigator and/or speaker for Abbott, Leo Pharma, Galderma, GSK, Novartis, Merck, Epiphany, Inhibitex, AiCuris, and Pfizer. Dr Kricorian, Yifei Shi, and Dr Klekotka are employees of Amgen Inc. and have received Amgen stock/stock options." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 87): "Each patient provided written informed consent and received a unique identification number and randomised assignment from an Interactive Web Response System" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 87): "Each patient provided written informed consent and received a unique identification number and randomised assignment from an Interactive Web Response System" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 87): "patients and clinicians were blinded throughout the study as to treatment assignments." Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote:"patients and clinicians were blinded throughout the study as to treatment assignments." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 124, analysed 124 Dropouts and withdrawals
Quote (p 89): "included in ITT efficacy analysis" Management of missing data: Quote (p 88): "Last observation carried forward imputation was used for missing values" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol available. The outcomes mentioned in the Methods section appeared to have been reported except for QoL |
Barker 2011.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: September 2005 ‐ June 2008 Location: 106 centres in Europe |
|
| Participants |
Randomised: 868 participants (mean age 43 years, 586 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Reasons not stated at week 16 |
|
| Interventions |
Intervention A. Infliximab (n = 653), IV, 5 mg/kg, weeks 0, 2, 6, 14, 22 Control intervention B. Methotrexate (n = 215), orally, 15 mg/week for 22 weeks |
|
| Outcomes | Assessment at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: financial support for this study was provided by Schering‐Plough Research Institute, now Merck, Sharp & Dohme Corporation, Whitehouse Station, NJ, USA Declarations of interest: (Quote Appendix 1): "J.B. has served as a consultant and/or paid speaker for, and/or participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis including Abbott, Celgene, Centocor, Janssen‐Cilag, Johnson and Johnson, Merck, Novartis, Pfizer, Schering‐Plough and Wyeth. M.H. has served as a consultant and/or paid speaker for, and/or has participated in clinical trials sponsored by Abbott, Amgen, Essex, Janssen, Leo, Medac, Novartis, Pfizer, Schering‐Plough and Wyeth. G.W. has no conflicts of interest to disclose. J.‐P.O. has been a consultant for Schering‐Plough, Abbott, Merck‐Serono, Centocor, Wyeth, Janssen‐Cilag, Meda‐Pharma, Pierre‐Fabre and Galderma. H.Z. is an employee of Merck, Sharp & Dohme. H.v.H. was an employee of Merck, Sharp & Dohme at the time of the RESTORE1 study and during the preparation of this manuscript. K.R. has served as a consultant and/or paid speaker for, and/or participated in clinical trials sponsored by Abbott, Celgene, Centocor, Janssen‐Cilag, Leo, Medac and Merck." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1110): “At each eligible subject's baseline visit, study centres telephoned the Interactive Voice REsponse Syste .... for randomisation" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1110): “At each eligible subject's baseline visit, study centres telephoned the Interactive Voice REsponse Syste .... for randomisation" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 1110): “open‐label trial” Comment: no blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 1110): “open‐label trial” Comment: no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 868, analysed 868 Quote (p 1110‐11): "Primary and secondary efficacy analyses were based on the ITT population, the ITT population included all randomised patients. At week 16, patients who dropped out early or had missing data for PASI 75 ... were considered nonresponders" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00251641). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
BE ABLE 1 2018.
| Study characteristics | ||
| Methods | RCT, phase 2, randomised, double‐blinded, placebo‐controlled, parallel‐group, dose‐ranging study Date of study: 25 August 2016 ‐ 1 March 2017 Location: 6 countries (Canada, Czech Republic, Hungary, Japan, Poland, and USA) |
|
| Participants |
Randomised: 250 participants (Age 44 years old, 163 males) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Bime 64 (3), Bime 160 (5), Bime 320/160 (6), Bime 320 (3), Bime 480 (4), PBO (5)
|
|
| Interventions |
Intervention: A. Bimekizumab every 4 weeks at doses of 64 mg, n = 39 Control intervention: B. Bimekizumab every 4 weeks at doses of 160 mg, n = 43 C. Bimekizumab every 4 weeks at doses of 160 mg (with 320 mg loading dose at baseline), n = 40 D. Bimekizumab every 4 weeks at doses of 320 mg, n = 43 E. Bimekizumab every 4 weeks at doses of 480 mg, n = 43 F Placebo, n = 42 |
|
| Outcomes |
At week 12 Primary outcome:
Secondary outcomes:
|
|
| Notes | Funding Quote (p 277): "Supported by UCB Pharma." Conflicts of interest Quote (p 277): "Dr Papp has received consultant fees from Astellas, AstraZeneca, Baxalta, Baxter, Boehringer Ingelheim, Bristol‐Myers Squibb, CanFite, Celgene, Coherus, Dermira, Dow Pharma, Eli Lilly, Forward Pharma, Galderma, Genentech, Janssen, Kyowa Hakko Kirin, LEO Pharma, Meiji, Seika Pharma, MSD, Merck Serono, Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Roche, Sanofi/Genzyme, Takeda, UCB, and Valeant; investigator fees from Astellas, Baxalta, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Coherus, Dermira, Dow Pharma, Eli Lilly, Galderma, Genentech, GSK, Janssen, Kyowa Hakko Kirin, LEO Pharma, MedImmune, MSD, Merck‐Serono, Novartis, Pfizer, Regeneron, Roche, Sanofi/Genzyme, Takeda, UCB, and Valeant; speaker fees from Astellas, Celgene, Eli Lilly, Galderma, Kyowa Hakko Kirin, LEO Pharma, MSD, Novartis, Pfizer, and Valeant; has participated in advisory boards for Astellas, Baxter, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dow Pharma, Eli Lilly, Galderma, Janssen, MSD, Novartis, Pfizer, Regeneron, Sanofi/Genzyme, UCB, and Valeant; is a steering committee member for Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, Kyowa Hakko Kirin, MSD, Merck‐Serono, Novartis, Pfizer, Regeneron, Sanofi/Genzyme, and Valeant; and is a scientific officer for Kyowa Hakko Kirin. Dr Merola has received honoraria from AbbVie, Celgene, Eli Lilly, Janssen, Novartis, Pfizer, Samumed, and UCB. Dr Gottlieb has received consultant fees, advisory board fees, or speaker fees from AbbVie, Allergan, Beiersdorf Inc, Bristol‐Myers Squibb, Celgene, Dermira, Lilly, Incyte, Janssen, Novartis, Reddy Labs, Sun Pharmaceutical Industries, UCB, and Valeant; and research grants from Allergan, Incyte, Janssen, LEO, Eli Lilly and Company, and Novartis. Dr Blauvelt has received consultant fees from Eli Lilly and Company, Janssen, Regeneron, and Sanofi Genzyme; and is a scientific adviser or clinical study investigator for AbbVie, Aclaris, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira Inc, Eli Lilly and Company, Genentech/Roche, GlaxoSmithKline, Janssen, Leo, Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, UCB Pharma, Valeant, and Vidac. Dr Griffiths has received grants and personal fees from AbbVie, Celgene, LEO, Eli Lilly and Company, Janssen, Novartis, Pfizer, and UCB Pharma; grants from Sandoz; personal fees from Almirall and Galderma. Dr Griffiths has received research grants from AbbVie, Celgene, Novartis, Eli Lilly and Company, Janssen, Sandoz, Pfizer, LEO, and UCB. Mr Patterson and Dr Cioffi own stock in UCB. Dr Cross has no further conflicts to disclose. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p279): "An interactive voice or web response system was used for assigning eligible patients to a treatment regimen according to a randomization schedule produced by an independent biostatistician who was not associated with the design or analysis of the study. Treatment assignment was stratified by geographic region and prior biologic exposure." Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 279): "An interactive voice or web response system was used for assigning eligible patients to a treatment regimen according to a randomization schedule produced by an independent biostatistician who was not associated with the design or analysis of the study. Treatment assignment was stratified by geographic region and prior biologic exposure." Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 279 and supplemental appendix): "Bimekizumab was provided in single‐use vials containing 160 mg/mL. Due to differences in presentation and to ensure study blinding, bimekizumab and placebo injections were prepared and administered at the investigational sites by unblinded, dedicated study personnel"; "Additional details of blinding: Bimekizumab was provided in single‐use vials containing 160 mg/mL. Placebo was supplied as 0.9% saline solution. Treatments were administered as 3 subcutaneous injections (lateral abdominal wall and upper outer thigh). During each dosing visit, each of the 3 injections was administered at a separate injection site, and sites were rotated. Due to differences in presentation and to ensure study blinding, bimekizumab and placebo injections were prepared and administered at the investigational sites by unblinded, dedicated study personnel. The unblinded personnel were not involved in the study in any way other than assuring the medication was taken from the correct kit and administered to patients. All other study personnel remained blinded and did not have access to medication‐related information. To preserve the blinding of treatment doses, each administration consisted of 3 subcutaneous injections" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 279 and supplemental appendix): "Bimekizumab was provided in single‐use vials containing 160 mg/mL. Due to differences in presentation and to ensure study blinding, bimekizumab and placebo injections were prepared and administered at the investigational sites by unblinded, dedicated study personnel"; "Additional details of blinding: Bimekizumab was provided in single‐use vials containing 160 mg/mL. Placebo was supplied as 0.9% saline solution. Treatments were administered as 3 subcutaneous injections (lateral abdominal wall and upper outer thigh). During each dosing visit, each of the 3 injections was administered at a separate injection site, and sites were rotated. Due to differences in presentation and to ensure study blinding, bimekizumab and placebo injections were prepared and administered at the investigational sites by unblinded, dedicated study personnel. The unblinded personnel were not involved in the study in any way other than assuring the medication was taken from the correct kit and administered to patients. All other study personnel remained blinded and did not have access to medication‐related information. To preserve the blinding of treatment doses, each administration consisted of 3 subcutaneous injections" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (p281): "Efficacy analyses included patients who received 1 dose of study treatment and had a valid measurement of the primary efficacy variable at baseline (full analysis set)...Patients with missing efficacy data were imputed as nonresponders" 250 randomised, 250 analysed Comment: Done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02905006) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Bissonnette 2013.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, single‐blind Date of study: May 2009 ‐ June 2011 Location: Montréal, Quebec, Canada (5 centres) |
|
| Participants |
Randomised: 30 participants (median age 56 years (adalimumab) and 57 years (placebo), 23 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab (n = 20), SC, 80/40 mg, eow Control intervention B. Topical treatment, phototherapy or no treatment (n = 10) |
|
| Outcomes | Assessment at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: Abbott Laboratories Declarations of interest: (quote p 89) "Dr Bissonnette and Dr Bolduc have been investigators, advisors and/ or consultants and received grants and/or honoraria from Abbott, Amgen, Astellas, Novartis, Janssen Ortho, Pfizer, Celgene, and Tribute. Drs Tardif, Harel, Pressacco, and Guertin have no conflicts of interest to declare." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 84): "were randomised a concealed computer generated code created by the sponsor" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 84): "were randomised a concealed computer generated code created by the sponsor" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (pp 83‐4): "single‐blind (cardiologist and all staff involved in vascular imaging and analysis were blinded to treatment assignment)" Comment: no blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (pp 83‐4): "single‐blind (cardiologist and all staff involved in vascular imaging and analysis were blinded to treatment assignment)" Comment: probably done, but no statement about secondary outcomes |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 30, analysed 30 Quote (p 84): "For all end points, the analysis was conducted on the ITT population, ... for the PASI 75 end point,... a nonresponder imputation method was used" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00940862) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Bissonnette 2015.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: 20 August 2010 ‐ 14 May 2014 Location: 65 centres in Europe, North and South America, and Australia |
|
| Participants |
Randomised: 674 participants (mean age 46 years, 458 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 338), orally, 10 mg twice daily Control intervention B. Tofacitinib (n = 336), orally, 5 mg twice daily |
|
| Outcomes | Assessment at 24 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1395 & 1400): "This study was sponsored by Pfizer Inc. Pfizer conducted the data analysis and the authors interpreted the data and collaborated in the manuscript preparation. All authors have access to the study data." Declaration of interest: (Quote: Appendix 1): "R.B. has received honoraria, grants or worked as a consultant for AbbVie, Amgen, Apopharma, Astellas, Celgene, Eli Lilly, Incyte, Janssen, LEO Pharma, Merck, Novartis, Pfizer and Tribute. L.I. has served as a consultant and/or paid speaker for, and/or participated in clinical trials sponsored by, AbbVie, Almirall, Amgen, Celgene, Centocor, Eli Lilly, Janssen‐Cilag, LEO Pharma, MSD, Novartis, Pfizer and UCB. H.S. has served as a principal investigator and consultant for Pfizer, Celgene, Janssen, Amgen, Novartis, Eli Lilly and Merck. C.E.M.G has received grant/research support and/or received honoraria from AbbVie, Actelion, Biotest, Celgene, Eli Lilly, Incyte, Janssen, LEO Pharma, MSD, Novartis, Pfizer, Sandoz, Stiefel U.K., Trident, Zymogenetics and UCB. P.F. has served as a consultant for Galderma, LEO/Peplin, Ascent, Clinuvel, Aspen, Janssen‐Cilag, Eli Lilly, Australian Ultraviolet Services, Novartis, Wyeth/Pfizer, Mayne Pharma, MedyTox and Roche. He has also served on advisory boards/speaker’s bureaus and/or as a clinical trial investigator for CSL, Galderma, 3M/iNova/Valeant, LEO/Peplin, Ascent, Clinuvel, GSK/Stiefel, Abbott/AbbVie, BiogenIdec, Janssen‐Cilag, Merck Serono, ScheringPlough/MSD, Wyeth/Pfizer, Amgen, Novartis, Eli Lilly, Celgene, Roche, Aspen, Actelion, Sanofi Aventis, MedyTox, Shape and BMS. He has received travel grants from Galderma, LEO/ Peplin, BiogenIdec, Merck Serono, Ascent, Abbott/Abbvie, Schering‐Plough/MSD, Janssen–Cilag, Wyeth/Pfizer, Novartis and Roche. R.R. is a consultant, investigator and/or speaker for AbbVie, Eli Lilly, Galderma, Janssen‐Cilag, LEO Pharma, Novartis and Pfizer. M.B., S.T.R., H.T., J.P., H.V., L.M., P.G. and R.W. are employees of Pfizer Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1398): "A computer‐generated central randomisation schema was implemented using an automated web/telephone sytem." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1398): "A computer‐generated central randomisation schema was implemented using an automated web/telephone sytem." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1398, ClinicalTrials.gov, NCT01186744): "Masking: Double Blind (Subject, Caregiver, Investigator, Outcomes Assessor) " Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1397): "Masking: Double Blind (Subject, Caregiver, Investigator, Outcomes Assessor) " Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 674, analysed 662 Dropouts and withdrawals: Tofacitinib 5 mg twice‐daily group (39), tofacitinib 10 mg twice‐daily group (41) Imbalanced numbers for withdrawal of consent: tofacitinib 5 mg twice‐daily group (12), tofacitinib 10 mg twice‐daily group (0) Management of missing data: Quote (p 1398): "Efficacy analysis was performed on the full analysis set comprising patients who were randomised and received one or more doses of the study drug" (p 1400) "666 patients with moderate‐severe psoriasis were randomised to the initial period and received study medication". However only 662 patients were analysed for the outcomes. Comment: we judged this as a high risk of bias |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCTNCT01186744) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
BRIDGE 2017.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind Date of study: November 2012 ‐ November 2015 Setting: 57 centres in Austria, Germany, the Netherlands and Poland |
|
| Participants |
Randomised: 704 participants (mean age 44.5 years, 452 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Dimethyl fumarate (DMF) (n = 280), orally, maximum daily dose of 720 mg DMF Control intervention B. DMF + salt of monoethyl fumarate (n = 286), orally, maximum daily dose of 720 mg DMF C. Placebo (n = 138) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1) “This research was funded by Almirall S.A.”. Declarations of interest (p 1): "U.M. has been an advisor and/or received speaker honoraria and/or received grants and/or participated in clinical trials for the following companies: Abbott/AbbVie, Almirall Hermal, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Foamix, Forward Pharma, Galderma, Janssen, LEO Pharma, Lilly, Medac, Miltenyi Biotec, MSD, Novartis, Pfizer, Teva, UCB, VBL and XenoPort. J.C.S. receives advisory board/consulting fees from AbbVie, Biogen, Biogenetica International Laboratories, Egis Pharmaceuticals, Fresenius, LEO Pharma, Lilly, Novartis, Pierre Fabre, Polpharma, Sandoz and Toray Corporation; and receives speaker fees from AbbVie, Actavis, Adamed, Astellas, Berlin‐Chemie Menarini, Fresenius, Janssen‐Cilag, LEO Pharma, Mitsubishi Tanabe Pharma, Novartis, Pierre Fabre, Takeda and Vichy, and clinical trial funding from AbbVie, Actelion, Almirall, Amgen, GlaxoSmithKline, Janssen‐Cilag, Merck, Mitsubishi Tanabe Pharma, Novartis, Regeneron and Takeda. P.V.K. declares consultancy fees for Celgene, Centocor, Almirall, Amgen, Pfizer, Philips, Abbott, Lilly, Galderma, Novartis, Janssen‐Cilag, LEO Pharma, Sandoz and Mitsubishi Tanabe Pharma and carries out clinical trials for Basilea, Pfizer, Lilly, Amgen, AbbVie, Philips Lighting, Janssen‐Cilag and LEO Pharma. R.L." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 2): “Randomisation was performed by the investigators using an interactive web‐based response system.” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 2): “Randomisation was performed by the investigators using an interactive web‐based response system. The randomisation sequence was kept concealed from the investigators during the trial.” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 2): “Treatment was uptitrated over the first 9 weeks, with placebo or up to a maximum daily dose of 720 mg DMF in the LAS41008 or Fumaderm® groups” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 2): “Treatment was uptitrated over the first 9 weeks, with placebo or up to a maximum daily dose of 720 mg DMF in the LAS41008 or Fumaderm® groups” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 704, analysed 671 Management of missing data: Quote (p 4): “All statistical analyses were based on the full analysis set (FAS) and the per protocol set (PPS). As the results of both were consistent, data are presented here only for the FAS. A last‐observation‐carried‐forward approach was used to handle missing data for the PASI‐ and PGA‐derived end points.” DMF/DMF + MEF/placebo Randomised 280/286/138 Safety set analysis 279/283/137 (not‐treated participants excluded) Full set analysis 267/273/131 (not explained) Comment: not ITT analysis |
| Selective reporting (reporting bias) | High risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01726933). Some prespecified outcomes and those mentioned in the Methods section as DLQI had not been reported |
Cai 2016.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: 14 August 2012 ‐ 21 December 2013 Location: China |
|
| Participants |
Randomised: 425 participants (mean age 43 years, 310 men) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab (n = 338), SC, 40 mg, week 0, 2 injections, eow 1 injection Control intervention B. Placebo (n = 87), SC |
|
| Outcomes | Assessment at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 2): "Abbvie Inc participated in the study design, study research, collection, analysis and interpretation of data" Declarations of interest: Quote (p 2): "L Cai, J Gu, J Zheng, M Zheng, G Wang, L‐Y Xi, F Hao, X‐M Liu, Q‐N Sun, Y Wang, W Lai, H Fang, Y‐T Tu, Q Sun, J Chen and X‐H Gao were investigators for this study, and J‐Z Zhang was the principal investigator for this study; all declare no financial, professional or personal relationships that might be perceived as a conflict of interest. Y Gu and HD Teixeira receive a salary as employees of AbbVie and may also receive stock, stock options and/or stock grants. MM Okun is a former AbbVie employee." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 2 & Appendix): "The randomisation schedule was prepared by the Statistics Department of AbbVie, US. Randomization was performed using an adequate block size.“ Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 2 & Appendix): “An interactive voice/web response system determined patient randomisation. The randomisation schedule was prepared by the Statistics Department of AbbVie, US. Randomization was performed using an adequate block size.“ Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 2 & Appendix): “Patients in Period A were randomised 4:1 to receive adalimumab 40 mg every‐other‐week (following a single 80 mg dose), or matching placebo...All AbbVie personnel with direct oversight of the conduct and management of the trial (with the exception of the drug supply team), the investigator, study‐site personnel and the patient remained blinded to each patient’s treatment throughout the 12 week blinded period of the study." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 2 & Appendix): “Patients in Period A were randomised 4: 1 to receive adalimumab 40 mg every‐other‐week (following a single 80 mg dose), or matching placebo...All AbbVie personnel with direct oversight of the conduct and management of the trial (with the exception of the drug supply team), the investigator, study‐site personnel and the patient remained blinded to each patient’s treatment throughout the 12 week blinded period of the study.“ Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned: 425, analysed 425 (ITT) Quote (p 3): "Efficacy was analysed in Period A for all randomised patients [intent‐to‐treat (ITT_A Population)]... Missing data were handled using non‐responder imputation (NRI) for categorical variables and last‐observation‐carried‐forward (LOCF) for continuous variables." Comment: ITT analyses |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01646073) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Caproni 2009.
| Study characteristics | ||
| Methods | RCT, active‐controlled Date of study: not stated Location: not stated |
|
| Participants |
Randomised: 60 participants (age range 28 ‐ 67 years (etanercept), 32 ‐ 65 years (acitretin), 24 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 30), SC, 50 mg, twice a week, 12 weeks Control intervention B. Acitretin (n = 30), orally, 0.4 mg/kg/day, 12 weeks |
|
| Outcomes | Assessment at 12 weeks Primary and secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 211): "Patients were randomly assigned to one of the two groups" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: probably open‐label trial; term "blind" not used |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: probably open‐label trial; term "blind" not used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no description of the method used to manage the missing data. No ITT analyses mentioned |
| Selective reporting (reporting bias) | Unclear risk | Comment: no primary or secondary outcomes stated |
CARIMA 2019.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: April 2014 ‐ April 2016 Location: Germany (23 sites, multicentre) Phase 3 |
|
| Participants |
Randomised: 151 participants Key inclusion criteria
Key exclusion criteria
Baseline characteristics N = 151, mean age of 51.93 years and 67% men Dropouts and withdrawals
Secukinumab 300 group (1), Secukinumab 150 group (5), Placebo group (5)
|
|
| Interventions |
Intervention A. Secukinumab 300 (300 mg every week for 4 weeks followed by 300 mg secukinumab every 4 weeks until week 48) (n = 48) Control interventions B. Secukinumab 150 (150 mg every week for 4 weeks followed by 300 mg secukinumab every 4 weeks until week 48) (n = 54) C. Placebo (n = 49) |
|
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
|
| Notes | On ClinicalTrials.gov, results submitted without PASI or IGA outcomes Funding Quote (p 1061):"The CARIMA study was funded by Novartis Pharma GmbH, Germany. Medical writing assistance was provided by Evelyn Altemeyer, Novartis Ireland Ltd., and funded by Novartis Pharma GmbH, Germany, in line with Good Publication Practice 3 guidelines." Conflict of interest Quote (p 1061): "EVS received grants from the Deutsche Forschungsgemeinschaft. KR has served as advisor and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Affibody, Amgen, Biogen, Boehringer Ingelheim Pharma, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, Kyowa Kirin, Leo, Lilly, Medac, Merck Sharp & Dohme, Novartis, Ocean Pharma, Pfizer, Regeneron, Sanofi, Takeda, UCB Pharma, and Xenoport. DT has received research support/acted as Principal Investigator (clinical trials) from AbbVie, Almirall, Amgen, Astellas, Biogen‐Idec, Boehringer‐Ingelheim, Celgene, Dignity, Eli Lilly, Forward‐Pharma, GlaxoSmithKline, Leo, Janssen‐Cilag, Maruho, Merck Sharp & Dohme, Mitsubishi Pharma, Novartis, Pfizer, Roche, and Sandoz; has acted as a consultant for AbbVie, Biogen‐Idec, Celgene, Dignity, Maruho, Mitsubishi, Novartis, Pfizer, and Xenoport; has received honoraria from AbbVie, Biogen‐Idec, Celgene, Janssen, Leo, Pfizer, Roche‐Possay, Novartis, and Mundipharma; and has participated in scientific advisory boards for AbbVie, Amgen, Biogen‐Idec, Celgene, Eli Lilly, GlaxoSmithKline, Pfizer, Novartis, Janssen, Mundipharma, and Sandoz. WK served on the executive steering committee of JUPITER and CANTOS; served as a consultant for Amgen, DalCor, Kowa, Novartis, Pfizer, and Sanofi; and has received fees for lectures from Amgen, AstraZeneca, Novartis, Pfizer, and Sanofi. AP is a speaker for AbbVie, Almirall‐Hermal, Amgen, Biogen Idec, Celgene, Eli Lilly, Galderma, Janssen, Leo Pharma, Medac, Novartis, Pfizer, and UCB Pharma; served as an advisor for AbbVie, Almirall‐Hermal, Amgen, Celgene, Eli Lilly, Janssen, Leo Pharma, and Novartis; and has participated in clinical trials funded by AbbVie, Almirall‐Hermal, Amgen, Biogen Idec, Boehringer‐Ingelheim, Celgene, Glax‐ oSmithKline, Eli Lilly, Galderma, Hexal, Janssen, Leo Pharma, Medac, Merck Serono, Mitsubishi, Merck Sharp & Dohme, Novartis, Pfizer, Tigercat Pharma, Regeneron, Roche, Sandoz Biopharmaceuticals, Schering‐Plough, and UCB Pharma. AK has received honoraria from Novartis, Eli Lilly, Leo Pharma, Almirall, Janssen, UCB Pharma, Merck Sharp & Dohme, and Pfizer and has received fees for board participation from Novartis, Leo Pharma, Janssen, and Eli Lilly. TR has received fees and honoraria from AstraZeneca, Bayer, Boehringer Ingelheim, and Novartis. DY, JF, CS, and NM are employees of Novartis. NNM is a full‐time US government employee. TG has received grant support and speaker honoraria from Abbott Vascular." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 1059): "CARIMA was a multicenter, double‐blind, randomized, placebo‐ controlled, parallel‐group, exploratory trial in patients with plaque‐type psoriasis." Comment: No description |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 1059): "CARIMA was a multicenter, double‐blind, randomized, placebo‐ controlled, parallel‐group, exploratory trial in patients with plaque‐type psoriasis." Comment: No description |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1059): "CARIMA was a multicenter, double‐blind, randomized, placebo‐ controlled, parallel‐group, exploratory trial in patients with plaque‐type psoriasis." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1059): "CARIMA was a multicenter, double‐blind, randomized, placebo‐ controlled, parallel‐group, exploratory trial in patients with plaque‐type psoriasis." Quote (p 1060): " The FMD analysis was performed in a blinded fashion by a core laboratory (University Medical Center Mainz; see Supplementary Materials)." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dealing with missing data: Quote (p 1060 ‐ 1): "The full analysis set comprised all randomly assigned patients to whom treatment was administered. All analyses were as observed; missing values were not imputed. " Results for PASI 75 and 90 were reported as percentage number not reported impossible to state if all randomised particiants were analysed |
| Selective reporting (reporting bias) | High risk | Comment: The protocol for the study was available on ClinicalTrials.gov (NCT02559622). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported except for IGA. Results posted in ClinicalTrials.gov. |
CHAMPION 2008.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: unreported Location: multicentre (n = 28) in Europe and Canada |
|
| Participants |
Randomised: 271 participants (mean age 42, 178 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab (n = 108), SC, 80 mg at week 0, 40 mg at week 1 and 40 mg eow Control intervention B. Methotrexate (n = 110), orally, 7.5 ‐ 25 mg weekly C. Placebo (n = 53), SC and orally (same drug administration) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 561): "Abbott Laboratories funded this study and participated in the study design, data collection, data management, data analysis and preparation of the manuscript" Declarations of interest (p 558): "J.‐H.S., G.S., L.D., K.P. and J.‐P.O. have served as consultants for Abbott Laboratories. In addition, they have participated in continuing medical education events supported by unrestricted educational grants from Abbott. R.G.L. reports receiving fees as a consultant or advisory board member for Abbott, Amgen, Astellas, Boehringer‐ Ingelheim, Barrier Therapeutics and Genentech; he has received lecture fees from Abbott, Amgen/ Wyeth and Biogen‐Idec, and has been the principal investigator and received grants from Abbott, Amgen, Astellas, Centocor, Galderma and Genentech. K.U., M.K. and A.C. are employees of Abbott. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 559):"Randomisation was completed through a central computer‐generated scheme stratified by centre, with block sizes of four" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 559): "Patient numbers were centrally assigned by an interactive voice‐response system in consecutive order". Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 559): "Adalimumab (Humira; Abbott Laboratories) or matching placebo for SC injection was provided as sterile preservative‐free solution in prefilled syringes. Oral methotrexate tablets were supplied by Wyeth Pharma (Münster, Germany), and placebo tablets were supplied by Abbott GmbH & Co. KG (Ludwigshafen, Germany). Both the methotrexate and placebo tablets were administered as capsules (encapsulated tablets) as a single weekly dose. The capsules for both methotrexate and
placebo were supplied by Fisher Clinical Services (Basel, Switzerland)." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 559): "Adalimumab (Humira; Abbott Laboratories) or matching placebo for SC injection was provided as sterile preservative‐free solution in prefilled syringes. Oral methotrexate tablets were supplied by Wyeth Pharma (Münster, Germany), and placebo tablets were supplied by Abbott GmbH & Co. KG (Ludwigshafen, Germany). Both the methotrexate and placebo tablets were administered as capsules (encapsulated tablets) as a single weekly dose. The capsules for both methotrexate and
placebo were supplied by Fisher Clinical Services (Basel, Switzerland)." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 271, analysed 271 Management of missing data: Quote (p 562): "Data for 16 patients with missing week 16 assessments for PASI, including the 15 patients who discontinued and one additional patient in the methotrexate group, were imputed as nonresponse." Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00235820). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except for DLQI that was published in a second study |
Chaudhari 2001.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: single centre, New Jersey, USA |
|
| Participants |
Randomised: 33 participants (age mean 35 years (infliximab 10), 51 years (infliximab 5), 45 years (placebo), 23 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Infliximab (n = 11), IV, 5 mg/kg, weeks 0, 2, 6, 10 Control intervention B. Infliximab (n = 11), IV, 10 mg/kg, weeks 0, 2, 6, 10 C. Placebo (n = 11), IV, 20 mL, weeks 0, 2, 6, 10 |
|
| Outcomes | Assessment at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: Y Johnson and Johnson, Centocor Inc Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1843): "...were randomly assigned... by means of a lock‐of‐six randomisation scheme" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1843): "Placebo was supplied in a identical manner except that it did not contain IFX...The infliximab infusion solution was given by investigators unaware of treatment assignment..." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1843): "All assessments were done in a masked manner" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 33, analysed 33 Dropouts and withdrawals
Management of missing data: Quote (p 1844): "The primary analysis was done according to ITT, all randomised patients were included" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Chladek 2005.
| Study characteristics | ||
| Methods | RCT, active‐controlled Date of study: not stated Location: Prague, Czech Republic |
|
| Participants |
Randomised: 41 participants (mean age 50 years (A), 46 years (B), 44 years (C), 41 years (D), 24 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 12), 7.5 mg/week, 2.5 ‐ 2.5 ‐ 2.5 at 12 hours, for 13 weeks Control intervention B. Methotrexate (n = 12), 15 mg/week, 5 ‐ 5 ‐ 5 at 12 hours, 13 weeks C. Methotrexate (n = 7), 7.5 mg/week, once a week, for 13 weeks D. Methotrexate (n = 10), 15 mg/week, once a week, 13 weeks |
|
| Outcomes | Assessment at 13 weeks Primary or secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding: Czech Ministry of Education Declarations if interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 247): "were randomly assigned" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 247): "were randomly assigned" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: probably open‐label trial, term "blind" not used |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: probably open‐label trial, term "blind" not used |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no description of the method used to manage the missing data. No ITT analyses mentioned |
| Selective reporting (reporting bias) | Unclear risk | Comment: no primary or secondary outcomes stated |
CIMPACT 2018.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: January 2015 ‐ December 2016 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 559 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Certolizumab pegol (SC injection 400 mg at weeks 0, 2, 4, followed by certolizumab pegol 200 mg every 2 weeks from week 6 to week 14), n = 165 Control intervention B. Certolizumab pegol (SC injection 400 mg every 2 weeks through week 14), n = 167 C. Etanercept (SC injection 50 mg twice weekly through week 12), n = 170 D. Placebo, n = 57 |
|
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
|
| Notes | Funding source : Quote (p 226): "Funding sources: Supported by Dermira Inc and UCB Inc. UCB is the regulatory sponsor of certolizumab pegol in psoriasis." Conflicts of interest: Quote (p 226): "Dr Lebwohl is an employee of Mount Sinai which receives research funds from AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Incyte, Janssen/Johnson & Johnson, Leo Pharmaceutucals, Medimmune/Astra Zeneca, Novartis, Pfizer, Sciderm, UCB, Valeant, and ViDac; and is a consultant for Allergan, Aqua, Boehringer‐Ingelheim, LEO Pharma, Menlo, and Promius. Dr Blauvelt has received honoraria or fees for consulting, serving as a clinical investigator, and/or speaking for AbbVie, Aclaris, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira Inc, Eli Lilly and Company, Genentech/Roche, GSK, Janssen, LEO Pharma, Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, UCB, Valeant, and Vidac. Dr Paul is a consultant and investigator for AbbVie, Almirall, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Janssen/Johnson & Johnson, LEO Pharma, Novartis, Pierre Fabre, Pfizer, and Sanofi/Regeneron. Dr Sofen has received honoraria or fees for consulting, serving as a clinical investigator, and/or speaking for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Dermira Inc, Janssen, Eli Lilly, Merck, Novartis, Pfizer, Sun Pharma, UCB, and Valeant. Dr Węgłowska is an investigator and/or speaker for Amgen, Celgene, Coherus, Dermira Inc, Eli Lilly and Company, Galderma, Janssen, LEO Pharma, Merck, Pfizer, Regeneron, Sandoz, and UCB. Dr Piguet has received honoraria or fees for consulting and/or speaking for AbbVie, Almirall, Celgene, Janssen, Novartis, and Pfizer; and has received departmental support for Cardiff University from AbbVie, Almirall, Alliance, Beiersdorf UK Ltd, Biotest, Celgene, Dermal, Eli Lilly, Galderma, Genus Pharma, GlobeMicro, Janssen‐Celag, LaRoche‐Posay, L'Oreal, LEO Pharma, Meda, MSD, Novartis, Pfizer, Sinclair Pharma, Spirit, Stiefel, Samumed, Thornton Ross, TyPham, and UCB. Dr Augustin has received honoraria or fees for consulting and/or speaking for clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis, including AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly and Company, GSK, Hexal, Janssen‐Cilag, LEO Pharma, Medac, Merck, MSD, Mundipharma, Novartis, Pfizer, Sandoz, UCB BioSciences Inc, and Xenoport. Ms Drew and Dr Burge have received stock options from Dermira Inc. Mr Peterson owns stock in UCB Inc. Dr Rolleri has received stock options from UCB Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 286): "Study drug kits were distributed based on the subject’s interactive voice web response system assigned randomization number; the randomization schedule was produced by an independent biostatistician." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 286): "Study drug kits were distributed based on the subject’s interactive voice web response system assigned randomization number; the randomization schedule was produced by an independent biostatistician." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 268): "Double‐blind CZP and placebo treatments were administered subcutaneously at the study site by study personnel not involved in any other study procedures; etanercept treatment was administered subcutaneously on‐site by unblinded study staff or self‐administered off‐site by the patient after sufficient training. To maintain the single‐blind for etanercept, efficacy assessments were performed by a designated blinded assessor not involved in any other study procedures during blinded study periods." Comment: participants not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 268): "Double‐blind CZP and placebo treatments were administered subcutaneously at the study site by study personnel not involved in any other study procedures; etanercept treatment was administered subcutaneously on‐site by unblinded study staff or self‐administered off‐site by the patient after sufficient training. To maintain the single‐blind for etanercept, efficacy assessments were performed by a designated blinded assessor not involved in any other study procedures during blinded study periods." Comment: assessment by a blinded assessor |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote (p 269): "Analyses were based on the randomized set (all randomized patients)...Imputation of missing data was performed using the Markov chain Monte Carlo method for multiple imputation during the initial period " Included population 559, Table 2 559 Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02346240) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
CIMPASI‐1 2018.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: December 2014 ‐ October 2016 Location: World‐wide Phase 3 |
|
| Participants |
Randomised: 234 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Certolizumab pegol (400 mg at weeks 0, 2, 4, followed by certolizumab pegol 200 mg every 2 weeks from week 6 to week 14) (n = 95) Control intervention B. Certolizumab pegol (certolizumab pegol 400 mg every 2 weeks through week 14) (n = 88) C. Placebo (n = 51) |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 302): "Supported by Dermira Inc and UCB Inc." Conflicts of interest Quote (p 302): "Dr Gottlieb has consulted and/or received other fees from Janssen Inc, Celgene Corp, Bristol‐Myers Squibb Co, Beiersdorf Inc, AbbVie, UCB, Novartis, Incyte, Eli Lilly, Reddy Labs, Valeant, Dermira Inc, Allergan, and Sun Pharmaceutical Industries; and has received research or educational grants (paid to TuftsMedical Center) from Janssen Incyte, Lilly, Novartis, Allergan, and LEO Pharma. Dr Blauvelt has received honoraria or fees for consulting, being a clinical investigator, and/or speaker for AbbVie, Aclaris, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira Inc, Eli Lilly, Genentech/Roche, GlaxoSmith‐Kline, Janssen, LEO Pharma,Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, UCB Pharma, Valeant, and Vidac. Dr Leonardi has received fees or honoraria for consulting, speaking, or serving on the advisory board for AbbVie, Actavis, Amgen, Boehringer Ingelheim Pharma, Celgene, Coherus, Corrona, Dermira Inc, Eli Lilly, Galderma, Glenmark, Janssen, LEO Pharma, Merck, Novartis, Pfizer, Sandoz, Stiefel, UCB Pharma, Vitae, and Wyeth. Dr Poulin has received research grants as an investigator for AbbVie, Baxter, Boehringer Ingelheim Pharma, Celgene, Centocor/Janssen, Eli Lilly, EMD Serono, GlaxoSmithKline, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Takeda, and UCB Pharma; and has received honoraria speaking for AbbVie, Celgene, Janssen, Eli Lilly, LEO Pharma, Novartis, Regeneron, and Sanofi Genzyme. Dr Reich has received speaker’s fees or honoraria from and/or served on the advisory board for AbbVie, Amgen, Biogen, Boehringer Ingelheim Pharma, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Eli Lilly, Medac, Merck Sharp & Dohme, Novartis, Ocean Pharma, Pfizer, Regeneron, Takeda, UCB Pharma, and Xenoport. Dr Thac¸has received research support from AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Celgene, Dignity, Eli Lilly, Forward‐Pharma, GlaxoSmithKline, LEO Pharma, Janssen‐Cilag, Maruho, Merck Sharp & Dohme, Mitsubishi Pharma, Novartis, Pfizer, Roche, Regeneron, and Sandoz; received honoraria from AbbVie, Biogen, Celgene, Janssen, LEO Pharma, Pfizer, Roche‐Possay, Novartis, and Mundipharma; served as a consultant for AbbVie, Biogen, Celgene, Dignity, Galapagos, Maruho, Mitsubishi, Novartis, Pfizer, and Xenoport; and sat on the scientific advisory boards for AbbVie, Amgen, Biogen, Celgene, Eli Lilly, GlaxoSmithKline, LEO Pharma, Pfizer, Novartis, Janssen, Mundipharma, and Sandoz. Ms Drew and Dr Burge have received stock options fromDermira Inc. Mr Peterson owns stock in UCB Inc. Dr Arendt owns stock in and has received stock options from UCB Inc. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (pp 303‐4): " CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... At the baseline visit, an interactive voice web response system was used to assign patients to... according to the randomization schedule produced by an independent biostatistician (2:2:1, stratified by site)." Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (pp 303‐4): " CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... At the baseline visit, an interactive voice web response system was used to assign patients to... according to the randomization schedule produced by an independent biostatistician (2:2:1, stratified by site)." Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 303‐4): " CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... to assign patients to subcutaneous treatment with CZP 400 mg every 2 weeks, CZP 200 mg every 2 weeks (after loading dose of CZP 400 mg at weeks 0, 2, and 4), or placebo every 2 weeks until week 16 (initial treatment period)" Comment: Probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 303‐4): " CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... to assign patients to subcutaneous treatment with CZP 400 mg every 2 weeks, CZP 200 mg every 2 weeks (after loading dose of CZP 400 mg at weeks 0, 2, and 4), or placebo every 2 weeks until week 16 (initial treatment period)" Comment: Probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 234 Management of missing data: Quote (p 308): "Efficacy analyses were performed on the randomized set (all randomized patients)...The Markov chain Monte Carlo method for multiple imputation was used to account for missing data." Table 2: 234 analysed participants Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02326298) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
CIMPASI‐2 2018.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: December 2014 ‐ December 2016 Location: World‐wide Phase 3 |
|
| Participants |
Randomised: 227 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Certolizumab pegol (400 mg at weeks 0, 2, 4, followed by certolizumab pegol 200 mg every 2 weeks from week 6 to week 14) (n = 91) Control intervention B. Certolizumab pegol (certolizumab pegol 400 mg every 2 weeks through week 14) (n = 87) C. Placebo (n = 49) |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 302): "Supported by Dermira Inc and UCB Inc." Conflicts of interest Quote (p 302): "Dr Gottlieb has consulted and/or received other fees from Janssen Inc, Celgene Corp, Bristol‐Myers Squibb Co, Beiersdorf Inc, AbbVie, UCB, Novartis, Incyte, Eli Lilly, Reddy Labs, Valeant, Dermira Inc, Allergan, and Sun Pharmaceutical Industries; and has received research or educational grants (paid to TuftsMedical Center) from Janssen Incyte, Lilly, Novartis, Allergan, and LEO Pharma. Dr Blauvelt has received honoraria or fees for consulting, being a clinical investigator, and/or speaker for AbbVie, Aclaris, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira Inc, Eli Lilly, Genentech/Roche, GlaxoSmith‐Kline, Janssen, LEO Pharma,Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, UCB Pharma, Valeant, and Vidac. Dr Leonardi has received fees or honoraria for consulting, speaking, or serving on the advisory board for AbbVie, Actavis, Amgen, Boehringer Ingelheim Pharma, Celgene, Coherus, Corrona, Dermira Inc, Eli Lilly, Galderma, Glenmark, Janssen, LEO Pharma, Merck, Novartis, Pfizer, Sandoz, Stiefel, UCB Pharma, Vitae, and Wyeth. Dr Poulin has received research grants as an investigator for AbbVie, Baxter, Boehringer Ingelheim Pharma, Celgene, Centocor/Janssen, Eli Lilly, EMD Serono, GlaxoSmithKline, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Takeda, and UCB Pharma; and has received honoraria speaking for AbbVie, Celgene, Janssen, Eli Lilly, LEO Pharma, Novartis, Regeneron, and Sanofi Genzyme. Dr Reich has received speaker’s fees or honoraria from and/or served on the advisory board for AbbVie, Amgen, Biogen, Boehringer Ingelheim Pharma, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Eli Lilly, Medac, Merck Sharp & Dohme, Novartis, Ocean Pharma, Pfizer, Regeneron, Takeda, UCB Pharma, and Xenoport. Dr Thac¸has received research support from AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Celgene, Dignity, Eli Lilly, Forward‐Pharma, GlaxoSmithKline, LEO Pharma, Janssen‐Cilag, Maruho, Merck Sharp & Dohme, Mitsubishi Pharma, Novartis, Pfizer, Roche, Regeneron, and Sandoz; received honoraria from AbbVie, Biogen, Celgene, Janssen, LEO Pharma, Pfizer, Roche‐Possay, Novartis, and Mundipharma; served as a consultant for AbbVie, Biogen, Celgene, Dignity, Galapagos, Maruho, Mitsubishi, Novartis, Pfizer, and Xenoport; and sat on the scientific advisory boards for AbbVie, Amgen, Biogen, Celgene, Eli Lilly, GlaxoSmithKline, LEO Pharma, Pfizer, Novartis, Janssen, Mundipharma, and Sandoz. Ms Drew and Dr Burge have received stock options fromDermira Inc. Mr Peterson owns stock in UCB Inc. Dr Arendt owns stock in and has received stock options from UCB Inc. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (pp 303‐4): "CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... At the baseline visit, an interactive voice web response system was used to assign patients to... according to the randomization schedule produced by an independent biostatistician (2:2:1, stratified by site)." Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (pp 303‐4): "CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... At the baseline visit, an interactive voice web response system was used to assign patients to... according to the randomization schedule produced by an independent biostatistician (2:2:1, stratified by site)." Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 303‐4): "CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... to assign patients to subcutaneous treatment with CZP 400 mg every 2 weeks, CZP 200 mg every 2 weeks (after loading dose of CZP 400 mg at weeks 0, 2, and 4), or placebo every 2 weeks until week 16 (initial treatment period)" Comment: Probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 303‐4): "CIMPASI‐1 (NCT02326298) and CIMPASI‐2 (NCT02326272) are ongoing, replicate, phase 3, randomized, double‐blinded, multicenter... to assign patients to subcutaneous treatment with CZP 400 mg every 2 weeks, CZP 200 mg every 2 weeks (after loading dose of CZP 400 mg at weeks 0, 2, and 4), or placebo every 2 weeks until week 16 (initial treatment period)" Comment: Probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 227 Management of missing data: Quote (p 308): "Efficacy analyses were performed on the randomized set (all randomized patients)...The Markov chain Monte Carlo method for multiple imputation was used to account for missing data." Table 2: 227 analysed participants Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02326272). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
CLARITY 2018.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: July 2016 ‐ July 2018 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 1102 participants (mean age 46 years, 458 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab 300 (300 mg, SC at randomisation, weeks 1, 2 and 3 and thereafter 4‐weekly till week 48), n = 550 Control intervention B. Ustekinumab 45/90 (45 mg or 90 mg SC based on participant's weight (at randomisation visit) to be administered at randomisation, week 4, 16, 28 and 40), n = 552 |
|
| Outcomes |
Assessment at week 12 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 572): "Funding: Novartis Pharma AG, Basel, Switzerland." Declarations of interest: Quote (p 578): Disclosures. Jerry Bagel is an investigator and/or consultant and/or speaker for AbbVie, Amgen, Boehringer‐Ingelheim, Janssen, Leo, Novartis, Celgene, Eli Lilly, Sun, and Valiant. Manmath Patekar is an employee of Novartis Pharma AG, Basel, Switzerland. Ana de Vera is an employee of Novartis Pharma AG, Basel, Switzerland. Sophie Hugot is an employee ofNovartis Pharma AG, Basel, Switzerland. Isabelle Gilloteau is an employee of Novartis Pharma AG, Basel, Switzerland. Elisa Muscianisi is an employee of Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. Kuan Sheng is an employee of Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA. Summer Xia is an employee of Beijing Novartis Pharma Co. Ltd, Shanghai, China. Andrew Blauvelt has served as a scientific consultant and clinical study investigator for AbbVie, Aclaris, Akros, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira, Eli Lilly and Company, Galderma, Genentech/Roche, GlaxoSmithKline, Janssen, Leo, Meiji, Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Revance, Sandoz, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, UCB, Valeant, and Vidac and as a paid speaker for Janssen, Regeneron, and Sanofi Genzyme. Mark Lebwohl is an employee of Mount Sinai which receives research funds from AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Incyte, Janssen/Johnson & Johnson, Leo Pharmaceuticals, Medimmune/Astra Zeneca, Novartis, Pfizer, Sciderm, UCB, Valeant, and Vidac. Mark Lebwohl is also a consultant for Allergan, Aqua, Boehringer‐Ingelheim, LEO Pharma, Menlo, and Promius. John Nia and Peter W. Hashim have nothing to disclose. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 572): "CLARITY (NCT02826603) is a multicenter, randomized, double‐blinded, active‐controlled, parallel‐group, phase 3b trial. Eligible patients were randomized 1:1 to receive either..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 572): “CLARITY (NCT02826603) is a multicenter, randomized, double‐blinded, active‐controlled” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 572): “CLARITY (NCT02826603) is a multicenter, randomized, double‐blinded, active‐controlled” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1102 Management of missing data: Quote (p 573): "Missing values were handled by multiple imputation except for DLQI 0/1, where missing values were handled using last observation carried forward." Table 2: 1101 analysed participants Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02826603). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
CLEAR 2015.
| Study characteristics | ||
| Methods | (applé THACI clear ds cochrane)RCT, active‐controlled, double‐blind Date of study: 27 February 2014 – 11 May 2015 Location: 137 centres in Europe, Australia and Asia |
|
| Participants |
Randomised: 676 participants (mean age 46 years, 481 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab (n = 334), SC, 300 mg weeks 0, 1, 2, 3 then monthly Control intervention B. Ustekinumab (n = 335), SC, 45/90 mg weeks 0, 4 then every 12 weeks |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 400): "Novartis Pharma supported this study" Declarations of interest (p 400): "Dr Thaçi has served as a consultant, served as an advisory board member, and/or received honoraria for lecturing for AbbVie, Amgen, Biogen‐Idec, Celgene, Eli Lilly, Janssen‐Cilag, Leo Pharma, MSD, Novartis, Pfizer, Regeneron, and Sanofi. Dr Blauvelt has served as a scientific consultant and clinical study investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen Ortho Biotech, Merck, Novartis, Pfizer, and Sandoz. Dr Reich has served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis including AbbVie, Amgen, Biogen‐Idec, Celgene, Centocor, Covagen, Eli Lilly, Forward Pharma, GSK, Janssen‐Cilag, Leo Pharma, Medac, MSD, Novartis, Pfizer, Vertex, Takeda, and Xenoport..." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 402): “were randomised via an interactive response technology system" Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject to a treatment arm and specified unique medication pack number Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 402): “were randomised via an interactive response technology system “ Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 402) : “To maintain blinding, placebo injections matching the secukinumab regimen were given in the ustekinumab group” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 402) : “To maintain blinding, placebo injections matching the secukinumab regimen were given in the ustekinumab group” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 676, analysed 669 Management of missing data: Quote (p 403): “Missing values with respect to response variables based on PASI and IGA mod 2011 scores were imputed as nonresponse (nonresponder imputation)." Comment: It was not an ITT analysis as 7 participants were not taken into account, but low rate of dropout |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02074982) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Dogra 2012.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind Date of study: August 2008 ‐ September 2009 Location: Chandigarh, India |
|
| Participants |
Randomised: 60 participants (mean age 37 years, 48 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 30), orally, 10 mg/week, for 12 weeks Control intervention B. Methotrexate (n = 30), orally, 25 mg/week, for 12 weeks |
|
| Outcomes | Assessment at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: none declared Declarations of interest: none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 730): “The randomisation list was generated using a random number table, and the code was kept by an investigator who was not directly involved in the study” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 730): “The randomisation list was generated using a random number table, and the code was kept by an investigator who was not directly involved in the study. All tablets were supplied in sealed envelopes bearing the code for any particular patient according to the randomisation list” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 730‐1): “Double blind study, …, the 10 mg group was also given an oral placebo tablet in addition to the MTX to give an equal number of tablets in both groups. The placebo tablets were identical in appearance to the MTX tablets in colour, texture, size, shape and markings. All tablets were supplied in sealed envelopes bearing the code for any particular patient according to the randomisation list” Comment: clearly described |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 730‐1): “Double blind study, …, the 10 mg group was also given an oral placebo tablet in addition to the MTX to give an equal number of tablets in both groups. The placebo tablets were identical in appearance to the MTX tablets in colour, texture, size, shape and markings. All tablets were supplied in sealed envelopes bearing the code for any particular patient according to the randomisation list” Comment: clearly described |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 60, analysed 51 Dropouts and withdrawals
Management of missing data: no ITT analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Dogra 2013.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double blind Date of study: March 2008 ‐ March 2009 Location: Chandigarh, India |
|
| Participants |
Randomised: 61 participants (mean age 37 years, 51 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 20), orally, 25 mg/day, for 12 weeks Control intervention B. Acitretin (n = 20), orally, 35 mg/day, for 12 weeks C. Acitretin (n = 21), orally, 50 mg/day, for 12 weeks |
|
| Outcomes | Assessment at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding (quote e305): none declared Declarations of interest (quote e305): none declared |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p e306): “Randomization list was generated using random number table and code was kept with a study coordinator who was not directly involved in assessment of endpoint” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p e306): “Randomization list was generated using random number table and code was kept with a study coordinator who was not directly involved in assessment of endpoint” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (p e306): “double blind” Comment: no description of the method used to guarantee blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p e306): “double blind” “Randomization list was generated using random number table and code was kept with a study coordinator who was not directly involved in assessment of endpoint” Comment: no description of the method used to guarantee blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 61, analysed 48 Dropouts and withdrawals:
Not ITT analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Dubertret 1989.
| Study characteristics | ||
| Methods | RCT, active‐controlled Date of study: July 1987 ‐ January 1988 Location: Paris, France |
|
| Participants |
Randomised: 37 participants (mean age, sex ratio: not stated) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Cyclosporin (n = 18), orally, 2.5 mg/kg/d Control intervention B. Cyclosporin (n = 19), orally, 5 mg/kg/d |
|
| Outcomes | Time to assessment for the primary outcome: not stated Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: not stated, but 1 out of 4 authors was a staff member of Sandoz pharmaceutical company Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 136): "The patients were randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 136): "The patients were randomised..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not specified as blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: not specified as blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 37, analysed 37 Dropouts and withdrawals Not stated Management of missing data: no description of the method used to guarantee management of missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
ECLIPSE 2019.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: April 2017‐ September 2018 Location: world‐wide (142 sites) Phase 3 |
|
| Participants |
Randomised: 1048 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 1048, mean age of 46 years and 67% men Dropouts and withdrawals
Guselkumab 100 group (27), Secukinumab 300 group (48)
|
|
| Interventions |
Intervention A. Guselkumab 100mg (TREMFYA) S.C injection plus placebo (one injection) at weeks 0, 4, 12, and every 8 weeks thereafter until week 44, n=534 Control intervention B. Secukinumab 300mg (COSENTYX) administered as two 150mg S.C injections at weeks 0, 1, 2, 3, and 4, and every 4 weeks thereafter until week 44, n=514 |
|
| Outcomes |
At week 48 Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (p831):"This study was funded by Janssen Research & Development." Conflict of interest: " Quote (p838): "KR has served as an advisor and paid speaker and has participated in clinical trials for AbbVie, Affibody, Almirall, Amgen, Avillion, Biogen, Boehringer Ingelheim, Celgene, Covagen, Forward Pharma, Fresenius Medical Care, GlaxoSmithKline, Janssen, Janssen‐Cilag, Kyowa Kirin, LEO Pharma, Eli Lilly, Medac, Merck Sharp & Dohme, Novartis, Miltenyi Biotech, Ocean Pharma, Pfizer, Regeneron, Samsung Bioepis, Sanofi, Sun Pharma, Takeda, UCB, Valeant, XBiotech, and Xenoport. AWA has served as a consultant, research investigator, speaker, or data safety board member for AbbVie, Boehringer Ingelheim/Parexel, Bristol‐Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly, Genentech, GlaxoSmithKline, Janssen, Janssen‐Ortho, Kyowa Hakko Kirin, LEO Pharma, Menlo Therapeutics, Merck, Modernizing Medicine, Novartis Pharmaceutical Corp, Ortho Dermatologics, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, Science 37, UCB Pharma, and Valeant. RGL has served as principle investigator, as a speaker, and on the scientific advisory board for and received compensation in the form of honoraria from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Janssen, LEO Pharma, Eli Lilly, Merck, Novartis, Pizer, Sun, and UCB Pharma. SF, BR, SL, M‐CH, and PB are all employees of Janssen Research & Development and own stock in Johnson & Johnson, of which Janssen is a subsidiary. AB has served as a scientific advisor or clinical study investigator for AbbVie, Aclaris, Allergan, Almirall, Amgen, Arena, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly, FLX Bio, Galderma, Genentech/Roche, GlaxoSmithKline, Janssen, LEO Pharma, Meiji, Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Revance, Sandoz, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, UCB Pharma, Valeant, and Vidac, and as a paid speaker for Janssen, Regeneron, and Sanofi Genzyme." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p833): "Patients were randomly assigned (1:1) to receive either guselkumab or secukinumab. An outside vendor (Paraxel, Waltham, MA, USA) used an interactive web response system to randomly assign patients based on computer‐ generated permuted blocks." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p833): "An outside vendor (Paraxel, Waltham, MA, USA) used an interactive web response system to randomly assign patients based on computer‐ generated permuted blocks." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (p832, 833):"A phase 3, multicentre, randomised, double‐blind, comparator‐controlled study (ECLIPSE)... ." "Patients, investigators, and the funder of the study were masked throughout the 56‐week database lock, with the exception of the unmasked site personnel who dispensed or administered the study agent." Comment: unclear if the process guarented blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p832, 833):"A phase 3, multicentre, randomised, double‐blind, comparator‐controlled study (ECLIPSE)... ." "Patients, investigators, and the funder of the study were masked throughout the 56‐week database lock, with the exception of the unmasked site personnel who dispensed or administered the study agent." Comment: unsure that the process guarented the blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (p834, 835):" For efficacy analyses, we included all patients according to the random treatment allocation (intention‐to‐treat [ITT] population), regardless of the treatment received... Patients with missing data were considered non‐ responders (non‐responder imputation)." Randomly assigned 1048, analysed 1048 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03090100). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. Results are posted on ClinicalTrials.gov. |
EGALITY 2017.
| Study characteristics | ||
| Methods | Randomised, active‐controlled, double‐blind phase 3 trial date: 24 June 2013 to 30 March 2015 Location: 74 centres in 11 European countries and South Africa |
|
| Participants |
Total sample size: 531 Inclusion criteria
Exclusion Criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. GP2015, n = 264 Control intervention B. Etanercept ((Enbrel; Amgen Inc., Thousand Oaks, CA, USA; European Union authorised), n = 267 50 mg subcutaneous injection until week 12 |
|
| Outcomes |
Assessment at week 12 Primary outcome
Secondary outcomes
|
|
| Notes | Funding source: Quote (p 928): "The study was funded by Hexal AG, a Sandoz company. The funder had a role in the study design, data collection, data analysis and manuscript preparation." Conflict of interest Quote (appendix): "Dr Gerdes has been an advisor and/or received speakers’ honoraria and/or received grants and/or participated in clinical trials of the following companies: Abbott/AbbVie, Almirall‐Hermal, Amgen, Bayer HealthCare, Biogen Idec, Bioskin, Boehringer‐Ingelheim, Celgene, Centocor, Dermira, Eli Lilly, Foamix, Forward Pharma, Galderma, Hexal AG, Isotechnika, Janssen‐Cilag, Leo Pharma, Medac, Merck Serono, Mitsubishi Tanabe, MSD, Novartis, Pfizer, Sandoz Biopharmaceuticals, Schering‐Plough, Takeda, Teva, UCB Pharma, VBL therapeutics and Wyeth Pharma. Professor Thaci has received research support from Abbvie, Almiral, Amgen, Astellas, Biogen‐Idec, Boehringer‐ Ingelheim, Celgene, Dignity, Elli‐Lilly, Forward‐Pharma, GlaxoSmithKline, Leo, Janssen‐Cilag, Maruho, MSD, Mitsubishi Pharma, Novartis, Pfizer, Roche and Sandoz and honoraria from AbbVie, Biogen‐Idec, Celgene, Janssen, Leo, Mundipharma, Novartis, Pfizer and Roche‐Possay. Professor Thaci has acted as a consultant for Abbvie, Biogen‐Idec, Celgene, Dignity, Galapagos, Maruho, Mitsubishi, Novartis, Pfizer and Xenoport and been part of scientific advisory boards for AbbVie, Amgen, Biogen‐Idec, Celgene, Eli‐Lilly, GlaxoSmithKline, Janssen, Leo‐Pharma, Mundipharma, Novartis, Pfizer and Sandoz. Professor Griffiths has received consultancy/honoraria and/or research funding from Abbvie, Galderma, Janssen, LEO‐Pharma, Lilly, MSD, Novartis, Pfizer, Regeneron, Roche, Sandoz, Sun Pharmaceuticals and UCB Pharma. Professor Arenberger has received grants from Novartis. J Poetzl and H Woehling are employees of Hexal AG. G Wuerth and M Afonso were employees of Hexal AG at the time of the study.3 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 929‐Supplemental Appendix): "EGALITY was a multicentre, randomized, double‐blind, confirmatory efficacy and safety study conducted..In treatment period 1, patients were randomized 1 : 1 to self‐administer50 mg GP2015 or 50 mg ETN."; " During treatment period 1, patients were randomised via the Interactive Response Technology (IRT) that assigned a unique patient identification number in the IRT system with the treatment arm to which the patient had been assigned. Randomisation was stratified by body weight (<90 kg; ≥90 kg) and prior therapy (no prior systemic therapy, any prior systemic therapy including biologic immunomodulating agents, or prior treatment with a tumour necrosis factor [TNF antagonist])." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 929‐Supplemental Appendix): "EGALITY was a multicentre, randomized, double‐blind, confirmatory efficacy and safety study conducted..In treatment period 1, patients were randomized 1 : 1 to self‐administer50 mg GP2015 or 50 mg ETN."; " During treatment period 1, patients were randomised via the Interactive Response Technology (IRT) that assigned a unique patient identification number in the IRT system with the treatment arm to which the patient had been assigned. Randomisation was stratified by body weight (<90 kg; ≥90 kg) and prior therapy (no prior systemic therapy, any prior systemic therapy including biologic immunomodulating agents, or prior treatment with a tumour necrosis factor [TNF antagonist])" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 929): "EGALITY was a multicentre, randomized, double‐blind, confirmatory efficacy and safety study conducted..In treatment period 1, patients were randomized 1 : 1 to self‐administer50 mg GP2015 or 50 mg ETN." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 929): "EGALITY was a multicentre, randomized, double‐blind, confirmatory efficacy and safety study conducted..In treatment period 1, patients were randomized 1 : 1 to self‐administer50 mg GP2015 or 50 mg ETN." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 531 Management of missing data: Quote (Supplemental appendix): "The FAS during treatment period 1 included all randomised patients to whom the study treatment was assigned. For the primary endpoint analysis based on the FAS missing values with respect to the PASI response at week 12 were included as non‐responders regardless of the reason for missing data." Equivalence trial: Quote (p 931): "The primary efficacy analysis was based on the per protocol set (PPS), which consisted of all patients who completed the study until week 12 without major protocol deviations...The analysis was repeated on the full analysis set (FAS) following the intent‐to‐treat principle as a sensitivity analysis." Table 1: Both per protocol and full‐set analyses Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01891864) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. Results posted on ClinicalTrials.gov |
Elewski 2016.
| Study characteristics | ||
| Methods | Randomised, placebo‐controlled, double‐blind trial date: January 2014 to April 2016 Location: worldwide |
|
| Participants |
Total sample size: 217 Inclusion criteria
Exclusion Criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab, SC, 40 mg, eow for 25 weeks starting 1 week after initial loading dose of 80 mg, n = 109 Control intervention B. Placebo, n = 108 |
|
| Outcomes |
At week 12 mNAPSI 75, PGA of fingernails of clear or minimal PASI 75/90/100 for participants with baseline PASI at 5 |
|
| Notes | Funding source: Quote (p 90): "AbbVie funded this study and participated in the study design; study research; collection, analysis and interpretation of data; and writing, review, and approval of this article. All authors had access to the data and participated in the development, review, and approval of this article and in the decision to submit it for publication." Conflict of interest Quote (p 90): "Dr Elewski has received research funding (paid to her institution) from AbbVie, Amgen, Boehinger Ingelheim, Celgene, Incyte, Lilly, Merck, Novan, Novartis, Pfizer, Valeant, and Viament and honoraria for serving as a consultant to Anacor, Celgene, Lilly, Novartis, Pfizer, and Valeant. Dr Okun has received honoraria for serving on an advisory board and/or as a speaker for AbbVie, Crescendo Biosciences, Gilead Science, and UCB, and he is a former AbbVie employee. Dr Papp has received honoraria for serving on an advisory board or panel, serving as a consultant and speaker for and has received grants (as an investigator) from Allergan, Amgen, Celgene, Centocor, Eli Lilly, Galderma, Genentech, Janssen, LEO Pharma, Merck, Merck‐Serono, Novartis, Pfizer, Schering Plough, and Wyeth. In addition, Dr Papp has received honoraria (as a consultant) and grants (as an investigator) from Astellas, Apotex, Baxter, Boehringer Ingelheim, Kyowa Kirin, Regeneron, and UCB; received honoraria (for serving on an advisory board and panel) from AbbVie, Apotex, Baxter, Boehringer Ingelheim, and UCB; received honoraria (as a consultant) from AbbVie and Bristol‐Myers Squibb; received honoraria (as a speaker) from AbbVie, Astellas, and Janssen‐Cilag; and received grants (as an investigator) from Bristol‐Myers Squibb and GlaxoSmithKline Beecham. Mr Baker has received honoraria (for serving on an advisory board and panel) from Abbvie, Pfizer, Novartis, and Celgene. Dr Crowley has received honoraria (as a consultant and speaker) from AbbVie, Amgen, Celgene, Lilly, and Novartis and has received grants (as an investigator) from AbbVie, Amgen, Astra‐Zeneca, Boehringer Ingelheim, Celgene, Janssen, Lilly, Maruho, Merck, Novartis, Pfizer, Regeneron, and Sandoz. Dr Guillet has received grants (as an investigator) from AbbVie. Dr Sudaram is a former AbbVie employee. Dr Poulin has received grants (as an investigator) and honoraria (as a speaker and for serving on advisory boards) from AbbVie, Amgen, and Centocor/Janssen‐Ortho and has received grants (as an investigator) from Aquinox, Baxter, Boehringer Ingelheim, Bristol‐Myers‐Squibb, Celgene, DS Biopharma, Eli Lilly, Galderma, Genentech, GlaxoSmithKline Beecham, LEO Pharma, Medimmune, Merck, Novartis, Pfizer, Regeneron, Schering Plough, Serono, Takeda, and UCB Pharma. Ms Gu, Dr Geng, and Dr Williams are salaried employees of AbbVie and they receive stocks and stock options. Dr Rich has received honoraria (for serving on an advisory board) from AbbVie, Eli Lilly, Novartis, Sandoz, and Valeant; honoraria (as a consultant) from AbbVie, Novartis, Polichem, and Valeant; and grants (as an investigator) from AbbVie, Allergan, Amgen, Anacor, Cassiopea, Dusa, Eli Lilly, Galderma, Janssen, Leo, Meiji, Merck, Neothetics, Novartis, Pfizer, Psolar, Sandoz, Ranbaxy, and Viamet. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (pp 91‐2): "This was a phase 3, multicenter, double‐blind, randomized, parallel‐arm, placebo‐controlled trial...Randomization was determined by an interactive voice/web response system." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (pp 91‐2): "This was a phase 3, multicenter, double‐blind, randomized, parallel‐arm, placebo‐controlled trial...Randomization was determined by an interactive voice/web response system." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 91‐2): "This was a phase 3, multicenter, double‐blind, randomized, parallel‐arm, placebo‐controlled trial...The investigator, study site, and patients remained blinded to treatment." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 91‐2): "This was a phase 3, multicenter, double‐blind, randomized, parallel‐arm, placebo‐controlled trial...The investigator, study site, and patients remained blinded to treatment." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 217 Management of missing data: Quote (p 90): "The primary efficacy analysis was performed for the period A intent‐to‐treat population. The primary analysis and ranked secondary end points were tested in ranked order to control multiplicity, and missing data were handled by multiple imputation for all end points." Table 2: 217 analysed participants Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02016482) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results posted on ClinicalTrials.gov |
Ellis 1991.
| Study characteristics | ||
| Methods | RCT, active, controlled, double‐blind Date of study: not stated Location: single‐centre (University of Michigan Medical Center, Ann Arbor, USA) |
|
| Participants |
Randomised: 85 participants (mean age 46 years (cyclosporin 3), 42 years (cyclosporin 5), 46 years (cyclosporin 7.5), 43 years (placebo), 66 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ciclosporin (Sandimmun) (n = 15), orally, 7.5 mg/kg, 8 weeks Control intervention B. Ciclosporin (Sandimmun) (n = 20), orally, 5 mg/kg, 8 weeks C. Ciclosporin (Sandimmun) (n = 25), orally, 3 mg/kg, 8 weeks D. Vehicle (Sandimmun oral olive oil) (n = 25), orally, 8 weeks |
|
| Outcomes | Assessment at 8 weeks Primary or secondary outcomes not stated Outcomes
|
|
| Notes | Funding (p 277): Sandoz research Institute, the Babcock Dermatologic Endowment (Ann Arbor) and a Clinical research centre grant (M01‐RR‐00042) from the National Institutes of Health Declarations of interest: not stated (p 277) "Drs Ellis and Voorhees are consultants to Sandoz Pharmaceuticals corporation (the manufacturer of cyclosporine). |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 278): "patients were assigned numbers in consecutive order; each number had been preassigned to one of four treatments groups by means of a computer generated random code in blocks 17" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 278): "The preparation of cyclosporine and vehicle were identical …patients were blinded to their treatment" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 278): "Other physician who were blinded to group assignment and laboratory findings evaluated the patient" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 85, analysed not stated Dropouts and withdrawals Not stated Quote (p 279): "In the primary, intention‐to‐treat analysis" Management of missing data: no description of the method used to guarantee management of missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Engst 1994.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: not stated Location: not stated |
|
| Participants |
Randomised: 22 participants (mean age 45.9 years, 18 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ciclosporin A (n = 10), orally, 1.25 mg/kg/d (increase to 2.5 if PASI > 50% of initial PASI), 12 months Control intervention B. Ciclosporin A, (n = 12), orally, 2.5 mg/kg/d (increase to 5 if PASI > 50% of initial PASI), 12 months |
|
| Outcomes | Assessment period: not stated but longer than 16 weeks Primary or secondary outcomes of the trial: not stated Outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 189): "Patients enrolled in the study were randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 189): "Patients enrolled in the study were randomised..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not blinded (open‐label) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: not blinded (open‐label) |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk |
Dropouts and withdrawals
Management of missing data: no description of the method used to guarantee management of missing data, ITT analyses not mentioned |
| Selective reporting (reporting bias) | High risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section were not reported in Results section |
ERASURE 2014.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: June 2011 ‐ April 2013 Location: 88 centres worldwide (Erasure) |
|
| Participants |
Randomised: 738 participants mean age 45 years, 509 male Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab 300 (n = 245), SC, 300 mg, weeks 0, 1, 2, 3, 4 and every 4 weeks, 12 weeks Control intervention B. Secukinumab 150 (n = 245), SC, 150 mg, weeks 0, 1, 2, 3, 4 and every 4 weeks, 12 weeks C. Placebo (n = 248), SC, weeks 0, 1, 2, 3, 4 and every 4 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 326): "funded by Novartis Pharmaceuticals" Declarations of interest (p 337): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Langley received personal fees from Eli Lilly, Leo, Novartis, Janssen, Amgen, AbbVie, Celgene, Merck, Pfizer |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol and Appendix): "Randomization numbers were generated by the Interactive Response Technology (IRT) provider using a validated system, which automated the random assignment of subject numbers to randomisation numbers..." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (protocol and Appendix): "Randomization numbers were generated by the Interactive Response Technology (IRT) provider using a validated system, which automated the random assignment of subject numbers to randomisation numbers..." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol and Appendix): “Subjects, investigator staff, persons performing the assessments, and data analysts were blinded to the identity of the treatment from the time of randomisation until primary objective analyses" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol and Appendix): “Subjects, investigator staff, persons performing the assessments, and data analysts were blinded to the identity of the treatment from the time of randomisation until primary objective analyses" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 738 included/738 analysed Quote (p 329): "The analyses of the efficacy end points included all the patients who underwent randomisation according to the treatment assigned at randomisation... Missing values ... were conservatively imputed as nonresponses, regardless the reason of missing data" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01365455) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
ESTEEM‐1 2015.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: September 2010 ‐ December 2012 Location: 72 centres in USA, Canada, Australia, Belgium, France, UK, Italy, Germany |
|
| Participants |
Randomised: 844 participants (apremilast (562) mean age 46 years, 379 male; placebo (282) mean age 47 years, 194 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Apremilast (n = 562), orally, 30 mg, twice a day, 16 weeks Control intervention B. Placebo (n = 282), orally, twice a day, 16 weeks |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source quote (p 37): "This study was sponsored by Celgene Corporation" Declarations of interest (p 48): "Dr Papp has served as an investigator for Abbott (AbbVie), Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Galderma, Genentech, Incyte, Isotechnika, Janssen, LEO Pharma, Lilly, MedImmune, Merck Sharp & Dohme, Merck‐Serono, Novartis, Pfizer, Stiefel, and Wyeth; a consultant for Abbott, Amgen, Astellas, Biogen Idec, Boehringer Ingelheim, BMS, Celgene, Centocor, Forward Pharma, Galderma, Genentech, Incyte, Isotechnika, Janssen, Johnson &Johnson, Kyowa Kirin, LEO Pharma, Lilly, MedImmune, Merck Sharp & Dohme, Merck‐Serono, Novartis, Pfizer, Takeda Pharmaceuticals, UCB, and Wyeth; and a speaker for Abbott, Amgen, Astellas, Celgene, Centocor, Isotechnika, Janssen, Novartis, and Pfizer. Dr Reich has served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis including AbbVie, Amgen, Biogen Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Takeda, and Vertex. Dr Leonardi has served on the advisory board and as an investigator and/or speaker for Abbott, Amgen, Celgene,Centocor, Galderma, Genentech, GlaxoSmithKline, Lilly, Novartis, Novo Nordisk, Pfizer, Sirtris, Stiefel, Vascular Biogenics, and Wyeth." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 38): "ESTEEM 1 was.. multicenter, randomised, double‐blind, placebo controlled study". Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 38): "ESTEEM 1 was.. multicenter, randomised, double‐blind, placebo controlled study" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 38): "ESTEEM 1 was.. multicenter, randomised, double‐blind, placebo controlled study... Blinding was maintained until all patients discontinued or completed the week 52 visit" Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 38‐9): "ESTEEM 1 was.. multicenter, randomised, double‐blind, placebo controlled study... Blinding was maintained until all patients discontinued or completed the week 52 visit" Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 844 included/844 analysed Quote (p 39): "Efficacy data were assessed for the full analysis set (all randomised patients)...Missing data were handled with the last‐observation‐carried‐forward methodology" Comment: done |
| Selective reporting (reporting bias) | Unclear risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01194219) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except the number of participants with a psoriasis flare or rebound during placebo‐controlled phase |
ESTEEM‐2 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: 29 October 2012 – 25 March 2016 Location: 40 centres in Europe & USA |
|
| Participants |
Randomised: 413 participants (mean age 45 years, 276 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Apremilast (n = 275), orally, 30 mg twice a day until week 32 Control intervention B. Placebo (n = 138), orally (same drug administration) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1387): "This study was sponsored by Celgene Corporation" Declarations of interest (Appendix): C.P. has served as an investigator and consultant for AbbVie, Amgen, Celgene, Eli Lilly, Janssen, LEO Pharma, Novartis and Pfizer. J. Cather has been an investigator for Amgen, Celgene, Galderma, Merck, Novartis and Pfizer, and has served on advisory boards for AbbVie, Janssen, OrthoBiotech and Medac. M.G. has been an investigator for AbbVie, Allergan, Celgene, Dermira, Dr. Reddy’s Laboratories, Eli Lilly, Galderma, Janssen Pharmaceutical, Kythera, Kyowa Hakko Kirin Pharma, LEO Pharma, Merck, Novartis, Pfizer, Regeneron and Takeda, and has served as a speaker for AbbVie, Actelion, Amgen, Astellas, Galderma, Janssen Pharmaceutical, LEO Pharma, Novartis and Pfizer. Y.P. has been an investigator for AbbVie, Amgen, Astellas, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Centocor/Janssen, Eli Lilly, Galderma, Isotechnika, LEO Pharma, Merck, Novartis, Pfizer, Pharmascience, Regeneron, Schering and Stiefel/GSK, and has served as a speaker for AbbVie, Amgen, Galderma, Janssen, LEO Pharma and Novartis. U.M. has been an advisor for and/or received speaker honoraria from and/or received grants from and/or participated in clinical trials for Abbott/AbbVie, Almirall‐Hermal, Amgen, BASF, Biogen Idec, Celgene, Centocor, Eli Lilly, Forward Pharma, Galderma, Janssen, LEO Pharma, Medac, MSD, Miltenyi Biotech, Novartis, Pfizer, Teva, VBL and XenoPort. C.F. has served on the advisory board for and/or received speaker honoraria from Celgene, Novartis, Janssen and AbbVie. J. Crowley has been an investigator for AbbVie, Amgen, AstraZeneca, Celgene, Janssen, Maruho, Merck, Pfizer and Regeneron; has served on the advisory board for AbbVie, Amgen, Celgene and Lilly; and has been a speaker for AbbVie and Amgen." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 1388): "Patient were randomised (2:1) via an interactive voice response system..." Comment: no description of the method used to guarantee the random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote (p 1388): "Patient were randomised (2:1) via an interactive voice response system..." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1388) "identically matching placebo tablets twice daily during the placebo controlled phase" Comment: Probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1388): "double‐blind" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 413, analysed 411 Management of missing data: Quote (pp 1389‐90): "Efficacy assessments were conducted for the modified intention‐to‐treat population... The last‐observation‐carried‐forward methodology was used...." Comment: we judged this as a low risk of bias |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00235820) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
EXPRESS 2005.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: 32 centres in Europe and Canada |
|
| Participants |
Randomised: 378 participants (mean age 43 years, 268 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals (week 24)
|
|
| Interventions |
Intervention A. Infliximab (n = 301), IV, 5 mg/kg weeks 0, 2, 6 and every 8 weeks, 10 weeks Control intervention B. Placebo (n = 77), IV, equivalent, weeks 0, 2, 6 and every 8 weeks, 10 weeks |
|
| Outcomes | Assessments at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source (p 386): This study was funded by Centocor, and Schering‐Plough, Kenilworth, NJ, USA" Declarations of interest (p 386): "Consultancies: Dr Reich (Abbott, Biogen Idec, Centocor, Schring‐Plough, Essex, Serano, Wyeth), Dr Nestle (Biogen Idec, Centocor, Schring‐Plough, Genentech, Galderma)..." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1368): "An adaptative treatment allocation was used... The treatment assignment was stored electronically and the stored data were used to allocate future patients in such a way that the imbalance between treatment groups was kept to a minimum" “Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject to a treatment arm and specified unique medication pack number" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1368): "An adaptative treatment allocation was used... The treatment assignment was stored electronically and the stored data were used to allocate future patients in such a way that the imbalance between treatment groups was kept to a minimum" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1368): "The investigators, study site personnel, and patients remained blinded until the database lock at week 50... placebo group" Comment: probably done, placebo controlled trial |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1368): "The investigators, study site personnel, and patients remained blinded until the database lock at week 50... placebo group" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 378 included / 378 analysed Quote (p 1368): "The primary endpoint ... as well as.. were analysed on an intention‐to‐treat basis... In patients who discontinued the study agent ... the patients were regarded as not achieving the endpoints for binary responses" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
EXPRESS‐II 2007.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: not stated Location: 63 centres in Europe, USA, Canada |
|
| Participants |
Randomised: 835 participants (mean age 44 years, 551 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Infliximab (n = 313), IV, 3 mg/kg, weeks 0, 2, 6; 10 weeks Control intervention B. Infliximab (n = 314), IV, 5 mg/kg, weeks 0, 2, 6; 10 weeks C. Placebo (n = 208), IV, weeks 0, 2, 6; 10 weeks |
|
| Outcomes | Assessments at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding (p 31. e1) by Centocor, Inc, Malvern, Penn, and Schering‐Plough, Kenilworth, NJ. Declarations of interest (appendix): "Dr Menter has received consulting, research, and/or speaking support from Abbott Laboratories, Allergan Inc, Allermed, Amgen Inc, Astralis Inc, Berlex Inc, Biogen Idec Inc, Centocor Inc, Cephalon, Collagenex Pharmaceuticals, CombinatoRx, Connetics Corp, Corixa Corporation, Dermik Laboratories, Doak Dermatologics, Dow, Ferndale Laboratories Inc, Fujisawa Healthcare Inc, Galderma, Genentech Inc, Genzyme, GlaxoSmithKline, Ligand Pharmaceuticals, Medicis, Med‐Immune Inc, Novartis Pharmaceuticals, Otsuka Pharmaceutical Inc, Protein Design Labs, QLT USA, Regeneration Pharma AG, Roche Laboratories, Serono, Sinclair, Synta Pharma, Thermosurgery, 3M Pharmaceuticals, Vertex, XOMA, and Zars Inc. Dr Feldman has received consulting, research, and/or speaking support from Amgen, Centocor, and Biogen. Dr Papp's support is as follows: Abbott: Investigator, Consultant; Amgen: Investigator, Consultant, Speaker, Advisory Boards; Centocor: Investigator, Consultant, Speaker, Senior Medical Officer for Canada (non‐compensatory), Advisory Boards; Genentech: Investigator, Consultant, Speaker, Senior Medical Officer for Canada (non‐compensatory), Advisory Boards; Serono: Investigator, Consultant, Speaker, Advisory Boards; Schering: Investigatory, Consultant, Speaker, Advisory Boards; and Wyeth: Speaker, Advisory Boards. Dr Weinstein has received consulting, research, and/or speaking support from Allergan, Amgen, Centocor, Biogen, Genentech, Valeant, Collagenex, CombinatoRx, Fujisawa, Abbott, and QLT. Dr Gottlieb has received research support from and/or is a consultant and/or speaker for Amgen, Inc, BiogenIdec, Inc, Centocor, Inc, Genentech, Inc, Abbott Labs, Ligand Pharmaceuticals, Inc, Beiersdorf, Inc, Fujisawa Healthcare, Inc, Celgene Corp, Bristol Myers Squibb, Inc, Warner Chilcott, Paradigm, Wyeth Pharmaceuticals, Schering‐Plough Corp, Eisai, Roche, Sankyo, Medarex, Kemia, Celera, TEVA, Actelion, and Amarill. At the time of the study, Dr Gottlieb was affiliated with the Clinical Research Center, University of Medicine and Dentistry of New Jersey, Robert Wood Johnson Medical School, New Brunswick, NJ. Dr Guzzo, Dr Dooley, Ms Li, and Ms Arnold are employees of Centocor, Inc. Mr Evans was an employee of Centocor, Inc at the time this study was conducted and is currently an employee of Scios, Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 31; e2): "Randomizations were performed by ClinPhone (Lawrenceville, NJ), allocating patients using a minimization algorithm with a biased coin assignment by means of an interactive voice response system" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 31; e2): "Randomizations were performed by ClinPhone (Lawrenceville, NJ), allocating patients using a minimization algorithm with a biased coin assignment by means of an interactive voice response system" "Patients, investigators, and all study staff except pharmacists were blinded to treatment assignments" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 31. e2): "Patients, investigators, and all study staff except pharmacists were blinded to treatment assignments... to receive IFX 3 mg/Kg or 5mg/Kg or placebo" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 31. e2): "Patients, investigators, and all study staff except pharmacists were blinded to treatment assignments... to receive IFX 3 mg/Kg or 5mg/Kg or placebo" Comment: placebo‐controlled, probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 835 included / 835 analysed Quote (p 31.e3/4): "For patients who discontinued... these patients were considered as not meeting the respective end‐points regardless of the observed data" Comment: ITT |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Fallah Arani 2011.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: October 2006 ‐ February 2009 Location: Rotterdam/Eindhoven, Netherlands |
|
| Participants |
Randomised: 60 participants (mean age 41 years (methotrexate) and 43 years (fumarate), 36 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 30), orally, 15 mg/week, Weinstein schema 15 mg weekly in 3 equal doses of 5 mg each 12 hours apart, 16 weeks Control intervention B. Fumarate (n = 30), orally, 720 mg, 30 mg followed by 120 mg and max 720 mg after week 9, 16 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source (p 855): none Declarations of interest (p 855): "none declared" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 856): “patients were randomly assigned ... randomisation was performed centrally according to a computered‐generated randomisation list” Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 856): “Only the research nurse, who had no contact with the patients before randomisation had insight into the allocation schedule” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 856): “could not be blinded because treatment intake differed in both groups” Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 857): “by the same trained assessors (one trained physician and a research nurse in consensus in each site)” Comment: not specified whether "trained assessors" were blinded |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 60, analysed 51 Management of missing data: Quote (p 857): “Analysis was by Intention‐to‐treat...” Comment: ITT analysis not performed |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
FEATURE 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: May 2012 ‐ January 2013 Location: 32 centres in the USA/Germany/France/Estonia/India/Switzerland |
|
| Participants |
Randomised: 177 participants (mean age 45 years (secukinumab 300 mg), 46 years (secukinumab 150 mg), 47 years (placebo), 117 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab (n = 59), SC, 300 mg, weeks 1, 2, 3, 4, 8, 12 B. Secukinumab (n = 59), SC, 150 mg, weeks 1, 2, 3, 4, 8, 12 Control intervention C. Placebo (n = 59), SC, weeks 1, 2, 3, 4, 8, 12 |
|
| Outcomes | Assessment at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
AEs |
|
| Notes | Funding: Novartis Pharmaceuticals, Basel, Switzerland Declarations of interest (quote p 484): "A.B. has served as a scientific consultant and clinical study investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Janssen, Lilly, Merck, Novartis, Pfizer and Sandoz. J.C.P. has served as a consultant, investigator, speaker or advisory board member for Abbott, Biogen‐Idec (formerly Biogen), Centocor, Essex Pharma, Galderma, Janssen‐Cilag/Janssen‐Ortho, Merck‐Serono (formerly Serono), MSD, Novartis, Pfizer and Wyeth, and has received unrestricted research grants from Biogen‐Idec and Wyeth. A.B.G. has served as scientific consultant and/or clinical study investigator for Abbott, Abbvie, Actelion, Akros Pharma, Amgen, Astellas Pharma, Beiersdorf, BMS, Canfite, Celgene, Coronado BioSciences, CSL Behring, GSK, Immune Control, Incyte, Janssen‐Ortho, Lerner Medical Devices, Lilly ICOS, Merck, Novartis, Novo Nordisk, Pfizer, Teva, UCB, Vertex Pharmaceuticals and Xenoport. K.K. has served as a study investigator for Celgene, Hexal, Mitsubishi and Novartis. H.S. has served as a study investigator, consultant and speaker for Novartis. M.R.‐M. has served as a study investigator for Novartis. V.S., R.P., C.P. and S.C. are full‐time employees of Novartis. C.P. and S.C. own stock in Novartis" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 486): “were randomised via interactive response technology to one of the treatment arms...using a validate system that automated the random assignment of subject numbers to randomisation numbers” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 486): “were randomised via interactive response technology to one of the treatment arms...using a validate system that automated the random assignment of subject numbers to randomisation numbers” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 486): “Subjects, study management team, investigator staff, persons performing the assessments and data analysts were blinded...” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 486): “Subjects, study management team, investigator staff, persons performing the assessments and data analysts were blinded...” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 177, analysed 177 Dropouts and withdrawals
Management of missing data: Quote (supplemental appendix) "Missing values were imputed as non‐response for all efficacy analyses regardless of the reason of missing data" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01555125) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
FIXTURE 2014.
| Study characteristics | ||
| Methods | RCT, active, placebo‐controlled, double‐blind trial Date of study: June 2011 ‐ June 2013 Location: 231 centres worldwide (Fixture) |
|
| Participants |
Randomised: 1306 participants, mean age 44 years, 929 male Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Sekunimab 300 (n = 327), SC, 300 mg, weeks 0, 1, 2, 3, 4 and every 4 weeks, 12 weeks Control intervention B. Sekunimab 150 (n = 327), SC, 150 mg, weeks 0, 1, 2, 3, 4 and every 4 weeks, 12 weeks C. Etanercept 50 (n = 326), SC, 50 mg/week twice a week, 12 weeks D. Placebo (n = 326), SC, weeks 0, 1, 2, 3, 4 and every 4 weeks, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 326): "funded by Novartis Pharmaceuticals" Declarations of interest (p 337): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Langley received personal fees from Eli Lilly, Leo, Novartis, Janssen, Amgen, AbbVie, Celgene, Merck, Pfizer." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol and Appendix): "Randomization numbers were generated by the Interactive Response Technology (IRT) provider using a validated system, which automated the random assignment of subject numbers to randomisation numbers..." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (protocol and Appendix): “Subjects, investigator staff, persons performing the assessments, and data analysts were blinded to the identity of the treatment from the time of randomisation until primary objective analyses" "Randomization numbers were generated by the Interactive Response Technology (IRT) provider" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol and Appendix): “Subjects, investigator staff, persons performing the assessments, and data analysts were blinded to the identity of the treatment from the time of randomisation until primary objective analyses Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol and Appendix): “Subjects, investigator staff, persons performing the assessments, and data analysts were blinded to the identity of the treatment from the time of randomisation until primary objective analyses Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote (p 329): "The analyses of the efficacy end points included all the patients who underwent randomisation according to the treatment assigned at randomisation... Missing values ... were conservatively imputed as nonresponses, regardless the reason of missing data" 1306 included/1306 analysed Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01358578) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Flytström 2008.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: February 2002 ‐ February 2005 Location: multicentre (n = 5), Sweden |
|
| Participants |
Randomised: 84 participants (mean age: 48 years (methotrexate), 46 years (ciclosporin); 55 male) Inclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate + folic acid (n = 41), orally, 7.5 mg/kg /week (5 mg folic acid except days of methotrexate), 12 weeks Control intervention B. Ciclosporin (n = 43), orally, 3 mg/kg, divided into 2 doses, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding (p 121): "Financial support from the Swedish Psoriasis Association and the Welander foundation" Declarations of interest (p 116): "none declared" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 117): "Randomization was performed with the use of computer‐generated random numbers, numbers by calling a central telephone number" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 117): "Randomization was performed with the use of computer‐generated random numbers, numbers by calling a central telephone number" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 117): "Blinded assessors performed the PASI at baseline and monthly thereafter" Comment: no description of method used to guarantee no communication between care givers or participants and assessors |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 84, analysed 68 Management of missing data: not ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Gisondi 2008.
| Study characteristics | ||
| Methods | RCT, active‐controlled, investigator‐blinded pilot trial Date of study: February 2002 ‐ February 2005 Location: Verona, Italy |
|
| Participants |
Randomised: 60 participants (mean age 55 years (acitretin); 55 years (etanercept), 53 years (acitretin + etanercept), 33 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (25 mg) and acitretin (0.4 mg/kg) (n = 18), SC (etanercept) and orally (acitretin), twice a week (etanercept) and once a day (acitretin), 24 weeks Control intervention B. Acitretin (n = 20), orally, 0.4 mg/kg, once a day, 24 weeks C. Etanercept (n = 22), SC, 25 mg, twice a week, 24 weeks |
|
| Outcomes | Assessments at 24 weeks Primary outcomes of the trial ≥ PASI 75 improvement from baseline Secondary outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest (p 1345): "PG has received lecture fees from Merck‐Serono, Schering‐Plough, Wyeth. GG has received consultation and lecture fees from Abbott, Janssen‐Cilag, Merck‐Serono, Schering‐Plough, Wyeth." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1346): "Randomization was performed with the use of computer‐generated random numbers and block size of four patients" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 1346): "Randomization was performed with the use of computer‐generated random numbers and block size of four patients" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 1346): "The PASI assessor was blinded concerning the group allocation of the patient" Comment: acitretin provide visible AEs |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 60, analysed 60 Management of missing data, quote (p 1346): "An ITT analysis was performed" Comment: no description of the method used to manage the missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Goldfarb 1988.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: not stated |
|
| Participants |
Randomised: 38 participants (mean age 45 ‐ 48 years, 31 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 10), orally, 10 ‐ 25 mg/day, 8 weeks B. Acitretin (n = 16), orally, 50 ‐ 75 mg/day, 8 weeks Control intervention C. Placebo (n = 12), orally, daily, 8 weeks |
|
| Outcomes | Assessments at 8 weeks Primary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding sources, quote (p 655): "Supported in part by Hoffman‐La Roche Inc., Nutley, NJ, and the Babcock Dermatologic Endowment" Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 656): "21 patients were randomly and equally divided into 4 groups" Comment: no description of the method used to generate the sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 656): "21 patients were randomly and equally divided into 4 groups" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 656): "we have studied 38 patients in a double‐blind fashion" Comment: visible side effect of acitretin |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 656): "we have studied 38 patients in a double‐blind fashion" Comment: visible side effect of acitretin |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 38, analysed 38 No mention of how the missing data were managed |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Gordon 2006.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: March 2003 ‐ June 2004 Location: Multicentre (n = 18) in USA, Canada |
|
| Participants |
Randomised: 148 participants (mean age 44 years, 99 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab (n = 46), SC, 40 mg, 12 weeks, week 0: 2 injections, 1 injection eow B. Adalimumab, (n = 50), SC, 40 mg, 12 weeks, week 0, week 1: 2 injections, 1 injection weekly Control intervention C. Placebo (n = 52), SC, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding, Quote (p 598): "Supported by Abbott Laboratories" Declarations of interest (p 598): "Dr Gordon has received research support and honoraria and is a consultant for Abbott. Dr Langley is an investigator and has received research funding to conduct research studies with Abbott. Dr Leonardi is a consultant and speaker for Abbott. Dr Menter has received honoraria and is a consultant for Abbott. Dr Kang is an ad‐hoc consultant for Abbott. Dr Heffernan is a consultant for and has received research funding from Abbott. Drs Zhong, Hoffman, and Okun and Ms Lim are full‐time employees of Abbott." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 599): "Patients were centrally randomised..." Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 599): "Patients were centrally randomised..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 599): "To maintain blinding, prefilled syringes were identically labelled and all patients received the same number of injections at the same time points" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 599): "To maintain blinding, prefilled syringes were identically labelled and all patients received the same number of injections at the same time points" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 148, analysed 147 Dropouts and withdrawals
Management of missing data, quote (p 601): "modified intent‐to‐treat analysis... a patient with missing data was counted as a nonresponder at that visit" Comment: few lost to follow‐up, well‐balanced number and reasons between groups |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Gordon X‐PLORE 2015.
