Abstract
Background/Aim: High-flow nasal cannula (HFNC), a new method for postoperative oxygenation, has increasingly received attention during postoperative care. However, its importance for obese patients undergoing cardiac surgery remains controversial. This systematic review and meta-analysis compared and evaluated HFNC and conventional oxygen therapy (COT) in this patient group. Materials and Methods: Literature was retrieved by searching eight public databases. Randomized controlled trials (RCTs) were selected. RevMan 5.3 was used to analyze the results and any potential bias. The primary outcome included atelectasis score at 24 h postoperatively. The secondary outcomes included PaO2/FiO2 (ratio), dyspnea score at 24 h postoperatively, intensive care unit (ICU) length of stay, and reintubation. Results: The search strategy yielded 382 studies after duplicates were removed. Finally, 3 RCTs with a total of 526 patients were included in the present study. Compared with COT, there was no significant difference in atelectasis score, dyspnea score, reintubation, and ICU length of stay. Conclusion: For obese patients undergoing cardiac surgery, postoperative use of HFNC can maintain patient’s oxygenation. Additional clinical studies are needed to investigate the role of HFNC in this patient group.
Keywords: High-flow nasal cannula, HFNC, obese, cardiac surgery, postoperation oxygenation, atelectasis score, dyspnea score, review
Obesity is a global problem. At present, more than one-third of the world’s population are overweight, which leads to an increased risk of circulatory and respiratory dysfunction. The increase in body mass index (BMI) will be accompanied by respiratory system problems, especially the decrease in functional residual capacity (FRC) (1). Thus, obese patients have a higher risk of complications such as reduction of lung volume and atelectasis after general anaesthesia. In addition, obesity and obesity-related diseases are critical risk factors for several cardiovascular diseases. At the same time, obesity is also a risk factor for hypoxemia after cardiac surgery (2), a condition leading mostly to atelectasis (3). Therefore, in order to maintain tissue oxygenation and avoid complications of alveolar collapse and atelectasis after cardiac surgery (4), it is necessary to provide patients with oxygen.
High-flow nasal cannula (HFNC) provides high-flow (8-80 l/min) inhalation gas with adjustable and relatively constant oxygen concentration (21%~100%), temperature (31-37℃) and humidity (5,6). Compared with conventional oxygenation methods, the advantage of HFNC is that the continuous positive airway pressure (CPAP) can cause mild lung recruitment (7,8), thus, it can reduce the ventilation dead space to improve the oxygenation of critically ill patients and improve patient comfort (9-11). In addition, some features of HFNC, such as increasing FRC and end-expiratory lung volume (EELV), can improve the oxygenation status of obese patients (12,13).
At present, the postoperative oxygenation strategy for obese patients undergoing cardiac surgery remains controversial. The purpose of our research was to compare the effects of HFNC and conventional oxygen therapy (COT) in obese patients undergoing cardiac surgery. As far as we know, this is the first systematic review and meta-analysis on this topic.
Materials and Methods
Study selection. This systematic review and meta-analysis were performed in accordance with the PRISMA guidelines (14). We searched for articles published before April 10th from PubMed, Embase, Web of science, Scopus, Cochrane, and Clinicalkey databases. We used a Boolean approach. The search terms were High-flow Nasal Cannula OR HFNC OR High flow nasal cannula therapy OR high-flow oxygen therapy through nasal cannula OR nasal high flow, Obese patients, OR obesity OR overweight OR fat OR corpulent. The restrictive conditions of all search formulas were the search of titles, abstracts, and keywords. No restrictions on language were applied. The searched literature was managed with EndNote X9 (Thomson Reuters, New York, NY, USA). After excluding duplicate and non-clinical studies, we screened the titles and abstracts of the retrieved articles. Then, we screened the full text and finally included three studies. When the results of the investigators diverged, the opinion of a fourth researcher (J.L) was adopted.
Eligibility criteria. The studies included in the meta-analysis met the following criteria: clinical studies, comparison of HFNC and COT, and obese patients (BMI≥30 kg/m2) receiving post-cardiac surgery. Studies with the following characteristics were excluded: animal studies, study protocol, reviews, guidelines or conference abstracts, case reports, and inconsistent inclusion criteria.
