Abstract
Background
Lactation results in substantial maternal bone loss that is recovered following weaning. However, the mechanisms underlying this recovery, and in particular the role of insulin-like growth factor 1 (IGF-I), is not clear. Furthermore, there is little data regarding whether recovery is affected by advanced maternal age.
Methods
Using micro-computed tomography, we studied bone recovery following lactation in mice at 2, 5 and 7 months of age. We also investigated the effects of reduced IGF-I availability using mice lacking PAPP-A2, a protease of insulin-like growth factor binding protein 5 (IGFBP-5).
Results
In 2 month old mice, lactation affected femoral trabecular and cortical bone, but only cortical bone showed recovery 3 weeks after weaning. This recovery was not affected by deletion of the Pappa2 gene. The amount of trabecular bone was reduced in 5 and 7 month old mice, and was not further reduced by lactation. However, the recovery of cortical bone was impaired at 5 and 7 months compared with at 2 months.
Conclusions
Recovery of the maternal skeleton after lactation is impaired in moderately-aged mice compared with younger mice. Our results may be relevant to the long-term effects of breastfeeding on the maternal skeleton in humans, particularly given the increasing median maternal age at childbearing.
Introduction
Lactation has a profound effect on the maternal skeleton. Bone mineral density (BMD) decreases dramatically, regardless of the use of calcium supplements, declining 1–3% per month during lactation [1, 2]. In contrast, the decline in BMD is 1.2% per year in the first 5 years of menopause [3]. Remarkably, there appears to be complete recovery of the maternal skeleton after weaning [1], and numerous studies have found no long-term effects of parity or lactation history on menopausal risk of low BMD and/or fractures [4, 5]. However, the effects of maternal age on recovery are less clear. It has been hypothesized that pregnancy prior to the acquisition of peak BMD may impair maximum mineralization achieved, and thus may have long-term effects [6]. Some studies have found support for this hypothesis [7–11], although a few have found ambiguous results [12], no effect [5, 13], or the opposite pattern [14].
In contrast to studies of younger mothers, there has been no study of the long-term effects of lactation at advanced maternal age on skeletal health. However, a shorter-term study did find some evidence that recovery after lactation could be impaired at older maternal age; the increase in bone mineral content from parturition to 2 years postpartum was negatively related to age [15]. Given that some bone loss occurs before menopause [16–19] and that the perimenopausal rate of bone loss is higher than that in the early menopause [3], it might be expected that pregnancies at older ages could impact BMD. Such effects would not have been detected in previous studies that found no effect of lactation on menopausal skeletal health because they would not have included the proportions of older mothers that make up today’s population as a result of delayed childbearing [20].
In addition to uncertainty regarding the effects of maternal age, the mechanisms underlying the remarkable recovery of the skeleton post lactation are unknown [2]. Insulin-like growth factor 1 (IGF-I) is a likely candidate given its important roles in bone physiology [21–23]. IGF-I availability is regulated by insulin-like growth factor binding proteins (IGFBPs), among which IGFBP-5 is one of the most abundant in bone [24]. IGFBP-5 influences bone mineral density (BMD) [25–27] by regulating IGF availability as well as through IGF-independent effects [28, 29]. The release of IGF-I from IGFBP-5 is regulated by proteases, including pregnancy-associated pregnancy protein-A2 (PAPP-A2) [30–33]. Loss-of-function mutations in the human PAPPA2 gene cause short stature and reduced bone density [34, 35], and these conditions are improved by treatment with IGF-I [36–38]. In mice, deletion of Pappa2 reduces the linear growth of bones [39–41] and affects bone composition and microarchitecture [42, 43].
The goal of the present study was to assess the effects of maternal age and Pappa2 deletion on the recovery of the maternal skeleton after lactation in a mouse model. We predict that recovery after lactation will decrease at older maternal ages, and that recovery will be impaired by deletion of Pappa2 as a result of reduced IGF availability. Despite differences between rodents and humans [6], changes in the circulating levels of minerals and many of the key hormones involved in calcium homeostasis during pregnancy and lactation are similar in humans and mice [4].
Materials and methods
Mice
All work was carried out in accordance with the guidelines of the Canadian Council on Animal Care and was approved by the SFU University Animal Care Committee (protocol 1188–11). Mice were housed in individually ventilated cages (50 air changes/hour; in pairs for breeding and up to 5 mice per cage otherwise) with Enrich-o’Cobs bedding (Andersons Lab Bedding, Maumee, OH) on a 12:12 hour light:dark cycle, at constant temperature (21 ± 1°C), 50% humidity, with water and food available ad libitum (maintenance diet: 5001; breeding diet: Prolab RMH 3000, LabDiet, St. Louis, MO). Animal health was monitored daily, and apart from 9 mice culled due to dystocia or other ill health, there was no mortality outside of planned euthanasia. Euthanasia was performed by isoflurane anesthesia followed by CO2 inhalation.
Mice homozygous for a constitutive Pappa2 deletion allele (Pappa2KO/KO) with a C57BL/6 background were generated as previously described [40, 44]. As controls, we used mice homozygous for a conditional deletion allele (where the Pappa2 gene is intact, but exon 2 is flanked by LoxP sites [40], i.e., floxed, Pappa2fl/fl). We have previously shown that postnatal growth does not differ between Pappa2fl/fl and Pappa2wt/wt mice [44]. The use of Pappa2fl/fl as controls enabled a reduction in the number of mice used, since we needed to breed these mice to maintain the colony. Genotypes were confirmed by PCR using ear-clip tissue obtained at weaning, as previously described [44].
Mice were bred for the first time at either 2 months, 5 months or 7 months. Mice breed well at 2 and 5 months, but reproductive performance declines by 7 months (personal observation). Peak BMD is achieved shortly before 19 weeks [45], but trabecular bone peaks at 2 months and declines thereafter [46]. Thus, 2 month mice are young breeders, who have not yet achieved peak BMD, 5 month mice have achieved peak BMD and show some trabecular bone loss, while 7 month mice have more bone loss and are approaching reproductive senescence.
Females were euthanized after 3 weeks of lactation (the normal duration of mouse lactation in the lab), or 3 weeks after weaning. In mice, the recovery of the vertebrae is complete by 4 weeks post-weaning, whereas the recovery of the femur is incomplete after 3–4 weeks [47, 48]. We therefore focused on recovery of the femur 3 weeks after weaning as this skeletal site and time point would allow assessment of variation in recovery. Mice bred at 7 months were very poor breeders; many did not become pregnant, and among those who did, many took a long time to become pregnant and/ or cannibalized their litter. Therefore, at 7 months, we only collected mice 3 weeks after weaning to obtain a sufficient sample size. For mice bred at 2 months and 5 months, we only included females who had given birth to, and lactated for, a single litter. However, since breeding performance was so poor at 7 months, at this age we also included females that cannibalized a first litter, but successfully reared a second litter.