| Study characteristics | ||
| Methods | RCT, active placebo‐controlled, double‐blind Date of study: October 2011 ‐ August 2013 Location: multicentre (n = 31), Europe and North America |
|
| Participants |
Randomised: 293 participants (mean age 47 years, 207 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Guselkumab (n = 41), SC, 5 mg weeks 0, 4, 16 Control intervention B. Guselkumab (n = 41), SC, 15 mg weeks 0, 4, 16 C. Guselkumab(n = 42), SC, 50 mg weeks 0, 4, 16 D. Guselkumab (n = 42), SC, 100 mg weeks 0, 4, 16 E. Guselkumab (n = 42), SC, 200 mg weeks 0, 4, 16 F. Adalimumab (n = 43), SC, 40 mg 2 injections week 0, 1 injection week 1, 1 injection eow G Placebo (n = 42), SC (100 mg weeks 0, 4, 16) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 137): “This study was sponsored by Janssen Research and Development. Janssen supplied the study agents and collected and analysed the data. All the authors had full access to the data”. Declarations of interest (p 144): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Gordon received grants and personal fees from Abbvie, Amgen, Celgene, Eli Lilly, Novartis; and personal fees from Pfizer and Medac. Reich received personal fees from Celgene, Centocor/Janssen, Forward Pharma, GSK, Janssen Cilag, LEO Pharma, Lilly Medoc, MSD, Novartis, Ocean Pharma, Pfizer, Regeneron, Takeda, Vertex. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 137): “patients were randomised…” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 137): “patients were randomised…” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 137, p 143): “double‐blind… Adalimumab was not administered in a blinded, placebo‐controlled manner”, “Another potential issue was to use of a blinded efficacy evaluator at each site instead of the administration of ADA in a blinded manner” Quote (p 553‐4): "Double Blind (Subject, Caregiver, Investigator, Outcomes Assessor ), Patients and study personnel were masked to treatment assignment: the study drug packaging was labelled.... " Comment: adalimumab group was not double‐blind |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 137): “to ensure objectivity, all efficacy assessment were performed by an evaluator at each study site who was unaware of the study group” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 293, analysed 293 Dropouts and withdrawals
Management of missing data: Quote (p 138): “Patients with missing PGA or PASI score at week 16 were categorized as not having had a response” Comment: low number of withdrawals, balanced number and reasons between groups |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01483599) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Gottlieb 2003a.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: August 2000 ‐ January 2001 Location: multicentre (locations not specified) |
|
| Participants |
Randomised: 112 participants (mean age 47 years, 70 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 57), SC, auto‐administered, 25 mg twice a week, 24 weeks Control intervention B. Placebo (n = 55), SC, auto‐administered, twice a week, 24 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial At 4, 8, 12, 24 weeks
|
|
| Notes | Funding source, quote (p 1631): "This study was sponsored by Immunex Corp, a subsidiary of Amgem, Inc.)" Declarations of interest not stated except "Dr Zitnik is an employee of Amgen" (p 1627) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1628): "Patients ... were to be randomised in block of 6 with equal allocation between the treatment group...Patients were assigned numbers based on randomisation tables verified by Immunex Pharmaceutical Planning" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 1628): "Patients ... were to be randomised in block of 6 with equal allocation between the treatment group...Patients were assigned numbers based on randomisation tables verified by Immunex Pharmaceutical Planning, after which the Immunex Clinical Distribution Department shaped blind‐labelled vials of study drug to the pharmacies". Comment: we do not know whether the investigators were blinded or the numbers of participants per block. This probably was a centralised randomisation but this is not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1628): "... performed blinded labelling and packaging of the study drug. ... multicenter, randomised, double‐blind" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1628): "... performed blinded labelling and packaging of the study drug. ... multicenter, randomised, double‐blind" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 112, 112 participants analysed for the primary endpoint Dropouts and withdrawals
Management of missing data: Quote (p 1628): "Patients were analysed on an intent‐to‐treat basis... If a patient discontinued treatment before the end of the study, the last observation was carried forward for efficacy analyses" Comment: high rate of withdrawal in placebo group and imbalanced reasons for withdrawal |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Gottlieb 2004a.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: 2001 ‐ 2003 Location: 24 centres in USA |
|
| Participants |
Randomised: 249 participants (mean age 44 years, 174 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals after a 30‐week study period
Reasons
|
|
| Interventions |
Intervention A. Infliximab (n = 99), IV, 3 mg/kg, weeks 0, 2, 6, for 10 weeks Control intervention B. Infliximab (n = 99), IV, 5 mg/kg, weeks 0, 2, 6, for 10 weeks C. Placebo (n = 51), IV, equivalent, weeks 0, 2, 6, for 10 weeks |
|
| Outcomes | Assessments at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, Quote (p 534): "Supported by Centocor Inc" Declarations of interest (p 534): "Drs Gottlieb and Menter have received research support from and served as consultants for Centocor Inc. Drs Baker, Bala, Dooley, Evans, Guzzo, and Marano, and Ms Li, are employees of Centocor Inc. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 535): "Randomisation was carried out using adaptive treatment allocation and was stratified by the investigational site". Comment: no description of the method used to generate random sequence |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 535): "Randomissation was carried out using adaptive treatment allocation and was stratified by the investigational site". Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 535): "Patients and investigators were unaware of treatment assignments. Double blind was achieved and maintained by using an independent pharmacist or staff member to prepare all study infusion" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 535): "Patients and investigators were unaware of treatment assignments. Double blind was achieved and maintained by using an independent pharmacist or staff member to prepare all study infusion" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 249 randomised, 249 analysed Methods for dealing with missing data: Quote (p 536): "All randomised patients were included in the efficacy analysis at week 10... Patients who discontinued... were considered to have not achieved the dichotomous end points or were assigned the baseline value for continuous end points after the event occurrence" Comment: done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Gottlieb 2011.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: June 2008 ‐ March 2009 Location: 33 centres in the USA |
|
| Participants |
Randomised: 209 participants (mean age 43.5 years, 145 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 141), SC, auto‐administered, 50 mg twice a week, 11 weeks Control intervention B. Placebo (n = 68), SC, auto‐administered, twice a week |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial At 4, 8, 12 weeks
|
|
| Notes | Funding source, quote (Appendix 1): "Abbott Laboratories funded this study and participated in the study design, data collection, data management, data analysis and preparation of the manuscript. All of the authors had full access to the data and were involved in the analysis of data, development and revision of the manuscript, and decision to submit the manuscript for publication. The corresponding author takes responsibility for the integrity of the data and the accuracy of the data analysis..)" Declarations of interest, quote (Appendix 1): "A.B.G. has been a consultant or served on an advisory board for Amgen, Centocor, Celgene, Bristol Myers Squibb, Beiersdorf, Abbott, TEVA, Actelion, UCB, Novo Nordisk, Immune Control, DermiPsor, Incyte, PureTech, Magen Biosciences, Cytokine Pharmasciences, Alnylam, Ono, Pfizer, Schering, Canfite, Schering, UCB, BIND Biosciences and Merck, and has received research/educational grants (paid to Tufts Medical Center) from Centocor, Amgen, Immune Control, Abbott, Novo Nordisk, UCB and Novartis. C.L. has been an investigator for Abbott, Allergan, Altana, Alza, Amgen, Astellas, Celgene, Centocor, Genentech, Bristol Myers, Eli Lilly, Galderma, Genzyme, Pfizer, Incyte, CombinatoRx, 3M Pharmaceuticals, Perrigo Israel Pharmaceutical, ScheringPlough, RTL, Novartis, Vitae and Wyeth; has served on an advisory board and has been a speaker for Abbott, Amgen and Centocor; and has been a consultant for Abbott, Amgen, Centocor and Pfizer. F.K. has been an investigator for Abbott, Centocor, Amgen, Wyeth, Novartis and Merck; and has served on an advisory board and has been a speaker for Abbott, Centocor, Amgen, Eisai, Astellas and Wyeth. S.M. has been an investigator for Abbott, Amgen, Celgene, Centocor, Graceway and Novo Nordisk; and has been a speaker for Abbott. M.O. and D.A.W. are employees of Abbott." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 653): "Patients were randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 653): "Patients were randomised" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 653): “Patients enrolled in the placebo arm received SC injections matching active treatment to maintain the blind. To maintain the blind, all patients received two SC injections at weeks 0 and 4 and one SC injection at week 8, consisting of either briakinumab or matching placebo, depending on the treatment arm. In addition, each patient also received two SC injections biweekly, 3 days apart, week 0 through week 11, consisting of either etanercept or matching placebo, depending on the treatment arm.” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 653): “Patients enrolled in the placebo arm received SC injections matching active treatment to maintain the blind. To maintain the blind, all patients received two SC injections at weeks 0 and 4 and one SC injection at week 8, consisting of either briakinumab or matching placebo, depending on the treatment arm. In addition, each patient also received two SC injections biweekly, 3 days apart, week 0 through week 11, consisting of either etanercept or matching placebo, depending on the treatment arm.” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 209, analysed 209 Management of missing data: Quote (p 654): “The primary efficacy analysis consisted of four comparisons performed in the intent‐to‐treat population (i.e. all randomised patients), …, Nonresponder imputation was used to handle missing data.” Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00691964) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Gottlieb 2012.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: November 2010 – December 2011 Location: Multicentre in Boston, USA |
|
| Participants |
Randomised: 478 participants (methotrexate: mean age 43 years and 153 male; placebo: mean age 45 years and 167 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 239), orally, 15 mg/week 7.5 mg ‐ 10 mg to a maximum of 15 mg, 24 weeks + etanercept, SC, 50 mg x 2/weeks, S1 ‐ S12 and 50 mg/week, S12 ‐ S24, 24 weeks Control intervention B. Placebo (n = 239), orally, 24 weeks + etanercept, SC, 50 mg x 2/weeks, S1 ‐ S12 and 50 mg/week, S12 ‐ S24, 24 weeks |
|
| Outcomes | Assessments at 24 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 649): "This study was funded by Immunex Corporation, a wholly owned subsidiary of Amgen Inc, and by Wyeth, which was acquired by Pfizer..." Declarations of interest (Appendix): "A.B.G. is a consultant and/or advisory board member for Abbott, Actelion, Amgen, Astellas, Beiersdorf, Bristol‐Myers Squibb, Can‐Fite, Celgene, Centocor (Janssen), Dermipsor, Incyte, Lilly, Merck, Novartis, Novo Nordisk, Pfizer, TEVA, and UCB and is a recipient of research/educational grants paid to Tufts Medical Center by Abbott, Amgen, Celgene, Centocor (Janssen), Immune Control, Novartis, Novo Nordisk, Pfizer, and UCB. R.G.L. has served as an investigator, on the scientific advisory board, and speaker for Abbott, Amgen, Centocor, and Pfizer, and as an advisor and investigator for Celgene, Novartis, and Johnson & Johnson. B.E.S. has served as an advisor, consultant, investigator, and speaker for Abbott, Amgen, and Centocor, and as an advisor, consultant, and investigator for Celgene, Novartis, Maruho, and Pfizer. K.A.P. has been a consultant, advisory board member, and investigator for Abbott, Amgen, Celgene, Centocor, Janssen‐Ortho, MedImmune, Merck, Pfizer, Schering‐Plough, and Wyeth (Wyeth was acquired by Pfizer in October 2009); has consulted for Astellas and UCB; and has served as a speaker for Abbott, Amgen, Celgene, Janssen‐Ortho, Pfizer, Schering‐Plough, and Wyeth. P.K., K.C., E.H.Z.T., M.H., and G.K. are employees and stockholders of Amgen Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 650): "This was a randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 650): "This was a randomised...study" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 650): “double‐blinded placebo‐controlled” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 650): “double‐blinded placebo‐controlled” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 478, analysed 478 Management of missing data: Quote (p 651): “Efficacy analyses were performed using the ITT set (all randomised patients)... Missing postbaseline data were imputed using last observation carried forward for primary analyses of all efficacy endpoints...” Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01001208) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Gurel 2015.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, single‐blind Date of study: not stated Location: one centre, Turkey |
|
| Participants |
Randomised: 50 participants (mean age 43 years, 25 male) Inclusion criteria
Exclusion criteria
Dropouts No participants lost to follow‐up |
|
| Interventions |
Intervention Acitretine (0.3 ‐ 0.5 mg/kg/day, 25 mg) (n = 25) Control intervention Placebo (n = 25) Co‐invervention NBUVB |
|
| Outcomes | Assessment at 12 weeks Primary outcome
Outcomes:
|
|
| Notes | Funding: none Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 3): "The physicians were not blinded" Comment: high risk of performance bias |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "An independent assessor who is not from the team performed the outcome assessment." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomised 50, analysed 50, no loss to follow‐up during the 12 weeks Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Heydendael 2003.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: October 1998‐June 2000 Location: multicentre (> 1) in Amsterdam/the Netherlands |
|
| Participants |
Randomised: 88 participants, mean age 40 years, 57 male Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 44), orally, 15 mg/week until 4 weeks then increase up to 22.5 mg if reduction from baseline PASI < 25%, 3 divided doses with 12‐h interval, 12 weeks Control intervention B. Ciclosporin (n = 44), orally, 3 mg/kg until 4 weeks then increase up to 5 mg/kg if reduction from baseline PASI < 25%, 2 divided doses, 12 weeks |
|
| Outcomes | Assessments at weeks 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding sources, Quote (p 664): "Supported by a grant (OG 97‐009) from the Dutch Health Authorities" Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 660): "Randomisation was performed centrally with the use of computer‐generated random numbers and block size of eight patients" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 660): "Randomisation was performed centrally with the use of computer‐generated random numbers and block size of eight patients" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 660): "The score of the PASI ... was determined... by trained assessors who were unaware of the treatment assignment" Comment: no description of method used to guarantee no communication between care givers or participants and assessors |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 88 randomised, 85 analysed Quote (pp 660‐1): "If a patient missed a visit, we used the score from the previous visit". Comment: few lost to follow‐up, well‐balanced number and reasons between groups |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Hunter 1963.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: not stated Location: 1 centre in London, UK |
|
| Participants |
Randomised: 41 participants (no description of the study population) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 19), orally, 2.5 mg every day for 1 week and 1 week after Control intervention B. Placebo (n = 17), orally, every day for 1 week and 1 week after |
|
| Outcomes | Assessments not clearly stated (reported at 4 weeks) Primary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee random sequence generation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 1 and 2): “Control tablet of identical appearance... thus neither physician, patient nor pharmacist was aware whether drug or control had been dispensed” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 1 and 2): “Control tablet of identical appearance... thus neither physician, patient nor pharmacist was aware whether drug or control had been dispensed” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 41 randomised participants and 38 analysed Comment: no description of the method used to manage missing data Not ITT analyses |
| Selective reporting (reporting bias) | High risk | No pre‐specified outcomes mentioned in the Methods section |
Igarashi 2012.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: March 2008 ‐ March 2010 Location: 35 centres in Japan |
|
| Participants |
Randomised: 160 participants (age median 45 years, 126 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab (n = 64), SC, 45 mg, weeks 0 ‐ 4, every 12 weeks, 64 weeks Control intervention B. Ustekinumab (n = 62), SC, 90 mg, weeks 0 ‐ 4, every 12 weeks, 64 weeks C. Placebo (n = 32), SC, weeks 0 ‐ 4, every 12 weeks, 64 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, Quote (p 242): "This study was supported by Janssen pharmaceutical KK, a part of the Johnson & Johnson family of companies. Declarations of interest (p 242): "Igarashi has served as a consultant and speaker for Janssen Pharmaceutical K.K.; H. Nakagawa has served as a consultant for Abbott Japan and Tanabe Mitsubishi, and as a consultant and speaker for Janssen Pharmaceutical K.K.; M. Song is an employee of Centocor Research & Development, Inc., a division of Johnson & Johnson Pharmaceutical Research & Development, L.L.C., and owns stock in Johnson & Johnson; T. Kato and M. Kato are employees of Janssen Pharmaceutical K.K. and own stock in Johnson & Johnson." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 244): “randomised” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 244): “randomised” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 243): “double‐blind placebo‐control” Comment: used a placebo without visible side effect |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 243): “double‐blind placebo‐control” Comment: used a placebo without visible side effect |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 160 randomised, 157 analysed (2 did not received a dose of the drug and 1 was excluded in the placebo group due to lack of efficacy data after receiving a single dose) Methods for dealing with missing data Quote (p 244): “Efficacy analyses were based on all randomised patients with efficacy data after randomisation... Patients who discontinued the study... were considered as treatment failures” Comment: few lost at follow‐up, well‐balanced number and reasons between groups. |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Ikonomidis 2017.
| Study characteristics | ||
| Methods | RCT, active‐controlled, single‐blinded trial Date of study: January 2013 ‐ still ongoing Location: 1 centre, Athens, Greece |
|
| Participants |
Randomised: 150 participants (age median 51 years, 93 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab 45 mg, SC, at baseline and at 4 and 16 weeks (n = 50) Control intervention B. Etanercept 50 mg SC, 2 days a week for 16 weeks (n = 50) C. Cyclosporine 2.5 to 3 mg/kg daily (n = 50) for 16 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, Quote (p 12): "This study was supported by a grant from the Hellenic Cardiology Society and Hellenic Society of Lipidiology and Atherosclerosis. This study was not funded by any pharmaceutical company and that none of the coauthors received support from the manufacturers of the agents used for treatment" Declarations of interest (p 12): "none" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 5) "Patients were randomized to receive ... Randomization was performed by an attending dermatologist (E.P.) using a table of random numbers as reproduced from the online randomization software http://www.graphpad.com/quickcalcs/ index.cfm." Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 5) "Patients were randomized to receive ... Randomization was performed by an attending dermatologist (E.P.) using a table of random numbers as reproduced from the online randomization software http://www.graphpad.com/quickcalcs/ index.cfm." Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 5): "Studies were performed using a Vivid 7 (GE Medical Systems, Horten, Norway) ultrasound system. All studies were digitally stored in a computerized station (Echopac 201; GE Medical Systems, Horten, Norway) and were analyzed by 2 observers, blinded to clinical and laboratory data." Comment: participants not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 5): "Studies were performed using a Vivid 7 (GE Medical Systems, Horten, Norway) ultrasound system. All studies were digitally stored in a computerized station (Echopac 201; GE Medical Systems, Horten, Norway) and were analyzed by 2 observers, blinded to clinical and laboratory data." Comment: participants not blinded. Physicians were blinded for cardiac outcomes, but not for PASI evaluation, so rated high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote (p 6): "All analyses were intention to treat." No statement on number of missing data and how authors dealt with it |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02144857) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
IMMerge 2021.
| Study characteristics | ||
| Methods | RCT, active‐controlled, single‐blind study (outcomes assessor) Date of study: March 2018 ‐ March 2020 Location: worldwide (64 sites) Phase 3 |
|
| Participants |
Randomised: 327 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 327, mean age of 47 years and 65% men Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Risankizumab (2 SC injections of 75 mg (150 mg total) at weeks 0 and 4, and every 12 weeks thereafter until the last dose at week 40, except for participants in France, who received additional doses at weeks 52 and 64 to allow for continuous treatment until it was commercially available for patients in France), n = 164 Control interventions B. Secukinumab (2 SC injections of 150 mg (300 mg total) at weeks 0, 1, 2, 3 and 4,and every 4 weeks thereafter until the last dose at week 48), n = 163 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 1): "AbbVie Inc. funded this study, and participated inthe study design, research, analysis, data collection, interpretation of data, reviewing and approval ofthe publication. All authors had access to the data and participated in the development, review, critique and approval of the manuscript throughoutthe editorial process, and approved the final manuscript draft submitted for publication. All authors agree to be accountable for all aspects of the work, ensuring the accuracy and integrity of the publication. Medical writing support was paid for by AbbVie) Conflicts of interest Quote (appendix 1): "R.B.W. has received research grants from and leads clinical trials for AbbVie, Almirall, Amgen, Bristol Myers Squibb, Celgene, Eli Lilly, Janssen, LEO Pharma, Novartis, Pfizer and UCB Pharma; and has received consulting fees from AbbVie, Almirall, Amgen, Arena Pharmaceuticals, Avillion, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Janssen, LEO Pharma, Eli, Lilly, Novartis, Pfizer, Sanofi and UCB Pharma. A.B. has served as a scientific adviser and/or clinical study investigator for AbbVie, Aclaris, Almirall, Arena, Pharmaceuticals, Athenex, Boehringer Ingelheim, Bristol Myers Squibb, Dermavant, Dermira, Eli Lilly and Company, Forte, Galderma, Janssen, LEO, Novartis, Ortho, Pfizer, Rapt, Regeneron, Sandoz, Sanofi Genzyme, Sun Pharma and UCB Pharma; and as a paid speaker for AbbVie. Y.P. has received grant funding and honoraria for services as an investigator, speaker and member of advisory boards from AbbVie, Amgen, Bausch, Janssen‐Ortho and UCB Pharma; and has received grant funding as an investigator from Baxter, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Eli Lilly, Galderma, Genentech, GlaxoSmithKline, Incyte, LEO Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Sanofi, Serono and Takeda. C.P. has received grants from and has been a consultant for AbbVie, Almirall, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, LEO Pharma, Merck, Novartis, Pfizer, Sandoz and UCB Pharma. S.B., M.K., T.W. and Z.G. are full‐time employees of AbbVie Inc. and may hold AbbVie stock and/or stock options." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1) : "IMMerge was a phase III, international, multicentre, randomized, ... randomized in a 1: 1 ratio via a centralized Interactive Response Technology system to open‐label treatment with risankizumab or secukinumab for up to 64 weeks" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1) : "IMMerge was a phase III, international, multicentre, randomized.....randomized in a 1: 1 ratio via a centralized Interactive Response Technology system to open‐label treatment with risankizumab or secukinumab for up to 64 weeks" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 1) : open‐label, efficacy–assessor‐blinded, active‐comparator study Comment: no blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3) : "Efficacy assessments were performed by a qualified physician or designee at each study site at all appropriate study visits.The efficacy assessor was fully trained on the protocol and could not perform efficacy assessments prior to having completed all necessary training. The efficacy assessor remained blinded to each patient’s treatment and clinical laboratory results, and all safety data during the course of the study. The efficacy assessor was instructed to document the dermatological assessments on paper worksheets and was not allowedaccess to patient electronic case report forms" Comment: clearly defined |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (p 4 ): "Missing efficacy data were accounted for using nonresponder imputation, whereby any patient who had a missing valueat a study visit was categorized as a nonresponder for that visit, unless the patient was a responder both before and after a specific visit window. Safety analyses were performed on all intent‐to‐treat patients who received at least one dose of study drug (safety population)." Randomised 327, analysed 327 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03478787) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported No results were posted on ClinicalTrials.gov on the 21 September 2020 |
IMMvent 2019.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: February 2016 ‐ August 2017 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 605 participants planned Inclusion criteria
Exclusion criteria Patients with
Dropouts and withdrawals
|
|
| Interventions |
Intervention Risankizumab: 150 mg (2 syringes of 75 mg) at Weeks 0, 4 and every 12 weeks, n = 301 Control intervention Adalimumab: 80 mg at randomisation; then 40 mg at Weeks 1, 3, 5 and every other week, n = 304 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Abbvie, Boehringer Ingelheim Conflict of interest; not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (Protocol): "Active‐controlled, double‐blind, double dummy, randomized, parallel design comparison of BI 655066 and adalimumab over 44 weeks... An IRT will be used to allocate medication to patients through medication numbers. At randomization as well as subsequent medication dispense visit, IRT will assign medication numbers" Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (Protocol): "Active‐controlled, double‐blind, double dummy, randomized, parallel design comparison of BI 655066 and adalimumab over 44 weeks... An IRT will be used to allocate medication to patients through medication numbers. At randomization as well as subsequent medication dispense visit, IRT will assign medication numbers" Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (Protocol and statistical plan): "Active‐controlled, double‐blind, double dummy, randomized, parallel design comparison of BI 655066 and adalimumab over 44 weeks...Subjects will be blinded to treatment. Subjects in each dose group will receive the same injections at each designated time point, in order to maintain blinding." Comment: Probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (Protocol and statistical plan): "Active‐controlled, double‐blind, double dummy, randomized, parallel design comparison of BI 655066 and adalimumab over 44 weeks...Subjects will be blinded to treatment. Subjects in each dose group will receive the same injections at each designated time point, in order to maintain blinding." Comment: Probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (Protocol and statistical plan): "Efficacy variables will be summarized in all ITT populations... The NRI will be the primary approach in the analyses of categorical variables" Results posted on ClinicalTrials.gov: ITT results |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02694523) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
IXORA‐P 2018.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: August 2015 ‐ August 2017 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 1227 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ixekizumab (160 mg ixekizumab given as 2 SC injections at baseline and then 80 mg ixekizumab given as 1 SC injection every 2 weeks to week 52), n = 611 Control interventions B. Ixekizumab (160 mg ixekizumab given as 2 SC injections at baseline and then 80 mg ixekizumab given as 1 SC injection every 4 weeks to week 52), n = 310 C. Ixekizumab (160 mg ixekizumab given as 2 SC injections at baseline and then 80 mg ixekizumab given as 1 SC injection every 4 weeks to week 52, with a dose adjustment to Q2W until week 50 for patients meeting prespecified criteria to which investigators were blinded (Q4W/Q2W dose adjustment), n = 306 |
|
| Outcomes |
At week 52 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 1315): "This study was funded in full by Eli Lilly and Company, Indianapolis, IN, U.S.A" Conflict of interest Quote (p 1323): "R.G.L. has been a consultant and/or scientific adviser and/or investigator and/or scientific officer and/or speaker for AbbVie, Amgen, Celgene, Pfizer, Eli Lilly and Company, Novartis and Boehringer Ingelheim. K.P. has been a consultant and/or scientific adviser and/or investigator and/or scientific officer and/or speaker for Amgen, Anacor, AbbVie, Akros, Allergan, Astellas, AstraZeneca, Baxalta, Baxter, Bristol‐Myers Squibb, Boehringer Ingelheim, Can‐Fite, Celgene, Coherus, Dermira, Dow Pharma, Eli Lilly and Company, Forward Pharma, Galderma, Genentech, GlaxoSmithKline, Janssen, Kyowa Hakko Kirin, LEO Pharma, Medimmune, Meiji Seika Pharma, Merck (MSD), Merck‐Serono, Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Roche, Sanofi/Genzyme, Takeda, UCB and Valeant. M.G. has been a consultant and/or scientific adviser and/or investigator and/or scientific officer and/or speaker for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Galderma, Janssen, LEOPharma, Novartis, Pfizer, Akros, Dermira, UCB and Coherus. A.B. has been a consultant and/or scientific adviser and/or investigator and/or scientific officer and/or speaker for AbbVie, Aclaris, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira, Genentech/Roche, GlaxoSmithKline, Janssen, Eli Lilly and Company, LEO Pharma, Merck Sharp& Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sun Pharma, Sienna Pharmaceuticals, UCB, Valeant and Vidac. P.F. has been a consultant and/or scientific adviser and/or investigator and/or scientific officer and/or speaker for Abbot/AbbVie, Amgen, Bristol‐Myers Squibb, Boehringer Ingelheim, Celgene, Celtaxsys, Cutanea, Galderma, Genentech, GlaxoSmithKline/Stiefel, Janssen, LEO Pharma, Eli Lilly and Company, Novartis, Regeneron, Roche, Sanofi, Schering‐Plough/Merck, 3M/iNova/Valeant, UCB and Wyeth/Pfizer. C.M., L.Z., N.A. and P.P. are employees of/and or own stock in Eli Lilly and Company. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1316): "This multicentre, randomized, double‐blinded, parallel group, phase III trial was conducted...Assignment to dosing regimens was determined by a computer‐generated random sequence using an interactive web response system (IWRS). Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1316): "This multicentre, randomized, double‐blinded, parallel group, phase III trial was conducted...Assignment to dosing regimens was determined by a computer‐generated random sequence using an interactive web response system (IWRS). Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1316): "This multicentre, randomized, double‐blinded, parallel group, phase III trial was conducted...... To maintain investigator blinding, site personnel entered an sPGA score into the IWRS every 4 weeks, beginning at week 0 through week 48." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1316): "This multicentre, randomized, double‐blinded, parallel group, phase III trial was conducted...... To maintain investigator blinding, site personnel entered an sPGA score into the IWRS every 4 weeks, beginning at week 0 through week 48." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote (p 1317): "Missing data were imputed as nonresponse (NRI). The multiple imputation (MI) method was also used to impute missing values as a sensitivity analysis..." Included population 1227, table 2 1227 Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02513550) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
IXORA‐R 2020.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: November 2018 ‐ July 2019 Location: 124 sites, USA and Canada Phase IV |
|
| Participants |
Randomised: 1027 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals: Total : Ixekizumab : 32/520, Guselkumab 26 /507 Withdrawal participants: Ixekizumab 11, Guselkumab 4 Adverse events: Ixekizumab 6, Guselkumab 7 Lost of follow‐up : Ixekizumab 6, Guselkumab 5 protocol deviation: Ixekizumab 3, Guselkumab 0 Lack of efficacy : Ixekizumab 2, Guselkumab 1 Screen failure: Ixekizumab 1, Guselkumab 1 Other: Ixekizumab 3, Guselkumab 2 |
|
| Interventions |
Intervention A. Ixekizumab 160 mg at week 0 then 80 every 2 weeks from weeks 2 ‐ 12 Control interventions B. Guselkumab 100 mg at week 0, 4 and 12 Participants on guselkumab received placebo injection at weeks 0, 2, 6, 8 and 10 |
|
| Outcomes |
At week 12 Primary outcome
Secondary outcome
|
|
| Notes | Funding for this study was provided by Eli Lilly and Company, Indianapolis, IN, U.S.A. Eli Lilly and Company contributed to study design, data collection, data analysis, data interpretation, manuscript preparation and the decision to submit the paper for publication. An advisory committee was involved in the study design and data interpretation, together with authors from Eli Lilly and Company. Authors had full access to all group‐level data in the study, but not individual‐level data that would risk unblinding those authors who were also study investigators. Authors had final responsibility for the decision to submit for publication COI: Conflicts of interest: A.B. has served as a scientific adviser and/or clinical study investigator for AbbVie, Aclaris, Almirall, Arena, Athenex, Boehringer Ingelheim, Bristol‐Myers Squibb, Dermavant, Dermira, Eli Lilly and Company, FLX Bio, Forte, Galderma, Janssen, LEO, Novartis, Ortho, Pfizer, Regeneron, Sandoz, Sanofi Genzyme, Sun Pharma and UCB Pharma, and as a paid speaker for AbbVie. K.P. has served as a scientific adviser and/or clinical study investigator for AbbVie, Akros, Allergan, Almirall, Amgen, Arcutis, Avillion, Bausch Health, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly and Company, Galderma, Genentech/Roche, GlaxoSmithKline, Janssen, Kyowa Kirin, LEO, Meiji, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, Takeda, UCB and Valeant; and as a paid speaker for AbbVie, Akros, Allergan, Almirall, Amgen, Bausch Health, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly and Company, Galderma, Genentech/Roche, Janssen, Kyowa Kirin, LEO, Meiji, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma, Takeda, UCB and Valeant. A.G. has served as a consultant or speaker for Janssen, Celgene, Beiersdorf, Bristol‐Myers Squibb, AbbVie, UCB, Novartis, Incyte, Eli Lilly and Company, Allergan, Sun Pharmaceutical Industries, Xbiotech, LEO, Avotres Therapeutics and Boehringer Ingelheim; and received research/educational grants from Janssen, Incyte, Novartis, Xbiotech, UCB and Boehringer Ingelheim. A.J. has served as scientific advisor or clinical study investigator for AbbVie, Asana Biosciences, Castle Biosciences, Inc., Bristol‐Myers Squibb, Celgene, Dermira, Eli Lilly and Company, Galderma, Genentech/Roche, GlaxoSmithKline, LEO Pharma, Novartis, Pfizer, Purdue Pharma, Regeneron, Sanofi Genzyme, Sienna Pharmaceuticals, Sun Pharma and UCB Pharma, and as a paid speaker for Castle Biosciences, Inc., Eli Lilly and Company, Novartis, Regeneron and Sanofi Genzyme. K.R. has served as an advisor and paid speaker and has participated in clinical trials for AbbVie, Affibody, Almirall, Amgen, Avillion, Biogen, Boehringer Ingelheim, Celgene, Covagen, Forward Pharma, Fresenius Medical Care, GlaxoSmithKline, Janssen, Janssen‐Cilag, Kyowa Kirin, LEO Pharma, Eli Lilly and Company, Medac, Merck Sharp & Dohme, Novartis, Miltenyi Biotech, Ocean Pharma, Pfizer, Regeneron, Samsung Bioepis, Sanofi, Sun Pharma, Takeda, UCB, Valeant, XBiotech and Xenoport. C.M. has served as principal investigator, as a speaker or on a scientific advisory board for and received compensation in the form of honoraria from AbbVie, Amgen, Celgene, Janssen, LEO Pharma, GlaxoSmithKline, Bausch Health, Eli Lilly and Company, Novartis, Pfizer and UCB Pharma. K.B.G. has consulting relationships with AbbVie, Amgen, Celgene, Eli Lilly and Company, Janssen, Novartis, Pfizer, Dermira and Boehringer Ingelheim and has received grants from AbbVie, Amgen, Celgene and Janssen. L.K.F. has been an investigator and consultant for Eli Lilly and Company, Janssen and Pfizer; a consultant for UCB; and an investigator for AbbVie, Amgen, Galderma, LEO Pharma and Regeneron. R.G. Langley has served as principal investigator, as a speaker and on the scientific advisory board for and received compensation in the form of honoraria from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Janssen, LEO Pharma, Eli Lilly and Company, Merck, Novartis, Pfizer, Sun and UCB Pharma. Y.T. received grants for research from Maruho, LEO Pharma, Eisai, AbbVie, Kyowa Hakko Kirin, Taiho Pharmaceutical, Celgene, and Eli Lilly and Company, and honoraria for lectures from Torii Pharmaceutical, Maruho, LEO Pharma, Eisai, AbbVie, Kyowa Hakko Kirin, Eli Lilly and Company, Taiho Pharmaceutical, Mitsubishi Tanabe Pharma and Janssen. R.G. Lima, H.E., G.G., L.R., S.Y.P. and R.B. are employees and stockholders of Eli Lilly and Company. J.B. is a speaker and investigator for AbbVie, Celgene, Eli Lilly and Company, Janssen, Novartis and Ortho Dermatologics. He is an investigator for Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb and LEO Pharma. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 3): "Patients were allocated to treatment by a computer‐generated random sequence." Comment: adequate process |
| Allocation concealment (selection bias) | Low risk | Quote: "supplementary material S 2 interactive web‐response system (IWRS). The IWRS was used to assign double‐blind investigational product to each patient. The Unblinded Site Personnel at the site confirmed that they located the correct assigned study drug package by entering a confirmation number found on the package into the IWRS.Designated Unblinded Site Personnel were responsible for receipt of study drug shipments, dispensing study drug, administering study drug (ixekizumab, guselkumab, and placebo), recording information in the Study Drug Administration Log, and confirming treatment assignments "Comment:interactive web‐response system guarentee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (p 3): "Patients, investigators and all other personnel involved in the conduct of this ongoing study are to remain blinded to individual treatment assignments until all patients have completed the study." Comment: Because the syringes look different, participants were not allowed to see the syringe before, during, or after the drug administration Comment: not sure that the method has been efficiant to guarentee blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 3): "Patients, investigators and all other personnel involved in the conduct of this ongoing study are to remain blinded to individual treatment assignments until all patients have completed the study.Because the syringes look different, patients were not allowed to see the syringe before, during, or after the drug administration. Unblinded Site Personnel were responsible for maintaining the blind of the patient (e.g., by means of a blindfold or other appropriate physical barrier means communicated to the sponsor for final approval). Designated Unblinded Site Personnel were not involved in any clinical aspects of the study, including clinical evaluations and adverse event assessments." Comment: no detailled description of means used to guarentee absence of communication between blinded and unblinded personnel |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: Analysis for primary outcome and major secondary outcome was performed as ITT. Missing data were imputed using a nonresponder imputation method. Number of withdrawal was low and reasons comparable in each group |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03573323) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
IXORA‐S 2017.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: September 2015 ‐ October 2017 Location: USA (multicentric) Phase 3 |
|
| Participants |
Randomised: 302 participants (median age 43.5, males 202) Inclusion criteria:
Exclusion criteria
Dropouts and withdrawals
Ixe group (4), USK group (2)
|
|
| Interventions |
Intervention Ixekizumab (160 mg ixekizumab given as 2 SC injections at baseline followed by 80 mg ixekizumab given as a single SC injection once every 2 weeks from week 2 through week 12. After week 12 participants will receive 80 mg ixekizumab every 4 weeks through week 52), n = 136 Control intervention Ustekinumab (45 mg ustekinumab given as SC injection for participants ≤ 100 kg and 90 mg SC injection for participants > 100 kg at weeks 0, 4, 16, 28, and 40), n = 166 |
|
| Outcomes |
At week 12, Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 1014): "This study was funded in full by Eli Lilly and Company, Indianapolis, IN, U.S.A" Conflicts of interest Quote (Appendix 1): "K.R. has served as advisor and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, Takeda, UCB Pharma and Xenoport. A.P. has served as an advisor and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron and UCB. J.P.L. has served as an advisor and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Amgen, Boehringer Ingelheim, Celgene, Galderma, Janssen, LEO Pharma, Lilly, Merck‐Serono, Novartis, Pfizer, Regeneron, Roche and UCB Pharma. C.F. has served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis, including AbbVie, Amgen, Celgene, Centocor, Janssen‐Cilag, LEO Pharma, Lilly, Merck Sharp & Dohme, Novartis and Pfizer. G.M. has served as an investigator for Lilly. L.E.F. has served as an advisor for and/or participated in clinical trials sponsored by AbbVie, Amgen, Celgene, Eli Lily and Company, Galderma, Janssen‐Cilag and Novartis. M.L. has worked as a consultant and/or clinical trial investigator for AbbVie, Allergan Amgen, Anacor, Boehringer Ingelheim, Celgene, Dr Reddy’s, Janssen, LEO Pharma, Lilly, Merck‐Serono, Novartis, Oncobio‐ logics, Pfizer, Regeneron, Roche, Xenon Pharma, Valeant, Bayer, L’Oreal and Galderma. Y.D, C.H., S.W. and S.H. are employees of Eli Lilly and Company, and receive salary from and own stock in the company. C.P. has served as a consultant and/or investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, LEO Pharma, Novartis and Pfizer." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1015): "This 52‐week, phase IIIb, multicentre, controlled, double‐blind, parallel‐group trial (IXORA‐S, NCT02561806) was conducted at 51 sites across 13 countries. Patients were randomized (1: 1) via an interactive web‐response system to receive either ixekizumab or ustekinumab. Randomization was stratified by study centre and patient weight (≤ 1000 kg vs. > 1000 kg)." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1015): "This 52‐week, phase IIIb, multicentre, controlled, double‐blind, parallel‐group trial (IXORA‐S, NCT02561806) was conducted at 51 sites across 13 countries. Patients were randomized (1: 1) via an interactive web‐response system to receive either ixekizumab or ustekinumab. Randomization was stratified by study centre and patient weight (≤ 1000 kg vs. > 1000 kg)." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1015): "To maintain the blinding, patients randomized to ixekizumab received placebo injections matching the ustekinumab dose regimen, and patients in the ustekinumab group received dummy injections of ixekizumab. Unblinded site personnel responsible for ustekinumab and ustekinumab placebo injections were involved in neither the clinical assessments nor the treatment decisions, and kept the patients and investigators blinded from treatment allocation" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1015): "To maintain the blinding, patients randomized to ixekizumab received placebo injections matching the ustekinumab dose regimen, and patients in the ustekinumab group received dummy injections of ixekizumab. Unblinded site personnel responsible for ustekinumab and ustekinumab placebo injections were involved in neither the clinical assessments nor the treatment decisions, and kept the patients and investigators blinded from treatment allocation" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Qjuote (p 1016): "Patients were analysed according to the treatment they were assigned at randomization (intention‐to‐treat population). The primary‐analysis model was a logistic regression for the PASI 90 response end point after 12 weeks of treatment, with terms for treatment group, weight and geographical region. Missing data were imputed via nonresponder imputation (NRI), assuming that patients without data had no response" Patients randomized, patients analyzed Comment: Done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02561806) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
Jin 2017.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled trial Date of study: not stated Location: China (number of centres not specified |
|
| Participants |
Randomised: 18 participants (age median 48 years, 11 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 7), orally 10 mg, twice a day, 16 weeks Control intervention B. Tofacitinib (n = 5), orally, 5 mg, twice a day, 16 weeks C. Placebo (n = 6) |
|
| Outcomes | Assessments at 16 weeks Outcomes of the trial (not primary ou secondary outcomes)
|
|
| Notes | Funding source: Not stated Declarations of interest (p 169): "The authors have no conflict of interest to declare" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (supplemental appendix) "The patients were randomized to receive placebo or tofacitinib 5or 10mg twice daily (b.i.d.) for 16 weeks" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee random allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (supplemental appendix) "The patients were randomized to receive placebo or tofacitinib 5or 10mg twice daily (b.i.d.) for 16 weeks" Comment: no more description than using a placebo |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (supplemental appendix) "The patients were randomized to receive placebo or tofacitinib 5or 10mg twice daily (b.i.d.) for 16 weeks" Comment: no more description than using a placebo |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote (supplemental appendix): "All analyses were intention to treat." No statement on number of missing data and how authors dealt with it |
| Selective reporting (reporting bias) | Low risk | Comment: no protocol for the study available on ClinicalTrials.gov The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
JUNCTURE 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: 7 June 2012 – 4 January 2013 Location: 38 centres worldwide |
|
| Participants |
Randomised: 182 participants (mean age 45 years, 125 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab (n = 61), SC, 150 mg weeks 0, 1, 2, 3 then monthly Control intervention B. Secukinumab (n = 60), SC, 300 mg weeks 0, 1, 2, 3 then monthly C. Placebo (n = 61), (same drug administration) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (supplemental file) “The study was sponsored by Novartis Pharma and designed by the scientific steering committee and Novartis personnel. Novartis conducted the data analysis, and all authors had access to the data”. Declarations of interest (p 29): "Dr Paul has served as a consultant for AbbVie Pharmaceuticals, Amgen, Celgene Corporation, Eli Lilly and Company, Janssen Pharmaceuticals, LEO Pharma, Novartis Pharmaceuticals Corporation, Pfizer Inc and Pierre Fabre. Dr Lacour has participated in clinical trials sponsored by Novartis and has received honoraria as a coordinator of clinical trials sponsored by Novartis. Dr Kreutzer has received honoraria for giving speeches for, has received travel grants from, and conducts clinical trials for AbbVie Pharmaceuticals, Biogen, Novartis and Janssen‐Cilag. Dr Jazayeri has served as investigator for and received grants from Novartis. Dr Adams has served as investigator for and received grants from Amgen, Eli Lilly and Company and Novartis. Ms Guindon and Dr Papavassilis are full‐time employees of and own stock in Novartis. Mr You is a full‐time employee of Novartis. Dr Tedremets has no conflicts of interest to declare." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 28 and supplemental file): “were randomly allocated”, “Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject to a treatment arm and specified unique medication pack number" Comment: no description of the method used to guarantee the random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote: “Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject to a treatment arm and specified unique medication pack number" Comment: well described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1083): “During the induction period, subjects…in the secu 150 mg group were administrated one 150 mg injection and one placebo,….,in the placebo group…2 placebo autoinjections” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1083): “During the induction period, subjects … in the secu 150 mg group were administrated one 150 mg injection and one placebo, …., in the placebo group … 2 placebo autoinjections” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 182, analysed 181 Management of missing data: Quote (Supplemental file): “Missing values with respect to response variables based on PASI score or IGA mod 2011 score were imputed as nonresponse regardless of the reason for missing data” Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01636687) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Khatri 2016.
| Study characteristics | ||
| Methods | Randomised, double‐blind, active‐controlled trial Date: April 2015 ‐ August 2016 Location: USA (1 centre: Mont Sinai) |
|
| Participants |
Total sample size: 12 Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention: A. Ixekizumab once every 2 weeks, SC, 160 mg 2 injections at week 0 followed by 80 mg ixekizumab given as a single SC injection once every 2 weeks through week 12. After week 12 participants will receive 80 mg ixekizumab every 4 weeks through week 44, n = 6 Control intervention: B. Ixekizumab once every 4 weeks, SC, 160 mg, 2 injections at week 0 followed by 80 mg ixekizumab given as a single SC injection once every 4 weeks through week 44, n = 6 |
|
| Outcomes |
At week 12, Primary outcome
Secondary outcomes
|
|
| Notes | FUNDING: Quote (p 33) "Funding provided by Eli Lilly and Company." Conflict of interest: Quote (p 33) "Dr. Khattri has received grant/research support from and is an investigator for Eli Lilly and Company. Dr. Lebwohl is an employee of Mount Sinai, which receives research funds from AbGenomics, Amgen, Anacor, Boehringer Ingelheim, Celgene, Ferndale, Janssen Biotech, Kadmon, LEO Pharma, Eli Lilly and Company, Medimmune, Novartis, Pfizer, Sun Pharma, and Valeant. Dr. Goldblum, Ms. Solotkin, Ms. Ridenour, and Dr. Yang own stock and are employees of Eli Lilly and Company. Dr. Amir and Dr. Min have no conflicts of interest relevant to the content of this article." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 34): "For this 48‐week, randomized, single‐center, open‐label study, patients were randomized at a ratio of 1:1 to receive 80mg of ixekizumab either every two (Q2W) or four (Q4W) weeks during the induction dosing period (0–12 weeks) following an initial 160mg dose of ixekizumab." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee random allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 34): "For this 48‐week, randomized, single‐center, open‐label study, patients were randomized at a ratio of 1:1 to receive 80mg of ixekizumab either every two (Q2W) or four (Q4W) weeks during the induction dosing period (0–12 weeks) following an initial 160mg dose of ixekizumab." Comment: no blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 34): "For this 48‐week, randomized, single‐center, open‐label study, patients were randomized at a ratio of 1:1 to receive 80mg of ixekizumab either every two (Q2W) or four (Q4W) weeks during the induction dosing period (0–12 weeks) following an initial 160mg dose of ixekizumab." Comment: no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote (p 35 ‐ ClinicalTrials.gov): "Response rates were summarized using nonresponder imputation to account for missing data." No missing data at week 12 Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02387801) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Krueger 2007.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: June 2003 – March 2005 Location: 46 centres in Utah, USA |
|
| Participants |
Randomised: 320 participants Ustekinumab 12/23 45 mg (64) (mean age 46 years; 38 male) Ustekinumab 12/23 90 mg (64) (mean age 46 years; 47 male) Ustekinumab 12/23 45 mg 4‐weekly (64) (mean age 45 years; 39 male) Ustekinumab 12/23 90 mg 4‐weekly (64) (mean age 44 years; 52 male) Placebo (64) (mean age 44 years; 46 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab 12/23 (n = 64), SC, 45 mg, 45 mg 1 dose, 1 week Control intervention B. Ustekinumab 12/23 (n = 64), SC, 90 mg, 45 mg 1 dose, 1 week C. Ustekinumab 12/23 (n = 64), SC, 45 mg, 45 mg/week, 4 weeks D. Ustekinumab 12/23 (n = 64), SC, 90 mg, 45 mg/week, 4 weeks E. Placebo (n = 64), SC |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source (p 590): "Supported by Centocore, Malvern, PA" Declarations of interest (p 590‐1): "Dr. Krueger reports receiving fees as a consultant or advisory board member for Abbott, Almirall, Alza, Amgen, Astellas, Boehringer Ingelheim, Barrier Therapeutics, Bristol‐Myers Squibb, Centocor, Connetics, and Genentech; Dr. Langley, for Centocor, Abbott, and Amgen/Wyeth; Dr. Leonardi, for Abbott, Amgen, Centocor, and Genentech; and Dr. Lebwohl, for Abbott, Amgen, Astellas, Centocor, Connetics, Galderma, Genentech, Novartis, PharmaDerm, and Warner Chilcott. Dr. Krueger reports receiving lecture fees from Abbott, Amgen, Boehringer Ingelheim, Centocor, and Connetics; Dr. Langley, from Abbott and Amgen/ Wyeth; Dr. Leonardi, from Abbott, Amgen, Centocor, and Genentech; and Dr. Lebwohl, from Abbott, Astellas, Amgen, Centocor, Connetics, Galderma, Genentech, PharmaDerm, and Warner Chilcott. Dr. Krueger reports receiving stipends for a clinical research fellowship from Amgen and Centocor; Dr. Langley, grant support from Centocor, Abbott, and Amgen/Wyeth; Dr. Leonardi, educational grants from Amgen and Genentech; and Dr. Lebwohl, grants from Abbott, Amgen, Astellas, Centocor, Connetics, Galderma, Genentech, PharmaDerm, and Warner Chilcott. Drs. Yeilding, Guzzo, Wang, and Dooley report being employees of Centocor. Dr. Krueger reports owning stock options from ZARS Pharma; Drs. Yeilding, Guzzo, and Dooley report holding stock and stock options in Johnson & Johnson; and Dr. Wang reports being a stockholder in Johnson & Johnson. No other potential conflict of interest relevant to this article was reported." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 581): “Patients ... were randomly assigned” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 581): “Patients ... were randomly assigned” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 581): “This placebo‐controlled, double‐blind...phase 2 study” Comment: placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 581): “This placebo‐controlled, double‐blind...phase 2 study” Comment: no specific description of the method used to guarantee blinding of outcome assessment, but considering that this is a placebo‐controlled trial with no known systematic AEs we considered the risk as low |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 320 included, 320 analysed Quote (p 582): "Efficacy data from all patients who underwent randomisation were analysed... Missing values at week 12 were replaced with the most recently available values for all efficacy variables, missing data at other time points were not imputed" Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00320216) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Krueger 2016a.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: March 2013 ‐ November 2013 Location: 6 centres in the USA |
|
| Participants |
Randomised: 12 participants (mean age 45.5 years, 8 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 9), orally, 10 mg twice daily Control intervention B. Placebo (n = 3) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1079): “This study was sponsored by Pfizer Inc. Both Pfizer Inc and non‐Pfizer Inc authors have participated in the study design, data collection, data analysis, and open scientific discussion of the data; its interpretation; and the development of the associated manuscript. The views and opinions expressed within the manuscript are those of all authors and do not necessarily represent those of the funding organization. Medical writing support was funded by Pfizer Inc.”. Declarations of interest (p 1079) : "J. Krueger received research funding from Novartis, Pfizer Inc, Janssen, Lilly, Merck, Kadmon, Dermira, Boehringer, BMS, and Paraxel during the conduct of the study; grants paid to institutions from Amgen, Innovaderm and Kyowa; and personal fees from Serono, BiogenIdec, Delenex, AbbVie, Sanofi, Baxter, Xenoport, and Kineta. M. Suárez‐Fariñas receives research funding and speakers' fees from Pfizer. J. D. Clark, H. Tan, R. Wolk, S. T. Rottinghaus, M. Z. Whitley, H. Valdez, D. von Schack, S. P. O'Neil, P. S. Reddy, and S. Tatulych are employees of Pfizer Inc. The rest of the authors declare that they have no relevant conflicts of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1079): “Patients were randomised 3:1 to receive 10 mg of oral tofacitinib or placebo twice daily for 12 weeks by using an automated Web or telephone randomization system” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1079): “Patients were randomised 3:1 to receive 10 mg of oral tofacitinib or placebo twice daily for 12 weeks by using an automated Web or telephone randomisation system” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1079): “This was a phase 2, randomised, placebo‐controlled, double‐blind study carried out in 6 centers” Comment: placebo‐controlled, probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1079): “This was a phase 2, randomised, placebo‐controlled, double‐blind study carried out in 6 centers” Comment: placebo‐controlled, probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 12, analysed 11 Management of missing data: not mentioned |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01710046) The prespecified outcomes in the protocol or those mentioned in the Methods section have been reported in the Results section |
Laburte 1994.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: not stated Location: 27 centres worldwide |
|
| Participants |
Randomised: 251 participants (mean age 41 years, 176 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ciclosporin A (n = 119), orally, 2.5 mg/kg/d, 12 weeks Control intervention B. Ciclosporin A (n = 132), orally, 5 mg/kg/d, 12 weeks |
|
| Outcomes | Period assessments: 12 weeks Primary or secondary outcomes of the trial:
Outcmes of the trial
|
|
| Notes | Funding and declarations of interest: not stated, but the first author was employed by Sandoz Pharma Ltd | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 367): "... was an open randomised study in parallel group" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 367): "... was an open randomised study in parallel group" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 367): "... was an open randomised study in parallel group" Comment: no blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 367): "... was an open randomised study in parallel group" Comment: no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Management of missing data: no description of the method used to guarantee management of missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Lee 2016.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, open‐label trial Date of study: July 2009 ‐ April 2011 Setting: Korea (multicentric) |
|
| Participants |
Total sample size: 60 Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept + acitretin (combination of etanercept, 25 mg twice a week and acitretin 10 mg twice a day for 24 weeks), n = 20 Control intervention B. Etanercept, 50 mg twice a week for 12 weeks followed by 25 mg twice a week for 12 weeks, n = 21 C. Acitretin, 10 mg twice a day for 24 weeks, n = 19 |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 8): "This study was funded by Pfizer Pharmaceuticals Korea Limited; etanercept is a product of Pfizer." Conflics of interest Quote (p 8): "Hyun‐Jeong Yoo is an employee of Pfizer Pharmaceuticals Korea Limited; etanercept is a product of Pfizer. All other authors report no competing interests." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 2): "In this multicenter, randomized, open‐label trial, patients were randomly assigned to one of three treatment groups: (a) etanercept 50 mg twice weekly (BIW) for 12 weeks followed by etanercept 25 mg BIW for a further 12 weeks (ETN–ETN); (b) etanercept 25 mg BIW and acitretin 10 mg twice daily (BID) for 24 weeks (ETN‐ACT); (c) acitretin 10 mg BID for 24 weeks (ACT;Fig. 1)" Comment: No description |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 2): "In this multicenter, randomized, open‐label trial, patients were randomly assigned to one of three treatment groups: (a) etanercept 50 mg twice weekly (BIW) for 12 weeks followed by etanercept 25 mg BIW for a further 12 weeks (ETN–ETN); (b) etanercept 25 mg BIW and acitretin 10 mg twice daily (BID) for 24 weeks (ETN‐ACT); (c) acitretin 10 mg BID for 24 weeks (ACT;Fig. 1)" Comment: No description |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 2): "In this multicenter, randomized, open‐label trial, patients were randomly assigned to one of three treatment groups: (a) etanercept 50 mg twice weekly (BIW) for 12 weeks followed by etanercept 25 mg BIW for a further 12 weeks (ETN–ETN); (b) etanercept 25 mg BIW and acitretin 10 mg twice daily (BID) for 24 weeks (ETN‐ACT); (c) acitretin 10 mg BID for 24 weeks (ACT;Fig. 1)" Comment: Not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 2): "In this multicenter, randomized, open‐label trial, patients were randomly assigned to one of three treatment groups: (a) etanercept 50 mg twice weekly (BIW) for 12 weeks followed by etanercept 25 mg BIW for a further 12 weeks (ETN–ETN); (b) etanercept 25 mg BIW and acitretin 10 mg twice daily (BID) for 24 weeks (ETN‐ACT); (c) acitretin 10 mg BID for 24 weeks (ACT;Fig. 1)" Comment: Not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote (p 2): "Efficacy evaluation was performed on the modified intent‐to‐treat (mITT) and per protocol (PP) population sets. The mITT population included all randomly assigned patients who received at least one dose of test medication and had both baseline and on‐therapy PASI evaluation...and the patients who did not experience the event were censored at the time of last observation" Included population 60, Table 59 Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00936065) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
Leonardi 2003.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: December 2001 ‐ April 2002 Location: 47 centres in USA |
|
| Participants |
Randomised: 672 participants (mean age 45 years, 672 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept LD (n = 169), SC auto‐administered, 25 mg, once/week, 12 weeks Control intervention B. Etanercept MD (n = 167), SC auto‐administered, 25 mg, twice/week, 12 weeks C. Etanercept HD (n = 168), SC auto‐administered, 50 mg, twice/week, 12 weeks D. Placebo (n = 168), SC, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 2021): "Supported by Immunex, Seattle, a wholly‐owned subsidiary of Agen, Thousand Oaks, Calif" Declarations of interest (p 2021): "Drs. Leonardi, Powers, Goffe, and Gottlieb report having served as consultants for Amgen, and Drs. Leonardi, Goffe, and Gottlieb report having served as paid lecturers for Amgen. Dr. Gottlieb reports having served as a consultant and paid lecturer for Johnson & Johnson, Genentech, and Biogen; Dr. Leonardi reports having served as a consultant and paid lecturer for Johnson & Johnson and Genentech; Dr. Powers reports having served as a consultant for Genentech and Biogen; and Dr. Goffe reports having served as a consultant and paid lecturer for Biogen. Dr. Zitnik and Ms. Wang report owning equity in Amgen." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 2016): "Patients underwent central randomisation with the use of a permuted block randomisation list, with equal allocation to each of the four treatment groups" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Comment: no description of the method used to guarantee the allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 2015): "Double‐blind... Etanercept ... was supplied to patients in syringes, each containing the contents of one reconstituted vial of etanercept or matching placebo...All patients received two injections per dose of study" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 2015): "Double‐blind... Etanercept ... was supplied to patients in syringes, each containing the contents of one reconstituted vial of etanercept or matching placebo...All patients received two injections per dose of study" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 672 randomised participants, 652 analysed (20 participants did not receive the treatment and were excluded from the analyses) Comment: modified ITT but number of participants not receiving treatment and not included in the analysis low and comparable between groups |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Leonardi 2012.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: April 2010 ‐ May 2011 Location: 23 centres internationally |
|
| Participants |
Randomised: 142 participants (mean age 46 years, 81 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Placebo (n = 27), SC, 0, 2, 4, 8, 12, 16 weeks, 16 weeks Control intervention B. Ixekizumab (n = 28), SC, 10 mg, 0, 2, 4, 8, 12, 16 weeks, 16 weeks C. Ixekizumab (n = 30), SC, 25 mg, 0, 2, 4, 8, 12, 16 weeks, 16 weeks C. Ixekizumab (n = 29), SC, 75 mg, 0, 2, 4, 8, 12, 16 weeks, 16 weeks C. Ixekizumab (n = 28), SC, 150 mg, 0, 2, 4, 8, 12, 16 weeks, 16 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 1190): "Funded by Eli Lilly" Declarations of interest (p 1198): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Leonardi received personal fees from Abbott, Amgen, Certocor, Eli Lilly and Pfizer. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol p 44): “... from the central randomisation center using an IVRS” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (protocol p 44): “... from the central randomisation center using an IVRS” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol p 22): “The investigators and patients are blinded while the sponsor is unblinded to study assignment” Comment: placebo‐controlled trial, no systematic AE for the drug, probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol p 22): “The investigators and patients are blinded while the sponsor is unblinded to study assignment” Comment: placebo‐controlled trial, no systematic AE for the drug, probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Included 142/141 analysed (1 in the placebo group who did not have any post‐baseline assessment) Quote (protocol p 62 and p 1192): "All efficacy and health outcome analyses will be conducted on all patients who received any amount of study drug and have any post‐baseline efficacy assessment....Missing data for the primary timepoint at week 12 will be imputed by the last observation carried forward method" Comment: m‐ITT and 1 participant out of 142 was not included in the analyses |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01107457) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
LIBERATE 2017.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: October 2012 ‐ April 2016 Location: 82 centres worldwide (USA, Europe, Australia) |
|
| Participants |
Randomised: 250 participants (mean age 45 years, 157 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Apremilast (n = 83), orally, 30 mg twice daily Control intervention B. Etanercept (n = 83), SC, 50 mg weekly D. Placebo (n = 84) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 2): "This study was sponsored by Celgene Corporation." Declarations of interest (p 1): "K. Reich has received honoraria as a consultant and/or advisory board member and/or acted as a paid speaker and/or participated in clinical trials sponsored by AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene Corporation, Centocor, Covagen, Eli Lilly, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Medac, Merck Sharp & Dohme Corp., Novartis, Ocean Pharma, Pfizer, Regeneron, Takeda, UCB Pharma and XenoPort. M. Gooderham has received honoraria, grants and/or research funding as a speaker, investigator, advisory board member, data safety monitoring board member and/or consultant for AbbVie, Actelion, Amgen, Astellas Pharma US, Boehringer Ingelheim, Celgene Corporation, Dermira, Eli Lilly, Galderma, Janssen, Kyowa Hakko Kirin Pharma, LEO Pharma, MedImmune, Merck & Co., Inc., Novartis, Pfizer, Regeneron, Roche" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 3): "Eligible patients were randomised (1 : 1: 1) via an interactive
voice response system to placebo; apremilast oral tablet, 30 mg twice daily; or etanercept subcutaneous injection, 50 mg QW".“Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject to a treatment arm and specified unique medication pack number" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 3): "Eligible patients were randomised (1 : 1: 1) via an interactive
voice response system to placebo; apremilast oral tablet, 30 mg twice daily; or etanercept subcutaneous injection, 50 mg QW". Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "Per the double dummy design, patients received oral tablets (apremilast 30 mg or placebo) twice daily and two subcutaneous injections (etanercept 25 mg each dose or saline placebo) QW." Comment: clearly defined |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "Per the double dummy design, patients received oral tablets (apremilast 30 mg or placebo) twice daily and two subcutaneous injections (etanercept 25 mg each dose or saline placebo) QW." Comment: clearly defined |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 250, 250 analysed Management of missing data: quote (p 3): "Efficacy assessments were conducted for the modified intent‐to treat (mITT) population (all randomised patients who received ≥1 dose of study medication and had both baseline PASI and ≥1 post‐treatment PASI evaluations)... Last‐observation‐carried‐forward (LOCF) methodology was used to impute missing efficacy measurements." Comment: done |
| Selective reporting (reporting bias) | High risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01241591) The prespecified outcomes and those mentioned in the Methods section have not been reported as DLQI |
LOTUS 2013.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind (LOTUS) Date of study: 23 October 2009 ‐ 07 July 2011 Location: 14 centres in China |
|
| Participants |
Randomised: 322 participants (mean age 40 years, 248 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab (n = 160), SC, 45 mg, week 0, week 4, 4 weeks Control intervention B. Placebo (n = 162), SC, week 0, week 4, 4 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 173): "This study was supported by Janssen Research & Development" Declarations of interest (p 173): "Drs Zhu, Zang and Wand served as investigators for this Janssen RD‐sponsored study..." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 167): "The LOTUS study is a phase 3, multicenter, randomized, double blind, placebo‐controlled..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 167): Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 167): "The LOTUS study is a phase 3, multicenter, randomized, double blind, placebo‐controlled..." Comment: placebo‐controlled study |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 167): "The LOTUS study is a phase 3, multicenter, randomized, double blind, placebo‐controlled..." Comment: no description of the method used to guarantee blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 322, analysed 322 Quote (p 167): "For efficacy analyses, all randomized patients were included... Patients who discontinued study treatment... were considered treatment failures" Comment: ITT analyses |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01008995) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Lowe 1991.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: not stated Location: 2 centres in Santa Monica and New York City, USA |
|
| Participants |
Randomised: 34 participants, age range 20 ‐ 75 years, 24 male Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 16), orally, 50 mg, daily, 12 weeks Control intervention B. Placebo (n = 18), orally, daily, 12 weeks Co‐intervention: UVB (phototherapy) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source (p 591): Quote: "Supported by Roche dermatologics, Nutley, New Jersey and the Skin Research Foundation of California, Santa Monica, California" Declarations of interest; not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 592): "Patients receiving UVB phototherapy were randomly assigned" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 592): "Patients receiving UVB phototherapy were randomly assigned" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 592): "were randomly assigned to either acitretin or placebo" Comment: no more precision however adverse effects of acitretin such as cheilitis are visible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 592): "were randomly assigned to either acitretin or placebo... the same observer who was unaware of patient group examined the patients throughout the investigation" Comment: no more precision but adverse effects of acitretin such as cheilitis are visible |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 34 included / 34 analysed (Table 2) Comment: no description of the method used to manage the missing data or to perform the analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Mahajan 2010.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: January 2007 – September 2007 Location: 1 centre in Chandighar, India |
|
| Participants |
Randomised: 40 participants (mean age 37 years, 29 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate 0.5 mg/kg + folic acid, (n = 20), orally 5 mg/d Day‐1; Day+1 + NBUVB 3/week max 1200 mJ/cm2 Control intervention B. Placebo + folic acid (n = 20), orally, 5 mg/d Day‐1; Day+1 + NBUVB 3/week max 1200 mJ/cm2 |
|
| Outcomes | Assessments at 6 months Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: not stated Declarations of interest (p 595): "not declared" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 596): “... were randomised by way of random number table” Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 596): “... were randomised by way of random number table” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 596): “patient‐blinded study” Comment: not double blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 596): “patient‐blinded study” Comment: not double blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 20/20 included; 20/20 analysed Quote (p 596):“Intention to treat principle was followed for the analysis of the observations” Comment: no description of the method used to manage the missing data |
| Selective reporting (reporting bias) | Low risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Meffert 1997.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: 17 centres in Germany |
|
| Participants |
Randomised: 128 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ciclosporin (n = 43), orally, 1.25 mg/kg/d, 10 weeks Control intervention B. Ciclosporin (n = 41), orally, 2.5 mg/kg/d, 10 weeks C. Placebo (n = 44), orally, 10 weeks |
|
| Outcomes | Assessments at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source not stated but 3 out of 4 authors from Sandoz pharmaceuticals Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 77): "patients were randomised" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (p 77): "double blind study period" Comment: no description of the method used to guarantee blinding regarding the need of hypertension and renal function surveillance and modification in ciclosporin groups |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 77): "double blind study period" Comment: no description of the method used to guarantee blinding, regarding the need of hypertension and renal function surveillance and modification in ciclosporin groups |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 128 included/120 analysed Comment: methods for dealing with missing data not specified, not ITT analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
METOP 2017.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled Date of study: 22 February 2013 ‐ 13 May 2015 Location: 13 centres in Europe |
|
| Participants |
Randomised: 120 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 91), SC, IM, 17.5 ‐ 22.5 mg/week, 12 weeks Control intervention B. Placebo (n = 29) |
|
| Outcomes | 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 528) "Funding source: Medac. The funder of the study had no role in study design, data collection, data analysis, data interpretation or writing of the report. The corresponding author had full access to all the data in the study and all authors had final responsibility for the decision to submit for publication" Declarations of interest (p 536): "RBW has received personal fees from AbbVie, Almirall, Amgen, Boehringer Ingelheim Pharma, Celgene, Janssen‐Cilag, Leo, Lilly, Novartis, Pfizer, and Xenoport outside the submitted work. UM has been an advisor to, received speakers honoraria or grants from, or participated in clinical for Abbott/AbbVie, Almirall Hermal, Amgen, BASF, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, Foamix, Forward Pharma, Galderma, Janssen, Leo Pharma, Medac, MSD, Miltenyi Biotech, Novartis, Pfizer, Teva, VBL, and Xenoport. RvK has been an investigator, consultant, advisor, or speaker for Abbvie, Almirall, Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Eli Lilly, GSK, Leo, Janssen‐Cilag, MSD, Novartis, Pfizer, UCB, and VBL Pharma. JN has received grants from Amgen, Novartis, Janssen‐Cilag, LEO, Lilly, Medac, Regeneron, and Dermapharm, outside the submitted work. DW‐T has been an advisor to, received speakers honoraria or grants from, or participated in clinical for Abbvie, Almirall, Amgen, Biogen, Boehringer Ingelheim Pharma, Celgene, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, Leo, Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, UCB Pharma, and VBL. KG has been an advisor to, received speakers honoraria or grants from, or participated in clinical for Abbott/AbbVie, Almirall, Biogen, Boehringer Ingelheim, Celgene, Delenex, Eli Lilly, Galderma, Janssen, Medac, MSD, Novartis, and Pfizer. KR has received personal fees from AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, Leo, Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, Takeda, UCB Pharma, and Xenoport, outside the submitted work. IZ, TMF, and NB‐S declare no competing interests." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 3): "Eligible patients were randomly assigned (3:1), via computer‐generated random numbers (RandList 1.2) in an ascending order, to receive either methotrexate or placebo injections for the first 16 weeks of the study (phase 1)." Comments: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 3): "Eligible patients were randomly assigned (3:1), via computer‐generated random numbers (RandList 1.2) in an ascending order, to receive either methotrexate or placebo injections for the first 16 weeks of the study (phase 1)." Comments: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "Study phase 1 was done in a double‐blind manner, with group allocation concealed from participants and investigators from the time of randomisation until an interim database lock at week 16...The syringes for placebo and active drug were not distinguishable and were fully coated to prevent identification of colour differences between injections" Comments: clearly defined |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "Study phase 1 was done in a double‐blind manner, with group allocation concealed from participants and investigators from the time of randomisation until an interim database lock at week 16...The syringes for placebo and active drug were not distinguishable and were fully coated to prevent identification of colour differences between injections" Comments: clearly defined |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Number of randomised participants, n = 120, 120 analysed Quote (p 4): "All outcomes were analysed in the modified intention to‐treat population of patients who had received at least one injection of study drug, with missing data treated as indicating no response (non‐responder imputation)." Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02902861) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Nakagawa 2016.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: October 2012 – March 2013 Setting: multicentre (56) in Japan |
|
| Participants |
Randomised: 151 participants (mean age 45 years, 120 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Brodalumab (n = 39), SC, 70 mg, 2 injections week 0, 1 injection eow Control intervention B. Brodalumab (n = 37), SC, 140 mg, 2 injections week 0, 1 injection eow C. Brodalumab (n = 37), SC, 210 mg, 2 injections week 0, 1 injection eow D. Placebo (n = 38), orally (same drug administration) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 51) “The study was supported by Kyowa Hakko Kirin Co., Ltd.” Declarations of interest (p 51): "H. Nakagawa is a consultant and/or received research grants and/or speaker honoraria from for Kyowa Hakko Kirin Co., Ltd., AbbVie, Mitsubishi‐Tanabe Pharma, Janssen Pharmaceutical K.K., Novartis Pharma K.K., Eli Lilly Japan K.K., LEO Pharma Maruho Corporation Limited and MSD K.K.H. Niiro has no conflict of interest to declare. K. Ootaki is an employee of Kyowa Hakko Kirin Co., Ltd." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 45): “were randomised to receive…” Comment: not stated |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 45): “were randomised to receive…” Comment: not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (p 51): “double‐blind…” Comment: not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | No description of the method used to guarantee blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 151, analysed 151 Comment: no supplementary explanation about the management of missing data |
| Selective reporting (reporting bias) | High risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01748539) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except for participant‐reported outcome |
NCT02134210.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: June 2014 ‐ May 2016 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 521 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
CHS‐0214 group (6), Enbrel group (19) Reasons not stated |
|
| Interventions |
Intervention A. CHS‐0214 50 mg twice weekly times 12 weeks, n = 261 Control intervention B. Enbrel 50 mg twice weekly times 12 weeks, n = 260 |
|
| Outcomes |
At week 12 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) Coherus Biosciences, Inc. Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (ClinicalTrials.gov): "A Double‐Blind, Randomized, Parallel‐Group, Active‐Control Study to Compare the Efficacy and Safety of CHS‐0214 Versus Enbrel...Allocation: randomized" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Masking: Quadruple (Participant, Care Provider, Investigator, Outcomes Assessor)" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dealing with missing data: not stated Results posted on ClinicalTrials.gov: ITT analyses Reasons for treatment 's discontinuation not stated |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02634801) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
NCT02313922.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: August 2014 ‐ October 2016 Location: China (19 centres) Phase 4 |
|
| Participants |
Randomised: 466 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 466, mean age of 43 years and 76% men Dropouts and withdrawals
Methotrexate group (13), Placebo group (11)
|
|
| Interventions |
Intervention A. Methotrexate (initial dose of 7.5 mg/week to a maximum dose of 15 mg/week or the maximum tolerated dose within 8 weeks), n = 233 Control intervention B. Placebo, n = 233 Co‐intervention: etanercept (50 mg subcutaneously once weekly) |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
|
| Notes | Funding "This research was supported by Zhejiang Public Walfare Technology Research Project (Grant number: LGF20H110002). Med‐ ical Health Science and Technology Project of Zhejiang Provincial Health Commission (Grant Number: 2018KY088) and 3SBIO INC." Conflict of interest "The authors declare that they have no conflict of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote:""All eligible patients were randomly assigned by a random number created by a computer‐generated coding system to receive either the combination of rhTNFR‐Fc and MTX (combination group) or rhTNFR‐Fc plus placebo (monotherapy group)." |
| Allocation concealment (selection bias) | Unclear risk | Quote:"Then patients were randomized 1:1 to receive 50 mg rhTNFR‐Fc subcutaneously once weekly and oral MTX (from an initial dose of 7.5 mg/week to a maximum dose of 15 mg/week or the maximum tolerated dose within 8 weeks) or receive rhT‐ NFR‐Fc (as that in combination group) and a matched placebo (as MTX in combination group) for 24 weeks." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote:"This was a multicentre, randomized, double‐blind, placebo‐controlled trial of rhTNFR‐Fc..." Comment: no description of the method used to guarantee allocation blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote:"This was a multicentre, randomized, double‐blind, placebo‐controlled trial of rhTNFR‐Fc..." Comment: no description of the method used to assess the primary outcome |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dealing with missing data:no information on how were handled missing data Quote:"Efficacy analysis was performed using the intent‐to‐treat principle, in which all randomized patients who received any part of the study medication treatment and received at least one evaluation of therapeutic effectiveness were included in the analysis. All results of the efficacy analysis were analysed in the full analysis set (FAS). Safety was analysed in a safety analysis set (SAS), which included all patients who had received at least 1 dose of the study drug." Randomised 466; analysed 466 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02313922). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. No results are posted on ClinicalTrials.gov. |
NCT02581345.
| Study characteristics | ||
| Methods | RCT, active‐controlled, triple‐blind trial Date of study: September 2015 ‐ April 2017 Location: world‐wide |
|
| Participants |
Randomised: 572 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Biosimilar group (15), Humira group (23)
|
|
| Interventions |
Intervention A. Biological: M923, S/C, Biosimilar adalimumab week 0: 80 mg, week 1: 40 mg, then 40 mg EOW, n = 286 Control Intervention B. Biological: M923, S/C, adalimumab (Humira) week 0: 80mg, week 1: 40 mg, then 40 mg EOW, n = 286 |
|
| Outcomes |
At 16 weeks Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov): Novartis Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and Statistical analysis plan): "Allocation: randomized... The blocking scheme will be specified in the randomization specifications. Randomization will occur via an Interactive Response Technology (IRT) System until..." Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and Statistical analysis plan): "Allocation: randomized... The blocking scheme will be specified in the randomization specifications. Randomization will occur via an Interactive Response Technology (IRT) System until..." Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Masking: Triple (Participant, Care Provider, Investigator)" Comment:probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Masking: Triple (Participant, Care Provider, Investigator)" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (Statistical analysis plan): "The primary analysis will be based on the non‐responder imputation (NRI) method." Results posted on ClinicalTrials.gov: Per protocol analyses (non‐inferiority trial) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02581345) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
NCT02672852.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: February 2016 ‐ July 2018 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 507 participants Inclusion criteria
Exclusion criteria:
Dropouts and withdrawals
Risankizumab group (4), Placebo group (3)
|
|
| Interventions |
Intervention A. Risankizumab 150 mg by subcutaneous injection at Weeks 0 and 4, n = 407 Control intervention B. Placebo by subcutaneous injection at Weeks 0 and 4, n = 100 |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding: AbbVie, Boehringer Ingelheim Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and study protocol/statistical analysis plan): "This is a confirmatory, multinational, multicenter, randomized, double‐blind, placebo controlled, study... During Visit 2 and after the patient’s eligibility has been confirmed, the treatment will be assigned via Interactive Response Technology (IRT). To facilitate the use of the IRT, the Investigator will receive all necessary instructions." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and study protocol/statistical analysis plan): "This is a confirmatory, multinational, multicenter, randomized, double‐blind, placebo controlled, study... During Visit 2 and after the patient’s eligibility has been confirmed, the treatment will be assigned via Interactive Response Technology (IRT). To facilitate the use of the IRT, the Investigator will receive all necessary instructions." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and study protocol/statistical analysis plan): "Injections should be at least 2 cm. apart and should not be close to a vein. The injection sites should avoid sites of psoriasis involvement as well as sites where the skin is tender, bruised, erythematous, or indurated, and should be alternated to other areas for subsequent doses. Injections will be given in a double blind fashion with each patient receiving 2 injections of BI 655066 or matching placebo administered within approximately 5 minutes at each dosing visit as indicated in the Flow Charts" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and study protocol/statistical analysis plan): "Injections should be at least 2 cm. apart and should not be close to a vein. The injection sites should avoid sites of psoriasis involvement as well as sites where the skin is tender, bruised, erythematous, or indurated, and should be alternated to other areas for subsequent doses. Injections will be given in a double blind fashion with each patient receiving 2 injections of BI 655066 or matching placebo administered within approximately 5 minutes at each dosing visit as indicated in the Flow Charts" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (statistical analysis plan): "The NRI will be the primary approach in the analyses of categorical variables." ITT results on ClinicalTrials.gov |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02672852) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
NCT02690701.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: February 2016 ‐ February 2018 Location: USA (12 centres) Phase 4 |
|
| Participants |
Randomised: 91 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 91, mean age of 47.5 years and 67% men Dropouts and withdrawals
Secukinumab group (2), Placebo group (3)
|
|
| Interventions |
Intervention A. Secukinumab 300 (300 mg once weekly at baseline, weeks 1, 2, 3 and 4 followed by monthly dosing starting at week 8 through week 48 inclusive), n = 46 Control intervention B. Placebo, n = 45 |
|
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
|
| Notes | Funding "This study is funded by Novartis Pharmaceuticals Corporation, East Hanover, NJ." Conflict of interest "Dr Gelfand served as a consultant for BMS, Boehringer Ingelheim, Janssen Biologics, Novartis Corp, UCB (DSMB), Sanofi, and Pfizer, receiving honoraria; and receives research grants (to the Trustees of the University of Pennsylvania) from AbbVie, Boehringer Ingelheim, Janssen, Novartis, Celgene, Ortho Dermatologics, and Pfizer; and received payment for continuing medical education work related to psoriasis that was supported indirectly by Lilly, Ortho Dermatologics, and Novartis. Dr Gelfand is a Deputy Editor for the Journal of Investigative Dermatology receiving honoraria from the Society for Investigative Dermatology. Dr Duffin has received research grants from AbbVie, Amgen, Bristol‐Myers Squibb, Celgene, Eli Lilly, Janssen, Novartis, Pfizer, Sienna Biopharmaceuticals, Stiefel Laboratories, and UCB; and has received consulting fees from AbbVie, Amgen, Bristol‐Myers Squibb, Celgene, Eli Lilly, Janssen, Novartis, Ortho Dermatologic, Pfizer, Sienna Biopharmaceuticals, Stiefel Laboratories, and UCB; and is on the speaker's bureau for Novartis. Dr Armstrong has served as investigator, advisor, and/or consultant to Leo, AbbVie, UCB, Janssen, Novartis, Eli Lilly, Sun, Dermavant, BMS, Regeneron Pharmaceuticals, Inc., Sanofi U.S., Dermira, Modmed, and Ortho Dermatologics, Inc. Dr Blauvelt has served as a scientific adviser and/or clinical study investigator for AbbVie, Aclaris, Akros, Allergan, Almirall, Amgen, Arena, Athenex, Boehringer Ingelheim, Bristol‐ Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly, FLX Bio, Forte, Galderma, Genentech/Roche, GlaxoSmithKline, Janssen, Leo, Meiji, Merck Sharp & Dohme, Novartis, Ortho, Pfizer, Purdue Pharma, Regeneron, Revance, Sandoz, Sanofi Genzyme, SiennaPharmaceuticals, Sun Pharma, UCB Pharma, and Vidac and as a paid speaker for AbbVie, Regeneron, and Sanofi Genzyme. Dr Trying has conducted studies sponsored by the producer of secukinumab. Dr Menter has received compensation from or served as an investigator, consultant, advisory board member, or speaker for Abbott Labs, AbbVie, Allergan, Amgen, Anacor, Boehringer Ingelheim, Celgene, Dermira, Eli Lilly, Galderma, Janssen, Leo, Merck & Co, Neothetics, Novartis, Pfizer, Regeneron, Sienna, Symbio/Maruho, UCB, Vitae, and Xenoport. Dr Gottlieb is currently serving as consultant, advisory board member, speaker for Janssen, Celgene, Bristol Myers Squibb, Beiersdorf, Abbvie, UCB, Novartis, Incyte, Lilly, Reddy Labs, Valeant, Dermira, Allergan, Sun Pharmaceutical Industries, Xbiotech, Leo, Avotres Therapeutics. Research/Educational Grants: Janssen, Incyte, UCB, Novartis, Lilly Xbiotech, Boeringer Ingelheim. Dr Lockshin reports personal fees from Lilly, Novartis, Janssen, and Abbott; has served as a speaker for Novartis, Eli Lilly, and Abbvie; conducted research for Celgene, Abbvie, Novartis, Eli Lilly, and Strata, and served as a consultant for Novartis, Lilly, AstraZeneca, Abbive. Dr. Simpson reports grants from Eli Lilly, Kyowa Hakko Kirin, Leo Pharmaceutical, Merck, Pfizer, and Regeneron, and personal fees from Menlo Therapeutics, Valeant, Novartis, Eli Lilly, Galderma, Dermira, Sanofi Genzyme, Pfizer, Regeneron, and Leo Pharmaceuticals. Dr Shin, Dr Ahlman, Dr Playford, Dr Joshi, Dr Dey, Dr Werner and Dr Alavi have nothing to disclose. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "This was a randomized, double‐blinded, placebo‐controlled, parallel‐group, multicenter study in adult patients (≥18 years of age) with moderate‐to‐severe chronic plaque psoriasis....Eligible patients were randomized via Interactive Response Technology in a 1:1 ratio to either secukinumab 300 mg or placebo." |
| Allocation concealment (selection bias) | Low risk | Quote: "The Investigator or his/her delegate will contact the IRT after confirming that the subject fulfills all the inclusion/exclusion criteria. The IRT will assign a randomization number to the subject, which will be used to link the subject to a treatment group and will specify a unique medication number for the first box of study treatment to be dispensed to the subject. The randomization number will not be communicated to the caller. The identity of secukinumab and placebo prefilled syringes (PFS) will be concealed by identical packaging, labeling, schedule of administration, and appearance." Comment: adequate procedure to guarentee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote:"Patients, investigators/site staff, persons performing assessments, and Novartis study personnel remained blinded to individual treatment assignment from time of randomization until the final database lock at Week 52." Comment: adequate procedure to guarentee blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote:"Patients, investigators/site staff, persons performing assessments, and Novartis study personnel remained blinded to individual treatment assignment from time of randomization until the final database lock at Week 52." Comment: adequate procedure to guarentee blinding of assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote:"The primary analysis was based on the full analysis set.For the primary efficacy variable, data for patients with missing post‐baseline value were not imputed, and patients were included in the analysis if they had both baseline and post‐baseline assessments. The primary analysis was based on the full analysis set. Changes from baseline in each cardiometabolic biomarker were analyzed at each time point using the same ANCOVA model as for the primary efficacy variable; missing data were imputed using the last‐observation‐carried‐forward method." Randomised 91; analysed 91 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02690701) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. Results are posted on ClinicalTrials.gov |
NCT02748863.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: April 2016 ‐ June 2018 Location: worldwide (52 sites) Phase 3 |
|
| Participants |
Randomised: 214 participants Inclusion criteria People eligible for inclusion in this study must fulfil all of the following criteria:
Exclusion criteria
Baseline characteristics N = 214 and 62% men Dropouts and withdrawals
Secukinumab 2 mL group (0), Secukinumab 1 mL group (2), Placebo group (2)
|
|
| Interventions |
Intervention
A.Secukinumab 2 mL form (secukinumab 300 mg/2 mL + 2 x 1 mL placebo SC. at randomisation, weeks 1, 3, 4, thereafter 4‐weekly until week 48), n = 72 Control interventions B.Secukinumab 1 mL form (secukinumab 150 mg/1 mL x 2 + 2 mL placebo SC. at randomisation, weeks 1, 3, 4, thereafter 4‐weekly until week 48), n = 71 C.Placebo (2 mL + 2 x 1 mL placebo SC at randomisation, weeks 1, 3, and 4, thereafter 4‐weekly until week 48), n = 71 |
|
| Outcomes |
At week 12 Primary composite outcome
Secondary outcomes
|
|
| Notes | Completed results on ClinicalTrials.gov Funding: Quote (ClinicalTrials.gov) Novartis Pharmaceuticals Conflict of interest: not stated RoB completed according to ClinicalTrials.gov protoco. In ClinicalTrials.gov, Other prespecified outcomes" such as assess the participant usability and assessment of Dermatology Life Quality Index (DLQI) scores are exploratory in nature and are not reported in these results |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol p17):"This is a 52‐week multicenter, randomized, double‐blind, placebo‐controlled, parallel‐group trial in approximately 210 subjects with moderate to severe plaque‐type psoriasis." Quote (protocol p26):"At Baseline/Randomization visit, all eligible subjects will be randomized via Interactive Response Technology (IRT) to one of the treatment arms. The investigator or his/her delegate will contact the IRT after confirming that the subject fulfills all the inclusion/exclusion criteria. The IRT will assign a randomization number to the subject, which will be used to link the subject to a treatment arm and will specify a unique medication number for the package of study drug to be dispensed to the subject." Comment: adequate process |
| Allocation concealment (selection bias) | Low risk | Quote (protocol p17):"This is a 52‐week multicenter, randomized, double‐blind, placebo‐controlled, parallel‐group trial in approximately 210 subjects with moderate to severe plaque‐type psoriasis." Quote (protocol p26):"Subjects, investigators/site personnel and Novartis clinical team reviewing data will remain blind to the identity of the treatment from the time of randomization, using the following methods: (1) randomization data are kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study. (2) the identity of the treatments will be concealed by the use of investigational treatment that are all identical in packaging, labeling, appearance, and schedule of administration." Comment: adequate process |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol p26):"Subjects, investigators/site personnel and Novartis clinical team reviewing data will remain blind to the identity of the treatment from the time of randomization, using the following methods: (1) randomization data are kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study. (2) the identity of the treatments will be concealed by the use of investigational treatment that are all identical in packaging, labeling, appearance, and schedule of administration." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol p26):"Subjects, investigators/site personnel and Novartis clinical team reviewing data will remain blind to the identity of the treatment from the time of randomization, using the following methods: (1) randomization data are kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study. (2) the identity of the treatments will be concealed by the use of investigational treatment that are all identical in packaging, labeling, appearance, and schedule of administration." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (protocol p67‐8):"The co‐primary efficacy variables are PASI 75 response at Week 12 and IGA mod 2011 0 or 1 response at Week 12. The analysis of the co‐primary variables will be based on the full analyses set (FAS)....Response variables based on PASI score and IGA mod 2011 categories will be imputed with multiple imputations (MI) method as primary imputation method." Randomised 214; analysed 214 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02748863). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported except for DLQI. Results posted on ClinicalTrials.gov |
NCT02850965.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind trial Date of study: August 2016 ‐ January 2018 Location: world‐wide |
|
| Participants |
Randomised: 318 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Biosimilar group (18), Humira group (25)
|
|
| Interventions |
Intervention A. Biological: BI 695501, S/C, Biosimilar adalimumab week 0: 80 mg, week 1: 40 mg, then 40 mg EOW (n = 159) Control Intervention B. Biological: adalimumab (Humira) week 0: 80 mg, week 1: 40 mg, then 40 mg EOW (n = 159) |
|
| Outcomes |
At 16 weeks Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov): Boehringer Ingelheim Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and clinical trial synopsis): "Allocation: randomized...Randomization will be performed in a blinded fashion via IRT. Patients will be randomized sequentially (the lowest sequentially available randomization number)." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and clinical trial synopsis): "Allocation: randomized...Randomization will be performed in a blinded fashion via IRT. Patients will be randomized sequentially (the lowest sequentially available randomization number)." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Double (Participant, Investigator)" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Double (Participant, Investigator)" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: not stated Results posted on ClinicalTrials.gov: Per protocol analyses (non‐inferiority trial) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02850965) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
NCT03051217.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: February 2017 Location: Japan (33 centres) Phase 2/3 |
|
| Participants |
Randomised: 127 participants Inclusion criteria
For patients with moderate‐to‐severe chronic plaque psoriasis (PSO)
Exclusion criteria
Baseline characteristics N = 127, mean age of 50 years and 62% men Dropouts and withdrawals
Certolizumab Pegol 200 group (2), Certolizumab Pegol 400 group (2), Placebo group (3)
|
|
| Interventions |
Intervention A. Certolizumab Pegol SC injection 400 mg at weeks 0, 2, 4, followed by Certolizumab Pegol SC injection 200 mg every 2 weeks (Q2W) with PBO administered to maintain the blind, starting at week 6, n = 48 Control interventions B. Certolizumab Pegol SC injection 400 mg every 2 weeks (Q2W), n = 53 C. Placebo SC injection every 2 weeks (Q2W), n = 26 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) "UCB Biopharma S.P.R.L." Conflict of interest: not stated RoB completed according to ClinicalTrials.gov protocol Actual Primary Completion Date: November 2018 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (study protocol p21, p43):"This is a phase 2/3, multicenter, randomised, double‐blind, PBO‐controlled study..."."An IRT will be used for assigning to a treatment (as applicable) based on predertermined production randomization and/or packaging schedule by UCB." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (study protocol p21, p43):"This is a phase 2/3, multicenter, randomised, double‐blind, PBO‐controlled study..."."An IRT will be used for assigning to a treatment (as applicable) based on predertermined production randomization and/or packaging schedule by UCB." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (study protocol p21, p43):Due to differences in presentation of the IMP
(CZP andPBO), special precautions will be taken
to ensure study blinding, and study sites will have blinded and unblinded personnel.
Certolizumab pegol and placebo injections will be prepared and administered at the study sites
by unblinded dedicated study personnel who will only be responsible for dosing and drug
accountability."This is a phase 2/3, multicenter, randomised, double‐blind, PBO‐controlled study." "Study sites will be required to have written blinding plan in place, signed by the principal investigator, which will detailed the site's steps for ensuring that hte double‐blind nature of study is maintained". Comment: uncertainity on the possibility of this process to guarentee blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (study protocol p43):Due to differences in presentation of the IMP
(CZP andPBO), special precautions will be taken
to ensure study blinding, and study sites will have blinded and unblinded personnel.
Certolizumab pegol and placebo injections will be prepared and administered at the study sites
by unblinded dedicated study personnel who will only be responsible for dosing and drug
accountability."Blinded study monitors and study site personnel, blinded to treatment assignment, will not discuss or have access to any drug‐related information." Comment: uncertainity on the possibility of this process to guarentee blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (study protocol p93):"Missing data for the primary endpoint will be handled using MCMC method for mutliple imputation...Additionnaly, algorithms for imputing missing or partial data for safety evaluations will be detailed in SAP." Randomized 127; analyzed 127 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03051217). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. Results are posted on ClinicalTrials.gov. |
NCT03055494.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: April 2017 Location: USA Phase 4 |
|
| Participants |
Randomised: 102 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 82, mean age of 44.5 years and 63% men Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab 300 mg SC at randomisation, weeks 1, 2, 3, and 4 followed by monthly dosing up to week 48, n = 54 Control interventions B. Placebo, n = 28 |
|
| Outcomes |
At week 12 Primary composite outcome
Secondary outcome
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) Novartis Pharmaceuticals Conflict of interest: not stated RoB completed according protocol posted on ClinicalTrials.gov |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (study protocol p 18, p 19):"This study uses a randomized, double‐blind, placebo‐controlled, parallel‐group, multicenter design. At the start of the Double‐blind Treatment Period, eligible patients will be randomized via Interactive Response Technology (IRT) in a 2:1 ratio to one of two treatment arms (secukinumab300 mg or placebo). Randomization will be stratified by body weigth collected at visit 2 (<90kg or >‐ 90kg)." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (study protocol p 18, p 19): "This study uses a randomized, double‐blind, placebo‐controlled, parallel‐group, multicenter desing... At the start of the Double‐blind Treatment Period, eligible patients will be randomized via Interactive Response Technology (IRT) in a 2:1 ratio to one of two treatment arms (secukinumab300 mg or placebo). Randomization will be stratified by body weigth collected at visit 2 (<90kg or >‐ 90kg)." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (study protocol p 32): "Patients, investigators/site staff, persons performing assessments, and Novartis study personnel will remain blinded to individual treatment assignment from the time of randomization until the final database lock at Week 53,using the following methods:1.Randomization data will be kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study with the following exceptions: specific vendors whose role in trial conduct requires their unblinding (e.g.,IRT), Drug Supply Management (DSM); 2.The identity of secukinumab and placebo prefilled syringes (PFS) will be concealed by identical packaging,labeling,schedule of administration, and appearance." Comment: clearly defined |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (study protocol p 32): "Patients, investigators/site staff, persons performing assessments, and Novartis study personnel will remain blinded to individual treatment assignment from the time of randomization until the final database lock at Week 53,using the following methods:1.Randomization data will be kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study with the following exceptions: specific vendors whose role in trial conduct requires their unblinding (e.g.,IRT), Drug Supply Management (DSM); 2.The identity of secukinumab and placebo prefilled syringes (PFS) will be concealed by identical packaging,labeling,schedule of administration, and appearance. At the Week 12 primary analysis time point, there will be a database lock after all patients have completed the Week 12 visit. At that time, onlythe statistician and programmer(s) from the designated CRO will be unblinded in order to perform the analysis." Comment: clearly defined |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Dealing with missing data: Quote (study protocol p 65): "For the two primary efficacy variables at Week 12 (and other time points), a patient with a missing assessment will be considered as a non‐responder." Randomised 102, analysed 82 In ClinicalTrials.gov (results section) :"a total of 133 patients were screened for the study, with 82 (61.7%) of these completing the screening phase". We are waiting for the publication to compare the number of randomised and analysed participants |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03055494) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
NCT03066609.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: February 2017 ‐ November 2018 Location: China, Hungary, Malaysia, Turkey, Thailand, Philippines Phase 3 |
|
| Participants |
Randomised: 543 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 543, mean age of 50 years and 62% men Dropouts and withdrawals
Secukinumab 150 group (2), Secukinumab 300 group (2), Placebo group (2)
|
|
| Interventions |
Intervention A. Secukinumab 150 mg: 150 mg SC at randomisation, weeks 1, 2, 3, 4 and every 4 weeks til week 48, n = 136 Control interventions B. Secukinumab 300 mg: 300 mg SC at randomisation, weeks 1, 2, 3, 4 and every 4 weeks til week 48, n = 272 C. Placebo, n = 135 |
|
| Outcomes |
At week 12 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) Novartis Pharmaceuticals. Conflict of interest: not stated RoB completed according to ClinicalTrials.gov protocol Actual Primary Completion Date: November 2018 |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and study protocol p 29):"A Randomized, Double‐blind, Placebo Controlled, Multicenter Study of Subcutaneous Secukinumab..." and "At Baseline visit all eligible subjects will be randomized via Interactive Response Technology (IRT) to one of the treatment arms. Randomization will be stratified by geographical region and presence of psoriatic arthritis collected at the Randomization." Comment: adequate process |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and study protocol p 29):"A Randomized, Double‐blind, Placebo Controlled, Multicenter Study of Subcutaneous Secukinumab..." and "The randomization numbers will be generated using the following procedure, to ensure that treatment assignment is unbiased and concealed from subjects and investigator staff. A subject randomization list will be produced by the IRT provider using a validated system that automates the random assignment of subject numbers to randomization numbers. These randomization numbers are linked to the different treatment arms, which in turn are linked to medication numbers." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (study protocol p 29):"Subjects, investigator staff, persons performing the assessments and data analyst will remain blind to the identity of the treatment from the time of randomization until database lock, using the following methods: (1) Randomization data are kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study. (2) the identity of the treatments will be concealed by the use of investigational treatment that are all identical in packaging, labeling, schedule of administration, appearance, taste and odor." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (study protocol p 29):"Subjects, investigator staff, persons performing the assessments and data analyst will remain blind to the identity of the treatment from the time of randomization until database lock, using the following methods: (1) Randomization data are kept strictly confidential until the time of unblinding, and will not be accessible by anyone else involved in the study. (2) the identity of the treatments will be concealed by the use of investigational treatment that are all identical in packaging, labeling, schedule of administration, appearance, taste and odor." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (study protocol p 68):"Response variables based on PASI score and IGA mod 2011 score will be imputed with multiple imputation (MI) as primary imputation method for the missing values." Randomly assigned 543,analysed 543 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03066609) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
NCT03255382.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label study with blinded assessment of the efficacy outcome Date of study: August 2017 ‐ July 2018 Location: Germany (23 sites) Phase 3 |
|
| Participants |
Randomised: 120 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 120, mean age of 42 years and 59% men Dropouts and withdrawals
Risankizumab group (0), Fumaderm 300 group (13)
|
|
| Interventions |
Intervention A. Risankizumab 150 mg by subcutaneous injection at weeks 0, 4, and 16, n = 60 Control intervention B. Fumaderm 30 mg administered as a tablet orally once daily from week 0 to Week 2, then up to 240 mg, n = 60 |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) AbbVie Conflict of interest: not stated RoB completed according to ClinicalTrials.gov protocol |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (study protocol p 59):"All subjects will be centrally randomized using an Interactive Voice Response System/Interactive Web Response System (IVRS/IWRS). Before the study is initiated, the telephone number/call‐in directions and web based information for the IVRS/IWRS will be provided to each site.'' Comment: adequate process |
| Allocation concealment (selection bias) | Low risk | Quote (study protocol p 59):"All subjects will be centrally randomized using an Interactive Voice Response System/Interactive Web Response System (IVRS/IWRS). Before the study is initiated, the telephone number/call‐in directions and web based information for the IVRS/IWRS will be provided to each site.'' Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (study protocol p 60):"This is an open‐label study; however, the efficacy assessor will be blinded to the patient's study treatment." |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (study protocol p 60):"This is an open‐label study; however, the efficacy assessor will be blinded to the patient's study treatment." Comment: no description of method used to guarantee no communication between participants and assessors. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (ClinicalTrials.gov and study protocol p7):"The efficacy analysis will be performed in the Intent to Treat (ITT) set which includes all subjects who are randomized. Missing data will be imputed using non‐responder imputation, i.e., a subject with missing PASI90 at Week 24 will be considered a non‐responder in the primary analysis... For categorical secondary endpoints, the same statistical test as for the primary endpoint will be used, missing data will be imputed using non‐responder imputation." Randomly assigned 120, analysed 120 Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03255382) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
NCT03331835.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label study with blinded assessment of the efficacy outcome Date of study: November 2017 ‐ March 2019 Location: Germany (30 sites) Phase 4 |
|
| Participants |
Randomised: 210 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 210 and 69% men Dropouts and withdrawals
Reasons not stated |
|
| Interventions |
Intervention A. Brodalumab (Kyntheum® (brodalumab) pre‐filled syringe 210 mg/1.5 mL solution for subcutaneous injections. First 3 injections are administered weekly, and thereafter every 2 weeks (Q2W)), n = 105 Control interventions B. Fumaric acid esters (Fumaderm® initial dose tablets (30 mg dimethyl fumarate, 67 mg ethyl hydrogen fumarate calcium salt, 5 mg ethyl hydrogen fumarate magnesium salt, 3 mg ethyl hydrogen fumarate zinc salt) Fumaderm® tablets (120 mg dimethyl fumarate, 87 mg ethyl hydrogen fumarate calcium salt, 5 mg ethyl hydrogen fumarate magnesium salt, 3 mg ethyl hydrogen fumarate zinc salt) Fumaderm® tablets are administered orally up to 3 times daily in accordance with the dosing scheme in the label), n = 105 |
|
| Outcomes |
At week 24 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) LEO pharma Conflict of interest: not stated RoB completed according to ClinicalTrials.gov protocol |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: (protocol p46) Randomisation will be with stratification by body weight (<100 kg or ≥100 kg) using an IWRS system. Coments: adequate process |
| Allocation concealment (selection bias) | Low risk | Quote (study protocol p46):"Treatment assignment will be pre‐planned according to a computer generated randomisation schedule in a 1:1 ratio. Randomisation will be with stratification by body weight (<100 kg or ≥100 kg) using an IWRS system". Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (study protocol p46):"This is an open‐label trial... Blinded assessments of PASI, sPGA, BSA, and NAPSI will be performed. Blinded assessors who perform the assessment must be medically qualified physicians trained in the assessments. During the assessments, the subjects will be instructed not to reveal the treatment allocation and the blinded assessor must avoid asking questions that could reveal treatment allocation. All involved personnel will be instructed to desist from any discussions regarding safety, efficacy, treatment allocation of the study and subjects in the presence of the blinded assessor. In case a blinded assessor becomes unblinded, a new assessor should be appointed to perform the assessments of the subject going forward." |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (study protocol p46):"This is an open‐label trial... Blinded assessments of PASI, sPGA, BSA, and NAPSI will be performed. Blinded assessors who perform the assessment must be medically qualified physicians trained in the assessments. During the assessments, the subjects will be instructed not to reveal the treatment allocation and the blinded assessor must avoid asking questions that could reveal treatment allocation. All involved personnel will be instructed to desist from any discussions regarding safety, efficacy, treatment allocation of the study and subjects in the presence of the blinded assessor. In case a blinded assessor becomes unblinded, a new assessor should be appointed to perform the assessments of the subject going forward." |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dealing with missing data: Quote (ClinicalTrials.gov and study protocol p7):"All subjects randomised are included in the full analysis set (FAS) and will be used for efficacy analyses. Missing data for categorical endpoints will be imputed with non‐responder imputation. Missing data for continuous endpoints will be dealt with by a mixed model for repeated measurements." Randomly assigned 210 Safety set analysis 206; Full set analysis 196/185/81 Comment: not ITT analysis, reasons for withdrawal not reported |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03331835) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
NCT03482011.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: April 2018 ‐ January 2020 Location: worldwide (45 sites) Phase 3 |
|
| Participants |
Randomised: 530 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 530, mean age of 46.5 years and 70% men Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Mirikizumab, 250 mg, SC every 4 weeks, , n = 423 Control interventions B. Placebo, SC every 4 weeks, , n = 107 |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcome
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) Eli Lilly and Company Conflict of interest: not stated RoB completed according study protocol posted on ClinicalTrials.gov |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (study protocol p 28):" Study AMAK is a Phase 3, multicenter, randomized, double‐blind, placebo‐controlled, parallel‐group, multi‐period study..." (protocol p 42): "Assignment to treatment groups will be determined by a computer‐generated random sequence unsing an interactive web‐response system(IWRS).IWRS will be used to assign prefilled syringes containing double‐blind investigational product to each patient." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (study protocol p 28):" Study AMAK is a Phase 3, multicenter, randomized, double‐blind, placebo‐controlled, parallel‐group, multi‐period study..." (protocol p 42): "Assignment to treatment groups will be determined by a computer‐generated random sequence unsing an interactive web‐response system (IWRS). IWRS will be used to assign prefilled syringes containing double‐blind investigational product to each patient." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (study protocol p 42): "This is a double blind study. The blinding applies to patients, site personnel and sponsor personnel." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (study protocol p 42): "This is a double blind study. The blinding applies to patients, site personnel and sponsor personnel." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (study protocol p 70):"Efficacy analysis for induction outcomes will be conducted on the Induction intent‐to‐treat (ITT) population." Quote (study protocol p 72): "Non‐Responder Imputation (NRI) for Binary Clinical Response: Patients will be considered non‐responders for the NRI analysis if they do not meet the clinical response criteria or have missing clinical response data at the analysis time point. Mixed‐Effects Model for Repeated Measures (MMRM): It will be the primary analysis method for longitudinal continuous measurements." Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: The protocol for the study was available on ClinicalTrials.gov (NCT03482011). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
Nugteren‐Huying 1990.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: not stated Setting: multicentre in the Netherlands |
|
| Participants |
Randomised: 39 participants (mean age 44 years, 27 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Dimethylfumarate (n = 12), orally, 120 mg, gradual increase 1 ‐ 6 tablets, once a day, 16 weeks Control intervention B. Octyl hydrogen fumarate (n = 10), orally, 284 mg, gradual increase 1 ‐ 6 tablets, once a day, 16 weeks C. Placebo (n = 12), orally, once a day, 16 weeks |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 331): "The patients were randomly assigned..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 331): "The patients were randomly assigned..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 331): “The double‐blind treatment lasted 16 weeks for each patients... All tablets (provided by Fumapharm AG, Muri, Switzerland) had the same appearance, size and colour” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 331): “The double‐blind treatment lasted 16 weeks for each patients...All tablets (provided by Fumapharm AG, Muri, Switzerland) had the same appearance, size and color” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 39, analysed 34 Comment: no description of the method used to perform analyses of the primary outcome and to manage missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Ohtsuki 2017.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial, phase 2 Date of study: July 2013 ‐ December 2015 Location: Japan |
|
| Participants |
Randomised: 254 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Apremilast 30 group (9), Apremilast 20 group (16), Placebo group (12)
|
|
| Interventions |
Intervention: A. Apremilast (30 mg tablet twice a day for 68 weeks), n = 85 Control intervention: B. Apremilast (20 mg tablet twice a day for 68 weeks), n = 85 C. Placebo, n = 84 |
|
| Outcomes |
At week 16 Primary outcome:
Secondary outcomes:
|
|
| Notes | Funding Quote (p 883): "The authors received editorial support in the preparation of the manuscript from Kathy Covino, Ph.D., of Peloton Advantage, LLC, funded by Celgene Corporation. This study was funded by Celgene Corporation." Conflict of interest Quote (p 883): "Mamitaro Ohtsuki reports consultancy and speaker fees. Yukari Okubo reports consultancy fees. Shinichi Imafuku reports research funds, consultancy fees and speaker fees. Robert M. Day, Peng Chen, Rosemary Petric and Allan Maroli report stock or shares in Celgene Corporation and/or employment by Celgene Corporation. Osamu Nemoto has no relevant financial or personal relationships and no potential conflicts of interest to declare." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 874): "After the screening period, eligible patients began a 16‐week placebo‐controlled period and were randomized via a centralized interactive web response system or interactive voice response system (1:1:1) to placebo, apremilast 20 mg b.i.d. or apremilast 30 mg b.i.d." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 874): "After the screening period, eligible patients began a 16‐week placebo‐controlled period and were randomized via a centralized interactive web response system or interactive voice response system (1:1:1) to placebo, apremilast 20 mg b.i.d. or apremilast 30 mg b.i.d." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 874): "This phase 2b multicenter, randomized, double‐blind, placebo‐controlled study" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 874): "This phase 2b multicenter, randomized, double‐blind, placebo‐controlled study" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (p 874): "Efficacy and safety assessments were conducted for the modified intent‐to‐treat (mITT) population, which included all patients who were randomized and received at least one dose of study medication; patients not dispensed study medication were excluded from the mITT population... For the primary analysis of PASI‐75, missing values were accounted for using the last observation carried forward methodology; multiple sensitivity analyses (including nonresponder imputation [NRI]) were conducted for the primary end‐point" Randomised 254; analysed 254 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01988103) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. |
Ohtsuki 2018.