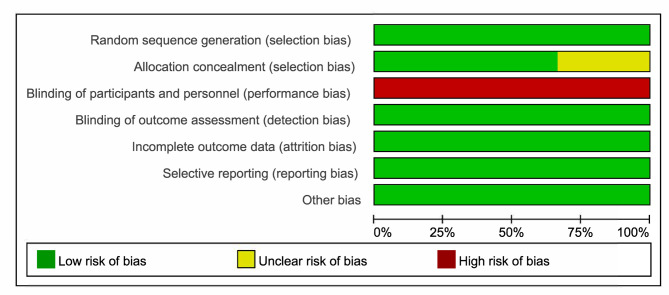
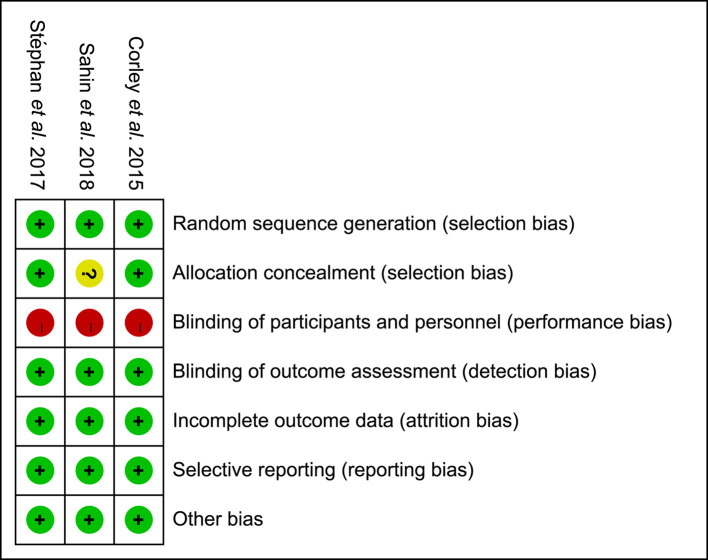
Risk of bias assessment. Three investigators used the Cochrane collaboration tool (15) to evaluate the bias of the included studies, and RevMan 5.3 (Review Manager, Version 5.3, Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) to make the graph (Figure 1) and summary (Figure 2). The bias evaluated included: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias such as baseline imbalance and conflict of interest. Assessments were stored and managed in RevMan 5.3. If there were different evaluation results, an additional researcher was consulted (N.L).
Figure 1. Risk of bias graph: review authors’ judgements about each risk of bias item presented as percentage across all included studies.
Figure 2. Risk of bias summary: review authors’ judgements about each risk of bias item for each included study.
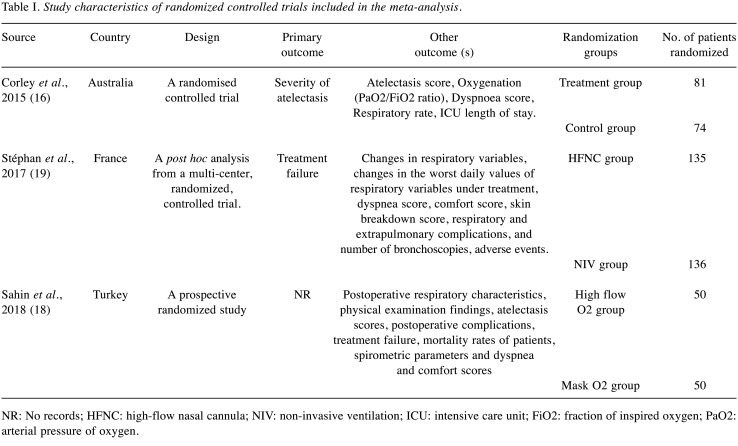
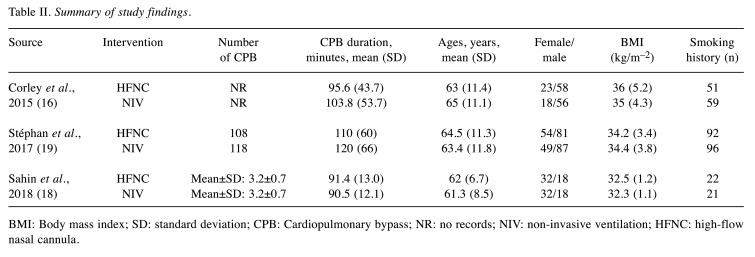
Data extraction. The three investigators independently completed the data extraction work. Table I shows the RCTs study characteristics. These data included: source of the included study, year, primary outcome, other outcome(s), randomization groups, and number of patients randomized. A summary of study findings is presented in Table II, and mainly includes age, gender, BMI, interventions, smoking history, number of CPB (Cardiopulmonary bypass), and CPB duration. The fourth researcher (J.L) is responsible for resolving disputes in the data extraction process.
