Abstract
Introduction/Purpose
Diagnostic ultrasound of the respiratory system and peripheral muscular systems is increasingly being used by clinicians. The aim of this study was to evaluate the knowledge outcomes of a bespoke one‐day curriculum for physiotherapists that incorporated lung, diaphragm and lower limb muscle diagnostic ultrasound theory and practical training in image acquisition and analysis.
Methods
A one‐day course comprised of three instructors and 32 participants on key diagnostic ultrasound findings of the lungs, diaphragm and lower limb musculature included didactic lectures combined with expert‐led hands‐on training in practical sessions. Participants undertook pre‐ and post‐course knowledge questionnaire covering key ultrasound findings for normal lungs, pleural/pulmonary pathologies and normal and abnormal findings for the diaphragm and key lower limb muscle groups. The pre‐test and post‐test questionnaire and survey results were reported using parametric descriptive statistics (means SD) as the data were normally distributed.
Results
Of the 32 physiotherapists who undertook the one‐day training, 25 (78%) completed the pre‐ and post‐course questionnaires. The pre‐course knowledge scores (mean percentage, SD) were 63% (21), and the post‐course scores were 62% (20) after training.
Discussion
This novel diagnostic ultrasound course led to limited improvements of ultrasound knowledge in the specific areas of the key ultrasound findings pulmonary system and lower limb muscle anatomy. The pre‐reading material and course structure may have been too burdensome for the participants.
Conclusion
Combined lung and muscle diagnostic ultrasound course may require more than the standard one‐day training for appropriate knowledge acquisition, and use of online pre‐course video lectures may facilitate learning.
Keywords: curriculum, diagnostics, education, physical therapy, ultrasonography
Introduction
In the acute care setting, physiotherapists routinely utilise combinations of clinical examination, lung auscultation and the interpretation of the chest radiograph findings to assist with clinical decision‐making about the requirement for and response(s) to chest physiotherapy.1 Thoracic ultrasound has greater diagnostic accuracy and beneficial impact on clinical decision‐making by physicians for the key pulmonary (interstitial syndrome, lung collapse/consolidation) and pleural pathologies (pneumothorax, pleural effusion) when compared to the portable chest radiograph.2, 3, 4, 5 A formal one‐day diagnostic thoracic ultrasound training course specifically designed for respiratory physiotherapists demonstrated improvements in ultrasound knowledge of lung and pleural pathology, image acquisition and image interpretation skills in a subset of the participants with no previous diagnostic thoracic ultrasound knowledge.6
In addition, the evaluation of lower limb muscle quantity and muscle architectural quality utilising diagnostic ultrasound is also being increasingly used in acute care.7 Ultrasound measures of muscle mass (as a surrogate measure of muscle function) can provide accurate muscle quantification and may be combined with measures of physical function as a means of tracking patient progress and evaluating therapy effectiveness in acute care.8 The use of diagnostic muscle ultrasound for clinical and research purposes requires appropriate training.9 Currently, to the best of our knowledge, there is no formal training programme or standardised protocol used to educate clinicians, healthcare providers or researchers in the use of diagnostic ultrasound for muscle health. Importantly, reliability, reproducibility and accuracy should not be assumed with ultrasound image acquisition and any training programmes must also address these aspects.8
Diagnostic ultrasound is not new to physiotherapy;10 however, to the best of our knowledge, it is not routinely utilised by physiotherapists to examine the respiratory system and limb muscle systems in the acute setting. Various short courses have been developed for training medical clinicians in the use of point of care diagnostic ultrasound (POCUS) for lungs and or cardiac function utilising a variety of training methods (simulation based, e‐learning, hands‐on classroom‐based learning), different durations and methods of evaluation.11, 12, 13, 14, 15, 16, 17, 18 The only previous evaluation of a diagnostic lung ultrasound training course for physiotherapists6 reported it to be effective for knowledge acquisition and image interpretation in a small group of 12 respiratory physiotherapists conducted in Singapore. International experts from the key critical care societies (e.g. ESICM, AACP, SRLF) through a consensus of opinion have recommended a framework of training for intensive care physicians required to achieve competence in critical care ultrasonography (inclusive of thoracic, abdominal, vascular and echocardiography).19, 20 Further developments include a consensus statement on characteristic ultrasound signs for key lung and pleural pathologies21 that should be incorporated as part of thoracic ultrasound training programmes. The incorporation of diagnostic ultrasound for the monitoring of lung, diaphragm and limb muscle function within acute care8, 22, 23 provides physiotherapists with accurate bedside tools to identify pulmonary pathology amenable to chest physiotherapy,2, 22, 24 suitability for weaning from mechanical ventilation25 and tracking of muscle function during critical illness and in response to therapy interventions.7 We are not aware of any studies reporting on the educational requirements and efficacy of a training programme that combines limb muscle and thoracic diagnostic ultrasound designed for use in acute care by physiotherapy.