| Study characteristics | ||
| Methods | RCT, phase 3, randomised, double‐blind, placebo‐controlled study Date of study: 15 January 2015 ‐ 11 November 2016 Location: Japan (35 sites) |
|
| Participants |
Randomised: 192 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Gusel 100 group (1), Gusel 50 group (2), Placebo group (12)
|
|
| Interventions |
Intervention: A. Guselkumab 100 mg with SC injections at weeks 0, 4, and every 8 weeks thereafter (n = 63) Control intervention: B. Guselkumab 50 mg with SC injections at weeks 0, 4, and every 8 weeks thereafter (n = 65) C. Placebo (n = 64) |
|
| Outcomes |
At week 16 Primary outcome:
Secondary outcomes:
|
|
| Notes | Funding Quote (p 883): "Funding: This study was funded by Janssen Pharmaceutical,Tokyo, Japan." Conflict of interest Quote (p 1062): "M. O. has received honoraria and/or research grants as a consultant and/or advisory board member and/or paid speaker and/or investigator from Abbvie, Boehringer‐Ingelheim, Celgene, Eisai, Janssen, Kyowa‐Kirin, LEO Pharma, Eli Lilly, Maruho, Novartis, Pfizer, Tanabe‐Mitsubishi, Nichiiko, Torri, Bayer, Pola Pharma, Taiho, Bristol‐Myers Squibb, Astellas, Otsuka, Mochida, Nippon Zoki, Actelion, Sanofi, Kaken Pharmaceuticals, Teijin Pharma, Nippon Kayaku, Shionogi, Ono and Galderma. H. N. has received honoraria and/or research grants as an advisory board member and/or speaker from ABC Pharma, Kyowa Hakko Kirin, Abbvie, Mitsubishi‐Tanabe Pharma, LEO Pharma, Maruho, Eli Lilly Japan, Janssen. H. K., H. M., R. G. and R. Z. are employees of Janssen Pharmaceutical." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1054): "Randomization was performed centrally using a computer‐generated randomization scheme, balanced using randomly permuted blocks and stratified by presence of PsA." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1054): "Randomization was performed centrally using a computer‐generated randomization scheme, balanced using randomly permuted blocks and stratified by presence of PsA." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1054): "This was a phase 3, randomized, double‐blind, placebo‐controlled study conducted in Japan... Study site personnel, investigators and patients were blinded to treatment allocation until week 52 database lock." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1054): "This was a phase 3, randomized, double‐blind, placebo‐controlled study conducted in Japan... Study site personnel, investigators and patients were blinded to treatment allocation until week 52 database lock." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dealing with missing data: Quote (p 1054): "The randomized analysis set included all randomized patients for efficacy analyses, and data were analyzed by treatment groups...Last observation was carried forward for other patients with missing data." Randomised: 192; analysed: 192 Imbalance reasons and number of withdrawal: Gusel 100 group (1%), Gusel 50 group (2%), Placebo group (20%) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02325219) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Olsen 1989.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: not stated Setting: not stated |
|
| Participants |
Randomised: 15 participants, age range 23 ‐ 72 years, 11 male Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 10), orally, 25/50 mg, daily, 8 weeks Control intervention B. Placebo (n = 5), orally, daily, 8 weeks |
|
| Outcomes | Assessments at 8 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding by Hoffman‐La Roche Inc Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 681): "Patients were assigned to... in a random, double‐blind fashion" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 681): "Patients were assigned to... in a random, double‐blind fashion" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 681): "Patients were assigned to... in a random, double‐blind fashion" Comment: visible adverse effects of acitretin such as cheilitis were visible |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 681): "Patients were assigned to... in a random, double‐blind fashion" Comment: visible adverse effects of acitretin such as cheilitis were visible |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 15 included / Number of participants analysed not stated Comment: no description of the methods used to perform the efficacy analyses and to manage the missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section were reported |
OPT Pivotal‐1 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double blind Date of study: 12 January 2012–18 September 2014 Location: multicentre (74) in USA, Canda, Colombia, Germany, Japan, Hungary, Serbia, Taiwan, Ukraine |
|
| Participants |
Randomised: 901 participants (mean age 46 years, 643 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 363), orally, 5 mg twice daily Control intervention B. Tofacitinib (n = 360), orally, 10 mg twice daily B. Placebo (n = 177), orally (same drug administration) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 949): "Pfitzer Inc" Declarations of interest (appendix): "K.A.P. has participated in advisory boards or panels for AbbVie, Amgen, Astellas, Baxter, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, LEO Pharma, Merck, Novartis, Pfizer Inc. and UCB. He has been an investigator for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Genentech, Janssen, LEO Pharma, Merck, Novartis, Pfizer, Takeda and UCB. He has acted as a consultant for AbbVie, Amgen, Astellas, Baxter, Boehringer Ingelheim, Celgene, Eli Lilly, Forward Pharma, Janssen, Merck, Novartis, Pfizer Inc., Takeda and UCB. He has been a speaker for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Genentech, Janssen, LEO Pharma, Merck, Novartis, Pfizer and UCB. M.A.M. has participated in advisory boards or panels for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Genentech, Janssen Biotech, LEO Pharma and Pfizer Inc. He has served as a consultant for AbbVie, Allergan, Amgen, Convoy Therapeutics, Eli Lilly, Janssen Biotech, LEO Pharma, Novartis, Pfizer Inc., Syntrix, Wyeth and XenoPort. He has been an Investigator for AbbVie, Allergan, Amgen, ApoPharma, Boehringer Ingelheim, Celgene, Convoy Technologies, Eli Lilly, Genentech, Janssen Biotech, LEO Pharma, Merck, Novartis, Pfizer Inc., Symbio/Maruho, Syntrix and Wyeth. He has been a speaker for AbbVie, Amgen, Janssen Biotech, LEO Pharma and Wyeth. He has received grants from AbbVie, Allergan, Amgen, ApoPharma, Boehringer Ingelheim, Celgene, Convoy Technologies, Genentech, Janssen Biotech, LEO Pharma, Merck, Pfizer Inc., Symbio/Maruho and Syntrix. He has received honoraria from AbbVie, Allergan, Amgen, Boehringer Ingelheim, Convoy Technologies, Eli Lilly, Genentech, Janssen Biotech, LEO Pharma, Novartis, Pfizer Inc., Syntrix, Wyeth and XenoPort." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 951): “Randomization using an automated web/telephone randomization system at the study site ensured patient, investigator and sponsor blinding ” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 951): “Randomization using an automated web/telephone randomization system at the study site ensured patient, investigator and sponsor blinding ” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 951): “Investigator and sponsor blinding… with placebo tablets according to the treatment group, appropriately labelled to avoid treatment‐group conflict. All patients took a total of two tablets for each dose” Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 951): “Investigator and sponsor blinding… with placebo tablets according to the treatment group, appropriately labelled to avoid treatment‐group conflict. All patients took a total of two tablets for each dose” Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 901, analysed 900 Management of missing data: Quote (p 951): "The full analysis set included all patients who were randomised and received at least one dose of the study drug...Nonresponder imputation was used to manage missing values." Comment: withdrawal for lack of efficacy: tofacitinib 5 group 5% (20/363), tofacitinib 10 group 4% (15/360), placebo group 14% (25/177) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01276639). The pre‐specified outcomes and those mentioned in the methods section appeared to have been reported. |
OPT Pivotal‐2 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: 4 March 2011 – 18 September 2014 Location: multicentre (94) in Mexico, Poland, Puerto Rico, Serbia, Taiwan, Ukraine |
|
| Participants |
Randomised: 960 participants (mean age 46 years, 648 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 382), orally, 5 mg twice daily Control intervention B. Tofacitinib (n = 381), orally, 10 mg twice daily C. Placebo (n = 196), orally (same drug administration) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 949): "Pfitzer Inc" Declarations of interest (appendix) : "K.A.P. has participated in advisory boards or panels for AbbVie, Amgen, Astellas, Baxter, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, LEO Pharma, Merck, Novartis, Pfizer Inc. and UCB. He has been an investigator for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Genentech, Janssen, LEO Pharma, Merck, Novartis, Pfizer, Takeda and UCB. He has acted as a consultant for AbbVie, Amgen, Astellas, Baxter, Boehringer Ingelheim, Celgene, Eli Lilly, Forward Pharma, Janssen, Merck, Novartis, Pfizer Inc., Takeda and UCB. He has been a speaker for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Genentech, Janssen, LEO Pharma, Merck, Novartis, Pfizer and UCB. M.A.M. has participated in advisory boards or panels for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Genentech, Janssen Biotech, LEO Pharma and Pfizer Inc. He has served as a consultant for AbbVie, Allergan, Amgen, Convoy Therapeutics, Eli Lilly, Janssen Biotech, LEO Pharma, Novartis, Pfizer Inc., Syntrix, Wyeth and XenoPort. He has been an Investigator for AbbVie, Allergan, Amgen, ApoPharma, Boehringer Ingelheim, Celgene, Convoy Technologies, Eli Lilly, Genentech, Janssen Biotech, LEO Pharma, Merck, Novartis, Pfizer Inc., Symbio/Maruho, Syntrix and Wyeth. He has been a speaker for AbbVie, Amgen, Janssen Biotech, LEO Pharma and Wyeth. He has received grants from AbbVie, Allergan, Amgen, ApoPharma, Boehringer Ingelheim, Celgene, Convoy Technologies, Genentech, Janssen Biotech, LEO Pharma, Merck, Pfizer Inc., Symbio/Maruho and Syntrix. He has received honoraria from AbbVie, Allergan, Amgen, Boehringer Ingelheim, Convoy Technologies, Eli Lilly, Genentech, Janssen Biotech, LEO Pharma, Novartis, Pfizer Inc., Syntrix, Wyeth and XenoPort." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 951): “Randomization using an automated web/telephone randomization system at the study site ensured patient, investigator and sponsor blinding ” Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 951): “Randomization using an automated web/telephone randomization system at the study site ensured patient, investigator and sponsor blinding ” Comment: no description of the method to guarantee the allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 951): “Investigator and sponsor blinding… with placebo tablets according to the treatment group, appropriately labelled to avoid treatment‐group conflict. All patients took a total of two tablets for each dose” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 951): “Investigator and sponsor blinding… with placebo tablets according to the treatment group, appropriately labelled to avoid treatment‐group conflict. All patients took a total of two tablets for each dose” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 960, analysed 959 Management of missing data: Quote (p 951): "The full analysis set included all patients who were randomised and received at least one dose of the study drug...Nonresponder imputation was used to manage missing values." Comment: imbalance of withdrawal between groups: lack of efficacy: tofacitinib 5 group (15), tofacitinib 10 group (2), placebo group (24) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01276639) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. |
ORION 2020.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: March 2017 ‐ 07 February 2018 Location: world‐wide Phase 3 |
|
| Participants |
Randomised: 78 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Guselkumab group (3), Placebo group (1)
|
|
| Interventions |
Intervention A. Guselkumab (100 mg guselkumab administered as a 100 mg/mL solution in a single‐use prefilled syringe (PFS) assembled in a self‐dose device at weeks 0, 4, 12, 20, and 28), n = 62 Control intervention Placebo, n = 16 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (p 7): "Janssen Research & Development, LLC funded this study. Authors employed by Janssen participated in designing the study; collecting, analyzing, and interpreting the data; and in preparing, reviewing, and approving the manuscript. A professional medical writer supported by Janssen provided editorial and submission support." Conflict of interest: Quote (p 7): "Laura K. Ferris has been an investigator and consultant for EliLilly, Janssen, and Pfizer; a consultant for UCB; and an investigator for AbbVie, Amgen, Galderma, Leo Pharma, and Regeneron. H. Chih‐Ho Hong has been an investigator/consultant/or advisory board member for AbbVie, Amgen, Eli Lilly, Galderma, Janssen, Leo Pharma, Merck, Novartis, Pfizer, Regeneron, Sanofi, and UCB. Elyssa Ott, Jingzhi Jiang, Shu Li, and Chenglong Han are employed by Janssen Research & Development, LLC and own stock/stock options in its parent company. Wojciech Baran has been an investigator and consultant for AbbVie, Amgen, Eli Lilly, Janssen, Leo Pharma, Merck, Mylan, Novartis, Pfizer, and Regeneron." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and p 2): "Allocation: randomized"; "ORION (Clinicaltrials.gov identifier: NCT02905331) was a Phase 3, multicentre, double‐blind, placebo‐controlled study in which patients were centrally randomized (4:1) to receive...Randomization employed a computer‐generated permuted block schedule with stratification by country. An interactive web response system assigned a unique treatment code dictating treatment assignment and matching study drug kit. Codes were not provided to investigators. Guselkumab and placebo were delivered by identical devices (see Interventions)." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and p 2): "Allocation: randomized"; "ORION (Clinicaltrials.gov identifier: NCT02905331) was a Phase 3, multicentre, double‐blind, placebo‐controlled study in which patients were centrally randomized (4:1) to receive...Randomization employed a computer‐generated permuted block schedule with stratification by country. An interactive web response system assigned a unique treatment code dictating treatment assignment and matching study drug kit. Codes were not provided to investigators. Guselkumab and placebo were delivered by identical devices (see Interventions)." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and p 2): "Double (Participant, Investigator)"; " Patients randomized to guselkumab received placebo at Week 16 to maintain the blind...Guselkumab and placebo were delivered by identical devices (see Interventions)." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and p 2): "Double (Participant, Investigator)"; " Patients randomized to guselkumab received placebo at Week 16 to maintain the blind...Guselkumab and placebo were delivered by identical devices (see Interventions)." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (p 3):"Efficacy analyses employed all randomized patients who received 1 injection of study agent, analyzed according to assigned treatment groups (full analysis set). The co‐primary endpoints were the proportions of patients achieving IGA 0/1 and PASI90 responses at Week 16. Patients who met treatment failure criteria (discontinued study agent due to lack of efficacy/an AE of worsening psoriasis or started a protocol‐prohibited treatment before Week 16) were considered nonresponders for the co‐primary endpoints at Week 16, as were patients who did not return for evaluation at Week 16." Randomised 78; analysed 78 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02905331) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Ortonne 2013.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label study Date of study: 21 September 2007 ‐ August 2009 Setting: 17 centres in Austria, France, Greece and Italy |
|
| Participants |
Randomised: 72 participants randomised, 69 analysed (mean age 46 years, 50 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept twice‐a‐week/once‐a‐week group (n = 38), 50 mg SC twice a week for 12 weeks then 50 mg once a week to week 24 Control intervention B. Etanercept once‐a‐week/once‐a‐week group (n = 34), 50 mg SC injections once a week for the full 24‐week treatment period |
|
| Outcomes | Assessments at 24 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 1080): "TWyeth Research, which was acquired by Pfizer in October 2009, sponsored this clinical trial and was responsible for the collection and analysis of data. Editorial ⁄medical writing assistance was funded by Pfizer Inc." Declarations of interest (p 1080):" J.P.O. has been an investigator or consultant for Schering‐Plough, Abbott, Merck‐Serono, Centocor, Pfizer, Janssen‐Cilag, Meda‐Pharma, Pierre‐Fabre, Galderma and Leo‐Pharma. C.P. has been an investigator or consultant for Abbott, Amgen, Celgene, Janssen Cilag, Leo Pharma, Novartis and Pfizer Inc. E.B. has no conflicts of interest. V.M., G.G., Y.B. and J.M.G. are employees of Pfizer Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1081): “Patients were randomised by the investigator or other authorized person using an automatic online enrolment system in a 1:1 ratio” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1081): “Patients were randomised by the investigator or other authorized person using an automatic online enrolment system in a 1:1 ratio” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 1081): “This was a multicenter, multinational, randomised, open‐label study” Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 1081): “This was a multicenter, multinational, randomised, open‐label study” Comment: not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 72 included/69 analysed Quote (p 1082): "All efficacy analyses were based on the modified intent‐to treat (mITT) population, which was defined as all patients who had received one or more doses of ETN and had baseline and post baseline data...The MMRM and GEE models have been developed for the analysis of longitudinal categorical data and to handle missing data without any imputation; this kind of model is preferred to the last‐observation carried forward approach for analysis of longitudinal data" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: The protocol for the study was available on ClinicalTrials.gov (NCT00581100) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Papp 2005.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: 50 centres in USA, Canada and Western Europe |
|
| Participants |
Randomised: 611 participants (mean age 45 years, male 382 out of 583 participants who received 1 dose) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 204), SC, 25 mg twice a week, 12 weeks Control intervention B. Etanercept (n = 203), SC, 50 mg twice a week, 12 weeks C. Placebo (n = 204), SC, twice a week, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 1304): "This study was supported by Immunex Corporation (Seattle, WA, U.S.A)" Declarations of interest: (p 1304) S.T. has received research support from Amgen; C.E.M.G. has been a paid consultant for Wyeth and Amgen; A.M.N and R.Z. are both full‐time employees of Amgen." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 1305): "Patients were randomly assigned (using an Interactive Voice Response system) to receive placebo or etanercept) Comment: not stated |
| Allocation concealment (selection bias) | Low risk | Quote (p 1305): "Patients were randomly assigned (using an Interactive Voice Response system) to receive placebo or etanercept) Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1305): “ the patients, study site personnel and all sponsor representatives remained blinded to the initial randomisation treatment groups...” Comment: placebo‐controlled, probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1305): “ the patients, study site personnel and all sponsor representatives remained blinded to the initial randomisation treatment groups...” Comment: placebo‐controlled, probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 611 randomised participants, 583 analysed (28 participants did not receive the treatment and were excluded from the analyses) Sensitivity analysis (Table 2) were performed with the 611 randomised participants Management of missing data: Quote "In the analyses, missing post baseline efficacy data were imputed using last observation carried forward. In addition, a sensitivity analysis was performed on the binary efficacy endpoints to evaluate the robustness of the primary analysis. This sensitivity analysis included all randomised patients. In addition, rather than using LOCF imputation patients with missing data at a given visit were assumed to have not met the response criteria for that endpoint". Comment: the main result (primary outcome) was not an ITT analysis |
| Selective reporting (reporting bias) | High risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported except for the results of participant‐reported endpoints summarised in a separate publication |
Papp 2012a.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: December 2009 – April 2010 Location: 23 centres worldwide |
|
| Participants |
Randomised: 198 participants (mean age 42 years, 107 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Brodalumab 70 (n = 39), SC, 70 mg, day 1‐weeks 1, 2, 4, 6, 8, 10, 10 weeks Control intervention B. Brodalumab 140 (n = 39), SC, 140 mg, day 1 and weeks 1, 2, 4, 6, 8, 10, 10 weeks C. Brodalumab 210 (n = 40), SC, 210 mg, day 1 and weeks 1, 2, 4, 6, 8, 10, 10 weeks D. Brodalumab 280 (n = 42), SC, 280 mg, day 1 and weeks 1, 2, 4, 6, 8, 10, 10 weeks E. Placebo (n = 38), SC, day 1 and weeks 1, 2, 4, 6, 8, 10, 10 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 1182): "The study was funded by Amgen" Declarations of interest (pp 1188‐9): "Dr. Papp reports receiving consulting fees from Abbott, Amgen, Astellas, Celgene, Centocor, Eli Lilly, Galderma, Graceway Pharmaceuticals, Janssen, Johnson & Johnson, Merck, Norvartis, Pfizer, and UCB, lecture fees from Abbott, Amgen, Astellas, Celgene, Centocor, Galderma, Janssen, LEO Pharma, Merck, Novartis, Pfizer, and Stiefel, and grant support from Abbott, Amgen, Astellas, Celgene, Centocor, Eli Lilly, Galderma, Glaxo‐SmithKline, Graceway Pharmaceuticals, Janssen, Johnson & Johnson, Medimmune, Merck, Novartis, Pfizer, Stiefel, and UCB; Dr. Leonardi, receiving consulting fees from Abbott, Amgen, Centocor, Eli Lilly, and Pfizer, lecture fees from Abbott and Amgen, and investigator fees from Abbott, Amgen, Celgene, Centocor, Galderma, GlaxoSmithKline, Incyte, Maruho, Novartis, Novo Nordisk, Pfizer, Schering‐Plough (now Merck), Sirtris, Stiefel, Vascular Biogenics, and Wyeth (now Pfizer); Dr. Menter, receiving consulting fees from Abbott, Amgen, Astellas, Centocor, Galderma, Genentech, and Wyeth, lecture fees from Abbott, Amgen, Centocor, Galderma, and Wyeth, and fees for expert testimony from Galderma; Dr. Krueger, receiving consulting fees from Centocor, Eli Lilly, and Pfizer and grant support from Amgen, Centocor, Eli Lilly, Merck, and Pfizer; and Drs. Krikorian, Aras, Li, Russell, Thompson, and Baumgartner being full‐time employees of Amgen. No other potential conflict of interest was relevant to this article was reported." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (protocol p 30): “Randomization: IVRS will be used to randomise subjects into the study. The randomisation list will be generated by Amgen using a permuted block design within each of 4 strata based on BMI at baseline, and participation in the PK study” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (protocol p 30): “Randomization: IVRS will be used to randomise subjects into the study." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (protocol p 24 and 50): “double‐blind placebo controlled... Subjects randomised to active drug will receive additional placebo injections as necessary to maintain the blind” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (protocol p 39): "PASI assessments will be performed by a blinded assessor. The blinded assessor will be a healthcare professional who has been certified as trained with the standard PASI" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 198 included/198 analysed Quote (p 1183): "The analyses of efficacy endpoints were performed on data from all patients who underwent randomisation (full set analysis), according to the intention‐to‐treat principle... Missing data were handled by means of the baseline‐value‐carried‐forward method or the imputation of no response" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00307437) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Papp 2012b.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: July 2008 ‐ August 2009 Location: 42 centres in USA, Canada |
|
| Participants |
Randomised: 197 participants (tofacitinib 2 mg (49) mean age 46 years, 29 male; tofacitinib 5 (49) mean age 44 years, 29 male; tofacitinib 15 (49) mean age 44 years, 31 male; placebo (n = 50) mean age 44 years, 36 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tofacitinib (n = 49), orally, 2 mg, twice a day, 12 weeks Control intervention B. Tofacitinib, (n = 49), orally, 5 mg, twice a day, 12 weeks C. Tofacitinib (n = 49), orally, 15 mg, twice a day, 12 weeks D. Placebo (n = 50), orally, twice a day, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 668): "This study was funded by Pfizer Inc" Declarations of interest (appendix): "K.A.P. has been a principal investigator, an advisor or consultant, a Scientific Officer, member of a Scientific Advisory Board and a speaker for the following groups: Abbott, Amgen, Astellas, Celgene, Centocor‐Ortho Biotech, Incyte, Isotechnika, Janssen, Lilly, Medimmune, Merck, Pfizer Inc. and Novartis. A.M. has been on the Advisory Board, been a consultant to, been an investigator for, been a speaker for, obtained a research grant from, or obtained honoraria from the following groups: Abbott, Allergan, Amgen, Astellas, Asubio, Celgene, Centocor, DUSA, Eli Lilly, Galderma, Genentech, Novartis, Novo Nordisk, Pfizer Inc., Promius, Stiefel, Syntrix Biosystems, Warner Chilcott and Wyeth. B.S. has been a principal investigator, an advisor or consultant, or a speaker for the following groups: Abbot, Amgen, Celgene, Centocor‐Ortho Biotech, Janssen, Pfizer Inc., Maruho and Novartis. R.G.L. has been an investigator, served as a principal investigator or on the Advisory Board, or been a speaker for the following groups: Abbott, Amgen, Centocor⁄Ortho Biotech, Pfizer Inc., Novartis and Celgene. R.W., S.K., H.T., P.G. and M.B. are employees of Pfizer Inc. J.A.H. was a full‐time employee of Pfizer Inc. during the conduct and reporting of the study and now works at Novartis Pharma AG, Basel, Switzerland. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 669): "A computer‐generated central randomisation schema was implemented in an automated web ⁄telephone system." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 669): "A computer‐generated central randomisation schema was implemented in an automatedTreatment identification was concealed by use of study drugs that were identical in labelling, packaging, appearance and odour" web ⁄telephone system." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 669): "Patients, investigational site staff, the Pfizer study team and data analysts were blinded to treatment from the time of randomisation until database lock... Treatment identification was concealed by use of study drugs that were identical in labelling, packaging, appearance and odour" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 669): "Patients, investigational site staff, the Pfizer study team and data analysts were blinded to treatment from the time of randomisation until database lock... Treatment identification was concealed by use of study drugs that were identical in labelling, packaging, appearance and odour" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 197 included / 195 analysed Quote (p 670): "The full analysis set included all randomised patients who received one or more doses of investigational drug...This population ... represents a modified intent‐to‐treat analysis... Patients with missing values had the missing values imputed but last observation carried forward.... As a sensitivity analysis the patients [with missing values] were also considered nonresponders (NRI)" Comment: mITT and 2 participants out of 197 not analysed |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00678210) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Papp 2012c.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: September 2008 ‐ October 2009 Location: 35 centres in Canada and USA |
|
| Participants |
Randomised: 352 participants (mean age 44 years, 221 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Apremilast (n = 88), orally, 30 mg, twice a day, 16 weeks Control intervention B. Apremilast (n = 176), orally, 10 ‐ 20 mg twice a day, 16 weeks C. Placebo (n = 88), orally, twice a day 16 weeks |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source Quote (p 738): "Funding Celgene Corporation" Declarations of interest quote (p 745): "KP has served as an investigator for Abbott, Amgen, Celgene, Centocor, Galderma, Incyte, Isotechnika, Janssen, Lilly, Medimmune, Merck, Novartis, and Pfizer; an adviser for Abbott, Amgen, Astellas, BMS, Celgene, Centocor, Galderma, Incyte, Isotechnika, Janssen, Johnson & Johnson, Lilly, Medimmune, Merck, Novartis, Pfizer, and UCB; and a speaker for Abbott, Amgen, Astellas, Celgene, Centocor, Isotechnika, Janssen, Novartis, and Pfizer. JCC has served as an investigator for Celgene, Centocor, Novartis, and Pfizer; as a speaker for Centocor and Abbott; and as an adviser for Pfizer, Abbott, and Novartis. LR has been a paid investigator for doing clinical trials for Amgen, Genentech, Abbott, Centocor, Basilea, Leo, Isotechnika, Stiefel, GSK, Galderma, 3‐M, Serono, Novartis, Astellas, UCB, Celgene, Johnson & Johnson, and Pfizer. HS has served as an investigator for Abbott, Centocor, Celgene, Amgen, and Pfizer; as a speaker for Abbott and Centocor; and as an adviser for Centocor. RGL has served as an investigator for Abbott, Centocor, Celgene, Amgen, Pfizer, Johnson & Johnson/Ortho Biotech, and Novartis; as a speaker for Abbott, Centocor, Amgen, Pfizer, Johnson & Johnson/Ortho Biotech, and Novartis; and as an adviser for Abbott, Centocor, Celgene, Amgen, Pfizer, Johnson & Johnson/Ortho Biotech, and Novartis. RTM has served as an investigator for Abbott, Centocor, Celgene, Amgen, Novartis, Lilly, Pfizer, Allergan, and Galderma; as a speaker for Centocor and Amgen; and as an adviser for Centocor. CH and RMD are employees of Celgene Corporation." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 739): "Eligible patients were randomly assigned in a 1:1:1:1 ratio to oral apremilast 10 mg twice daily, apremilast 20 mg twice daily, apremilast 30 mg twice daily, or placebo, with a permuted‐block randomisation list generated by an interactive voice response system (ClinPhone, East Windsor, NJ, USA)." Comment: clearly described |
| Allocation concealment (selection bias) | Low risk | Quote (p 739): "Eligible patients were randomly assigned in a 1:1:1:1 ratio to oral apremilast 10 mg twice daily, apremilast 20 mg twice daily, apremilast 30 mg twice daily, or placebo, with a permuted‐block randomisation list generated by an interactive voice response system (ClinPhone, East Windsor, NJ, USA)." Comment: clearly described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 739): "Treatment was double‐blind for the first 16 weeks of the 24‐week treatment phase." Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 739): "Treatment was double‐blind for the first 16 weeks of the 24‐week treatment phase." Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 352 included / 352 analysed Quote (p 740): "Efficacy data were assessed by intention to treat. Missing data were handled with the last‐observation carried‐forward method." Comment: number of lost to follow‐up and reasons comparable across group |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00773734) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Papp 2013a.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: March 2010 ‐ February 2011 Location: 19 international centres |
|
| Participants |
Randomised: 125 participants (mean age 46 years, 91 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab (n = 29), SC, 25 mg, 0, 4, 8 weeks, 12 weeks Control intervention B. Secukinumab (n = 26), SC, 3 x 25 mg, 0, 4, 8 weeks, 12 weeks C. Secukinumab (n = 21), SC, 3 x 75 mg, 0, 4, 8 weeks, 12 weeks D. Secukinumab (n = 27), SC, 3 x 150 mg, 0, 4, 8 weeks, 12 weeks E. Placebo (n = 22), SC, 0, 4, 8 weeks, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source (p412): "Novartis Pharm AG, Basel, Switzerland" Declarations of interest (Appendix): "K.A.P. has received honoraria for lecturing at industry‐sponsored meetings and has received industry funding for presentations and consultation at national and international meetings; he has also received research grants from and been a paid consultant to Novartis and other pharmaceutical companies; has served as a scientific officer for pharmaceutical and biotechnology corporations; and is a participant on clinical, scientific and corporate advisory boards. R.G.L. has been a member of scientific advisory boards and served as a clinical investigator for Abbott, Amgen, Celgene, Centocor⁄Johnson & Johnson, Eli Lilly, Fujisawa, Novartis and Pfizer, and has served as a speaker for Abbott, Amgen, Centocor⁄Johnson & Johnson, Fujisawa and Novartis. B.S. has consulted for Novartis and several other pharmaceutical companies; he has been a member of an advisory board for Novartis and several other pharmaceutical companies. S.H., H.J.T., C.P. and H.B.R. are full‐time employees of and own stock in Novartis. M.A., D.R.B. and P.K. declare no conflicts of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 414): “The randomisation numbers were generated by an interactive voice response provider using a validated automated system” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 414): “The randomisation numbers were generated by an interactive voice response provider using a validated automated system” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 413‐4): “Double‐blind, placebo controlled...Patients, investigator staff, persons performing the assessments and data analysts were blinded ... remained blind until final database lock” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 413‐4): “Double‐blind, placebo controlled...Patients, investigator staff, persons performing the assessments and data analysts were blinded ... remained blind until final database lock” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 125 included/125 analysed Quote (p 415): "The full analysis set consisted of all patients who were randomised... The missing score was imputed by carrying forward the last non missing post baseline PASI" Comment: very high number of withdrawals (38%) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01071252) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Papp 2013b.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: April 2006 ‐ May 2007 Location: multicentre (30) in Canada, the Czech Republic, and Germany |
|
| Participants |
Randomised: 260 participants (mean age 46 years, 163 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Apremilast (n = 173), orally, 10 ‐ 20 mg, twice a day, 12 weeks Control intervention B. Placebo (n = 87) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source quote (p 27): "This study was sponsored by Celgene Corporation" Declarations of interest (p27): "Dr Papp is a consultant and investigator for Celgene Corporation, Abbott, Amgen, Centocor, Janssen‐Ortho, Merck, Novartis and Pfizer and an investigator for Astellas, Leo Pharma and Galderma, receiving honoraria and grants. Dr Kaufmann is an investigator for Abbott, Centocor, Leo, Novartis, Wyeth and Celgene Corporation, but has not received financial compensation. The Department of Dermatology received investigator fees for performing the clinical trials. He served as a speaker for Basilea and Allmiral and received honoraria from each. Dr Thac ¸ is on the advisory board of and is a consultant, investigator and speaker for Abbott, Leo, Novartis, Pfizer, Biogen‐Idec, Janssen‐Cilag and MSD, and received honoraria from each. He is also an investigator for Celgene Corporation. The Department of Dermatology received honoraria ⁄ compensation for conducting studies; no direct compensation was received. Ms Hu receives a salary as an employee of Celgene Corporation. Ms Sutherland receives a salary, stocks and stock options as an employee of Celgene Corporation. Dr Rohane received a salary and stock options as a former employee of Celgene Corporation. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 377): " investigators randomised subjects 1 : 1: 1 to double‐blind treatments for 12 weeks with placebo, apremilast 20 mg QD or apremilast 20 mg twice daily" Comment: no description of the method to guarantee the random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote (p 377): "Using an interactive voice response system, investigators randomised subjects 1 : 1: 1 to double‐blind treatments" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 377): "One capsule of placebo or apremilast was taken orally in the morning before meals, and one capsule of placebo or apremilast was taken in the evening" Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 377): "One capsule of placebo or apremilast was taken orally in the morning before meals, and one capsule of placebo or apremilast was taken in the evening" Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 260 included / 260 analysed Management of missing data was not stated and substantial number lost to follow‐up (18%) |
| Selective reporting (reporting bias) | High risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00606450). The pre‐specified outcomes listed on ClinicalTrials.gov were not detailed, the choice of the primary outcome was not clearly defined. In the Methods section, PASI 75 was defined as the primary outcome, no QoL outcomes were listed in the Methods section although they were in the protocol on ClinicalTrials.gov |
Papp 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: November 2010 ‐ June 2012 Location: 64 centres in Europe, Asia and North America |
|
| Participants |
Randomised: 355 participants (mean age 45 years, 270 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Tildrakizumab (n = 42), SC, 5 mg weeks 0, 4, every 12 weeks Control intervention B. Tildrakizumab (n = 92), SC, 15 mg weeks 0, 4, every 12 weeks C. Tildrakizumab (n = 89), SC, 50 mg weeks 0, 4, every 12 weeks D. Tildrakizumab (n = 86), SC, 100 mg weeks 0, 4, every 12 weeks E. Tildrakizumab (n = 46), SC, 200 mg weeks 0, 4, every 12 weeks |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 930): “This study was funded by Merck & Co, nc., Kenilworth, NJ, USA”. Declarations of interest (Appendix 1): "E.P.B., A.M., Q.L., Y.Z. and R.S. are current or former employees of Merck & Co., Inc. K.P. has served as a consultant, advisory board member and/or investigator for Abbott (AbbVie), Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Foreward Pharma, Galderma, Genentech, Incyte, Isotechnika, Janssen, Kyowa Kirin, LEO Pharma, Lilly, Medimmune, Merck Sharp Dome, Merck Serono, Novartis, Regeneron, Stiefel, Takeda, Pfizer and USB. D.T. has served as a consultant, advisory board member and/or investigator for Abbott (AbbVie), Almiral, Amgen, Astellas, Biogen Idec, Boehringer Ingelheim, Celgene, Dignity, Forward Pharma, Galderma, GlaxoSmithKline, Isotechnika, Janssen‐Cilag, LEO Pharma, Lilly, Maruho, Medac, Medimmune, Merck Sharp Dome, Merck Serono, Novartis, Regeneron, Sandoz, Sanofi‐Aventis, Takeda and Pfizer. K.R. has served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Amgen, Biogen Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Lilly, Medac, Merck, Novartis, Pfizer, Vertex and Takeda. E.R. has received travel support and nonfinancial support for histology study report preparation from Merck & Co., Inc., and has received speaker’s fees and travel support, or served on advisory boards for Abb‐ Vie, Novartis, Pfizer, Janssen and Amgen. R.G.L. has served as a consultant and/or paid speaker for and/or participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis, including AbbVie, Celgene, Centocor, Janssen‐Cilag, LEO Pharma, Merck, MSD (formerly Essex, Schering‐Plough), Novartis and Pfizer (formerly Wyeth). J.G.K. has received personal fees (consulting and/or speaking fees) and grants paid to his institution from Novartis, Pfizer, Janssen, Lilly, Merck, Kadmon, Dermira, Boehringer and BMS; Amgen, Innovaderm, Paraxel and Kyowa have paid grants to J.G.K.’s institution; J.G.K. has also received personal fees from Serono, Biogen Idec, Delenex, AbbVie, Sanofi, Baxter, Xenoport and Kineta. A.B.G. has current consulting/advisory board agreements with Amgen Inc., Astellas, Akros, Centocor (Janssen) Inc., Celgene Corp., Bristol Myers Squibb Co., Beiersdorf Inc., Abbott Labs (AbbVie), TEVA, Actelion, UCB, Novo Nordisk, Novartis, Dermipsor Ltd, Incyte, Pfizer, Canfite, Lilly, Coronado, Vertex, Karyopharm, CSL Behring Biotherapies for Life, GlaxoSmithKline, Xenoport, Catabasis Meiji Seika Pharma Co., Ltd, Takeda, Mitsubishi Tanabe Pharma Development America, Inc, and has received research/educational grants (paid to Tufts Medical Center) from Centocor (Janssen), Amgen, Abbott (Abb‐ Vie), Novartis, Celgene, Pfizer, Lilly, Coronado, Levia, Merck and Xenoport. H.N. has received consultancy/speaker honoraria and/or grants from Novartis, Tanabe Mitsubishi, Maruho, Abbott/AbbVie, Eli Lilly, Merck Sharp & Dohme, Janssen and LEO Pharma." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 931): “Randomisation of treatment and allocation was done centrally by means of an interactive web response system…" Comment: no description of the method used to guarantee the random sequence generation |
| Allocation concealment (selection bias) | Low risk | Quote (p 931): “Randomisation of treatment and allocation was done centrally by means of an interactive web response system…” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (p 931): “double‐blind" Comment: no description of the method used to guarantee blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 932): “double‐blind" Comment: no description of the method used to guarantee blinding |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 355, analysed 352 Management of missing data: Quote (p 932): “The primary analysis was performed on all randomised participants who received at least one or more doses of treatment. Participants who discontinued treatment prior to week 16... were considered to not have achieved PASI 75 at week 16" Comment: low number lost to follow‐up |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01225731) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Papp 2017a.
| Study characteristics | ||
| Methods | RCT, phase 3, randomised, double‐blind, active‐controlled study Date of study: August 2014 ‐ March 2015 Location: world‐wide |
|
| Participants |
Randomised: 350 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Biosimilar group (23), Humira 50 group (19)
|
|
| Interventions |
Intervention: A. ABP 501 at an initial loading dose of 80 mg subcutaneously on week 1/day 1, followed by 40 mg subcutaneously every other week (starting at week 2) for 16 weeks, n = 175 Control intervention: B. Adalimumab, Humira, at an initial loading dose of 80 mg subcutaneously on week 1/day 1, followed by 40 mg subcutaneously every other week (starting at week 2) for 16 weeks, n = 175 |
|
| Outcomes |
At week 16 Primary outcome:
Secondary outcomes:
|
|
| Notes | Funding Quote (p 1093): "Amgen Inc funded this study and participated in the design and conduct of the study; collection, management, analysis, and interpretation of data; and preparation, review, and approval of the manuscript. All authors were involved in the decision to submit the manuscript for publication, and had the right to accept or reject comments or suggestions. A medical writer employed by MedVal Scientific Information Services LLC and funded by Amgen Inc participated in the writing of this manuscript and is acknowledged." Conflicts of interes t Quote (p 1093): "Dr Papp has served as a consultant, speaker, scientific officer, steering committee member, investigator,or advisory board member for3M, Abbott, Akesis, Akros, Alza, Amgen, Astellas, Baxter, BMS, Boehringer Ingelheim, CanFite, Celgene, Cipher, Dermira, Eli Lilly, Forward Pharma, Funxional Therapeutics, Galderma, GSK, Isotechnika, Janssen, Johnson & Johnson, Kirin, Kyowa, Lypanosys, MedImmune, Merck‐Serono, Mitsubishi Pharma, MSD, Novartis, Pfizer, Roche, Takeda, UCB, Valeant, and Vertex. Dr Bachelez has served as a consultant, speaker, steering committee member, investigator, or advisory board member for AbbVie, Amgen, Baxalta, Boehringer‐Ingelheim, Celgene, Janssen, LEO Pharma, Lilly, MSD, Novartis, Pfizer, and Takeda, and received grant support from Pfizer. Dr Costanzo has been an investigator/consultant and speaker for AbbVie, Amgen, Celgene, Janssen, Lilly, Novartis, and Pfizer. Dr Foley has served as a consultant, investigator, speaker, and/or advisor for, and/or received travel grants from Galderma, LEOPharma/Peplin, Ascent,Clinuvel, Janssen‐Cilag, Eli Lilly, Australian Ultraviolet Services, Roche, CSL, 3M/iNova/Valeant, GSK/ Stiefel, Abbott/AbbVie, Biogen Idec, Merck Serono, Schering‐Plough/MSD, Wyeth/Pfizer, Amgen, Novartis, Celgene, Aspen, Boehringer Ingelheim, and BMS. Dr Gooderham has been an investigator, consultant, and/or speaker for AbbVie,Amgen, Boehringer Ingelheim, Celgene,Coherus, Dermira, Galderma, Janssen, LEO Pharma, Lilly, Medimmune, Merck Serono, Novartis, Regeneron, Roche, Sanofi Genzyme, Takeda, and Pfizer. Dr Kaur is an Amgen employee and stockholder. Dr Narbutt is an investigator for Amgen. Dr Philipp has been investigator, consultant, and/or speaker for AbbVie, Amgen, Almirall, Biogen, Boehringer‐Ingelheim, BMS, Celgene, Janssen, LEO Pharma, Lilly, MSD, Novartis, Pfizer, and UCB. Dr Spelman has served on advisory boards for Galderma, Novartis, and AbbVie; undertakes sponsored clinical research for AbbVie, Amgen, Anacor, Ascend Biopharmaceuticals, Astellas, Australian Wool Innovation Limited, Blaze Bioscience, Celgene, Dermira, Eli Lilly, Galderma, Genentech, GlaxoSmith Kline, Kythera, LEO Pharma, Merck, Novartis, Phosphagenics, Regeneron, and Trius; and has received sponsored travel from Abbott, Novartis, and Janssen‐Cilag. Dr Weglowska has been an investigator for Amgen, Pfizer, Novartis, Galderma, Eli Lilly, Dermira, Roche, Janssen‐Cilag, Coherus, Genentech, LEO Pharma, Merck, Mylan, and Regeneron. Dr Zhang is an Amgen employee and stockholder. Dr Strober has served on a speakers bureau for AbbVie, receiving honoraria; is a consultant and advisory board member for AbbVie, Amgen, Astra Zeneca, Celgene, Dermira, Forward Pharma, Janssen, LEO Pharma, Eli Lilly, Cutanea‐Maruho, Medac, Novartis, Pfizer, Sun, Stiefel/GlaxoSmithKline, UCB, and Boehringer Ingelheim, receiving honoraria for all; is an investigator for AbbVie, Amgen, GlaxoSmithKline, Novartis, Lilly, Janssen, Merck, XenoPort, Xoma, Celgene (payments to the University of Connecticut); is scientific director for Corrona Psoriasis Registry, receiving a consulting fee; received grant support to the University of Connecticut for a fellowship program fromAbbVie and Janssen." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1095): "This randomized, double‐blind, multicenter, active‐controlled phase III trial consisted of a 4‐week screening period, after which eligible patients were randomized 1:1 to receive treatment with ABP 501 or adalimumab...Randomization was carried out by a computer‐generated randomization schedule with stratification by prior biologic use and geographic region. Patients were allocated by an interactive voice and web response system." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1095): "This randomized, double‐blind, multicenter, active‐controlled phase III trial consisted of a 4‐week screening period, after which eligible patients were randomized 1:1 to receive treatment with ABP 501 or adalimumab...Randomization was carried out by a computer‐generated randomization schedule with stratification by prior biologic use and geographic region. Patients were allocated by an interactive voice and web response system." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1095): "This randomized, double‐blind, multicenter, active‐controlled phase III trial consisted of a 4‐week screening period, after which eligible patients were randomized 1:1 to receive treatment with ABP 501 or adalimumab...During the study, the patients, investigators, study center personnel, and sponsor remained blinded to the patient’s randomized treatment assignment. ABP 501 and adalimumab were administered in identical syringes" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1095): "This randomized, double‐blind, multicenter, active‐controlled phase III trial consisted of a 4‐week screening period, after which eligible patients were randomized 1:1 to receive treatment with ABP 501 or adalimumab...During the study, the patients, investigators, study center personnel, and sponsor remained blinded to the patient’s randomized treatment assignment. ABP 501 and adalimumab were administered in identical syringes" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (p1096): "Efficacy data were analyzed using the full analysis set, which included all patients initially randomized in the study with missing values imputed using the last observation carried forward method." Randomised 350; analysed 345 (equivalence design) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01970488) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. |
Papp 2017b.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial, phase 2 Date of study: February 2014 ‐ July 2015 Location: world‐wide |
|
| Participants |
Randomised: 166 participants Inclusion criteria
Exclusion criteria
With regards to TB the following applies:
Dropouts and withdrawals
Risan 18 (4), Risan 90 (2), Risan 180 (2), USK (1)
|
|
| Interventions |
Intervention A. Drug: Risankizumab (low dose) (18 mg BI 655066 administered by SC injection plus 2 placebo‐matching BI 655066 injections at week 0, followed by 2 placebo‐matching BI 655066 injections each at weeks 4 and 16), n = 43 Control intervention B. Drug: BI 655066 (median dose) (90 mg BI 655066 administered by SC injection plus 2 placebo‐matching BI 655066 injections at week 0, followed 90 mg BI 655066 plus 1 placebo‐matching BI 655066 injection at weeks 4 and 16), n = 41 C. Drug: BI 655066 (high dose) (180 mg BI 655066 administered by SC injection as 2 injections plus a placebo‐matching BI 655066 injection at week 0, followed 180 mg BI 655066 administered as 2 injections at 2eeks 4 and 16), n = 42 D. Drug: ustekinumab (Stelara administered by SC injection plus 2 saline injections at week 0, Stelara injection plus 1 saline injection at weeks 4 and 16. Stelara dose was 45 mg for participants with body weight ≤ 100 kg at randomisation or 90 mg for participants with body weight > 100 kg at randomisation), n = 40 |
|
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 1553): "The trial was funded by Boehringer Ingelheim" Conflicts of interest Quote (p 1560): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 1552): "This 48‐week, multicenter, randomized, dose‐ranging, phase 2 trial." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 1552): "The trial was double blind within the risankizumab dose groups and single blind (to patients) with regard to drug (ustekinumab or risankizumab). All efficacy assessments were conducted by an assessor who was unaware of the treatment assignments." Comment: No blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1552): "The trial was double blind within the risankizumab dose groups and single blind (to patients) with regard to drug (ustekinumab or risankizumab). All efficacy assessments were conducted by an assessor who was unaware of the treatment assignments." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (p 1553): "Primary and other end points were analyzed on an intention‐to‐treat basis... In the primary analyses, last observation carried forward was prespecified in the trial protocol as the method of handling missing data; a sensitivity analysis with nonresponse imputation was also performed" 166 randomised, 166 analysed Comment: Done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02054481) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results posted on ClinicalTrials.gov |
Papp 2018.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial, phase 2 Date of study: Novermber 2016 ‐ November 2017 Location: 82 sites In the USA, Japan, Poland, Canada, Germany, Latvia, Mexico, and Australia |
|
| Participants |
Randomised: 267 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
BMS‐986165_3EOD (10), BMS‐986165_3 (8), BMS‐986165_3*2 (3), BMS‐986165_6*2 (6), BMS‐986165_12 (2), PBO (14)
|
|
| Interventions |
Intervention: A. BMS‐986165 3 mg every other day (EOD) (by mouth), n = 44 Control intervention: B. BMS‐986165 3 mg a day (by mouth), n = 44 C. BMS‐986165 3 mg*2 a day (by mouth), n = 45 D. BMS‐986165 6 mg*2 a day (by mouth), n = 45 E. BMS‐986165 12 mg a day (by mouth), n = 44 F Placebo, n = 45 |
|
| Outcomes |
At week 12 Primary outcome:
Secondary outcomes:
|
|
| Notes | Funding Quote (p 1320): "Supported by Bristol‐Myers Squibb." Conflicts of interest Quote (p 1320‐21): "Dr. Papp reports receiving grant support, consulting fees, advisory board fees, and fees for serving on a speakers’ bureau from Amgen, AbbVie, Boehringer Ingelheim, Eli Lilly, Janssen, Leo Pharma, Novartis, Pfizer, UCB, Valeant Pharmaceuticals, and Kyowa Hakko Kirin, grant support, consulting fees, and fees for serving as a scientific officer from Akros Pharma, consulting fees from Can‐Fite BioPharma, grant support, consulting fees, advisory board fees, fees for serving on a speakers’ bureau, and travel support from Celgene, grant support, consulting fees, and advisory board fees from Merck Sharp & Dohme, PRCL Research, and Takeda, grant support from Anacor Pharmaceuticals, GlaxoSmithKline, and Meiji Seika Pharma, and grant support and consulting fees from Coherus BioSciences and Dermira; Dr. Gordon, receiving grant support and consulting fees from AbbVie, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Eli Lilly, Janssen, Novartis, and UCB and consulting fees from Amgen, Almirall, Dermira, Leo Pharma, Pfizer, and Sun Pharma; Dr. Thaçi, receiving grant support, lecture fees, consulting fees, and advisory board fees from AbbVie, lecture fees, consulting fees, and advisory board fees from Almirall, Pfizer, Sandoz/Hexal, UCB, Regeneron Pharmaceuticals, and Sanofi, consulting fees and advisory board fees from Boehringer Ingelheim, grant support, lecture fees, consulting fees, advisory board fees, and writing assistance from Celgene and Novartis, and lecture fees, consulting fees, advisory board fees, and writing assistance from Eli Lilly, Leo Pharma, and Janssen‐Cilag; Dr. Morita, receiving grant support and lecture fees from AbbVie, Esai, Kyowa Hakko Kirin, Leo Pharma, Maruho, Mitsubishi Tanabe Pharma, Novartis, and Torii Pharmaceutical and lecture fees from Celgene, Eli Lilly Japan, and Janssen Pharmaceutical; Dr. Gooderham, receiving advisory board fees, fees for serving as principal investigator, and lecture fees from AbbVie, Galderma, Leo Pharma, Pfizer, and Regeneron Pharmaceuticals, advisory board fees and lecture fees from Actelion Pharmaceuticals, fees for serving as principal investigator and consulting fees from Akros Pharma, advisory board fees, fees for serving as principal investigator, lecture fees, and consulting fees from Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen, Novartis Pharmaceuticals, Sanofi Genzyme, and Valeant Pharmaceuticals, fees for serving as principal investigator from Arcutis Pharmaceuticals, Bristol‐Myers Squibb, Dermira, GlaxoSmithKline, MedImmune, Merck, Roche Laboratories, and UCB, and fees for serving as principal investigator and lecture fees from Glenmark; Dr. Foley, receiving grant support, advisory board fees, fees for serving on a speakers’ bureau, and travel support from AbbVie, Celgene, CSL, Galderma, iNova Pharmaceuticals, Janssen, Leo Pharma, Eli Lilly, Novartis, Pfizer, and Sanofi, grant support and advisory board fees from Amgen and Sun Pharma, grant support from Boehringer Ingelheim, Celtaxsys, Cutanea Life Sciences, Dermira, Genentech, and Regeneron Pharmaceuticals, grant support, advisory board fees, and fees for serving on a speakers’ bureau from GlaxoSmithKline, grant support and consulting fees from Bristol‐Myers Squibb, and grant support, fees for serving on a speakers’ bureau, and travel support from Roche; Dr. Kundu, being employed by Bristol‐Myers Squibb; and Dr. Banerjee, being employed by and holding stock in Bristol‐Myers Squibb. No other potential conflict of interest relevant to this article was reported." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1314):"Randomization was stratified according to previous treatment with a biologic agent (yes or no) and geographic region (Japan or the rest of the world), with the use of a central interactive Web‐response system." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1314):"Randomization was stratified according to previous treatment with a biologic agent (yes or no) and geographic region (Japan or the rest of the world), with the use of a central interactive Web‐response system." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1314): "Patients were randomly assigned to one of five oral doses of BMS‐986165 (3 mg every other day, 3 mg daily, 3 mg twice daily, 6 mg twice daily, or 12 mg daily) or matching oral placebo in a ratio of 1:1:1:1:1:1. Capsules of the active drug (3 mg) or matched placebo were combined as appropriate to provide the required daily dose and were taken each morning and again 12 hours later...Patients, investigators, and the trial sponsor were unaware of the trial‐group assignments." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1314): "Patients were randomly assigned to one of five oral doses of BMS‐986165 (3 mg every other day, 3 mg daily, 3 mg twice daily, 6 mg twice daily, or 12 mg daily) or matching oral placebo in a ratio of 1:1:1:1:1:1. Capsules of the active drug (3 mg) or matched placebo were combined as appropriate to provide the required daily dose and were taken each morning and again 12 hours later...Patients, investigators, and the trial sponsor were unaware of the trial‐group assignments.'' Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (p 1315): "For the primary end point of PASI 75 and other binary end points (PASI 50, PASI 90, PASI 100, an sPGA score of 0 or 1, and a DLQI score of 0 or 1), patients who discontinued the trial regimen early or who had a missing value at any time point had outcomes imputed as a nonresponse at that time point, regardless of the status of response at the time of discontinuation." Randomised 267, analysed 267 Comment: Done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02931838) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
PEARL 2011.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: December 2008 ‐ March 2010 Location: 13 centres in Taiwan and Korea |
|
| Participants |
Randomised: 121 participants (mean age 41 years, 103 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab, SC, 45 mg, weeks 0, 4, 16 + placebo week 12, 16 weeks (n = 61) Control intervention B. Placebo, SC, weeks 0 ‐ 4 + ustekinumab 45 mg weeks 12 to 16 (n = 60) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source quote (p 162): "This study was supported by Centocore, Inc" Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 155): “Patients were enrolled in this multicenter..., double‐blind, placebo‐controlled study... Randomization was performed via an interactive voice response system based on minimization with bias‐coin assignment...”“Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject to a treatment arm and specified unique medication pack number" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 155): “Patients were enrolled in this multicenter..., double‐blind, placebo‐controlled study... Randomization was performed via an interactive voice response system based on minimization with bias‐coin assignment...” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 155): “Patients were enrolled in this multicenter..., double‐blind, placebo‐controlled study..." Comment: placebo trial, probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 155): “Patients were enrolled in this multicenter..., double‐blind, placebo‐controlled study..."Comment: placebo trial, probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 121, analysed 121 Quote (p 156): “For all efficacy analyses, patients were analysed by assigned treatment groups...Data were analysed by intent‐to‐treat for the primary endpoint... Patients who discontinued study treatment... were judged as non‐responders for binary endpoints” Comment: ITT analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available The prespecified outcomes mentioned in the Methods section appeared to have been reported |
PHOENIX‐1 2008.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: December 2005 – September 2007 Location: 48 centres in USA, Canada, Belgium |
|
| Participants |
Randomised: 766 participants (mean age 45 years, 531 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab (n = 255), SC, 45 mg, weeks 0 ‐ 4 and every 12 weeks, 40 weeks Control intervention B. Ustekinumab (n = 256), SC, 90 mg, weeks 0 ‐ 4 and every 12 weeks, 40 weeks C. Placebo (n = 255), SC, weeks 0 ‐ 4, 40 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, Quote (p 1665): Centocor Inc. Declarations of interest (p 1673): "CLL has served as a consultant for Abbott, Amgen, Centocor, and Genentech, as an investigator for Abbott, Allergan, Altana, Alza, Amgen, Astellas, Celgene, Centocor, Genentech, Bristol Myers, Eli Lilly, Fujisawa, Galderma, CombinatoRx, 3M Pharmaceuticals, Perrigo Isreal Pharamceutical, ScheringPlough, Serono, RTL, Novartis, Vitae, and Wyeth, and as a speaker for Abbott, Amgen, Centocor, Genentech, and Warner Chilcott. ABK has served as an investigator and consultant for Abbott, Amgen, and Centocor and has been a study steering committee member, speaker, and fellowship funding recipient from Centocor. KAP has served as a consultant and advisory board member for Abbott, Alza, Amgen, Celgene, Centocor, Johnson and Johnson, Isotechnika, Janssen Ortho Biotech, Medimmune, MerckSerono, and Wyeth. KBG has served as a consultant for Abbott, Amgen, Astellas, Centocor, and Genentech and has received grant support from Abbott, Astellas, and Centocor. NY, CG, YW, SL, and LTD are employees of Centocor and own stock in Johnson and Johnson." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (pp 1667‐68): “...via a centralised interactive voice response system” Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (pp 1667‐68): “...via a centralised interactive voice response system” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 1666‐67): “This phase 3, double‐blind, placebo‐controlled... Patients received placebo injections as needed to preserve the blind. The study sponsor was unblinded to treatment... Site monitors, investigators, site personnel involved in the study conduct, and patients remained blinded until week 76” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 1666‐67): “This phase 3, double‐blind, placebo‐controlled... Patients received placebo injections as needed to preserve the blind. The study sponsor was unblinded to treatment... Site monitors, investigators, site personnel involved in the study conduct, and patients remained blinded until week 76” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Included 255/256/255 Analysed 255/256/255 Quote (p 1668): "Efficacy data from all randomised patients were analysed according to the assigned treatment group.... Patients who discontinued study treatment... were deemed to be treatment failures" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00267969) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
PHOENIX‐2 2008.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: March 2006 – September 2007 Location: 70 centres in Europe and North America |
|
| Participants |
Randomised: 1230 participants (mean age 45 years, 840 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ustekinumab (n = 409), SC, 45 mg, weeks 0 ‐ 4 and every 12 weeks, 52 weeks Control intervention B. Ustekinumab (n = 411), SC, 90 mg, weeks 0 ‐ 4 and every 12 weeks, 52 weeks C. Placebo (n = 410), SC, weeks 0 ‐ 4, 4 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding Centocor Inc (p 1675) Declaration of interest (p 1684): "KP has served as a consultant and advisory board member for Abbott, Alza, Amgen, Celgene, Centocor, Isotechnika, Janssen Ortho Biotech, Johnson & Johnson, Medimmune, MerckSerono, and Wyeth. RGL has received research grants, served on scientific advisory boards, and has been a speaker for Amgen, Biogen‐Idec, Centocor, Genentech, Novartis, Schering‐Plough, and Serono. ML has received honoraria, served as a speaker and advisory board member for Abbott, Amgen, Centocor, Genentech, and Stiefel, and has served as an advisory board member for Astellas and a consultant for UCB. GK has received fees as a consultant or advisory board member for Abbott, Almirall, Alza, Amgen, Anacor, Astellas, Barrier Therapeutics, Boehringer Ingleheim, Bristol Myers Squibb, Centocor, CombinatoRx, Exelixis, Genentech, Genzyme, Isis, L’Oreal, Lupin Limited, Magen Biosciencs, MedaCorp, Medicis, Novartis, Nova Nordisc, Schering‐Plough, Somagenics, theDerm.org, Synvista, Warner Chilcot, UCB, USANA Health Sciences, and ZARS, owns equities and stock in ZARS, and has received lecture fees from Abbott, Amgen, Astellas, Boehringer Ingleheim, Centocor, Connetics, National Psoriasis Foundation, The Foundation for Better Health Care, and Warner Chilcot, and has received partial stipend support for a clinical research fellowship from Abbott, Amgen, and Centocor. KR has received honoraria as a consultant and advisory board member and acted as a paid speaker for Abbot, Biogen‐Idec, Centocor, Janssen‐Cilag, Schering‐Plough, MerckSerono, UCB, and Wyeth. PS, NY, CG, M‐CH, YW, SL, and LTD are employees of Centocor. PS, NY, CG, YW, SL, and LTD own stock in Johnson and Johnson." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1676): “Patients were randomly assigned... with bias coin assignment via a centralised interactive voice response system (ClinPhone, East Windsor, NJ, USA)” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1676): “Patients were randomly assigned... with bias coin assignment via a centralised interactive voice response system (ClinPhone, East Windsor, NJ, USA)” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 1676‐7): “Double‐blind,..., placebo‐controlled...Site monitors investigators personnel involved in the study conduct,and patients remained blinded... until W52” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 1676‐7): “Double‐blind,..., placebo‐controlled...Site monitors investigators personnel involved in the study conduct,and patients remained blinded... until W52” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1230 included/ 1230 analysed Quote (p 1679): "Efficacy data were analysed by the assigned treatment group... Non‐responder status was assigned for binary variables ... for those patients who discontinued study treatment ..." Comment: ITT analyses |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00307437) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
PIECE 2016.
| Study characteristics | ||
| Methods | RCT, active‐controlled Date of study: April 2009 and June 2011 Location: 5 centres in The Netherlands |
|
| Participants |
Randomised: 50 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention (n = 48) A. Infliximab (n = 25), IV, 5 mg/kg, weeks 0, 2, 6, 15, 22 Control intervention B. Etanercept (n = 23), SC, 50 mg twice weekly |
|
| Outcomes | Assessment at 24 weeks Primary outcomes of the trial PASI 75 Secondary outcomes of the trial QoL scale, Global assessment, treatment satisfaction |
|
| Notes | Funding source quote (p 1): "study was funded by a program grant from the Netherlands Organization for Scientific Research‐Medical Sciences (NWO‐MW; project 152001006)." Declaration of interest: "A.C.Q. de Vries: none reported; H.B. Thio: has been a consultant and invited speaker for Biogen/Idec, Janssen, Abbvie, Pfizer, MSD, Leopharma, Teva and Novartis. He has received educational grants from Abbvie, Janssen, Pfizer and Biogen/Idec.; W.J.A. de Kort: medical advisor for Novartis; B.C. Opmeer: none reported; H.M. van der Stok: Involved in performing clinical trials with Abbvie, Pfizer, Novartis, Janssen, BioClinic, AMGEN and LeoPharma.; E.M.G.J. de Jong: received research grants for the independent research fund of the department of dermatology of University Medical Centre St Radboud Nijmegen, the Netherlands from AbbVie, Pfizer, and Janssen. Has acted as consultant and/or paid speaker for and/or participated in research sponsored by companies that manufacture drugs used for the treatment of psoriasis including AbbVie, Janssen, MSD, and Pfizer.; B. Horvath: Unrestricted Educational Grant from AbbVie, IIS Studies by Janssen, AbbVie, Performing clinical trial Novartis, Solenne B.V., Consultancies: Abbvie, Janssen, Philips, Galderma.; J.J.V.Busschbach: none reported; T.E.C. Nijsten: received research grants for the independent research fund of the department of dermatology of Erasmus MC, Rotterdam, the Netherlands from AbbVie, Leo Pharma, MSD, Pfizer, and Janssen. Has acted as consultant and/or paid speaker for and/or participated in research sponsored by companies that manufacture drugs used for the treatment of psoriasis including AbbVie, Leo Pharma, Galderma, Janssen, MSD, and Pfizer. ; Ph.I. Spuls: consultancies in the past for Leopharma, AbbVie and Novartis. In the past an independent research grant from Schering Plough and from Leopharma. Involved in performing clinical trials with many pharmaceutical industries that manufacture drugs used for the treatment of psoriasis." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (pp 4 & 8): “...was a multi‐centre, single‐blind, investigator initiated, randomised controlled trial comparing infliximab and etanercept in the treatment of moderate to severe chronic plaque type psoriasis... Adequate generation of an unpredictable allocation sequence and concealment of allocation was achieved by using a secure online internet facility (the TEN‐ALEA Clinical Trial Data Management System, provided by the Trans European Network http://www.tenalea.com/) performed in the coordinating centre by the main investigators. The sequence was generated in random block sizes of two and four to ensure it was unknown and not predictable by the investigators involved in randomising participants." Comment: done |
| Allocation concealment (selection bias) | Low risk | Quote (pp 4 & 8): “...was a multi‐centre, single‐blind, investigator initiated, randomised controlled trial comparing infliximab and etanercept in the treatment of moderate to severe chronic plaque type psoriasis... Adequate generation of an unpredictable allocation sequence and concealment of allocation was achieved by using a secure online internet facility (the TEN‐ALEA Clinical Trial Data Management System, provided by the Trans European Network http://www.tenalea.com/) performed in the coordinating centre by the main investigators. The sequence was generated in random block sizes of two and four to ensure it was unknown and not predictable by the investigators involved in randomising participants." Comment: done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (pp 4 & 8): “...was a multi‐centre, single‐blind, investigator initiated, randomised controlled trial comparing infliximab and etanercept in the treatment of moderate to severe chronic plaque type psoriasis..." Comment: no blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 8): "Efficacy outcomes were carried out by trained assessors who were blinded to treatment allocation." Comment: no clear description of measures taken to guarantee the blinding of investigators |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 50, analysed 48 Quote (pp 8 & 9): "Missing data on primary endpoint were imputed using last observation carried forward. Analyses were carried out according to intention‐to‐treat (ITT) principle, apart from the longer term data where a per protocol analysis (PPA) was performed" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | The trial was prospectively registered on the Dutch Trial Register: www.trialregister.nl/trialreg/index.asp; NTR 1559 The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Piskin 2003.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label trial Date of study: not stated Location: Amsterdam and throughout the Netherlands, number not stated |
|
| Participants |
Randomised: 10 participants (ciclosporin (5), mean age 41 years, 4 male; methotrexate (5), mean age 45 years, 3 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ciclosporin (n = 5), orally, 3 mg/kg/d, 16 weeks Control intervention B. Methotrexate (n = 5), orally, 15 mg/kg/week, 16 weeks |
|
| Outcomes | Assessments at 12 weeks Primary and secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding not declared Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 559): "Patients were randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 559): "Patients were randomised..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 559): “Laboratory results were obtained in a blinded fashion before randomisation and at week 12 of therapy. The code was broken only after all definitive results were obtained from all participating patients." Comment: open‐label trial, no double dummy used to guarantee blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: no description of the method used to guarantee blinding of outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 10 included/10 analysed Comment: no statistical analyses section; however, the results were available for the 10 participants initially randomised. Methods for dealing with missing data: not applicable |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
POLARIS 2020.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label study Date of study: November 2016 ‐ September 2017 Location: Germany (multicentric) Phase 3 |
|
| Participants |
Randomised: 119 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Guselkumab group (4), FAEs group (23)
|
|
| Interventions |
Intervention A. Guselkumab (100 mg administered as 100 mg/mL solution SC by single‐use prefilled syringe (PFS) at weeks 0, 4, 12 and 20), n = 60 Control intervention B. FAEs (to this aim, FAE doses will be slowly increased beginning with increasing doses of Fumaderm initial (containing 30 mg dimethylfumarate) over the first 3 weeks. Thereafter, participants will be switched to Fumaderm tablets (containing 120 mg dimethylfumarate) starting with 1 tablet a day. Fumaderm dose may be increased to a maximum of 3 x 2 tablets a day), n = 59 |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (ClinicalTrials.gov): Janssen‐Cilag G.m.b.H Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "Procedures for Randomization Central randomization is implemented in this study. Subjects will be randomly assigned to 1 of 2 treatment groups (1:1 ratio) based on a computer generated randomization schedule prepared before the study by or under the supervision of the sponsor. Therandomization will be balanced by using randomly permuted blocks. The interactive web based eCRF will assign a unique treatment code, which will dictate the treatment assignment at baseline visit of the subject. The investigator will not be provided with randomization codes. The randomization codes will be stored invisible for the investigator in a separate, blind part of the EDC system." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "Procedures for Randomization Central randomization is implemented in this study. Subjects will be randomly assigned to 1 of 2 treatment groups (1:1 ratio) based on a computer generated randomization schedule prepared before the study by or under the supervision of the sponsor. Therandomization will be balanced by using randomly permuted blocks. The interactive web based eCRF will assign a unique treatment code, which will dictate the treatment assignment at baseline visit of the subject. The investigator will not be provided with randomization codes. The randomization codes will be stored invisible for the investigator in a separate, blind part of the EDC system." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (ClinicalTrials.gov and statistical analysis plan): "Blinding: As this is an open study, blinding procedures for the treatment are not applicable. However, a blinded efficacy evaluator will assess effectiveness of treatment as described in Section 9.2.3 of the CSP)... An independent, blinded efficacy assessor, approved by the Sponsor, will be designated at each study site to perform all efficacy assessments (BSA%, IGA, ssIGA, and PASI) starting with baseline visit until end of treatment phase (ie, Week 56)" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "Blinding: As this is an open study, blinding procedures for the treatment are not applicable. However, a blinded efficacy evaluator will assess effectiveness of treatment as described in Section 9.2.3 of the CSP)... An independent, blinded efficacy assessor, approved by the Sponsor, will be designated at each study site to perform all efficacy assessments (BSA%, IGA, ssIGA, and PASI) starting with baseline visit until end of treatment phase (ie, Week 56)" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dealing with missing data: Quote (ClinicalTrials.gov and statistical analysis plan): "Nonresponder imputation will be applied for binary endpoints i.e., subjects with missing data at Week 4/16/24 will be considered non‐responders at Week 4/16/24" Results posted on ClinicalTrials.gov: ITT Unbalance discontinuation proportion (< 1% for Guselkumab and 39% for FAEs) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02951533) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
PRESTA 2010.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind Date of study: December 2005 ‐ May 2008 Location: centres (n = 98) world‐wide |
|
| Participants |
Randomised: 754 participants (mean age 46 years, 473 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept, SC, 50 mg, twice a week, 12 weeks (n = 379) Control intervention B. Etanercept, SC, 50 mg, once a week, 12 weeks (n = 373) |
|
| Outcomes | Assessments at 12 weeks Primary and secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding, quote (p 8): "Wyeth Research, which was acquired by Pfizer in October 2009, sponsored this clinical trial and was responsible for the collection and analysis of data..." Declarations of interest (p 8): "WS has received fees for speaking/consulting from Abbott, Schering‐Plough, Wyeth, and Janssen‐Cilag. J‐PO has received fees for speaking/conferences/consulting from Schering‐Plough, Abbott, Merck‐Serono, Centocor, Wyeth, Janssen‐Cilag, MedPharma, Laboratorios Pierre‐Fabre, Galderma Laboratories, and Leo Pharma. BK has served on advisory boards for Schering‐Plough and Roche; has received funds for research/travel/conferences from Wyeth, Centocor, Abbott, Schering‐Plough, Roche, and Bristol‐Myers Squibb; and has served on a speaker panel for Bristol‐Myers Squibb. OB has received fees from Wyeth, Schering‐Plough, Abbott, Roche, Chugai, and Bristol‐Myers Squibb. DR, RDP, JE, CM, and BF are all employees of Pfizer." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 3): "We randomly assigned participants to ..." Comment: no description of the method used to generate random sequences |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 3): "We randomly assigned participants to ..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "In the double blind period..." Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "In the double blind period..." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 754 included/752 analysed Quote (p 4): "The modified intention‐to‐treat (ITT) population included all randomised participants who took at least one dose of the test drug and at least one post baseline efficacy evaluation... Efficacy analyses used the last observation carried forward method for imputation of missing data" Comment: mITT and only 2 of 754 participants not included in the analysis of the primary outcome |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00245960) The prespecified outcomes mentioned in the Methods section appeared to have been reported, except for the results of participant‐reported end points summarised in a separate publication |
PRIME 2017.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label study Date of study: June 2015 ‐ June 2016 Location: USA (multicentric) Phase 3 |
|
| Participants |
Randomised: 202 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Secu group (6), FAEs group (56)
|
|
| Interventions |
Intervention A. Secukinumab (300 mg at weeks 0, 1, 2, 3, 4, 8, 12, 16 and 20), n = 105 Control intervention B. Fumaderm® (week 0: 1 tablet of Fumaderm® INITIAL in the evening, n =97 Week 1: 1 tablet Fumaderm® INITIAL, in the morning and evening Week 2: 1 tablet Fumaderm® INITIAL in the morning, at noon and in the evening until the last tablet of a 40‐tablet‐blister is consumed Week 2‐3: At the day after the last tablet of the Fumaderm® INITIAL 40‐tablet‐blister is consumed and through week 3, 1 tablet of Fumaderm® in the evening Week 4: 1 tablet Fumaderm® in the morning and evening Week 5: 1 tablet Fumaderm® in the morning, at noon and in the evening Week 6: 1 tablet of Fumaderm® in the morning and at noon, 2 tablets of Fumaderm® in the evening Week 7: 2 tablets of Fumaderm® in the morning, 1 tablet of Fumaderm® at noon, 2 tablets of Fumaderm® in the evening Weeks 8‐24: 2 tablets of Fumaderm® in the morning, at noon and in the evening) |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 1024): "Novartis Pharma GmbH" Conflicts of interest Quote (Appendix): " M.S. is an advisor and/or paid speaker for and/or has participated in clinical trials sponsored by AbbVie, Actelion, Almirall, Biogen, Boehringer Ingelheim, Celgene, GlaxoSmithKline, Janssen Cilag, LEO Pharma, Eli Lilly, Merck Sharp & Dohme, Mibe, Mundipharma, Novartis, Pfizer, Regeneron and Sanofi. U.M. has been an advisor for and/or received speaker honoraria and/or grants from and/or participated in clinical trials sponsored by Abbott/AbbVie, Almirall Hermal, Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, Foamix, Forward Pharma, Janssen Cilag, LEO Pharma, Medac, MSD, Miltenyi Biotech, Novartis, Pfizer, VBL and Xenoport. M.A. has served as a consultant for, or has been a paid speaker for clinical trials sponsored by AbbVie, Almirall, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, GlaxoSmithKline, Janssen Cilag, LEO Pharma, Medac, Merck, MSD, Novartis, Pfizer, UCB and Xenoport. D.T. is an advisor or consultant for AbbVie, Amgen, Biogen Idec, Cel‐gene, Dignity, Eli Lilly, Galapagos, GlaxoSmithKline, Janssen, LEO Pharma, Maruho, Mitsubishi, Mundipharma, Novartis, Pfizer, Sandoz and Xenoport. He has participated in clinical trials sponsored by AbbVie, Almirall, Amgen, Astellas, Biogen Idec, Boehringer Ingelheim, Celgene, Dignity, Eli Lilly, Forward Pharma, GlaxoSmithKline, LEO Pharma, Janssen Cilag, Maruho, MSD, Mitsubishi Pharma, Novartis, Pfizer, Roche and Sandoz. He has received honoraria from AbbVie, Biogen Idec, Celgene, Janssen Cilag, LEO Pharma, Pfizer, Roche Possay, Novartis and Mundipharma. K.R. has served as an advisor and/or paid speaker for, and/or has participated in clinical trials sponsored by AbbVie, Amgen, Biogen, Boehringer Ingelheim Pharma, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen Cilag, LEO Pharma, Eli Lilly, Medac, Merck Sharp & Dohme, Novartis, Ocean Pharma, Pfizer, Regeneron, Takeda, UCB Pharma and Xenoport. N.M., C.S., C.H. and J.K. are employees of and/or own stock in Novartis" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1025): "This 24‐week, randomized, open‐label, active‐comparator, parallel‐group, superiority study was conducted... Eligible patients were randomized 1: 1 to receive subcutaneous injections of secukinumab 300 mg or oral FAEs per label, via an automated randomization list. Randomization numbers were assigned to patients by the investigators in consecutive order, who then assigned the treatment displayed on the card. Randomization lists and sealed envelopes were generated by personnel who were not otherwise involved in the trial." Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 1025): "This 24‐week, randomized, open‐label, active‐comparator, parallel‐group, superiority study was conducted... Eligible patients were randomized 1: 1 to receive subcutaneous injections of secukinumab 300 mg or oral FAEs per label, via an automated randomization list. Randomization numbers were assigned to patients by the investigators in consecutive order, who then assigned the treatment displayed on the card. Randomization lists and sealed envelopes were generated by personnel who were not otherwise involved in the trial." Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 1025): "This 24‐week, randomized, open‐label, active‐comparator, parallel‐group, superiority study was conducted... The blinded assessor and all involved personnel were instructed to desist from any discussions regarding safety, efficacy and treatment allocation of the study and patients in the presence of the blinded assessor. Efficacy parameters were assessed by blinded assessors who were not involved in any other study procedures and who did not have access to the allocation data or case report forms." Comment: Participants not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1025): "This 24‐week, randomized, open‐label, active‐comparator, parallel‐group, superiority study was conducted... The blinded assessor and all involved personnel were instructed to desist from any discussions regarding safety, efficacy and treatment allocation of the study and patients in the presence of the blinded assessor. Efficacy parameters were assessed by blinded assessors who were not involved in any other study procedures and who did not have access to the allocation data or case report forms." Comment: Probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dealing with missing data Quote (p 1026): "Efficacy end points were assessed for the full analysis set, consisting of all randomized patients who had received at least one dose of study drug. Between treatments, comparisons were made by logistic regression models adjusted for centre and baseline values of PASI scores. Odds ratios (ORs), 95% confidence intervals (CIs) and P‐values were derived from these models. Patients with missing assessments were considered responders if they had already met the response criterion at the time of dropout for the primary end point and all other end points where response was investigated. Otherwise they were considered nonresponders" Randomized 202, analyzed 201 Unbalance proportion regarding discontinuation: 5.7% for Secukinumab vs 57.7% for FAE |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02474082) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
PRISTINE 2013.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind Date of study: April 2008 ‐ March 2012 Location: 32 centres in Europe, Latin America and Asia |
|
| Participants |
Randomised: 273 participants (mean age 44 years, 190 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 137), SC, 50 mg, once a week, 24 weeks Control intervention B. Etanercept (n = 136), SC, 50 mg, twice a week, 24 weeks |
|
| Outcomes | Assessments at 24 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source, quote (p 177): "The PRISTINE trial was sponsored by Pfizer Inc..." Declarations of interest (pp 177‐8): "Robert Strohal has been a paid consultant of and has received research grants from Pfizer Inc, which provided funding for the PRISTINE study. He is also a member of the Pfizer European Expert Board and of the Pfizer Speakers Bureau. Luis Puig has been a paid consultant of and has received research grants from Pfizer; he has served on Pfizer advisory boards and the Speakers Bureau. Edgardo Chouela is a paid consultant and speaker for Pfizer Inc and Galderma and has conducted clinical studies for Novartis, Jannssen, Pfizer and Roche. Tsen‐Fang Tsai has been a paid consultant of Pfizer Inc; he has served as an investigator and received honoraria for serving as an advisor and speaker for Pfizer. Jeffrey Melin, Bruce Freundlich and Charles Molta were previous employees of Wyeth and Pfizer Inc. Joanne Fuiman, Ronald Pedersen and Deborah Robertson are current employees of Pfizer Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 170): "Subjects were randomly assigned to one of the 2 etanercept treatment groups... in 1:1 treatment allocation" Comment: not specified |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 170): "Subjects were randomly assigned to one of the 2 etanercept treatment groups... in 1:1 treatment allocation" Comment: not specified |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 170): "The study consisted of a 12‐week double‐blind treatment period" Comment: probably done, placebo‐controlled |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 170): "The study consisted of a 12‐week double‐blind treatment period" Comment: probably done, placebo‐controlled |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 273 enrolled and randomised, and 270 analysed Quote (p 171): "All efficacy analyses were performed using the modified intent‐to‐treat population which included all randomised subjects who received at least one dose of etanercept and had both baseline and on therapy PASI evaluations. The last observation‐carried‐forward method was used for the imputation of missing data..." Comment: mITT and only 3 of 273 participants not included in the analyses of the primary outcome |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00663052) The prespecified outcomes mentioned in the Methods section appeared to have been reported |
PsOsim 2017.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: May 2016 ‐ March 2017 Location: Multicentre (99 centres worldwilde) Phase 3 |
|
| Participants |
Randomised: 545 participants Key inclusion criteria
Key exclusion criteria
Baseline characteristics N = 545, 72% men Dropouts and withdrawals Total CHS‐1420: 54/274, Adalimumab: 19 /136 Reasons not reported |
|
| Interventions |
Intervention A. Adalimumab (Humira) 40 mg 2 doses at week 0/Day 0, then 1 dose every 2 weeks starting at Week 1 until week 15. At week 16 participants initially randomised to adalimumab will be reassigned (1:1) to CHS‐1420 or continue adalimumab treatment, 1 dose every 2 weeks for weeks 17 ‐ 23, n = 274. At week 24 participants will switch to CHS‐1420 open‐label until study end Control interventions B. CHS‐1420 (Biosimilar) 40 mg 2 doses at week 0/Day 0 then 1 dose every 2 weeks starting at week 1 for 23 weeks, n = 271. At week 24 participants will continue on to CHS‐1420 open label until study end |
|
| Outcomes |
Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (ClinicalTrials.gov) Coherus Biosciences, Inc. Conflict of interest: not stated. On ClinicalTrials.gov (NCT02489227), Waiting for the publication to contact the main author RoB completed according study protocol posted on ClinicalTrials.gov. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (protocol) : "Once the subject has signed the ICF at Screening, site personnel will assign a subject identification number (ID). The subject ID will include the site number (3 digits), and 3 digit subject number, assigned sequentially starting with 001 "Comment: Suggest centrally with the use of computer‐generated but unsure |
| Allocation concealment (selection bias) | Low risk | Quote (protocol) : "Once the subject ID has been assigned, the site will contact the Interactive Voice Response System/Interactive Web‐based Response System (IXRS) to register the subject ID" Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "This is a double‐blind study. The Humira and CHS‐1420 syringes will be matched in appearance. Blinded study drug will be shipped under appropriate storage conditions to site personnel according to the regulations of the study country" Comment: Probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "This is a double‐blind study. The Humira and CHS‐1420 syringes will be matched in appearance. Blinded study drug will be shipped under appropriate storage conditions to site personnel according to the regulations of the study country" Comment: Probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote: "Subjects who lack a PASI assessment at Week 12 will be considered non‐responders in the primary analyses. As a sensitivity analysis, the last available score will be used" Comment: reasons for withdrawal not reported |
| Selective reporting (reporting bias) | High risk | None of the secondary outcomes were reported, but results on ClinicalTrials.gov |
Reich 2012a.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: October 2005 ‐ November 2006 Location: 15 centres in France and Germany |
|
| Participants |
Randomised: 176 participants, mean age 43 years, 123 male Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Certolizumab (n = 59), SC, 200 mg, Certolizumab pegol (CZP) 400 mg week 0 – certolizumab 200 mg weeks 1‐10, 10 weeks Control intervention B. Certolizumab (n = 58), SC, 400 mg, certolizumab 400 mg week 0 – certolizumab 400 mg weeks 1 ‐ 10, 10 weeks C. Placebo (n = 59), SC, certolizumab 400 mg week 0 – placebo weeks 1 ‐ 10, 10 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source quote (p 180): "This study was funded by UCB Pharma, Brussels, Belgium" Declarations of interest (p 180): "K.R. has served as consultant and ⁄ or paid speaker for and ⁄ or has participated in clinical trials sponsored by companies that manufacture drugs used for the treatment of psoriasis, including Abbott, Biogen Idec, Celgene, Centocor, Janssen‐Cilag, Leo, Medac, Merck, MSD (formerly Essex, Schering‐Plough), Novartis and Pfizer (formerly Wyeth). J.‐P.O. is a consultant for Abbott, Centocor, Galderma, Janssen‐ Cilag, Leo, Meda Pharma, Merck Serono and UCB Pharma. A.B.G. has current consulting ⁄ advisory board agreements with Amgen, Astellas, Centocor (Janssen), Celgene, Bristol‐Myers Squibb, Beiersdorf, Abbott, TEVA, Actelion, UCB Pharma, Novo Nordisk, Novartis, Dermipsor, Incyte, Pfizer, Canfite, Merck and Lilly. Research ⁄ educational grants paid to Tufts Medical Center: Centocor (Janssen), Amgen, Immune Control, Abbott, Novo Nordisk, UCB Pharma, Novartis, Celgene and Pfizer. I.J.T. and G.C. are full‐time employees of UCB Pharma. C.T. is a former employee of UCB Pharma. P.M. has served as consultant and ⁄ or paid speaker for and has received grants, consulting and ⁄ or speaker fees from Abott Amgen, Biogen Idec, Bristol‐Myers Squibb, Celgene, Janssen, Novartis, Merck, Pfizer and UCB Pharma." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 181): "Eligible patients were randomised to receive... Randomization was centralized using a dynamic allocation procedure... Treatment was assigned using an interactive voice‐response system"“Randomization was conducted via Interactive Response Technology, which assigned a randomisation number that linked the subject treatment arm and specified unique medication pack number Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 181): "Eligible patients were randomised to receive... Randomization was centralized using a dynamic allocation procedure... Treatment was assigned using an interactive voice‐response system" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 181): "CZP... or matching placebo in liquid formulation for subcutaneous injection... Study doses of CZP or placebo were prepared containing the same volume and labelled in the same manner by designed unblinded pharmacists" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 181): "CZP... or matching placebo in liquid formulation for subcutaneous injection... Study doses of CZP or placebo were prepared containing the same volume and labelled in the same manner by designed unblinded pharmacists" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 176 included/176 analysed Quote (p 182): "Co‐primary efficacy assessments were performed on the intention‐to‐treat population... Nonresponder imputations for missing values were used for the primary analysis" Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00245765). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except for pharmacokinetic profile of CDP870 |
Reich 2015.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: December 2008 ‐ July 2009 Location: 14 centres in the USA and Canada |
|
| Participants |
Randomised: 100 participants (mean age 44 years, 100 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab (n = 30), SC, 3 mg/kg, 1 infusion (day 1) Control intervention B. Secukinumab (n = 29), SC, 10 mg/kg, 1 infusion (day 1) C. Secukinumab (n = 31), SC, 10 mg/kg, 3 infusions (says 1, 15, 29) D. Placebo (n = 10) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 534): "This trial and publication were found by Novartis Pharma AG, Basel, Switzerland." Declarations of interest (p 534): " KR has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, AbbVie, Amgen, Biogen‐Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, Leo, Lilly, Medac, MSD, Novartis, Pfizer, Takeda and Vertex. KAP has received grants and has consulted and served as an investigator for AbbVie, Amgen, Astellas, Biogen‐Idec, Celgene, Centocor, Eli Lilly, Forward Pharma, Fujisawa, GlaxoSmithKline, Janssen, Kyowa‐Kirin, Leo, MSD, Novartis (outside the submitted work), Pfizer and Takeda. RTM has received grants/clinical trial stipends from Novartis. JHT served as a clinical investigator for Novartis during conduct of this study. RB received grants from Novartis during the conduct of this study and has received grants, personal fees and non‐ financial support from AbbVie, Amgen, Astellas, Celgene, Eli Lilly, Janssen, Pfizer and Tribute. MB has served as a clinical trial sponsor for Amgen, Eli Lilly and Novartis. DG has served as a clinical trial investigator for Novartis. RAK is a member of an advisory board for Novartis and several other pharmaceutical companies. YP has received grants from AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Merck, Pfizer and Novartis (outside the submitted work). LAR, WMB, TMF and NAB‐S declare no conflict of interests. GS has received grants/clinical trial payments from Janssen, MSD and Novartis (unrelated to secukinumab). JMS, US, TP, EK, GAW, FK and CCB are full‐time employees of Novartis. WH and DML are full‐time employees of and own stock in Novartis. MMS was a full‐time employee of Novartis at the time the study was conducted and the manuscript" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (supplemental appendix): "The randomisation scheme was generated by Novartis Drug Supply Management using a validated system. The randomisation scheme was reviewed and approved by the Biostatistics Quality Assurance group of Novartis and was locked after approval. Subjects were assigned randomisation numbers, according to the randomisation schedule. Each site, upon evaluation of a qualified subject for the trial, faxed the enrolment sheet to the clinical trial leader (CTL) at the fax number provided. The CTL then assigned the randomisation number in a sequential manner and faxed it back to the unblinded pharmacist or qualified site personnel at the site, who then prepared and provided the study medication for the clinic in a blinded fashion." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (supplemental appendix): "Each site, upon evaluation of a qualified subject for the trial, faxed the enrolment sheet to the clinical trial leader (CTL) at the fax number provided. The CTL then assigned the randomisation number in a sequential manner and faxed it back to the unblinded pharmacist or qualified site personnel at the site, who then prepared and provided the study medication for the clinic in a blinded fashion... Treatment allocation and clinical assessment of the subjects were blinded. For preparation of the study medication from bulk supplies, treatment allocation cards were sent to the pharmacist or qualified site personnel at the investigator’s site." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (supporting information): "To maintain the blind of the study, the appearance of placebo infusion bags, ready to administer to the subject, was identical to that of active drug infusion bags. Placebo and active medication were prepared by an unblinded pharmacist or qualified site personnel assigned at each site." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (supporting information): "To maintain data integrity, no subject‐level data were circulated; therefore, blinding was maintained at the individual subject level" Comment probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 100 randomised participants, 94 analysed for PASI 75 or 90, 87 analysed for primary outcome (change in PASI) Quote (p 530): "Efficacy and pharmacodynamic parameters were evaluated in all subjects who received ≥ 1 dose of study medication and had a major protocol deviations... Subjects lost to follow‐up were considered relapsed on the day of th first visit without available PASI data" Comment: low rate of loss to follow‐up and reasons comparable between groups |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00805480) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Reich 2019.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: September 2016 ‐ June 2017 Location: 40 study sites (Canada, Germany, Japan, Poland and the USA, worldwide). Phase 2 |
|
| Participants |
Randomised: 205 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 205, mean age of 47 years and 74% men Dropouts and withdrawals
Mirikizumab 30 group (2), Mirikizumab 100 group (0), Mirikizumab 300 group (2), Placebo group (2)
|
|
| Interventions |
Intervention A. Mirikizumab, 30 mg SC at weeks 0 and 8, n = 51 Control interventions B. Mirikizumab, 100 mg SC at weeks 0 and 8, n = 51 C. Mirikizumab, 300mg SC at weeks 0 and 8, n = 51 D. Placebo SC at weeks 0 and 8, n = 52 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 88):"This study was funded in full by Eli Lilly and Company, Indianapolis, IN, U.S.A." Conflict of interest Quote (p 95):"K.R. has served as advisor and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO Pharma, Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, Takeda, UCB Pharma and Xenoport. P.R. has been a principal investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Merck, Novartis, Pfizer and Sandoz; a consultant for AbbVie, Novartis and Polichem; and an advisory board participant for AbbVie, Eli Lilly, Novartis and Sandoz. C.M. has been an advisory board member, investigator and/or speaker for: AbbVie, Amgen, Celgene, Eli Lilly and Company, served as a speaker, advisor, investigator and/or received grant/research support from AbbVie, Amgen, BMS, Boehringer Ingelheim, Celgene, Eli Lilly and Company, Galderma, GSK Steifel, Incyte, Janssen, Leo Pharma, Merck, Novartis, Pfizer and Kineta. C.L. is in the speakers bureau of AbbVie, Celgene and Leo Pharma; is a consultant for AbbVie, Amgen, Dermira, Eli Lilly and Company, Janssen, Leo Pharma, Pfizer, Sandoz and UCB Pharma; and has a conflict with AbbVie, Actavis, Amgen, Celgene, Cermira, Coherus, Eli Lilly and Company, Galderma, Janssen, Leo Pharma, Merck, Novartis, Pfizer, Sandoz, Stiefel and Wyeth. A.M. has served as a speaker, advisor, investigator and/or received honoraria and/or grant/research support from AbbVie, Allergan, Amgen, Boehringer Ingelheim, Celgene, Dermira, Eli Lilly and Company, Galderma, Janssen Biotech, LEO Pharma, Merck, Neothetics, Novartis, Pfizer, Regeneron and Syntrix. A.I. has received honoraria or fees for serving on advi‐ sory boards, as a speaker and as a consultant, and grants for being an investigator from AbbVie, Celgene, Eli Lilly, Janssen, Kyowa Hakko Kirin, Maruho and Novartis. P.K., D.P., J.L., J.T., M.M.‐C., E.E.‐H. and S.F. are current employees and shareholders of Eli Lilly and Company. K.P. has served as a speaker, advisor, investigator and/or received grant/research support from AbbVie, Akros, Allergan, Amgen, Anacor, Arcutis, Astellas, AstraZeneca, Baxalta, Baxter, Boehringer‐Ingelheim, Bristol‐ Myers Squibb, Can Fite, Celgene, Coherus, Dermira, Dow Pharma, Eli Lilly, Forward Pharma, Galderma, Genentech, GSK, Janssen, Kyowa Hakko Kirin, Leo, Medimmune, Meiji Seika Pharma, Merch (MSD), Merck‐Serono, Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Roche, Sanofi‐Aventis/Genzyme, Takeda, UCB and Valeant." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 89): "Assignment to study drug groups was determined by a computer‐generated random sequence using an interactive web‐response system. To maintain blinding, the investigational product was prepared at the site by unblinded pharmacists or other trained personnel, and administered at the site by blinded nurses or other trained personnel." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 89): "Assignment to study drug groups was determined by a computer‐generated random sequence using an interactive web‐response system. To maintain blinding, the investigational product was prepared at the site by unblinded pharmacists or other trained personnel, and administered at the site by blinded nurses or other trained personnel." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 89): "Assignment to study drug groups was determined by a computer‐generated random sequence using an interactive web‐response system. To maintain blinding, the investigational product was prepared at the site by unblinded pharmacists or other trained personnel, and administered at the site by blinded nurses or other trained personnel." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 89): "Assignment to study drug groups was determined by a computer‐generated random sequence using an interactive web‐response system. To maintain blinding, the investigational product was prepared at the site by unblinded pharmacists or other trained personnel, and administered at the site by blinded nurses or other trained personnel." Comment: no destriction of who assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Abstract:"Missing data were imputed as nonresponses." Quote (p 90):"All randomized patients were analysed according to the dose group to which they were assigned (intent to treat). Safety analyses were performed for all patients who received at least one dose of the study drug." Randomly assigned 205, analysed 205 Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02899988) The pre‐specified outcomes and those mentioned in the methods section appeared to have been reported. |
Reich 2020.
| Study characteristics | ||
| Methods | RCT, active‐controlled, single‐blind study Date of study: December 2015 ‐ November 2017 Location: Germany (multicentric) Phase 3 |
|
| Participants |
Randomised: 162 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Ixe group (4), FAEs group (31), Methotrexate group (5)
|
|
| Interventions |
Intervention Ixekizumab (60 mg ixekizumab given as 2 SC injections followed by 80 mg ixekizumab given SC every 2 weeks until week 12 and then 80 mg ixekizumab given SC every 4 weeks until week 24), n = 54 Control interventions FAEs (105 mg FAE given orally followed by 215 mg FAE given orally 1 ‐ 3 times/day until week 24), n = 54 Methotrexate (7.5 mg starting dose up to 30 mg methotrexate given orally once a week until week 24), n = 54 |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcome
|
|
| Notes | Funding Quote (ClinicalTrials.gov): "Sponsor: Eli Lilly and Company" Conflict of interest Not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (ClinicalTrials.gov): "Allocation: randomized" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (ClinicalTrials.gov): "Masking: Single (Outcomes Assessor)" Comment: no double‐blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov): "Masking: Single (Outcomes Assessor)" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dealing with missing data: not stated Results posted on clinical.Trials: ITT analyses Unbalance discontinuation treatments: Ixe group (4), FAEs group (31), Methotrexate group (5) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02634801) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
ReSURFACE‐1 2017.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: 10 December 2012 ‐ 28 October 2015 Location: at 118 sites (including hospital dermatology units, specialty clinics, private practices, and research sites) in Australia, Canada, Japan, the UK, and the USA Phase 3 |
|
| Participants |
Randomised: 772 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Tildra 200 (10), Tildra 100 (9), PBO (9)
|
|
| Interventions |
Intervention A. Tildrakizumab 200 mg (SC on weeks 0, 4, 16, 28, 40 and 52), n = 308 Control interventions B. Tildrakizumab 100 mg (SC on weeks 0, 4, 16, 28, 40 and 52), n = 309 C. Placebo, n = 155 |
|
| Outcomes |
At week 12 Primary outcome (composite outcome)
Secondary outcomes
|
|
| Notes | Funding Quote (p 276): "Funding Merck & Co" Conflicts of interest Quote (p 287): "Declaration of interests: KR has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, Abbvie, Amgen, Biogen‐Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, Leo, Lilly, Medac, Merck & Co, Novartis, Pfizer, Vertex, and Takeda. KAP has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, Amgen, Anacor, AbbVie, Active Biotech, Allergan, Astellas, AstraZeneca, Basilea, Bayer, Biogen‐Idec, BMS, Boehringer‐Ingelheim, CanFite, Celgene, Dermira, Eli‐Lilly, Forward Pharma, Genentech, GlaxoSmithKline, Janssen, Kyowa Hako Kirin, Kythera, Leo Pharma, Merck & Co, Merck‐Serono, Novartis, Pfizer, Regeneron, Rigel, Roche, Sanofi‐Genzyme, Takeda, UCB, Valeant, Xenon, and Xoma. AB has served as a scientific adviser and clinical study investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Dermira, Genentech, GSK, Janssen, Lilly, Merck & Co, Novartis, Pfizer, Regeneron, Sandoz, Sanofi Genzyme, Sun, UCB, and Valeant, and as a paid speaker for Lilly. SKT has participated in trials supported by grants from Merck & Co. RS has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, Leo Pharma, Amgen, Novartix, Merck & Co, Celgene, Coherus Biosciences, Janssen, Regeneron, MedImmune, GlaxoSmithKline, Cutanea, Samson Clinical, Boehringer Ingelheim, Pfiizer, MSD, Oncobiologics, Roche, Eli Lilly, and Bayer. DT has served as a consultant, advisory board member, or an investigator for Abbott (AbbVie), Almiral, Amgen, Astellas, Biogen‐Idec, Boehringer Ingelheim, Celgene, Dignity, Forward‐Pharma, Galderma, GlaxoSmithKline, Isotechnika, Janssen‐Cilag, Leo Pharma, Lilly, Maruho, Medac, Medimmune, Merck & Co, Merck‐Serono, Novartis, Pfizer, Regeneron, Sandoz, Sanofi‐Aventis, and Takeda. KN is a former employee of Merck & Co; AM, NC, QL, KL, CLR, and SG are current Merck & Coemployees. ABK is a consultant and investigator for Merck & Co, Amgen, AbbVie, Janssen, Novartis, Dermira, and Pfizer, a consultant for Sun Pharmaceuticals, Bristol‐Myers Squibb, Lilly, and VBL, and has received fellowship funding from Janssen." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 278): "In reSURFACE 1, participants were randomly assigned (2:2:1) to tildrakizumab 200 mg, tildrakizumab 100 mg, or placebo...In reSURFACE 2, participants were randomly assigned (2:2:1:2) to tildrakizumab 200 mg, tildrakizumab 100 mg, placebo, or etanercept 50 mg...Parexel International,
the contract research organisation, generated computer generated randomisation sequences, and an interactive voice‐response system and interactive web‐response system was used by Parexel to allocate participants to groups. Randomised treatment assignments on day 1 were done by region" Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 278): "In reSURFACE 1, participants were randomly assigned (2:2:1) to tildrakizumab 200 mg, tildrakizumab 100 mg, or placebo...In reSURFACE 2, participants were randomly assigned (2:2:1:2) to tildrakizumab 200 mg, tildrakizumab 100 mg, placebo, or etanercept 50 mg...Parexel International,
the contract research organisation, generated computer generated randomisation sequences, and an interactive voice‐response system and interactive web‐response system was used by Parexel to allocate participants to groups. Randomised treatment assignments on day 1 were done by region" Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 279): "Investigators, participants, and study personnel were blinded to group allocation and remained blinded until completion of the studies. A double‐masking technique
was used, in which tildrakizumab and its matching placebo or etanercept and its matching placebo were identical in appearance and packaging. Additional placebo doses were administered to maintain masking. The team doing the analysis was blinded until the database was locked." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 279): "Investigators, participants, and study personnel were blinded to group allocation and remained blinded until completion of the studies. A double‐masking technique
was used, in which tildrakizumab and its matching placebo or etanercept and its matching placebo were identical in appearance and packaging. Additional placebo doses were administered to maintain masking. The team doing the analysis was blinded until the database was locked." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (pp 280‐1): "We specified full‐analysis‐set, intention‐to‐treat, and per protocol patient populations in the study protocols...Patients with missing data were treated as non‐responders (non‐responder imputation [NRI])." Randomised 772, Analysed 772 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01722331) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
ReSURFACE‐2 2017.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: 12 February 2013 ‐ 28 September 2015 Location: 132 sites in Austria, Belgium, Canada, Czech Republic, Denmark, France, Germany, Hungary, Italy, Israel, Netherlands, Poland, and the USA Phase 3 |
|
| Participants |
Randomised: 1090 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Tildra 200 (14), Tildra 100 (12), ETA (24), PBO (14)
|
|
| Interventions |
Intervention Tildrakizumab 200 mg (SC on weeks 0, 4, 16, 28, 40 and 52), n = 314 Control interventions Tildrakizumab 100 mg (SC on weeks 0, 4, 16, 28, 40 and 52), n = 307 Etanercept 50 mg (twice weekly until week 12 and once weekly from week 12 to week 28), n = 313 Placebo, n = 156 |
|
| Outcomes |
At week 12 Primary outcome (composite outcome)
Secondary outcomes
|
|
| Notes | Funding Quote (p 276): "Funding Merck & Co" Conflicts of interest Quote (p 287): "Declaration of interests: KR has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, Abbvie, Amgen, Biogen‐Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, Leo, Lilly, Medac, Merck & Co, Novartis, Pfizer, Vertex, and Takeda. KAP has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, Amgen, Anacor, AbbVie, Active Biotech, Allergan, Astellas, AstraZeneca, Basilea, Bayer, Biogen‐Idec, BMS, Boehringer‐Ingelheim, CanFite, Celgene, Dermira, Eli‐Lilly, Forward Pharma, Genentech, GlaxoSmithKline, Janssen, Kyowa Hako Kirin, Kythera, Leo Pharma, Merck & Co, Merck‐Serono, Novartis, Pfizer, Regeneron, Rigel, Roche, Sanofi‐Genzyme, Takeda, UCB, Valeant, Xenon, and Xoma. AB has served as a scientific adviser and clinical study investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Dermira, Genentech, GSK, Janssen, Lilly, Merck & Co, Novartis, Pfizer, Regeneron, Sandoz, Sanofi Genzyme, Sun, UCB, and Valeant, and as a paid speaker for Lilly. SKT has participated in trials supported by grants from Merck & Co. RS has served as a consultant or paid speaker for, or participated in clinical trials sponsored by, Leo Pharma, Amgen, Novartix, Merck & Co, Celgene, Coherus Biosciences, Janssen, Regeneron, MedImmune, GlaxoSmithKline, Cutanea, Samson Clinical, Boehringer Ingelheim, Pfiizer, MSD, Oncobiologics, Roche, Eli Lilly, and Bayer. DT has served as a consultant, advisory board member, or an investigator for Abbott (AbbVie), Almiral, Amgen, Astellas, Biogen‐Idec, Boehringer Ingelheim, Celgene, Dignity, Forward‐Pharma, Galderma, GlaxoSmithKline, Isotechnika, Janssen‐Cilag, Leo Pharma, Lilly, Maruho, Medac, Medimmune, Merck & Co, Merck‐Serono, Novartis, Pfizer, Regeneron, Sandoz, Sanofi‐Aventis, and Takeda. KN is a former employee of Merck & Co; AM, NC, QL, KL, CLR, and SG are current Merck & Coemployees. ABK is a consultant and investigator for Merck & Co, Amgen, AbbVie, Janssen, Novartis, Dermira, and Pfizer, a consultant for Sun Pharmaceuticals, Bristol‐Myers Squibb, Lilly, and VBL, and has received fellowship funding from Janssen." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 278): "In reSURFACE 1, participants were randomly assigned (2:2:1) to tildrakizumab 200 mg, tildrakizumab 100 mg, or placebo...In reSURFACE 2, participants were randomly assigned (2:2:1:2) to tildrakizumab 200 mg, tildrakizumab 100 mg, placebo, or etanercept 50 mg...Parexel International, the contract research organisation, generated computergenerated randomisation sequences, and an interactive voice‐response system and interactive web‐response system was used by Parexel to allocate participants to groups. Randomised treatment assignments on day 1 were done by region" Comment: Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 278): "In reSURFACE 1, participants were randomly assigned (2:2:1) to tildrakizumab 200 mg, tildrakizumab 100 mg, or placebo...In reSURFACE 2, participants were randomly assigned (2:2:1:2) to tildrakizumab 200 mg, tildrakizumab 100 mg, placebo, or etanercept 50 mg...Parexel International, the contract research organisation, generated computergenerated randomisation sequences, and an interactive voice‐response system and interactive web‐response system was used by Parexel to allocate participants to groups. Randomised treatment assignments on day 1 were done by region" Comment: Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 279): "Investigators, participants, and study personnel were blinded to group allocation and remained blinded until completion of the studies. A double‐masking technique was used, in which tildrakizumab and its matching placebo or etanercept and its matching placebo were identical in appearance and packaging. Additional placebo doses were administered to maintain masking. The team doing the analysis was blinded until the database was locked." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p279): "Investigators, participants, and study personnel were blinded to group allocation and remained blinded until completion of the studies. A double‐masking technique was used, in which tildrakizumab and its matching placebo or etanercept and its matching placebo were identical in appearance and packaging. Additional placebo doses were administered to maintain masking. The team doing the analysis was blinded until the database was locked." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (pp 280‐1): "We specified full‐analysis‐set, intention‐to‐treat, and per protocol patient populations in the study protocols...Patients with missing data were treated as non‐responders (non‐responder imputation [NRI])." Randomised 1090, Analysed 1090 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01729754) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
REVEAL 2008.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: December 2004 ‐ August 2007 Setting: 81 centres (67+14) in USA, Canada |
|
| Participants |
Randomised: 1212 participants (mean age 44 years, 803 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Adalimumab (n = 814), SC, 40 mg, week 0: 2 injections, week 1: eow, 16 weeks Control intervention B. Placebo, SC (n = 398), week 0: 2 injections/week 1: eow, 16 weeks |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source quote (p 106): "Supported by Abbott Laboratories" Declarations of interest (p 106): "Dr Menter has received research support and/or lecture honoraria from Abbott, Amgen, Astellas, Biogen, Centocor, Genentech, and Wyeth. Dr Tyring has received research support from, has consulted for, and is part of the speakers’ bureaus for Abbott. Dr Gordon has received research support and honoraria from Abbott, Amgen, and Centocor. Dr Kimball is an investigator, speaker, and consultant for Abbott, Amgen, Biogen, Centocor, and Genentech. Dr Leonardi is a consultant for Abbott, Amgen, Centocor, and Genentech and is an investigator for Abbott, Allergan, Altana, Amgen, Astellas, Biogen, Bristol Myers, Centocor, Fujisawa, Galderma, Genentech, Serono, CombinatoRx, 3M Pharmaceuticals, Schering Plough, RTL, and Vitae; he also received an educational grant from Amgen and Genentech, and is part of the speakers’ bureaus for Abbott, Amgen, Centocor, Genentech, and Warner Chilcott. Dr Langley is a scientific advisory board member, investigator, and speaker for Abbott, Amgen, Astellas, Centocor, Norvartis, and Wyeth. Dr Strober serves on the advisory boards of, has received honoraria from, and is an investigator for Abbott, Amgen, Astellas, Centocor, Genentech, and Wyeth, and is part of the speakers’ bureaus for Abbott, Amgen, Astellas, Genentech, and Wyeth. Dr Kaul, Ms Gu, and Dr Okun are employees of Abbott Laboratories. Dr Papp is a consultant for and has received honoraria and travel grants from Abbott, Alza, Amgen, Astellas, Celgene, Centocor, Genentech, Isotechnika, Johnson and Johnson, Serono, Schering‐Plough, and UCB." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 107): ”Randomization schedules were generated by one of our data management departments before study inception” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 107): ”Patients were randomised by centre via an interactive voice response system". "ADA and placebo‐filled syringes were identically labelled and packaged, and self‐administrated by patients" Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 107): "Double‐blind, placebo‐controlled... ADA and placebo‐filled syringes were identically labelled and packaged, and self‐administrated by patients" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 107): "Double‐blind, placebo‐controlled... ADA and placebo‐filled syringes were identically labelled and packaged, and self‐administrated by patients" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 1212 included/1212 analysed Quote (p 109): "The primary efficacy analyses were conducted on ITT population... a patient with missing data for a visit... had the last observation carried forward" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT002377887) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported, except for participant‐reported outcome |
Rich 2013.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: July 2009 ‐ December 2010 Location: 60 centres in Portland, USA |
|
| Participants |
Randomised: 404 participants Secukinimab A (66) (mean age 43 years, 53 male) Secukinimab B (138) (mean age 44 years, 104 male) Secukinimab C (133) (mean age 45 years, 105 male) Placebo (67) (mean age 44 years, 44 male) Inclusion criteria
Exclusion criteria
|
|
| Interventions |
Intervention A. Secukinumab (n = 66), SC, 150 mg, week 0, 12 weeks Control intervention B. Secukinumab (n = 138), SC, 150 mg, weeks 0, 4, 8, 12 weeks C. Secukinumab (n = 133), SC, 150 mg, weeks 0, 1, 2, 4, 12 weeks D. Placebo (n = 67), SC, weeks 0, 1, 2, 4, 8, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding support quote (p 402): "Novartis Pharma AG, Basel, Switzerland" Declarations of interest (appendix): "P.R. has received honoraria for lecturing in industry‐sponsored meetings and has received research grants from pharmaceutical companies as an investigator. B.S. has consulted for Novartis and several other pharmaceutical companies; he has served on an advisory board for Novartis and several other pharmaceutical companies. D.T. has served as a speaker and served on advisory boards for Abbott, Biogen‐Idec, Janssen‐Cilag, Leo, MSD, Novartis and Pfizer. C. Paul has received honoraria from and has been a paid consultant to Abbott, Amgen, Celgene, Janssen‐Cilag, Novartis and Pierre Fabre. K.R., E.H., A.G., M.M. and C. Papavassilis are full‐time employees of, and own stock in Novartis. J.‐P.O., A.M. and R.E.S. declare no conflicts of interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 404): “Randomization numbers were generated by the interactive response technology provider using a validated system that automated the random assignment of patients numbers to randomisation numbers” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 404): “Randomization numbers were generated by the interactive response technology provider using a validated system that automated the random assignment of patients numbers to randomisation numbers” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 404): “Patients, investigator staff, persons performing the assessments and data analysts were blinded to the identity of treatment from the time of randomisation until primary outcome analysis” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 404): “Patients, investigator staff, persons performing the assessment and data analysts were blinded to the identity of treatment from the time of randomisation until primary outcome analysis” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 404 included/404 analysed Quote (p 405): "Following th intent‐to‐treat principle, data were analysed... Missing values were replaced using the last‐observation‐carried‐forward approach" Comment: ITT analyses |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00941031) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Ruzicka 1990.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: December 1986 ‐ March 1988 Location: 7 centres in Germany |
|
| Participants |
Randomised: 82 participants (mean age 44 years, 55 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin, orally, 35 mg, daily, 8 weeks (n = 42) Control intervention B. Placebo, orally, daily, 8 weeks (n = 40) |
|
| Outcomes | Assessments at 8 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding sources: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 483): "The study was designed as a randomized, double‐blind, placebo‐controlled parallel group trial" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 483): "The study was designed as a randomized, double‐blind, placebo‐controlled parallel group trial" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 483): "The study was designed as a randomized, double‐blind, placebo‐controlled parallel group trial" Comment: no description of the method used to guarantee blinding as visible side effects are related to acitretin |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 483): "The study was designed as a randomized, double‐blind, placebo‐controlled parallel group trial... the investigators blinded to treatment assignment" Comment: no description of the method used to guarantee blinding of outcome assessment as visible side effects are related to acitretin |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 82 included/78 analysed Quote (p 483): "... according to the intention‐to‐treat principle.. Dropout data were evaluated on the date of dropout" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Sandhu 2003.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label Date of study: not stated Location: multicentric (number not stated) in North India |
|
| Participants |
Randomised: 30 participants (methotrexate: mean age 39 years, 12 male; ciclosporin: mean age 46 years, 13 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Methotrexate (n = 15), orally, 0.5 mg/kg dose tapered after PASI 75 obtained Control intervention B. Ciclosporin (n = 15), orally, 3 mg/kg increased to 4 if no change or rise of dose tapered after PASI 75 obtained |
|
| Outcomes | Assessments at 12 weeks Primary or secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding source: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 459): "Patients were randomly assigned to either..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 459): "Patients were randomly assigned to either..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not blind |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: not blind |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 30 included/30 analysed Methods for dealing with missing data: not stated |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported.No primary outcome declared |
Saurat 1988.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: not stated Location: 6 centres in France and Switzerland |
|
| Participants |
Randomised: 42 participants (placebo (22) mean age 43 years, 16 male; acitretin (20), mean age 46 years, 16 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 20), orally, 2 x 25/d 2 weeks and 25/d + UVA 3/weeks, daily, 10 weeks Control intervention C. Placebo, orally (n = 22), daily, 10 weeks Co‐intervention: UVA 3/week, 10 weeks |
|
| Outcomes | Assessments not clearly stated (reported at 8 weeks) Primary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 219): "This multicenter study was performed in a double‐blind, parallel fashion... The patients were randomly allocated to ..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 219): "This multicenter study was performed in a double‐blind, parallel fashion... The patients were randomly allocated to ..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p 219): "This multicenter study was performed in a double‐blind, parallel fashion...All patients initially received 2 capsules of test medication (placebo, acitretin 2x25 mg, ...." Comment: no description of the method used to guarantee blinding of outcome assessment with visible AEs in both acitretin and etretinate groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: no description of the method used to guarantee blinding of outcome assessment with visible AEs in both acitretin and etretinate groups |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Quote (p 220): "Patients who left the study ... were not included in the evaluation of efficacy" Comment: not ITT analyses (number lost to follow‐up unknown) |
| Selective reporting (reporting bias) | Low risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
SCULPTURE 2015.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind Date of study: August 2011 – March 2013 Setting: 133 centres in North and South America, Europe and Asia |
|
| Participants |
Randomised: 966 participants (mean age 46 years, 635 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Secukinumab (n = 482), SC, 150 mg weeks 0, 1, 2, 3 then monthly Control intervention B. Secukinumab (n = 484), SC, 300 mg weeks 0, 1, 2, 3 then monthly |
|
| Outcomes | Assessments at 52 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 27) “Study funded by Novartis Pharma...Novartis conducted data analyses, and all authors had access to data”. Declarations of interest (p 27): "The authors received writing and editorial support from Barry Weichman and Jinling Wu in the preparation of the manuscript from BioScience Communications, New York, NY, supported by Novartis. Dr Mrowietz has served as advisor and/or received speaker honoraria and/or received grants and/or participated in clinical trials for Abbott/AbbVie, Almirall, Amgen, BASF, Biogen Idec, Celgene, Centocor, Eli Lilly, Forward Pharma, Galderma, Janssen, Leo Pharma, Medac, MSD, Miltenyi Biotech, Novartis, Pfizer, Teva, VBL, and Xenoport. Dr Leonardi has served as consultant and/or investigator and/or participated in a speaker’s bureau for AbbVie, Amgen, Celgene, Dermira, Eli Lilly, Galderma, Janssen, Leo Pharma, Merck, Novartis, Pfizer, Sandoz, Stiefel, and UCB. Dr Girolomoni has received advisory/speaker honoraria and/or research funding from AbbVie, Almirall, Boehringer Ingelheim, Celgene, Dompe, Eli Lilly, Galderma, Janssen, Leo Pharma, Merck Serono, Maruho, MSD, Novartis, and Pfizer. Dr Toth has served as investigator for Novartis, Amgen, Eli Lilly, Johnson & Johnson, Abbott, Celgene, Merck, Galderma, and Leo Pharma. Dr Morita has served as consultant and/or paid speaker for and/or participated in psoriasis clinical trials sponsored by AbbVie, Mitsubishi Tanabe, Janssen, Novartis, Eli Lilly, Kyowa‐Kirin, Leo Pharma, Maruho, and MSD. Dr Szepietowski has served as advisor and/or received speakers honoraria and/or participated in clinical trials for Abbott/AbbVie, Actavis, Amgen, BASF, Astellas, Berlin‐Chemie/Menarini, Biogenetica International Laboratories, Centocor, Fresenius, Janssen, Leo Pharma, Mitsubishi Tanabe, Novartis, Pierre‐Fabre, Takeda, Toray Corporation, and Vichy. Dr Regnault, Ms Thurston, and Dr Papavassilis are employees of and/or own stock in Novartis. Dr Balki has no conflicts of interest to declare." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 28): “were randomised” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 28): “administered via 2 150‐mg SC injections or one 150‐mg SC and one placebo SC injection respectively” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 28): "administered via 2 150‐mg SC injections or one 150‐mg SC and one placebo SC injection respectively" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 966, analysed 966 Management of missing data: Quote (p 29): “Missing values for PASI or IGA 2011 modified version responses were imputed as non response regardless of the reason for missing data” Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01406938). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Shehzad 2004.