Within 4 days of birth, litter size was adjusted to 7 pups to reduce variability in maternal lactational demands. Bred females were excluded from analyses if they weaned fewer than 5 pups. Where possible, for each breeding female, we also collected a virgin age-matched control (AMC), usually a sibling of a bred mouse. All mice (bred and virgin) were kept in identical conditions, including changes to a breeder diet during breeding.
Micro-computed tomography
Following sacrifice, mice were stored at -20°C, and later exposed to dermestid beetles for removal of soft tissue. Femurs were scanned using micro-computed tomography (micro-CT) with an isotropic voxel size of 7.4 μm (Scanco Medical μCT100, Switzerland; 70 kVp, 114 μA, 100 ms integration time). For trabecular bone, the region of interest was proximal to the distal growth plate, 222 μm proximal from where the four sections of the bone appeared to fuse in cross-section. The region of interest for cortical bone was the mid-shaft, immediately distal to the third trochanter (where the cross-section of the bone transitioned from a teardrop shape and became rounder). For both trabecular and cortical bone, 5% of the total length of bone was analysed. Apart from knowledge of bone length, the selection of the region of interest was performed blind to age, genotype and breeding status. Measures of trabecular bone microarchitecture included bone volume fraction (BV/TV, %), trabecular number (Tb.N, mm-1), trabecular separation (Tb.Sp, μm), and trabecular thickness (Tb.Th, μm) [49]. Measures of cortical bone morphology included cortical area fraction (Ct.Ar/Tt.Ar, %), average cortical thickness (Ct.Th, μm), and cortical porosity (Ct.Po, %) [49].
Serum IGF-I and IGFBP-5
At collection, females were blood sampled by cardiac puncture, and serum was stored at -80°C. We measured serum IGF-I and IGFBP-5 using the IGF-1 DuoSet ELISA kit (#DY791, R&D Systems) and the IGFBP-5 DuoSet ELISA kit (#DY578, R&D Systems), respectively, following the manufacturer’s instructions.
Statistical analyses
Data were analysed using general linear models (proc GLM, SAS, version 9.4). The specific models and sample sizes are described below.
Results and discussion
Skeletal traits affected by lactation
To identify traits that were affected by lactation and that showed recovery after three weeks, we first analysed the effects of breeding (bred mice vs. AMC) and timing (collected at wean vs. three weeks after wean) in Pappa2fl/fl mice (with intact Pappa2) at 2 months of age to facilitate comparison with previous studies [47, 48]. These analyses used general linear models including effects of breeding, timing and the interaction between breeding and timing. An effect of breeding indicated that a trait was affected by lactation, whereas an effect of timing indicated a change with age (since it occurred in AMC as well). A significant interaction between breeding and timing potentially indicated recovery from the effects of lactation, if bred mice were more similar to AMC after three weeks of recovery than at wean. Trabecular bone volume fraction was reduced by both breeding and 3 weeks of aging, while trabecular number declined and trabecular separation increased with 3 weeks of aging, and trabecular thickness was reduced by breeding (Table 1). However, none of these traits showed an interaction between breeding and timing, suggesting no evidence of recovery (Table 1). In contrast, cortical area fraction and cortical thickness were reduced by breeding and increased with 3 weeks of aging, but the interaction between breeding and timing was significant, such that values increased more in bred mice over the 3 weeks following weaning, and were more similar to AMC after three weeks of recovery than at wean (Table 1). Cortical porosity showed a similar but inverse pattern (i.e., increased by breeding, etc., Table 1).
Table 1. Effects of lactation and recovery after weaning on skeletal traits in 2 month old control mice.
| Bred females | Age-matched controls | Breeding (bred vs. AMC) | Timing (at wean vs. 3 weeks after) | Breeding*timing interaction | |||
|---|---|---|---|---|---|---|---|
| At wean | 3 weeks after wean | At wean | 3 weeks after wean | P | P | P | |
| Sample size | 17 | 17 | 16 | 15 | |||
| Trabecular | |||||||
| Bone volume fraction (%) | 6.4±0.4 | 3.9±0.4 | 7.2±0.4 | 4.8±0.4 | 0.04 | < 0.0001 | 0.85 |
| Trabecular number (mm-1) | 3.84±0.09 | 3.33±0.09 | 3.79±0.09 | 3.25±0.09 | 0.45 | < 0.0001 | 0.89 |
| Trabecular separation (μm) | 260±8 | 302±8 | 262±8 | 310±8 | 0.55 | < 0.0001 | 0.78 |
| Trabecular thickness (μm) | 37.4±0.9 | 36.4±0.9 | 43.4±0.9 | 41.4±1.0 | < 0.0001 | 0.11 | 0.59 |
| Cortical | |||||||
| Cortical area fraction (%) | 36.6±0.6 | 43.4±0.6 | 45.5±0.6 | 46.8±0.6 | < 0.0001 | < 0.0001 | < 0.0001 |
| Cortical thickness (μm) | 147±2 | 182±2 | 185±2 | 193±2 | < 0.0001 | < 0.0001 | < 0.0001 |
| Cortical porosity (%) | 6.3±0.2 | 5.1±0.2 | 5.2±0.2 | 5.1±0.2 | 0.008 | 0.006 | 0.01 |
Values are least squares means ± standard error from a general linear model including effects of breeding (bred vs. age-matched control), timing (at wean vs. 3 weeks after), and the breeding*timing interaction.
Our finding that both trabecular and cortical bone were affected by lactation, but that cortical bone showed more recovery, is consistent with previous work. In a previous study of C57BL/6J mice, femoral trabecular bone volume fraction, trabecular number and trabecular spacing showed little recovery 3 weeks after weaning [47]. In contrast, while cortical thickness, cortical area fraction and cortical porosity still showed an effect of lactation 3 weeks after weaning, the difference between bred mice and non-lactating controls was smaller after recovery than at wean [47]. Similar results were observed after 4 weeks of recovery in CD-1 mice [48]. In rats, tibial cortical bone showed complete recovery 6 weeks after weaning whereas the recovery of trabecular bone was incomplete [50, 51]. The reduction in cortical bone during lactation is due to both reduced periosteal bone formation [52] and increased endocortical bone resorption [53] with the latter being reversed after weaning [54].
