Abstract
Alcohol and cannabis co-use is highly prevalent and associated with various negative consequences. The likelihood of same day co-use is high, especially among men, however, underlying mechanisms to their co-use and its sex-dependent nature remain poorly understood. This study aims to elucidate the effects of controlled alcohol administration on the urge to use cannabis and considers sex-dependent effects. A community sample of non-treatment-seeking heavy drinkers (N = 37, 46% female) reporting cannabis use in the past six months completed an alcohol administration paradigm. Participants rated their urge to use cannabis and drink alcohol at baseline and at rising levels of breath alcohol concentration (BrAC). Mixed model analyses examined the effects of BrAC, sex, and their interaction on craving for cannabis. The relationships across urge for cannabis, urge for alcohol, and subjective responses to alcohol were also tested. There was a significant BrAC × Sex interaction on the urge to use cannabis, such that males reported increases in the urge to use cannabis at rising BrACs but females did not. Urge for alcohol significantly predicted urge for cannabis across rising levels of BrAC and this relationship was stronger in males than in females. Lastly, stimulation, but not sedation, during alcohol administration was positively associated with the urge for cannabis. Overall, these results suggest that the pharmacological effects of alcohol on the urge to use cannabis are sex dependent and that the stimulant effects of alcohol are associated with a higher urge for cannabis.
Keywords: alcohol, cannabis, co-use, sex differences, craving
INTRODUCTION
Concurrent use of alcohol and cannabis is highly prevalent (Hasin et al., 2015) and associated with a host of negative consequences, including greater psychiatric comorbidity, increased risk-taking behavior, heavier alcohol use, and poorer mental health treatment outcomes (Brière, Fallu, Descheneaux, & Janosz, 2011; Metrik, Gunn, Jackson, Sokolovsky, & Borsari, 2018; Midanik, Tam, & Weisner, 2007; Staiger, Richardson, Long, Carr, & Marlatt, 2013; Subbaraman, Metrik, Patterson, & Swift, 2017; Volkow, Baler, Compton, & Weiss, 2014). It is estimated that 68% of individuals with a current DSM-5 cannabis use disorder (CUD) diagnosis and over 86% of those with a lifetime CUD diagnosis will also meet diagnostic criteria for lifetime alcohol use disorder (AUD) (Agrawal, Lynskey, Madden, Bucholz, & Heath, 2007; WHO, 2014). Further, it has been shown that individuals who report regularly using alcohol and cannabis frequently consume these two substances at the same time (i.e., in a single episode) (Midanik, et al., 2007; Subbaraman & Kerr, 2015). In fact, a recent study by our group found that drinking alcohol on a given day was associated with a 2.5-fold increase in the likelihood of same-day cannabis use (Roche et al., 2019). Notably, in this study, the observed effect of alcohol on the increased likelihood of same-day cannabis use was greater for men than for women.
Epidemiological studies consistently report that men tend to use cannabis more frequently (SAMHSA, 2014), are at a greater risk for developing a CUD (Stinson, Ruan, Pickering, & Grant, 2006), and seek treatment for CUD at higher rates than women do (SAMHSA, 2014). Despite these findings, it has also been shown that women show a quicker progression from initiation of cannabis use to the development of cannabis-related problems, than men do (i.e., the “telescoping effect”) (Ehlers et al., 2010; Hernandez-Avila, Rounsaville, & Kranzler, 2004; Schepis et al., 2011). Additionally, recent studies found that a growing number of women have reported using cannabis for medicinal purposes, compared to men (Finseth et al., 2015; McConnell, Applegate, Keniston, Kluger, & Maa, 2014; Ryan-Ibarra, Induni, & Ewing, 2015). A recent review by Cooper and Craft examined sex differences in cannabis research at the both preclinical and clinical levels of analyses (Cooper & Craft, 2018) and found that women exhibit higher withdrawal symptoms, while men use cannabis at higher rates. Females have also been found to exhibit higher levels of cue-induced cannabis craving than males (Fattore, 2013) and it has been documented that women with a lifetime diagnosis of CUD are more likely than men to have a comorbid AUD (Calakos, Bhatt, Foster, & Cosgrove, 2017); however, the intersection between cannabis and alcohol remains poorly understood.
In sum, while alcohol and cannabis are often used concurrently, and alcohol may precipitate the use of simultaneous cannabis use, the underlying mechanisms to their co-use and its sex-dependent nature remain poorly understood. An early study by Chait and Perry (1994) provided little evidence that acute alcohol ingestion increases cannabis use overall; however, the authors did find considerable individual differences between subjects in the effects of alcohol on cannabis consumption. In a more recent study by Ballard and de Wit (2011), which examined the separate and combined effects of acute low-dose alcohol and THC ingestion on subjective drug effects, it was found that THC alone did not impact ratings for wanting more of the drug. Instead, THC was found to attenuate the increased ratings observed after alcohol was administered. It is possible that within both of these studies, subjective craving may be a putative mechanism by which alcohol and cannabis are co-used – perhaps synergistically.
