Abstract
Introduction/purpose
Diagnostic thoracic ultrasound is increasingly being used by non‐physicians; hence, we evaluated a curriculum for acute care physiotherapists in critical care.
Methods
The one‐day course included didactic lectures combined with expert‐led hands‐on training. Participants undertook pre‐ and post‐course knowledge questionnaire covering key ultrasound findings for normal lungs, pleural and pulmonary pathologies. Course participants who worked at the institution where the course was undertaken undertook a practical examination. We also did a 4‐ to 6‐week follow‐up survey of participants. The pretest and post‐test questionnaire and survey results were reported using descriptive statistics (means SD or median and IQR).
Results
A total of 12 acute care physiotherapists undertook the training and questionnaire scores (mean percentage, SD, 95% CI) increased from 73.3 ± 15.5% (63.4–83.2) before the training to 86.3 ± 5.5% (82.8–89.8) after training.
Discussion
This diagnostic thoracic ultrasound training course resulted in improvements of diagnostic thoracic ultrasound knowledge including lung and pleural pathology image recognition skills in a small group of acute care physiotherapists with nil previous diagnostic thoracic ultrasound skills. Two‐thirds of the participants who responded to the survey undertook only one to three scans in clinical practice, and the most frequent barrier to clinical use of diagnostic thoracic ultrasound was time constraints.
Conclusion
Further investigation of such a diagnostic thoracic ultrasound training programme on knowledge and skills retention and image acquisition and interpretation in real life clinical practice in a larger group of acute care physiotherapists is warranted.
Keywords: ultrasonography, curriculum, diagnostics, physical therapy
Introduction
In the critical care environment, physiotherapists routinely utilise combinations of clinical examination, lung auscultation and the interpretation of the chest radiograph findings to assist with clinical decision‐making about the requirement for and response(s) to chest physiotherapy.1 There is an increasing evidence base within critical care demonstrating the improved diagnostic accuracy and beneficial impact of diagnostic thoracic ultrasound (DTU) on clinical decision‐making by intensivists for the detection of key pulmonary (interstitial syndrome, lung collapse/consolidation) and pleural pathologies (pneumothorax, pleural effusion).2, 3, 4, 5 Comparisons of the performance of the standard clinical assessment tools with DTU on clinical decision‐making and impact on patient outcomes have yet to be fully investigated. The incorporation of DTU within critical care6, 7 thus provides acute care physiotherapists with an ideal tool for the identification of pulmonary pathology that may be amenable to chest physiotherapy.2, 6, 8
Diagnostic ultrasound is not new to physiotherapy;9 however, to the best of our knowledge, it is not routinely utilised by physiotherapists to examine the respiratory system in the critical care setting, with many now advocating for its uptake.6, 10 Various short courses have been developed for training medical clinicians in the use of point of care diagnostic ultrasound (POCUS) and utilise different training methods (simulation‐based, e‐learning, hands‐on classroom‐based learning), different durations and methods of evaluation.11, 12, 13, 14, 15, 16, 17, 18 While there is some attempt to standardise the skills required to achieve competence in DTU among critical care physicians19 and the standards by which they are trained,20 various minimum standards and timeframes have been recommended to achieve competence, predominantly based on expert opinion. There are also no standards on the content, methods of delivery and assessments specifically for acute care physiotherapists in the critical care setting. However, a recent publication reported that a minimum of 10 lung ultrasound scans were required by non‐physician trainees (respiratory therapists) to acquire competence for independent practice in lung ultrasound for key pulmonary pathologies in the critical care setting (excluded pleural effusions).21
The primary objective of this study was to evaluate the impact of a one‐day DTU curriculum course (including pre‐reading, didactic lectures, practical training and image recognition skills) on the short‐term knowledge acquisition by group of acute care physiotherapists.
Methods
This study was approved by the University of Technology Sydney HREC (ETH: 160965). We invited a group of acute care physiotherapists to undertake a one‐day DTU course that included 2.5 h of didactic lectures and 4 h of expert‐led practical skill training (Table 1). Half of the course participants were staff members of the institution conducting the DTU course and they were expected to also undertake a practical skill examination on the day after the course. The general objective of the course was to assess the knowledge acquisition before and after the course and views of the participants.