The primary objective of this study was to assess the participant knowledge before and after a one‐day diagnostic lung, diaphragm and lower limb muscle ultrasound curriculum course (including pre‐reading, didactic lectures, practical training and image recognition skills) and participant satisfaction of a group of physiotherapists.
Methods
The one‐day training course (total teaching time of 6.5 h) was run as a post‐congress workshop at the World Confederation of Physical Therapy Conference (WCPT) and conducted on 05 July 2017 and included training of 32 qualified physiotherapists. This study received ethical approval from the University of Technology Sydney HREC (ETH171615).
The one‐day diagnostic ultrasound training course comprised of three instructors and 32 participants involved 2.5 h of didactic lectures and 4 h of expert‐led practical skills training. The methods used for this training programme were based on a previous pilot programme for diagnostic thoracic ultrasound for physiotherapists.6 To optimise participant learning, we included (i) pre‐reading material with two comprehensive review articles that included key aspects of diagnostic thoracic26 and muscle ultrasound,27 (ii) evaluation of participant baseline knowledge with a pre‐course questionnaire, (iii) group training with instructors: trainee ratio of 1:10 (this instructor to participant ratio was used as recommended by course organisers from WCPT to ensure financial viability of the course) being less than the recommended ratio of 1:5 by the Australian Society of Ultrasound Medicine see link http://www.asum.com.au/files/public/Education/CAHPU/CAHPUForms/CAHPU-Unit-Accreditation-Application-Form.pdf) and a (iv) post‐workshop knowledge acquisition test. The full one‐day course content and structure are detailed in Table 1.
Table 1.
Diagnostic ultrasound course curriculum (one‐day course)
| Pre‐reading | Attendees were emailed 1‐week pre‐course, the two review articles: |
| Duration | One‐day course outline |
| 10 min | Pre‐workshop quiz (15 multiple‐choice questions) based on pre‐reading articles |
| 50 min | Didactic lecture: Physics of ultrasound – Knobology/image optimisation |
| 50 min |
Practical stations: Knobology and image optimisation Expert‐led stationsa 10 identical groups of approximately three participants, with each participant acting as models for image optimisation |
|
15 min 15 min |
Didactic Lecture: Normal anatomy: abdomen/thorax landmarks. Didactic Lecture: Normal anatomy: lower limb muscle landmarks. |
| 60 min |
Practical stations:
|
| 30 min |
Didactic lecture: Ultrasound diagnosis of pulmonary conditions
|
|
30 min 30 min |
Didactic lecture: Ultrasound diagnosis of lower limb pathology (including muscle mass and architecture analysis techniques) Quadriceps/Tibialis anterior Practical stations: lower limb pathology 1 and 2a |
| 40 min |
Practical stations: Expert‐led rotating stations (four stations with 40 min at each station)a.
|
| 20 min |
Didactic lecture: Ultrasound applications for physiotherapy in intensive care Didactic lecture: Current use of ultrasound guidance during acute care rehabilitation |
| 20 min | Post‐workshop participant questionnaire evaluating knowledge acquisition from course |
| 10 min | Satisfaction survey of attendees regarding course content and structure |
Only three experts for ALL the practical stations.
The two summary articles26, 27 were emailed to participants approximately one week prior to the one‐day course to enhance learning and reduce the cognitive load during the workshop. The articles covered the basics of diagnostic ultrasound theory and its practical applications in acute care including the identification of the key findings lung/pleural pathology and lower limb muscle ultrasonography in adults. At enrolment prior to course commencement, a 15‐item multiple‐choice survey was administered to evaluate participant baseline knowledge of lung and lower limb muscle ultrasound acquired from the pre‐reading and prior experience26, 27 (see Appendix 1 for further detail). During the course, multiple teaching modalities were applied. These consisted of lecture notes for each session reporting on the educational objectives, including the specific scanning techniques, patient positioning, general anatomy and key pathological findings on ultrasound, live demonstrations using participants for ultrasound imaging of normal findings for thorax/lung/diaphragm and lower limb muscles, tutoring during live ultrasound imaging of course participants for normal image identification, acquisition and image optimisation procedures, the use of phantom models (for imaging of simulated pleural effusions) and tutor guidance for the ultrasound identification lung and pleural pathology using patient video clips (de‐identified). Lecture notes for each session were developed describing intended learning outcomes and included specifics on scanning techniques, patient positioning, general anatomy and clinical relevance. A post‐course questionnaire was based on the ultrasound learning goals and included 30 multiple‐choice questions covering key aspects from the one‐day course (see Appendix 2).
