ABSTRACT
Background
Trends in junk food consumption, a risk for obesity, are not well established.
Objectives
We examined national trends in types of junk food (excluding beverages) and their sources (grocery, restaurants, schools, etc.), overall and in population subgroups.
Methods
We assessed 29,970 children (aged 2–19 y) and 44,501 adults (aged ≥20 y) with 24-h dietary recall data from 9 NHANES cycles (2001–2002 to 2017–2018). Trends in junk food were assessed over time using 1-d values for individuals with single recalls and 2-d means for others.
Results
From 2001 to 2018, percent energy (%E) from junk food remained stable for children (from 18.1% to 17.5%, P-trend = 0.25) and decreased for adults (14.1% to 13.0%, P-trend = 0.002). Among children, increases occurred in %E from crackers (1.19% to 1.35%) and snack/meal bars (0.38% to 0.69%) and decreases in candy (2.58% to 1.96%) and other desserts (3.11% to 2.48%) (all P-trends < 0.01). Among adults, increases occurred in snack/meal bars (0.31% to 0.78%, P-trend < 0.001) and decreases in candy (1.97% to 1.55%; P-trend < 0.001), sweet bakery products (5.52% to 4.98%; P-trend = 0.04), and other desserts (2.19% to 1.86%; P-trend = 0.001). In 2017–2018, grocery stores provided the largest proportion of junk food (72.7% for children, 77.1% for adults), followed by other sources (13.1%, 12.1%), restaurants (8.05%, 9.11%), schools (4.86%), and worksites (1.99%). In both children and adults, junk food intake was higher among non-Hispanic white and black Americans compared with Mexican Americans, among those with higher compared with lower education, among women compared with men, and among older compared with younger adults. In sensitivity analyses using only 1-d recalls, mean junk food intake each cycle was ∼0.8–1.0 and 0.3–0.4%E units higher in children and adults, respectively, with otherwise similar trends and subgroup differences over time.
Conclusions
From 2001 to 2018, %E from junk food represented nearly 1 in 5 calories among children, without change, and nearly 1 in 7 calories, with modest decrease, among adults, with disparities in subgroups.
Keywords: junk food, % of energy (%E), NHANES, children, adults, grocery stores, restaurants, school, worksite
See corresponding editorial on page 837.
Introduction
Obesity is a significant and growing public health concern in the United States (US) and worldwide, increasing risk of several chronic conditions, including type 2 diabetes, cardiovascular diseases, and cancers (1). Unhealthy diet is a major contributing factor to obesity and other chronic conditions. In the US, 32% of adults and 49% of children have poor diet quality, whereas dietary disparities persist or are worsening among racial/ethnic minorities and groups with lower education and income (2, 3). Hence, promoting healthy eating for all Americans plays a vital role in preventing adverse health outcomes and alleviating disparities. A healthy diet is particularly important for children because diet quality at an early age influences food preferences and health outcomes over the life course (4).
A range of highly processed and packaged salty snacks, candy, and sweet desserts, commonly termed junk food, have been linked to obesity and other adverse health outcomes (5). To help curb consumption, junk food taxes have been proposed or implemented in several US localities and Mexico and Hungary (5–7). A national (federal) junk food tax has been examined and found to be legally and administratively feasible in the US (5). Modeling studies conducted in the US and United Kingdom suggest that junk food taxes or similar economic disincentives could effectively reduce obesity, diabetes, and cardiovascular diseases (8, 9). Although sugar-sweetened beverages (SSBs) have been extensively studied, much less is known about distributions and trends in nonbeverage junk food. One prior study evaluated trends in foods defined as junk food according to specific Chilean nutrient criteria among US youth from 2003 to 2016 (10). Yet, this study did not evaluate more traditional categories of junk food, junk food consumption among adults, or sources (e.g., grocery stores, schools, worksites) of junk food.
Understanding these distributions and trends, overall and in population subgroups at risk for health disparities, is crucial to inform priorities and policies to discourage junk food intake and improve dietary quality and diet-related health disparities.
In this investigation, we assessed food categories defined for junk food taxes proposed or implemented across US localities (5) and used for prior health impact modeling studies (9). We examined current levels and historical trends in total and subtypes of junk food consumption, focusing on foods (rather than SSBs) and their food sources overall and in population subgroups among nationally representative samples of US children and adults.
Methods
Data source, study population, and dietary assessment
NHANES is a series of cross-sectional surveys using a complex, multistage sampling design to enroll a nationally representative sample of the civilian, noninstitutionalized US population (11). The protocol was approved by the CDC/National Center for Health Statistics (NCHS) Ethics Review Board, and all participants provided written informed consent. Details on the NHANES study protocol and data collection methods are documented (12). Because the data are publicly available and deidentified, institutional review board approval was not required for the present study.
This investigation used data across the most recent 9 cycles of NHANES (2001–2002 through 2017–2018), including US children aged 2–19 y and adults aged ≥20 y who completed at least 1 valid 24-h diet recall, as determined by NCHS criteria. All participants were eligible for dietary assessment with up to two 24-h recalls in which respondents reported all foods and beverages consumed during the previous 24 h (midnight to midnight). Through a computer-assisted dietary interview, trained NHANES interviewers used the 4-step Multiple-Pass Method in 2001 and the new 5-step Automated Multiple-Pass Method from 2002 and onward to collect dietary intakes. Both methods have been validated as research-based multiple-pass approaches to enhance complete and accurate food recall and reduce respondent burden (13). The 1-d value was used for individuals with single recalls and 2-d means for those with 2 recalls. The protocol and data collection methods for the 24-h recall dietary assessment have been described in detail (14) (see Supplemental Methods). The same computer-assisted dietary interview system was used for both mobile examination centers in-person and phone follow-up dietary interviews. The food composition tables are updated with each cycle of NHANES to account for changes in food supply and are considered the best available by the USDA at the time of release. The flowchart for participants is shown in Supplemental Figure 1.
Assessment of junk food consumption
The primary outcome variables were the mean consumption of junk food (excluding SSBs) and its subtypes in percent energy (%E). Absolute energy intake, which varies with age, sex, physical activity, and metabolism, was assessed in secondary analyses. Junk food was characterized based on the most common specified categories used for junk food taxes across US localities, Mexico, and Hungary (Supplemental Table 1). Main subgroups were based on the USDA Food and Nutrient Database for Dietary Studies food grouping codes in combination with the USDA What We Eat in America food categories, including sweet bakery products, savory snacks, crackers, snack/meal bars, candy, and other desserts (15). To exclude potentially healthy options in these categories, we excluded any products with higher-quality fats (for products with ≥5% energy from fat), defined as an unsaturated to saturated fatty acid ratio of 4:1 or higher; higher-quality carbohydrates (for products with ≥10% energy from carbohydrate), defined as a carbohydrate to fiber ratio of 10:1 or lower; and with sodium content at or below the 2-y category-specific draft FDA voluntary sodium guidelines (16). In sensitivity analysis, we applied alternative nutrient thresholds and criteria from the Chilean Food Regulation used to define “unhealthy food” and jointly mandate front-of-package warning labels, restrict child-directed marketing, and ban sales in schools (Supplemental Methods).
Sources of junk food
Secondary outcome variables were sources of junk food, obtained through the question, “Where did you get (this/most of the ingredients for this) {FOODNAME}?” “Was it from a supermarket, a convenience-type store, a fast food place, a restaurant, from someone else, or another source?” For this investigation, food sources were grouped according to the NHANES Dietary Interviewers Procedures Manual (17) into 1) grocery stores (grocery or supermarket), 2) restaurants (restaurant fast food/pizza, restaurant with waiter/waitress, restaurant no additional information), 3) school/childcare for children (cafeteria in a K–12 school and childcare center; hereafter referred to as schools) and worksites for adults (cafeteria not in a K–12 school, vending machine, common coffee pot or snack tray), and 4) other sources (e.g., from someone else/gift; sport, recreation, or entertainment facility; food truck).
