Abstract
Background:
Premature ovarian insufficiency may impair the quality of life and expose women to disorders such as cardiovascular disease, osteoporosis, and depression. This study aimed to evaluate the effect of mindfulness on the quality of life in women with premature ovarian insufficiency.
Methods:
This study involved 62 women who were randomly allocated into two groups of mindfulness and control. The mindfulness group received eight sessions of training. A demographic questionnaire, menopause-specific quality of life and a checklist (for assessing hot flashes) were used to collect the data. The quality of life, frequency, and intensity of hot flashes were measured before the intervention, immediately, and 3 months after it. Independent t-test, the Chi-square test, and the repeated measure test were used for data analysis.
Results:
The scores of quality of life dropped from 95.6 ± 9.77 at baseline to 77.32 ± 7.93 after intervention and 48.32 ± 4.96 at 3-months follow-up in the mindfulness group but rose from 99.5 ± 16.1 at baseline to 100.2 ± 15.33 after intervention, and 102.6 ± 14.9 3-months after it in the control group, P < 0.001. The scores of vasomotor, psychological, physical, and sexual domains also improved significantly in the mindfulness group compared to the control group. The mean of hot flashes in the mindfulness group was 1.30 ± 0.69 and decreased to 1.1 ± 0.56 and 0.66 ± 0.58 immediately and in 3 months after intervention, respectively. The frequency of hot flashes was 14.74 ± 10.4 per week before intervention in the mindfulness group which reduced to 12.38 ± 8.66 and 6.74 ± 6.34 per week, immediately and 3 months after the intervention, while in the control group, there was an increase in the frequency of hot flashes (P < 0.0001).
Conclusion:
According to the results of this study, mindfulness could improve quality of life and reduce hot flashes, so mindfulness training for women with premature ovarian insufficiency is strongly recommended.
Keywords: Mindfulness, premature ovarian insufficiency, quality of life
INTRODUCTION
Premature ovarian insufficiency is defined as the permanent cessation of menstruation before the age of 40. It affects around 1% of women worldwide.[1] This condition may be spontaneous or induced. The cause of premature spontaneous ovarian insufficiency is often genetic and related to premature ovarian failure.[2] However may also happen after chemotherapy or surgical removal of ovaries.[3]
Regardless of the causes, women with premature ovarian insufficiency are at a greater risk of cardiovascular diseases, neurological and psychiatric disorders, osteoporosis, and overall higher morbidity and mortality.[4] In general, the symptoms that women with premature ovarian insufficiency experience are the same as those of women with natural menopause.[5] These women may have menstrual abnormalities such as amenorrhea, infertility, along with some menopause symptoms such as hot flashes, vaginal dryness, sexual problem, anxiety, and depression.[6] Changes in the level of hormones, hot flashes, and sleep disturbances may affect the quality of life in women.[7]
Benetti-Pinto et al. found significantly low score in some domains of quality of life among women with premature ovarian insufficiency.[8] Ganz et al. also found that women with premature ovarian insufficiency were more likely to have a lower score of a psycho-social domain of quality of life in comparison to women with natural menopause.[9] Menopausal problems are more severe among younger women or those experiencing premature ovarian insufficiency following chemotherapy.[10]
Hormone replacement therapy (HRT) including estrogen and progesterone is recommended for women with premature ovarian insufficiency. HRT is recommended for the prevention of both short-term and long-term menopausal problems such as hot flashes, vaginal dryness, osteoporosis, and cardiovascular disease.[11]
Although recommended for women with premature ovarian insufficiency, HRT cannot eliminate all menopausal problems.[4] In fact, HRT is not regarded as a treatment for menopausal problems, and some women prefer to use complementary and alternative medicine for their menopausal problems.[12]
Mindfulness is one of the methods in psychotherapy in which clients learn to have self-control, more flexibility, concentration, and acceptance.[13] According to Wong et al. mindfulness-based stress reduction (MBSR) could significantly improve anxiety and depression in postmenopausal women.[14] Enjezab et al. also considered mindfulness-based cognitive therapy an effective treatment for improving the quality of life in perimenopausal women.[15]
Despite a number of studies on the effect of mindfulness on menopausal problems, there is a lack of sufficient information regarding the effect of this method on premature ovarian insufficiency. Therefore, this study was conducted to evaluate the effect of mindfulness on the quality of life in women with premature ovarian insufficiency.
