Abstract
Gender is an important risk factor for the development of obesity. Female gender is associated with twice the risk of being overweight or having obesity. Women are also at higher risk for developing obesity-related physical and psychological comorbidities and have a twofold higher mortality risk than overweight men. Several risk factors have been described to explain the gender bias associated with an obese phenotype and these disparities have far-reaching implications on the medical, psychosocial, and the economical impact of an individual. Despite extensive awareness about gender differences related to obesity, this is still considered as an unchartered territory in obesity medicine. This is probably because of the complex multiple dimensions involved with the understanding of subject coupled with the lack of composite outcomes measures that could assist in the study of these factors. In this scoping review, we share the existing literature regarding the magnitude of gender disparities and gender discrimination in people living with obesity. We describe key factors leading to this gender bias and the impact of this discrimination on the psychological, social, and metabolic health of a given individual with obesity. We also discuss the possible implications of gender disparities on treatment of obesity which may help reduce the current mortality gap between overweight women and men.
Keywords: Androgynous, gender bias, gender disparity, obesity, South Asian phenotype
INTRODUCTION
To minimize gender inequality, in all spheres of life is a hallmark of human development. Significant progress in this regard has been made following the Beijing Declaration in 1995.[1] Nevertheless, gender discrimination is still a reality in many developing countries and is a major concern pertaining to those affected by medical disorders. A greater depth of understanding on this subject with respect to specific disease conditions would help to further minimize this mismatch.
Despite extensive awareness about gender disparity over the past two decades, this is still considered an unchartered territory in the field of obesity medicine. This is probably because of the complex multiple dimensions involved with understanding these subjects coupled with the lack of composite outcomes measures that could assist in studying impact of gender on people living with obesity.[2] Moreover, obesity is determined by a complex interaction between genetic predisposition, psychologic makeup, and environmental factors.[3,4] Figure 1 details the complex interaction between gender inequality and the pathogenesis of obesity.
Figure 1.
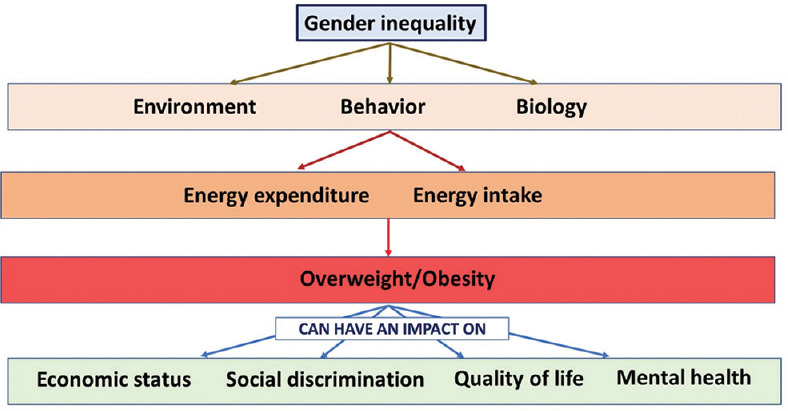
The complex interaction and impact of gender inequality on obesity
In this scoping review, we discuss the magnitude of gender disparities and gender discrimination in people living with obesity. We describe the key factors that possibly lead to this gender bias and detail the impact of this discrimination on the psychological, social, and metabolic health of a given individual with obesity. We also explore its possible implications on obesity treatment and propose future research questions based on the knowledge gaps we have found.