Population subgroups
To evaluate population subgroups at risk for diet-related health disparities, findings were stratified by age (2–5 y, 6–11 y, 12–19 y, 20–34 y, 35–49 y, 50–64 y, ≥65 y), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican American), educational level (less than high school graduate, high school graduate or general equivalency diploma, some college, college or higher), and household income (ratio of family income to the federal poverty level <1.30, 1.30–3.49, ≥3.50). For children, parental education attainment was used. Information on race/ethnicity was collected by trained NHANES interviewers according to the fixed categories provided by the NCHS using the Computer-Assisted Personal Interview system, with classification identified by a household proxy for participants younger than 16 y and by the respondents directly for those aged 16 y and older. Race/ethnicity-specific results were presented for Mexican American individuals as opposed to all Hispanic individuals due to participant sampling changes over time (18). Trends in junk food consumption for other Hispanic and other race or mixed-race groups were not presented separately due to their small sample sizes.
Statistical analyses
The nationally representative population mean intake of junk food and its component food subgroups (%E and absolute intake) was estimated for each NHANES cycle among children and adults. Proportions of junk food from major sources were similarly assessed. The statistical significance of trends was assessed by treating survey year as a continuous variable in a survey-weighted linear regression model. Mean differences and uncertainty (95% CIs) in junk food consumption and proportions of junk food from major sources between the earliest (NHANES 2001–2002) and latest (2017–2018) cycles were calculated. Sensitivity analyses evaluated findings using data for each participant from their 24-h recalls for day 1 or 2 only. To understand whether observed trends could be driven by population demographic shifts, sensitivity analyses were adjusted for age, sex, race/ethnicity, education, and income levels within each cycle.
To evaluate potential differences in trends by population subgroups (age, sex, race/ethnicity, educational level, and income level), a survey-weighted Wald F test was used to test an interaction term between the 2-y cycle and subgroups.
Analyses were performed using Stata version 14 (StataCorp), with a 2-sided α = 0.05. Survey weights, accounting for sampling procedures, stratification, and clustering, were applied to all analyses to generate nationally representative estimates. Alpha values were not corrected for the possibility of type I error from multiple comparisons, so nominal P values should be interpreted accordingly.
Results
Population characteristics
A total of 74,471 participants were analyzed, including 29,970 children aged 2–19 y (49.2% female) and 44,501 adults aged 20 y and older (51.9% female). Participant characteristics in 2017–2018 are shown in Supplemental Table 2. In total, 92.7% of US children and 86.0% of US adults reported at least some junk food consumption on any given day. Higher percentages of junk food consumption among children compared with adults were observed across all population subgroups.
Junk food consumption and trends
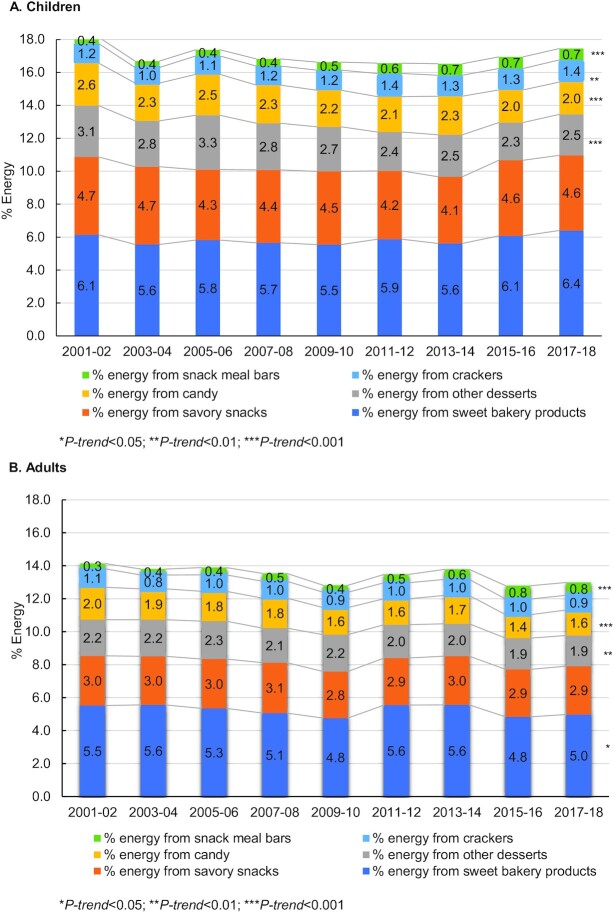
From 2001–2002 to 2017–2018, the %E from junk food among children was high (nearly 1 in 5 calories) and remained stable (from 18.1% to 17.5%, P-trend = 0.25) (Table 1). The %E was modestly lower (nearly 1 in 7 calories) and decreased over this period among adults (14.1% to 13.0%, P-trend = 0.002) (Table 2). The major subtype in both children and adults was sweet bakery products, followed by savory snacks, other desserts, candy, crackers, and snack/energy bars. Evaluating trends in subtypes of junk food among children, increases were observed in %E from crackers (1.19% to 1.35%; P-trend = 0.006) and snack/meal bars (0.38% to 0.69%; P-trend < 0.001) and decreases from candy (2.58% to 1.96%; P-trend < 0.001) and other desserts (3.11% to 2.48%; P-trend < 0.001) (Figure 1). Trends were similar among adults, with increases in %E from snack/meal bars (0.31% to 0.78%) and decreases in %E from candy (1.97% to 1.55%; P-trend < 0.001), sweet bakery products (5.52% to 4.98%; P-trend = 0.04), and other desserts (2.19% to 1.86%; P-trend = 0.001).
TABLE 1.
