ABSTRACT
Background
Accurate estimates of the usual intake of nutrients are important for monitoring nutritional adequacy and diet quality of populations. In Canada, comprehensive, nationally representative nutrient estimates have not been available since the Canadian Community Health Survey (CCHS)–Nutrition 2004 survey.
Objective
The objective of this research was to assess nutrient intakes, distributions, and adequacy of the intakes of Canadian adults.
Methods
Participants’ first 24-h dietary recall, and the second-day recall from a subset of participants from the recently released CCHS 2015 Public Use Microdata File (PUMF) were used to estimate usual intakes of macronutrients, vitamins, and minerals in adults [≥19 y, excluding lactating females and those with invalid energy intake (EI)]. Usual intakes by DRI age-sex groups were estimated using the National Cancer Institute method, adjusted for age, sex, misreporting status, weekend/weekday, and sequence of recall analyzed (first/second) with outliers removed (final sample, n = 11,992). Usual intakes from food were assessed for prevalence of inadequacy in relation to DRI recommendations.
Results
Canadian macronutrient intakes were within the recommended acceptable macronutrient distribution ranges. EI was 2154 kcal/d for males (19+) and 1626 kcal/d for females (19+). A high prevalence of inadequate intakes was seen for vitamin A (>47%), vitamin D (>94%), vitamin C (>29% for nonsmokers and >59% for smokers), magnesium (>45%), and calcium (>44%), whereas <25% and <40% of adults (19+) had intakes above the adequate intake for fiber and potassium, respectively. Canadians continue to consume sodium in excess of recommendations (74.8% of males and 47.6% of females).
Conclusions
A significant number of Canadian adults may not be meeting recommendations for several essential nutrients, contributing to nutrient inadequacies. These results highlight the nutrients of concern by specific age-sex groups that may be important for public health interventions aimed at improving diet quality and nutrient adequacy for Canadian adults.
Keywords: dietary assessment, CCHS national nutrition survey, nutrient intakes, Canada, nutrient adequacy, National Cancer Institute (NCI) method, adults, DRI age-sex groups
Introduction
Canadians’ adherence to dietary guidelines and recommendations is low and, together with physical inactivity, consumption of energy-rich, nutrient-poor foods predisposes many Canadians to noncommunicable diseases (NCDs) (1). The prevalence of obesity and diet-related NCDs is a concern, with 61.3% of Canadian adults currently overweight or obese (2). Following a healthy eating pattern that includes nutrient-dense foods can help ensure nutrient intakes are met, while supporting periods of growth, development, and aging, as well as a healthy body weight (3).
National, population-level health and nutrition surveys that include information on anthropometric data, socioeconomic status, and dietary intakes were collected in Canada in the d2004 and 2015 cycles of the Canadian Community Health Survey (CCHS)–Nutrition (4). Key findings from 2004 CCHS indicated that a quarter of Canadian adults had total fat intakes above the acceptable macronutrient distribution range (AMDR), whereas many had inadequate intakes of magnesium, calcium, vitamin A, and vitamin D; median sodium intakes also exceeded recommendations (4). Recent findings from analysis of single day intakes from the 2015 CCHS survey revealed that intakes of total sugars has increased over time (5) and that fewer Canadians are consuming the recommended intakes of fruits and vegetables (6). Additionally, Canadians reported consuming a higher percentage of energy from protein and fat and a lower percentage of energy from carbohydrates in 2015 compared with 2004, whereas sodium intakes continued to exceed recommendations (7–9).
Up-to-date, accurate data on the food and nutrient intakes of Canadians is important for monitoring the nutritional health and diet quality of Canadians and can be used to inform policy, public health interventions, clinical practice, and national dietary guidelines (10, 11). To date, Health Canada has released data on intakes of macronutrients (by DRI age-sex groups) and sodium (overall only) using 2015 CCHS–Nutrition data (7, 8); however, these results were from analyses using the first day of dietary recall data only. Recently, Health Canada released an excel spreadsheet of micronutrient intakes and prevalence of inadequacy (9), utilizing the CCHS Share Files (a subset of CCHS 2015, which is not available publicly) without any accompanying interpretation of the results, thereby limiting evaluations and comparability. The objectives of this study, therefore, were to estimate the distributions and usual intakes of macronutrients and micronutrients among Canadian adults (≥19 y) by DRI age-sex groups, and to compare these intakes to the DRIs (12, 13) to assess the prevalence of inadequate and excessive nutrient intakes. SAS and R-Studio macros were developed to analyze the 2015 CCHS–Nutrition Public Use Microdata File (PUMF) of all survey respondents, the latter is freely available and downloadable from Statistics Canada (14). Coding was adapted and developed to apply the National Cancer Institute (NCI) method (15), adjusted for misreporting bias and covariates when calculating nutrient inadequacies, correction for missing measured body weight, and outlier removal.
Methods
Data source and study population
The 2015 CCHS–Nutrition is the Canadian national representative health and nutrition survey which provides food and beverage intake data for Canadians in addition to information on general health and anthropometric measures (14). The publicly available 2015 CCHS–Nutrition PUMF (14) was used for this study. The 2015 CCHS–Nutrition is a multicluster, cross-sectional design with individuals per household randomly selected to complete the survey (16). Two questionnaires were administered per household from 2 January, 2015 to 31 December, 2015: 1) a 24-h dietary recall to assess all food and beverage intake by the selected individual for the past 24-h, and 2) a general health questionnaire to collect general health status, demographic, and lifestyle data. Trained interviewers measured heights and weights and administered the first 24-h dietary recall in-home. (16). A computerized, Canadian modification of the USDA 5-step Automated Multiple-Pass Method was used for all dietary recalls (17), as it captures intakes with less bias and has been shown to accurately estimate group total energy and nutrient intakes (18). Energy and nutrient content of all reported items were derived from Health Canada's Canadian Nutrient File, version 2015 (19).
Respondents from 2015 CCHS–Nutrition included those aged ≥1 y residing in Canada's 10 provinces and excluded individuals living in the territories and on reserve, full-time members of the Canadian Armed Forces, and institutionalized populations (16). In 2015 CCHS–Nutrition, 20,487 respondents completed the initial 24-h dietary recall and a random subsample of 7608 were selected to complete a second recall by phone 3–10 d after the first recall; response rates were 61.6% and 68.6%, respectively (16). Applying the survey weights provided by Statistics Canada ensured all analyses were nationally representative (16). Additional detailed information on 2015 CCHS–Nutrition can be found in the user guide (20).
For the purpose of this study, participants were excluded if they were aged <19 y (n = 6568), lactating (n = 188), or if no food item was reported (n = 4) (16). The 2015 CCHS–Nutrition PUMF does not identify pregnant participants; we were therefore unable to exclude pregnant individuals from analyses. Underweight respondents aged 19 y and older with a BMI <18.5 kg/m2 were excluded since there were no energy expenditure equations for this population (16), leaving a final analytical sample size of n = 11,992 adults after exclusions; 3805 of these respondents completed a second recall (Supplementary Figure 1). All data were collected under the authority of the Statistics Act of Canada.
Adjustment for dietary misreporting
To account for over- and underreporting of energy intake (EI), total energy expenditure (TEE) for each respondent was calculated based on the method proposed by Garriguet (21) and compared with respondents’ reported EI; under- and overreporting was defined as the ratio of EI: TEE <0.7 and >1.42, respectively, whereas those in-between were considered plausible reporters. Institute of Medicine equations were used to predict TEE based on age, sex, measured BMI, and physical activity levels (i.e., sedentary, low active, moderately active, and highly active) (22). For those respondents where measured height and weight were not available, a Statistics Canada correction factor was applied (23). To categorize physical activity levels, respondents’ average physical activity per day in minutes was computed by dividing the CCHS variable “PHSDAPA” (hours of physical activity per week) by 7 and multiplying by 60. Cut-offs to define sedentary, low active, active, and very active were then applied from Health Canada's Reference Guide to Understanding and Using the Data (16).