To fill this gap in the literature, the present study assessed the effects of controlled alcohol administration on the urge to use cannabis, a factor that is hypothesized to impact subsequent cannabis use and considers sex-dependent effects. Specifically, our aims were to test: (a) the effects of controlled alcohol administration on craving for cannabis, (b) whether alcohol’s effect on cannabis craving is moderated by sex, and (c) explore the association between measures of subjective response to alcohol, namely stimulation and sedation, and the urge to use cannabis during the alcohol administration. Given the finding that drinking alcohol on a given day was associated with a 2.5-fold increase in the likelihood of same-day cannabis use (Roche et al., 2019), especially in men, we hypothesized that alcohol administration would be associated with an increased craving for cannabis across both males and females and that this relationship would be greater in men than in women.
METHOD
Participants
All study procedures were approved by the University of California, Los Angeles Institutional Review Board; the protocol number is 14–000501 and the title is "Modeling alcohol reward and reinforcement in the human laboratory." A community sample of non-treatment-seeking heavy drinkers was recruited via online and print advertisements. Preliminary eligibility screening was conducted through online and telephone surveys followed by an in-person screening/assessment visit. After providing written informed consent and receiving a full explanation of the study procedures, participants were breathalyzed, provided a urine sample for urine toxicology testing, and completed a series of self-report questionnaires and semi-structured interviews on substance use and related individual differences.
All participants were required to: (i) have a breath alcohol concentration (BrAC) of 0.000 g/dl (i.e., 0mg%) at the time of the study visit; (ii) test negative for all drugs (except cannabis) on a urine toxicology screen; (iii) test negative on a urine pregnancy test (if female); (iv) be between the ages of 21 and 45; (v) be current heavy drinkers based on NIAAA recommendations (i.e., ≥ 14 drinks per week for men or ≥ 7 drinks per week for women); (vi) be non-treatment-seeking for AUD; (vii) not be experiencing significant withdrawal from alcohol; and (viii) not meet current (i.e., past 3-month) DSM-5 diagnostic criteria for any substance use disorder other than nicotine or alcohol. Participants were not required to test positive for cannabis on the urine toxicology screen. Current (i.e., past 3-month) DSM-5 CUD was an exclusionary criterion for the current study, whereas lifetime CUD was not. Following the in-person screening visit, a physical examination ensured medical eligibility. For the purposes of the present study, participants who endorsed any cannabis use in the past six months per the Cannabis Use Disorders Identification Test – Revised (CUDIT) (Adamson, 2010 #107) at the time of the initial in-person screening visit were selected for the analyses presented herein.
Alcohol Administration Procedure
The alcohol administration procedure was conducted at the UCLA Clinical and Translational Research Center (CTRC) and comprehensive methodology is discussed elsewhere (Bujarski et al., 2018). Briefly, participants’ height, weight, and vital signs were collected and intravenous (IV) lines were placed by a nurse prior to beginning the alcohol administration procedure. All participants also completed baseline assessment measures prior to alcohol infusion, at a BrAC of 0.00 g/dl.
Alcohol was then administered IV (6% ethanol v/v in saline) using the Computerized Alcohol Infusion System (CAIS) (Plawecki, Han, Doerschuk, Ramchandani, & O'Connor, 2008; Zimmermann et al., 2008; Zimmermann, O’Connor, & Ramchandani, 2011). Throughout the alcohol challenge, participants were administered IV alcohol in amounts designed to reach target BrACs of 0.02, 0.04, and 0.06 g/dl, each over 15 minutes. After reaching each target BrAC, BrAC level was clamped by pausing the alcohol infusion for approximately 5 minutes to allow participants to complete various self-report questionnaires.
Measures
Substance Use Measures.
All of the following measures were completed at the initial in-person screening visit, with the exception of the Timeline Follow-Back (TLFB) (Sobell & Sobell, 1992), which was administered both at the screening visit and at the time of the alcohol infusion. The Structured Clinical Interview for DSM-5 (SCID) (adapted from First, Williams, Karg, & Spitzer, 2015) assessed for current (i.e., past 3-month) AUD and CUD. The Clinical Institute Withdrawal Assessment for Alcohol (CIWA-Ar) (Sullivan, Sykora, Schneiderman, Naranjo, & Sellers, 1989) measured the presence and severity of alcohol withdrawal. The TLFB measured past-month alcohol and cannabis use quantity and frequency. The Alcohol Use Disorders Identification Test (AUDIT) (Allen, Litten, Fertig, & Babor, 1997) and the Alcohol Dependence Scale (ADS) (Skinner & Allen, 1982) assessed alcohol dependence severity. The CUDIT (Adamson et al., 2010) measured problems associated with cannabis use. The Penn Alcohol Craving Scale (PACS) (Flannery, Volpicelli, & Pettinati, 1999) measured tonic levels of alcohol craving. The Biphasic Effects of Alcohol Scale (BAES) (Martin, Earleywine, Musty, Perrine, & Swift, 1993) and the Urge Form (UF) (Ray et al., 2007) were administered during the alcohol administration only. The BAES captures alcohol-induced feelings of stimulation and sedation (i.e., via distinct subscales) at baseline and across rising levels of BrAC. The UF was the primary outcome of the present analyses; it measured “state levels” of craving for cannabis at baseline and across rising BrAC levels. At each BrAC level, participants were asked to rate their urge to use both alcohol and cannabis as responses to the following questions: “How strong is your urge to drink right now?” and “How strong is your urge to smoke marijuana right now?” on a scale from 0 (“no urge at all to drink/smoke”) to 11 (“very strong urge to drink/smoke”).