Descriptive statistics
Summary (mean, SD) and descriptive statistics of participants scores (percentage correct) on pre‐ and post‐course questionnaires and the participant evaluations of course satisfaction were reported using Microsoft Excel (version 15.4).
Results
Thirty‐two physiotherapists participated in this training programme, with a 78% response rate (25/32) to the questionnaires (2 Australia, 5 South Africa, 3 Singapore, 2 Chile, 2 Canada, 2 Iran, 1 New Zealand, 1 Switzerland, 1 Brazil, 1 Nigeria, 1 East Africa, 2 West Africa, 1 Pakistan, 1 United Arab Emirates, 1 unknown). Participants had a median of 13 (7–21) years of clinical experience as working registered physiotherapists, and 70% of participants reported no prior experience in the use of diagnostic ultrasound with most of the remaining participants (30%) reporting some experience with use of ultrasound for musculoskeletal management (Table 2).
Table 2.
Professional experience
| Professional experience | Results |
|---|---|
| Years of work (median, IQR) | 13 (7–21) |
| Areas of work* | |
| Intensive care | 11 |
| Medical/surgical wards | 10 |
| University | 9 |
| Emergency ward | 1 |
| Other | 7 |
The participants often worked in multiple areas.
The percentage of correct answers for the 15 pre‐course questions (mean, SD) were 61% (23). The question on ultrasound appearances of lung consolidation and the 2 questions muscle fibre types and fibre arrangement scored lowest with less than 40% correct.
The percentage of correct answers for the 30 post‐course questions (mean, SD) were 62% (20). Two questions on the ultrasound signs of pneumothorax and three questions on muscle fibre arrangement, recommendations for ultrasound measurement technique of tibialis anterior and muscle fibre physiology scored lowest with less than 40% correct.
To explore the potential impact of the participants pre‐reading, we report on the pre‐course and post‐course results. Of the three participants out of 25 who completed all the pre‐reading, the mean (SD) pre‐course score was 84% (8), for the 16 of 25 participants who only partially completed the pre‐reading (unknown which of the specific content or articles were undertaken) 60% (26) and for the remaining participants who did not do the pre‐reading 52% (24). For the post‐course scores, the mean (SD) of the three of 25 participants who completed all the pre‐reading was lower than their pre‐course score at 73% (9), for the 16 of 25 who only partially completed the pre‐reading, their mean post‐course score was unchanged at 60% (27), and of the remaining participants who did not do the pre‐reading, their mean post‐course score was higher at 62% (28). The participants who undertook all or partial completion of the pre‐reading demonstrated better knowledge acquisition on the pre‐course questionnaire. Of the participants who undertook all the pre‐reading, they scored higher on the post‐course questionnaire than the other participants. Only the participants who did not undertake their pre‐reading demonstrated greater increase in pre‐ to post‐course knowledge scores compared with those who only partially completed or who undertook all the pre‐reading. But importantly, the participants who did not undertake their pre‐reading achieved lower scores than those that completed the pre‐reading.
Course satisfaction
Of the 32 participants in the course, a maximum of 24 participants responded to the questions on course satisfaction. Twenty participants felt the course pre‐reading was appropriate and that the course was at an appropriate level in terms of theory and practical skill acquisition; however, four felt the course was too advanced. Eighteen of the participants felt that this course would impact on their clinical practice and they felt confident that they would begin to use diagnostic ultrasound in their clinical work, but one reported the absence of an ultrasound machine in their work place as a limitation to the use of ultrasound. Of note, 11 of the 23 participants felt that there was insufficient time allocated to the practical sessions. Of note, several participants identified they would have preferred the course material and questionnaires to be provided in languages other than English. Twenty‐four of the participants rated their satisfaction with of each of the didactic and practical sessions, with further detail provided in Figure 1 below. All of the sessions were most frequently rated as good (except for the lecture on the use of ultrasound for acute care respiratory physiotherapy rated equally frequently at good and excellent and the lecture on use of ultrasound for acute care rehabilitation rated most frequently as excellent).