Trends in estimated percent energy (%E) from total and subtypes of junk food among US children aged 2–19 years by NHANES cycle, 2001–20181
| Survey-weighted mean %E (95% CI)2 | Mean change from | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated percentage of energy, % | 2001–2002 (n = 4288) | 2003–2004 (n = 3825) | 2005–2006 (n = 4029) | 2007–2008 (n = 3109) | 2009–2010 (n = 3280) | 2011–2012 (n = 3134) | 2013–2014 (n = 3021) | 2015–2016 (n = 2901) | 2017–2018 (n = 2383) | P-trend | 2001–2002 to 2015–2016 (95% CI) |
| Total junk food3 | 18.1 (17.2, 19.1) | 16.7 (16.0, 17.4) | 17.4 (16.5, 18.3) | 16.8 (16.0, 17.6) | 16.6 (15.8, 17.5) | 16.6 (15.7, 17.4) | 16.5 (15.8, 17.3) | 16.9 (16.1, 17.8) | 17.5 (16.7, 18.2) | 0.25 | –0.69 (–1.90, 0.52) |
| Savory snacks | |||||||||||
| Potato chips | 1.34 (1.12, 1.56) | 1.56 (1.32, 1.80) | 1.31 (1.08, 1.54) | 1.27 (1.01, 1.53) | 1.21 (1.07, 1.36) | 1.15 (0.97, 1.33) | 1.15 (0.99, 1.32) | 1.58 (1.36, 1.81) | 1.36 (1.16, 1.55) | 0.74 | 0.02 (–0.28, 0.31) |
| Tortilla, corn, or otherchips | 2.34 (2.09, 2.58) | 1.84 (1.65, 2.03) | 1.84 (1.63, 2.04) | 1.85 (1.65, 2.04) | 2.11 (1.82, 2.40) | 1.78 (1.45, 2.12) | 1.60 (1.34, 1.87) | 1.82 (1.53, 2.11) | 1.88 (1.58, 2.18) | 0.02 | –0.46 (–0.84, –0.07) |
| Popcorn | 0.51 (0.35, 0.67) | 0.81 (0.70, 0.92) | 0.63 (0.52, 0.74) | 0.69 (0.52, 0.87) | 0.58 (0.49, 0.67) | 0.61 (0.46, 0.76) | 0.54 (0.40, 0.68) | 0.62 (0.48, 0.76) | 0.62 (0.49, 0.76) | 0.50 | 0.12 (–0.10, 0.33) |
| Pretzels/snack mix | 0.55 (0.41, 0.68) | 0.51 (0.40, 0.62) | 0.50 (0.34, 0.67) | 0.62 (0.35, 0.89) | 0.55 (0.41, 0.69) | 0.61 (0.40, 0.82) | 0.76 (0.44, 1.07) | 0.57 (0.41, 0.74) | 0.71 (0.49, 0.93) | 0.07 | 0.16 (–0.10, 0.42) |
| Crackers | |||||||||||
| Crackers excludessaltines | 1.06 (0.91, 1.21) | 0.80 (0.70, 0.90) | 0.98 (0.87, 1.10) | 1.03 (0.75, 1.31) | 1.12 (0.90, 1.34) | 1.24 (1.01, 1.47) | 1.18 (0.92, 1.44) | 1.20 (0.96, 1.44) | 1.25 (1.01, 1.49) | 0.001 | 0.20 (–0.08, 0.48) |
| Saltine crackers | 0.14 (0.07, 0.20) | 0.15 (0.11, 0.19) | 0.14 (0.11, 0.17) | 0.12 (0.08, 0.16) | 0.10 (0.06, 0.13) | 0.16 (0.12, 0.20) | 0.09 (0.06, 0.12) | 0.10 (0.06, 0.13) | 0.10 (0.06, 0.13) | 0.03 | –0.04 (–0.11, 0.03) |
| Snack/meal bars | |||||||||||
| Cereal bars | 0.35 (0.24, 0.46) | 0.34 (0.25, 0.44) | 0.36 (0.28, 0.44) | 0.40 (0.34, 0.47) | 0.48 (0.37, 0.59) | 0.56 (0.45, 0.67) | 0.57 (0.45, 0.69) | 0.58 (0.44, 0.73) | 0.54 (0.44, 0.65) | <0.001 | 0.19 (0.04, 0.34) |
| Nutrition bars | 0.03 (0, 0.07) | 0.04 (0.01, 0.07) | 0.02 (0, 0.03) | 0.03 (0.30, 0.06) | 0.001 (0, 0.003) | 0.07 (0.04, 0.11) | 0.13 (0.05, 0.21) | 0.12 (0.06, 0.18) | 0.15 (0.05, 0.25) | <0.001 | 0.12 (0.02, 0.23) |
| Sweet bakery products | |||||||||||
| Cakes and pies | 2.06 (1.51, 2.61) | 1.83 (1.54, 2.12) | 1.78 (1.47, 2.09) | 1.80 (1.46, 2.15) | 1.54 (1.28, 1.80) | 1.43 (1.16, 1.70) | 1.37 (1.10, 1.64) | 1.55 (1.35, 1.75) | 1.63 (1.16, 2.11) | 0.03 | –0.43 (–1.20, 0.30) |
| Cookies and brownies | 2.94 (2.65, 3.22) | 2.43 (2.13, 2.73) | 2.57 (2.30, 2.84) | 2.40 (2.12, 2.68) | 2.77 (2.48, 3.05) | 3.06 (2.78, 3.34) | 2.92 (2.56, 3.28) | 3.14 (2.77, 3.51) | 3.35 (2.95, 3.75) | <0.001 | 0.41 (–0.08, 0.91) |
| Doughnuts, sweetrolls, pastries | 1.14 (0.95, 1.33) | 1.30 (1.09, 1.51) | 1.47 (1.17, 1.77) | 1.45 (1.20, 1.70) | 1.24 (1.03, 1.45) | 1.38 (1.15, 1.62) | 1.33 (1.09, 1.56) | 1.39 (1.15, 1.63) | 1.41 (1.04, 1.78) | 0.35 | 0.27 (–0.15, 0.69) |
| Candy | 2.58 (2.32, 2.84) | 2.29 (1.99, 2.58) | 2.48 (2.19, 2.76) | 2.31 (2.06, 2.57) | 2.22 (1.94, 2.49) | 2.15 (1.81, 2.49) | 2.34 (2.13, 2.56) | 1.98 (1.74, 2.22) | 1.96 (1.68, 2.23) | <0.001 | –0.63 (–1.0, –0.25) |
| Candy containingchocolate | 1.14 (0.94, 1.33) | 1.16 (0.92, 1.41) | 1.17 (1.02, 1.31) | 1.13 (0.89, 1.36) | 0.97 (0.77, 1.18) | 0.98 (0.75, 1.21) | 0.99 (0.82, 1.16) | 0.91 (0.70, 1.12) | 0.80 (0.60, 1.0) | 0.001 | –0.34 (–0.61, –0.06) |
| Candy not containingchocolate | 1.44 (1.28, 1.61) | 1.12 (1.0, 1.24) | 1.31 (1.11, 1.52) | 1.19 (1.05, 1.32) | 1.25 (1.11, 1.38) | 1.17 (0.95, 1.38) | 1.36 (1.17, 1.54) | 1.07 (0.98, 1.17) | 1.15 (0.96, 1.35) | 0.06 | –0.29 (–0.54, –0.04) |
| Other desserts | |||||||||||
| Ice cream and frozendairy desserts | 2.37 (1.96, 2.78) | 2.09 (1.75, 2.43) | 2.60 (2.15, 3.04) | 2.14 (1.88, 2.40) | 2.04 (1.78, 2.29) | 1.87 (1.55, 2.19) | 2.16 (1.83, 2.50) | 1.96 (1.64, 2.28) | 2.24 (1.82, 2.67) | 0.18 | –0.13 (–0.72, 0.46) |
| Pudding | 0.21 (0.12, 0.29) | 0.19 (0.13, 0.24) | 0.26 (0.15, 0.37) | 0.15 (0.09, 0.20) | 0.24 (0.09, 0.38) | 0.27 (0, 0.54) | 0.15 (0.07, 0.24) | 0.13 (0.08, 0.19) | 0.08 (0.03, 0.13) | 0.01 | –0.13 (–0.23, –0.03) |
| Gelatins, ices, sorbets | 0.53 (0.35, 0.71) | 0.51 (0.37, 0.66) | 0.45 (0.32, 0.59) | 0.54 (0.44, 0.65) | 0.43 (0.30, 0.56) | 0.22 (0.14, 0.30) | 0.23 (0.14, 0.32) | 0.20 (0.15, 0.24) | 0.16 (0.10, 0.23) | <0.001 | –0.37 (–0.56, –0.18) |
The survey-weighted mean consumption from the major subcategory totals is shown in Figure 1.
Data were weighted to be nationally representative. P-trend was calculated with linear regression models and statistical significance was set at a 2-tailed α = 0.05.
Junk food and its subgroups were defined according to the specified categories based on the USDA Food and Nutrient Database for Dietary Studies food grouping codes, including sugars and sweets; cakes, cookies, pies, pastries, and bars; crackers and salted snacks from grain products; milk desserts and puddings; and potato chips. To allow for potentially healthy options in these categories, we excluded any products with higher-quality fats (for products with ≥5% energy from fat), defined as an unsaturated to saturated fatty acid ratio of 4:1 or higher; higher-quality carbohydrates (for products with ≥10% energy from carbohydrate), defined as a carbohydrate to fiber ratio of 10:1 or lower; and with sodium content at or below the 2-y category-specific draft FDA voluntary sodium guidelines.