Anxiety and Depression Measures.
Anxious and depressive symptomatology were assessed during the in-person screening visit using the Beck Anxiety Inventory (BAI) (Beck, Epstein, Brown, & Steer, 1988) and the Beck Depression Inventory – II (BDI-II) (Beck, Steer, & Brown, 1996), respectively.
Data Analysis
Analyses were conducted using a multilevel mixed model in SAS Version 9.4 using PROC MIXED. The analyses examined the effects of BrAC, a four-level within-subjects factor (0.00, 0.02, 0.04, and 0.06 g/dl, coded 1 – 4), and sex (i.e., male vs. female, coded 0 and 1, respectively), and their interaction on craving for cannabis during the alcohol administration. Urge for cannabis was predicted as a function of BrAC, sex, and their interaction, adjusting for craving for alcohol measured at each BrAC level via the UF. Other relevant covariates (i.e., AUDIT, CUDIT, BAI and BDI-II scores) were entered into the models to probe for the robustness of the findings. Multilevel mixed models were also used to examine the relationships across subjective response to alcohol, urge for alcohol, and urge for cannabis during the alcohol administration. These mixed models also account for the effect of BrAC level and for sex differences. In all models, a random intercept approach was used along with an unstructured covariance matrix.
RESULTS
Sample Characteristics
Thirty-seven (45.9% female) non-treatment-seeking heavy drinkers who reported cannabis use in the past six months were included in the present analyses. Sample characteristics are presented in Table 1. This sample consisted of heavy drinkers (i.e., average AUDIT score of 12.90 (SD = 4.91)) with sub-hazardous levels of cannabis use (i.e., average CUDIT score of 4.32 (SD = 2.84)). A series of independent-samples t-tests were performed to examine differences between males and females on aforementioned individual differences and substance use variables. Results indicated no significant group differences on any mood or substance use variable (p’s > 0.07). The only exception to that was the BAI score, in which females, on average, reported higher anxiety symptomatology than males (t(35) = −2.25, p < 0.05).
Table 1.
Sample Characteristics.
| Variablea | Males (n = 20) | Females (n = 17) | Test for Difference |
|---|---|---|---|
|
| |||
| Age | 27.70 (5.86) | 27.06 (4.39) | t(35) = 0.37, p = 0.71 |
| AUDITb | 12.90 (3.88) | 13.12 (6.03) | t(35) = −0.13, p = 0.90 |
| ADSc | 11.55 (4.72) | 9.88 (4.83) | t(35) = 1.06, p = 0.30 |
| PACSd | 8.15 (3.88) | 9.41 (5.40) | t(35) = −0.82, p = 0.42 |
| CUDITe | 4.45 (2.68) | 4.18 (3.09) | t(35) = 0.29, p = 0.77 |
| Cannabis use daysf | 1.70 (1.42) | 3.24 (3.03) | t(21.87) = −1.92, p = 0.07 |
| Drinking daysf | 19.90 (6.22) | 16.06 (5.90) | t(35) = 1.92, p = 0.06 |
| DPDDg, f | 5.44 (1.87) | 4.38 (1.63) | t(35) = 1.81, p = 0.08 |
| Alcohol and cannabis co-use daysf | 1.30 (1.42) | 1.59 (1.62) | t(35) = −0.58, p = 0.57 |
| Tobacco use daysf | 7.95 (12.38) | 4.47 (9.23) | t(35) = 0.95, p = 0.35 |
| BDI-IIh | 6.75 (6.62) | 11.18 (9.74) | t(35) = 1.64, p = 0.11 |
| BAIi | 4.55 (4.30) | 8.29 (5.80) | t(35) = −2.25, p < 0.05* |
Standard deviations appear within parentheses for continuous variables.
Alcohol Use Disorders Identification Test (AUDIT).
Alcohol Dependence Scale (ADS).
Penn Alcohol Craving Scale (PACS).
Cannabis Use Disorders Identification Test – Revised (CUDIT).
Assessed by the Timeline Follow Back (TLFB) interview for the past 30 days.
Drinks per drinking day (DPDD).
Beck Depression Inventory – II (BDI-II).
Beck Anxiety Inventory (BAI).
Single asterisks denote group differences.