METHODS
Sixty-two women with premature ovarian insufficiency were recruited and randomly allocated into two groups of intervention and control in this randomized controlled trial. This study started in March 2019 and was completed in August 2019. The protocol of the study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref No: IRAJUMS.REC.1398.098). All participants provided written informed consent before data collection.
Setting
The phone number of women with premature ovarian insufficiency was found from two major hospitals (Imam Khomeini and Amir al-Mu'minin) and three public health centers were collected. Then, one of the researchers (FP) made a phone call to them and they requested to attend the postmenopausal clinic in Imam Khomeini hospital.
We calculated the necessary sample size based on our main primary outcome measure, with an expected 15 units increase in the mean score of quality of life in women with premature ovarian insufficiency. These calculations were based on previous study.[15] To detect this difference with 85% power, type 1 error of 5% and S = 18.65, 28 women for whom data could be analyzed were needed in each group.
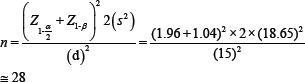
With an assumption of 10% withdrawals or protocol violations, we aimed to recruit 31 women in each group.
Women with the following criteria were recruited: women with premature ovarian insufficiency (before age of 40 years) due to any reason (including chemotherapy, surgery, or natural menopause), basic literacy, at least 1 year passing from their last menstruation or having follicle-stimulating hormone >40 IU, and obtaining a moderate or low score from the quality of life questionnaire. Women who had depression, or were doing extreme physical activity, or had received HRT were excluded from the study.
Measurements
A demographic questionnaire, the menopause-specific quality of life (MENQOL) and a checklist were used to collect data. The demographic questionnaire includes age, age of menopause, menopause duration, age of marriage, marital status, economic status, number of children, level of education of women and that of their husbands, age of their husbands, the job of women and that of their husbands, mode of delivery, body mass index, and the number and severity of hot flashes.
The MENQOL consists of 27 questions in four domains, namely vasomotor, psychosocial, physical, and sexual. Each question scored from one to six, with one indicating no problem and six indicating very severe problems. Lower scores indicated the good quality of life. Women were requested to complete the MENQOL before an 8-session intervention, and immediately and 3 months after. This questionnaire was designed by Hilditch et al. in Canada[16] and validated in Iran by Ghazanfarpour et al. in 2015.[17]
A checklist was designed for recording the number and severity of hot flashes. Women were requested to mark the checklist in case they had hot flashes, and for the severity of hot flashes, they were asked to choose one of the categories that matched best their situation as follows: If women just felt hot without sweating, it was considered mild. If they felt hot with sweating, it was considered moderate, and if they felt hot with sweating that interfered with their daily activities, it was considered an example of severe hot flashes. The validity of the demographic questionnaire and the checklist were assessed by consensual validity (by five faculty members).
Randomisation
Eligible women were randomly assigned into two groups of mindfulness or control, using blocked randomization with randomly selected block sizes and the ratio of 1:1. Due to the nature of this study, blinding of researchers and participants was not possible. Therefore, to avoid selection bias, random block sizes were used. After randomization, codes allocated to each participant were kept by the secretary of the counseling clinic for preserving allocation concealment. Therefore, neither the participant nor the researcher was aware of the allocation order until the commencement of the intervention.
Intervention
Women in the mindfulness group received eight sessions of mindfulness training targeting quality of life (1 session per week). Women in the mindfulness group were divided into two groups of 10 and one group of 11. Each group received eight 90-min sessions. In the first session, they received information about menopause, menopause consequences, how to dealing with complications of menopause, how to explore the body, mindful eating, and mindful sitting.
In the second session, they received information about awareness, being present, observing or witnessing, the power of breathing, putting aside behavioral habits (reducing fatigue and improving vitality), paying attention without judgment, direct experiences of physical emotions and inner experiences, and awareness of daily activities.
In the third session, they received counseling about paying attention, not being judgmental, identifying behavioral patterns, self-reflection and observation, and not being reactive. In the fourth session, participants received counseling about acceptance, direct experiences of external events and experiences, goals and objectives, values, obstacles, and obligations. In the fifth session, participants received information about stress, getting involved in stressful reactions, answering instead of reacting, dealing with physical and emotional symptoms, and sleeping without stress.