TABLE 2.
Trends in estimated percent energy (%E) from total and subtypes of junk food among US adults aged 20+ y by NHANES cycle, 2001–20181
| Survey-weighted mean %E (95% CI)2 | Mean change from 2001–2002 to 2015–2016 (95% CI) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimated percentage of energy, % | 2001–2002 (n = 4744) | 2003–2004 (n = 4448) | 2005–2006 (n = 4520) | 2007–2008 (n = 5420) | 2009–2010 (n = 5762) | 2011–2012 (n = 4801) | 2013–2014 (n = 5047) | 2015–2016 (n = 5017) | 2017–2018 (n = 4742) | P-trend | |
| Total junk food3 | 14.1 (13.6, 14.7) | 13.8 (13.2, 14.4) | 13.9 (13.1, 14.7) | 13.5 (12.7, 14.3) | 12.8 (12.4, 13.2) | 13.5 (12.6, 14.3) | 13.8 (13.0, 14.5) | 12.8 (12.3, 13.3) | 13.0 (12.4, 13.6) | 0.002 | –1.20 (–2.0, –0.32) |
| Savory snacks | |||||||||||
| Potato chips | 0.90 (0.75, 1.04) | 1.03 (0.92, 1.14) | 1.04 (0.92, 1.17) | 1.08 (0.95, 1.20) | 0.90 (0.79, 1.0) | 1.01 (0.90, 1.13) | 0.96 (0.87, 1.04) | 1.05 (0.90, 1.20) | 1.04 (0.92, 1.16) | 0.44 | 0.14 (–0.05, 0.33) |
| Tortilla, corn, or otherchips | 1.18 (1.05, 1.31) | 1.03 (0.86, 1.20) | 1.15 (0.97, 1.33) | 1.09 (0.95, 1.24) | 1.10 (0.96, 1.24) | 1.09 (0.86, 1.32) | 1.13 (0.99, 1.26) | 1.02 (0.91, 1.13) | 1.04 (0.90, 1.18) | 0.26 | –0.14 (–0.33, 0.05) |
| Popcorn | 0.52 (0.42, 0.61) | 0.50 (0.39, 0.60) | 0.46 (0.37, 0.54) | 0.50 (0.40, 0.59) | 0.49 (0.40, 0.58) | 0.38 (0.27, 0.48) | 0.44 (0.35, 0.54) | 0.50 (0.39, 0.60) | 0.46 (0.37, 0.56) | 0.36 | –0.05 (–0.19, 0.08) |
| Pretzels/snack mix | 0.42 (0.31, 0.52) | 0.40 (0.30, 0.50) | 0.34 (0.23, 0.46) | 0.39 (0.23, 0.56) | 0.34 (0.28, 0.40) | 0.37 (0.25, 0.49) | 0.44 (0.33, 0.54) | 0.30 (0.26, 0.35) | 0.38 (0.28, 0.49) | 0.55 | –0.03 (–0.18, 0.12) |
| Crackers | |||||||||||
| Crackers excludessaltines | 0.86 (0.67, 1.06) | 0.61 (0.55, 0.67) | 0.75 (0.66, 0.84) | 0.79 (0.67, 0.91) | 0.72 (0.62, 0.81) | 0.76 (0.63, 0.88) | 0.77 (0.68, 0.86) | 0.82 (0.70, 0.94) | 0.69 (0.57, 0.80) | 0.93 | –0.17 (–0.40, 0.05) |
| Saltine crackers | 0.26 (0.20, 0.33) | 0.24 (0.19, 0.28) | 0.25 (0.18, 0.32) | 0.23 (0.20, 0.26) | 0.21 (0.16, 0.26) | 0.21 (0.17, 0.25) | 0.19 (0.15, 0.24) | 0.14 (0.11, 0.18) | 0.20 (0.12, 0.28) | 0.009 | –0.07 (–0.17, 0.04) |
| Snack/meal bars | |||||||||||
| Cereal bars | 0.21 (0.13, 0.28) | 0.24 (0.18, 0.30) | 0.37 (0.26, 0.48) | 0.40 (0.31, 0.49) | 0.35 (0.28, 0.42) | 0.36 (0.29, 0.43) | 0.43 (0.34, 0.53) | 0.43 (0.33, 0.54) | 0.35 (0.25, 0.45) | 0.001 | 0.14 (0.01, 0.27) |
| Nutrition bars | 0.11 (0.05, 0.16) | 0.12 (0.07, 0.18) | 0.07 (0.04, 0.1) | 0.08 (0.06, 0.11) | 0.07 (0.05, 0.09) | 0.14 (0.09, 0.18) | 0.18 (0.12, 0.25) | 0.37 (0.25, 0.48) | 0.43 (0.24, 0.62) | <0.001 | 0.32 (0.12, 0.52) |
| Sweet bakery products | |||||||||||
| Cakes and pies | 2.38 (2.07, 2.68) | 2.71 (2.38, 3.05) | 2.59 (2.3, 2.87) | 2.44 (2.13, 2.74) | 2.16 (1.88, 2.43) | 2.27 (1.96, 2.58) | 2.31 (2.04, 2.58) | 1.88 (1.59, 2.18) | 1.87 (1.64, 2.10) | <0.001 | –0.51 (–0.89, –0.13) |
| Cookies and brownies | 2.20 (2.01, 2.39) | 1.92 (1.70, 2.13) | 1.90 (1.75, 2.05) | 1.81 (1.68, 1.94) | 1.89 (1.74, 2.05) | 2.47 (2.35, 2.58) | 2.42 (2.27, 2.56) | 2.20 (2.02, 2.37) | 2.29 (2.11, 2.47) | <0.001 | 0.09 (–0.17, 0.35) |
| Doughnuts, sweetrolls, pastries | 0.95 (0.73, 1.16) | 0.93 (0.82, 1.04) | 0.86 (0.64, 1.07) | 0.81 (0.67, 0.95) | 0.70 (0.60, 0.81) | 0.81 (0.66, 0.95) | 0.83 (0.74, 0.92) | 0.76 (0.65, 0.87) | 0.82 (0.63, 1.01) | 0.13 | –0.13 (–0.41, 0.16) |
| Candy | |||||||||||
| Candy containingchocolate | 1.29 (1.09, 1.49) | 1.35 (1.16, 1.55) | 1.29 (1.19, 1.39) | 1.34 (1.14, 1.55) | 1.10 (0.98, 1.23) | 1.06 (0.88, 1.25) | 1.15 (0.98, 1.32) | 0.97 (0.81, 1.12) | 1.06 (0.85, 1.27) | <0.001 | –0.23 (–0.52, 0.06) |
| Candy not containingchocolate | 0.68 (0.55, 0.81) | 0.52 (0.41, 0.62) | 0.53 (0.36, 0.69) | 0.48 (0.39, 0.57) | 0.53 (0.47, 0.60) | 0.51 (0.39, 0.62) | 0.57 (0.46, 0.68) | 0.46 (0.37, 0.54) | 0.49 (0.37, 0.62) | 0.1 | –0.19 (–0.37, –0.005) |
| Other desserts | |||||||||||
| Ice cream and frozendairy desserts | 1.84 (1.64, 2.04) | 1.85 (1.66, 2.03) | 1.95 (1.73, 2.17) | 1.75 (1.60, 1.89) | 1.92 (1.66, 2.19) | 1.71 (1.47, 1.95) | 1.70 (1.47, 1.92) | 1.69 (1.45, 1.94) | 1.67 (1.44, 1.89) | 0.04 | –0.17 (–0.47, 0.13) |
| Pudding | 0.22 (0.18, 0.27) | 0.19 (0.16, 0.21) | 0.24 (0.18, 0.30) | 0.24 (0.20, 0.28) | 0.19 (0.16, 0.21) | 0.20 (0.15, 0.26) | 0.20 (0.15, 0.25) | 0.14 (0.11, 0.17) | 0.14 (0.08, 0.21) | 0.002 | –0.08 (–0.15, –0.001) |
| Gelatins, ices, sorbets | 0.14 (0.09, 0.18) | 0.19 (0.13, 0.24) | 0.09 (0.05, 0.13) | 0.10 (0.08, 0.13) | 0.13 (0.09, 0.16) | 0.12 (0.09, 0.15) | 0.07 (0.04, 0.09) | 0.06 (0.04, 0.08) | 0.05 (0.03, 0.07) | <0.001 | –0.08 (–0.13, –0.04) |
The survey-weighted mean consumption from the major subcategory totals is shown in Figure 1.