| Study characteristics | ||
| Methods | RCT, active‐controlled, open‐label Date of study: March 2001 ‐ November 2001 Location: 1 centre in Karachi, Pakistan |
|
| Participants |
Randomised: 40 participants (age from 18‐50 years, % male unknown) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. PUVA therapy (+ psoralen) (n = 20), 4 times/week Control intervention B. Methothrexate (n = 20), orally, 10 mg/week, 5 mg Saturday + Sunday |
|
| Outcomes | Time of assessments: not stated Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Immunex Corporation Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (in the Method section): “The selected patients ... randomly allocated to...” Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (in the Method section): “The selected patients ... randomly allocated to...” Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Comment: not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: no description of the methods used to manage missing data, no description of the methods used to assess the primary outcome (ITT, PP...) |
| Selective reporting (reporting bias) | High risk | Comment: no protocol was available. The outcomes mentioned in the Results section were not specified in the Methods section |
SIGNATURE 2019.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind trial (SIGNATURE) Date of study: October 2013‐July 2016 Location: UK‐Ireland |
|
| Participants |
Randomised: 235 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Secu 150 group (13), Secu 300 group (12)
|
|
| Interventions |
Intervention A. Biological: secukinumab 150 mg at day 0 (initiation of study drug) and at weeks 1, 2, 3 and 4, n = 116 Control Intervention B. Biological: secukinumab 300 mg at day 0 (initiation of study drug) and at weeks 1, 2, 3 & 4, n = 119 |
|
| Outcomes |
At 16 weeks Primary outcome
Secondary outcomes
|
|
| Notes | Funding: Quote (Clinical.Trials.gov): Novartis Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (Clinical.Trials.gov): "Allocation: randomized" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (Clinical.Trials.gov): "Masking: None (Open Label)" Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (Clinical.Trials.gov): "Masking: None (Open Label)" Comment: not blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: not stated but reasonable rate of withdrawal (10%) and number and reason comparable between groups Results posted on ClinicalTrials.gov: ITT analyses |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01961609) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Sommerburg 1993.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: 1986 ‐ 1988 Location: 7 centres in Germany |
|
| Participants |
Randomised: 88 participants (mean age 45 years, 68 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 44), orally, 50 mg (15 days) then 25 mg, daily, 8 weeks Control intervention B. Placebo (n = 44), orally, daily, 8 weeks Co‐intervention PUVA (8‐methoxypsoralen), orally 0.6 mg/kg, 3 ‐ 5/week, 8 weeks |
|
| Outcomes | Assessments at 8 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 310): "The study was designed as a randomised, double‐blind, parallel groups trial... Both investigators and biostatisticians were blinded" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 310): "The study was designed as a randomised, double‐blind, parallel groups trial... Both investigators and biostatisticians were blinded" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote (pp 310‐1): "The study was designed as a randomised, double‐blind, parallel group trial... Both investigators and biostatisticians were blinded… however due to well know side effect pattern of acitretin, ..., the possibility of an investigator bias cannot be excluded" Comment: visible AEs in acitretin groups |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (pp 310‐1): " The study was designed as a randomised, double‐blind, parallel group trial... Both investigators and biostatisticians were blinded… however due to well know side effect pattern of acitretin, ..., the possibility of an investigator bias cannot be excluded" Comment: visible AEs in acitretin groups |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 88 included/83 analysed Quote (p 311): "Patients who discontinued the trial prematurely were evaluated on the date of discontinuation of therapy" Comment: not ITT, low number of dropouts |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Strober 2011.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: July 2008 ‐ April 2009 Location: 41 centres in the USA |
|
| Participants |
Randomised: 211 participants (mean age 45 years, 131 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 139), SC auto‐administered, 50 mg twice a week, 11 weeks Control intervention B. Placebo (n = 72), SC auto‐administered, twice a week |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial At 4, 8, 12 weeks
|
|
| Notes | Funding source, quote (Appendix 1): "Abbott Laboratories funded this study and participated in the study design, data collection, data management, data analysis and preparation of the manuscript. All of the authors had full access to the data and were involved in the analysis of data, development and revision of the manuscript, and decision to submit the manuscript for publication. The corresponding author takes responsibility for the integrity of the data and the accuracy of the data analysis." Declarations of interest (appendix 1): "B.E.S. has been an investigator, consultant, speaker, and served on an advisory board for Amgen, Abbott and Centocor; and has also been a speaker for Astellas. J.J.C. has received research support from Abbott, Amgen, Centocor, Celgene and Eli Lilly; has been a consultant for Abbott, Amgen and Centocor; and has been a speaker for Abbott. P.S.Y. has served as a consultant, principle investigator, speaker or advisory board member for Abbott, Amgen, Astellas and Centocor. M.O. and D.A.W. are employees of Abbott." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 662): "Patients were randomised..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 662): "Patients were randomised" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 662): “Patients enrolled in the placebo arm received SC injections matching active treatment to maintain the blind. To maintain the blind, all patients received two SC injections at weeks 0 and 4 and one SC injection at week 8, consisting of either briakinumab or matching placebo, depending on the treatment arm. In addition, each patient also received two SC injections biweekly, 3 days apart, week 0 through week 11, consisting of either etanercept or matching placebo, depending on the treatment arm.” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 662): “Patients enrolled in the placebo arm received SC injections matching active treatment to maintain the blind. To maintain the blind, all patients received two SC injections at weeks 0 and 4 and one SC injection at week 8, consisting of either briakinumab or matching placebo, depending on the treatment arm. In addition, each patient also received two SC injections biweekly, 3 days apart, week 0 through week 11, consisting of either etanercept or matching placebo, depending on the treatment arm.” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 211, analysed 211 Management of missing data: Quote (p 663): “The primary efficacy analysis consisted of four comparisons performed in the intent‐to‐treat population (i.e. all randomised patients), …, Nonresponder imputation was used to handle missing data.” Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00710580) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
STYLE 2020.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: May 2017 ‐ January 2019 Location: 13 sites in Canada and 28 sites the USA Phase 3 |
|
| Participants |
Randomised: 303 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 303, mean age of 46.9 years and 62% men Dropouts and withdrawals
Apremilast group (33), Placebo group (18)
|
|
| Interventions |
Intervention A. Apremilast 30 mg tablets orally twice a day for 16 weeks Control intervention B. Placebo tablets twice a day for 16 weeks |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 2): "The authors acknowledge financial support for this study from Celgene Corporation. The authors received editorial support in the preparation of this report from Amy Shaberman, PhD, of Peloton Advantage, LLC, an OPEN Health company, Parsippany, NJ, USA, sponsored by Celgene Corporation, Summit, NJ, USA. The authors, however, directed and are fully responsible for all content and editorial decisions for this report." Conflict of interests Quote (p 3‐4):"ASVV: AbbVie, Allergan, Celgene Corporation, Derm Tech, Dermira, Novartis, and Valeant – honoraria for advisory board and/or consulting; Merck – pension (ex‐spouse). LSG: Celgene Corporation, LEO Pharma, Novartis, Pfizer, and Stiefel/GlaxoSmithKline – investigator and/or consultant. ML: Mount Sinai (which receives funds from Boehringer Ingelheim, Celgene Corporation, Eli Lilly, Janssen/Johnson & Johnson, Kadmon, MedImmune/AstraZeneca, Novartis, Pfizer, and ViDac). BS: AbbVie, Almirall, Amgen, Arena, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene Corporation, Dermavant, Dermira, Eli Lilly, GlaxoSmithKline, Janssen, Kyowa Hakko Kirin, LEO Pharma, Medac, Meiji Seika Pharma, Menlo Therapeutics, Novartis, Ortho Dermatologics/Valeant, Pfizer, Regeneron, Sanofi‐Genzyme, Sebela Pharmaceuticals, Sun Pharma, and UCB Pharma – honoraria as a consultant and advisory board member; AbbVie, Boehringer Ingelheim, Celgene Corporation, Eli Lilly, Galderma, GlaxoSmithKline, Janssen, Merck, Pfizer, and Sienna – payments (to the University of Connecticut) as an investigator; Corrona Psoriasis Registry – fees as a scientific director; AbbVie and Janssen – grant support (to the University of Connecticut for Fellowship Program). CL: AbbVie, Boehringer Ingelheim, Celgene Corporation, Eli Lilly, Janssen, Merck, Novartis, Pfizer, Sun Pharma, and Valeant – principal investigator/consultant. ST: No conflicts or potential conflicts of interest to disclose. AC: AbbVie, Amgen, AstraZeneca, Boehringer Ingelheim, Celgene Corporation, Dermira, Eli Lilly, Janssen, Maruho, Novartis, Pfizer, Stiefel/ GlaxoSmithKline, Sun Pharma, and UCB – investigator; Celgene Corporation – consultant. HS: Celgene Corporation, Janssen, Lilly, and Novartis – grants received as an investigator. ZZ, MP, & YW: Celgene Corporation – employment." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 9): "For the placebo‐controlled phase, study personnel randomized patients (2:1), using a permuted block randomization and centralized interactive response technology, to receive apremilast 30 mg BID or placebo for 16 weeks." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 9): "For the placebo‐controlled phase, study personnel randomized patients (2:1), using a permuted block randomization and centralized interactive response technology, to receive apremilast 30 mg BID or placebo for 16 weeks." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 9): "The study sponsor, site, contract research organization (CRO) personnel, and patients were blinded to treatment allocation through Week 16" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 9): "The study sponsor, site, contract research organization (CRO) personnel, and patients were blinded to treatment allocation through Week 16 Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 303, analysed 303 Management of missing data:Quote (p 9, 10):"missing values at Week 16 were imputed using the MI method... Primary and secondary endpoints were analyzed in the intent‐to‐treat (ITT) population, defined as all randomized patients." Results for PASI and PGA were reported in supplmentary appendix Comment: number of analysed pateints not reported for PGA and PASI |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03123471). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported. Results are posted on ClinicalTrials.gov. |
SustaIMM 2019.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind study Date of study: December 2016 ‐ June 2018 Location: multicentre, Japan Phase 2/3 |
|
| Participants |
Randomised: 171 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Risan 150 group (0), Risan 75 group (0), Placebo group (4= AEs) |
|
| Interventions |
Intervention A. Risankizumab 150 mg by SC injection at Weeks 0 and 4 (Part A), n = 55 Control intervention B. Risankizumab 75 mg by SC injection at Weeks 0 and 4, n = 58 C. Placebo, n = 55 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (ClinicalTrials.gov): AbbVie Boehringer Ingelheim Conflict of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "This randomized, double‐blind, double‐dummy, placebo controlled, parallel design study compares two different dose regiments of risankizumab with placebo...After the eligibility criteria are confirmed, the investigator or designee will randomise the patient on Day 1 (Visit 2) through IRT call or website entry. At visits where study medication is to be administered, study sites will be required to complete the medication resupply module in the IRT. Details regarding the use of the IRT are described in the site‐user manual available in the ISF." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "This randomized, double‐blind, double‐dummy, placebo controlled, parallel design study compares two different dose regiments of risankizumab with placebo...After the eligibility criteria are confirmed, the investigator or designee will randomise the patient on Day 1 (Visit 2) through IRT call or website entry. At visits where study medication is to be administered, study sites will be required to complete the medication resupply module in the IRT. Details regarding the use of the IRT are described in the site‐user manual available in the ISF." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "Study drugs will be administered subcutaneously. Injections will be given in a double blind/double‐dummy fashion with each patient receiving 2 injections at each dosing visit: 2 injections of BI 655066, one injection of BI 655066 and one injection of matching placebo or 2 injections of matching placebo depending on randomized dosing group. Syringes will be administered per Flow Chart schedule as assigned by IRT." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (ClinicalTrials.gov and statistical analysis plan): "Study drugs will be administered subcutaneously. Injections will be given in a double blind/double‐dummy fashion with each patient receiving 2 injections at each dosing visit: 2 injections of BI 655066, one injection of BI 655066 and one injection of matching placebo or 2 injections of matching placebo depending on randomized dosing group. Syringes will be administered per Flow Chart schedule as assigned by IRT." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (ClinicalTrials.gov and statistical analysis plan): "The primary analysis will be carried out in the ITT Population and the PP Population. Non‐responder imputation will be used as the primary approach for missing values. LOCF and MI will be performed as sensitivity analyses." Results posted on ClinicalTrials.gov: ITT |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT03000075) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Tanew 1991.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: 2 centres in Austria (Vienna, Innsbruck) |
|
| Participants |
Randomised: 60 participants (mean age 40 years (acitretin), 49 years (placebo); 42 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 30), orally, 1 mg/kg, daily, 12 weeks or until complete clearing Control intervention B. Placebo (n = 30), orally, daily, 12 weeks Co‐intervention PUVA, phototherapy, 4 times/week, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary and secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding: supported by a grant from Hoffma La Roche & Co Ltd Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 682): "Only patients ... were included and assigned randomly..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 682): "Only patients ... were included and assigned randomly..." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (p682): "Acitretin ... or placebo..." Comment: no description of the method used to guarantee blinding of participants and personnel as acitretin leads to visible adverse effects (cheilitis) |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p682): "Acitretin ... or placebo..." Comment: no description of the method used to guarantee blinding of participants and personnel as acitretin leads to visible adverse effects (cheilitis) |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Randomly assigned 60, analysed 48 Quote (p 683): "Of the 60 patients, 48 completed the study and were included in the statistical analysis" Comment: not ITT |
| Selective reporting (reporting bias) | Unclear risk | No protocol available, no outcomes defined in the Method section |
Torii 2010.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: not stated Location: 28 centres in Japan |
|
| Participants |
Randomised: 54 participants (mean age 46 years, 36 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Infliximab (n = 35), IV, 5 mg/kg, weeks 0, 2, 6; 10 weeks Control intervention B. Placebo (n = 19), IV, weeks 0, 2, 6; 10 weeks |
|
| Outcomes | Assessments at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 41): "Eligible patients were randomised in a 2:1 ratio to either... using the dynamic allocation method" Comment: no description of the methods used to guarantee the random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 41): "Eligible patients were randomised in a 2:1 ratio to either... using the dynamic allocation method" Comment: no description of the methods used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 41): "The induction phase of the treatment was .. double‐blind placebo controlled trial... Infliximab or placebo was administered by IV drip infusion over a period of at least 2h ..." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 41): "The induction phase of the treatment was .. double‐blind placebo controlled trial... Infliximab or placebo was administered by intravenous drip infusion over a period of at least 2h ..." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 54, analysed 54 Quote (p 42): "This primary endpoint analysis was performed on an "intent‐to‐treat" basis...Patients who discontinued the study treatment ... were handled as "not improved" in the assessment"" Comment: probably done |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available The prespecified outcomes mentioned in the Methods section appeared to have been reported |
TRANSFIGURE 2016.
| Study characteristics | ||
| Methods | RCT, active‐controlled, double‐blind trial, phase 3 Date of study: November 2013 ‐ January 2017 Location: world‐wide |
|
| Participants |
Randomised: 198 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Secu 150 (4), Secu 300 (1), PBO (7)
|
|
| Interventions |
Intervention A. Biological: secukinumab 150 mg weekly for 5 weeks, then once every 4 weeks up to and including Week 128, n = 67 ControlIntervention B. Biological: secukinumab 300 mg weekly for 5 weeks, then once every 4 weeks up to and including Week 128, n = 66 C. Biological: Placebo, n = 65 |
|
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 1): "Funding sources: This study was funded by Novartis Pharma AG, Basel, Switzerland." Conflicts of interest Quote (Appendix): "Conflicts of interest. K.R. has participated in clinical trials sponsored by AbbVie, Amgen, Biogen Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐ Cilag, LEO, Lilly, Medac, MSD, Novartis, Pfizer, Takeda and Vertex; and has served as a consultant for AbbVie, Amgen, Biogen Idec, Celgene, Centocor, Covagen, Forward Pharma, GlaxoSmithKline, Janssen‐Cilag, LEO, Lilly, Medac, MSD, Novartis, Pfizer, Takeda and Vertex. J.S. has received educational grants from Novartis, AbbVie and Pfizer; and has received consultancy fees from Novartis, AbbVie, Pfizer and Eli Lilly. P.A. has received grants from Novartis. U.M. has received grants and/or participated in clinical trials for Abbott/AbbVie, Almirall, Amgen, BASF, Biogen Idec, Celgene, Centocor, Eli Lilly, Forward Pharma, Galderma, Janssen, LEO Pharma, Medac, MSD, Miltenyi Biotech, Novartis, Pfizer, Teva, VBL and Xenoport; has served as an advisor for and/or received speaker honoraria and/or grants from Abbott/Abb‐ Vie, Almirall, Amgen, BASF, Biogen Idec, Celgene, Centocor, Eli Lilly, Forward Pharma, Galderma, Janssen, LEO Pharma, Medac, MSD, Miltenyi Biotech, Novartis, Pfizer, Teva, VBL and Xenoport; has participated in clinical trials by Novartis, AbbVie, UCB, Valeant, Athenex, MC2 Therapeutics, Dermira, Kadmon, Boehringer Ingelheim, Galderma, Regeneron, Coherus, Tolmar, Amgen, Total, Watson, Sandoz, Xenoport, AbGenomics and Lilly; and has received consulting fees or speaker honoraria from Novartis, Celgene and AbbVie. M.A. has received grants from and/or participated in clinical trials for AbbVie, Almirall, Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, Janssen‐Cilag, LEO, Medac, MSD (formerly Essex, Schering‐Plough), Mundipharma, Novartis, Pfizer (formerly Wyeth), Pohl Boskamp, Sandoz and Xenoport; and has served as an advisor for and/or received speaker honoraria from AbbVie, Almirall, Amgen, Biogen Idec, Boehringer Ingelheim, Celgene, Centocor, Eli Lilly, Janssen‐Cilag, LEO, Medac, MSD (formerly Essex, Schering‐Plough), Mundipharma, Novartis, Pfizer (formerly Wyeth), Pohl Boskamp, Sandoz and Xenoport. A.P., P.R., R.Y. and M.M. are full‐time employees of Novartis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 2):"Randomization was managed via a central interactive randomization system and ensured that an equal number of patients were allocated to secukinumab 300 mg, secukinumab 150 mg or placebo, stratified by body weight (< 90 kg or ≥ 90 kg). At week 16, all patients receiving placebo were rerandomized 1: 1 to receive either 300 mg or 150 mg secukinumab." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 2):"Randomization was managed via a central interactive randomization system and ensured that an equal number of patients were allocated to secukinumab 300 mg, secukinumab 150 mg or placebo, stratified by body weight (< 90 kg or ≥ 90 kg). At week 16, all patients receiving placebo were rerandomized 1: 1 to receive either 300 mg or 150 mg secukinumab." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 2): " TRANSFIGURE was a randomized, double‐blind, placebo‐controlled trial...Patients received subcutaneous treatments of identical appearance once a week for 5 weeks (at baseline and weeks 1, 2, 3 and 4), followed by dosing every 4 weeks, starting at week 4 (Appendixes S3 and S4; see Supporting Information)." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 2): " TRANSFIGURE was a randomized, double‐blind, placebo‐controlled trial...Patients received subcutaneous treatments of identical appearance once a week for 5 weeks (at baseline and weeks 1, 2, 3 and 4), followed by dosing every 4 weeks, starting at week 4 (Appendixes S3 and S4; see Supporting Information)." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data Quote (p 2): "Missing values for PASI and Investigator’s Global Assessment (IGA) mod 2011 were imputed using multiple imputation. Missing patient reported outcome values were imputed with last observation carried forward" On ClinicalTrials.gov, randomized 198, analyzed 198 |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01807520) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported REsults are posted on ClinicalTrials.gov |
Tyring 2006.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: June 2003 – January 2004 Location: 39 centres in Houston, USA and Canada |
|
| Participants |
Randomised: 620 participants (mean age 46 years, 419 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept (n = 311), 50 mg, SC, twice weekly, 12 weeks Control intervention B. Placebo (n = 309), SC, twice weekly, 12 weeks |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding, Quote (p 361): "The study was designed by Immunex, S Tyring, and other members of the Etanercept Psoriasis study group (The complete data set was held at the central data‐processing facility at Amgen) Declarations of interest (pp 367‐8): "S Tyring has received research support from Amgen. A Gottlieb is a consultant for several companies (Amgen, BiogenIdec, CellGate, Centocor, Genentech, Novartis AG, Wyeth Pharmaceuticals, Schering‐Plough Corporation, Eisai, Celgene, Bristol Myers Squibb, Beiersdorf, Warner Chilcott, Abbott Labs, Allergan, Kemia, Roche, Sankyo, Medarex, Celera, TEVA, Actelion, and Advanced ImmuniT) and is on the speaker’s bureau for Amgen, BiogenIdec, and Wyeth Pharmaceuticals. She has also received research funding from Amgen, BiogenIdec, Centocor, Genentech, Abbott Labs, Ligand Pharmaceuticals, Beiersdorf, Fujisawa Healthcare, Celgene Corp, Synta, Bristol Myers Squibb, Warner‐Chilcott, and Paradigm. K Papp is a consultant, has received research funding, and has served as a speaker for Amgen, BiogenIdec, Centocor, Genentech, Novartis, Wyeth, Schering‐Plough, Abbott, Allergan, Medimmune, Serono, Xoma, Isotechnica, and GlaxoSmithKline. He has also served as a medical or scientific officer for Amgen, Centocor, Genentech, and Serono. K Gordon has received research support and honoraria from Abbott, Amgen, Biogen‐IDEC, Centocor, Genentech, and Synta. C Leonardi is: a consultant, investigator, and speaker for Amgen and Genentech and has received educational grants from these companies; a consultant, investigator, and speaker for Centocor; a consultant and investigator for Serono; and a consultant, investigator, and speaker for Abbott..." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 30): “Randomisation code lists were generated in the Biostatistics Department at Amgen by a designed person with no other association with the study” Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 30): “Randomisation code lists were generated in the Biostatistics Department at Amgen by a designed person with no other association with the study” Comment: no precision |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 30): "All patients received 2 injections per dose of investigational product” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 30): “To prevent study assessors from being influenced by the presence of an injection site reaction, patients applied dressings to the last three injection sites and to any erythematous injection sites before each psoriasis evaluation” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 620, analysed 617 for the primary outcome Management of missing data: quote (p 31): “The primary analyses for all efficacy endpoints included all randomised patients who received at least one dose of investigational product. Missing values were imputed using last observation carried forward” Comment: only 2 participants did not receive at least 1 dose, 618 participants should be involved in the mITT, however 617 participants were analysed for the primary outcome |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT00111449) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
UltIMMa‐1 2018.
| Study characteristics | ||
| Methods | RCT, placebo/active‐controlled, double‐blind study Date of study: 24 February 2016 to 31 August 2016 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 506 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Risankizumab, S/C, 150 mg, n = 304 Control interventions B. Ustekinumab, S/C, based on weight per label (45 mg for participants with body weight ≤ 100 kg or 90 mg for participants with body weight > 100 kg), n = 100 C. Placebo, n = 102 |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 650): "AbbVie and Boehringer Ingelheim" Conflict of interest Quote (p 660): " KBG has received honoraria for serving as a consultant and/or grants as an investigator from AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermira, Eli Lilly, GlaxoSmithKline, Janssen, Leo Pharma, Novartis, Pfizer, Regeneron, Sanofi‐Aventis, Sun, and UCB. BS has received honoraria as a consultant for AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly, Galderma, GlaxoSmithKline, Janssen, Leo Pharma, Medac, Meiji Seika Pharma, Menlo Therapeutics, Merck, Novartis, Ortho Dermatologics/Valeant, Pfizer, Regeneron, Sanofi Genzyme, Sebela, Sienna, Sirtris, Sun Pharma, and UCB pharma, and as scientific director for the CORRONA‐NPF Psoriasis Registry. He is an investigator for AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Galderma, GlaxoSmithKline, Janssen, Merck, Pfizer, and Sienna. ML has received grants as an investigator from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen Research & Development, Kadmon, Leo Pharma, Novartis, Pfizer, and ViDac and has received honoraria for serving as a consultant for Allergan, Aqua, Boehringer Ingelheim, Leo Pharma, Menlo, and Promius. MA has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant; and grants as an investigator from AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Hexal, Janssen, Leo Pharma, Eli Lilly, Medac, Mundipharma, MSD, Novartis, Pfizer, Sandoz, UCB, and Xenoport. AB has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant; and grants as an investigator from AbbVie, Aclaris, Akros, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira, Eli Lilly, Genentech/Roche, GlaxoSmithKline, Janssen, Leo Pharma, Meiji, Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sienna pharmaceuticals, UCB, Valeant, and Vidac. YP has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Amgen, Baxalta, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermira, Eli Lilly, Galderma, GlaxoSmithKline, Incyte, Janssen/Centocor, Leo Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi‐Genzyme, Sun Pharma, Takeda, Valeant, and UCB. KAP has received honoraria or fees for serving on advisory boards, as a speaker, as a consultant, or as a steering committee member or grants as an investigator from AbbVie, Akros, Allergan, Amgen, Anacor, Arcutis, Astellas, AstraZeneca, Baxalta, Baxter, Boehringer Ingelheim, Bristol‐Myers Squibb, CanFite, Celgene, Coherus, Dermira, Eli Lilly, Forward Pharma, Galderma, Genentech, GlaxoSmithKline, Janssen, Kyowa‐Hakko Kirin, Leo Pharma, MedImmune, Meiji Seika Pharma, Merck (MSD), Merck‐Serono, Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Roche, Sanofi Genzyme, Takeda, UCB, and Valeant. HS has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novartis, and Pfizer. LP has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Amgen, Baxalta, Biogen, Boehringer Ingelheim, Eli Lilly, Janssen, Leo Pharma, Merck‐Serono, MSD, Novartis, Pfizer, Regeneron, Roche; Sandoz, and Sanofi Genzyme. PF has received honoraria and/or research grants from and/or served as an investigator and/or advisory board member for AbbVie, Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Celtaxsys, CSL, Cutanea, Dermira, Galderma, Genentech, GSK, iNova, Janssen, Leo Pharma, Lilly, Merck, Novartis, Pfizer, Regeneron Pharmaceuticals, Roche, Sanofi, Sun Pharma, UCB Pharma, and Valeant. MO has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Actelion, Astellas, Bayer, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Eisai, Eli Lilly, and Company, Galderma, Janssen, Kaken, Kyowa‐Kirin, Leo Pharma, Maruho, Mochida, Nichi‐Iko, Nippon Kayaku, Nippon Zoki, Novartis, Ono, Ohtsuka, Pola Pharma, Pfizer, Sanofi, Shionogi, Taiho, Tanabe‐Mitsubishi, Teijin, and Torii. MF is a full‐time employee of Boehringer Ingelheim. ZG, YG, and JMV are full‐time employees of AbbVie and own stock or options. EHZT, a former employee of AbbVie, currently owns stock. HB has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Almirall, Amgen, Bayer, Baxalta, Biocad, Boehringer Ingelheim, Celgene, Dermavant, Eli Lilly, Janssen, Leo Pharma, Menarini, MSD, Novartis, Pfizer, Pierre Fabre, Sandoz, Sun Pharmaceuticals, and UCB. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3,randomised, double‐blind, placebo‐controlled and active comparator‐controlled...In each study, patients were randomly assigned (3:1:1) to receive risankizumab, ustekinumab, or matching placebo (appendix). Randomisation was stratified by weight (≤100 kg vs >100 kg) and previous exposure to tumour necrosis factor (TNF) inhibitor (yes vs no); there was no restriction on the number of patients with prior TNF inhibitor exposure. Interactive response technology was used for randomisation and allocation of double‐blind treatment to each patient." Comment Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3,randomised, double‐blind, placebo‐controlled and active comparator‐controlled...In each study, patients were randomly assigned (3:1:1) to receive risankizumab, ustekinumab, or matching placebo (appendix). Randomisation was stratified by weight (≤100 kg vs >100 kg) and previous exposure to tumour necrosis factor (TNF) inhibitor (yes vs no); there was no restriction on the number of patients with prior TNF inhibitor exposure. Interactive response technology was used for randomisation and allocation of double‐blind treatment to each patient." Comment Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3,randomised, double‐blind, placebo‐controlled and active comparator‐controlled...Patients, investigators, and study personnel involved in the trial conduct or analyses remained masked to treatment assignments until study completion. To maintain blinding, the studies utilised a double‐dummy strategy where in risankizumab and its matching placebo or ustekinumab and its matching placebo were identical in appearance." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3,randomised, double‐blind, placebo‐controlled and active comparator‐controlled...Patients, investigators, and study personnel involved in the trial conduct or analyses remained masked to treatment assignments until study completion. To maintain blinding, the studies utilised a double‐dummy strategy where in risankizumab and its matching placebo or ustekinumab and its matching placebo were identical in appearance." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 506 Management of missing data: Quote (p 652‐3): "For both UltIMMa‐1 and UltIMMa‐2 studies, efficacy analyses were done in the intention‐to‐treat population (all randomised patients)... Missing efficacy data for categorical variables were handled with non‐responder imputation and for continuous variables with last observation carried forward" Table 2: 506 analysed participants Comment: done |
| Selective reporting (reporting bias) | Unclear risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02684370) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
UltIMMa‐2 2018.
| Study characteristics | ||
| Methods | RCT, placebo/active‐controlled, double‐blind study Date of study: 1 March 2016 and 30 August 2016 Location: worldwide Phase 3 |
|
| Participants |
Randomised: 491 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Risankizumab, S/C, 150 mg, n = 294 Control interventions B. Ustekinumab, S/C, based on weight per label (45 mg for patients with body weight ≤100 kg or 90 mg for patients with body weight >100 kg), n = 99 C. Placebo, n = 98 |
|
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
|
| Notes | Funding source Quote (p 650): "AbbVie and Boehringer Ingelheim" Conflict of interest Quote (p 660): "KBG has received honoraria for serving as a consultant and/or grants as an investigator from AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermira, Eli Lilly, GlaxoSmithKline, Janssen, Leo Pharma, Novartis, Pfizer, Regeneron, Sanofi‐Aventis, Sun, and UCB. BS has received honoraria as a consultant for AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermavant, Dermira, Eli Lilly, Galderma, GlaxoSmithKline, Janssen, Leo Pharma, Medac, Meiji Seika Pharma, Menlo Therapeutics, Merck, Novartis, Ortho Dermatologics/Valeant, Pfizer, Regeneron, Sanofi Genzyme, Sebela, Sienna, Sirtris, Sun Pharma, and UCB pharma, and as scientific director for the CORRONA‐NPF Psoriasis Registry. He is an investigator for AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Galderma, GlaxoSmithKline, Janssen, Merck, Pfizer, and Sienna. ML has received grants as an investigator from AbbVie, Amgen, Boehringer Ingelheim, Celgene, Eli Lilly, Janssen Research & Development, Kadmon, Leo Pharma, Novartis, Pfizer, and ViDac and has received honoraria for serving as a consultant for Allergan, Aqua, Boehringer Ingelheim, Leo Pharma, Menlo, and Promius. MA has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant; and grants as an investigator from AbbVie, Amgen, Biogen, Boehringer Ingelheim, Celgene, Centocor, Hexal, Janssen, Leo Pharma, Eli Lilly, Medac, Mundipharma, MSD, Novartis, Pfizer, Sandoz, UCB, and Xenoport. AB has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant; and grants as an investigator from AbbVie, Aclaris, Akros, Allergan, Almirall, Amgen, Boehringer Ingelheim, Celgene, Dermavant, Dermira, Eli Lilly, Genentech/Roche, GlaxoSmithKline, Janssen, Leo Pharma, Meiji, Merck Sharp & Dohme, Novartis, Pfizer, Purdue Pharma, Regeneron, Sandoz, Sanofi Genzyme, Sienna pharmaceuticals, UCB, Valeant, and Vidac. YP has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Amgen, Baxalta, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Dermira, Eli Lilly, Galderma, GlaxoSmithKline, Incyte, Janssen/Centocor, Leo Pharma, MedImmune, Merck, Novartis, Pfizer, Regeneron, Roche, Sanofi‐Genzyme, Sun Pharma, Takeda, Valeant, and UCB. KAP has received honoraria or fees for serving on advisory boards, as a speaker, as a consultant, or as a steering committee member or grants as an investigator from AbbVie, Akros, Allergan, Amgen, Anacor, Arcutis, Astellas, AstraZeneca, Baxalta, Baxter, Boehringer Ingelheim, Bristol‐Myers Squibb, CanFite, Celgene, Coherus, Dermira, Eli Lilly, Forward Pharma, Galderma, Genentech, GlaxoSmithKline, Janssen, Kyowa‐Hakko Kirin, Leo Pharma, MedImmune, Meiji Seika Pharma, Merck (MSD), Merck‐Serono, Mitsubishi Pharma, Novartis, Pfizer, Regeneron, Roche, Sanofi Genzyme, Takeda, UCB, and Valeant. HS has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Amgen, Boehringer Ingelheim, Eli Lilly, Janssen, Merck, Novartis, and Pfizer. LP has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Amgen, Baxalta, Biogen, Boehringer Ingelheim, Eli Lilly, Janssen, Leo Pharma, Merck‐Serono, MSD, Novartis, Pfizer, Regeneron, Roche; Sandoz, and Sanofi Genzyme. PF has received honoraria and/or research grants from and/or served as an investigator and/or advisory board member for AbbVie, Amgen, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Celtaxsys, CSL, Cutanea, Dermira, Galderma, Genentech, GSK, iNova, Janssen, Leo Pharma, Lilly, Merck, Novartis, Pfizer, Regeneron Pharmaceuticals, Roche, Sanofi, Sun Pharma, UCB Pharma, and Valeant. MO has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Actelion, Astellas, Bayer, Boehringer Ingelheim, Bristol‐Myers Squibb, Celgene, Eisai, Eli Lilly, and Company, Galderma, Janssen, Kaken, Kyowa‐Kirin, Leo Pharma, Maruho, Mochida, Nichi‐Iko, Nippon Kayaku, Nippon Zoki, Novartis, Ono, Ohtsuka, Pola Pharma, Pfizer, Sanofi, Shionogi, Taiho, Tanabe‐Mitsubishi, Teijin, and Torii. MF is a full‐time employee of Boehringer Ingelheim. ZG, YG, and JMV are full‐time employees of AbbVie and own stock or options. EHZT, a former employee of AbbVie, currently owns stock. HB has received honoraria or fees for serving on advisory boards, as a speaker, and as a consultant, and grants as an investigator from AbbVie, Almirall, Amgen, Bayer, Baxalta, Biocad, Boehringer Ingelheim, Celgene, Dermavant, Eli Lilly, Janssen, Leo Pharma, Menarini, MSD, Novartis, Pfizer, Pierre Fabre, Sandoz, Sun Pharmaceuticals, and UCB. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (pp 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3, randomised, double‐blind, placebo‐controlled and active comparator‐controlled...In each study, patients were randomly assigned (3:1:1) to receive risankizumab, ustekinumab, or matching placebo (appendix). Randomisation was stratified by weight (≤100 kg vs >100 kg) and previous exposure to tumour necrosis factor (TNF) inhibitor (yes vs no); there was no restriction on the number of patients with prior TNF inhibitor exposure. Interactive response technology was used for randomisation and allocation of double‐blind treatment to each patient." Comment Probably done |
| Allocation concealment (selection bias) | Low risk | Quote (pp 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3, randomised, double‐blind, placebo‐controlled and active comparator‐controlled...In each study, patients were randomly assigned (3:1:1) to receive risankizumab, ustekinumab, or matching placebo (appendix). Randomisation was stratified by weight (≤100 kg vs >100 kg) and previous exposure to tumour necrosis factor (TNF) inhibitor (yes vs no); there was no restriction on the number of patients with prior TNF inhibitor exposure. Interactive response technology was used for randomisation and allocation of double‐blind treatment to each patient." Comment Probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (pp 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3, randomised, double‐blind, placebo‐controlled and active comparator‐controlled...Patients, investigators, and study personnel involved in the trial conduct or analyses remained masked to treatment assignments until study completion. To maintain blinding, the studies utilised a double‐dummy strategy where in risankizumab and its matching placebo or ustekinumab and its matching placebo were identical in appearance." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (pp 651‐2): "UltIMMa‐1 and UltIMMa‐2 were replicate phase 3, randomised, double‐blind, placebo‐controlled and active comparator‐controlled...Patients, investigators, and study personnel involved in the trial conduct or analyses remained masked to treatment assignments until study completion. To maintain blinding, the studies utilised a double‐dummy strategy where in risankizumab and its matching placebo or ustekinumab and its matching placebo were identical in appearance." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 491 Management of missing data: Quote (pp 652‐3): "For both UltIMMa‐1 and UltIMMa‐2 studies, efficacy analyses were done in the intention‐to‐treat population (all randomised patients)... Missing efficacy data for categorical variables were handled with non‐responder imputation and for continuous variables with last observation carried forward" Table 2: 491 analysed participants Comment: done |
| Selective reporting (reporting bias) | Unclear risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT0268435). The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
UNCOVER‐1 2016.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: November 2011 to June 2014 Location: multicentre (104) in Europe, Australia, North America |
|
| Participants |
Randomised: 1296 participants (mean age 45 years, 883 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ixekizumab (n = 432), SC, 80 mg, 2 injections week 0, 1 injection monthly Control intervention B. Ixekizumab (n = 433), SC, 80 mg, 2 injections week 0, 1 injection eow C. Placebo (n = 431), SC |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 346): “The trials were sponsored by Eli Lilly and were designed by the scientific steering committee and Eli Lilly personnel. The site investigators collected the data, Eli Lilly personnel performed the data analyses, and all the authors had access to the data.” Declarations of interest (p 355): "Disclosure forms provided by the authors are available with the full text of this article at NEJM.org." Gordon received grants and personal fees from Abbvie, Amgen, Celgene, Eli Lilly, Novartis; and personal fees from Pfizer and Medac |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (supplemental appendix): “Patients were assigned to treatment groups as determined by a computer‐generated random sequence .." Comment: clearly defined |
| Allocation concealment (selection bias) | Low risk | Quote (supplemental appendix): “Patients were assigned to treatment groups as determined by a computer‐generated random sequence using an interactive voice response system (IVRS). Site personnel confirmed that they had located the correct assigned investigational product package by entering a confirmation number found on the package into the IVRS” Comment: clearly defined |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 346): “double‐blind, placebo‐controlled” Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 346): “double‐blind, placebo‐controlled” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1296, analysed 1296 Management of missing data: Quote (p 348): “Unless otherwise specified, all analyses of efficacy during the induction period were performed according to the intention‐to‐treat principle. Missing values for the PASI and the sPGA score were imputed conservatively as nonresponses, regardless of the reason for the missing data” Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01474512) The prespecified outcomes mentioned in the protocol and in the Methods section appeared to have been reported |
UNCOVER‐2 2015.
| Study characteristics | ||
| Methods | RCT, active, placebo‐controlled, double‐blind Date of study: 10 May 2012 ‐ 7 May 2015 Location: 118 centres in Europe, Australia, North America |
|
| Participants |
Randomised: 1224 participants (mean age 45 years, 821 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ixekizumab (n = 347), SC, 80 mg, 2 injections week 0, 1 injection monthly Control intervention B. Ixekizumab (n = 351), SC, 80 mg, 2 injections week 0, 1 injection eow C. Etanercept (n = 358), SC, 50 mg 1 injection twice weekly D. Placebo (n = 168), SC |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 543): “The funder Eli Lilly. Data were collected by investigators, gathered by Parexel International, and analysed by the funder”. agents and collected and analysed the data. All the authors had full access to the data”. Declarations of interest, Quote (pp 550‐1): "CEMG has received grants and personal fees from Eli Lilly, Abbvie, Janssen, Novartis, Sandoz, Pfizer, and GlaxoSmithKline; personal fees from Actelion, Amgen, and UCB Pharma; grants from LEO Pharma and Merck Sharp & Dohme; and is president of the International Psoriasis Council. KR has received personal fees from AbbVie, Amgen, Biogen, Celgene, Forward Pharma, Janssen‐Cilag, LEO Pharma, Eli Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, and Takeda. ML is an employee of the Mount Sinai Medical Center which receives research funds from AbGenomics, AbbVie, Amgen, Anacor, Aqua, Canfite Biopharma, Celgene, Clinuvel, Coronado Biosciences, Ferndale, Lilly, Janssen Biotech, LEO Pharmaceuticals, Merz, Novartis, Pfizer, Sandoz, and Valeant. PvdK has received grants from Celgene, Centocor, Allmiral, Pfizer, Philips, AbbVie, Eli Lilly, Galderma, Novartis, Janssen Cilag, and Leo Pharma; and has served as a speaker for Amgen, a consultant for Sandoz and Mitisibishu, and a speaker and consultant for Celgene, AbbVie, Eli Lilly, Galderma, Novartis, Janssen Cilag, and Leo Pharma. CP has received grants and personal fees from Amgen, Abbvie, Celgene, Eli Lilly, Novartis, Janssen, Pfizer, and Leo Pharma. KP has received honoraria as consultant and/or scientific officer and/or advisory board and/or steering committee member and/or acted as a paid speaker and/ or participated in clinical trials and/or received clinical research grants sponsored by 3M, Abbott/AbbVie, Akesis, Akros, Allergan, Alza, Amgen, Anacor, Apotex, Astellas, Baxter, Berlex, Biogen, Boehringer Ingelheim, Celgene, Celtic, Centocor, Cipher, Dermira, Dow Pharma, Eli Lilly, Forward Pharma, Fujisawa, Funxional Therapeutics, Galderma, Genentech, Genexion, GlaxoSmithKline, Isotechnika, Janssen, Janssen Biotech, Johnson & Johnson, Kataka, Kirin, Kyowa, Leo Pharma, Lypanosys, Medical Minds, Medimmune, Merck, Mitsubishi, Novartis, NovImmune, Pan Genetics, Pfizer, Roche, Regneron, Merck‐Serono, Stiefel, Takeda, UCB, Vertex, Wyeth/Pfizer, and Xoma. AM has served as an advisory board member and/or consultant and/or investigator and/or speaker and/or received compensation in the form of grants and/or honoraria from AbbVie, Allergan, Amgen, ApoPharma, Boehringer Ingelheim, Celgene, Convoy Therapeutics, Eli Lilly, Genentech, Janssen Biotech, LEO Pharma, Merck, Novartis, Pfizer, Symbio and Maruho, Syntrix, Wyeth, and XenoPort. GSC, JE, LZ, RJS, SB, DKB, OOO, MPH, and BJN were employees of and hold stock in Eli Lilly & Co during the conduct of this study. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 542): “randomly assigned”, “An interactive voice response system" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 542): “An interactive voice response system was used to assign double‐blind investigational product to every patient. Site personnel confirmed that they had located the correct assigned investigational product package by entering a confirmation number found in the package into to IVRS” Comment: clearly defined |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 542): “Patients, investigators and study personnel were masked to the treatment allocation. A double‐dummy design was used” Comment: clearly defined |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 542): “Patients, investigators and study personnel were masked to the treatment allocation. A double‐dummy design was used” Comment: clearly defined |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1224, analysed 1224 Management of missing data: Quote (p 543): “All missing data were imputed using non‐responder imputation (NRI)” Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01597245) One prespecified outcome in the protocol missing from the Results section (assessment of efficacy at 60 weeks), but as we assessed outcomes at induction phase (between 8 ‐ 24 weeks), we judged that the risk of selective reporting was low |
UNCOVER‐3 2015.
| Study characteristics | ||
| Methods | RCT, active, placebo‐controlled, double‐blind Date of study: 18 July 2012 ‐18 January 2016 Location: 101 in Europe, Asia, North and South America |
|
| Participants |
Randomised: 1346 participants (mean age 46 years, 918 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Ixekizumab (n = 386), SC, 80 mg, 2 injections week 0, 1 injection monthly Control intervention B. Ixekizumab (n = 385), SC, 80 mg, 2 injections week 0, 1 injection eow C. Etanercept (n = 382), SC, 50 mg 1 injection twice weekly D. Placebo (n = 193), SC |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 543): “The funder Eli Lilly. Data were collected by investigators, gathered by Parexel International, and analysed by the funder”. agents and collected and analysed the data. All the authors had full access to the data”. Declarations of interest: Quote (pp 550‐1): "CEMG has received grants and personal fees from Eli Lilly, Abbvie, Janssen, Novartis, Sandoz, Pfizer, and GlaxoSmithKline; personal fees from Actelion, Amgen, and UCB Pharma; grants from LEO Pharma and Merck Sharp & Dohme; and is president of the International Psoriasis Council. KR has received personal fees from AbbVie, Amgen, Biogen, Celgene, Forward Pharma, Janssen‐Cilag, LEO Pharma, Eli Lilly, Medac, Merck Sharp & Dohme, Novartis, Pfizer, Regeneron, and Takeda. ML is an employee of the Mount Sinai Medical Center which receives research funds from AbGenomics, AbbVie, Amgen, Anacor, Aqua, Canfite Biopharma, Celgene, Clinuvel, Coronado Biosciences, Ferndale, Lilly, Janssen Biotech, LEO Pharmaceuticals, Merz, Novartis, Pfizer, Sandoz, and Valeant. PvdK has received grants from Celgene, Centocor, Allmiral, Pfizer, Philips, AbbVie, Eli Lilly, Galderma, Novartis, Janssen Cilag, and Leo Pharma; and has served as a speaker for Amgen, a consultant for Sandoz and Mitisibishu, and a speaker and consultant for Celgene, AbbVie, Eli Lilly, Galderma, Novartis, Janssen Cilag, and Leo Pharma. CP has received grants and personal fees from Amgen, Abbvie, Celgene, Eli Lilly, Novartis, Janssen, Pfizer, and Leo Pharma. KP has received honoraria as consultant and/or scientific officer and/or advisory board and/or steering committee member and/or acted as a paid speaker and/ or participated in clinical trials and/or received clinical research grants sponsored by 3M, Abbott/AbbVie, Akesis, Akros, Allergan, Alza, Amgen, Anacor, Apotex, Astellas, Baxter, Berlex, Biogen, Boehringer Ingelheim, Celgene, Celtic, Centocor, Cipher, Dermira, Dow Pharma, Eli Lilly, Forward Pharma, Fujisawa, Funxional Therapeutics, Galderma, Genentech, Genexion, GlaxoSmithKline, Isotechnika, Janssen, Janssen Biotech, Johnson & Johnson, Kataka, Kirin, Kyowa, Leo Pharma, Lypanosys, Medical Minds, Medimmune, Merck, Mitsubishi, Novartis, NovImmune, Pan Genetics, Pfizer, Roche, Regneron, Merck‐Serono, Stiefel, Takeda, UCB, Vertex, Wyeth/Pfizer, and Xoma. AM has served as an advisory board member and/or consultant and/or investigator and/or speaker and/or received compensation in the form of grants and/or honoraria from AbbVie, Allergan, Amgen, ApoPharma, Boehringer Ingelheim, Celgene, Convoy Therapeutics, Eli Lilly, Genentech, Janssen Biotech, LEO Pharma, Merck, Novartis, Pfizer, Symbio and Maruho, Syntrix, Wyeth, and XenoPort. GSC, JE, LZ, RJS, SB, DKB, OOO, MPH, and BJN were employees of and hold stock in Eli Lilly & Co during the conduct of this study. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 542): “randomly assigned” "An interactive voice response system" Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 542): “An interactive voice response system was used to assign double‐blind investigational product to every patient. Site personnel confirmed that they had located the correct assigned investigational product package by entering a confirmation number found in the package into to IVRS” Comment: clearly defined |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 542): “Patients, investigators and study personnel were masked to the treatment allocation. A double‐dummy design was used” Comment: clearly defined |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 542): “Patients, investigators and study personnel were masked to the treatment allocation. A double‐dummy design was used” Comment: clearly defined |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 1346, analysed 1346 Management of missing data: Quote (p 543): “All missing data were imputed using non‐responder imputation (NRI)” Comment: probably done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01646177) One prespecified outcome in the protocol missing from the Results section (assessment of efficacy at 60 weeks), but as we assessed outcomes at induction phase (between 8 ‐ 24 weeks), we judged that the risk of selective reporting was low |
Van Bezooijen 2016.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: 2013 and June 2015 Location: single centre in the Netherlands |
|
| Participants |
Randomised: 33 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Fumaric acid (n = 18), from 215 mg once daily up to a maximum of 215 mg 4 times a day, 24 weeks Control intervention B. Placebo Co‐intervention Etanercept (n = 15) (50 mg SC twice weekly for 12 weeks followed by 50 mg once weekly for an additional 12 weeks) |
|
| Outcomes | Assessments at 24 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding: Quote (supplemental appendix): "This investigator‐initiated study was supported by a grant of Pfizer Pharmaceuticals. Pfizer was not involved in any study procedure, but Pfizer was granted the right to read, but not to edit, the manuscript prior to submission for publication." Declarations of interest (p 413): "Investigator‐initiated project grant from Pfizer. E. Prens has acted as a consultant for AbbVie, Amgen, Astra‐Zeneca, Baxter, Eli Lilly, Galderma, Janssen‐Cilag, Novartis and Pfizer and has received investigator‐initiated research grants (paid to Erasmus MC) from Pfizer, Janssen‐Cilag and AbbVie. M.B.A. van Doorn has acted as a consultant for Abbott, Janssen, LEO Pharma, MSD and Pfizer, and has been an investigator for Eli Lilly, Idera Pharmaceu‐ticals, Cutanea and Novartis. T. van Gelder has been on the speakers’ bureau or worked as consultant for Sandoz, Novartis, Teva, Chiesi, Astellas and Roche". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (supplemental appendix): “Using a computer‐generated randomisation list, patients were randomised at baseline to a 1:1 ratio to receive either etanercept combined with oral fumarates (combination group) or etanercept only (monotherapy group). ” Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (supplemental appendix): “Using a computer‐generated randomisation list, patients were randomised at baseline to a 1:1 ratio to receive either etanercept combined with oral fumarates (combination group) or etanercept only (monotherapy group).” Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (supplemental appendix): "Patients and the study physicians were not blinded for the allocated treatment group.” Comment: not blinded |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (supplemental appendix): “The independent PASI assessor (E.P.P.) was blinded to treatment throughout the course of the study.” Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 33, analysed 33 for the primary outcome Management of missing data: Quote (supplemental appendix): “Patients lost to follow‐up were not included in the PASI 75 response and PGA score analyses. ” Comment: not ITT analyses, but all randomised participants reached the primary outcome assessment |
| Selective reporting (reporting bias) | Unclear risk | Comment: the protocol for the study was available on European Clinical Trials Database (EudraCT) (EudraCT No. 2011‐005685‐38) (not found) The prespecified results mentioned in the Methods section appeared to have been reported |
Van de Kerkhof 2008.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: Jun 2006 ‐ May 2007 Location: multicentre (numbers of centres not stated) in Belgium, France, Germany, Hungary, Italy, Netherlands, Poland, Romania, Spain |
|
| Participants |
Randomised: 142 participants (mean age 45 years, 84 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Etanercept, 50 mg, self‐administered SC, once a week, 12 weeks (n = 96) Control intervention B. Placebo, self‐administered SC, once a week, 12 weeks (n = 46) |
|
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source (p 1184): "This study was supported financially by Wyeth Pharmaceuticals, Collegeville, PA, USA)" Comments: 3 authors were employed by Wyeth pharmaceuticals which supported this study financially Declarations of interest (p 1177): "C.Z., M.P.B., L.P. and J.W. are employed by Wyeth Pharmaceuticals, which supported this study financially. " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 1178): "Patients were randomly assigned (using the Clinical Operations Randomization Environment system) ... according to a 2:1 treatment allocation" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote (p1178): "Patients were randomly assigned (using the Clinical Operations Randomization Environment system) ... according to a 2:1 treatment allocation" Comment: not specified |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1178): "In both the double blind controlled study..., etanercept was supplied as a sterile lyophilised powder. All study drugs were self‐administrated QW by the patient by subcutaneous injections" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1178): "In both the double blind controlled study..., etanercept was supplied as a sterile lyophilised powder. All study drugs were self‐administrated QW by the patient by subcutaneous injections" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 142, analysed 142 Management of missing data, quote (p 1179): "The primary population for efficacy and safety analyses ... was the modified intent‐to‐treat population. The last observations were carried forward in cases of missing efficacy data" Comment: done |
| Selective reporting (reporting bias) | Unclear risk | Comment: the specified outcomes mentioned in the Methods section appeared to have been reported, but no protocol was available |
VIP Trial 2018.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: February 2012 ‐ October 27, 2016 Location: 8 centres in the USA Phase 4 |
|
| Participants |
Randomised: 96 participants Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
ADA group (1), UV group (3), Placebo group (1)
|
|
| Interventions |
Intervention A. Adalimumab (Humira). Humira will be given at an initial dose of 80 mg followed by 40 mg the 2nd week, subsequent doses will be given at 40 mg and follow FDA dosing schedule, n = 33 Control intervention B. NB‐UVB phototherapy. Phototherapy will be given 3 times a week according to the Fitzpatrick scale for skin types, n = 33 C. Placebo injection will be given according to the same dose and schedule as the active comparator, n = 1 |
|
| Outcomes |
At weeks 12 Primary outcome measures
Secondary outcome measures:
|
|
| Notes | Funding Quote (p 10): "This study was supported by grants (National Heart, Lung, and Blood Institute R01‐HL111293, K24‐AR‐064310) and by an unrestricted grant from AbbVie (to the Trustees of the University of Pennsylvania). Dr Mehta is supported by National Institutes of Health Intramural Research Program (Z01 HL‐06193). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the article; and decision to submit the article for publication." Conflict of interest Quote (p 10): Dr Mehta is a full‐time US Government Employee and receives research grants to the National Heart, Lung, and Blood Institute (NHLBI) from AbbVie, Janssen, Celgene, and Novartis. Dr Gelfand in the past 12 months has served as a consultant for Coherus (DSMB), Dermira, Janssen Biologics, Merck (DSMB), Novartis Corp, Regeneron, Dr. Reddy’s Laboratories, Sanofi and Pfizer Inc, receiving honoraria; and receives research grants (to the Trustees of the University of Pennsylvania) from Abbvie, Janssen, Novartis Corp, Regeneron, Sanofi, Celgene, and Pfizer Inc; and received payment for continuing medical education work related to psoriasis that was supported indirectly by Lilly and Abbvie. Dr Gelfand is a copatent holder of resiquimod for treatment of cutaneous T cell lymphoma. Dr Takeshita receives a research grant from Pfizer Inc (to the Trustees of the University of Pennsylvania) and has received payment for continuing medical education work related to psoriasis that was supported indirectly by Eli Lilly. A.B. Troxel is a co‐patent holder of resiquimod for treatment of cutaneous T cell lymphoma. Dr Tyring conducts clinical studies sponsored by the following companies: Abbvie/ BI; Celgene; Coherus; Dermira; Eli Lilly; Janssen; Leo; Merck; Novartis; Pfizer; Regeneron/Sanofi; and Valeant. He is a speaker for Abbvie, Eli Lilly, Janssen, Leo, Novartis, Pfizer, Regeneron/Sanofi, and Valeant. Dr Armstrong has received research grants and honorarium from AbbVie, Celgene, Janssen, Novartis, Eli Lilly, Regeneron, Sanofi, and Valeant and has participated in continuing medical education work related to psoriasis that was indirectly supported by Eli Lilly and AbbVie. Dr Duffin has received grant/research/clinical trial support from Amgen, Abbvie, Celgene, Eli Lilly, Janssen, Bristol‐Myers Squibb, Stiefel, Novartis, and Pfizer over the last 24 months. Additionally, Dr Duffin has served as a consultant/ on the advisory boards for Amgen, Abbvie, Celgene, Eli Lilly, Janssen, Bristol‐Myers Squibb, Stiefel, Novartis, and Pfizer. Dr Chiesa Fuxench has no conflicts of interest. However, she was being funded, at the time, by a research grant from the National Psoriasis Foundation and a training grant from the National Institutes of Health. Dr Hubbard receives grant funding from the National Institutes of Health and Patient‐Centered Outcomes Research Institute. Dr Rader is the co‐founder of Vascular Strategies and holds equity in the company. Dr Kalb has received grants/research funding from AbbVie, Amgen, Boehringer Ingelheim, Janssen‐ Ortho Inc, Merck & Co, Inc, and Novartis Pharmaceuticals Corp over the last 24 months. During this time frame, he has also served as a consultant honoraria for Dermira, Janssen‐Ortho Inc, Sun Pharmaceutical Industries Ltd, and a DSMB member honoraria for Eli Lilly and Co. Dr Simpson has served as a consultant for AbbVie, Anacor, Celgene, Dermira, Genentech, Leo, Glaxo Smith Kline, Pfizer, Regeneron, Sanofi‐Genzyme, Menlo, and Eli Lilly in the last 24 months. During this time frame, he has also acted as the primary investigator for the following sponsored trials: Anacor, Celgene, Chugai, Dermira, Eli Lilly, Genentech, MedImmune, Merck, Novartis, Regeneron, Roivant, Tioga, and Vanda. Dr Torigian is the co‐founder of Quantitative Radiology Solutions LLC. Dr Van Voorhees has served on the advisory board of Celgene, Dermira, Allergan, Merck, Pfizer, Aqua, Astra Zeneca, Jannsen, Amgen, Leo, Allergan, and Lilly. For Novartis and AbbVie, Dr Van Voorhees acts as a consultant as well as serves on the board. Dr Van Voorhees has received a portion of ex‐spouse pension from Merck. Dr Menter in the last 24 months has served on the advisory board for AbbVie, Allergan, Amgen, Boehringer Ingelheim, Eli Lilly, Janssen Biotech, Inc, and LEO Pharma. He has also worked as a consultant for AbbVie, Allergan, Amgen, Eli Lilly, Galderma, Janssen Biotech, Inc, LEO Pharma, Novartis, Pfizer, Vitae, and Xenoport. Additionally, he has acted as an investigator for AbbVie, Allergan, Amgen, Anacor, Boehringer Ingelheim, Celgene, Dermira, Eli Lilly, Janssen Biotech, Inc, LEO Pharma, Merck, Neothetics, Novartis, Pfizer, Regeneron, Symbio/Maruho, and Xenoport. He also serves as a speaker for AbbVie, Amgen, Janssen Biotech, Inc, and LEO Pharma. He has received compensation in the form of grants from AbbVie, Allergan, Amgen, Anacor, Boehringer Ingelheim, Celgene, Dermira, Janssen Biotech, Inc, LEO Pharma, Merck, Neothetics, Novartis, Pfizer, Regeneron, Symbio/Maruho, and Xenoport. He has also received honoraria from AbbVie, Allergan, Amgen, Boehringer Ingelheim, Eli Lilly, Galderma, Janssen Biotech, Inc, LEO Pharma, Novartis, Pfizer, Vitae, and Xenoport. The other authors report no conflicts. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 2): "The study was a multicenter randomized controlled trial designed to enroll 96 patients across 8 centers in the United States with 1:1:1 allocation to..." Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "Adalimumab (or corresponding placebo) therapy was administered in a double‐blind manner as a subcutaneous injection with an initial 80 mg dose at week 0, followed by maintenance doses of 40 mg every other week, starting from week 1 and then continued throughout the study" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote (p 3): "Adalimumab (or corresponding placebo) therapy was administered in a double‐blind manner as a subcutaneous injection with an initial 80 mg dose at week 0, followed by maintenance doses of 40 mg every other week, starting from week 1 and then continued throughout the study" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomised: 96; analysed 92 Dealing with missing data: not stated but few withdrawal (1/3/0) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01553058) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
VIP‐U Trial 2020.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: July 2014 ‐ September 2018 Location: University of Pennsylvania, USA (40 sites, multicentre) Phase 4 |
|
| Participants |
Randomised: 43 participants Inclusion criteria
Exclusion criteria
Baseline characteristics N = 43, mean age of 42.5 years and 70% men Dropouts and withdrawals
Ustekinumab group (2), Placebo group (6) Before cross‐over
After cross‐over
|
|
| Interventions |
Intervention A. Ustekinumab (Stelara) subcutaneous injection 45 mg (if person's weight is 100 kg or less) or 90 mg (if person's weight is > 100 kg) at day 0 and week 4 followed by every 12‐week dosing thereafter, Participant will receive total of 52 weeks of ustekinumab (12 weeks during RCT phase, 40 weeks post‐RCT phase) n = 22 Control intervention B. Placebo, Placebo subcutaneous injection will be given according to the same dose and schedule as the active comparator until week 12 (end of RCT phase). At week 12, ustekinumab will be administered according according to the same injection schedule as the active comparator arm for 52 weeks. Patient will receive total of 52 weeks of ustekinumab (0 weeks during RCT phase, 52 weeks post RCT phase). n = 21 |
|
| Outcomes |
At week 52 Primary outcome
Secondary outcomes
|
|
| Notes | In ClinicalTrials.gov, the secondary outcomes are different from paper
Funding Quote (p92): " This study was funded by a grant to the Trustees of the University of Pennsylvania from Janssen Pharmaceuticals (JMG). JMG received additional funding from NIAMS K24AR064310. JT is funded in part by K23 AR068433. NNM received additional funding from NHLBI Intramural Research Program (HL006193‐05). We thank the patients who volunteered for this study and Suzette Baez Vanderbeek for her project management expertise. " Conflict of interest Quote (p92):"Outside of the submitted work, JMG served and received honoraria as a consultant for BMS, Boehringer Ingelheim, Janssen Biologics, Novartis Corp, UCB (DSMB), Sanofi, and Pfizer Inc.; and received research grants (to the Trustees of the University of Pennsylvania) from AbbVie, Boehringer Ingelheim, Janssen, Novartis Corp, Celgene, Ortho Dermatologics, and Pfizer Inc.; and received payment for continuing medical education work related to psoriasis that was supported indirectly by Eli Lilly, Ortho Dermatologics, and Novartis. JMG is a co‐patent holder of resiquimod for treatment of cutaneous T‐cell lymphoma, and is a Deputy Editor for the Journal of Investigative Dermatology receiving honoraria from the Society for Investigative Dermatology. DAT is a cofounder of Quantitative Radiology Solutions LLC. MHN receives a research grant via the Trustees of the University of Pennsylvania from Boehringer Ingelheim, and she is supported by a K23‐AR073932 career development award from the National Institute of Arthritis and Musculo‐skeletal and Skin Diseases. MHN has also received payments for work done as in independent contractor from UptoDate and Derm101. JT receives a grant from NIAMS K23‐AR068433 and a research grant (both to the Trustees of the University of Pennsylvania) from Pfizer Inc., and has received payment for continuing medical education work related to psoriasis that was supported indirectly by Eli Lilly and Novartis. NNM is a full time US government employee. NNM has served as a consultant for Amgen, Eli Lilly, and Leo Pharma receiving grants and/or other payments; as a principal investigator and/or investigator for AbbVie, Celgene, Janssen Pharmaceuticals Inc, and Novartis receiving grants and/or research funding; and as a principal investigator for the National Institute of Health receiving grants and/or research funding. All the other authors state no conflict of interest " |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p89, 91):"The study was a randomized, double‐blind, placebo‐controlled trial designed to enroll 42 patients with allocation ratio of 1:1 to ustekinumab subcutaneous injections or placebo injections at baseline and week 4.... Study group assignment was performed via block randomization (of four and eight), using a computerized system at the Investigational Drug Services, University of Pennsylvania." Comment: adequate procedure |
| Allocation concealment (selection bias) | Unclear risk | Quote (p89, 90):"The study was a randomized, double‐blind, placebo‐controlled trial designed to enroll 42 patients with allocation ratio of 1:1 to ustekinumab subcutaneous injections or placebo injections at baseline and week 4... Ustekinumab (or corresponding placebo) therapy was administered in a double‐blind manner as subcutaneous injections." Comment: lack of information on appearance of ustekinumab and placebo, no information on process of treatment dispensation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p89, 91):"The study was a randomized, double‐blind, placebo‐controlled trial designed to enroll 42 patients with allocation ratio of 1:1 to ustekinumab subcutaneous injections or placebo injections at baseline and week 4....Study investigators, staff, and patients were blinded to ustekinumab or placebo status during the placebo‐controlled period. All scans were read in a blinded fashion to patient characteristics, treatment allocation, and visit dates (i.e., baseline, week 12, or end of study). " Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p89, 91):"The study was a randomized, double‐blind, placebo‐controlled trial designed to enroll 42 patients with allocation ratio of 1:1 to uste‐ kinumab subcutaneous injections or placebo injections at baseline and week 4....Study investigators, staff, and patients were blinded to ustekinumab or placebo status during the placebo‐controlled period. All scans were read in a blinded fashion to patient characteristics, treatment allocation, and visit dates (i.e., baseline, week 12, or end of study). " Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Dealing with missing data: Quote (p91):"The missing data were summarized using frequencies for each outcome measure...The primary analyses were restricted to subjects who completed the trial (i.e., had primary outcome measures assessed at baseline and week 12)."The primary analyses were restricted to subjects who completed the trial (i.e., had primary outcome measures assessed at baseline and week 12). For TBRmax, additional multivariate linear regression models were fitted to assess sensitivity to potential imbalance of covariates (which may occur by chance in smaller randomized controlled trials), such as age, sex, and major cardiovascular disease risk factors (serum glucose, systolic and diastolic blood pressure, tobacco use, family history, serum LDL, HDL, total cholesterol, body mass index, psoriatic arthritis, and PASI). For binary outcomes, the treatment group comparisons were assessed using logistic regression models. Randomly assigned 43 |
| Selective reporting (reporting bias) | High risk | Comment: In clinicaltrials, the secondary outcomes are different from paper the protocol for the study was available on ClinicalTrials.gov (NCT02187172) Results are posted on ClinicalTrials.gov. |
VOYAGE‐1 2016.
| Study characteristics | ||
| Methods | RCT, active placebo‐controlled, double‐blind Date of study: December 2014 ‐ April 2016 Location: 101 centres worldwide |
|
| Participants |
Randomised: 837 participants (mean age 44 years, 608 male) Inclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Guselkumab (n = 334), SC, 100 mg, weeks 0 and 4, then every 8 weeks Control intervention B. Adalimumab (n = 329), 80 mg week 0, then 40 mg week 1, and every 2 weeks C. Placebo (n = 174) |
|
| Outcomes | Assessment at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 405): "Supported by Janssen Research & Development LLC, Spring House, PA." DEclarations of interest Quote (p 405): "Dr Blauvelt has served as a scientific adviser and clinical study investigator for AbbVie, Amgen, Boehringer Ingelheim, Celgene, Dermira, Genentech, GSK, Janssen, Eli Lilly, Merck, Novartis, Pfizer, Regeneron, Sandoz, Sanofi‐Genzyme, Sun, UCB, and Valeant, and as a paid speaker for Eli Lilly. Dr Papp has received honoraria or clinical research grants as a consultant, speaker, scientific officer, advisory board member, and/or steering committee member for AbbVie, Akesis, Akros, Allergan, Alza, Amgen, Anacor, Artax, Astellas, AstraZeneca, Baxalta, Baxter, Biogen, Boehringer Ingelheim, Bristol‐Myers Squibb, CanFite, Celgene, Celtic, Cipher, Dermira, Dow Pharmaceuticals, Eli Lilly, Ferring Pharmaceuticals, Formycon, Forward Pharma, Funxional Therapeutics, Fujisawa, Galderma, Genentech, Genexion, Genzyme, Gilead, GSK, Janssen, Kyowa Hakko Kirin, Leo, Lypanosys, Medimmune, Meiji Seika Pharma, Merck (MSD), Merck‐Serono, Mitsubishi Pharma, Mylan, Novartis, NovImmune, Pan Genetics, Pfizer, Regeneron, Roche, Sanofi‐Aventis, Stiefel, Takeda, UCB, Vertex, and Valeant. Dr Griffiths has received honoraria and/or grants as an investigator, speaker, and/or advisory board member for AbbVie, Eli Lilly, Janssen, Leo, Novartis, Pfizer, Sandoz, and Sun Pharma. Dr Kimball has received honoraria as a consultant for AbbVie, BMS, Dermira, Eli Lilly ICOS LLC, Merck, and Novartis; and received grants and/or funding for research or the residency/fellowship program as a principal investigator for AbbVie, Amgen, Boehringer Ingelheim, Dermira, Janssen, Merck, and Novartis. Drs Randazzo, Wasfi, Shen, and Li are all employees of Janssen Research & Development LLC (subsidiary of Johnson & Johnson) and own stock in Johnson & Johnson." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 3): "Patients were randomised using a permuted block method Central randomisation was implemented using an interactive World Wide Web response system (Perceptive Informatics, East Windsor, NJ)." Comment: clearly defined |
| Allocation concealment (selection bias) | Low risk | Quote (p 3): "Central randomisation was implemented using an interactive World Wide Web response system (Perceptive Informatics, East Windsor, NJ)." Comment: clearly defined |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "To maintain the blind, matching placebos were used." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "To maintain the blind, matching placebos were used." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 837, 837 analysed Management of missing data: quote (page 3): "Patients who discontinued study agent because of lack of efficacy or anAE of psoriasis worsening or who started a protocol‐prohibited psoriasis treatment were considered nonresponders (binary end points) or had baseline values carried over (continuous end points). Other patients with missing data were considered nonresponders for binary end points (nonresponder imputation) and had last observation carried forward for continuous end points (and all PSSD end points)." Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02207231) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
VOYAGE‐2 2017.
| Study characteristics | ||
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: November 2014 ‐ May 2016 Location: 115 centres world‐wide |
|
| Participants |
Randomised: 992 participants (mean age 44 years, 692 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Guselkumab (n = 496), SC, 100 mg, weeks 0 and 4, then every 8 weeks Control intervention B. Adalimumab (n = 248), 80 mg week 0, then 40 mg week 1, and every 2 weeks C. Placebo (n = 248) |
|
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: Quote (p 1): "Supported by Janssen Research & Development, LLC." Declarations of interest (p 1): "Dr Reich has served as advisor and/or paid speaker for and/or participated in clinical trials sponsored by AbbVie, Amgen, Biogen, Boehringer Ingelheim Pharma, Celgene, Covagen, Eli Lilly, Forward Pharma, GlaxoSmithKline, Janssen, Leo, Medac, Merck Sharp & Dohme, Novartis, Ocean Pharma, Pfizer, Regeneron, Takeda, UCB Pharma, and Xenoport. Dr Armstrong has served as investigator and/or advisor/consultant for AbbVie, Amgen, Celgene, Eli Lilly, Janssen, Merck, Novartis, and Pfizer. Dr Foley has served as a consultant, investigator, speaker, and/or advisor for and/or received travel grants from 3M/iNova/Valeant, Abbott/AbbVie, Amgen, Biogen Idec, BMS, Boehringer Ingelheim, Celtaxsys, Celgene, Cutanea, Eli Lilly, Galderma, GSK/Stiefel, Janssen, LEO/Peplin, Novartis, Regeneron, Schering‐Plough/MSD, UCB, and Wyeth/Pfizer. Dr Gordon has received research support from AbbVie, Amgen, Boeringher Ingelheim, Eli Lilly, and Janssen, and consultant/ honoraria from AbbVie, Amgen, Boeringher Ingelheim, Celgene, Eli Lilly, Janssen, Novartis, and Pfizer. Drs Song, Wasfi, Randazzo, Li, and Shen are all employees of Janssen Research & Development, LLC (subsidiary of Johnson & Johnson) and own stock in Johnson & Johnson." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 3): "Patients were randomized 2:1:1 using a permuted block method at baseline to guselkumab 100 mg at weeks 0, 4, 12, and 20; placebo at weeks 0, 4, and 12, then guselkumab at weeks 16 and 20; or adalimumab 80 mg at week 0, 40 mg at week 1, and every 2 weeks thereafter through week 23 (Fig 1). Central randomization occurred using an interactive web based response system (Perceptive Informatics, East Windsor, NJ)." Comment: clearly defined |
| Allocation concealment (selection bias) | Low risk | Quote (p 3): "Patients were randomized using a permuted block method at baseline in a 2:1:2 ratio to guselkumab 100 mg at weeks 0, 4, 12, and every 8 weeks through week 44; placebo at weeks 0, 4, and 12 followed by guselkumab 100 mg at weeks 16 and 20, and every 8 weeks through week 44; or adalimumab 80 mg at week 0, 40 mg at week 1, and 40 mg every 2 weeks through week 47. Central randomization was implemented using an interactive World Wide Web response system (Perceptive Informatics, East Windsor, NJ)." Comment: clearly defined |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 3): "double‐blind, placebo‐ and adalimumab comparator controlled study" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 3): "double‐blind, placebo‐ and adalimumab comparator controlled study" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Randomly assigned 992, 992 analyzed Management of missing data: quote (p 3): "All randomized patients were included in the primary analysis and some secondary efficacy analyses according to their assigned treatment group.... Patients who discontinued treatment due to lack of efficacy or an adverse event [AE] of worsening of psoriasis, or started a protocol‐prohibited medication/therapy to improve psoriasis were considered treatment failures." Comment: done |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT02207244) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported |
Yang 2012.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind Date of study: February 2009 ‐ February 2010 Location: 9 centres in China |
|
| Participants |
Randomised: 129 participants (mean age 39 years (infliximab) and 40 years (placebo), 95 male) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Infliximab (n = 84), IV, 5 mg/kg, weeks 0, 2, 6, 14, 22; 22 weeks Control intervention B. Placebo (n = 45), IV, weeks 0, 2, 6 then infliximab 5 mg/kg weeks 10, 12, 16 |
|
| Outcomes | Assessments at 10 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
|
| Notes | Funding source: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (p 1846): "This randomised, double‐blind, placebo controlled trial... Eligible patients were randomly assigned in a 1:2 ratio to the placebo and infliximab" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 1846): "This randomised, double‐blind, placebo controlled trial... Eligible patients were randomly assigned in a 1:2 ratio to the placebo and infliximab" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 1846): "This randomised, double‐blind, placebo controlled trial... Eligible patients were randomly assigned in a 1:2 ratio to the placebo and infliximab... Infliximab 5 mg/kg or placebo was administered by intravenous drip infusion over a period of at least 2 hours on the starting day of treatment (week 0) and at weeks 2 and 6 (induction)". Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 1846): "This randomised, double‐blind, placebo controlled trial... Eligible patients were randomly assigned in a 1:2 ratio to the placebo and infliximab... Infliximab 5 mg/kg or placebo was administered by intravenous drip infusion over a period of at least 2 hours on the starting day of treatment (week 0) and at weeks 2 and 6 (induction)". Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 129, 129 Analysed Quote: "In the primary efficacy analysis, data from all randomised subjects were analysed according to their assigned treatment group..." Comment: no description of the method used to manage the missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The prespecified outcomes mentioned in the Methods section appeared to have been reported |
Yilmaz 2002.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, open‐label trial Date of study: unreported Location: Turkey |
|
| Participants |
Randomised: 50 participants (no description of the study population) Inclusion/exclusion criteria
Dropouts and withdrawals
|
|
| Interventions |
Intervention A. Acitretin (n = 50), orally, 0.5‐0.7 mg/kg, daily Control intervention B. Placebo (n = 50). Co‐intervention PUVA, twice weekly, 8‐MOP at a dosage of 0.4 ‐ 0.6 g/kg, 2 hours before UVA exposure |
|
| Outcomes | Time of assessments not stated Primary or secondary outcomes of the trial
Outcomes of the trial
|
|
| Notes | Funding source: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote (abstract): "The patients were equally allocated to treatment groups in the study" Comment: no description of the method used to guarantee random sequence generation |
| Allocation concealment (selection bias) | Unclear risk | Quote (abstract): "The patients were equally allocated to treatment groups in the study" Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote (abstract): "We performed an open, controlled study..." Comment: not blinded, subjective outcome |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (abstract): "We performed an open, controlled study..." Comment: not blinded, subjective outcome |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Randomly assigned 50 Comment: no description of the number of participants analysed, no description of the method used to manage missing data |
| Selective reporting (reporting bias) | Unclear risk | Comment: only an abstract available |
Yu 2019.
| Study characteristics | ||
| Methods | RCT, active‐controlled Date of study: not stated Location: China |
|
| Participants |
Randomised: 30 participants Key inclusion criteria
Key exclusion criteria
Baseline characteristics N = 30, mean age of 51.93 years and 67% men Dropouts and withdrawals No withdrawals occured |
|
| Interventions |
Intervention A. methotrexate (combination of etanercept, SC injection 50 mg weekly and methotrexate, PO 7.5 ‐ 15 mg weekly), n = 15 Control intervention B. No treatment n = 15 CO‐intervention Etanercept (SC injection 50 mg every week through week 24), |
|
| Outcomes |
At week 24 Outcomes
|
|
| Notes | Funding Quote (p 449): "This work was supported by grants from National Natural Science Foundation of China (No. 81673050, 81872522), the Program of Science and Technology Commission of Shanghai Municipality (No. 18140901800), Innovation Program of Shanghai Municipal Education Commission (No.2019‐01‐07‐00‐07‐E00046), Excellent Subject Leader Program of Shanghai Municipal Commission of Health and Family Planning (No. 2018BR30), Clinical Research Program of Shanghai Hospital Development Center (No. SHDC12018X06)." Conflict of interest Quote (p 449): "There is no conflicting interest." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 443): "Randomization was undertaken with the use of computer‐generated random numbers." Comment: adequate process |
| Allocation concealment (selection bias) | Unclear risk | Quote (p 443): "Randomization was undertaken with the use of computer‐generated random numbers." Comment: no description of the method used to guarantee allocation concealment |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Comment: no description of the method used to guarantee blinding |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote (p 443): "The PASI score was determined by a dermatologist at 2, 6, 12, 18 and 24 weeks of treatment." Comment: Physicians were not blinded for for PASI evaluation, that’s why we chose high risk of bias |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 15 included/15 analysed Comment: no description of the method used to manage the missing data or to perform the analyses |
| Selective reporting (reporting bias) | Unclear risk | Comment: no protocol was available. The pre‐specified outcomes mentioned in the methods section appeared to have been reported |
Zhang 2017.
