Abstract
Clinical exome sequencing (CES) is an established method for genetic diagnosis and is used widely in clinical practice. Studies of the parental experience of CES, which inform guidelines for best practices for genetic counseling, have been predominately comprised of White, non-Latinx participants. The aim of this study was to explore the parental experiences of CES in a Latinx community and to understand how their experiences are influenced by culture and language. We conducted semi-structured interviews in English and Spanish with 38 Latinx parents of children who had CES. Some of the themes that emerged were common to those previously identified, including a sense of obligation to pursue testing and a mixed emotional response to their child’s results. Parents who had lower education level and/or received care from a provider who did not share their language had more confusion about their child’s CES results and greater dissatisfaction with care compared with parents who had higher education level and/or received care from a provider who spoke their language. We also found evidence of hampered shared-decision making and/or dis-empowered patient decision making regarding CES testing. Our data suggest unique needs for Latinx families having CES, particularly those who are non-English speaking when an interpreter is used. Our data support the value in continuing to take steps to improve culturally competent care by improving interpretation services and recruiting and training a genetic workforce that is ethnically, linguistically and culturally diverse.
Keywords: exome sequencing, underrepresented populations, genetic counseling, genetic services
INTRODUCTION
Clinical exome sequencing (CES) is an established method for genetic diagnosis for certain complex conditions. Compared to other genetic testing methodologies, CES can provide an earlier diagnosis, reduce the cost of testing, and increase the diagnostic yield (Kuperberg et al., 2016; Nolan & Carlson, 2016; Valencia et al., 2015; Vissers et al., 2017). The family experience of having CES is varied and dependent on multiple factors. Parents of children who have multiple health concerns are motivated to pursue CES by the hope for a diagnosis and treatment and the potential to improve their child’s quality of life (Rosell et al., 2016). An array of psychosocial responses have been reported. Parents have reported increased feelings of empowerment upon receiving results but also fears related to the potential of a diagnosis with a shortened lifespan, and frustration when results do not identify a genetic diagnosis (Clift et al., 2015; Rosell et al., 2016; Wynn et al., 2018). With adequate pre-test counseling, parents have been able to accurately understand their results and the limitations of the CES (Rosell et al., 2016; Wynn et al., 2018).
Studies of the parental experience of CES have been largely composed of White, non-Latinx participants. Although the Latinx population represents a rapidly increasing portion of the U.S. population, it is underrepresented and under-served across all genetic research and medicine to date (Kinney, Gammon, Coxworth, Simonsen, & Arce-Laretta, 2010). For example, Latinx women, compared with White, non-Latinx women, are diagnosed with breast cancer at a later stage, are less aware of the availability of genetic risk assessment, and are referred less frequently for genetic testing (Lantz et al., 2006; Sussner, Thompson, Valdimarsdottir, Redd, & Jandorf, 2009). These discrepancies are inversely associated with level of acculturation, the extent to which an individual adopts the values and norms of a mainstream culture (Lantz et al., 2006; Marin, Sabogal, Vanoss Marin, Otero-Sabogal, & Perez-Stable, 1987; Sussner et al., 2009). As acculturation increases, Latinxs report fewer barriers to, more perceived benefits of, and more favorable attitudes toward genetic testing.(Sussner et al., 2009). Latinxs understand genetic testing and believe that it can provide valuable health information and may lead to preventative measures (Hamilton et al. 2016). Within the prenatal setting Latinxs expressed similar views on the potential benefits of prenatal screening as White, non-Latinxs (Floyd, Allyse, & Michie, 2016). Barriers can intrude on Latinx uptake of genetic services and their experiences with these services. For example, language barriers, discrimination, low numeracy, and literacy, lower frequency of health insurance coverage compared with White, non-Latinx U.S. populations, and socioeconomic disadvantages can all negatively influence the implementation of genetics into the healthcare for Latinxs (Kamara, Weil, Youngblom, Guerra, & Joseph, 2018). Spanish speaking Latinxs are more likely to pursue prenatal testing based on recommendation by their provider, less likely to question a recommendation, and more likely to prefer a provider driving decision making approach than individuals who are non-Latinx or English speaking Latinx. (Floyd et al., 2016; Molina, Dehlendorf, Gregorich, & Kuppermann, 2019). Logistical challenges of research studies, including travel to a medical center, additional visits, and study materials only available in English also contribute to low representation of Latinxs in research.
Inclusion of Latinxs and other minorities in genetic research is important to ensure that guidelines and policies developed from these studies equitably benefit the diverse US population. The aim of this study was to explore the parental experiences of CES in a Latinx community and understand how their experiences were influenced by culture and language.
METHODS
We conducted a qualitative study of semi-structured interviews of parents of children who had completed CES. The study was approved by the Columbia University Institutional Review Board.
Participants
Potential participants included parents of children seen in the Division of Clinical Genetics at The Children’s Hospital of New York who met the following eligibility requirements: 1) patient was Latinx, 2) patient was a minor or adult with a medical guardian, 3) patient had CES for any indication except non-syndromic cancer, cardiomyopathy, or cardiac arrhythmia, 4) family had been notified of results, and 5) parent/guardian was able to speak English or Spanish. Potentially eligible patients were identified by filtering the database of patients for those who had (1) undergone CES within the 12 months prior to data collection, (2) familial ethnicity (i.e. proband, parent, and/or grandparent ethnicity) of "Hispanic" or "not given", (3) familial country of origin (i.e. birth country of proband or parent) of Latin American country, (4) and primary language of "English," "Spanish," or "not listed.” For the purpose of this study, Latin American countries were inclusive of Puerto Rico, Dominican Republic, Cuba and all counties in Central America and South America excluding Guyana, Suriname, and French Guiana. Eligibility was confirmed when the parent was invited to the study.
Procedures
All eligible parents identified were sent a bi-lingual invitation letter from their child’s treating geneticist. Invitation letters were followed by up to three invitation phone calls made by bilingual research assistants (RA). On the phone call, eligibility was confirmed, and the parent was invited to the study. If interested, verbal consent was obtained, and the interview was scheduled. Written consent forms in English or Spanish were sent to parents via email link to REDCap (Research Electronic Data Capture) (Harris et al., 2009) or paper through the mail, per parent request. The interview was completed following receipt of the signed consent form.
In-depth, semi-structured, telephone interviews were conducted in English or Spanish per parent choice. Interviews lasted between 30 and 60 minutes and were attended by genetic counseling interns. Parents were emailed or mailed the acculturation survey following their interview. We interviewed parents until we reached saturation of themes. One interviewer was a genetic counselor who was fluent, though not a native, Spanish speaker. For interviews carried out by this genetic counselor, a native Spanish-speaking RA was present on the interview phone calls to provide clarification as needed. Interviews were recorded and transcribed. Spanish interviews were translated into English. Quotes used for interpretation of a parent’s experience and presented in this manuscript were translated back into Spanish by a native Spanish-speaking RA different from the RA who had completed the original translation to ensure reliability of the translation. Parents received a $25 Amazon gift card upon completion of the interview and survey.
Instrumentation
The interview guide was developed by a geneticist, two genetic counselors, native Spanish speaking genetic RAs, and two genetic counseling interns. The interview guide was developed from guides used in previous studies that had gathered data on the CES experiences of parents (Krabbenborg et al., 2016; Rossi et al., 2017; Wynn et al., 2018). The guide included questions targeting previously recognized categories, such as impact of testing, sharing results, emotional reactions to, and understanding of results. The guide also included prompts to capture the Latinx experience with healthcare, including access, language barriers, logistical barriers, and cost. The interview guide was written in English and translated to Spanish. Following the first four interviews, the guide was adjusted to improve flow and remove questions that did not add new content to the interviews. In response to participant explanations during the first several interviews, questions regarding the optimal timing of the test, ability to pay for the test, and participant’s perception of the finality of the CES results were added to the guide (Supplement 1).
