Key Points
Question
What is the association between dietary patterns consumed and all-cause mortality?
Findings
In this systematic review of 1 randomized clinical trial and 152 observational studies on dietary patterns and all-cause mortality, evidence demonstrated that dietary patterns characterized by increased consumption of vegetables, fruits, legumes, nuts, whole grains, unsaturated vegetable oils, fish, and lean meat or poultry (when meat was included) among adults and older adults were associated with decreased risk of all-cause mortality. These healthy patterns consisted of relatively low intake of red and processed meat, high-fat dairy, and refined carbohydrates or sweets.
Meaning
This review found that a dietary pattern with nutrient-dense foods was associated with reduced risk of death from all causes.
Abstract
Importance
The 2020 Dietary Guidelines Advisory Committee conducted a systematic review of existing research on diet and health to inform the current Dietary Guidelines for Americans. The committee answered this public health question: what is the association between dietary patterns consumed and all-cause mortality (ACM)?
Objective
To ascertain the association between dietary patterns consumed and ACM.
Evidence Review
Guided by an analytical framework and predefined inclusion and exclusion criteria developed by the committee, the US Department of Agriculture’s Nutrition Evidence Systematic Review (NESR) team searched PubMed, the Cochrane Central Register of Controlled Trials, and Embase and dual-screened the results to identify articles that were published between January 1, 2000, and October 4, 2019. These studies evaluated dietary patterns and ACM in participants aged 2 years and older. The NESR team extracted data from and assessed risk of bias in included studies. Committee members synthesized the evidence, developed conclusion statements, and graded the strength of the evidence supporting the conclusion statements.
Findings
A total of 1 randomized clinical trial and 152 observational studies were included in the review. Studies enrolled adults and older adults (aged 17-84 years at baseline) from 28 countries with high or very high Human Development Index; 53 studies originated from the US. Most studies were well designed, used rigorous methods, and had low or moderate risks of bias. Precision, directness, and generalizability were demonstrated across the body of evidence. Results across studies were highly consistent. Evidence suggested that dietary patterns in adults and older adults that involved higher consumption of vegetables, fruits, legumes, nuts, whole grains, unsaturated vegetable oils, fish, and lean meat or poultry (when meat was included) were associated with a decreased risk of ACM. These healthy patterns were also relatively low in red and processed meat, high-fat dairy, and refined carbohydrates or sweets. Some of these dietary patterns also included intake of alcoholic beverages in moderation. Results based on additional analyses with confounding factors generally confirmed the robustness of main findings.
Conclusions and Relevance
In this systematic review, consuming a nutrient-dense dietary pattern was associated with reduced risk of death from all causes.
This systematic review describes the combinations of foods, beverages, and food groups that were associated with beneficial outcomes, according to existing research on diet and nutrition.
Introduction
Every 5 years, the US Department of Agriculture and Department of Health and Human Services convene the Dietary Guidelines Advisory Committee to review existing evidence on diet and health to inform the Dietary Guidelines for Americans. Over time, the committee’s focus has shifted away from single nutrients or foods and toward overall dietary patterns. Nutrient and food analyses cannot account for the interactions among or the degree of independent variation of coingested nutrients and food components.1 To advance nutrition research and inform the 2020-2025 Dietary Guidelines for Americans, understanding the role of dietary patterns in optimizing health and reducing the risk of chronic disease across the lifespan is a high priority.2
Dietary patterns are the quantities, proportions, variety, or combination of different foods, beverages, and nutrients in diets as well as the frequency with which they are habitually consumed.3,4 Different approaches can be used to study dietary patterns. A priori methods are based on scientific consensus or evidence-based approaches and use scores that reflect the degree of adherence.5,6,7 A posteriori methods identify which factors explain the variation in patterns or aggregate individuals into groups with nonoverlapping patterns.8 Other approaches can include hybrid methods, clinical trials that assign consumption to a specific pattern, and/or observational studies on food avoidance (eg, vegetarian diets).
The 2015 committee reviewed the associations between dietary patterns and multiple outcomes, including cause-specific mortality from cardiovascular disease (CVD) and dementia.3 Other literature reviews have examined specific diets or foods and cause-specific mortality.9,10,11,12 In line with these studies, the 2020 committee,13 with support from the Nutrition Evidence Systematic Review (NESR) team of the US Department of Agriculture, conducted a systematic review of the literature to ascertain the association between dietary patterns consumed and all-cause mortality (ACM).
Methods
The systematic review question was, “what is the relationship between dietary patterns consumed and ACM?” It also addressed the topic of diets on the basis of macronutrient distribution. Presented in full detail elsewhere,14 the review used NESR systematic review methods, which are summarized herein. We followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline.
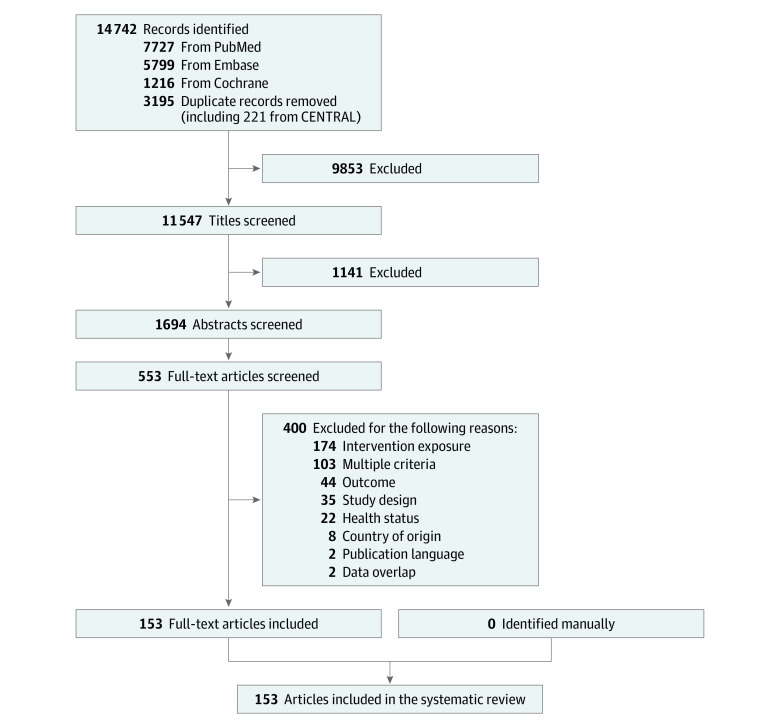
The committee developed a protocol, including an analytical framework (Figure 1) and inclusion and exclusion criteria (Table). The protocol was made available for public comment and was discussed by the committee in public meetings before evidence synthesis.
Figure 1. Analytic Framework for the Systematic Review Question .
This analytic framework visually represents the overall scope of the systematic review question and depicts the contributing elements that were examined and evaluated, including the target population, exposure, comparison, outcomes, and key confounders. Reproduced from the 2020 Dietary Guidelines Advisory Committee and Nutrition Evidence Systematic Review Team.14
Table. Inclusion and Exclusion Criteria for Relevant Articles That Examined Dietary Patterns and All-Cause Mortalitya.
| Category | Inclusion criteria | Exclusion criteria |
|---|---|---|
| Study design |
|
|
| Intervention/exposure |
|
|
| Comparator |
|
NA |
| Outcomes | Studies that reported ACM (ie, total mortality): the total number of deaths from all causes during a specific period | Studies that only reported cause-specific mortality (ie, total number of deaths from a specific disease, such as cardiovascular disease or cancer) |
| Date of publication | January 2000 to October 2019 | Articles published before January 2000 or after October 2019 |
| Publication status | Work that had been peer reviewed and published in peer-reviewed journals | Work that had not been peer reviewed and had not been published in peer-reviewed journals, including unpublished data, manuscripts, preprints, reports, abstracts, and conference proceedings |
| Language of publication | Published in English | Published in languages other than English |
| Country of origind | Conducted in countries ranked as high or higher human development | Conducted in countries ranked as medium or lower human development |
| Study participants |
|
|
| Age of study participants |
|
|
| Health status of study participants |
|
|
Abbreviations: ACM, all-cause mortality; AMDR, acceptable macronutrient distribution range; NA, not applicable.
Adapted from the 2020 Dietary Guidelines Advisory Committee and Nutrition Evidence Systematic Review Team.14
Data from Trumbo et al.15
Macronutrient percentage of energy outside of the AMDR were as follows: (1) carbohydrate for all age groups: <45% or >65% of energy; (2) protein for children aged 1-3 y: <5% or >20% of energy, protein for children aged 4-18 y: <10% or >30% of energy, protein for adults aged ≥19 y: <10% or >35% of energy; and (3) fat for children aged 1-3 y: <30% or >40% of energy, fat for children aged 4-18 y: <25% or >35% of energy, fat for adults aged ≥19 y: <20% or >35% of energy.
The classification for countries was based on the Human Development Index (HDI) from the year the study intervention occurred or data were collected.16 If the study did not report the year in which the intervention occurred or data were collected, the HDI classification for the year of publication was applied. HDI values were available from 1980 and then from 1990 to present. If a study was conducted before 1990, the HDI classification from 1990 was applied. If a study was conducted in 2018 or 2019, the most current HDI classification was applied. When a country was not included in the HDI ranking, the current country classification from the World Bank17 was used instead.
The NESR librarians developed and implemented literature searches in PubMed, the Cochrane Central Register of Controlled Trials, and Embase to identify articles that were published from January 1, 2000, to October 4, 2019.14 These studies evaluated dietary patterns and ACM in participants aged 2 years and older. Two NESR analysts independently screened the search results to identify articles that met the predetermined criteria (Table), and then they manually searched the reference lists of the included articles. The NESR staff extracted data from and completed 2 independent risk-of-bias assessments of each included article.
The 2020 committee synthesized the evidence qualitatively. The evidence was synthesized not by diet type or label but rather by similarities and differences in the foods and beverages that made up the dietary patterns that were examined. This synthesis approach was taken because the results of this systematic review were intended to inform dietary guidance and to allow for conclusions to be drawn regarding which dietary pattern components were most associated with risk of ACM.
The results of the systematic review were organized according to a dietary pattern approach (a priori, a posteriori, and other). Based on the synthesized evidence, the committee developed conclusion statements to answer the systematic review question and graded the strength of evidence for the conclusions as follows: strong, moderate, limited, or grade not assignable. Grades were assigned using the NESR’s predefined criteria for grading elements (risks of bias, consistency, directness, precision, and generalizability) and approach, which takes study design into consideration. Future research recommendations for strengthening the body of evidence were based on the gaps and limitations that were identified during the systematic review process.