| Study characteristics | ||
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: December 2013 ‐ July 2015 Location: China (multicentric) Phase 3 |
|
| Participants |
Randomised: 266 participants (mean age 41 years, 194 men) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
Tofacitinib 5 group (4), Tofacitinib 10 group (7), Placebo group (11)
|
|
| Interventions |
Intervention A. Tofacitinib 5 mg twice a day, n = 88 Control intervention B. Tofacitinib 10 mg twice a day, n = 90 C. Placebo, n = 88 |
|
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
|
| Notes | Funding Quote (p 44):
"This study was sponsored by Pfizer Inc. Medical writing support, under the guidance of the authors, was provided by Complete Medical Communications and funded by Pfizer Inc." Conflicts of interest Quote (p 44): "J.Z. Zhang conducted clinical trials or received honoraria for serving as a consultant for AbbVie, Bayer, Janssen‐Cilag and Pfizer Inc. T.F. Tsai conducted clinical trials or received honoraria for serving as a consultant for AbbVie, Boehringer Ingelheim, Celgene, Eli Lilly, Galderma, Janssen‐Cilag, Leo, Novartis Pharmaceuticals, Pfizer Inc, and Serono International SA (now Merck Serono International). M.G. Lee conducted clinical trials for Eli Lilly, Janssen‐Cilag, Novartis Pharmaceuticals, and Pfizer Inc, and received honoraria for acting as a speaker for Janssen‐Cilag. M. Zheng conducted clinical trials or received honoraria for serving as a consultant for AbbVie, Janssen‐Cilag and Pfizer Inc. G. Wang has conducted clinical trials for AbbVie, Janssen‐Cilag, and Pfizer Inc, and has acted as a consultant or speaker for La Roche‐Posay China, LEO Pharma China, and Xian‐Janssen. H.Z. Jin conducted clinical trials or received honoraria for serving as a consultant for AbbVie, Boehringer Ingelheim, Galderma, Janssen‐Cilag, and Pfizer Inc. J. Gu conducted clinical trials or received honoraria for serving as a speaker for AbbVie, Galderma, Janssen‐Cilag, Novartis, and Pfizer Inc. R.Y. Li conducted clinical trials or received honoraria for serving as a consultant for AbbVie, Galderma, Leo Pharma China, Novartis Pharmaceuticals, Pfizer Inc, and Xian‐Janssen Pharmaceuticals. Q.Z. Liu conducted clinical trials for Bayer, Ipsen, and Pfizer Inc. J. Chen conducted clinical trials for AbbVie, AstraZeneca, and Pfizer Inc. C.X. Tu conducted clinical trials for Janssen‐Cilag and Pfizer Inc, and has acted as a consultant for Astellas Pharma Inc and Janssen‐Cilag. C.M. Qi, H. Zhu, W. Ports, and T. Crook are employees and shareholders of Pfizer Inc." |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote (p 37): "This was a Phase 3, randomized, double‐blind, placebo‐controlled, parallel‐group study (NCT01815424) carried out between December 2013 and July 2015 (Fig. 1). A computer‐generated randomization schedule was developed by Pfizer and an automated telephone/web‐based interactive response system was used to assign patients 2:2:1:1 to receive tofacitinib 5 mg BID, tofacitinib 10 mg BID, placebo advanced to tofacitinib 5 mg BID, or placebo advanced to tofacitinib 10 mg BID." Comment: probably done |
| Allocation concealment (selection bias) | Low risk | Quote (p 37): "This was a Phase 3, randomized, double‐blind, placebo‐controlled, parallel‐group study (NCT01815424) carried out between December 2013 and July 2015 (Fig. 1). A computer‐generated randomization schedule was developed by Pfizer and an automated telephone/web‐based interactive response system was used to assign patients 2:2:1:1 to receive tofacitinib 5 mg BID, tofacitinib 10 mg BID, placebo advanced to tofacitinib 5 mg BID, or placebo advanced to tofacitinib 10 mg BID." Comment: probably done |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote (p 37): "This was a Phase 3, randomized, double‐blind, placebo‐controlled, parallel‐group study (NCT01815424) carried ... Patients, investigators, and the sponsor were blinded to study treatment. Placebo was provided as oral tablets matching those of tofacitinib." Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote (p 37): "This was a Phase 3, randomized, double‐blind, placebo‐controlled, parallel‐group study (NCT01815424) carried ... Patients, investigators, and the sponsor were blinded to study treatment. Placebo was provided as oral tablets matching those of tofacitinib." Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Dealing with missing data Quote (p 38): "Data were analyzed for the full analysis set: all randomized patients who received >= dose of study drug. All binary variables... were analyzed..., with non‐responder imputation for missing data." 266 randomized, 266 analyzed imbalance reasons and number of withdrawal: Insufficient clinical response: Tofacitinib 5 group (0), Tofacitinib 10 group (2), Placebo group (4) |
| Selective reporting (reporting bias) | Low risk | Comment: the protocol for the study was available on ClinicalTrials.gov (NCT01815424) The prespecified outcomes and those mentioned in the Methods section appeared to have been reported Results are posted on ClinicalTrials.gov |
AEs: adverse events; ACR: American College of Rheumatology; ALT: alanine aminotransferase; AST: aspartate aminotransferase; BSA: Body Surface Area; eow: every other week; CIN: cervical intraepithelial neoplasia; DLQI: Dermatology Life Quality Index; ECG: electrocardiogram; eow: every other week; HD: high dose; IGA: Investigator’s Global Assessment; IM: intramuscular; ITT: intention‐to‐treat; IV: intravenous; LD: low dose; m‐ITT: modified ITT; MD: medium dose; NAPSI: Nail psoriasis severity index; NBUVB: narrow‐band UVB; PASI: Psoriasis Area and Severity Index; PGA: Physician Global Assessment; PP: per protocol; PSI: Psoriasis Severity Index; PSSI: Psoriasis Scalp Severity Index; PUVA: psoralen plus ultraviolet A; QoL: quality of life; RCT: randomised controlled trial; SAEs; serious adverse events; SC: subcutaneous; SF36: 36‐item Short Form Health Survey; SIAQ: Self‐ Injection Assessment Questionnaire; TB: tuberculosis; TBR: target background ratio; UVB: ultraviolet B; VAS: visual analogue scale Please note that the term “conventional” in these tables is replaced with “non‐biological treatment” in the main text of this review.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abe 2017 | Post hoc subgroup analyses of an already included trial |
| Abufarag 2010 | Other treatment |
| Adsit 2017 | Post hoc subgroup analyses of an already included trial |
| Akhyani 2010 | Other treatment |
| Altmeyer 1994 | Not plaque‐type psoriasis |
| Angsten 2007 | Not a trial |
| Anonymous 2005 | Not a trial |
| Anonymous 2008 | Not a trial |
| Anonymous 2019 | Not a randomised trial |
| Araujo 2017 | Not moderate‐to‐severe psoriasis |
| Araujo 2019 | Not moderate‐to‐severe psoriasis |
| Arifov 1998 | Not a randomised trial |
| Armati 1972 | Other treatment |
| Augustin 2017 | Dose de‐escalation strategy study |
| Avgerinou 2011 | Not a randomised trial |
| Bachelez 2017 | Post hoc subgroup analyses of an already included trial |
| Bagel 2017a | Open‐label extension restricted to good responders |
| Bagel 2017b | Not a randomised trial |
| Bagel 2017c | Not moderate‐to‐severe psoriasis |
| Bagel 2018b | Not a randomised trial |
| Bagherani 2017 | Commentary/editorial |
| Bagot 1994 | Other treatment |
| Bartlett 2008 | Not a trial |
| Barzegari 2004 | Other treatment |
| Batchelor 2009 | Not a trial |
| Bayerl 1992 | Other treatment |
| Beissert 2009 | Other treatment |
| Berbis 1989 | Assessment < 8 weeks |
| Bhat 2017 | Post hoc subgroup analyses of an already included trial |
| Bhuiyan 2010 | Other treatment |
| Bian 2018 | Open‐label extension restricted to good responders |
| Bigby 2004 | Not a trial |
| Bissonnette 2006 | Other treatment |
| Bissonnette 2010 | Other treatment |
| Bissonnette 2017a | Open‐label extension restricted to good responders |
| Bissonnette 2017b | Not moderate‐to‐severe psoriasis |
| Bissonnette 2018 | Not moderate‐to‐severe psoriasis |
| Bjerke 1989 | Other treatment |
| Blauvelt 2016a | Ineligible study design |
| Blauvelt 2016b | Open‐label extension restricted to good responders |
| Blauvelt 2017a | Pooled trials |
| Blauvelt 2017b | Open‐label extension restricted to good responders |
| Blauvelt 2017c | Open‐label extension restricted to good responders |
| Blauvelt 2017d | Open‐label extension restricted to good responders |
| Blauvelt 2017e | Pooled trials |
| Blauvelt 2017f | Ineligible study design |
| Blauvelt 2017g | Open‐label extension restricted to good responders |
| Blauvelt 2017h | Open‐label extension restricted to good responders |
| Blauvelt 2017i | Open‐label extension restricted to good responders |
| Blauvelt 2017j | Pooled trials |
| Blauvelt 2017k | Open‐label extension restricted to good responders |
| Blauvelt 2018a | Not a randomised trial |
| Blauvelt 2018b | Open‐label extension restricted to good responders |
| Blauvelt 2018c | Open‐label extension restricted to good responders |
| Blauvelt 2018d | Pooled trials |
| Blauvelt 2018e | Pooled trials |
| Blauvelt 2018f | Pooled trials |
| Blauvelt 2018g | Pooled trials |
| Blauvelt 2018h | Pooled trials |
| Blauvelt 2018i | Pooled trials |
| Branigan 2017 | Open‐label extension restricted to good responders |
| Brasil 2012 | Ineligible study design |
| Brasil 2013 | Ineligible patient population |
| Brasil 2016 | Ineligible patient population |
| Burden 2017 | Commentary/editorial |
| Burkhardt 2017 | Ineligible study design |
| Callis Duffin 2017 | Comparison of the same drug with the same dosages |
| Cassano 2006 | Identical dosing regimens |
| Cassano 2010 | Not a trial |
| Cather 2006 | Dose‐ranging after remission |
| Cather 2018 | Ineligible patient population |
| Chakravadhanula 2017 | Ineligible intervention |
| Chapman 2018 | Ineligible study design |
| ChiCTR‐INR‐16009710 | Assessment at 4 weeks |
| Chládek 2002 | Basic science (aim of study: to understand the physiopathology of the disease) |
| Chodorowska 1999a | Not a trial |
| Chodorowska 1999b | Not a trial |
| Choi 2017 | Not moderate‐to‐severe psoriasis |
| Crowley 2018a | Not moderate‐to‐severe psoriasis |
| Crowley 2018b | Open‐label extension restricted to good responders |
| CTRI/2018/01/011373 | 2 different schemas of administration (same drug, same dosage) |
| De Jong 2003 | Other treatment |
| De Mendizabal 2017 | Post hoc subgroup analyses of an already included trial |
| Dubiel 1972 | Not a trial |
| Duffin 2016 | Comparison of 2 different ways of drug injection for the same drug and the same dosage |
| Duffin 2017 | Ineligible study design |
| Ecker‐Schlipf 2009 | Other treatment |
| Edson‐Heredia 2013 | Post hoc subgroup analyses of an already included trial |
| Egeberg 2016 | Commentary/editorial |
| Elewski 2007 | Pooled trials |
| Elewski 2017 | Post hoc subgroup analyses of an already included trial |
| Elewski 2018a | Ineligible study design |
| Elewski 2018b | Ineligible study design |
| Ellis 1986 | Assessment < 8 weeks |
| Ellis 2001 | Another intervention |
| Ellis 2002 | Medico‐economic study |
| Ellis 2012 | Other treatment |
| Engst 1989 | Assessment < 8 weeks |
| Erkko 1997 | Basic science (aim of study: to understand the physiopathology of the disease) |
| EUCTR2007‐004328‐18‐FR | Ineligible intervention |
| EUCTR2012‐005685‐35‐DE | Withdrawn trial, NCT01815723 |
| EUCTR2016‐001593‐15‐ES | Withdrawal trial, DEEP Study |
| EUCTR2016‐003592‐21‐GB | Withdrawal trial |
| EUCTR2018‐001021‐10‐SE | Not moderate‐to‐severe psoriasis |
| EUCTR2019‐000817‐35‐DE | Not moderate‐to‐severe psoriasis |
| Ezquerra 2007 | Other treatment |
| Feldman 2017 | Not moderate‐to‐severe psoriasis |
| Fernandes 2013 | Not a trial |
| Fernandez 2017 | Not a randomised trial |
| Finzi 1993 | Other treatment |
| Fitz 2018 | Post hoc subgroup analyses of an already included trial |
| Fleischer 2005 | Other treatment |
| Foley 2017 | Pooled trials |
| Foley 2018 | Pooled trials |
| Fredriksson 1971 | Other treatment |
| Fredriksson 1978 | Other treatment |
| Friedrich 2001 | Other treatment |
| Gambichler 2011 | Other treatment |
| Ganguly 2004 | Pooled trials |
| Gil 2003 | Not a randomised trial |
| Glatt 2017 | Ineligible study design |
| Goerz 1978 | Not a trial |
| Gold 2018 | Ineligible study design |
| Goll 2017 | Not moderate‐to‐severe psoriasis |
| Goll 2018 | Ineligible study design |
| Gollnick 1988 | Other treatment |
| Gollnick 1993 | Other treatment |
| Gollnick 2002 | Other treatment |
| Gordon 2014 | Ineligible study design |
| Gordon 2015 | Ineligible study design |
| Gordon 2018a | Open‐label extension restricted to good responders |
| Gordon 2018b | Post hoc subgroup analyses of an already included trial |
| Gordon 2018c | Pooled trials |
| Gordon 2018d | Post hoc subgroup analyses of an already included trial |
| Gottlieb 2002 | Other treatment |
| Gottlieb 2003b | Other treatment |
| Gottlieb 2003c | Open‐label extension restricted to good responders |
| Gottlieb 2004b | Pooled trials |
| Gottlieb 2005 | Other treatment |
| Gottlieb 2006a | Ineligible intervention |
| Gottlieb 2006b | Ineligible intervention |
| Gottlieb 2010 | Cross‐over trial |
| Gottlieb 2016 | Pooled trials |
| Gottlieb 2017a | Not moderate‐to‐severe psoriasis |
| Gottlieb 2017b | Not moderate‐to‐severe psoriasis |
| Gottlieb 2017c | Post hoc subgroup analyses of an already included trial |
| Gottlieb 2017d | Pooled trials |
| Gottlieb 2018a | Pooled trials |
| Gottlieb 2018b | Pooled trials |
| Goupille 1995 | Not a randomised trial |
| Goupille 2018 | Not moderate‐to‐severe psoriasis |
| Griffiths 1998 | Other treatment |
| Griffiths 2002a | Pooled trials |
| Griffiths 2002b | Pooled trials |
| Griffiths 2005 | Pooled trials |
| Griffiths 2010 | Open‐label extension restricted to good responders |
| Griffiths 2016 | Post hoc subgroup analyses of an already included trial |
| Griffiths 2017 | Open‐label extension restricted to good responders |
| Griffiths 2018a | Ineligible study design |
| Griffiths 2018b | Post hoc subgroup analyses of an already included trial |
| Griffiths 2018c | Pooled trials |
| Grim 2000 | Basic science (aim of study: to understand the physiopathology of the disease) |
| Grossman 1994 | Other treatment |
| Guenther 2020 | Not moderate‐to‐severe psoriasis |
| Gulliver 1996 | Not a trial |
| Gupta 2005 | Other treatment |
| Gupta 2007 | Other treatment |
| Gupta 2008 | Other treatment |
| Han 2013 | Other treatment |
| Hashizume 2007 | Comparison of 2 methods of administration |
| Hawkes 2018 | Ineligible study design |
| Heule 1988 | Assessment < 8 weeks |
| Ho 2010 | Other treatment |
| Holzer 2020 | No efficacy or safety assessment ‐ the study assessed cardiovascular outcomes |
| Hsu 2018 | Post hoc subgroup analyses of an already included trial |
| Hunter 1972 | Other treatment |
| Iest 1989 | Not a randomised trial |
| Imafuku 2017 | Post hoc subgroup analyses of an already included trial |
| Iversen 2018 | Ineligible comparator |
| Jackson 2018 | Ineligible study design |
| Jacobe 2008 | Another intervention |
| JapicCTI‐194706 2019 | Comparison of different schemas of administraton (same drug, same dosage) |
| jRCTs041180012 2018 | Not moderate‐to‐severe psoriasis |
| Kaur 2018 | Ineligible outcomes |
| Kavanaugh 2009 | Not a randomised trial |
| Kemeny 2019 | Post hoc subgroup analyses of an already included trial |
| Kimball 2008 | Drug withdrawn for safety reasons |
| Kimball 2011 | Drug withdrawn for safety reasons |
| Kimball 2018 | Ineligible study design |
| Koo 1998 | Other treatment |
| Kopp 2015 | Phase 1 trial |
| Kragballe 1989 | Other treatment |
| Krishnan 2005 | Pooled trials |
| Krishnan 2018 | Pooled trials |
| Kristensen 2017 | Not moderate‐to‐severe psoriasis |
| Krueger 1980 | Other treatment |
| Krueger 2002a | Another intervention |
| Krueger 2002b | Not a trial |
| Krueger 2003 | Not a trial |
| Krueger 2012 | Phase 1 trial |
| Krueger 2015 | Phase 1 trial |
| Krueger 2016b | Phase I trial |
| Krupashankar 2014 | Another intervention |
| Kuijpers 1998 | Other treatment |
| Lajevardi 2015 | Other treatment |
| Lambert 2018 | Post hoc subgroup analyses of an already included trial |
| Langewouters 2005 | Other treatment |
| Langley 2006 | Other treatment |
| Langley 2010 | Other treatment |
| Langley 2016 | Open‐label extension restricted to good responders |
| Langley 2018 | Ineligible study design |
| Langner 2004 | Not plaque‐type psoriasis |
| Lauharanta 1989 | Other treatment |
| Lawrence 1983 | Other treatment |
| Leavell 1970 | Other treatment |
| Lebwohl 2003 | Another intervention |
| Lebwohl 2003a | Pooled trials |
| Lebwohl 2009 | Pooled trials |
| Lebwohl 2012 | Other treatment |
| Lebwohl 2013 | Other treatment |
| Ledo 1988 | Other treatment |
| Legat 2005 | Other treatment |
| Leonardi 2010a | Pooled trials |
| Leonardi 2010b | Not a randomised trial |
| Leonardi 2010c | Pooled trials |
| Leonardi 2011a | Open‐label extension restricted to good responders |
| Leonardi 2011b | Not plaque‐type psoriasis |
| Levell 1995 | Other treatment |
| Li 2018 | Post hoc subgroup analyses of an already included trial |
| Liang 1995 | Assessment < 8 weeks |
| Louw 2017 | Open‐label extension restricted to good responders |
| Lui 2011 | Other treatment |
| Lui 2012 | Other treatment |
| Lynde 2012 | Other treatment |
| Macdonald 1972 | Not a randomised trial |
| Mahrle 1995 | Other treatment |
| Malik 2010 | Other treatment |
| Marecki 2004 | Other treatment |
| Marks 1986 | Not a randomised trial |
| Mate 2017 | Not moderate‐to‐severe psoriasis |
| Mate 2018 | Open‐label extension restricted to good responders |
| McInnes 2013 | Pooled trials |
| McInnes 2017 | Not moderate‐to‐severe psoriasis |
| Mease 2011 | Drug withdrawn for safety reasons |
| Mease 2016a | Not moderate‐to‐severe psoriasis |
| Mease 2016b | Not moderate‐to‐severe psoriasis |
| Mease 2017a | Not moderate‐to‐severe psoriasis |
| Mease 2017b | Not moderate‐to‐severe psoriasis |
| Mease 2017c | Not moderate‐to‐severe psoriasis |
| Mease 2018 | Not moderate‐to‐severe psoriasis |
| Meffert 1989 | Other treatment |
| Menon 2012 | Basic science (aim of study: to understand the physiopathology of the disease) |
| Menter 2007 | Pooled trials |
| Menter 2014 | Drug withdrawn for safety reasons |
| Merola 2017 | Post hoc subgroup analyses of an already included trial |
| Merola 2018 | Not moderate‐to‐severe psoriasis |
| Meyer 2011 | Other treatment |
| Mittal 2009 | Other treatment |
| Moller 2009 | Other treatment |
| Monk 1986 | Not a randomised trial |
| Montgomery 1993 | Other treatment |
| Mrowietz 1991 | The 2 study arms compared the same molecule with the same dosage |
| Mrowietz 2012 | Pooled trials |
| Narang 2012 | Other treatment |
| Nash 2015 | Not moderate‐to‐severe psoriasis |
| NCT00106847 | Dose de‐escalation strategy study |
| NCT00111111 | Dose de‐escalation strategy study |
| NCT00258713 | Ineligible intervention |
| NCT00358670 | Open‐label extension restricted to good responders |
| NCT00377325 | Withdrawal trial |
| NCT00438360 | Open‐label extension restricted to good responders |
| NCT00585650 | Ineligible patient population |
| NCT00645892 | Open‐label extension restricted to good responders |
| NCT00646191 | Open‐label extension restricted to good responders |
| NCT00647400 | Open‐label extension restricted to good responders |
| NCT00832364 | Withdrawal trial |
| NCT01163253 | Not a randomised trial |
| NCT01235442 | Ineligible intervention |
| NCT01276847 | Phase I trial |
| NCT01412944 | Open‐label extension restricted to good responders |
| NCT01443338 | Ineligible comparator |
| NCT01544595 | Open‐label extension restricted to good responders |
| NCT01550744 | Open‐label extension restricted to good responders |
| NCT01624233 | Not a randomised trial |
| NCT01722214 | Not moderate‐to‐severe psoriasis |
| NCT01806597 | Ineligible patient population |
| NCT01815723 | Withdrawal trial |
| NCT01828086 | Phase I trial |
| NCT01936688 | Withdrawal trial |
| NCT02362789 | Withdrawal trial |
| NCT02409667 | Open‐label extension restricted to good responders |
| NCT02798211 | Not moderate‐to‐severe psoriasis |
| NCT03010527 | Open‐label extension restricted to good responders |
| NCT03020199 | Ineligible comparator |
| NCT03073213 | Phase I trial |
| Nemoto 2018 | Phase I trial |
| Nieboer 1990 | Other treatment |
| Nijsten 2008 | Not a trial |
| Noda 2011 | Not a randomised trial |
| Noor 2017 | Not a randomised trial |
| Novotny 1973 | Not a trial |
| Nyfors 1978 | Not a trial |
| Okubo 2019 | Open‐label extension restricted to good responders |
| Orfanos 1978 | Other treatment |
| Orfanos 1979 | Other treatment |
| Ortonne 2008 | Comparison of 2 schemes of administration |
| Ortonne 2011 | Other treatment |
| Osamu 2014 | Phase 1 trial |
| Page 2020 | Phase 1 trial |
| Pakozdi 2018 | Post hoc subgroup analyses of an already included trial |
| Papp 2001 | Other treatment |
| Papp 2006 | Other treatment |
| Papp 2008 | Other treatment |
| Papp 2009 | Pooled data |
| Papp 2011a | Pooled trials |
| Papp 2011b | Drug withdrawn for safety reasons |
| Papp 2011c | Drug withdrawn for safety reasons |
| Papp 2012d | Phase 1 trial |
| Papp 2012e | Pooled trials |
| Papp 2017c | Open‐label extension restricted to good responders |
| Papp 2018a | Ineligible outcomes |
| Papp 2018b | Ineligible outcomes |
| Park 2013 | Other treatment |
| Paul 2012 | Other treatment |
| Paul 2014 | Other treatment |
| Paul 2018 | Pooled trials |
| Perks 2017 | Ineligible study design |
| Pettit 1979 | Assessment < 8 weeks |
| Petzelbauer 1990 | Not a randomised trial |
| Piascik 2003 | Not a trial |
| Ports 2013 | Other treatment |
| Puig 2018 | Ineligible outcomes |
| Punwani 2012 | Other treatment |
| Rabasseda 2012 | Not a trial |
| Radmanesh 2011 | Comparison of 2 schemes of administration |
| Raman 1998 | Other treatment |
| Reich 2004 | Ineligible intervention |
| Reich 2011 | Pooled trials |
| Reich 2014 | Other treatment |
| Reich 2016a | Ineligible study design |
| Reich 2016b | Ineligible study design |
| Reich 2017a | Ineligible study design |
| Reich 2017b | Open‐label extension restricted to good responders |
| Reich 2017c | Pooled trials |
| Reich 2018a | Ineligible outcomes |
| Reich 2018b | Ineligible |
| Reich 2018c | Open‐label extension restricted to good responders |
| Reitamo 1999 | Other treatment |
| Reitamo 2001 | Other treatment |
| Rim 2003 | Other treatment |
| Rinsho Iyaku 1991 | Other treatment |
| Ritchlin 2006a | Not a randomised trial |
| Ritchlin 2006b | Not a randomised trial |
| Romiti 2017 | Post hoc subgroup analyses of an already included trial |
| RPCEC00000201 | Ineligible intervention |
| Ryan 2018 | Not moderate‐to‐severe psoriasis |
| Saeki 2017 | Not a randomised trial |
| Salim 2006 | Other treatment |
| Scholl 1981 | Other treatment |
| Schopf 1998 | Other treatment |
| Schulze 1991 | Other treatment |
| Shintani 2011 | Comparison of 2 schemes of administration |
| Shiohara 1992 | Not a trial |
| Shupack 1997 | Not a trial |
| Simonova 2005 | Other treatment |
| Sinclair 2017 | Pooled trials |
| Sofen 2011 | Basic science (aim of study: to understand the physiopathology of the disease) |
| Sofen 2014 | Phase 1 trial |
| Spadaro 2008 | Not a trial |
| Spuls 2012 | Not a trial |
| Stein Gold 2018 | Not moderate‐to‐severe psoriasis |
| Sticherling 1994 | Not a trial |
| Strober 2004 | Not a trial |
| Strober 2012 | Not a randomised trial |
| Strober 2017a | Pooled trials |
| Strober 2017b | Not moderate‐to‐severe psoriasis |
| Strober 2017c | Ineligible outcomes |
| Strober 2018 | Ineligible study design |
| Sun 2019 | Not psoriasis |
| Sweetser 2006 | Cross‐over trial |
| Syversen 2020 | NCT03074656 ‐ pragmatic trial according to anti TNF dosages |
| Talwar 1992 | Not a randomised trial |
| TCTR20190705002 | Comparison of 2 different schema of administration (same drug same dosage) |
| Tejasvi 2012 | Other treatment |
| Thaçi 2002 | The 2 study arms compared the same molecule with the same dosage |
| Thaçi 2010 | Other treatment |
| Thaçi 2018 | Ineligible outcomes |
| Tong 2008 | Other treatment |
| Tsakok 2018 | Commentary/editorial |
| Vaclavkova 2014 | Another intervention |
| Valenzuela 2017 | Post hoc subgroup analyses of an already included trial |
| Van de Kerkhof 2017 | Post hoc subgroup analyses of an already included trial |
| Van Joost 1988 | Assessment < 8 weeks |
| Vena 2005 | Comparison of 2 schemes of administration |
| Vena 2012 | Other treatment |
| Viglioglia 1978 | Not a trial |
| Witkamp 1995 | Other treatment |
| Wolf 2012 | Other treatment |
| Wright 1966 | Not a randomised trial |
| Wu 2015 | Other treatment |
| Yan 2011 | Another intervention |
| Yesudian 2013 | Other treatment |
| Yoon 2007 | Dose‐escalation study |
| Yosipovitch 2018 | Not moderate‐to‐severe psoriasis |
| Zachariae 2008 | Other treatment |
| Zhang 2007 | Other treatment |
| Zhang 2009a | Other treatment |
| Zhang 2009b | Other treatment |
| Zhu 2009 | Pooled trials |
| Zhuang 2016 | Phase 1 trial |
| Zobel 1987 | Not a trial |
Characteristics of studies awaiting classification [ordered by study ID]
Chow 2015.
| Methods | RCT, active/placebo‐controlled, double‐blind Date of study: not stated Location: Canada, Germany and Poland |
| Participants |
Randomised: 455 participants (mean age 43, 313 male) Inclusion criteria
Exclusion criteria
|
| Interventions |
Interventions (n = 366) Drug: voclosporin 0.8 mg/kg/day Drug: ciclosporin 3.0 mg/kg/day Control intervention (n = 89) Drug: placebo |
| Outcomes |
At week 24, Primary outcome measures
Secondary outcome measures
|
| Notes | Randomised, placebo and ciclosporin controlled study of ISA247 in plaque psoriasis patients (ESSENCE), NCT00408187 Participants in the voclosporin and ciclosporin arms (n = 355) were treated for 24 weeks; these participants were combined into a ‘24‐week treatment group'. In the placebo group, 89 participants were included. As the authors presented their results grouping ciclosporin and voclosporin together, we asked them to provide the results for the subgroup of participants with ciclosporin treatment arm Two emails were sent without response (8 November 2016, 16 December 2016) |
CTRI/2015/05/005830.
| Methods | Randomised, parallel‐group, multiple‐arm trial Date of study: 10 December 2013 (starting date) Location: India |
| Participants |
Total sample size: 120 Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention 1: acitretin: orally, 25 ‐ 50 mg/day, daily single dose Total duration: 90 days Intervention 2: ciclosporin: orally 2.5 ‐ 5 mg/kg/day, daily in 2 divided doses Total duration: 90 days Intervention 3: methotrexate: orally 7.5 ‐ 15 mg/week in 3 divided doses Total duration: 90 days Control Intervention 1: palmoplantar psoriasis: variant of psoriasis in which only palms and soles are affected Control Intervention 2: psoriasis vulgaris: variant of psoriasis in which lesions appear on body skin |
| Outcomes |
At 90 days
|
| Notes | Starting date: 10 December 2013. Recruitment status: open to recruitment (10 January 2020) We sent an email to Prof. Shah (5 and 12 January 2017) without response New email sent to Prof. Kale (11 February 2020) tapdia.raj@gmail.com |
CTRI/2017/09/009850.
| Methods | RCT, active/placebo‐controlled, open‐label Date of study: August 2017 (Starting date) ‐ May 2018 Location: worldwide |
| Participants |
Number of patients : 566 Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention 1: Ixekizumab
160 milligrams (mg) ixekizumab given subcutaneously (SC) at baseline for all participants
80 mg ixekizumab given once every 2 weeks (Q2W) SC from week 2 to week 12 and once every 4 weeks (Q4W) thereafter for participants with moderate‐to‐severe plaque Ps
80 mg ixekizumab given SC Q4W starting week 4 for participants not meeting criteria for moderate‐to‐severe plaque Ps Adalimumab Intervention 2: adalimumab 80 mg given SC at baseline followed by 40 mg Q2W given SC starting week 1 for participants with moderate‐to‐severe plaque Ps 40 mg adalimumab given Q2W SC at baseline followed by 40 mg Q2W starting at Week 2 given SC for participants not meeting criteria for moderate‐to‐severe plaque Ps |
| Outcomes |
Primary outcome :Percentage of participants simultaneously achieving American College of Rheumatology 50 (ACR50) and Psoriasis Area and Severity Index 100 (PASI100) at Week 24 Secondary outcome: ACR50at week 24 PASI 100 at week 24 Change From Baseline in TJC Week 52 Change From Baseline in SJC Week 52 Change From Baseline in Participant's Assessment of Pain VAS Week 52 Change From Baseline in Participant's Global Assessment of Disease Activity Week 52 Change From Baseline in Physician's Global Assessment of Disease Activity Week 52 Change From Baseline in C‐Reactive Protein Week 52 Change From Baseline in HAQ‐DI Week 52 Percentage of participants simultaneously achieving ACR50 and PASI100 Week 52 Change From Baseline in Disease Activity Score‐CRP (DAS28‐CRP) Week 52 Percentage of participants achieving Minimal Disease Activity (MDA) Week 52 Percentage of participants achieving Psoriatic Arthritis Response Criteria (PsARC) Week 52 ] Change From Baseline in Modified Composite Psoriatic Disease Activity Index (CPDAI) Score (Modified) Week 52 Change From Baseline in the Spondyloarthritis Research Consortium of Canada (SPARCC) Enthesitis Index in Participants With Enthesitis Week 52 Change From Baseline in the Leeds Enthesitis Index (LEI) in Participants With Enthesitis at Baseline Week 52 Change From Baseline in the Leeds Dactylitis Index‐Basic (LDI‐B) in Participants With Dactylitis at Baseline Week 52 Change From Baseline in Psoriasis Body Surface Area (BSA) Week 52 Change From Baseline in the Nail Psoriasis Severity Index (NAPSI) Fingernails Score in the Subgroup of Participants With Fingernail Involvement at Baseline Week 52 Change From Baseline in the Itch NRS Week 52 Change From Baseline in Fatigue Severity NRS (Fatigue NRS) Score Week 52 Change From Baseline in Medical Outcomes Study 36‐item Short Form Health Survey (SF‐36): Physical Component Summary (PCS) Week 52 SF‐36 is a standardised participant‐administered measure designed to evaluate 8 domains of functional health and well‐being. Change From Baseline in Measures of Health Utility (EuroQol‐5 Dimensions 5 Level [EQ‐5D 5L]) Week 52 Change From Baseline in Dermatology Life Quality Index (DLQI) Total Score Week 52 Change From Baseline on the Treatment Satisfaction Questionnaire Week 52 Change From Baseline in Columbia Suicide Severity Rating Scale (C‐SSRS) Week 52 |
| Notes |
NCT03151551 Lilly |
DRKS00000716.
| Methods | Randomised, active‐controlled, parallel‐group, simple blind Date of study: 3 June 2008 (starting date) Location: Germany |
| Participants |
Inclusion criteria
Exclusion criteria
|
| Interventions |
|
| Outcomes | Week 8:
PASI
DLQI
Immunhistologie Week 24: PASI DLQI Immunhistologie |
| Notes | Starting date: 03 June 2008, Prof. Arnd Jacobi, Klinik für Dermatologie und Allergologie Philipps‐Universität Marburg Recruitment status on ICTRP search portal: complete: follow‐up complete We emailed Prof. Jacobi (5 January 2017) without response |
EUCTR2010‐020168‐39‐DE.
| Methods | Randomised, placebo‐controlled, parallel‐group, double‐blind Date of study: September 2010 (starting date) Location: Germany |
| Participants |
Total sample size: 252 Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention 1:FP‐187 at a daily dose of 750 mg divided in 3 doses (250mg TID) Intervention 2: FP‐187 at a daily dose of 750 mg divided in 2 doses (375mg BID) Intervention 3: FP‐187 at a daily dose of 500 mg divided in 2 doses (250mg BID) Intervention 4: Placebo |
| Outcomes |
Primary outcome:
Secondary outcome
|
| Notes | Study completion date on ClinicalTrials.gov MAY 2012 NCT01230138 |
EUCTR2015‐005279‐25‐DE.
| Methods | Randomised, placebo‐controlled, parallel‐group, double‐blind Date of study: September 2016 (starting date) Location: Germany |
| Participants |
Total sample size: 36 Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention 1: LEO 32731 30 mg twice a day for 16 weeks Intervention 2: placebo |
| Outcomes |
Primary outcome
Secondary outcome
|
| Notes | Study completion date on ClinicalTrials.gov July 2017 NCT02888236 |
EUCTR2017‐001615‐36‐DE.
| Methods | Randomised, placebo‐controlled, parallel‐group, double‐blind Date of study: March 2018 (starting date) Location: Germany |
| Participants |
Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention 1: 2 mg ABY‐035 SC 12 weeks Intervention 2: 20 mg ABY‐035 SC 12 weeks Intervention 3: 80 mg ABY‐035 SC 12 weeks Intervention 4: 160 mg ABY‐035 SC 12 weeks Intervention 5: Placebo 12 weeks After the first 12 weeks of treatment, the participants randomised to placebo will receive active treatment. The dose levels and dosing intervals are adjusted depending on the absolute PASI score, to obtain an individualised treatment regimen |
| Outcomes |
Primary outcome
Secondary outcome measures
|
| Notes |
NCT03591887 Contact: sgerdes@dermatology.uni‐kiel.de Sascha Gerdes, Dr. med |
Goldust 2019.
| Methods | Randomised controlled clinical trial study, 4 were randomly assigned to receive combination therapy (efficacy assessments were performed) |
| Participants | 48 patients with moderate‐to‐severe plaque psoriasis |
| Interventions | In this 24‐week study, intervention 1: adalimumab sc 80 mg at weeks 1 and 2 then 40 mg every 2 weeks intervention 2: no intervention or placebo ?? Co‐intervention: methotrexate 15 – 20 mg a week or methotrexate monotherapy |
| Outcomes | PASI Hospital Anxiety and Depression scale |
| Notes | ABSTRACT |
Han 2007.
| Methods | Randomised, double‐blind, active‐controlled trial Date: not stated Location: China |
| Participants | No statement except a total number of participants (n = 144) |
| Interventions |
Intervention Recombinant human tumour necrosis factor receptor (50 mg/week) Control intervention Methotrexate (7.5 mg/week) |
| Outcomes |
At 12 weeks Proportion of PASI 50, PASI 75, PASI 90 |
| Notes |
Abstract in Journal of Clinical Dermatology 2007 (730‐2) HAN Ling, FANG Xu, HUANG Qiong, YANG Qin‐ping, FU Wen‐wen, ZHENG Zhi‐zhong, GU Jun, SUN Jiao‐fang, XU Ai‐e (Department of Dermatology,Huashan Hospital, Fudan University, Shanghai 200040, China) Objective: To evaluate the effect of recombinant human tumour necrosis factor receptor (rhTNFR:Fc) in the treatment of moderate to severe plaque psoriasis on psoriasis area and severity index (PASI). Methods: Using randomised, double‐blind and double‐simulated, parallel‐controlled with positive drug, multicenter, clinical trial was employed to investigate 144 cases of patients with moderate to severe plaque psoriasis, of which there were 72 cases in both trial group and the control group respectively, to evaluate the effect on PASI. Results: 124 cases of patients had accomplished the 12‐week clinical trial. After 12 weeks the rate of PASI50, PASI75, PASI90 were significantly higher than those of the control group (P < 0.01). The therapeutic effects on trunk and limbs of the trial group were also much better. Conclusion: The effect of rhTNFR:Fc is more quick and significant, especially assessed by PASI sore. Abstract not available at the BIUM and United States NLM libraries. No email address for the authors available When we searched Google, we found another abstract of the same study. "Chinese Journal of Dermatology 2007, 40(11) 655‐658" manu41.magtech.com.cn/Jwk_cmazp/EN/abstract/abstract11844.shtml#), which had no supplemental information to enable contacting the authors: Abstract "Objective To investigate the efficacy and tolerability of a recombinant human tumour necrosis factor:Fc fusion protein (rhTNFR:Fc,with a trade name of Yisaipu) in the treatment of moderate to severe psoriasis vulgaris. Methods A multicentre,randomised,double blind,and parallel‐controlled trial was performed. One hundred and forty‐four patients with moderate to severe psoriasis vulgaris from four centres were randomly assigned and treated with either once‐weekly subcutaneous injection of rhTNFR:Fc (50 mg) or oral methotrexate (methotrexate)(7.5 mg) for 12 weeks.Patients were followed up at 2,4,8,12 weeks after the treatment. Results One hundred and twenty‐four patients finished the 12‐week course of treatment. At 12 weeks after the treatment,a 50%, 75%, 90% improvement in psoriasis area and severity index (PASI) was achieved by 86.11%, 76.39%, 52.78% respectively of rhTNFR:Fc‐treated patients,and by 63.89%, 44.44%, 22.22% respectively in methotrexate‐treated patients,and all the three improvement rates were of significant difference between the two groups of patients (all P<0.01).Physician global assessment (PGA), dermatology life quality index (DLQI) and 10‐cm visual analogue scale (VAS) all reduced more significantly, and more patients were cured or approximately cured in rhTNFR:Fc‐treated patients than in MTX‐treated patients (all P<0.05).Adverse reactions,mainly including decrease of leucocytes or neutrophils,infection, dysfunction of liver, edema and pruritus at the injection site,etc,occurred in 26.39% of rhTNFR:Fc‐treated patients and 29.17% of MTX‐treated patients (P>0.05). Conclusion Compared with MTX,rhTNFR:Fc acts more quickly with a higher cure rate and less toxic reactions in the treatment of psoriasis vulgaris." No contact with the authors, as we could not find the authors' emails |
Ikonomidis 2019.
| Methods | Effects of treatment with biological agents on vascular and cardiac function in psoriasis Phase 4, RCT, parallel arms, investigator‐blind Monocentric: Attikon Hospital, Athens Starting date: May 2014 |
| Participants | Randomised: 200
Incusion criteria
Exclusion criteria:
|
| Interventions | Intervention 1: Etanercept 50 mg Intervention 2: Ustekinumab 45 mg Intervention 3: Cyclosporine 2.5 ‐ 3 mg/kg Intervention 4: Secukinumab 300 mg Intervention 5: Apremilast 30 mg |
| Outcomes |
Primary outcome:
Secondary outcome:
|
| Notes |
NCT02144857 Contact: Ignatios Ikonomidis, Dr2105831264ignoik@gmail.com Contact: Maria Varoudi, Dr6909001116mvaroudi@gmail.com |
Krishna 2016.
| Methods | RCT, active‐controlled, double‐blind trial, phase 3 Date of study: November 2013 ‐ January 2015 Location: India |
| Participants |
Randomised: 50 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention Methotrexate 10 mg/week Control intervention Methotrexate 25 mg/week |
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
| Notes | On ClinicalTrials.gov (NCT02248792) Recruitment Status: Unknown Verified September 2014 by C V Krishna, Narayana Medical College & Hospital. Recruitment status was: Recruiting Estimated Enrolment: 50 Study start date: November 2013 Estimated primary completion date: January 2015 (final data collection date for primary outcome measure) Emails sent to Prof. Krishna (5 and 12 January 2017; 11 February 2020) |
Makavos 2020.
| Methods | RCT, active‐controlled, open trial Date of study: not stated Setting: not stated |
| Participants |
Randomised: 150 participants, mean age 52; 92 men Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
| Interventions |
Intervention A. Secukinumab, 300 mg SC, W0, 1, 2, 3, 4 and 300 mg once monthly Control intervention B. Ciclosporin, 2.5 to 3 mg/Kg daily C. Methotrexate (non‐randomised controlled group, n = 50) |
| Outcomes | Assessments at 16 weeks Primary outcome
Secondary outcomes
|
| Notes | Authors were asked whether ‐ methotrexate group was randomised or not ‐ Included patients were moderate‐to‐severe psoriasis ‐ randomisation was stratified according psoriatic arthritis or not ‐ subgroup results for plaques psoriasis for our outcomes |
Mrowietz 2005.
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: not stated Setting: not stated |
| Participants |
Randomised: 175 participants (characteristics not stated) Inclusion criteria
Exclusion criteria
Dropouts and withdrawals
|
| Interventions |
Intervention A. Dimethyl fumarate (n = 105), orally, 240 mg, 3 times/day; 16 weeks Control Intervention B. Placebo (n = 70), orally, 2 capsules, 3 times/day; 16 weeks |
| Outcomes | Assessments at 16 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
| Notes | Funding, quote (abstract) by Biogen Idec, Inc and Fumapharm Abstracts: “Results of a phase III study of a novel oral formulation of dimethyl fumarate in the treatment of moderate to severe plaque psoriasis: efficacy, safety, and quality of life effects” published in 2005 in the JEADV, Suppl. 2 (Poster P/06.97) We asked the study authors to provide the protocol and results by email. Additional data to the publication not provided Finally, as the 'Risk of bias' tool assessment was not possible and there were missing data for the results, Mrowietz 2005 was included in Studies awaiting classification |
NCT01088165.
| Methods | RCT, active‐controlled, triple‐blind trial Date of study: May 2010 ‐ Setting: Austria |
| Participants |
Randomised: 66 participants (characteristics not stated) Inclusion criteria
Non‐response or contraindication to previous systemic and/or light treatment
Exclusion criteria
Dropouts and withdrawals
|
| Interventions |
Intervention A. Adalimumab treatment arm: day 1: 2 x 40 mg SC, day 8: 40 mg SC., thereafter 40 mg SC at bi‐weekly intervals Control Intervention B. Fumaric acid esters treatment group C. Narrow‐band UVB radiation |
| Outcomes | Assessments at 12 weeks Primary outcomes of the trial
Secondary outcomes of the trial
|
| Notes | Funding, quote (ClinicalTrials.gov, NCT01088165) by Medical University of Vienna Recruitment Status: Unknown Verified January 2012 by Gregor Holzer, Medical University of Vienna. We sent an email to Prof. Holzer to be sure this trial is still ongoing (3 June 2019 and 11 February 2020) without response |
NCT01558310.
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: March 2012 Location: USA Phase 4 |
| Participants |
Randomised: 30 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention Ustekinumab (at weeks 0, 4, 16, 28, and week 40 and placebo at weeks 12 and 52. The participants when assigned to ustekinumab, depending on body weight, will receive either 45 mg or 9 mg ustekinumab doses) Control intervention Placebo |
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
| Notes | On ClinicalTrials.gov Estimated enrolment: 30 We emailed Dr Yamauchi (5 and 12 January 2017) Email response: Dear Dr Sbidian, Thank you for your kind email, forwarded to me by Dr Paul Yamauchi, MD,PhD. Our " Study to Evaluate the Effectiveness of STELARA ™ (USTEKINUMAB) in the Treatment of Scalp Psoriasis (NCT 01558310)” completed enrolment in December 2016 and the last subject will complete in December 2017, as such we do not have the final data analysis. What is you absolute cut‐ off for publication data ? Would an interim analysis report be acceptable? Best regards, Rickie Patnaik Director, Clinical Science Institute Will be included when published |
NCT02655705.
| Methods | RCT, placebo‐controlled, open‐label study Date of study: September 2015 ‐ Location: Korea Phase 4 |
| Participants | Inclusion Criteria:
Exclusion Criteria:
|
| Interventions |
Intervention Ciclosporin A (men 200 mg/day, women 150 mg/day for 16 weeks) Control intervention Methotrexate (initial dose 10 mg/week, increasing 2.5 mg every 2 weeks up to 15 mg/week) |
| Outcomes |
At week 16 Primary outcome
Secondary outcome
|
| Notes | Published articles without outcomes of interest Emails sent to Pr Sang Woong Youn, Seoul National University Hospital (3 June 2019 and 11 February 2020) |
NCT02714322.
| Methods | RCT, active‐controlled, double‐blind study Date of study: June 2015 Location: Russia, Estonia, Hungary, Poland, Bulgaria |
| Participants |
Randomised: 294 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Biological: MYL‐1401A (Adalimumab) MYL‐1401A initial dose of 80 mg administered SC, followed by 40 mg SC given every other week starting 1 week after the initial dose Control intervention B. Humira® (Adalimumab) Humira® initial dose of 80 mg administered SC, followed by 40 mg SC given every other week starting 1 week after the initial dose |
| Outcomes |
At week 12 Primary outcome
Secondary outcomes Proportion of participants showing at least a 75% improvement in PASI (PASI 75 response rate) (Time frame: week 12) |
| Notes | No principal investigator stated on ClinicalTrials.gov; waiting for results publication |
NCT02762994.
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: June 2016 Location: Russia Phase 2 |
| Participants |
Randomised: 120 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. BCD‐085, 40 mg: Participant will receive 40 mg of BCD‐085 subcutaneously at weeks 0, 1, 2, 4, 6, 8, 10 Control interventions B. BCD‐085, 80 mg: Participant will receive 80 mg of BCD‐085 subcutaneously at weeks 0, 1, 2, 4, 6, 8, 10 C. BCD‐085, 120 mg: Participant will receive 80 mg of BCD‐085 subcutaneously at weeks 0, 1, 2, 4, 6, 8, 10 D. Placebo |
| Outcomes |
At week 12 Primary outcome
Secondary outcome
|
| Notes | Results submitted to ClinicalTrials.gov: July 2020 Sponsor: Biocad Ongoing study Last checked in September 2020 |
NCT02982005.
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: January 2017 Location: Korea Phase 3 |
| Participants |
Randomised: 62 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention KHK4827 (SC, dosage not stated) Control intervention Placebo |
| Outcomes |
At week 12 Primary composite outcome
Secondary outcomes
|
| Notes | Ongoing study Last checked in September 2020 |
NCT03025542.
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: December 2016 Location: USA, Australia, Canada Phase 2 |
| Participants |
Randomised: 49 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Bimekizumab Control interventions B. Placebo |
| Outcomes |
At week 16 Primary composite outcome Change from baseline in PASI at week 28 (Time frame: week 28) |
| Notes | Ongoing study Last checked in September 2020 |
NCT03210259.
| Methods | RCT, active‐controlled, double‐blind study Date of study: July 2017 Location: world‐wide Phase 3 |
| Participants |
Randomised: 259 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention BI 695501 Control interventions Humira® |
| Outcomes |
At week 30 Primary composite outcome
|
| Notes | Ongoing study Last checked in September 2020 |
NCT03364309.
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: 26 April 2018 Location: China Phase 3 |
| Participants |
Randomised: 438 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Ixekizumab dose schedule 1: Ixekizumab given SC Control interventions B. Ixekizumab dose schedule 2: Ixekizumab given SC C. Placebo |
| Outcomes |
At week 12 Primary composite outcome PGA0/1 ‐ PASI 75 Secondary outcome PASI 90, PASI 100 BSA SF‐36 DLQI |
| Notes | Ongoing study Last checked in September 2020 |
NCT03370133.
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: December 2017 Location: worldwide Phase 3 |
| Participants |
Randomised: 570 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Bimekizumab Control interventions B. Ustekinumab C. Placebo |
| Outcomes |
At week 16 Primary composite outcome PASI 90 ‐ IGA 0/1 Secondary outcome PASI 75 AE, SAE |
| Notes | Ongoing study Last checked in September 2020 |
NCT03412747.
| Methods | RCT, active‐controlled, double‐blind study Date of study: January 2018 Location: worldwide Phase 3 |
| Participants |
Randomised: 480 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Bimekizumab dose regimen 1 Control interventions B. Bimekizumab dose regimen 2 C. Adalimumab |
| Outcomes |
At week 16 Primary composite outcome PASI 90 ‐ IGA 0/1 Secondary outcome PASI 75 PASI 100 AEs SAEs |
| Notes | Ongoing study Last checked in September 2020 |
NCT03518047.
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: July 2018 Location: Russia Phase 3 |
| Participants |
Randomised: 50 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Risankizumab Control interventions B. Placebo |
| Outcomes |
At week 16 Primary outcome PASI 90 Secondary outcome PGA 0/1 PASI 75 PASI 100 DLQI |
| Notes | Ongoing study Last checked in September 2020 |
NCT03589885.
| Methods | RCT, active‐controlled, double‐blind study Date of study: December 2018 Location: USA, Germany, Spain, Iceland, Poland Phase IIIB |
| Participants |
Randomised: 122 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Secukinumab 2 mL auto‐injector Control interventions B. Secukinumab 1 mL pre‐filled syringe C. Placebo |
| Outcomes |
At week 12 Primary composite outcome PASI 75 ‐ IGA 0/1 Secondary outcome PASI 90 DLQI |
| Notes | Ongoing study Last checked in September 2020 |
NCT03875482.
| Methods | RCT, active/placebo‐controlled, double‐blind trial, multicentric Date of study: May 2019 Location: USA Phase 3 |
| Participants |
Randomized : 157 Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention: Risankizumab Comparator: Placebo |
| Outcomes |
Primary outcome :
Percentage of participants achieving PASI 90 at week 16
Percentage of participants achieving sPGA of clear or almost clear at week 16 Secondary outcomes: Percentage of participants achieving PASI 100 at week 16 Percentage of participants achieving sPGA of clear at week 16 |
| Notes | Funding Abbvie Last checked in September 2020 |
NCT04488185.
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: June 2020 Location: unknown |
| Participants |
Inclusion criteria: Clinical diagnosis of chronic plaque‐type psoriasis confirmed through physical examination by a dermatologist, with at least 6 months of clinical history prior to the baseline visit Moderate‐to‐severe plaque psoriasis at baseline, defined as:
Candidate for systemic therapy, defined as having psoriasis inadequately controlled by current topical and/or systemic treatment(s) (including topical corticosteroids), phototherapy, or previous systemic therapies Presence of sonographic enthesitis at screening, in at least 1 enthesis, defined by the presence of at least abnormal thickening and hypoechogenicity of the tendon insertion, with or without presence of Doppler signal (Grade 0 ‐ 3), or by the presence of grade ≥ 2 Doppler signal, independent of gray scale abnormalities Exclusion criteria:
|
| Interventions |
Intervention A. Secukinumab 300 mg administered SC (2 single‐use prefilled syringes of 150 mg/mL), on Days 1, 8, 15, 22, 29, 57, 85. Control intervention B. Placebo |
| Outcomes |
At week 16 Primary outcome
Secondary outcome
|
| Notes | Waiting for subgroup analyses for participants with moderate‐to‐severe psoriasis |
AEs: adverse effects; BMI: body mass index; BSA: body surface area;DLQI: Dermatology Life Quality Index; ECG: electrocardiogram; eow: every other week; FAEs: fumaric acid esters; IGA: Investigator's Global Assessment; IM: intramuscular; IV: intravenous; NAPSI: Nail Psoriasis Severity Index; PASI: Psoriasis Area and Severity Index; PGA: Physician's Global Assessment; PUVA: psoralen plus ultraviolet A; RCT: randomised controlled trial; SC: subcutaneous; SF36: short‐form 36; SPGA: static physician global assessment; TB: tuberculosis; UVB: ultraviolet B; VAS: visual analogue scale Please note that the term “conventional” in these tables is replaced with “non‐biological treatment” in the main text of this review.
Characteristics of ongoing studies [ordered by study ID]
CTRI/2016/10/007345.
| Study name | A randomised, double‐blind, placebo‐controlled, comparative, prospective, multicentre trial to assess efficacy and safety of apremilast tablets in subjects with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy |
| Methods | Phase 3 RCT, placebo‐controlled, double‐blind trial Date of study: October 2016 Location: India |
| Participants |
Randomised: 231 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention Apremilast 30 mg tablets: administered 1 tablet twice daily for 16 weeks Control intervention Placebo tablets: administered 1 tablet twice daily for 16 weeks |
| Outcomes |
At week 16 Primary outcome
Secondary outcomes
|
| Starting date | 20 October 2016 |
| Contact information | Dr Piyush Agarwal, DrPiyush.Agarwal@glenmarkpharma.com |
| Notes | Ongoing study Last checked in April 2019, 7 September 2020 |
CTRI/2019/01/017362.
| Study name | A study to assess the effects of Apremilast and Methotrexate in the treatment of patients with psoriasis |
| Methods | Open‐labelled randomised India |
| Participants |
Randomised: 40 Inclusion criteria:
Exclusion criteria:
|
| Interventions | apremilast methotrexate |
| Outcomes |
Primary Outcome PASI 75 week 12 Secondary outcome Improvement in PASI at week 3 and week 9 |
| Starting date | 04 February 2019 |
| Contact information | Dr RATHIPRIYADHARSHINI RDepartment of Dermatology, Chettinad hospital and Research Institute, Rajiv Gandhi Salai, Kelambakkam No.7E,Kulaal street,Pattukkottai, Thanjavur dt‐614601 Kancheepuram TAMIL NADU 603103 India rathiii5893@gmail.com |
| Notes | Protocol article present: An open‐labelled randomised comparative evaluation of therapeutic efficacy and safety of Apremilast versus Methotrexate in the treatment of patients with chronic plaque psoriasis. Rathipriyadharshini R 2020 |
CTRI/2019/07/020274.
| Study name | Comparative efficacy of methotrexate, apremilast and their combination in psoriasis vulgaris |
| Methods | Randomised, parallel‐group, multiple arm trial India |
| Participants | Randomised: 30 Inclusion criteria:
Exclusion criteria
|
| Interventions |
Intervention 1: Apremilast 30 mg twice a day, starting at 10 mg/day with an increment of 10 mg/day over 5 days, for 8 weeks Intervention 2: Oral methotrexate 0.2 mg/kg/week, maximum 25 mg/week for 8 weeks Intervention 3: Oral methotrexate 0.2 mg/kg/week, maximum 25 mg/week along with oral apremilast 30 mg twice a day, starting at 10 mg/day with an increment of 10 mg/day over 5 days, for 8 weeks |
| Outcomes |
Primary outcome: To compare the efficacy of apremilast and methotrexate and their combination in patients with psoriasis vulgaris by comparing the PASI score before and after start of the therapy. 0,2,4,6,8 weeks. Secondary outcome: To assess the safety of all the three treatment modalities by assessing the side effects. 0,2,4,6,8 weeks |
| Starting date | 22 July 2019 |
| Contact information | Dr Nainika Goel Government Medical College and Hospital, Chandigarh
Address Department of dermatology, D block, 5th floor, GMCH, sector 32, Chandigarh
Chandigarh
CHANDIGARH
160030 dr.nainika1311@gmail.com |
| Notes | Last checked on 7 September 2020, not yet recruiting |
EUCTR2013‐004918‐18‐NL.
| Study name | Optimising adalimumab treatment in psoriasis with concomitant methotrexate ‐ OPTIMAP |
| Methods | Phase 4 RCT, placebo‐controlled, open‐label trial Date of study: February 2014 Location: The Netherlands |
| Participants |
Randomised: number of participants not stated Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention Adalimumab with methotrexate Control intervention Adalimumab monotherapy Dosage and frequency of adalimumab and methotrexate: not stated |
| Outcomes |
Primary end point(s)
Timepoint(s) of evaluation of this endpoint: week 49 Secondary end point(s)
Time point(s) of evaluation of this endpoint: week 13, 25, 37 and 49 |
| Starting date | 12 December 2013 |
| Contact information | Prof Phyllis Spuls Department of Dermatology Academic Medical Center Meibergdreef 9 1105AZ Amsterdam, Netherlands |
| Notes | Recruitment status (ICTRP search portal): authorised recruitment may be ongoing or finished Target sample: not specified We emailed Prof. Phyllis Spuls (5 January 2017) Email response "The study is currently ongoing and has not yet been analysed. Therefore, we are not able to provide data on efficacy or safety. We can provide you with the study protocol. Will this be helpful? Kind regards, Phyllis Spuls and Celine Busard " Will be included when published |
EUCTR2017‐003367‐35‐PL.
| Study name | Efficacy, safety, and immunogenicity of AVT02 with moderate‐to‐severe chronic plaque psoriasis |
| Methods | Phase 3 RCT, active‐controlled, double‐blind Date of study: February 2019 Location: Poland, Estonia, Georgia, Ukraine |
| Participants |
Randomised: 413 Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention AVT02 (adalimumab biosimilar) 80 mg (2 × 40 mg) administered subcutaneously (SC), followed by 40 mg given SC once every other week (EOW) until week 48 Control intervention Humira 80 mg (2 × 40 mg) administered SC, followed by 40 mg given SC EOW until week 48 |
| Outcomes | Primary outcome measures : Psoriasis Area and Severity Index (PASI) [ Time Frame: baseline to week 16 ] Percent (%) change in PASI Secondary outcome measures: PASI [ Time frame: Percent improvement in PASI from BL to week 8, 12, 24, 32, 42, and 50 ] Percent (%) change in PASI |
| Starting date | Study start date: February 2019 Actual study completion date: July 2020 Last update posted: July 2020, completed |
| Contact information | Investigator: Steve Feldman, MD PhD, Wake Forest University Health Sciences |
| Notes | NCT03849404 funding: Alvotech Swiss AG (Alvotech) |
EUCTR2018‐001238‐16‐FR.
| Study name | A study to evaluate further therapeutic strategies with guselkumab in participants with moderate‐to‐severe plaque‐type psoriasis (GUIDE) |
| Methods | Phase 3b RCT, double‐blind, parallel‐group, multicentre study Date of study: February 2019 Location: France, Germany |
| Participants |
Randomised: 888 participants Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention: Guselkumab 100 mg guselkumab subcutaneously at weeks 0, 4, 12 and 20 Control intervention: placebo then re‐randomisation |
| Outcomes |
Primary outcome:
Secondary outcome:
|
| Starting date | Study start date: February 2019 Estimated study completion date: October 2023 Last update posted: September 2, 2020, recruiting |
| Contact information | |
| Notes |
NCT03818035 Funding Jansssen‐Cilag Germany JNJ.CT@sylogent.com |
EUCTR2018‐001926‐25‐ES.
| Study name | An investigational study to evaluate experimental medication BMS‐986165 compared to placebo and a currently available treatment in participants with moderate to severe plaque psoriasis (POETYK‐PSO‐1) |
| Methods | Phase 3b RCT, double‐blind, parallel group, placebo and active comparator, multicentre study Date of study: August 2018 Location: Wordwide |
| Participants |
Randomised: 600 Inclusion criteria: Plaque psoriasis for at least 6 months Moderate‐to‐severe disease Candidate for phototherapy or systemic therapy Exclusion criteria: Other forms of psoriasis History of recent infection Prior exposure to BMS‐986165 or active comparator |
| Interventions |
Intervention BMS‐986165 Comparator 1 Apremilast Comparator 2 Placebo |
| Outcomes |
Primary outcome:
Secondary outcomes :
|
| Starting date | Study start date: August 2018 Estimated study completion date: August 2020 Last update posted: August 2020, active, not recruiting |
| Contact information | |
| Notes | NCT03624127‐ funding Bristol Myers Squibb |
NCT02258282.
| Study name | Safety and efficacy of etanercept in patients with psoriasis |
| Methods | RCT, placebo‐controlled, double‐blind trial Date of study: May 2014 Location: China Phase 4 |
| Participants |
Randomised: 80 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention Etanercept (participants under the treatment of 50 mg etanercept) Control intervention Placebo |
| Outcomes |
At week 24 Primary outcome
Secondary outcomes
|
| Starting date | Study start date: May 2014 Estimated primary completion date: December 2022 Last update posted: April 2017, active, not recruiting |
| Contact information | Yang Min, Ph.D, Chengdu PLA General Hospital |
| Notes | On ClinicalTrials.gov Ongoing study |
NCT02325219.
| Study name | An efficacy and safety of CNTO 1959 (guselkumab) in participants with moderate to severe plaque‐type psoriasis |
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: December 2014 Location: Japan Phase 3 |
| Participants |
Randomised: 192 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention CNTO 1959 50 mg (50 mg at weeks 0, 4 and then every 8 weeks thereafter) Control interventions CTNO 1959 100 mg (100 mg at weeks 0, 4 and then every 8 weeks thereafter) Placebo |
| Outcomes |
At week 16 Primary composite outcome
Secondary outcomes
|
| Starting date | Study start date: December 2014 Study final completion date: 8 February 2019 Last update posted: May 2020 |
| Contact information | Janssen Pharmaceutical K.K. |
| Notes | Guselkumab, an anti‐interleukin‐23 monoclonal antibody, for the treatment of moderate to severe plaque‐type psoriasis in Japanese patients: Efficacy and safety results from a phase3, randomised, double‐blind, placebo‐controlled study, Mamitaro OHTSUKI 2018 Ongoing study Last checked in September 2020 |
NCT02701205.
| Study name | Safety and efficacy study of etanercept (Qiangke®) to treat moderate to severe plaque psoriasis |
| Methods | RCT, placebo and active‐controlled, double‐blind study Date of study: January 2015 ‐ Location: China |
| Participants |
Randomised: 216 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Recombinant Human TNF Receptor‐Ig Fusion Protein for Injection 50 mg twice a week by subcutaneous injection for 12 weeks. At the end of the first 12 weeks, all subjects will be treated with Recombinant Human TNF Receptor‐Ig Fusion Protein for Injection 50 mg once a week for an additional 12 weeks Control intervention B. Recombinant Human TNF Receptor‐Ig Fusion Protein for Injection 25mg twice a week by subcutaneous injection for 12 weeks, At the end of the first 12 weeks, all participants will be treated with Recombinant Human TNF Receptor‐Ig Fusion Protein for Injection 50 mg once a week for an additional 12 weeks C. Placebo |
| Outcomes |
At week 12 Primary outcome
Secondary outcomes
|
| Starting date | Study start date: January 2015 Estimated study completion date: December 2017 Last update posted: March 2016, unknown |
| Contact information | Contact: Hongzhong Jin, M.D.; jinhongzhong@263.net |
| Notes | Ongoing study Emails sent to Prof Hongzhong Jin (3 June 2019 and 11 February 2020 (not delivered)) |
NCT02762955.
| Study name | Comparative clinical trial of efficacy and safety of BCD‐057 and Humira® in patients with moderate to severe plaque psoriasis (CALYPSO) |
| Methods | RCT, active‐controlled, double‐blind study Date of study: December 2016 Location: Russia |
| Participants |
Randomised: 344 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention
BCD‐057 group includes participants with moderate‐to‐severe plaque psoriasis, who will receive BCD‐057 SC at a dose 80 mg on week 0, then at a dose 40 mg on weeks 1, 3, 5, 7, 9, 11, 13, 15, 17, 19, 21 and 23 Control interventions Humira® group includes participants with moderate‐to‐severe plaque psoriasis, who will receive Humira® SC at a dose 80 mg on week 0, then at a dose 40 mg on weeks 1, 3, 5, 7, 9, 11, 13, 15, 17, 19, 21, 23 |
| Outcomes |
At week 16 Primary outcome
Secondary outcome
|
| Starting date | Study start date: December 2016 Estimated study completion date: December 2018 Last update posted: March 2018, unknown |
| Contact information | Study Chair: Roman Ivanov, PhD, JCS BIOCAD |
| Notes | Ongoing study |
NCT02829424.
| Study name | Multicenter randomised double‐blind controlled‐study to assess the potential of methotrexate versus placebo to improve and maintain response to anti TNF‐ alpha agents in adult patients with moderate to severe psoriasis (METHOBIO) |
| Methods | RCT, active‐controlled, double‐blind study Date of study: April 2016 Location: France Phase 4 |
| Participants |
Randomised: 330 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Methotrexate (low dose) Control interventions B. Placebo Co‐intervention: anti‐TNF agent |
| Outcomes |
At week 24 Primary outcome Loss of PASI 75 Secondary outcome PASI 75 PASI 50 Maintenance of response rates proportion DLQI |
| Starting date | Study start date: April 2016 Estimated study completion date: October 2020 Last update posted: July 2016, recruiting |
| Contact information | Prof MA Richard: mrichard@ap‐hm.fr |
| Notes | Ongoing study Last checked in September 2020 |
NCT03384745.
| Study name | A Phase 2b Study of the Efficacy, Safety, and Tolerability of M1095 in Subjects With Moderate to Severe Psoriasis |
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: July 2018 Location: worldwide Phase 2b |
| Participants |
Randomised: 300 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. M1095, 30 mg, given at week 0, 2, 4, 8, 12 and every four weeks. Control interventions B. M1095, 60 mg, given at week 0, 2, 4, 8, 12 and every four weeks. C. M1095, 120 mg, given at week 0, 2, 4, 8, 12 and every eight weeks. D. M1095, 120 mg, given at week 0, 2, 4, 8, 12 and every four weeks. E. Placebo |
| Outcomes |
At week 12 Primary outcome IGA 0/1 Secondary outcomes PASI 75 PASI 100 |
| Starting date | Study start date: July 2018 Estimated Study completion date: August 2020 Last Update Posted: January 2020, active, not recruiting |
| Contact information | Principal investigator: Dr Kim Papp Contact: Dr Mark Weinberg +44 (0)203 764 9530 mark@avillionllp.com |
| Notes | Sponsor: Bond Avillion 2 Development LP Ongoing study Last checked in September 2020 |
NCT03410992.
| Study name | A Study With a Initial Treatment Period Followed by a Randomized‐withdrawal Period to Evaluate the Efficacy and Safety of Bimekizumab in Adult Subjects With Moderate to Severe Chronic Plaque Psoriasis (BE READY) |
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: February 2018 Location: worldwide Phase 3 |
| Participants |
Randomised: 435 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Bimekizumab Control interventions B. Placebo |
| Outcomes |
At week 16 Primary composite outcome PASI 90 ‐IGA 0/1 Secondary outcomes PASI 100, PASI 75 AEs, SAEs |
| Starting date | Study start date: February 2018 Estimated Study completion date: January 2020 Last Update Posted: January 27, 2020, active, not recruiting |
| Contact information | Study director: UCB cares +1 844 599 2273 (UCB) |
| Notes | Ongoing study Last checked in September 2020 |
NCT03421197.
| Study name | A study to assess the efficacy and safety of PPC‐06 (Tepilamide Fumarate) |
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: January 2018 Location: USA Phase 2 |
| Participants |
Randomised: 400 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Tepilamide fumarate 400 mg tablet once a day Control interventions B. Tepilamide fumarate 400 mg tablet twice a day C. Tepilamide fumarate tablets 600 mg twice a day D. Placebo |
| Outcomes |
At week 24 Primary composite outcome PASI 75 and IGA 0/1 Secondary outcome PASI 50, PASI 75 IGA BSA |
| Starting date | Study start date: January 2018 Estimated study completion date: March 2020 Last update posted: March 2020, active not recruiting |
| Contact information | Dr. Reddy's Laboratories Limited Study director: Srinivas Sidgiddi, MD |
| Notes | Ongoing study Last checked in September 2020 |
NCT03478280.
| Study name | Effect of brodalumab compared to placebo on vascular inflammation in moderate‐to‐severe psoriasis |
| Methods | RCT, placebo‐controlled, double‐blind study Date of study: September 2018 Location: Aarhus University Hospital, Denmark Phase 4 |
| Participants |
Randomised: 50 participants Inclusion criteria
Exclusion criteria Non‐Danish speaking |
| Interventions |
Intervention A. Participants will receive 210 mg of Kyntheum administered by subcutaneous injection at weeks 0, 1 and 2 followed by 210 mg every other week (EOW) thereafter Control interventions B. Placebo |
| Outcomes |
At week 16 Primary outcome Average of maximum TBR values (MeanTBRmax) of the entire aorta at baseline and at week 16 (aortic wall inflammation) Secondary outcome The splenic inflammation at baseline and at week 16 in brodalumab‐treated psoriasis participants compared to placebo. (Time frame: 16 weeks); the spleen‐to‐liver ratio (SLR) based on splenic and liver mean standardised uptake values (SUVmean) |
| Starting date | Study start date: September 2018 Estimated study completion date: March 2020 Last update posted: July 2019, Recruiting |
| Contact information | Contact: Anne Bregnhøj, MD, PhD +45 2183 5720 annebreg@rm.dk |
| Notes | Ongoing study Last checked in September 2020 |
NCT03504852.
| Study name | Efficacy and safety of 2 secukinumab regimens in 90 kg or higher subjects with moderate to severe chronic plaque‐type psoriasis |
| Methods | RCT, active‐controlled, double‐blind study Date of study: June 2018 Location: world‐wide Phase 3 |
| Participants |
Randomised: 331 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Secukinumab 300 mg every 2 weeks Control interventions B. Secukinumab 300 mg every 4 weeks |
| Outcomes |
At week 16 Primary outcome PASI 90 Secondary outcome IGA 0/1 |
| Starting date | Study start date: June 2018 Estimated study completion date: July 2020 Last update posted: July 2020, active, not recruiting |
| Contact information | Study Director: Novartis Pharmaceuticals |
| Notes | Ongoing study Last checked in September 2020 |
NCT03535194.
| Study name | A study to assess if mirikizumab is effective and safe compared to secukinumab and placebo in moderate‐to‐severe plaque psoriasis (OASIS‐2) |
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: May 2018 Location: world‐wide Phase 3 |
| Participants |
Randomised: 1484 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Mirikizumab Control interventions B. Secukinumab C. Placebo |
| Outcomes |
At week 16 Primary composite outcome PASI 90 ‐ IGA 0/1 Secondary outcome PASI 75 DLQI SF‐36 Change from baseline in quick inventory of depressive symptomology |
| Starting date | Study start date: May 2018 Actual study completion date: May 2020 Last update posted: August 2020, active, recruiting |
| Contact information | Study Director: call 1‐877‐CTLILLY (1‐877‐285‐4559) |
| Notes | Sponsor: Eli Lilly and Company Ongoing study Last checked in September 2020 |
NCT03536884.
| Study name | A study to evaluate the efficacy and safety of bimekizumab compared to an active comparator in adult subjects with moderate to severe chronic plaque psoriasis (BE RADIANT) |
| Methods | RCT, active‐controlled, double‐blind study Date of study: June 2018 Location: world‐wide Phase 3 |
| Participants |
Randomised: 743 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Bimekizumab dosage regimen 1 Control interventions B. bimekizumab dosage regimen 2 C. Secukinumab |
| Outcomes |
At week 16 Primary outcome PASI 100 Secondary outcome PASI 75, PASI 90, PASI 100 IGA SAEs, AEs |
| Starting date | Study start date: June 2018 Estimated study completion date: May 2022 Last update posted: August 2020, active, not recruiting |
| Contact information | Study Director UCB cares +1 844 599 2273 |
| Notes | Ongoing study Last checked in September 2020 |
NCT03598790.
| Study name | A study to assess the safety, tolerability and efficacy of bimekizumab in adult subjects with moderate to severe chronic plaque psoriasis (BE BRIGHT) |
| Methods | RCT, active‐controlled, open‐label study Date of study: September2018 Location: wordwide Phase 3 |
| Participants |
Randomised: 1355 participants Inclusion criteria Person is considered reliable and capable of adhering to the protocol (e.g. able to understand and complete diaries), visit schedule, and medication intake according to the judgement of the Investigator |
| Interventions |
Intervention A. Bimekizumab dose regimen 1 Control interventions B. Bimekizumab dose regimen 2 |
| Outcomes |
At week 68 Primary composite outcome Number of treatment‐emergent adverse events Secondary outcome Number of SAEs PASI 90 IGA |
| Starting date | Study start date: September2018 Estimated study completion date: December 2022 Last update posted: June 2020, active, not recruiting |
| Contact information | Contact: UCB Cares +1844599 ext 2273 |
| Notes | Ongoing study Last checked in September 2020 |
NCT03611751.
| Study name | An investigational study to evaluate experimental medication BMS‐986165 compared to placebo and a currently available treatment in participants with moderate‐to‐severe plaque psoriasis (POETYK‐PSO‐2) |
| Methods | RCT, active/placebo‐controlled, double‐blind study Date of study: August 2018 Location: world‐wide Phase 3 |
| Participants |
Randomised: 1000 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. BMS‐986165 Control interventions B. Apremilast C. Placebo |
| Outcomes |
At week 16 Primary composite outcome PASI 75 ‐ IGA 0/1 Secondary outcome PASI 90 (Time frame: week 16) |
| Starting date | Study start date: August 2018 Estimated study completion date: December 2020 Last update posted: August 2020, active, not recruiting |
| Contact information | clinical.trials@bms.com (sponsor: Bristol‐Myers Squibb) |
| Notes | Ongoing study |
NCT03897075.
| Study name | Efficacy and safety study of tildrakizumab in the treatment of nail psoriasis |
| Methods | RCT, parallel arms, double‐blind, multicentric Location ? Phase 3 |
| Participants |
Randomised: 146 Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention: Tildrakizumab Comparator: Placebo |
| Outcomes |
Primary Outcome:
Secondary Outcome:
Other Outcome
|
| Starting date | Estimated study start date: September 2020 Estimated study completion date: April 2024 Last update posted: July 2020, not yet recruiting |
| Contact information | Head, Clinical development91 2266455645clinical.trials@sparcmail.com |
| Notes | Funding: Sun Pharma Global FZE |
NCT03897088.
| Study name | Efficacy and safety of tildrakizumab in the treatment of scalp psoriasis |
| Methods | RCT, multicentre, double‐blind, placebo‐controlled Location: USA, Australia |
| Participants |
Randomised: 136 Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention: Tildrakizumab Comparator: Placebo |
| Outcomes |
Primary outcome:
Secondary outcome:
Other outcome:
|
| Starting date | Estimated study start date: May 2019 Estimated study completion date: August 2022 Last update posted: July 2020, recruiting |
| Contact information | Head, Clinical development91 2266455645clinical.trials@sparcmail.com |
| Notes | Funding: Sun Pharma Global FZE Last checked in September 2020 |
NCT03927352.
| Study name | The purpose of this research study is to compare the efficacy and safety of SCT630 and adalimumab (HUMIRA®) in adults with plaque psoriasis |
| Methods | RCT, phase 3, parallel arms, double‐blind Location: ? |
| Participants | Randomised 330 Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention 1: SCT630 80 mg subcutaneously on week 1/day 1 (initial loading dose) and 40 mg at week 2 and every 2 weeks thereafter until week 16
Participants with a PASI 50 response at week 16 continued to receive 40 mg SCT630 until week 48 Intervention 2: Adalimumab 80 mg subcutaneously on week 1/day 1 (initial loading dose) and 40 mg at week 2 and every 2 weeks thereafter until week 16 At week 16 participants with a PASI 50 response were re‐randomised to treatment with adalimumab or were transitioned to SCT630 until week 48 |
| Outcomes |
Primary outcome :
Secondary outcome
|
| Starting date | Estimated study start date: June 2019 Estimated study completion date: December 2022 Last update posted: July 2020, not yet recruiting |
| Contact information | Guo Ming+86‐10‐58628288‐9138ming_guo@sinocelltech.com |
| Notes | Funding: Sinocelltech Ltd. Last checked in September 2020 |
NCT04167462.
| Study name | An investigational study to evaluate experimental medication BMS‐986165 compared to placebo in participants with plaque psoriasis (POETYK‐PSO‐3) in mainland China, Taiwan, and South Korea (POETYK‐PSO‐3) |
| Methods | Phase 3, RCT, double‐blind, placebo‐controlled, parallel arms, multicentric Location: China, Taiwan, Korea |
| Participants | Randomised: 180 Inclusion criteria:
Exclusion criteria:
|
| Interventions | Intervention: BMS‐986165 Comparator: Placebo |
| Outcomes |
Primary outcome :
Secondary outcome measures :
|
| Starting date | Estimated study start date: November 2019 Estimated study completion date: January 2022 Last update posted: August 2020, recruiting |
| Contact information | ‐ |
| Notes | Bristol‐Myers Squibb Last checked in September 2020 |
NCT04237116.
| Study name | A study of secukinumab treatment in patients with plaque psoriasis and co‐existing non‐alcoholic fatty liver disease (NAFLD) (pINPOINt) |
| Methods | RCT, double‐blind, parallel‐arm, multicentric Phase 3 Location: Germany |
| Participants | Randomized: 90 Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention 1: secukinumab 300 mg s.c. weekly in first 4 weeks, followed by every 4 weeks up to week 20; and placebo 300 mg s.c. at weeks 13, 14 and 15 to maintain the blind Intervention 2: placebo 300 mg s.c. weekly in first 4 weeks, followed by every 4 weeks up to week 8; and secukinumab 300 mg s.c. weekly for 4 weeks starting at week 12, followed by every 4 weeks up to week 20 |
| Outcomes |
Primary outcome :
Secondary outcome :
|
| Starting date | Estimated study start date: February 2020 Estimated study completion date: February 2022 Last update posted: August 2020, recruiting |
| Contact information | Novartis Pharmaceuticals novartis.email@novartis.com |
| Notes | Funding: Novartis Pharmaceuticals Last checked in September 2020 |
NCT04306315.
| Study name | Adjusted brodalumab dose compared with standard brodalumab dose in subjects with moderate‐to‐severe plaque psoriasis and ≥ 120 kg body weight (ADJUST) |
| Methods | RCT, placebo‐controlled, double‐blind trial, parallel arms Phase 4 Location: ? |
| Participants |
Randomised: 384 participants Inclusion criteria:
Exclusion criteria:
|
| Interventions |
Intervention A. Brodalumab 210 mg + brodalumab 70 mg add‐on (subcutaneously at week 0, week 1, and week 2, and then once every 2 weeks. Participants not fulfilling a predefined response at any visit with efficacy assessments after week 16 will receive a dose adjustment to 280 mg brodalumab every 2 weeks) Control intervention B. Brodalumab 210 mg + placebo add‐on (subcutaneously at week 0, week 1, and week 2, and then once every 2 weeks. Participants not fulfilling a predefined response at any time visit with efficacy assessments week 16 will receive a dose adjustment to 210 mg brodalumab + placebo every 2 weeks) |
| Outcomes |
Primary outcome :
Secondary outcomes :
|
| Starting date | Estimated study start date: June 2020 Estimated study completion date: August 2024 Last update posted: April 2020, not yet recruiting |
| Contact information | LEO Pharma raleodk@leo‐pharma.com |
| Notes | Ongoing study Funding: LEO Pharma Last checked in September 2020 |
NCT04453137.
| Study name | Multicentre, double‐blind, randomised, parallel‐ group, study evaluating PK efficacy, safety, and immunogenicity in patients with plaque psoriasis receiving Humira or AVT02 followed by safety extension phase of AVT02 |
| Methods | RCT, active‐controlled, double‐blind trial, parallel arms Phase 3 Location: Georgia, Iceland, Poland, Russian Federation, Ukraine |
| Participants |
Randomised: 448 participants Inclusion criteria:
Exclusion criteria
|
| Interventions |
Intervention A. AVT02 (Adalimimab Biosimilar) Control intervention B. Adalimumab (initial dose of 80 mg (2 × 40 mg) administered SC, followed by 40 mg SC given every other week starting 1 week after the initial dose |
| Outcomes |
At 26 weeks to 28 weeks Primary outcome :
Secondary outcomes :
|
| Starting date | Estimated study start date: June 2020 Estimated study completion date: February 2022 Last update posted: August 2020, recruiting |
| Contact information | Roshan Dias, MSc roshan.dias@alvotech.com Heimo Stroissnig, MD heimo.stroissnig@alvotech.com Principal investigator: Steven Feldman, MD, PhD Wake Forest University Health Sciences |
| Notes | Ongoing study Funding: Alvotech Swiss AG Last checked in September 2020 |
TCTR20161028001.
| Study name | A randomised, double‐blind, placebo controlled, multicentre study of subcutaneous secukinumab, to demonstrate efficacy after 12 weeks of treatment and to assess safety, tolerability and long‐term efficacy up to 1 year in subjects with moderate‐to‐severe chronic plaque‐type psoriasis with or without psoriatic arthritis comorbidity |
| Methods | RCT, active/placebo‐controlled, double‐blind trial Date of study: February 2017 Location: Thailand |
| Participants |
Randomised: 40 participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention A. Secukinumab 300 mg SC (administration not specified) Control intervention B. Secukinumab 150 mg SC (administration not specified) C. Placebo |
| Outcomes |
At week 12 Primary outcome (composite)
Secondary outcomes
|
| Starting date | 28 February 2017; not yet recruiting (24 April 2019) |
| Contact information | Kerstin Letzelter, kerstin.letzelter@novartis.com |
| Notes | Ongoing study Last checked in September 2020 |
AE: Adverse events; BMI: body mass index; BSA: Body Surface Area; ECG: electrocardiogram; FAEs: fumaric acid esters; IV: intravenous; NAPSI: Nail Psoriasis Severity Index; PASI: Psoriasis Area and Severity Index; PGA: Physician's Global Assessment; QoL: quality of life; RCT: randomised controlled trial: SC: subcutaneous; sPGA: static physician global assessment; TB: tuberculosis; UVA/B: ultraviolet A/B; SAE: Serious adverse event
Differences between protocol and review
A. Between the previous review (January 2019) and the last update search (September 2020)
1. Methods: Data collection and analysis > Data synthesis > Network meta‐analysis
We will provide new networks and re‐analyse the data every six months instead of three months, to have enough new data to integrate.
2. Methods: Data collection and analysis > Assessment of heterogeneity
To better reassure the plausibility of transitivity, we excluded from the main analysis trials including biological‐naïve participants, but assessing efficacy of a biological agent.
3. Methods: Data collection and analysis > Sensitivity analysis
We added two new sensitivity analyses: (1) including trials irrespective of the previous treatments received by the participants, and (2) using another definition of the safety primary outcomes: SAEs after excluding flares of psoriasis.
4. Methods: Data collection and analysis > Summary of Findings and Assessment of certainty of the evidence
We did not include 'Summary of findings' (SoF) tables because the format of an SoF table does not allow us to present a summary of comparisons across the different drugs. The SoF tables in the last version of the review only focused on the comparisons against placebo.
We did not use GRADE assessment for the new update of this review, but CiNeMa is tool specifically dedicated to network meta‐analysis.
We therefore explained the methodology, and added in the Methods section:
We assessed the confidence of the evidence estimates from network meta‐analysis, based on the CINeMA approach which relies on the contributions of the direct comparisons to the estimation in the network meta‐analysis (CINeMA 2017; Salanti 2014). CINeMA (Confidence in Network Meta‐Analysis) is a web application that simplifies the evaluation of confidence in the findings from network meta‐analysis.
It is based on six domains: within‐study bias (referring to the impact of risk of bias in the included studies), across‐studies bias (publication or reporting bias), indirectness (relevance to the research question and transitivity), imprecision (comparing the range of treatment effects included in the 95% confidence interval with the range of equivalence), heterogeneity (predictive intervals), and incoherence (if estimates from direct and indirect evidence disagree) (Salanti 2014).
The confidence in each NMA (network meta‐analysis) RR (risk ratio)AB between two given drugs A and B was evaluated for six domains. The software required some input in each domain in order to recommend whether there were 'major concerns', 'some concerns' or 'no concerns' for the particular domain.
Thus, threshold values and evaluation rules to be decided were finalised through discussions. After determining these rules, the remaining synthesis of confidence in the evidence can automatically be calculated with the CINeMA web app. One review author input all the data and obtained the results.
Within‐trial bias: we estimated it as the weighted average of the overall risk of bias of all the trials contributing information to the estimation of RRAB.
Reporting bias: also known as 'publication bias'. We assessed publication bias by considering the comprehensive search strategy that we performed and the risk of publication bias in the specific field. The comparison‐adjusted funnel plots that test the presence of small‐study effects in the network assisted our judgements.
Indirectness: since the included studies matched the clinical question of the review, we had 'no concern' about any of the evaluated RRAB.
Imprecision: which was rated based on whether the 95% CI of RR allowed recommendations to be made. We set the margin of equivalent effects (where none of the drugs is favoured) to between RR 0.95 and 1.05. These values were motivated by the fact that assuming 3% response rate (reaching PASI 90) for placebo, then an RRAB of 1.05 indicated a response for drug A higher than those obtained with placebo, which we considered as clinically meaningful. Then, the degree of overlap between the 95% CI of RRAB and the margin of equivalent effects suggests the judgement.
Heterogeneity: this was evaluated by monitoring the agreement between confidence intervals (CIs) and prediction intervals (PIs). CINeMA judges whether the two intervals and their overlap with the margin of equivalent effects provide similar conclusions.
(6) Incoherence: this was evaluated by monitoring the level of disagreement between confidence intervals (CIs) of the direct and indirect RRAB and their overlap with the margin of equivalent effects5.
After the judgement for all the six domains, we summarised our overall confidence in evidence for each or between any two drugs into high, moderate, low and very low ratings. Starting with high confidence, we downgraded by one level for each ‘major concern’ in any of the six domains; then two‐thirds of a level down for ‘some concerns’ in ‘within‐study bias’; one‐third of a level down for each rating of ‘some concerns’ in any of the other five domains. To obtain the final level, we rounded the number of downgrades to their nearest integer.
For each drug, we calculated the percentage of the four levels based on all comparisons including that drug, combining both efficacy and acceptability.
It is important to note that the CiNeMa tool was also used in the previous version of our review and results were presented with those from GRADE scoring. Evaluation rules were not the same, however, especially for the margin of equivalent effects which was RR = 1.5. We discussed this point and because the margin of effect was too large, so we have changed this rule for this update.
B. Between the previous review (Sbidian 2017) and the first update search (January 2019)
1. Background: Why it is important to do this review
We provided a rationale for maintaining the review as a living systematic review (LSR).
This review includes some new methods relevant for living systematic reviews, which are included in the Methods section, and also described in Appendix 4.
2. Methods: Search methods for identification of studies
Changes between search methods in the existing review and the LSR Older versions of this review included searches of the Cochrane Skin Specialised Register and LILACS. The Skin Register is no longer being maintained so we will not search it separately for the LSR. The Cochrane Skin Information Specialist has analysed the results of previous searches for this review and has established that no unique studies were identified through LILACS. We will not therefore search LILACS for the LSR.
We did not identify unique trials through our previous searches of the trial results databases of various pharmaceutical companies. We will therefore not search these resources regularly for the LSR.
For the existing review, we searched five trials registries:
the ISRCTN registry (www.isrctn.com);
ClinicalTrials.gov (www.clinicaltrials.gov);
the Australian New Zealand Clinical Trials Registry (www.anzctr.org.au);
the World Health Organization International Clinical Trials Registry Platform (ICTRP) (apps.who.int/trialsearch/); and
the EU Clinical Trials Register (www.clinicaltrialsregister.eu).
For the LSR we will search only those that are mandatory under the MECIR standards, i.e. ClinicalTrials.gov and WHO ICTRP. WHO ICTRP is an aggregator of the other three trials registries listed.
3. Interventions
Interventions belonging to the systemic conventional treatments, anti‐TNF alpha, and anti IL12/23 classes were identical to the previous review.
Ponesimod (belonging to the small molecules class), itolizumab and alefacept (belonging to other biologics class) were withdrawn from the updated review as they are no longer used as systemic treatment for psoriasis.
Bimekizumab (anti‐IL17 class), risankizumab and mirikizumab (anti‐IL23 class) and BMS‐986165 (small molecules class) are new included drugs for the updated review.
We added new molecules to the search strategy for the update and the LSR searches.
4. Outcomes
Primary and secondary outcomes are identical to the previous review, except for one secondary endpoint: 'Proportion of participants who achieve PASI 75 at 52 weeks' and 'Proportion of participants who achieve PASI 90 at 52 weeks'. These replace 'Proportion of participants with at least one relapse in the maintenance phase (between 52 to 104 weeks)' because this outcome was never available in the maintenance‐phase trials, and our replacement outcomes answer the same question.
Secondary endpoints
1. Proportion of participants who achieve PASI 75 at induction phase
2. Proportion of participants who achieve a Physician Global Assessment (PGA) value of 0 or 1 at induction phase
3. Quality of life measured by a specific scale. Available validated scales are the Dermatology Life Quality Index (DLQI), Skindex, Psoriasis Disability Index (PDI), or Psoriasis Symptom Inventory (PSI) at induction phase
4. Proportions of participants with adverse effects (AEs) at induction phase
5. Proportion of participants who achieve PASI 75 at 52 weeks
6. Proportion of participants who achieve PASI 90 at 52 weeks
To avoid selection of good responders from participants entering into long‐term extension, we selected participants who have been randomised since the induction phase.
The timing of outcomes was also slightly edited: primary outcomes were restricted to only being measured during induction phase (from 8 to 24 weeks after randomisation). All secondary outcomes, except proportion of participants who achieve PASI 75 at 52 weeks and proportion of participants who achieve PASI 90 at 52 weeks, were also restricted to the induction phase. We did not include timings outside these ranges. We also clarified that if there were multiple time points within a phase we would use the longest one.
By expanding the timings (in the previous review, we only analysed trials with short‐term assessment defined as 12 to 16 weeks), we aimed to include more trials.
We also clarified that 'Proportions of participants with adverse effects (AE) at induction phase' did not include serious adverse events.
5. Data collection and analysis: Selection of studies
We used Covidence (Covidence 2019) to screen the titles, abstracts and full texts.
5. Data collection and analysis: Assessement of heterogeneity
For the network meta‐analysis, to further assure the plausibility of the transitivity assumption, we only excluded from our analyses trials involving co‐interventions. We kept in our analyses all trials with a short‐term outcome assessment from 8 to 24 weeks, and not only from 12 to 16 weeks as we had previously. We performed sensitivity analyses including only studies with a short‐term outcome assessment from 12 to 16 weeks. We also performed sensitivity analyses excluding trials of systemic‐treatment‐naïve participants.
6. Data collection and analysis: 'Summary of findings' table
We used another method to assess confidence in the our results.
"We also performed full evaluation of the confidence in the results using the web application CINeMA (CINeMA 2017). CINeMA (Confidence in Network Meta‐Analysis) is a web application that simplifies the evaluation of confidence in the findings from network meta‐analysis. It is based on six domains: within‐study bias (referring to the impact of risk of bias in the included studies), across‐studies bias (publication or reporting bias), indirectness (relevance to the research question and transitivity), imprecision (comparing the range of treatment effects included in the 95% confidence interval with the range of equivalence), heterogeneity (predictive intervals) and incoherence (if estimates from direct and indirect evidence disagree) (Salanti 2014).Judgements across the six domains are then summarised to obtain four levels of confidence for each relative treatment effect, corresponding to the usual GRADE approach: very low, low, moderate or high."
7. Data collection and analysis: Dealing with missing data
We clarified out approach for dealing with missing data for safety outcomes: “For the main analysis, we assumed that any participant with missing outcome data did not experience clearance (for efficacy outcomes) or did not experience AEs (for safety outcomes), whatever the group."
C. Between the first protocol submission (January 2014) and the first search (February 2015)
1. We identified and added in the protocol new systemic therapeutics for psoriasis.
Background: Description of the intervention
Oral treatment
Biological therapies
Background: How the intervention might work?
Oral treatment
Biological therapies
Objectives
We expanded our objectives to clarify the types of systemic treatments for psoriasis. We changed: "To assess the effects of systemic pharmacological treatments for chronic plaque psoriasis" to "To compare the efficacy and safety of conventional systemic agents (acitretin, ciclosporin, fumaric acid esters, methotrexate), small molecules (apremilast, tofacitinib, ponesimod), anti‐TNF alpha (etanercept, infliximab, adalimumab, certolizumab), anti‐IL12/23 (ustekinumab), anti‐IL17 (secukinumab, ixekizumab, brodalumab), anti‐IL23 (guselkumab, tildrakizumab), and other biologics (alefacept, itolizumab) for patients with moderate to severe psoriasis and to provide a ranking of these treatments according to their efficacy and safety."
Methods: Types of intervention
We changed: "Systemic treatments include the following: fumaric acid esters, retinoids (acitretin), ciclosporin, methotrexate, infliximab, etanercept, adalimumab, ustekinumab, briakinumab, alefacept, brodalumab, ixekizumab" to the following:
"Systemic treatments included the following:
Systemic conventional treatments:
Fumaric acid esters
Acitretin
Ciclosporin
Methotrexate
Small molecules
Apremilast
Tofacitinib
Ponesimod
Anti‐TNF alpha
Infliximab
Etanercept
Adalimumab
Certolizumab
Anti‐IL12/23
Ustekinumab
Anti‐IL17
Secukinumab
Brodalumab
Ixekizumab
Anti‐IL23
Tildrakizumab
Guselkumab
Other biologic treatment
Itolizumab
Alefacept
A new anti‐IL23 molecule (BI 655066, risankizumab) appeared after we began this review and was not included in this systematic review. However, the ongoing studies of risankizumab have been reported in this review."
2. Background: Why it is important to do this review
We updated the published literature on other systemic reviews and meta‐analyses.
3. Methods: Criteria for considering studies for this review
Selection of trials
We added: "Phase I trials were not eligible because participants, outcomes, dosages, and schema of administration of interventions are too different from phase II, III, and IV studies."
Outcomes
Primary outcome 1
In the Protocol, we wrote, "The proportion of participants who achieved clear or almost clear skin. (By clear or almost clear, we mean a Physician Global Assessment (PGA) value of 0 or 1 or a 90/100 PASI.)"
In the review, we changed this sentence to "The proportion of participants who achieved clear or almost clear skin, that is, at least PASI 90".
As PASI and PGA are two different scales, we preferred to assess them separately and added as a secondary outcome 'Proportion of participants who achieve a Physician Global Assessment (PGA) value of 0 or 1'.
Primary outcome 1
We also modified the sentence about serious adverse effects (SAEs). In the protocol we had said we would use the FDA's definition): "The proportion of participants with serious adverse effects (SAE). We used the definition of severe adverse effects from the International Conference of Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use, which includes death, life‐threatening events, initial or prolonged hospitalisation, and adverse events requiring intervention to prevent permanent impairment or damage." The definition remains the same.
Secondary outcome 3
For 'Quality of life measured by a specific scale', we listed Dermatology Life Quality Index (DLQI), Skindex, Psoriasis Disability Index (PDI), or Psoriasis Symptom Inventory (PSI). It is not an exhaustive list. Moreover, we had PSI as a validated scale because it was used by some study authors.
Timings
We modified the period of the induction therapy assessment to less than 24 weeks after randomisation instead of 12 to 24 weeks, because Nast 2015b defined the induction period as being of a duration less than 24 weeks.
To avoid duplicating text, we removed the text discussing timing for remission, as published in the protocol, and edited the timings for induction and maintenance therapy to include the relevant short‐ or long‐term remission classification. We also removed the timings given in the protocol for the quality‐of‐life outcome for the same reason (we felt the text was duplicative).
We clarified that our inclusion criterion was to only include studies that reported our timings of interest by editing as follows: "We did not include studies that had timings outside of these time ranges in our analyses" to "We did not include studies that had timings outside of these time ranges in our review."
4. Methods: Search methods for identification of studies
We removed the following two sentences from the review:
"We contacted key investigators and experts in the field to identify further published or unpublished data."
"We contacted pharmaceuticals companies producing fumaric acid esters, and retinoids (fumaric acid esters, retinoids (acitretin), ciclosporin, methotrexate, alefacept, infliximab, etanercept, adalimumab, certolizumab, ustekinumab, secukinumab, brodalumab, ixekizumab, tildrakizumab, guselkumab, Itolizumab, apremilast, tofacitinib, ponesimod."
We replaced them with the following:
"We searched in the trial results databases of each company to identify ongoing and unpublished trials."
5. Methods: Data extraction and management
We added some details about the data extraction (outcome data, other data) for greater clarity and added the sentence, "We extracted the data from the reports of the US Food and Drug Administration (FDA) when available, if not from the US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov), and finally from the published reports."
6. Methods: Assessment of risk of bias in included studies
We added information about the network meta‐analysis 'Risk of bias' assessment (under "Overall risk of bias").
Network meta‐analysis
"To summarise the quality of evidence and to interpret the network results, we used these six RoB criteria (random sequence generation, allocation concealment, blinding of participants, blinding of outcome assessor, incomplete outcome data, and selective outcome reporting) in order to classify each trial.
We would classify the trial as having low risk of bias if we rated none of the domains above as high risk of bias and two or fewer as unclear risk.
We would classify the trial as having moderate risk of bias if we rated one domain as high risk of bias, one or less domains as unclear risk, or no domains as high risk of bias but three or fewer were rated as unclear risk.
All other cases were assumed to pertain to high risk of bias."
7. Methods: Measure of treatment effect
We added an explanation about relative treatment ranking.
8. Methods: Dealing with missing data
We clarified who the authors or sponsors we contacted were: "We contacted trial authors or sponsors by email to request missing outcome data (numbers of events and numbers of participants for important dichotomous clinical outcomes) when these were not available in study reports that were less than 10 years old."
9. Methods: Assessment of reporting bias and assessment of heterogeneity
We added an explanation of the network meta‐analysis:
"We undertook meta‐analyses only if we judged participants, interventions, comparisons, and outcomes to be sufficiently similar (section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions) (Higgins 2017). Potential sources of heterogeneity included participants' baseline characteristics (weight, the duration of previous treatment, treatment doses, co‐interventions, and duration of treatment). When enough data were available, we investigated the distributions of these characteristics across studies and treatment comparisons. The latter allows assessing transitivity, i.e. whether there were important differences between the trials evaluating different comparisons other than the treatments being compared (Salanti 2014). To further reassure the plausibility of the transitivity assumption, we only included in our analyses trials not involving co‐interventions.
In the classical meta‐analyses, we assessed statistical heterogeneity by visual inspection of the forest plots and using the Q‐test and the I2 statistic. We interpreted the I2 statistic according to the following thresholds (section 9.5.2 of the Cochrane Handbook for Systematic Reviews of Interventions; Higgins 2017): 0% to 40% might not be important; 30% to 60% may represent moderate heterogeneity; 50% to 90% may represent substantial heterogeneity; 75% to 100% represents considerable heterogeneity.
In the network meta‐analysis, the assessment of statistical heterogeneity in the entire network was based on the estimated heterogeneity standard deviation parameter (τ) estimated from the network meta‐analysis models (Jackson 2014). We also estimated the prediction intervals to assess how much the estimated heterogeneity affects the relative effects with respect to the additional uncertainly anticipated in future studies (Riley 2011). Where feasible, we would have investigated the possible sources of heterogeneity in subgroup analyses and meta‐regression.
Although we restricted the risk of important heterogeneity in our data by considering eligible only studies with a follow‐up period between 12 and 16 weeks and without co‐interventions, we investigated differences in heterogeneity across the different analyses. Specifically, we observed whether splitting the nodes of the network and analysing each drug separately reduced the heterogeneity estimate. We also ran a series of sensitivity analyses (see Sensitivity analysis), and we monitored whether heterogeneity became smaller or larger compared to the primary analysis."
Assessment of reporting biases
To assess reporting biases, we used an adaptation of the funnel plot by subtracting from each study‐specific effect size the mean of meta‐analysis of the study‐specific comparison, which we plotted against the study standard error (Chaimani 2013). We employed this 'comparison‐adjusted funnel plot' for all comparisons of an active treatment against placebo. When we detected funnel plot asymmetry for the two primary outcomes, we investigated the presence of small‐study effects in the network meta‐regression (Chaimani 2012).
10. Methods: Data synthesis
We added the software used for the review: "We conducted pair‐wise meta‐analyses using Review Manager 5 (RevMan 5) (Revman 2020), and we performed all other analyses in Stata 14 using the 'network' (www.stata-journal.com/article.html?article=st0410) and 'network graphs' packages (www.stata-journal.com/article.html?article=st0411)."
11. Methods: Sensitivity analysis
We added "To assess the robustness of our results, we performed the following sensitivity analyses for the two primary outcomes: (1) running the analysis at dose‐level considering that each different drug dose is a different intervention; (2) excluding trials at high risk of bias; (3) excluding trials with a total sample size smaller than 50 randomised participants; and (4) analysing only the observed participants and assuming that missing participants are missing at random."
12. Methods: 'Summary of findings' table
We added a section detailing the methods used to create the 'Summary of findings' tables; we also explained how we used GRADE to assess the certainty (quality/confidence) of the evidence.
13. Contributions of authors
We changed or added authors' contributions: LLC, GD, IGD, and ES screened papers against eligibility criteria. LLC, GD, IGD, CH, CM, CD, and ES appraised the quality of papers. LLC, GD, IGD, CH, CM, CD, and ES extracted data for the review and sought additional information about papers. AC responded to the methodological and statistical comments of the referees instead of LT (Ludovic Trinquard was no longer available and was replaced by Anna Chaimani). AC, LLC, and ES worked on the Methods sections instead of LT, ES, and LLC (Ludovic Trinquard was replaced by Anna Chaimani).
Contributions of authors
ES and LLC were the contacts with the editorial base. ES co‐ordinated contributions from the co‐authors and wrote the final draft of the review. LD performed the search. LLC, SA, CD, IGD, and ES screened papers against eligibility criteria. ES obtained data on ongoing and unpublished studies. LLC, SA, and ES appraised the quality of papers. LLC, SA, and ES extracted data for the review and sought additional information about papers. LLC, SA and ES entered data into RevMan. AC analysed and interpreted data. AC, LLC, and ES worked on the Methods sections. ES and LLC drafted the clinical sections of the Background and responded to the clinical comments of the referees. AC responded to the methodology and statistical comments of the referees. CH was the consumer co‐author and checked the review for readability and clarity, as well as ensuring outcomes are relevant to consumers. She also wrote the Plain Language Summary. All of the authors read and amended the manuscript. ES is the guarantor of the update.
Sources of support
Internal sources
No sources of support provided
External sources
-
The National Institute for Health Research (NIHR), UK
The NIHR, UK, is the largest single funder of the Cochrane Skin Group.
-
The French Society of Dermatology (SFD), France, France
The funding agencies have no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation and review of the manuscript.
-
French Ministry of Health, France, Other
Grant support was from the Programme Hospitalier de Recherche Clinique (DGOS n°APHP‐180680).
The funding agencies have no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation and review of the manuscript.
Declarations of interest
Emilie Sbidian: reports receipt of two grants to support this work: one from the French Ministry of Health, France (Programme Hospitalier de Recherche Clinique (DGOS no.APHP180680) and one from The French Society of Dermatology (SFD); both paid to institution. The funding agencies have no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or preparation and review of the manuscript.
Anna Chaimani: has declared that they have no conflict of interest.
Ignacio Garcia‐Doval: reports payment from Novartis for a presentation unrelated to psoriasis; personal payment. IG‐D also reports receiving meeting expenses from Janssen for the Spanish Academy of Dermatology annual Congress; personal payment.
Liz Doney: has declared that they have no conflict of interest.
Corinna Dressler: reports an unrestricted research grant from Eli Lilly for a time‐effectiveness analysis of psoriasis; paid to institution. CD also reports a grant from the European Dermatology Forum to fund a European Guideline Development Centre (EuroGuiDerm); paid to institution.
Camille Hua: has declared that they have no conflict of interest.
Carolyn Hughes: has declared that they have no conflict of interest.
Luigi Naldi: reports an unrestricted grant from AbbVie to conduct a survey on hidradenitis suppurativa; paid to institution. LN also reports compensation for consultancy or participating in advisory board meetings from the following pharmaceutical companies: AbbVie, Almirall, Janssen‐Cilag (Psolar registry), Novartis, Sanofi Aventis, and L'Oreal (sunscreens); personal payment.
Sivem Afach: has declared that they have no conflict of interest.
Laurence Le Cleach: reports receipt of two grants to support this work: one from the French Ministry of Health, France (Programme Hospitalier de Recherche Clinique (DGOS no.14‐0322) and one from The French Society of Dermatology (SFD); both paid to institution.
Clinical referees: Brandon Adler: Dr. Adler has served as an investigator for AbbVie (non‐psoriasis trials). Alex Ortega‐Loayza: Has served on Advisory boards for Janssen and BMS.
Edited (no change to conclusions)
References
References to studies included in this review
ACCEPT 2010 {published data only}
- Griffiths CE, Strober BE, Van de Kerkhof P, Ho V, Fidelus-Gort R, Yeilding N, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. New England Journal of Medicine 2010;362(2):118-28. [CENTRAL: CN-00734856] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Young MS, Horn EJ, Cather JC. The ACCEPT study: ustekinumab versus etanercept in moderate-to-severe psoriasis patients. Expert Review of Clinical Immunology 2011;7(1):9-13. [CENTRAL: CN-00780322] [PMID: ] [DOI] [PubMed] [Google Scholar]
ADACCESS 2018 {published data only}
- Blauvelt A, Lacour J, Fowler JF, Schuck E, Jauch-Lembach J, Balfour A, et al. Long-term efficacy, safety, and immunogenicity data from a phase iii confirmatory study comparing GP2017, a proposed biosimilar, with reference adalimumab. United European Gastroenterology Journal 2017;5(Suppl 1):A301. [CENTRAL: CN-01439136] [Google Scholar]
- Blauvelt A, Lacour JP, Fowler JF Jr, Weinberg JM, Gospodinov D, Schuck E, et al. Phase III randomized study of the proposed adalimumab biosimilar GP2017 in psoriasis: impact of multiple switches. British Journal of Dermatology 2018;179(3):623-31. [CENTRAL: CN-01617973] [DOI] [PubMed] [Google Scholar]
- NCT02016105. Study to demonstrate equivalent efficacy and to compare safety of biosimilar adalimumab (GP2017) and humira (ADACCESS). clinicaltrials.gov/show/nct02016105 (first received 19 December 2013). [CENTRAL: CN-01479872]
Akcali 2014 {published data only}
- Akcali C, Guven EH, Kirtak N, Inaloz HS, Ozgoztasi O, Guvenc U. Serum concentrations of interleukin-2 and tumour necrosis factor-alpha under cyclosporine versus acitretin treatment in plaque-type psoriasis. Journal of International Medical Research 2014;42(5):1118-22. [CENTRAL: CN-01114333] [PMID: ] [DOI] [PubMed] [Google Scholar]
Al‐Hamamy 2014 {published data only}
- Al-Hamamy HR, Al-Mashhadani SA, Mustafa IN. Comparative study of the effect of narrowband ultraviolet B phototherapy plus methotrexate vs. narrowband ultraviolet B alone and methotrexate alone in the treatment of plaque-type psoriasis. International Journal of Dermatology 2014;53(12):1531-5. [CENTRAL: CN-01089920] [PMID: ] [DOI] [PubMed] [Google Scholar]
AMAGINE‐1 2016 {published data only}
- Papp KA, Reich K, Paul C, Blauvelt A, Baran W, Bolduc C, et al. A prospective phase III, randomized,double-blind, placebo-controlled study of brodalumab in patients withmoderate-to-severe plaque psoriasis. British Journal of Dermatology 2016;175(2):273-86. [CENTRAL: CN-01208651] [DOI] [PubMed] [Google Scholar]
AMAGINE‐2 2015 {published data only}
- Lebwohl M, Strober B, Menter A, Gordon K, Weglowska J, Puig L, et al. Phase 3 studies comparing brodalumab with ustekinumab in psoriasis. New England Journal of Medicine 2015;373(14):1318-28. [CENTRAL: CN-01089800] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Menter A, Sobell J, Silverberg JI, Lebwohl M, Rastogi S, Pillai R, et al. Long-term efficacy of brodalumab for the treatment of moderate-to-severe psoriasis: data from a pivotal Phase III clinical trial. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Suppl 1):S26-7. [CENTRAL: CN-01713709] [Google Scholar]
- Papp KA, Lebwohl MG, Green LJ, Yamauchi PS, Rastogi S, Israel R, et al. Maintenance of clinical efficacy in moderate-to-severe plaque psoriasis: a 52-week evaluation of brodalumab in three multicenter, double-blind studies of 4363 subjects. Journal of Clinical and Aesthetic Dermatology 2017;10(5 Suppl 1):S23-4. [CENTRAL: CN-01713074] [Google Scholar]
AMAGINE‐3 2015 {published data only}
- Lebwohl M, Strober B, Menter A, Gordon K, Weglowska J, Puig L, et al. Phase 3 studies comparing brodalumab with ustekinumab in psoriasis. New England Journal of Medicine 2015;373(14):1318-28. [CENTRAL: CN-01089800] [PMID: ] [DOI] [PubMed] [Google Scholar]
Asahina 2010 {published data only}
- Asahina A, Nakagawa H, Etoh T, Ohtsuki M, Adalimumab M04-688 Study Group. Adalimumab in Japanese patients with moderate to severe chronic plaque psoriasis: efficacy and safety results from a Phase II/III randomized controlled study. Journal of Dermatology 2010;37(4):299-310. [CENTRAL: CN-00762123] [PMID: ] [DOI] [PubMed] [Google Scholar]
Asahina 2016 {published data only}
- Asahina A, Etoh T, Igarashi A, Imafuku S, Saeki H, Shibasaki Y, et al. Oral tofacitinib efficacy, safety and tolerability in Japanese patients with moderate to severe plaque psoriasis and psoriatic arthritis: a randomized, double-blind, phase 3 study. Journal of Dermatology 2016;43(8):869-80. [CENTRAL: CN-01380021] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Asawanonda 2006 {published data only}
- Asawanonda P, Nateetongrungsak Y. Methotrexate plus narrowband UVB phototherapy versus narrowband UVB phototherapy alone in the treatment of plaque-type psoriasis: a randomized, placebo-controlled study. Journal of the American Academy of Dermatology 2006;54(6):1013-8. [CENTRAL: CN-00556468] [PMID: ] [DOI] [PubMed] [Google Scholar]
AURIEL‐PsO 2020 {published data only}
- Hercogova J, Papp KA, Chyrok V, Ullmann M, Vlachos P, Edwards CJ. AURIEL-PsO: A randomised, double-blind Phase III equivalence trial to demonstrate the clinical similarity of the proposed biosimilar MSB11022 to reference adalimumab in patients with moderate-to-severe chronic plaque-type psoriasis. British Journal of Dermatology 2020;182(2):316-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02660580. MSB11022 in moderate to severe chronic plaque psoriasis (AURIEL-PsO). clinicaltrials.gov/show/nct02660580 (first received 21 January 2016). [CENTRAL: CN-01555234]
Bachelez 2015 {published data only}
- Bachelez H, Van de Kerkhof PC, Strohal R, Kubanov A, Valenzuela F, Lee JH, et al. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomised non-inferiority trial. Lancet 2015;386(9993):552-61. [CENTRAL: CN-01091031] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Valenzuela F, Paul C, Mallbris L, Tan H, Papacharalambous J, Valdez H, et al. Tofacitinib versus etanercept or placebo in patients with moderate to severe chronic plaque psoriasis: patient-reported outcomes from a Phase 3 study. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;30(10):1753-9. [CENTRAL: CN-01368560] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bagel 2012 {published data only}
- Bagel J, Kricorian G, Klekotka P, Tyring S. Etanercept therapy for moderate to severe plaque psoriasis with involvement of the scalp. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB150. [CENTRAL: CN-00843659] [DOI] [PubMed] [Google Scholar]
- Bagel J, Lynde C, Tyring S, Kricorian G, Shi Y, Klekotka P. Moderate to severe plaque psoriasis with scalp involvement: a randomized, double-blind, placebo-controlled study of etanercept. Journal of the American Academy of Dermatology 2012;67(1):86-92. [CENTRAL: CN-00870940] [PMID: ] [DOI] [PubMed] [Google Scholar]
Barker 2011 {published data only}
- Barker J, Hoffmann M, Wozel G, Ortonne JP, Zheng H, Van Hoogstraten H, et al. Efficacy and safety of infliximab vs. methotrexate in patients with moderate-to-severe plaque psoriasis: results of an open-label, active-controlled, randomized trial (RESTORE1). British Journal of Dermatology 2011;165(5):1109-17. [CENTRAL: CN-00805921] [PMID: ] [DOI] [PubMed] [Google Scholar]
BE ABLE 1 2018 {published data only}
- Blauvelt A, Papp KA, Merola JF, Gottlieb AB, Cross N, Madden C, et al. Bimekizumab for patients with moderate-to-severe plaque psoriasis: 60-week results from BE ABLE 2, a randomized, double-blinded, placebo-controlled phase 2b extension study. Journal of the American Academy of Dermatology 2020;83(5):1367-1374. [DOI: 10.1016/j.jaad.2020.05.105] [PMID: ] [DOI] [PubMed] [Google Scholar]
- NCT02905006. Study to evaluate safety and efficacy of different doses of bimekizumab in patients with chronic plaque psoriasis (BE ABLE 1). clinicaltrials.gov/show/nct02905006 (first received 19 September 2016). [CENTRAL: CN-01520880]
- Papp KA, Merola JF, Gottlieb AB, Griffiths CE, Cross N, Peterson L, et al. Dual neutralization of both interleukin 17A and interleukin 17F with bimekizumab in patients with psoriasis: results from BE ABLE 1, a 12-week randomized, double-blinded, placebo-controlled phase 2b trial. Journal of the American Academy of Dermatology 2018;79(2):277-86.e10. [CENTRAL: CN-01665198] [DOI] [PubMed] [Google Scholar]
Bissonnette 2013 {published data only}
- Bissonnette R, Tardif J-C, Harel F, Pressacco J, Bolduc C, Guertin MC. Effects of the tumor necrosis factor-alpha antagonist adalimumab on arterial inflammation assessed by positron emission tomography in patients with psoriasis: Results of a randomized controlled trial. Circulation: Cardiovascular Imaging 2013;6(1):83-90. [CENTRAL: CN-00906599] [EMBASE: 2013325307] [DOI] [PubMed] [Google Scholar]
Bissonnette 2015 {published data only}
- Bissonnette R, Iversen L, Sofen H, Griffiths CE, Foley P, Romiti R, et al. Tofacitinib withdrawal and retreatment in moderate-to-severe chronic plaque psoriasis: A randomized controlled trial. British Journal of Dermatology 2015;172(5):1395-406. [CENTRAL: CN-01254758] [PMID: ] [DOI] [PubMed] [Google Scholar]
BRIDGE 2017 {published data only}
- Anonymous. Corrigendum to: Efficacy and safety of LAS41008 (dimethyl fumarate) in adults with moderate-to-severe chronic plaque psoriasis: a randomized, double-blind, Fumaderm - and placebo-controlled trial (BRIDGE) (British Journal of Dermatology 2017;176(3):615-23, 10.1111/bjd.14947). British Journal of Dermatology 2018;178(1):308. [DOI] [PubMed] [Google Scholar]
- Mrowietz U, Szepietowski JC, Loewe R, Van de Kerkhof P, Lamarca R, Ocker WG, et al. Efficacy and safety of LAS41008 (dimethyl fumarate) in adults with moderate-to-severe chronic plaque psoriasis: a randomized, double-blind, Fumaderm® - and placebo-controlled trial (BRIDGE). British Journal of Dermatology 2017;176(3):615-23. [CENTRAL: CN-01336917] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Van de Kerkhof PCM, Loewe R, Mrowietz U, Falques M, Pau-Charles I, Szepietowski JC. Quality of life outcomes in adults with moderate-to-severe plaque psoriasis treated with dimethylfumarate (DMF): a post-hoc analysis of the BRIDGE study. Journal of the European Academy of Dermatology & Venereology 2020;34(1):119-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cai 2016 {published data only}
- Cai L, Gu J, Zheng J, Zheng M, Wang G, Xi LY, et al. Efficacy and safety of adalimumab in Chinese patients with moderate-to-severe plaque psoriasis: results from a phase 3, randomized, placebo-controlled, double-blind study. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;31(1):89-95. [CENTRAL: CN-01248561] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Caproni 2009 {published data only}
- Caproni M, Antiga E, Melani L, Volpi W, Bianco E, Fabbri P. Serum levels of IL-17 and IL-22 are reduced by etanercept, but not by acitretin, in patients with psoriasis: a randomized-controlled trial. Journal of Clinical Immunology 2009;29(2):210-4. [CENTRAL: CN-00685566] [PMID: ] [DOI] [PubMed] [Google Scholar]
CARIMA 2019 {unpublished data only}
- NCT02559622. Evaluation of cardiovascular risk markers in psoriasis patients treated with secukinumab (CARIMA). clinicaltrials.gov/ct2/show/NCT02559622 (first received 4 August 2015).