Assessing nutrient inadequacy
The prevalence of nutrient inadequacy was assessed by comparing Canadians’ estimated usual nutrient intakes to the age- and sex-specific DRI values (24). The DRI reference values in this study included the AMDR, estimated average requirement (EAR), tolerable upper intake level (UL), adequate intake (AI), and chronic disease risk reduction (CDRR) intake (24). Although no DRIs have been defined for some nutrients (e.g., saturated fat), international recommendations for such nutrients were used (25). A low prevalence of nutrient inadequacy was defined as <10% of the sample failing to meet the EAR according to Health Canada definitions (4, 26). The full probability approach was used in place of the EAR cut-point method for accessing iron inadequacy among females of menstruating age, as the iron distribution requirements are known to be skewed for this age/sex group (24, 27–29).
Since the previous 2004 CCHS–Nutrition, advances in statistical methods and new methods have been proposed for the analysis of usual dietary intakes (15, 30). The NCI method has been recommended by a technical working group comprised of statisticians, for the analysis of the 2015 CCHS–Nutrition survey data (15, 30). The NCI method has advantages over earlier methods, as it accounts for correlations between amount consumed and probability of consumption, adjusts for covariates (especially for subpopulations, e.g., by DRI age-sex groups), and provides estimates for usual intakes of episodically consumed foods (31, 32). Further details on the development and application of the NCI method can be found elsewhere (31, 32). Application of the NCI method requires statistical considerations during the analysis of usual dietary intakes (30). These considerations include the type of NCI model used [e.g., 1-part (amount only) or 2-part (both the probability of consumption and the amount consumed)], choice of covariates, stratification compared with pooling the data by specific age-sex groups, and outlier removal (16). Application of the NCI method included these statistical considerations and was guided by the recommendations of Health Canada's working group, detailed in the article by Davis et al. (30).
Both available days of 24-h dietary recall were analyzed to assess usual nutrient intakes using the NCI method (15). The NCI method estimates usual dietary intake from a single day of dietary recall and at least a proportion of second-day dietary recalls, accounting for random error (i.e., day-to-day variation in dietary intake), skewness, and correlations between dietary components in addition to adjustments for covariates of interest (15). In all NCI models, the following covariates were included: age group, sex, misreporting, sequence of recall analyzed (first/second), and weekend/weekday (with Friday considered a weekend day). As indicated by Davis et al., the 1-part (amount only) model was used in cases where zero consumption of a nutrient was <5%; for episodic dietary components, the 2-part model was used (e.g., alcohol) (30). The method used stratified analysis by DRI age-sex groups and pooled analysis of the 19+ males and females and outlier removal due to implausible nutrient intakes (30).
Statistical analysis
Analyses were conducted using R-Studio (v1.1.447) and SAS version 9.4 (SAS Institute Inc.). Data manipulation was conducted using R-Studio, whereas analysis was conducted using SAS. Bootstrap balanced repeated (BRR) replication with 500 replicates was used to estimate all CIs, SEs, and CVs. Survey weights provided by Statistics Canada were applied to all analyses to ensure nationally representative estimates (16). Estimated nutrient intakes were assessed and stratified according to DRI age-sex groups for adults aged 19+ y. Descriptive statistics based on estimated usual dietary intakes (e.g., means, SEs, and percentiles) and prevalence of inadequacy for nutrients were calculated and presented by nutrient for each age-sex group. Data manipulation and analytic codes, for 2015 CCHS PUMF, are available upon request from the authors.
Results
Detailed estimated usual intakes across percentiles (5th, 10th, 25th, 50th, 75th, 90th, and 95th) and per cent below EAR, within AMDR, above AI, and above UL/CDRR, where applicable, by DRI age-sex groups are found in Supplementary Tables 1–28.
Macronutrient intakes
Canadian adults obtained most of their daily EI from carbohydrates (49.3%), followed by total fat (33.8%) and protein (16.4%). A smaller proportion of Canadian adults had intakes within the AMDR for carbohydrates and total fat (70% and 66%, respectively), in comparison to 100% of adults having protein intakes within the AMDR (Table 1; Supplementary Figure 2; Supplementary Tables 2–4).
TABLE 1.
Percentage of total energy from macronutrients and types of dietary fats (%). Usual intakes from food and beverages by DRI age-sex group, Canadian adults (19+ y), n = 11,992 before outlier removal1–3
| Carbohydrates | Protein | Total fat | Saturated fat | PUFA | MUFA | Linoleic acid (LNA) | α-Linolenic acid (ALA) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n 4 | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | |
| Males | ||||||||||||||||||||||||
| 19–30 | 765 | 49.4 | 0.5 | 764 | 16.2 | 0.2 | 765 | 33.4 | 0.3 | 765 | 10.8 | 0.2 | 764 | 7.1 | 0.1 | 765 | 12.3 | 0.2 | 764 | 6.1 | 0.1 | 765 | 0.8 | 0.01 |
| 31–50 | 1838 | 49.3 | 0.4 | 1838 | 16.2 | 0.2 | 1839 | 33.4 | 0.3 | 1839 | 10.8 | 0.2 | 1839 | 7.1 | 0.1 | 1839 | 12.3 | 0.2 | 1839 | 6.1 | 0.1 | 1838 | 0.7 | 0.01 |
| 51–70 | 1964 | 49.3 | 0.4 | 1964 | 16.2 | 0.2 | 1964 | 33.4 | 0.3 | 1964 | 10.8 | 0.2 | 1963 | 7.1 | 0.1 | 1964 | 12.3 | 0.2 | 1964 | 6.1 | 0.1 | 1960 | 0.7 | 0.01 |
| >70 | 1105 | 49.4 | 0.4 | 1105 | 16.2 | 0.2 | 1105 | 33.4 | 0.3 | 1105 | 10.8 | 0.2 | 1105 | 7.1 | 0.1 | 1105 | 12.3 | 0.2 | 1105 | 6.1 | 0.1 | 1105 | 0.7 | 0.01 |
| 19+ | 5670 | 49.4 | 0.6 | 5671 | 16.4 | 0.3 | 5673 | 33.8 | 0.7 | 5673 | 10.7 | 0.2 | 5671 | 7.5 | 0.1 | 5673 | 12.7 | 0.2 | 5672 | 6.2 | 0.1 | 5668 | 0.8 | 0.02 |
| Females | ||||||||||||||||||||||||
| 19–30 | 814 | 49.4 | 0.5 | 815 | 16.2 | 0.2 | 815 | 32.4 | 0.3 | 815 | 10.8 | 0.2 | 814 | 7.1 | 0.1 | 815 | 12.3 | 0.2 | 814 | 6.1 | 0.1 | 814 | 0.7 | 0.01 |
| 31–50 | 2056 | 49.4 | 0.4 | 2056 | 16.2 | 0.2 | 2056 | 33.4 | 0.3 | 2056 | 10.8 | 0.2 | 2056 | 7.1 | 0.1 | 2056 | 12.3 | 0.2 | 2056 | 6.1 | 0.1 | 2054 | 0.7 | 0.01 |
| 51–70 | 2107 | 49.4 | 0.4 | 2107 | 16.2 | 0.2 | 2107 | 33.4 | 0.3 | 2107 | 10.8 | 0.2 | 2107 | 7.1 | 0.1 | 2107 | 12.3 | 0.2 | 2107 | 6.1 | 0.1 | 2107 | 0.7 | 0.01 |
| >70 | 1338 | 49.3 | 0.4 | 1340 | 16.2 | 0.2 | 1340 | 33.4 | 0.3 | 1340 | 10.8 | 0.2 | 1340 | 7.1 | 0.1 | 1340 | 12.3 | 0.2 | 1340 | 6.1 | 0.1 | 1340 | 0.7 | 0.01 |
| 19+ | 6315 | 49.3 | 0.6 | 6318 | 16.4 | 0.3 | 6318 | 33.8 | 0.7 | 6318 | 10.7 | 0.2 | 6317 | 7.5 | 0.1 | 6318 | 12.7 | 0.2 | 6317 | 6.2 | 0.1 | 6315 | 0.8 | 0.02 |
Data Source: Statistics Canada, Canadian Community Health Survey, Nutrition (2015) – Public Use Microdata File (PUMF).