Results
Study Characteristics
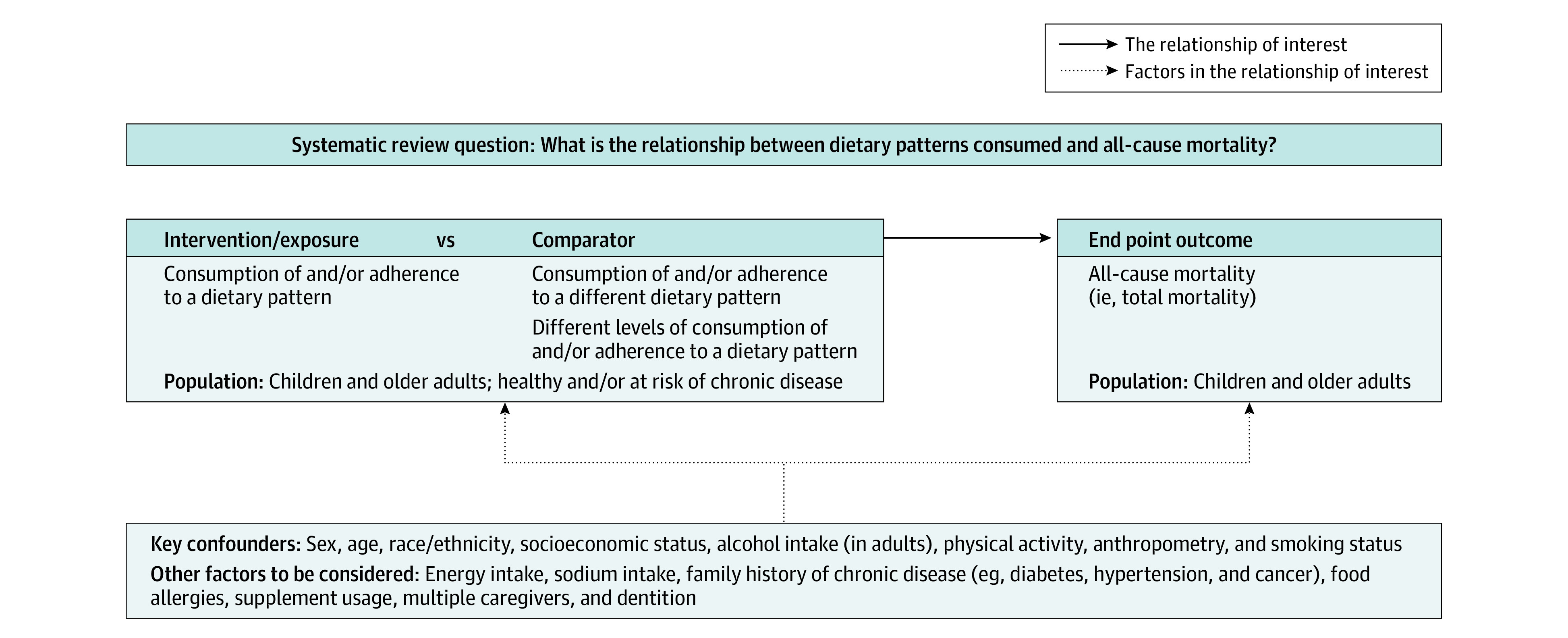
After dual screening, 11 547 relevant studies were identified. The body of evidence included 153 articles (involving 6 550 664 individuals), of which 1 was from a randomized clinical trial (RCT)18 and 152 were from observational studies19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166,167,168,169,170(Figure 2). Multiple articles used data from the same study but used different methods or represented unique subsamples or dietary patterns. Studies enrolled adults and older adults (aged 17-84 years at baseline) from 28 countries with a high or very high Human Development Index16 classification (Australia, Belgium, Canada, Czech Republic, Croatia, Denmark, Finland, France, Germany, Greece, Hong Kong, Hungary, Iran, Italy, Japan, Korea, Norway, Netherlands, Poland, Portugal, Russia, Serbia, Singapore, Spain, Sweden, Switzerland, United Kingdom, and United States). Fifty-three studies21,23,24,27,29,32,33,37,39,40,42,43,44,46,47,52,56,57,58,59,60,61,72,73,74,78,83,86,94,95,96,98,100,101,102,104,107,110,118,125,126,127,129,135,137,150,158,160,161,163,166 originated from the US. Some studies exclusively enrolled female 29,37,46,58,67,74,82,86,99,124,127,128,135,144,163 or male22,31,40,54,62,80,81,105,106,110,118,130,141,142,147,153 participants.
Figure 2. Literature Search and Screening Flowchart.
The literature search yielded 11 547 studies after the removal of duplicate articles. Dual screening resulted in the exclusion of 400 full-text articles or at least 1 reason, which may not reflect all possible reasons. The body of evidence included 153 articles.
The approaches for assessing dietary patterns included an RCT18; a priori methods, such as index or score analysis19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128; a posteriori methods, such as factor or cluster analysis29,36,56,93,109,129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146,147,148; and other methods,136,149,150,151,152,153,154,155,156,157,158 such as reduced rank regression and comparisons by animal product avoidance or ultraprocessed food consumption. eTable 1 in the Supplement describes the 185 dietary patterns that were examined. The ACM data were collected through validated methods (population-level registries, electronic databases, or medical or historical records) or active follow-up.
Evidence Synthesis
A Priori Studies
In the RCT, participants at high-risk for CVD were randomized to a Mediterranean diet with extra-virgin olive oil or mixed nuts or to a control diet.18 Consumption of either intervention diet was associated with reduced ACM risk after a median follow-up of 4.8 years. Results were similar in subanalyses, which removed participants with protocol deviations and randomization issues. Most included studies of dietary patterns (110 of 153 [72%])19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39 used index or score analysis. Many different measures were reported, including variations of Mediterranean diet (n = 31), DASH (Dietary Approaches to Stop Hypertension) diet scores (n = 1), country-specific indices (n = 16), Healthy Eating Index or Dietary Guidelines for Americans scores (n = 7), and other indices or scales (n = 24) (eTable 1 in the Supplement). A complete description of these components and the scoring procedures has been published elsewhere.14
Findings were consistent across the studies, despite the variety of indices or scores used (eTable 2 in the Supplement). Nutrient-dense dietary patterns, regardless of pattern label or name, were associated with significantly lower ACM risk. For example, all 12 comparisons that examined DASH diet scores suggested that higher adherence was associated with lower ACM risk,26,46,47,48,52,69,84,88,98,101,107,127 and 54 of the 63 comparisons that were reported in 44 articles that examined a Mediterranean-type index or score suggested that higher adherence was associated with lower ACM risk.24,25,30,32,34,35,46,47,48,49,50,51,52,53,63,64,68,69,71,76,79,81,83,88,97,98,104,106,107,108,111,112,113,114,115,116,117,122,123,124,125,127,128,141
A few articles reported nonsignificant results with similar patterns.21,31,33,36,39,42,62,93,102,110 Common elements of these dietary indices or scores were (1) relatively higher intake of vegetables (with or without potatoes); legumes; fruit; nuts; either whole grains specifically, cereals unspecified, or nonrefined grains; fish and/or seafood; lean meat or poultry, when included (Dietary Guidelines for Americans or Healthy Eating Index scores reflect total protein foods and/or ratio of white to red meat); and unsaturated fats vs saturated fats; and (2) relatively lower intake of red and processed meat and/or meat and meat products; refined grains; added sugars and/or sugar-sweetened beverages; solid fats, saturated fats, and/or trans fat; and excessive sodium.
Many of the indices considered alcoholic beverage intake in low to moderate amounts or within a threshold (eg, 10-25 g/d; 0.5-1.5 drinks/d for women and 0.5-2.0 drinks/d for men) as a positive component within the context of the entire dietary pattern. However, measurement and scoring procedures varied between indices.
The associations reported between a priori–derived dietary patterns and ACM remained in sensitivity or subgroup analyses after combining the dietary patterns with anthropometry, physical activity, and/or smoking status24,35,37,44,53,118; performing stratification or additional adjustment for anthropometry, sex, age, educational level, race/ethnicity, and/or smoking status25,34,37,46,47,52,76,83,85,86,87,95,96,98,99,104,111,113,115,119,125,126; excluding early deaths or the first few years of follow-up results25,35,49,57,58,63,65,72,76,82,96,99,111,112,113,119,125,128; accounting for chronic disease status (eg, diabetes or CVD28,30,34,37,51,58,64,65,71,72,80,96,111,125); or underreporting or misreporting chronic disease.28,34,106,112 When adherence to dietary patterns was combined with other healthier lifestyle factors (eg, not smoking and meeting recommended physical activity levels), stronger associations were typically observed. For example, participants who adhered to a Mediterranean diet met recommended physical activity recommendations, were long-term nonsmokers, and had a lower mortality risk (relative risk [RR], 0.65; 95% CI, 0.63-0.68) compared to those that only followed the Mediterranean diet (RR, 0.86; 95% CI, 0.83-0.88).24
A Posteriori Studies
Most of the 25 articles (19 [76%]) that examined dietary patterns by using factor or cluster analysis reported significantly lower ACM risk when comparing higher with lower adherence to the same derived pattern29,56,93,130,131,134,135,139,140,141,142,143,144,145,146,147,148 or to different patterns109,138 (eTable 2 in the Supplement). For example, participants with higher vs lower adherence to the Prudent pattern had lower mortality risk (Quintile 1: reference; Q2: RR, 0.85 [95% CI, 0.78-0.92; Q3: RR, 0.84 [95% CI, 0.78-0.91]; Q4: RR, 0.81 [95% CI, 0.74-0.88]; Q5: RR, 0.83 [95% CI, 0.76-0.90]; P for trend <.001).135 Participants with higher vs lower adherence to the Western pattern had higher mortality risk (Q1: reference; Q2: RR, 1.00 [95% CI, 0.92-1.08]; Q3: RR, 1.10 [95% CI, 1.02-1.20]; Q4: RR, 1.16 [95% CI, 1.06-1.26]; Q5: RR, 1.21 [95% CI, 1.12-1.32]; P for trend <.001).135 Dietary patterns were given different labels, such as healthy, prudent, and Mediterraneanlike, but were similarly characterized by higher intake of vegetables, fruits, fish or other seafood, legumes and/or whole grains, nuts, vegetable or olive oils, and/or poultry (eg, white meat, such as chicken or turkey140).
