Abstract
BACKGROUND
Moebius syndrome (MBS) is a nonprogressive and rare congenital neuromuscular disorder involving the facial nerve and abductor nerve; it mainly manifests as facial paralysis and eye strabismus paralytic symptoms. Tissues in the oral cavity are also compromised, characterized by microstomia, micrognathia, tongue malformation, cleft lip, high arched palate or cleft palate, bifid uvula, and dental malocclusion. Therefore, dentistry plays a fundamental and crucial role in caring for these individuals. However, there is limited available data on MBS treatment, particularly regarding dental management.
CASE SUMMARY
This case report presents dental treatment of a 21-year-old man with MBS and discusses crucial interactions among oral complications of MBS. In this case, the patient was clinically characterized by congenital neuromuscular disorder, occlusal disorders, and tooth and gum problems. It is noteworthy that the patient presented early eruption of deciduous teeth 2 mo after birth, which has not been reported in other MBS cases and suggests a potentially new clinical manifestation of this syndrome. It is important to note that MBS cannot be cured, and oral manifestations of this syndrome can be managed by a multidisciplinary health care team that helps the patient maintain oral hygiene and dental health. After a series of oral treatments, no obvious poor oral hygiene, swollen gums, or abnormal imaging results were observed after 2 years of follow-up.
CONCLUSION
This case addressed the oral clinical manifestations of MBS and difficulties experienced during dental management, and suggested early tooth eruption as a potentially new clinical manifestation of this syndrome. Knowledge of the loop-mediated association among oral complications of this syndrome is essential to perfecting treatments.
Keywords: Dental treatment, Moebius syndrome, Oral complications, Oral anomalies, Early tooth eruption, Case report
Core Tip: Moebius syndrome (MBS) is a nonprogressive and rare congenital neuromuscular disorder involving the facial nerve and abductor nerve. Tissues in the oral cavity are also compromised. We present herein a series of oral treatments of a 21-year-old man with Moebius syndrome. Notably, the patient presented early eruption of deciduous teeth 2 mo after birth, which has not been reported in other MBS cases, suggesting a potential new clinical manifestation of this syndrome. Orofacial manifestations of MBS are quite complicated. This case report highlights the crucial interactions among oral complications of MBS and provides detailed pictures and specific plans. The most effective approach for MBS dental management is to remove some of the complications by feasible means. The manifestations of this syndrome can be managed by a multidisciplinary health care team that helps the patient maintain oral hygiene and dental health.
INTRODUCTION
Moebius syndrome (MBS), a nonprogressive and rare congenital neuromuscular disorder[1] involving the facial nerve (VIIth cranial nerves) and abductor nerve (VIth cranial nerves), mainly manifests as bilateral or unilateral, complete or partial facial paralysis and eye strabismus paralytic symptoms[2-5]. It affects both males and females equally[6].
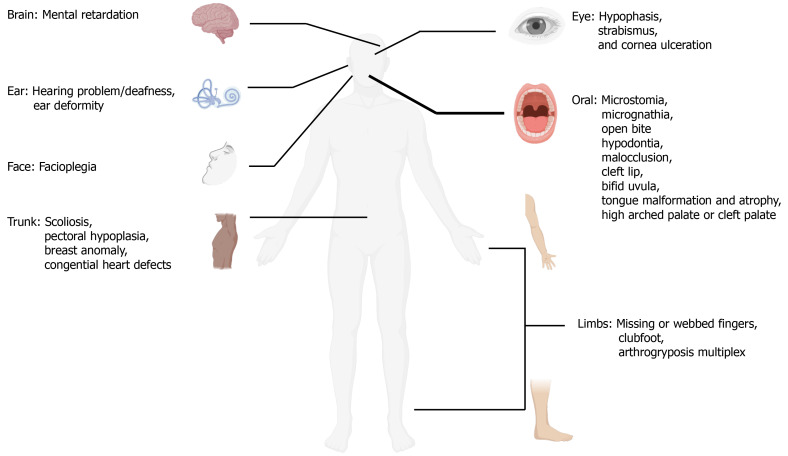
MBS patients may have limb symptoms, such as anomalies in the extremities resulting in clubfoot and missing or webbed fingers[7-9]. Other less common anomalies may include congenital heart defects, arthrogryposis multiplex, pharyngeal and laryngeal paralysis, anosmia, and hypogonadotropic hypogonadism[1,10,11]. In addition, difficulties in hearing, chewing, swallowing, and speech[12,13], as well as moderate mental retardation have also been reported in 10%-15% of patients[14-16].