Table 1.
Diagnostic thoracic ultrasound course curriculum (one‐day course)
| Pre‐reading |
Participants were emailed 1 week pre‐course the review article: Via et al.22 |
| Duration | One‐day course outline |
| 20 min | Online Quiz (10 multiple‐choice questions) based on pre‐reading22 see link https://goo.gl/forms/ffIxy8YW45arZDux1 |
| 35 min | Didactic lecture: Physics of ultrasound – Knobology/image optimisation |
| 40 min |
Practical stations: DTU image optimisation Expert‐led stations Four identical groups of three participants using normal individuals as models for DTU image optimisation |
| 25 min | Didactic Lecture: Normal anatomy: abdomen/thorax landmarks |
| 70 min |
Practical stations: DTU imaging abdomen/thorax anatomy/landmarks on normal models Expert–instructor‐led stations using normal individuals (each participant alternately acted as a model for imaging purposes) for DTU image identification, acquisition and image optimisation procedures |
| 30 min |
Didactic lecture: DTU presentation of pulmonary conditions1
|
| 30 min |
Didactic lecture: DTU presentation of pulmonary condition2
|
| 120 min |
Practical stations: Expert‐led rotating stations (Four stations with 40 min at each station).
|
| 30 min | Didactic lecture DTU applications for physiotherapy in intensive care |
| 20 min | Post‐workshop knowledge‐based quiz evaluating course content see link https://goo.gl/forms/4mOFoLtxyTF5JUGg1 |
| 10 min | Online evaluation satisfaction survey of attendees regarding course content and structure |
- Bilateral Diaphragmatic Dysfunction
- Central Pneumonia
- Empyema
- Pneumonia
- Small Pleural Effusion
- Bilateral Pulmonary Oedema
- Complete Pleural Effusion
- Normal, Enhanced Heart and Lungs
- Pneumothorax
- Unilateral Diaphragmatic Dysfunction
There were six strategies that were used to optimise participant learning, and they included (i) identification of the appropriate pre‐reading material (a comprehensive review article that included key aspects of diagnostic thoracic ultrasound in critical care22), (ii) evaluation of participant readiness at baseline, (iii) small group training with a high expert instructors:trainee ratio (1:3 ratio was used in this course as we were able to provide a greater ratio than the recommendations from Australian Society of Ultrasound Medicine see link http://www.asum.com.au/files/public/Education/CAHPU/CAHPUForms/CAHPUUnit-Accreditation-Application-Form.pdf), (iv) post‐workshop knowledge test, (v) practical test (only half of participants invited as mentioned earlier), (vi) establish a post‐course peer support group (set‐up of secure WhatsApp chat group https://www.whatsapp.com) & ongoing mentoring ( https://www.whatsapp.com) provided by the primary instructor (GN).
The full one‐day course content and structure are detailed in Table 1.
Prior to the course the participants were sent a key narrative review article,22 for its comprehensiveness to enhance learning and reduce the cognitive load during the workshop, that covered the basics of DTU theory and its practical applications in critical care including the identification of the key pulmonary pathologies such as pneumothorax, pleural effusion, lung collapse, lung consolidation, pneumonia and interstitial oedema. At enrolment prior to course commencement, the participants were given an online questionnaire with 10 multiple‐choice questions (see link https://goo.gl/forms/ffIxy8YW45arZDux1) to evaluate the basic knowledge acquired from the pre‐reading.22 All the participants then underwent the one‐day course which included didactic lectures and expert‐led practical training (Table 1). The experts who led the practical training sessions included three medical doctors (HCT, RPS, WDS), one experienced trained ultrasonographer and an experienced trained critical care physiotherapist (GN) all with current clinical and teaching experience in diagnostic thoracic ultrasound. A post‐course questionnaire included 21 multiple‐choice questions (see link https://goo.gl/forms/4mOFoLtxyTF5JUGg1) covering key aspects covered in the one‐day course including the DTU findings for normal lungs, pleural pathology (pleural effusion, pneumothorax) and key acute pulmonary pathologies (pulmonary oedema, pneumonia, lung collapse). Half of the participants, who worked at the health institution where the course was conducted, also undertook a practical examination of their DTU skills (Table 2). The skill test lasted 15 min, and the clinician was assessed on their ability for key thoracic and abdominal organ identification (normal lung/chest, lung aeration (A lines, B lines), pleura, ribs, heart, liver or spleen), image optimisation (depth/gain), calliper measurements, still image/video clip acquisition, image storage and image review utilising a normal male model (physiotherapy students). These same participants then also reviewed four sample DTU video clips of key unlabelled pulmonary and pleural pathology.