Several articles (5 of 25 [20%]) reported that the dietary patterns associated with significantly higher ACM risk (and/or shorter survival129,130,133,135,148) emphasized the following commonalities: higher intake of (1) meat and meat products such as beef, pork, sausage133; red meat and meat products130; red meat and processed meats135; fresh and processed meats and seafood148; (2) high-fat dairy products such as ice cream, cheese, and whole milk129; and/or (3) refined grains130,135 or flour-based foods such as pastries133 and/or sweets and desserts133,135,148 such as cake, cookies, chocolate, and candy129; as well as lower intake of (4) low-fat dairy products, rice and pasta, fruits, fish and other seafood, and dark green vegetables.129
Results were similar whether stratified by country,131 after excluding participants with CVD or cancer at baseline,147 or in models that accounted for co-twin pairs.133 Stratification by sex was inconsistent, with no significant associations in women only but significant associations in pooled analyses.138 For example, Krieger et al138 reported lower risk of ACM at mean follow-up of 25 years in overall analyses, with men and women pooled and when comparing fish (hazard ratio [HR], 0.87; 95% CI, 0.78-0.97) and traditional (HR, 0.89; 95% CI, 0.80-0.98) dietary patterns to the sausage and vegetables dietary pattern (reference; HR, 1.0). However, in the Krieger et al138 analyses, which were stratified by sex, the results in women only were not statistically significant: sausage and vegetables pattern (reference; HR, 1.0) was compared with meat and salad (HR, 0.93; 95% CI, 0.80-1.08), fish (HR, 0.98; 95% CI, 0.83-1.15), traditional (HR, 1.02; 95% CI, 0.87-1.19), and high-fiber foods (HR, 0.91; 95% CI, 0.79-1.05) patterns.
Nonsignificant associations were reported between a posteriori–derived dietary patterns and ACM, although the direction generally aligned with the significant results we have described, and may be attributed to smaller sample sizes,137 the sample evaluated,138 or the gradient between exposure comparisons.135
Other Studies
Dietary patterns that were derived from reduced rank regression showed inconsistent results (eTable 2 in the Supplement).136,150,153 Five articles examined the dietary patterns based on avoidance of animal-based products (eg, vegetarian diets).149,151,154,155,158 Vegetarian or plant-based patterns were associated with significantly lower ACM risk in 2 studies,155,158 but no significant associations were found in other exposure groups (eg, vegetarian vs pescovegetarian, and meat eaters vs vegetarian or vegan).149,151,154
Three studies reported that the dietary pattern of higher vs lower consumption of ultraprocessed foods was associated with higher ACM risk152,156,157 as defined by the fourth level of the NOVA Food Classification System. These patterns differed by the foods comprising the pattern (eg, some of which included highly palatable foods, such as ice cream and processed meats, and others included artificial flavors and texturizing agents), reducing the generalizability of these patterns and thus the results.
Assessment of Evidence
Most studies were conducted with rigorous methods and at low or moderate risks of bias across domains.14 Most studies accounted for potential confounders except for race/ethnicity, which was often homogenous or not reported. In addition, most studies assessed dietary intake once and were, therefore, at risk of bias because of potential changes in dietary patterns among participants over time. However, these studies used validated methods, and their results aligned with findings of studies that assessed diet over time. Several studies did not account for missing data, primarily diet or exposure data at baseline. Participants with implausible energy intake, incomplete dietary data, and/or a history or presence of chronic diseases or medical conditions at baseline were typically removed from the studies or analyses.
Dietary patterns that were examined with different approaches showed consistent direction and magnitude of associations with ACM. Precision was indicated by relatively narrow CIs between studies. Most studies did not report power analyses or sample size calculations but reported analytic sample sizes that were large enough to investigate the association, ranging from 161 participants68 to 451 256 participants.69 Total number of deaths ranged from 53 with approximately 4 years of total follow-up38 to 51 702 with approximately 13 to 18 years of follow-up.69 Although the incident number of deaths differed between studies, the number of events reported within groups confirmed precision across the body of evidence. The evidence base had directness and was generalizable to the US population. Results may be less generalizable to younger or less healthy populations. Results are likely generalizable to adults of various underreported racial/ethnic backgrounds, although it is difficult to ascertain exactly how race and/or ethnicity was involved in the association between dietary patterns and ACM because many studies did not report that information.
The 2020 committee used multiple databases to obtain publications from a large, comprehensive search. Most of the studies identified had large prospective cohorts, but smaller sample sizes were also included. Therefore, risk of publication bias was low. Details regarding how the NESR accounted for publication bias have been described elsewhere.13 Primary and secondary analyses were included from the PREDIMED (Prevención con Dieta Mediterránea) trial, which reported randomization issues.171 However, PREDIMED investigators republished the data after reanalysis and reconfirmed the initial findings.18
Discussion
Despite the different approaches, study designs, dietary assessment methods, geographical regions, and dietary pattern labels, the evidence demonstrated that dietary patterns associated with lower ACM risk were consistently characterized by higher intake of vegetables; legumes; fruits; nuts; either whole grains, cereals, or nonrefined grains; fish; and unsaturated vegetable oils. These patterns were also characterized by lower or no consumption of animal products (red and processed meat, meat and meat products, and high-fat dairy products), refined grains, and sweets (ie, higher in added sugars). Labels that were assigned to the dietary patterns varied widely (eg, Mediterranean, prudent, Healthy Eating Index, DASH, and plant-based), highlighting that high-quality diets with nutrient-dense foods are associated with better health, regardless of diet type or dietary pattern name. Although we believe this systematic review is the most comprehensive examination of US dietary patterns and ACM that is currently available, its findings align with the results of previous meta-analyses that focused on select diet types and/or cause-specific mortality.9,10,11,12,172
This systematic review included the most suitable study designs available to answer the question. Given the nature of the outcome (ACM), expense, duration, and power necessary for an experimental study design to explore this question, it is unlikely that many RCTs or non-RCTs would be available (funded, conducted, or published) for consideration. Studies that were included for this review were well designed and conducted using rigorous methods. Despite the preponderance of evidence from observational studies, this review presented a conclusion statement that was assigned a grade of strong, which was in accordance with studies at generally low or moderate risks of bias and with high consistency in direction and magnitude of findings, precision, directness, and generalizability. The methods used for grading the evidence underlying this conclusion statement align with other grading approaches173,174,175 and ensure that strengths and weaknesses in study design as well as each grading element were considered.176
The findings of this review are further supported by a central tenet behind other works of the 2020 committee: a nutrient-dense dietary pattern can minimize the risk of multiple diet-related chronic diseases, such as CVD, obesity, diabetes, and some cancers, and can support bone and neurocognitive health.176,177 For women who are pregnant, a similar healthful dietary pattern has been associated with lower risk of poor maternal-fetal outcomes.178 Achieving a healthy dietary pattern at each life stage should also support health in subsequent life stages. The core elements of these dietary patterns across the committee’s reviews reflect higher diet quality, are appropriate to consume across the lifespan, and have the potential to substantially minimize chronic disease risk and mortality risk.
Studies in this review suggested that dietary patterns containing nutrient-dense foods and alcoholic beverages that were within a given threshold or at low to moderate levels were associated with lower risk of ACM. However, the preponderance of this evidence varied in the methodological assessment of alcohol intake and scoring procedures within the context of the dietary patterns that were assessed. The committee conducted a separate systematic review179 to answer the question, what is the association between alcoholic beverages and ACM? Briefly, the focused analysis on alcoholic beverage consumption suggested that alcohol may increase ACM risk, but only minimally at low levels of intake. The committee concluded that moderating alcohol consumption to lower levels is recommended to better protect health. Other recommendations that were incorporated into the Dietary Guidelines for Americans, 2020-2025 were for individuals to not start drinking, avoid heavy drinking, and proceed with caution regarding alcoholic beverage consumption because it can contribute to increased rates of liver disease180 and excess energy intake, which is not advisable.
Dietary patterns provide a meaningful and interpretable database on foods and food groups. This review found that multiple food choices can be made toward a healthy diet that promotes beneficial outcomes. Dietary pattern approaches are advantageous because they place an emphasis on the combination of foods and beverages that meet total energy needs and are associated with health, instead of the selection of specific nutrients or foods alone, which may be more difficult for consumers to translate into a total diet. We believe such an approach provides flexibility, allowing consumers the freedom to tailor food and food group combinations that were identified as healthful to their preferences (eg, cultural acceptability and taste) and needs (eg, cost).
Limitations
This study has several limitations. Observing study participants over time provides valuable insights regarding risk for mortality, although many included studies examined diet at only 1 time point (ie, baseline), which may or may not reflect usual dietary patterns. Most of the available evidence on dietary patterns was derived from studies that were conducted in adults. Data on dietary patterns earlier in the life course and ACM were unavailable. However, this lack of data was likely associated with the challenge and expense of undertaking long-term RCTs and/or studies with repeated measures over time, particularly starting in childhood, that examine mortality as an outcome. As a result, longitudinal data, particularly information on dietary patterns from childhood and continuing throughout the life course, are still greatly needed. Further exploration is also needed on the factors that modify or mediate the association between dietary patterns and ACM as well as the role that selected food groups, such as meat, plays in this association. In addition, the available evidence does not identify the inadequate or excessive intake or quantify the types and amounts of foods and food groups consumed in the context of dietary patterns.
Active ongoing cohorts informed most of the findings reported herein, which showed consistency across the US and more than 20 other middle- to high-income countries. Results indicated good external validity, but future work is needed within population subgroups that could not be analyzed in this review because of the lack of reported details on individuals from racial/ethnic minority groups. The available evidence was not sufficient to assess how race/ethnicity affects the association between dietary patterns and ACM. In addition, this systematic review was conducted to identify the nature and direction of the association between dietary patterns and ACM, with an intention to consider dietary patterns regardless of label, name, or type. Because of this comprehensive approach, the methodological heterogeneity of the dietary patterns included in this review was best suited for qualitative synthesis of quantitative data. However, in the future, it may be worth exploring whether and how the magnitude of these findings could be quantified through a meta-analysis.
Conclusions
Evidence from this systematic review by the 2020 Dietary Guidelines Advisory Committee demonstrated that nutrient-dense dietary patterns, which were characterized by higher intake of vegetables, fruits, legumes, nuts, whole grains, unsaturated vegetable oils, fish, and lean meat or poultry, when included, were associated with decreased ACM risk in broadly generalizable populations of adults and older adults. These dietary patterns included relatively lower intake of red and processed meat, high-fat dairy, and refined carbohydrates or sweets. Some of these dietary patterns also included moderate intake of alcoholic beverages. Results based on additional analyses with confounding factors generally confirmed the robustness of the main findings.
eTable 1. Description of All Dietary Patterns Examined in Relation to All-Cause Mortality Outcomes in All Included Articles
eTable 2. Results by All Included Articles for Dietary Pattern and All-Cause Mortality (ACM) Analyses
eReferences.
