Abstract
Esophageal fibrovascular polyp is rare in esophageal neoplasms and usually very large. Here, we present a case of giant esophageal fibrovascular polyp. The patient had dysphagia and choking sensation at presentation. She underwent positron emission-computed tomography (PET-CT), endoscopy, endoscopic ultrasonography, and fine needle aspiration. She was clinically diagnosed as having an esophageal benign tumor and underwent endoscopic submucosal dissection. The polyp was successfully resected; however, the process was very difficult, and the lesion was too large to pass through the upper esophagus. Finally, we removed the lesion surgically. Fibrovascular polyps are often large, and if endoscopic resection is chosen, it is necessary to consider the difficulties that may be encountered during resection, before initiating treatment.
Keywords: Giant esophageal fibrovascular polyp, endoscopic ultrasonography and fine needle aspiration, difficult endoscopic resection, surgical resection, positron emission tomography-computed tomography, case report
Introduction
Esophageal fibrovascular polyp is a relatively rare disease, accounting for approximately 0.03% of esophageal tumors.1 With developments in endoscopic technology, the detection and diagnosis rates of esophageal fibrovascular polyps are increasing. Although benign, these polyps can grow in size to seriously affect the patient's quality of life or even cause fatal complications.2 Here, we present a case of esophageal fibrovascular polyp, and we review the literature.
Case report
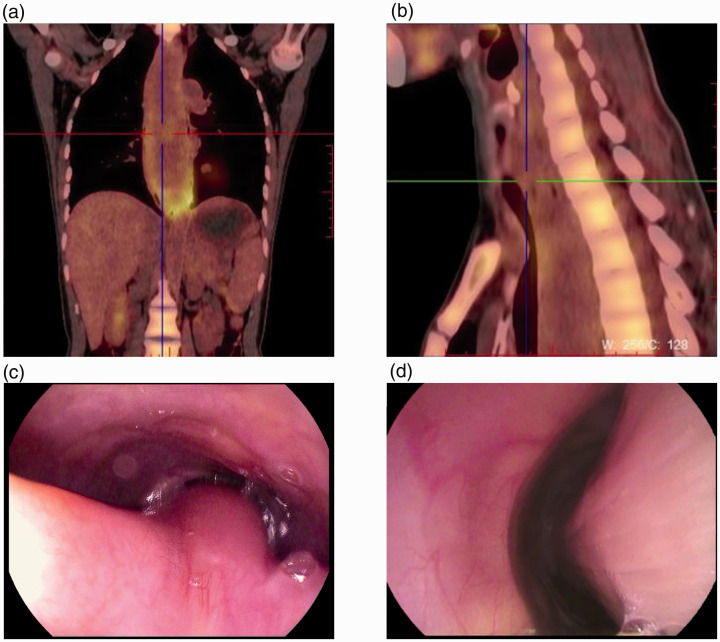
A 43-year-old woman presented with dysphagia. At presentation, she had been suffering with dysphagia for 2 months, sometimes accompanied by choking, shortness of breath, and fever. Blood laboratory testing showed elevated inflammatory markers and decreased hemoglobin and albumin concentrations. The proportion of neutrophils was 80%, C-reactive protein concentration was 98 mg/L, hemoglobin was 98 g/L, and albumin was 31 g/L. Positron emission tomography-computed tomography (PET-CT) was performed and revealed obvious esophageal dilatation and a visible columnar soft tissue mass shadow in the esophagus. The lesion appeared to have a wide base connected to the right anterior wall of the upper esophagus (Figure 1a and b). 18F-fluoroxy-d-glucose (FDG) metabolism was not increased in the upper segment of the lesion, which suggested a benign lesion. FDG metabolism (maximum standardized uptake value (SUVmax)/mean: 3.6/2.5) in the lower segment of the lesion was slightly increased, and a local inflammatory lesion was considered.
Figure 1.
Endoscopic findings in the case. (a) There was a columnar mass occupying the entire esophageal cavity. (b) The broad base of the lesion appeared to be connected to the right anterior wall of the upper esophagus. (c) The lesion began 15 cm from the incisors and connected with the esophageal wall. (d) From 15 cm from the incisors to the lower esophagus (mass length: 15 cm), the lesion comprised a rod-shaped mass with a smooth mucosal surface.