Tissues in the oral cavity are also compromised, characterized by microstomia, micrognathia, tongue malformation, cleft lip, high arched palate or cleft palate, bifid uvula, and dental malocclusion[17-19]. Regarding dental aspects, MBS patients have more early carious lesions than normal populations, which might be attributed to impaired masticatory function and altered saliva[18,20]. Hypodontia (both deciduous and permanent) and hypoplastic teeth occasionally appear but are rare[21]. These oral complications, which can psychosocially impact the patients’ quality of life, signify the great need for multidisciplinary treatments. It is therefore apparent that dentistry plays a fundamental and crucial role in caring for these individuals. Nevertheless, the lack of muscle elasticity and microstomia makes dental treatment extremely difficult. Publications involving dental treatment in MBS patients are quite few (Figure 1)[8,21-23]. Here, we report a clinical case of Moebius syndrome, address dental management, clarify the association of clinical manifestations, and emphasize the significance of an accurate diagnosis.
Figure 1.
Clinical manifestations of Moebius syndrome. Art adapted from BioRender.
CASE PRESENTATION
Chief complaints
A 21-year-old man native to Shaoxing, Zhejiang Province, together with his mother, visited the Oral Medicine Department of our hospital, seeking comprehensive dental treatment for his severe caries in March 2019 (Figure 2).
Figure 2.
Pretreatment intraoral photographs. A: Right lateral view; B: Left lateral view; C: Frontal view; D: Occlusal view of the maxillary arch; E: Occlusal view of the mandibular arch.
History of present illness
The patient’s symptoms began with severe caries several years prior to visiting the Oral Medicine Department of our hospital.
History of past illness
According to medical records, the patient showed clinical symptoms of clubfoot and expressionless face after birth. Notably, thanks to the detailed original medical records and clear memories of the patient's family members, he presented early eruption of deciduous teeth 2 mo after birth, which has not been reported in other MBS cases and suggests a potential new clinical manifestation of this syndrome. At the age of 4, he underwent surgery on his feet to improve the motor function of his limbs. Between the ages of 5 and 7, he was diagnosed with severe deafness and was advised to wear hearing aids. At the age of 9, the patient was diagnosed with Moebius syndrome by Peking Union Medical College Hospital. In 2010, he visited several hospitals for dental treatment, and according to oral medical records, he had severely swollen gingiva, cervical demineralization, and tongue dysfunction. However, because of his heavy study task and limited time, his mother decided to postpone his dental treatment, except for lingual frenectomy, to relieve his asophia.
Personal and family history
The patient denied related personal and family history except for dystocia.
Physical examination
During the inquiry, our medical staff had to talk to the patient in a loud voice to be heard. Extraoral examination revealed irregular eye function and incomplete mouth closure, absence of facial expression, and limited mouth opening (25 mm) (Figure 3A and B). Intraoral examination presented poor oral hygiene, crowded dentition, swollen and hyperplastic gingiva, dental calculus of degree I, bleeding on probing, and impacted teeth (38, 48), as well as carious teeth (11-13, 21-23, 31-33, 41 neck of labial side and 14, 17, 24, 25, 34, 35, 44, and 45 occlusal surface), carious residual roots (15, 16, 26, 27, 36, 37, 46, and 47), carious residual crowns (17, 42, and 43), and fistula on the labial side of the mandibular right canine tooth (43) (Figure 2). In addition, a soft and thin tongue with deep central sulci and a high arched palate was observed (Figures 2D and 3C).
Figure 3.
Extraoral facial photographs. A: Frontal photograph; B: Limited mouth opening; C: Tongue malformation.
Laboratory examinations
The blood biochemistry and urine analyses were normal.