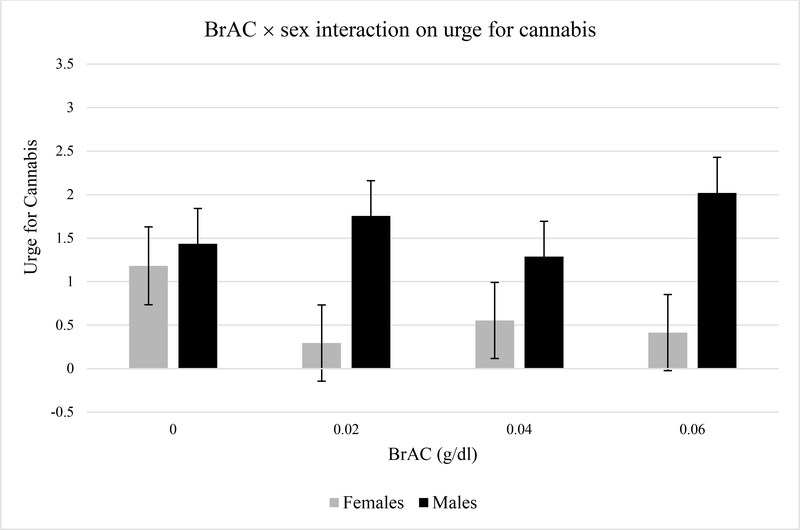
Effects of Alcohol on Urge for Cannabis
Across both males and females there was a non-significant effect of breath alcohol concentration on the urge to use cannabis [F(3,108) = 2.32, p = 0.079]. However, once Sex and BrAC × Sex were entered into the model, there was a significant BrAC × Sex interaction on the urge to use cannabis [F(3,104) = 2.99, p < 0.05], while adjusting for the urge to use alcohol [F(1,104) = 22.92, p < 0.0001]. As shown in Figure 1 and confirmed through simple effects tests, these results suggest that male participants reported increases in the urge to use cannabis across rising BrAC levels [F(3,144) = 3.24, p < 0.05] while female participants did not [F(3,124) = 0.68, p = 0.57]; in fact, they show reductions in their craving for cannabis across rising BrAC levels, although those reductions were not statistically significant. In sum, craving for cannabis across rising BrAC levels is going in different directions for males and females, with males having a significant increase and females having a nonsignificant decrease in craving.
Figure 1.
Predicted values of urge to use cannabis across rising blood alcohol concentration (BrAC) levels by sex, adjusting for urge to drink alcohol.
To further probe these effects, we re-ran the mixed models adjusting for scores on the AUDIT, CUDIT, BAI, and BDI-II (each covariate tested separately), given their putative role as third variables of interest. Results of the BrAC × Sex interaction on the urge for cannabis remained significant in all models. Notably, none of the covariates were statistically significant in these models, with only CUDIT score having a marginal effect on the urge for cannabis [F(1,104) = 3.77, p = 0.055]. The results also remained robust when removing the urge for alcohol variable as a covariate. Together, these findings suggest that males experienced greater increases in the urge to use cannabis across rising BrAC levels than females, and that this sex-dependent effect was not accounted for by differences in alcohol use severity, severity of hazardous cannabis use, depression, or anxiety symptomatology.
Relationship between Urge for Alcohol and Urge for Cannabis
We examined the association between ratings of urge to drink and urge to use cannabis at baseline and at rising levels of BrAC using a multilevel modeling approach, in which alcohol urge ratings predicted cannabis urge ratings. The relationship between the urge for alcohol and the urge for cannabis across levels of BrAC was robust and statistically significant [t(110) = 5.38, p < 0.0001, B = 0.27, SE = 0.05]. There was no significant effect of BrAC [F(3,104) = 0.12, p = 0.95] or BrAC × Urge for Alcohol [F(3,104) = 0.26, p = 0.86] in predicting the urge for cannabis. This suggests that the association between urge for alcohol and urge for cannabis was relatively stable across BrAC levels.
A test of sex effects on the relationship between urge for alcohol and urge for cannabis, found a significant Sex × Urge for Alcohol interaction in predicting the urge for cannabis [t(109) = −2.14, p < 0.05, B = −0.21, SE = 0.10]. When probing for this interaction by testing simple effects in males and females separately, we found a stronger relationship between urge for alcohol and urge for cannabis during the alcohol administration in males [t(59) = 4.85, p < 0.0001, B = 0.34, SE = 0.07], and a smaller, yet statistically significant effect, of urge for alcohol on urge for cannabis in females [t(50) = 2.05, p < 0.05, B = 0.13, SE = 0.06]. As with the models for the effects of alcohol, we probed for these effects by adjusting for scores on the AUDIT, CUDIT, BAI, and BDI-II (each covariate tested separately). The Sex × Urge for Alcohol in predicting the urge for cannabis remained significant in all models. CUDIT score was the only covariate found to have effect on the urge for cannabis [F(1,109) = 4.63, p < 0.05]. These results indicate that the relationship between urge for alcohol and urge for cannabis during alcohol administration was stronger for males than for females, and that this effect was not accounted for by differences in alcohol use severity, cannabis use severity, depression, or anxiety.