Table I. Study characteristics of randomized controlled trials included in the meta-analysis.
NR: No records; HFNC: high-flow nasal cannula; NIV: non-invasive ventilation; ICU: intensive care unit; FiO2: fraction of inspired oxygen; PaO2: arterial pressure of oxygen.
Table II. Summary of study findings.
BMI: Body mass index; SD: standard deviation; CPB: Cardiopulmonary bypass; NR: no records; NIV: non-invasive ventilation; HFNC: high-flow nasal cannula.
Outcomes. The primary outcome of this systematic review was atelectasis score at 24 h postoperatively. The secondary outcomes were the PaO2/FiO2 (ratio) and dyspnea score, at 24 h postoperatively. In addition, we also evaluated ICU length of stay and reintubation.
Statistical analysis. RevMan 5.3 computer software was used for all data analyses in this study. Data involving continuous variables are shown as mean±SD. When only the median and quartile were provided in the study (16), we calculated the outcome according to the method of Wan et al. (17). Furthermore, when using a histogram or line chart to represent the results of the research, we used WebPlotDigitizer (WebPlotDigitizer, Version: 4.4, Ankit Rohatgi, Pacifica, CA, USA, November, 2020) to extract the data. The inverse variance random effects model was used to analyze continuous variables and expressed as the MD (mean difference) of the 95%CI. For binary variables, we reported the odds ratios (OR), and used the Mantel-Haenszel method for analysis. For the data of p<0.05 or I2>50% for heterogeneity detection, the random-effect model was used for analysis, while p>0.05 or I2≤50% was selected for the fixed-effect model.
Results
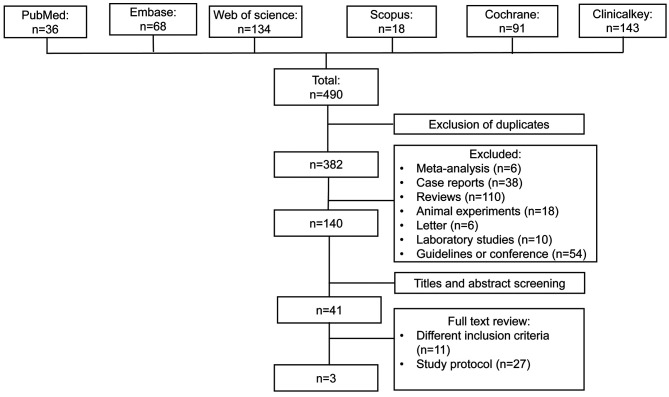
Literature search findings. By searching PubMed, Embase, Web of science, Scopus, Cochrane, and Clinicalkey databases, 490 articles were obtained. We found 108 duplicates, and analyzed 140 clinical trials (review: 110; meta-analysis: 6; case report: 38; animal experiments: 18; letter: 6; laboratory studies: 10; guidelines or conference abstract: 54). Through the screening of abstracts, titles, and keywords, we obtained 41 studies related to HFNC or obese patients. After screening the full texts, 3 studies were finally included [excluded studies were due to different inclusion criteria of the studies (n=11) and study protocol variance (n=27)]. The literature retrieval process is shown in Figure 3.
Figure 3. Flow diagram of search strategy and included studies.
Study and patient characteristics. We summarized the study and patient characteristics included in the studies in Table I and Table II. Among the included studies, two studies (16,18) were RCTs. The study of Stéphan et al. (19) is a post hoc analysis of a predesigned RCT (20). This meta-analysis included a total of 526 patients from Australia, France, and Turkey. All studies were randomly divided into two groups; the intervention measures were HFNC and non-invasive ventilation (NIV). The mean age of the patients in the three studies was over 60 years old, and BMI was >30 kg/m–2. Furthermore, most of the patients had a smoking history in the two studies (70.96%, 69.37%) (16,19), but only 43% of patients in the study by Sahin et al. (18) had a smoking history. This difference in smoking history may be due to the difference in the gender ratio of the included patients. Compared with the other two studies, Sahin et al. included more female patients. In the included studies, all patients underwent CPB, and the duration of CPB in the patients of the study of Stéphan et al. was longer.