Imaging examinations
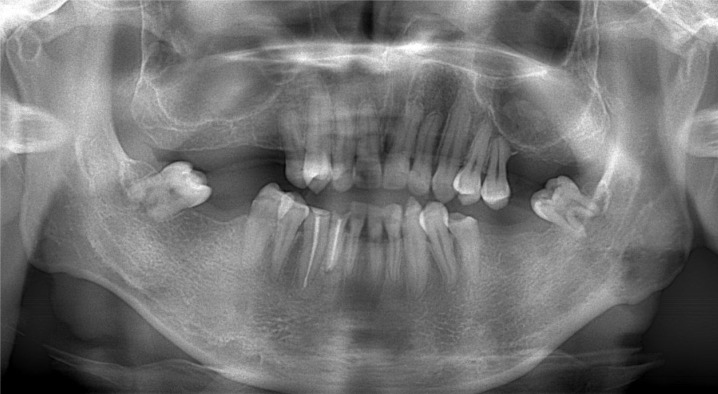
The initial panoramic image showed a low-density shadow in the periapical area of the mandibular right canine tooth (43) (Figure 4).
Figure 4.
Initial panoramic image (2019).
FINAL DIAGNOSIS
The final diagnosis of the presented case was orofacial manifestations of Moebius syndrome.
TREATMENT
In this clinical context, after finishing preoperative examination and obtaining consent, a series of oral treatments were initiated: (1) Ultrasonic supragingival scaling and oral hygiene instructions were carried out to address the patient’s poor oral hygiene and swollen gums; (2) Teeth (15-17, 26, 27, 36, 37, 46, and 47) were extracted under infiltration anesthesia; (3) Two weeks after ultrasonic supragingival scaling, the symptoms of gingival redness and swelling were relieved, and ultrasonic subgingival scaling was subsequently performed; (4) Decayed dentine (teeth 11-14, 21-25, 31-35, 41, 44, and 45) was removed by a high-speed air turbine handpiece and hand instruments (small spoon excavator for caries removal), and the cavity was restored with composite resin (3M ESPE Filtek Z350 XT) (Figure 5); (5) Since decayed tissues of 42 and 43 involved dental pulp, root canal therapy (RCT) was performed; (6) Three weeks after RCT, the fistula on the labial side of the mandibular right canine tooth (43) disappeared, and the patient underwent periapical surgery under infiltration anesthesia; and (7) At the subsequent visit after 1 wk, the patient showed no obvious discomfort and had maintained good oral hygiene (Figure 5).
Figure 5.
Posttreatment intraoral photographs. A: Right lateral view; B: Left lateral view; C: Frontal view; D: Occlusal view of the maxillary arch; E: Occlusal view of the mandibular arch.
Taking into account the patient's condition, such as missing teeth and weak chewing ability, we referred the patient to orthodontists and prosthodontists. However, due to the inadequate intraoral space and the long treatment period, the specialist and the patient failed to come to an agreement.
OUTCOME AND FOLLOW-UP
The patient is currently scheduled for regular follow-up. No obvious poor oral hygiene, swollen gums, or abnormal imaging results were observed after the 2-year follow-up (Figures 6 and 7).
Figure 6.
Two-year follow-up photographs.
Figure 7.
Two-year follow-up panoramic image (2021).
DISCUSSION
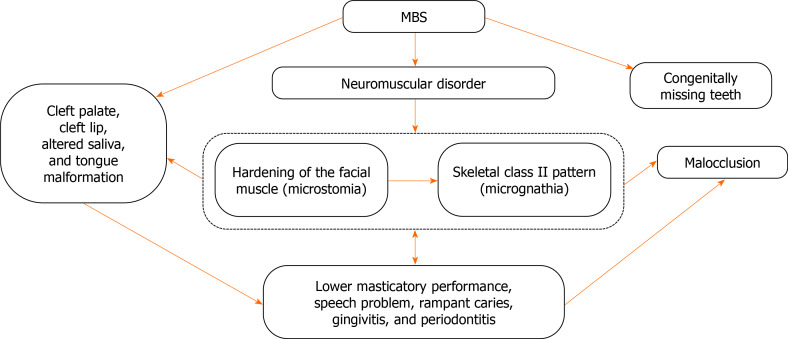
As discussed above, we have described craniofacial abnormalities and dysfunction in a young man with Moebius syndrome. For oral-maxillofacial malformations, prominent symptoms included microstomia, micrognathia, malocclusion, tongue malformation, cleft lip, high arched palate or cleft palate, hypodontia, and bifid uvula[17,18,24]. Although the etiology is not clear, it was proposed that malformations might have been related to neuromuscular deficiency during the embryonic development period[23,25]. Furthermore, there are interactions of MBS symptoms from the etiological perspective. Since muscles can exert secretory stimuli on the skeleton, the lack of muscle contraction caused by facial paralysis could result in disordered palatogenesis and micrognathia[26-28]. In addition, palatal shelf elevation may lead to functional changes in tongue movements, which contribute to the development of micrognathia[29]. Meanwhile, micrognathia could induce cleft palate in turn by impeding tongue development[30,31]. In addition, missing teeth may result in malocclusion, periodontal damage, insufficient alveolar bone growth, reduced chewing ability, inarticulate pronunciation, and other problems[32-34]. As reported in most studies, MBS patients lack of lip seal, which is closely related to the high prevalence of the Class II pattern with micrognathia and excessive maxillary development, attributed to the alteration of the motor and sensitive facial nerves and to the maldevelopment of the brainstem[35-37]. It was observed that the early use of orthopedic appliances was important to prevent malocclusion and glossoptosis[38,39]. Therefore, orthodontic treatment is indispensable in most cases. However, in this case, orthodontic treatment is not anticipated due to the patient’s low motivation.