All intakes are based on food and beverage consumption only and exclude intakes from supplements. All tables exclude lactating women, but not pregnant women as they were not identifiable in the PUMF.
The National Cancer Institute method (NCI method) for estimating usual dietary intake was used. The following covariates were adjusted for in all NCI models: age, sex, dietary misreporting status, day of the week (weekend versus weekday), and sequence of dietary recall analyzed (first or second). Outliers for nutrient intake were defined and removed using the methodology reported in Davis et al. (30). The NCI methodology was applied to each nutrient by DRI age-sex grouping and to the 19+ y pooled sample separately, hence small discrepancies between sample sizes and point estimates. The number of respondents removed due to outlier methodology varied between 1 and 33 respondents for each nutrient. All estimates were weighted for population-level estimates using sampling survey weights provided by Statistics Canada. All reported SEs were bootstrapped using the 500 boot weights provided by Statistics Canada.
For detailed intake distributions and comparisons to the acceptable macronutrient distribution range (AMDR) for each nutrient, see Supplementary Tables.
Sample size after outliers were removed.
Energy
Estimated usual mean EI for males 19+ y was 2154 ± 40 kcal/d and for females was 1626 ± 16 kcal/d (Table 2; Supplementary Table 1).
TABLE 2.
Energy, fiber, cholesterol, and alcohol intake. Usual intakes from food and beverages by DRI age-sex group, Canadian adults (19+ y), n = 11,992 before outlier removal1–3
| Energy (kcal/d) | Fiber (g/d) | Cholesterol (mg/d) | Alcohol (g/d) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n 4 | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | |
| Males | ||||||||||||
| 19–30 y | 765 | 2155 | 22 | 765 | 18.1 | 0.5 | 765 | 223 | 5 | 765 | 13.7 | 1.1 |
| 31–50 y | 1839 | 2123 | 32 | 1839 | 18.9 | 0.5 | 1839 | 202 | 8 | 1839 | 13.4 | 1.0 |
| 51–70 y | 1964 | 2072 | 41 | 1965 | 18.2 | 0.4 | 1965 | 215 | 4 | 1964 | 12.5 | 1.0 |
| >70 y | 1105 | 2030 | 59 | 1105 | 17.9 | 0.4 | 1105 | 229 | 7 | 1105 | 12.4 | 1.6 |
| 19+ y | 5673 | 2154 | 40 | 5674 | 18.4 | 0.2 | 5674 | 319 | 9 | 5673 | 13.0 | 1.0 |
| Females | ||||||||||||
| 19–30 y | 815 | 1680 | 21 | 814 | 14.4 | 0.6 | 815 | 288 | 7 | 815 | 6.9 | 0.9 |
| 31–50 y | 2056 | 1641 | 14 | 2054 | 16.3 | 0.5 | 2056 | 297 | 7 | 2056 | 6.9 | 0.9 |
| 51–70 y | 2107 | 1605 | 18 | 2107 | 16.5 | 0.3 | 2106 | 302 | 10 | 2107 | 7.2 | 1.2 |
| >70 y | 1340 | 1563 | 29 | 1339 | 15.5 | 0.4 | 1340 | 311 | 15 | 1340 | 6.9 | 1.2 |
| 19+ y | 6318 | 1626 | 16 | 6314 | 16.2 | 0.3 | 6317 | 227 | 4 | 6318 | 7.0 | 1.0 |
Data Source: Statistics Canada, Canadian Community Health Survey, Nutrition (2015) – Public Use Microdata File (PUMF).
All intakes are based on food and beverage consumption only and exclude intakes from supplements. All tables exclude lactating women, but not pregnant women as they were not identifiable in the PUMF.
The National Cancer Institute method (NCI method) for estimating usual dietary intake was used. The following covariates were adjusted for in all NCI models: age, sex, dietary misreporting status, day of the week (weekend versus weekday), and sequence of dietary recall analyzed (first or second). Outliers for nutrient intake were defined and removed using the methodology reported in Davis et al. (30). The NCI methodology was applied to each nutrient by DRI age-sex grouping and to the 19+ y pooled sample separately, hence small discrepancies between sample sizes and point estimates. The number of respondents removed due to outlier methodology varied between 1 and 33 respondents for each nutrient. All estimates were weighted for population-level estimates using sampling survey weights provided by Statistics Canada. All reported SEs were bootstrapped using the 500 boot weights provided by Statistics Canada.
For detailed intake distributions and comparisons to the DRIs for each nutrient, see Supplementary Tables.
Sample size after outliers were removed.
Saturated, monounsaturated, and polyunsaturated fats
For adults aged 19+ y, mean percentage of total energy from saturated fat was 10.7%± 0.18 (Table 1, Supplementary Figure 2, Supplementary Table 5), with 38% meeting the WHO recommendation of <10% energy from saturated fat (Supplementary Table 5), whereas mean percentage of total energy from MUFAs and PUFAs was 12.7% ± 0.19 and 7.5% ± 0.13, respectively (Table 1, Supplementary Tables 6 and 7). About 76% of Canadian adults had linoleic and α-linolenic acid intakes within the AMDR, with 6.2% ± 0.11 and 0.75% ± 0.02 total energy from linoleic acid and α-linolenic acid, respectively (Table 1; Supplementary Tables 8 and 9). Mean cholesterol intake was 319 ± 8.6 mg/d for males and 227 ± 3.9 mg/d for females, corresponding to a cholesterol density of 148 mg/1000 kcal and 139 mg/1000 kcal for males and females, respectively (Table 2; Supplementary Table 11).
Dietary fiber
Mean fiber intake for all adults aged ≥19 y (males: 18.4 ± 0.2 g/d; females: 16.2 ± 0.3 g/d) fell below their respective AIs (Table 2; Supplementary Table 10), and only 1.3% to 6.3% of males and 4.2% to 21.5% of females had intakes above the AI. However, because there is no EAR for dietary fiber, the prevalence of inadequacy could not be determined.
Vitamins and minerals with an EAR
Detailed distributions of intakes for each nutrient across percentiles (5th, 10th, 25th, 50th, 75th, 90th, and 95th) by DRI age-sex groups are found in Supplementary Tables 13–26.
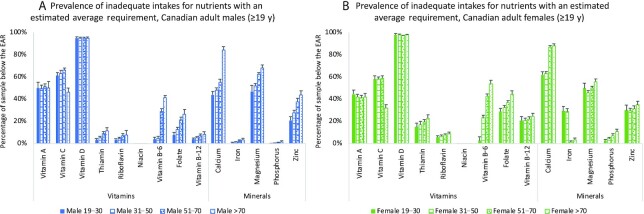
For adults aged 19+ y, a low prevalence of inadequate intakes (<10% of the sample below EAR) was observed for niacin and riboflavin (Table 3, Figure 1, Supplementary Tables 17–18) and phosphorus (Table 3, Figure 1, 9). With respect to B-vitamins, for vitamin B-12 and thiamin (Table 3, Figure 1, Supplementary Tables 16 and 21), a low prevalence of inadequate intakes was seen in Canadian males aged 19+ y, in comparison to females, where the prevalence of inadequate intakes was 21% ± 1.8 and 24.4% ± 9.1, respectively. Although the prevalence of inadequate intakes for vitamin B-6 was low for males aged 19–50 y and females 19–30 y, 29% to 41% of males aged ≥51 y and 23% to 54% of females ≥31 y consumed vitamin B-6 in inadequate amounts (Table 3, Figure 1, Supplementary Table 19). Similarly, although <10% of males aged 19–30 y had inadequate folate intakes, the prevalence of inadequate intakes of folate ranged from >12% for males 31 y and older and >35% for females aged 19–70 y (Table 3, Figure 1, Supplementary Table 20).