Data were weighted to be nationally representative. P-trend was calculated with linear regression models and statistical significance was set at a 2-tailed α = 0.05.
Junk food and its subgroups were defined according to the specified categories based on the USDA Food and Nutrient Database for Dietary Studies food grouping codes, including sugars and sweets; cakes, cookies, pies, pastries, and bars; crackers and salted snacks from grain products; milk desserts and puddings; and potato chips. To allow for potentially healthy options in these categories, we excluded any products with higher-quality fats (for products with ≥5% energy from fat), defined as an unsaturated to saturated fatty acid ratio of 4:1 or higher; higher-quality carbohydrates (for products with ≥10% energy from carbohydrate), defined as a carbohydrate to fiber ratio of 10:1 or lower; and with sodium content at or below the 2-y category-specific draft FDA voluntary sodium guidelines.
FIGURE 1.
Trends in mean percent energy from major subtypes of junk food among US children (aged 2–19 y, n = 29,970) and adults (aged 20+ y, n = 44,501) from 2001 to 2018. Data were adjusted for NHANES survey weights to be nationally representative.
Findings for absolute energy intake from junk food are shown in Supplemental Tables 3–4. In sensitivity analyses using only the first day 24-h recall per person, the mean intake of junk food in each NHANES cycle was about 0.8–1.0% energy units higher in children and 0.3–0.4% energy units higher in adults, compared with using the average of both 24-h recalls per person (Supplemental Tables 5–7). These absolute differences corresponded to about 5% higher junk food intake in children and 2% higher junk food intake in adults, using only the first day compared with both days of 24-h recalls. However, inferences on subtypes of junk food and trends over time in children and adults were not materially altered. Results were also not materially altered by adjustment for sociodemographic characteristics over time (Supplemental Tables 8–11). Results were also largely consistent in sensitivity analyses including only products in these categories that also met the nutrient threshold/criteria from the Chilean food regulation (Supplemental Tables 12–15).
Junk food intake by sources
Among different venues, most junk food (>70%) was obtained from grocery stores among both children and adults throughout the study period, followed by other sources, restaurants, and then schools or worksites (Table 3,Supplemental Figure 2). From 2003–2004 (the first cycle of available data) to 2017–2018 among children, the proportion of junk food from grocery stores decreased from 80.6% to 72.7% (P-trend < 0.001) but increased from restaurants (4.70% to 8.05%; P-trend < 0.001) and other sources (10.0% to 13.1%; P-trend = 0.001) and remained stable from schools (4.89% to 4.86%; P-trend = 0.94). Among adults, proportions of junk food from grocery stores modestly decreased (78.7% to 77.1%; P-trend = 0.002) but increased from restaurants (8.11% to 9.11%; P-trend = 0.002) and other sources (from 10.2% to 12.1%; P-trend = 0.001) and decreased from worksites (3.69% to 1.99%; P-trend < 0.001). Details of sources of subtypes of junk food consumption are provided in Supplemental Tables 16 and 17.
TABLE 3.
Trends in estimated proportions of total junk food from different food sources among US children aged 2–19 y and US adults aged 20+ y by NHANES cycle, 2003–20181
| Estimated proportions of the total energy from junk food, % | Survey-weighted proportions (95% CI)2 | Mean change from 2002–2004 to 2015–2016 (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2003–2004 (n = 3825) | 2005–2006 (n = 4029) | 2007–2008 (n = 3109) | 2009–2010 (n = 3280) | 2011–2012 (n = 3134) | 2013–2014 (n = 3021) | 2015–2016 (n = 2901) | 2017–2018 (n = 2383) | P-trend | ||
| Junk food sources among children | ||||||||||
| Grocery store | 80.6 (79.0, 82.2) | 78.0 (76.4, 79.5) | 75.6 (72.8, 78.5) | 77.8 (76.1, 79.6) | 74.2 (72.7, 75.8) | 73.6 (72.3, 75.0) | 72.6 (69.2, 75.9) | 72.7 (71.1, 74.3) | <0.001 | –7.80 (–10.0, –5.60) |
| Restaurants | 4.70 (4.10, 5.30) | 6.43 (5.69, 7.16) | 5.53 (4.26, 6.79) | 4.67 (3.77, 5.56) | 6.85 (5.13, 8.57) | 7.48 (6.29, 8.67) | 7.75 (6.20, 9.30) | 8.05 (6.39, 9.71) | <0.001 | 3.35 (1.58, 5.11) |
| Schools | 4.89 (3.26, 6.52) | 4.23 (3.58, 4.88) | 5.40 (4.06, 6.75) | 4.94 (3.65, 6.23) | 4.23 (3.36, 5.10) | 5.23 (4.16, 6.31) | 4.66 (3.55, 5.76) | 4.86 (3.27, 6.44) | 0.94 | –0.03 (–2.30, 2.24) |
| Others | 10.0 (8.98, 11.1) | 11.0 (9.55, 12.4) | 12.4 (10.4, 14.4) | 11.6 (10.6, 12.6) | 14.0 (12.1, 16.0) | 12.5 (11.0, 14.0) | 13.7 (10.9,16.5) | 13.1 (11.6, 14.5) | 0.001 | 3.06 (1.28, 4.84) |
| Junk food sources among adults | 2003–2004 (n = 4448) | 2005–2006 (n = 4520) | 2007–2008 (n = 5420) | 2009–2010 (n = 5762) | 2011–2012 (n = 4801) | 2013–2014 (n = 5047) | 2015–2016 (n = 5017) | 2017–2018 (n = 4742) | ||
| Grocery store | 78.7 (77.3, 80.0) | 78.8 (77.6, 80.1) | 80.2 (78.8, 81.6) | 80.2 (78.4, 81.9) | 75.9 (73.2, 78.6) | 76.2 (75.1, 77.3) | 77.0 (74.5, 79.4) | 77.1 (75.1, 79.1) | 0.002 | –1.55 (–3.97, 0.87) |
| Restaurants | 8.11 (6.98, 9.23) | 7.54 (6.55, 8.54) | 7.23 (6.48, 8.07) | 6.54 (5.78, 7.31) | 8.56 (7.74, 9.39) | 10.1 (8.85, 11.3) | 8.78 (7.14, 10.4) | 9.11 (8.07, 10.2) | 0.002 | 1.01 (–0.53, 2.54) |
| Worksites | 3.69 (2.89, 4.49) | 3.30 (2.45, 4.15) | 2.31 (1.73, 2.88) | 2.52 (1.76, 3.29) | 2.69 (2.17, 3.22) | 1.72 (1.45, 1.99) | 1.54 (1.05, 2.04) | 1.99 (1.41, 2.56) | <0.001 | –1.70 (–2.69, –0.72) |
| Others | 10.2 (9.30, 11.1) | 10.8 (9.41, 12.2) | 10.4 (9.39, 11.4) | 11.1 (9.94, 12.3) | 13.3 (11.1, 15.4) | 12.3 (11.4, 13.2) | 12.9 (11.1, 14.7) | 12.1 (10.4, 13.8) | 0.001 | 1.84 (–0.07, 3.76) |
Junk food and its subgroups were defined according to the specified categories based on the USDA Food and Nutrient Database for Dietary Studies food grouping codes, including sugars and sweets; cakes, cookies, pies, pastries, and bars; crackers and salted snacks from grain products; milk desserts and puddings; and potato chips. To allow for potentially healthy options in these categories, we excluded any products with higher-quality fats (for products with ≥5% energy from fat), defined as an unsaturated to saturated fatty acid ratio of 4:1 or higher; higher-quality carbohydrates (for products with ≥10% energy from carbohydrate), defined as a carbohydrate to fiber ratio of 10:1 or lower; and with sodium content at or below the 2-y category-specific draft FDA voluntary sodium guidelines.