Relationship between Subjective Response to Alcohol and Urge for Cannabis
We examined the association between alcohol-induced stimulation (measured by the BAES) and urge to use cannabis at baseline and at rising levels of BrAC using a multilevel modeling approach, in which ratings of stimulation predicted cannabis urge ratings. The relationship between stimulation and the urge for cannabis across levels of BrAC was positive and statistically significant [t(110) = 2.32, p < 0.05, B = 0.03, SE = 0.01]. When BrAC was added to the model, we found a significant effect of BrAC [F(3,104) = 4.03, p < 0.01] and BrAC × Stimulation interaction [F(3,104) = 7.52, p < 0.001] in predicting the urge for cannabis. Probing for this interaction revealed that the association between stimulation and urge for cannabis was not significant at baseline (BrAC = 0.00 g/dl) [t(65) = −0.44, p = 0.66], but became significant at BrAC = 0.02 g/dl [t(65) = 2.71, p < 0.01], and remained significant at BrAC = 0.04 g/dl [t(65) = 2.62, p < 0.05] and BrAC = 0.06 g/dl [t(65) = 2.40, p < 0.05]. In other words, stimulation was positively associated with urge for cannabis once alcohol was administered, but not at baseline. The association between stimulation and urge for cannabis was not moderated by gender [t(109) = −1.74, p = 0.09].
Contrary to the findings for stimulation, the effects for alcohol-induced sedation (measured by the BAES) on urge to use cannabis was generally non-significant. There was no significant relationship between sedation and the urge for cannabis [t(110) = 0.06, p = 0.95] nor a BrAC × Sedation [F(3,104) = 0.11, p = 0.74] effect in predicting the urge for cannabis. The association between sedation and urge for cannabis was not moderated by gender [t(109) = 0.35, p = 0.73].
DISCUSSION
This study examined the pharmacological effects of alcohol on craving for cannabis. Specifically, we predicted that urge to use cannabis would increase with rising levels of BrAC, and given the previous literature implicating sex differences in same day co-use of alcohol and cannabis (Roche et al., 2019), we expected that this relationship would be stronger for males than females. Contrary to our hypothesis, there was not a significant effect of alcohol (i.e., rising BrAC) on cannabis craving (p = 0.079), suggesting that across both males and females, alcohol administration did not significantly modulate participants’ urge to use cannabis. Instead, our results implicated a host of sex-dependent effects on the relationship between alcohol administration and craving for cannabis. Specifically, males reported significantly higher levels of cannabis craving than females at rising BrAC levels. This sex-dependent effect remained robust after considering a host of potential confounds, such as cannabis and alcohol use severity and mood symptomatology. The stronger association between alcohol and cannabis craving in males is consistent with previous work from our laboratory (Roche et al., 2019); in a separate and large sample (N = 551), we found that alcohol use was more strongly related to same-day cannabis use in males than females. Given the literature suggesting that higher levels of alcohol craving is associated with increased likelihood of subsequent alcohol use (McHugh, Fitzmaurice, Griffin, Anton, & Weiss, 2016) and that alcohol use is likely to be met with concurrent cannabis use (Midanik et al., 2007; Subbaraman & Kerr, 2015), craving may be a mechanism through which alcohol use increases the likelihood of simultaneous cannabis use in males, but not females. Additional analyses of the association between alcohol and cannabis craving during alcohol administration suggested that the two are more strongly linked in males, as compared to females, in this study. While it is speculated that in co-users, the use of one substance triggers craving for another (Metrik et al., 2018), this is the first study to provide data on the direct pharmacological effects of alcohol on the urge for cannabis and to explore the interplay between alcohol craving and cannabis craving. The extent to which these effects are sex-dependent add to a growing body of literature in the field of cannabis research suggesting differential behavioral and clinical responses as a function of sex (Cooper & Craft, 2018).
Another interesting finding from this controlled experimental paradigm has to do with the association between the stimulant effects of alcohol and the urge for cannabis in this sample. Interestingly, across males and females, higher levels of alcohol-induced stimulation were associated with a higher urge for cannabis. This effect was not present at baseline (i.e., BrAC = 0.00 g/dl) but reached significance and remained significant when alcohol was on board (i.e., BrACs of 0.02, 0.04, and 0.06 g/dl). This finding suggests that the stimulant effects of alcohol may underlie the association between drinking alcohol and having an increased urge for cannabis. Perhaps the stimulant effects of alcohol may increase the urge for the mostly sedative and anxiolytic effects of cannabis. Drug co-use is often influenced by stimulant/sedative properties of alcohol and drugs of abuse.
These results must be interpreted in light of the study’s strengths and limitations. A strength of the study is that males and females in the sample did not differ on age, mood, or substance use variables, aside from anxiety symptomatology, allowing for an adequate comparison between groups. Another strength of this study includes the use of controlled alcohol administration as a function of BrAC level. While the intravenous mode of alcohol administration lacks ecological relevance, the model results in precise blood alcohol levels and assesses behavioral outcomes as a function of dose. As the current design lacks a matched placebo condition, we were not able to speak to the extent to which the findings are related to rising blood alcohol levels over the course of the session or whether craving increases simply as a function of session duration (i.e., time). A future direction for research might include the comparison between alcohol and placebo (i.e., saline) administration so as to more clearly elucidate the pharmacological effect of alcohol on cannabis craving. Furthermore, additional opportunities for future research includes testing whether the effects of alcohol on urge to use cannabis predicts the decision to use cannabis by assessing the impact of alcohol exposure on cannabis self-administration. In brief, experimental paradigms that manipulate the exposure to both alcohol and cannabis cues and/or administration are needed to fully elucidate these cross-substance effects.
