1. Background
It is estimated that 54,870 women will be diagnosed with endometrial cancer in the United States in 2015 [1]. Among those diagnosed, 10,170 women are predicted to die of the disease. Over the course of lifetime, the estimated risk of developing endometrial cancer is 2.8%, with median age at diagnosis of 62 years. Literature suggests that obesity is one of the most significant risk factors for endometrial cancer [2–4], and continues to be a long-term threat to health and quality of life survivors [5–8].
In order to improve quality of life and reduce obesity-related comorbidities of endometrial cancer patients, there has been an increased interest in delivering lifestyle interventions to this population [9–10]. However, behavioral interventions targeted at changing patterns of sedentary and physical activities in cancer survivors have often shown to have low adherence [6,11]. Existing literature suggests associations between physical activity and quality of life [12–13], but limited data exist on whether baseline quality of life is associated with completion of exercise intervention studies in cancer survivors.
The aim of this study is to explore linear- and non-linear associations between various domains of quality of life and study completion in a sample of endometrial cancer survivors. We hypothesized that (1) participants’ reporting higher quality of life would be more likely to be study completers, and that (2) associations between important quality of life factors and odds of study completion would be non-linear.
2. Methods
2.1. Sample
This study is a secondary data analysis of the Steps to Health project, which was a one-arm longitudinal study designed to investigate factors influencing exercise adoption in endometrial cancer survivors receiving an exercise intervention. Participants were recruited from M.D. Anderson Cancer Center’s Gynecologic Oncology Center and the Gynecologic Oncology outreach program, as well as the Gynecological Oncology of Houston, a Houston-based community practice (study conducted from January 2007 to December 2009). Potentially eligible participants were identified using medical records data, and were approached through telephone, mail, or during the clinic appointment. Inclusion criteria were: 1) endometrial cancer survivors diagnosed with Stage I, II, or IIIa in the last five years who finished surgery or radiation treatment for at least six months; 2) able to speak and read English; 3) oriented to person, time, and place such as one’s ability to simply identify their name, where they currently are, and day of the week; and 4) who had physician approval to engage in moderate physical activity. Interested participants were excluded from the study if they had met physical activity guidelines for at least 6 months which was defined as doing moderate-to-vigorous intensity exercise 5 days per week for at least 30 minutes or doing vigorous intensity exercise 3 days per week for at least 20 minutes. Survivors participated in a 6-month longitudinal study with assessment periods: baseline (T0), 2 months (T1), 4 months (T2), and 6 months (T3). All assessment periods had laboratory and home-based components. Laboratory assessments included cardiorespiratory fitness test and questionnaires. Home-based components used ecological momentary assessment (EMA) to capture participants’ behavior or state and real time and accelerometers to measure physical activity in real living conditions. Previous publications from this study reported associations between participants’ self-efficacy and exercise behavior [14] and differences between obese and non-obese participants in their response to the exercise intervention [16]. Further details on the study design have published previously [14–16].
2.2. Intervention
The intervention included: a personalized exercise prescription given at the baseline assessment based on cardiorespiratory fitness, 14 telephone counseling sessions, printed support materials, and a pedometer. The exercise recommendation was prepared by a masters-level exercise physiologist to provide at least 30 minutes of moderate-intensity exercise per day, for at least five days per week. The telephone counseling sessions consisted of 20- to 30-minute calls designed to increase adherence by providing feedback on participant exercise progress, discussing health issues that may interfere with exercise, and suggesting behavioral skills to overcome such barriers. The calls were scheduled weekly in months 1 and 2, bi-weekly in months 3 and 4, and monthly in months 5 and 6. Printed support materials describing the behavioral techniques were mailed to participants prior to telephone counseling. Pedometers were provided to help participants track their levels of exercise.
2.3. Measures
Quality of Life
Quality of life was measured using five different questionnaires self-administered at the T0 and T3 assessments.
SF-36
The Medical Outcomes Study (SF-36) US Standard Version 1.0 is a 36-item survey that measures physical and mental health. The questionnaire consists of 8 scales (physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional and mental health). The possible answers to the questions are either dichotomous “yes-no” or Likert scaled responses of varied length. For each of the 8 subscales, percentage score is calculated to represent score range from 0 (lowest level of functioning) to 100 (highest level of functioning). The SF-36 Version 1.0 was found to have high internal consistency reliability coefficients above .80 (the accepted standard) in all scales except Social Functioning which had a median coefficient of .76 [17]. Internal consistency (Cronbach’s alpha) in this sample was high for the subscales (α ≥.80) except for mental health (α=.77), and general health (α=.77).