Table 2.
Practical examination (15‐min duration)
|
Practical examination (set‐up)
|
|
Practical instrumentation/use of ultrasound controls (Score 4/4)
|
|
Normal anatomy of pleura, diaphragm, key abdominal organs (Score 8/8)
|
|
Key pathologies – review video clips (Score 4/4)
|
| Total score = /16 |
Descriptive statistics
Summary and descriptive statistics of participants’ scores (percentage correct) on pre‐ and post‐course questionnaires were reported. The participant evaluations of course satisfaction and follow‐up surveys were also reported.
Results
A total of 12 physiotherapists were included in this training programme. The percentage of correct answers for the 10 pre‐course questions are summarised in Figure 1 below. The Questions 3 and 8 were scored the lowest with only 42% of participants answering the questions correctly.
Figure 1.
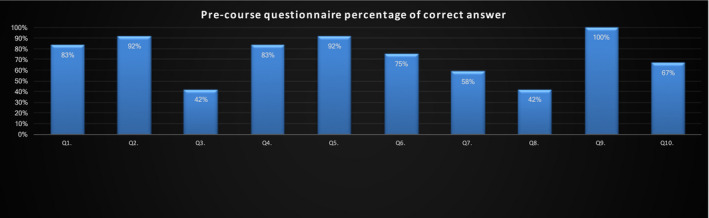
Pre‐Course Assessment (Based on Review of Material from22 See Link for Details of Questions https://goo.gl/forms/ffIxy8YW45arZDux1).
Only seven of 12 (58%) of the participants reported they had read all of the recommended pre‐course material. The pre‐course assessment results (mean ± SD) for seven participants who completed all the pre‐reading was 81 ± 8.9% as compared to 62 ± 16.4% for the five who did not complete all the pre‐reading. The percentage of correct answers for the 21 post‐course questionnaire results are summarised in Figure 2 below. There was one question that was poorly answered by the cohort being question 8 (investigated the reasoning behind the evaluation of the lung sliding sign) with only 42% getting the question correct.
Figure 2.
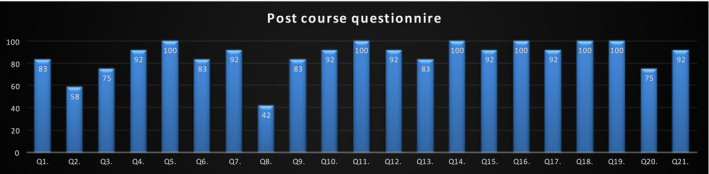
Post‐Course Questionnaire (See Link for Details of Questions https://goo.gl/forms/kAOiUxiQoSnkAude2).
The assessment scores (mean percentage, SD, 95% CI) increased from a mean of 73.3 ± 15.5% (63.4–83.2) before the training (Figure 3) to 86.3 ± 5.5% (82.8–89.8) after training. Separating out the participants on the basis of whether they undertook the pre‐reading, it was the five participants who did not undertake the pre‐reading that had greater improvement in their post‐test scores compared with their pre‐test scores, mean difference (95% CI) 20.8, 5.7–35.9%. The participants who undertook all their pre‐reading improved their post‐test scores by a smaller mean difference (95% CI) 7.42, −0.97–15.8 compared with the participants who did not complete the pre‐reading.
Figure 3.