The sixth session, involved nonsexual communication, communication with oneself, communication with others, beliefs and feelings about menopause, sexual intercourse, psychological differences between men and women, and couples' sexual beliefs. In the seventh session, the participants learned about sexual intercourse, and received sexual literacy that includes the genital tract anatomy, the sexual reaction cycle, sexual stimuli, and gender differences, intercourse, three stages of sexual intercourse, and common sexual problems. Finally, the 8th session was the wrap-up of the previous sessions. In each session, participants did the exercise with the researcher and had to practice at home. Women in the control group received routine care. It is worth mentioning that routine care for premature ovarian insufficiency may include HRT, but only few women in Iran are willing to undergo this treatment, and we excluded women receiving hormone therapy in this study. To abide by ethical considerations, women in the control group received a compact disk on mindfulness at the end of the study.
Statistics
All data were analyzed by IBM SPSS Statistics for Windows, Armonk, NY: IBM Corp, using the Shapiro-Wilk test to check the normal distribution of data. Independent t-test was used to compare means of two groups regarding continuous data, and Chi-square test was used to compare categorical data. For data with more than two measurements, the repeated measure test was used. P <0.05 was considered statistically significant.
RESULTS
In this study, 62 women were recruited and none of them dropped out [Figure 1]. The demographic characteristics of the participants in the two groups are illustrated in Table 1. As evident in this table, the two groups of mindfulness and control did not show any significant difference regarding age, number of children, number of pregnancies, age of marriage, age of their husbands, and duration of menopause. Most of the women in the two groups had high school diploma and were married and employees with a moderate economic status.
Figure 1.
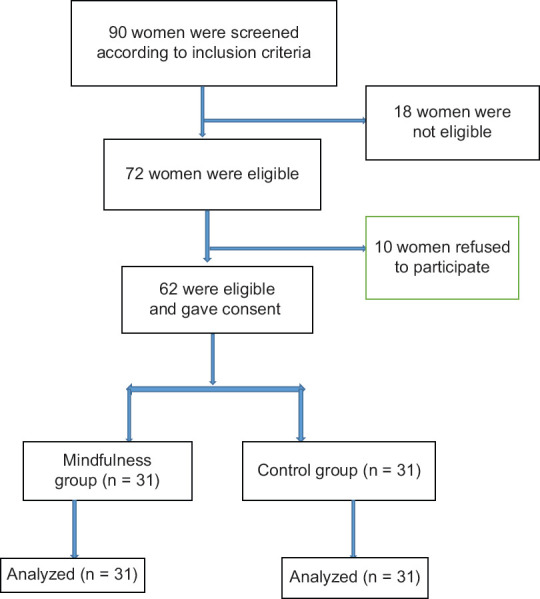
Flow diagram of recruitment and retention of participants in the study
Table 1.
Demographic characteristics of participants in the mindfulness and control groups
| Variables | Mean±SD | |
|---|---|---|
|
| ||
| Mindfulness (n=31) | Control (n=31) | |
| Age (years) | 41.1±3.28 | 41.8±3.2 |
| Number of children | 2.77±1.49 | 2.35±1.47 |
| Number of pregnancies | 3.3±1.93 | 2.35±1.47 |
| Age of marriage (years) | 19.8±3.8 | 18.7±4.3 |
| Age of husband (years) | 46.3±4.39 | 46.57±5.6 |
| Duration of menopause (years) | 5.03±3.21 | 4.93±2.67 |
| BMI (kg/m2) | 29.5±3.44 | 27.9±3.68 |
| Age of menopause (years) | 36.3±2.02 | 36.8±1.99 |
| Occupation, n (%) | ||
| House maker | 10 (32.3) | 10 (32.3) |
| Employee | 21 (67.7) | 21 (67.7) |
| Education, n (%) | ||
| Primary | 10 (32.3) | 10 (32.3) |
| Diploma | 15 (48.4) | 14 (45.2) |
| University education | 6 (19.4) | 7 (22.6) |
| Economic status, n (%) | ||
| Good | 6 (19.4) | 3 (9.7) |
| Moderate | 19 (61.3) | 20 (64.5) |
| Weak | 6 (19.4) | 8 (25.8) |
| Marital status, n (%) | ||
| Single | 5 (16.1) | 5 (16.1) |
| Married | 25 (80.6) | 25 (80.6) |