QLACS
The Quality of Life in Adult Cancer Survivors (QLACS) is a 47-item survey which has 28 cancer-specific items and 19 generic items [18]. Five cancer-specific domains (appearance concerns, financial problems, distress over recurrence, family-related distress, and benefits of cancer) and 7 generic domains (negative feelings, positive feelings, cognitive problems, sexual problems, physical pain, fatigue, and social avoidance) are identified. The responses used a scale from 1 (Never) to 7 (Always). Initial psychometric evaluations indicate that the Cronbach’s alphas were greater than 0.8 with a range from 0.81 to 0.88 for the cancer-specific domains [18], and above 0.7 with a range of 0.72 to 0.91 for generic domains [18]. Internal consistency (Cronbach’s alpha) in this sample was high for the subscales (≥.80) in this sample except negative feelings (α =.74), and appearance concerns (α =.56).
Perceived Stress Scale (PSS)
The Perceived Stress Scale (PSS) is a 14-item questionnaire that measures the participant’s perceived stress in addition to their view of their lives [19–20]. The survey uses Likert rating scales with questions that measure the frequency of experiences during the last 4 weeks from “Never” (0) to “Very Often” (4). The PSS had high Cronbach alphas ranging 0.84 to 0.86 across the three samples tested during the initial development of the instrument [19]. A perceived stress score is derived as sum of the responses. Internal consistency (Cronbach’s alpha) in this sample was high (α=.86).
Pittsburgh Sleep Quality Index (PSQI)
The Pittsburgh Sleep Quality Index (PSQI) is a 19-item survey that measures the quality and patterns of sleep in the last 4 weeks [21]. The responses are on a “Not during the past month (0)” or “Very good (0)” to “Three of more times a week (3)” or “Very Bad (3)” Likert-ranking scale where a higher score indicates poorer sleep. The PSQI results in seven components scores that are calculated into a global score where a score greater than 5 reflects a person with poor sleep. The instrument reports a Cronbach’s alpha of 0.83 across the seven components [21]. Internal consistency (Cronbach’s alpha) in this sample was α=.71.
Brief Symptom Inventory 18 (BSI-18)
The Brief Symptom Inventory 18 (BSI-18) is an 18-item survey that identifies psychological distress and psychiatric disorders with 6-items on each of the following specific criteria: somatization, depression, and anxiety [22]. The three criteria are summed to comprise the Global Severity Index (GSI). The responses are on a 0 to 4 Likert Scale where 0 represents “Not at all” and 4 represents “Extremely”. Across the four criteria, the internal consistency reliability coefficient was at least 0.74 (Somatization) with a maximum of 0.89 (GSI). Internal consistency (Cronbach’s alpha) for the GSI in this sample was high (α=.84).
Study completion
Participants who have completed any of the the laboratory (cardiorespiratory fitness test or questionnaires) or the home-based components (EMA or accelerometer) for all scheduled assessment times (T0, T1, T2, T3) were considered as completers. Otherwise, they were considered to be non-completers. For example, if an individual missed all laboratory and home-based components at any of the scheduled assessment times, then the individual is classified as a non-completer. On the contrary, if an individual completed any of the laboratory or home-based component for all assessment times, then the person was considered a completer.
2.4. Statistical Methods
Sample characteristics between study completers and non-completers were compared using Fisher’s exact and Welch’s two sample t-tests. Associations between baseline quality of life factors and study completion were examined using generalized additive models [23]. Generalized additive models (GAMs) are an extension of the generalized linear models that accommodates response variables with distributions other than the normal distribution (i.e. counts or binary outcomes), as well as non-linear associations between the predictors (e.g., quality of life subscale) and the response function (e.g. log odds of study completion). In GAMs, the effects of predictor variables are estimated by fitting a smoothing curve through the data. The estimated effect of the predictor from GAM can either be linear or non-linear, depending on the nature of association. This approach is particularly attractive when there is no a priori reason for choosing a particular response function (i.e. linear, quadratic, cubic, log, square root, etc.). A logit link function was used to associate log odds of study completion to the covariates.