TABLE 3.
Micronutrient usual intakes from food and beverages by DRI age-sex group, Canadian adults (19+ y), n = 11,992 before outlier removal1–3
| Vitamin A (RAE/d) | Vitamin D (µg/d) | Thiamin (mg/d) | Riboflavin (mg/d) | Niacin (NE/d) | Vitamin B-6 (mg/d) | Folate (DFE/d) | Vitamin B-12 (µg/d) | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n 4 | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | |
| Males | ||||||||||||||||||||||||
| 19–30 y | 764 | 662 | 36 | 765 | 5.1 | 0.2 | 765 | 1.95 | 0.04 | 764 | 2.26 | 0.05 | 765 | 52.4 | 1.3 | 762 | 2.00 | 0.05 | 765 | 545 | 14 | 765 | 4.7 | 0.1 |
| 31–50 y | 1832 | 669 | 21 | 1837 | 5.1 | 0.1 | 1838 | 1.86 | 0.03 | 1837 | 2.20 | 0.04 | 1839 | 48.1 | 0.9 | 1836 | 1.98 | 0.04 | 1837 | 511 | 10 | 1830 | 4.6 | 0.1 |
| 51–70 y | 1959 | 663 | 18 | 1961 | 5.0 | 0.1 | 1965 | 1.73 | 0.03 | 1964 | 2.08 | 0.07 | 1965 | 42.4 | 0.7 | 1965 | 1.85 | 0.04 | 1964 | 464 | 9 | 1961 | 4.3 | 0.2 |
| >70 y | 1099 | 669 | 39 | 1104 | 5.0 | 0.2 | 1105 | 1.64 | 0.04 | 1105 | 2.02 | 0.12 | 1105 | 38.3 | 0.9 | 1105 | 1.62 | 0.04 | 1105 | 432 | 13 | 1099 | 4.1 | 0.3 |
| 19+ y | 5654 | 665 | 12 | 5667 | 5.1 | 0.1 | 5673 | 1.80 | 0.03 | 5670 | 2.16 | 0.05 | 5674 | 45.5 | 0.7 | 5668 | 1.91 | 0.03 | 5671 | 493 | 9 | 5655 | 4.5 | 0.2 |
| Females | ||||||||||||||||||||||||
| 19–30 y | 814 | 574 | 27 | 815 | 4.1 | 0.3 | 814 | 1.37 | 0.07 | 814 | 1.67 | 0.06 | 814 | 34.8 | 2.2 | 814 | 1.48 | 0.07 | 815 | 417 | 17 | 812 | 3.3 | 0.2 |
| 31–50 y | 2054 | 589 | 15 | 2055 | 4.2 | 0.2 | 2055 | 1.37 | 0.04 | 2055 | 1.67 | 0.03 | 2056 | 33.8 | 1.1 | 2056 | 1.52 | 0.05 | 2056 | 403 | 10 | 2048 | 3.3 | 0.1 |
| 51–70 y | 2101 | 598 | 15 | 2107 | 4.3 | 0.1 | 2106 | 1.34 | 0.03 | 2107 | 1.65 | 0.02 | 2107 | 32.1 | 0.5 | 2105 | 1.40 | 0.02 | 2107 | 381 | 7 | 2098 | 3.2 | 0.1 |
| >70 y | 1336 | 595 | 22 | 1340 | 4.3 | 0.1 | 1340 | 1.28 | 0.04 | 1339 | 1.60 | 0.03 | 1340 | 29.7 | 0.6 | 1340 | 1.29 | 0.03 | 1340 | 352 | 9 | 1337 | 3.1 | 0.1 |
| 19+ y | 6305 | 590 | 12 | 6317 | 4.2 | 0.2 | 6315 | 1.36 | 0.04 | 6315 | 1.68 | 0.02 | 6317 | 33.2 | 0.9 | 6315 | 1.46 | 0.03 | 6318 | 391 | 8 | 6295 | 3.2 | 0.1 |
| Calcium (mg/d) | Iron (mg/d) | Magnesium (mg/d) | Phosphorus (mg/d) | Zinc (mg/d) | Potassium (mg/d) | Sodium (mg/d) | |||||||||||||||
| n 4 | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | n | Mean | SE | |
| Males | |||||||||||||||||||||
| 19–30 y | 765 | 901 | 21 | 765 | 15.0 | 0.3 | 765 | 352 | 15 | 764 | 1560 | 32 | 765 | 13.5 | 0.4 | 764 | 3073 | 66 | 766 | 3350 | 76 |
| 31–50 y | 1839 | 868 | 20 | 1837 | 14.4 | 0.3 | 1838 | 358 | 7 | 1837 | 1484 | 26 | 1839 | 12.7 | 0.4 | 1839 | 3028 | 47 | 1839 | 3200 | 59 |
| 51–70 y | 1965 | 813 | 29 | 1964 | 13.5 | 0.4 | 1963 | 328 | 6 | 1965 | 1372 | 43 | 1964 | 11.5 | 0.4 | 1965 | 2927 | 70 | 1965 | 2972 | 77 |
| >70 y | 1105 | 722 | 43 | 1105 | 12.8 | 0.5 | 1104 | 309 | 10 | 1105 | 1299 | 70 | 1105 | 10.7 | 0.5 | 1104 | 2877 | 107 | 1105 | 2831 | 126 |
| 19+ y | 5674 | 849 | 23 | 5671 | 14.0 | 0.3 | 5670 | 341 | 7 | 5671 | 1440 | 31 | 5673 | 12.1 | 0.4 | 5672 | 2974 | 52 | 5674 | 3133 | 66 |
| Females | |||||||||||||||||||||
| 19–30 y | 815 | 746 | 23 | 815 | 10.9 | 0.4 | 815 | 263 | 11 | 815 | 1172 | 53 | 815 | 9.0 | 0.5 | 815 | 2386 | 88 | 815 | 2393 | 99 |
| 31–50 y | 2055 | 741 | 16 | 2054 | 11.0 | 0.2 | 2056 | 287 | 6 | 2056 | 1146 | 23 | 2056 | 8.9 | 0.2 | 2055 | 2423 | 41 | 2056 | 2352 | 46 |
| 51–70 y | 2107 | 686 | 15 | 2107 | 10.6 | 0.1 | 2107 | 278 | 4 | 2107 | 1102 | 16 | 2107 | 8.6 | 0.2 | 2107 | 2434 | 39 | 2107 | 2279 | 33 |
| >70 y | 1340 | 670 | 25 | 1339 | 9.9 | 0.2 | 1340 | 263 | 6 | 1340 | 1032 | 22 | 1340 | 8.2 | 0.3 | 1340 | 2395 | 55 | 1340 | 2155 | 48 |
| 19+ y | 6317 | 720 | 10 | 6315 | 10.8 | 0.1 | 6318 | 279 | 4 | 6318 | 1120 | 14 | 6318 | 8.8 | 0.1 | 6317 | 2431 | 27 | 6318 | 2325 | 32 |
Data Source: Statistics Canada, Canadian Community Health Survey, Nutrition (2015) – Public Use Microdata File (PUMF).
All intakes are based on food and beverage consumption only and exclude intakes from supplements. All tables exclude lactating women, but not pregnant women as they were not identifiable in the PUMF.