The patient then underwent endoscopic examination, which revealed that the lesion began 15 cm from the incisors and connected with the esophageal wall. From 15 cm from the incisors to the lower segment of the esophagus, the lesion was a rod-shaped mass with a smooth mucosal surface and measured 15 cm in length (Figure 1c and 1d). Ultrasonography showed that the lesion was located in the submucosa, with moderate echogenicity and homogeneous internal echogenicity with focal hypoechogenicity. Fine-needle aspiration was performed, and the pathology results suggested fibroblastic hyperplasia with no evidence of malignancy. According to the results of the examinations, the esophageal submucosal tumor was considered a benign lesion, and endoscopic submucosal dissection (ESD) was used to resect the lesion after obtaining informed consent.
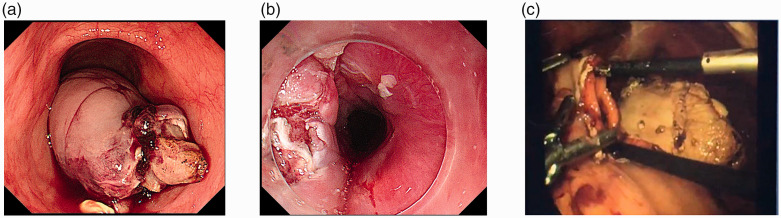
First, we injected a mixture of normal saline and methylene blue into the base of the lesion. Next, we used an IT knife (Olympus, Tokyo, Japan) and a Dual Knife (Olympus) to cut into the submucosa, and gradually stripped the lesion. Bleeding occurred repeatedly during resection, and the bleeding was stopped using coagulation forceps. Finally, the oral side of the lesion was completely dissected (Figure 2a and 2b). After resection, the surgeon attempted to remove the lesion with a snare and foreign body forceps; however, the lesion was too large to pass through the upper esophagus. Laser resection also failed, and finally, it was necessary to remove the lesion surgically. We cut the anterior wall of the gastric body, pulled the tumor from the esophagus into the stomach with grasping forceps, and removed it from the stomach (Figure 2c). The pathological results showed that the tumor was a fibrovascular polyp (Figure 3a and 3b). Follow-up gastroscopy was performed 1 and 6 months postoperatively; scar formation was visible, and no recurrence was found (Figure 3c).
Figure 2.
Resection of the giant esophageal polyp. (a) The oral side of the lesion was completely dissected. (b) The photograph shows the wound after removing the lesion. (c) The lesion was removed surgically. We cut the anterior wall of the gastric body, pulled the tumor from the esophagus into the stomach with grasping forceps, and then removed the polyp from the stomach.
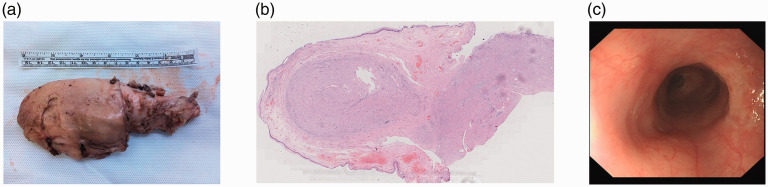
Figure 3.
Pathological results of the case. (a) The polyp measured 15 cm. (b) The polyp consisted mainly of fibrous, fatty, and vascular tissue. (c) One month postoperatively, the patient was re-examined by gastroscopy; scar formation was visible, and no recurrence was found.
The reporting of this study conforms to the CARE guideline.3 In this report, we have de-identified all of the patient’s details such that the patient’s identity may not be ascertained in any way.
Discussion
Fibrovascular polyps are benign neoplasms that usually occur in the cervical esophagus, but may also be seen in the pharynx. Fibrovascular polyps are usually elongated and covered with normal esophageal mucosa, with the largest reported size of 25 cm.4 These polyps are less likely to become malignant.5 Patients usually have no obvious symptoms in the early stage, and polyps often reach a large size by the time symptoms appear. Clinical symptoms caused by fibrovascular polyps comprise dysphagia, foreign body sensation, coughing, dyspnea, and even choking. Our patient presented with dysphagia, shortness of breath, and a giant esophageal polyp. This case reminds us that we should be alert to this disease when we encounter similar symptoms.
Fibrovascular polyps are rare clinically and are difficult to diagnose. Supplementary examinations play an important role in determining the nature and origin of the lesion. Upper gastrointestinal tract barium contrast examination usually reveals a dilated esophagus and long, smooth filling defects in the lumen of the upper esophagus,4 which can be used as a primary screening examination. CT and magnetic resonance imaging (MRI) can provide effective diagnostic information as non-invasive tests.6 Cervicothoracic CT provides information regarding the signal characteristics of the mass, the relationship with the surrounding organs and tissues, and the nutrient vessels, which play important roles in guiding the clinical treatment.7 In this case, the patient underwent PET-CT in addition to plain CT, which not only provided the above information, but also indicated additional FDG values at different locations within the polyp, which further helped determine the benign and malignant nature of the lesion. Therefore, PET-CT can be included in the pre-treatment adjuvant examinations for some patients who are diagnostically difficult, where financially feasible.