In order to avoid fitting large number GAMs for each of the quality of life factors measured with instruments: SF-36, QLACS, PSS, PQSI, and BSI-18, we performed a variable and function selection procedure [24–25]. The objective of this variable selection procedure was to identify a handful of quality of life factors highly associated with the odds of study completion among: i) 8 subscales and 2 composite scores (Physical and Mental Component Scores) from SF-36, ii) 12 subdomains and 2 total scores (for cancer specific and generic) from QLACS, iii) 3 symptom specific and 1 total score from BSI-18, and iv) two global scores from each of PSS and PQSI. Our variable selection procedure considered all 30- quality of life factors described above, both in linear and in non-linear form. This helped us to simultaneously evaluate important qualify of life factors associated with study completion, and also examine whether the association can be best explained in linear or non-linear fashion. Specifically, the variable selection procedure was carried out by introducing a binary latent variable for each of the coefficients of a saturated model including all potential predictors specified in both linear and non-linear fashion [24–25]. The binary (1 or 0) indicator variable represented a decision whether to include or exclude the variable (either in linear or non-linear associations to the outcome). A measure of variable importance was quantified as a probability of the indicator being 1, generated using a Markov chain Monte Carlo (MCMC) inference. The variable selection algorithm was implemented using an R package spikeSlabGAM [24], by generating the posterior distribution of the inclusion probability. The MCMC inference was based on 60,000 samples from 3 Markov chains, each running after a burn-in sample of 10,000. We selected quality of life factors with highest posterior inclusion probability (with minimum value of marginal inclusion probability specified as .25, as suggested by [24]).
Final models presented in this study fitted GAMs for each quality of life factors identified by the variable selection procedure, in associations to the log odds of study completion, adjusting for important covariates. If non-linear associations between the quality of life factor and the outcome variable were identified in the variable selection procedure, cubic splines (to allow for wide range of possible shapes) were used to estimate the smoothing curves in the GAMs. Optimal smoothing parameters were chosen using the generalized cross validation procedure [26], with the maximum number of knots restricted to 4, following the widely adopted suggestion by Keele [27]. In order to control for the type I error in testing multiple hypotheses for associations between quality of life factors and odds of study completion, p-values were adjusted for false discovery rate [28]. In this method, adjusted values are simply obtained by ordering the p-values from smallest to largest and multiplying it by N/rank, where N is the number of tests. If the adjusted p-value is larger than the largest p-value, then it is substituted with the largest p-value. All statistical analyses were performed using R version 3.2.0 [29]. The GAMs were fitted using the mgcv package [30]. Statistical significance level was set at 0.05 for all tests.
3. Results
3.1. Descriptive Statistics
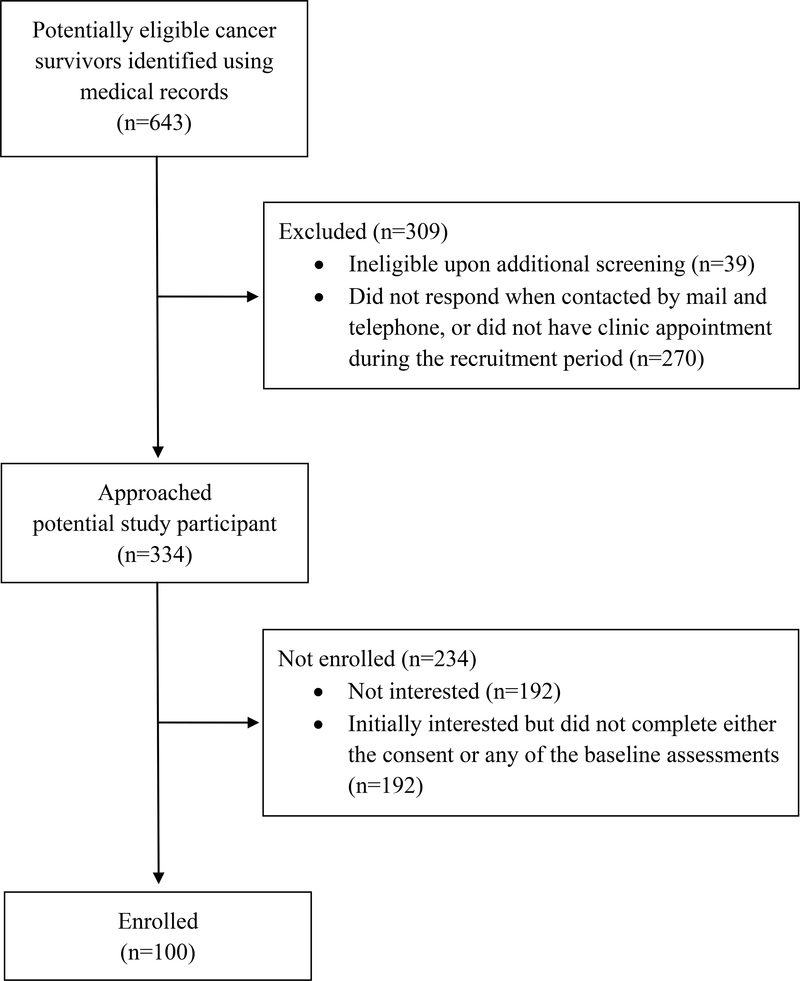
A flow diagram illustrates cancer survivors who were potentially eligible, approached, and enrolled to the study (Figure 1). The majority of the participants were non-Hispanic whites (75%), had at least some college education or received a two-year degree (77%), and obese (64%). On average, participants were aged 57 years (Range: 25–76), had Body mass index (BMI, kg/m2) of 34 (Range: 19–69), and 2.2 years (Range: .5–5.2) from time of diagnosis of endometrial cancer.