Figure 1.
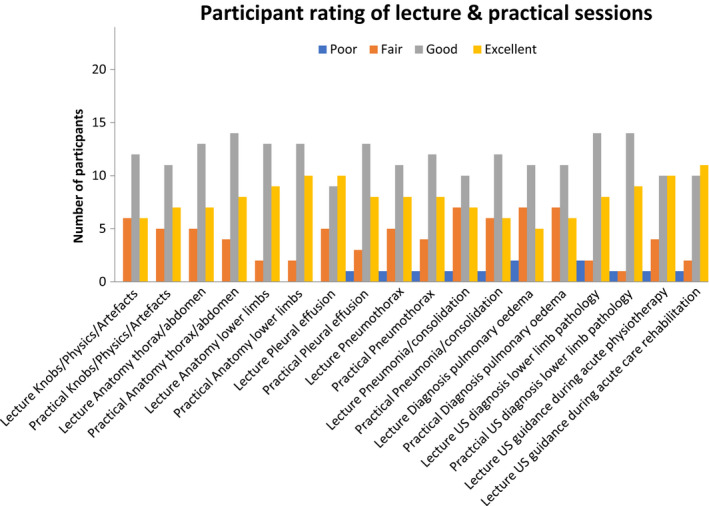
Participant Rating of Lecture and Practical Sessions.
Discussion
This novel intensive one‐day diagnostic ultrasound training programme of lung, diaphragm and lower limb muscle for physiotherapists failed to improve short‐term knowledge acquisition. The high participant to tutor ratio (10:1) and the combination of lung/diaphragm and lower limb muscle ultrasound content to be covered in a single day of training (as compared with previous lung ultrasound alone courses) may have been too burdensome for the participants and provided insufficient training to facilitate further knowledge acquisition beyond the pre‐reading material. In addition, the detailed pre‐course reading material may have also been too burdensome.
In a previous report of the effectiveness of the impact of a curriculum for a one‐day lung ultrasound course,6 more of the participants (58% vs. 12%) reported they had read the recommended pre‐course material. For this course and the previous one‐day lung ultrasound course,6 the pre‐course assessment results (mean, SD) for participants who completed all the pre‐reading was similar at 84% (8) and 81% (8.9), respectively. For the participants in this course who only partially completed the pre‐reading, the pre‐course assessment results (mean, SD) were also similar at 60% (26) as compared to 62% (16.4) for the lung ultrasound course, respectively. As only 12% of participants in this course completed all of the pre‐reading, this indicates that potentially the time available for reading or the amount of pre‐reading material may have been an issue for participants. The absence of improvement in post‐course knowledge questionnaire scores for this current course with combined lung and muscle diagnostic ultrasound may be due to the curriculum content and/or practical skills workshops being too burdensome or inadequate in terms of allocated time and the high participant to instructor ratio. As highlighted previously, 48% of the participants felt that there was insufficient time allocated to the practical sessions. Participant suggestions to improve the course included an increase in the course duration to 2 days (by 10 participants), more time for practical training (three participants) and optimising instructor: participant ratio to enable improved access to instructor feedback as has been recommended with previous training programmes.28
For this course and the previous lung ultrasound course,6 the lung ultrasound knowledge sections of the questionnaire where participants scored poorly (<40%) were the questions associated with the evaluation of lung aeration such as the sliding sign or signs of pneumothorax. The muscle ultrasound questions answered poorly (<40%) related to the understanding of muscle physiology and ultrasound measurement techniques for the tibialis anterior. This should be addressed in future course potentially by including more suitable pre‐reading material (such as video) and e‐learning strategies.
This intensive one‐day diagnostic ultrasound curriculum programme that combined thoracic and lower limb ultrasound pre‐reading, didactic lectures and practical sessions paired with less than adequate instructor:participant ratio was not optimally effective in improving the basic knowledge and image interpretation skills for a cohort of physiotherapists from diverse clinical and or academic backgrounds. Only the participants who did not undertake any of their pre‐reading improved their post‐test knowledge scores. Potentially the pre‐reading provided a useful a strategy in preparation for the workshop, but as the number of participants who undertook all the pre‐reading was so limited, alternative strategies should be used for future courses (e‐learning or limit the quantity of reading material). Additional time may be required (2 days) for courses such as this which combine lung and muscle ultrasound training so as to provide sufficient time for practice and develop knowledge and skills during the practical workshops.