EPIDEMIOLOGY
The gender differences in the prevalence of obesity are well studied. The current evidence supports that female gender is a potential risk factor for developing obesity.[5,6] A study across 68 countries demonstrated that gender inequalities were associated with obesity in both developed and developing European countries.[7] Another study, across developed nations, showed that gender inequalities were more noted in the lower socioeconomic status.[8] Inequalities in literacy and poverty have also been demonstrated in women living with obesity in several studies.[9,10] This is especially relevant in many nonindustrialized developing countries where the role of environmental influences on gender health may be significant.[11,12]
A contemporary study from the Asia-Pacific region examined 1178 participants for gender differences with respect to obesity and its associated cardiometabolic risk factors.[13] The Asia-Pacific guidelines were used to define obesity. Women were found to have a higher age-adjusted central obesity in about half of the subjects. Moreover, significant sex differences were found among different cardiometabolic risk factors across different levels of central obesity. It was also noted that women had 2.5 times more likelihood of having central obesity compared to men, after adjustment of the cardiometabolic and sociodemographic determinants. Similar findings have been replicated in other south Asian studies.[14,15,16]
ETIOPATHOGENESIS AND PRESENTATION
Gender-based differences in food craving have been studied extensively before.[17] This is also an important factor determining the gender-based differences in the prevalence of obesity. Overall, women have been shown to have significantly higher craving scores than men. Functional cranial imaging using a magnetic resonance imaging has shown greater neural reactivity to palatable food images in women for both craving- and taste-related regions of the brain as compared to men.[18]
Gender disparities may also depend on associated comorbidities. About half of the malignancies that occur in women and a quarter that occur in men are associated with obesity.[19] Although obesity is associated with significant alterations in the hormonal, metabolic, and inflammatory milieu of a given patient, the key mechanisms that alter the risk between men and women include the differences in the insulin/insulin-like growth factor-1 axis, the impact of gonadal hormones, and the emerging role of adipocytokines.[20,21,22] Overall, the obesity-related malignancies are more common in women and include endometrial, ovarian, and postmenopausal breast cancers. Among the malignancies that affect both genders, esophageal cancers are more prevalent in men. The role of obesity becomes more relevant in carcinogenesis as is evidenced by the lowering of cancer risk following bariatric surgery.[23] Bariatric surgery has shown to reduce malignancy risk in women within 1st 5 years after surgery which is mainly attributed to the reduction in non-Hodgkin's lymphoma and breast and endometrial malignancies.[19]
In addition to hormone dependent malignancies, gender differences with respect to other obesity related comorbidities including type 2 diabetes mellitus, nonalcoholic fatty liver disease, obesity hypoventilation syndrome, pulmonary functions, psychological disorders and health related quality of life also affect women more often than men (QoL).[24,25,26,27,28,29]
Table 1 summarizes the key risk factors that drive the gender disparities related to obesity. These results provide evidence to support the development of gender-based, population-level interventions to tackle the pandemic of obesity and cardiometabolic disorders.
Table 1.
Factors leading to gender disparities in obesity
| Disparate socioeconomic status |
| Dissimilar literacy rates |
| Mismatched sociocultural factors |
| Feeding practices in the postpartum period |
| Nonidentical threshold for metabolic complications |
| Contrasting biological craving of food |
| Distinct hormone-related comorbidities |
| Divergent customs - women homebound in some cultures |
CLINICAL IMPLICATIONS
Female gender is associated with twice the risk of being overweight or having obesity. Women are also at higher risk for developing obesity-related comorbidities as compared to men and have a twofold higher mortality risk than overweight men. While this disproportionately large obesity-related disease burden in women is partly due to differences in medical comorbidities, it is also related to emotional and psychological issues.
In a study of 4181 men and women aged between 18 and 65 years for associations between gender, medical comorbidities, health-related (HRQoL), and obesity status, women were found to bear a disproportionately large share of the disease, with an important role being played by emotional well-being and psychological components.[30] This is supported by another large study which estimated the burden of disease attributable to obesity by gender, with life expectancy, quality-adjusted life expectancy, years of life lost annually, and quality-adjusted life years lost annually as outcome measures. In this study, overweight men and women lost 0.3 and 1.8 million quality-adjusted life years, respectively, relative to their normal-weight counterparts. Obese men and women lost 1.9 million and 3.4 million quality-adjusted life years, respectively, per year. Much of the disease burden in obese women was attributed to lower HRQoL and late-life mortality.[31]
One of the reasons for a higher health-related impairment in women as compared to men is probably a lower threshold of development of physical and psychological comorbidities in women.[32,33] This is even true in the south Asian context where comorbidities are described at lower body mass index (BMI).[34,33,34,35,35,36,37] The clinical determinants of weight alterations in women are summarized in Figure 2.