Figure 1.
Consort diagram.
All participants in the Steps to Health study completed at least one of the laboratory or home-based component at baseline. On month 2, 13 individuals missed all laboratory and home-based components. Subsequently, only 83 and 79 participants completed at least one of the laboratory or home-based components, respectively, at months 4 and 6. Overall, 74 participants were classified as completing the study, since they completed at least one component from laboratory or home-based assessment for all measurement periods. The remaining 26 percent of the participants missed all scheduled assessments, for at least one measurement time. Participant characteristics of race and disease stage differed between completers and non-completers in Fisher’s exact tests (Table 1): the completer group had higher proportions of non-Hispanic whites, and survivors diagnosed with disease stages II or higher. Among non-completers, participant who completed no measurement components beyond baseline were younger in age compared to those who completed at least one during months 2, 4, and 6 (p=.004), while no statistically significant differences were found between characteristics of race, education, disease stage, and treatment.
Table 1.
Sample characteristics.
| Characteristic | N (%) | P-value | |
| Completers | Non-completers | ||
| N=74 | N=26 | ||
|
| |||
| Race | 0.020a | ||
| Black/non-Hispanic | 5 (6.8) | 2 (7.7) | |
| White/non-Hispanic | 60 (81.1) | 15 (57.7) | |
| Asian/non-Hispanic | 4 (5.4) | 1 (3.8) | |
| White/Hispanic | 5 (6.8) | 7 (26.9) | |
| American Indian/non-Hispanic | 0 (0) | 1 (3.8) | |
| Education | 0.059a | ||
| < High school | 1 (1.4) | 1 (3.8) | |
| High school diploma/GED | 7 (9.5) | 6 (23.1) | |
| Technical/vocational degree | 3 (4.1) | 5 (19.2) | |
| Some college/Two-year degree | 29 (39.2) | 7 (26.9) | |
| Four-year degree | 20 (27.0) | 4 (15.4) | |
| Advanced degree | 14 (18.9) | 3 (11.5) | |
| Disease stage | 0.016a | ||
| I | 55 (74.3) | 25 (96.2) | |
| II | 16 (21.6) | 0 (0) | |
| IIIa | 3 (4.1) | 1 (3.8) | |
| Treatment | 0.489a | ||
| Surgery only | 41 (55.4) | 17 (65.4) | |
| Surgery + radiotherapy | 33 (44.6) | 9 (34.6) | |
|
| |||
| Mean (SD) |
P-value | ||
| Completers | Non-completers | ||
|
| |||
| Age, years | 57.7 (10.3) | 55.0 (12.6) | 0.337b |
| Years since diagnosis | 2.3 (1.3) | 2.1 (1.1) | 0.393b |
| Body mass index (BMI), kg/m2 | 33.7 (9.6) | 36.2 (8.8) | 0.225b |
| Minutes of moderate-vigorous physical activity per dayc | 15.3 (11.8) | 11.8 (11.7) | 0.204b |
Fisher’s exact was performed to examine independence between completion status and sample characteristic.
Welch’s two sample t-tests were performed (assuming nonhomogeneity of variance).
Minutes of moderate-vigorous physical activity (MVPA) were quantified as a combination of EMA and accelerometry measurements. Participants reported duration of MVPA through EMA in real-time upon completion of exercise, and at night time of each measurement day. Participants were also asked to wear accelerometers during the same period. Since EMA or accelerometer measurements were missing for some days, the minutes of MVPA per day combined the EMA and accelerometer measures in the following hierarchy: i) real-time EMA minutes used as a primary measure, ii) night-time EMA minutes used if real-time minutes were missing, iii) accelerometer MVPA minutes (quantified using Freedson’s (1998) cut-point) used if both EMA assessments were missing.