Future programmes could be improved by including the ability to image patients’ real time with key pathologies during the practical training. Given that this will be difficult to arrange, the use of computerised mannequins and phantom models allow for the greater understanding of the key ultrasound findings with lung and or pleural pathologies.17, 29 For competence to be developed, we recommended that the clinicians need to apply the ultrasound skills within their own clinical practice with an expert mentor to further guide image acquisition and interpretation skills, with the participants using a logbook to record and review mentored image acquisitions. The training requirements for physiotherapists to reach competence in diagnostic ultrasound for point of care purposes should include an understanding of the ultrasonographic features of common normal anatomy of the thorax (lungs, heart, pleura) and abdomen (liver, spleen, kidney) and detail acute pleural diseases such as pleural effusion, pneumothorax and parenchymal diseases such as pulmonary oedema, lung collapse and pneumonia20 and lower limb muscle ultrasonography.27 Physiotherapists would need to be able to demonstrate correct acquisition and interpretation of these ultrasound images real time with the correct integration of the ultrasound findings with clinical assessments to facilitate safe and effective practice of physiotherapy. Participants also need to appreciate the limitations of diagnostic ultrasound imaging, understand the clinical governance issues and requirements for further training and skill development (ongoing mentored training) to attain competence. Participants also need to appreciate and be taught about care of the ultrasound machine/probe, especially infection control strategies (either following their hospital's local guideline or a relevant body's guideline).
The number of ultrasound procedures required to achieve competence has been suggested by some to include at least 100 chest ultrasound procedures30 or three months of supervised/mentored practice.31 Some have suggested that if ultrasound procedures are included as part of daily patient care, then diagnostic thoracic ultrasound competence may be achieved within 6 weeks.32 The requirements for the acquisition of limb muscle ultrasound knowledge and competence are unknown. The instructors in the course did not specify or recommend a particular credentialing pathway for attainment of competence as the participants originated from many different countries. We, however, did identify the principles of having an expert mentor at their place of work and utilising a logbook to document procedures undertaken.
There are several limitations to our study. This was a small study and single group intervention with physiotherapists from a wide variety of clinical and or academic backgrounds. We did not evaluate which of the pre‐reading material (lung and or muscle ultrasound) the participants had reviewed. The lack of information gathered on the knowledge retention beyond the course (3–6 months) limited our understanding of knowledge retention. The multiple‐choice questions pre‐ and post‐course differed both in number and in content, and hence, we are unclear as to the real impact of the one‐day training. However, we wanted to ascertain the impact of the training course and hence specifically designed the pre‐course assessment to test the knowledge attained from the pre‐reading material. Also as some of the participants identified a preference for the teaching material and assessments to be provided in their native languages, this must have limited their knowledge acquisition and ability to answer the questionnaire and satisfaction assessments. Importantly, the course was overall favourably reviewed by participants in terms of satisfaction.
Larger investigations are required to evaluate level of training required for physiotherapists to acquire diagnostic ultrasound skills, to apply them in clinical practice, evaluate the quality of imaging and interpretation and then explore the impact of diagnostic ultrasound on clinical decision‐making by physiotherapists.
Conclusion
This pilot programme demonstrated that a novel intensive single‐day diagnostic ultrasound training course in lung, diaphragm and lower limb muscle failed to lead to improvements of ultrasound knowledge of lung, pleural pathology and lower limb muscle in a diverse group of physiotherapists with predominantly nil previous diagnostic ultrasound skills. Limiting the course content, utilising alternative pre‐course learning materials, increased time allocation for practical skill acquisition and greater tutor to participant ratio should translate to improved knowledge acquisition, but requires further investigation.
Declarations of interest
The authors report no declarations of interest.
Disclosure statement
GN, SP and ALM received funding support from the World Confederation of Physical Therapy to undertake the ultrasound workshop. GN and ALN are also regularly supported by Sonosite with in‐kind provision of ultrasound machines for ultrasound training courses. For this course, both Sonosite and GE Medical provided ultrasound machines for the training. SP is currently in receipt of a NHMRC Early Career Research Fellowship (#1111640).
Authorship declaration
The authorship listing conforms with the journal's authorship policy, and all authors are in agreement with the content of the submitted manuscript.
