Antibacterial, antifungal, antiviral, and antiparasitic treatments developed in the past century have improved survival outcomes, even in high-mortality conditions such as sepsis, a condition that is mostly caused by bacteria but can also be due to other infections. In the 21st century, of all therapies that have improved the outcomes of patients with sepsis, the appropriate and early administration of antibiotics has been shown to be the most effective therapy to save lives.1 However, despite highly effective antibiotics that can kill microorganisms causing sepsis, and cultures showing eradication of these organisms, overall mortality from the condition remains high. In part, this high mortality might be explained by dysregulated immune responses arising from redundant pathways in the human immune system, which have developed—along with the array of defensive mechanisms involving the innate and adaptive responses, inflammation, and coagulation—as a result of the selective pressure of thousands of years of exposure to infections, zoonoses, and resulting epidemics and pandemics. This dysregulated immune response can be as harmful as, or more harmful than, the pathogens themselves.2 Accordingly, two original studies showed significant reduction in mortality due to sepsis among solid organ transplant recipients compared with patients without transplants.3, 4 This finding suggests that immunosuppressive drugs, required lifelong to avoid transplant graft rejection, might have been protective by decreasing dysfunctional responses to sepsis. These lessons learned from bacterial sepsis are highly relevant in the context of COVID-19.
Although one antiviral, remdesivir, has already shown significant clinical benefits in hospitalised patients with COVID-19,5 death from COVID-19 can occur because of a dysregulated immune response (akin to sepsis despite the use of effective antibiotics). This fact poses the question of whether any host immune interventions could improve the survival of patients with COVID-19. Again, similar to bacterial sepsis, studies evaluating steroid use in COVID-19 have produced both positive and negative results. However, the only positive study was an open-label trial,6 and no placebo-controlled double-blind studies have shown positive results to date.
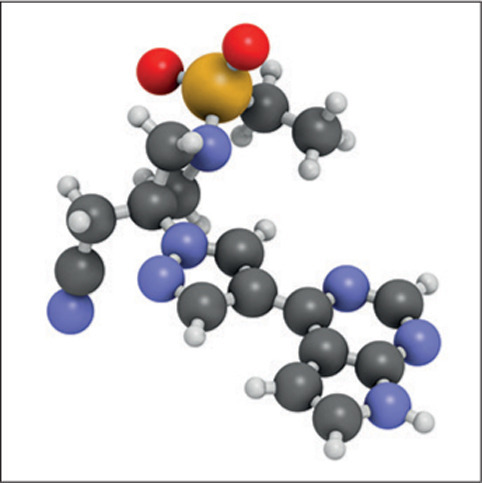
Another immunomodulatory approach that has been evaluated is the use of Janus kinase (JAK) inhibitors. Baricitinib, an inhibitor of JAK1 and JAK2, has been appraised in artificial intelligence and mechanistic laboratory studies and human clinical trials, with multiple mechanisms of action identified, including anticytokine effects and inhibition of host cell viral propagation.7 Potential side-effects of the drug, such as secondary infections and venous thrombosis, are related to changes in the inflammatory and coagulation cascades. However, these side-effects have been rare in patients with rheumatoid arthritis, the approved indication for baricitinib.8
In The Lancet Respiratory Medicine, Vincent Marconi and colleagues9 assessed the use of baricitinib in a randomised, placebo-controlled, double-blind trial (the COV-BARRIER study). Importantly, the study's randomisation was done strictly through an interactive response system and stratified by disease severity, age, region, and steroid use. The trial was conducted in 101 centres across 12 countries, and enrolled 1525 patients. Compared with placebo, patients who received baricitinib had a 38·2% relative reduction and 5 percentage points absolute reduction in 28-day all-cause mortality (hazard ratio [HR] 0·57 [95% CI 0·41–0·78]; nominal p=0·0018), with a number needed to treat (NNT) to prevent one additional death of 20. No other anti-COVID-19 therapy has shown such a profound reduction in mortality. For comparison, the only other two immunomodulatory treatments that were associated with a reduction in mortality were dexamethasone (which showed a 17% relative reduction and 2·8% absolute reduction in mortality and an NNT of 36)6 and tocilizumab (which showed a 15% relative reduction and 4% absolute reduction in mortality and an NNT of 25);10 however, these treatments were assessed in open-label trials with a high-risk of bias.
Although the COV-BARRIER trial did not show a statistically significant difference between groups for the composite primary disease progression outcome, a similar outcome was achieved in the Adaptive Covid Treatment Trial (ACTT)-2 study1, which also compared baricitinib against placebo, but in combination with remdesivir. There are two likely explanations for the differences between these trials. First, a synergistic effect of baricitinib with remdesivir could have further accelerated clinical recovery in ACTT-2 but not in COV-BARRIER (because only 18·9% received remdesivir). Second, administration of respiratory supportive care was heterogeneous in the 12 countries involved in the COV-BARRIER study, because both the indication and the timing of respiratory support interventions (ie, oxygen supplementation, high-flow oxygen, and invasive ventilation) were subject to indication bias, which can vary widely among countries. ACTT-2 was predominantly done in the USA, so a more homogeneous approach could have enabled the detection of the beneficial effects of baricitinib on clinical recovery.