Factors affecting circulating IGF-I and IGFBP-5 levels
We analysed circulating IGF-I and IGFBP-5 levels in 2 month old mice using general linear models including the effects of breeding, timing, and genotype, as well as the interaction between breeding and timing (as above), and the three-way interactions between breeding, timing and genotype (to test whether recovery differed between genotypes). IGF-I levels were significantly lower in Pappa2KO/KO mice than Pappa2fl/fl mice (P = 0.0001), but were not influenced by any other factor (breeding P = 0.28; timing P = 0.13; breeding* timing P = 0.28; breeding*timing*genotype P = 0.92; S1 Fig). Conversely, IGFBP-5 levels were significantly higher in Pappa2KO/KO mice than Pappa2fl/fl mice (P < 0.0001), but were not influenced by any other factor (breeding P = 0.21; timing P = 0.73; breeding* timing P = 0.51; breeding*timing*genotype P = 0.34; S2 Fig).
The increase in IGFBP-5 levels as a result of the deletion of Pappa2, a gene encoding an IGFBP-5 protease, was expected, and consistent with our previous work [42, 44]. Similarly, this increase in IGFBP-5 would be expected to reduce available IGF-I levels, and such an increase has previously been observed in an independent transgenic mouse carrying a mutation eliminating the proteolytic activity of PAPP-A2 [55]. However, while we found that IGF-I levels were not altered by breeding or recovery, a previous study found IGF-I levels to be significantly elevated 3 weeks after weaning, although there was no difference between lactating and non-lactating mice at wean [47].
Effects of age and Pappa2 deletion on the recovery of the skeleton after lactation
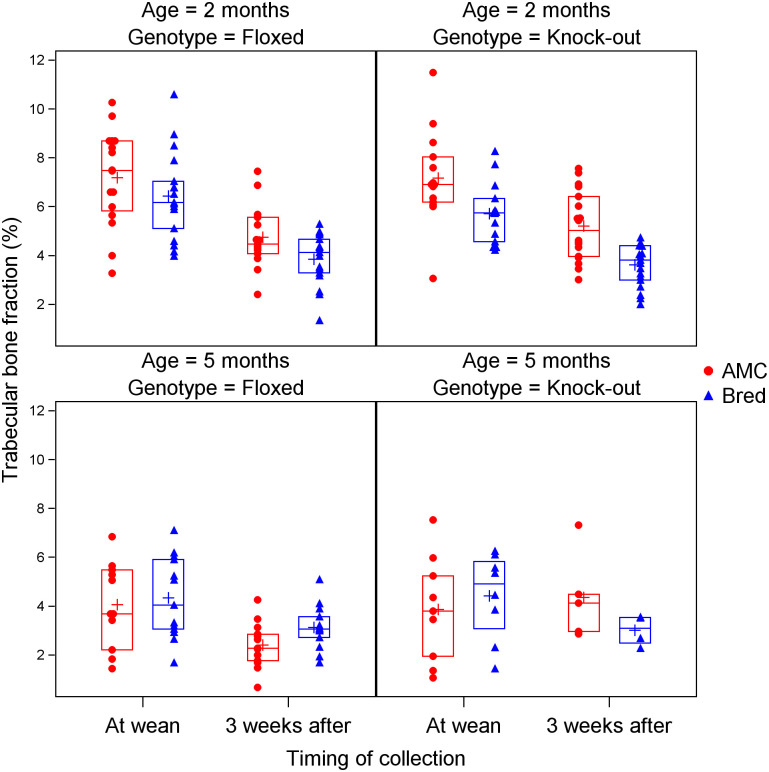
To examine the effects of age and Pappa2 deletion on the recovery of the skeleton after lactation, we performed analyses including both Pappa2KO/KO and Pappa2fl/fl mice at 2 and 5 months of age; sample sizes are shown in Table 2. We did not include 7 month old mice in this analysis since these were not collected at wean. General linear models included effects of breeding, timing, genotype, age, as well as the interaction between breeding and timing (as above), and three-way interactions between breeding, timing and genotype (to test whether recovery differed between genotypes) and between breeding, timing and age (to test whether recovery differed between ages) (Table 3). Trabecular bone volume fraction was reduced by breeding and by aging (both between wean and 3 weeks afterwards, and between 2 and 5 months) (Table 3; Fig 1). The three-way interaction between breeding, timing and age was significant, whereby trabecular bone volume fraction was reduced by breeding at 2 months, but there was little effect of breeding at 5 months, either at wean or 3 weeks later (Table 3; Fig 1). A potential explanation for this result was that trabecular bone was already greatly reduced at 5 months even in virgin mice, such that it could not provide a substantial amount of calcium for lactation. Trabecular number showed a similar pattern, except that this trait declined between wean and recovery at 2 months but not 5 months (Table 3; S3 Fig). Trabecular spacing showed only increases with aging (both between wean and 3 weeks afterwards, and between 2 and 5 months, Table 3; S4 Fig). Trabecular thickness showed an effect of breeding (reduced in bred mice), age (increased at 5 months) and genotype (higher in Pappa2KO/KO mice) (Table 3; S5 Fig).
Table 2. Sample sizes in analyses of the effects of age and Pappa2 deletion on the recovery of the skeleton after lactation.
| Age | Breeding | Timing | Genotype | Sample size |
|---|---|---|---|---|
| 2 months | Bred | At wean | Floxed | 17 |
| Knock-out | 14 | |||
| 3 weeks after | Floxed | 17 | ||
| Knock-out | 19 | |||
| AMC | At wean | Floxed | 16 | |
| Knock-out | 14 | |||
| 3 weeks after | Floxed | 15 | ||
| Knock-out | 18 | |||
| 5 months | Bred | At wean | Floxed | 13 |
| Knock-out | 8 | |||
| 3 weeks after | Floxed | 13 | ||
| Knock-out | 4 | |||
| AMC | At wean | Floxed | 11 | |
| Knock-out | 9 | |||
| 3 weeks after | Floxed | 13 | ||
| Knock-out | 5 | |||
| 7 months | Bred | 3 weeks after | Floxed | 3 |
| Knock-out | 4 | |||
| AMC | 3 weeks after | Floxed | 5 | |
| Knock-out | 10 |
Table 3. Effects of age and Pappa2 genotype on the recovery of skeletal traits in 2 and 5 month old mice.
| Breeding (bred vs. AMC) | Timing (at wean vs. 3 weeks after) | Age (2 vs. 5 months) | Genotype (Pappa2KO/KO vs. Pappa2fl/fl) | Breeding*timing interaction | Breeding*timing*age interaction | Breeding*timing*genotype interaction | |
|---|---|---|---|---|---|---|---|
| Trabecular | |||||||
| Bone volume fraction (%) | 0.02 | <0.0001 | <0.0001 | 0.82 | 0.50 | 0.0012 | 0.14 |
| Trabecular number (mm-1) | 0.34 | <0.0001 | <0.0001 | 0.95 | 0.34 | 0.0032 | 0.33 |
| Trabecular separation (μm) | 0.15 | <0.0001 | <0.0001 | 0.84 | 0.18 | 0.14 | 0.37 |
| Trabecular thickness (μm) | <0.0001 | 0.84 | <0.0001 | 0.03 | 0.20 | 0.74 | 0.11 |
| Cortical | |||||||
| Cortical area fraction (%) | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.36 |
| Cortical thickness (μm) | <0.0001 | <0.0001 | 0.59 | 0.27 | <0.0001 | <0.0001 | 0.54 |
| Cortical porosity (%) | <0.0001 | <0.0001 | 0.0036 | 0.12 | 0.0002 | 0.0013 | 0.97 |
P-values are from general linear models included effects of breeding, timing, age, genotype, the interaction between breeding and timing, and three-way interactions between breeding, timing and genotype (to test whether recovery differed between genotypes) and between breeding, timing and age (to test whether recovery differed between ages). AMC = age-matched controls.