Risk of bias assessment and study quality. The bias in the study was evaluated by RevMan 5.3. It is expressed as high risk, low risk, and unclear. In the generation of random sequences, all studies were low-risk. For the concealment of random sequences, there were two studies (16,19) that were of good quality. However, Sahin et al.’s study (18) did not mention it, therefore we are unclear whether Sahin et al. successfully concealed the allocation. Due to the particularity of interventions, all studies cannot be blind regarding patients or medical staff.
Meta-analysis and synthesis
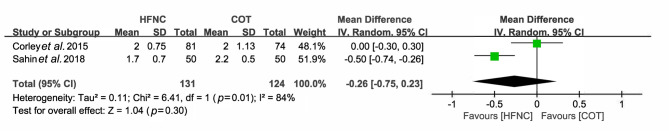
Atelectasis score at 24 h postoperative. Two studies reported the atelectasis score at 24 h postoperative and the sample size was 255 cases. In the report by Corley et al. (16), the atelectasis score [median (IQR)] was 2 (1.5-2.5) for the HFNC group: and 2 (1.5-3) for the COT group. The atelectasis score (mean±SD) reported by Sahin et al. (18) was 1.7±0.7 for the HFNC group and 2.2±0.5 for the COT group. The pooled MD (95%CI) of the atelectasis score was –0.26 (–0.75, 0.23), I2=84%, n=2 (Figure 4). Using the random-effects model, the result was not found to be statistically significant (p=0.30).
Figure 4. Comparison of atelectasis score at 24 h postoperative between high-flow nasal cannula (HFNC) and conventional oxygen therapy (COT).
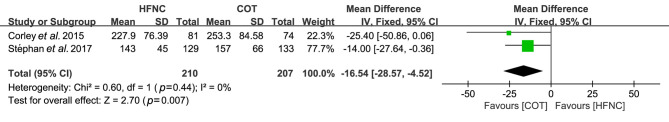
PaO2/FiO2 at 24 h postoperative. Two studies reported the PaO2/FiO2 at 24 h postoperative and the sample size was 417 cases. In the report by Corley et al. (16), the PaO2/FiO2 (mean±SD) was 227.9±76.39 for the HFNC group and 253.3±84.58 for the COT group. The PaO2/FiO2 (mean±SD) reported by Stéphan et al. (19) was 143±45 for the HFNC group and 157±66 for the COT group. The pooled MD (95%CI) of the PaO2/FiO2 was –16.54 (–28.57, –4.52), I2=0%, n=2 (Figure 5). Using the fixed-effects model, the result was statistically significant (p=0.007).
Figure 5. Comparison of PaO2/FiO2 at 24 h postoperative between high-flow nasal cannula (HFNC) and conventional oxygen therapy (COT).
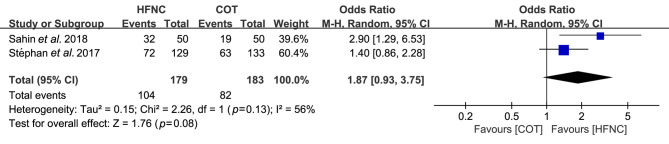
Dyspnea score at 24 h postoperative (improvement). Two studies reported the dyspnea score at 24 h postoperative and the sample size was 362 cases. In the report by Sahin et al. (18), the number of dyspnea score improvement was 32 for the HFNC group and 19 for the COT group. The dyspnea score reported by Stéphan et al. (19) was 72 for the HFNC group and 63 for the COT group. The pooled OR (95%CI) of it was 1.87 (0.93-3.75), I2=56%, n=2 (Figure 6). Using a random-effects model, the result was not statistically significant (p=0.08).
Figure 6. Comparison of dyspnea score at 24 h postoperative (improvement) between HFNC and conventional oxygen therapy (COT).