The four-question Marin’s Short Acculturation Scale for Hispanics (SASH) was completed by the participants following the interview. The SASH is a validated questionnaire designed to measure the acculturation level of Latinx respondents (Hamilton et al. 2009; Marin et al. 1987). Questions ask about preferred language in different contexts, and responses are on a 5-point Likert scale of “only Spanish” to “only English.” The five questions were averaged to provide a final score of 1 through 5; a score above 2.99 is considered high acculturation (Marin et al., 1987).
Data Analysis
De-identified English language transcripts were coded in NVivo software (QSR International Inc., Burlington, MA, USA). Coding was conducted by three investigators. A grounded theory approach with an inductive coding style was used. First, open line-by-line coding was applied, followed by advanced theory construction. All three coders independently coded three information-dense interviews. Common themes were identified among the three coders during regular meetings with one another and were used to develop a refined codebook. The remaining interviews were coded first by a primary coder (rotated among the three coders), and then this code was reviewed and refined by the other two coders, independently. Discrepancies in coding were resolved by consensus discussions.
The team met at regular intervals during the coding process to discuss emerging themes and refine the codebook. Themes with low rater concordance were adjusted accordingly and arranged into mutually agreed themes and subthemes. After all interviews were coded, the team solidified key themes that arose from the interviews including previously identified issues and issues apparently unique to Latinxs. The final themes included understanding and motivators for CES, comprehension of their child’s CES results, using faith to cope, experiences with cost and ability to pay for testing, and experience of having an interpreter.
We assigned parent understanding of their child’s CES results based on their response to the question about what they understood their child’s results to be, as well as when they spontaneously offered reference to their child’s results or answered a question about the finality of their child’s results. Parent understanding of the results was categorized as one of the following: accurate, accurate plus, accurate minus, or inaccurate. A parent’s understanding of the results was classified as accurate if they recalled their child’s genetic diagnosis (e.g. a pathogenic variant) or the absence of a genetic diagnosis (e.g. no pathogenic variants), accurate plus if they also discussed the correct recurrence risk and/or nuances of a negative result (e.g. the potential that testing was unable correctly identify a genetic diagnosis that was present) and accurate minus if they expressed some misunderstanding of recurrence risk and/or nuances of a negative result. A parent’s understanding of the CES result was assigned inaccurate if they did not recall their child’s test result or recalled the result to be something other than what was reported in the medical record. Parental understanding was assigned independently by two coders and confirmed by two other coders; discrepancies were resolved through discussion.
Descriptive analysis was performed to best capture the participants’ demographics, SASH acculturation scores, and understanding of their child’s CES results.
RESULTS
Demographics
We identified 102 potentially eligible parents. After speaking with them, 11 did not identify as Latinx so they were not eligible for the study. Of the 91 invited, 38 (42%) consented to the study and were interviewed, including a mother of two affected children. Those not interviewed included 20 who could not be reached by phone, 15 who declined to participate (6 Spanish speaking, 9 English speaking) and 17 who initially expressed interest but were not interviewed either because they could not be reached for follow up or did not keep their scheduled interview. Interviews were completed from October 2018 to July 2019.
Of the 38 interviews, 13 were completed in English and 25 in Spanish. Except for one father, each parent was a mother age 24 to 53 years, with an average age of 36 years. Most had a high school education or greater (n=32) and were born outside of the United States (n=30). All parents spoke at least some Spanish and 22 spoke only Spanish. The average acculturation score was 2.24 (n=35) with a range of 1.00 to 4.25 (Cronbach alpha 0.92). Three parents who completed the interview in Spanish did not complete the acculturation survey. Parents who completed the interview in Spanish had lower acculturation scores (n=22; mean 1.46; range 1.00-2.25) than those who completed the interview in English (n=13; mean 3.52; range 2.25-4.25) (Table 1 and Supplement 2).
Table 1.
Characteristics of the parents interviewed
| n | % | |
|---|---|---|
| Female | 37 | 97 |
| Age mean and range* | 36* | 24-53* |
| Highest education level | ||
| Less than high school | 6 | 16 |
| High school degree | 17 | 45 |
| Greater than high school | 15 | 39 |
| Not born in the United States | 30 | 79 |
| Work status | ||
| Employed (full and part time) | 21 | 57 |
| Married | 25 | 66 |
| Acculturation SASH score mean and range** | 2.24** | 1.00-4.25** |
| Low acculturation (SASH score <2.99) | 22 | 67 |
| High acculturation score | 11 | 33 |
| Languages spoken | ||
| Only Spanish | 22 | 58 |
| English and Spanish | 16 | 42 |
| Genetics appointment language | ||
| English (P-P concordant) (2 interview Span., P-P discordant) | 13 | 34 |
| Spanish (P-P concordant) | 2 | 5 |
| English with GC and Spanish with MD (P-P concordant) | 2 | 5 |
| Interpreter (P-P discordant) | 23 | 61 |
| Language of the interview | ||
| English | 13 | 34 |
| Spanish | 25 | 66 |
Abbreviations: Short Acculturation Scale for Hispanics (SASH), genetic counselor (GC), medical geneticist doctor (MD), parent-provider language concordance (P-P concordance)
The mean age (in years) is represented in the n column, and the age range (in years) is represented in the % column.
The mean SASH score of 33 parents interviewed is represented in the n column, and the SASH score range of the 33 parents is represented in the % column.
The families were seen in the clinical genetics department by one of seven genetic counselors (GCs), one of whom was native Spanish speaking, and one of five geneticists (MDs), two of whom were either native or non-native, fluent Spanish speaking. The clinical session was conducted in English for 13 parents including two of whom completed the study interview in Spanish. For two parents, both the MD and GC spoke Spanish, and the session was conducted in Spanish. Two parents spoke with the GC in English and the MD in Spanish (they both completed the interview in English). Twenty-one parents had an interpreter for some or all of the session, including 6 who had a phone interpreter for the full session, 12 who had a phone interpreter for part of the session, and three where the GC provided interpretation. We classified the parents as language concordant when they spoke English with their provider and English in the study interview or when they spoke Spanish with their providers (without an interpreter) and Spanish in the study interview (n=15). Otherwise, parents were classified as language discordant (n=23).
The most common clinical indications for CES included developmental delay (n=15), autism (n=11), and seizures (n=3). Children ranged in age from 1.5 to 20 years at the time their parent was interviewed and over half were male (n=24). Almost all (n=35) were insured through Medicaid or Medicare. Many children had CES ordered concurrently with other genetic testing as part of their initial genetic evaluation (n=7) or as reflex testing after their initial genetic evaluation was non diagnostic (n=13). The remaining (n=18) had more than one clinical visit and genetic test before CES was ordered (Table 2). One child had CES ordered by her neurologist but was referred to genetics after testing was completed, and results were disclosed by the genetic providers. The time from when parents received results to when the parent was interviewed ranged from 6 to 23 months with an average of 13 months. Eighteen children had results which did not identify any variants, 10 had variants of uncertain significance (VUS) and 10 had pathogenic variants that confirmed or identified a genetic diagnosis. Of the pathogenic results, four were de novo, two were X-linked and maternally inherited, two were autosomal recessive with bi-parental inheritance, and two were autosomal dominant and the mothers were negative but fathers were not tested (Table 2 and Supplement 2).
Table 2.