3.2. Associations between study completion and quality of life
Generalized additive models were used to explore associations between study completion and quality of life, adjusting for individuals’ race (dichotomized as non-Hispanic whites vs. other), and disease stage (dichotomized as disease stage I vs. higher), which significantly differed between completers and non-completers.
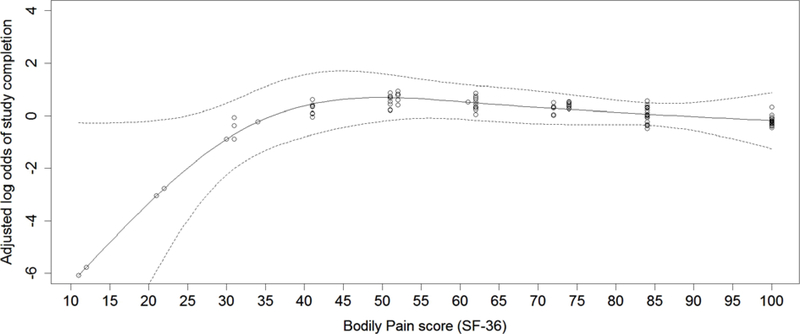
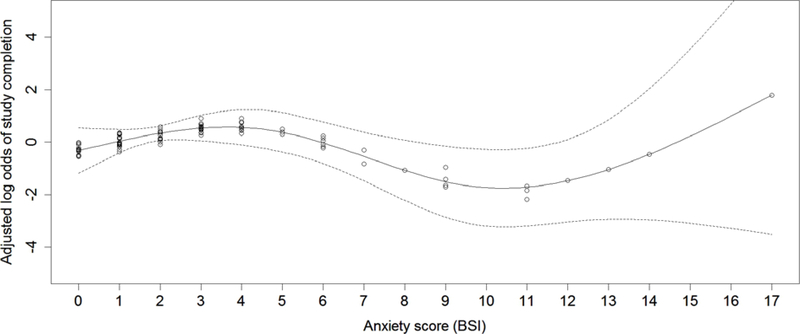
Important quality of life factors associated with the odds of study completion were identified using a variable selection procedure described in the statistical methods section. A total of thirty quality of life factors from five different questionnaires were considered. The variable and function selection algorithm suggested considering non-linear associations between subscales of bodily pain (SF-36) and anxiety (BSI-18), and the odds of study completion. Therefore, we fitted two GAMs, each considering bodily pain (SF-36) and anxiety (BSI-18) scores as main predictors, adjusting for individuals’ race (dichotomized as non-Hispanic whites vs. other) and disease stage (dichotomized as disease stage I vs. higher). Both quality of life factors, bodily pain (p=.025) and anxiety (p=.035) were significantly associated with the odds of study completion (p-values were adjusted for false discovery rate as described in the statistical methods section). The non-linear associations between the quality of life factors and the odds of study completion were interpreted visually. The estimated smoothing curve for the bodily pain score (Figure 2) indicate that improvements in the bodily pain quality of life were associated with increased odds of study completion, especially for individuals in lower range (i.e. 10–45), when the model was adjusted for covariates of race and disease stage. An improvement in the bodily pain quality of life did not seem to contribute to the increase in the odds of study completion for individuals with relatively higher score (i.e. 45–100). Associations between the odds of study completion and anxiety score (BSI-18) showed two different trends (Figure 3): whereas increases in anxiety was associated with higher odds of completion for individuals with low (i.e. anxiety score 0–4) anxiety levels, increase in anxiety contributed to lower odds of study completion for individuals with anxiety scores of approximately 5 to 10. Although individuals with high anxiety levels (i.e. anxiety score 10–17) showed a similar trend as individuals with low anxiety (i.e. anxiety score 0–4), there were greater degree of uncertainty in this score range, since only a small fraction of individuals had anxiety scores higher than 10. The model was adjusted for covariates of race and disease stage.
Figure 2.
Association between bodily pain (SF-36) and study completion.
Note 1: Circles in the plots represents predicted values based on the observed data. Multiple individuals had same subscale score: individuals with the same subscale score have the same predicted values on the estimated smoothed function. To visualize the number of observations across the subscale score range and to prevent overlapping values due to same subscale score, values were jittered by adding random noise.