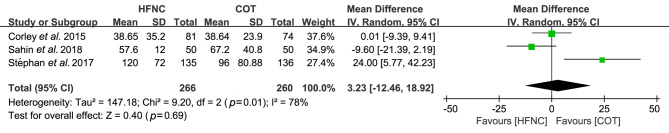
ICU length of stay (hours). Three studies reported the ICU length of stay and the sample size was 526. In the report by Corley et al. (16), the ICU length of stay (mean ± SD, hours) was 38.65±35.2 h for the HFNC group and 38.64±23.9 h for the COT group. The ICU length reported by Stéphan et al. (19) was 120±72 h for the HFNC group and 96±80.88 h for the COT group. That reported by Sahin et al. (18) was 57.6±12 h for the HFNC group and 67.2±40.8 h for the COT group. The pooled MD (95%CI) of it was 3.23 (–12.46-18.92), I2=78%, n=3 (Figure 7). Using a random-effects model, the result was not found to be statistically significant (p=0.69).
Figure 7. Comparison of ICU length of stay (hours) between high-flow nasal cannula (HFNC) and conventional oxygen therapy (COT).
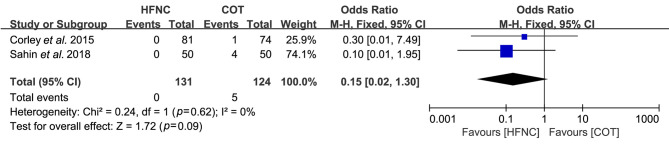
Reintubation. Two studies reported the reintubation and the sample size was 255. In the report by Sahin et al. (18), the number of reintubation was 0 for the HFNC group and 4 for the COT group. The nosocomial pneumonia reported by Corley et al. (16) was 0 for the HFNC group and 1 for the COT group. The pooled OR (95%CI) of it was 0.15 (0.02-1.30), I2=0%, n=2 (Figure 8). Using a fixed-effects model, the result was not found to be statistically significant (p=0.09).
Figure 8. Comparison of reintubation between high-flow nasal cannula (HFNC) and conventional oxygen therapy (COT).
Discussion
This is the first meta-analysis to evaluate the effect of HFNC on postoperative oxygen in obese patients undergoing cardiac surgery. It included 3 RCTs and enrolled a total of 526 patients. Compared with COT, HFNC did not improve patients’ atelectasis score, PaO2/FiO2 (ratio), and dyspnea score at 24 h postoperative. Also, there was no significant difference between the two regarding ICU length of stay and reintubation.
Patients are prone to atelectasis after undergoing cardiac surgery, and BMI>30 kg/m2 exacerbates this risk. Severe atelectasis can lead to postoperative hypoxemia, respiratory and circulatory depression, and increase in the occurrence of adverse events. Furthermore, most patients undergoing major surgery have atelectasis lasting for at least 24 h, as seen on computed tomography scans (21). Therefore, we chose atelectasis score at 24 h postoperative as the primary outcome of this study. Through searching, we found only two meta-analyses (22) of the effect of HFNC and COT in cardiac surgery; Zhu et al. did not use atelectasis score as an outcome. Our analysis showed that there was no significant difference in atelectasis index between HFNC and COT in obese patients undergoing cardiac surgery 24 h after oxygenation. We found similar results in the meta-analysis of Du et al. (23). In different operations, compared with COT, the use of HFNC on patients after surgery has been shown to prevent atelectasis (24-27). For cardiac surgery, especially in obese patients, the prevention of atelectasis by HFNC is still controversial. In this regard, there are fewer reports of HFNC in cardiac surgery and obese patients, and most studies do not report on postoperative atelectasis. Therefore, whether HFNC can reduce the occurrence of atelectasis after cardiac surgery in obese patients should be further investigated.
Both PaO2/FiO2 (ratio) and dyspnea score (improvement) can be used to evaluate the oxygenation status of patients after receiving HFNC and COT. Several studies (28,29) have pointed out that, compared with COT, HFNC can effectively improve the oxygenation status of patients, which is due to the tighter fit of the nasal catheter than the mask and the inhalation of high-flow gas (13,30). According to our results, the COT group had better oxygenation than HFNC group. This result is not surprising, because the conclusion of some previous studies (31,32) is similar to ours. The evaluation of the number of patient reintubation can provide theoretical support for the choice of HFNC or COT. Different from our results, some studies (33,34) have suggested the postoperative use of HFNC can reduce reintubation, but there is a lack of relevant studies for obese or cardiac surgery patients.