COV-BARRIER showed marked reductions in 28-day and 60-day mortality, and ACTT-2, despite not being powered for mortality outcomes, showed a consistently better survival and a significant reduction in 28-day mortality (hazard ratio [HR] 0·47 [95% CI 0·24–0·93]) in patients who required supplemental or high-flow oxygen, very similar to that seen in the COV-BARRIER study (HR 0·57 [95% CI 0·41–0·78]). Importantly, the COV-BARRIER study showed that the survival benefits provided by baricitinib were independent of the presence or absence of concomitant use of steroids (mostly dexamethasone)—ie, an absence of treatment interaction. This finding is highly relevant because tocilizumab, another immunomodulatory drug, showed benefits in an open-label trial11 only if concomitant steroids were given; otherwise, it showed no benefits or was potentially harmful—ie, a significant treatment interaction was present.
From the bedside perspective, the safety results of the COV-BARRIER study confirmed the findings of ACTT-210 (ie, that treatment with baricitinib was not associated with more side-effects than placebo). This finding is noteworthy because, based on the ad hoc designs of both the COV-BARRIER and ACTT-2 studies, more secondary infections and thrombotic events could be expected in the baricitinib group. However, in more than 2500 patients, the safety of baricitinib was almost identical to that of placebo. In fact, in ACTT-2, the number of secondary infections was significantly lower in the baricitinib group than in the placebo group, suggesting that the immunomodulation provided by baricitinib might be protective and not as immunosuppressive as other drugs such as steroids. Furthermore, even with the addition of steroids (which were allowed for COVID-19 treatment in COV-BARRIER but not in ACTT-2), baricitinib was not associated with more infections. This finding not only confirms the safety profile in ACTT-2, but also provides reassurance for the first time that the combination of baricitinib and steroids might be safe. Because both baricitinib and steroids come in tablet form and are affordable, they lend themselves to use in low-income and middle-income countries. Baricitinib has few drug–drug interactions, is excreted largely unchanged, and can be used in older adults with comorbidities, such as a decreased glomerular filtration rate.
During the COVID-19 pandemic so far, only a few clinical trials have been done with the highest scientific rigour12 (placebo-controlled, double-blind, and with randomisation stratified by disease severity and site location), such as the ACTT5, 11 and COV-BARRIER trials. The clinical benefits and significant reduction in mortality, as well as the absence of safety concerns found by both the COV-BARRIER and ACTT-2 studies, place baricitinib among the few proven treatments of choice for hospitalised patients with COVID-19.
JS reports personal fees from Vaccitech, Heat Biologics, Eli Lilly, Alveo Technologies, Agenus, Equilibre Biopharmaceuticals, Graviton Bioscience Corporation, Greenmantle, Zedsen, BenevolentAI, Lansdowne Partners, Vitruvian, BB Healthcare Trust PLC, and Celltrion; lecture fees from Eli Lilly; and advisory board participation (without fees) for Pear Bio, Certis Oncology Solutions, Bryologyx, the College of Experts for the DHSC/UKRI Global Effect on COVID-19 Health Research funding opportunity, and Volvox, all outside of the submitted work. JS is also on the board of directors for Xerion (without fees); and is the co-editor-in-chief of Oncogene (with stipend received from Springer Nature), outside of the submitted work. ACK declares no competing interests.
References
- 1.Kalil AC, Johnson DW, Lisco SJ, Sun J. Early goal-directed therapy for sepsis: a novel solution for discordant survival outcomes in clinical trials. Crit Care Med. 2017;45:607–614. doi: 10.1097/CCM.0000000000002235. [DOI] [PubMed] [Google Scholar]
- 2.Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kalil AC, Syed A, Rupp ME, et al. Is bacteremic sepsis associated with higher mortality in transplant recipients than in nontransplant patients? A matched case-control propensity-adjusted study. Clin Infect Dis. 2015;60:216–222. doi: 10.1093/cid/ciu789. [DOI] [PubMed] [Google Scholar]
- 4.Donnelly JP, Locke JE, MacLennan PA, et al. Inpatient mortality among solid organ transplant recipients hospitalized for sepsis and severe sepsis. Clin Infect Dis. 2016;63:186–194. doi: 10.1093/cid/ciw295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of COVID-19—final report. N Engl J Med. 2020;383:1813–1826. doi: 10.1056/NEJMoa2007764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horby P, Lim WS, Emberson JR, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stebbing J, Krishnan V, de Bono S, et al. Mechanism of baricitinib supports artificial intelligence-predicted testing in COVID-19 patients. EMBO Mol Med. 2020;12 doi: 10.15252/emmm.202012697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smolen JS, Genovese MC, Takeuchi T, et al. Safety profile of baricitinib in patients with active rheumatoid arthritis with over 2 years median time in treatment. J Rheumatol. 2019;46:7–18. doi: 10.3899/jrheum.171361. [DOI] [PubMed] [Google Scholar]
- 9.Marconi VC, Ramanan AV, de Bono S, et al. Efficacy and safety of baricitinib for the treatment of hospitalised adults with COVID-19 (COV-BARRIER): a randomised, double-blind, parallel-group, placebo-controlled phase 3 trial. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(21)00331-3. published online Sept 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.RECOVERY Collaborative Group Tocilizumab in patients admitted to hospital with COVID-19 (RECOVERY): a randomised, controlled, open-label, platform trial. Lancet. 2021;397:1637–1645. doi: 10.1016/S0140-6736(21)00676-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with COVID-19. N Engl J Med. 2021;384:795–807. doi: 10.1056/NEJMoa2031994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kalil AC. Treating COVID-19-off-label drug use, compassionate use, and randomized clinical trials during pandemics. JAMA. 2020;323:1897–1898. doi: 10.1001/jama.2020.4742. [DOI] [PubMed] [Google Scholar]