The National Cancer Institute method (NCI method) for estimating usual dietary intake was used. The following covariates were adjusted for in all NCI models: age, sex, dietary misreporting status, day of the week (weekend versus weekday), and sequence of dietary recall analyzed (first or second). Outliers for nutrient intake were defined and removed using the methodology reported in Davis et al. (30). The NCI methodology was applied to each nutrient by DRI age-sex grouping and to the 19+ y pooled sample separately, hence small discrepancies between sample sizes and point estimates. The number of respondents removed due to outlier methodology varied between 1 and 33 respondents for each nutrient. All estimates were weighted for population-level estimates using sampling survey weights provided by Statistics Canada. All reported SEs were bootstrapped using the 500 boot weights provided by Statistics Canada. DFE; Dietary Folate Equivalent, NE; Niacin Equivalent, RAE; Retinol Activity Equivalent.
For detailed intake distributions and comparisons to the DRIs for each nutrient, see Supplementary Tables.
Sample size after outliers were removed.
FIGURE 1.
Prevalence of inadequate intakes for nutrients with an estimated average requirement of Canadian adults (aged ≥19 y) A) males and B) females. Data Source: Statistics Canada, Canadian Community Health Survey, Nutrition (2015) – Public Use Microdata File. All intakes are based on food and beverage consumption only and exclude intakes from vitamin or mineral supplements. The National Cancer Institute method (NCI method) for estimating usual dietary intake was used. The following covariates were adjusted for in all NCI models: age, sex, dietary misreporting status, day of the week (weekend versus weekday), and sequence of dietary recall analyzed (first or second). Outliers for nutrient intake were defined and removed using the methodology reported in Davis et al. (31). The number of respondents removed due to outlier methodology varied between 1 and 33 respondents for each nutrient. The analytical sample size before outlier removal was n = 11,992. All estimates were weighted for population-level estimates using sampling survey weights provided by Statistics Canada. All reported SEs were bootstrapped using the 500 boot weights provided by Statistics Canada. EAR, estimated average requirement.
With respect to the consumption of trace elements, a low prevalence of inadequate iron intake was seen in males and females aged ≥51 y; however, nearly 30% of females aged 19–50 y consumed iron in amounts that fell below the EAR (Table 3, Figure 1, Supplementary Table 23). A significant proportion of Canadian adults had inadequate intakes of zinc (21.1% to 43.5% for males and 29.8% to 34.8% for females) (Table 3, Figure 1, Supplementary Table 26). The prevalence of inadequate intakes was also high for magnesium and calcium, increasing with older age (Table 3, Figure 1, Supplementary Tables 22 and 24). More than 40% of males and 60% of females had inadequate calcium intakes, respectively, with ≤84% ± 3.3 for males and 88% ± 1.8 for females aged 71+ y. Similarly, more than half the sample of both males (58% ± 2.1) and females (66% ± 2.1) had inadequate intakes of magnesium, also increasing with older age (Table 3, Figure 1, Supplementary Table 24).
The prevalence of inadequate intakes was highest for vitamin A, vitamin C, and vitamin D. More than 40% of Canadians aged 19 and older (males: 50.5% ± 1.8; females: 47% ± 1.8) consumed vitamin A in quantities below the EAR (Table 3, Figure 1, Supplementary Tables 13–15). Although the prevalence of inadequate vitamin C intakes ranged from 38% to 64% in males and 28% to 59% in females (inclusive of smokers/nonsmokers), nonsmokers had a relatively low prevalence of inadequate intakes of this nutrient in comparison to smokers (41% ± 4 of nonsmoking males and 29% ± 2 of nonsmoking females compared with 64% ± 2 for smoking males and 59% ± 2 for smoking females) (Table 4, Figure 1, Supplementary Table 14). Almost all Canadian adults had a high prevalence of inadequate intakes of vitamin D (males: 94% ± 0.8 and females: 98% ± 0.8) (Table 3, Figure 1, Supplementary Table 15).
TABLE 4.
Vitamin C (mg/d). Usual intakes from food and beverages by DRI age-sex group and smoking status, Canadian adults (19+ y), n = 11,992 before outlier removal1–3
| Smoking status | n 4 | Mean | SE | |
|---|---|---|---|---|
| Males | ||||
| 19–30 y | — | 765 | 105 | 5 |
| 31–50 y | — | 1839 | 103 | 4 |
| 51–70 y | — | 1965 | 98 | 3 |
| >70 y | — | 1105 | 94 | 3 |
| 19+ y | Nonsmoker | 4431 | 100 | 3 |
| Smoker | 1237 | 102 | 3 | |
| Females | ||||
| 19–30 y | — | 815 | 95 | 4 |
| 31–50 y | — | 2056 | 95 | 3 |
| 51–70 y | — | 2107 | 94 | 2 |
| >70 y | — | 1340 | 90 | 3 |
| 19+ y | Nonsmoker | 5248 | 94 | 2 |
| Smoker | 1067 | 94 | 3 |
Data Source: Statistics Canada, Canadian Community Health Survey, Nutrition (2015) – Public Use Microdata File (PUMF).
Intakes are based on food and beverage consumption only and exclude intakes from vitamin or mineral supplements. All tables exclude lactating women, but not pregnant women, as they were not identifiable in the PUMF.
The National Cancer Institute method (NCI method) for estimating usual dietary intake was used. The following covariates were adjusted for in all NCI models: age, sex, dietary misreporting status, day of the week (weekend compared with weekday), and sequence of dietary recall analyzed (first or second). Outliers for nutrient intake were defined and removed using the methodology reported in Davis et al. (30). The NCI methodology was applied to each nutrient by DRI age-sex grouping and to the 19+ y pooled sample separately, hence small discrepancies between sample sizes and point estimates. All estimates were weighted for population-level estimates using sampling survey weights provided by Statistics Canada. All reported SEs were bootstrapped using the 500 boot weights provided by Statistics Canada.
For detailed intake distribution and comparisons to the DRIs, see Supplementary Tables.
Sample size after outliers were removed.
The prevalence of intakes greater than the UL from foods and beverages was very low for most vitamins and minerals.
Vitamins and minerals with an AI and CDRR
The mean potassium intakes of Canadian adults 19+ y (males: 2974 ± 52 mg/d and females: 2431 ± 27 mg/d) were below the AI of 3400 mg/d for males and 2600 mg/d for females (Table 3, Supplementary Table 27).
The mean sodium intakes for all Canadian adults exceeded the CDRR (2300 mg/d). Males had higher sodium intakes compared with females (3133 mg/d compared with 2325 mg/d), with 75% of males aged 19+ y exceeding the CDRR compared with 48% of females aged 19+ y; males 19–30 y had the highest sodium intake at 3350 mg/d (Table 3, Supplementary Table 28).
Discussion
This study presents results from the most recent large, nationally representative survey of Canadian adults to estimate usual nutrient intakes and assess the prevalence of inadequate intakes in relation to the DRIs. The majority of Canadian adults consumed macronutrients within the AMDR; however, inadequate intakes of some B vitamins and trace elements (in specific age-sex groups) and of vitamin A, vitamin D, vitamin C, magnesium, and calcium were observed. For nutrients with an AI, adults may not be meeting their needs for potassium and fiber and the majority of Canadian adults consumed sodium in excess of CDRR recommendations.
When adjusted for age and sex using 2-d dietary recalls, EIs in this study were found to be slightly lower compared with earlier 2015 CCHS results (7, 33), which used only the 1-d dietary recall. Similarly, the proportion of total energy from carbohydrates, total fat, and protein differed slightly from those published using the 1-d recall data (7) but were similar to those using 2-d recall data (9). EIs (adjusted for age and sex) were also slightly lower (except for females aged >70 y) compared with those published for the 2004 CCHS–Nutrition (34, 35). These results likely do not represent a substantial change in energy or macronutrient intakes over the last 11 y; rather, differences are likely due to small differences in data collection and survey design between 2004 and 2015 CCHS–Nutrition (16), as well as small methodological differences in the ascertainment of Canadians’ EI between this study and other published studies (34, 35). The methodological differences in surveys and with other published studies are discussed further below (in Strengths and Limitations).