Acknowledgements
We appreciate the in‐kind support from Sonosite (https://www.sonosite.com) and GE Health Care (http://www3.gehealthcare.com/en) for the provision of the ultrasound machines for training and survival technology for the provision of the thorax mannequin (Limbs and Things).
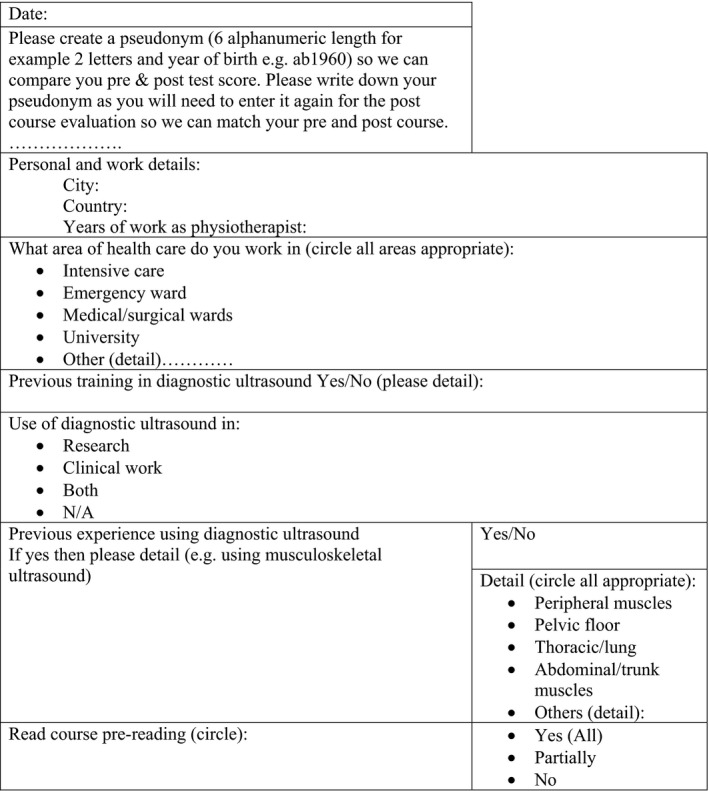
Appendix 1.
Figure A1: Participant details.
Pre‐course knowledge questionnaire
1. Ultrasound waves cannot pass through bone and hence are reflected back
True
False
2. Hyperechoic means
An increase in echogenicity when compared with the surrounding area
A decrease in echogenicity when compared with the surrounding area
An area in an image that is free of echoes and displays acoustic enhancement
3. The advantages of lung ultrasound over standard chest radiograph are:
Non‐invasive
No radiation
Repeatable
Increased sensitivity, specificity and diagnostic accuracy compared with CXR for most acute pathology in ICU acute care
Ideal clinical and research tool
All of the above
4. The sliding/gliding lung sign refers to
Chest wall movement with breathing
Chest wall expansion with respiration
Movement of the visceral and parietal pleura past each other during respiration causing artefacts indicative of aeration of lung in that region
Movement of the diaphragm on respiration
Appearance of the lung sliding beneath a pneumothorax
5. Pulmonary edema is characterized by which of the following ultrasound features?
Sliding‐lung sign
Multiple comet‐tail or B‐lines artifacts in most regions of the lungs
Lung pulse or K‐lines
Hepatization or a liver appearance
None of the above
6. Pleural effusions …
are seen as an echo free or anechoic space between the visceral and parietal pleura
are only seen through the liver
are only seen when scanning through the spleen
can only be detected when they contain over 1000 millilitres of fluid
may be seen with ultrasound, but are more accurately detected by plain chest radiography
7. Alveolar consolidation can demonstrate which of the following findings?
Hepatization of the lung
Double sliding‐lung sign
Air bronchograms
Choices A and C
A, B and C
8. The lung gliding/sliding lung sign
should be checked for in just one location
is seen in normal patients
is a finding noted on trans‐oesophageal echocardiography
is helpful in the evaluation of aeration on the lungs
is accentuated by the presence of a pleural effusion
can only be assessed in the anterior aspects of the chest wall
B and D
9. Lung ultrasound cannot assist in the detection of lung consolidation and pneumonia.
True
False
10. Which statement is true?
A high frequency linear transducer is useful for high resolution superficial imaging
A low frequency transducer is useful for imaging deep structures such as abdominal and thoracic organs.