Fig 1. Effects of age, Pappa2 genotype, lactation and recovery after weaning on trabecular bone fraction.
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
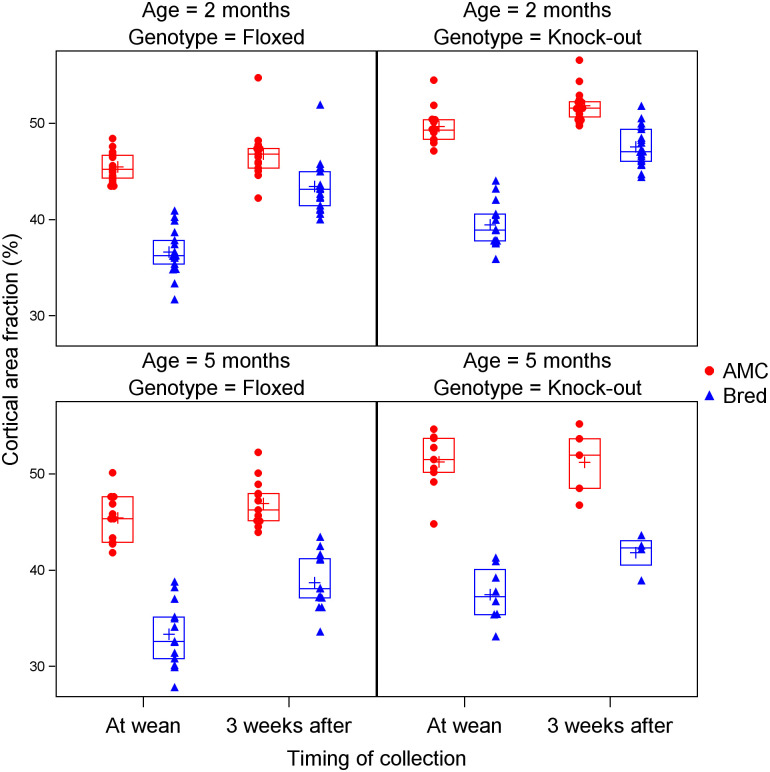
Cortical area fraction showed significant effects of breeding (lower in bred mice), timing (higher after 3 weeks), age (higher at 5 months), genotype (higher in Pappa2KO/KO mice), and a significant interaction between breeding and timing, as described above (Table 3; Fig 2). Moreover, there was a significant three-way interaction between breeding, timing and age, whereby the difference between bred and AMC mice diminished between wean and 3 weeks later (reflecting the breeding by timing interaction), but did so to a greater extent at 2 months, indicating that recovery was impaired at 5 months of age (Fig 2). Cortical thickness showed similar patterns, and although the effects of age and genotype were not significant, the three-way interaction between breeding, timing and age was significant (Table 3; S6 Fig). Cortical porosity also showed similar patterns (Table 3; S7 Fig).
Fig 2. Effects of age, Pappa2 genotype, lactation and recovery after weaning on cortical area fraction.
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
No trait showed a significant three-way interaction between breeding, timing and genotype (Table 3), suggesting that recovery was not impaired by Pappa2 deletion. While this result is surprising given the roles of IGF-I and IGFBP-5 in bone physiology, IGF-I availability may not be crucial for recovery after lactation. A previous study found that osteocyte-derived IGF-I is not required for the recovery of bone following dietary calcium deprivation [56]. Pappa2 deletion has previously been shown to affect bone growth in virgin animals, and in the present study we found that it increased cortical area fraction and trabecular thickness. The increase in cortical area fraction is consistent with previous work [42], and is likely the result of reduced IGF-I availability, given that it was also observed with a knock-in Pappa2 allele coding for protein that lacked proteolytic activity [55].
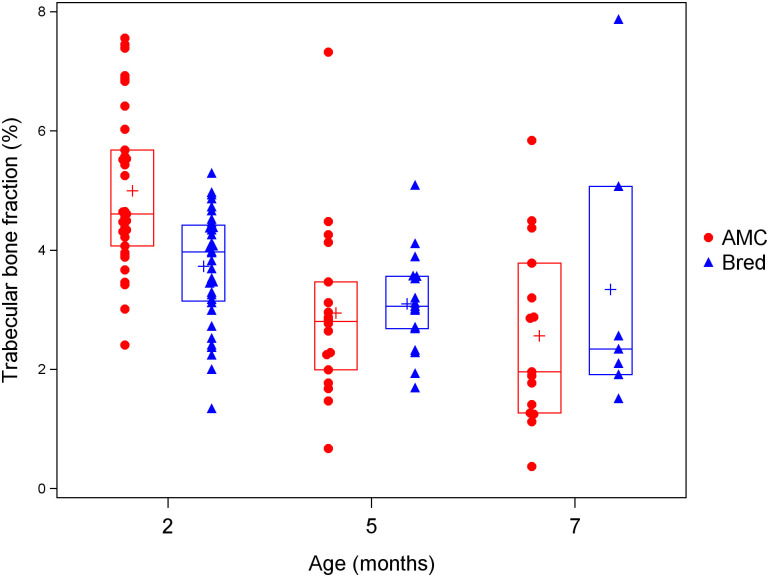
Because 7 month old mice were not collected at wean, we also performed analyses including Pappa2KO/KO and Pappa2fl/fl mice at 2, 5 and 7 months of age, including only those mice collected 3 weeks after weaning. General linear models included effects of breeding, age and genotype, as well as the interactions between breeding and age and between genotype and age. Because these analyses included only mice collected 3 weeks after weaning, the effect of breeding was used to assess recovery (a significant effect of breeding 3 weeks after weaning indicated that recovery was not complete), and the breeding by age interaction was used to test whether recovery differed between ages. Similar to the previous analysis, for trabecular bone volume fraction, the effect of age was significant and there was a significant interaction between age and breeding. Trabecular bone volume fraction was reduced by breeding at 2 months, but not at 5 and 7 months (Table 4; Fig 3). For trabecular number and spacing, only the effect of age was significant, with number decreasing and spacing increasing with age (Table 4; S8 and S9 Figs). Trabecular thickness increased with age and was reduced by breeding, but there was no significant interaction between age and breeding (Table 4; S10 Fig).