Characteristics of children of parents interviewed
| n | % | |
|---|---|---|
| Male | 24 | 63 |
| Age mean and range* | 7* | (2-18)* |
| Insurance | ||
| Medicaid or Medicare | 35 | 92 |
| Private insurance | 3 | 8 |
| Diagnosis | ||
| Childhood autism | 13 | 34 |
| Developmental delay | 12 | 32 |
| Seizure(s) | 2 | 5 |
| Congenital malformation(s) | 4 | 11 |
| Other(s) | 7 | 18 |
| CES Test Results | ||
| No variant identified | 18 | 47 |
| Pathogenic variant | 13 | 34 |
| VUS | 7 | 18 |
Abbreviations: Clinical exome sequencing (CES), Variant of uncertain significance (VUS)
The mean age (in years) is represented in the n column, and the age range (in years) is represented in the % column.
Interviews
When an interview was conducted in Spanish, the English translated quote is shown as well as the Spanish quote shown in brackets. The participant identification number (ID), SASH acculturation score, and child’s CES results are shown in parentheses.
Understanding and motivation to have CES
In general, parents were able to recall that their child had a genetic test but were only able to provide a limited description and often could not recall the term “exome sequencing.” Most parents did not distinguish CES from other genetic tests their child had concurrently or in an earlier evaluation, though some recalled a discussion of the comprehensive nature of the testing or the occurrence of parental sample collection. Though often unable to provide a detailed description of CES, most parents reported sentiments of impartiality with the information provided to them. For example, one parent explained:
Well eh, they drew his blood, and they did some tests with the blood, but right now I do not remember what the tests were. However, what they told me was that it was a genetic test to see if the child has a problem with his head or something like that, with his development.[Bueno eh, le sacaron sangre y le hicieron unas pruebas de sangre, pero ahora mismo yo no recuerdo no cuales fueron las pruebas. Pero me dijeron que era un examen genético para ver si el niño tenía algún problema como de la cabeza o algo así, con el desarrollo.](ID1571, SASH 1.25, negative result)
Families expressed an obligation to pursue testing, often regardless of potential treatment options. For example one mother stated, “I needed to know what was going on with my daughter” (ID1526, SASH 3.75, no variants). However, many parents communicated hope that CES would provide a diagnosis for which there was a treatment or cure for their child’s condition, as reflected by one participant who said, “I wanted to do the testing because I wanted to see if there was a possibility to find a remedy” ["Bueno yo quiera hacer la prueba porque yo quiera a ver si había alguna posibilidad de buscar algún remedio"] (ID1590, SASH 1.38, pathogenic variant). Several also feared the potential of learning of a poor prognosis if a diagnosis was identified. Some parents (n=15), particularly those with low acculturation scores (n=11), did not share their own motivation for testing but rather reported they had the testing because it was what the doctor said to do:
That was the decision made by the doctors. I could not make that choice. I didn’t even know what the test was for. [Eso fue la decisión que tomado los médicos. Yo no podía tomarla. Y ni si sabía para que era la prueba.] (ID1588, SASH 1.25, VUS, suspected pathogenic)
One mother pursued the test because she incorrectly thought it was what she needed to do before her son could get treatment (prosthetic teeth for anodontia).
Many parents (n=24) referenced the concept of inheritance when talking about what the test might tell them. Some expressed a desire to know from which side of the family the condition came (n=9), one parent reporting “I wanted to know what was going on -- like, did she get it from me? Did she get it from her dad? Or is this something that happened on her own?” (ID1539, SASH 3.88, pathogenic variant). Others referenced inheritance in the context of how results might inform them of recurrence risk (n=6) sometimes explicitly expressing feelings of guilt or blame:
I wanted to know if was something like that, about the genetics, because that way at least more or less, you know … I would not attempt to have another child if my child is going to go through the same thing. [Entonces es que yo quería saber si era algo si era algo así sobre la genética, porque así pues ya una más o menos sabe … no me atreveré tener otro hijo si mi hijo va a pasar lo mismo.] (ID1574, SASH 1.75, no variants)
Most parents remembered being told that the results would take several months to complete and also expressed the anxiety of this time lag and frequently (n=14) considered it to be the most difficult part of the entire CES process. One participant described waiting for results: “We waited a while, a long time, because I was desperate to know. To me, it was like a long time” (ID1509, SASH 3.25, pathogenic variant).
Of the 26 parents who were asked about the optimal time to do the test, 14 indicated a desire to have it done sooner, though two would have preferred to wait until their child was older. The preferred timing of CES was described by one mother:
It was good when the test performed because I had many questions. I would have liked to have done it at 1-year-old or before, when he was appearing of all these things. I was filled with questions. Even though the doctors answered my questions, I would still be filled with more questions. The study alleviated all of those questions. [Estuvo bien cuando se le hizo porque cómo le digo estaba llena de preguntas. Estuvo bien. Me hubiera gustado al año o antes ya que el niño parecía de tantas cosas. Yo estaba llena de preguntas. Aunque me contestaba mucho los doctores, pero igualmente so seguía llega de preguntas. El estudio ayudo que se alivian todas esas preguntas.] (ID1562, SASH 1.25, pathogenic variant)
Overall, most parents (n=32) were able to accurately recall their child’s CES results (Supplement 2). Nine parents communicated a deeper understanding of their child’s genetic test result, such as conveying that a negative result does not eliminate a genetic diagnosis or recalling relevant inheritance patterns. For example, a parent with understanding classified as accurate + explained, “In the future, he can have a test done again maybe in 20 years, 30 years, and they say, oh, well now we know something about this that we didn’t know back then” (ID1533, SASH 3.63, no variants). Another parent whose understanding of results was classified as accurate + described the inheritance pattern of the familial condition:
…[they] discovered that it was me, I was the one that has the gene in my blood. I passed it on to my child and that is why she has that genetic condition. [descubrieron que soy yo, la que tiene ese gen en mi sangre. Yo se lo pase a la niña y por eso salió con esa condición genética.] (ID1585, SASH 1.13, pathogenic variant)
However, for some, understanding of CES results was incomplete (n=10). Sometimes participants provided only vague descriptions of their child’s. One parent with inaccurate classification of understanding stated:
My husband and I have some -- some cells -- I don’t know that did not combine with mine. More or less. [Mi esposo y yo teníamos cómo un -- unas células -- no sé que no combinaba con la mía. Más o menos] (ID1590, SASH 1.38, pathogenic variant de novo)
Often, parents of children with no variants reported through CES did not communicate an understanding of residual risk for a genetic condition in their children. Also, parents suggested lack of understanding of recurrence risks regardless of their child's test results, indicating they were unaware of their chances to have another child with the same health condition. One parent did not recall learning about their child’s results and five had an inaccurate understanding of their child’s pathogenic results (n=2) or VUS (n=3).
Frequency of inaccurate result interpretation was higher in parents who had provider language discordance (Figure 1), low acculturation scores (Figure 2) and less than a HS education (Figure 3). No pattern was present for these variables when looking at frequency of accurate parent interpretations of their child’s results.