| Widow | 1 (3.2) | 1 (3.2) |
| Occupation of husband, n (%) | ||
| Employee | 23 (88.5) | 23 (88.5) |
| Not employed | 2 (7.7) | 3 (11.5) |
| Retired | 1 (3.8) | 0 |
SD: Standard deviation, BMI: Body mass index
Table 2 shows the domains of quality of life before the intervention, and immediately and 3 months after in two groups of mindfulness and control. As can be seen from this table, the quality of life was not different between the two groups before the intervention. However, the score of quality of life improved significantly immediately and 3 months after intervention in the mindfulness group compared to the control group (dropped from 95.6 ± 9.77 at baseline to 77.32 ± 7.93 after intervention and 48.32 ± 4.96 3 months after it in the mindfulness group but rose from 99.5 ± 16.1 at baseline to 100.2 ± 15.33 after intervention and 102.6 ± 14.9 3 months after it in the control group, P < 0.001). The scores of vasomotor, psychological, physical, and sexual domains also improved significantly in the mindfulness group compared to the control group. Although the scores of these domains also changed in the control group, the changes were in the negative direction.
Table 2.
Mean of quality of life domains in two groups of mindfulness and control
| Variables | Mean±SD | P | P* | ||
|---|---|---|---|---|---|
|
| |||||
| Before intervention | After intervention | Three months follow-up | |||
| Quality of life | |||||
| Mindfulness (n=31) | 95.6±9.77 | 77.32±7.93 | 48.32±4.96 | <0.0001 | <0.0001 |
| Control (n=31) | 99.5±16.1 | 100.2±15.33 | 102.6±14.9 | <0.0001 | |
| P | 0.25 | <0.0001 | <0.0001 | ||
| Vasomotor | |||||
| Mindfulness (n=31) | 7.96±3.45 | 6.58±2.5 | 4.61±1.49 | <0.0001 | <0.0001 |
| Control (n=31) | 9.67±3.9 | 9.58±3.87 | 9.67±3.95 | 0.04 | |
| P | 0.081 | 0.001 | <0.0001 | ||
| Psychological | |||||
| Mindfulness (n=31) | 26.5±5.15 | 20.5±3.69 | 11.32±1.79 | <0.0001 | <0.0001 |
| Control (n=31) | 28.3±5.6 | 28.7±5.27 | 29.4±5.16 | <0.0001 | |
| P | 0.18 | <0.0001 | <0.0001 | ||
| Physical | |||||
| Mindfulness (n=31) | 54.09±5.7 | 44.2±4.75 | 29±2.56 | <0.0001 | <0.0001 |
| Control (n=31) | 53.09±10.33 | 53.9±9.6 | 55.06±9.4 | <0.0001 | |
| P | 0.64 | <0.0001 | <0.0001 | ||
| Sexual | |||||
| Mindfulness (n=31) | 7.45±3.12 | 5.93±2.36 | 3.22±1.3 | <0.0001 | <0.0001 |
| Control (n=31) | 8.22±3.44 | 7.87±3.3 | 8.06±3.4 | 0.06 | |
| P | 0.17 | 0.002 | <0.0001 | ||
*P value was calculated using repeated measure test. SD: Standard deviation
Table 3 shows the frequency and severity of hot flashes in two groups of mindfulness and control before the intervention, and immediately and 3 months after it. The mean severity of hot flashes in the mindfulness group was 1.30 ± 0.69 at the baseline, which decreased to 1.1 ± 0.56 after intervention and 0.66 ± 0.58 3-months thereafter. These changes were significantly more than those in the control group (P < 0.0001). The frequency of hot flashes was 14.74 ± 10.4 per week before intervention in the mindfulness which reduced to 12.38 ± 8.66 and 6.74 ± 6.34 per week, immediately and 3 months after intervention, respectively, while in the control group the frequency of hot flashes was increased (P < 0.0001).
Table 3.