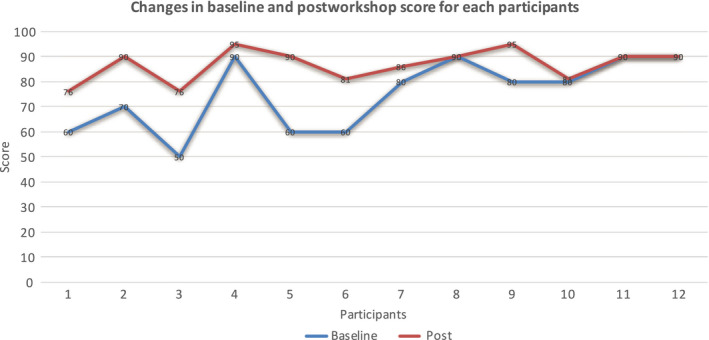
Pre‐ and Post‐Course Assessment Scores (%).
Practical test
Half of the participants, who were employees of the tertiary hospital where the course was conducted, undertook a practical skill examination by the lead course instructor (GN) the day after the course. The course organisers’ intention was to support the development of the lung ultrasound training skills for these specific participants as it was believed they could be more directly mentored further by the course organisers. The practical examination covered basic practical skills and image acquisition and interpretation with knobology, anatomy and viewing of examples of selected pulmonary pathology (Table 2). The median (IQR) assessment scores for the key sections were knobology (4, 4‐4), anatomy (7.5, 7–8), key pathologies (4, 4–4), with overall course assessment outcome 15.5 (14.2–16).
Course satisfaction
All 12 participants felt the course pre‐reading was appropriate and that the course content was aimed at the appropriate level in terms of DTU theory and practical skill acquisition. All participants felt that this course would impact on their clinical practice and they felt confident that they would begin to use DTU in their clinical work. However, five of the 12 participants felt that there was insufficient time allocated to the practical sessions (two of these participants had not completed the pre‐reading and the remaining three had completed their pre‐reading). Participant rating of each of the didactic and practical sessions was favourably reported (Figure 4).
Figure 4.
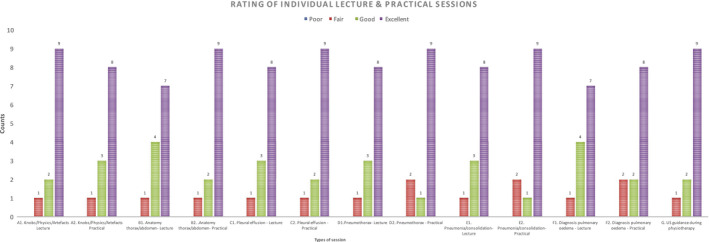
Participant Rating of Individual Sessions.
Follow‐up survey of learning strategies, barriers and enablers to use of ultrasound
Only six of the 12 participants (50%) responded to the 4‐ to 6‐week follow‐up survey of actual ultrasound scanning over that time period. Four of the six participants performed from one to three ultrasound scans and the remaining two participants performed four to six scans. The most challenging factor to performing ultrasound scans was a lack of time (4/6 participants) followed by lack of ultrasound equipment (one participant) and a combination of lack of time and suitable patients for scanning (one participant). Other barriers cited to inhibit the participants use of ultrasound in their workplace included a lack of appropriate patients to image (n = 3), a lack of confidence in undertaking the imaging (n = 3) and lack of a mentor (n = 2). In terms of the methods used by the participants to engage in further learning after the course, all six found the social media platform (Whatsapp https://www.whatsapp.com) discussions including the reviewing of ultrasound images/clips with the course coordinators extremely useful. Watching YouTube ( https://www.youtube.com) video clips of ultrasound and reading relevant articles were somewhat useful by four of six participants. Being coached/mentored by work colleagues was extremely useful for five of six participants, and individual practice was considered extremely useful by one participant and only somewhat useful for four of six participants. The strategies mentioned by participants that facilitated learning DTU included practising ultrasound imaging on colleagues, discussing ultrasound findings with physiotherapy and medical consultant colleagues and reviewing the lecture material from the course.