Compared with COT, the use of HFNC can shorten the length of stay in the ICU (35,36). Our results showed that this is not consistent among obese patients undergoing cardiac surgery. The two meta-analysis of Du et al. (23) and Corley et al. (37) derived conclusions similar to ours. This suggests that compared with COT, the use of HFNC has not significantly changed the ICU length of stay of obese patients undergoing cardiac surgery.
This meta-analysis has the following limitations. First, because there are few related clinical studies and only 3 RCTs were included, the conclusion may not have clinical significance. Second, the included studies are heterogeneous, and there are certain differences in the methods of cardiac surgery and the characteristics of the included patients. Third, because there are few meta-analyses on a similar topic, it is difficult to compare it with other related studies. Finally, for the data that are not represented by the mean±SD, we used formula conversion. In addition, we used measurement software to estimate the data displayed on the graph. This may have inevitably affected the accuracy of the data.
Conclusion
This systematic review and meta-analysis showed that for obese patients undergoing cardiac surgery, the postoperative use of HFNC can maintain oxygenation. However, compared with COT, there is no significant difference in atelectasis score, dyspnea score, reintubation, and ICU length of stay. More clinical studies are needed to confirm the role of HFNC.
Conflicts of Interest
The Authors have no conflicts of interest to declare in relation to this study.
Authors’ Contributions
Y.L.W. contributed to the design of the study, conducted the study, analyzed the data, and wrote the manuscript. Y.L.W. is also the senior author and was responsible for archiving the study files. J.K.Z., X.F.W., G.Z.L., and X.H.M. contributed to the execution of the study, analyzed the data, and wrote the manuscript. N.L. contributed to data analysis. J.L. is the corresponding author and was mainly responsible for the supervision of the study.
References
- 1.Pelosi P, Ravagnan I, Giurati G, Panigada M, Bottino N, Tredici S, Eccher G, Gattinoni L. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology. 1999;91(5):1221–1231. doi: 10.1097/00000542-199911000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Lopez-Delgado JC, Esteve F, Manez R, Torrado H, Carrio ML, Rodríguez-Castro D, Farrero E, Javierre C, Skaltsa K, Ventura JL. The influence of body mass index on outcomes in patients undergoing cardiac surgery: does the obesity paradox really exist. PLoS One. 2015;10(3):e0118858. doi: 10.1371/journal.pone.0118858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tenling A, Hachenberg T, Tydén H, Wegenius G, Hedenstierna G. Atelectasis and gas exchange after cardiac surgery. Anesthesiology. 1998;89(2):371–378. doi: 10.1097/00000542-199808000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Zarbock A, Mueller E, Netzer S, Gabriel A, Feindt P, Kindgen-Milles D. Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: a prospective, randomized, controlled trial in 500 patients. Chest. 2009;135(5):1252–1259. doi: 10.1378/chest.08-1602. [DOI] [PubMed] [Google Scholar]
- 5.Renda T, Corrado A, Iskandar G, Pelaia G, Abdalla K, Navalesi P. High-flow nasal oxygen therapy in intensive care and anaesthesia. Br J Anaesth. 2018;120(1):18–27. doi: 10.1016/j.bja.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Roca O, Hernández G, Díaz-Lobato S, Carratalá JM, Gutiérrez RM, Masclans JR, Spanish Multidisciplinary Group of High Flow Supportive Therapy in Adults (HiSpaFlow) Current evidence for the effectiveness of heated and humidified high flow nasal cannula supportive therapy in adult patients with respiratory failure. Crit Care. 2016;20(1):109. doi: 10.1186/s13054-016-1263-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rajan S, Joseph N, Tosh P, Kadapamannil D, Paul J, Kumar L. Effectiveness of transnasal humidified rapid-insufflation ventilatory exchange versus traditional preoxygenation followed by apnoeic oxygenation in delaying desaturation during apnoea: A preliminary study. Indian J Anaesth. 2018;62(3):202–207. doi: 10.4103/ija.IJA_717_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berlin D, Singh I, Barjaktarevic I, Friedman O. A technique for bronchoscopic intubation during high-flow nasal cannula oxygen therapy. J Intensive Care Med. 2016;31(3):213–215. doi: 10.1177/0885066615582020. [DOI] [PubMed] [Google Scholar]