References
- 1.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13(1):3-9. doi: 10.1097/00041433-200202000-00002 [DOI] [PubMed] [Google Scholar]
- 2.US Department of Health & Human Services, National Institutes of Health . 2020-2030 Strategic plan for NIH Nutrition Research. Accessed May 12, 2020. https://www.niddk.nih.gov/about-niddk/strategic-plans-reports/strategic-plan-nih-nutrition-research
- 3.US Department of Agriculture, Agricultural Research Service, Dietary Guidelines Advisory Committee. Scientific report of the 2015 Dietary Guidelines Advisory Committee : advisory report to the Secretary of Health and Human Services and the Secretary of Agriculture. Published 2015. Accessed June 25, 2020. https://health.gov/sites/default/files/2019-09/Scientific-Report-of-the-2015-Dietary-Guidelines-Advisory-Committee.pdf
- 4.US Department of Agriculture, Center for Nutrition Policy and Promotion, Nutrition Evidence Library, Dietary Patterns Technical Expert Collaborative . A series of systematic reviews on the relationship between dietary patterns and health outcomes. Published 2014. Accessed May 12, 2020. https://nesr.usda.gov/sites/default/files/2019-06/DietaryPatternsReport-FullFinal2.pdf
- 5.Schulze MB, Hoffmann K. Methodological approaches to study dietary patterns in relation to risk of coronary heart disease and stroke. Br J Nutr. 2006;95(5):860-869. doi: 10.1079/BJN20061731 [DOI] [PubMed] [Google Scholar]
- 6.Schulze MB, Martínez-González MA, Fung TT, Lichtenstein AH, Forouhi NG. Food based dietary patterns and chronic disease prevention. BMJ. 2018;361:k2396. doi: 10.1136/bmj.k2396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reedy J, Wirfält E, Flood A, et al. Comparing 3 dietary pattern methods—cluster analysis, factor analysis, and index analysis—with colorectal cancer risk: the NIH-AARP Diet and Health Study. Am J Epidemiol. 2010;171(4):479-487. doi: 10.1093/aje/kwp393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Edefonti V, De Vito R, Dalmartello M, Patel L, Salvatori A, Ferraroni M. Reproducibility and validity of a posteriori dietary patterns: a systematic review. Adv Nutr. 2020;11(2):293-326. doi: 10.1093/advances/nmz097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Becerra-Tomás N, Blanco Mejía S, Viguiliouk E, et al. Mediterranean diet, cardiovascular disease and mortality in diabetes: a systematic review and meta-analysis of prospective cohort studies and randomized clinical trials. Crit Rev Food Sci Nutr. 2020;60(7):1207-1227. doi: 10.1080/10408398.2019.1565281 [DOI] [PubMed] [Google Scholar]
- 10.Eleftheriou D, Benetou V, Trichopoulou A, La Vecchia C, Bamia C. Mediterranean diet and its components in relation to all-cause mortality: meta-analysis. Br J Nutr. 2018;120(10):1081-1097. doi: 10.1017/S0007114518002593 [DOI] [PubMed] [Google Scholar]
- 11.Hlaing-Hlaing H, Pezdirc K, Tavener M, James EL, Hure A. Diet quality indices used in Australian and New Zealand adults: a systematic review and critical appraisal. Nutrients. 2020;12(12):E3777. doi: 10.3390/nu12123777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soltani S, Jayedi A, Shab-Bidar S, Becerra-Tomás N, Salas-Salvadó J. Adherence to the Mediterranean diet in relation to all-cause mortality: a systematic review and dose-response meta-analysis of prospective cohort studies. Adv Nutr. 2019;10(6):1029-1039. doi: 10.1093/advances/nmz041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.US Department of Agriculture, Agricultural Research Service, Dietary Guidelines Advisory Committee. Scientific report of the 2020 Dietary Guidelines Advisory Committee : advisory report to the Secretary of Health and Human Services and the Secretary of Agriculture. Accessed January 27, 2020. https://www.dietaryguidelines.gov/sites/default/files/2020-07/ScientificReport_of_the_2020DietaryGuidelinesAdvisoryCommittee_first-print.pdf
- 14.US Department of Agriculture . Nutrition Evidence Systematic Review. Systematic review question: what is the relationship between dietary patterns consumed and all-cause mortality? Conclusion statement. Accessed July 27, 2021. https://nesr.usda.gov/2020-dietary-guidelines-advisory-committee-systematic-reviews
- 15.Trumbo P, Schlicker S, Yates AA, Poos M; Food and Nutrition Board of the Institute of Medicine, The National Academies . Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc. 2002;102(11):1621-1630. doi: 10.1016/S0002-8223(02)90346-9 [DOI] [PubMed] [Google Scholar]
- 16.United Nations Development Programme, Human Development Reports. Human Development Index 1990-2017. Accessed January 27, 2020. http://hdr.undp.org/en/data
- 17.The World Bank . World Bank country and lending groups. Accessed February 2020. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-country-and-lending-groups
- 18.Estruch R, Ros E, Salas-Salvadó J, et al. ; PREDIMED Study Investigators . Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25):e34. doi: 10.1056/NEJMoa1800389 [DOI] [PubMed] [Google Scholar]
- 19.Abe S, Zhang S, Tomata Y, Tsuduki T, Sugawara Y, Tsuji I. Japanese diet and survival time: the Ohsaki cohort 1994 study. Clin Nutr. 2020;39(1):298-303. doi: 10.1016/j.clnu.2019.02.010 [DOI] [PubMed] [Google Scholar]
- 20.Akbaraly TN, Ferrie JE, Berr C, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr. 2011;94(1):247-253. doi: 10.3945/ajcn.111.013128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Rifai M, Greenland P, Blaha MJ, et al. Factors of health in the protection against death and cardiovascular disease among adults with subclinical atherosclerosis. Am Heart J. 2018;198:180-188. doi: 10.1016/j.ahj.2017.10.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. High diet quality is associated with a lower risk of cardiovascular disease and all-cause mortality in older men. J Nutr. 2014;144(5):673-680. doi: 10.3945/jn.113.186486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baden MY, Liu G, Satija A, et al. Changes in plant-based diet quality and total and cause-specific mortality. Circulation. 2019;140(12):979-991. doi: 10.1161/CIRCULATIONAHA.119.041014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Behrens G, Fischer B, Kohler S, Park Y, Hollenbeck AR, Leitzmann MF. Healthy lifestyle behaviors and decreased risk of mortality in a large prospective study of U.S. women and men. Eur J Epidemiol. 2013;28(5):361-372. doi: 10.1007/s10654-013-9796-9 [DOI] [PubMed] [Google Scholar]
- 25.Bellavia A, Tektonidis TG, Orsini N, Wolk A, Larsson SC. Quantifying the benefits of Mediterranean diet in terms of survival. Eur J Epidemiol. 2016;31(5):527-530. doi: 10.1007/s10654-016-0127-9 [DOI] [PubMed] [Google Scholar]
- 26.Biesbroek S, Verschuren WMM, Boer JMA, et al. Does a better adherence to dietary guidelines reduce mortality risk and environmental impact in the Dutch sub-cohort of the European Prospective Investigation into Cancer and Nutrition? Br J Nutr. 2017;118(1):69-80. doi: 10.1017/S0007114517001878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bittoni MA, Wexler R, Spees CK, Clinton SK, Taylor CA. Lack of private health insurance is associated with higher mortality from cancer and other chronic diseases, poor diet quality, and inflammatory biomarkers in the United States. Prev Med. 2015;81:420-426. doi: 10.1016/j.ypmed.2015.09.016 [DOI] [PubMed] [Google Scholar]
- 28.Bo S, Ponzo V, Goitre I, et al. Predictive role of the Mediterranean diet on mortality in individuals at low cardiovascular risk: a 12-year follow-up population-based cohort study. J Transl Med. 2016;14:91. doi: 10.1186/s12967-016-0851-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boggs DA, Ban Y, Palmer JR, Rosenberg L. Higher diet quality is inversely associated with mortality in African-American women. J Nutr. 2015;145(3):547-554. doi: 10.3945/jn.114.195735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bonaccio M, Di Castelnuovo A, Costanzo S, et al. Mediterranean diet and mortality in the elderly: a prospective cohort study and a meta-analysis. Br J Nutr. 2018;120(8):841-854. doi: 10.1017/S0007114518002179 [DOI] [PubMed] [Google Scholar]
- 31.Bongard V, Arveiler D, Dallongeville J, et al. Food groups associated with a reduced risk of 15-year all-cause death. Eur J Clin Nutr. 2016;70(6):715-722. doi: 10.1038/ejcn.2016.19 [DOI] [PubMed] [Google Scholar]
- 32.Booth JN III, Colantonio LD, Howard G, et al. Healthy lifestyle factors and incident heart disease and mortality in candidates for primary prevention with statin therapy. Int J Cardiol. 2016;207:196-202. doi: 10.1016/j.ijcard.2016.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown JC, Harhay MO, Harhay MN. Physical activity, diet quality, and mortality among community-dwelling prefrail and frail older adults. J Nutr Gerontol Geriatr. 2016;35(4):253-266. doi: 10.1080/21551197.2016.1247022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Buckland G, Agudo A, Travier N, et al. Adherence to the Mediterranean diet reduces mortality in the Spanish cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Spain). Br J Nutr. 2011;106(10):1581-1591. doi: 10.1017/S0007114511002078 [DOI] [PubMed] [Google Scholar]
- 35.Cárdenas-Fuentes G, Subirana I, Martinez-Gonzalez MA, et al. Multiple approaches to associations of physical activity and adherence to the Mediterranean diet with all-cause mortality in older adults: the Prevención con Dieta Mediterránea study. Eur J Nutr. 2019;58(4):1569-1578. doi: 10.1007/s00394-018-1689-y [DOI] [PubMed] [Google Scholar]
- 36.Chan RSM, Yu BWM, Leung J, et al. How dietary patterns are related to inflammaging and mortality in community-dwelling older Chinese adults in Hong Kong - a prospective analysis. J Nutr Health Aging. 2019;23(2):181-194. doi: 10.1007/s12603-018-1143-0 [DOI] [PubMed] [Google Scholar]