- Von Stebut E, Reich K, Thaçi D, Koenig W, Pinter A, Korber A, et al. Impact of secukinumab on endothelial dysfunction and other cardiovascular disease parameters in psoriasis patients over 52 weeks. Journal of Investigative Dermatology 2019;139(5):1054-62. [DOI] [PubMed] [Google Scholar]
CHAMPION 2008 {published data only}
- Navarini AA, Poulin Y, Menter A, Gu Y, Teixeira HD. Analysis of body regions and components of PASI scores during adalimumab or methotrexate treatment for patients with moderate-to-severe psoriasis. Journal of Drugs in Dermatology 2014;13(5):554-62. [CENTRAL: CN-00993155] [PMID: ] [PubMed] [Google Scholar]
- Prussick R, Unnebrink K, Valdecantos WC. Efficacy of adalimumab compared with methotrexate or placebo stratified by baseline BMI in a randomized placebo-controlled trial in patients with psoriasis. Journal of Drugs in Dermatology 2015;14(8):864-8. [CENTRAL: CN-01132989] [PMID: ] [PubMed] [Google Scholar]
- Reich K, Signorovitch J, Ramakrishnan K, Yu AP, Wu EQ, Gupta SR, et al. Benefit-risk analysis of adalimumab versus methotrexate and placebo in the treatment of moderate to severe psoriasis: comparison of adverse event-free response days in the CHAMPION trial. Journal of the American Academy of Dermatology 2010;63(6):1011-8. [CENTRAL: CN-00791143] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Revicki D, Willian MK, Saurat JH, Papp KA, Ortonne JP, Sexton C, et al. Impact of adalimumab treatment on health-related quality of life and other patient-reported outcomes: results from a 16-week randomized controlled trial in patients with moderate to severe plaque psoriasis. British Journal of Dermatology 2008;158(3):549-57. [CENTRAL: CN-00628564] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Saurat JH, Langley RG, Reich K, Unnebrink K, Sasso EH, Kampman W. Relationship between methotrexate dosing and clinical response in patients with moderate to severe psoriasis: subanalysis of the CHAMPION study. British Journal of Dermatology 2011;165(2):399-406. [CENTRAL: CN-00800067] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Saurat JH, Stingl G, Dubertret L, Papp K, Langley RG, Ortonne JP, et al. Efficacy and safety results from the randomized controlled comparative study of adalimumab vs. methotrexate vs. placebo in patients with psoriasis (CHAMPION). British Journal of Dermatology 2008;158(3):558-66. [CENTRAL: CN-00628565] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaudhari 2001 {published data only}
- Chaudhari U, Romano P, Mulcahy LD, Dooley LT, Baker DG, Gottlieb AB. Efficacy and safety of infliximab monotherapy for plaque-type psoriasis: a randomised trial. Lancet 2001;357(9271):1842-7. [CENTRAL: CN-00348743] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gottlieb AB, Chaudhari U, Mulcahy LD, Li S, Dooley LT, Baker DG. Infliximab monotherapy provides rapid and sustained benefit for plaque-type psoriasis. Journal of the American Academy of Dermatology 2003;48(6):829-35. [CENTRAL: CN-00438058] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gottlieb AB, Masud S, Ramamurthi R, Abdulghani A, Romano P, Chaudhari U, et al. Pharmacodynamic and pharmacokinetic response to anti-tumor necrosis factor-alpha monoclonal antibody (infliximab) treatment of moderate to severe psoriasis vulgaris. Journal of the American Academy of Dermatology 2003;48(1):68-75. [CENTRAL: CN-00466030] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chladek 2005 {published data only}
- Chladek J, Grim J, Martinkova J, Simkova M, Vaneckova J. Low-dose methotrexate pharmacokinetics and pharmacodynamics in the therapy of severe psoriasis. Basic & Clinical Pharmacology & Toxicology 2005;96(3):247-8. [CENTRAL: CN-00513064] [PMID: ] [DOI] [PubMed] [Google Scholar]
CIMPACT 2018 {unpublished data only}
- Lebwohl M, Blauvelt A, Paul C, Sofen H, Weglowska J, Piguet V, et al. Certolizumab pegol for the treatment of chronic plaque psoriasis: Results through 48 weeks of a phase 3, multicenter, randomized, double-blind, etanercept- and placebo-controlled study (CIMPACT). Journal of the American Academy of Dermatology 2018;79(2):266-76.e5. [CENTRAL: CN-01665155] [DOI] [PubMed] [Google Scholar]
- NCT02346240. Efficacy and safety study of certolizumab pegol (CZP) versus active comparator and placebo in subjects with plaque psoriasis (PSO) (CIMPACT). clinicaltrials.gov/ct2/show/NCT02346240 (first received 20 January 2015). [CENTRAL: CN-01551710]
CIMPASI‐1 2018 {published data only}
- Gottlieb AB, Blauvelt A, Thaçi D, Leonardi CL, Poulin Y, Drew J, et al. Certolizumab pegol for the treatment of chronic plaque psoriasis: Results through 48 weeks from 2 phase 3, multicenter, randomized, double-blinded, placebo-controlled studies (CIMPASI-1 and CIMPASI-2). Journal of the American Academy of Dermatology 2018;79(2):302-14.e6. [CENTRAL: CN-01665156] [DOI] [PubMed] [Google Scholar]
- NCT02326298. An efficacy and safety study of two dose levels of certolizumab pegol (CZP) in subjects with plaque psoriasis (PSO). clinicaltrials.gov/show/nct02326298 (first received 29 December 2014). [CENTRAL: CN-01575600]
CIMPASI‐2 2018 {published and unpublished data}
- Gottlieb AB, Blauvelt A, Thaçi D, Leonardi CL, Poulin Y, Drew J, et al. Certolizumab pegol for the treatment of chronic plaque psoriasis: Results through 48 weeks from 2 phase 3, multicenter, randomized, double-blinded, placebo-controlled studies (CIMPASI-1 and CIMPASI-2). Journal of the American Academy of Dermatology 2018;79(2):302-14.e6. [CENTRAL: CN-01665156] [DOI] [PubMed] [Google Scholar]
- NCT02326272. A study to evaluate the efficacy and safety of two dose levels of certolizumab pegol (CZP) in subjects with plaque psoriasis (PSO) (CIMPASI-2). clinicaltrials.gov/ct2/show/NCT02326272 (first received 22 December 2014). [CENTRAL: CN-01575599]
CLARITY 2018 {unpublished data only}
- Anonymous. Secukinumab is superior to ustekinumab in clearing skin and improving quality of life in patients with moderate to severe plaque psoriasis: CLARITY, a randomized, controlled, phase 3b trial. Journal of the American Academy of Dermatology 2019;81(4 Supp 1):AB274. [Google Scholar]
- Bagel J, Blauvelt A, Nia J, Hashim P, Patekar M, Vera A, et al. Secukinumab maintains superiority over ustekinumab in clearing skin and improving quality of life in patients with moderate to severe plaque psoriasis: 52-week results from a double-blind phase 3b trial (CLARITY). Journal of the European Academy of Dermatology & Venereology 2020 May 4 [Epub ahead of print]. [DOI: 10.1111/jdv.16558] [DOI] [PMC free article] [PubMed]
- Bagel J, Nia J, Hashim P, Patekar M, De Vera A, Hugot S, et al. Secukinumab is superior to ustekinumab in clearing skin of patients with moderate-tosevere plaque psoriasis: CLARITY, a randomized, controlled, Phase IIIb trial. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Suppl 1):S27-8. [CENTRAL: CN-01713715] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagel J, Nia J, Hashim PW, Patekar M, De Vera A, Hugot S, et al. Secukinumab is superior to ustekinumab in clearing skin in patients with moderate to severe plaque psoriasis (16-week CLARITY results). Dermatology and Therapy 2018;8(4):571-9. [CENTRAL: CN-01667027] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02826603. Study of secukinumab compared to ustekinumab in subjects with plaque psoriasis (CLARITY). clinicaltrials.gov/ct2/show/NCT02826603 (first received 11 July 2016). [CENTRAL: CN-01506686]
CLEAR 2015 {published data only}
- Blauvelt A, Korman N, Mollon P, Zhao Y, Milutinovic M, You R, et al. Secukinumab treatment provides faster and more effective relief from patient-reported quality of life impact than ustekinumab in subjects with moderate to severe plaque psoriasis. Journal of Clinical and Aesthetic Dermatology 2017;10(5 Suppl 1):S15-6. [CENTRAL: CN-01713052] [Google Scholar]
- Blauvelt A, Reich K, Mehlis S, Vanaclocha F, Sofen H, Abramovits W, et al. Secukinumab demonstrates greater sustained improvements in daily activities and personal relationships than ustekinumab in patients with moderate-to-severe plaque psoriasis: 52-week results from the CLEAR study. Journal of the European Academy of Dermatology and Venereology 2017;31(10):1693-9. [CENTRAL: CN-01615823] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blauvelt A, Reich K, Tsai TF, Tyring S, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate-to-severe plaque psoriasis up to 1 year: results from the CLEAR study. Journal of the American Academy of Dermatology 2017;76(1):60-9.e9. [CENTRAL: CN-01368612] [DOI] [PubMed] [Google Scholar]
- Herranz Pinto P, Rivera R, Blauvelt A, Thaçi D, Oliver Vigueras J. Secukinumab 300mg is more efficacious than ustekinumab 90mg: analysis of the CLEAR study. Journal of Clinical and Aesthetic Dermatology 2017;10(5 Suppl 1):S18-9. [CENTRAL: CN-01713059] [Google Scholar]
- Spelman L, Pinto PH, Rivera R, Blauvelt A, Thaçi D, Vigueras JO. Secukinumab 300mgs is more efficacious than ustekinumab 90mgs: analysis of patients with body weights over 100kg from the CLEAR study. Australasian Journal of Dermatology 2017;58(Suppl 1):86-7. [CENTRAL: CN-01378828] [Google Scholar]
- Thaçi D, Blauvelt A, Reich K, Tsai TF, Vanaclocha F, Kingo K, et al. Secukinumab delivers greater improvement in health-related quality of life compared to ustekinumab in subjects with moderate-to-severe plaque psoriasis: 16-week data from the CLEAR study. Journal of Clinical and Aesthetic Dermatology 2016;9(5 Suppl 1):S17-8. [CENTRAL: CN-01713053] [Google Scholar]
- Thaçi D, Blauvelt A, Reich K, Tsai TF, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. Journal of the American Academy of Dermatology 2015;73(3):400-9. [CENTRAL: CN-01090628] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dogra 2012 {published data only}
- Dogra S, Krishna V, Kanwar AJ. Efficacy and safety of systemic methotrexate in two fixed doses of 10 mg or 25 mg orally once weekly in adult patients with severe plaque-type psoriasis: a prospective, randomized, double-blind, dose-ranging study. Clinical and Experimental Dermatology 2012;37(7):729-34. [CENTRAL: CN-00879485] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dogra 2013 {published data only}
- Dogra S, Jain A, Kanwar AJ. Efficacy and safety of acitretin in three fixed doses of 25, 35 and 50 mg in adult patients with severe plaque type psoriasis: A randomized, double blind, parallel group, dose ranging study. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(3):e305-11. [CENTRAL: CN-00911790] [EMBASE: 2013118368] [DOI] [PubMed] [Google Scholar]
Dubertret 1989 {published data only}
- Dubertret L, Perussel M, Robiola O, Feutren G. Cyclosporin in psoriasis. A long-term randomized study on 37 patients. Acta Dermato-Venereologica, Supplement 1989;69(146):136. [CENTRAL: CN-00064909] [PMID: ] [PubMed] [Google Scholar]
ECLIPSE 2019 {published data only}
- NCT03090100. A study to evaluate the comparative efficacy of CNTO 1959 (guselkumab) and secukinumab for the treatment of moderate to severe plaque-type psoriasis (ECLIPSE). clinicaltrials.gov/show/nct03090100 (first received 24 March 2017).
- Reich K, Armstrong AW, Langley RG, Flavin S, Randazzo B, Li S, et al. Guselkumab versus secukinumab for the treatment of moderate-to-severe psoriasis (ECLIPSE): results from a phase 3, randomised controlled trial. Lancet 2019;394(10201):831-9. [DOI] [PubMed] [Google Scholar]
EGALITY 2017 {published data only}
- Gerdes S, Thaçi D, Griffiths CE, Arenberger P, Poetzl J, Wuerth G, et al. Multiple switches between GP2015, an etanercept biosimilar, with originator product do not impact efficacy, safety and immunogenicity in patients with chronic plaque-type psoriasis: 30-week results from the phase 3, confirmatory EGALITY study. Journal of the European Academy of Dermatology and Venereology : JEADV 2018;32(3):420-7. [CENTRAL: CN-01643364] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths CE, Reich K, Thaçi D, Gerdes S, Arenberger P, Kingo K, et al. Switching treatments of etanercept biosimilar GP2015 with originator product does not impact efficacy, safety and immunogenicity in patients with chronic plaque-type psoriasis. Journal of Investigative Dermatology 2017;137(10 Suppl 2):S193. [CENTRAL: CN-01416626] [Google Scholar]
- Griffiths CE, Thaçi D, Gerdes S, Arenberger P, Pulka G, Kingo K, et al. The EGALITY study: a confirmatory, randomized, double-blind study comparing the efficacy, safety and immunogenicity of GP2015, a proposed etanercept biosimilar, vs. the originator product in patients with moderate-to-severe chronic plaque-type psoriasis. British Journal of Dermatology 2017;176(4):928-38. [CENTRAL: CN-01424735] [DOI] [PubMed] [Google Scholar]
- NCT01891864. Study to demonstrate equivalent efficacy and to compare safety of biosimilar etanercept (GP2015) and Enbrel (EGALITY). clinicaltrials.gov/show/nct01891864 (first received 3 July 2013). [CENTRAL: CN-01597476]
Elewski 2016 {published data only}
- Elewski BE, Okun MM, Papp K, Baker CS, Crowley JJ, Guillet G, et al. Adalimumab for nail psoriasis: efficacy and safety from the first 26 weeks of a phase 3, randomized, placebo-controlled trial. Journal of the American Academy of Dermatology 2018;78(1):90-99.e1. [CENTRAL: CN-01443156] [DOI: 10.1016/j.jaad.2017.08.029] [DOI] [PubMed] [Google Scholar]
- Elewski BE, Rich PA, Behrens F, Guillet G, Geng Z, Reyes Servin O. Primary efficacy and safety of adalimumab in nail psoriasis from the first 26 weeks of a phase-3, randomized, placebo-controlled trial with subanalysis in patients with and without psoriatic arthritis. Annals of the Rheumatic Diseases 2017;76(Suppl 2):1319-20. [CENTRAL: CN-01467694] [DOI: 10.1136/annrheumdis-2017-eular.2148] [DOI] [Google Scholar]
- Elewski BE, Rich PA, Behrens F, Guillet G, Geng Z, Servin OR. Primary efficacy and safety of adalimumab in nail psoriasis from the first 26 weeks of a phase-3, randomized, placebo-controlled trial with subanalysis in patients with and without psoriatic arthritis. Acta Dermato-Venereologica 2018;98(Suppl 219):26-7. [CENTRAL: CN-01620195] [Google Scholar]
- Elewski BE, Rich PA, Okun MM, Papp K, Baker CS, Crowley JJ, et al. Adalimumab for nail psoriasis: efficacy and safety from the first 26 weeks of a Phase-3, randomized, placebo-controlled trial. Journal of the European Academy of Dermatology and Venereology: JEADV 2016;30(Suppl 6):65. [CENTRAL: CN-01786943] [EMBASE: 611235503] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ellis 1991 {published data only}
- Ellis CN, Fradin MS, Messana JM, Brown MD, Siegel MT, Hartley AH, et al. Cyclosporine for plaque-type psoriasis. Results of a multidose, double-blind trial. New England Journal of Medicine 1991;324(5):277-84. [CENTRAL: CN-00072304] [PMID: ] [DOI] [PubMed] [Google Scholar]
Engst 1994 {published data only}
- Engst RH, Bubl R, Huber J, Schober C, Jessberger B. Long-term cyclosporin A for psoriasis. Acta Dermatovenerologica Alpina, Panonica et Adriatica 1994;3(4):188-92. [CENTRAL: CN-00178929] [EMBASE: 1995061459] [Google Scholar]
ERASURE 2014 {published data only}
- Gottlieb AB, Langley RG, Philipp S, Sigurgeirsson B, Blauvelt A, Martin R, et al. Secukinumab improves physical function in subjects with plaque psoriasis and psoriatic arthritis: Results from two randomized, phase 3 trials. Journal of Drugs in Dermatology 2015;14(8):821-33. [CENTRAL: CN-01132993] [PMID: ] [PubMed] [Google Scholar]
- Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. Secukinumab in plaque psoriasis--results of two phase 3 trials. New England Journal of Medicine 2014;371(4):326-38. [CENTRAL: CN-00999505] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Ohtsuki M, Morita A, Abe M, Takahashi H, Seko N, Karpov A, et al. Secukinumab efficacy and safety in Japanese patients with moderate-to-severe plaque psoriasis: Subanalysis from ERASURE, a randomized, placebo-controlled, phase 3 study. Journal of Dermatology 2014;41(12):1039-46. [CENTRAL: CN-01037251] [PMID: ] [DOI] [PubMed] [Google Scholar]
ESTEEM‐1 2015 {published data only}
- Bissonnette R, Pariser DM, Wasel NR, Goncalves J, Day RM, Chen R, et al. Apremilast, an oral phosphodiesterase-4 inhibitor, in the treatment of palmoplantar psoriasis: Results of a pooled analysis from phase II PSOR-005 and phase III Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis (ESTEEM) clinical trials in patients with moderate to severe psoriasis. Journal of the American Academy of Dermatology 2016;75(1):99-105. [CENTRAL: CN-01470982] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Papp K, Reich K, Leonardi CL, Kircik L, Chimenti S, Langley RG, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: Results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). Journal of the American Academy of Dermatology 2015;73(1):37-49. [CENTRAL: CN-01085116] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Rich P, Gooderham M, Bachelez H, Goncalves J, Day RM, Chen R, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in patients with difficult-to-treat nail and scalp psoriasis: Results of 2 phase III randomized, controlled trials (ESTEEM 1 and ESTEEM 2). Journal of the American Academy of Dermatology 2016;74(1):134-42. [CENTRAL: CN-01127546] [PMID: ] [DOI] [PubMed] [Google Scholar]
ESTEEM‐2 2015 {published data only}
- Paul C, Cather J, Gooderham M, Poulin Y, Mrowietz U, Ferrandiz C, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). British Journal of Dermatology 2015;173(6):1387-99. [CENTRAL: CN-01133855] [PMID: ] [DOI] [PubMed] [Google Scholar]
EXPRESS 2005 {published data only}
- Reich K, Nestle FO, Papp K, Ortonne JP, Evans R, Guzzo C, et al. Infliximab induction and maintenance therapy for moderate-to-severe psoriasis: a phase III, multicentre, double-blind trial. Lancet 2005;366(9494):1367-74. [CENTRAL: CN-00531178] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Reich K, Nestle FO, Papp K, Ortonne JP, Wu Y, Bala M, et al. Improvement in quality of life with infliximab induction and maintenance therapy in patients with moderate-to-severe psoriasis: a randomized controlled trial. British Journal of Dermatology 2006;154(6):1161-8. [CENTRAL: CN-00565410] [PMID: ] [DOI] [PubMed] [Google Scholar]
EXPRESS‐II 2007 {published data only}
- Feldman SR, Gottlieb AB, Bala M, Wu Y, Eisenberg D, Guzzo C, et al. Infliximab improves health-related quality of life in the presence of comorbidities among patients with moderate-to-severe psoriasis. British Journal of Dermatology 2008;159(3):704-10. [CENTRAL: CN-00668311] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Menter A, Feldman SR, Weinstein GD, Papp K, Evans R, Guzzo C, et al. A randomized comparison of continuous vs. intermittent infliximab maintenance regimens over 1 year in the treatment of moderate-to-severe plaque psoriasis. Journal of the American Academy of Dermatology 2007;56(1):31.e1-15. [CENTRAL: CN-00576883] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Reich K, Nestle FO, Wu Y, Bala M, Eisenberg D, Guzzo C, et al. Infliximab treatment improves productivity among patients with moderate-to-severe psoriasis. European Journal of Dermatology 2007;17(5):381-6. [CENTRAL: CN-00699412] [DOI] [PubMed] [Google Scholar]
- Reich K, Ortonne JP, Kerkmann U, Wang Y, Saurat JH, Papp K, et al. Skin and nail responses after 1 year of infliximab therapy in patients with moderate-to-severe psoriasis: a retrospective analysis of the EXPRESS trial. Dermatology 2010;221(2):172-8. [CENTRAL: CN-01628937] [PMID: 20628238] [DOI] [PubMed] [Google Scholar]
Fallah Arani 2011 {published data only}
- Fallah Arani S, Neumann H, Hop WC, Thio HB. Fumarates vs. methotrexate in moderate to severe chronic plaque psoriasis: a multicentre prospective randomized controlled clinical trial. British Journal of Dermatology 2011;164(4):855-61. [CENTRAL: CN-00785701] [PMID: ] [DOI] [PubMed] [Google Scholar]
- ISRCTN76608307. A comparison of the efficacy of oral fumarate and methotrexate therapy in the treatment of severe psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=ISRCTN76608307 (first received 1 September 2006).
FEATURE 2015 {published data only}
- Blauvelt A, Prinz JC, Gottlieb AB, Kingo K, Sofen H, Ruer-Mulard M, et al. Secukinumab administration by pre-filled syringe: efficacy, safety and usability results from a randomized controlled trial in psoriasis (FEATURE). British Journal of Dermatology 2015;172(2):484-93. [CENTRAL: CN-01052626] [PMID: ] [DOI] [PubMed] [Google Scholar]
FIXTURE 2014 {published data only}
- Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. Secukinumab in plaque psoriasis--results of two phase 3 trials. New England Journal of Medicine 2014;371(4):326-38. [CENTRAL: CN-00999505] [PMID: ] [DOI] [PubMed] [Google Scholar]
Flytström 2008 {published data only}
- Flytström I, Stenberg B, Svensson A, Bergbrant IM. Methotrexate vs. ciclosporin in psoriasis: effectiveness, quality of life and safety. A randomized controlled trial. British Journal of Dermatology 2008;158(1):116-21. [CENTRAL: CN-00628309] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gisondi 2008 {published data only}
- Gisondi P, Del Giglio M, Cotena C, Girolomoni G. Combining etanercept and acitretin in the therapy of chronic plaque psoriasis: a 24-week, randomized, controlled, investigator-blinded pilot trial. British Journal of Dermatology 2008;158(6):1345-9. [CENTRAL: CN-00638916] [PMID: ] [DOI] [PubMed] [Google Scholar]
Goldfarb 1988 {published data only}
- Goldfarb MT, Ellis CN, Gupta AK, Tincoff T, Hamilton TA, Voorhees JJ. Acitretin improves psoriasis in a dose-dependent fashion. Journal of the American Academy of Dermatology 1988;18(4 Pt 1):655-62. [CENTRAL: CN-00053926] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gupta AK, Goldfarb MT, Ellis CN, Voorhees JJ. Side-effect profile of acitretin therapy in psoriasis. Journal of the American Academy of Dermatology 1989;20(6):1088-93. [CENTRAL: CN-00061373] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gordon 2006 {published data only}
- Gordon KB, Langley RG, Leonardi C, Toth D, Menter MA, Kang S, et al. Clinical response to adalimumab treatment in patients with moderate to severe psoriasis: double-blind, randomized controlled trial and open-label extension study. Journal of the American Academy of Dermatology 2006;55(4):598-606. [CENTRAL: CN-00568251] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Shikiar R, Heffernan M, Langley RG, Willian MK, Okun MM, Revicki DA. Adalimumab treatment is associated with improvement in health-related quality of life in psoriasis: patient-reported outcomes from a phase II randomized controlled trial. Journal of Dermatological Treatment 2007;18(1):25-31. [CENTRAL: CN-00579275] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Shikiar R, Willian MK, Okun MM, Thompson CS, Revicki DA. The validity and responsiveness of three quality of life measures in the assessment of psoriasis patients: Results of a phase II study. Health and Quality of Life Outcomes 2006;27(4):71. [CENTRAL: CN-00576575] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gordon X‐PLORE 2015 {published data only}
- Gordon KB, Duffin KC, Bissonnette R, Prinz JC, Wasfi Y, Li S, et al. A phase 2 trial of guselkumab versus adalimumab for plaque psoriasis. New England Journal of Medicine 2015;373(2):136-44. [CENTRAL: CN-01076768] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gottlieb 2003a {published data only}
- Gottlieb AB, Matheson RT, Lowe N, Krueger GG, Kang S, Goffe BS, et al. A randomized trial of etanercept as monotherapy for psoriasis. Archives of Dermatology 2003;139(12):1627-32. [CENTRAL: CN-00459604] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gottlieb 2004a {published data only}
- Feldman SR, Gordon KB, Bala M, Evans R, Li S, Dooley LT, et al. Infliximab treatment results in significant improvement in the quality of life of patients with severe psoriasis: a double-blind placebo-controlled trial. British Journal of Dermatology 2005;152(5):954-60. [CENTRAL: CN-00513174] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gottlieb AB, Evans R, Li S, Dooley LT, Guzzo CA, Baker D, et al. Infliximab induction therapy for patients with severe plaque-type psoriasis: a randomized, double-blind, placebo-controlled trial. Journal of the American Academy of Dermatology 2004;51(4):534-42. [CENTRAL: CN-00501751] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gottlieb 2011 {published data only}
- Gottlieb AB, Leonardi C, Kerdel F, Mehlis S, Olds M, Williams DA. Efficacy and safety of briakinumab vs. etanercept and placebo in patients with moderate to severe chronic plaque psoriasis. British Journal of Dermatology 2011;165(3):652-60. [CENTRAL: CN-00811739] [PMID: ] [DOI] [PubMed] [Google Scholar]
Gottlieb 2012 {published data only}
- Gottlieb AB, Langley RG, Strober BE, Papp KA, Klekotka P, Creamer K, et al. A randomized, double-blind, placebo-controlled study to evaluate the addition of methotrexate to etanercept in patients with moderate to severe plaque psoriasis. British Journal of Dermatology 2012;167(3):649-57. [CENTRAL: CN-00842357] [22533447] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gurel 2015 {published data only}
- Gurel G, Saracotlu ZN, Aksu AE. A single-blind study comparing acitretin and narrow-band UVB with the combination of placebo and narrow-band UVB in the treatment of plaque-type psoriasis [Plak tip psoriasis tedavisinde asitretin ve dar bant UVB ile plasebo ve dar bant UVB kombinasyonunun karsilastirilditi tek kor calisma]. Türkderm 2015;49(1):2-6. [CENTRAL: CN-01102298] [EMBASE: 2015064189] [Google Scholar]
Heydendael 2003 {published data only}
- Heydendael VM, Spuls PI, Opmeer BC, De Borgie CA, Reitsma JB, Goldschmidt WF, et al. Methotrexate versus cyclosporine in moderate-to-severe chronic plaque psoriasis. New England Journal of Medicine 2003;349(7):658-65. [CENTRAL: CN-00439969] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Opmeer BC, Heydendael VM, De Borgie CA, Spuls PI, Bossuyt PM, Bos JD, et al. Costs of treatment in patients with moderate to severe plaque psoriasis: economic analysis in a randomized controlled comparison of methotrexate and cyclosporine. Archives of Dermatology 2004;140(6):685-90. [CENTRAL: CN-00468098] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hunter 1963 {published data only}
- Hunter GA, Turner AN. Methotrexate in the treatment of psoriasis: a controlled clinical trial. Australasian Journal of Dermatology 1963;7(2):91-2. [CENTRAL: CN-01437408] [PMID: ] [DOI] [PubMed] [Google Scholar]
Igarashi 2012 {published data only}
- Igarashi A, Kato T, Kato M, Song M, Nakagawa H, Japanese Ustekinumab Study Group. Efficacy and safety of ustekinumab in Japanese patients with moderate-to-severe plaque-type psoriasis: Long-term results from a phase 2/3 clinical trial. Journal of Dermatology 2012;39(3):242-52. [CENTRAL: CN-00860708] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Nakagawa H, Schenkel B, Kato M, Kato T, Igarashi A, Japanese Ustekinumab Study Group. Impact of ustekinumab on health-related quality of life in Japanese patients with moderate-to-severe plaque psoriasis: results from a randomized, double-blind, placebo-controlled phase 2/3 trial. Journal of Dermatology 2012;39(9):761-9. [CENTRAL: CN-00860068] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ikonomidis 2017 {published data only}
- Ikonomidis I, Papadavid E, Makavos G, Andreadou I, Varoudi M, Gravanis K, et al. Lowering interleukin-12 activity improves myocardial and vascular function compared with tumor necrosis factor-a antagonism or cyclosporine in psoriasis. Circulation. Cardiovascular imaging 2017;10(9):e006283. [CENTRAL: CN-01412809] [DOI] [PubMed] [Google Scholar]
- Ikonomidis I, Varoudi M, Makavos G, Papadavid E, Kapniari I, Andreadou I, et al. Greater improvement of coronary artery function, left ventricular deformation and twisting by treatment with IL-17A antagonist compared to Cyclosporine in psoriasis. European Heart Journal 2017;38(Suppl 1):688. [CENTRAL: CN-01468831] [Google Scholar]
- Ikonomidis I, Varoudi M, Makavos G, Papadavid E, Kapniari I, Andreadou I, et al. Treatment with IL-17A antagonist results in a greater improvement of coronary artery function, left ventricular deformation and twisting than cyclosporine in psoriasis. European Heart Journal - Cardiovascular Imaging 2017;18(Suppl 3):iii341. [CENTRAL: CN-01452103] [DOI: 10.1093/ehjci/jex298] [DOI] [Google Scholar]
IMMerge 2021 {published data only}
- NCT03478787. Risankizumab versus secukinumab for subjects with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct03478787 (first received 27 March 2018).
- Warren RB, Blauvelt A, Poulin Y, Beeck S, Kelly M, Wu T, et al. Efficacy and safety of risankizumab vs. secukinumab in patients with moderate-to-severe plaque psoriasis (IMMerge): Results from a phase 3, randomised, open-label, efficacy assessor-blinded clinical trial. British Journal of Dermatology 2021;184(1):50-9. [DOI: 10.1111/bjd.19341] [DOI] [PMC free article] [PubMed] [Google Scholar]
IMMvent 2019 {unpublished data only}
- EUCTR2015-003623-65. BI 655066 (risankizumab) versus adalimumab in a randomised, double blind, parallel group trial in moderate to severe plaque psoriasis to assess safety and efficacy after 16 weeks of treatment and after inadequate adalimumab treatment response (IMMvent) - BI 655066 (risankizumab) versus adalimumab. www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number%3A2015-003623-65/EUCTR2015-003623-65 (first received 17 May 2016). [CENTRAL: CN-01855355]
- NCT02694523. BI 655066/ABBV-066 (risankizumab) compared to active comparator (adalimumab) in patients with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/nct02694523 (first received 29 February 2016). [CENTRAL: CN-01556126]
- Reich K, Gooderham M, Thaçi D, Crowley JJ, Ryan C, Krueger JG, et al. Risankizumab compared with adalimumab in patients with moderate-to-severe plaque psoriasis (IMMvent): a randomised, double-blind, active-comparator-controlled phase 3 trial. Lancet 2019;394(10198):576-86. [DOI: 10.1016/S0140-6736(19)30952-3] [DOI] [PubMed] [Google Scholar]
IXORA‐P 2018 {unpublished data only}
- Langley RG, Papp K, Gooderham M, Zhang L, Mallinckrodt C, Agada N, et al. Efficacy and safety of continuous every-2-week dosing of ixekizumab over 52 weeks in patients with moderate-to-severe plaque psoriasis in a randomized phase III trial (IXORA-P). British Journal of Dermatology 2018;178(6):1315-23. [CENTRAL: CN-01606242] [DOI] [PubMed] [Google Scholar]
- NCT02513550. A study comparing different dosing regimens of ixekizumab (LY2439821) in participants with moderate to severe plaque psoriasis (IXORA-P). clinicaltrials.gov/ct2/show/NCT02513550 (first received 30 July 2015). [CENTRAL: CN-01491284]
- Papp K, Orasan RI, Polzer P, Hennege C, Nica RD, Wilhelm S, et al. Absolute and relative pasi improvements with ixekizumab treatment: results at week 12 from IXORA-P. Acta Dermato-Venereologica 2018;98(Suppl 219):44-5. [CENTRAL: CN-01620199] [Google Scholar]
IXORA‐R 2020 {published data only}
- Blauvelt A, Leonardi C, Elewski B, Crowley JJ, Guenther LC, Gooderham M, et al. A head-to-head comparison of ixekizumab vs. guselkumab in patients with moderate-to-severe plaque psoriasis: 24-week efficacy and safety results from a randomized, double-blinded trial. British Journal of Dermatology 2020 Sep 2 [Epub ahead of print]. [DOI: 10.1111/bjd.19509] [DOI] [PMC free article] [PubMed]
- Blauvelt A, Papp K, Gottlieb A, Jarell A, Reich K, Maari C, et al. A head-to-head comparison of ixekizumab versus guselkumab in patients with moderate-to-severe plaque psoriasis: 12-week efficacy, safety, and speed of response from a randomized, double-blinded trial. British Journal of Dermatology 2020;182(6):1348-58. [DOI: 10.1111/bjd.18851] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT03573323. A study of ixekizumab (LY2439821) compared to guselkumab in participants with moderate-to-severe plaque psoriasis (IXORA-R). clinicaltrials.gov/show/nct03573323 (first received 29 June 2018).
IXORA‐S 2017 {unpublished data only}
- Anonymous. Rapid clinical response predicts consistent long-term response in patients with moderate-to-severe psoriasis: Ixekizumab vs. ustekinumab. Journal of the American Academy of Dermatology 2019;81(4 Suppl 1):AB113. [Google Scholar]
- Blauvelt A, Lomaga M, Burge R, Zhu B, Henneges C, Shen W, et al. Ixekizumab provides greater cumulative benefits versus ustekinumab over 24 weeks for patients with moderate-to-severe psoriasis in a randomized, double-blind phase 3b clinical trial. Acta Dermato-Venereologica 2018;98(Suppl 219):55-6. [CENTRAL: CN-01620173] [Google Scholar]
- Blauvelt A, Lomaga M, Burge R, Zhu B, Shen W, Shrom D, et al. Greater cumulative benefits from ixekizumab versus ustekinumab treatment over 52 weeks for patients with moderate-to-severe psoriasis in a randomized, double-blinded phase 3b clinical trial. Journal of Dermatological Treatment 2020;31(2):141-6. [DOI] [PubMed] [Google Scholar]
- Burge RT, Papadimitropoulos M, Henneges C, Garcia EG, Romiti R. Ixekizumab treatment leads to early resolution of bothersome symptoms versus ustekinumab. Value in Health 2017;20(9):A902. [CENTRAL: CN-01431388] [Google Scholar]
- Burkhardt N, Reich K, Lomaga M, Henneges C, Dossenbach M, Wilhelm S, et al. Efficacy and safety of ixekizumab (IXE) compared to ustekinumab (UST) in patients with moderate-to-severe plaque psoriasis: a randomised head-to-head trial. Australasian Journal of Dermatology 2017;58(Suppl 1):43. [CENTRAL: CN-01378805] [Google Scholar]
- Burkhardt N, Wilhelm S, Riedl E, Kelin K, Henneges C, Smith SD, et al. Comparison of ixekizumab with ustekinumab in patients with baseline PASI>15 and/or at-least 3-previous-non-biologic-therapies-treatment-failures: 24-week post-hoc-analysis from a randomized trial (IXORA-S;NCT02561806). Australasian Journal of Dermatology 2018;59(Suppl 1):41. [CENTRAL: CN-01606958] [Google Scholar]
- Ghislain PD, Conrad C, Dutronc Y, Henneges C, Calderon DS, Vincent M, et al. Comparison of ixekizumab and ustekinumab efficacy in the treatment of nail lesions of patients with moderate-to-severe plaque psoriasis: 24-week data from a phase 3 trial. Arthritis and Rheumatology 2017;69(Suppl 10):1827. [Google Scholar]
- NCT02561806. A study of Ixekizumab (LY2439821) in participants with moderate-to-severe plaque psoriasis. clinicaltrials.gov/ct2/show/NCT02561806 (first received 25 September 2015). [CENTRAL: CN-01492565]
- Paul C, Griffiths CE, Van de Kerkhof PCM, Puig L, Dutronc Y, Henneges C, et al. Ixekizumab provides superior efficacy compared with ustekinumab over 52 weeks of treatment: results from IXORA-S, a phase 3 study. Journal of the American Academy of Dermatology 2019;80(1):70-9.e3. [CENTRAL: CN-01913461] [DOI] [PubMed] [Google Scholar]
- Paul C, Puig L, Dutronc Y, Henneges C, Reich K. Consistency of response across subgroups of patients with moderate-to-severe plaque psoriasis following 52 weeks of treatment with ixekizumab compared to ustekinumab. Journal of Investigative Dermatology 2018;138(5 Suppl 1):S81. [CENTRAL: CN-01605382] [Google Scholar]
- Paul C, Van De Kerkhof P, Dutronc Y, Henneges C, Dossenbach M, Hollister K, et al. 52-week results from IXORA-S: a randomized head-to-head trial of ixekizumab and ustekinumab in patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology 2017;177(5):e293. [CENTRAL: CN-01452513] [Google Scholar]
- Reich K, Pinter A, Lacour JP, Ferrandiz C, Micali G, French LE, et al. Comparison of ixekizumab with ustekinumab in moderate-to-severe psoriasis: 24-week results from IXORA-S, a phase III study. British Journal of Dermatology 2017;177(4):1014-23. [CENTRAL: CN-01393820] [DOI] [PubMed] [Google Scholar]
Jin 2017 {published data only}
- Huang YW, Tsai TF. Efficacy of tofacitinib in patients with moderate-to-severe psoriasis who had inadequate responses to prior biologics. Dermatologica Sinica 2019;37(4):205-8. [Google Scholar]
- Jin T, Sun Z, Chen X, Wang Y, Li R, Ji S, et al. Serum human beta-defensin-2 is a possible biomarker for monitoring response to JAK inhibitor in psoriasis patients. Dermatology 2017;233(2-3):164-9. [CENTRAL: CN-01622175] [DOI] [PubMed] [Google Scholar]
JUNCTURE 2015 {published data only}
- Lacour JP, Paul C, Jazayeri S, Papanastasiou P, Xu C, Nyirady J, et al. Secukinumab administration by autoinjector maintains reduction of plaque psoriasis severity over 52 weeks: results of the randomized controlled JUNCTURE trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2017;31(5):847-56. [CENTRAL: CN-01342022] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Paul C, Lacour JP, Tedremets L, Kreutzer K, Jazayeri S, Adams S, et al. Efficacy, safety and usability of secukinumab administration by autoinjector/pen in psoriasis: A randomized, controlled trial (JUNCTURE). Journal of the European Academy of Dermatology and Venereology : JEADV 2015;29(6):1082-90. [CENTRAL: CN-01043227] [PMID: ] [DOI] [PubMed] [Google Scholar]
Khatri 2016 {published data only}
- Khatri S, Amir Y, Min M, Goldblum O, Solotkin K, Yang F, et al. Early onset of clinical improvement with ixekizumab in patients with moderate-to-severe plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;30(S6):73-4. [CENTRAL: CN-01786974] [EMBASE: 611235569] [Google Scholar]
- Khattri S, Goldblum O, Solotkin K, Amir Y, Min MS, Ridenour T, et al. Early onset of clinical improvement with ixekizumab in a randomized, open-label study of patients with moderate-to-severe plaque psoriasis. Journal of Clinical and Aesthetic Dermatology 2018;11(5):33-7. [CENTRAL: CN-01610571] [PMC free article] [PubMed] [Google Scholar]
Krueger 2007 {published data only}
- Krueger GG, Langley RG, Leonardi C, Yeilding N, Guzzo C, Wang Y, et al. A human interleukin-12/23 monoclonal antibody for the treatment of psoriasis. New England Journal of Medicine 2007;356(6):580-92. [CENTRAL: CN-00575216] [PMID: ] [DOI] [PubMed] [Google Scholar]
Krueger 2016a {published data only}
- Krueger J, Clark JD, Suarez-Farinas M, Fuentes-Duculan J, Cueto I, Wang CQ, et al. Tofacitinib attenuates pathologic immune pathways in patients with psoriasis: A randomized phase 2 study. Journal of Allergy and Clinical Immunology 2016;137(4):1079-90. [CENTRAL: CN-01153710] [PMID: ] [DOI] [PubMed] [Google Scholar]
Laburte 1994 {published data only}
- Laburte C, Grossman R, Abi-Rached J, Abeywickrama KH, Dubertret L. Efficacy and safety of oral cyclosporin A (CyA; Sandimmun) for long-term treatment of chronic severe plaque psoriasis. British Journal of Dermatology 1994;130(3):366-75. [CENTRAL: CN-00100273] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lee 2016 {published data only}
- Lee JH, Youn JI, Kim TY, Choi JH, Park CJ, Choe YB, et al. A multicenter, randomized, open-label pilot trial assessing the efficacy and safety of etanercept 50 mg twice weekly followed by etanercept 25 mg twice weekly, the combination of etanercept 25 mg twice weekly and acitretin, and acitretin alone in patients with moderate to severe psoriasis. BMC Dermatology 2016;16(1):11. [CENTRAL: CN-01177229] [PMID: ] [DOI] [PMC free article] [PubMed]
Leonardi 2003 {published data only}
- Feldman SR, Kimball AB, Krueger GG, Woolley JM, Lalla D, Jahreis A. Etanercept improves the health-related quality of life of patients with psoriasis: results of a phase III randomized clinical trial. Journal of the American Academy of Dermatology 2005;53(5):887-9. [CENTRAL: CN-00561361] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gordon KB, Gottlieb AB, Leonardi CL, Elewski BE, Wang A, Jahreis A, et al. Clinical response in psoriasis patients discontinued from and then reinitiated on etanercept therapy.[Erratum appears in J Dermatolog Treat. 2006;17(3):192]. Journal of Dermatological Treatment 2006;17(1):9-17. [CENTRAL: CN-00555056] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Krueger GG, Elewski B, Papp K, Wang A, Zitnik R, Jahreis A. Patients with psoriasis respond to continuous open-label etanercept treatment after initial incomplete response in a randomized, placebo-controlled trial. Journal of the American Academy of Dermatology 2006;54(3 Suppl 2):S112-9. [CENTRAL: CN-01625470] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Leonardi CL, Powers JL, Matheson RT, Goffe BS, Zitnik R, Wang A, et al. Etanercept as monotherapy in patients with psoriasis. New England Journal of Medicine 2003;349(21):2014-22. [CENTRAL: CN-00459025] [14627786] [DOI] [PubMed] [Google Scholar]
Leonardi 2012 {published data only}
- Edson-Heredia E, Banerjee S, Zhu B, Maeda-Chubachi T, Cameron GS, Shen W, et al. A high level of clinical response is associated with improved patient-reported outcomes in psoriasis: analyses from a phase 2 study in patients treated with ixekizumab. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;30(5):864-5. [CENTRAL: CN-01601237] [PMID: 25773781 ] [DOI] [PubMed] [Google Scholar]
- Gordon KB, Leonardi CL, Lebwohl M, Blauvelt A, Cameron GS, Braun D, et al. A 52-week, open-label study of the efficacy and safety of ixekizumab, an anti-interleukin-17A monoclonal antibody, in patients with chronic plaque psoriasis. Journal of the American Academy of Dermatology 2014;71(6):1176-82. [CENTRAL: CN-01091643] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Langley RG, Rich P, Menter A, Krueger G, Goldblum O, Dutronc Y, et al. Improvement of scalp and nail lesions with ixekizumab in a phase 2 trial in patients with chronic plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2015;29(9):1763-70. [CENTRAL: CN-01089988] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Leonardi C, Matheson R, Zachariae C, Cameron G, Li L, Edson-Heredia E, et al. Anti-interleukin-17 monoclonal antibody ixekizumab in chronic plaque psoriasis. New England Journal of Medicine 2012;366(13):1190-9. [CENTRAL: CN-00814008] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tham LS, Tang CC, Choi SL, Satterwhite JH, Cameron GS, Banerjee S. Population exposure-response model to support dosing evaluation of ixekizumab in patients with chronic plaque psoriasis. Journal of Clinical Pharmacology 2014;54(10):1117-24. [CENTRAL: CN-01048421] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Zhu B, Edson-Heredia E, Cameron GS, Shen W, Erickson J, Shrom D, et al. Early clinical response as a predictor of subsequent response to ixekizumab treatment: results from a phase II study of patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology 2013;169(9):1337-41. [CENTRAL: CN-01121535] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Zhu B, Edson-Heredia E, Guo J, Maeda-Chubachi T, Shen W, Kimball AB. Itching is a significant problem and a mediator between disease severity and quality of life for patients with psoriasis: Results from a randomized controlled trial. British Journal of Dermatology 2014;171(5):1215-9. [CENTRAL: CN-01036585] [PMID: ] [DOI] [PubMed] [Google Scholar]
LIBERATE 2017 {published data only}
- Reich K, Gooderham M, Bewley A, Green L, Soung J, Petric R, et al. Safety and efficacy of apremilast through 104 weeks in patients with moderate to severe psoriasis who continued on apremilast or switched from etanercept treatment: findings from the LIBERATE study. Journal of the European Academy of Dermatology and Venereology : JEADV 2018;32(3):397-402. [CENTRAL: CN-01643202] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reich K, Gooderham M, Green L, Bewley A, Zhang Z, Khanskaya I, et al. The efficacy and safety of apremilast, etanercept, and placebo, in patients with moderate to severe plaque psoriasis: 52-week results from a phase 3b, randomized, placebo-controlled trial (LIBERATE). Journal of the European Academy of Dermatology and Venereology : JEADV 2017;31(3):507-17. [CENTRAL: CN-01285623] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
LOTUS 2013 {published data only}
- Zheng M, Zhu X-J, Song M, Shen Y-K, Wang B-X. A randomized, double-blind, placebo-controlled study of ustekinumab in Chinese patients with moderate to severe plaque psoriasis: LOTUS trial results. Journal of Dermatology 2012;39(s1):238-9. [CENTRAL: CN-01032271] [EMBASE: 70801108] [Google Scholar]
- Zhu X, Zheng M, Song M, Shen YK, Chan D, Szapary PO, et al. Efficacy and safety of ustekinumab in Chinese patients with moderate to severe plaque-type psoriasis: results from a phase 3 clinical trial (LOTUS). Journal of Drugs in Dermatology 2013;12(2):166-74. [CENTRAL: CN-00965604] [PMID: ] [PubMed] [Google Scholar]
- Zhu X-J, Zheng M, Song M, Han C, Chan D, Shen Y-K, et al. Ustekinumab improves health-related quality of life in Chinese patients with moderate-to-severe plaque psoriasis: results from the LOTUS trial and curative effect observation. Journal of Clinical Dermatology 2014;43(9):521-6. [CENTRAL: CN-01037236] [EMBASE: 2014949827] [Google Scholar]
Lowe 1991 {published data only}
- Lowe NJ, Prystowsky JH, Bourget T, Edelstein J, Nychay S, Armstrong R. Acitretin plus UVB therapy for psoriasis. Comparisons with placebo plus UVB and acitretin alone. Journal of the American Academy of Dermatology 1991;24(4):591-4. [CENTRAL: CN-00075422] [PMID: ] [DOI] [PubMed] [Google Scholar]
Mahajan 2010 {published data only}
- Mahajan R, Kaur I, Kanwar AJ. Methotrexate/narrowband UVB phototherapy combination vs. narrowband UVB phototherapy in the treatment of chronic plaque-type psoriasis--a randomized single-blinded placebo-controlled study. Journal of the European Academy of Dermatology and Venereology : JEADV 2010;24(5):595-600. [CENTRAL: CN-00759274] [PMID: ] [DOI] [PubMed] [Google Scholar]
Meffert 1997 {published data only}
- Meffert H, Bräutigam M, Färber L, Weidinger G. Low-dose (1.25 mg/kg) cyclosporin A: treatment of psoriasis and investigation of the influence on lipid profile. Acta Dermato-Venereologica 1997;77(2):137-41. [CENTRAL: CN-00138820] [PMID: ] [DOI] [PubMed] [Google Scholar]
METOP 2017 {published data only}
- Warren RB, Mrowietz U, Von Kiedrowski R, Niesmann J, Wilsmann-Theis D, Ghoreschi K, et al. An intensified dosing schedule of subcutaneous methotrexate in patients with moderate to severe plaque-type psoriasis (METOP): a 52 week, multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017;389(10068):528-37. [CENTRAL: CN-01330160] [PMID: ] [DOI] [PubMed] [Google Scholar]
Nakagawa 2016 {published data only}
- Nakagawa H, Niiro H, Ootaki K, Japanese Brodalumab Study Group. Brodalumab, a human anti-interleukin-17-receptor antibody in the treatment of Japanese patients with moderate-to-severe plaque psoriasis: efficacy and safety results from a phase II randomized controlled study. Journal of Dermatological Science 2016;81(1):44-52. [CENTRAL: CN-01133729] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Umezawa Y, Nakagawa H, Niiro H, Ootaki K, Japanese Brodalumab Study Group. Long-term clinical safety and efficacy of brodalumab in the treatment of Japanese patients with moderate-to-severe plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;30(11):1957-60. [CENTRAL: CN-01457411] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCT02134210 {published data only}
- Kivitz AJ, Papp K, Devani A, Pinter A, Sinclair R, Ziv M, et al. Randomized, double-blind study comparing CHS-0214 with etanercept (ENBREL) in patients with psoriasis and psoriatic arthritis. Arthritis and Rheumatology 2016;68(Suppl 10):2142-3. [CENTRAL: CN-01292943] [Google Scholar]
- Leonardi C, Tang H, Kelleher C, Finck B. Evaluation of CHS-0214 as a proposed biosimilar to etanercept for the treatment of chronic plaque psoriasis: one-year results from a randomized, double-blind global trial. Journal of the American Academy of Dermatology 2017;76(6):AB128. [Google Scholar]
- NCT02134210. Comparison of CHS-0214 to Enbrel (etanercept) in patients with chronic plaque psoriasis (PsO). clinicaltrials.gov/show/nct02134210 (first received 9 May 2014). [CENTRAL: CN-01545599]
NCT02313922 {unpublished data only}
- Liu LF, Chen JS, Gu J, Xu JH, Jin HZ, Pang XW, et al. Etanercept biosimilar (recombinant human tumor necrosis factor-alpha receptor II: IgG Fc fusion protein) and methotrexate combination therapy in Chinese patients with moderate-to-severe plaque psoriasis: a multicentre, randomized, double-blind, placebo-controlled trial. Archives of Dermatological Research 2020;312(6):437-45. [DOI] [PubMed] [Google Scholar]
- NCT02313922. Optimizing psoriasis treatment of etanercept combined methotrexate. clinicaltrials.gov/ct2/show/NCT02313922 (first received 10 December 2014).
NCT02581345 {published data only}
- NCT02581345. Phase 3 study of M923 and Humira® in subjects with chronic plaque-type psoriasis. clinicaltrials.gov/show/nct02581345 (first received 21 October 2015). [CENTRAL: CN-01587601]
NCT02672852 {unpublished data only}
- Blauvelt A, Papp K, Gooderham M, Langley RG, Leonardi C, Lacour JP, et al. Efficacy and safety of risankizumab, an IL-23 inihibitor in patients with moderate-to-severe chronic plaque psoriasis:16-week phase 3 IMMhance trial results. Journal der Deutschen Dermatologischen Gesellschaft [Journal of the German Society of Dermatology] 2018;16(Suppl 1):18. [CENTRAL: CN-01467570] [Google Scholar]
- Blauvelt A, Papp KA, Gooderham M, Langley RG, Leonardi C, Lacour JP, et al. Efficacy and safety of risankizumab, an interleukin-23 inhibitor, in patients with moderate-to-severe chronic plaque psoriasis: 16-week results from the phase III IMMhance trial. British Journal of Dermatology 2017;177(5):e248. [CENTRAL: CN-01452512] [Google Scholar]
- Blauvelt A, Papp KA, Gooderham M, Langley RG, Leonardi C, Lacour JP, et al. Risankizumab efficacy/safety in moderate-to-severe plaque psoriasis: 16-week results from IMMhance. Acta Dermato-venereologica 2018;98(Suppl 219):30. [CENTRAL: CN-01620186] [Google Scholar]
- NCT02672852. BI 655066 / ABBV-066 (Risankizumab) in moderate to severe plaque psoriasis with randomized withdrawal and re-treatment. clinicaltrials.gov/ct2/show/NCT02672852 (first received 1 February 2016). [CENTRAL: CN-01555522]
NCT02690701 {unpublished data only}
- Gelfand JM, Shin DB, Duffin KC, Armstrong AW, Blauvelt A, Tyring SK, et al. A randomized placebo controlled trial of secukinumab on aortic vascular inflammation in moderate to severe plaque psoriasis (VIP-S). Journal of Investigative Dermatology 2020;140(9):1784-93.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02690701. Study to evaluate the effect of secukinumab compared to placebo on aortic vascular inflammation in subjects with moderate to severe plaque psoriasis (VIP-S). clinicaltrials.gov/ct2/show/NCT02690701 (first received 24 February 2016).
NCT02748863 {unpublished data only}
- EUCTR2015-005170-38-BE. Study of efficacy and safety of secukinumab 2 mL pre-filled syringe (300 mg) in subjects with moderate to severe plaque psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-005170-38-BE (first received 29 July 2016).
- NCT02748863. Study of secukinumab with 2 mL pre-filled syringes (ALLURE). clinicaltrials.gov/ct2/show/NCT02748863 (first received 22 April 2016).
NCT02850965 {published data only}
- NCT02850965. Efficacy, safety and immunogenicity of BI 695501 versus Humira® in patients with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/nct02850965 (first received 1 August 2016). [CENTRAL: CN-01507166]
NCT03051217 {published data only}
- NCT03051217. A study to test the efficacy and safety of certolizumab pegol in Japanese subjects with moderate to severe chronic psoriasis. clinicaltrials.gov/show/nct03051217 (first received 13 February 2017).
NCT03055494 {published data only}
- NCT03055494. Study to explore the effect of secukinumab, compared to placebo, on fat tissue and skin in plaque psoriasis patients (ObePso-S). clinicaltrials.gov/show/nct03055494 (first received 16 February 2017).
NCT03066609 {published data only}
- Anonymous. Secukinumab 300 mg showed faster and higher efficacy in Chinese moderate to severe plaque psoriasis patients. Journal of the American Academy of Dermatology 2019;81(4 Suppl 1):AB445. [Google Scholar]
- NCT03066609. Study of efficacy and safety of secukinumab in subjects with moderate to severe chronic plaque-type psoriasis. clinicaltrials.gov/show/nct03066609 (first received 28 February 2017).
NCT03255382 {published data only}
- NCT03255382. A study to assess the efficacy of risankizumab compared to FUMADERM® in subjects with moderate to severe plaque psoriasis who are naive to and candidates for systemic therapy. clinicaltrials.gov/show/nct03255382 (first received 21 August 2017).
NCT03331835 {published data only}
- NCT03331835. A trial comparing the efficacy of subcutaneous injections of brodalumab to oral administrations of fumaric acid esters in adults with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct03331835 (first received 6 November 2017).
NCT03482011 {published data only}
- Anonymous. Efficacy, safety, and quality of life in patients with moderate-to-severe plaque psoriasis treated with mirikizumab (LY3074828) in a phase 2 study. Journal of the American Academy of Dermatology 2018;79(3 Suppl 1):AB126. [Google Scholar]
- NCT03482011. A study to evaluate the efficacy and safety of mirikizumab (LY3074828) in participants with moderate-to-severe plaque psoriasis. clinicaltrials.gov/show/nct03482011 (first received 29 March 2018).
Nugteren‐Huying 1990 {published data only}
- Nugteren-Huying WM, Schroeff JG, Hermans J, Suurmond D. Fumaric acid therapy in psoriasis; a double-blind, placebo-controlled study [Fumaarzuurtherapie tegen psoriasis; een dubbelblind, placebo-gecontroleerd onderzoek]. Nederlands Tijdschrift voor Geneeskunde 1990;134(49):2387-91. [CENTRAL: CN-00072165] [PMID: ] [PubMed] [Google Scholar]
- Nugteren-Huying WM, Van der Schroeff JG, Hermans J, Suurmond D. Fumaric acid therapy for psoriasis: a randomized, double-blind, placebo-controlled study. Journal of the American Academy of Dermatology 1990;22(2 Pt 1):311-2. [CENTRAL: CN-00066354] [DOI] [PubMed] [Google Scholar]
Ohtsuki 2017 {unpublished data only}
- NCT01988103. Efficacy and safety study of two doses of Apremilast (CC-10004) in Japanese subjects with moderate-to-severe plaque-type psoriasis. clinicaltrials.gov/ct2/show/NCT01988103 (first received 24 May 2013). [CENTRAL: CN-01479115]
- Ohtsuki M, Okubo Y, Komine M, Imafuku S, Day RM, Chen P, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in the treatment of Japanese patients with moderate to severe plaque psoriasis: efficacy, safety and tolerability results from a phase 2b randomized controlled trial. Journal of Dermatology 2017;44(8):873-84. [CENTRAL: CN-01600552] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ohtsuki 2018 {published data only}
- Ohtsuki M, Kubo H, Morishima H, Goto R, Zheng R, Nakagawa H. Guselkumab, an anti-interleukin-23 monoclonal antibody, for the treatment of moderate to severe plaque-type psoriasis in Japanese patients: Efficacy and safety results from a phase 3, randomized, double-blind, placebo-controlled study. Journal of Dermatology 2018;45(9):1053-62. [CENTRAL: CN-01646020] [DOI] [PMC free article] [PubMed] [Google Scholar]
Olsen 1989 {published data only}
- Olsen EA, Weed WW, Meyer CJ, Cobo LM. A double-blind, placebo-controlled trial of acitretin for the treatment of psoriasis. Journal of the American Academy of Dermatology 1989;21(4 Pt 1):681-6. [CENTRAL: CN-00063370] [PMID: ] [DOI] [PubMed] [Google Scholar]
OPT Pivotal‐1 2015 {published data only}
- Papp KA, Menter MA, Abe M, Elewski B, Feldman SR, Gottlieb AB, et al. Tofacitinib, an oral Janus kinase inhibitor, for the treatment of chronic plaque psoriasis: results from two randomized, placebo-controlled, phase III trials. British Journal of Dermatology 2015;173(4):949-61. [CENTRAL: CN-01105187] [PMID: ] [DOI] [PubMed] [Google Scholar]
OPT Pivotal‐2 2015 {published data only}
- Papp KA, Menter MA, Abe M, Elewski B, Feldman SR, Gottlieb AB, et al. Tofacitinib, an oral Janus kinase inhibitor, for the treatment of chronic plaque psoriasis: results from two randomized, placebo-controlled, phase III trials. British Journal of Dermatology 2015;173(4):949-61. [CENTRAL: CN-01105187] [PMID: ] [DOI] [PubMed] [Google Scholar]
ORION 2020 {unpublished data only}
- Ferris L, Ott E, Jiang G, Chih-Ho Hong H, Baran W. Efficacy and safety of guselkumab administered with a novel self-injection device for the treatment of moderate-to-severe psoriasis: results from the phase III ORION self-dose study through week 16. Acta Dermato-Venereologica 2018;98(Suppl 219):29. [CENTRAL: CN-01620189] [Google Scholar]
- Ferris LK, Ott E, Jiang J, Hong HC, Li S, Han C, et al. Efficacy and safety of guselkumab, administered with a novel patient-controlled injector (One-Press), for moderate-to-severe psoriasis: results from the phase 3 ORION study. Journal of Dermatological Treatment 2020;31(2):152-9. [DOI] [PubMed] [Google Scholar]
- NCT02905331. Efficacy and safety study of guselkumab in the treatment of participants with moderate to severe plaque-type psoriasis. clinicaltrials.gov/ct2/show/NCT02905331 (first received 14 September 2016). [CENTRAL: CN-01520887]
Ortonne 2013 {published data only}
- Ortonne JP, Paul C, Berardesca E, Marino V, Gallo G, Brault Y, et al. A 24-week randomized clinical trial investigating the efficacy and safety of two doses of etanercept in nail psoriasis. British Journal of Dermatology 2013;168(5):1080-7. [CENTRAL: CN-00967538] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2005 {published data only}
- Krueger GG, Langley RG, Finlay AY, Griffiths CE, Woolley JM, Lalla D, et al. Patient-reported outcomes of psoriasis improvement with etanercept therapy: results of a randomized phase III trial. British Journal of Dermatology 2005;153(6):1192-9. [CENTRAL: CN-00553127] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Papp KA, Tyring S, Lahfa M, Prinz J, Griffiths CE, Nakanishi AM, et al. A global phase III randomized controlled trial of etanercept in psoriasis: safety, efficacy, and effect of dose reduction. British Journal of Dermatology 2005;152(6):1304-12. [CENTRAL: CN-00522450] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2012a {published data only}
- Gordon KB, Kimball AB, Chau D, Viswanathan HN, Li J, Revicki DA, et al. Impact of brodalumab treatment on psoriasis symptoms and health-related quality of life: Use of a novel patient-reported outcome measure, the Psoriasis Symptom Inventory. British Journal of Dermatology 2014;170(3):705-15. [CENTRAL: CN-00981224] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papp K, Leonardi C, Menter A, Thompson EH, Milmont CE, Kricorian G, et al. Safety and efficacy of brodalumab for psoriasis after 120 weeks of treatment. Journal of the American Academy of Dermatology 2014;71(6):1183-90.e3. [CENTRAL: CN-01107365] [EMBASE: 2015237135] [DOI] [PubMed] [Google Scholar]
- Papp K, Menter A, Strober B, Kricorian G, Thompson EH, Milmont CE, et al. Efficacy and safety of brodalumab in subpopulations of patients with difficult-to-treat moderate-to-severe plaque psoriasis. Journal of the American Academy of Dermatology 2015;72(3):436-9.e1. [CENTRAL: CN-01111298] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Papp KA, Leonardi C, Menter A, Ortonne JP, Krueger JG, Kricorian G, et al. Brodalumab, an anti-interleukin-17-receptor antibody for psoriasis. New England Journal of Medicine 2012;366(13):1181-9. [CENTRAL: CN-00814009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2012b {published data only}
- Bushmakin AG, Mamolo C, Cappelleri JC, Stewart M. The relationship between pruritus and the clinical signs of psoriasis in patients receiving tofacitinib. Journal of Dermatological Treatment 2015;26(1):19-22. [CENTRAL: CN-01051702] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mamolo C, Harness J, Tan H, Menter A. Tofacitinib (CP-690,550), an oral Janus kinase inhibitor, improves patient-reported outcomes in a phase 2b, randomized, double-blind, placebo-controlled study in patients with moderate-to-severe psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2014;28(2):192-203. [CENTRAL: CN-00959043] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Mamolo CM, Bushmakin AG, Cappelleri JC. Application of the Itch Severity Score in patients with moderate-to-severe plaque psoriasis: clinically important difference and responder analyses. Journal of Dermatological Treatment 2015;26(2):121-3. [CENTRAL: CN-01083900] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Papp KA, Menter A, Strober B, Langley RG, Buonanno M, Wolk R, et al. Efficacy and safety of tofacitinib, an oral Janus kinase inhibitor, in the treatment of psoriasis: a Phase 2b randomized placebo-controlled dose-ranging study. British Journal of Dermatology 2012;167(3):668-77. [CENTRAL: CN-00856433] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Strober B, Buonanno M, Clark JD, Kawabata T, Tan H, Wolk R, et al. Effect of tofacitinib, a Janus kinase inhibitor, on haematological parameters during 12 weeks of psoriasis treatment. British Journal of Dermatology 2013;169(5):992-9. [CENTRAL: CN-01122547] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Valenzuela F, Papp KA, Pariser D, Tyring SK, Wolk R, Buonanno M, et al. Effects of tofacitinib on lymphocyte sub-populations, CMV and EBV viral load in patients with plaque psoriasis. BMC Dermatology 2015;15:8. [CENTRAL: CN-01109432] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Papp 2012c {published data only}
- Papp K, Cather JC, Rosoph L, Sofen H, Langley RG, Matheson RT, et al. Efficacy of apremilast in the treatment of moderate to severe psoriasis: a randomised controlled trial. Lancet 2012;380(9843):738-46. [CENTRAL: CN-00859723] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Strand V, Fiorentino D, Hu C, Day RM, Stevens RM, Papp KA. Improvements in patient-reported outcomes with apremilast, an oral phosphodiesterase 4 inhibitor, in the treatment of moderate to severe psoriasis: results from a phase IIb randomized, controlled study. Health and Quality of Life Outcomes 2013;10(11):82. [CENTRAL: CN-00876574] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Papp 2013a {published data only}
- Papp KA, Langley RG, Sigurgeirsson B, Abe M, Baker DR, Konno P, et al. Efficacy and safety of secukinumab in the treatment of moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled phase II dose-ranging study. British Journal of Dermatology 2013;168(2):412-21. [CENTRAL: CN-00967073] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Sigurgeirsson B, Kircik L, Nemoto O, Mikazans I, Haemmerle S, Thurston HJ, et al. Secukinumab improves the signs and symptoms of moderate-to-severe plaque psoriasis in subjects with involvement of hands and/or feet: Subanalysis of a randomized, double-blind, placebo-controlled, phase 2 dose-ranging study. Journal of the European Academy of Dermatology and Venereology : JEADV 2014;28(8):1127-9. [CENTRAL: CN-01041806] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2013b {published data only}
- Papp KA, Kaufmann R, Thaçi D, Hu C, Sutherland D, Rohane P. Efficacy and safety of apremilast in subjects with moderate to severe plaque psoriasis: results from a phase II, multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-comparison study. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(3):e376-83. [CENTRAL: CN-01124587] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2015 {published data only}
- Papp K, Thaçi D, Reich K, Riedl E, Langley RG, Krueger JG, et al. Tildrakizumab (MK-3222), an anti-interleukin-23p19 monoclonal antibody, improves psoriasis in a phase IIb randomized placebo-controlled trial. British Journal of Dermatology 2015;173(4):930-9. [CENTRAL: CN-01105188] [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2017a {published data only}
- NCT01970488. Study to compare efficacy and safety of ABP 501 and adalimumab (HUMIRA®) in adults with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct01970488 (first received 28 October 2013). [CENTRAL: CN-01478635]
- Papp K, Bachelez H, Costanzo A, Foley P, Gooderham M, Kaur P, et al. Clinical similarity of biosimilar ABP 501 to adalimumab in the treatment of patients with moderate to severe plaque psoriasis: a randomized, double-blind, multicenter, phase III study. Journal of the American Academy of Dermatology 2017;76(6):1093-102. [CENTRAL: CN-01401166] [DOI] [PubMed] [Google Scholar]
Papp 2017b {unpublished data only}
- NCT02054481. BI 655066 dose ranging in psoriasis, active comparator ustekinumab. clinicaltrials.gov/ct2/show/NCT02054481 (first received 3 February 2014).
- Papp KA, Blauvelt A, Bukhalo M, Gooderham M, Krueger JG, Lacour JP, et al. Risankizumab versus ustekinumab for moderate-to-severe plaque psoriasis. New England Journal of Medicine 2017;376(16):1551-60. [CENTRAL: CN-01368160] [DOI] [PubMed] [Google Scholar]
Papp 2018 {published data only}
- Catlett IM, Hu S, Banerjee S, Gordon K, Krueger JG. A selective inhibitor of TYK2, BMS-986165, improves molecular, cellular, and clinical biomarkers associated with efficacy in moderate-to-severe psoriasis. Experimental Dermatology 2018;27(Suppl 2):55. [CENTRAL: CN-01791579] [Google Scholar]
- EUCTR2016-002481-31-LV. Study to evaluate effectiveness and safety in subjects with moderate to severe Psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2016-002481-31-LV (first received 28 November 2016).
- Gooderham M, Papp K, Gordon K, Foley P, Morita A, Thaçi D, et al. Influence of baseline demographics on efficacy of a selective oral TYK2 inhibitor, BMS-986165, in patients with moderate-to-severe plaque psoriasis: a Phase 2, randomized, placebo-controlled trial. Experimental Dermatology 2018;27(Suppl 2):32. [CENTRAL: CN-01791582] [Google Scholar]
- Gordon K, Papp K, Gooderham M, Thaçi D, Foley P, Morita A, et al. Evaluating influence of baseline characteristics on efficacy of a selective oral TYK2 inhibitor, BMS-986165, in patients with moderate-to-severe plaque psoriasis in a Phase 2 trial. Experimental Dermatology 2018;27(Suppl 2):29-30. [CENTRAL: CN-01787103] [Google Scholar]
- Gordon K, Papp K, Gooderham M, Thaçi D, Foley P, Morita A, et al. Influence of baseline demographics and disease characteristics on efficacy of an oral, selective TYK2 inhibitor, BMS-986165, in patients with plaque psoriasis in a phase 2 trial. Annals of the Rheumatic Diseases 2019;78(Suppl 2):907-8. [Google Scholar]
- NCT02931838. Study to evaluate effectiveness and safety in subjects with moderate to severe psoriasis. clinicaltrials.gov/show/nct02931838 (first received 13 October 2016). [CENTRAL: CN-01521531]
- Papp K, Gordon K, Thaçi D, Morita A, Gooderham M, Foley P, et al. Phase 2 trial of selective tyrosine kinase 2 inhibition in psoriasis. New England Journal of Medicine 2018;379(14):1313-21. [CENTRAL: CN-01652897] [DOI] [PubMed] [Google Scholar]
- Thaçi D, Papp K, Gordon K, Morita A, Gooderham M, Foley P, et al. Selective oral tyrosine kinase 2 (TYK2) inhibitor (BMS-986165) impact on quality of life (QOL) in patients with moderate to severe plaque psoriasis (PSO) in a phase 2 trial as assessed by the dermatology life quality index (DLQI). Journal of the European Academy of Dermatology and Venereology : JEADV 2019;33(S3):71-2. [Google Scholar]
PEARL 2011 {published data only}
- Tsai TF, Ho JC, Song M, Szapary P, Guzzo C, Shen YK, et al. Efficacy and safety of ustekinumab for the treatment of moderate-to-severe psoriasis: a phase III, randomized, placebo-controlled trial in Taiwanese and Korean patients (PEARL). Journal of Dermatological Science 2011;63(3):154-63. [CENTRAL: CN-00810821] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tsai TF, Song M, Shen YK, Schenkel B, Choe YB, Kim NI, et al. Ustekinumab improves health-related quality of life in Korean and Taiwanese patients with moderate to severe psoriasis: results from the PEARL trial. Journal of Drugs in Dermatology 2012;11(8):943-9. [CENTRAL: CN-00859638] [PMID: ] [PubMed] [Google Scholar]
PHOENIX‐1 2008 {published data only}
- Guenther L, Han C, Szapary P, Schenkel B, Poulin Y, Bourcier M, et al. Impact of ustekinumab on health-related quality of life and sexual difficulties associated with psoriasis: results from two phase III clinical trials. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25(7):851-7. [CENTRAL: CN-00887488] [EMBASE: 2011360521] [DOI] [PubMed] [Google Scholar]
- Hu C, Szapary PO, Yeilding N, Zhou H. Informative dropout modeling of longitudinal ordered categorical data and model validation: application to exposure-response modeling of physician's global assessment score for ustekinumab in patients with psoriasis. Journal of Pharmacokinetics and Pharmacodynamics 2011;38(2):237-60. [CENTRAL: CN-00787444] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kimball AB, Gordon KB, Fakharzadeh S, Yeilding N, Szapary PO, Schenkel B, et al. Long-term efficacy of ustekinumab in patients with moderate-to-severe psoriasis: results from the PHOENIX 1 trial through up to 3 years. British Journal of Dermatology 2012;166(4):861-72. [CENTRAL: CN-00841277] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kimball AB, Papp KA, Wasfi Y, Chan D, Bissonnette R, Sofen H, et al. Long-term efficacy of ustekinumab in patients with moderate-to-severe psoriasis treated for up to 5 years in the PHOENIX 1 study. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(12):1535-45. [CENTRAL: CN-00915003] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Lebwohl M, Leonardi C, Griffiths CE, Prinz JC, Szapary PO, Yeilding N, et al. Long-term safety experience of ustekinumab in patients with moderate-to-severe psoriasis (Part I of II): results from analyses of general safety parameters from pooled Phase 2 and 3 clinical trials. Journal of the American Academy of Dermatology 2012;66(5):731-41. [CENTRAL: CN-00860736] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Lebwohl M, Papp K, Han C, Schenkel B, Yeilding N, Wang Y, et al. Ustekinumab improves health-related quality of life in patients with moderate-to-severe psoriasis: results from the PHOENIX 1 trial. British Journal of Dermatology 2010;162(1):137-46. [CENTRAL: CN-00743778] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Leonardi CL, Kimball AB, Papp KA, Yeilding N, Guzzo C, Wang Y, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet 2008;371(9625):1665-74. [CENTRAL: CN-00631485] [18486739] [DOI] [PubMed] [Google Scholar]
- Papp KA, Griffiths CE, Gordon K, Lebwohl M, Szapary PO, Wasfi Y, et al. Long-term safety of ustekinumab in patients with moderate-to-severe psoriasis: final results from 5 years of follow-up. British Journal of Dermatology 2013;168(4):844-54. [CENTRAL: CN-01616926] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Reich K, Papp KA, Griffiths CE, Szapary PO, Yeilding N, Wasfi Y, et al. An update on the long-term safety experience of ustekinumab: results from the psoriasis clinical development program with up to four years of follow-up. Journal of Drugs in Dermatology 2012;11(3):300-12. [CENTRAL: CN-00860086] [PMID: ] [PubMed] [Google Scholar]
- Rich P, Bourcier M, Sofen H, Fakharzadeh S, Wasfi Y, Wang Y, et al. Ustekinumab improves nail disease in patients with moderate-to-severe psoriasis: Results from PHOENIX 1. British Journal of Dermatology 2014;170(2):398-407. [CENTRAL: CN-00982377] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Zhou H, Hu C, Zhu Y, Lu M, Liao S, Yeilding N, et al. Population-based exposure-efficacy modeling of ustekinumab in patients with moderate to severe plaque psoriasis. Journal of Clinical Pharmacology 2010;50(3):257-67. [CENTRAL: CN-00752537] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Zhu Y, Hu C, Lu M, Liao S, Marini JC, Yohrling J, et al. Population pharmacokinetic modeling of ustekinumab, a human monoclonal antibody targeting IL-12/23p40, in patients with moderate to severe plaque psoriasis. Journal of Clinical Pharmacology 2009;49(2):162-75. [CENTRAL: CN-01753183] [PMID: ] [DOI] [PubMed] [Google Scholar]
PHOENIX‐2 2008 {published data only}
- Langley RG, Feldman SR, Han C, Schenkel B, Szapary P, Hsu MC, et al. Ustekinumab significantly improves symptoms of anxiety, depression, and skin-related quality of life in patients with moderate-to-severe psoriasis: results from a randomized, double-blind, placebo-controlled phase iii trial. Journal of the American Academy of Dermatology 2010;63(3):457-65. [CENTRAL: CN-00761719] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Langley RG, Lebwohl M, Krueger GG, Szapary PO, Wasfi Y, Chan D, et al. Long-term efficacy and safety of ustekinumab, with and without dosing adjustment, in patients with moderate-to-severe psoriasis: Results from the PHOENIX 2 study through 5 years of follow-up. British Journal of Dermatology 2015;172(5):1371-83. [CENTRAL: CN-01254538] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Papp KA, Langley RG, Lebwohl M, Krueger GG, Szapary P, Yeilding N, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet 2008;371(9625):1675-84. [CENTRAL: CN-00631486] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Reich K, Schenkel B, Zhao N, Szapary P, Augustin M, Bourcier M, et al. Ustekinumab decreases work limitations, improves work productivity, and reduces work days missed in patients with moderate-to-severe psoriasis: results from PHOENIX 2. Journal of Dermatological Treatment 2011;22(6):337-47. [CENTRAL: CN-00860939] [PMID: ] [DOI] [PubMed] [Google Scholar]
PIECE 2016 {published data only}
- De Vries AC, Thio HB, De Kort WJ, Opmeer BC, Van der Stok HM, De Jong EM, et al. A prospective randomized controlled trial comparing infliximab and etanercept in patients with moderate-to-severe chronic plaque-type psoriasis: the Psoriasis Infliximab vs. Etanercept Comparison Evaluation (PIECE) study. British Journal of Dermatology 2016;176(3):624-33. [CENTRAL: CN-01336979] [PMID: ] [DOI] [PubMed] [Google Scholar]
Piskin 2003 {published data only}
- Piskin G, Heydendael VM, Rie MA, Bos JD, Teunissen MB. Cyclosporin A and methotrexate are equally effective in reducing T cell numbers in psoriatic skin lesions but have no consistent effect on IFN-gamma and IL-4 expression in psoriatic skin in situ. Archives of Dermatological Research 2003;294(12):559-62. [CENTRAL: CN-00456554] [PMID: ] [DOI] [PubMed] [Google Scholar]
POLARIS 2020 {unpublished data only}
- NCT02951533. A study to compare the efficacy of guselkumab to fumaric acid esters for the treatment of participants with moderate to severe plaque psoriasis (POLARIS). clinicaltrials.gov/ct2/show/NCT02951533 (first received 28 October 2016). [CENTRAL: CN-01559701]
- Thaçi D, Pinter A, Sebastian M, Termeer C, Sticherling M, Gerdes S, et al. Guselkumab is superior to fumaric acid esters in patients with moderate-to-severe plaque psoriasis who are naïve to systemic treatment: Results from a randomised, active comparator-controlled phase 3b trial (POLARIS). British Journal of Dermatology 2020;183(2):265-75. [DOI: 10.1111/bjd.18696] [DOI] [PubMed] [Google Scholar]
PRESTA 2010 {published data only}
- Damjanov N, Karpati S, Kemeny L, Bakos N, Bobic B, Majdan M, et al. Efficacy and safety of etanercept in psoriasis and psoriatic arthritis in the PRESTA study: analysis in patients from Central and Eastern Europe. Journal of Dermatological Treatment 2018;29(1):8-12. [CENTRAL: CN-01458628] [DOI] [PubMed] [Google Scholar]
- Gniadecki R, Robertson D, Molta CT, Freundlich B, Pedersen R, Li W, et al. Self-reported health outcomes in patients with psoriasis and psoriatic arthritis randomized to two etanercept regimens. Journal of the European Academy of Dermatology and Venereology : JEADV 2012;26(11):1436-43. [CENTRAL: CN-00971660] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Griffiths CE, Sterry W, Brock F, Dilleen M, Stefanidis D, Germain JM, et al. Pattern of response in patients with moderate-to-severe psoriasis treated with etanercept. British Journal of Dermatology 2015;172(1):230-8. [CENTRAL: CN-01116415] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kirkham B, De Vlam K, Li W, Boggs R, Mallbris L, Nab HW, et al. Early treatment of psoriatic arthritis is associated with improved patient-reported outcomes: findings from the etanercept PRESTA trial. Clinical and Experimental Rheumatology 2015;33(1):11-9. [CENTRAL: CN-01090489] [PMID: ] [PubMed] [Google Scholar]
- Prinz JC, Fitzgerald O, Boggs RI, Foehl J, Robertson D, Pedersen R, et al. Combination of skin, joint and quality of life outcomes with etanercept in psoriasis and psoriatic arthritis in the PRESTA trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25(5):559-64. [CENTRAL: CN-00802619] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Sterry W, Ortonne JP, Kirkham B, Brocq O, Robertson D, Pedersen RD, et al. Comparison of two etanercept regimens for treatment of psoriasis and psoriatic arthritis: PRESTA randomised double blind multicentre trial. BMJ (Clinical Research Ed.) 2010;340:c147. [CENTRAL: CN-00734727] [PMID: ] [DOI] [PubMed] [Google Scholar]
PRIME 2017 {unpublished data only}
- Anonymous. Corrigendum to: Secukinumab is superior to fumaric acid esters in treating patients with moderate-to-severe plaque psoriasis who are naive to systemic treatments: results from the randomized controlled PRIME trial (British Journal of Dermatology 2017; 177(4):1024-32, 10.1111/bjd.15707). British Journal of Dermatology 2017;177(6):1772. [DOI] [PubMed] [Google Scholar]
- NCT02474082. Study of secukinumab compared to fumaderm® in adults with moderate to severe psoriasis (PRIME). clinicaltrials.gov/ct2/show/NCT02474082 (first received 16 April 2015). [CENTRAL: CN-01552941]
- Sticherling M, Mrowietz U, Augustin M, Thaçi D, Melzer N, Hentschke C, et al. Secukinumab is superior to fumaric acid esters in treating patients with moderate-to-severe plaque psoriasis who are naive to systemic treatments: results from the randomized controlled PRIME trial. British Journal of Dermatology 2017;177(4):1024-32. [CENTRAL: CN-01427286] [DOI] [PubMed] [Google Scholar]
PRISTINE 2013 {published data only}
- Puig L, Strohal R, Husni ME, Tsai TF, Noppakun N, Szumski A, et al. Cardiometabolic profile, clinical features, quality of life and treatment outcomes in patients with moderate-to-severe psoriasis and psoriatic arthritis. Journal of Dermatological Treatment 2015;26(1):7-15. [CENTRAL: CN-01051703] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Strohal R, Puig L, Chouela E, Tsai TF, Melin J, Freundlich B, et al. The efficacy and safety of etanercept when used with as-needed adjunctive topical therapy in a randomised, double-blind study in subjects with moderate-to-severe psoriasis (the PRISTINE trial). Journal of Dermatological Treatment 2013;24(3):169-78. [CENTRAL: CN-00881482] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Thaçi D, Galimberti R, Amaya-Guerra M, Rosenbach T, Robertson D, Pedersen R, et al. Improvement in aspects of sleep with etanercept and optional adjunctive topical therapy in patients with moderate-to-severe psoriasis: results from the PRISTINE trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2014;28(7):900-6. [CENTRAL: CN-01041533] [PMID: ] [DOI] [PubMed] [Google Scholar]
PsOsim 2017 {published data only}
- EUCTR2015-000632-15-EE. A study to compare the efficacy and safety of CHS-1420 against Humira®. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-000632-15-EE (first received 22 September 2015).
- Hodge J, Tang H, O'Connor P, Finck B. Switching from adalimumab to CHS-1420: a randomized, double-blind global clinical trial in patients with psoriasis and psoriatic arthritis. Arthritis and Rheumatology 2017;69:Suppl 10. [Google Scholar]
- NCT02489227. Comparison of CHS-1420 versus Humira in subjects with chronic plaque psoriasis (PsOsim). clinicaltrials.gov/show/nct02489227 (first received 2 July 2015).
Reich 2012a {published data only}
- Reich K, Ortonne JP, Gottlieb AB, Terpstra IJ, Coteur G, Tasset C, et al. Successful treatment of moderate to severe plaque psoriasis with the PEGylated Fab' certolizumab pegol: results of a phase II randomized, placebo-controlled trial with a re-treatment extension. British Journal of Dermatology 2012;167(1):180-90. [CENTRAL: CN-00856435] [PMID: ] [DOI] [PubMed] [Google Scholar]
Reich 2015 {published data only}
- Reich K, Papp KA, Matheson RT, Tu JH, Bissonnette R, Bourcier M, et al. Evidence that a neutrophil-keratinocyte crosstalk is an early target of IL-17A inhibition in psoriasis. Experimental Dermatology 2015;24(7):529-35. [CENTRAL: CN-01171151] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reich 2019 {published data only}
- NCT02899988. A study of mirikizumab (LY3074828) in participants with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct02899988 (first received 14 September 2016).
- Papp K, Maari C, Rich P, Klekotka P, Li J, Tuttle J, et al. Response to mirikizumab at Week 52 among patients who did not achieve a PASI 90 response at Week 16. Journal of Clinical and Aesthetic Dermatology 2019;12(5 Suppl 1):S29. [Google Scholar]
- Reich K, Bissonnette R, Menter A, Klekotka P, Patel D, Li J, et al. Efficacy and safety of mirikizumab (LY3074828) in the treatment of moderate-to-severe plaque psoriasis: results from a phase II study. British Journal of Dermatology 2017;177(5):e249. [DOI] [PubMed] [Google Scholar]
- Reich K, Rich P, Maari C, Bissonnette R, Leonardi C, Menter A, et al. Efficacy and safety of mirikizumab (LY3074828) in the treatment of moderate-to-severe plaque psoriasis: results from a randomized phase II study. British Journal of Dermatology 2019;181(1):88-95. [DOI: 10.1111/bjd.17628] [DOI] [PubMed] [Google Scholar]
Reich 2020 {unpublished data only}
- NCT02634801. A study of Ixekizumab (LY2439821) in participants with moderate-to-severe plaque psoriasis naive to systemic treatment. clinicaltrials.gov/ct2/show/NCT02325219 (first received 16 December 2015). [CENTRAL: CN-01554547]
- Reich K, Augustin M, Thaci D, Pinter A, Leutz A, Henneges C, et al. A 24-week multicentre, randomised, open-label, parallel-group study comparing the efficacy and safety of ixekizumab to fumaric acid esters and methotrexate in patients with moderate-to-severe plaque psoriasis naïve to systemic treatment. British Journal of Dermatology 2020;182(4):869-79. [DOI: 10.1111/bjd.18384] [DOI] [PMC free article] [PubMed] [Google Scholar]
ReSURFACE‐1 2017 {published data only}
- Anonymous. Erratum: Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials (Lancet 2017; 390(10091):276-288). Lancet 2017;390(10091):230. [DOI] [PubMed] [Google Scholar]
- Blauvelt A, Sofen H, Papp K, Gooderham M, Tyring S, Zhao Y, et al. Tildrakizumab efficacy and impact on quality of life up to 52 weeks in patients with moderate-to-severe psoriasis: a pooled analysis of two randomized controlled trials. Journal of the European Academy of Dermatology and Venereology : JEADV 2019;33(12):2305-2312. [DOI: 10.1111/jdv.15862] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01722331. A study to evaluate the efficacy and safety of subcutaneous MK-3222, followed by an optional long-term safety extension study, in participants with moderate-to-severe chronic plaque psoriasis (MK-3222-010). clinicaltrials.gov/ct2/show/NCT01722331 (first received 16 March 2017).
- Reich K, Blauvelt A, Thaçi D, Papp KA, Kimball A, Sinclair R, et al. Safety and tolerability of tildrakizumab in patients with chronic plaque psoriasis: Results from long-term extensions of 2 phase 3 studies. Australasian Journal of Dermatology 2018;59(Suppl 1):110-1. [CENTRAL: CN-01606961] [Google Scholar]
- Reich K, Papp KA, Blauvelt A, Tyring SK, Sinclair R, Thaçi D, et al. Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials. Lancet 2017;390(10091):276-88. [CENTRAL: CN-01422560] [DOI] [PubMed] [Google Scholar]
ReSURFACE‐2 2017 {unpublished data only}
- NCT01729754. A study to evaluate the efficacy and safety/tolerability of subcutaneous tildrakizumab (SCH 900222/MK-3222) in participants with moderate-to-severe chronic plaque psoriasis followed by a long-term extension study (MK-3222-011). clinicaltrials.gov/ct2/show/NCT01729754 (first received 13 November 2012). [CENTRAL: CN-01538777]
- Reich K, Papp KA, Blauvelt A, Tyring SK, Sinclair R, Thaçi D, et al. Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials. Lancet 2017;390(10091):276-88. [CENTRAL: CN-01422560] [DOI] [PubMed] [Google Scholar]
REVEAL 2008 {published data only}
- Armstrong AW, Villanueva Quintero DG, Echeverria CM, Gu Y, Karunaratne M, Reyes Servin O. Body region involvement and quality of life in psoriasis: analysis of a randomized controlled trial of adalimumab. American Journal of Clinical Dermatology 2016;17(6):691-9. [CENTRAL: CN-01286209] [PMID: 27815915 ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon K, Papp K, Poulin Y, Gu Y, Rozzo S, Sasso EH. Long-term efficacy and safety of adalimumab in patients with moderate to severe psoriasis treated continuously over 3 years: results from an open-label extension study for patients from REVEAL. Journal of the American Academy of Dermatology 2012;66(2):241-51. [CENTRAL: CN-00860821] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Kimball AB, Bensimon AG, Guerin A, Yu AP, Wu EQ, Okun MM, et al. Efficacy and safety of adalimumab among patients with moderate to severe psoriasis with co-morbidities: Subanalysis of results from a randomized, double-blind, placebo-controlled, phase III trial. American Journal of Clinical Dermatology 2011;12(1):51-62. [CENTRAL: CN-00779604] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Menter A, Augustin M, Signorovitch J, Yu AP, Wu EQ, Gupta SR, et al. The effect of adalimumab on reducing depression symptoms in patients with moderate to severe psoriasis: a randomized clinical trial. Journal of the American Academy of Dermatology 2010;62(5):812-8. [CENTRAL: CN-00743358] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Menter A, Gordon KB, Leonardi CL, Gu Y, Goldblum OM. Efficacy and safety of adalimumab across subgroups of patients with moderate to severe psoriasis. Journal of the American Academy of Dermatology 2010;63(3):448-56. [CENTRAL: CN-00761638] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Menter A, Tyring SK, Gordon K, Kimball AB, Leonardi CL, Langley RG, et al. Adalimumab therapy for moderate to severe psoriasis: a randomized, controlled phase III trial. Journal of the American Academy of Dermatology 2008;58(1):106-15. [CENTRAL: CN-00703914] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Papp K, Menter A, Poulin Y, Gu Y, Sasso EH. Long-term outcomes of interruption and retreatment vs. continuous therapy with adalimumab for psoriasis: subanalysis of REVEAL and the open-label extension study. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(5):634-42. [CENTRAL: CN-00970158] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Revicki DA, Willian MK, Menter A, Gordon KB, Kimball AB, Leonardi CL, et al. Impact of adalimumab treatment on patient-reported outcomes: results from a Phase III clinical trial in patients with moderate to severe plaque psoriasis. Journal of Dermatological Treatment 2007;18(6):341-50. [CENTRAL: CN-00628656] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rich 2013 {published data only}
- Augustin M, Abeysinghe S, Mallya U, Qureshi A, Roskell N, McBride D, et al. Secukinumab treatment of plaque psoriasis shows early improvement in DLQI response - results of a phase II regimen-finding trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2016;30(4):645-9. [CENTRAL: CN-01265142] [PMID: 26660143] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul C, Reich K, Gottlieb AB, Mrowietz U, Philipp S, Nakayama J, et al. Secukinumab improves hand, foot and nail lesions in moderate-to-severe plaque psoriasis: Subanalysis of a randomized, double-blind, placebo-controlled, regimen-finding phase 2 trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2014;28(12):1670-5. [CENTRAL: CN-01119275] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Rich P, Sigurgeirsson B, Thaçi D, Ortonne JP, Paul C, Schopf RE, et al. Secukinumab induction and maintenance therapy in moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled, phase II regimen-finding study. British Journal of Dermatology 2013;168(2):402-11. [CENTRAL: CN-00965685] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ruzicka 1990 {published data only}
- Ruzicka T, Sommerburg C, Braun-Falco O, Köster W, Lengen W, Lensing W, et al. Efficiency of acitretin in combination with UV-B in the treatment of severe psoriasis. Archives of Dermatology 1990;126(4):482-6. [CENTRAL: CN-00066767] [PMID: ] [PubMed] [Google Scholar]
Sandhu 2003 {published data only}
- Sandhu K, Kaur I, Kumar B, Saraswat A. Efficacy and safety of cyclosporine versus methotrexate in severe psoriasis: a study from north India. Journal of Dermatology 2003;30(6):458-63. [CENTRAL: CN-00456950] [PMID: ] [DOI] [PubMed] [Google Scholar]
Saurat 1988 {published data only}
- Saurat JH, Geiger JM, Amblard P, Beani JC, Boulanger A, Claudy A, et al. Randomized double-blind multicenter study comparing acitretin-PUVA, etritinate-PUVA and placebo-PUVA in the treatment of severe psoriasis. Dermatologica 1988;177(4):218-24. [CENTRAL: CN-00058056] [PMID: ] [DOI] [PubMed] [Google Scholar]
SCULPTURE 2015 {published data only}
- Mrowietz U, Leonardi CL, Girolomoni G, Toth D, Morita A, Balki SA, et al. Secukinumab retreatment-as-needed versus fixed-interval maintenance regimen for moderate to severe plaque psoriasis: A randomized, double-blind, noninferiority trial (SCULPTURE). Journal of the American Academy of Dermatology 2015;73(1):27-36.e1. [CENTRAL: CN-01109352] [PMID: ] [DOI] [PubMed] [Google Scholar]
Shehzad 2004 {published data only}
- Shehzad T, Dar NR, Zakria M. Efficacy of concomitant use of puva and methotrexate in disease clearance time in plaque type psoriasis. Journal of the Pakistan Medical Association 2004;54(9):453-5. [CENTRAL: CN-00727152] [PMID: ] [PubMed] [Google Scholar]
SIGNATURE 2019 {unpublished data only}
- NCT01961609. Secukinumab in TNF-IR psoriasis patients (SIGNATURE). clinicaltrials.gov/ct2/show/NCT01961609 (first received 10 October 2013). [CENTRAL: CN-01536745]
- Warren RB, Barker JNWB, Finlay AY, Burden AD, Kirby B, Armendariz Y, et al. Secukinumab for patients failing previous tumour necrosis factor-alpha inhibitor therapy: results of a randomized open-label study (SIGNATURE). British Journal of Dermatology 2019;183(1):60-70. [DOI: 10.1111/bjd.18623] [DOI] [PubMed] [Google Scholar]
Sommerburg 1993 {published data only}
- Sommerburg C, Kietzmann H, Eichelberg D, Goos M, Heese A, Holzle E, et al. Acitretin in combination with PUVA: A randomized double-blind placebo- controlled study in severe psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 1993;2(4):308-17. [CENTRAL: CN-00180920] [EMBASE: 1993350796] [Google Scholar]
Strober 2011 {published data only}
- Strober BE, Crowley JJ, Yamauchi PS, Olds M, Williams DA. Efficacy and safety results from a phase III, randomized controlled trial comparing the safety and efficacy of briakinumab with etanercept and placebo in patients with moderate to severe chronic plaque psoriasis. British Journal of Dermatology 2011;165(3):661-8. [CENTRAL: CN-00811738] [PMID: ] [DOI] [PubMed] [Google Scholar]
STYLE 2020 {published data only}
- Van Voorhees AS, Stein Gold L, Lebwohl M, Strober B, Lynde C, Tyring S, et al. Efficacy and safety of apremilast in patients with moderate to severe plaque psoriasis of the scalp: results of a phase 3b, multicenter, randomized, placebo-controlled, double-blind study. Journal of the American Academy of Dermatology 2020;83(1):96-103. [DOI] [PubMed] [Google Scholar]
SustaIMM 2019 {published data only}
- NCT03000075. BI 655066 (Risankizumab) compared to placebo in Japanese patients with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/nct03000075 (first received 21 December 2016). [CENTRAL: CN-01560779]
- Ohtsuki M, Fujita H, Watanabe M, Suzaki K, Flack M, Huang X, et al. Efficacy and safety of risankizumab in Japanese patients with moderate to severe plaque psoriasis: results from the SustaIMM phase 2/3 trial. Journal of Dermatology 2019;46(8):686-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tanew 1991 {published data only}
- Tanew A, Guggenbichler A, Hönigsmann H, Geiger JM, Fritsch P. Photochemotherapy for severe psoriasis without or in combination with acitretin: a randomized, double-blind comparison study. Journal of the American Academy of Dermatology 1991;25(4):682-4. [CENTRAL: CN-00612571] [PMID: ] [DOI] [PubMed] [Google Scholar]
Torii 2010 {published data only}
- JPRN-JapicCTI-060318. Clinical study to evaluate the efficacy and safety of TA-650 in patients with psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-JapicCTI-060318 (first received 1 November 2006).