Table 4. Effects of age and Pappa2 genotype on the recovery of skeletal traits in 2, 5 and 7 month old mice, including only mice collected 3 weeks after weaning.
| Breeding (bred vs. AMC) | Age (2 vs. 5 vs. 7 months) | Genotype (Pappa2KO/KO vs. Pappa2fl/fl) | Breeding*age interaction | Genotype*age interaction | |
|---|---|---|---|---|---|
| Trabecular | |||||
| Bone volume fraction (%) | 0.54 | <0.0001 | 0.36 | 0.002 | 0.0007 |
| Trabecular number (mm-1) | 0.66 | <0.0001 | 0.82 | 0.71 | 0.57 |
| Trabecular separation (μm) | 0.62 | <0.0001 | 0.25 | 0.39 | 0.15 |
| Trabecular thickness (μm) | 0.0002 | <0.0001 | 0.55 | 0.81 | 0.01 |
| Cortical | |||||
| Cortical area fraction (%) | <0.0001 | <0.0001 | <0.0001 | <0.0001 | 0.11 |
| Cortical thickness (μm) | <0.0001 | 0.02 | 0.01 | <0.0001 | 0.06 |
| Cortical porosity (%) | <0.0001 | 0.01 | 0.02 | 0.0004 | 0.40 |
P-values are from general linear models included effects of breeding, age, genotype, the interaction between breeding and age, and the interaction between genotype and age. AMC = age-matched controls.
Fig 3. Effects of age and lactation on trabecular bone fraction among mice collected 3 weeks after weaning.
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
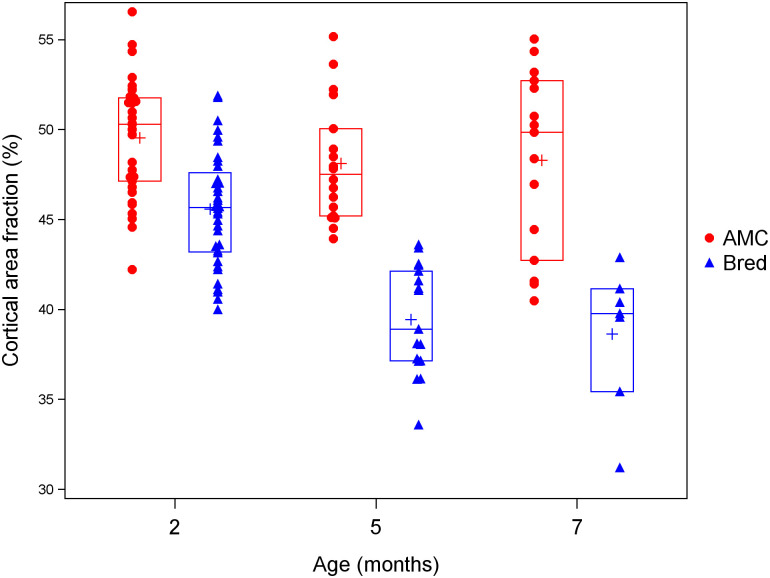
Cortical area fraction showed significant effects of breeding (lower in bred mice), age (decrease with age), genotype (higher in Pappa2KO/KO mice), and a significant interaction between breeding and age, whereby the difference between bred and AMC after 3 weeks of recovery was smaller at 2 months than at 5 or 7 months (Table 4; Fig 4). Cortical thickness and porosity showed similar patterns (Table 4; S11 and S12 Figs). Trabecular bone volume fraction and trabecular thickness showed significant genotype by age interactions, whereby these traits were elevated in Pappa2KO/KO mice at 5 months but reduced at 7 months (S13 and S14 Figs). These results including 7 month old mice are consistent with the analyses above including only 2 and 5 month old mice collected at both wean and after 3 weeks of recovery: the recovery of cortical bone is impaired at older ages, whereas trabecular bone is not affected by breeding even at wean in older mice, potentially because levels are so low that it cannot provide a substantial amount of calcium.
Fig 4. Effects of age and lactation on cortical area fraction among mice collected 3 weeks after weaning.
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
Effects of pregnancy vs. lactation on bone
Pregnancy itself affects bone mass and microarchitecture [2, 57], and therefore the effects of lactation described above could have been due, at least in part, to pregnancy. To distinguish between effects of pregnancy and lactation, we analysed females that had given birth, but lost the litter soon after birth, and were collected 3 weeks after birth, i.e., at the time when lactating females would have been collected at wean. We identified 6 such females that could be matched to both a bred female collected at wean and an age-matched control of the same age and genotype collected around the same time. Cortical traits were all significantly reduced in females that had successfully reared a litter, while females that had been pregnant but lost their litters were not significant different from age-matched controls (Table 5). Thus, at 3 weeks after birth, cortical traits were affected by lactation but not by pregnancy. Trabecular thickness showed a similar pattern, although bred females were not statistically different from those who lost a litter (Table 5). Trabecular separation was significantly higher in females that had been pregnant but lost their litters than in age-matched controls (Table 5). While there were no significant differences among groups for bone volume fraction and trabecular number, these traits showed a similar pattern to trabecular separation, i.e., females that had been pregnant but lost their litters had the lowest amount of bone (Table 5). These results suggest that these females may have not been able to lactate successfully because of reduced trabecular calcium stores.
Table 5. Effects of pregnancy vs. lactation on skeletal traits.
| AMC (no pregnancy, no lactation) | Lost litter (pregnancy but no lactation) | Weaned pups (pregnancy and lactation) | Group (AMC vs. lost litter vs. weaned pups) | Cohort | |
|---|---|---|---|---|---|
| P | P | ||||
| Trabecular | |||||
| Bone volume fraction (%) | 5.3±0.4a | 3.6±0.4a | 4.2±0.4a | 0.06 | 0.04 |
| Trabecular number (mm-1) | 3.2±0.1a | 2.9±0.1a | 3.1±0.1a | 0.08 | 0.0003 |
| Trabecular separation (μm) | 313±11a | 360±11b | 337±11ab | 0.045 | 0.0002 |
| Trabecular thickness (μm) | 44±1a | 41±1ab | 38±1b | 0.02 | 0.005 |
| Cortical | |||||
| Cortical area fraction (%) | 48±1a | 49±1a | 36±1b | <0.0001 | 0.014 |
| Cortical thickness (μm) | 193±6a | 198±6a | 141±6b | <0.0001 | 0.23 |
| Cortical porosity (%) | 5.3±0.3a | 5.1±0.3a | 6.9±0.3b | 0.004 | 0.70 |
Six females that lost their litter soon after birth were collected 3 weeks after birth and were matched with a female who bred successfully and an age-matched control (AMC) of the same age and genotype. A matched trio of 3 mice (lost litter, bred successfully and AMC) were considered a cohort. Values are least squares means ± standard error from a general linear model including effects of group and cohort. Values with the same superscript letter are not significantly different.