Figure 2.
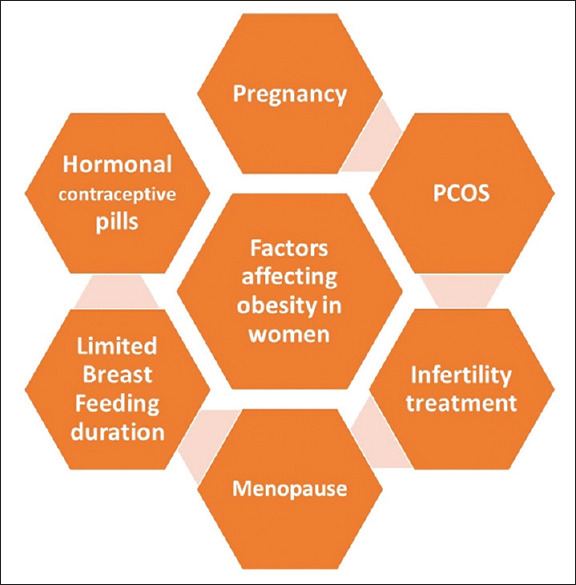
The clinical determinants of obesity in women
However, the most alarming fact that highlights the importance of understanding the clinical implications of gender disparities in obesity is the large difference in the mortality risk among men and women.[31] Overweight women have been found to have twice the risk of mortality as compared to overweight men. This underscores the need for incorporating gender differences in screening, diagnostic, and therapeutic obesity management protocols.
IMPACT ON MANAGEMENT
The key to successful management of obesity is to provide an individualized person-centric management plan to each patient.[38] No single management plan works for all patients and gender is an important component to be kept in mind while evaluating an treating obesity in a given patient. At present, literature is emerging on the importance of incorporating gender-related issues like phases of the menstrual cycle, use of hormonal contraception, and the impact of menopause while evaluating a patient with obesity. These may alter several aspects of energy expenditure and substrate utilization. In a recent review, the current evidence relating to gender-specific alterations during physical activity, thermogenesis, and fat oxidation has been well summarized based on which gender-centric recommendations for obesity management can be derived. The key therapeutic implications that emerge based on existing literature on the subject suggest that women could benefit more with low-intensity isometric physical activities than men. It is also suggested that manipulation of dietary protein content may be less effective in women who are using the combined oral contraceptive pill.[39]
Another area of future research relating to therapeutics of obesity is that in transgenders and those who undergo a sex change operation. Cross-sex hormone treatment has been shown to significantly alter the body composition of the patient. Male-to-female transgender individuals have a significant increase in BMI, increase in body fat percentage by 38%, and an increase in abdominal subcutaneous fat area by 54% and visceral fat area by 17%. This is often coupled with a worsening of insulin and lipid profiles following 12 months of hormone treatment. Female-to-male transgender individuals treated with testosterone exhibit no change in BMI but increment in visceral fat area by 18%.[40]
Gender dimorphic response is also expected with the use of anti-obesity medications. Gender-based differential response for some currently used drugs including liraglutide, bupropion/naltrexone, and phentermine/topiramate has been reviewed by experts.[41] Although initial studies were not specifically designed to study the gender disparities in their response, there is an urgent need of new real-life data on gender-related difference in the pharmacology of these new obesity drugs.[41]
Similar gender dimorphic responses have also been noted in patients who undergo bariatric surgery. In a recently published study by Bal et al., it was found that men were more likely to undergo sleeve gastrectomy than Laparoscopic Roux-en-Y gastric bypass and also had higher complication rates for both. Even though women were noticed to have higher readmission rates regardless of the choice of surgery, overall postoperative morbidity was found to be lower in women.[42]
CONCLUSION