Both A and B
11. Which of the following muscles have a pennate fibre arrangement?
Sartorius
flexor pollicis longus
Rectus femoris
Both B and C
12. Type 1 fibres have which of the following characteristics:
aerobic, fast speed of contraction and moderate fatigability
anaerobic, fast speed of contraction and high fatigability
aerobic, slow speed of contraction and low fatigability
anaerobic, slow speed of contraction and low fatigability
13. Normal ‘healthy’ muscle on ultrasound has which of the following features
speckled ‘starry’ sky appearance and largely dark
non‐homogenous appearance to the muscle largely hyperechoic
hyperechoic muscle with reduce bone echogenicity
None of the above
14. Pennation angle is defined as:
length of individual muscle fibre in cross‐sectional image
angle between direction of muscle fibres and line of force of action represented by external tendon or aponeurosis
angle of a group of muscle fibres in multi‐pennate muscles only
angle which is observed in paediatric population to describe the development of muscle fibres along the aponeurosis
15. All ‘healthy’ skeletal muscles have the same characteristic appearance on ultrasound imaging:
True
False
Appendix 2.
Post‐course knowledge questionnaire
1. There is enhanced ultrasound transmission through fluids
True
False
2. Anechoic means
An increase in echogenicity when compared with the surrounding area
A decrease in echogenicity when compared with the surrounding area
An area in an image that is free of echoes and displays acoustic enhancement
3. The advantages of lung ultrasound over standard chest radiograph are:
Non‐invasive
No radiation
Repeatable
Increased sensitivity, specificity and diagnostic accuracy compared with CXR for most acute pathology in ICU acute care
Ideal clinical and research tool
All of the above
4. To identify whether your ultrasound probe is over major abdominal organs or in the thorax you should
Use a longitudinal view with the orientation marker on your screen pointing towards the head of the patient
Use a transverse view to allow you to orient the anterior from posterior parts of the chest wall
Look at the patients chest wall and abdomen whilst imaging to ensure you know where you are
None of the above
5. The sliding/gliding sign refers to
Chest wall movement with breathing
Chest wall expansion with respiration
Movement of the visceral and parietal pleura past each other during respiration causing artefacts indicative of aeration of lung in that region
Movement of the diaphragm on respiration
Appearance of the lung sliding beneath a pneumothorax
6. Pleural sliding/gliding is sought first on the anterior chest of a supine patient because …
air collects posteriorly and interferes with visualisation of lung sliding
air collects anteriorly, in the least gravitationally – dependent space
the posterolateral chest wall precludes ultrasound signal transmission
free air within thoracic cavity accumulates in the most dependent position
it is easier and convenient
7. Pulmonary edema is characterized by which of the following ultrasound features?
Sliding‐lung sign
Multiple comet‐tail or B‐lines artifacts in most regions of the lungs
Lung pulse or K‐lines
Hepatization
None of the above
8. All of the following could cause identification of a false lung point (indicative of pneumothorax) except …
Acute Respiratory Distress Syndrome (ARDS)
underlying pathologic lung conditions
heart border
esophageal reflux
a pleural adhesion
ultra‐low tidal volume ventilation during ECMO
9. Pleural effusions …
are seen as an echo free or anechoic space between the visceral and parietal pleura
are only seen through the liver
are only seen when scanning through the spleen
can only be detected when they contain over 1000 millilitres of fluid
may be seen with ultrasound, but are more accurately detected by plain chest radiography
10. One way to estimate the size of a pleural effusion is to:
Use a curvilinear low frequency probe and see how anechoic the collection is
Use a curved low frequency probe in a transverse view at the base of the lung at end of expiration for the septal distance of the effusions and multiply the distance in mm by 20.