All the interactions that we discussed above revealed that there is a loop-mediated association among these abnormal manifestations (Figure 8).
Figure 8.
Interactions among oral complications of Moebius syndrome. MBS: Moebius syndrome.
Unlike previous cases, cleft lip/palate, bifid uvula, or hypodontia was not observed in our patient. This patient exhibited rampant caries, gingivitis, and periapical periodontitis and particularly presented unsatisfactory oral hygiene due to dysfunction of the tongue and masticatory muscle. In addition, these individuals exhibit decreased salivary flow, decreased buffering capacity and amylase activity[18,40], and poor swallowing capability. They have to eat a soft diet, which is easily retained in the oral cavity, increasing the risk of caries[10].
Therefore, caries may well be attributed to inadequate saliva flow, inappropriate diet, and poor oral hygiene. Evidence suggests an interactive association between malocclusion and dental caries[41,42]. Moreover, as a potential new clinical manifestation not reported in other MBS cases, this 21-year-old patient was found to have early tooth eruption (ETE) 2 mo after birth, which may add to the etiology of dental caries because ETE could possibly increase cariogenic contact[43].
Orofacial manifestations of MBS are quite complicated. The greatest challenge was to perform dental treatment in such a small space due to limited mouth opening (Figure 3B). The impaired functions of the tongue and masticatory muscle restricted the use of standard handpieces and instruments and prevented an adequate amount of light from entering the oral cavity. It is important to note that MBS cannot be cured, and the most effective method for prevention and treatment is to remove some of the complications by feasible means. Therefore, early diagnosis and dental evaluation are fundamental for MBS patients to reestablish aesthetics, function, and self-esteem. In particular, multidisciplinary cooperation is indispensable to determine an appropriate treatment plan. In this context, dental professionals must obviously carry out periodic controls for the frequent buccodental disorders found in this group of patients during the patients’ entire lifetime.
CONCLUSION
Although patients with MBS cannot be cured, knowing and clarifying the loop-mediated association among oral complications of MBS is essential to perfecting treatments. Early tooth eruption, which may contribute to the etiology of dental caries, is a potentially new clinical manifestation of this syndrome. Multidisciplinary cooperation is indispensable in determining an appropriate therapy plan. Then the manifestations of this syndrome can be managed with correct diagnosis and prompt follow-up.
Footnotes
Informed consent statement: Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest to report.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Peer-review started: May 5, 2021
First decision: June 6, 2021
Article in press: July 5, 2021
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Maglangit SACA, Salimi M S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Li JH
Contributor Information
Ben Chen, Department of Oral Medicine, The Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou 310009, Zhejiang Province, China.
Ling-Xia Li, Department of Generality, Hospital of Stomatology, Zhejiang Chinese Medical University, Hangzhou 310000, Zhejiang Province, China.
Li-Li Zhou, Department of Oral Medicine, The Second Affiliated Hospital, School of Medicine, Zhejiang University, Hangzhou 310009, Zhejiang Province, China. zhoulili2012@zju.edu.cn.