Gender disparity is an important aspect of obesity. Although several risk factors have been identified for the current trend on women getting more affected with obesity, limited literature is available on how to incorporate this information in the prevention, evaluation, and treatment of a given individual. This paper summarizes the existing literature regarding the magnitude of gender disparities and gender discrimination in people living with obesity. It describes key factors leading to this gender bias and the impact of this discrimination on the psychological, social, and metabolic health of a given individual with obesity. Understanding the gender differences with respect to obesity can have a major impact in the treatment of obesity, and on planning community and individual interventions for the prevention and management of this pandemic. Further research is needed to decipher the gender dimorphic responses using different therapeutic strategies for the management of obesity.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Would suggest this reference instead United Nations Fourth World Conference on Women: Declaration and Platform for Action. International Legal Materials. 1996;35:401–82. [Google Scholar]
- 2.Ferretti F, Mariani M. Gender discrimination, gender disparities in obesity and human development. Heliyon. 2017;3:e00263. doi: 10.1016/j.heliyon.2017.e00263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akabas SR, Lederman SA, Moore BJ. Textbook of Obesity: Biological, Psychological and Cultural Influences. Chichester, UK: John Wiley and Sons; 2012. [Google Scholar]
- 4.Kapoor N, Chapla A, Furler J, Paul TV, Harrap S, Oldenburg B, et al. Genetics of obesity in consanguineous populations – A road map to provide novel insights in the molecular basis and management of obesity. EBioMedicine. 2019;40:33–4. doi: 10.1016/j.ebiom.2019.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandola T, Kuper H, Singh-Manoux A, Bartley M, Marmot M. The effect of control at home on CHD events in the Whitehall II study: Gender differences in psychosocial domestic pathways to social inequalities in CHD. Soc Sci Med. 2004;58:1501–9. doi: 10.1016/S0277-9536(03)00352-6. [DOI] [PubMed] [Google Scholar]
- 6.Kanter R, Caballero B. Global gender disparities in obesity: A review. Adv Nutr. 2012;3:491–8. doi: 10.3945/an.112.002063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wells JC, Marphatia AA, Cole TJ, McCoy D. Associations of economic and gender inequality with global obesity prevalence: Understanding the female excess. Soc Sci Med. 2012;75:482–90. doi: 10.1016/j.socscimed.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 8.Wardle J, Waller J, Jarvis MJ. Sex differences in the association of socioeconomic status with obesity. Am J Public Health. 2002;92:1299–304. doi: 10.2105/ajph.92.8.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Saint Pol T. Evolution of obesity by social status in France, 1981-2003. Econ Hum Biol. 2009;7:398–404. doi: 10.1016/j.ehb.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 10.Doyal L. Sex, gender, and health: The need for a new approach. BMJ. 2001;323:1061–3. doi: 10.1136/bmj.323.7320.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Monteiro CA, Moura EC, Conde WL, Popkin BM. Socioeconomic status and obesity in adult populations of developing countries: A review. Bull World Health Organ. 2004;82:940–6. [PMC free article] [PubMed] [Google Scholar]
- 12.Kalra S, Kapoor N. Environmental endocrinology: An expanding horizon. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dungan K, editors. Endotext. South Dartmouth (MA): MDText.Com, Inc. Copyright © 2000-2021, MDText.Com, Inc; 2000. [PubMed] [Google Scholar]