Conclusions
In young mice with intact Pappa2, lactation affects femoral trabecular and cortical bone, but only cortical bone shows some recovery 3 weeks after lactation. The deletion of Pappa2 does not impair this recovery. In mice bred at 5 and 7 months, trabecular bone is no longer affected by lactation, perhaps because levels are so low that it cannot provide a substantial amount of calcium. However, the recovery of cortical bone is impaired at 5 and 7 months. Our results may be relevant to the long-term effects of breastfeeding on the maternal skeleton in humans, particularly given the increasing median maternal age at childbearing [20].
Supporting information
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote bred mice, and red circles denote age-matched controls (AMC). Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote Pappa2fl/fl mice and red circles denote Pappa2KO/KO mice. Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
Blue triangles denote Pappa2fl/fl mice and red circles denote Pappa2KO/KO mice. Crosses denote means, while horizontal lines denote the 25th, 50th and 75th percentiles.
(TIF)
(XLSX)
Acknowledgments
We thank Lauren Pettifer, Amritdeep Randhawa and Kaytlyn Tasalloti for assistance with the isolation of bones, and the Animal Care staff at Simon Fraser University for maintaining the animals. We thank Guobin Sun, Jonathan Villareal and Nancy Ford at the Centre for High-Throughput Phenogenomics at the University of British Columbia for performing the micro-CT scans. The Centre for High-Throughput Phenogenomics is supported by the Canada Foundation for Innovation, British Columbia Knowledge Development Foundation, and the UBC Faculty of Dentistry.
Data Availability
All relevant data are within the paper and its S1 File and S1–S14 Figs files.
Funding Statement
This study was funded by a Natural Sciences and Engineering Research Council of Canada Discovery Grant (JKC; grant number RGPIN-2016-04047) and an NSERC Undergraduate Student Research Award (NB). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Kovacs CS. The Skeleton Is a Storehouse of Mineral That Is Plundered During Lactation and (Fully?) Replenished Afterwards. J Bone Miner Res. 2017;32: 676–680. doi: 10.1002/jbmr.3090 [DOI] [PubMed] [Google Scholar]
- 2.Liu XS, Wang L, de Bakker CMJ, Lai X. Mechanical Regulation of the Maternal Skeleton during Reproduction and Lactation. Curr Osteoporos Rep. 2019;17: 375–386. doi: 10.1007/s11914-019-00555-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prior JC. Perimenopause: the complex endocrinology of the menopausal transition. Endocr Rev. 1998;19: 397–428. doi: 10.1210/edrv.19.4.0341 [DOI] [PubMed] [Google Scholar]
- 4.Kovacs CS. Maternal Mineral and Bone Metabolism During Pregnancy, Lactation, and Post-Weaning Recovery. Physiol Rev. 2016;96: 449–547. doi: 10.1152/physrev.00027.2015 [DOI] [PubMed] [Google Scholar]
- 5.Grizzo FMF, Alarcão ACJ, Dell’ Agnolo CM, Pedroso RB, Santos TS, Vissoci JRN, et al. How does women’s bone health recover after lactation? A systematic review and meta-analysis. Osteoporos Int. 2020;31: 413–427. doi: 10.1007/s00198-019-05236-8 [DOI] [PubMed] [Google Scholar]
- 6.Winter EM, Ireland A, Butterfield NC, Haffner-Luntzer M, Horcajada MN, Veldhuis-Vlug AG, et al. Pregnancy and lactation, a challenge for the skeleton. Endocr Connect. 2020;9: R143–R157. doi: 10.1530/EC-20-0055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sahin Ersoy G, Giray B, Subas S, Simsek E, Sakin O, Turhan OT, et al. Interpregnancy interval as a risk factor for postmenopausal osteoporosis. Maturitas. 2015;82: 236–240. doi: 10.1016/j.maturitas.2015.07.014 [DOI] [PubMed] [Google Scholar]
- 8.Okyay DO, Okyay E, Dogan E, Kurtulmus S, Acet F, Taner CE. Prolonged breast-feeding is an independent risk factor for postmenopausal osteoporosis. Maturitas. 2013;74: 270–275. doi: 10.1016/j.maturitas.2012.12.014 [DOI] [PubMed] [Google Scholar]
- 9.Schnatz PF, Barker KG, Marakovits K a, O’Sullivan DM. Effects of age at first pregnancy and breast-feeding on the development of postmenopausal osteoporosis. Menopause. 2010;17: 1161–6. doi: 10.1097/gme.0b013e3181e0efb3 [DOI] [PubMed] [Google Scholar]
- 10.Yun BH, Choi YR, Choi YS, Cho S, Lee BS, Seo SK. Age at First Delivery and Osteoporosis Risk in Korean Postmenopausal Women: The 2008–2011 Korea National Health and Nutrition Examination Survey (KNHANES). PLoS One. 2015;10: e0123665. doi: 10.1371/journal.pone.0123665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cho GJ, Shin JH, Yi KW, Park HT, Kim T, Hur JY, et al. Adolescent pregnancy is associated with osteoporosis in postmenopausal women. Menopause. 2012;19: 456–460. doi: 10.1097/gme.0b013e3182337150 [DOI] [PubMed] [Google Scholar]
- 12.Cavkaytar S, Seval MM, Atak Z, Findik RB, Ture S, Kokanali D. Effect of reproductive history, lactation, first pregnancy age and dietary habits on bone mineral density in natural postmenopausal women. Aging Clin Exp Res. 2015;27: 689–694. doi: 10.1007/s40520-015-0333-4 [DOI] [PubMed] [Google Scholar]
- 13.Madimenos FC, Snodgrass JJ, Liebert MA, Cepon TJ, Sugiyama LS. Reproductive effects on skeletal health in Shuar women of Amazonian Ecuador: A life history perspective. Am J Hum Biol. 2012;24: 841–852. doi: 10.1002/ajhb.22329 [DOI] [PubMed] [Google Scholar]
- 14.Chantry CJ, Auinger P, Byrd RS, HJ K, MH L, Pediatrics AA et al. Lactation among adolescent mothers and subsequent bone mineral density. Arch Pediatr Adolesc Med. 2004;158: 650. doi: 10.1001/archpedi.158.7.650 [DOI] [PubMed] [Google Scholar]
- 15.Hopkinson JM, Butte NF, Ellis K, Smith EO. Lactation delays postpartum bone mineral accretion and temporarily alters its regional distribution in women. J Nutr. 2000;130: 777–783. doi: 10.1093/jn/130.4.777 [DOI] [PubMed] [Google Scholar]