Discussion
This one‐day DTU curriculum programme with a combination of pre‐reading, didactic lectures paired with expert‐led hands‐on DTU training to ultrasound‐naive acute care physiotherapists appears to be effective in providing the basic knowledge and image interpretation skills necessary for initial DTU clinical skill acquisition. The post‐test scores of the participants who did not complete all their pre‐reading improved more than the participants who completed all their pre‐reading. This suggests either that the workshop alone can increase the knowledge acquired, or that the questionnaire failed to address the key learning issues of the pre‐reading material. But we also cannot rule out the possible effect of pre‐reading material in reducing the cognitive load and hence facilitating the learning from the workshop and the long‐term retention effect of the material. Only half of the participants completed the follow‐up survey, with most stating they had only practised ultrasound imaging acquisition from one to three occasions in the 4‐ to 6‐week period after the course. The most frequent barriers reported to the participants’ use of diagnostic ultrasound was inadequate time for imaging, a lack of confidence in imaging and a lack of mentors. The strategies the participants reported that most assisted them with further practice and learning included involvement in a social media chat platform for the sharing of ultrasound clips and discussions, being coached and mentored by work colleagues.
This one‐day course utilised the participants themselves agreeing to be imaged by fellow participants for normal real‐time ultrasound views of key anatomical structures (chest wall, lungs, diaphragm, pleura, intercostal spaces, liver, spleen, kidneys). We also utilised commercially available simulation mannequins to display common pulmonary and pleural pathologies ( http://caehealthcare.com/images/uploads/documents/Vimedix_1.14_Available_Pathologies-1-12-15.pdf). Future programmes could be improved by including patients with key pathologies for real‐time imaging by participants. For competence to be developed, we recommended that the clinicians need to apply DTU within their own clinical practice with an expert mentor to further guide image acquisition and interpretation skills, with the participants using a log book to record and review mentored image acquisitions. The training requirements for acute care physiotherapists to reach competence in DTU should include an understanding of the ultrasonographic features of common normal anatomy of the thorax (lungs, heart, pleura) and abdomen (liver, spleen, kidney) and detail acute pleural diseases such as pleural effusion, pneumothorax and parenchymal diseases such as pulmonary oedema, lung collapse and pneumonia.23 Physiotherapists utilising ultrasound for clinical practice must be able to demonstrate the acquisition and interpretation of these ultrasound images in real time. They also must be able to integrate the ultrasound findings with overall clinical assessments to facilitate safe and effective practice of physiotherapy in the acute care settings. Acute care physiotherapists need to also appreciate the limitations of DTU, understand the clinical governance issues and importantly the requirements for further training and skill development (ongoing mentored training) to attain competence.
There is no consistency in the literature in regard to the numbers of ultrasound procedures undertaken by clinicians in training to achieve competence in diagnostic thoracic ultrasound. Some recommend to include at least 100 chest ultrasound procedures24 or three months of supervised/mentored practise25 to achieve competence. Others have suggested that if ultrasound procedures are incorporated as part of daily clinical care, then the competence in identifying key pleural and pulmonary pathologies such as pleural effusion, lung consolidation and alveolar interstitial syndrome may be achieved within 6 weeks.26
There are several limitations to our study. We did not report on the participants age, clinical physiotherapy experience or previous post graduate training. The small sample size of participants and lack of information gathered on the knowledge retention on extended periods (3–6 months) after the course restricted our understanding of the clinical impact of the course. We also only obtained information from half of the participants on the limited utilisation of DTU within clinical practice beyond the one‐day course. Some of the positive benefits of the study immediately after the completion of the course may also be due to recall bias. The multiple‐choice questions pre‐ and post‐course differed both in number and in content, and hence, we are unclear as to the real impact of the training. However, we wanted to ascertain the impact of the training course and hence specifically designed the pre‐course assessment to test the knowledge attained from the recommended pre‐reading material.
There is mounting evidence that the diagnostic accuracy of DTU is superior to standard clinical assessments such as lung auscultation and the portable chest radiograph.2, 8, 27 Larger investigations are required to evaluate level of training required for acute care physiotherapists to acquire DTU skills, to apply them in clinical practice, to evaluate the quality of imaging and interpretation and then explore the impact of DTU on clinical decision‐making by physiotherapists.