Figure 1:
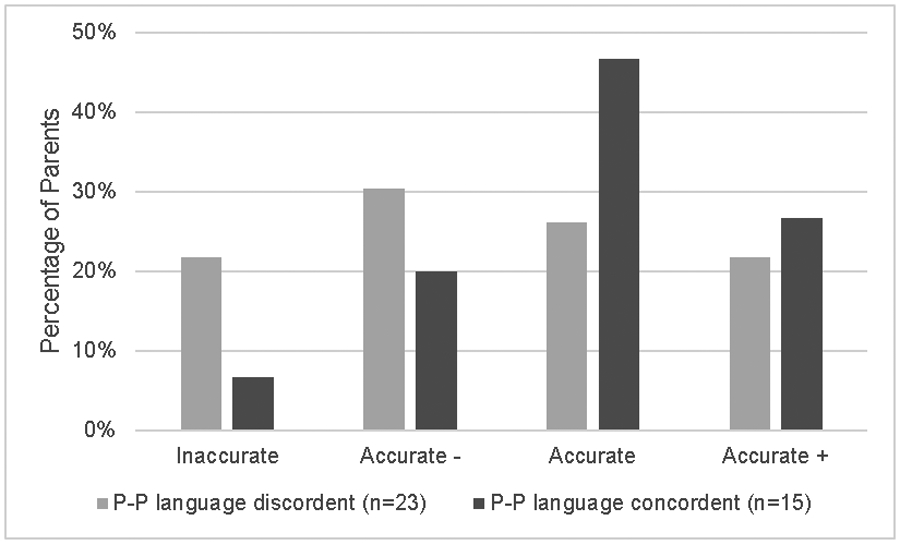
Parental interpretation of results according to parent-provider (P-P) language
Figure 2:
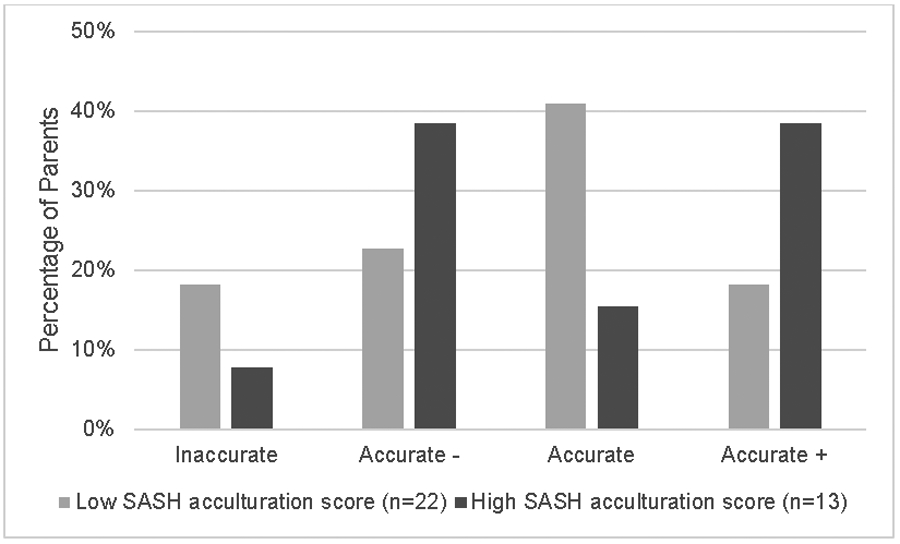
Parental interpretation of results according to SASH acculturation scores.
Abbreviations: Marin’s Short Acculturation Scale for Hispanics (SASH)
Figure 3:
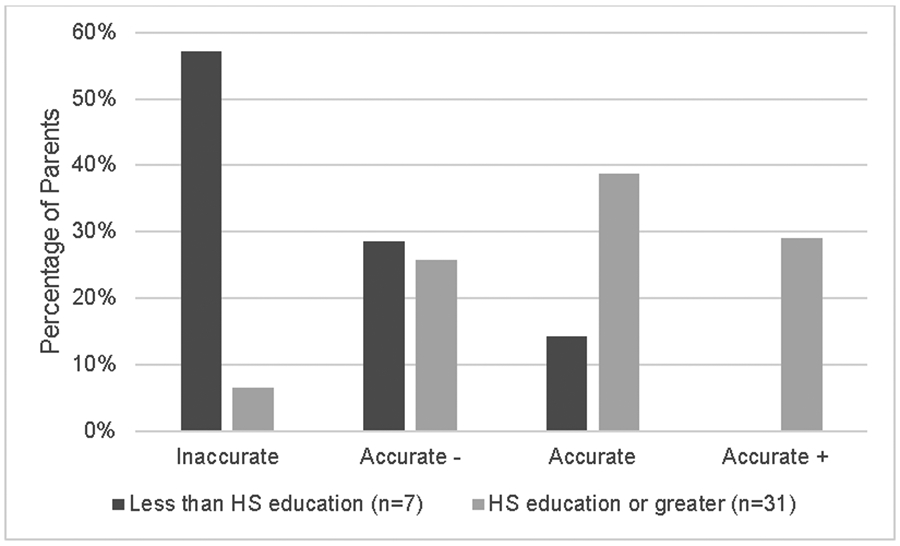
Parental interpretation of results according to parental education.
Abbreviations: high school (HS)
Reaction to and coping with results
Parents reported mixed reactions to learning their child’s CES result. Parents whose child had an identified pathogenic variant often expressed feelings of shock or sadness. One parent vividly described:
And obviously, that day I was devastated; I couldn’t ask -- once they told me about the syndrome, from there, I couldn’t hear; I couldn’t speak; I couldn’t do anything else, because obviously, I was done, you know? We knew what actually was going on, and now we need to do something about it, but my brain, my mind, my feelings were not there. (ID1509, SASH 3.25, pathogenic variant)
Another parent whose child had a pathogenic result expressed disappointment:
I just wish that there was more -- a more concrete definition of the diagnosis. Because I feel like -- and you know, obviously, it’s just because it’s highly uncommon, so I -- you know, I highly -- I completely understand it, but it’s just, it’s very -- like, it’s very broad type of diagnosis where -- you know, like I said, it’s kind of, you don’t know what’s going to happen, and you’re kind of out there, and you don’t know, oh, well if this is this. (ID1549, SASH 3.88, pathogenic result)
Other emotions included hope that the CES result would provide guidance about prognosis and potential treatment.
Parents whose children had no variants identified or whose children had VUS results expressed feelings of confusion and disappointment that the diagnosis remained unknown for their child. Yet others reported feeling hopeful that their child’s condition was not genetic:
I felt very good and with more hope because--, additionally, you know, my son was diagnosed when he was young so knowing that he didn’t have anything genetic, from either side gave me more hope that the autism diagnosis was an error, maybe he’s just delayed. [Yo me sentí muy bien y con más esperanza porque--, incluso, tu sabe, mi hijo fue diagnosticado cuando era pequeño entonces el saber que él no tenía nada genético, nada de ningún lado, me dio más esperanza que el diagnostico de autismo si fue un error, que tuviera un retraso en vez.] (ID1559, SASH 2.00, no variants)
To cope, some parents searched for additional information online, through other providers, or through support groups. Additionally, all parents reported sharing their child’s results with someone such as their family members, friends, or their child’s other healthcare providers. Motivations behind sharing were both to inform these people of their child’s testing but also to receive support and guidance. One participant said, “[I told] just, my closest friends and family, especially the people I know I can count on.” (ID1504, SASH 3.71, no variants). Some parents reported having specific people with whom they chose not to share as they did not think they would be supportive, or they did not feel it was information they needed. By not sharing with those individuals, parents chose to protect their child’s privacy. A parent described:
[We talked] maybe with the doctors, but nothing, nobody outside the family because you know, they’re like, some people do not believe he has autism, and just him, us raising him in the wrong way. So, they don’t fully understand it. … That’s why we keep some things to ourselves. (ID1534, SASH 3.25, pathogenic variant)
Some parents (n=6), all with low acculturation scores, expressed the importance of their faith when coping with their child’s diagnosis or test results. One participant said:
Again, I tell you, God over all things because God knows why he gave him to me like this. … They said that God is the only one that knows. [Pero vuelvo y le digo, Dios sobre todas las cosas y Dios sabe por qué me lo dio a mi así. … Dijeron que Dios es el único que sabe.] (ID1554, SASH 1.00, VUS)
Another parent similarly described the role of faith:
There’s no reason to be prepared for the worst because nothing worse will come out. God gave us this blessing and we need to take advantage. [No hay que está preparado para lo peor porque no va salir nada peor. Dios nos dio esta bendición y hay que aprovechar.] (ID1567, SASH 1.13, VUS, likely pathogenic)
Cost and logistical barriers to care
While few parents (n=2) reported having an out-of-pocket cost for the test, potential cost was a factor in the decision to have their child tested through CES. Some (n=10) indicated that any out of pocket cost or a cost above a certain level would prevent them from pursuing testing. A parent conveyed this sentiment:
Well, if it costs too much, that I wouldn’t be able to pay for it, I wouldn’t have done it because my husband and I don’t have the funds. [Bueno si el costo era muy alto, que yo no podría pagarlo, no se la había hecho, no, porque no tenemos fondos mi esposo y yo.] (ID1590, SASH 1.38, pathogenic variant)
One mother expressed frustration and confusion about being told by her GC to ignore the multiple mailings titled 'Explanation of Benefits' from her health insurance company that indicated that she might have a large out-of pocket-cost, though she ultimately did not have any out-of-pocket cost. Several other parents stated the cost of recommended therapies or interventions prevented them from pursuing the presented options.