Frequency and severity of hot flashes in two groups of mindfulness and control
| Variables | Mean±SD | P | |
|---|---|---|---|
|
| |||
| Mindfulness (n=31) | Control (n=31) | ||
| Severity of hot flashes (per week) | |||
| Before | 1.30±0.69 | 1.32±0.63 | 0.88 |
| After | 1.1±0.56 | 1.34±0.63 | 0.004 |
| 3 months later | 0.66±0.58 | 1.4±0.65 | <0.0001 |
| Frequency of hot flashes per week | |||
| Before | 14.74±10.4 | 20.96 | 0.01 |
| After | 12.38±8.66 | 2.9±13.37 | 0.001 |
| 3 months later | 6.74±6.34 | 23.4±13.9 | <0.0001 |
SD: Standard deviation
DISCUSSION
This study was conducted to evaluate the effect of mindfulness on the quality of life of women with premature ovarian insufficiency. The results of this study showed that immediately and 3 months after the intervention, the total score of quality of life and its domains including vasomotor, psychological, physical, and sexual improved significantly in the mindfulness group in comparison to the control group. Although we could not find any study on the effect of mindfulness on quality of life in women with premature ovarian insufficiency, there were some studies addressing the effect of mindfulness on menopausal symptoms in peri or postmenopausal period. Sood et al. for example in their study on 1744 women aged 40–65 found that women with higher mindfulness scores had significantly lower scores of stress and menopausal symptoms.[18] Another study was conducted by Garcia et al. on 60 postmenopausal women who were randomly allocated into two groups of mindfulness and relaxation training and one control group. They found that 8 weeks of training could significantly improve the sleep quality and quality of life and reduce the vasomotor symptoms.[19] The results of Sood et al. and Garcia et al. are consistent with our results.
In the present study, the frequency and severity of hot flashes in the mindfulness group decreased immediately and 3 months after intervention in comparison with the control group. In their study on 110 peri and postmenopausal women postmenopausal women with >5 moderate-to-severe hot flashes per day Carmody et al. found that MBSR could significantly reduce the frequency of hot flashes and improved the quality of life immediately and 3 months after intervention.[20] Our results regarding the quality of life and frequency of hot flashes are similar to those of Kumari et al. Menopause is associated with a number of physical, psychological, and social changes that affect the quality of life.[21]
Although the precise statistics on premature ovarian insufficiency are not available in Iran, only a small number of women with premature ovarian insufficiency undergo HRT. Therefore, using nonhormonal treatments such as mindfulness can help to reduce menopausal problems and improve the quality of life.
Strengths and limitations of the study
This was randomized controlled trial with rigorous 8 weeks of mindfulness training and 12 weeks of follow-up. Despite its strengths, this study also has some weaknesses. First, women in mindfulness did not get counseling according to their level of education. Although we selected the participants from two hospitals and some public health centers, we did not select them randomly and this may affect the generalizability of the study (participants were randomly allocated into two groups).
CONCLUSION
The results of this study showed that 8 weeks of mindfulness training could significantly improve the quality of life and reduce the frequency and intensity of hot flashes in women with premature ovarian insufficiency. Therefore, mindfulness training for women with premature ovarian insufficiency is strongly recommended.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This was a Master thesis of FP. All expenses of this research were provided by Ahvaz Jundishapur University of Medical Sciences.