Intakes of saturated fat and monounsaturated fat were similar to those found in 2004 (4, 35), and the majority of Canadian adults were meeting intake recommendations for ω-3s, although intakes were higher than those in 2004 (35).
Estimating the prevalence of inadequate fiber intake is not possible given the limited usefulness of the AI in assessing usual nutrient intakes of groups (22, 24), however, intakes were comparable to 2004 (35), with >80% of Canadians having intakes below the AI. Despite this limitation, promoting increased fiber intake remains important, as other research indicates intakes of fruits and vegetables have decreased, these being important sources of fiber and other nutrients (36).
Micronutrient intakes are largely consistent with data from the 2004 survey (4), with the recently released 2015 CCHS data tables (9), and with results for the US population (37, 38). In contrast to the 2004 survey (22), a larger proportion of nonsmoking Canadians had a high prevalence of inadequate intakes of vitamin C (29–41% of the 2015 CCHS sample compared with 10–35% in 2004 CCHS). Methodological differences, such as the handling of outliers and covariate adjustment in our study, may account for some of these differences.
A higher prevalence of inadequate intakes of vitamin D was found for Canadian adults, compared with 2004 (22). This is likely a reflection of a significant decrease in fluid milk consumption, which has decreased by almost 20 L per capita per year since 2004 (39, 40), as all fluid milk in Canada is fortified with vitamin D, and the change in DRI recommendations from an AI (5–15 µg/d, depending on age-sex group) to a higher EAR (10 µg/d for adults aged 19+ y) (12). Estimates of the prevalence of inadequate intakes of vitamin D from food, however, does not necessarily reflect status, as vitamin D can be synthesized by the body from sunlight (41). Additionally, this study does not consider vitamin D intake from supplement use. Approximately 34% of Canadians took a vitamin D supplement (based on information collected during the past month), with the likelihood of supplement use highest among older adults (33). Data from the Canadian Health Measures Survey (cycle 2) showed that only 32% of the Canadians had blood concentrations of vitamin D below international thresholds for bone health (42). Canada's Food Guide (10) was recently updated with the “Milk and Alternatives” and “Meat and Alternatives” as now part of a protein food group. It will, therefore, be important to monitor vitamin D intakes and status in the coming years.
There was a slightly higher prevalence of inadequate intakes of vitamin A, calcium, and magnesium compared with CCHS 2004, likely also a reflection of the change in fluid milk consumption and lower intakes of vegetables (39, 40).
Sodium intakes in this study were similar to those published for 2015 CCHS–Nutrition (9), indicating that most Canadians are still consuming too much sodium, particularly males aged 19–30 y. Although the results in the present study indicate sodium intakes were lower compared with 2004, most likely due to changes in the food supply (4, 35), some of the variation may also be due to methodological differences. However, due to the continued high prevalence of hypertension and high sodium intakes among Canadians, sodium reduction, in the form of reformulation of the food supply and other proposed regulations such as mandatory front-of-pack labeling, continue to be public health policy priorities in Canada (43, 44).
Results for Canada are similar to other international studies identifying nutrients with the highest prevalence of inadequacy, although survey methodologies, times of data collection, and dietary habits differ across countries. The 2015–2016 US NHANES found that ∼75% of the US adult population follows an eating pattern that is low in fruits and vegetables, resulting in excessive intakes of saturated fat, sodium and added sugars, and micronutrient inadequacies (37, 45). A study evaluating the consumption of major foods and nutrients across 195 countries also found less than recommended intakes of foods and nutrients that should be encouraged, with intakes of foods and nutrients that should be limited exceeding recommended levels (46). Similarly, the prevalence of nutrient inadequacy in Europe was highest for calcium, vitamin C, vitamin D, and magnesium (47, 48).
Considering the less than recommended intakes for many nutrients by Canadian adults, there is a continuing need for policies and programs to foster healthy eating. Addressing this need, Health Canada recently released the Healthy Eating Strategy, to improve Canadians’ nutrition and diet quality at the population level (11), including revised nutrient labels, a revised Canada's Food Guide in 2019 (10), updated sodium targets (44), a trans-fat ban, proposed regulations requiring mandatory front-of-pack labels (49), and restrictions on marketing to kids (50). The results of this study will be critical in providing baseline estimates to monitor the impact of such policies on improved diet quality and nutrient intakes of Canadians.
Strengths and limitations
This study is novel as it provides results based on the use of publicly available files (i.e., 2015 CCHS–Nutrition PUMF) to analyze usual nutrient intakes and prevalence of inadequacy among Canadian adults, using 2 d of dietary recalls, stratified by age-sex groups in addition to providing interpretation of the results and implications of these findings. The use of 2-d dietary recalls and the NCI method (15) strengthens our results, as most Canadian research published to date utilized only a single day of dietary recall, which is inappropriate to estimate usual intake. Additionally, this study accounts for misreporting bias, corrects for misreporting of weight data (i.e., BMI correction), adjusts for covariates when calculating nutrient inadequacies, and applied a robust outlier removal method recommended by Health Canada (30). The present study also provides detailed tabulations and interpretation of usual intake means, percentiles, and proportions meeting recommendations by DRI age-sex groups as well as pooled estimates for all adults (19+ y) in the supplementary tables, allowing application to research, public health, and policy.
This study, as in other national nutrition surveys, is limited by the use of self-reported measurement of intakes, which are subject to both random and systematic measurement error. We have limited this report to the nutrient estimates from food and beverages only; the results do not account for intakes from supplements. The 2015 CCHS–Nutrition relies on estimating nutrient intakes based on the foods and beverages found in the most recent Canadian Nutrient File (51), which may not be updated for all nutrients and/or products, therefore the estimates are reflective of the currency of the Canadian Nutrient File 2015. Additionally, our ability to make direct comparisons between the 2004 and 2015 CCHS–Nutrition is limited due to some of the methodological differences in data collection, data processing, and analysis between the 2 surveys (16). Some of the methodological differences include different sample sizes and response rates, updates to the nutrient databases, use of the Software for Intake Distribution Estimation (SIDE) method (2004 CCHS–Nutrition) compared with the NCI method (used in this study for 2015 CCHS–Nutrition), and adjustment for certain covariates. Further details on the differences between the 2 survey cycles can be found elsewhere (16).
Conclusions
The present study suggests that a significant number of Canadian adults may not be meeting recommendations for a number of essential nutrients, i.e., vitamin A, vitamin C, vitamin D, magnesium, calcium, and potentially potassium as well as for some B-vitamins in certain age-sex groups. In addition, sodium intakes of the Canadian population were very high, with most Canadian adults exceeding the UL (and current CDRR). These results highlight nutrients of concern by specific age-sex groups that may be important for public health interventions aimed at improving diet quality and nutrient adequacy of Canadian adults.
Supplementary Material
Acknowledgments
We would like to acknowledge the assistance of Mahsa Jessri (Assistant Professor, University of British Columbia) for estimates of EI.
The authors’ contributions were as follows—APN, MA, and MRL'A: conceptualized and designed the study; APN: developed the coding for the analysis; APN and MA: conducted the statistical analyses, drafted and revised the manuscript; MRL'A: reviewed the manuscript; and all authors: read and approved the final manuscript. MA was Mitacs Elevate Postdoctoral Fellowship from September 2017 to September 2019, which is jointly funded by Government of Canada Mitacs Program and Nestlé Research Centre; however, neither of the organizations had a role in this research. All other authors report no conflicts of interest.
Notes
Support for this research was obtained from the Earle W McHenry Research Chair Award (to MRL'A), Lawson Centre for Child Nutrition and Health Grant (#002/2017/471141), and Canadian Institutes of Health Research Project Grant (#152179).