Conclusion
This pilot programme demonstrated that a single‐day DTU training course led to improvements of DTU knowledge including normal lung and abnormal lung and pleural pathology image recognition skills in a small group of acute care physiotherapists with nil previous DTU skills. The minimum standards and methods required for training, documentation and clinical governance need to be further explored before DTU could be implemented by physiotherapists more widely.
Declarations of interest
The authors report no declarations of interest.
Disclosure statement
GN was supported by the Singapore Government HDMP Visiting Experts Program for funding the workshop. GN is also supported by Sonosite with in‐kind provision of ultrasound machines for ultrasound training courses.
Authorship declaration
The authorship listing conforms with the journal's authorship policy, and all authors are in agreement with the content of the submitted manuscript.
Acknowledgements
We are indebted to the course coordinator Dr Hwee Ong and the course instructors Dr Sewa Duu Wen, Dr. Hong Chuen TOH, Dr. Rafael Pulido Saclolo, Ms Sally Lee Hsueh Er. We also appreciate the in‐kind support from Sonosite ( https://www.sonosite.com) for the provision of the ultrasound machines for training and CAE for the provision of the simulation mannequin ( https://caehealthcare.com/ultrasound-simulation/vimedix) and support staff.
We sincerely appreciate the Singapore General Hospital Academic Health Sciences Centre for allowing us the use of the teaching facilities and to the Singapore Government HDMP Visiting Experts Program for funding the workshop.
References
- 1.Hanekom SD, Faure M, Coetzee A. Outcomes research in the ICU: an aid in defining the role of physiotherapy. Physiother Theory Pract 2007; 23(3): 125–35. [DOI] [PubMed] [Google Scholar]
- 2.Inglis AJ, Nalos M, Sue KH, Hruby J, Campbell DM, Braham RM, et al. Bedside lung ultrasound, mobile radiography and physical examination: a comparative analysis of diagnostic tools in the critically ill. Crit Care Resusc 2016; 18(2): 124. [PubMed] [Google Scholar]
- 3.Abdalla W, Elgendy M, Abdelaziz AA, Ammar MA. Lung ultrasound versus chest radiography for the diagnosis of pneumothorax in critically ill patients: a prospective, single‐blind study. Saudi J Anaesth 2016; 10(3): 265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouhemad B, Mongodi S, Via G, Rouquette I. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology 2015; 122(2): 437–47. [DOI] [PubMed] [Google Scholar]
- 5.Xirouchaki N, Kondili E, Prinianakis G, Malliotakis P, Georgopoulos D. Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med 2014; 40(1): 57–65. [DOI] [PubMed] [Google Scholar]
- 6.Leech M, Bissett B, Kot M, Ntoumenopoulos G. Lung ultrasound for critical care physiotherapists: a narrative review. Physiotherapy Res Int 2014; 20(2): 69–76. [DOI] [PubMed] [Google Scholar]
- 7.Xirouchaki N, Georgopoulos D. Impact of lung ultrasound on clinical decision making in critically ill patients: response to O'Connor et al.. Intensive Care Med 2014; 40(7): 1063. [DOI] [PubMed] [Google Scholar]
- 8.Ntoumenopoulos G, Hough J. Diagnostic thoracic ultrasound within critical care. J Physiotherapy 2014; 60(2): 112. [DOI] [PubMed] [Google Scholar]
- 9.McKiernan K, Chiarelli P, Warren‐Forward H. Diagnostic ultrasound use in physiotherapy, emergency medicine and anaesthesiology. Radiography 2010; 16: 154–9. [Google Scholar]
- 10.Leech M, Bissett B, Kot M, Ntoumenopoulos G. Physiotherapist‐initiated lung ultrasound to improve intensive care management of a deteriorating patient and prevent intubation: a case report. Physiother Theory Pract 2015; 31(5): 372–6. [DOI] [PubMed] [Google Scholar]