Data were weighted to be nationally representative. P-trend was calculated with linear regression models and statistical significance was set at a 2-tailed α = 0.05.
Junk food intake and trends in population subgroups
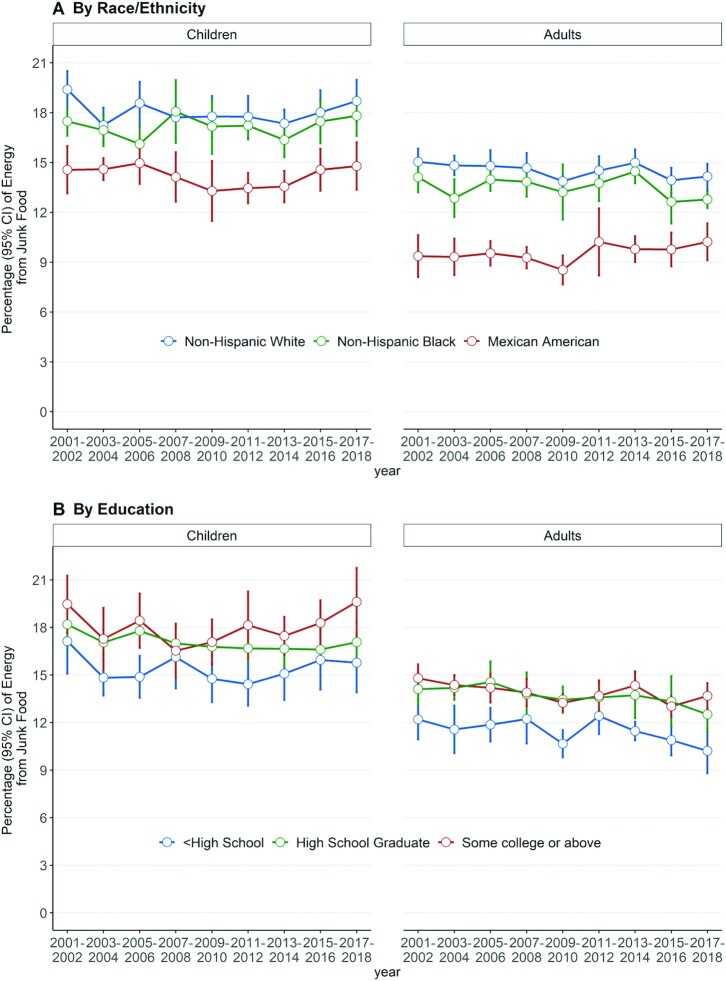
Junk food consumption (%E) during this period by education and income is shown in Figure 2 and Supplemental Figure 3 and by these factors as well as age, sex, and income (%E, absolute energy) in Supplemental Tables 18–21. Among children, junk food consumption was higher throughout this period among non-Hispanic white and black Americans compared with Mexican Americans, as well as among children with heads of households with higher education and income levels compared with less than high school education and an income/poverty ratio <1.3. Junk food intake levels in children (%E) tended to be higher among 6- to 11-y-olds compared with 12- to 19-y-olds but were more similar by sex. In adults, similar differences in junk food consumption were seen as in children by race/ethnicity, education, and income. In addition, women tended to have higher intake levels than men (e.g., in 2017–2018, 13.8%E compared with 12.1%E, respectively), and surprisingly, older adults tended to have higher intake levels than younger adults (e.g., in 2017–2018, 11.1%, 12.1%, 13.3%, and 16.2% among ages 20–34 y, 35–49 y, 50–64 y, and ≥65 y, respectively).
FIGURE 2.
Trends in mean percent energy from total junk food among US children (aged 2–19 y) and adults (aged 20+ y) from 2001 to 2018 by race/ethnicity (n = 24,661 for children and n = 36,786) and education (n = 28,857 for children and n = 44,454). Data were adjusted for NHANES survey weights to be nationally representative. Error bars indicate 95% CIs. By race/ethnicity, all P-trends > 0.05 for children; among adults, all P-trends > 0.05 except a P-trend for non-Hispanic white = 0.05. By education, all P-trends > 0.05 for children and all P-trends ≤ 0.05 for adults.
The overall national trends in junk food consumption seen between 2001–2002 and 2017–2018 were generally similar in each population subgroup (Supplemental Tables 18–21). One exception was differences in trends over time by age among adults (P-interaction = 0.007): among younger adults (ages 20–34 and 35–49 y), %E from junk food decreased by ∼2%E during this period, whereas among older adults (ages 50–64 and 65+ y), no significant decreases were evident. Findings for subtypes of junk food consumption in different population subgroups are shown in Supplemental Tables 22–26.
Discussion
In this nationally representative investigation, we found that from 2001–2002 to 2017–2018, the %E consumed from junk food was high and remained stable among children and was a bit lower and modestly decreased over time among adults. The major subtype in both children and adults was sweet bakery products, followed by savory snacks, other desserts, candy, crackers, and snack/energy bars. Grocery stores were the primary source of junk food among both children and adults, followed by other sources, restaurants, schools, and worksites. Over this study period, grocery stores significantly decreased as a source, especially for children, whereas restaurants and other venues significantly increased as a source.
Among subtypes of junk food, snack bars were an increasing source for both children and adults, whereas candy and other desserts were a decreasing source (sweet bakery products also decreased in adults only). Crackers were also an increasing source for children. Persistent disparities in junk food consumption were also evident in population subgroups. Among both children and adults, junk food intake was higher among non-Hispanic white and black Americans compared with Mexican Americans and among those with higher education compared with less than high school education (parental education for children). Among adults, junk food intake was also higher among women compared with men and among older compared with younger adults; decreasing trends over time were also seen in younger but not older adults. Our investigation focused on junk food consumption, and other studies have assessed SSBs and overall diet quality by sociodemographic subgroups (2, 19–21).
This investigation is the first, to our knowledge, examining sources of trends in intake of total and subtypes of junk food as a contribution to the overall diets of both US children and adults. Factors that may have contributed to modest declining trends among adults and for certain junk food categories such as candy and other desserts include nationwide health promotion efforts (22–24), added sugar labeling (25, 26), menu calorie labeling (27, 28), junk food or beverage taxes (5, 29), the FDA's voluntary short-term sodium reformulation goals (30, 31), and a growing sociocultural recognition of the importance of dietary habits for health and well-being (32). On the other hand, intakes of snack bars increased in both children and adults, which offset declines in other subtypes in children. This suggests the need to focus on this growing category with public health education and policy actions to discourage consumption and/or ensure healthier accessible, affordable, and convenient snack bar options.