Note 2: Solid line represents the estimated function from GAM, when adjusted for covariates of race (dichotomized as non-Hispanic whites vs. other) and disease stage (dichotomized as disease stage I vs. higher).
Note 3: The dotted lines represent 95% confidence bands.
Figure 3.
Association between anxiety (BSI) and study completion.
Note 1: Circles in the plots represents predicted values based on the observed data. Multiple individuals had same subscale score: individuals with the same subscale score have the same predicted values on the estimated smoothed function. To visualize the number of observations across the subscale score range and to prevent overlapping values due to same subscale score, values were jittered by adding random noise.
Note 2: Solid line represents the estimated function from GAM, when adjusted for covariates of race (dichotomized as non-Hispanic whites vs. other) and disease stage (dichotomized as disease stage I vs. higher).
Note 3: The dotted lines represent 95% confidence bands.
4. Conclusions
4.1. Summary of Findings
In summary, results from this study indicate that quality of life domains of pain and anxiety may be important factors associated with study completion in exercise intervention studies for endometrial cancer survivors. Quality of life domains of bodily pain contributed in a non-linear way, suggesting that improvements in this factor may be associated with participants’ study completion, especially for individuals under greater impairments. Lastly, increased levels of anxiety were associated with lower odds of study completion for individuals with BSI subscale score between 5–10, but associated with higher odds of study completion for individuals for very low anxiety (BSI-18 subscale score between 0–4).
4.2. Implications
Participants’ study completion can be challenging in studies delivering lifestyle exercise interventions to cancer survivors. Endometrial cancer survivors have a high BMI compared to all other cancer types [31], and the comorbidities associated with obesity generally have a negative impact on quality of life outcomes [32–33].
While several studies have reported differences in the quality of life between study completers and non-completers in exercise studies of non-cancer patients [34–35], these results may not be generalizable to cancer survivors. For example, in the Program for All-Inclusive Care of Elders (PACE), a study aimed at increasing moderate exercise among functional impaired older African American women [34], non-completers were more likely to report higher scores on scales related to depression than completers. In another investigation of non-cancer patients called the Look AHEAD (Action for Health in Diabetes) study [35], subjects who missed visits had lower functioning scores in the SF-36 domains of general health, role emotional, and mental health than completers in this study. Interestingly, none of these quality of life factors have been identified as important attributes relating to study completion in our investigation of endometrial cancer survivors. This suggests that endometrial cancer survivors may have different domains of quality of life factors associated with study completion.
Several existing literature have suggested non-linear relations between different health-related quality of life factors [36], between health-related quality of life factors and response to environmental stress [37], or between quality of life factors and disease status [38]. However, non-linear associations between quality of life factors and odds of study completion have rarely been investigated. To our knowledge, this is a first study to examine non-linear associations between quality of life factors and study completion, in a sample of endometrial cancer survivors. We have implemented an exhaustive exploration of a total of 30 quality of life factors from five instruments to determine linear and non-linear associations to the odds of study completion through a MCMC inference.
Findings from our study fill the gap in the literature on health-related quality of life factors contributing to completion of study delivering lifestyle exercise intervention for endometrial cancer survivors. Results suggest that study completion may be improved if participants with more disruptions in quality of life from pain and anxiety were identified at the beginning of the study. While our findings for pain may simply suggest a threshold where improvements in the pain related quality of life no longer affects the odds of staying in the study, the relation between anxiety and study completion is more intriguing. Such inverse-U shaped curve has often been proposed to study optimum levels of stress and arousal for effective learning [39] and sports performance [40]. The theory that performance of a certain task may be impaired under conditions above or below the optimal arousal or stress levels may to be relevant in explaining the inverse-U shaped curve we have found in explaining the associations between anxiety and the odds of study completion.
In summary, conclusions from this study suggest that study completion rates may be improved by providing additional support and follow-up for participants at high risk of dropping-out and tailoring study requirements to participants’ quality of life. Strengths of the current study include the exhaustive variable and function selection procedure to identify the health-related quality of life factor and its associational form to the odds of study completion. Further research is needed to assess whether the non-linear associations between the quality of life factors of pain and anxiety and the odds of study completion can be replicated in an independent, larger sample of endometrial cancer survivors receiving similar lifestyle intervention. In addition, conclusions drawn from this study only suggest possible associations between the quality of life factors and study completion. A randomized, controlled study is needed to draw and causative conclusions between the quality of life factors and study completion.