However, the present study has a number of limitations, such as the relatively small sample size, the lack of a placebo-alcohol condition, the limited overlapping co-use in the sample, the focus on smoking cannabis (i.e., instead of other routes of administration), and the overall low subjective craving ratings. Additionally, given that inclusion in the present study was based on report of any cannabis use in the past six months, these analyses were limited by a sample of participants reporting relatively light to modest levels of cannabis use frequency and severity, on average. For instance, only 18.9% of the sample (n = 7) tested positive for THC at the time of the in-person screening visit, indicating a lack of recency of use. Further, 18.9% (n = 7) also denied any cannabis use in the past month. As such, these findings may not be generalizable to heavier cannabis users and additional studies with heavy drinking and heavy cannabis use samples are needed to extend the present findings. Furthermore, the pharmacological effects of alcohol on the urge for cannabis among heavy cannabis users, a population that is at greatest risk for the negative effects of alcohol-cannabis co-use, remains unknown. Lastly, given that the present analyses were limited to BrAC levels that peaked at 0.06 g/dl, future research might consider the examination of participants’ urge to use cannabis at higher levels of BrAC approaching the binge-intoxication cycle.
In conclusion, alcohol administration increased the urge to use cannabis in male but not female heavy drinkers who also report cannabis use. There was a positive relationship between urge for alcohol and urge for cannabis across rising levels of BrAC; however, this relationship was stronger among males. This formative work suggests a possible mechanism by which males in particular report alcohol and cannabis co-use. Given that females reported higher levels of anxiety than males, on average, in this sample, a potential future direction is to examine the role of anxiety in alcohol and cannabis co-use. This line of inquiry might be especially relevant for females given the baseline differences in this sample, as it has been shown that anxiety and stress symptomatology are common precipitants of cannabis consumption (Temple, Driver, & Brown, 2014). Further research on the alcohol and cannabis relationship, its sex-dependent effects, and associated clinical implications is needed, especially as cannabis use becomes increasingly frequent as a result of public policy changes.
Table 2.
Urges for alcohol and cannabis at baseline and across rising BrAC level.
| Variablea | Males (n = 20) | Females (n = 17) | Test for Difference |
|---|---|---|---|
|
| |||
| Urge for alcohol (0.00 g/dl)b | 2.10 (2.00) | 1.18 (2.16) | t(35) = 1.35, p = 0.19 |
| Urge for alcohol (0.02 g/dl)b | 3.35 (2.72) | 2.41 (2.81) | t(35) = 1.03, p = 0.31 |
| Urge for alcohol (0.04 g/dl)b | 3.80 (2.55) | 2.76 (3.01) | t(35) = 1.13, p = 0.27 |
| Urge for alcohol (0.06 g/dl)b | 4.25 (2.67) | 3.29 (2.73) | t(35) = 1.07, p = 0.29 |
| Urge for cannabis (0.00 g/dl)b | 1.10 (1.62) | 0.65 (1.41) | t(35) = 0.90, p = 0.38 |
| Urge for cannabis (0.02 g/dl)b | 1.75 (2.34) | 0.29 (1.21) | t(29.44) = 2.43, p = 0.02* |
| Urge for cannabis (0.04 g/dl)b | 1.40 (2.23) | 0.65 (1.37) | t(32.04) = 1.26, p = 0.22 |
| Urge for cannabis (0.06 g/dl)b | 2.25 (3.01) | 0.65 (1.41) | t(27.90) = 2.13, p = 0.04* |
a Standard deviations appear within parentheses for continuous variables.
Assessed by the Urge Form (UF).
Single asterisks denote group differences.
Public Significance Statement:
Despite their frequent co-use, the underlying mechanisms and sex-dependent nature of alcohol and cannabis co-use remain poorly understood. In a sample of non-treatment-seeking heavy drinkers, males reported an increased urge for cannabis at rising BrACs, whereas females did not. This may imply that the pharmacological effects of alcohol on the urge for cannabis are sex dependent, suggesting a possible mechanism by which males in particular report alcohol and cannabis co-use.
Disclosures and Acknowledgements:
This work was supported by the National Institute on Alcohol Abuse and Alcoholism [R21AA022752 and K24AA025704 to LAR and 3R01AA026190-02S1 to AV], the National Institute on Drug Abuse [5T32DA024635 to LRM], and the Tobacco Related Disease Research Program [T30DT0950 to RG]. None of the authors have any conflicts of interest to disclose.