Even excluding SSBs to focus on junk foods, intake represented nearly 1 in 5 calories in children and 1 in 7 calories in adults. Taxes, front-of-pack labels, and other policy measures could be implemented at municipal, state, or even federal levels to discourage consumption, perhaps with a particular focus on the largest categories of sweet bakery products and savory snacks (5, 6). Among lower-income Americans participating in the Supplemental Nutrition Assistance Program, a combination of financial incentives for healthier foods plus disincentives for junk food and other less healthy foods could preserve choice while meaningfully improving health and health equity and reducing health care costs (9). The challenges of coronavirus disease 2019, including far worse outcomes for individuals with diet-related conditions such as obesity, diabetes, and hypertension; increases in food insecurity; and highest risk among black and Latino Americans, make addressing healthier eating and nutrition security for all Americans a major national priority.
The higher consumption among oldest adults, plus declining intakes among younger but not older adults, was unexpected, given the conventional notion that younger people seek junk food and have less traditional diets. Yet, older adults may experience challenges in buying, storing, and preparing less processed foods, and at the same time, younger adults are increasingly aware of and making food purchasing decisions based on considerations of health and environmental sustainability. Our novel findings suggest the importance of focusing on adults across the life span, including older adults, for reducing junk food consumption. More research is also needed to quantify the relation between total and subtypes of junk food consumption and specific health outcomes.
Several prior studies have examined earlier trends in snacking among US youth [up to 2005–2006 (33), 2009–2010 (34), 2014 (35), and 2016 (10)] and adults [up to 2006 (36) and 2012 (37)]. Consistent with our more contemporary findings, these studies reported high levels of calories contributed by snack foods. A more recent study evaluated trends in unhealthy foods (termed junk foods) among US children from 2003 to 2016, based on food categories with at least half of products defined as unhealthy food using the Chilean regulation phase 2 nutrient criteria, including calories, saturated fat, total sugar, and sodium (10). The identified calories from “junk food” as defined in that study were ∼3 times higher than in our investigation, as any food consumed in the United States in a category in which half of the products met these limited nutrient criteria was considered junk food. Our investigation builds on and greatly expands these prior reports by evaluating total and subcategories of junk food consumption, defined based on US junk food tax bills or laws, and their sources among both US children and adults using the latest available national data.
This investigation has several strengths. We assessed the most up-to-date available data from serial nationally representative samples to evaluate intakes and trends in US junk food consumption over 18 y. Junk food consumption was defined based on the most common food categories used for US junk food tax bills and laws, with exclusion of products considered healthier by different sets of nutrient criteria. We evaluated sources and trends in junk food, as well as detailed investigation of potential differences among key sociodemographic subgroups at risk for diet-related health disparities. We adjusted for demographic shifts over time to assess the potential influence of such changes on the findings.
This study has potential limitations. Although NHANES uses a range of high-quality standardized methods to maximize the quality and validity of the dietary data, self-reported intakes are subject to random error (within-person variation) and systematic error. The day 1 recall was performed in person and the day 2 recall by phone, and reported junk food intakes in the day 2recalls were modestly lower. Due to absence of any consensus external definition of junk food, we applied a definition derived from junk food categories used for taxation, and results could vary with differing definitions. On the other hand, results were not materially altered in several sensitivity analyses. We focused on foods, excluding SSBs, due to several recent reports evaluating trends and disparities in SSB intake (19, 38). Our investigation cannot determine the underlying reasons for the observed intake levels and trends, highlighting the need for more research on whether and how sociocultural drivers, dietary guidelines and education, built environmental changes, and other policies may influence junk food consumption overall and in population subgroups.
Conclusions
From 2001–2002 to 2017–2018, %E from junk food (excluding sugary beverages) represented nearly 1 in 5 calories among children, without change, and nearly 1 in 7 calories, with modest decrease, among adults, with disparities in population subgroups.
Supplementary Material
Acknowledgments
The authors’ contributions were as follows—JL and DM: designed the research; YLee, RM, and YLi: conducted the research; JL: conducted data analyses and drafted the manuscript; DM: contributed to the draft of the manuscript; JL had full access to the data and takes responsibility for the integrity of the data and accuracy of the data analyses. All authors: read and approved the final manuscript.
Author disclosures: All authors report support from NIH grants during the conduct of the study. In addition, RM reports research funding from Unilever and personal fees from the World Bank and Bunge and from Development Initiatives for serving as chair of the Global Nutrition Report, all outside the submitted work. DM reports research funding from the NIH, the Gates Foundation, and the Rockefeller Foundation; personal fees from Acasti Pharma, America's Test Kitchen, Barilla, Cleveland Clinic Foundation, Danone, GOED, and Motif FoodWorks; scientific advisory board, Beren Therapeutics, Brightseed, Calibrate, DayTwo (ended June 2020), Elysium Health, Filtricine, Foodome, HumanCo, January Inc., Season, and Tiny Organics; and chapter royalties from UpToDate, all outside the submitted work. All other authors report no conflicts of interest.
Notes
This research was supported by a postdoctoral fellowship award (17POST33670808) from the American Heart Association (JL) and the NIH, National Heart, Lung, and Blood Institute (R01HL130735, 2R01HL115189). The funding agencies did not contribute to design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Supplemental Tables 1–26 and Supplemental Figures 1–3 are available from the “supplemental data” link in the online posting of the article at https://academic.oup.com/ajcn/.
Abbreviations used: %E, percent energy; NCHS, National Center for Health Statistics; SSB, sugar-sweetened beverage.
Contributor Information
Junxiu Liu, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA.
Yujin Lee, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA; Department of Food and Nutrition, Myongji University, Yongin, South Korea.
Renata Micha, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA.
Yan Li, Department of Population Health Science and Policy, Icahn School of Medicine at Mount Sinai, New York, NY, USA; Department of Obstetrics, Gynecology, and Reproductive Science, Icahn School of Medicine at Mount Sinai, New York, NY, USA.
Dariush Mozaffarian, Friedman School of Nutrition Science and Policy, Tufts University, Boston, MA, USA.
Data Availability
Data described in the manuscript, code book, and analytic code will be made available pending e-mail request to the corresponding author.