Other parents stated that they would be able to find the means to cover an out-of-pocket cost had there been one (n=4). The over-arching desire to know what was afflicting her child is expressed by a parent:
It does not matter to me the amount of money for a test if it is something that will help understand what he has. [Ósea, no me importaría el monto de una prueba si eso va ayudar a entender lo que él tiene.] (ID1598, SASH 1.63, pathogenic variant)
Aside from costs or perception of possible costs, some parents also reported challenges related to having access to transportation to get to medical visits, childcare for other children, ability to take time off work, or other logistical barriers that took precedence over pursuing CES for their child.
Language and impact of interpreters
Parents had mixed reactions about having the assistance of an interpreter. A total of eight parents (two of the six who had an interpreter for the full session and six of the 15 who had an interpreter for part of the session) expressed some frustration. Parents felt that they could not always understand the phone interpreter or that information was lost in translation. Some also felt they received a different level of care and it slowed things down. Other parents could not recall whether they used an interpreter. Another parent expressed that she preferred a phone interpreter, rather than an in-person interpreter, because it was more private. Some parents also recalled providers speaking to them in English and feeling like they did not fully understood the information provided. The clarity, or lack thereof, that parents had is demonstrated by one parent:
Because I don’t speak much English, but yes … I understood everything the doctor would tell me, but I would like if they spoke to me in Spanish, in my language so that it would have been clearer what she was telling me. [Porque ya yo no hablo mucho inglés, pero si … yo entendía todo lo que la doctora me decía, pero me gusta que me hablen en español, en mi idioma para que me quede más clara lo que me está diciendo.] (ID1500, SASH 2.13, no variants)
Conversely, some parents who were fluent in English expressed a preference to speak with providers in English as they may not know the Spanish words for certain medical terms or because they were concerned speaking Spanish may mean that their records were in Spanish and that would complicate communication across providers. One parent described her language preference:
Sometimes the doctor has to go and take time translating information, and I told them that I don’t want this to happen if I have an emergency, because this is a time that I don’t want to waste, somebody translating anything. So, every time they see my face, they see that I’m Spanish, they give me papers and things in Spanish; I say, please give me this in English. (ID1523, SASH 3.25, no variants)
Impact of acculturation on healthcare experiences
Parents whose child's CES experience was facilitated by a provider speaking a discordant language and/or those with low acculturation scores more frequently reported dissatisfaction with the experience (n=13) when compared with parents who had provider language concordance and/or high acculturation scores (n=4). Much of the dissatisfaction was related to not having a provider who spoke Spanish and the feeling that, because of language discordance, care was different for their child. For example, one parent describes frustration felt in the waiting room:
People that speak English -- they don’t have to wait so long because they know English and the people who don't speak English, they need to find a translator and wait more time. That’s what I think. [Si hablaran inglés, gente que hablen inglés -- este no lo hacen esperar tanto porque saben inglés y las persona que no hablan inglés hay que buscarle un traductor y esperar más tiempo. Yo pienso así] (ID1582, SASH 1.00, no variants)
For some, receiving the results report and/or results letter in English was not ideal, as explained be one participant:
Everything was fine because he gave me the information that I needed at the time. The only thing that I tell you is that it [results report] came in English and that is that part I wanted to tell you about. [Quedo todo bien porque él me dio la información que necesitaba en ese tiempo. Lo único que te digo es que vino en inglés y la parte que quiera decir, por eso.] (ID1588, SASH 1.25, VUS)
Besides language discordance, other descriptions of dissatisfaction, regardless of participant acculturation score, included feeling overwhelmed by the information or frustration by lack of a clear diagnosis, prognosis, or treatment. Parents expressed frustration with lack of help regarding follow up care or understanding what the next steps were and finding additional resources. A quarter (4/16) who looked for additional in information in Spanish, expressed that they had difficulty finding information. Parents' lack of time, the scarcity of Spanish resources, and the demands of caring for a child with medical needs were the most commonly reported reasons preventing parents from looking for more resources or identifying a support group. One parent conveyed:
There is very little information in Spanish. Up until now, I still have very little information in Spanish, so I would like to know how the symptoms are or what happens next or how do treatments work and almost all of that isn’t in Spanish. There is very little.[Si, hay muy poca información en español. Hasta la vez tengo muy poca información en español, entonces yo quiera saber cómo son los síntomas o que viene después o cómo actúan los tratamientos y casi eso no hay en español. Muy poquito lo que hay.] (ID1556, SASH 1.63, pathogenic variant)
Another parent similarly expressed desire for more resources suitable for her family: “Well finding me a place where I can do his therapy and continue with his medicines, that they used to attend to him, and that they can understand me well because I want what is best for him.” (ID1500, SASH 2.13, no variants)
When asked directly whether their Latinx culture influenced CES experiences, most parents suggested their culture did not influence the experience. Many felt that other Latinx people might be more impacted by cultural beliefs or educational level and have a different experience, but this did not apply to them. One participant expressed this point:
Yeah, maybe. Like, it depends -- it depends on the person you are. So for instance, like, some -- some people, they do, you know, go straight for what their background tells them more or their culture -- their parents, their ancestors. So maybe, yeah. But for me, it’s not the case. (ID1539, SASH 3.88, pathogenic variant)
Many shared that other Latinxs might not pursue a genetic evaluation because of fear of misunderstanding the information, lack of education, beliefs that their child's problems are behavioral rather than medical, or beliefs in alternative treatments to cure their child. One participant expressed this point citing the heterogeneity of Latinxs and how acculturation or absence of acculturation could impact experiences:
We [Latinx people] don’t all think the same way .… It took me many years to accept that my son had a problem, to accept everything. [todos no pensamos de la misma manera … Me costó muchos años el aceptar que mi hijo tenía un problema, de aceptar todo.] (ID1567, SASH 1.13, VUS)
DISCUSSION
We present a study of semi-structured interviews of the experience of Latinx mothers and one father of children who had CES at a single institution. Throughout the interviews we found that families expressed experiences and feelings similar to those previously reported in the literature. However, there were several themes unique to this study related to degree of acculturation and parent-provider language concordance. In particular, parental understanding of their child’s CES results and overall satisfaction was lower among parents who had less than a high school education or did not have a provider who shared their language. Much of the dissatisfaction was related to language discordance. Also, parents with low acculturation scores more frequently reported provider-directed decisions and using faith to cope with the experience.