- 13.Prasad DS, Kabir Z, Revathi Devi K, Peter PS, Das BC. Gender differences in central obesity: Implications for cardiometabolic health in South Asians. Indian Heart J. 2020;72:202–4. doi: 10.1016/j.ihj.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kapoor N, Jiwanmall SA, Nandyal MB, Kattula D, Paravathareddy S, Paul TV, et al. Metabolic Score for Visceral Fat (METS-VF) estimation – A novel cost-effective obesity indicator for visceral adipose tissue estimation. Diabetes Metab Syndr Obes. 2020;13:3261–7. doi: 10.2147/DMSO.S266277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kapoor N, Lotfaliany M, Sathish T, Thankappan KR, Thomas N, Furler J, et al. Obesity indicators that best predict type 2 diabetes in an Indian population: Insights from the Kerala Diabetes Prevention Program. J Nutr Sci. 2020;9:e15. doi: 10.1017/jns.2020.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kapoor N, Lotfaliany M, Sathish T, Thankappan KR, Thomas N, Furler J, et al. Prevalence of normal weight obesity and its associated cardio-metabolic risk factors – Results from the baseline data of the Kerala Diabetes Prevention Program (KDPP) PLoS One. 2020;15:e0237974. doi: 10.1371/journal.pone.0237974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hallam J, Boswell RG, DeVito EE, Kober H. Gender-related differences in food craving and obesity. Yale J Biol Med. 2016;89:161–73. [PMC free article] [PubMed] [Google Scholar]
- 18.Uher R, Treasure J, Heining M, Brammer MJ, Campbell IC. Cerebral processing of food-related stimuli: Effects of fasting and gender. Behav Brain Res. 2006;169:111–9. doi: 10.1016/j.bbr.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 19.Argyrakopoulou G, Dalamaga M, Spyrou N, Kokkinos A. Gender differences in obesity-related cancers. Curr Obes Rep. 2021;10:100–15. doi: 10.1007/s13679-021-00426-0. [DOI] [PubMed] [Google Scholar]
- 20.Spyrou N, Avgerinos KI, Mantzoros CS, Dalamaga M. Classic and novel adipocytokines at the intersection of obesity and cancer: Diagnostic and therapeutic strategies. Curr Obes Rep. 2018;7:260–75. doi: 10.1007/s13679-018-0318-7. [DOI] [PubMed] [Google Scholar]
- 21.Karim R, Mack WJ, Hodis HN, Roy S, Stanczyk FZ. Influence of age and obesity on serum estradiol, estrone, and sex hormone binding globulin concentrations following oral estrogen administration in postmenopausal women. J Clin Endocrinol Metab. 2009;94:4136–43. doi: 10.1210/jc.2009-0643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalra S, Kapoor N, Bhattacharya S, Aydin H, Coetzee A. Barocrinology: The endocrinology of obesity from bench to bedside. Med Sci (Basel) 2020;8:51. doi: 10.3390/medsci8040051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schauer DP, Feigelson HS, Koebnick C, Caan B, Weinmann S, Leonard AC, et al. Bariatric surgery and the risk of cancer in a large multisite cohort. Ann Surg. 2019;269:95–101. doi: 10.1097/SLA.0000000000002525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Awa WL, Fach E, Krakow D, Welp R, Kunder J, Voll A, et al. Type 2 diabetes from pediatric to geriatric age: Analysis of gender and obesity among 120,183 patients from the German/Austrian DPV database. Eur J Endocrinol. 2012;167:245–54. doi: 10.1530/EJE-12-0143. [DOI] [PubMed] [Google Scholar]
- 25.Choo J, Jeon S, Lee J. Gender differences in health-related quality of life associated with abdominal obesity in a Korean population. BMJ Open. 2014;4:e003954. doi: 10.1136/bmjopen-2013-003954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jonikas JA, Cook JA, Razzano LA, Steigman PJ, Hamilton MM, Swarbrick MA, et al. Associations between gender and obesity among adults with mental illnesses in a community health screening study. Community Ment Health J. 2016;52:406–15. doi: 10.1007/s10597-015-9965-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.BaHammam AS, Pandi-Perumal SR, Piper A, Bahammam SA, Almeneessier AS, Olaish AH, et al. Gender differences in patients with obesity hypoventilation syndrome. J Sleep Res. 2016;25:445–53. doi: 10.1111/jsr.12400. [DOI] [PubMed] [Google Scholar]