References
- 1.Kuklík M. Poland-Möbius syndrome and disruption spectrum affecting the face and extremities: a review paper and presentation of five cases. Acta Chir Plast. 2000;42:95–103. [PubMed] [Google Scholar]
- 2.Kumar D. Moebius syndrome. J Med Genet. 1990;27:122–126. [PMC free article] [PubMed] [Google Scholar]
- 3.Gaudin RA, Jowett N, Banks CA, Knox CJ, Hadlock TA. Bilateral Facial Paralysis: A 13-Year Experience. Plast Reconstr Surg. 2016;138:879–887. doi: 10.1097/PRS.0000000000002599. [DOI] [PubMed] [Google Scholar]
- 4.Gasteratos K, Azzawi SA, Vlachopoulos N, Lese I, Spyropoulou GA, Grobbelaar AO. Workhorse Free Functional Muscle Transfer Techniques for Smile Reanimation in Children with Congenital Facial Palsy: Case Report and Systematic Review of the Literature. J Plast Reconstr Aesthet Surg. 2021;74:1423–1435. doi: 10.1016/j.bjps.2021.01.007. [DOI] [PubMed] [Google Scholar]
- 5.Domeshek LF, Zuker RM, Borschel GH. Management of Bilateral Facial Palsy. Otolaryngol Clin North Am. 2018;51:1213–1226. doi: 10.1016/j.otc.2018.07.014. [DOI] [PubMed] [Google Scholar]
- 6.Carta A, Favilla S, Calzetti G, Casalini MC, Ferrari PF, Bianchi B, Simonelli MB, Farci R, Gandolfi S, Mora P. The epidemiology of Moebius syndrome in Italy. Orphanet J Rare Dis. 2021;16:162. doi: 10.1186/s13023-021-01808-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.K McClure P, Kilinc E, Oishi S, I Riccio A, A Karol L. Mobius Syndrome: A 35-Year Single Institution Experience. J Pediatr Orthop. 2017;37:e446–e449. doi: 10.1097/BPO.0000000000001009. [DOI] [PubMed] [Google Scholar]
- 8.Picciolini O, Porro M, Cattaneo E, Castelletti S, Masera G, Mosca F, Bedeschi MF. Moebius syndrome: clinical features, diagnosis, management and early intervention. Ital J Pediatr. 2016;42:56. doi: 10.1186/s13052-016-0256-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koehler DM, Goldfarb CA, Snyder-Warwick A, Roberts S, Wall LB. Characterization of Hand Anomalies Associated With Möbius Syndrome. J Hand Surg Am. 2019;44:548–555. doi: 10.1016/j.jhsa.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 10.Ha CY, Messieha ZS. Management of a patient with Möbius syndrome: a case report. Spec Care Dentist. 2003;23:111–116. doi: 10.1111/j.1754-4505.2003.tb01671.x. [DOI] [PubMed] [Google Scholar]
- 11.Ghosh R, Shetty V, Hegde S, Babu GS, Ajila V, Kishore P N, Nair M. Rare features associated with Mobius syndrome: Report of two cases. J Dent Res Dent Clin Dent Prospects. 2017;11:60–65. doi: 10.15171/joddd.2017.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Renault F, Flores-Guevara R, Baudon JJ, Sergent B, Charpillet V, Denoyelle F, Thierry B, Amiel J, Gitiaux C, Vazquez MP. Orofacial motor dysfunction in Moebius syndrome. Dev Med Child Neurol. 2020;62:521–527. doi: 10.1111/dmcn.14379. [DOI] [PubMed] [Google Scholar]
- 13.Bell C, Nevitt S, McKay VH, Fattah AY. Will the real Moebius syndrome please stand up? Am J Med Genet A. 2019;179:257–265. doi: 10.1002/ajmg.a.60683. [DOI] [PubMed] [Google Scholar]
- 14.Briegel W. Neuropsychiatric findings of Möbius sequence -- a review. Clin Genet. 2006;70:91–97. doi: 10.1111/j.1399-0004.2006.00649.x. [DOI] [PubMed] [Google Scholar]
- 15.Sjögreen L, Eklund K, Nilsson A, Persson C. Speech production, intelligibility and oromotor function in seven individuals with Möbius sequence. Int J Speech Lang Pathol. 2015;17:537–544. doi: 10.3109/17549507.2015.1016108. [DOI] [PubMed] [Google Scholar]