REFERENCES
- Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, & Sellman JD (2010). An improved brief measure of cannabis misuse: the Cannabis Use Disorders Identification Test-Revised (CUDIT-R). Drug and alcohol dependence, 110(1–2), 137–143. [DOI] [PubMed] [Google Scholar]
- Agrawal A, Lynskey MT, Madden PA, Bucholz KK, & Heath AC (2007). A latent class analysis of illicit drug abuse/dependence: results from the National Epidemiological Survey on Alcohol and Related Conditions. Addiction, 102(1), 94–104. [DOI] [PubMed] [Google Scholar]
- Allen JP, Litten RZ, Fertig JB, & Babor T (1997). A review of research on the Alcohol Use Disorders Identification Test (AUDIT). Alcoholism: clinical and experimental research, 21(4), 613–619. [PubMed] [Google Scholar]
- Ballard ME, & de Wit H (2011). Combined effects of acute, very-low-dose ethanol and delta (9)-tetrahydrocannabinol in healthy human volunteers. Pharmacology Biochemistry and Behavior, 97(4), 627–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, & Steer RA (1988). An inventory for measuring clinical anxiety: psychometric properties. Journal of consulting and clinical psychology, 56(6), 893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck depression inventory-II. San Antonio, 78(2), 490–498. [Google Scholar]
- Blanco C, Hasin DS, Wall MM, Flórez-Salamanca L, Hoertel N, Wang S, … Olfson M (2016). Cannabis use and risk of psychiatric disorders: prospective evidence from a US national longitudinal study. JAMA psychiatry, 73(4), 388–395. [DOI] [PubMed] [Google Scholar]
- Brière F, Fallu J-S, Descheneaux A, & Janosz M (2011). Predictors and consequences of simultaneous alcohol and cannabis use in adolescents. Addictive Behaviors, 36(7), 785–788. [DOI] [PubMed] [Google Scholar]
- Bujarski S, Jentsch JD, Roche DJ, Ramchandani VA, Miotto K, & Ray LA (2018). Differences in the subjective and motivational properties of alcohol across alcohol use severity: application of a novel translational human laboratory paradigm. Neuropsychopharmacology, 43(9), 1891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calakos KC, Bhatt S, Foster DW, & Cosgrove KP (2017). Mechanisms underlying sex differences in cannabis use. Current addiction reports, 4(4), 439–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chait L, & Perry J (1994). Effects of alcohol pretreatment on human marijuana self-administration. Psychopharmacology, 113(3–4), 346–350. [DOI] [PubMed] [Google Scholar]
- Cooper ZD, & Craft RM (2018). Sex-dependent effects of cannabis and cannabinoids: a translational perspective. Neuropsychopharmacology, 43(1), 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers CL, Gizer IR, Vieten C, Gilder DA, Stouffer GM, Lau P, & Wilhelmsen KC (2010). Cannabis dependence in the San Francisco Family Study: age of onset of use, DSM-IV symptoms, withdrawal, and heritability. Addictive behaviors, 35(2), 102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattore L (2013). Considering gender in cannabinoid research: a step towards personalized treatment of marijuana addicts. Drug testing and analysis, 5(1), 57–61. [DOI] [PubMed] [Google Scholar]
- Finseth TA, Hedeman JL, Brown RP, Johnson KI, Binder MS, & Kluger BM (2015). Self-reported efficacy of cannabis and other complementary medicine modalities by Parkinson’s disease patients in Colorado. Evidence-Based Complementary and Alternative Medicine, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M, Williams J, Karg R, & Spitzer R (2015). Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV) Arlington, VA: American Psychiatric Association, 1–94. [Google Scholar]
- Flannery B, Volpicelli J, & Pettinati H (1999). Psychometric properties of the Penn alcohol craving scale. Alcoholism: Clinical and Experimental Research, 23(8), 1289–1295. [PubMed] [Google Scholar]
- Hasin DS, Saha TD, Kerridge BT, Goldstein RB, Chou SP, Zhang H, … Smith SM (2015). Prevalence of marijuana use disorders in the United States between 2001–2002 and 2012–2013. JAMA psychiatry, 72(12), 1235–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayley AC, Stough C, & Downey LA (2017). DSM-5 cannabis use disorder, substance use and DSM-5 specific substance-use disorders: Evaluating comorbidity in a population-based sample. European Neuropsychopharmacology, 27(8), 732–743. [DOI] [PubMed] [Google Scholar]
- Hernandez-Avila CA, Rounsaville BJ, & Kranzler HR (2004). Opioid-, cannabis-and alcohol-dependent women show more rapid progression to substance abuse treatment. Drug and alcohol dependence, 74(3), 265–272. [DOI] [PubMed] [Google Scholar]
- Martin CS, Earleywine M, Musty RE, Perrine M, & Swift RM (1993). Development and validation of the biphasic alcohol effects scale. Alcoholism: Clinical and Experimental Research, 17(1), 140–146. [DOI] [PubMed] [Google Scholar]