Gastroscopy and endoscopic ultrasonography (EUS) are important for the diagnosis and differential diagnosis of esophageal fibrovascular polyps. Gastroscopic observation of the lesion provides better visualization, and the location, size, and surface of the lesion can be more accurately described. Endoscopically, fibrovascular polyps usually appear as a relatively large intraluminal mass that is movable and which covers the normal esophageal mucosa. However, these polyps sometimes escape diagnosis when the normal mucosa covers their surface and are misdiagnosed as malignant tumors because the pedicles are not easily found.8 EUS permits real-time ultrasonographic scanning to obtain information such as the location of the polyp's origin, echogenicity, and vascularity.9 In addition to routine biopsy, EUS can also permit fine-needle aspiration for lesions under ultrasound guidance, which improves the positivity rate of biopsy.10 Histopathologically, the main body of fibrovascular polyps consist of fibrous, fatty, and vascular tissue, which is covered with squamous epithelium. Histopathological features are critical to the differential diagnosis.11
To relieve symptoms and prevent serious complications, such as bleeding, infection, and asphyxia, fibrovascular polyps should be removed promptly after discovery. Depending on the characteristics of the polyp, such as size and location, different treatment options are possible and mainly comprise endoscopic or surgical removal.12 A systematic review of esophageal lipomas and liposarcomas summarized the therapeutic approach to esophageal lipoma in 165 patients reported between 1955 and May 2020 (Table 1).13 Endoscopic treatment and surgical resection each have advantages and weaknesses. For example, endoscopic resection is relatively minimally invasive, but exposing the lesion is more difficult, and the risk of unmanageable bleeding is higher. In addition, surgeons must choose a more specific method according to the condition, such as whether to cut under gastroscopy or laryngoscopy, and whether to perform transthoracic or laparoscopic surgery.14–19 Regardless of the treatment modality chosen, a thorough and accurate preoperative evaluation of the polyp and the patient's general condition is necessary.20,21 Adequate preoperative preparation is also critical to the final success of the treatment. The patient in this case was inadequately prepared despite adequate preoperative evaluation. Although the lesion was eventually successfully resected, we were forced to convert the endoscopic procedure to surgery, urgently and unexpectedly.
Table 1.
Therapeutic approach to esophageal lipoma in 165 patients.13
| Therapy | n (%) | Morbidity | Mortality |
|---|---|---|---|
| Cervicotomy | 63 (38.2) | 1 | 0 |
| Endoscopy | 46 (27.9) | 1 | 1 |
| Flexible | 39 (23.7) | ||
| Rigid | 7 (4.2) | ||
| Thoracotomy | 44 (26.7) | 1 | 0 |
| Esophagectomy | 5 (3) | 2 | 0 |
| Laparoscopy | 3 (1.8) | 0 | 0 |
| Thoracoscopy | 3 (1.8) | 0 | 0 |
| Laparotomy | 1 (0.6) | 0 | 0 |
The pathological results in this case were consistent with a fibrovascular polyp. Because the polyp was difficult to remove, the specimen was cut. However, because the specimen was not intact, we could not examine the resection margins. There is a published review of the clinical-pathological and molecular features of esophageal lipoma and liposarcoma that found MDM2 amplification by fluorescence in situ hybridization in all cases, with some patients developing recurrent disease.13 Unfortunately, we did not perform MDM2 amplification by fluorescence in situ hybridization for the polyp in our patient. In the future, with these lesions, we will take care to improve detection to help determine the nature of the lesions.
In the cited review, there were five reported recurrences or malignant transformations after initial snare excision of an apparently benign lipoma.13 Given the potential malignancy of esophageal lipomatous neoplasms, careful histopathological assessment of the margin is recommended after resection, and patients should be advised regarding the need for endoscopic/radiologic surveillance.