Some parents, particularly those with low acculturation scores who were also usually Spanish speaking, reported having CES for their child because it was recommended by their physician, indicating a provider-driven rather than shared-decision making process. This is a pattern documented in the literature. An examination of cancer genetic counseling sessions conducted in Spanish via phone interpreters found absence of patient participation in the decision making (Kamara et al., 2018). Studies in the prenatal and breast cancer settings found Spanish speaking Latinxs to more frequently prefer provider-driven decision making compared to both English speaking Latinxs and other non-Latinx individuals (López et al., 2014; Molina et al., 2019). Furthermore, studies of non-genetic medical decisions suggest that Latinxs are more frequently comfortable with a provider-driven approach than White, non-Latinx individuals, and may see non-directiveness as indication that a procedure or testing is not important (Browner, Preloran, Casado, Bass, & Walker, 2003; Kamara et al., 2018; Vadaparampil, McIntyre, & Quinn, 2010) and prefer a healthcare provider to make a medical decision (Katz et al., 2011; Riffin, Pillemer, Reid, & Löckenhoff, 2016).
The model of shared-decision making, in which patient and physician explore the available evidence and consider options together to help the patient achieve the best decision, is central to informed consent for genetic testing (Elwyn, Gray, & Clarke, 2000). While not all patients may be familiar with this model or initially comfortable with it, we believe genetic service providers should still strive to guide patients to take an active role in decision making. Providers should implement methods to increase patient participation including encouraging participants to share their beliefs, goals and values, help them to identify the information they need to participate in medical decisions, and provide this in accessible manners that take into account patients’ learning styles, literacy levels, cultures, and other factors that influence how they receive new information. Additionally, effort should be made to resolve potential uncertainties and to minimize decisional conflict or regret (Gustafson, 2017; Truglio-Londrigan, Slyer DNP, Singleton, & Worral, 2014).
Several parents reported using faith to cope. All of these parents had low acculturation scores, indicating they had not adopted Americanized culture, lifestyle, behaviors, or other customs highly represented in Western medicine. Other studies have observed a relationship between spirituality and faith as a coping mechanism for health related issues among Latinx women (Jurkowski, Kurlanska, & Ramos, 2010) and identified faith as a source of support among families of children with developmental delay (Skinner, Correa, Skinner, & Bailey, 2001). Helping patients to identify positive and effective coping strategies consistent with their culture and values is a critical role of a genetic counselor. Effective coping strategies may help patients to conceptualize and adapt to new information. These strategies are influenced by culture and acculturation which cannot be assumed; rather they need to be elicited through open-ended questions to identify how they have coped effectively in other stressful or new situations or how they envision coping with the experience, which may or may not include their faith.
We observed inaccurate recall and misunderstanding of their child’s CES results among parents who had lower than a high school education and/or parent-provider language discordance. Additionally, parents with provider language discordance and/or low acculturation more frequently expressed some level of dissatisfaction relative to parents with provider language concordance and/or higher acculturation. The influence of these factors on patient experiences are clearly intertwined, and it is difficult to conclude which has the greatest influence and how this should guide the genetic counseling practice.
Low education level and non-English language proficiency are recognized barriers to medical care in the United States. English language skills correlate with better health outcomes even when race, age, and income are controlled for, and lower education and/or lower proficiency in English corresponds with lower health literacy and fewer regular medical visits (Bruce, Schwei, Park, & Jacobs, 2014; Kamara et al., 2018; Ponce, Hays, & Cunningham, 2006; Van Der Heide et al., 2013). Review of genetic counseling sessions for hereditary breast and ovarian cancer aided by interpreters found the interpreters provided misinterpretation which resulted in misinformation and misunderstanding by patients (Kamara et al., 2018). Education and income levels predicted knowledge of availability of direct to consumer genetic testing (Goddard et al., 2009), though another study found no association between educational level and knowledge of genetic testing option or pursuit of a cancer genetic test (Krakow, Ratcliff, Hesse, & Greenberg-Worisek, 2018). There are also mixed results regarding patient-provider ethnic concordance. Some studies suggest that racial and/or ethnic concordance improves patient outcomes and satisfaction (Laveist & Nuru-Jeter, 2002; Ma, Sanchez, & Ma, 2019). However other studies found no difference in satisfaction between patient-provider ethnic concordant and discordant pairs and detected lower uptake of breast cancer screening in Latinxs with concordant providers (Malhotra et al., 2017; Sweeney, Zinner, Rust, & Fryer, 2016). Parent-provider racial and/or ethnic concordance was not measured in our study, though we suspect concordance was present for only a modest number of our patients as only one of the GCs identifies as Caribbean Latino, the predominant ancestry of the Latinx served by our hospital.
There is no universal answer of how to best address the factors confounding equitable health care. These factors, including lower education, lower acculturation, and/or provider language or ethnic discordance, have the potential to overwhelm, intimidate and isolate the patient which in turn effects the equity of healthcare provided and received. Greater awareness of patient and family experiences, such as those demonstrated by our study and elucidation of patients’ values and priorities – which may or may be apparent at the onset of a session – can improve the patient-provider relationship, patient understanding, and overall experience.
Study Limitations
We present findings from a small, non-random, purposive sample of participants from a single institution. Eligible parents who declined may have had different experiences from those who participated in the study. Interviews were conducted by genetic counselors with differing language abilities in order to promote a sample linguistically representative of the Latinx population served by our institution. Despite the semi-structured nature of the interviews, differences in interview style as well as language may have affected responses. Native speakers experienced with medical translations translated the Spanish interviews, and all quotes were back translated by a second person for accuracy. It is controversial whether non-English interviews can be analyzed after translation, however others argue that a “good enough” translation can be achieved through rigorous examination of the context and process of translation (Temple, Edwards, & Alexander, 2006). The sample was composed primarily of mothers; fathers likely have different experiences from some of those described by our participants. Healthcare services provided to participants differed and may have affected experiences in ways that cannot be measured. Furthermore, while it was communicated with the parents that their responses were confidential and would not be shared with their child’s providers, parents may not have communicated negative experiences to the interviewers, who were affiliated with the hospital where their child received care. While most parents were interviewed six to 18 months after receiving their child’s test results, there were some who received results over 18 months prior to the study, and recall bias may have influenced participants’ responses. However, we found that participants' responses to prompts about understanding their child's test results were similar regardless of the amount of time between result disclosure and the interview. Finally, while we did not ask about patricipants’ familial countries of origin, it is likely that most participants were of Dominican or Puerto Rican ancestry, the two most prevalent Latinx communities in the Washington Heights area of New York where the hospital is located. Regardless of the number of countries of origin represented, the term Latinx describes a heterogeneous community that differs in ancestry, culture, beliefs, language, and other manners. Our findings should not be generalized to reflect the realities or experiences of all Latinx parents and/or patients.
Practice Recommendations
There is a need to examine how we practice culturally competent genetic counseling and use interpretive services. Joseph and colleagues (2017), who documented higher levels of patient misunderstanding and miscommunication when cancer genetic sessions involved an interpreter, recommend a restructuring of genetic counseling sessions with the provider prioritization of information that has direct utility for the patient and organization of the presented information into short- and long-term goals. They suggest these strategies could reduce information overload and improve comprehension for the patient and interpreter. We support these recommendations. However, we feel that many of the inequities revealed in our study could be addressed within the current model of genetic counseling, for example with improved ‘contracting,’ or the dialogue exchanged at the start of a genetic session that establishes the patient-provider relationship. This strategy could include directly asking patients their preferred language (even when patients respond in English), establishing a patient’s educational level and psychosocial needs, and tailoring the session to meet these needs. Using this information providers can then adjusted session content according to patients educational and cultural needs and help to create an environment to facilitate shared decision allowing patients to make an informed choice aligned with their beliefs and values. Other inequities may be resolved with minor changes to current practice including longer appointment times for sessions with an interpreter as these sessions may take longer than monolingual sessions. Additionally, when working with an interpreter, more frequent assessment of patient understanding (e.g., through using open-ended questions, asking the patient to repeat back their understanding, and reiterating key points) can help to reduce misunderstandings.