- 9.Maggiore SM, Idone FA, Vaschetto R, Festa R, Cataldo A, Antonicelli F, Montini L, De Gaetano A, Navalesi P, Antonelli M. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014;190(3):282–288. doi: 10.1164/rccm.201402-0364OC. [DOI] [PubMed] [Google Scholar]
- 10.Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard JD. Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care. 2012;27(3):324.e9–324.13. doi: 10.1016/j.jcrc.2011.07.075. [DOI] [PubMed] [Google Scholar]
- 11.Sztrymf B, Messika J, Bertrand F, Hurel D, Leon R, Dreyfuss D, Ricard JD. Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med. 2011;37(11):1780–1786. doi: 10.1007/s00134-011-2354-6. [DOI] [PubMed] [Google Scholar]
- 12.Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF. Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth. 2011;107(6):998–1004. doi: 10.1093/bja/aer265. [DOI] [PubMed] [Google Scholar]
- 13.Papazian L, Corley A, Hess D, Fraser JF, Frat JP, Guitton C, Jaber S, Maggiore SM, Nava S, Rello J, Ricard JD, Stephan F, Trisolini R, Azoulay E. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med. 2016;42(9):1336–1349. doi: 10.1007/s00134-016-4277-8. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, Cochrane Bias Methods Group , Cochrane Statistical Methods Group The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Corley A, Bull T, Spooner AJ, Barnett AG, Fraser JF. Direct extubation onto high-flow nasal cannulae post-cardiac surgery versus standard treatment in patients with a BMI ≥30: a randomised controlled trial. Intensive Care Med. 2015;41(5):887–894. doi: 10.1007/s00134-015-3765-6. [DOI] [PubMed] [Google Scholar]
- 17.Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. doi: 10.1186/1471-2288-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sahin M, El H, Akkoç I. Comparison of mask oxygen therapy and high-flow oxygen therapy after cardiopulmonary bypass in obese patients. Can Respir J. 2018;2018:1039635. doi: 10.1155/2018/1039635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stéphan F, Bérard L, Rézaiguia-Delclaux S, Amaru P, BiPOP Study Group High-flow nasal cannula therapy versus intermittent noninvasive ventilation in obese subjects after cardiothoracic surgery. Respir Care. 2017;62(9):1193–1202. doi: 10.4187/respcare.05473. [DOI] [PubMed] [Google Scholar]
- 20.Stéphan F, Barrucand B, Petit P, Rézaiguia-Delclaux S, Médard A, Delannoy B, Cosserant B, Flicoteaux G, Imbert A, Pilorge C, Bérard L, BiPOP Study Group High-flow nasal oxygen vs noninvasive positive airway pressure in hypoxemic patients after cardiothoracic surgery: a randomized clinical trial. JAMA. 2015;313(23):2331–2339. doi: 10.1001/jama.2015.5213. [DOI] [PubMed] [Google Scholar]
- 21.Miskovic A, Lumb AB. Postoperative pulmonary complications. Br J Anaesth. 2017;118(3):317–334. doi: 10.1093/bja/aex002. [DOI] [PubMed] [Google Scholar]
- 22.Zhu Y, Yin H, Zhang R, Wei J. High-flow nasal cannula oxygen therapy vs conventional oxygen therapy in cardiac surgical patients: A meta-analysis. J Crit Care. 2017;38:123–128. doi: 10.1016/j.jcrc.2016.10.027. [DOI] [PubMed] [Google Scholar]
- 23.Du X, Yang C, Pan P, Yu X. Effect of high-flow nasal cannula oxygen therapy on improving the atelectasis in adults after cardiac surgeries: a Meta-analysis. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 2018;30(8):748–753. doi: 10.3760/cma.j.issn.2095-4352.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 24.Ferrando C, Puig J, Serralta F, Carrizo J, Pozo N, Arocas B, Gutierrez A, Villar J, Belda FJ, Soro M. High-flow nasal cannula oxygenation reduces postoperative hypoxemia in morbidly obese patients: a randomized controlled trial. Minerva Anestesiol. 2019;85(10):1062–1070. doi: 10.23736/S0375-9393.19.13364-0. [DOI] [PubMed] [Google Scholar]