- 16.Losito L, Gennaro L, Cacudi M, De Rinaldis M, Trabacca A. Moebius syndrome and hydrosyringomyelia: description of a new association. J Child Neurol. 2013;28:801–804. doi: 10.1177/0883073812450946. [DOI] [PubMed] [Google Scholar]
- 17.Domingos AC, Lopes SL, Almeida SM, Boscolo FN, Whaites EJ. Poland-Moebius syndrome: a case with oral anomalies. Oral Dis. 2004;10:404–407. doi: 10.1111/j.1601-0825.2004.01045.x. [DOI] [PubMed] [Google Scholar]
- 18.Castro T, Ortega AO, Mussi MC, Braga MM, Gallottini M. Caries Experience in Individuals with Moebius Syndrome. Pediatr Dent. 2016;38:68–71. [PubMed] [Google Scholar]
- 19.Pagella P, Jiménez-Rojo L, Mitsiadis TA. Roles of innervation in developing and regenerating orofacial tissues. Cell Mol Life Sci. 2014;71:2241–2251. doi: 10.1007/s00018-013-1549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shashikiran ND, Subba Reddy VV, Patil R. "Moebius syndrome": a case report. J Indian Soc Pedod Prev Dent. 2004;22:96–99. [PubMed] [Google Scholar]
- 21.Strömland K, Sjögreen L, Miller M, Gillberg C, Wentz E, Johansson M, Nylén O, Danielsson A, Jacobsson C, Andersson J, Fernell E. Mobius sequence--a Swedish multidiscipline study. Eur J Paediatr Neurol. 2002;6:35–45. doi: 10.1053/ejpn.2001.0540. [DOI] [PubMed] [Google Scholar]
- 22.Abramson DL, Cohen MM Jr, Mulliken JB. Möbius syndrome: classification and grading system. Plast Reconstr Surg. 1998;102:961–967. doi: 10.1097/00006534-199809040-00004. [DOI] [PubMed] [Google Scholar]
- 23.Lehky T, Joseph R, Toro C, Wu T, Van Ryzin C, Gropman A, Facio FM, Webb BD, Jabs EW, Barry BS, Engle EC, Collins FS, Manoli I Moebius Syndrome Research Consortium. Differentiating Moebius syndrome and other congenital facial weakness disorders with electrodiagnostic studies. Muscle Nerve. 2021;63:516–524. doi: 10.1002/mus.27159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carvalho LRRA, Pinto LSS, de Sousa GP, Correia JPDP, de Moura MS. Oromandibular Limb Hypogenesis Syndrome: Overlap of Moebius and Ankyloglossia Superior With Severe Limb Defects. Cleft Palate Craniofac J. 2021;58:518–524. doi: 10.1177/1055665620954736. [DOI] [PubMed] [Google Scholar]
- 25.Kadakia S, Helman SN, Schwedhelm T, Saman M, Azizzadeh B. Examining the genetics of congenital facial paralysis--a closer look at Moebius syndrome. Oral Maxillofac Surg. 2015;19:109–116. doi: 10.1007/s10006-015-0485-6. [DOI] [PubMed] [Google Scholar]
- 26.Rot I, Kablar B. Role of skeletal muscle in palate development. Histol Histopathol. 2013;28:1–13. doi: 10.14670/HH-28.1. [DOI] [PubMed] [Google Scholar]
- 27.Rot I, Mardesic-Brakus S, Costain WJ, Saraga-Babic M, Kablar B. Role of skeletal muscle in mandible development. Histol Histopathol. 2014;29:1377–1394. doi: 10.14670/HH-29.1377. [DOI] [PubMed] [Google Scholar]
- 28.Ortega Ade O, Marques-Dias MJ, Santos MT, Castro T, Gallottini M. Oral motor assessment in individuals with Moebius syndrome. J Oral Pathol Med. 2014;43:157–161. doi: 10.1111/jop.12107. [DOI] [PubMed] [Google Scholar]
- 29.Kouskoura T, El Fersioui Y, Angelini M, Graf D, Katsaros C, Chiquet M. Dislocated Tongue Muscle Attachment and Cleft Palate Formation. J Dent Res. 2016;95:453–459. doi: 10.1177/0022034515621869. [DOI] [PubMed] [Google Scholar]