Supplemental Tables 1–28 and Supplemental Figures 1 and 2 are available from the “Supplementary data” link in the online posting of the article and from the same link in the online table of contents at https://academic.oup.com/ajcn/.
Abbreviations used: AI, adequate intake; AMDR, acceptable macronutrient distribution ranges; CCHS, Canadian Community Health Survey; CDRR, chronic disease risk reduction; EAR, estimated average requirement; EI, energy intake; NCD, noncommunicable disease; NCI, National Cancer Institute; PUMF, Public Use Microdata File; SIDE, software for intake distribution estimation; TEE, total energy expenditure; UL, tolerable upper intake level.
Contributor Information
Mavra Ahmed, Department of Nutritional Sciences, University of Toronto, Toronto, Canada; Joannah and Brian Lawson Center for Child Nutrition, University of Toronto, Toronto, Canada.
Alena (Praneet) Ng, Department of Nutritional Sciences, University of Toronto, Toronto, Canada.
Mary R L'Abbe, Department of Nutritional Sciences, University of Toronto, Toronto, Canada; Joannah and Brian Lawson Center for Child Nutrition, University of Toronto, Toronto, Canada.
Data Availability
Data described in the manuscript, reference guide, and data dictionary are publicly and freely available without restriction at Statistics Canada, https://www150.statcan.gc.ca/n1/pub/11-625-x/11-625-x2010000-eng.htm. Analytic code (R-Studio and SAS) can be made available to researchers upon request to the author.
References
- 1.Bacon SL, Campbell NRC, Raine KD, Tsuyuki RT, Khan NA, Arango M, Kaczorowski J. Canada's new Healthy Eating Strategy: implications for health care professionals and a call to action. Can Pharm J (Ott). 2019;152(3):151–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Statistics Canada. Table 13-10-0794-01: Measured adult body mass index (BMI) (World Health Organization classification), by age group and sex, Canada and provinces, Canadian Community Health Survey - Nutrition 2017 [Internet]. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310079401&pickMembers%5B0%5D=1.1&pickMembers%5B1%5D=2.1&pickMembers%5B2%5D=3.1&pickMembers%5B3%5D=5.5. [Google Scholar]
- 3.Smolin LA, Grosvenor MB, Gurfinkel D. Nutrition: Science and Applications. Third Canadian edition. Toronto, Ontario: John Wiley & Sons Canada, Ltd; 2020. [Google Scholar]
- 4.Health Canada . Do Canadian adults meet their nutrient requirements through food intake alone? [Electronic monograph in PDF format]. [Ottawa]: Health Canada; 2012. [Internet]. Available from: http://resource.library.utoronto.ca/eir/EIRdetail.cfm?Resources__ID=1579433. [Google Scholar]
- 5.Langlois K, Garriguet D, Gonzalez A, Sinclair S, Colapinto CK. Change in total sugars consumption among Canadian children and adults. Health Rep. 2019;30(1):10─19. [PubMed] [Google Scholar]
- 6.Colapinto CK, Graham J, St-Pierre S. Trends and correlates of frequency of fruit and vegetable consumption, 2007 to 2014. Health Rep. 2018;29(1):9–14. [PubMed] [Google Scholar]
- 7.Statistics Canada . Canadian Community Health Survey – Nutrition: Nutrient Intakes from Food and Nutritional Supplements; Available in CANSIM: tables 105–2017 to 105–2022, 105–2027 and 105–2028. 2017; [Internet]. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/170620/dq170620b-cansim-eng.htm. [Google Scholar]
- 8.Health Canada . Sodium Intake of Canadians in 2017. 2017; [Internet]. Available from: https://www.canada.ca/en/health-canada/services/publications/food-nutrition/sodium-intake-canadians-2017.html#a9. [Google Scholar]
- 9.Health Canada . Usual Intakes from Food for Energy, Nutrients and Other Dietary Components (2004 and 2015 CCHS-Nutrition) derived from Statistics Canada's 2004 and 2015 Canadian Community Health Survey, Nutrition, Share file Ottawa. 2019; [Internet]. Available from: https://open.canada.ca/data/en/dataset/31599960-2c1e-4d90-a9d9-979ad0e1abb4. [Google Scholar]
- 10.Health Canada . Canada's Food Guide 2019. 2019. [Internet]. Available from: https://food-guide.canada.ca/en/. [Google Scholar]
- 11.Health Canada . Healthy Eating Strategy: Toward Front-of-Package Nutrition Labels for Canadians: Consultation Document Canada. 2016; [Internet]. Available from: https://www.canada.ca/en/services/health/campaigns/vision-healthy-canada/healthy-eating.html. [Google Scholar]
- 12.Institute of Medicine . Dietary Reference Intakes 1995–2019. 2019; [Internet].Available from:https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/dietary-reference-intakes/consumer-guide-dris-dietary-reference-intakes.html. [Google Scholar]
- 13.National Academies of Sciences and Medicine . Dietary Reference Intakes for Sodium and Potassium. Oria M, Harrison M, Stallings VA, . Washington, DC: National Academies Press; 2019. [PubMed] [Google Scholar]
- 14.Statistics Canada . Canadian Community Health Survey – Nutrition: Public Use Microdata File. 2019; [Internet]. Available from: https://www150.statcan.gc.ca/n1/en/catalogue/82M0024X. [Google Scholar]
- 15.National Cancer Institute . Usual Dietary Intake: SAS Macros for the NCI Method. 2018; [Internet]. Available from: https://epi.grants.cancer.gov/diet/usualintakes/macros.html. [Google Scholar]
- 16.Health Canada . 2015 Canadian Community Health Survey – Reference Guide to Understanding and Using the Data. 2017; [Internet]. Available from: http://sda.chass.utoronto.ca/sdaweb/dli2/cchs/cchs2015_nu/more_doc/CCHS_NU_2015_PUMF_User_Guide.pdf; https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/reference-guide-understanding-using-data-2015.html#a4.2. [Google Scholar]
- 17.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul D, Sebastian R, Kuczynski K, Ingwersen Let al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr. 2008;88(2):324–32. [DOI] [PubMed] [Google Scholar]
- 18.National Cancer Institute . Dietary Assessment Primer 2019. [Internet]. Available from: https://dietassessmentprimer.cancer.gov. [Google Scholar]
- 19.Health Canada . Canadian Nutrient File 2015. [Internet]. Available from: https://food-nutrition.canada.ca/cnf-fce/index-eng.jsp. [Google Scholar]
- 20.Health Canada . 2015 Canadian Community Health Survey – Nutrition User Guide. 2018; [Internet]. Available from: http://sda.chass.utoronto.ca/sdaweb/dli2/cchs/cchs2015_nu/more_doc/CCHS_NU_2015_PUMF_User_Guide.pdf. [Google Scholar]
- 21.Garriguet D. Accounting for Misreporting When Comparing Energy Intake Across Time in Canada. 2018; [Internet]. Available from: https://www150.statcan.gc.ca/n1/en/pub/82-003-x/2018005/article/54965-eng.pdf. [PubMed] [Google Scholar]
- 22.Institute of Medicine (U.S.). Panel on Macronutrients, Institute of Medicine (U.S.) . Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: National Academies Press; 2005. p. xxv, 1–972, 1259-331. [Google Scholar]
- 23.Statistics Canada . Correction Equations to Adjust Self-Reported Estimates of Weight, Height and Body Mass Index (BMI), by Sex, Full and Reduced Models, Household Population Aged 18 Years or Older. 2015; [Internet]. Available from: https://www150.statcan.gc.ca/n1/pub/82-003-x/2008003/article/10680/t/5202385-eng.htm. [Google Scholar]
- 24.Institute of Medicine (U.S.). Subcommittee on Interpretation and Uses of Dietary Reference Intakes, Institute of Medicine (U.S.). Subcommittee on Upper Reference Levels of Nutrients, Institute of Medicine (U.S.) . Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes. Applications in Dietary Assessment: a report of the Subcommittees on Interpretation and Uses of Dietary Reference Intakes and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food and Nutrition Board, Institute of Medicine. Washington, DC: National Academies Press; 2000. pp. xvii, 287. [Google Scholar]