- 25.Roncin C, Scemama U, Zieleskiewicz L, Loundou A, Lesavre N, Vialet R. Atelectasis prevention during anaesthesia using high-flow nasal cannula therapy: A paediatric randomised trial using MRI images. Anaesth Crit Care Pain Med. 2020;39(6):819–824. doi: 10.1016/j.accpm.2020.08.009. [DOI] [PubMed] [Google Scholar]
- 26.Lee JH, Ji SH, Jang YE, Kim EH, Kim JT, Kim HS. Application of a high-flow nasal cannula for prevention of postextubation atelectasis in children undergoing surgery: a randomized controlled trial. Anesth Analg. 2020;133(2):474–482. doi: 10.1213/ANE.0000000000005285. [DOI] [PubMed] [Google Scholar]
- 27.Xia M, Li W, Yao J, Jin Y, Du G, Xu Q, Yi X, Nv X, Wu Y, He P, Wu W. A postoperative comparison of high-flow nasal cannula therapy and conventional oxygen therapy for esophageal cancer patients. Ann Palliat Med. 2021;10(3):2530–2539. doi: 10.21037/apm-20-1539. [DOI] [PubMed] [Google Scholar]
- 28.Hayes-Bradley C, Lewis A, Burns B, Miller M. Efficacy of nasal cannula oxygen as a preoxygenation adjunct in emergency airwaymanagement. Ann Emerg Med. 2016;68(2):174–180. doi: 10.1016/j.annemergmed.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 29.Doyle AJ, Stolady D, Mariyaselvam M, Wijewardena G, Gent E, Blunt M, Young P. Preoxygenation and apneic oxygenation using Transnasal Humidified Rapid-Insufflation Ventilatory Exchange for emergency intubation. J Crit Care. 2016;36:8–12. doi: 10.1016/j.jcrc.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 30.Drake MG. High-flow nasal cannula oxygen in adults: An evidence-based assessment. Ann Am Thorac Soc. 2018;15(2):145–155. doi: 10.1513/AnnalsATS.201707-548FR. [DOI] [PubMed] [Google Scholar]
- 31.Guitton C, Ehrmann S, Volteau C, Colin G, Maamar A, Jean-Michel V, Mahe PJ, Landais M, Brule N, Bretonnière C, Zambon O, Vourc’h M. Nasal high-flow preoxygenation for endotracheal intubation in the critically ill patient: a randomized clinical trial. Intensive Care Med. 2019;45(4):447–458. doi: 10.1007/s00134-019-05529-w. [DOI] [PubMed] [Google Scholar]
- 32.Simon M, Wachs C, Braune S, de Heer G, Frings D, Kluge S. High-flow nasal cannula versus bag-valve-mask for preoxygenation before intubation in subjects with hypoxemic respiratory failure. Respir Care. 2016;61(9):1160–1167. doi: 10.4187/respcare.04413. [DOI] [PubMed] [Google Scholar]
- 33.Hernández G, Vaquero C, González P, Subira C, Frutos-Vivar F, Rialp G, Laborda C, Colinas L, Cuena R, Fernández R. Effect of postextubation high-flow nasal cannula vs conventional oxygen therapy on reintubation in low-risk patients: a randomized clinical trial. JAMA. 2016;315(13):1354–1361. doi: 10.1001/jama.2016.2711. [DOI] [PubMed] [Google Scholar]
- 34.Ni YN, Luo J, Yu H, Liu D, Liang BM, Yao R, Liang ZA. Can high-flow nasal cannula reduce the rate of reintubation in adult patients after extubation? A meta-analysis. BMC Pulm Med. 2017;17(1):142. doi: 10.1186/s12890-017-0491-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parashar N, Amidon M, Milad A, Devine A, Yi L, Penk J. Noninvasive neurally adjusted ventilatory assist versus high flow cannula support after congenital heart surgery. World J Pediatr Congenit Heart Surg. 2019;10(5):565–571. doi: 10.1177/2150135119859879. [DOI] [PubMed] [Google Scholar]
- 36.Coon ER, Stoddard G, Brady PW. Intensive care unit utilization after adoption of a ward-based high-flow nasal cannula protocol. J Hosp Med. 2020;15(6):325–330. doi: 10.12788/jhm.3417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Corley A, Rickard CM, Aitken LM, Johnston A, Barnett A, Fraser JF, Lewis SR, Smith AF. High-flow nasal cannulae for respiratory support in adult intensive care patients. Cochrane Database Syst Rev. 2017;5:CD010172. doi: 10.1002/14651858.CD010172.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]