- Torii H, Nakagawa H, Japanese Infliximab Study investigators. Infliximab monotherapy in Japanese patients with moderate-to-severe plaque psoriasis and psoriatic arthritis. A randomized, double-blind, placebo-controlled multicenter trial. Journal of Dermatological Science 2010;59(1):40-9. [CENTRAL: CN-00760986] [PMID: ] [DOI] [PubMed] [Google Scholar]
TRANSFIGURE 2016 {published and unpublished data}
- Reich K, Sullivan J, Arenberger P, Mrowietz U, Jazayeri S, Augustin M, et al. Secukinumab shows significant efficacy in nail psoriasis: week 32 results from the TRANSFIGURE study. Annals of the Rheumatic Diseases 2016;75(Suppl 2):603-4. [CENTRAL: CN-01761193] [Google Scholar]
Tyring 2006 {published data only}
- Krishnan R, Cella D, Leonardi C, Papp K, Gottlieb AB, Dunn M, et al. Effects of etanercept therapy on fatigue and symptoms of depression in subjects treated for moderate to severe plaque psoriasis for up to 96 weeks. British Journal of Dermatology 2007;157(6):1275-7. [CENTRAL: CN-00627972] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tyring S, Bagel J, Lynde C, Klekotka P, Thompson EH, Gandra SR, et al. Patient-reported outcomes in moderate-to-severe plaque psoriasis with scalp involvement: results from a randomized, double-blind, placebo-controlled study of etanercept. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(1):125-8. [CENTRAL: CN-00971136] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tyring S, Gordon KB, Poulin Y, Langley RG, Gottlieb AB, Dunn M, et al. Long-term safety and efficacy of 50 mg of etanercept twice weekly in patients with psoriasis. Archives of Dermatology 2007;143(6):719-26. [CENTRAL: CN-00589825] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Tyring S, Gottlieb A, Papp K, Gordon K, Leonardi C, Wang A, et al. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet 2006;367(9504):29-35. [CENTRAL: CN-00532672] [PMID: ] [DOI] [PubMed] [Google Scholar]
UltIMMa‐1 2018 {unpublished data only}
- Gooderham M, Lebwohl M, Gordon K, Wu T, Photowala H, Bachelez H. High and durable clearance through 52 weeks of risankizumab treatment in patients with moderate-to-severe plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2019;33(S3):20. [Google Scholar]
- Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab: results from two double-blind, placebo-and ustekinumab-controlled, phase 3 trials in moderate-to-severe plaque psoriasis. Acta Dermato-Venereologica 2018;98(Suppl 219):28-9. [DOI] [PubMed] [Google Scholar]
- Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet 2018;392(10148):650-61. [CENTRAL: CN-01649259] [DOI] [PubMed] [Google Scholar]
- NCT02684357. BI 655066 compared to placebo & active comparator (Ustekinumab) in patients with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/ct2/show/NCT02684357 (first received 18 February 2016). [CENTRAL: CN-01555862]
UltIMMa‐2 2018 {unpublished data only}
- Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab: results from two double-blind, placebo-and ustekinumab-controlled, phase 3 trials in moderate-to-severe plaque psoriasis. Acta Dermato-venereologica 2018;98(Suppl 219):28-9. [DOI] [PubMed] [Google Scholar]
- Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. Lancet 2018;392(10148):650-61. [CENTRAL: CN-01649259] [DOI] [PubMed] [Google Scholar]
- NCT02684370. BI 655066 (Risankizumab) compared to placebo and active comparator (Ustekinumab) in patients with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/ct2/show/NCT02684370 (first received 18 February 2016). [CENTRAL: CN-01555863]
UNCOVER‐1 2016 {published data only}
- Armstrong AW, Lynde CW, McBride SR, Stahle M, Edson-Heredia E, Zhu B, et al. Effect of ixekizumab treatment on work productivity for patients with moderate-to-severe plaque psoriasis: analysis of results from 3 randomized phase 3 clinical trials. JAMA Dermatology 2016;152(6):661-9. [CENTRAL: CN-01166284] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Gordon KB, Blauvelt A, Papp KA, Langley RG, Luger T, Ohtsuki M, et al. Phase 3 trials of ixekizumab in moderate-to-severe plaque psoriasis. New England Journal of Medicine 2016;375(4):345-56. [CENTRAL: CN-01167902] [PMID: ] [DOI] [PubMed] [Google Scholar]
UNCOVER‐2 2015 {published data only}
- Griffiths CE, Reich K, Lebwohl M, Van de Kerkhof P, Paul C, Menter A, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet 2015;386(9993):541-51. [CENTRAL: CN-01091029] [PMID: ] [DOI] [PubMed] [Google Scholar]
UNCOVER‐3 2015 {published data only}
- Griffiths CE, Reich K, Lebwohl M, de Kerkhof P, Paul C, Menter A, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet 2015;386(9993):541-51. [CENTRAL: CN-01091029] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Van de Kerkhof P, Guenther L, Gottlieb AB, Sebastian M, Wu JJ, Foley P, et al. Ixekizumab treatment improves fingernail psoriasis in patients with moderate-to-severe psoriasis: results from the randomized, controlled and open-label phases of UNCOVER-3. Journal of the European Academy of Dermatology and Venereology : JEADV 2017;31(3):477-82. [CENTRAL: CN-01287590] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van Bezooijen 2016 {published data only}
- Van Bezooijen JS, Balak DM, Van Doorn MB, Looman CW, Schreurs MW, Koch BC, et al. Combination therapy of etanercept and fumarates versus etanercept monotherapy in psoriasis: a randomized exploratory study. Dermatology 2016;232(4):407-14. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Van de Kerkhof 2008 {published data only}
- Reich K, Segaert S, Van de Kerkhof P, Durian C, Boussuge MP, Paolozzi L, et al. Once-weekly administration of etanercept 50 mg improves patient-reported outcomes in patients with moderate-to-severe plaque psoriasis. Dermatology (Basel, Switzerland) 2009;219(3):239-49. [CENTRAL: CN-00730853] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Van de Kerkhof PC, Segaert S, Lahfa M, Luger TA, Karolyi Z, Kaszuba A, et al. Once weekly administration of etanercept 50 mg is efficacious and well tolerated in patients with moderate-to-severe plaque psoriasis: a randomized controlled trial with open-label extension. British Journal of Dermatology 2008;159(5):1177-85. [CENTRAL: CN-00681015] [PMID: ] [DOI] [PubMed] [Google Scholar]
VIP Trial 2018 {unpublished data only}
- Mehta NN, Shin DB, Joshi AA, Dey AK, Armstrong AW, Duffin KC, et al. Effect of 2 psoriasis treatments on vascular inflammation and novel inflammatory cardiovascular biomarkers: a randomized placebo-controlled trial. Circulation. Cardiovascular imaging 2018;11(6):e007394. [CENTRAL: CN-01652064] [DOI: 10.1161/CIRCIMAGING.117.007394] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT01553058. Vascular Inflammation in Psoriasis Trial (The VIP Trial) (VIP). clinicaltrials.gov/ct2/show/NCT01553058 (first received 14 February 2012). [CENTRAL: CN-01591340]
VIP‐U Trial 2020 {published data only}
- Gelfand JM, Shin DB, Alavi A, Torigian DA, Werner T, Papadopoulos M, et al. A phase IV, randomized, double-blind, placebo-controlled crossover study of the effects of ustekinumab on vascular inflammation in psoriasis (the VIP-U Trial). Journal of Investigative Dermatology 2020;140(1):85-93.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT02187172. Vascular inflammation in psoriasis-ustekinumab (VIP-U). clinicaltrials.gov/show/nct02187172 (first received 10 July 2014).
VOYAGE‐1 2016 {published data only}
- Armstrong AW, Reich K, Foley P, Han C, Song M, Shen YK, et al. Improvement in patient-reported outcomes (Dermatology Life Quality Index and the Psoriasis Symptoms and Signs Diary) with guselkumab in moderate-to-severe plaque psoriasis: results from the phase III VOYAGE 1 and VOYAGE 2 studies. American Journal of Clinical Dermatology 2018;20(1):155-64. [CENTRAL: CN-01943968] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blauvelt A, Papp KA, Griffiths CE, Randazzo B, Wasfi Y, Shen Y-K, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: Results from the phase III, double-blinded, placebo- and active comparator-controlled VOYAGE 1 trial. Journal of the American Academy of Dermatology 2016;76(3):405-17. [CENTRAL: CN-01341398] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Griffiths CE, Papp KA, Kimball AB, Randazzo B, Wasfi Y, Li S, et al. Two-year efficacy and safety of guselkumab for treatment of moderate-to-severe psoriasis: phase 3 VOYAGE 1 trial. Annals of the Rheumatic Diseases 2018;77(Suppl 2):1580-1. [CENTRAL: CN-01647499] [Google Scholar]
VOYAGE‐2 2017 {published data only}
- Reich K, Armstrong AW, Foley P, Song M, Wasfi Y, Randazzo B, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the treatment of patients with moderate to severe psoriasis with randomized withdrawal and retreatment: Results from the phase III, double-blind, placebo- and active comparator-controlled VOYAGE 2 trial. Journal of the American Academy of Dermatology 2017;76(3):418-31. [CENTRAL: CN-01341399] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yang 2012 {published data only}
- Yang HZ, Wang K, Jin HZ, Gao TW, Xiao SX, Xu JH, et al. Infliximab monotherapy for Chinese patients with moderate to severe plaque psoriasis: a randomized, double-blind, placebo-controlled multicenter trial. Chinese Medical Journal 2012;125(11):1845-51. [CENTRAL: CN-00904898] [PMID: ] [PubMed] [Google Scholar]
Yilmaz 2002 {published data only}
- Yılmaz E, Yılmaz F, Yerebakan O. Re-PUVA therapy for psoriasis vulgaris: an effective choice [Psoriazis vulgaris tedavisinde etkili bir seçenek: asitretin ile PUVA kombinasyonu (Re-PUVA)]. Türkiye Klinikleri Dermatoloji Dergisi 2002;12(4):204-8. [CENTRAL: CN-01951242] [Google Scholar]
- Yilmaz E, Yilmaz F, Yerebakan O. Re-PUVA therapy for psoriasis vulgaris: an effective choice. Journal of the European Academy of Dermatology and Venereology : JEADV 2002;16(Suppl s1):258. [CENTRAL: CN-00416979] [Google Scholar]
Yu 2019 {published data only}
- Yu Q, Tong Y, Cui L, Zhang L, Gong Y, Diao H, et al. Efficacy and safety of etanercept combined plus methotrexate and comparison of expression of pro-inflammatory factors expression for the treatment of moderate-to-severe plaque psoriasis. International Immunopharmacology 2019;73:442-50. [DOI] [PubMed] [Google Scholar]
Zhang 2017 {published data only}
- NCT01815424. A study evaluating the efficacy and safety of CP-690,550 In Asian subjects with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct01815424 (first received 21 March 2013). [CENTRAL: CN-01541153]
- Zhang J, Tsai TF, Lee MG, Zheng M, Wang G, Jin H, et al. The efficacy and safety of tofacitinib in Asian patients with moderate to severe chronic plaque psoriasis: a Phase 3, randomized, double-blind, placebo-controlled study. Journal of Dermatological Science 2017;88(1):36-45. [CENTRAL: CN-01604532] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abe 2017 {published data only}
- Abe M, Nishigori C, Torii H, Ihn H, Ito K, Nagaoka M, et al. Tofacitinib for the treatment of moderate to severe chronic plaque psoriasis in Japanese patients: subgroup analyses from a randomized, placebo-controlled phase 3 trial. Journal of Dermatology 2017;44(11):1228-37. [CENTRAL: CN-01615689] [DOI] [PMC free article] [PubMed] [Google Scholar]
Abufarag 2010 {published data only}
- Abufarag A, Aigner S, Czeloth N, Dalken B, Koch H, Niemann G, et al. Selective activation of naturally occurring regulatory T cells (Tregs) by the monoclonal antibody BT-061 as a novel therapeutic opportunity in psoriasis: Early clinical results after single doses. Journal of Investigative Dermatology 2010;130(Suppl 2):S64. [CENTRAL: CN-00795758] [EMBASE: 70263767] [Google Scholar]
Adsit 2017 {published data only}
- Adsit S, Zaldivar ER, Sofen H, Dei-Cas I, Garcia CM, Penaranda EO, et al. Secukinumab is efficacious and safe in hispanic patients with moderate-to-severe plaque psoriasis: pooled analysis of four phase 3 trials. Advances in Therapy 2017;34(6):1327-39. [CENTRAL: CN-01443493] [DOI: 10.1007/s12325-017-0521-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Akhyani 2010 {published data only}
- Akhyani M, Chams-Davatchi C, Hemami MR, Fateh S. Efficacy and safety of mycophenolate mofetil vs. methotrexate for the treatment of chronic plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2010;24(12):1447-51. [CENTRAL: CN-00771805] [PMID: ] [DOI] [PubMed] [Google Scholar]
Altmeyer 1994 {published data only}
- Altmeyer PJ, Matthes U, Pawlak F, Hoffmann K, Frosch PJ, Ruppert P, et al. Antipsoriatic effect of fumaric acid derivatives. Results of a multicenter double-blind study in 100 patients. Journal of the American Academy of Dermatology 1994;30(6):977-81. [CENTRAL: CN-00101455] [PMID: ] [DOI] [PubMed] [Google Scholar]
Angsten 2007 {published data only}
- Angsten M, Schopf RE. Anti-TNF-alpha-therapy of psoriasis with infliximab or etanercept. Clinical, histological and immunohistochemical course. Aktuelle Dermatologie 2007;33(8-9):310-6. [CENTRAL: CN-00726884] [EMBASE: 2007503340] [Google Scholar]
Anonymous 2005 {published data only}
- Anonymous. Aldalimumab in psoriatic arthritis and as the initial therapy in rheumatoid arthritis [Adalimumab bei Psoriasis-Arthritis und zur Initialtherapie bei rheumatoider Arthritis]. Krankenpflege Journal 2005;43(7-10):244. [PMID: ] [PubMed] [Google Scholar]
Anonymous 2008 {published data only}
- Anonymous. Trial watch: novel biologic for psoriasis shows superiority over current best-seller. Nature Reviews. Drug Discovery 2008;7(11):880-1. [PMID: ] [DOI] [PubMed] [Google Scholar]
Anonymous 2019 {published data only}
- Anonymous. Evaluation of effectiveness and safety in two optimization strategies with secukinumab in the treatment of moderate severe psoriasis. Journal of the American Academy of Dermatology 2019;81 (4 Supplement 1):AB60. [Google Scholar]
Araujo 2017 {published data only}
- Araujo EG, Englbrecht M, Hoepken S, Finzel S, Hueber A, Rech J, et al. Ustekinumab is superior to TNF inhibitor treatment in resolving enthesitis in PSA patients with active enthesitis-results from the enthesial clearance in psoriatic arthritis (ECLIPSA) study. Annals of the Rheumatic Diseases 2017;76(Supplement 2):142. [CENTRAL: CN-01467990] [Google Scholar]
Araujo 2019 {published data only}
- Araujo EG, Englbrecht M, Hoepken S, Finzel S, Kampylafka E, Kleyer A, et al. Effects of ustekinumab versus tumor necrosis factor inhibition on enthesitis: Results from the enthesial clearance in psoriatic arthritis (ECLIPSA) study. Seminars in Arthritis and Rheumatism 2019;48(4):632-7. [CENTRAL: CN-01930220] [DOI] [PubMed] [Google Scholar]
Arifov 1998 {published data only}
- Arifov S, Vaisov A, Ismagilov A, Abidova Z. Acitretin (neotigason) in the treatment of psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 1998;11(Suppl 2):S290. [CENTRAL: CN-00465900] [Google Scholar]
Armati 1972 {published data only}
- Armati RP. Retinoic acid for psoriasis. Australasian Journal of Dermatology 1972;13(2):79-83. [CENTRAL: CN-00008047] [PMID: ] [DOI] [PubMed] [Google Scholar]
Augustin 2017 {published data only}
- Augustin M, Blome C, Paul C, Puig L, Luger T, Lambert J, et al. Quality of life and patient benefit following transition from methotrexate to ustekinumab in psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2017;31(2):294-303. [CENTRAL: CN-01368710] [DOI: 10.1111/jdv.13823] [DOI] [PubMed] [Google Scholar]
Avgerinou 2011 {published data only}
- Avgerinou G, Tousoulis D, Siasos G, Oikonomou E, Maniatis K, Papageorgiou N, et al. Anti-tumor necrosis factor alpha treatment with adalimumab improves significantly endothelial function and decreases inflammatory process in patients with chronic psoriasis. International Journal of Cardiology 2011;151(3):382-3. [CENTRAL: CN-00860819] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bachelez 2017 {published data only}
- Bachelez H, Griffiths CE, Papp K, Hall S, Merola JF, Feldman SR, et al. Effect of tofacitinib on efficacy and patient-reported outcomes in psoriasis patients with baseline psoriatic arthritis: a pooled analysis of 2 phase 3 studies. Arthritis and Rheumatology 2017;69(Suppl 10):613. [CENTRAL: CN-01602915] [Google Scholar]
Bagel 2017a {published data only}
- Bagel J, Duffin KC, Bukhalo M, Bobonich M, Gill A, Zhao F, et al. Ease of use and confidence using auto-injector to administer ixekizumab in a phase 3 trial evaluated with subcutaneous administration assessment questionnaire (SQAAQ). Journal of Clinical and Aesthetic Dermatology 2017;10(5 Supplement 1):S14-5. [CENTRAL: CN-01713047] [Google Scholar]
Bagel 2017b {published data only}
- Bagel J, Tyring S, Rice KC, Collier DH, Kricorian G, Chung J, et al. Open-label study of etanercept treatment in patients with moderate-to-severe plaque psoriasis who lost a satisfactory response to adalimumab. British Journal of Dermatology 2017;177(2):411-8. [CENTRAL: CN-01393822] [DOI: 10.1111/bjd.15381] [DOI] [PubMed] [Google Scholar]
Bagel 2017c {published data only}
- Bagel J, Duffin KC, Moore A, Ferris LK, Siu K, Steadman J, et al. The effect of secukinumab on moderate-to-severe scalp psoriasis: results of a 24-week, randomized, double-blind, placebo-controlled phase 3b study. Journal of the American Academy of Dermatology 2017;77(4):667-74. [CENTRAL: CN-01412958] [DOI] [PubMed] [Google Scholar]
Bagel 2018b {published data only}
- Bagel J, Samad AS, Stolshek BS, Aras GA, Chung JB, Kricorian G, et al. Open-label study to evaluate the efficacy of etanercept treatment in subjects with moderate to severe plaque psoriasis who have failed therapy with apremilast. Journal of Drugs in Dermatology: JDD 2018;17(10):1078-82. [CENTRAL: CN-01664523] [PubMed] [Google Scholar]
Bagherani 2017 {published data only}
- Bagherani N, Smoller BR. Efficacy of topical tofacitinib, a Janus kinase inhibitor, in the treatment of plaque psoriasis. Dermatologic Therapy 2017;30(3):e12467. [CENTRAL: CN-01600736] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bagot 1994 {published data only}
- Bagot M, Grossman R, Pamphile R, Binderup L, Charue D, Revuz J, et al. Additive effects of calcipotriol and cyclosporine A: from in vitro experiments to in vivo applications in the treatment of severe psoriasis. Comptes Rendus de l'Académie des Sciences. Série III, Sciences de la Vie 1994;317(3):282-6. [CENTRAL: CN-00107966] [PMID: ] [PubMed] [Google Scholar]
Bartlett 2008 {published data only}
- Bartlett BL, Tyring SK. Ustekinumab for chronic plaque psoriasis. Lancet 2008;371(9625):1639-40. [CENTRAL: CN-00631484] [PMID: ] [DOI] [PubMed] [Google Scholar]
Barzegari 2004 {published data only}
- Barzegari M, Ghaninejad H, Shizarpoor M. Comparison of bath PUVA and acitretin in treatment of psoriatic patients. Iranian Journal of Dermatology 2004;7(4):31-5. [CENTRAL: CN-00509588] [Google Scholar]
Batchelor 2009 {published data only}
- Batchelor JM, Ingram JR, Williams H. Adalimumab vs methotrexate for the treatment of chronic plaque psoriasis. Archives of Dermatology 2009;145(6):704-6. [CENTRAL: CN-01783607] [EMBASE: 2009300916] [DOI] [PubMed] [Google Scholar]
Bayerl 1992 {published data only}
- Bayerl C. Treatment of psoriasis vulgaris with etretinate versus cyclosporin A. Report on a study. [Parallelgruppenvergleich Etretinat versus Cyclosporin A bei Psoriasis vulgaris]. Aktuelle Dermatologie 1992;18(1-2):27-31. [CENTRAL: CN-00197510] [EMBASE: 1992096910] [Google Scholar]
Beissert 2009 {published data only}
- Beissert S, Pauser S, Sticherling M, Frieling U, Loske KD, Frosch PJ, et al. A comparison of mycophenolate mofetil with ciclosporine for the treatment of chronic plaque-type psoriasis. Dermatology (Basel, Switzerland) 2009;219(2):126-32. [CENTRAL: CN-00729115] [PMID: ] [DOI] [PubMed] [Google Scholar]
Berbis 1989 {published data only}
- Berbis P, Geiger JM, Vaisse C, Rognin C, Privat Y. Benefit of progressively increasing doses during the initial treatment with acitretin in psoriasis. Dermatologica 1989;178(2):88-92. [CENTRAL: CN-00058682] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bhat 2017 {published data only}
- Bhat RM, Leelavathy B, Aradhya SS, Gopal MG, Pratap DV, Mubashir M, et al. Secukinumab efficacy and safety in Indian patients with moderate-to-severe plaque psoriasis: Sub-analysis from FIXTURE, a randomized, placebo-controlled, phase 3 study. Indian Dermatology Online Journal 2017;8(1):16-24. [DOI: 10.4103/2229-5178.198765] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bhuiyan 2010 {published data only}
- Bhuiyan MS, Sikder MdA, Rashid MM, Rabin F. Role of oral colchicine in plaque type psoriasis. A randomized clinical trial comparing with oral methotrexate. Journal of Pakistan Association of Dermatologists 2010;20(3):146-51. [CENTRAL: CN-00789712] [EMBASE: 2010613015] [Google Scholar]
Bian 2018 {published data only}
- Bian M, Bissonnette R, Luger T, Thaçi D, Toth D, Xia S, et al. Secukinumab treatment in moderate-to-severe psoriasis patients demonstrates sustained low absolute PASI up to 4 years: results from SCULPTURE extension study. Australasian Journal of Dermatology 2018;59(Supplement 1):39. [CENTRAL: CN-01606960] [DOI: 10.1111/jdv.14878] [DOI] [Google Scholar]
Bigby 2004 {published data only}
- Bigby M. A randomized controlled trial of methotrexate and cyclosporine in the treatment of psoriasis. Archives of Dermatology 2004;140(3):347-8. [CENTRAL: CN-00515754] [EMBASE: 2004120959] [DOI] [PubMed] [Google Scholar]
Bissonnette 2006 {published data only}
- Bissonnette R, Papp K, Poulin Y, Lauzon G, Aspeslet L, Huizinga R, et al. A randomized, multicenter, double-blind, placebo-controlled phase 2 trial of ISA247 in patients with chronic plaque psoriasis. Journal of the American Academy of Dermatology 2006;54(3):472-8. [CENTRAL: CN-00555245] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bissonnette 2010 {published data only}
- Bissonnette R, Papp K, Maari C, Yao Y, Robbie G, White WI, et al. A randomized, double-blind, placebo-controlled, phase I study of medi-545, an anti-interferon-alfa monoclonal antibody, in subjects with chronic psoriasis. Journal of the American Academy of Dermatology 2010;62(3):427-36. [CENTRAL: CN-00734807] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bissonnette 2017a {published data only}
- Bissonnette R, Luger T, Thaçi D, Toth D, Messina I, You R, et al. Secukinumab sustains good efficacy and favourable safety in moderate-to-severe psoriasis after up to 3 years of treatment: results from a double-blind extension study. British Journal of Dermatology 2017;177(4):1033-42. [CENTRAL: CN-01419893] [DOI: 10.1111/bjd.15706] [DOI] [PubMed] [Google Scholar]
Bissonnette 2017b {published data only}
- Bissonnette R, Harel F, Krueger JG, Guertin MC, Chabot-Blanchet M, Gonzalez J, et al. TNF-α antagonist and vascular inflammation in patients with psoriasis vulgaris: a randomized placebo-controlled study. Journal of Investigative Dermatology 2017;137(8):1638-45. [CENTRAL: CN-01410690] [DOI: 10.1016/j.jid.2017.02.977] [DOI] [PubMed] [Google Scholar]
Bissonnette 2018 {published data only}
- Bissonnette R, Haydey R, Rosoph LA, Lynde CW, Bukhalo M, Fowler JF, et al. Apremilast for the treatment of moderate-to-severe palmoplantar psoriasis: results from a double-blind, placebo-controlled, randomized study. Journal of the European Academy of Dermatology and Venereology 2018;32(3):403-10. [CENTRAL: CN-01643330] [DOI: 10.1111/jdv.14647] [DOI] [PubMed] [Google Scholar]
Bjerke 1989 {published data only}
- Bjerke JR, Geiger JM. Acitretin versus etretinate in severe psoriasis. A double-blind randomized Nordic multicenter study in 168 patients. Acta Dermato-Venereologica. Supplementum 1989;146:206-7. [CENTRAL: CN-00064911] [PMID: ] [PubMed] [Google Scholar]
Blauvelt 2016a {published data only}
- Blauvelt A, Papp K, Griffiths CE, Mallbris L, Dutronic Y, Ilo D, et al. Efficacy and safety of ixekizumab in patients previously treated with etanercept. Experimental Dermatology 2016;25(S4):38-9. [CENTRAL: CN-01407588] [DOI: 10.1111/exd.13200] [DOI] [Google Scholar]
Blauvelt 2016b {published data only}
- Blauvelt A, Langley R, Leonardi C, Gordon K, Luger T, Ohtsuki M, et al. Ixekizumab, a novel anti-IL-17A antibody, exhibits low immunogenicity during long-term treatment in patients with psoriasis. Journal of Investigative Dermatology 2016;136(9 Supplement 2):S227. [CENTRAL: CN-01785592] [Google Scholar]
Blauvelt 2017a {published data only}
- Blauvelt A, Reich K, Lebwohl M, Burge D, Arendt C, Peterson L, et al. Certolizumab pegol for the treatment of patients with moderate-to-severe chronic plaque psoriasis: an overview of three randomized controlled trials. British Journal of Dermatology 2017;177(5):e249-50. [CENTRAL: CN-01452510] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blauvelt 2017b {published data only}
- Blauvelt A, Papp KA, Sofen H, Augustin M, Yosipovitch G, Katoh N, et al. Continuous dosing versus interrupted therapy with ixekizumab: an integrated analysis of two phase 3 trials in psoriasis. Journal of the European Academy of Dermatology and Venereology 2017;31(6):1004-13. [CENTRAL: CN-01459095] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blauvelt 2017c {published data only}
- Blauvelt A, Lacour JP, Fowler JF, Schuck E, Jauch-Lembach J, Balfour A, et al. Long-term efficacy, safety, and immunogenicity data from a phase III confirmatory study comparing GP2017, a proposed biosimilar, with reference adalimumab. American Journal of Gastroenterology 2017;112(Supplement 1):S419. [CENTRAL: CN-01463019] [Google Scholar]
Blauvelt 2017d {published data only}
- Blauvelt A, Reich K, Warren RB, Szepietowski JC, Sigurgeirsson B, Tyring SK, et al. Secukinumab re-initiation achieves regain of high response levels in patients who interrupt treatment for moderate to severe plaque psoriasis. British Journal of Dermatology 2017;177(3):879-81. [CENTRAL: CN-01622237] [DOI] [PubMed] [Google Scholar]
Blauvelt 2017e {published data only}
- Blauvelt A, Papp KA, Lebwohl MG, Green LJ, Hsu S, Bhatt V, et al. Rapid onset of action in patients with moderate-to-severe psoriasis treated with brodalumab: a pooled analysis of data from two phase 3 randomized clinical trials (AMAGINE-2 and AMAGINE-3). Journal of the American Academy of Dermatology 2017;77(2):372-4. [CENTRAL: CN-01622584] [DOI] [PubMed] [Google Scholar]
Blauvelt 2017f {published data only}
- Blauvelt A, Papp KA, Langley RG, Luger T, Ohtsuki M, Leonardi CL, et al. Efficacy and safety of continuous ixekizumab treatment for 60 weeks in moderate-to-severe plaque psoriasis: results from the UNCOVER-3 trial. Journal of Clinical and Aesthetic Dermatology 2017;10(5 Supplement 1):S15. [CENTRAL: CN-01713049] [Google Scholar]
Blauvelt 2017g {published data only}
- Blauvelt A, Papp KA, Griffiths CE, Puig L, Weisman J, Dutronc Y, et al. Efficacy and safety of switching to ixekizumab in etanercept non-responders: a subanalysis from two phase III randomized clinical trials in moderate-to-severe plaque psoriasis (UNCOVER-2 and -3). American Journal of Clinical Dermatology 2017;18(2):273-80. [CENTRAL: CN-01368347] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blauvelt 2017h {published data only}
- Blauvelt A, Reich K, Warren R, Sigurgeirsson B, Langley R, Papavassilis C, et al. Secukinumab retreatment shows rapid recapture of treatment response: an analysis of a phase 3 extension trial in psoriasis. International Journal of Dermatology 2017;56(11):1264-5. [CENTRAL: CN-01570754] [Google Scholar]
Blauvelt 2017i {published data only}
- Blauvelt A, Ferris LK, Yamauchi PS, Qureshi A, Leonardi CL, Farahi K, et al. Extension of ustekinumab maintenance dosing interval in moderate-to-severe psoriasis: results of a phase IIIb, randomized, double-blinded, active-controlled, multicentre study (PSTELLAR). British Journal of Dermatology 2017;177(6):1552-61. [CENTRAL: CN-01428390] [DOI] [PubMed] [Google Scholar]
Blauvelt 2017j {published data only}
- Blauvelt A, Lebwohl MG, Green LJ, Hsu S, Bhatt V, Rastogi S, et al. Median time to treatment response in patients with moderate-to-severe plaque psoriasis treated with brodalumab 210mg or ustekinumab: A pooled analysis of data from two phase 3 randomized clinical trials (AMAGINE-2 and AMAGINE-3). Journal of Clinical and Aesthetic Dermatology 2017;10(5 Supplement 1):S22-3. [CENTRAL: CN-01628810] [DOI] [PubMed] [Google Scholar]
Blauvelt 2017k {published data only}
- Blauvelt A, Gooderham M, Iversen L, Ball S, Zhang L, Agada N, et al. Efficacy and safety of ixekizumab for the treatment of plaque psoriasis: results through 108 weeks randomised, phase III clinical trial (UNCOVER-3). Journal of Investigative Dermatology 2017;137(10 Supplement 2):S260. [CENTRAL: CN-01416619] [DOI] [PubMed] [Google Scholar]
Blauvelt 2018a {published data only}
- Blauvelt A, Reich K, Papp KA, Tyring SK, Sinclair R, Thaçi D, et al. Predictors of response to tildrakizumab for moderate to severe chronic plaque psoriasis. Acta Dermato-Venereologica 2018;98(Supplement 219):22. [CENTRAL: CN-01620162] [Google Scholar]
Blauvelt 2018b {published data only}
- Blauvelt A, Sofen H, Papp K, Gooderham M, Zhao Y, Lowry S, et al. Tildrakizumab efficacy over time by week 28 response levels in two phase 3 clinical trials in patients with chronic plaque psoriasis. Acta Dermato-Venereologica 2018;98(Supplement 219):49. [CENTRAL: CN-01920779] [Google Scholar]
Blauvelt 2018c {published data only}
- Blauvelt A, Papp KA, Griffiths CE, Puig L, Weisman J, Dutronc Y, et al. Correction to: Efficacy and safety of switching to ixekizumab in etanercept non-responders: a subanalysis from two phase III randomized clinical trials in moderate-to-severe plaque psoriasis (UNCOVER-2 and -3). American Journal of Clinical Dermatology 2018;19(3):457. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blauvelt 2018d {published data only}
- Blauvelt A, Tyring S, Philipp S, Adam D, Song M, Wasf Y, et al. Speed of response of guselkumab compared with adalimumab for the treatment of moderate-to-severe psoriasis: results through week 24 from the phase 3, double-blinded, placebo-and active comparator-controlled voyage 1 and voyage 2 trials. Acta Dermato-Venereologica 2018;98(Supplement 219):21. [CENTRAL: CN-01620164] [Google Scholar]
Blauvelt 2018e {published data only}
- Blauvelt A, Strober B, Langley R, Burge D, Pisenti L, Yassine M, et al. Safety of certolizumab pegol over 48 weeks in chronic plaque psoriasis phase 3 trials. Acta Dermato-Venereologica 2018;98(Supplement 219):21. [CENTRAL: CN-01620163] [Google Scholar]
Blauvelt 2018f {published data only}
- Blauvelt A, Reich K, Lebwohl M, Burge D, Arendt C, Peterson L, et al. Certolizumab pegol for the treatment of patients with moderate-to-severe chronic plaque psoriasis: pooled analysis of week 16 data from three randomized controlled trials. Journal of the European Academy of Dermatology and Venereology 2018;33(3):546-52. [CENTRAL: CN-01915790] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blauvelt 2018g {published data only}
- Blauvelt A, Muram TM, See K, Mallinckrodt CH, Crowley JJ, Van de Kerkhof P. Improvements in psoriasis within different body regions vary over time following treatment with ixekizumab. Journal of Dermatological Treatment 2018;29(3):220-9. [CENTRAL: CN-01604313] [DOI] [PubMed] [Google Scholar]
Blauvelt 2018h {published data only}
- Blauvelt A, Reich K, Papp KA, Kimball AB, Gooderham M, Tyring SK, et al. Safety of tildrakizumab for moderate-to-severe plaque psoriasis: pooled analysis of three randomized controlled trials. British Journal of Dermatology 2018;179(3):615-22. [CENTRAL: CN-01645090] [DOI] [PubMed] [Google Scholar]
Blauvelt 2018i {published data only}
- Blauvelt A, Tyring S, Gooderham M, Koo J, Zhao Y, Lowry S, et al. Better skin clearance is associated with improved quality of life in moderate-to-severe psoriasis patients treated with tildrakizumab. Acta Dermato-Venereologica 2018;98(Supplement 219):31-2. [CENTRAL: CN-01620179] [Google Scholar]
Branigan 2017 {published data only}
- Branigan P, Liu X, Chen Y, Scott B, Yao Z, Li S, et al. Sustained response following withdrawal of guselkumab treatment correlates with reduced Th17 and Th22 effector cytokine levels. Journal of Investigative Dermatology 2017;137(10 Supplement 2):S194. [CENTRAL: CN-01416625] [Google Scholar]
Brasil 2012 {published data only}
- Brasil Ministério da Saúde Departamento de Gestão e Incorporação de Tecnologias em, Saúde. Medicamentos biológicos (infliximabe, etanercepte, adalimumabe e ustequinumabe) para o tratamento da psoríase moderada a grave em adultos. conitec.gov.br/images/Incorporados/Biologicos-Psoriase-final.pdf 2012 (accessed prior to 17 December 2019).
Brasil 2013 {published data only}
- Brasil Ministério da Saúde Departamento de Gestão e Incorporação de Tecnologias em, Saúde. Golimumabe para artrite psoriásica. conitec.gov.br/images/Incorporados/Golimumabe-ArtritePsoriasica-final.pdf 2013 (accessed prior to 17 December 2019).
Brasil 2016 {published data only}
- Brasil Ministério da Saúde Comissão Nacional de Incorporação de Tecnologias no SUS. Golimumabe para o tratamento da artrite psoriásica. conitec.gov.br/images/Relatorios/2016/Relatorio_Golimumabe_ArtritePsoriasica_final.pdf 2016 (accessed prior to 17 December 2019).
Burden 2017 {published data only}
- Burden AD. Etanercept or infliximab for psoriasis? An independent randomized clinical trial. British Journal of Dermatology 2017;176(3):565. [CENTRAL: CN-01336581] [DOI] [PubMed] [Google Scholar]
Burkhardt 2017 {published data only}
- Burkhardt N, Mrowietz U, Carrascosa JM, Fernandez-Penas P, Guede D, Wilhelm S, et al. Absolute and relative PASI over 1 year of treatment with ixekizumab (IXE): Descriptive analysis in patients with moderate-to-severe plaque psoriasis. Australasian Journal of Dermatology 2017;58(Supplement 1):42. [CENTRAL: CN-01378807] [Google Scholar]
Callis Duffin 2017 {published data only}
- Callis Duffin K, Bagel J, Bukhalo M, Mercado Clement IJ, Choi SL, Zhao F, et al. Phase 3, open-label, randomized study of the pharmacokinetics, efficacy and safety of ixekizumab following subcutaneous administration using a prefilled syringe or an autoinjector in patients with moderate-to-severe plaque psoriasis (UNCOVER-A). Journal of the European Academy of Dermatology and Venereology : JEADV 2017;31(1):107-13. [CENTRAL: CN-01368719] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cassano 2006 {published data only}
- Cassano N, Loconsole F, Galluccio A, Miracapillo A, Pezza M, Vena GA. Once-weekly administration of high-dosage Etanercept in patients with plaque psoriasis: results of a pilot experience (power study). International Journal of Immunopathology and Pharmacology 2006;19(1):225-9. [CENTRAL: CN-00563725] [PubMed] [Google Scholar]
Cassano 2010 {published data only}
- Cassano N, Loconsole F, Miracapillo A, Travaglini M, Digiuseppe MD, Congedo M, et al. Treatment of psoriasis with different dosage regimens of etanercept: preliminary results from the Talpharanta Plastic Study Group. International Journal of Immunopathology and Pharmacology 2010;23(3):797-802. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cather 2006 {published data only}
- Cather J, Krueger G, Jackson M, Samstov A. Efficacy and safety of low-dose acitretin for the treatment of moderate to severe plaque-type psoriasis. Abstract P2877. American Academy of Dermatology 64th Annual Meeting March 3-7, 2006. Journal of the American Academy of Dermatology 2006;54(3 Suppl):AB217. [CENTRAL: CN-00602420] [Google Scholar]
Cather 2018 {published data only}
- Cather JC, Meeuwis K, Burge R, Bleakman AP, Lin CY, Gottlieb A, et al. Ixekizumab improves impact of genital psoriasis on sexual activity: results from a phase 3b study. Acta Dermato-Venereologica 2018;98(Supplement 219):11. [CENTRAL: CN-01620184] [Google Scholar]
Chakravadhanula 2017 {published data only}
- Chakravadhanula U, Chandrashekar BS, Parekh M, Krupashankar DS, Swaroop HS, Pawar D. One-year pilot study to evaluate sequential therapy with ciclosporin and itolizumab in treatment of chronic plaque psoriasis. British Journal of Dermatology 2017;177(5):e291. [CENTRAL: CN-01452514] [Google Scholar]
Chapman 2018 {published data only}
- Chapman M, Cirulli J, McBride S. Sustained improvement in patient-reported outcomes with continued apremilast treatment over 104 weeks in patients with moderate to severe psoriasis. Australasian Journal of Dermatology 2018;59(Supplement 1):46. [CENTRAL: CN-01606954] [Google Scholar]
ChiCTR‐INR‐16009710 {unpublished data only}
- ChiCTR-INR-16009710. Acitretin plus methotrexate in the treatment of moderate to severe psoriasis vulgaris [The role of keratin 17 in the pathogenesis of psoriasis through PI3K/Akt signal pathways]. www.chictr.org.cn/showprojen.aspx?proj=16444/ChiCTR-INR-16009710 (first received 2 November 2016).
Chládek 2002 {published data only}
- Chládek J, Grim J, Martínková J, Simková M, Vanìèková J, Koudelková V, et al. Pharmacokinetics and pharmacodynamics of low-dose methotrexate in the treatment of psoriasis. British Journal of Clinical Pharmacology 2002;54(2):147-56. [CENTRAL: CN-00409768] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chodorowska 1999a {published data only}
- Chodorowska G, Czelej D, Juszkiewicz-Borowiec M, Pietrzak A, Wojnowska D, Krasowska D. Selected cytokines and acute phase proteins in psoriatic patients treated with cyclosporin A or Re-PUVA methods. Annales Universitatis Mariae Curie-Sklodowska. Section D: Medicina 1999;54:173-80. [CENTRAL: CN-00325819] [PubMed] [Google Scholar]
Chodorowska 1999b {published data only}
- Chodorowska G, Czelej D, Juszkiewicz-Borowiec M, Pietrzak A, Wojnowska D, Krasowska D. Plasma levels of selected cytokines and acute phase proteins in 2 groups of psoriatic patients treated with cyclosporine A or RE-PUVA method. Journal of the European Academy of Dermatology and Venereology : JEADV 1999;12(Suppl 2):S330. [CENTRAL: CN-00478492] [PubMed] [Google Scholar]
Choi 2017 {published data only}
- Choi CW, Kim BR, Seo E, Youn SW. The objective Psoriasis Area and Severity Index: a randomized controlled pilot study comparing the effectiveness of ciclosporin and methotrexate. British Journal of Dermatology 2017;177(6):1740-1. [CENTRAL: CN-01914246] [DOI] [PubMed] [Google Scholar]
Crowley 2018a {published data only}
- Crowley J, Gisondi P, Geng Z, Servin OR. Long-term safety and efficacy of adalimumab from the phase 3 randomized, placebo-controlled trial in patients with nail and skin psoriasis. Acta Dermato-Venereologica 2018;98(Supplement 219):25. [CENTRAL: CN-01620198] [Google Scholar]
Crowley 2018b {published data only}
- Crowley J, Papp KA, Hong C, Parno J, Mendelsohn AM, Li Q, et al. Efficacy of tildrakizumab in etanercept partial responders or nonresponders. Acta Dermato-Venereologica 2018;98(Supplement 219):29. [CENTRAL: CN-01620188] [Google Scholar]
CTRI/2018/01/011373 {published data only}
- CTRI/2018/01/011373. Comparison of efficacy and safety of oral vs subcutaneous methotrexate in psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/01/011373 (first received 16 January 2018).
De Jong 2003 {published data only}
- De Jong EM, Mork NJ, Seijger MM, De La Brassine M, Lauharanta J, Jansen CT, et al. The combination of calcipotriol and methotrexate compared with methotrexate and vehicle in psoriasis: results of a multicentre placebo-controlled randomized trial. British Journal of Dermatology 2003;148(2):318-25. [CENTRAL: CN-00422725] [DOI] [PubMed] [Google Scholar]
De Mendizabal 2017 {published data only}
- De Mendizabal NV, Heathman M, Jackson K. A longitudinal PKPD model describing the effect of ixekizumab on static physician's global assessment score (sPGA) in patients with moderate-to-severe plaque psoriasis. Journal of Pharmacokinetics and Pharmacodynamics 2017;44(1 Supplement 1):S102. [Google Scholar]
Dubiel 1972 {published data only}
- Dubiel W, Happle R. Experimental treatment with fumaric acid monoethylester in psoriasis vulgaris [Behandlungsversuch mit Fumarsauremonoathylester bei Psoriasis vulgaris]. Zeitschrift fur Haut- und Geschlechtskrankheiten 1972;47(13):545-50. [PMID: ] [PubMed] [Google Scholar]
Duffin 2016 {published data only}
- Duffin KC, Bagel J, Bukhalo M, Clement IJ, Zhao F, Gill A, et al. Comparison of the pharmacokinetics of ixekizumab following subcutaneous administration using a prefilled syringe versus an autoinjector in patients with moderate-to-severe psoriasis. Journal of the American Academy of Dermatology 2016;74(5 Suppl 1):AB242. [EMBASE: 72275926] [DOI] [PMC free article] [PubMed] [Google Scholar]
Duffin 2017 {published data only}
- Duffin KC, Papp KA, Bagel J, Pharm DEL, Chen R, Gottlieb AB. Evaluation of the physician global assessment and body surface area composite tool for assessing psoriasis response to apremilast therapy: results from ESTEEM 1 and ESTEEM 2. Journal of Drugs in Dermatology 2017;16(2):147-53. [CENTRAL: CN-01416699] [PubMed] [Google Scholar]
Ecker‐Schlipf 2009 {published data only}
- Ecker-Schlipf B. Psoriasis vulgaris: How effective and safe is the calcineurin inhibitor voclosporin? [Psoriasis vulgaris: Wie wirksam und sicher ist der calcineurin- inhibitor voclosporin?]. Arzneimitteltherapie 2009;27(3):97-8. [EMBASE: 2009143373] [Google Scholar]
Edson‐Heredia 2013 {published data only}
- Edson-Heredia E, Banerjee S, Zhu B, Maeda-Chubachi T, Cameron G, Shen W, et al. A PASI ≥ 90 response is associated with improved patient reported outcomes: Results from a phase 2 study in patients with psoriasis treated with ixekizumab. Journal of the European Academy of Dermatology and Venereology 2013;27(Suppl 4):25. [DOI: 10.1111/jdv.12186] [DOI] [PubMed] [Google Scholar]
Egeberg 2016 {published data only}
- Egeberg A. Phase 3 trials of ixekizumab in moderate-to-severe plaque psoriasis. New England Journal of Medicine 2016;375(21):2101-2. [CENTRAL: CN-01296632] [DOI: 10.1056/NEJMc1610828] [DOI] [PubMed] [Google Scholar]
Elewski 2007 {published data only}
- Elewski B, Leonardi C, Gottlieb AB, Strober BE, Simiens MA, Dunn M, et al. Comparison of clinical and pharmacokinetic profiles of etanercept 25 mg twice weekly and 50 mg once weekly in patients with psoriasis. British Journal of Dermatology 2007;156(1):138-42. [CENTRAL: CN-00577519] [DOI] [PubMed] [Google Scholar]
Elewski 2017 {published data only}
- Elewski BE, Puig L, Mordin M, Gilloteau I, Sherif B, Fox T, et al. Psoriasis patients with Psoriasis Area and Severity Index (PASI) 90 response achieve greater health-related quality-of-life improvements than those with PASI 75-89 response: results from two phase 3 studies of secukinumab. Journal of Dermatological Treatment 2017;28(6):492-9. [CENTRAL: CN-01443627] [DOI] [PubMed] [Google Scholar]
Elewski 2018a {published data only}
- Elewski B, Menter M, Crowley J, Tyring J, Zhao Y, Lowry S, et al. Sustained and improved efficacy of tildrakizumab from week 28 to week 52 in treating moderate-to-severe plaque psoriasis. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Supplement 1):S25. [CENTRAL: CN-01713707] [Google Scholar]
Elewski 2018b {published data only}
- Elewski B, Menter A, Crowley J, Tyring S, Zhao Y, Lowry S, et al. Sustained and improved efficacy of tildrakizumab from week 28 to week 52 in treating moderate-to-severe plaque psoriasis. Acta Dermato-Venereologica 2018;98(Supplement 219):31. [CENTRAL: CN-01620180] [Google Scholar]
Ellis 1986 {published data only}
- Ellis CN, Gorsulowsky DC, Hamilton TA, Billings JK, Brown MD, Headington JT, et al. Cyclosporine improves psoriasis in a double-blind study. JAMA 1986;256(22):3110-6. [CENTRAL: CN-00045553] [PubMed] [Google Scholar]
Ellis 2001 {published data only}
- Ellis CN, Krueger GG. Treatment of chronic plaque psoriasis by selective targeting of memory effector T lymphocytes. New England Journal of Medicine 2001;345(4):248-55. [CENTRAL: CN-00349381] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Ellis CN, Mordin MM, Adler EY. Effects of alefacept on health-related quality of life in patients with psoriasis: results from a randomized, placebo-controlled phase II trial. American Journal of Clinical Dermatology 2003;4(2):131-9. [CENTRAL: CN-00435105] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ellis 2002 {published data only}
- Ellis CN, Reiter KL, Bandekar RR, Fendrick AM. Cost-effectiveness comparison of therapy for psoriasis with a methotrexate-based regimen versus a rotation regimen of modified cyclosporine and methotrexate. Journal of the American Academy of Dermatology 2002;46(2):242-50. [CENTRAL: CN-01783592] [PMID: ] [DOI] [PubMed] [Google Scholar]
Ellis 2012 {published data only}
- Chow C, Zhang Z, Goldfarb MT, Simpson MJ, Ellis CN. Evaluation of Psoriasis Area and Severity Index, Static Physician's Global Assessment, and Lattice System - Physician's Global Assessment for assessing severity of psoriasis. Journal of the American Academy of Dermatology 2012;131(Suppl 1):S81. [CENTRAL: CN-00843715] [Google Scholar]
Engst 1989 {published data only}
- Engst R, Huber J. Results of cyclosporin treatment of severe, chronical psoriasis vulgaris. Hautarzt 1989;40(8):486-9. [EMBASE: 1989202264] [PubMed] [Google Scholar]
Erkko 1997 {published data only}
- Erkko P, Granlund H, Nuutinen M, Reitamo S. Comparison of cyclosporin A pharmacokinetics of a new microemulsion formulation and standard oral preparation in patients with psoriasis. British Journal of Dermatology 1997;136(1):82-8. [PMID: ] [PubMed] [Google Scholar]
EUCTR2007‐004328‐18‐FR {published data only}
- EUCTR2007-004328-18-FR. A 12 week double-blind, randomised, placebo-controlled, modified dose-escalation trial to investigate safety, efficacy, and pharmacokinetics of BIRT 2584XX tablets at doses of 100, 300 and 500 mg administered once daily in patients with moderate to severe psoriasis with a 12 week treatment extension for PASI 50 responders. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2007-004328-18-FR (first received 14 November 2007).
EUCTR2012‐005685‐35‐DE {published data only}
- EUCTR2012-005685-35-DE. A study to compare the efficacy of a new developed product, FP187, to a marketed product, to each other but also to placebo, in patients with moderate to severe plaque psoriasis. The patients will be assigned to one of the three treatment arms by chance, and neither the investigator nor the patient will know the assigned group. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2012-005685-35-DE (first received 26 July 2013).
EUCTR2016‐001593‐15‐ES {published data only}
- EUCTR2016-001593-15-ES. Study to evaluate the efficacy and safety of high induction doses of adalimumab in moderate to severe psoriasis patients. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2016-001593-15-ES (first received 23 August 2016).
EUCTR2016‐003592‐21‐GB {published data only}
- EUCTR2016-003592-21-GB. Evaluating the benefits of using secukinumab rather than standard treatments as the first systemic treatment in moderate to severe psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2016-003592-21-GB (first received 17 October 2016).
EUCTR2018‐001021‐10‐SE {published data only}
- EUCTR2018-001021-10-SE. A clinical study with brodalumab for patients suffering from psoriasis and not benefitting the TNF-alpha treatment. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2018-001021-10-SE (first received 17 May 2018).
EUCTR2019‐000817‐35‐DE {published data only}
- EUCTR2019-000817-35-DE. An open-label, randomized, Phase IV study, to assess the efficacy and safety of tildrakizumab in patients with moderate to severe chronic plaque psoriasis who are non-responders to dimethyl fumarate therapy. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2019-000817-35-DE (first received 6 June 2019).
- NCT04263610. Efficacy and safety of tildrakizumab in participants with moderate-to-severe chronic plaque psoriasis who are non-responders to dimethyl fumarate therapy (TRANSITION). clinicaltrials.gov/show/NCT04263610 (first received 11 February 2020).
Ezquerra 2007 {published data only}
- Ezquerra GM, Regana MS, Millet PU. Combination of acitretin and oral calcitriol for treatment of plaque-type psoriasis. Acta Dermato-Venereologica 2007;87(5):449-50. [CENTRAL: CN-00619032] [DOI] [PubMed] [Google Scholar]
Feldman 2017 {published data only}
- Feldman SR, Green L, Kimball AB, Siu K, Zhao Y, Herrera V, et al. Secukinumab improves scalp pain, itching, scaling and quality of life in patients with moderate-to-severe scalp psoriasis. Journal of Dermatological Treatment 2017;28(8):716-21. [CENTRAL: CN-01454207] [DOI] [PubMed] [Google Scholar]
Fernandes 2013 {published data only}
- Fernandes IC, Torres T, Selores M. Maintenance treatment of psoriasis with cyclosporine A: comparison between continuous and weekend therapy. Journal of the American Academy of Dermatology 2013;68(2):341-2. [CENTRAL: CN-00841435] [DOI] [PubMed] [Google Scholar]
Fernandez 2017 {published data only}
- Fernandez Penas P, Goldblum O, Berggren L, Burkhardt N, Jullien D. Long-term clinical outcomes after 2 years of ixekizumab treatment in patients with moderate-to-severe psoriasis with a focus on absolute PASI. Journal of Investigative Dermatology 2017;137(5 Supplement 1):S58. [CENTRAL: CN-01375458] [Google Scholar]
Finzi 1993 {published data only}
- Italian Multicenter Study Group on Cyclosporin in Psoriasis. Cyclosporin versus etretinate: Italian multicenter comparative trial in severe plaque-form psoriasis. Dermatology (Basel, Switzerland) 1993;187(Suppl 1):8-18. [CENTRAL: CN-00095652] [DOI] [PubMed] [Google Scholar]
Fitz 2018 {published data only}
- Fitz L, Zhang W, Soderstrom C, Fraser S, Lee J, Quazi A, et al. Association between serum interleukin-17A and clinical response to tofacitinib and etanercept in moderate to severe psoriasis. Clinical and Experimental Dermatology 2018;43(7):790-7. [CENTRAL: CN-01923580] [DOI] [PubMed] [Google Scholar]
Fleischer 2005 {published data only}
- Fleischer AB, Carroll C, Hartle JE, Krejci-Manwaring J, McCarty MA, Feldman SR. A randomized, double-blind, right/left comparative study of the efficacy of acitretin with and without the co-administration of 0.1 percent tacrolimus ointment in the treatment of moderate to severe psoriasis. Journal of Investigative Dermatology 2005;124(4 Suppl):A46. [CENTRAL: CN-00550944] [Google Scholar]
Foley 2017 {published data only}
- Foley P, Song M, Shen YK, You Y, Wasfi Y, Griffiths CE. Guselkumab treatment provided higher frequency of complete skin clearance compared with adalimumab treatment among patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology 2017;177(5):e273-4. [DOI: 10.1111/bjd.16059] [DOI] [Google Scholar]
Foley 2018 {published data only}
- Foley P, Gordon K, Griffiths CE, Wasfi Y, Randazzo B, Song M, et al. Efficacy of guselkumab compared with adalimumab and placebo for psoriasis in specific body regions: a secondary analysis of 2 randomized clinical trials. JAMA Dermatology 2018;154(6):676-83. [CENTRAL: CN-01611616] [DOI] [PMC free article] [PubMed] [Google Scholar]
Fredriksson 1971 {published data only}
- Fredriksson T. Antipsoriatic activity of retinoic acid (vitamin A acid). Dermatologica 1971;142(3):133-6. [CENTRAL: CN-00006362] [DOI] [PubMed] [Google Scholar]
Fredriksson 1978 {published data only}
- Fredriksson T, Pettersson U. Severe psoriasis--oral therapy with a new retinoid. Dermatologica 1978;157(4):238-44. [CENTRAL: CN-00382865] [DOI] [PubMed] [Google Scholar]
Friedrich 2001 {published data only}
- Friedrich M, Sterry W, Klein A, Ruckert R, Docke WD, Asadullah K. Addition of pentoxifylline could reduce the side effects of fumaric acid esters in the treatment of psoriasis. Acta Dermato-Venereologica 2001;81(6):429-30. [CENTRAL: CN-00388555] [DOI] [PubMed] [Google Scholar]
Gambichler 2011 {published data only}
- Gambichler T, Tigges C, Scola N, Weber J, Skrygan M, Bechara FG, et al. Etanercept plus narrowband ultraviolet b phototherapy of psoriasis is more effective than etanercept monotherapy at 6 weeks. British Journal of Dermatology 2011;164(6):1383-6. [CENTRAL: CN-00812147] [DOI] [PubMed] [Google Scholar]
Ganguly 2004 {published data only}
- Ganguly R, Singh A, Sato R. Etanercept therapy provides clinically meaningful improvement in dermatology quality of life index in patients with chronic plaque psoriasis. Journal of the European Academy of Dermatology and Venereology: JEADV 2004;18(6):807. [CENTRAL: CN-00550919] [Google Scholar]
Gil 2003 {published data only}
- Gil JM, Sanchez-Regana M, PaIazon DB, Cuchillero RO, Ezquerra GM, Millet PU. Association between calcitriol per os and acitretinoin in the treatment of psoriasis. Journal of the European Academy of Dermatology and Venereology: JEADV 2003;17(Suppl 3):383. [CENTRAL: CN-00478546] [Google Scholar]
Glatt 2017 {published data only}
- Glatt S, Helmer E, Haier B, Strimenopoulou F, Price G, Vajjah P, et al. First-in-human randomized study of bimekizumab, a humanized monoclonal antibody and selective dual inhibitor of IL-17A and IL-17F, in mild psoriasis. British Journal of Clinical Pharmacology 2017;83(5):991-1001. [CENTRAL: CN-01447402] [DOI] [PMC free article] [PubMed] [Google Scholar]
Goerz 1978 {published data only}
- Goerz G, Orfanos CE. Systemic treatment of psoriasis with a new aromatic retinoid. Preliminary evaluation of a multicenter controlled study in the Federal Republic of Germany. Dermatologica 1978;157(Suppl 1):38-44. [PMID: ] [PubMed] [Google Scholar]
Gold 2018 {published data only}
- Gold LS, Forman S, Lebwohl M, Jackson JM, Goncalves J, Levi E, et al. Impact on quality of life and satisfaction with apremilast in patients with moderate plaque psoriasis: 52-week results of the UNVEIL study. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Supplement 1):S23-4. [CENTRAL: CN-01713690] [Google Scholar]
Goll 2017 {published data only}
- Goll GL, Jorgensen KK, Sexton J, Olsen IC, Bolstad N, Lorentzen M, et al. Long-term safety and efficacy of biosimilar infliximab (CT-P13) after switching from originator infliximab: results from the 26-week open label extension of a randomized Norwegian trial. Arthritis and Rheumatology 2017;69(Supplement 10):2800. [CENTRAL: CN-01423748] [Google Scholar]
Goll 2018 {published data only}
- Goll GL, Jorgensen KK, Sexton J, Olsen IC, Bolstad N, Lorentzen M, et al. Long-term safety and efficacy of biosimilar infliximab (CT-P13) after switching from originator infliximab: results from the 26-week open label extension of a Norwegian randomised trial. Annals of the Rheumatic Diseases 2018;77(Supplement 2):1383-4. [CENTRAL: CN-01647461] [DOI: 10.1136/annrheumdis-2018-eular.4620] [DOI] [Google Scholar]
Gollnick 1988 {published data only}
- Gollnick H, Bauer R, Brindley C, Orfanos CE, Plewig G, Wokalek H, et al. Acitretin versus etretinate in psoriasis. Clinical and pharmacokinetic results of a German multicenter study. Journal of the American Academy of Dermatology 1988;19(3):458-68. [CENTRAL: CN-00055942] [DOI] [PubMed] [Google Scholar]
Gollnick 1993 {published data only}
- Gollnick HP, Zaun H, Ruzicka T, Sommerburg C, Loew S, Mahrle G, et al. Relapse rate of severe generalized psoriasis after treatment with acitretin or etretinate. Results of the first randomized double-blind multicenter half-year follow-up study. European Journal of Dermatology 1993;3(6):442-6. [CENTRAL: CN-00181049] [Google Scholar]
Gollnick 2002 {published data only}
- Gollnick H, Altmeyer P, Kaufmann R, Ring J, Christophers E, Pavel S, et al. Topical calcipotriol plus oral fumaric acid is more effective and faster acting than oral fumaric acid monotherapy in the treatment of severe chronic plaque psoriasis vulgaris. Dermatology (Basel, Switzerland) 2002;205(1):46-53. [CENTRAL: CN-00397743] [DOI] [PubMed] [Google Scholar]
Gordon 2014 {published data only}
- Gordon K, Leonardi C, Braun D, Cameron G, Erickson J, Lebwohl M, et al. Results after at least 52 weeks of open label treatment with ixekizumab, an anti-IL-17A monoclonal antibody, in a phase 2 study in chronic plaque psoriasis. Journal of the American Academy of Dermatology 2014;70(5 Suppl 1):AB183. [CENTRAL: CN-01057458] [Google Scholar]
Gordon 2015 {published data only}
- Gordon KB, Leonardi C, Lebwohl M, Cameron G, Erickson J, Braun D, et al. Results after at least 52 weeks of open label treatment with ixekizumab, an anti-IL-17A monoclonal antibody, in a Phase 2 study in chronic plaque psoriasis. Journal of Clinical and Aesthetic Dermatology 2015;8(5 Supplement 1):S17-8. [CENTRAL: CN-01378778] [Google Scholar]
Gordon 2018a {published data only}
- Gordon K, Armstrong A, Foley P, Wasfi Y, Song M, Shen YK, et al. Long-term efficacy of guselkumab treatment after drug withdrawal and retreatment in patients with moderate-severe plaque psoriasis: results from voyage 2. Acta Dermato-Venereologica 2018;98(Supplement 219):22-3. [CENTRAL: CN-01620161] [DOI: 10.2340/00015555-2978] [DOI] [Google Scholar]
Gordon 2018b {published data only}
- Gordon K, Reich K, Pariser D, Menter A, Tyring S, Sofen H, et al. Efficacy of tildrakizumab in moderate to severe psoriasis patients with prior exposure to apremilast. Acta Dermato-Venereologica 2018;98(Supplement 219):29-30. [CENTRAL: CN-01620187] [DOI: 10.2340/00015555-2978] [DOI] [Google Scholar]
Gordon 2018c {published data only}
- Gordon K, Crowley J, Poulin Y, Mendelsohn A, Parno J, Rozzo S, et al. Disease severity and efficacy insights: patient-level pasi scores in tildrakizumab psoriasis trials. Acta Dermato-Venereologica 2018;98(Supplement 219):30-1. [DOI: 10.2340/00015555-2978] [DOI] [Google Scholar]
Gordon 2018d {published data only}
- Gordon KB, Armstrong AW, Han C, Foley P, Song M, Wasfi Y, et al. Anxiety and depression in patients with moderate-to-severe psoriasis and comparison of change from baseline after treatment with guselkumab vs. adalimumab: results from the Phase 3 VOYAGE 2 study. Journal of the European Academy of Dermatology and Venereology 2018;32(11):1940-9. [CENTRAL: CN-01617890] [DOI] [PubMed] [Google Scholar]
Gottlieb 2002 {published data only}
- Gottlieb AB, Vaishnaw K, Rizova E. Alefacept (AMEVIVETM) does not blunt primary or secondary immune responses. Journal of Investigative Dermatology 2002;118(6):1098. [CENTRAL: CN-00790440] [Google Scholar]
Gottlieb 2003b {published data only}
- Gottlieb AB, Casale TB, Frankel E, Goffe B, Lowe N, Ochs HD, et al. CD4+ T-cell-directed antibody responses are maintained in patients with psoriasis receiving alefacept: results of a randomized study. Journal of the American Academy of Dermatology 2003;49(5):816-25. [CENTRAL: CN-00474727] [DOI] [PubMed] [Google Scholar]
Gottlieb 2003c {published data only}
- Gottlieb AB, Feng A, Zitnik R. Prolonged response durability following ENBRELA® (etanercept) monotherapy. Journal of Investigative Dermatology 2003;121(1):68. [CENTRAL: CN-00795277] [Google Scholar]
Gottlieb 2004b {published data only}
- Gottlieb B, Goffe B, Veith J, Stevens S, Nakanishi A. Safety of etanercept in an integrated multistudy database of patients with psoriasis. Journal of Investigative Dermatology 2004;122(3):A55. [CENTRAL: CN-00509648] [Google Scholar]
Gottlieb 2005 {published data only}
- Gottlieb AB, Griffiths CE, Ho VC, Lahfa M, Mrowietz U, Murrell DF, et al. Oral pimecrolimus in the treatment of moderate to severe chronic plaque-type psoriasis: A double-blind, multicentre, randomized, dose-finding trial. British Journal of Dermatology 2005;152(6):1219-27. [CENTRAL: CN-00522446] [DOI] [PubMed] [Google Scholar]
Gottlieb 2006a {published data only}
- Gottlieb A, Zhang Y. A phase II trial of a new anti-inflammatory combination drug, CRx-140, in subjects with severe psoriasis. Journal of the American Academy of Dermatology 2006;54(3 Suppl):AB8. [CENTRAL: CN-00602228] [Google Scholar]
Gottlieb 2006b {published data only}
- Gottlieb A, Cather J, Hamilton T, Sherman M. Preliminary clinical safety and efficacy results from an open-label Phase 2 study of STA-5326, an oral IL-12/IL-23 inhibitor, in patients with moderate to severe chronic plaque psoriasis. Journal of the American Academy of Dermatology 2006;54(3 Suppl):AB10. [CENTRAL: CN-00602166] [Google Scholar]
Gottlieb 2010 {published data only}
- Gottlieb A, Menter A, Mendelsohn A, Shen YK, Li S, Guzzo C, Fretzin S, et al. Ustekinumab, a human interleukin 12/23 monoclonal antibody, for psoriatic arthritis: Randomised, double-blind, placebo-controlled, crossover trial. Lancet 2009;373(9664):633-40. [CENTRAL: CN-00686924] [DOI] [PubMed] [Google Scholar]
Gottlieb 2016 {published data only}
- Gottlieb A, Gerdes S, Lacour J, Korman N, Papp K, Dutronic Y, et al. Efficacy of ixekizumab in moderate-to-severe psoriasis patients who have or have not received prior biologic therapies: an integrated analysis of 3 phase 3 studies. Journal of Investigative Dermatology 2016;136(9 Supplement 2):S169. [CENTRAL: CN-01747590] [Google Scholar]
Gottlieb 2017a {published data only}
- Gottlieb A, Sullivan J, Kubanov A, You R, Regnault P, Frueh J. Secukinumab shows high and sustained efficacy in patients with moderate-to-severe palmoplantar psoriasis: 2.5-year results from the GESTURE study. British Journal of Dermatology 2017;177(5):e261. [CENTRAL: CN-01452515] [DOI] [PubMed] [Google Scholar]
Gottlieb 2017b {published data only}
- Gottlieb A, Sullivan J, Van Doorn M, Kubanov A, You R, Parneix A, et al. Secukinumab shows significant efficacy in palmoplantar psoriasis: results from GESTURE, a randomized controlled trial. Journal of the American Academy of Dermatology 2017;76(1):70-80. [CENTRAL: CN-01368596] [DOI] [PubMed] [Google Scholar]
Gottlieb 2017c {published data only}
- Gottlieb AB, Merola JF, Chen R, Levi E, Duffin KC. Assessing clinical response and defining minimal disease activity in plaque psoriasis with the Physician Global Assessment and body surface area (PGA x BSA) composite tool: an analysis of apremilast phase 3 ESTEEM data. Journal of the American Academy of Dermatology 2017;77(6):1178-80. [CENTRAL: CN-01443069] [DOI] [PubMed] [Google Scholar]
Gottlieb 2017d {published data only}
- Gottlieb AB, Lacour JP, Korman N, Wilhelm S, Dutronc Y, Schacht A, et al. Treatment outcomes with ixekizumab in patients with moderate-to-severe psoriasis who have or have not received prior biological therapies: an integrated analysis of two Phase III randomized studies. Journal of the European Academy of Dermatology and Venereology 2017;31(4):679-85. [CENTRAL: CN-01244380] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gottlieb 2018a {published data only}
- Gottlieb AB, Gordon K, Hsu S, Elewski B, Eichenfield LF, Kircik L, et al. Improvement in itch and other psoriasis symptoms with brodalumab in phase 3 randomized controlled trials. Journal of the European Academy of Dermatology and Venereology 2018;32(8):1305-13. [CENTRAL: CN-01572384] [DOI] [PubMed] [Google Scholar]
Gottlieb 2018b {published data only}
- Gottlieb AB, Blauvelt A, Thaçi D, Leonardi C, Poulin Y, Peterson L, et al. Durable reduction in absolute pasi with certolizumab pegol in patients with chronic plaque psoriasis. Acta Dermato-Venereologica 2018;98(Supplement 219):24. [CENTRAL: CN-01620157] [Google Scholar]
Goupille 1995 {published data only}
- Goupille P, Valat JP. Is methotrexate really effective in patients with psoriatic arthritis? Journal of Rheumatology 1995;22(12):2369-70. [PMID: ] [PubMed] [Google Scholar]
Goupille 2018 {published data only}
- Goupille P, Roussou E, Burmester G, Mease PJ, Gottlieb AB, Garces S, et al. Safety of ixekizumab in patients with psoriatic arthritis: results from a pooled analysis of three clinical trials. Annals of the Rheumatic Diseases 2018;77(Supplement 2):1039-40. [DOI: 10.1136/annrheumdis-2018-eular.2132] [DOI] [Google Scholar]
Griffiths 1998 {published data only}
- Griffiths CM, Boffa M, Wishart J, Adam C, Inglesias L, Van de Kerkhof P, et al. A double-blind, randomised trial to compare the effects of oral liarozole with acitretin in the treatment of chronic plaque psoriasis. British Journal of Dermatology 1998;139(Suppl 51):19. [CENTRAL: CN-00415772] [Google Scholar]
Griffiths 2002a {published data only}
- Griffiths CE, Humbert P, Koo J, Ortonne JP, Christophers E. Relationship between clinical response and quality of life in psoriasis patients treated with alefacept. Journal of the European Academy of Dermatology and Venereology : JEADV 2002;16(Suppl S1):292. [CENTRAL: CN-00478562] [Google Scholar]
Griffiths 2002b {published data only}
- Griffiths CE, Ortonne JP, Christophers E. Effect of alefacept based on patients' response to prior therapy for psoriasis. British Journal of Dermatology 2002;147(Suppl 62):45. [CENTRAL: CN-00406976] [Google Scholar]
Griffiths 2005 {published data only}
- Griffiths CE. A higher treatment standard for patients with moderate to severe psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2005;19(Suppl 2):7. [CENTRAL: CN-00602410] [Google Scholar]
Griffiths 2010 {published data only}
- Griffiths CE, Menter A, Strober BE, Yeilding N. Ustekinumab treatment in patients with moderate to severe psoriasis who are nonresponders to etanercept: results from a phase III clinical trial. Journal of the American Academy of Dermatology 2010;62(3 Suppl 1):AB137. [CENTRAL: CN-00843739] [DOI: 10.1016/j.jaad.2009.11.527] [DOI] [Google Scholar]
Griffiths 2016 {published data only}
- Griffiths CE, Warren R, Ilo D, Kerr L, Kent T, Mallbris L. Efficacy and safety of ixekizumab in patients with psoriasis who failed initial etanercept treatment: a subanalysis from UNCOVER 2, a randomized, double-blind, multicentre, phase III clinical trial. British Journal of Dermatology 2016;175(Suppl S1):68-9. [CENTRAL: CN-01303311] [DOI: 10.1111/bjd.14524] [DOI] [Google Scholar]
Griffiths 2017 {published data only}
- Griffiths CE, Vender R, Sofen H, Kircik L, Tan H, Rottinghaus ST, et al. Effect of tofacitinib withdrawal and re-treatment on patient-reported outcomes: results from a phase 3 study in patients with moderate to severe chronic plaque psoriasis. Journal of the European Academy of Dermatology & Venereology 2017;31(2):323-32. [CENTRAL: CN-01332752] [DOI: 10.1111/jdv.13808] [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffiths 2018a {published data only}
- Griffiths CE, Papp KA, Kimball AB, Randazzo B, Song M, Li S, et al. Long-term efficacy of guselkumab for the treatment of moderate-to-severe psoriasis: results from the phase 3 VOYAGE 1 trial through two years. Journal of Drugs in Dermatology 2018;17(8):826-32. [CENTRAL: CN-01655581] [PubMed] [Google Scholar]
Griffiths 2018b {published data only}
- Griffith C, Radtke MA, Youn SW, Bissonnette R, Song M, Wasfi Y, et al. Clinical response after guselkumab treatment among adalimumab PASI 90 non-responders: results from the voyage 1 and 2 trials. Acta Dermato-Venereologica 2018;98(Supplement 219):20. [CENTRAL: CN-01620165] [Google Scholar]
Griffiths 2018c {published data only}
- Griffiths C, Blauvelt A, Reich K, Leonardi C, Mehta N, Tsai T, et al. Secukinumab's long-term safety remains favorable up to 5 years of treatment. Acta Dermato-Venereologica 2018;98(Supplement 219):46. [CENTRAL: CN-01920781] [Google Scholar]
Grim 2000 {published data only}
- Grim J, Chladek J, Martinkova J, Simkova M, Vaneckova J, Koudelkova V. Pharmacokinetics (PK) and pharmacodynamics (PD) of low dose methotrexate (LDMTX) in the treatment of psoriasis. British Journal of Clinical Pharmacology 2000;50(4):390-1. [EMBASE: 2000362454] [Google Scholar]
Grossman 1994 {published data only}
- Grossman RM, Thivolet J, Claudy A, Souteyrand P, Guilhou JJ, Thomas P, et al. A novel therapeutic approach to psoriasis with combination calcipotriol ointment and very low-dose cyclosporine: results of a multicenter placebo-controlled study. Journal of the American Academy of Dermatology 1994;31(1):68-74. [CENTRAL: CN-00102638] [DOI] [PubMed] [Google Scholar]
Guenther 2020 {published data only}
- Guenther L, Potts Bleakman A, Weisman J, Poulin Y, Spelman L, Burge R, et al. Ixekizumab results in persistent clinical improvement in moderate-to-severe genital psoriasis during a 52 week randomized, placebo-controlled, phase 3 clinical trial. Acta Dermato-Venereologica 2020;100(1):adv00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gulliver 1996 {published data only}
- Gulliver WP, Murphy GF, Hannaford VA, Primmett DR. Increased bioavailability and improved efficacy, in severe psoriasis, of a new microemulsion formulation of cyclosporin. British Journal of Dermatology 1996;135(s48):35-9. [EMBASE: 1996272533] [DOI] [PubMed] [Google Scholar]
Gupta 2005 {published data only}
- Gupta SK, Dogra A, Kaur G. Comparative efficacy of methotrexate and hydroxyurea in treatment of psoriasis. Journal of Pakistan Association of Dermatologists 2005;15(3):247-51. [CENTRAL: 2005580293] [Google Scholar]
Gupta 2007 {published data only}
- Gupta R, Gupta S. Methotrexate-betamethasone weekly oral pulse in psoriasis. Journal of Dermatological Treatment 2007;18(5):291-4. [CENTRAL: CN-00619338] [DOI] [PubMed] [Google Scholar]
Gupta 2008 {published data only}
- Gupta AK, Langley RG, Lynde C, Barber K, Gulliver W, Lauzon G, et al. ISA247: quality of life results from a phase II, randomized, placebo-controlled study. Journal of Cutaneous Medicine and Surgery 2008;12(6):268-75. [CENTRAL: CN-00683900] [DOI] [PubMed] [Google Scholar]
Han 2013 {published data only}
- Han C, Kavanaugh A, Genovese MC, Hsu B, Deodhar AA, Hsia EC. Sustained improvement in health-related quality of life, work productivity, employability, and reduced healthcare resource utilization of patients with rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis treated with golimumab: 5-year results from 3 phase III studies. Arthritis and Rheumatism 2013;65(S10):S137. [CENTRAL: CN-01062782] [Google Scholar]
Hashizume 2007 {published data only}
- Hashizume H, Ito T, Yagi H, Takigawa M, Kageyama H, Furukawa F, et al. Efficacy and safety of preprandial versus postprandial administration of low-dose cyclosporin microemulsion (Neoral) in patients with psoriasis vulgaris. Journal of Dermatology 2007;34(7):430-4. [CENTRAL: CN-00610280] [DOI] [PubMed] [Google Scholar]
Hawkes 2018 {published data only}
- Hawkes JE, Lebwohl M, Elewski B, Kircik L, Reich K, Muscianisi E, et al. Secukinumab for the treatment of scalp, nail, and palmoplantar psoriasis. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Supplement 1):S28. [Google Scholar]
Heule 1988 {published data only}
- Heule F, Meinardi MM, Van Joost T, Bos JD. Low-dose cyclosporine effective in severe psoriasis: a double-blind study. Transplantation Proceedings 1988;20(3 Suppl 4):32-41. [CENTRAL: CN-00054273] [PubMed] [Google Scholar]
Ho 2010 {published data only}
- Ho SG, Yeung CK, Chan HH. Methotrexate versus traditional Chinese medicine in psoriasis: a randomized, placebo-controlled trial to determine efficacy, safety and quality of life. Clinical and Experimental Dermatology 2010;35(7):717-22. [CENTRAL: CN-00761451] [DOI] [PubMed] [Google Scholar]
Holzer 2020 {published data only}
- Holzer G, Hoke M, Sabeti-Sandor S, Perkmann T, Rauscher A, Strassegger B, et al. Disparate effects of adalimumab and fumaric acid esters on cardiovascular risk factors in psoriasis patients: results from a prospective, randomized, observer-blinded head-to-head trial. Journal of the European Academy of Dermatology & Venereology 2020;19:19. [DOI] [PubMed] [Google Scholar]
Hsu 2018 {published data only}
- Hsu S, Green L, Keegan BR, Kircik L, Rastogi S, Pillai R, et al. Efficacy of brodalumab in ustekinumab-naive and-experienced patients with moderate-to-severe plaque psoriasis. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Supplement 1):S27. [Google Scholar]
Hunter 1972 {published data only}
- Hunter GA, Simmons IJ, Thomas BM. A clinical trial of hydroxyurea for psoriasis. Australasian Journal of Dermatology 1972;13(3):93-9. [CENTRAL: CN-00008809] [DOI] [PubMed] [Google Scholar]
Iest 1989 {published data only}
- Iest J, Boer J. Combined treatment of psoriasis with acitretin and UVB phototherapy compared with acitretin alone and UVB alone. British Journal of Dermatology 1989;120(5):665-70. [CENTRAL: CN-00568569] [DOI] [PubMed] [Google Scholar]
Imafuku 2017 {published data only}
- Imafuku S, Torisu-Itakura H, Nishikawa A, Zhao F, Cameron GS, Japanese Uncover-Study Group. Efficacy and safety of ixekizumab treatment in Japanese patients with moderate-to-severe plaque psoriasis: subgroup analysis of a placebo-controlled, phase 3 study (UNCOVER-1). Journal of Dermatology 2017;44(11):1285-90. [CENTRAL: CN-01615794] [DOI] [PMC free article] [PubMed] [Google Scholar]
Iversen 2018 {published data only}
- Iversen L, Eidsmo L, Austad J, De Rie M, Osmancevic A, Skov L, et al. Secukinumab treatment in new-onset psoriasis: aiming to understand the potential for disease modification - rationale and design of the randomized, multicenter STEPIn study. Journal of the European Academy of Dermatology and Venereology 2018;32(11):1930-9. [CENTRAL: CN-01630270] [DOI] [PubMed] [Google Scholar]
Jackson 2018 {published data only}
- Jackson JM, Alikhan A, Lebwohl M, Stein Gold L, Levi E, Bagel J. Improvement in scalp and nails with apremilast in patients with moderate plaque psoriasis naive to systemic and biologic therapy: 52-week results of the UNVEIL study. Journal of Clinical and Aesthetic Dermatology 2018;11(5 Supplement 1):S20-S21. [Google Scholar]
Jacobe 2008 {published data only}
- Jacobe H, Winterfield L, Kim F, Huet-Adams B, Cayce R. The role of narrowband UV-B plus alefacept combination therapy in the treatment of psoriasis. Archives of Dermatology 2008;144(8):1067-8; author reply 1068-9. [CENTRAL: CN-00650560] [PMID: ] [DOI] [PubMed] [Google Scholar]
JapicCTI‐194706 2019 {published data only}
- JPRN-JapicCTI-194706. A multicenter, randomized, open-label study to evaluate the safe and effective use of the prefilled safety syringe or the auto-injector for the subcutaneous self-injection of bimekizumab solution by subjects with moderate to severe chronic plaque psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-JapicCTI-194706 (first received 11 April 2019).
jRCTs041180012 2018 {published data only}
- JPRN-jRCTs041180012. Comparison of phototherapy alone or together with apremilast in psoriasis vulgaris patients. www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-jRCTs041180012 (first received 9 November 2018).
Kaur 2018 {published data only}
- Kaur S, Shafiq N, Dogra S, Mittal BR, Attri SV, Bahl A, et al. 18F-fluorodeoxyglucose positron emission tomography-based evaluation of systemic and vascular inflammation and assessment of the effect of systemic treatment on inflammation in patients with moderate-to-severe psoriasis: a randomized placebo-controlled pilot study. Indian Journal of Dermatology, Venereology and Leprology 2018;84(6):660-6. [CENTRAL: CN-01670374] [DOI] [PubMed] [Google Scholar]
Kavanaugh 2009 {published data only}
- Kavanaugh A. The efficacy of ustekinumab on the articular and dermatologic manifestations of psoriatic arthritis. Current Rheumatology Reports 2009;11(4):233-4. [CENTRAL: CN-00958869] [DOI] [PubMed] [Google Scholar]
Kemeny 2019 {published data only}
- Kemeny L, Berggren L, Dossenbach M, Dutronc Y, Paul C. Efficacy and safety of ixekizumab in patients with plaque psoriasis across different degrees of disease severity: results from UNCOVER-2 and UNCOVER-3. Journal of Dermatological Treatment 2019;30(1):19-26. [CENTRAL: CN-01913619] [DOI] [PubMed] [Google Scholar]
Kimball 2008 {published data only}
- Kimball AB, Gordon KB, Langley RG, Menter A, Chartash EK, Valdes J, et al. Safety and efficacy of ABT-874, a fully human interleukin 12/23 monoclonal antibody, in the treatment of moderate to severe chronic plaque psoriasis: results of a randomized, placebo-controlled, phase 2 trial. Archives of Dermatology 2008;144(2):200-7. [CENTRAL: CN-00630180] [DOI] [PubMed] [Google Scholar]
Kimball 2011 {published data only}
- Kimball AB, Gordon KB, Langley RG, Menter A, Perdok RJ, Valdes J. Efficacy and safety of ABT-874, a monoclonal anti-interleukin 12/23 antibody, for the treatment of chronic plaque psoriasis: 36-week observation/retreatment and 60-week open-label extension phases of a randomized phase II trial. Journal of the American Academy of Dermatology 2011;64(2):263-74. [CENTRAL: CN-00770794] [DOI] [PubMed] [Google Scholar]
Kimball 2018 {published data only}
- Kimball AB, Luger T, Gottlieb A, Puig L, Kaufmann R, Burge R, et al. Long-term impact of ixekizumab on psoriasis itch severity: results from a phase III clinical trial and long-term extension. Acta Dermato-Venereologica 2018;98(1):98-102. [CENTRAL: CN-01446779] [DOI] [PubMed] [Google Scholar]
Koo 1998 {published data only}
- Koo J. A randomized, double-blind study comparing the efficacy, safety and optimal dose of two formulations of cyclosporin, Neoral and Sandimmun, in patients with severe psoriasis. OLP302 Study Group. British Journal of Dermatology 1998;139(1):88-95. [CENTRAL: CN-00155452] [DOI] [PubMed] [Google Scholar]
Kopp 2015 {published data only}
Kragballe 1989 {published data only}
- Kragballe K, Jansén CT, Geiger JM, Bjerke JR, Falk ES, Gip L, et al. A double-blind comparison of acitretin and etretinate in the treatment of severe psoriasis. Results of a Nordic multicentre study. Acta Dermato-Venereologica 1989;69(1):35-40. [CENTRAL: CN-00057941] [PubMed] [Google Scholar]
Krishnan 2005 {published data only}
- Krishnan KR, Cella D, Woolley M, Lalla D, Zitnik R, Brajac D. Etanercept improves symptoms of depression and fatigue in patients with psoriasis. In: 158th Annual Meeting of the American Psychiatric Association; 2005 May 21-26; Atlanta, GA. Vol. 158. 2005:NR293. [CENTRAL: CN-00595903]
Krishnan 2018 {published data only}
- Krishnan E, Zhang N, Wang H. Injection site reactions and injection site pain for the adalimumab biosimilar ABP 501: results from two double-blind randomized controlled studies. United European Gastroenterology Journal 2018;6(8 Supplement):A451. [CENTRAL: CN-01787637] [Google Scholar]
Kristensen 2017 {published data only}
- Kristensen LE, Merola JF, Dutz J, Adams DH, Kerr L, Rich P. Ixekizumab improves nail and skin lesions in patients with active psoriatic arthritis and prior TNF inadequate response. Annals of the Rheumatic Diseases 2017;76(Supplement 2):937. [CENTRAL: CN-01467783] [Google Scholar]
Krueger 1980 {published data only}
- Krueger GG, Shelby NJ, Hansen CD, Taylor MB. Comparison of labelling indices of skin involved and uninvolved with psoriasis: Placebo and oral retinoid RO 10-9359 vs. time. Clinical Research 1980;28(1):21A. [CENTRAL: CN-00192437] [Google Scholar]
Krueger 2002a {published data only}
- Feldman SR, Menter A, Koo JY. Improved health-related quality of life following a randomized controlled trial of alefacept treatment in patients with chronic plaque psoriasis. British Journal of Dermatology 2004;150(2):317-26. [CENTRAL: CN-00471158] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Krueger GG, Papp KA, Stough DB, Loven KH, Gulliver WP, Ellis CN, et al. A randomized, double-blind, placebo-controlled phase III study evaluating efficacy and tolerability of 2 courses of alefacept in patients with chronic plaque psoriasis. Journal of the American Academy of Dermatology 2002;47(6):821-33. [CENTRAL: CN-00411712] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Krueger GG. Clinical response to alefacept: Results of a phase 3 study of intravenous administration of alefacept in patients with chronic plague psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2003;17(Suppl 2):17-24. [CENTRAL: CN-00456895] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Menter A, Cather JC, Baker D, Farber HF, Lebwohl M, Darif M. The efficacy of multiple courses of alefacept in patients with moderate to severe chronic plaque psoriasis. Journal of the American Academy of Dermatology 2006;54(1):61-3. [CENTRAL: CN-00622887] [EMBASE: 2005584777] [DOI] [PubMed] [Google Scholar]
Krueger 2002b {published data only}
- Krueger G, Vaishnaw A, Rizova E. Pharmacodynamic effects of IM or IV Alefacept: Selective reductions in memory- effector (CD45RO+) cells are related to clinical improvement in psoriasis. Journal of Investigative Dermatology 2002;118(6):1098. [CENTRAL: CN-00795004] [Google Scholar]
Krueger 2003 {published data only}
- Krueger GG, Gordon KB, Van de Kerkhof P, Sterry W. Repeated courses of IM alefacept in psoriasis: rationale and design of an international study that mimics the clinical practice setting. Journal of Investigative Dermatology 2003;121(2):57. [CENTRAL: CN-00550788] [Google Scholar]
Krueger 2012 {published data only}
- Krueger JG, Fretzin S, Suarez-Farinas M, Haslett PA, Phipps KM, Cameron GS, et al. IL-17A is essential for cell activation and inflammatory gene circuits in subjects with psoriasis. Journal of Allergy and Clinical Immunology 2012;130(1):145-54.e9. [CENTRAL: CN-00832721] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Krueger 2015 {published data only}
- Krueger JG, Ferris LK, Menter A, Wagner F, White A, Visvanathan S, et al. Anti-IL-23A mAb BI 655066 for treatment of moderate-to-severe psoriasis: Safety, efficacy, pharmacokinetics, and biomarker results of a single-rising-dose, randomized, double-blind, placebo-controlled trial. Journal of Allergy and Clinical Immunology 2015;136(1):116-24.e7. [CENTRAL: CN-01110170] [PMID: ] [DOI] [PubMed] [Google Scholar]
Krueger 2016b {published data only}
- Krueger JG, Wharton K, Schlitt T, Torene R, Jiang X, Wang CQ, et al. Secukinumab, a new anti-IL17A biologic therapy, induces rapid and durable clinical, histological, and molecular resolution of psoriasis plaques over 1 year of administration. Experimental Dermatology 2016;25(Supplement 4):26. [Google Scholar]
Krupashankar 2014 {published data only}
- Dogra S, Krupashankar DS, Budamakuntla L, Srinivas CR, Khopkar U, Gupta S, et al. Long-term efficacy and safety of itolizumab in patients with moderate-to-severe chronic plaque psoriasis: a double-blind, randomized-withdrawal, placebo-controlled study. Journal of the American Academy of Dermatology 2015;73(2):331-3.e1. [CENTRAL: CN-01108850] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Krupashankar DS, Dogra S, Kura M, Saraswat A, Budamakuntla L, Sumathy TK, et al. Efficacy and safety of itolizumab, a novel anti-CD6 monoclonal antibody, in patients with moderate to severe chronic plaque psoriasis: Results of a double-blind, randomized, placebo-controlled, phase-III study. Journal of the American Academy of Dermatology 2014;71(3):484-92. [CENTRAL: CN-01002561] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kuijpers 1998 {published data only}
- Kuijpers AL, Van Pelt JP, Bergers M, Boegheim PJ, Den Bakker JE, Siegenthaler G, et al. The effects of oral liarozole on epidermal proliferation and differentiation in severe plaque psoriasis are comparable with those of acitretin. British Journal of Dermatology 1998;139(3):380-9. [CENTRAL: CN-00159672] [DOI] [PubMed] [Google Scholar]
Lajevardi 2015 {published data only}
- Lajevardi V, Hallaji Z, Daklan S, Abedini R, Goodarzi A, Abdolreza M. The efficacy of methotrexate plus pioglitazone vs. methotrexate alone in the management of patients with plaque-type psoriasis: a single-blinded randomized controlled trial. International Journal of Dermatology 2015;54(1):95-101. [CENTRAL: CN-01052011] [DOI] [PubMed] [Google Scholar]
Lambert 2018 {published data only}
- Lambert J, Ghislain P-D, Merola J, Potts-Bleakman A, Brnabic AJ, Burge R, et al. Clinical signs of epithelial surface disruption impact pain and sexual health in patients with moderate-to-severe genital psoriasis. British Journal of Dermatology 2018;179(Supplement 1):36. [CENTRAL: CN-01620064] [Google Scholar]
Langewouters 2005 {published data only}
- Langewouters AM, Bovenschen HJ, De Jong EM, Erp PJM, Van de Kerkhof PC. The effect of topical corticosteroids in combination with alefacept on circulating T-cell subsets in psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2005;19(Suppl 2):240. [CENTRAL: CN-00602421] [DOI] [PubMed] [Google Scholar]
Langley 2006 {published data only}
- Langley R, Leondardi C, Okun M. Long-term safety and efficacy of adalimumab in psoriasis. In: 4th European Association of Dermatology and Venereology (EADV) Spring Symposium Saariselka, Lapland, Finland. February 9-12th, 2006. Vol. Suppl. 2006:P-021. [CENTRAL: CN-00602234]
Langley 2010 {published data only}
- Langley RG, Papp K, Bissonnette R, Toth D, Matheson R, Hultquist M, et al. Safety profile of intravenous and subcutaneous siplizumab, an anti-CD2 monoclonal antibody, for the treatment of plaque psoriasis: results of two randomized, double-blind, placebo-controlled studies. International Journal of Dermatology 2010;49(7):818-28. [CENTRAL: CN-00761682] [DOI] [PubMed] [Google Scholar]
Langley 2016 {published data only}
- Langley R, Feldman S, Paul C, Gordon K, Strand V, Toth D, et al. Treatment with ixekizumab over 60 weeks provides sustained improvements in healthrelated quality of life: results from UNCOVER-1, a randomized phase 3 trial. Journal of Investigative Dermatology 2016;136(9 Supplement 2):S169. [CENTRAL: CN-01383388] [Google Scholar]
Langley 2018 {published data only}
- Langley RG, Tsai TF, Flavin S, Song M, Randazzo B, Wasfi Y, et al. Efficacy and safety of guselkumab in patients with psoriasis who have an inadequate response to ustekinumab: results of the randomized, double-blind, phase III NAVIGATE trial. British Journal of Dermatology 2018;178(1):114-23. [CENTRAL: CN-01421735] [DOI: 10.1111/bjd.15750] [DOI] [PubMed] [Google Scholar]
Langner 2004 {published data only}
- Langner A, Roszkiewicz J, Baran E, Placek W. Results of a phase II study of a novel oral fumarate, BG-12, in the treatment of severe psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2004;18(6):798. [CENTRAL: CN-00550917] [Google Scholar]
Lauharanta 1989 {published data only}
- Lauharanta J, Geiger JM. A double-blind comparison of acitretin and etretinate in combination with bath PUVA in the treatment of extensive psoriasis. British Journal of Dermatology 1989;121(1):107-12. [CENTRAL: CN-00061540] [DOI] [PubMed] [Google Scholar]
Lawrence 1983 {published data only}
- Lawrence CM, Marks J, Shuster S. Addition of retinoids to PUVA for psoriasis. Lancet 1983;1(8326 Pt 1):706. [CENTRAL: CN-00030597] [DOI] [PubMed] [Google Scholar]
Leavell 1970 {published data only}
- Leavell UW, Yarbro JW. Hydroxyurea. A new treatment for psoriasis. Archives of Dermatology 1970;102(2):144-50. [CENTRAL: CN-00004668] [DOI] [PubMed] [Google Scholar]
Lebwohl 2003 {published data only}
- Finlay AY, Salek MS, Haney J, Alefacept Clinical Study Group. Intramuscular alefacept improves health-related quality of life in patients with chronic plaque psoriasis. Dermatology (Basel, Switzerland) 2003;206(4):307-15. [CENTRAL: CN-00437818] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Lebwohl M, Christophers E, Langley R, Ortonne JP, Roberts J, Griffiths CE, et al. An international, randomized, double-blind, placebo-controlled phase 3 trial of intramuscular alefacept in patients with chronic plaque psoriasis. Archives of Dermatology 2003;139(6):719-27. [CENTRAL: CN-00438439] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Ortonne JP, Lebwohl M, Griffiths CE. Alefacept-induced decreases in circulating blood lymphocyte counts correlate with clinical response in patients with chronic plaque psoriasis. European Journal of Dermatology 2003;13(2):117-23. [CENTRAL: CN-00436640] [PMID: ] [PubMed] [Google Scholar]
- Ortonne JP. Clinical response to alefacept: results of a phase 3 study of intramuscular administration of alefacept in patient with chronic plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2003;17(Suppl 2):12-6. [CENTRAL: CN-00456894] [PMID: ] [DOI] [PubMed] [Google Scholar]
Lebwohl 2003a {published data only}
- Lebwohl M. The effect of psoriasis and its treatments on circulating T-cell subsets: results of alefacept studies. Journal of the European Academy of Dermatology and Venereology : JEADV 2003;17(Suppl 3):377. [CENTRAL: CN-00478640] [Google Scholar]
Lebwohl 2009 {published data only}
- Lebwohl M, Kimball A, Gordon K, Szapary P. Comparable efficacy and safety of ustekinumab in moderate to severe psoriasis patients previously treated with systemic therapies and treatment-naive patients. Journal of the American Academy of Dermatology 2009;67th Annual Meeting of the American Academy of Dermatology, AAD San Francisco, CA United States:Supplemental. [Google Scholar]
Lebwohl 2012 {published data only}
- Lebwohl MG, Kircik L, Callis Duffin K, Pariser D, Hooper M, Wenkert D, et al. Safety and efficacy of adding topical therapy to etanercept in patients with moderate to severe plaque psoriasis. Dermatology and Therapy 2012;2:S39. [CENTRAL: CN-01027857] [DOI] [PubMed] [Google Scholar]
Lebwohl 2013 {published data only}
- Lebwohl MG, Kircik L, Callis Duffin K, Pariser D, Hooper M, Wenkert D, et al. A randomized study to evaluate the efficacy and safety of adding topical therapy to etanercept in patients with moderate to severe plaque psoriasis. Journal of the American Academy of Dermatology 2013;69(3):385-92. [CENTRAL: CN-00964028] [DOI] [PubMed] [Google Scholar]
Ledo 1988 {published data only}
- Ledo A, Martin M, Geiger JM, Marron JM. Acitretin (Ro 10-1670) in the treatment of severe psoriasis. A randomized double-blind parallel study comparing acitretin and etretinate. International Journal of Dermatology 1988;27(9):656-60. [CENTRAL: CN-00058382] [DOI] [PubMed] [Google Scholar]
Legat 2005 {published data only}
- Legat LJ, Hofer A, Wackernagel A, Salmhofer W, Kerl H, Wolf P. Alefacept plus 311 nm narrowband ultraviolet B (NB-UVB) phototherapy in the treatment of psoriasis. Journal of Investigative Dermatology 2005;125(1):A4. [CENTRAL: CN-00550842] [Google Scholar]
Leonardi 2010a {published data only}
- Leonardi C, Guenther L, Wasel N, Yeilding N, Szapary PO, Hsu MC, et al. Characterization of infections associated with ustekinumab in moderate to severe psoriasis patients. Journal of the European Academy of Dermatology and Venereology 2010;24(Suppl 4):22. [EMBASE: 70238720] [Google Scholar]
Leonardi 2010b {published data only}
- Leonardi C, Menter A, Gu Y, Okun M. Efficacy and safety of weekly adalimumab in psoriasis patients with a less than PASI 50 response to 40 mg every other week: results from an open-label extension study. Journal of the European Academy of Dermatology and Venereology 2010;24(Suppl 4):9-10. [EMBASE: 70238693] [Google Scholar]
Leonardi 2010c {published data only}
- Leonardi C, Papp K, Asahina A, Gu Y, Rozzo S. Long-term safety of adalimumab for psoriasis: An analysis of all adalimumab exposure in all global clinical trials. Journal of the European Academy of Dermatology and Venereology 2010;24:26. [CENTRAL: 70238729] [Google Scholar]
Leonardi 2011a {published data only}
- Leonardi C, Kimball A, Schenkel B, Papp K. Sustained improvement in skin disease specific quality of life in patients with moderate to severe psoriasis receiving ustekinumab maintenance therapy: long-term results from PHOENIX 1. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB149. [CENTRAL: CN-00843843] [DOI: 10.1016/j.jaad.2010.09.608] [DOI] [Google Scholar]
Leonardi 2011b {published data only}
- Leonardi C, Langley RG, Papp K, Tyring SK, Wasel N, Vender R, et al. Adalimumab for treatment of moderate to severe chronic plaque psoriasis of the hands and feet: efficacy and safety results from REACH, a randomized, placebo-controlled, double-blind trial. Archives of Dermatology 2011;147(4):429-36. [CENTRAL: CN-00785710] [DOI] [PubMed] [Google Scholar]
Levell 1995 {published data only}
- Levell NJ, Shuster S, Munro CS, Friedmann PS. Remission of ordinary psoriasis following a short clearance course of cyclosporin. Acta Dermato-Venereologica 1995;75(1):65-9. [CENTRAL: CN-00113972] [DOI] [PubMed] [Google Scholar]
Li 2018 {published data only}
- Li N, Teeple A, Muser E, McElligott S, You Y, Song M, et al. Work/study productivity gain and indirect cost savings with guselkumab compared with adalimumab in moderate to severe psoriasis: results from the VOYAGE 1 study. Journal of Managed Care and Specialty Pharmacy 2018;24(10 A):S81. [CENTRAL: CN-01670028] [DOI] [PubMed] [Google Scholar]
Liang 1995 {published data only}
- Liang GS, Kerdel FA. Combination therapy and the use of an initial dose of intramuscular methotrexate in patients hospitalized for psoriasis. Journal of Dermatological Treatment 1995;6(2):73-6. [CENTRAL: CN-00171665] [Google Scholar]
Louw 2017 {published data only}
- Louw I, Kivitz AJ, Takeuchi T, Tanaka Y, Nakashima S, Hodge J, et al. The long-term safety and durability of response of CHS-0214, a proposed biosimilar to etanercept: an open-label safety extension study. Arthritis and Rheumatology 2017;69(Supplement 10):2492. [CENTRAL: CN-01423778] [Google Scholar]
Lui 2011 {published data only}
- Lui H, Tan J, Shear N, Bissonnette R, Gulliver W. Efficacy and safety of alefacept in combination with narrowband uvb compared to alefacept alone in subjects with moderate to severe psoriasis: results of the Canadian alefacept phototherapy psoriasis study. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB150. [CENTRAL: CN-00843846] [Google Scholar]
Lui 2012 {published data only}
- Lui H, Gulliver W, Tan J, Hong CH, Hull P, Shear NH, et al. A randomized controlled study of combination therapy with alefacept and narrow band UVB phototherapy (UVB) for moderate to severe psoriasis: efficacy, onset, and duration of response. Journal of Drugs in Dermatology 2012;11(8):929-37. [CENTRAL: CN-01164684] [PubMed] [Google Scholar]
Lynde 2012 {published data only}
- Lynde CW, Gupta AK, Guenther L, Poulin Y, Levesque A, Bissonnette R. A randomized study comparing the combination of nbUVB and etanercept to etanercept monotherapy in patients with psoriasis who do not exhibit an excellent response after 12 weeks of etanercept. Journal of Dermatological Treatment 2012;23(4):261-7. [CENTRAL: CN-00972294] [PMID: ] [DOI] [PubMed] [Google Scholar]
Macdonald 1972 {published data only}
- Macdonald A, Fry L. Retinoic acid in the treatment of psoriasis. British Journal of Dermatology 1972;86(5):524-7. [CENTRAL: CN-00007340] [DOI] [PubMed] [Google Scholar]
Mahrle 1995 {published data only}
- Mahrle G, Schulze HJ, Farber L, Weidinger G, Steigleder GK. Low-dose short-term cyclosporine versus etretinate in psoriasis: improvement of skin, nail, and joint involvement. Journal of the American Academy of Dermatology 1995;32(1):78-88. [CENTRAL: CN-00109143] [DOI] [PubMed] [Google Scholar]
Malik 2010 {published data only}
- Malik T, Ejaz A. Comparison of methotrexate and azathioprine in the treatment of psoriasis: A randomized controlled trial. Journal of Pakistan Association of Dermatologists 2010;20(3):152-7. [CENTRAL: CN-00789615] [Google Scholar]
Marecki 2004 {published data only}
- Marecki S, Kirkpatrick P. Efalizumab. Nature Reviews. Drug Discovery 2004;3(6):473-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Marks 1986 {published data only}
- Marks JM. Cyclosporin A treatment of severe psoriasis. British Journal of Dermatology 1986;115(6):745-6. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mate 2017 {published data only}
- Mate E, Bagel J, Callis-Duffin K, Moore A, Ferris L, Siu K, et al. Secukinumab is efficacious in clearing moderate-tosevere scalp psoriasis: 12 week results of a randomized phase IIIb study. Australasian Journal of Dermatology 2017;58(Supplement 1):71. [CENTRAL: CN-01378822] [Google Scholar]
Mate 2018 {published data only}
- Mate E, Bissonnette R, Luger T, Thaçi D, Toth D, Lacombe A, et al. Secukinumab demonstrates high sustained efficacy and a favourable safety profile through 5 years of treatment in moderate to severe psoriasis. Australasian Journal of Dermatology 2018;59(Supplement 1):86. [CENTRAL: CN-01919964] [Google Scholar]
McInnes 2013 {published data only}
- McInnes IB, Papp K, Puig L, Reich K, Ritchlin CT, Strober B, et al. Safety of ustekinumab from the placebo-controlled periods of psoriatic arthritis and psoriasis clinical developmental programs. Arthritis and Rheumatism 2013;72:Suppl. [CENTRAL: CN-01058553] [Google Scholar]
McInnes 2017 {published data only}
- McInnes IB, Mease PJ, Ritchlin CT, Rahman P, Gottlieb AB, Kirkham B, et al. Secukinumab sustains improvement in signs and symptoms of psoriatic arthritis: 2 year results from the phase 3 FUTURE 2 study. Rheumatology 2017;56(11):1993-2003. [CENTRAL: CN-01424217] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mease 2011 {published data only}
- Mease P, Genovese MC, Gladstein G, Kivitz AJ, Ritchlin C, Tak PP, et al. Abatacept in the treatment of patients with psoriatic arthritis: results of a six-month, multicenter, randomized, double-blind, placebo-controlled, phase II trial. Arthritis and Rheumatism 2011;63(4):939-48. [CENTRAL: CN-00779390] [DOI] [PubMed] [Google Scholar]
Mease 2016a {published data only}
- Mease PJ, Okada M, Kishimoto M, Shuler CL, Carlier H, Lin CY, et al. Efficacy and safety of ixekizumab in patients with active psoriatic arthritis: 52 week results from a phase 3 study. Arthritis and Rheumatology 2016;68(Supplement 10):1270-1. [CENTRAL: CN-01296553] [DOI] [PubMed] [Google Scholar]
Mease 2016b {published data only}
- Mease P, Van Der Heijde D, Ritchlin C, Cuchacovich R, Shuler C, Lin CY, et al. A randomized, double-blind, active- and placebo-controlled phase 3 study of efficacy and safety of ixekizumab, adalimumab, and placebo therapy in patients naive to biologic disease modifying antirheumatic drugs with active psoriatic arthritis. Journal of Rheumatology 2016;43(6):1169. [CENTRAL: CN-01294588] [Google Scholar]
Mease 2017a {published data only}
- Mease PJ, Van der Heijde D, Ritchlin CT, Okada M, Cuchacovich RS, Shuler CL, et al. Ixekizumab, an interleukin-17A specific monoclonal antibody, for the treatment of biologic-naive patients with active psoriatic arthritis: results from the 24-week randomised, double-blind, placebo-controlled and active (adalimumab)-controlled period of the phase III trial SPIRIT-P1. Annals of the Rheumatic Diseases 2017;76(1):79-87. [CENTRAL: CN-01374947] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mease 2017b {published data only}
- Mease P, Kishimoto M, Okada M, Lee C, Moriarty S, Mou J, et al. 52-Week efficacy and safety results from SPIRIT-P1: A phase 3 study of ixekizumab in patients with active psoriatic arthritis. Journal of Rheumatology 2017;44(6):925. [CENTRAL: CN-01398036] [DOI] [PubMed] [Google Scholar]
Mease 2017c {published data only}
- Mease P, Okada M, Kishimoto M, Shuler C, Carlier H, Lin C, et al. Fifty two-week efficacy and safety results from SPIRIT-P1: a phase 3 study of ixekizumab in patients with active psoriatic arthritis. Journal of Investigative Dermatology 2017;137(10 Supplement 2):S260. [CENTRAL: CN-01416618] [Google Scholar]
Mease 2018 {published data only}
- Mease P, Van der Heijde D, Landewe R, Mpofu S, Rahman P, Tahir H, et al. Secukinumab improves active psoriatic arthritis symptoms and inhibits radiographic progression: primary results from the randomised, double-blind, phase III FUTURE 5 study. Annals of the Rheumatic Diseases 2018;77(6):890-7. [CENTRAL: CN-01606299] [DOI] [PMC free article] [PubMed] [Google Scholar]
Meffert 1989 {published data only}
- Meffert H, Sönnichsen N. Acitretin in the treatment of severe psoriasis: a randomized double-blind study comparing acitretin and etretinate. Acta Dermato-Venereologica. Supplementum 1989;146:176-7. [CENTRAL: CN-00064910] [PubMed] [Google Scholar]
Menon 2012 {published data only}
- Menon S, Boy MG, Wang C, Wilkinson BE, Zwillich SH, Chan G, et al. Single and multiple-dose pharmacokinetics of tofacitinib (CP-690,550) from a double-blind, placebo-controlled, dose-escalation study in medically stable subjects with psoriasis. Clinical Pharmacology and Therapeutics 2012;91:S33. [CENTRAL: CN-01034861] [Google Scholar]
Menter 2007 {published data only}
- Menter A, Guzzo C, Li S, Gottlieb AB. Efficacy of infliximab in patients with severe psoriasis: Subgroup analysis from clinical trials. Journal of the American Academy of Dermatology 2007;56(2):AB174. [CENTRAL: CN-00615988] [Google Scholar]
Menter 2014 {published data only}
- Menter A, Papp KA, Tan H, Tyring S, Wolk R, Buonanno M. Efficacy of tofacitinib, an oral janus kinase inhibitor, on clinical signs of moderate-to-severe plaque psoriasis in different body regions. Journal of Drugs in Dermatology 2014;13(3):252-6. [CENTRAL: CN-00985274] [PubMed] [Google Scholar]
Merola 2017 {published data only}
- Merola JF, Elewski B, Tatulych S, Lan S, Tallman A, Kaur M. Efficacy of tofacitinib for the treatment of nail psoriasis: two 52-week, randomized, controlled phase 3 studies in patients with moderate-to-severe plaque psoriasis. Journal of the American Academy of Dermatology 2017;77(1):79-87.e1. [CENTRAL: CN-01401051] [DOI] [PubMed] [Google Scholar]
Merola 2018 {published data only}
- Merola JF, Kishimoto M, Adams D, Park SY, Thaçi D. Ixekizumab improves nail and skin psoriasis through 52 weeks of treatment in patients with active psoriatic arthritis: Results from two randomized, double-blind, phase 3, clinical trials (SPIRIT-P1 and SPIRIT-P2). Acta Dermato-Venereologica 2018;98(Supplement 219):16. [CENTRAL: CN-01620172] [Google Scholar]
Meyer 2011 {published data only}
- Meyer MW, Zachariae C, Bendtzen K, Skov L. Immunogenicity of tumour necrosis factor inhibitors in patients with psoriasis receiving long-term treatment. British Journal of Dermatology 2011;165(6):e17. [EMBASE: 70610785] [Google Scholar]
Mittal 2009 {published data only}
- Mittal R, Malhotra S, Pandhi P, Kaur I, Dogra S. Efficacy and safety of combination Acitretin and Pioglitazone therapy in patients with moderate to severe chronic plaque-type psoriasis: a randomized, double-blind, placebo-controlled clinical trial. Archives of Dermatology 2009;145(4):387-93. [CENTRAL: CN-00682023] [DOI] [PubMed] [Google Scholar]
Moller 2009 {published data only}
- Moller I. Efficacy of leflunomide in patients with psoriatic arthritis [Eficacia del tratamiento con leflunomida en pacientes con artritis psoriasica]. Seminarios de la Fundacion Espanola de Reumatologia 2009;10(2):48-52. [PMID: 2009314647] [Google Scholar]
Monk 1986 {published data only}
- Monk BE. Cyclosporin A and psoriasis. British Journal of Dermatology 1986;115(2):249-50. [PMID: ] [DOI] [PubMed] [Google Scholar]
Montgomery 1993 {published data only}
- Montgomery JA, Snyder HW Jr, Walsh DA, Walsh GM. BCX-34. Purine nucleoside phosphorylase (PNP) inhibitor. Drugs of the Future 1993;18(10):887-90. [EMBASE: 1994025323] [Google Scholar]
Mrowietz 1991 {published data only}
- Mrowietz U, Christophers E. Low-dose ciclosporin A (Sandimmun) in psoriasis: a multicenter dose-finding study. Zeitschrift fur Hautkrankheiten 1991;66(Suppl 1):25-9. [CENTRAL: CN-00182853] [Google Scholar]
Mrowietz 2012 {published data only}
- Mrowietz U, Reich K, Rozzo S, Gu Y. Achievement of European Consensus Programme treatment goals in three clinical trials of adalimumab in moderate-to-severe psoriasis. Journal of the American Academy of Dermatology 2012;66(4 Suppl 1):AB183. [EMBASE: 70704582] [Google Scholar]
Narang 2012 {published data only}
- Narang T, Dogra S, Handa S. Serendipity opens new avenues: a pilot study to evaluate the efficacy of saxagliptin in combination with cyclosporine and acitretin in diabetic psoriasis patients. Dermatology and Therapy 2012;2(Suppl 1):S36-7. [CENTRAL: CN-01027858] [Google Scholar]
Nash 2015 {published data only}
- Nash P, Gottlieb A, Mease P, McInnes I, Kirkham B, Kavanaugh A, et al. Secukinumab, a human anti-interleukin-17a monoclonal antibody, significantly reduces psoriasis burden in patients with psoriatic arthritis: results from a phase 3 randomized controlled trial. Internal Medicine Journal 2015;45(Suppl 2):42. [CENTRAL: CN-01361215] [Google Scholar]
NCT00106847 {published data only}
- NCT00106847. A study of the safety and effectiveness of infliximab in patients with plaque-type psoriasis. clinicaltrials.gov/ct2/show/NCT00106847 (first received 1 April 2005).