- 37.Cheng E, Um CY, Prizment A, Lazovich D, Bostick RM. Associations of evolutionary-concordance diet, Mediterranean diet and evolutionary-concordance lifestyle pattern scores with all-cause and cause-specific mortality. Br J Nutr. 2018;1-10. doi: 10.1017/S0007114518003483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chrysohoou C, Pitsavos C, Lazaros G, Skoumas J, Tousoulis D, Stefanadis C; Ikaria Study Investigators . Determinants of all-cause mortality and incidence of cardiovascular disease (2009 to 2013) in older adults: the Ikaria Study of the Blue Zones. Angiology. 2016;67(6):541-548. doi: 10.1177/0003319715603185 [DOI] [PubMed] [Google Scholar]
- 39.Cuenca-García M, Artero EG, Sui X, Lee DC, Hebert JR, Blair SN. Dietary indices, cardiovascular risk factors and mortality in middle-aged adults: findings from the Aerobics Center Longitudinal Study. Ann Epidemiol. 2014;24(4):297-303.e2. doi: 10.1016/j.annepidem.2014.01.007 [DOI] [PubMed] [Google Scholar]
- 40.Dai J, Krasnow RE, Reed T. Midlife moderation-quantified healthy diet and 40-year mortality risk from CHD: the prospective National Heart, Lung, and Blood Institute Twin Study. Br J Nutr. 2016;116(2):326-334. doi: 10.1017/S0007114516001914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Drake I, Gullberg B, Sonestedt E, et al. Scoring models of a diet quality index and the predictive capability of mortality in a population-based cohort of Swedish men and women. Public Health Nutr. 2013;16(3):468-478. doi: 10.1017/S1368980012002789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ford DW, Hartman TJ, Still C, et al. Body mass index, poor diet quality, and health-related quality of life are associated with mortality in rural older adults. J Nutr Gerontol Geriatr. 2014;33(1):23-34. doi: 10.1080/21551197.2014.875819 [DOI] [PubMed] [Google Scholar]
- 43.Ford ES, Bergmann MM, Boeing H, Li C, Capewell S. Healthy lifestyle behaviors and all-cause mortality among adults in the United States. Prev Med. 2012;55(1):23-27. doi: 10.1016/j.ypmed.2012.04.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ford ES, Zhao G, Tsai J, Li C. Low-risk lifestyle behaviors and all-cause mortality: findings from the National Health and Nutrition Examination Survey III Mortality Study. Am J Public Health. 2011;101(10):1922-1929. doi: 10.2105/AJPH.2011.300167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fresán U, Sabaté J, Martínez-Gonzalez MA, Segovia-Siapco G, de la Fuente-Arrillaga C, Bes-Rastrollo M. Adherence to the 2015 Dietary Guidelines for Americans and mortality risk in a Mediterranean cohort: the SUN project. Prev Med. 2019;118:317-324. doi: 10.1016/j.ypmed.2018.11.015 [DOI] [PubMed] [Google Scholar]
- 46.George SM, Ballard-Barbash R, Manson JE, et al. Comparing indices of diet quality with chronic disease mortality risk in postmenopausal women in the Women’s Health Initiative Observational Study: evidence to inform national dietary guidance. Am J Epidemiol. 2014;180(6):616-625. doi: 10.1093/aje/kwu173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Harmon BE, Boushey CJ, Shvetsov YB, et al. Associations of key diet-quality indexes with mortality in the multiethnic cohort: the Dietary Patterns Methods Project. Am J Clin Nutr. 2015;101(3):587-597. doi: 10.3945/ajcn.114.090688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hashemian M, Farvid MS, Poustchi H, et al. The application of six dietary scores to a Middle Eastern population: a comparative analysis of mortality in a prospective study. Eur J Epidemiol. 2019;34(4):371-382. doi: 10.1007/s10654-019-00508-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Haveman-Nies A, de Groot L, Burema J, Cruz JA, Osler M, van Staveren WA; SENECA Investigators . Dietary quality and lifestyle factors in relation to 10-year mortality in older Europeans: the SENECA study. Am J Epidemiol. 2002;156(10):962-968. doi: 10.1093/aje/kwf144 [DOI] [PubMed] [Google Scholar]
- 50.Hodge AM, Bassett JK, Dugué PA, et al. Dietary inflammatory index or Mediterranean diet score as risk factors for total and cardiovascular mortality. Nutr Metab Cardiovasc Dis. 2018;28(5):461-469. doi: 10.1016/j.numecd.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hodge AM, English DR, Itsiopoulos C, O’Dea K, Giles GG. Does a Mediterranean diet reduce the mortality risk associated with diabetes: evidence from the Melbourne collaborative cohort study. Nutr Metab Cardiovasc Dis. 2011;21(9):733-739. doi: 10.1016/j.numecd.2010.10.014 [DOI] [PubMed] [Google Scholar]
- 52.Hu EA, Steffen LM, Coresh J, Appel LJ, Rebholz CM. Adherence to the Healthy Eating Index-2015 and other dietary patterns may reduce risk of cardiovascular disease, cardiovascular mortality, and all-cause mortality. J Nutr. 2020;150(2):312-321. doi: 10.1093/jn/nxz218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hulsegge G, Looman M, Smit HA, Daviglus ML, van der Schouw YT, Verschuren WM. Lifestyle changes in young adulthood and middle age and risk of cardiovascular disease and all-cause mortality: the Doetinchem cohort study. J Am Heart Assoc. 2016;5(1):e002432. doi: 10.1161/JAHA.115.002432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kaluza J, Håkansson N, Brzozowska A, Wolk A. Diet quality and mortality: a population-based prospective study of men. Eur J Clin Nutr. 2009;63(4):451-457. doi: 10.1038/sj.ejcn.1602968 [DOI] [PubMed] [Google Scholar]
- 55.Kaluza J, Håkansson N, Harris HR, Orsini N, Michaëlsson K, Wolk A. Influence of anti-inflammatory diet and smoking on mortality and survival in men and women: two prospective cohort studies. J Intern Med. 2019;285(1):75-91. doi: 10.1111/joim.12823 [DOI] [PubMed] [Google Scholar]
- 56.Kant AK, Graubard BI, Schatzkin A. Dietary patterns predict mortality in a national cohort: the National Health Interview Surveys, 1987 and 1992. J Nutr. 2004;134(7):1793-1799. doi: 10.1093/jn/134.7.1793 [DOI] [PubMed] [Google Scholar]
- 57.Kant AK, Leitzmann MF, Park Y, Hollenbeck A, Schatzkin A. Patterns of recommended dietary behaviors predict subsequent risk of mortality in a large cohort of men and women in the United States. J Nutr. 2009;139(7):1374-1380. doi: 10.3945/jn.109.104505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kant AK, Schatzkin A, Graubard BI, Schairer C. A prospective study of diet quality and mortality in women. JAMA. 2000;283(16):2109-2115. doi: 10.1001/jama.283.16.2109 [DOI] [PubMed] [Google Scholar]
- 59.Kappeler R, Eichholzer M, Rohrmann S. Meat consumption and diet quality and mortality in NHANES III. Eur J Clin Nutr. 2013;67(6):598-606. doi: 10.1038/ejcn.2013.59 [DOI] [PubMed] [Google Scholar]
- 60.Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Coresh J, Rebholz CM. Plant-based diets are associated with a lower risk of incident cardiovascular disease, cardiovascular disease mortality, and all-cause mortality in a general population of middle-aged adults. J Am Heart Assoc. 2019;8(16):e012865. doi: 10.1161/JAHA.119.012865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kim H, Caulfield LE, Rebholz CM. Healthy plant-based diets are associated with lower risk of all-cause mortality in US adults. J Nutr. 2018;148(4):624-631. doi: 10.1093/jn/nxy019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kim JY, Ko YJ, Rhee CW, et al. Cardiovascular health metrics and all-cause and cardiovascular disease mortality among middle-aged men in Korea: the Seoul male cohort study. J Prev Med Public Health. 2013;46(6):319-328. doi: 10.3961/jpmph.2013.46.6.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Knoops KT, de Groot LC, Kromhout D, et al. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: the HALE project. JAMA. 2004;292(12):1433-1439. doi: 10.1001/jama.292.12.1433 [DOI] [PubMed] [Google Scholar]
- 64.Knoops KT, Groot de LC, Fidanza F, Alberti-Fidanza A, Kromhout D, van Staveren WA. Comparison of three different dietary scores in relation to 10-year mortality in elderly European subjects: the HALE project. Eur J Clin Nutr. 2006;60(6):746-755. doi: 10.1038/sj.ejcn.1602378 [DOI] [PubMed] [Google Scholar]
- 65.Kurotani K, Akter S, Kashino I, et al. ; Japan Public Health Center based Prospective Study Group . Quality of diet and mortality among Japanese men and women: Japan Public Health Center based prospective study. BMJ. 2016;352:i1209. doi: 10.1136/bmj.i1209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kurotani K, Honjo K, Nakaya T, et al. ; Japan Public Health Center-based Prospective Study Group . Diet quality affects the association between census-based neighborhood deprivation and all-cause mortality in Japanese men and women: the Japan Public Health Center-Based Prospective Study. Nutrients. 2019;11(9):E2194. doi: 10.3390/nu11092194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lagiou P, Trichopoulos D, Sandin S, et al. Mediterranean dietary pattern and mortality among young women: a cohort study in Sweden. Br J Nutr. 2006;96(2):384-392. doi: 10.1079/BJN20061824 [DOI] [PubMed] [Google Scholar]
- 68.Lasheras C, Fernandez S, Patterson AM. Mediterranean diet and age with respect to overall survival in institutionalized, nonsmoking elderly people. Am J Clin Nutr. 2000;71(4):987-992. doi: 10.1093/ajcn/71.4.987 [DOI] [PubMed] [Google Scholar]
- 69.Lassale C, Gunter MJ, Romaguera D, et al. Diet quality scores and prediction of all-cause, cardiovascular and cancer mortality in a Pan-European cohort study. PLoS One. 2016;11(7):e0159025. doi: 10.1371/journal.pone.0159025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lim J, Lee Y, Shin S, et al. An association between Diet Quality Index for Koreans (DQI-K) and total mortality in Health Examinees Gem (HEXA-G) study. Nutr Res Pract. 2018;12(3):258-264. doi: 10.4162/nrp.2018.12.3.258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Limongi F, Noale M, Gesmundo A, Crepaldi G, Maggi S. Adherence to the Mediterranean diet and all-cause mortality risk in an elderly Italian population: data from the ILSA Study. J Nutr Health Aging. 2017;21(5):505-513. doi: 10.1007/s12603-016-0808-9 [DOI] [PubMed] [Google Scholar]