- 16.Berger C, Langsetmo L, Joseph L, Hanley DA, Davison KS, Josse R, et al. Change in bone mineral density as a function of age in women and men and association with the use of antiresorptive agents. C Can Med Assoc J. 2008;178: 1660–1668. doi: 10.1503/cmaj.071416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.MacDonald HM, Nishiyama KK, Kang J, Hanley DA, Boyd SK. Age-related patterns of trabecular and cortical bone loss differ between sexes and skeletal sites: A population-based HR-pQCT study. J Bone Miner Res. 2011;26: 50–62. doi: 10.1002/jbmr.171 [DOI] [PubMed] [Google Scholar]
- 18.Riggs BL, Melton LJ, Robb RA, Camp JJ, Atkinson EJ, McDaniel L, et al. A Population-Based Assessment of Rates of Bone Loss at Multiple Skeletal Sites: Evidence for Substantial Trabecular Bone Loss in Young Adult Women and Men. J Bone Miner Res. 2007;23: 205–214. doi: 10.1359/jbmr.071020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Runolfsdottir HL, Sigurdsson G, Franzson L, Indridason OS. Gender comparison of factors associated with age-related differences in bone mineral density. Arch Osteoporos. 2015;10: 214. doi: 10.1007/s11657-015-0214-7 [DOI] [PubMed] [Google Scholar]
- 20.Esencan E, Simsek B, Seli E. Analysis of female demographics in the United States: life expectancy, education, employment, family building decisions, and fertility service utilization. Curr Opin Obstet Gynecol. 2021;33: 170–177. doi: 10.1097/GCO.0000000000000704 [DOI] [PubMed] [Google Scholar]
- 21.Govoni KE, Baylink DJ, Mohan S. The multi-functional role of insulin-like growth factor binding proteins in bone. Pediatr Nephrol. 2005;20: 261–268. doi: 10.1007/s00467-004-1658-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohan S, Richman C, Guo RQ, Amaar Y, Donahue LR, Wergedal J, et al. Insulin-like growth factor regulates peak bone mineral density in mice by both growth hormone-dependent and -independent mechanisms. Endocrinology. 2003;144: 929–936. doi: 10.1210/en.2002-220948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yakar S, Isaksson O. Regulation of skeletal growth and mineral acquisition by the GH/IGF-1 axis: Lessons from mouse models. Growth Horm IGF Res. 2016;28: 26–42. doi: 10.1016/j.ghir.2015.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mukherjee A, Rotwein P. Insulin-like growth factor binding protein-5 in osteogenesis: Facilitator or inhibitor? Growth Horm IGF Res. 2007;17: 179–185. doi: 10.1016/j.ghir.2007.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salih DAM, Mohan S, Kasukawa Y, Tripathi G, Lovett FA, Anderson NF, et al. Insulin-like growth factor-binding protein-5 induces a gender-related decrease in bone mineral density in transgenic mice. Endocrinology. 2005;146: 931–940. doi: 10.1210/en.2004-0816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andress DL. IGF-binding protein-5 stimulates osteoblast activity and bone accretion in ovariectomized mice. Am J Physiol Metab. 2001;281: E283–E288. doi: 10.1152/ajpendo.2001.281.2.E283 [DOI] [PubMed] [Google Scholar]
- 27.Devlin RD, Du Z, Buccilli V, Jorgetti V, Canalis E. Transgenic mice overexpressing insulin-like growth factor binding protein-5 display transiently decreased osteoblastic function and osteopenia. Endocrinology. 2002;143: 3955–3962. doi: 10.1210/en.2002-220129 [DOI] [PubMed] [Google Scholar]
- 28.Mohan S, Baylink DJ. IGF-binding proteins are multifunctional and act via IGF-dependent and -independent mechanisms. J Endocrinol. 2002;175: 19–31. doi: 10.1677/joe.0.1750019 [DOI] [PubMed] [Google Scholar]
- 29.Miyakoshi N, Richman C, Kasukawa Y, Linkhart TA, Baylink DJ, Mohan S. Evidence that IGF-binding protein-5 functions as a growth factor. J Clin Invest. 2001;107: 73–81. doi: 10.1172/JCI10459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Overgaard MT, Boldt HB, Laursen LS, Sottrup-Jensen L, Conover CA, Oxvig C. Pregnancy-associated plasma protein-A2 (PAPP-A2), a novel insulin-like growth factor-binding protein-5 proteinase. J Biol Chem. 2001;276: 21849–21853. doi: 10.1074/jbc.M102191200 [DOI] [PubMed] [Google Scholar]
- 31.Bunn RC, Fowlkes JL. Insulin-like growth factor binding protein proteolysis. Trends Endocrinol Metab. 2003;14: 176–181. doi: 10.1016/s1043-2760(03)00049-3 [DOI] [PubMed] [Google Scholar]
- 32.Frystyk J, Teran E, Gude MF, Bjerre M, Hjortebjerg R. Pregnancy-associated plasma proteins and Stanniocalcin-2 –Novel players controlling IGF-I physiology. Growth Horm IGF Res. 2020;53–54: 101330. doi: 10.1016/j.ghir.2020.101330 [DOI] [PubMed] [Google Scholar]
- 33.Fujimoto M, Khoury JC, Khoury PR, Kalra B, Kumar A, Sluss P, et al. Anthropometric and biochemical correlates of PAPP-A2, free IGF-I, and IGFBP-3 in childhood. Eur J Endocrinol. 2020;182: 363–374. doi: 10.1530/EJE-19-0859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dauber A, Munoz-Calvo MT, Barrios V, Domene HM, Kloverpris S, Serra-Juhe C, et al. Mutations in pregnancy-associated plasma protein A2 cause short stature due to low IGF-I availability. EMBO Mol Med. 2016;8: 363–374. doi: 10.15252/emmm.201506106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Argente J, Pérez-Jurado LA. History and clinical implications of PAPP-A2 in human growth: When reflecting on idiopathic short stature leads to a specific and new diagnosis. Growth Horm IGF Res. 2018;40: 17–19. doi: 10.1016/j.ghir.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 36.Cabrera-Salcedo C, Mizuno T, Tyzinski L, Andrew M, Vinks AA, Frystyk J, et al. Pharmacokinetics of IGF-1 in PAPP-A2-Deficient Patients, Growth Response, and Effects on Glucose and Bone Density. J Clin Endocrinol Metab. 2017;102: 4568–4577. doi: 10.1210/jc.2017-01411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Muñoz-Calvo MT, Barrios V, Pozo J, Chowen JA, Martos-Moreno GÁ, Hawkins F, et al. Treatment with recombinant human insulin-like growth factor-1 improves growth in patients with PAPP-A2 deficiency. J Clin Endocrinol Metab. 2016;101: 3879–3883. doi: 10.1210/jc.2016-2751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hawkins-Carranza FG, Muñoz-Calvo MT, Martos-Moreno G, Allo-Miguel G, Del Río L, Pozo J, et al. rhIGF-1 Treatment Increases Bone Mineral Density and Trabecular Bone Structure in Children with PAPP-A2 Deficiency. Horm Res Paediatr. 2018;89: 200–204. doi: 10.1159/000486336 [DOI] [PubMed] [Google Scholar]