Funding
This study was supported by R01 CA 109919, R25T CA057730, R25E CA056452, P30 CA016672 (PROSPR Shared Resource), Center for Energy Balance in Cancer Prevention and Survivorship, Duncan Family Institute for Cancer Prevention and Risk Assessment, and by the National Institutes of Health through M. D. Anderson’s Cancer Center Support Grant (NCI Grant P30 CA016672).
Footnotes
Conflict of Interest
None of the authors have any relevant financial interests or conflicts to disclose.
COMPLIANCE WITH ETHICAL STANDARDS
Ethical Approval
Project Steps to Health procedures and materials have been reviewed and approved by the Institutional Review Boards of the University of Texas MD Anderson Cancer Center.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
REFERENCES
- 1.Surveillance Epidemiology and End Results. SEER State Fact Sheets: Corpus and Uterus, NOS. 2015; (Available from: http://seer.cancer.gov/statfacts/html/corp.html/.)
- 2.Chang SC, Lacey JV Jr., Brinton LA, et al. Lifetime weight history and endometrial cancer risk by type of menopausal hormone use in the NIH-AARP diet and health study. Cancer Epidemiology Biomarkers Prevention 2007;16(4):723–730. [DOI] [PubMed] [Google Scholar]
- 3.Friedenreich C, Cust A, Lahmann P, et al. Anthropometric factors and risk of endometrial cancer: the European prospective investigation into cancer and nutrition. Cancer Causes Control 2007;18(4): 399–413. [DOI] [PubMed] [Google Scholar]
- 4.McCullough ML, Patel AV, Patel R, et al. Body mass and endometrial cancer risk by hormone replacement therapy and cancer subtype. Cancer Epidemiology Biomarkers Prevention 2008;17(1):73–79. [DOI] [PubMed] [Google Scholar]
- 5.Fader A, Frasure H, Gil K, Berger N, von Gruenigen V. Quality of Life in Endometrial Cancer Survivors: What Does Obesity Have to Do with It? Obstetrics and Gynecology International 2011;2011(308609):01–6. DOI: 10.1155/2011/308609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rossi A, Moadel-Robblee A, Garber CE, et al. Physical activity for an ethnically diverse sample of endometrial cancer survivors: a needs assessment and pilot intervention. J Gynecologic Oncology 2015;26(2):141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smits A, Lopes A, Das N, Bekkers R, Galalla K. The impact of BMI on quality of life in obese endometrial cancer survivors: Does size matter? Gynecologic Oncology 2014;132(1): 137–141. [DOI] [PubMed] [Google Scholar]
- 8.Von Gruenigen V, Waggoner S, Frasure H, et al. Lifestyle Challenges in Endometrial Cancer Survivorship. Obstetrics and Gynecology 2011;117(1):93–100. [DOI] [PubMed] [Google Scholar]
- 9.McCarroll ML, Armbruster S, Frasure HE, et al. Self-efficacy, quality of life, and weight loss in overweight/obese endometrial cancer survivors (SUCCEED): A randomized controlled trial. Gynecologic Oncology 2013;132(2):397–402. [DOI] [PubMed] [Google Scholar]
- 10.Speck RM, Courneya KS, Mȃsse LC. An update of controlled physical activity trials in cancer survivors: a systematic review and meta-analysis. Journal of Cancer Survivorship 2010;4(2);87–100. [DOI] [PubMed] [Google Scholar]
- 11.Blanchard CM, Courneya KS, Stein K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: Results from the American Cancer Society’s SCS-II. Journal of Clinical Oncology 2008;26(36); 2198–2204. [DOI] [PubMed] [Google Scholar]
- 12.Buffart LM, Thong MSY, Schep G, et al. Self-reported physical activity: Its correlates and relationship with health-related quality of life in a large cohort of colorectal survivors. PLoS ONE 2012;7(5):1–9. DOI: 10.1371/journal.pone.0036164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Courneya KS, Friedenreich CM. Relationship between exercise pattern across the cancer experience and current quality of life in colorectal cancer survivors. Journal of Alternative Complement Medicine 1997;3:215–226. [DOI] [PubMed] [Google Scholar]
- 14.Basen-Engquist K, Carmack CL, Li Y, et al. Socialcognitive theory predictors of exercise behavior in endometrial cancer survivors. Health Psychology 2013;32:1137–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Basen-Engquist K, Carmack CL, Perkins H, et al. Design of the steps to health study of physical activity in survivors of endometrial cancer: testing a social cognitive theory model. Psychol Sport Exerc 2011;12:27–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basen-Engquist K, Carmack C, Brown J, et al. Response to an exercise intervention after endometrial cancer: Differences between obese and non-obese survivors. Gynecologic Oncology 2014;133:48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ware J, Snow K, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide, Nimrod Press: Boston, 1993. [Google Scholar]