- 72.Liu YH, Gao X, Mitchell DC, Wood GC, Still CD, Jensen GL. Diet quality is associated with mortality in adults aged 80 years and older: a prospective study. J Am Geriatr Soc. 2019;67(10):2180-2185. doi: 10.1111/jgs.16089 [DOI] [PubMed] [Google Scholar]
- 73.Loprinzi PD, Addoh O, Mann JR. Association between dietary behavior and mortality among American adults with mobility limitations. Disabil Health J. 2018;11(1):126-129. doi: 10.1016/j.dhjo.2017.05.006 [DOI] [PubMed] [Google Scholar]
- 74.Mai V, Kant AK, Flood A, Lacey JV Jr, Schairer C, Schatzkin A. Diet quality and subsequent cancer incidence and mortality in a prospective cohort of women. Int J Epidemiol. 2005;34(1):54-60. doi: 10.1093/ije/dyh388 [DOI] [PubMed] [Google Scholar]
- 75.Martínez-Gómez D, Guallar-Castillón P, León-Muñoz LM, López-García E, Rodríguez-Artalejo F. Combined impact of traditional and non-traditional health behaviors on mortality: a national prospective cohort study in Spanish older adults. BMC Med. 2013;11:47. doi: 10.1186/1741-7015-11-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Martínez-González MA, Guillén-Grima F, De Irala J, et al. The Mediterranean diet is associated with a reduction in premature mortality among middle-aged adults. J Nutr. 2012;142(9):1672-1678. doi: 10.3945/jn.112.162891 [DOI] [PubMed] [Google Scholar]
- 77.Martínez-González MA, Sánchez-Tainta A, Corella D, et al. ; PREDIMED Group . A provegetarian food pattern and reduction in total mortality in the Prevención con Dieta Mediterránea (PREDIMED) study. Am J Clin Nutr. 2014;100(suppl 1):320S-328S. doi: 10.3945/ajcn.113.071431 [DOI] [PubMed] [Google Scholar]
- 78.McCullough ML, Patel AV, Kushi LH, et al. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20(6):1089-1097. doi: 10.1158/1055-9965.EPI-10-1173 [DOI] [PubMed] [Google Scholar]
- 79.McNaughton SA, Bates CJ, Mishra GD. Diet quality is associated with all-cause mortality in adults aged 65 years and older. J Nutr. 2012;142(2):320-325. doi: 10.3945/jn.111.148692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Menotti A, Alberti-Fidanza A, Fidanza F, Lanti M, Fruttini D. Factor analysis in the identification of dietary patterns and their predictive role in morbid and fatal events. Public Health Nutr. 2012;15(7):1232-1239. doi: 10.1017/S1368980011003235 [DOI] [PubMed] [Google Scholar]
- 81.Menotti A, Kromhout D, Puddu PE, et al. Baseline fatty acids, food groups, a diet score and 50-year all-cause mortality rates: an ecological analysis of the Seven Countries Study. Ann Med. 2017;49(8):718-727. doi: 10.1080/07853890.2017.1372622 [DOI] [PubMed] [Google Scholar]
- 82.Michels KB, Wolk A. A prospective study of variety of healthy foods and mortality in women. Int J Epidemiol. 2002;31(4):847-854. doi: 10.1093/ije/31.4.847 [DOI] [PubMed] [Google Scholar]
- 83.Mitrou PN, Kipnis V, Thiébaut AC, et al. Mediterranean dietary pattern and prediction of all-cause mortality in a US population: results from the NIH-AARP Diet and Health Study. Arch Intern Med. 2007;167(22):2461-2468. doi: 10.1001/archinte.167.22.2461 [DOI] [PubMed] [Google Scholar]
- 84.Mokhtari Z, Sharafkhah M, Poustchi H, et al. Adherence to the Dietary Approaches to Stop Hypertension (DASH) diet and risk of total and cause-specific mortality: results from the Golestan cohort study. Int J Epidemiol. 2019;48(6):1824-1838. doi: 10.1093/ije/dyz079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Muller DC, Murphy N, Johansson M, et al. Modifiable causes of premature death in middle-age in Western Europe: results from the EPIC cohort study. BMC Med. 2016;14:87. doi: 10.1186/s12916-016-0630-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mursu J, Steffen LM, Meyer KA, Duprez D, Jacobs DR Jr. Diet quality indexes and mortality in postmenopausal women: the Iowa Women’s Health Study. Am J Clin Nutr. 2013;98(2):444-453. doi: 10.3945/ajcn.112.055681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nakamura Y, Ueshima H, Okamura T, et al. ; National Integrated Project for Prospective Observation of Non-Communicable Diseases and its Trends in the Aged, 1980 Research Group . A Japanese diet and 19-year mortality: national integrated project for prospective observation of non-communicable diseases and its trends in the aged, 1980. Br J Nutr. 2009;101(11):1696-1705. doi: 10.1017/S0007114508111503 [DOI] [PubMed] [Google Scholar]
- 88.Neelakantan N, Koh WP, Yuan JM, van Dam RM. Diet-quality indexes are associated with a lower risk of cardiovascular, respiratory, and all-cause mortality among Chinese adults. J Nutr. 2018;148(8):1323-1332. doi: 10.1093/jn/nxy094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nilsson LM, Winkvist A, Brustad M, et al. A traditional Sami diet score as a determinant of mortality in a general northern Swedish population. Int J Circumpolar Health. 2012;71(0):1-12. doi: 10.3402/ijch.v71i0.18537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Oba S, Nagata C, Nakamura K, et al. Diet based on the Japanese Food Guide Spinning Top and subsequent mortality among men and women in a general Japanese population. J Am Diet Assoc. 2009;109(9):1540-1547. doi: 10.1016/j.jada.2009.06.367 [DOI] [PubMed] [Google Scholar]
- 91.Okada E, Nakamura K, Ukawa S, et al. The Japanese food score and risk of all-cause, CVD and cancer mortality: the Japan collaborative cohort study. Br J Nutr. 2018;120(4):464-471. doi: 10.1017/S000711451800154X [DOI] [PubMed] [Google Scholar]
- 92.Olsen A, Egeberg R, Halkjær J, Christensen J, Overvad K, Tjønneland A. Healthy aspects of the Nordic diet are related to lower total mortality. J Nutr. 2011;141(4):639-644. doi: 10.3945/jn.110.131375 [DOI] [PubMed] [Google Scholar]
- 93.Osler M, Heitmann BL, Høidrup S, Jørgensen LM, Schroll M. Food intake patterns, self rated health and mortality in Danish men and women: a prospective observational study. J Epidemiol Community Health. 2001;55(6):399-403. doi: 10.1136/jech.55.6.399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Panizza CE, Shvetsov YB, Harmon BE, et al. Testing the predictive validity of the Healthy Eating Index-2015 in the multiethnic cohort: is the score associated with a reduced risk of all-cause and cause-specific mortality? Nutrients. 2018;10(4):E452. doi: 10.3390/nu10040452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Park YM, Steck SE, Fung TT, et al. Mediterranean diet and mortality risk in metabolically healthy obese and metabolically unhealthy obese phenotypes. Int J Obes (Lond). 2016;40(10):1541-1549. doi: 10.1038/ijo.2016.114 [DOI] [PubMed] [Google Scholar]
- 96.Park YM, Fung TT, Steck SE, et al. Diet quality and mortality risk in metabolically obese normal-weight adults. Mayo Clin Proc. 2016;91(10):1372-1383. doi: 10.1016/j.mayocp.2016.06.022 [DOI] [PubMed] [Google Scholar]
- 97.Prinelli F, Yannakoulia M, Anastasiou CA, et al. Mediterranean diet and other lifestyle factors in relation to 20-year all-cause mortality: a cohort study in an Italian population. Br J Nutr. 2015;113(6):1003-1011. doi: 10.1017/S0007114515000318 [DOI] [PubMed] [Google Scholar]
- 98.Reedy J, Krebs-Smith SM, Miller PE, et al. Higher diet quality is associated with decreased risk of all-cause, cardiovascular disease, and cancer mortality among older adults. J Nutr. 2014;144(6):881-889. doi: 10.3945/jn.113.189407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Roswall N, Sandin S, Löf M, et al. Adherence to the Healthy Nordic Food Index and total and cause-specific mortality among Swedish women. Eur J Epidemiol. 2015;30(6):509-517. doi: 10.1007/s10654-015-0021-x [DOI] [PubMed] [Google Scholar]
- 100.Seymour JD, Calle EE, Flagg EW, Coates RJ, Ford ES, Thun MJ; American Cancer Society . Diet quality index as a predictor of short-term mortality in the American Cancer Society Cancer Prevention Study II nutrition cohort. Am J Epidemiol. 2003;157(11):980-988. doi: 10.1093/aje/kwg077 [DOI] [PubMed] [Google Scholar]
- 101.Shah NS, Leonard D, Finley CE, et al. Dietary patterns and long-term survival: a retrospective study of healthy primary care patients. Am J Med. 2018;131(1):48-55. doi: 10.1016/j.amjmed.2017.08.010 [DOI] [PubMed] [Google Scholar]
- 102.Shahar DR, Yu B, Houston DK, et al. ; Health, Aging and Body Composition Study . Dietary factors in relation to daily activity energy expenditure and mortality among older adults. J Nutr Health Aging. 2009;13(5):414-420. doi: 10.1007/s12603-009-0077-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shivappa N, Hebert JR, Kivimaki M, Akbaraly T. Alternative Healthy Eating Index 2010, Dietary Inflammatory Index and risk of mortality: results from the Whitehall II cohort study and meta-analysis of previous Dietary Inflammatory Index and mortality studies. Br J Nutr. 2017;118(3):210-221. doi: 10.1017/S0007114517001908 [DOI] [PubMed] [Google Scholar]
- 104.Shvetsov YB, Harmon BE, Ettienne R, et al. The influence of energy standardisation on the alternate Mediterranean diet score and its association with mortality in the multiethnic cohort. Br J Nutr. 2016;116(9):1592-1601. doi: 10.1017/S0007114516003482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sijtsma FP, Soedamah-Muthu SS, de Hoon SE, Jacobs DR Jr, Kromhout D. Healthy eating and survival among elderly men with and without cardiovascular-metabolic diseases. Nutr Metab Cardiovasc Dis. 2015;25(12):1117-1124. doi: 10.1016/j.numecd.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 106.Sjögren P, Becker W, Warensjö E, et al. Mediterranean and carbohydrate-restricted diets and mortality among elderly men: a cohort study in Sweden. Am J Clin Nutr. 2010;92(4):967-974. doi: 10.3945/ajcn.2010.29345 [DOI] [PubMed] [Google Scholar]