- 39.Conover CA, Boldt HB, Bale LK, Clifton KB, Grell JA, Mader JR, et al. Pregnancy-Associated Plasma Protein-A2 (PAPP-A2): Tissue Expression and Biological Consequences of Gene Knockout in Mice. Endocrinology. 2011;152: 2837–2844. doi: 10.1210/en.2011-0036 [DOI] [PubMed] [Google Scholar]
- 40.Christians JK, de Zwaan DR, Fung SHY. Pregnancy Associated Plasma Protein A2 (PAPP-A2) affects bone size and shape and contributes to natural variation in postnatal growth in mice. PLoS One. 2013;8: e56260. doi: 10.1371/journal.pone.0056260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Amiri N, Christians JK. PAPP-A2 expression by osteoblasts is required for normal postnatal growth in mice. Growth Horm IGF Res. 2015;25: 274–80. doi: 10.1016/j.ghir.2015.09.003 [DOI] [PubMed] [Google Scholar]
- 42.Christians JK, Amiri N, Schipilow JD, Zhang SW, May-Rashke KI. Pappa2 deletion has sex- and age-specific effects on bone in mice. Growth Horm IGF Res. 2019;44: 6–10. doi: 10.1016/j.ghir.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 43.Rubio L, Vargas A, Rivera P, López-Gambero AJ, Tovar R, Christians JK, et al. Recombinant IGF-1 induces sex-specific changes in bone composition and remodeling in adult mice with Pappa2 deficiency. Int J Mol Sci. 2021;22: 4048. doi: 10.3390/ijms22084048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Christians JK, Bath AK, Amiri N. Pappa2 deletion alters IGFBPs but has little effect on glucose disposal or adiposity. Growth Horm IGF Res. 2015;25: 232–239. doi: 10.1016/j.ghir.2015.07.001 [DOI] [PubMed] [Google Scholar]
- 45.Beamer WG, Donahue LR, Rosen CJ, Baylink DJ. Genetic variability in adult bone density among inbred strains of mice. Bone. 1996;18: 397–403. doi: 10.1016/8756-3282(96)00047-6 [DOI] [PubMed] [Google Scholar]
- 46.Glatt V, Canalis E, Stadmeyer L, Bouxsein ML. Age-Related Changes in Trabecular Architecture Differ in Female and Male C57BL/6J Mice. J Bone Miner Res. 2007;22: 1197–1207. doi: 10.1359/jbmr.070507 [DOI] [PubMed] [Google Scholar]
- 47.Bornstein S, Brown SA, Le PT, Wang X, DeMambro V, Horowitz MC, et al. FGF-21 and Skeletal Remodeling During and After Lactation in C57BL/6J Mice. Endocrinology. 2014;155: 3516–3526. doi: 10.1210/en.2014-1083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Liu XS, Ardeshirpour L, VanHouten JN, Shane E, Wysolmerski JJ. Site-Specific Changes in Bone Microarchitecture, Mineralization, and Stiffness During Lactation and After Weaning in Mice. J Bone Miner Res. 2012;27: 865–875. doi: 10.1002/jbmr.1503 [DOI] [PubMed] [Google Scholar]
- 49.Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Mueller R. Guidelines for Assessment of Bone Microstructure in Rodents Using Micro-Computed Tomography. J Bone Miner Res. 2010;25: 1468–1486. doi: 10.1002/jbmr.141 [DOI] [PubMed] [Google Scholar]
- 50.de Bakker CMJ, Tseng WJ, Li Y, Zhao H, Altman-Singles AR, Jeong Y, et al. Reproduction Differentially Affects Trabecular Bone Depending on Its Mechanical Versus Metabolic Role. J Biomech Eng. 2017;139: 111006. doi: 10.1115/1.4038110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Bakker CMJ, Altman-Singles AR, Li Y, Tseng WJ, Li C, Liu XS. Adaptations in the Microarchitecture and Load Distribution of Maternal Cortical and Trabecular Bone in Response to Multiple Reproductive Cycles in Rats. J Bone Miner Res. 2017;32: 1014–1026. doi: 10.1002/jbmr.3084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vajda EG, Bowman BM, Miller SC. Cancellous and Cortical Bone Mechanical Properties and Tissue Dynamics During Pregnancy, Lactation, and Postlactation in the Rat. Biol Reprod. 2001;65: 689–695. doi: 10.1095/biolreprod65.3.689 [DOI] [PubMed] [Google Scholar]
- 53.Ross RD, Meagher MJ, Sumner DR. Calcium restriction during lactation has minimal effects on post-weaning mineral metabolism and bone recovery. J Bone Miner Metab. 2019;37: 648–657. doi: 10.1007/s00774-018-0969-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ardeshirpour L, Dann P, Adams DJ, Nelson T, VanHouten J, Horowitz MC, et al. Weaning Triggers a Decrease in Receptor Activator of Nuclear Factor-κB Ligand Expression, Widespread Osteoclast Apoptosis, and Rapid Recovery of Bone Mass after Lactation in Mice. Endocrinology. 2007;148: 3875–3886. doi: 10.1210/en.2006-1467 [DOI] [PubMed] [Google Scholar]
- 55.Fujimoto M, Andrew M, Liao L, Zhang D, Yildirim G, Sluss P, et al. Low IGF-I bioavailability impairs growth and glucose metabolism in a mouse model of human PAPPA2 p.ALA1033Val mutation. Endocrinology. 2019;160: 1363–1376. doi: 10.1210/en.2018-00755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lau KHW, Baylink DJ, Sheng MHC. Osteocyte-derived insulin-like growth factor I is not essential for the bone repletion response in mice. PLoS One. 2015;10: e0115897. doi: 10.1371/journal.pone.0115897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ó Breasail M, Prentice A, Ward K. Pregnancy-Related Bone Mineral and Microarchitecture Changes in Women Aged 30 to 45 Years. J Bone Miner Res. 2020;35: 1253–1262. doi: 10.1002/jbmr.3998 [DOI] [PMC free article] [PubMed] [Google Scholar]