- 30.Price KE, Haddad Y, Fakhouri WD. Analysis of the Relationship Between Micrognathia and Cleft Palate: A Systematic Review. Cleft Palate Craniofac J. 2016;53:e34–e44. doi: 10.1597/14-238. [DOI] [PubMed] [Google Scholar]
- 31.Van Lierde KM, Luyten A, Mortier G, Tijskens A, Bettens K, Vermeersch H. Overall intelligibility, articulation, resonance, voice and language in a child with Nager syndrome. Int J Pediatr Otorhinolaryngol. 2011;75:270–276. doi: 10.1016/j.ijporl.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 32.Ali B, Hussain SS. Association between hypodontia and Angles malocclusion. J Pak Med Assoc. 2016;66(Suppl 3):S27–S29. [PubMed] [Google Scholar]
- 33.Rakhshan V. Congenitally missing teeth (hypodontia): A review of the literature concerning the etiology, prevalence, risk factors, patterns and treatment. Dent Res J (Isfahan) 2015;12:1–13. doi: 10.4103/1735-3327.150286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pamplona MDC, Ysunza PA, Telich-Tarriba J, Chávez-Serna E, Villate-Escobar P, Sterling M, Cardenas-Mejia A. Diagnosis and treatment of speech disorders in children with Moebius syndrome. Int J Pediatr Otorhinolaryngol. 2020;138:110316. doi: 10.1016/j.ijporl.2020.110316. [DOI] [PubMed] [Google Scholar]
- 35.Cudziło D, Obłoj B, Obersztyn E, Bocian E, Matthews-Brzozowska T. [Moebius syndrome with facial-dental impairments - rare or rather seldom diagnosed syndrome? Med Wieku Rozwoj. 2012;16:273–279. [PubMed] [Google Scholar]
- 36.Magnifico M, Cassi D, Gandolfini M, Toffoli A, Zecca PA, Di Blasio A. Orthodontics and Moebius syndrome: an observational study. Minerva Stomatol. 2018;67:165–171. doi: 10.23736/S0026-4970.18.04095-5. [DOI] [PubMed] [Google Scholar]
- 37.Sforza C, Grandi G, Pisoni L, Di Blasio C, Gandolfini M, Ferrario VF. Soft tissue facial morphometry in subjects with Moebius syndrome. Eur J Oral Sci. 2009;117:695–703. doi: 10.1111/j.1600-0722.2009.00685.x. [DOI] [PubMed] [Google Scholar]
- 38.Magalhães M, Araújo L, Chiaradia C, Fraige A, Zamunaro M, Mantesso A. Early dental management of patients with Mobius syndrome. Oral Dis. 2006;12:533–536. doi: 10.1111/j.1601-0825.2006.01231.x. [DOI] [PubMed] [Google Scholar]
- 39.Cudzilo D, Matthews-Brzozowska T. Moebius syndrome: The challenge of dental management. Eur J Paediatr Dent. 2019;20:143–146. doi: 10.23804/ejpd.2019.20.02.12. [DOI] [PubMed] [Google Scholar]
- 40.Martins Mussi MC, Moffa E, Castro T, Lira Ortega A, Freitas G, Braga M, Siqueira WL, Cury Gallottini MH. Salivary parameters and oral health in the Moebius syndrome. Spec Care Dentist. 2016;36:265–270. doi: 10.1111/scd.12175. [DOI] [PubMed] [Google Scholar]
- 41.Sá-Pinto AC, Rego TM, Marques LS, Martins CC, Ramos-Jorge ML, Ramos-Jorge J. Association between malocclusion and dental caries in adolescents: a systematic review and meta-analysis. Eur Arch Paediatr Dent. 2018;19:73–82. doi: 10.1007/s40368-018-0333-0. [DOI] [PubMed] [Google Scholar]
- 42.Feldens CA, Dos Santos Dullius AI, Kramer PF, Scapini A, Busato AL, Vargas-Ferreira F. Impact of malocclusion and dentofacial anomalies on the prevalence and severity of dental caries among adolescents. Angle Orthod. 2015;85:1027–1034. doi: 10.2319/100914-722.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Carvalho JC. Caries process on occlusal surfaces: evolving evidence and understanding. Caries Res. 2014;48:339–346. doi: 10.1159/000356307. [DOI] [PubMed] [Google Scholar]