References
- 1.Luscher TF. Nutrition, obesity, diabetes, and cardiovascular outcomes: a deadly association. Eur Heart J. 2020;41(28):2603–7. [DOI] [PubMed] [Google Scholar]
- 2.Liu J, Rehm CD, Onopa J, Mozaffarian D. Trends in diet quality among youth in the United States, 1999–2016. JAMA. 2020;323(12):1161–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rehm CD, Penalvo JL, Afshin A, Mozaffarian D. Dietary intake among US Adults, 1999–2012. JAMA. 2016;315(23):2542–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Birch L, Savage JS, Ventura A. Influences on the development of children's eating behaviours: from infancy to adolescence. Can J Diet Pract Res. 2007;68(1):s1–s56. [PMC free article] [PubMed] [Google Scholar]
- 5.Pomeranz JL, Wilde P, Huang Y, Micha R, Mozaffarian D. Legal and administrative feasibility of a federal junk food and sugar-sweetened beverage tax to improve diet. Am J Public Health. 2018;108(2):203–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taillie LS, Rivera JA, Popkin BM, Batis C. Do high vs. low purchasers respond differently to a nonessential energy-dense food tax? Two-year evaluation of Mexico's 8% nonessential food tax. Prev Med. 2017;105:S37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bíró A. Did the junk food tax make the Hungarians eat healthier?. Food Policy. 2015;54:107–15. [Google Scholar]
- 8.Scheelbeek PFD, Cornelsen L, Marteau TM, Jebb SA, Smith RD. Potential impact on prevalence of obesity in the UK of a 20% price increase in high sugar snacks: modelling study. BMJ. 2019;366:l4786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mozaffarian D, Liu J, Sy S, Huang Y, Rehm C, Lee Y, Wilde P, Abrahams-Gessel S, de Souza Veiga Jardim T, Gaziano Tet al. . Cost-effectiveness of financial incentives and disincentives for improving food purchases and health through the US Supplemental Nutrition Assistance Program (SNAP): a microsimulation study. PLoS Med. 2018;15(10):e1002661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dunford EK, Popkin BM, Ng SW. Recent trends in junk food intake in U.S. children and adolescents, 2003–2016. Am J Prev Med. 2020;59(1):49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention .About the National Health and Nutrition Examination Survey. [Internet] [cited 2020 Jan 8]. Available from: https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. [Google Scholar]
- 12.Centers for Disease Prevention and Control . National Health and Nutrition Examination Survey. [Internet] [cited 2020 Jun 26]. Available from: https://www.cdc.gov/nchs/nhanes/index.htm#nav-group-15d6f. [Google Scholar]
- 13.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr. 2006;136(10):2594–9. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention . NHANES survey methods and analytic guidelines. [Internet] [cited 2019 Jun 8]. Available from: https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx. [Google Scholar]
- 15.US Department of Agriculture, Agricultural Research Service . USDA food and nutrient database for dietary studies 2015–2016. [Internet]. 2018; [cited 2020 Jun 26]. Available from: www.ars.usda.gov/nea/bhnrc/fsrg. [Google Scholar]
- 16.US Food and Drug Administration . Draft guidance for industry: voluntary sodium reduction goals: target mean and upper bound concentrations for sodium in commercially processed, packaged, and prepared foods. Silver Spring (MD): Food and Drug Administration; 2016. [Google Scholar]
- 17.Centers for Disease Control and Prevention . National Health and Nutrition Examination Survey, interviewer procedures manual. [Internet] [cited 2020 Jan 9]. Available from: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/manuals/2016_MEC_In-Person_Dietary_Interviewers_Procedures_Manual.pdf. [Google Scholar]
- 18.Curtin LR, Mohadjer LK, Dohrmann SM, Kruszon-Moran D, Mirel LB, Carroll MD, Hirsch R, Burt VL, Johnson CL. National Health and Nutrition Examination Survey: sample design, 2007–2010. Vital Health Statistics 2. 2013; (160):1–23. [PubMed] [Google Scholar]
- 19.Vercammen KA, Moran AJ, Soto MJ, Kennedy-Shaffer L, Bleich SN. Decreasing trends in heavy sugar-sweetened beverage consumption in the United States, 2003 to 2016. J Acad Nutr Diet. 2020;120(12):1974–85 e5. [DOI] [PubMed] [Google Scholar]
- 20.Bleich SN, Vercammen KA, Koma JW, Li Z. Trends in beverage consumption among children and adults, 2003–2014. Obesity (Silver Spring). 2018;26(2):432–41. [DOI] [PubMed] [Google Scholar]
- 21.Koma JW, Vercammen KA, Jarlenski MP, Frelier JM, Bleich SN. Sugary drink consumption among children by supplemental nutrition assistance program status. Am J Prev Med. 2020;58(1):69–78. [DOI] [PubMed] [Google Scholar]
- 22.US Department of Health and Human Services and US Department of Agriculture . 2015–2020 Dietary Guidelines for Americans. [Internet]. 8th ed. 2000; [cited 2020 Jan 11]. Available from: http://health.gov/dietaryguidelines/2000/guidelines/. [Google Scholar]
- 23.Child Nutrition . WIC Reauthorization Act of 2004. Public Law. 2004;108(265):118. [Google Scholar]
- 24.Gidding SS, Dennison BA, Birch LL, Daniels SR, Gillman MW, Lichtenstein AH, Rattay KT, Steinberger J, Stettler N, Van Horn Let al. . Dietary recommendations for children and adolescents: a guide for practitioners. Pediatrics. 2006;117(2):544–59. [DOI] [PubMed] [Google Scholar]
- 25.Food and Drug Administration . Food labeling: revision of the nutrition and supplement facts labels. Final rule. Fed Regist. 2016;81(103):33741. [PubMed] [Google Scholar]
- 26.Huang Y, Kypridemos C, Liu J, Lee Y, Pearson-Stuttard J, Collins B, Bandosz P, Capewell S, Whitsel L, Wilde Pet al. . Cost-effectiveness of the US Food and Drug Administration added sugar labeling policy for improving diet and health. Circulation. 2019;139(23):2613–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.US Department of Health and Human Services, Food and Drug Administration. The final rule for menu labeling. [Internet]. 2014; [cited 2020 Jan 12]. Available from: https://www.govinfo.gov/content/pkg/FR-2014-12-01/pdf/2014-27833.pdf. [Google Scholar]
- 28.Liu J, Mozaffarian D, Sy S, Lee Y, Wilde PE, Abrahams-Gessel S, Gaziano T, Micha R, Project F-P. Health and economic impacts of the national menu calorie labeling law in the United States: a microsimulation study. Circ Cardiovasc Qual Outcomes. 2020;13(6):e006313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee Y, Mozaffarian D, Sy S, Liu J, Wilde PE, Marklund M, Abrahams-Gessel S, Gaziano TA, Micha R. Health impact and cost-effectiveness of volume, tiered, and absolute sugar content sugar-sweetened beverage tax policies in the United States: a microsimulation study. Circulation. 2020;142(6):523–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.US Department of Health and Human Services, Food and Drug Adminstration . Voluntary sodium reduction goals: target mean and upper bound concentrations for sodium in commercially processed, packaged, and prepared foods: guidance for industry. Draft guidance. [Internet] [cited 2020 Jan 12]. Available from: https://www.fda.gov/media/98264/download. [Google Scholar]
- 31.Pearson-Stuttard J, Kypridemos C, Collins B, Mozaffarian D, Huang Y, Bandosz P, Capewell S, Whitsel L, Wilde P, O'Flaherty Met al. . Estimating the health and economic effects of the proposed US Food and Drug Administration voluntary sodium reformulation: microsimulation cost-effectiveness analysis. PLoS Med. 2018;15(4):e1002551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.US Department of Agriculture, US Department of Health and Human Services . Dietary Guidelines for Americans, 2020–2025. [Internet]. 9th ed. 2020; [cited 2021 Mar 22]. Available from: DietaryGuidelines.gov. [Google Scholar]
- 33.Piernas C, Popkin BM. Trends in snacking among U.S. children. Health Aff. 2010;29(3):398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bleich SN, Wolfson JA. Trends in SSBs and snack consumption among children by age, body weight, and race/ethnicity. Obesity. 2015;23(5):1039–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dunford EK, Popkin BM. 37 Year snacking trends for US children 1977–2014. Pediatr Obes. 2018;13(4):247–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Piernas C, Popkin BM. Snacking increased among U.S. adults between 1977 and 2006. J Nutr. 2010;140(2):325–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dunford EK, Popkin BM. Disparities in snacking trends in US adults over a 35 year period from 1977 to 2012. Nutrients. 2017;9(8):809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marriott BP, Hunt KJ, Malek AM, Newman JC. Trends in intake of energy and total sugar from sugar-sweetened beverages in the United States among children and adults, NHANES 2003–2016. Nutrients. 2019;11(9):2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data described in the manuscript, code book, and analytic code will be made available pending e-mail request to the corresponding author.