- 18.Avis NE, Smith KW, McGraw S, et al. Assessing Quality of Life in Adult Cancer Survivors (QLACS). Quality of Life Research 2005;14:1007–1023. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S, Kamarck T, Mermelstein R. A Global Measure of Perceived Stress. Journal of Health and Social Behavior 1983;24:385–96. [PubMed] [Google Scholar]
- 20.Cole S Assessment of differential item functioning in the Perceived Stress Scale-10. Journal of Epidemiologic Community Health 1999;52:319–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buyesse D, Reynolds C, Monk T, Berman S, Kupfer D. The Pittsburgh Sleep Quality Index: A new Instrument for Psychiatric Practice and Research. Psychiatry Research 1988;28:193–213. [DOI] [PubMed] [Google Scholar]
- 22.Derogatis L Brief Symptom Inventory (BSI) 18: Administration, Scoring, and Procedures Manual, NCA Pearson: Minneapolis, 2001. [Google Scholar]
- 23.Hastie T, Tibshirani R. Generalized additive models. Statistical Science 1986;1(3):297–318. [DOI] [PubMed] [Google Scholar]
- 24.Scheipl F spikeSlabGAM: Bayesian Variable Selection, ModelChoice and Regularization for Generalized Additive Mixed Models in R. Journal of Statistical Software 2011;43(14);1–24. [Google Scholar]
- 25.Scheipl F, Fahrmeir L, Kneib T. Spike-and-slab priors for function selection in structured additive regression models. Journal of the American Statistical Association 2012; 107(500);1518–1532. [Google Scholar]
- 26.Trevor T, Tibshirani R. Generalized Additive Models, Chapman and Hall: London, 1990. [Google Scholar]
- 27.Keele LJ. Semiparametric Regression for the Social Sciences, John Wiley & Sons: West Sussex, 2008. [Google Scholar]
- 28.Benjamini Y, Hochberg Y. Controlling for false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B 1995;57(1);289–300. [Google Scholar]
- 29.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, 2008. [Google Scholar]
- 30.Wood SN. Generalized Additive Models: An Introduction with R, Chapman & Hall/CRC: Boca Raton, 2006. [Google Scholar]
- 31.Arem H, Chlebowski R, Stefanick ML, et al. Body mass index, physical activity, and survival after endometrial cancer diagnosis: results from the Women’s Health Initiative. Gynecologic Oncology 2013;128(2):181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Demark-Wahnefried W, Morey M, Sloane R, et al. Reach out to enhance wellness home-based diet-exercise intervention promotes reproducible and sustainable long-term improvements in health behaviors, body weight, and physical functioning in older, overweight/obese cancer survivors. Journal of Clinical Oncologyl 2012;30(19):2354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Demark-Wahnefried W, Platz EA, Ligibel JA, et al. The role of obesity in cancer survival and recurrence. Cancer Epidemiology Biomarkers & Prevention 2012;21:1244–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sullivan-Marx EM, Mangione KK, Ackerson T, et al. Recruitment and retention strategies among older African American women enrolled in an exercise study at a PACE program. The Gerontologist 2011;51 (1):73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fitzpatrick SL, Jeffrey R, Johnson KC, Roche CC, Van Dorsten B. Baseline predictors of missed visits in the Look AHEAD study. Obesity 2013;22(1):131–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miller A, Dishon S. Health-related quality of life in multiple sclerosis: The impact of disability, gender and employment status. Quality of Life Research 2006;15(2); 259–271. [DOI] [PubMed] [Google Scholar]
- 37.Dratva J, Zemp E, Dietrich F. Impact of road traffic noise annoyance on health-related quality of life: results from a population-based study. Quality of Life Research 2010;19;37–46. [DOI] [PubMed] [Google Scholar]
- 38.Stahl E, Lindberg A, Jansson S-A, et al. Health-related quality of life is related to COPD disease severity. Health and Quality of Life Outcomes 2005;3(56);1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Salehi B, Cordero I, Sandi C. Learning under stress: The inverted-U-shape function revisited. Learning Memory 2010;17;522–530. [DOI] [PubMed] [Google Scholar]
- 40.Kerr JH. The experience of arousal: A new basis for studying arousal effects in sport. Journal of Sport Sciences 1985;3;169–179. [DOI] [PubMed] [Google Scholar]