- 107.Sotos-Prieto M, Bhupathiraju SN, Mattei J, et al. Association of changes in diet quality with total and cause-specific mortality. N Engl J Med. 2017;377(2):143-153. doi: 10.1056/NEJMoa1613502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Stefler D, Malyutina S, Kubinova R, et al. Mediterranean diet score and total and cardiovascular mortality in Eastern Europe: the HAPIEE Study. Eur J Nutr. 2017;56(1):421-429. doi: 10.1007/s00394-015-1092-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Struijk EA, Beulens JW, May AM, et al. Dietary patterns in relation to disease burden expressed in disability-adjusted life years. Am J Clin Nutr. 2014;100(4):1158-1165. doi: 10.3945/ajcn.113.082032 [DOI] [PubMed] [Google Scholar]
- 110.Thorpe RJ Jr, Wilson-Frederick SM, Bowie JV, et al. Health behaviors and all-cause mortality in African American men. Am J Mens Health. 2013;7(4suppl):8S-18S. doi: 10.1177/1557988313487552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Tognon G, Lissner L, Sæbye D, Walker KZ, Heitmann BL. The Mediterranean diet in relation to mortality and CVD: a Danish cohort study. Br J Nutr. 2014;111(1):151-159. doi: 10.1017/S0007114513001931 [DOI] [PubMed] [Google Scholar]
- 112.Tognon G, Nilsson LM, Lissner L, et al. The Mediterranean diet score and mortality are inversely associated in adults living in the subarctic region. J Nutr. 2012;142(8):1547-1553. doi: 10.3945/jn.112.160499 [DOI] [PubMed] [Google Scholar]
- 113.Tognon G, Rothenberg E, Eiben G, Sundh V, Winkvist A, Lissner L. Does the Mediterranean diet predict longevity in the elderly? A Swedish perspective. Age (Dordr). 2011;33(3):439-450. doi: 10.1007/s11357-010-9193-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Tong TY, Wareham NJ, Khaw KT, Imamura F, Forouhi NG. Prospective association of the Mediterranean diet with cardiovascular disease incidence and mortality and its population impact in a non-Mediterranean population: the EPIC-Norfolk Study. BMC Med. 2016;14(1):135. doi: 10.1186/s12916-016-0677-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med. 2003;348(26):2599-2608. doi: 10.1056/NEJMoa025039 [DOI] [PubMed] [Google Scholar]
- 116.Trichopoulou A, Orfanos P, Norat T, et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ. 2005;330(7498):991. doi: 10.1136/bmj.38415.644155.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Trichopoulou A, Bamia C, Trichopoulos D. Anatomy of health effects of Mediterranean diet: Greek EPIC prospective cohort study. BMJ. 2009;338:b2337. doi: 10.1136/bmj.b2337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.van Dam RM, Li T, Spiegelman D, Franco OH, Hu FB. Combined impact of lifestyle factors on mortality: prospective cohort study in US women. BMJ. 2008;337:a1440. doi: 10.1136/bmj.a1440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.van den Brandt PA. The impact of a Mediterranean diet and healthy lifestyle on premature mortality in men and women. Am J Clin Nutr. 2011;94(3):913-920. doi: 10.3945/ajcn.110.008250 [DOI] [PubMed] [Google Scholar]
- 120.van Lee L, Geelen A, Kiefte-de Jong JC, et al. Adherence to the Dutch dietary guidelines is inversely associated with 20-year mortality in a large prospective cohort study. Eur J Clin Nutr. 2016;70(2):262-268. doi: 10.1038/ejcn.2015.163 [DOI] [PubMed] [Google Scholar]
- 121.Voortman T, Kiefte-de Jong JC, Ikram MA, et al. Adherence to the 2015 Dutch dietary guidelines and risk of non-communicable diseases and mortality in the Rotterdam study. Eur J Epidemiol. 2017;32(11):993-1005. doi: 10.1007/s10654-017-0295-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Vormund K, Braun J, Rohrmann S, Bopp M, Ballmer P, Faeh D. Mediterranean diet and mortality in Switzerland: an alpine paradox? Eur J Nutr. 2015;54(1):139-148. doi: 10.1007/s00394-014-0695-y [DOI] [PubMed] [Google Scholar]
- 123.Wahlqvist ML, Darmadi-Blackberry I, Kouris-Blazos A, et al. Does diet matter for survival in long-lived cultures? Asia Pac J Clin Nutr. 2005;14(1):2-6. [PubMed]
- 124.Warensjö Lemming E, Byberg L, Wolk A, Michaëlsson K. A comparison between two healthy diet scores, the modified Mediterranean diet score and the Healthy Nordic Food Index, in relation to all-cause and cause-specific mortality. Br J Nutr. 2018;119(7):836-846. doi: 10.1017/S0007114518000387 [DOI] [PubMed] [Google Scholar]
- 125.Whalen KA, Judd S, McCullough ML, Flanders WD, Hartman TJ, Bostick RM. Paleolithic and Mediterranean diet pattern scores are inversely associated with all-cause and cause-specific mortality in adults. J Nutr. 2017;147(4):612-620. doi: 10.3945/jn.116.241919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Yu D, Sonderman J, Buchowski MS, et al. Healthy eating and risks of total and cause-specific death among low-income populations of African-Americans and other adults in the southeastern United States: a prospective cohort study. PLoS Med. 2015;12(5):e1001830. doi: 10.1371/journal.pmed.1001830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zaslavsky O, Zelber-Sagi S, Hebert JR, et al. Biomarker-calibrated nutrient intake and healthy diet index associations with mortality risks among older and frail women from the Women’s Health Initiative. Am J Clin Nutr. 2017;105(6):1399-1407. doi: 10.3945/ajcn.116.151530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zaslavsky O, Zelber-Sagi S, Shikany JM, et al. Anatomy of the Mediterranean diet and mortality among older women with frailty. J Nutr Gerontol Geriatr. 2018;37(3-4):269-281. doi: 10.1080/21551197.2018.1496217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Anderson AL, Harris TB, Tylavsky FA, et al. ; Health ABC Study . Dietary patterns and survival of older adults. J Am Diet Assoc. 2011;111(1):84-91. doi: 10.1016/j.jada.2010.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. Dietary patterns and the risk of CVD and all-cause mortality in older British men. Br J Nutr. 2016;116(7):1246-1255. doi: 10.1017/S0007114516003147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Bamia C, Trichopoulos D, Ferrari P, et al. Dietary patterns and survival of older Europeans: the EPIC-Elderly Study (European Prospective Investigation into Cancer and Nutrition). Public Health Nutr. 2007;10(6):590-598. doi: 10.1017/S1368980007382487 [DOI] [PubMed] [Google Scholar]
- 132.Brunner EJ, Mosdøl A, Witte DR, et al. Dietary patterns and 15-y risks of major coronary events, diabetes, and mortality. Am J Clin Nutr. 2008;87(5):1414-1421. doi: 10.1093/ajcn/87.5.1414 [DOI] [PubMed] [Google Scholar]
- 133.Granic A, Andel R, Dahl AK, Gatz M, Pedersen NL. Midlife dietary patterns and mortality in the population-based study of Swedish twins. J Epidemiol Community Health. 2013;67(7):578-586. doi: 10.1136/jech-2012-201780 [DOI] [PubMed] [Google Scholar]
- 134.Hamer M, McNaughton SA, Bates CJ, Mishra GD. Dietary patterns, assessed from a weighed food record, and survival among elderly participants from the United Kingdom. Eur J Clin Nutr. 2010;64(8):853-861. doi: 10.1038/ejcn.2010.93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008;118(3):230-237. doi: 10.1161/CIRCULATIONAHA.108.771881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hoffmann K, Boeing H, Boffetta P, et al. Comparison of two statistical approaches to predict all-cause mortality by dietary patterns in German elderly subjects. Br J Nutr. 2005;93(5):709-716. doi: 10.1079/BJN20051399 [DOI] [PubMed] [Google Scholar]
- 137.Hsiao PY, Mitchell DC, Coffman DL, et al. Dietary patterns and relationship to obesity-related health outcomes and mortality in adults 75 years of age or greater. J Nutr Health Aging. 2013;17(6):566-572. doi: 10.1007/s12603-013-0014-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Krieger JP, Cabaset S, Pestoni G, Rohrmann S, Faeh D; Swiss National Cohort Study Group . Dietary patterns are associated with cardiovascular and cancer mortality among Swiss adults in a census-linked cohort. Nutrients. 2018;10(3):E313. doi: 10.3390/nu10030313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Martínez-González MA, Zazpe I, Razquin C, et al. ; PREDIMED GROUP . Empirically-derived food patterns and the risk of total mortality and cardiovascular events in the PREDIMED study. Clin Nutr. 2015;34(5):859-867. doi: 10.1016/j.clnu.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 140.Masala G, Ceroti M, Pala V, et al. A dietary pattern rich in olive oil and raw vegetables is associated with lower mortality in Italian elderly subjects. Br J Nutr. 2007;98(2):406-415. doi: 10.1017/S0007114507704981 [DOI] [PubMed] [Google Scholar]
- 141.Menotti A, Alberti-Fidanza A, Fidanza F. The association of the Mediterranean Adequacy Index with fatal coronary events in an Italian middle-aged male population followed for 40 years. Nutr Metab Cardiovasc Dis. 2012;22(4):369-375. doi: 10.1016/j.numecd.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 142.Menotti A, Puddu PE, Maiani G, Catasta G. Cardiovascular and other causes of death as a function of lifestyle habits in a quasi extinct middle-aged male population. A 50-year follow-up study. Int J Cardiol. 2016;210:173-178. doi: 10.1016/j.ijcard.2016.02.115 [DOI] [PubMed] [Google Scholar]
- 143.Nanri A, Mizoue T, Shimazu T, et al. ; Japan Public Health Center-Based Prospective Study Group . Dietary patterns and all-cause, cancer, and cardiovascular disease mortality in Japanese men and women: the Japan public health center-based prospective study. PLoS One. 2017;12(4):e0174848. doi: 10.1371/journal.pone.0174848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Waijers PM, Ocké MC, van Rossum CT, et al. Dietary patterns and survival in older Dutch women. Am J Clin Nutr. 2006;83(5):1170-1176. doi: 10.1093/ajcn/83.5.1170 [DOI] [PubMed] [Google Scholar]