We have learned from this case that fibrovascular polyps are often large, and if endoscopic resection is chosen, it is necessary to consider the difficulties that may be encountered during resection, such as the method of removing the polyp, before initiating treatment, to avoid awkward and potentially difficult situations intraoperatively.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605211039801 for Difficult endoscopic resection of a giant esophageal fibrovascular polyp: case report and literature review by Dan Nie, Ye Zong and Jielin Li in Journal of International Medical Research
Footnotes
Author contributions: DN conceived the report and participated in drafting the manuscript. YZ participated in the data acquisition and critically reviewed the manuscript. JL participated in the conception and design of the report and critically revised the manuscript. All authors read and approved the final manuscript.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Ethics statement: Our institution does not require ethics approval for case reports. We have de-identified the details such that the patient’s identity may not be ascertained in any way; therefore, we did not obtain informed consent.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Dan Nie https://orcid.org/0000-0003-1665-8387
References
- 1.Plachta A.Benign tumors of the esophagus. Review of literature and report of 99 cases. Am J Gastroenterol. 1962; 38: 639–652. [PubMed] [Google Scholar]
- 2.Pallabazzer G, Santi S, Biagio S, et al. Difficult polypectomy-giant hypopharyngeal polyp: case report and literature review. World J Gastroenterol. 2013; 19: 5936–5939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache. 2013; 53: 1541–1547. [DOI] [PubMed] [Google Scholar]
- 4.Blacha MM, Sloots CE, Van Munster IP, et al. Dysphagia caused by a fibrovascular polyp: a case report. Cases J. 2008; 1: 334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caceres M, Steeb G, Wilks SM, et al. Large pedunculated polyps originating in the esophagus and hypopharynx. Ann Thorac Surg. 2006; 81: 393–396. [DOI] [PubMed] [Google Scholar]
- 6.Ascenti G, Racchiusa S, Mazziotti S, et al. Giant fibrovascular polyp of the esophagus: CT and MR findings. Abdom Imaging. 1999; 24: 109–110. [DOI] [PubMed] [Google Scholar]
- 7.Wang J, Han DM, Ni X, et al. Fibrovascular polyp of the hypopharynx and esophagus. Chin Med J (Engl). 2011; 124: 3182–3184. [PubMed] [Google Scholar]
- 8.Yannopoulos P, Manes K.Giant fibrovascular polyp of esophagus- imaging techniques can localize, preoperatively, the origin of the stalk and designate the way of surgical approach: a case report. Cases J. 2009; 2: 6854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Costa PM, Marques A, Tavora et al. Inflammatory fibroid polyp of the esophagus. Dis Esophagus. 2000; 13: 75–79. [DOI] [PubMed] [Google Scholar]
- 10.Zhang H, Nie RH.A rare case of giant fibrovascular polyp of the esophagus. Saudi Med J. 2015; 36: 1348–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jiang W, Wang YJ.Advances in the diagnosis and treatment of esophageal fibrovascular polyps. Natl Med J China. 2016; 96: 3434–3436. [Google Scholar]
- 12.McLean JN, DelGaudio JM.Endoscopic resection of a giant esophageal polyp: case report and review of the literature. Am J Otolaryngol. 2007; 28: 115–117. [DOI] [PubMed] [Google Scholar]
- 13.Ferrari D, Bernardi D, Siboni S, et al. Esophageal lipoma and liposarcoma: a systematic review. World J Surg. 2021; 45: 225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paik HC, Han JW, Jung EK, et al. Fibrovascular polyp of the esophagus in infant. Yonsei Med J. 2001; 42: 264–266. [DOI] [PubMed] [Google Scholar]
- 15.Chourmouzi D, Drevelegas A.Giant fibrovasular polyp of the oesophagus: a case report and review of the literature. J Med Case Rep. 2008; 2: 337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee SY, Chan Wh, Sivanandan R, et al. Recurrent giant fibrovascular polyp of the esophagus. World J Gastroenterol. 2009; 15: 3697–3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dutta R, Kumar A, Handa KK, et al. Large pedunculated fibrovascular polyp of oesophagus in a young woman. Interact Cardiovasc Thorac Surg. 2009; 9: 352–353. [DOI] [PubMed] [Google Scholar]
- 18.Lorenzo D, Gonzalez JM, Barthet M.Endoscopic resection of a giant esophageal fibrovascular polyp. Endoscopy. 2016; 48: E69–E70. [DOI] [PubMed] [Google Scholar]
- 19.Murino A, Eisendrath P, Blero D, et al. A giant fibrovascular esophageal polyp endoscopically resected using 2 gastroscopes simultaneously (with videos). Gastrointest Endosc. 2014; 79: 834–835. [DOI] [PubMed] [Google Scholar]
- 20.Haytoglu S, Tuhanioglu B, Bozkurttan A, et al. Giant hypopharyngeal fibrovascular polyp: a case report and review of the relevant literature. Case Rep Otolaryngol. 2015; 2015: 670302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park JS, Bang BW, Shin J, et al. A case of esophageal fibrovascular polyp that induced asphyxia during sleep. Clin Endosc. 2014; 47: 101–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605211039801 for Difficult endoscopic resection of a giant esophageal fibrovascular polyp: case report and literature review by Dan Nie, Ye Zong and Jielin Li in Journal of International Medical Research