The genetic counseling profession needs to continue to take steps to provide the highest level of care regardless of patient's language, race, ethnicity, or other demographics. This effort includes both improving how we offer language interpretation as well as continuing to recruit minorities into the genetic counseling workforce. Addressing language barriers through accurate and efficient interpretation services might be effective for some patients. Reducing language barriers is particularly relevant since technology such as voice recognition apps is increasingly allowing for effective, accessible interpretation. At the same time, increasing the linguistic and cultural diversity in our professional workforce will allow more patients the opportunity to have a provider with a shared language and/or culture, which may result in the best care for some patients.
Research Recommendations
This study provides some data to guide practice recommendations for CES in Latinx communities, but additional research is needed to support these conclusions as well as to explore parallels and differences among other minority groups. The results of this study should be used to inform quantitative research, particularly the importance of patient-provider language concordance versus cultural concordance and acceptable forms of interpretation and how or if this varies by acculturation and educational level.
Conclusion
Latinx parental experiences with clinical exome sequencing have parallels to those reported in primarily White, non-Latinx parents, including the sense of obligation to pursue testing, the mixed emotional reactions to results and overall understanding of results. However, there are unique experiences and needs within the Latinx community. Our data suggest a degree of misunderstanding of CES results, some degree of dissatisfaction with care, and evidence of provider driven decision making, among parents with high school education or lower, low acculturation scores from standardized evaluation, and/or with language abilities and preferences different from their provider’s. Education, acculturation and preferred language are not always apparent upon meeting a patient and rather genetic counselors must proactively illicit this information during contracting and adjust sessions to ensure that patients’ needs are met. Finally, our data indicate that providers' language skills and culture influence patients' satisfaction. Therefore, in order to enhance patient satisfaction across ethnicities, languages, and cultures, there is a need for patients to be serviced by genetic counselors and genetic providers with a more diverse array of ethnicity, culture, race, and language than that which is currently represented in the workforce.
Supplementary Material
ACKNOWLEDGEMENTS
We would like to thank the study participants and the clinicians who cared for the participants. Support was provided by the JPB Foundation and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1TR001873. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations.
Footnotes
CONFLICT OF INTEREST
Daniel Luksic declares that he has no conflict of interest.
Radha Sukhu declares that she had no conflict of interest
Carrie Koval declares that she has no conflict of interest.
Megan T. Cho declares that she has no conflict of interest.
Aileen Espinal declares that she has no conflict of interest.
Katiana Rufino declares that she has no conflict of interest.
Tania Vasquez Loarte declares that she has no conflict of interest.
Wendy K Chung declares that she has no conflict of interest.
Julia Wynn declares that she has no conflict of interest.
HUMAN STUDIES AND INFORMED CONSENT
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and international) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all respondents for being included in the study.
ANIMAL STUDIES
No nonhuman animal studies were carried out by the authors for this article.
REFERENCES
- Browner CH, Preloran HM, Casado MC, Bass HN, & Walker AP (2003). Genetic counseling gone awry: Miscommunication between prenatal genetic service providers and Mexican-origin clients. Social Science & Medicine, 56(9), 1933–1946. 10.1016/S0277-9536(02)00214-9 [DOI] [PubMed] [Google Scholar]
- Bruce KH, Schwei RJ, Park LS, & Jacobs EA (2014). Barriers and facilitators to preventive cancer screening in Limited English Proficient (LEP) patients: Physicians’ perspectives. Communication & Medicine, 11(3), 235–247. 10.1558/cam.v11i3.24051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clift KE, Halverson CME, Fiksdal AS, Kumbamu A, Sharp RR, & McCormick JB (2015). Patients’ views on incidental findings from clinical exome sequencing. Applied & Translational Genomics, 4, 38–43. 10.1016/j.atg.2015.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, Gray J, & Clarke A (2000). Shared decision making and non-directiveness in genetic counselling. Journal of Medical Genetics, 37(2), 135–138. 10.1136/jmg.37.2.135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floyd E, Allyse MA, & Michie M (2016). Spanish- and English-Speaking Pregnant Women’s Views on cfDNA and Other Prenatal Screening: Practical and Ethical Reflections. Journal of Genetic Counseling, 25(5), 965–977. 10.1007/s10897-015-9928-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goddard KAB, Duquette D, Zlot A, Johnson J, Annis-Emeott A, Lee PW, Bland MP, Edwards KL, Oehlke K, Giles RT, Rafferty A, Cook ML, & Khoury MJ (2009). Public awareness and use of direct-to-consumer genetic tests: results from 3 state population-based surveys, 2006. American Journal of Public Health, 99(3), 442–445. 10.2105/AJPH.2007.131631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson A (2017). Reducing patient uncertainty: Implementation of a shared decision-making process enhances treatment quality and provider communication. In Clinical Journal of Oncology Nursing (Vol. 21, Issue 1, pp. 113–115). Oncology Nursing Society. 10.1188/17.CJON.113-115 [DOI] [PubMed] [Google Scholar]
- Hamilton AS, Hofer TP, Hawley ST, Morrell D, Leventhal M, Deapen D, Salem B, & Katz SJ (2009). Latinas and breast cancer outcomes: population-based sampling, ethnic identity, and acculturation assessment. Cancer Epidemiology Biomarkers and Prevention, 18(7), 2022–2029. 10.1158/1055-9965.EPI-09-0238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton JG, Shuk E, Arniella G, González CJ, Gold GS, Gany F, Robson ME, & Hay JL (2016). Genetic Testing Awareness and Attitudes among Latinos: Exploring Shared Perceptions and Gender-Based Differences. Public Health Genomics, 19(1), 34–46. 10.1159/000441552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurkowski JM, Kurlanska C, & Ramos BM (2010). Latino Women’s Spiritual Beliefs Related to Health. American Journal of Health Promotion, 25(1), 19–25. 10.4278/ajhp.080923-QUAL-211 [DOI] [PubMed] [Google Scholar]
- Kamara D, Weil J, Youngblom J, Guerra C, & Joseph G (2018). Cancer Counseling of Low-Income Limited English Proficient Latina Women Using Medical Interpreters: Implications for Shared Decision-Making. Journal of Genetic Counseling, 27(1), 155–168. 10.1007/s10897-017-0132-5 [DOI] [PubMed] [Google Scholar]