- 28.Atri A, Jiwanmall SA, Nandyal MB, Kattula D, Paravathareddy S, Paul TV, et al. The prevalence and predictors of non-alcoholic fatty liver disease in morbidly obese women – A cross-sectional study from Southern India. Eur Endocrinol. 2020;16:152–5. doi: 10.17925/EE.2020.16.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ramasamy S, Joseph M, Jiwanmall SA, Kattula D, Nandyal MB, Abraham V, et al. Obesity indicators and health-related quality of life – Insights from a cohort of morbidly obese, middle-aged South Indian Women. Eur Endocrinol. 2020;16:148–51. doi: 10.17925/EE.2020.16.2.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mond JM, Baune BT. Overweight, medical comorbidity and health-related quality of life in a community sample of women and men. Obesity (Silver Spring) 2009;17:1627–34. doi: 10.1038/oby.2009.27. [DOI] [PubMed] [Google Scholar]
- 31.Muennig P, Lubetkin E, Jia H, Franks P. Gender and the burden of disease attributable to obesity. Am J Public Health. 2006;96:1662–8. doi: 10.2105/AJPH.2005.068874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Patterson RE, Frank LL, Kristal AR, White E. A comprehensive examination of health conditions associated with obesity in older adults. Am J Prev Med. 2004;27:385–90. doi: 10.1016/j.amepre.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 33.Scott KM, McGee MA, Wells JE, Oakley Browne MA. Obesity and mental disorders in the adult general population. J Psychosom Res. 2008;64:97–105. doi: 10.1016/j.jpsychores.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 34.Kapoor N, Furler J, Paul TV, Thomas N, Oldenburg B. The BMI-adiposity conundrum in South Asian populations: Need for further research. J Biosoc Sci. 2019;51:619–21. doi: 10.1017/S0021932019000166. [DOI] [PubMed] [Google Scholar]
- 35.Kapoor N, Furler J, Paul TV, Thomas N, Oldenburg B. Ethnicity-specific cut-offs that predict co-morbidities: The way forward for optimal utility of obesity indicators. J Biosoc Sci. 2019;51:624–6. doi: 10.1017/S0021932019000178. [DOI] [PubMed] [Google Scholar]
- 36.Kapoor N, Furler J, Paul TV, Thomas N, Oldenburg B. Normal weight obesity: An underrecognized problem in individuals of south Asian descent. Clin Ther. 2019;41:1638–42. doi: 10.1016/j.clinthera.2019.05.016. [DOI] [PubMed] [Google Scholar]
- 37.Kapoor N. Thin fat obesity: The tropical phenotype of obesity. In: Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dungan K, editors. Endotext. South Dartmouth (MA): MDText.Com, Inc. Copyright © 2000-2021, MDText.Com, Inc; 2000. [PubMed] [Google Scholar]
- 38.Kalra S, Kapoor N, Kota S, Das S. Person-centred obesity care – Techniques, thresholds, tools and targets. Eur Endocrinol. 2020;16:11–3. doi: 10.17925/EE.2020.16.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Isacco L, Miles-Chan JL. Gender-specific considerations in physical activity, thermogenesis and fat oxidation: Implications for obesity management. Obes Rev. 2018;19(Suppl 1):73–83. doi: 10.1111/obr.12779. [DOI] [PubMed] [Google Scholar]
- 40.Gooren LJ, Giltay EJ, Bunck MC. Long-term treatment of transsexuals with cross-sex hormones: Extensive personal experience. J Clin Endocrinol Metab. 2008;93:19–25. doi: 10.1210/jc.2007-1809. [DOI] [PubMed] [Google Scholar]
- 41.Cataldi M, Muscogiuri G, Savastano S, Barrea L, Guida B, Taglialatela M, et al. Gender-related issues in the pharmacology of new anti-obesity drugs. Obes Rev. 2019;20:375–84. doi: 10.1111/obr.12805. [DOI] [PubMed] [Google Scholar]
- 42.Bal J, Ilonzo N, Adediji T, Leitman IM. Gender as a deterministic factor in procedure selection and outcomes in bariatric surgery. JSLS. 2021;25:e2020.00077. doi: 10.4293/JSLS.2020.00077. [DOI] [PMC free article] [PubMed] [Google Scholar]