REFERENCES
- 1.Okeke T, Anyaehie U, Ezenyeaku C. Premature menopause. Ann Med Health Sci Res. 2013;3:90–5. doi: 10.4103/2141-9248.109458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luborsky JL, Meyer P, Sowers MF, Gold EB, Santoro N. Premature menopause in a multi-ethnic population study of the menopause transition. Hum Reprod. 2003;18:199–206. doi: 10.1093/humrep/deg005. [DOI] [PubMed] [Google Scholar]
- 3.Ikeme A, Okeke TC, Akogu S, Chinwuba N. Knowledge and perception of menopause and climacteric symptoms among a population of women in Enugu, South East, Nigeria. Ann Med Health Sci Res. 2011;1:31–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA. Premature menopause or early menopause: Long-term health consequences. Maturitas. 2010;65:161–6. doi: 10.1016/j.maturitas.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torrealday S, Pal L. Premature menopause. Endocrinol Metab Clin North Am. 2015;44:543–57. doi: 10.1016/j.ecl.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 6.Torrealday S, Kodaman P, Pal L. Premature ovarian insufficiency – An update on recent advances in understanding and management. F1000Res. 2017;6:2069. doi: 10.12688/f1000research.11948.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taffe JR, Dennerstein L. Menstrual patterns leading to the final menstrual period. Menopause. 2002;9:32. doi: 10.1097/00042192-200201000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Benetti-Pinto CL, de Almeida DM, Makuch MY. Quality of life in women with premature ovarian failure. Gynecol Endocrinol. 2011;27:645–9. doi: 10.3109/09513590.2010.520374. [DOI] [PubMed] [Google Scholar]
- 9.Ganz PA, Greendale GA, Petersen L, Kahn B, Bower JE. Breast cancer in younger women: reproductive and late health effects of treatment. J Clin Oncol. 2003;21:4184–93. doi: 10.1200/JCO.2003.04.196. [DOI] [PubMed] [Google Scholar]
- 10.Alder J, Zanetti R, Wight E, Urech C, Fink N, Bitzer J. Sexual dysfunction after premenopausal stage I and II breast cancer: do androgens play a role? J Sex Med. 2008;5:1898–906. doi: 10.1111/j.1743-6109.2008.00893.x. [DOI] [PubMed] [Google Scholar]
- 11.Pines A, Sturdee DW, Birkhauser MH, Schneider HPG, Gambacciani M, Panay N. IMS updated recommendations on postmenopausal hormone therapy. Climacteric. 2007;10:181–94. doi: 10.1080/13697130701361657. [DOI] [PubMed] [Google Scholar]
- 12.Johnson A, Roberts L, Elkins G. Complementary and Alternative Medicine for Menopause. J Evid Based Integr Med. 2019;24:2515690X19829380. doi: 10.1177/2515690X19829380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Davis DM, Hayes JA. What are the benefits of mindfulness. A practice review of psychotherapy-related research? Psychotherapy (Chic) 2011;48:198–208. doi: 10.1037/a0022062. [DOI] [PubMed] [Google Scholar]
- 14.Wong C, Yip BH, Gao T, Lam KY, Woo DM, Yip AL, et al. Mindfulness-Based Stress Reduction (MBSR) or Psychoeducation for the Reduction of Menopausal Symptoms: A Randomized, Controlled Clinical Trial. Sci Rep. 2018;8:6609. doi: 10.1038/s41598-018-24945-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Enjezab B, Zarehosseinabadi M, Farzinrad B, Dehghani A. The effect of mindfulness-based cognitive therapy on quality of life in perimenopausal women. Iran J Psychiatry Behav Sci. 2019;13:e86525. [Google Scholar]
- 16.Hilditch JR, Lewis J, Peter A, van Maris B, Ross A, Franssen E, et al. A menopause-specific quality of life questionnaire: Development and psychometric properties. Maturitas. 2008;61:107–21. doi: 10.1016/j.maturitas.2008.09.014. [DOI] [PubMed] [Google Scholar]
- 17.Ghazanfarpour M, Kaviani M, Rezaiee M, Ghaderi E, Zandvakili F. Cross cultural adaptation of the menopause specific questionnaire into the persian language. Ann Med Health Sci Res. 2014;4:325–9. doi: 10.4103/2141-9248.133453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sood R, Kuhle CL, Kapoor E, Thielen JM, Frohmader KS, Mara KC, et al. Association of mindfulness and stress with menopausal symptoms in midlife women. Climacteric. 2019;22:377–82. doi: 10.1080/13697137.2018.1551344. [DOI] [PubMed] [Google Scholar]
- 19.Garcia MC, Kozasa EH, Tufik S, Mello LE, Hachul H. The effects of mindfulness and relaxation training for insomnia (MRTI) on postmenopausal women: A pilot study. Menopause. 2018;25:992–1003. doi: 10.1097/GME.0000000000001118. [DOI] [PubMed] [Google Scholar]
- 20.Carmody JF, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: Results of a randomized trial. Menopause. 2011;18:611–20. doi: 10.1097/gme.0b013e318204a05c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumari M, Stafford M, Marmot M. The menopausal transition was associated in a prospective study with decreased health functioning in women who report menopausal symptoms. J Clin Epidemiol. 2005;58:719–27. doi: 10.1016/j.jclinepi.2004.09.016. [DOI] [PubMed] [Google Scholar]