- McConnell B, Applegate M, Keniston A, Kluger B, & Maa E (2014). Use of complementary and alternative medicine in an urban county hospital epilepsy clinic. Epilepsy & Behavior, 34, 73–76. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Fitzmaurice GM, Griffin ML, Anton RF, & Weiss RD (2016). Association between a brief alcohol craving measure and drinking in the following week. Addiction, 111(6), 1004–1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Gunn RL, Jackson KM, Sokolovsky AW, & Borsari B (2018). Daily patterns of marijuana and alcohol co-use among individuals with alcohol and cannabis use disorders. Alcoholism: Clinical and Experimental Research, 42(6), 1096–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midanik LT, Tam TW, & Weisner C (2007). Concurrent and simultaneous drug and alcohol use: results of the 2000 National Alcohol Survey. Drug and alcohol dependence, 90(1), 72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton TF, Reid MS, De La Garza R, Mahoney III JJ, Abad A, Condos R, … Anderson A (2008). Evaluation of subjective effects of aripiprazole and methamphetamine in methamphetamine-dependent volunteers. International Journal of Neuropsychopharmacology, 11(8), 1037–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plawecki MH, Han J-J, Doerschuk PC, Ramchandani VA, & O'Connor SJ (2008). Physiologically based pharmacokinetic (PBPK) models for ethanol. IEEE Transactions on Biomedical Engineering, 55(12), 2691–2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray LA, Miranda R, Kahler CW, Leventhal AM, Monti PM, Swift R, & Hutchison KE (2007). Pharmacological effects of naltrexone and intravenous alcohol on craving for cigarettes among light smokers: a pilot study. Psychopharmacology, 193(4), 449–456. [DOI] [PubMed] [Google Scholar]
- Roche D, Bujarski S, Green R, Hartwell E, Leventhal A, & Ray L (2019). Alcohol, tobacco, and marijuana consumption is associated with increased odds of same-day substance co-and tri-use. Drug and alcohol dependence, 200, 40–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan-Ibarra S, Induni M, & Ewing D (2015). Prevalence of medical marijuana use in C alifornia, 2012. Drug and alcohol review, 34(2), 141–146. [DOI] [PubMed] [Google Scholar]
- Schepis TS, Desai RA, Cavallo DA, Smith AE, McFetridge A, Liss TB, … Krishnan-Sarin S (2011). Gender differences in adolescent marijuana use and associated psychosocial characteristics. Journal of addiction medicine, 5(1), 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA, & Allen BA (1982). Alcohol dependence syndrome: measurement and validation. Journal of abnormal psychology, 91(3), 199. [DOI] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1992). Timeline follow-back Measuring alcohol consumption (pp. 41–72): Springer. [Google Scholar]
- Staiger PK, Richardson B, Long CM, Carr V, & Marlatt GA (2013). Overlooked and underestimated? Problematic alcohol use in clients recovering from drug dependence. Addiction, 108(7), 1188–1193. [DOI] [PubMed] [Google Scholar]
- Stinson FS, Ruan WJ, Pickering R, & Grant BF (2006). Cannabis use disorders in the USA: prevalence, correlates and co-morbidity. Psychological medicine, 36(10), 1447–1460. [DOI] [PubMed] [Google Scholar]
- Subbaraman MS, & Kerr WC (2015). Simultaneous versus concurrent use of alcohol and cannabis in the National Alcohol Survey. Alcoholism: Clinical and Experimental Research, 39(5), 872–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbaraman MS, Metrik J, Patterson D, & Swift R (2017). Cannabis use during treatment for alcohol use disorders predicts alcohol treatment outcomes. Addiction, 112(4), 685–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA). (2014). The TEDS report: Gender differences in primary substance of abuse across age groups. [PubMed]
- Abuse, S., & Administration, M. H. S. (2014). National survey on drug use and health.
- Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, & Sellers EM (1989). Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). British journal of addiction, 84(11), 1353–1357. [DOI] [PubMed] [Google Scholar]
- Temple EC, Driver M, & Brown RF (2014). Cannabis use and anxiety: is stress the missing piece of the puzzle? Frontiers in psychiatry, 5, 168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unit, W. H. O. M. o. S. A. (2014). Global status report on alcohol and health, 2014: World Health Organization. [Google Scholar]
- Volkow ND, Baler RD, Compton WM, & Weiss SR (2014). Adverse health effects of marijuana use. New England Journal of Medicine, 370(23), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Platt J, & Goodwin RD (2016). Is cannabis use associated with an increased risk of onset and persistence of alcohol use disorders? A three-year prospective study among adults in the United States. Drug and alcohol dependence, 161, 363–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann US, Mick I, Vitvitskyi V, Plawecki MH, Mann KF, & O’Connor S (2008). Development and pilot validation of computer-assisted self-infusion of ethanol (CASE): a new method to study alcohol self-administration in humans. Alcoholism: Clinical and Experimental Research, 32(7), 1321–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann US, O’Connor S, & Ramchandani VA (2011). Modeling alcohol self-administration in the human laboratory Behavioral neurobiology of alcohol addiction (pp. 315–353): Springer. [DOI] [PubMed] [Google Scholar]