- 11.Arntfield RT. The utility of remote supervision with feedback as a method to deliver high‐volume critical care ultrasound training. J Crit Care 2015; 30(2): 441. e1–6. [DOI] [PubMed] [Google Scholar]
- 12.Dinh VA, Giri PC, Rathinavel I, Nguyen E, Hecht D, Dorotta I, et al. Impact of a 2‐day critical care ultrasound course during fellowship training: a pilot study. Crit Care Res Pract 2015;2015(2090‐1305 (Print)):675041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edrich T, Stopfkuchen‐Evans M, Scheiermann P, Heim M, Chan W, Stone MB, et al. A comparison of web‐based with traditional classroom‐based training of lung ultrasound for the exclusion of Pneumothorax. Anest Analg 2016; 123(1): 123–8. [DOI] [PubMed] [Google Scholar]
- 14.Heiberg J, Hansen LS, Wemmelund K, Sorensen AH, Ilkjaer C, Cloete E, et al. Point‐of‐care clinical ultrasound for medical students. Ultrasound Int Open 2015; 1(2): E58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hulett CS, Pathak V, Katz JN, Montgomery SP, Chang LH. Development and preliminary assessment of a critical care ultrasound course in an adult pulmonary and critical care fellowship program. Ann Am Thorac Soc 2014;11(2325‐6621 (Electronic)):784–8. [DOI] [PubMed] [Google Scholar]
- 16.Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med 2007; 35(5 Suppl): S290–304. [DOI] [PubMed] [Google Scholar]
- 17.Silva JP, Plescia T, Molina N, Tonelli AC, Langdorf M, Fox JC. Randomized study of effectiveness of computerized ultrasound simulators for an introductory course for residents in Brazil. J Educ Eval Health Prof 2016;13(1975‐5937 (Electronic)):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turner EE, Fox JC, Rosen M, Allen A, Rosen S, Anderson C. Implementation and assessment of a curriculum for bedside ultrasound training. J Ultrasound Med 2015;34(1550‐9613 (Electronic)):823–8. [DOI] [PubMed] [Google Scholar]
- 19.Mayo PH, Beaulieu Y, Doelken P, Feller‐Kopman D, Harrod C, Kaplan A, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest 2009; 135(4): 1050–60. [DOI] [PubMed] [Google Scholar]
- 20.Cholley BP, Mayo PH, Poelaert J, Vieillard‐Baron A, Vignon P, Alhamid S, et al. International expert statement on training standards for critical care ultrasonography. Intensive Care Med 2011; 37(7): 1077–83. [DOI] [PubMed] [Google Scholar]
- 21.See KC, Ong V, Wong SH, Leanda R, Santos J, Taculod J, et al. Lung ultrasound training: curriculum implementation and learning trajectory among respiratory therapists. Intensive Care Med 2016; 42(1): 63–71. [DOI] [PubMed] [Google Scholar]
- 22.Via G, Storti E, Gulati G, Neri L, Mojoli F, Braschi A. Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol 2012; 78(11): 1282–96. [PubMed] [Google Scholar]
- 23.Mayo PH, Beaulieu Y, Doelken P, Feller‐Kopman D, Harrod C, Kaplan A, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest 2009;135(1931‐3543 (Electronic)):1050–60. [DOI] [PubMed] [Google Scholar]
- 24.Reissig A, Copetti R, Mathis G, Mempel C, Schuler A, Zechner P, et al. Lung ultrasound in the diagnosis and follow‐up of community‐acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest 2012; 142(4): 965–72. [DOI] [PubMed] [Google Scholar]
- 25.Tutino L, Cianchi G, Barbani F, Batacchi S, Cammelli R, Peris A. Time needed to achieve completeness and accuracy in bedside lung ultrasound reporting in intensive care unit. Scand J Trauma Resusc Emerg Med 2010; 18: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: bedside lung ultrasound in critical care practice. Crit Care 2007; 11(1): 205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nazerian P, Volpicelli G, Vanni S, Gigli C, Betti L, Bartolucci M, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med 2015; 33(5): 620–5. [DOI] [PubMed] [Google Scholar]