NCT00111111 {published data only}
- NCT00111111. An evaluation of etanercept in the treatment of subjects with psoriasis. clinicaltrials.gov/ct2/show/nct00111111 (first received 18 May 2005).
NCT00258713 {published data only}
- NCT00258713. A 36-week extension to protocol ISA04-03. clinicaltrials.gov/ct2/show/NCT00258713 (first received 28 November 2005).
NCT00358670 {published data only}
- NCT00358670. Long-term effects of infliximab in the treatment of moderate to severe psoriasis [Extension of Study P04271, NCT00251641] (P04563). clinicaltrials.gov/ct2/show/nct00358670 (first received 1 August 2006).
NCT00377325 {published data only}
- NCT00377325. The effectiveness of lower cyclosporine doses for psoriasis. clinicaltrials.gov/show/nct00377325 (first received 18 September 2006).
NCT00438360 {published data only}
- NCT00438360. Efficacy and safety of cyclosporine A microemulsion in maintenance patients with chronic plaque psoriasis. clinicaltrials.gov/show/nct00438360 (first received 22 February 2007).
NCT00585650 {published data only}
- NCT00585650. Study of tumor necrosis factor receptor fusion protein etanercept (enbrel) in psoriasis of the hands and/or feet. clinicaltrials.gov/show/nct00585650 (first received 3 January 2008).
NCT00645892 {published data only}
- NCT00645892. Extension study of two dosing schedules of adalimumab in subjects with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/nct00645892 (first received 28 March 2008).
NCT00646191 {published data only}
- NCT00646191. Study of the safety and efficacy of adalimumab in subjects with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/nct00646191 (first received 28 March 2008).
NCT00647400 {published data only}
- NCT00647400. Adalimumab in adult Japanese subjects with psoriasis. clinicaltrials.gov/show/nct00647400 (first received 31 March 2008).
NCT00832364 {published data only}
- NCT00832364. Trial of an injectable biologic and U0279 as combination therapy for severe plaque-type psoriasis. clinicaltrials.gov/show/nct00832364 (first received 30 January 2009).
NCT01163253 {published data only}
- NCT01163253. A long term study to evaluate the safety and tolerability of CP-690,550 for patients with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/nct01163253 (first received 15 July 2010).
NCT01235442 {published data only}
- NCT01235442. Evaluate efficacy, and safety of topical therapy and etanercept in subjects with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct01235442 (first received 5 November 2010).
NCT01276847 {published data only}
- NCT01276847. A study to assess the effect of ustekinumab (Stelara®) and etanercept (Enbrel®) in participants with moderate to severe psoriasis (MK-0000-206). clinicaltrials.gov/show/nct01276847 (first received 13 January 2011).
NCT01412944 {published data only}
- NCT01412944. Efficacy and safety of intravenous and subcutaneous secukinumab in moderate to severe chronic plaque-type psoriasis (STATURE). clinicaltrials.gov/show/nct01412944 (first received 9 August 2011).
NCT01443338 {published data only}
- NCT01443338. Study evaluating the efficacy and safety of Triptergium Wilfordii and acitretin in psoriasis vulgaris - CHINA201002016-2. clinicaltrials.gov/show/nct01443338 (first received 29 September 2011).
NCT01544595 {published data only}
- NCT01544595. Extension study of secukinumab prefilled syringes in subjects with moderate to severe chronic plaque-type psoriasis completing preceding psoriasis phase III studies with secukinumab. clinicaltrials.gov/show/nct01544595 (first received 6 March 2012).
NCT01550744 {published data only}
- NCT01550744. A study of ustekinumab to evaluate a "subject-tailored" maintenance dosing approach in subjects with moderate-to-severe plaque psoriasis (PSTELLAR). clinicaltrials.gov/show/nct01550744 (first received 12 March 2012).
NCT01624233 {published data only}
- NCT01624233. A study in Japanese participants with moderate-to-severe psoriasis (UNCOVER-J). clinicaltrials.gov/show/nct01624233 (first received 20 June 2012).
NCT01722214 {published data only}
- NCT01722214. Trial on the effect of adalimumab on vascular inflammation in patients with psoriasis. clinicaltrials.gov/show/nct01722214 (first received 6 November 2012).
NCT01806597 {published data only}
- NCT01806597. Study of safety, tolerability, and efficacy of secukinumab in subjects with moderate to severe palmoplantar psoriasis (GESTURE). clinicaltrials.gov/show/nct01806597 (first received 7 March 2013).
NCT01815723 {published data only}
- NCT01815723. Efficacy study on dimethyl fumarate to treat moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct01815723 (first received 21 March 2013).
NCT01828086 {published data only}
- NCT01828086. Single and multiple dose escalation study to assess the safety and tolerability of CJM112 in psoriasis. clinicaltrials.gov/show/nct01828086 (first received 10 April 2013).
NCT01936688 {published data only}
- EUCTR2013-001740-54-HU. A clinical research study of 28 weeks to test the safety/tolerability and effectiveness of an investigational study medication (subcutaneous SCH 900222/MK-3222) in improving the signs and symptoms of moderate-to-severe chronic plaque psoriasis, and to compare it to an approved medication for the treatment of psoriasis called etanercept. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2013-001740-54-HU (first received 18 September 2013).
- NCT01936688. A study to evaluate the efficacy and safety/tolerability of subcutaneous MK-3222 in participants with moderate-to-severe chronic plaque psoriasis (MK-3222-012). clinicaltrials.gov/show/nct01936688 (first received 6 September 2013).
NCT02362789 {published data only}
- NCT02362789. Secukinumab study in PSOriasis exploring pruRITUS intensity and lesional biomarkers (PSORITUS). clinicaltrials.gov/show/nct02362789 (first received 13 February 2015).
NCT02409667 {published data only}
- NCT02409667. Plaque psoriasis efficacy and safety with secukinumab (OPTIMISE). clinicaltrials.gov/show/nct02409667 (first received 7 April 2015).
NCT02798211 {published data only}
- NCT02798211. Study to evaluate the safety and efficacy of secukinumab 300 mg and 150 mg in adult patients with active psoriatic arthritis (PsA) after 16 weeks of treatment compared to placebo. clinicaltrials.gov/show/nct02798211 (first received 14 June 2016).
NCT03010527 {published data only}
- NCT03010527. Study to evaluate the long-term safety, tolerability and efficacy of bimekizumab in patients with chronic plaque psoriasis. clinicaltrials.gov/show/nct03010527 (first received 5 January 2017).
NCT03020199 {published data only}
- EUCTR2015-002423-26-FI. Study of the efficacy of early intervention with secukinumab 300 mg s.c. compared to narrow-band UVB in patients with new-onset moderate to severe plaque psoriasis. apps.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-002423-26-FI (first received 21 October 2016).
- NCT03020199. Study of the efficacy of early intervention with secukinumab 300 mg s.c. compared to narrow-band UVB in patients with new-onset moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct03020199 (first received 13 January 2017).
NCT03073213 {published data only}
- NCT03073213. A study of ixekizumab in Chinese participants with psoriasis vulgaris. clinicaltrials.gov/show/nct03073213 (first received 8 March 2017).
Nemoto 2018 {published data only}
- Nemoto O, Hirose K, Shibata S, Li K, Kubo H. Safety and efficacy of guselkumab in Japanese patients with moderate-to-severe plaque psoriasis: a randomized, placebo-controlled, ascending-dose study. British Journal of Dermatology 2018;178(3):689-96. [CENTRAL: CN-01449577] [DOI] [PubMed] [Google Scholar]
Nieboer 1990 {published data only}
- Nieboer C, De Hoop D, Langendijk PN, Van Loenen AC, Gubbels J. Fumaric acid therapy in psoriasis: a double-blind comparison between fumaric acid compound therapy and monotherapy with dimethylfumaric acid ester. Dermatologica 1990;181(1):33-7. [CENTRAL: CN-00351435] [DOI] [PubMed] [Google Scholar]
Nijsten 2008 {published data only}
- Nijsten T, Spuls P, Stern RS. STROBE: a Beacon for observational studies. Archives of Dermatology 2008;144(9):1200-4. [PMID: ] [DOI] [PubMed] [Google Scholar]
Noda 2011 {published data only}
- Noda S, Mizuno K, Adachi M. Treatment effect of adalimumab and infliximab in Japanese psoriasis patients: results in a single community-based hospital. Journal of Investigative Dermatology 2011;131(Suppl 2):S38. [EMBASE: 70520994] [DOI] [PubMed] [Google Scholar]
Noor 2017 {published data only}
- Noor SM, Ayub N, Paracha MM. Efficacy and safety of methotrexate versus acitretin in chronic plaque psoriasis. Journal of Postgraduate Medical Institute 2017;31(1):4-7. [CENTRAL: CN-01340758] [Google Scholar]
Novotny 1973 {published data only}
- Novotny F. Use of methotrexate in psoriasis. Ceskoslovenska Dermatologie 1973;48(5):301-5. [PMID: ] [PubMed] [Google Scholar]
Nyfors 1978 {published data only}
- Nyfors A. Benefits and adverse drug experiences during long-term methotrexate treatment of 248 psoriatics. Danish Medical Bulletin 1978;25(5):208-11. [PMID: ] [PubMed] [Google Scholar]
Okubo 2019 {published data only}
- Okubo Y, Ohtsuki M, Morita A, Yamaguchi M, Shima T, Tani Y, et al. Long-term efficacy and safety of secukinumab in Japanese patients with moderate to severe plaque psoriasis: 3-year results of a double-blind extension study. Journal of Dermatology 2019;46(3):186-92. [CENTRAL: CN-01794517] [DOI] [PMC free article] [PubMed] [Google Scholar]
Orfanos 1978 {published data only}
- Orfanos CE, Goerz G. Oral psoriasis treatment with a new aromatic retinoid (Ro 10-9359): a multi-centre controlled study of 291 patients (preliminary results). Deutsche Medizinische Wochenschrift 1978;103(5):195-9. [CENTRAL: CN-00017768] [DOI] [PubMed] [Google Scholar]
Orfanos 1979 {published data only}
- Orfanos CE, Steigleder GK, Pullmann H, Bloch PH. Oral retinoid and UVB radiation: a new, alternative treatment for psoriasis on an out-patient basis. Acta Dermato-Venereologica 1979;59(3):241-4. [CENTRAL: CN-00020394] [PubMed] [Google Scholar]
Ortonne 2008 {published data only}
- Ortonne JP, Griffiths CE, Dauden E, Strohal R, Robertson D, Pedersen R, et al. Efficacy and safety of continuous versus paused etanercept teatment in patients with moderate-to-severe psoriasis over 54 weeks: the CRYSTEL Study. Expert Review of Dermatology 2008;3(6):657-65. [CENTRAL: CN-00754922] [Google Scholar]
Ortonne 2011 {published data only}
- Ortonne JP, Chimenti S, Reich K, Gniadecki R, Sprøgel P, Unnebrink K, et al. Efficacy and safety of adalimumab in patients with psoriasis previously treated with anti-tumour necrosis factor agents: subanalysis of BELIEVE. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25(9):1012-20. [CENTRAL: CN-00812830] [DOI] [PubMed] [Google Scholar]
Osamu 2014 {published data only}
- Osamu N, Hirotaka N, Koji S, Kenji T. Clinical pharmacology of the anti-IL-17 receptor antibody brodalumab (KHK4827) in Japanese normal healthy volunteers and Japanese subjects with moderate to severe psoriasis: a randomized, dose-escalation, placebo-controlled study. Journal of Dermatological Science 2014;75(3):201-4. [CENTRAL: CN-00999213] [DOI] [PubMed] [Google Scholar]
Page 2020 {published data only}
- Page KM, Suarez-Farinas M, Suprun M, Zhang W, Garcet S, Fuentes-Duculan J, et al. Molecular and cellular responses to the TYK2/JAK1 inhibitor PF-06700841 reveal reduction of skin inflammation in plaque psoriasis. Journal of Investigative Dermatology 2020;140(8):1546-55.e4. [DOI] [PubMed] [Google Scholar]
Pakozdi 2018 {published data only}
- Pakozdi T, Georgantas RW, Grebe KM, Visvanathan S, Baum P, Davis W. RNA-seq genomic analysis demonstrated the molecular efficacy of risankizumab in a moderate-to-severe plaque psoriasis phase 2 clinical study. Experimental Dermatology 2018;27(Supplement 2):21. [CENTRAL: CN-01793116] [Google Scholar]
Papp 2001 {published data only}
- Papp K, Bissonnette R, Krueger JG, Carey W, Gratton D, Gulliver WP, et al. The treatment of moderate to severe psoriasis with a new anti-CD11a monoclonal antibody. Journal of the American Academy of Dermatology 2001;45(5):665-74. [CENTRAL: CN-00374574] [DOI] [PubMed] [Google Scholar]
Papp 2006 {published data only}
- Papp K, Langley R, Bissonnette R, Rosoph L. A Phase III, randomized, multicenter, double-blind, placebo-controlled. Journal of the American Academy of Dermatology 2006;54(3 Suppl):AB9. [CENTRAL: CN-00602194] [DOI] [PubMed] [Google Scholar]
Papp 2008 {published data only}
- Papp K, Bissonnette R, Rosoph L, Wasel N, Lynde CW, Searles G, et al. Efficacy of ISA247 in plaque psoriasis: a randomised, multicentre, double-blind, placebo-controlled phase III study. Lancet 2008;371(9521):1337-42. [CENTRAL: CN-00631348] [DOI] [PubMed] [Google Scholar]
Papp 2009 {published data only}
- Papp K, Okun M, Vender R. Adalimumab in the treatment of psoriasis: pooled efficacy and safety results from three pivotal studies. Journal of Cutaneous Medicine and Surgery 2009;13(Suppl 2):S58-66. [PMID: ] [DOI] [PubMed] [Google Scholar]
Papp 2011a {published data only}
- Papp K, Signorovitch J, Mulani P, Bao Y. Comparison of psoriasis sign and symptom reduction and complete clearance with adalimumab versus etanercept. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB153. [CENTRAL: CN-00843873] [Google Scholar]
Papp 2011b {published data only}
- Papp K, Signorovitch J, Sundaram M, Bao Y. Effects of abt-874 treatment on health-related quality of life and work productivity and activity impairment in patients with psoriasis. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB155. [CENTRAL: CN-00843874] [Google Scholar]
Papp 2011c {published data only}
- Papp K, Yu A, Sundaram M, Bao Y. Achieving long-term sustained response is associated with improvements in patient-reported outcomes in patients with psoriasis treated with abt-874. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB160. [CENTRAL: CN-00843875] [Google Scholar]
Papp 2012d {published data only}
- Papp KA, Reid C, Foley P, Sinclair R, Salinger DH, Williams G, et al. Anti-IL-17 receptor antibody AMG 827 leads to rapid clinical response in subjects with moderate to severe psoriasis: results from a phase I, randomized, placebo-controlled trial. Journal of Investigative Dermatology 2012;132(10):2466-9. [CENTRAL: CN-00854479] [DOI] [PubMed] [Google Scholar]
Papp 2012e {published data only}
- Papp KA, Poulin Y, Bissonnette R, Bourcier M, Toth D, Rosoph L, et al. Assessment of the long-term safety and effectiveness of etanercept for the treatment of psoriasis in an adult population. Journal of the American Academy of Dermatology 2012;66(2):e33-45. [CENTRAL: CN-00883092] [DOI] [PubMed] [Google Scholar]
Papp 2017c {published data only}
- Papp K, Bachelez H, Costanzo A, Foley P, Gooderham M, Kaur P, et al. Clinical similarity of the biosimilar ABP 501 compared with adalimumab after single transition: long-term results from a randomized controlled, double-blind, 52-week, phase III trial in patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology 2017;177(6):1562-74. [CENTRAL: CN-01440056] [DOI] [PubMed] [Google Scholar]
Papp 2018a {published data only}
- Papp K, Kimball A, Blauvelt A, Reich K, Gooderham M, Tyring S, et al. Effect of tildrakizumab on personal relationships in patients with moderate-to-severe chronic plaque psoriasis. Acta Dermato-Venereologica 2018;98(Supplement 219):54. [CENTRAL: CN-01620176] [Google Scholar]
Papp 2018b {published data only}
- Papp KA, Blauvelt A, Kimball AB, Han C, Randazzo B, Wasfi Y, et al. Patient-reported symptoms and signs of moderate-to-severe psoriasis treated with guselkumab or adalimumab: results from the randomized VOYAGE 1 trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2018;32(9):1515-22. [CENTRAL: CN-01665289] [DOI: 10.1111/jdv.14910] [DOI] [PMC free article] [PubMed] [Google Scholar]
Park 2013 {published data only}
- Park KK, Wu JJ, Koo J. A randomized, 'head-to-head' pilot study comparing the effects of etanercept monotherapy vs. etanercept and narrowband ultraviolet B (NB-UVB) phototherapy in obese psoriasis patients. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(7):899-906. [CENTRAL: CN-00969013] [DOI] [PubMed] [Google Scholar]
Paul 2012 {published data only}
- Paul C, Van de Kerkhof P, Puig L, Unnebrink K, Goldblum O, Thaçi D. Influence of psoriatic arthritis on the efficacy of adalimumab and on the treatment response of other markers of psoriasis burden: subanalysis of the BELIEVE study. European Journal of Dermatology 2012;22(6):762-9. [CENTRAL: CN-00966715] [DOI] [PubMed] [Google Scholar]
Paul 2014 {published data only}
- Paul C, Puig L, Kragballe K, Luger T, Lambert J, Chimenti S, et al. Transition to ustekinumab in patients with moderate-to-severe psoriasis and inadequate response to methotrexate: A randomized clinical trial (TRANSIT). British Journal of Dermatology 2014;170(2):425-34. [CENTRAL: CN-00982375] [DOI] [PubMed] [Google Scholar]
Paul 2018 {published data only}
- Paul C, Guenther L, Torii H, Sofen H, Burge R, Lin CY, et al. Impact of ixekizumab on facial psoriasis and related quality of life measures in moderate-to-severe psoriasis patients: 12-week results from two phase III trials. Journal of the European Academy of Dermatology and Venereology : JEADV 2018;32(1):68-72. [CENTRAL: CN-01449415] [DOI: 10.1111/jdv.14581] [DOI] [PubMed] [Google Scholar]
Perks 2017 {published data only}
- Perks B. Randomized non-inferiority trial fails to find inferiority switching from infliximab originator to CT-P13 biosimilar. GaBI Journal 2017;6(4):188-9. [DOI: 10.5639/gabij.2017.0604.042] [DOI] [Google Scholar]
Pettit 1979 {published data only}
- Pettit JH. Oral retinoid for psoriasis. A report of a double blind study. Acta Dermato-Venereologica. Supplementum 1979;59(85):133-6. [CENTRAL: CN-00021931] [MEDLINE: ] [PubMed] [Google Scholar]
Petzelbauer 1990 {published data only}
- Petzelbauer P, Honigsmann H, Langer K, Anegg B, Strohal R, Tanew A, et al. Cyclosporin A in combination with photochemotherapy (PUVA) in the treatment of psoriasis. British Journal of Dermatology 1990;123(5):641-7. [CENTRAL: CN-00351600] [DOI] [PubMed] [Google Scholar]
Piascik 2003 {published data only}
- Piascik P. Alefacept, first biologic agent approved for treatment of psoriasis. Journal of the American Pharmacists Association 2003;43(5):649-50. [PMID: ] [DOI] [PubMed] [Google Scholar]
Ports 2013 {published data only}
- Ports WC, Khan S, Lan S, Lamba M, Bolduc C, Bissonnette R, et al. A randomized phase 2a efficacy and safety trial of the topical Janus kinase inhibitor tofacitinib in the treatment of chronic plaque psoriasis. British Journal of Dermatology 2013;169(1):137-45. [CENTRAL: CN-00920320] [DOI] [PMC free article] [PubMed] [Google Scholar]
Puig 2018 {published data only}
- Puig L, Augustin M, Blauvelt A, Gottlieb AB, Vender R, Korman NJ, et al. Effect of secukinumab on quality of life and psoriasis-related symptoms: A comparative analysis versus ustekinumab from the CLEAR 52-week study. Journal of the American Academy of Dermatology 2018;78(4):741-8. [CENTRAL: CN-01463902] [DOI] [PubMed] [Google Scholar]
Punwani 2012 {published data only}
- Punwani N, Scherle P, Flores R, Shi J, Liang J, Yeleswaram S, et al. Preliminary clinical activity of a topical JAK1/2 inhibitor in the treatment of psoriasis. Journal of the American Academy of Dermatology 2012;67(4):658-64. [CENTRAL: CN-00881387] [DOI] [PubMed] [Google Scholar]
Rabasseda 2012 {published data only}
- Rabasseda X. A report from the American Academy of Dermatology 70th Annual Meeting (March 16-20, 2012 - San Diego, California, USA). Drugs of Today 2012;48(5):367-73. [PMID: ] [DOI] [PubMed] [Google Scholar]
Radmanesh 2011 {published data only}
- Radmanesh M, Rafiei B, Moosavi ZB, Sina N. Weekly vs. daily administration of oral methotrexate (MTX) for generalized plaque psoriasis: a randomized controlled clinical trial. International Journal of Dermatology 2011;50(10):1291-3. [CENTRAL: CN-00805615] [DOI] [PubMed] [Google Scholar]
Raman 1998 {published data only}
- Raman GV, Campbell SK, Farrer A, Albano JD, Cook J. Modifying effects of amlodipine on cyclosporin A-induced changes in renal function in patients with psoriasis. Journal of Hypertension. Supplement 1998;16(4):S39-41. [CENTRAL: CN-00308573] [PubMed] [Google Scholar]
Reich 2004 {published data only}
- Reich K. Alefacept in the treatment of psoriasis for whom conventional therapies are ineffective or inappropriate. Journal of the European Academy of Dermatology and Venereology : JEADV 2004;18(6):808. [CENTRAL: CN-00550795] [Google Scholar]
- Sclessinger J, Pariser R, Park S, Wierz G. Evaluation of the efficacy and safety of alefacept in patients for whom conventional psoriasis therapies are ineffective or inappropriate. Journal of the American Academy of Dermatology 2007;56(2):AB192. [CENTRAL: CN-00616055] [Google Scholar]
Reich 2011 {published data only}
- Reich K, Van Hoogstraten BJ, Wozel G, Zheng H, Flint L. Long-term efficacy and safety of maintenance versus intermittent infliximab therapy for moderate to severe plaque-type psoriasis: the restore2 trial. Journal of the American Academy of Dermatology 2011;64(2 Suppl 1):AB150. [CENTRAL: CN-00843879] [Google Scholar]
Reich 2014 {published data only}
- Reich K, Puig L, Paul C, Kragballe K, Luger T, Lambert J, et al. One-year safety and efficacy of ustekinumab and results of dose adjustment after switching from inadequate methotrexate treatment: the TRANSIT randomized trial in moderate-to-severe plaque psoriasis. British Journal of Dermatology 2014;170(2):435-44. [CENTRAL: CN-00982376] [DOI] [PubMed] [Google Scholar]
Reich 2016a {published data only}
- Reich K, Soung J, Gooderham M, Zhang Z, Nograles K, Goodfield M. LIBERATE trial: sustained efficacy of apremilast in patients with moderate-to-severe psoriasis who continued on apremilast or switched from etanercept treatment. British Journal of Dermatology 2016;175(S1):71-2. [CENTRAL: CN-01303307] [DOI: 10.1111/bjd.14524] [DOI] [Google Scholar]
Reich 2016b {published data only}
- Reich K, Choi SL, Jackson K, Mallbris L, Blauvelt A. Time course of ixekizumab drug levels and the relationship at week 60 to efficacy in patients with moderate-to- severe plaque psoriasis (UNCOVER-3). Experimental Dermatology 2016;25(S4):39. [CENTRAL: CN-01407586] [Google Scholar]
Reich 2017a {published data only}
- Reich K, Goodfield M, Green L, Nograles K, Chen R, Levi E, et al. Efficacy and safety of apremilast through 104 weeks in subjects with moderate to severe psoriasis randomized to placebo, apremilast, or etanercept who continued on or switched to apremilast after week 16 in a phase 3B study. Arthritis and Rheumatology 2017;69(Supplement 10):627. [Google Scholar]
Reich 2017b {published data only}
- Reich K, Armstrong AW, Foley P, Song M, Wasfi Y, Randazzo B, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the treatment of patients with moderate to severe psoriasis with randomized withdrawal and retreatment: Results from the phase III, double-blind, placebo- and active comparator-controlled VOYAGE 2 trial. Journal of the American Academy of Dermatology 2017;76(3):418-31. [CENTRAL: CN-01341399] [DOI] [PubMed] [Google Scholar]
Reich 2017c {published data only}
- Reich K, Papp K, Armstrong AW, Wasfi Y, Jiang G, Shen YK, et al. Safety of guselkumab in patients with plaque psoriasis through 2 years: a pooled analysis from VOYAGE 1 and VOYAGE 2. British Journal of Dermatology 2017;177(5):e297. [DOI: 10.1111/bjd.16059] [DOI] [PubMed] [Google Scholar]
Reich 2018a {published data only}
- Reich K, Sullivan J, Arenberger P, Mrowietz U, Jazayeri S, Augustin M, et al. Effect of secukinumab on the clinical activity and disease burden of nail psoriasis: 32-week results from the randomized placebo-controlled TRANSFIGURE trial. British Journal of Dermatology 2018 Oct 26 [Epub ahead of print]. [DOI: 10.1111/bjd.17351] [DOI] [PubMed]
Reich 2018b {published data only}
- Reich K, Jackson K, Ball S, Garces S, Kerr L, Chua L, et al. Ixekizumab pharmacokinetics, anti-drug antibodies, and efficacy through 60 weeks of treatment of moderate to severe plaque psoriasis. Journal of Investigative Dermatology 2018;138(10):2168-73. [CENTRAL: CN-01611449] [DOI] [PubMed] [Google Scholar]
Reich 2018c {published data only}
- Reich K, Gooderham M, Thaçi D, Crowley JJ, Ryan C, Krueger JG, et al. Efficacy and safety of risankizumab (RZB) compared with adalimumab (ADA) in patients with moderate-to-severe plaque psoriasis: Results from the phase 3 IMMvent trial. Experimental Dermatology 2018;27(Supplement 2):9-10. [CENTRAL: CN-01790123] [Google Scholar]
Reitamo 1999 {published data only}
- Reitamo S, Spuls P, Sassolas B, Lahfa M, Claudy A, Griffiths C, et al. A double-blind study in patients with severe psoriasis to assess the clinical activity and safety of Rapamycin (sirolimus) alone or in association with a reduced dose of cyclosporine. British Journal of Dermatology 1999;141(5):978-9. [CENTRAL: CN-00428747] [Google Scholar]
Reitamo 2001 {published data only}
- Reitamo S, Spuls P, Sassolas B, Lahfa M, Claudy A, Griffiths CE, et al. Efficacy of sirolimus (rapamycin) administered concomitantly with a subtherapeutic dose of cyclosporin in the treatment of severe psoriasis: a randomized controlled trial. British Journal of Dermatology 2001;145(3):438-45. [CENTRAL: CN-00356242] [DOI] [PubMed] [Google Scholar]
Rim 2003 {published data only}
- Rim JH, Park JY, Choe YB, Youn JI. The efficacy of calcipotriol + acitretin combination therapy for psoriasis: comparison with acitretin monotherapy. American Journal of Clinical Dermatology 2003;4(7):507-10. [CENTRAL: CN-00450180] [DOI] [PubMed] [Google Scholar]
Rinsho Iyaku 1991 {published data only}
- Clinical Study Group for Ciclosporin. Clinical efficacy of ciclosporin in the treatment of psoriasis: multicenter double blind study. Rincho Iyaku (Journal of Clinical Therapeutics and Medicines) 1991;7(3):617-33. [CENTRAL: CN-00545330] [Google Scholar]
Ritchlin 2006a {published data only}
- Ritchlin CT. The efficacy and safety of adalimumab in psoriatic arthritis. Current Rheumatology Reports 2006;8(5):329. [CENTRAL: CN-00898612] [DOI] [PubMed] [Google Scholar]
Ritchlin 2006b {published data only}
- Ritchlin CT. The efficacy and safety of alefacept in psoriatic arthritis. Current Rheumatology Reports 2006;8(5):330-1. [CENTRAL: CN-00898611] [DOI] [PubMed] [Google Scholar]
Romiti 2017 {published data only}
- Romiti R, Papadimitropoulos M, Lin C, Burge RT, Zhu B, Garcia EG. Ixekizumab treatment improves itching and health-related quality (HRQOL) of life in psoriasis patients in Latin America. Value in Health 2017;20(9):A807. [CENTRAL: CN-01431329] [Google Scholar]
RPCEC00000201 {unpublished data only}
- RPCEC00000201. Itolizumab for moderate-to-severe psoriasis-phase 3 [Randomized controlled double blind trial to study safety and efficacy of itolizumab (antiCD6) in moderate-to-severe psoriasis]. registroclinico.sld.cu/trials/RPCEC00000201-En (first received 15 October 2015). [CENTRAL: CN-01835365]
Ryan 2018 {published data only}
- Ryan C, Menter A, Guenther L, Blauvelt A, Bissonnette R, Meeuwis K, et al. Efficacy and safety of ixekizumab in a randomized, double-blinded, placebo-controlled phase IIIb study of patients with moderate-to-severe genital psoriasis. British Journal of Dermatology 2018;179(4):844-52. [CENTRAL: CN-01630323] [DOI] [PubMed] [Google Scholar]
Saeki 2017 {published data only}
- Saeki H, Nakagawa H, Nakajo K, Ishii T, Morisaki Y, Aoki T, et al. Efficacy and safety of ixekizumab treatment for Japanese patients with moderate to severe plaque psoriasis, erythrodermic psoriasis and generalized pustular psoriasis: results from a 52-week, open-label, phase 3 study (UNCOVER-J). Journal of Dermatology 2017;44(4):355-62. [DOI: 10.1111/1346-8138.13622] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Salim 2006 {published data only}
- Salim A, Tan E, Ilchyshyn A, Berth-Jones J. Folic acid supplementation during treatment of psoriasis with methotrexate: a randomized, double-blind, placebo-controlled trial. British Journal of Dermatology 2006;154(6):1169-74. [CENTRAL: CN-00565411] [DOI] [PubMed] [Google Scholar]
Scholl 1981 {published data only}
- Scholl E. Treatment of psoriasis on an outpatient-base using UVB-radiations, oral retinoid and ten percent saline baths. Schweizerische Rundschau für Medizin Praxis 1981;70(41):1806-16. [CENTRAL: CN-00026632] [PubMed] [Google Scholar]
Schopf 1998 {published data only}
- Schopf RE, Hultsch T, Lotz J, Brautigam M. Eosinophils, pruritus and psoriasis: effects of treatment with etretinate or cyclosporin-A. Journal of the European Academy of Dermatology and Venereology : JEADV 1998;11(3):234-9. [CENTRAL: CN-00158727] [PMID: ] [PubMed] [Google Scholar]
Schulze 1991 {published data only}
- Schulze HJ. Comparative trial of Sandimmune and etretinate for plaque-type psoriasis. Zeitschrift fur Hautkrankheiten 1991;66(Suppl 1):33-8. [CENTRAL: CN-00180765] [Google Scholar]
Shintani 2011 {published data only}
- Shintani Y, Kaneko N, Furuhashi T, Saito C, Morita A. Safety and efficacy of a fixed-dose cyclosporin microemulsion (100 mg) for the treatment of psoriasis. Journal of Dermatology 2011;38(10):966-72. [CENTRAL: CN-00811861] [DOI] [PubMed] [Google Scholar]
Shiohara 1992 {published data only}
- Shiohara T, Imanishi K, Sagawa Y, Nagashima M. Differential effects of cyclosporine and etretinate on serum cytokine levels in patients with psoriasis. Journal of the American Academy of Dermatology 1992;27(4):568-74. [CENTRAL: CN-00361111] [DOI] [PubMed] [Google Scholar]
Shupack 1997 {published data only}
- Shupack J, Abel E, Bauer E, Brown M, Drake L, Freinkel R, et al. Cyclosporine as maintenance therapy in patients with severe psoriasis. Journal of the American Academy of Dermatology 1997;36(3 pt 1):423-32. [CENTRAL: CN-00137758] [DOI] [PubMed] [Google Scholar]
Simonova 2005 {published data only}
- Simonova OV, Nemtsov BF. Psoriatic arthritis: combined treatment with prospidin and methotrexate. Terapevticheskii Arkhiv 2005;77(8):60-4. [CENTRAL: CN-00530903] [PubMed] [Google Scholar]
Sinclair 2017 {published data only}
- Sinclair R, Reich K, Papp K, Tyring SS, Thaçi D, Cichanowitz N, et al. Tildrakizumab, a selective IL-23p19 antibody, in the treatment of chronic plaque psoriasis: results from two randomised, controlled, phase 3 trials. Australasian Journal of Dermatology 2017;58(S1):9-10. [CENTRAL: CN-01378810] [DOI: 10.1111/ajd.12652] [DOI] [Google Scholar]
Sofen 2011 {published data only}
- Sofen H, Smith S, Matheson R, Leonardi C, Calderon C, Bouman-Thio E, et al. Results of a single ascending dose study to assess the safety and tolerability of CNTO 1959 following intravenous or subcutaneous administration in healthy subjects and in subjects with moderate to severe psoriasis. British Journal of Dermatology 2011;165(6):e10. [CENTRAL: CN-01020427] [Google Scholar]
Sofen 2014 {published data only}
- Sofen H, Smith S, Matheson RT, Leonardi CL, Calderon C, Brodmerkel C, et al. Guselkumab (an IL-23-specific mAb) demonstrates clinical and molecular response in patients with moderate-to-severe psoriasis. Journal of Allergy and Clinical Immunology 2014;133(4):1032-40. [CENTRAL: CN-00984656] [DOI] [PubMed] [Google Scholar]
Spadaro 2008 {published data only}
- Spadaro A, Ceccarelli F, Scrivo R, Valesini G. Life-table analysis of etanercept with or without methotrexate in patients with psoriatic arthritis. Annals of the Rheumatic Diseases 2008;67(11):1650-1. [CENTRAL: CN-00651403] [DOI] [PubMed] [Google Scholar]
Spuls 2012 {published data only}
- Spuls PI, Hooft L. Brodalumab and ixekizumab, anti-interleukin-17-receptor antibodies for psoriasis: a critical appraisal. British Journal of Dermatology 2012;167(4):710-3; discussion 714-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stein Gold 2018 {published data only}
- Stein Gold L, Bagel J, Lebwohl M, Jackson JM, Chen R, Goncalves J, et al. Efficacy and safety of apremilast in systemic- and biologic-naive patients with moderate plaque psoriasis: 52-week results of UNVEIL. Journal of Drugs in Dermatology: JDD 2018;17(2):221-8. [CENTRAL: CN-01627309] [PubMed] [Google Scholar]
Sticherling 1994 {published data only}
- Sticherling M. Symposium report: "Therapy of severe psoriasis with Sandimmune". Symposium of Nurnberg Sandoz AG 13 February 1993, Nurnberg. Hautarzt 1994;45(1):50-2. [PMID: ] [PubMed] [Google Scholar]
Strober 2004 {published data only}
- Strober BE, Clarke S. Etanercept for the treatment of psoriasis: combination therapy with other modalities. Journal of Drugs in Dermatology 2004;3(3):270-2. [PMID: ] [PubMed] [Google Scholar]
Strober 2012 {published data only}
- Strober BE, Sobell JM, Duffin KC, Bao Y, Guerin A, Yang H, et al. Sleep quality and other patient-reported outcomes improve after patients with psoriasis with suboptimal response to other systemic therapies are switched to adalimumab: results from PROGRESS, an open-label Phase IIIB trial. British Journal of Dermatology 2012;167(6):1374-81. [PMID: ] [DOI] [PubMed] [Google Scholar]
Strober 2017a {published data only}
- Strober B, Gottlieb AB, Sherif B, Mollon P, Gilloteau I, McLeod L, et al. Secukinumab sustains early patient-reported outcome benefits through 1 year: Results from 2 phase III randomized placebo-controlled clinical trials comparing secukinumab with etanercept. Journal of the American Academy of Dermatology 2017;76(4):655-61. [CENTRAL: CN-01368337] [DOI: 10.1016/j.jaad.2016.11.043] [DOI] [PubMed] [Google Scholar]
Strober 2017b {published data only}
- Strober B, Bagel J, Lebwohl M, Stein Gold L, Jackson JM, Chen R, et al. Efficacy and safety of apremilast in patients with moderate plaque psoriasis with lower BSA: week 16 results from the UNVEIL study. Journal of Drugs in Dermatology: JDD 2017;16(8):801-8. [CENTRAL: CN-01416087] [PubMed] [Google Scholar]
Strober 2017c {published data only}
- Strober B, Alikhan M, Lockshin B, Schafer P. Cytokine effects of apremilast as a mechanism of efficacy in systemic-naive patients with moderate plaque psoriasis: results from the UNVEIL trial. British Journal of Dermatology 2017;177(5):e256-7. [CENTRAL: CN-01452501] [DOI: 10.1111/bjd.16059] [DOI] [PubMed] [Google Scholar]
Strober 2018 {published data only}
- Strober B, Forman S, Bagel J, Lebwohl M, Stein Gold L, Jackson JM, et al. Efficacy and safety of apremilast in systemic- and biologic-naive patients with moderate plaque psoriasis (52-week results of the UNVEIL study). Journal of Clinical and Aesthetic Dermatology 2018;11(5 Supplement 1):S21-2. [CENTRAL: CN-01713688] [PubMed] [Google Scholar]
Sun 2019 {published data only}
- Sun J, Chen G, Wu M, Han Y, Gao H, Zhang T, et al. China-manufactured adalimumab biosimilar, HLX03, demonstrated pharmacokinetic equivalence and comparable safety to adalimumab. Annals of the Rheumatic Diseases 2019;78 Suppl 2:706. [Google Scholar]
Sweetser 2006 {published data only}
- Sweetser M, Ticho B, Swan S. Subcutaneous administration of alefacept is bioequivalent to intramuscular administration: Results of a randomized, open-label, crossover study in healthy volunteers. Journal of the American Academy of Dermatology 2006;54(3 Suppl):AB224. [CENTRAL: CN-00602513] [PubMed] [Google Scholar]
Syversen 2020 {published data only}
- Syversen SW, Goll GL, Jorgensen KK, Olsen IC, Sandanger O, Gehin JE, et al. Therapeutic drug monitoring of infliximab compared to standard clinical treatment with infliximab: study protocol for a randomised, controlled, open, parallel-group, phase IV study (the NOR-DRUM study). Trials 2020;21(1):13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Talwar 1992 {published data only}
- Talwar S. Methotrexate-puvasol combination in treatment of psoriasis. Indian Journal of Dermatology, Venereology and Leprology 1992;58(1):15-9. [CENTRAL: CN-00663131] [Google Scholar]
TCTR20190705002 {published data only}
- TCTR20190705002. Comparison of the clinical efficacy of subcutaneous versus oral administration of methotrexate in patients with psoriasis vulgaris. www.who.int/trialsearch/Trial2.aspx?TrialID=TCTR20190705002 (first received 4 July 2019).
Tejasvi 2012 {published data only}
- Tejasvi T, Chow C, Simpson MJ, Ellis CN. Use of clinical trial data to compare psoriasis area and severity index, static physician's global assessment, and lattice system-physician's global assessment in assessing severity of psoriasis. Dermatology and Therapy 2012;2:S55. [CENTRAL: 71025691] [Google Scholar]
Thaçi 2002 {published data only}
- Thaçi D, Bräutigam M, Kaufmann R, Weidinger G, Paul C, Christophers E. Body-weight-independent dosing of cyclosporine micro-emulsion and three times weekly maintenance regimen in severe psoriasis. A randomised study. Dermatology (Basel, Switzerland) 2002;205(4):383-8. [CENTRAL: CN-00411587] [DOI] [PubMed] [Google Scholar]
Thaçi 2010 {published data only}
- Thaçi D, Ortonne JP, Chimenti S, Ghislain PD, Arenberger P, Kragballe K, et al. A phase IIIb, multicentre, randomized, double-blind, vehicle-controlled study of the efficacy and safety of adalimumab with and without calcipotriol/betamethasone topical treatment in patients with moderate to severe psoriasis: the BELIEVE study. British Journal of Dermatology 2010;163(2):402-11. [CENTRAL: CN-00771848] [DOI] [PubMed] [Google Scholar]
Thaçi 2018 {published data only}
- Thaçi D, Gottlieb AB, Reich K, Bagel J, Peterson L, Purcaru O, et al. Certolizumab pegol improves patient-reported outcomes in chronic plaque psoriasis over 1 year. Acta Dermato-Venereologica 2018;98(Supplement 219):57-8. [CENTRAL: CN-01620168] [DOI: 10.2340/00015555-2978] [DOI] [Google Scholar]
Tong 2008 {published data only}
- Tong PZ, Si RL. Effectiveness observation on acitretin capsule for plaque psoriasis. Modern Journal of Integrated Traditional Chinese and Western Medicine [xian Dai Zhong Xi Yi Jie He za Zhi] 2008;17(3):364-5. [CENTRAL: CN-00792764] [Google Scholar]
Tsakok 2018 {published data only}
- Tsakok T, Jabbar-Lopez ZK, Smith CH. Subcutaneous methotrexate in patients with moderate-to-severe psoriasis: a critical appraisal. British Journal of Dermatology 2018;179(1):50-3. [CENTRAL: CN-01742390] [DOI] [PubMed] [Google Scholar]
Vaclavkova 2014 {published data only}
- Chimenti S, Arenberger P, Karpati S, Sator PG, Vaclavkova A, Burcklen M, et al. A phase II study of ponesimod, an oral, selective sphingosine 1-phosphate receptor-1 modulator, in chronic plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(Suppl 4):22. [CENTRAL: CN-01025267] [PMID: 23822555]23822555 [Google Scholar]
- Kemeny L, Yankova R, Talamonti M, Vaclavkova A, Burcklen M, Thomas G, et al. A phase II study of ponesimod in chronic plaque psoriasis: improvements in patient-reported outcomes. Journal of the European Academy of Dermatology and Venereology : JEADV 2013;27(Suppl 4):21. [CENTRAL: CN-01025268] [PMID: 23822555]23822555 [Google Scholar]
- Vaclavkova A, Chimenti S, Arenberger P, Hollo P, Sator PG, Burcklen M, et al. Oral ponesimod in patients with chronic plaque psoriasis: a randomised, double-blind, placebo-controlled phase 2 trial. Lancet 2014;384(9959):2036-45. [CENTRAL: CN-01040467] [PMID: ] [DOI] [PubMed] [Google Scholar]
Valenzuela 2017 {published data only}
- Valenzuela F, De la Cruz Fernandez C, Galimberti RL, Gurbuz S, McKean-Matthews M, Goncalves L, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis: Subgroup analysis of Latin American patients in the phase 3 randomized UNCOVER-3 study. Actas Dermo-Sifiliograficas 2017;108(6):550-63. [CENTRAL: CN-01464996] [DOI] [PubMed] [Google Scholar]
Van de Kerkhof 2017 {published data only}
- Van de Kerkhof P, Guenther L, Gottlieb AB, Sebastian M, Wu JJ, Foley P, et al. Ixekizumab treatment improves fingernail psoriasis in patients with moderate-to-severe psoriasis: results from the randomized, controlled and open-label phases of UNCOVER-3. Journal of the European Academy of Dermatology and Venereology : JEADV 2017;31(3):477-82. [CENTRAL: CN-01413633] [DOI: 10.1111/jdv.14033] [DOI] [PubMed] [Google Scholar]
Van Joost 1988 {published data only}
- Van Joost T, Bos JD, Heule F, Meinardi MM. Low-dose cyclosporin A in severe psorasis. A double-blind study. British Journal of Dermatology 1988;118(2):183-90. [CENTRAL: CN-00052789] [PMID: ] [DOI] [PubMed] [Google Scholar]
Vena 2005 {published data only}
- Vena GA, Cassano N, Galluccio A, Loconsole F, Coviello C, Fai D, et al. Evaluation of the efficacy and tolerability of a new intermittent treatment regimen with cyclosporin A in severe psoriasis. Giornale Italiano di Dermatologia e Venereologia 2005;140(5):575-82. [EMBASE: 2006301575] [Google Scholar]
Vena 2012 {published data only}
- Vena GA, Galluccio A, Pezza M, Vestita M, Cassano N. Combined treatment with low-dose cyclosporine and calcipotriol/betamethasone dipropionate ointment for moderate-to-severe plaque psoriasis: a randomized controlled open-label study. Journal of Dermatological Treatment 2012;23(4):255-60. [CENTRAL: CN-00882673] [DOI] [PubMed] [Google Scholar]
Viglioglia 1978 {published data only}
- Viglioglia PA, Barclay A. Oral retinoids and psoriasis. Dermatologica 1978;157(Suppl 1):32-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Witkamp 1995 {published data only}
- Witkamp L, Zonneveld IM, Jung EG, Schopf RE, Christophers E, Grossman R, et al. Efficacy and tolerability of multiple-dose SDZ IMM 125 in patients with severe psoriasis. British Journal of Dermatology 1995;133(1):95-103. [CENTRAL: CN-00118050] [DOI] [PubMed] [Google Scholar]
Wolf 2012 {published data only}
- Wolf P, Weger W, Legat FJ, Posch-Fabian T, Gruber-Wackernagel A, Inzinger M, et al. Treatment with 311-nm ultraviolet B enhanced response of psoriatic lesions in ustekinumab-treated patients: a randomized intraindividual trial. British Journal of Dermatology 2012;166(1):147-53. [CENTRAL: CN-00841290] [DOI] [PubMed] [Google Scholar]
Wright 1966 {published data only}
- Wright ET, Wolborsky M, Hamer EE. Human low-dosage parenteral methotrexate therapy. A controlled toxicity study. Archives of Dermatology 1966;93(6):731-6. [PMID: ] [PubMed] [Google Scholar]
Wu 2015 {published data only}
- Wu C, Jin HZ, Shu D, Li F, He CX, Qiao J, et al. Efficacy and safety of Tripterygium wilfordii Hook F versus acitretin in moderate to severe psoriasis vulgaris: a randomized clinical trial. Chinese Medical Journal 2015;128(4):443-9. [CENTRAL: CN-01047537] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yan 2011 {published data only}
- Yan H, Tang M, You Y, Yu JB, Zhang JA, Li XH, et al. Treatment of psoriasis with recombinant human LFA3-antibody fusion protein: a multi-center, randomized, double-blind trial in a Chinese population. European Journal of Dermatology 2011;21(5):737-43. [CENTRAL: CN-00810848] [PMID: ] [DOI] [PubMed] [Google Scholar]
Yesudian 2013 {published data only}
- Yesudian PD, Hashim N, Bharati A, Alkali A, Warren RB, Cox T, et al. A prospective, double-blind, randomized controlled trial of folic acid supplementation vs. placebo in patients with chronic plaque psoriasis treated with methotrexate and effects on serum homocysteine. British Journal of Dermatology 2013;169(Suppl 1):59. [CENTRAL: CN-00873113] [Google Scholar]
Yoon 2007 {published data only}
- Yoon HS, Youn JI. A comparison of two cyclosporine dosage regimens for the treatment of severe psoriasis. Journal of Dermatological Treatment 2007;18(5):286-90. [CENTRAL: CN-00619337] [DOI] [PubMed] [Google Scholar]
Yosipovitch 2018 {published data only}
- Yosipovitch G, Foley P, Ryan C, Cather JC, Meeuwis KA, Burge R, et al. Ixekizumab improved patient-reported genital psoriasis symptoms and impact of symptoms on sexual activity vs placebo in a randomized, double-blind study. Journal of Sexual Medicine 2018;15(11):1645-52. [CENTRAL: CN-01667932] [DOI] [PubMed] [Google Scholar]
Zachariae 2008 {published data only}
- Zachariae C, Mork NJ, Reunala T, Lorentzen H, Falk E, Karvonen SL, et al. The combination of etanercept and methotrexate increases the effectiveness of treatment in active psoriasis despite inadequate effect of methotrexate therapy. Acta Dermato-Venereologica 2008;88(5):495-501. [CENTRAL: CN-00669633] [DOI] [PubMed] [Google Scholar]
Zhang 2007 {published data only}
- Zhang M, Zhang Y-Z, Wang S. The effect of acitretin on moderate to severe plaque psoriasis. Journal of Clinical Dermatology 2007;36(9):592-3. [CENTRAL: CN-00642111] [Google Scholar]
Zhang 2009a {published data only}
- Zhang GL, Huang F, Zhang JL, Li XF. A clinical study of leflunomide and methotrexate therapy in psoriatic arthritis. Chung-Hua Nei Ko Tsa Chih (Chinese Journal of Internal Medicine) 2009;48(7):570-4. [CENTRAL: CN-00732533] [PubMed] [Google Scholar]
Zhang 2009b {published data only}
- Zhang LX, Bai YP, Song PH, You LP, Yang DQ. Effect of Chinese herbal medicine combined with acitretin capsule in treating psoriasis of blood-heat syndrome type. Chinese Journal of Integrative Medicine 2009;15(2):141-4. [CENTRAL: CN-00700202] [DOI] [PubMed] [Google Scholar]
Zhu 2009 {published data only}
- Zhu Y, Hu C, Lu M, Liao S, Marini JC, Yohrling J, et al. Population pharmacokinetic modeling of ustekinumab, a human monoclonal antibody targeting IL-12/23p40, in patients with moderate to severe plaque psoriasis. Journal of Clinical Pharmacology 2009;49(2):162-75. [PMID: ] [DOI] [PubMed] [Google Scholar]
Zhuang 2016 {published data only}
- Zhuang Y, Calderon C, Marciniak SJ Jr, Bouman-Thio E, Wasfi Y, Szapary P, et al. First-in-human study to assess guselkumab (anti-IL-23 mAb) pharmacokinetics/safety in healthy subjects and patients with moderate-to-severe psoriasis. European Journal of Clinical Pharmacology 2016;72(11):1303-10. [CENTRAL: CN-01307156] [DOI] [PubMed] [Google Scholar]
Zobel 1987 {published data only}
- Zobel AF. Cyclosporin is being tested for treatment of psoriasis. American Druggist 1987;195(3):102. [EMBASE: 1987106040] [Google Scholar]
References to studies awaiting assessment
Chow 2015 {published data only}
- Chow C, Simpson MJ, Luger TA, Chubb H, Ellis CN. Comparison of three methods for measuring psoriasis severity in clinical studies (Part 1 of 2): Change during therapy in Psoriasis Area and Severity Index, Static Physician's Global Assessment and Lattice System Physician's Global Assessment. Journal of the European Academy of Dermatology and Venereology : JEADV 2015;29(7):1406-14. [PMID: ] [DOI] [PubMed] [Google Scholar]
- Chow C, Simpson MJ, Zang Z, Goldfarb MT, Tejasvi T, Ellis CN. Longitudinal effects of active therapy in a clinical trial on Psoriasis Area and Severity Index, Static Physician's Global assessment and Lattice System- Physician's Global assessment for assessing severity of psoriasis. British Journal of Dermatology 2011;165(6):e30. [EMBASE: 70610815] [Google Scholar]
- Simpson MJ, Chow C, Morgenstern H, Luger TA, Ellis CN. Comparison of three methods for measuring psoriasis severity in clinical studies (Part 2 of 2): use of quality of life to assess construct validity of the Lattice System Physician's Global Assessment, Psoriasis Area and Severity Index and Static Physician's Global Assessment. Journal of the European Academy of Dermatology and Venereology : JEADV 2015;29(7):1415-20. [PMID: ] [DOI] [PubMed] [Google Scholar]
CTRI/2015/05/005830 {unpublished data only}
- CTRI/2015/05/005830. Role of oral methotrexate, cyclosporine and acitretin in treatment of palmoplantar psoriasis (redcoloured, painful, itchy, fissured lesions on hands and feet) and psoriasis vulgaris (red coloured,scaly, itchy, elevated lesions on skin over body). ctri.nic.in/Clinicaltrials/pdf_generate.php?trialid=10246 (first received 29 May 2015).
CTRI/2017/09/009850 {published data only}
- CTRI/2017/09/009850. Comparison of ixekizumab with adalimumab in patients with psoriatic arthritis. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2017/09/009850 (first received 19 September 2017).
- Mease PJ, Smolen JS, Behrens F, Nash P, Leage SL, Lingnan L, et al. Multicentre, randomised, open-label, assessor-blinded, parallel-group head-to-head comparison of the efficacy and safety of ixekizumab versus adalimumab in patients with psoriatic arthritis naive to biologic disease-modifying anti-rheumatic drugs: 24-week results. Annals of the Rheumatic Diseases 2019;78 Suppl 2:261-2. [Google Scholar]
- Mease PJ, Smolen JS, Behrens F, Nash P, Liu Leage S, Li L, et al. A head-to-head comparison of the efficacy and safety of ixekizumab and adalimumab in biological-naive patients with active psoriatic arthritis: 24-week results of a randomised, open-label, blinded-assessor trial. Annals of the Rheumatic Diseases 2019;28:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mease PJ, Smolen JS, Behrens F, Nash P, Liu Leage S, Li L, et al. A head-to-head comparison of the efficacy and safety of ixekizumab and adalimumab in biological-naive patients with active psoriatic arthritis: 24-week results of a randomised, open-label, blinded-assessor trial. Annals of the Rheumatic Diseases 2020;79(1):123-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
DRKS00000716 {unpublished data only}
- DRKS00000716. Regulatory T-cell function in psoriasis vulgaris. www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00000716 (first received 9 February 2011).
EUCTR2010‐020168‐39‐DE {published data only}
- EUCTR2010-020168-39-DE. A randomised, double blind, placebo controlled efficacy and safety trial of different doses/dose regimens of FP187 compared to placebo in moderate to severe plaque psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2010-020168-39-DE (first received 9 June 2010).
EUCTR2015‐005279‐25‐DE {published data only}
- EUCTR2015-005279-25-DE. A research study to evaluate the efficacy of LEO 32731 oral tablet formulation in patients with moderate to severe psoriasis vulgaris. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2015-005279-25-DE (first received 10 February 2016).
EUCTR2017‐001615‐36‐DE {published data only}
- EUCTR2017-001615-36-DE. A double-blind study in subjects with moderate to severe plaque psoriasis to evaluate efficacy, safety, tolerability of four different dose levels of ABY-035 compared to placebo. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2017-001615-36-DE (first received 7 September 2017).
Goldust 2019 {published data only}
- Goldust M. Depression and anxiety in patients with moderate-to-severe plaque psoriasis while on methotrexate plus adalimumab vs. methotrexate monotherapy. British Journal of Dermatology 2019;181(Suppl 1):190. [Google Scholar]
Han 2007 {published data only}
- Han L, Fang X, Huang Q, Yang QP, Fu WW, Zheng ZZ, et al. Analysis of the effect of recombinant human tumor necrosis factor receptor in the treatment of moderate to severe plaque psoriasis on PASI score. Journal of Clinical Dermatology 2007;36(11):730-2. [CENTRAL: CN-00708092] [Google Scholar]
Ikonomidis 2019 {published data only}
- Ikonomidis I, Varoudi M, Papadavid E, Makavos G, Kostelli G, Pavlidis G, et al. Improvement of endothelial glycocalyx thickness is related with reduced stiffness, wave reflections and arterial blood pressure, after treatment with IL-12/23 antagonist, in psoriasis. European Heart Journal Cardiovascular Imaging 2019;20 (Supplement 1):i969. [Google Scholar]
Krishna 2016 {unpublished data only}
- Krishna CV, Rao AV. Improvement in the quality of life of patients with severe plaque psoriasis treated with systemic methotrexate in fixed doses of 10 mg or 25 mg orally once weekly: a prospective, randomized, double-blind, parallel-group study. British Journal of Dermatology 2016;175(S1):65-6. [Google Scholar]
- NCT02248792. Quality of life of patients with psoriasis treated with methotrexate: prospective, randomized, double-blind, parallel group study. clinicaltrials.gov/ct2/show/NCT02248792 (first received 22 September 2014).
Makavos 2020 {published data only}
- Makavos G, Ikonomidis I, Andreadou I, Varoudi M, Kapniari I, Loukeri E, et al. Effects of Interleukin 17A Inhibition on myocardial deformation and vascular function in psoriasis. Canadian Journal of Cardiology 2020;36(1):100-11. [DOI] [PubMed] [Google Scholar]
Mrowietz 2005 {published data only}
- Mrowietz U, Spellman M. Dimethyl Fumarate (BG00012) as an oral therapy for moderate to severe psoriasis: results of a multicenter, randomized, double-blind, placebo-controlled trial. Journal of Investigative Dermatology 2005;125(3 Suppl):A69. [CENTRAL: CN-00792615] [Google Scholar]
- Mrowietz U, Spellman MC. Results of a phase III study of a novel oral formulation of dimethylfumarate in the treatment of moderate to severe plaque psoriasis: efficacy, safety, and quality of life effects. Journal of the European Academy of Dermatology and Venereology : JEADV 2005;19(Suppl 2):187. [CENTRAL: CN-00602493] [Google Scholar]
- Ortonne JP, Van de Kerkhof P, Mrowietz U. A novel oral agent improves quality of life (QOL) in patients with plaque psoriasis. In: 4th European Association of Dermatology and Venereology (EADV) Spring Symposium; 9-12 February 2006; Saariselka, Lapland, Finland. 2006:P-013. [CENTRAL: CN-00602214]
NCT01088165 {published data only}
- NCT01088165. The influence of adalimumab on cardiovascular and metabolic risk in psoriasis. clinicaltrials.gov/show/nct01088165 (first received 17 March 2010).
NCT01558310 {unpublished data only}
- NCT01558310. A study to evaluate the effectiveness of STELARA ™ (USTEKINUMAB) in the treatment of scalp psoriasis. clinicaltrials.gov/ct2/show/NCT01558310 (first received 20 March 2012).
NCT02655705 {unpublished data only}
- NCT02655705. Comparison study of psoriasis severity assessment tools. clinicaltrials.gov/ct2/show/NCT02655705 (first received 4 January 2016).
NCT02714322 {published data only}
- EUCTR2014-003420-46-BG. A study to evaluate the similarity in efficacy and safety of Mylan Adalimumab (MYL-1401A) compared with Humira® in subjects with moderate-to-severe chronic skin inflammatory disease. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2014-003420-46-BG (first received 19 June 2015).
- NCT02714322. MYL-1401A efficacy and safety comparability study to Humira®. clinicaltrials.gov/show/nct02714322 (first received 21 March 2016).
NCT02762994 {published data only}
- NCT02762994. International clinical trial to evaluate efficacy and safety of multiple subcutaneous injections of BCD-085 in various doses in patients with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct02762994 (first received 5 May 2016).
NCT02982005 {unpublished data only}
- NCT02982005. A study of KHK4827 (Brodalumab) in subjects with moderate to severe psoriasis in Korea. clinicaltrials.gov/ct2/show/NCT02982005 (first received 5 December 2016).
NCT03025542 {published data only}
- NCT03025542. Study to evaluate the pharmacokinetics (PK), pharmacodynamics (PD), and safety of bimekizumab in patients with chronic plaque psoriasis. clinicaltrials.gov/show/nct03025542 (first received 19 January 2017).
NCT03210259 {published data only}
- NCT03210259. The VOLTAIRE-X trial looks at the effect of switching between Humira® and BI 695501 in patients with plaque psoriasis. clinicaltrials.gov/show/nct03210259 (first received 6 July 2017).
NCT03364309 {published data only}
- NCT03364309. A study of ixekizumab (LY2439821) in Chinese participants with moderate-to-severe plaque psoriasis. clinicaltrials.gov/show/nct03364309 (first received 6 December 2017).
NCT03370133 {published data only}
- NCT03370133. A study to evaluate the efficacy and safety of bimekizumab compared to placebo and an active comparator in adult subjects with moderate to severe chronic plaque psoriasis (BE VIVID). clinicaltrials.gov/show/nct03370133 (first received 12 December 2017).
NCT03412747 {published data only}
- NCT03412747. A study to evaluate the efficacy and safety of bimekizumab in adult subjects with moderate to severe chronic plaque psoriasis (BE SURE). clinicaltrials.gov/show/nct03412747 (first received 26 January 2018).
NCT03518047 {published data only}
- NCT03518047. Risankizumab therapy versus placebo for subjects with psoriasis in the Russian Federation (IMMPRESS). clinicaltrials.gov/show/nct03518047 (first received 8 May 2018).
NCT03589885 {published data only}
- EUCTR2018-000518-39-DE. Study of efficacy and safety of secukinumab 2 mL auto-injector (300 mg) injections in subjects with moderate to severe plaque psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2018-000518-39-DE (first received 15 November 2018).
- NCT03589885. Study of efficacy and safety of secukinumab 2 mL auto-injector (300 mg) in subjects with moderate to severe plaque psoriasis (MATURE). clinicaltrials.gov/show/nct03589885 (first received 18 July 2018).
NCT03875482 {published data only}
- NCT03875482. A study to assess safety and efficacy of risankizumab using a new formulation in participants with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct03875482 (first received 14 March 2019).
NCT04488185 {published data only}
- NCT04488185. An efficacy study of secukinumab in plaque psoriasis patients with subclinical psoriatic arthritis as measured by musculoskeletal ultrasound (INTERCEPT). clinicaltrials.gov/show/NCT04488185 (first received 27 July 2020).
References to ongoing studies
CTRI/2016/10/007345 {unpublished data only}
- CTRI/2016/10/007345. A randomized, double-blind, placebo-controlled, comparative, prospective, multicentre trial to assess efficacy and safety of apremilast tablets in subjects with moderate to severe plaque psoriasis who are candidates for phototherapy or systemic therapy. www.ctri.nic.in/Clinicaltrials/pdf_generate.php?trialid=16164&EncHid=&modid=&compid=%27,%2716164det%27/CTRI/2016/10/007345 (first received 20 October 2016).
CTRI/2019/01/017362 {published data only}
- CTRI/2019/01/017362. A study to assess the effects of Apremilast and Methotrexate in the treatment of patients with psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/01/017362 (first received 31 January 2019).
CTRI/2019/07/020274 {published data only}
- CTRI/2019/07/020274. To compare the effect of three drugs- methotrexate, apremilast and their combination in patients suffering from psoriasis vulgaris. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2019/07/020274 (first received 17 July 2019).
EUCTR2013‐004918‐18‐NL {unpublished data only}
- Busard C, Menting S, Van Bezooijen SJ, Van den Reek J, Hutten B, Prens E, et al. Erratum to: Optimizing adalimumab treatment in psoriasis with concomitant methotrexate (OPTIMAP): study protocol for a pragmatic, single-blinded, investigator-initiated randomized controlled trial. Trials [Electronic Resource] 2017;18(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busard CI, Menting SP, Van Bezooijen JS, Van den Reek JM, Hutten BA, Prens EP, et al. Optimizing adalimumab treatment in psoriasis with concomitant methotrexate (OPTIMAP): study protocol for a pragmatic, single-blinded, investigator-initiated randomized controlled trial. Trials [Electronic Resource] 2017;18(1):52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EUCTR2013-004918-18-NL. Optimising adalimumab treatment in psoriasis with concomitant methotrexate - OPTIMAP [Optimising adalimumab treatment in psoriasis with concomitant methotrexate]. apps.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2013-004918-18-NL/EUCTR2013-004918-18-NL (first received 12 December 2013).
- Van Der Kraaij G, Busard C, Van Den Reek J, Menting S, De Jong E, De Kort W, et al. Optimizing adalimumab treatment in psoriasis with concomitant methotrexate: a randomized controlled trial. Journal of the European Academy of Dermatology and Venereology : JEADV 2019;33:25-6. [Google Scholar]
EUCTR2017‐003367‐35‐PL {published data only}
- EUCTR2017-003367-35-PL. A multicenter, double-blind, randomized, parallel-group, active control study to compare the efficacy, safety, and immunogenicity of AVT02 versus Humira® in patients with moderate-to-severe chronic plaque psoriasis (ALVOPAD PS). www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2017-003367-35-PL (first received 27 November 2018).
EUCTR2018‐001238‐16‐FR {published data only}
- EUCTR2018-001238-16-FR. A study to evaluate further therapeutic strategies with guselkumab in patients with moderate-to-severe plaque-type psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2018-001238-16-FR (first received 10 July 2019).
EUCTR2018‐001926‐25‐ES {published data only}
- EUCTR2018-001926-25-ES. Efficacy and safety of BMS-986165 versus placebo and active comparator in subjects with psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=EUCTR2018-001926-25-ES (first received 25 October 2018).
- JPRN-JapicCTI-184213. An investigational study to evaluate experimental medication BMS-986165 compared to placebo and a currently available treatment in participants with moderate to severe plaque psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=JPRN-JapicCTI-184213 (first received 21 November 2018).
NCT02258282 {unpublished data only}
- NCT02258282. Safety and efficacy of etanercept in patients with psoriasis. clinicaltrials.gov/ct2/show/NCT02258282 (first received 7 October 2014).
NCT02325219 {unpublished data only}
- NCT02325219. An efficacy and safety of CNTO 1959 (Guselkumab) in participants with moderate to severe plaque-type psoriasis. clinicaltrials.gov/ct2/show/NCT02325219 (first received 24 December 2014).
NCT02701205 {published data only}
- NCT02701205. Safety and efficacy study of etanercept (Qiangke®) to treat moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct02701205 (first received 8 March 2016).
NCT02762955 {published data only}
- CTRI/2018/03/012598. Comparative double-blind study of the efficacy and safety of BCD-057 and Humira® in patients with moderate to severe plaque psoriasis. www.who.int/trialsearch/Trial2.aspx?TrialID=CTRI/2018/03/012598 (first received 15 March 2018).
- NCT02762955. Comparative clinical trial of efficacy and safety of BCD-057 and Humira® in patients with moderate to severe plaque psoriasis. clinicaltrials.gov/show/nct02762955 (first received 5 May 2016).
NCT02829424 {published data only}
- NCT02829424. Multicenter randomized double blind controlled-study to assess the potential of methotrexate versus placebo to improve and maintain response to anti TNF- alpha agents in adult patients with moderate to severe psoriasis. clinicaltrials.gov/show/nct02829424 (first received 12 July 2016).
NCT03384745 {published data only}
- NCT03384745. A phase 2b study of the efficacy, safety, and tolerability of M1095 in subjects with moderate to severe psoriasis. clinicaltrials.gov/show/nct03384745 (first received 27 December 2017).
NCT03410992 {published data only}
- NCT03410992. A study with an initial treatment period followed by a randomized-withdrawal period to evaluate the efficacy and safety of bimekizumab in adult subjects with moderate to severe chronic plaque psoriasis (BE READY). clinicaltrials.gov/show/nct03410992 (first received 25 January 2018).
NCT03421197 {published data only}
- NCT03421197. A study to assess the efficacy and safety of PPC-06 (Tepilamide Fumarate). clinicaltrials.gov/show/nct03421197 (first received 5 February 2018).
NCT03478280 {published data only}
- NCT03478280. Effect of brodalumab compared to placebo on vascular inflammation in moderate-to-severe psoriasis. clinicaltrials.gov/show/nct03478280 (first received 27 March 2018).
NCT03504852 {published data only}
- NCT03504852. Efficacy and safety of 2 secukinumab regimens in 90 kg or higher subjects with moderate to severe chronic plaque-type psoriasis. clinicaltrials.gov/show/nct03504852 (first received 20 April 2018).
NCT03535194 {published data only}
- NCT03535194. A study to assess if mirikizumab is effective and safe compared to secukinumab and placebo in moderate to severe plaque psoriasis (OASIS-2). clinicaltrials.gov/show/nct03535194 (first received 24 May 2018).
NCT03536884 {published data only}
- NCT03536884. A study to evaluate the efficacy and safety of bimekizumab compared to an active comparator in adult subjects with moderate to severe chronic plaque psoriasis (BE RADIANT). clinicaltrials.gov/show/nct03536884 (first received 25 May 2018).
NCT03598790 {published data only}
- NCT03598790. A study to assess the safety, tolerability and efficacy of bimekizumab in adult subjects with moderate to severe chronic plaque psoriasis (BE BRIGHT). clinicaltrials.gov/show/nct03598790 (first received 25 July 2018).
NCT03611751 {published data only}
- NCT03611751. An investigational study to evaluate experimental medication BMS-986165 compared to placebo and a currently available treatment in participants with moderate-to-severe plaque psoriasis. clinicaltrials.gov/show/nct03611751 (first received 2 August 2018).
NCT03897075 {published data only}
- NCT03897075. Efficacy and safety study of tildrakizumab in the treatment of nail psoriasis. clinicaltrials.gov/show/nct03897075 (first received 1 April 2019).
NCT03897088 {published data only}
- NCT03897088. Efficacy and safety of tildrakizumab in the treatment of scalp psoriasis. clinicaltrials.gov/show/nct03897088 (first received 1 April 2019).
NCT03927352 {published data only}
- NCT03927352. The purpose of this research study is to compare the efficacy and safety of SCT630 and adalimumab (HUMIRA®) in adults with plaque psoriasis. clinicaltrials.gov/show/nct03927352 (first received 25 April 2019).
NCT04167462 {published data only}
- NCT04167462. An investigational study to evaluate experimental medication BMS-986165 compared to placebo in participants with plaque psoriasis in mainland China, Taiwan, and South Korea (POETYK-PSO-3). clinicaltrials.gov/show/NCT04167462 (first received 18 November 2019).
NCT04237116 {published data only}
- NCT04237116. A study of secukinumab treatment in patients with plaque psoriasis and coexisting Non-alcoholic Fatty Liver Disease (NAFLD) (pINPOINt). clinicaltrials.gov/show/NCT04237116 (first received 23 January 2020).
NCT04306315 {published data only}
- NCT04306315. Adjusted brodalumab dose compared with standard brodalumab dose in subjects with moderate-to-severe plaque psoriasis and ≥120 kg body weight. clinicaltrials.gov/show/NCT04306315 (first received 12 March 2020).
NCT04453137 {published data only}
- NCT04453137. Pharmacokinetic, efficacy, safety, and immunogenicity of AVT02 with moderate to severe chronic plaque psoriasis. clinicaltrials.gov/show/NCT04453137 (first received 1 July 2020).
TCTR20161028001 {unpublished data only}
- TCTR20161028001. A randomised, double-blind, placebo controlled, multicenter study of subcutaneous secukinumab, to demonstrate efficacy after twelve weeks of treatment and to assess safety, tolerability and long-term efficacy up to one year in subjects with moderate to severe chronic plaque-type psoriasis with or without psoriatic arthritis comorbidity. clinicaltrials.in.th/index.php?tp=regtrials&menu=trialsearch&smenu=fulltext&task=search&task2=view1&id=2148 (first received 28 February 2017).
Additional references
Afach 2021
Armstrong 2020
- Armstrong AW, Puig L, Joshi A, Skup M, Williams D, Li J, et al. Comparison of biologics and oral treatments for plaque psoriasis: a meta-analysis. JAMA Dermatology 2020;156(3):258-69. [DOI: 10.1001/jamadermatol.2019.4029] [DOI] [PMC free article] [PubMed] [Google Scholar]
Atwan 2015
- Atwan A, Ingram JR, Abbott R, Kelson MJ, Pickles T, Bauer A, et al. Oral fumaric acid esters for psoriasis. Cochrane Database of Systematic Reviews 2015, Issue 8. Art. No: CD010497. [DOI: 10.1002/14651858.CD010497.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Balak 2016
- Balak DM, Fallah Arani S, Hajdarbegovic E, Hagemans CA, Bramer WM, Thio HB, et al. Efficacy, effectiveness and safety of fumaric acid esters in the treatment of psoriasis: a systematic review of randomized and observational studies. British Journal of Dermatology 2016;175(2):250-62. [PMID: ] [DOI] [PubMed] [Google Scholar]
Bansback 2009
- Bansback N, Sizto S, Sun H, Feldman S, Willian MK, Anis A. Efficacy of systemic treatments for moderate to severe plaque psoriasis: systematic review and meta-analysis. Dermatology 2009;219(3):209-18. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Boehncke 2015
- Boehncke WH, Schon MP. Psoriasis. Lancet 2015;386(9997):983-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Brimhall 2008
- Brimhall AK, King LN, Licciardone JC, Jacobe H, Menter A. Safety and efficacy of alefacept, efalizumab, etanercept and infliximab in treating moderate to severe plaque psoriasis: a meta-analysis of randomized controlled trials. British Journal of Dermatology 2008;159(2):274-85. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Bucher 1997
- Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. Journal of Clinical Epidemiology 1997;50(6):683-91. [PMID: ] [DOI] [PubMed] [Google Scholar]
Campanati 2017
- Campanati A, Benfaremo D, Luchetti MM, Ganzetti G, Gabrielli A, Offidani A. Certolizumab pegol for the treatment of psoriasis. Expert Opinion on Biological Therapy 2017;17(3):387-94. [PMID: ] [DOI] [PubMed] [Google Scholar]
Capon 2017
- Capon F. The genetic basis of psoriasis. International Journal of Molecular Sciences 2017;18(12):E2526. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chaimani 2012
- Chaimani A, Salanti G. Using network meta-analysis to evaluate the existence of small-study effects in a network of interventions. Research Synthesis Methods 2012;3(2):161-76. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaimani 2013
- Chaimani A, Vasiliadis HS, Pandis N, Schmid CH, Welton NJ, Salanti G. Effects of study precision and risk of bias in networks of interventions: a network meta-epidemiological study. International Journal of Epidemiology 2013;42(4):1120-31. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaimani 2017a
- Chaimani A, Caldwell DM, Li T, Higgins JP, Salanti G. Additional considerations are required when preparing a protocol for a systematic review with multiple interventions. Journal of Clinical Epidemiology 2017;16(S0895):30775-2. [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaimani 2017b
- Chaimani A, Caldwell DM, Li T, Higgins JPT, Salanti G. Additional considerations are required when preparing a protocol for a systematic review with multiple interventions. Journal of Clinical Epidemiology 2017;83:65-74. [DOI] [PubMed] [Google Scholar]
Chaimani 2017c
- Chaimani A, Salanti G, Leucht S, Geddes JR, Cipriani A. Common pitfalls and mistakes in the set-up, analysis and interpretation of results in network meta-analysis: what clinicians should look for in a published article. Evidence-Based Mental Health 2017;20(3):88-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chiu 2014
- Chiu HY, Wang TS, Chan CC, Cheng YP, Lin SJ, Tsai TF. Human leucocyte antigen-Cw6 as a predictor for clinical response to ustekinumab, an interleukin-12/23 blocker, in Chinese patients with psoriasis: a retrospective analysis. British Journal of Dermatology 2014;171(5):1181-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Christophers 1992
- Christophers E, Mrowietz U, Henneicke HH, Farber L, Welzel D. Cyclosporine in psoriasis: a multicenter dose-finding study in severe plaque psoriasis. The German Multicenter Study. Journal of the American Academy of Dermatology 1992;26(1):86-90. [PMID: ] [DOI] [PubMed] [Google Scholar]
CINeMA 2017 [Computer program]
- Institute of Social and Preventive Medicine, University of Bern CINeMA: Confidence in Network Meta-Analysis. Bern: Institute of Social and Preventive Medicine, University of Bern, 2017.
Cipriani 2013
- Cipriani A, Higgins JP, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Annals of Internal Medicine 2013;159(2):130-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cohen 1988
- Cohen Jacob. Statistical power analysis for the behavioral sciences. Hillsdale, N.J: L. Erlbaum Associates, 1988. [Google Scholar]
Covidence 2019 [Computer program]
- Veritas Health Innovation Covidence. Version accessed prior to 19 August 2019. Melbourne, Australia: Veritas Health Innovation. Available at covidence.org.
Dechartres 2013
- Dechartres A, Trinquart L, Boutron I, Ravaud P. Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ (Clinical research ed.) 2013;346:f2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2021
- Deeks JJ, Higgins JP, Altman DG (editors). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). The Cochrane Collaboration, 2021. Available from www.training.cochrane.org/handbook.
Dias 2010
- Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Statistics in Medicine 2010;29(7-8):932-44. [PMID: ] [DOI] [PubMed] [Google Scholar]
Dong 2017
- Dong J, Goldenberg G. New biologics in psoriasis: an update on IL-23 and IL-17 inhibitors. Cutis 2017;99(2):123-7. [PMID: ] [PubMed] [Google Scholar]
Elder 2010
- Elder JT, Bruce AT, Gudjonsson JE, Johnston A, Stuart PE, Tejasvi T, et al. Molecular dissection of psoriasis: integrating genetics and biology. Journal of Investigative Dermatology 2010;130(5):1213-26. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Elliott 2017
- Elliott JH, Synnot A, Turner T, Simmonds M, Akl EA, McDonald S, et al. Living systematic review: 1. Introduction-the why, what, when, and how. Journal of Clinical Epidemiology 2017;91:23-30. [DOI] [PubMed] [Google Scholar]
Geng 2018
- Geng W, Zhao J, Fu J, Zhang H, Qiao S. Efficacy of several biological therapies for treating moderate to severe psoriasis: a network meta-analysis. Experimental and Therapeutic Medicine 2018;16(6):5085-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gisondi 2004
- Gisondi P, Gubinelli E, Cocuroccia B, Girolomoni G. Targeting tumor necrosis factor-alpha in the therapy of psoriasis. Current Drug Targets. Inflammation and Allergy 2004;3(2):175-83. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gómez‐García 2017
- Gómez-García F, Epstein D, Isla-Tejera B, Lorente A, Vélez García-Nieto A, Ruano J. Short-term efficacy and safety of new biological agents targeting the interleukin-23-T helper 17 pathway for moderate-to-severe plaque psoriasis: a systematic review and network meta-analysis. British Journal of Dermatology 2017;176(3):594-603. [PMID: ] [DOI] [PubMed] [Google Scholar]
Gospodarevskaya 2009
- Gospodarevskaya E, Picot J, Cooper K, Loveman E, Takeda A. Ustekinumab for the treatment of moderate to severe psoriasis. Health Technology Assessment 2009;13(Suppl 3):61-6. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Griffiths 2007
- Griffiths CE, Barker JN. Pathogenesis and clinical features of psoriasis. Lancet 2007;370(9583):263-71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Helliwell 2005
- Helliwell PS, Taylor WJ. Classification and diagnostic criteria for psoriatic arthritis. Annals of the Rheumatic Diseases 2005;64(Suppl 2):ii3-8. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2012
- Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Research Synthesis Methods 2012;3(2):98-110. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from training.cochrane.org/handbook.
Ho 1996
- Ho S, Clipstone N, Timmermann L, Northrop J, Graef I, Fiorentino D, et al. The mechanism of action of cyclosporin A and FK506. Clinical Immunology and Immunopathology 1996;80(3 Pt 2):S40-5. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ho 1999
- Ho VC, Griffiths CE, Albrecht G, Vanaclocha F, Leon-Dorantes G, Atakan N, et al. Intermittent short courses of cyclosporin (Neoral(R)) for psoriasis unresponsive to topical therapy: a 1-year multicentre, randomized study. The PISCES Study Group. British Journal of Dermatology 1999;141(2):283-91. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Jabbar‐Lopez 2017
- Jabbar-Lopez ZK, Yiu ZZN, Ward V, Exton LS, Mohd Mustapa MF, Samarasekera E, et al. Quantitative evaluation of biologic therapy options for psoriasis: a systematic review and network meta-analysis. Journal of Investigative Dermatology 2017;137(8):1646-54. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jackson 2014
- Jackson D, Barrett JK, Rice S, White IR, Higgins JP. A design-by-treatment interaction model for network meta-analysis with random inconsistency effects. Statistics in Medicine 2014;33(21):3639-54. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jariwala 2007
- Jariwala SP. The role of dendritic cells in the immunopathogenesis of psoriasis. Archives of Dermatological Research 2007;299(8):359-66. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kimball 2005
- Kimball AB, Jacobson C, Weiss S, Vreeland MG, Wu Y. The psychosocial burden of psoriasis. American Journal of Clinical Dermatology 2005;6(6):383-92. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Kremers 2007
- Kremers HM, McEvoy MT, Dann FJ, Gabriel SE. Heart disease in psoriasis. Journal of the American Academy of Dermatology 2007;57(2):347-54. [PMID: ] [DOI] [PubMed] [Google Scholar]
Lebwohl 2010
- Lebwohl M, Papp K, Han C, Schenkel B, Yeilding N, Wang Y, et al. Ustekinumab improves health-related quality of life in patients with moderate-to-severe psoriasis: results from the PHOENIX 1 trial. British Journal of Dermatology 2010;162(1):137-46. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Le Cleach 2008
- Le Cleach L, Chassany O, Levy A, Wolkenstein P, Chosidow O. Poor reporting of quality of life outcomes in dermatology randomized controlled clinical trials. Dermatology 2008;216(1):46-55. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Liang 2019
- Liang F, Wu Z, Mo M, Zhou C, Shen J, Wang Z, et al. Comparison of treatment effect from randomised controlled phase II trials and subsequent phase III trials using identical regimens in the same treatment setting. European Journal of Cancer 2019;121:19-28. [DOI] [PubMed] [Google Scholar]
Lin 2012
- Lin VW, Ringold S, Devine EB. Comparison of ustekinumab with other biological agents for the treatment of moderate to severe plaque psoriasis: a Bayesian network meta-analysis. Archives of Dermatology 2012;148(12):1403-10. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Loos 2018
- Loos AM, Liu S, Segel C, Ollendorf DA, Pearson SD, Linder JA. Comparative effectiveness of targeted immunomodulators for the treatment of moderate-to-severe plaque psoriasis: A systematic review and network meta-analysis. Journal of the American Academy of Dermatology 2018;79(1):135-44.e7. [DOI] [PubMed] [Google Scholar]
Loveman 2009
- Loveman E, Turner D, Hartwell D, Cooper K, Clegg A. Infliximab for the treatment of adults with psoriasis. Health Technology Assessment 2009;13(Suppl 1):55-60. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Lowes 2008
- Lowes MA, Kikuchi T, Fuentes-Duculan J, Cardinale I, Zaba LC, Haider AS, et al. Psoriasis vulgaris lesions contain discrete populations of Th1 and Th17 T cells. Journal of Investigative Dermatology 2008;128(5):1207-11. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Mason 2013
- Mason AR, Mason J, Cork M, Dooley G, Hancock H. Topical treatments for chronic plaque psoriasis. Cochrane Database of Systematic Reviews 2013, Issue 3. Art. No: CD005028. [DOI: 10.1002/14651858.CD005028.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mavridis 2014
- Mavridis D, Chaimani A, Efthimiou O, Leucht S, Salanti G. Addressing missing outcome data in meta-analysis. Evidence-Based Mental Health 2014;17(3):85-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Maza 2011
- Maza A, Montaudie H, Sbidian E, Gallini A, Aractingi S, Aubin F, et al. Oral cyclosporin in psoriasis: a systematic review on treatment modalities, risk of kidney toxicity and evidence for use in non-plaque psoriasis. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25 Suppl 2:19-27. [PMID: ] [DOI] [PubMed] [Google Scholar]
Montaudie 2011
- Montaudie H, Sbidian E, Paul C, Maza A, Gallini A, Aractingi S, et al. Methotrexate in psoriasis: a systematic review of treatment modalities, incidence, risk factors and monitoring of liver toxicity. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25 Suppl 2:12-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mossner 2009
- Mossner R, Reich K. Management of severe psoriasis with TNF antagonists. Adalimumab, etanercept and infliximab. Current Problems in Dermatology 2009;38:107-36. [PMID: ] [DOI] [PubMed] [Google Scholar]
Mrowietz 1995
- Mrowietz U, Farber L, Henneicke-von Zepelin HH, Bachmann H, Welzel D, Christophers E. Long-term maintenance therapy with cyclosporine and posttreatment survey in severe psoriasis: results of a multicenter study. German Multicenter Study. Journal of the American Academy of Dermatology 1995;33(3):470-5. [PMID: ] [DOI] [PubMed] [Google Scholar]
Naldi 2005
- Naldi L, Chatenoud L, Linder D, Belloni Fortina A, Peserico A, Virgili AR, et al. Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: results from an Italian case-control study. Journal of Investigative Dermatology 2005;125(1):61-7. [PMID: ] [DOI] [PubMed] [Google Scholar]
Naldi 2010
- Naldi L. Scoring and monitoring the severity of psoriasis. What is the preferred method? What is the ideal method? Is PASI passe? facts and controversies. Clinics in Dermatology 2010;28(1):67-72. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nast 2015a
- Nast A, Jacobs A, Rosumeck S, Werner RN. Efficacy and safety of systemic long-term treatments for moderate-to-severe psoriasis: a systematic review and meta-analysis. Journal of Investigative Dermatology 2015;135(11):2641-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Nast 2015b
- Nast A, Jacobs A, Rosumeck S, Werner RN. Methods Report: European S3-Guidelines on the systemic treatment of psoriasis vulgaris--update 2015--EDF in cooperation with EADV and IPC. Journal of the European Academy of Dermatology and Venereology 2015;29(12):e1-22. [DOI: 10.1111/jdv.13353] [DOI] [PubMed]
Nelson 2008
- Nelson AA, Pearce DJ, Fleischer AB Jr, Balkrishnan R, Feldman SR. Cost-effectiveness of biologic treatments for psoriasis based on subjective and objective efficacy measures assessed over a 12-week treatment period. Journal of the American Academy of Dermatology 2008;58(1):125-35. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Nijsten 2007
- Nijsten T, Looman CW, Stern RS. Clinical severity of psoriasis in last 20 years of PUVA study. Archives of Dermatology 2007;143(9):1113-21. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Ormerod 2004
- Ormerod AD, Mrowietz U. Fumaric acid esters, their place in the treatment of psoriasis. British Journal of Dermatology 2004;150(4):630-2. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Parisi 2013
- Parisi R, Symmons DP, Griffiths CE, Ashcroft DM, Identification and Management of Psoriasis and Associated ComorbidiTy (IMPACT) project team. Global epidemiology of psoriasis: a systematic review of incidence and prevalence. Journal of Investigative Dermatology 2013;133(2):377-85. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Rapp 1999
- Rapp SR, Feldman SR, Exum ML, Fleischer AB Jr, Reboussin DM. Psoriasis causes as much disability as other major medical diseases. Journal of the American Academy of Dermatology 1999;41(3 Pt 1):401-7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Reich 2008
- Reich K, Sinclair R, Roberts G, Griffiths CE, Tabberer M, Barker J. Comparative effects of biological therapies on the severity of skin symptoms and health-related quality of life in patients with plaque-type psoriasis: a meta-analysis. Current Medical Research and Opinion 2008;24(5):1237-54. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Reich 2012b
- Reich K, Burden AD, Eaton JN, Hawkins NS. Efficacy of biologics in the treatment of moderate to severe psoriasis: a network meta-analysis of randomized controlled trials. British Journal of Dermatology 2012;166(1):179-88. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Revman 2020 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Nordic Cochrane Centre, The Cochrane Collaboration, 2020. Copenhagen.
Riley 2011
- Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ (Clinical research ed.) 2011;342:d549. [PMID: ] [DOI] [PubMed] [Google Scholar]
Robinson 2012
- Robinson A, Kardos M, Kimball AB. Physician Global Assessment (PGA) and Psoriasis Area and Severity Index (PASI): why do both? A systematic analysis of randomized controlled trials of biologic agents for moderate to severe plaque psoriasis. Journal of the American Academy of Dermatology 2012;66(3):369-75. [PMID: ] [DOI] [PubMed] [Google Scholar]
Salanti 2011
- Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. Journal of Clinical Epidemiology 2011;64(2):163-71. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Salanti 2014
- Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PloS One 2014;9(7):e99682. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Savage 2015
- Savage LJ, Wittmann M, McGonagle D, Helliwell PS. Ustekinumab in the treatment of psoriasis and psoriatic arthritis. Rheumatology and Therapy 2015;2(1):1-16. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sbidian 2011
- Sbidian E, Maza A, Montaudie H, Gallini A, Aractingi S, Aubin F, et al. Efficacy and safety of oral retinoids in different psoriasis subtypes: a systematic literature review. Journal of the European Academy of Dermatology and Venereology : JEADV 2011;25 Suppl 2:28-33. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schmitt 2005
- Schmitt J, Wozel G. The psoriasis area and severity index is the adequate criterion to define severity in chronic plaque-type psoriasis. Dermatology 2005;210(3):194-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Schmitt 2008
- Schmitt J, Zhang Z, Wozel G, Meurer M, Kirch W. Efficacy and tolerability of biologic and nonbiologic systemic treatments for moderate-to-severe psoriasis: meta-analysis of randomized controlled trials. British Journal of Dermatology 2008;159(3):513-26. [PMID: ] [DOI] [PubMed] [Google Scholar]
Signorovitch 2010
- Signorovitch JE, Wu EQ, Yu AP, Gerrits CM, Kantor E, Bao Y, et al. Comparative effectiveness without head-to-head trials: a method for matching-adjusted indirect comparisons applied to psoriasis treatment with adalimumab or etanercept. Pharmacoeconomics 2010;28(10):935-45. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Signorovitch 2015
- Signorovitch JE, Betts KA, Yan YS, LeReun C, Sundaram M, Wu EQ, et al. Comparative efficacy of biological treatments for moderate-to-severe psoriasis: a network meta-analysis adjusting for cross-trial differences in reference arm response. British Journal of Dermatology 2015;172(2):504-12. [PMID: ] [DOI] [PubMed] [Google Scholar]
Spuls 1997
- Spuls PI, Witkamp L, Bossuyt PM, Bos JD. A systematic review of five systemic treatments for severe psoriasis. British Journal of Dermatology 1997;137(6):943-9. [MEDLINE: ] [PubMed] [Google Scholar]
Spuls 2010
- Spuls PI, Lecluse LL, Poulsen ML, Bos JD, Stern RS, Nijsten T. How good are clinical severity and outcome measures for psoriasis?: quantitative evaluation in a systematic review. Journal of Investigative Dermatology 2010;130(4):933-43. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Spuls 2016
- Spuls PI, Gerbens LA, Simpson E, Apfelbacher CJ, Chalmers JR, Thomas KS, et al. Patient-Oriented Eczema Measure (POEM), a core instrument to measure symptoms in clinical trials: a Harmonising Outcome Measures for Eczema (HOME) statement. British Journal of Dermatology 2016;176(4):979-84. [PMID: ] [DOI] [PubMed] [Google Scholar]
Stern 2004
- Stern RS, Nijsten T, Feldman SR, Margolis DJ, Rolstad T. Psoriasis is common, carries a substantial burden even when not extensive, and is associated with widespread treatment dissatisfaction. Journal of Investigative Dermatology. Symposium proceedings 2004;9(2):136-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Strober 2006
- Strober BE, Siu K, Menon K. Conventional systemic agents for psoriasis. A systematic review. Journal of Rheumatology 2006;33(7):1442-6. [MEDLINE: ] [PubMed] [Google Scholar]
Tan 2011
- Tan JY, Li S, Yang K, Ma B, Chen W, Zha C, et al. Ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: a meta-analysis. Journal of Dermatological Treatment 2011;22(6):323-36. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Torres 2015
- Torres T, Filipe P. Small molecules in the treatment of psoriasis. Drug Development Research 2015;76(5):215-27. [PMID: ] [DOI] [PubMed] [Google Scholar]
Tubach 2009
- Tubach F, Salmon D, Ravaud P, Allanore Y, Goupille P, Breban M, et al. Risk of tuberculosis is higher with anti-tumor necrosis factor monoclonal antibody therapy than with soluble tumor necrosis factor receptor therapy: The three-year prospective French Research Axed on Tolerance of Biotherapies registry. Arthritis and Rheumatism 2009;60(7):1884-94. [MEDLINE: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2009
- Turner D, Picot J, Cooper K, Loveman E. Adalimumab for the treatment of psoriasis. Health Technology Assessment 2009;13(Suppl 2):49-54. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Veroniki 2013
- Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G. Evaluation of inconsistency in networks of interventions. International Journal of Epidemiology 2013;42(1):332-45. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Veroniki 2018
- Veroniki AA, Straus SE, Rücker G, Tricco AC. Is providing uncertainty intervals in treatment ranking helpful in a network meta-analysis? Journal of Clinical Epidemiology 2018;100:122-9. [DOI] [PubMed] [Google Scholar]
White 2012
- White IR, Barrett JK, Jackson D, Higgins JP. Consistency and inconsistency in network meta-analysis: model estimation using multivariate meta-regression. Research Synthesis Methods 2012;3(2):111-25. [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilson 2007
- Wilson NJ, Boniface K, Chan JR, McKenzie BS, Blumenschein WM, Mattson JD, et al. Development, cytokine profile and function of human interleukin 17-producing helper T cells. Nature Immunology 2007;8(9):950-7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Wolkenstein 2009
- Wolkenstein P, Revuz J, Roujeau JC, Bonnelye G, Grob JJ, Bastuji-Garin S. Psoriasis in France and associated risk factors: results of a case-control study based on a large community survey. Dermatology (Basel, Switzerland) 2009;218(2):103-9. [PMID: ] [DOI] [PubMed] [Google Scholar]
Woolacott 2006
- Woolacott N, Hawkins N, Mason A, Kainth A, Khadjesari Z, Vergel YB, et al. Etanercept and efalizumab for the treatment of psoriasis: a systematic review. Health Technology Assessment 2006;10(46):1-233, i-iv. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Xu 2019
- Xu G, Xia M, Jiang C, Yu Y, Wang G, Yuan J, et al. Comparative efficacy and safety of thirteen biologic therapies for patients with moderate or severe psoriasis: A network meta-analysis. Journal of Pharmacological Sciences 2019;139(4):289-303. [DOI] [PubMed] [Google Scholar]
Zachariae 2003
- Zachariae H. Prevalence of joint disease in patients with psoriasis: implications for therapy. American Journal of Clinical Dermatology 2003;4(7):441-7. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
Zheng 2007
- Zheng Y, Danilenko DM, Valdez P, Kasman I, Eastham-Anderson J, Wu J, et al. Interleukin-22, a T(H)17 cytokine, mediates IL-23-induced dermal inflammation and acanthosis. Nature 2007;445(7128):648-51. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Sbidian 2015
- Sbidian E, Le Cleach L, Trinquart L, Do G, Hughes C, Naldi L, et al. Systemic pharmacological treatments for chronic plaque psoriasis. Cochrane Database of Systematic Reviews 2015, Issue 2. Art. No: CD011535. [DOI: 10.1002/14651858.CD011535] [DOI] [Google Scholar]
Sbidian 2017
- Sbidian E, Chaimani A, Garcia-Doval I, Do G, Hua C, Mazaud C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database of Systematic Reviews 2017, Issue 12. Art. No: CD011535. [DOI: 10.1002/14651858.CD011535.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sbidian 2020
- Sbidian E, Chaimani A, Afach S, Doney L, Dressler C, Hua C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta‐analysis. Cochrane Database of Systematic Reviews 2020, Issue 1. Art. No: CD011535. [DOI: 10.1002/14651858.CD011535.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]