- Katz JN, Lyons N, Wolff LS, Silverman J, Emrani P, Holt HL, Corbett KL, Escalante A, & Losina E (2011). Medical decision-making among Hispanics and non-Hispanic Whites with chronic back and knee pain: a qualitative study. BMC Musculoskeletal Disorders, 12, 78. 10.1186/1471-2474-12-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinney AY, Gammon A, Coxworth J, Simonsen SE, & Arce-Laretta M (2010). Exploring attitudes, beliefs, and communication preferences of Latino community members regarding BRCA1/2 mutation testing and preventive strategies. Genetics in Medicine, 12(2), 105–115. 10.1097/GIM.0b013e3181c9af2d [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krabbenborg L, Vissers LE, Schieving J, Kleefstra T, Kamsteeg EJ, Veltman JA, Willemsen MA, & Van der Burg S (2016). Understanding the psychosocial effects of WES test results on parents of children with rare diseases. Journal of Genetic Counseling, 25(6), 1207–1214. 10.1007/s10897-016-9958-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakow M, Ratcliff CL, Hesse BW, & Greenberg-Worisek AJ (2018). Assessing Genetic Literacy Awareness and Knowledge Gaps in the US Population: Results from the Health Information National Trends Survey. Public Health Genomics, 20(6), 343–348. 10.1159/000489117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuperberg M, Lev D, Blumkin L, Zerem A, Ginsberg M, Linder I, Carmi N, Kivity S, Lerman-Sagie T, & Leshinsky-Silver E (2016). Utility of Whole Exome Sequencing for Genetic Diagnosis of Previously Undiagnosed Pediatric Neurology Patients. Journal of Child Neurology, 31(14), 1534–1539. 10.1177/0883073816664836 [DOI] [PubMed] [Google Scholar]
- Lantz PM, Mujahid M, Schwartz K, Janz NK, Fagerlin A, Salem B, Liu L, Deapen D, & Katz SJ (2006). The influence of race, ethnicity, and individual socioeconomic factors on breast cancer stage at diagnosis. American Journal of Public Health, 96(12), 2173–2178. 10.2105/AJPH.2005.072132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laveist TA, & Nuru-Jeter A (2002). Is doctor-patient race concordance associated with greater satisfaction with care? Journal of Health and Social Behavior, 43(3), 296–306. 10.2307/3090205 [DOI] [PubMed] [Google Scholar]
- López ME, Kaplan CP, Nápoles AM, Hwang ES, Livaudais JC, & Karliner LS (2014). Satisfaction with treatment decision-making and treatment regret among Latinas and non-Latina whites with DCIS. Patient Education and Counseling, 94(1), 83–89. 10.1016/j.pec.2013.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma A, Sanchez A, & Ma M (2019). The Impact of Patient-Provider Race/Ethnicity Concordance on Provider Visits: Updated Evidence from the Medical Expenditure Panel Survey. Journal of Racial and Ethnic Health Disparities. 10.1007/s40615-019-00602-y [DOI] [PubMed] [Google Scholar]
- Malhotra J, Rotter D, Tsui J, Llanos AAM, Balasubramanian BA, & Demissie K (2017). Impact of patient–provider race, ethnicity, and gender concordance on cancer screening: Findings from Medical Expenditure Panel Survey. Cancer Epidemiology Biomarkers and Prevention, 26(12), 1804–1811. 10.1158/1055-9965.EPI-17-0660 [DOI] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Vanoss Marin B, Otero-Sabogal R, & Perez-Stable EJ (1987). Development of a Short Acculturation Scale for Hispanics. Hispanic Journal of Behavioral Sciences, 9(2), 183–205. [Google Scholar]
- Molina F, Dehlendorf C, Gregorich SE, & Kuppermann M (2019). Women’s preferences for and experiences with prenatal genetic testing decision making: Sociodemographic disparities in preference-concordant decision making. Patient Education and Counseling, 102(3), 595–601. 10.1016/j.pec.2018.10.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan D, & Carlson M (2016). Whole Exome Sequencing in Pediatric Neurology Patients. Journal of Child Neurology, 31(7), 887–894. 10.1177/0883073815627880 [DOI] [PubMed] [Google Scholar]
- Ponce NA, Hays RD, & Cunningham WE (2006). Linguistic disparities in health care access and health status among older adults. Journal of General Internal Medicine, 21(7), 786–791. 10.1111/j.1525-1497.2006.00491.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riffin C, Pillemer K, Reid MC, & Löckenhoff CE (2016). Decision Support Preferences Among Hispanic and Non-Hispanic White Older Adults With Chronic Musculoskeletal Pain. The Journals of Gerontology. Series B, 71(5), 914–925. 10.1093/geronb/gbv071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosell AMC, Pena LDM, Schoch K, Spillmann R, Sullivan J, Hooper SR, Jiang YH, Mathey-Andrews N, Goldstein DB, & Shashi V (2016). Not the end of the odyssey: parental perceptions of whole exome sequencing (WES) in pediatric undiagnosed disorders. Journal of Genetic Counseling, 25(5), 1019–1031. 10.1007/s10897-016-9933-1 [DOI] [PubMed] [Google Scholar]
- Rossi M, El-Khechen D, Black MH, Farwell Hagman KD, Tang S, & Powis Z (2017). Outcomes of Diagnostic Exome Sequencing in Patients With Diagnosed or Suspected Autism Spectrum Disorders. Pediatric Neurology, 70, 34–43.e2. 10.1016/j.pediatrneurol.2017.01.033 [DOI] [PubMed] [Google Scholar]
- Skinner DG, Correa V, Skinner M, & Bailey DB (2001). Role of Religion in the Lives of Latino Families of Young Children With Developmental Delays. American Journal of Mental Retardation, 106(4), 297–313. [DOI] [PubMed] [Google Scholar]
- Sussner KM, Thompson HS, Valdimarsdottir HB, Redd WH, & Jandorf L (2009). Acculturation and familiarity with, attitudes towards and beliefs about genetic testing for cancer risk within Latinas in East Harlem, New York City. Journal of Genetic Counseling, 18(1), 60–71. 10.1007/s10897-008-9182-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney CF, Zinner D, Rust G, & Fryer GE (2016). Race/ethnicity and health care communication. Medical Care, 54(11), 1005–1009. 10.1097/MLR.0000000000000578 [DOI] [PubMed] [Google Scholar]
- Temple B, Edwards R, & Alexander C (2006). Grasping at context: Cross language qualitative research as secondary qualitative data analysis. Qualitative Social Research, 7(4). 10.17169/fqs-7.4.176 [DOI] [Google Scholar]
- Truglio-Londrigan M, Slyer DNP JT, Singleton JK, & Worral PS (2014). A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Database of Systematic Reviews & Implementation Reports, 12(5), 121–194. 10.11124/jbisrir-2014-1414 [DOI] [PubMed] [Google Scholar]
- Vadaparampil ST, McIntyre J, & Quinn GP (2010). Awareness, perceptions, and provider recommendation related to genetic testing for hereditary breast cancer risk among at-risk hispanic women: Similarities and variations by sub-ethnicity. Journal of Genetic Counseling, 19(6), 618–629. 10.1007/s10897-010-9316-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valencia CA, Husami A, Holle J, Johnson JA, Qian Y, Mathur A, Wei C, Indugula SR, Zou F, Meng H, Wang L, Li X, Fisher R, Tan T, Hogart Begtrup A, Collins K, Wusik KA, Neilson D, Burrow T, Schorry E, Hopkin R, Keddache M, Harley JB, Kaufman KM, & Zhang K (2015). Clinical Impact and Cost-Effectiveness of Whole Exome Sequencing as a Diagnostic Tool: A Pediatric Center’s Experience. Frontiers Pediatrics, 3(67). 10.3389/fped.2015.00067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Der Heide I, Wang J, Droomers M, Spreeuwenberg P, Rademakers J, & Uiters E (2013). The relationship between health, education, and health literacy: Results from the dutch adult literacy and life skills survey. Journal of Health Communication, 18(SUPPL. 1), 172–184. 10.1080/10810730.2013.825668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vissers LELM, Van Nimwegen KJM, Schieving JH, Kamsteeg EJ, Kleefstra T, Yntema HG, Pfundt R, Van Der Wilt GJ, Krabbenborg L, Brunner HG, Van Der Burg S, Grutters J, Veltman JA, & Willemsen MAAP (2017). A clinical utility study of exome sequencing versus conventional genetic testing in pediatric neurology. Genetics in Medicine, 19(9), 1055–1063. 10.1038/gim.2017.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynn J, Ottman R, Duong J, Wilson AL, Ahimaz P, Martinez J, Rabin R, Rosen E, Webster R, Au C, Cho MT, Egan C, Guzman E, Primiano M, Shaw JE, Sisson R, Klitzman RL, Appelbaum PS, Lichter-Konecki U, Anyane-Yeboa K, Iglesias A, & Chung WK (2018). Diagnostic exome sequencing in children: A survey of parental understanding, experience and psychological impact. Clinical Genetics, 93(5), 1039–1048. 10.1111/cge.13200 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