- 25.World Health Organization . Healthy Diet 2020. [Internet]. Available from: https://www.who.int/news-room/fact-sheets/detail/healthy-diet. [Google Scholar]
- 26.Katamay SW, Esslinger KA, Vigneault M, Johnston JL, Junkins BA, Robbins LG, Sirois I, Jones-Mclean EM, Kennedy A, Busy Met al. Eating well with Canada's Food Guide (2007): development of the food intake pattern. Nutr Rev. 2007;65(4):155–66. [DOI] [PubMed] [Google Scholar]
- 27.Beaton G. Beaton's Full Probability Method for Iron. 2015; [Internet]. Available from: https://www.abs.gov.au/AUSSTATS/abs@.nsf/Lookup/4363.0.55.001Chapter6510312011-13. [Google Scholar]
- 28.Health Canada and Statistics Canada . Nutrient Intakes from Food: Provincial, Regional and National Summary Data Tables Volume 2. Ottawa: Ministry of Health; 2000; [Internet]. Available from:https://www.canada.ca/en/health-canada/services/food-nutrition/food-nutrition-surveillance/health-nutrition-surveys/canadian-community-health-survey-cchs/canadian-community-health-survey-cycle-2-2-nutrition-focus-food-nutrition-surveillance-health-canada.html#order. [Google Scholar]
- 29.Institute of Medicine (US) Panel on Micronutrients . Panel on Micronutrients Subcommittees on Upper Reference Levels of Nutrients and of Interpretation and Use of Dietary Reference Intakes and the Standing Committee on the Scientific Evaluation of Dietary Reference Intakes. Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc [S.l.]. Washington, DC: National Academies Press; 2001; [Internet]. Available from: http://www.nap.edu/openbook.php?record_id=10026http://www.ncbi.nlm.nih.gov/books/NBK222310. [PubMed] [Google Scholar]
- 30.Davis KA, Gonzalez A, Loukine L, Qiao C, Sadeghpour A, Vigneault M, Wang KC, Ibanez D. Early experience analyzing dietary intake data from the Canadian Community Health Survey-Nutrition Using the National Cancer Institute (NCI) Method. Nutrients. 2019;11(8):1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith S, Subar A, Dodd K. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med. 2010;29(27):2857–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll R, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc. 2006;106(10):1575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Statistics Canada . Canadian Community Health Survey – Nutrition: Nutrient Intakes From Food and Nutritional Supplements. 2017; [Internet]. Available from: https://www150.statcan.gc.ca/n1/daily-quotidien/170620/dq170620b-eng.htm. [Google Scholar]
- 34.Garriguet D, Statistics Canada . Health Statistics Division. Overview of Canadians' Eating Habits, 2004 [Electronic monograph in PDF format]. Ottawa: Statistics Canada, Health Statistics Division; 2006; [Internet]. Available from: http://publications.gc.ca/pub?id=294155&sl=0. [Google Scholar]
- 35.Health Canada and Statistics Canada .Canadian Community Health Survey, Cycle 2.2, Nutrition (2004) - Nutrient Intakes from Food, Volume 1–3: Provincial, Regional and National Summary Data Tables. Ottawa: Statistics Canada; 2009. [Google Scholar]
- 36.Statistics Canada . Fruit and Vegetable Consumption. 2017. [Internet]. Available from: https://www150.statcan.gc.ca/n1/pub/82-625-x/2019001/article/00004-eng.htm. [Google Scholar]
- 37.Cowan AE, Jun S, Tooze JA, Eicher-Miller HA, Dodd KW, Gahche JJ, Guenther PM, Dwyer J, Potischman N, Bhadra Aet al. Total usual micronutrient intakes compared to the dietary reference intakes among U.S. Adults by Food Security Status. Nutrients. 2019;12(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Herrick KA, Rossen LM, Parsons R, Dodd KW. Estimating usual dietary in take from National Health and Nutrition Examination survey data using the National Cancer Institute Method. Vital Health Stat. 2018;(178):1–63. [PubMed] [Google Scholar]
- 39.Tugault-Lafleur CN, Black JL. Differences in the quantity and types of foods and beverages consumed by Canadians between 2004 and 2015. Nutrients. 2019;11(3):526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Statista . Consumption of Milk Per Capita in Canada from 2004 to 2018. 2020; [Internet]. Available from: https://www.statista.com/statistics/438584/consumption-of-milk-per-capita-canada/. [Google Scholar]
- 41.Statistics Canada . Health at a Glance: Vitamin D Blood Levels of Canadians. 2015; [Internet]. Available from: https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11727-eng.htm. [Google Scholar]
- 42.Janz T, Pearson C. Vitamin D Blood Levels of Canadians. 2013; [Internet]. Available from: https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11727-eng.pdf. [Google Scholar]
- 43.Health Canada. Sodium Working Group . Sodium Reduction Strategy for Canada Recommendations of the Sodium Working Group [Electronic monograph in PDF format]. Ottawa: Health Canada; 2010; [Internet]. Available from: http://resource.library.utoronto.ca/eir/EIRdetail.cfm?Resources__ID=1573077. [Google Scholar]
- 44.Health Canada . Voluntary Sodium Reduction Targets for Processed Foods 2020–2025. 2020; [Internet]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/sodium/sodium-reduced-targets-2020-2025.html. [Google Scholar]
- 45.Dietary Guidelines Advisory Committee Members . Shifts Needed To Align With Healthy Eating Patterns. U.S Department of Health and Human Services; U.S. Department of Agriculture; 2015; [Internet]. Available from: https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/chapter-2/. [Google Scholar]
- 46.Global Burden of Disease Diet Collaborators . Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet North Am Ed. 2019;393(10184):1958–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Touvier M, Lioret S, Vanrullen I, Bocle JC, Boutron-Ruault MC, Berta JL, Voltier JL. Vitamin and mineral inadequacy in the French population: estimation and application for the optimization of food fortification. Int J Vitam Nutr Res. 2006;76(6):343–51. [DOI] [PubMed] [Google Scholar]
- 48.Roman Vinas B, Ribas Barba L, Ngo J, Gurinovic M, Novakovic R, Cavelaars A, de Groot L, Veer P, Matthys C, Serra-Majem L. Projected prevalence of inadequate nutrient intakes in Europe. Ann Nutr Metab. 2011;59(2–4):84–95. [DOI] [PubMed] [Google Scholar]
- 49.Health Canada . Summary of Proposed Amendments Published in Canada Gazette, Part I: Nutrition Symbols, Other Labelling Provisions, Partially Hydrogenated Oils and Vitamin D. 2018; [Internet]. Available from: https://www.canada.ca/en/health-canada/programs/consultation-front-of-package-nutrition-labelling-cgi/summary-of-proposed-amendments.html. [Google Scholar]
- 50.Health Canada . Restricting Advertising of Certain Foods to Children Under 13 Years of Age. 2019; [Internet]. Available from: https://www.canada.ca/en/health-canada/services/marketing-health-claims/restricting-advertising-children.html. [Google Scholar]
- 51.Health Canada . Search Online for Foods Using the Canadian Nutrient File. 2010; [Internet]. Available from: https://www.canada.ca/en/health-canada/services/food-nutrition/healthy-eating/nutrient-data.html. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, reference guide, and data dictionary are publicly and freely available without restriction at Statistics Canada, https://www150.statcan.gc.ca/n1/pub/11-625-x/11-625-x2010000-eng.htm. Analytic code (R-Studio and SAS) can be made available to researchers upon request to the author.