- 145.Zazpe I, Sánchez-Tainta A, Toledo E, Sánchez-Villegas A, Martínez-González MA. Dietary patterns and total mortality in a Mediterranean cohort: the SUN project. J Acad Nutr Diet. 2014;114(1):37-47. doi: 10.1016/j.jand.2013.07.024 [DOI] [PubMed] [Google Scholar]
- 146.Zhao W, Ukawa S, Okada E, et al. The associations of dietary patterns with all-cause mortality and other lifestyle factors in the elderly: an age-specific prospective cohort study. Clin Nutr. 2019;38(1):288-296. doi: 10.1016/j.clnu.2018.01.018 [DOI] [PubMed] [Google Scholar]
- 147.Menotti A, Puddu PE, Lanti M, Maiani G, Catasta G, Fidanza AA. Lifestyle habits and mortality from all and specific causes of death: 40-year follow-up in the Italian Rural Areas of the Seven Countries Study. J Nutr Health Aging. 2014;18(3):314-321. doi: 10.1007/s12603-013-0392-1 [DOI] [PubMed] [Google Scholar]
- 148.Odegaard AO, Koh WP, Yuan JM, Gross MD, Pereira MA. Dietary patterns and mortality in a Chinese population. Am J Clin Nutr. 2014;100(3):877-883. doi: 10.3945/ajcn.114.086124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Chang-Claude J, Hermann S, Eilber U, Steindorf K. Lifestyle determinants and mortality in German vegetarians and health-conscious persons: results of a 21-year follow-up. Cancer Epidemiol Biomarkers Prev. 2005;14(4):963-968. doi: 10.1158/1055-9965.EPI-04-0696 [DOI] [PubMed] [Google Scholar]
- 150.Héroux M, Janssen I, Lam M, et al. Dietary patterns and the risk of mortality: impact of cardiorespiratory fitness. Int J Epidemiol. 2010;39(1):197-209. doi: 10.1093/ije/dyp191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Key TJ, Appleby PN, Spencer EA, Travis RC, Roddam AW, Allen NE. Mortality in British vegetarians: results from the European Prospective Investigation into Cancer and Nutrition (EPIC-Oxford). Am J Clin Nutr. 2009;89(5):1613S-1619S. doi: 10.3945/ajcn.2009.26736L [DOI] [PubMed] [Google Scholar]
- 152.Kim H, Hu EA, Rebholz CM. Ultra-processed food intake and mortality in the USA: results from the Third National Health and Nutrition Examination Survey (NHANES III, 1988-1994). Public Health Nutr. 2019;22(10):1777-1785. doi: 10.1017/S1368980018003890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Meyer J, Döring A, Herder C, Roden M, Koenig W, Thorand B. Dietary patterns, subclinical inflammation, incident coronary heart disease and mortality in middle-aged men from the MONICA/KORA Augsburg cohort study. Eur J Clin Nutr. 2011;65(7):800-807. doi: 10.1038/ejcn.2011.37 [DOI] [PubMed] [Google Scholar]
- 154.Mihrshahi S, Ding D, Gale J, Allman-Farinelli M, Banks E, Bauman AE. Vegetarian diet and all-cause mortality: evidence from a large population-based Australian cohort - the 45 and Up Study. Prev Med. 2017;97:1-7. doi: 10.1016/j.ypmed.2016.12.044 [DOI] [PubMed] [Google Scholar]
- 155.Orlich MJ, Singh PN, Sabaté J, et al. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med. 2013;173(13):1230-1238. doi: 10.1001/jamainternmed.2013.6473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Rico-Campà A, Martínez-González MA, Alvarez-Alvarez I, et al. Association between consumption of ultra-processed foods and all cause mortality: SUN prospective cohort study. BMJ. 2019;365:l1949. doi: 10.1136/bmj.l1949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Schnabel L, Kesse-Guyot E, Allès B, et al. Association between ultraprocessed food consumption and risk of mortality among middle-aged adults in France. JAMA Intern Med. 2019;179(4):490-498. doi: 10.1001/jamainternmed.2018.7289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Song M, Fung TT, Hu FB, et al. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern Med. 2016;176(10):1453-1463. doi: 10.1001/jamainternmed.2016.4182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Bazelmans C, De Henauw S, Matthys C, et al. Healthy food and nutrient index and all cause mortality. Eur J Epidemiol. 2006;21(2):145-152. doi: 10.1007/s10654-005-5699-8 [DOI] [PubMed] [Google Scholar]
- 160.Diehr P, Beresford SA. The relation of dietary patterns to future survival, health, and cardiovascular events in older adults. J Clin Epidemiol. 2003;56(12):1224-1235. doi: 10.1016/S0895-4356(03)00202-6 [DOI] [PubMed] [Google Scholar]
- 161.Fung TT, van Dam RM, Hankinson SE, Stampfer M, Willett WC, Hu FB. Low-carbohydrate diets and all-cause and cause-specific mortality: two cohort studies. Ann Intern Med. 2010;153(5):289-298. doi: 10.7326/0003-4819-153-5-201009070-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hernández-Alonso P, Salas-Salvadó J, Ruiz-Canela M, et al. High dietary protein intake is associated with an increased body weight and total death risk. Clin Nutr. 2016;35(2):496-506. doi: 10.1016/j.clnu.2015.03.016 [DOI] [PubMed] [Google Scholar]
- 163.Kelemen LE, Kushi LH, Jacobs DR Jr, Cerhan JR. Associations of dietary protein with disease and mortality in a prospective study of postmenopausal women. Am J Epidemiol. 2005;161(3):239-249. doi: 10.1093/aje/kwi038 [DOI] [PubMed] [Google Scholar]
- 164.Leosdottir M, Nilsson P, Nilsson JA, Månsson H, Berglund G. The association between total energy intake and early mortality: data from the Malmö Diet and Cancer Study. J Intern Med. 2004;256(6):499-509. doi: 10.1111/j.1365-2796.2004.01407.x [DOI] [PubMed] [Google Scholar]
- 165.Leosdottir M, Nilsson PM, Nilsson JA, Månsson H, Berglund G. Dietary fat intake and early mortality patterns—data from the Malmö Diet and Cancer Study. J Intern Med. 2005;258(2):153-165. doi: 10.1111/j.1365-2796.2005.01520.x [DOI] [PubMed] [Google Scholar]
- 166.Mazidi M, Katsiki N, Mikhailidis DP, Sattar N, Banach M. Lower carbohydrate diets and all-cause and cause-specific mortality: a population-based cohort study and pooling of prospective studies. Eur Heart J. 2019;40(34):2870-2879. doi: 10.1093/eurheartj/ehz174 [DOI] [PubMed] [Google Scholar]
- 167.Nagata C, Nakamura K, Wada K, et al. Total fat intake is associated with decreased mortality in Japanese men but not in women. J Nutr. 2012;142(9):1713-1719. doi: 10.3945/jn.112.161661 [DOI] [PubMed] [Google Scholar]
- 168.Nakamura Y, Okuda N, Okamura T, et al. ; NIPPON DATA Research Group . Low-carbohydrate diets and cardiovascular and total mortality in Japanese: a 29-year follow-up of NIPPON DATA80. Br J Nutr. 2014;112(6):916-924. doi: 10.1017/S0007114514001627 [DOI] [PubMed] [Google Scholar]
- 169.Nilsson LM, Winkvist A, Eliasson M, et al. Low-carbohydrate, high-protein score and mortality in a northern Swedish population-based cohort. Eur J Clin Nutr. 2012;66(6):694-700. doi: 10.1038/ejcn.2012.9 [DOI] [PubMed] [Google Scholar]
- 170.Wakai K, Naito M, Date C, Iso H, Tamakoshi A; JACC Study Group . Dietary intakes of fat and total mortality among Japanese populations with a low fat intake: the Japan Collaborative Cohort (JACC) Study. Nutr Metab (Lond). 2014;11(1):12. doi: 10.1186/1743-7075-11-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Estruch R, Ros E, Salas-Salvadó J, et al. ; PREDIMED Study Investigators . Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368(14):1279-1290. Retracted and republished in: N Engl J Med. 2018;378(25):2441-2442. doi: 10.1056/NEJMc1806491 [DOI] [PubMed] [Google Scholar]
- 172.Zhong VW, Van Horn L, Greenland P, et al. Associations of processed meat, unprocessed red meat, poultry, or fish intake with incident cardiovascular disease and all-cause mortality. JAMA Intern Med. 2020;180(4):503-512. doi: 10.1001/jamainternmed.2019.6969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Berkman ND, Lohr KN, Ansari M, et al. Grading the strength of a body of evidence when assessing health care interventions for the effective health care program of the Agency for Healthcare Research and Quality: an update. In: Agency for Healthcare Research and Quality. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Agency for Healthcare Research and Quality; 2008. [PubMed] [Google Scholar]
- 174.Office of Health Assessment and Translation, Division of the National Toxicology Program, National Institute of Environmental Health Sciences. Handbook for conducting a literature-based health assessment using OHAT approach for systematic review and evidence integration. Accessed June 18, 2020. https://ntp.niehs.nih.gov/ntp/ohat/pubs/handbookjan2015_508.pdf
- 175.Schunemann H, Brożek J, Guyatt G, Oxman A, eds. Introduction to GRADE Handbook: handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach. GRADE Working Group. Updated October 2013. Accessed June 18, 2020. https://gdt.gradepro.org/app/handbook/handbook.html#h.svwngs6pm0f2
- 176.Dietary Guidelines Advisory Committee. Part C: methodology. In: Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 177.Dietary Guidelines Advisory Committee . Chapter 8: dietary patterns. In: Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 178.Dietary Guidelines Advisory Committee . Chapter 2: food, beverage, and nutrient consumption during pregnancy. In: Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 179.Dietary Guidelines Advisory Committee . Chapter 11: alcoholic beverages. In: Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
- 180.Dietary Guidelines Advisory Committee . Chapter 1: current intakes of foods, beverages, and nutrients. In: Scientific Report of the 2020 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and the Secretary of Agriculture. US Department of Agriculture, Agricultural Research Service; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Description of All Dietary Patterns Examined in Relation to All-Cause Mortality Outcomes in All Included Articles
eTable 2. Results by All Included Articles for Dietary Pattern and All-Cause Mortality (ACM) Analyses
eReferences.