None of the above
11. The signs indicating that pulmonary oedema is resolving…
a decrease in the density/number of comet tails throughout the lungs
an increase in the number of comet tails in the upper lung fields
an increase in the number of comet tails in the lower lung fields
an increase in the number of lung rockets
None of the above
12. The presence of a sliding‐lung sign is …
a 100 percent accurate method to detect a pneumothorax
a sign of pulmonary contusion
present only with a pneumothorax
a sign ruling out a pneumothorax only in the location where it is seen
None of the above
13. Alveolar consolidation can demonstrate which of the following findings?
Hepatization of the lung & Air bronchograms
Double sliding‐lung sign & Air bronchograms
Hepatization of the lung & Double sliding‐lung sign
Hepatization of the lung & Air bronchograms & Double sliding‐lung sign
14. The lung pulse indicates aeration and is resultant from…
the transmission of esophageal contraction through the lung parenchyma
the transmission of diaphragmatic contraction through the lung parenchyma
not helpful in the evaluation of a pneumothorax
the transmission of cardiac contractions through the lung parenchyma causing movement of the pleura
15. The pleural gliding/sliding lung sign …
should be checked for in just one location
is never seen in normal patients
is helpful in the evaluation of aeration on the lungs
is accentuated by the presence of a pleural effusion
can only be assessed in the anterior aspects of the chest wall
16. Lung ultrasound can assist in the detection of lung consolidation and pneumonia.
True
False
17. Which statement is true?
A low frequency linear transducer is useful for superficial imaging
The frequency of transducer does not matter when imaging superficial structures
A high frequency linear transducer is useful for high resolution superficial imaging
A curved low frequency transducer can image to about 6 cm depth.
18. Findings consistent with pneumonia on ultrasound include …
stone pulse
lung pulse
air esophagrams
hepatization of the lung tissue with a similar appearance to the liver or spleen
19. Dynamic air bronchograms …
are only seen in intubated patients
are hyperechoic areas that represent air moving through small airways (dilating during inspiration) within areas of lung consolidation
are a highly specific sign suggestive of esophageal rupture
are commonly seen during prolonged apneic episodes
20. Which of the following statements regarding A‐line artifacts is incorrect?
A‐line artifacts are commonly encountered in normal lungs
A‐line artifacts are only seen in pathologic conditions
A‐lines are a type of horizontal reverberation artifact
A‐line artifacts can be seen with pneumothorax
21. The presence of only one or two comet‐tail artifacts in one zone
indicates pulmonary edema
is consistent with a pleural effusion
is common in patients and is considered normal
is seen with a pneumothorax
indicates absent aeration of lung
22. Which of the following muscles have a pennate fibre arrangement?
Sartorius
flexor pollicus longus
Rectus femoris
Both B and C
23. Type 1 fibres have which of the following characteristics:
aerobic, fast speed of contraction and moderate fatigability
anaerobic, fast speed of contraction and high fatigability
aerobic, slow speed of contraction and low fatigability
anaerobic, slow speed of contraction and low fatigability
24. Normal ‘healthy’ muscle on ultrasound has which of the following features
speckled ‘starry’ sky appearance and largely dark
non‐homogenous appearance to the muscle largely hyperechoic
hyperechoic muscle with reduce bone echogenicity
None of the above
25. Pennation angle is defined as:
length of individual muscle fibre in cross‐sectional image
angle between direction of muscle fibres and line of force of action represented by external tendon or aponeurosis
angle of a group of muscle fibres in multi‐pennate muscles only
angle which is observed in paediatric population to describe the development of muscle fibres along the aponeurosis
26. All ‘healthy’ skeletal muscles have the same characteristic appearance on ultrasound imaging:
True
False
27. Recommendation for quadriceps imaging are:
Minimal compression technique, landmarks AIIS and superior border of patellar, 2/3 or " distance between landmarks
Maximal compression technique, landmarks ASIS and superior border of patellar, 2/3 or " distance between landmarks
Minimal compression technique, landmarks ASIS and superior border of patellar, 2/3 or " distance between landmarks
Maximal compression technique, landmarks AIIS and superior border of patellar, 3/5 distance between landmarks
28. Recommendations for tibialis anterior imaging are:
Minimal compression technique, landmarks tibial plateau and superior border of lateral malleolus, 1/3 distance between landmarks
Maximal compression technique, landmarks tibial plateau and superior border of lateral malleolus, 1/3 distance between landmarks
Minimal compression technique, landmarks tibial plateau and superior border of lateral malleolus, 15 cm inferior to tibial plateau
Minimal compression technique, landmarks tibial plateau and inferior border of lateral malleolus, 1/3 distance between landmarks
29. An increase in fascicle length results in a greater number of sarcomeres in parallel?
True
False
30. For muscle ultrasound imaging international standardised protocols exist for describing methods for training, image acquisition, analysis and reporting:
True
False
References
- 1.Hanekom SD, Faure M, Coetzee A. Outcomes research in the ICU: an aid in defining the role of physiotherapy. Physiother Theory Pract 2007; 23(3): 125–35. [DOI] [PubMed] [Google Scholar]
- 2.Inglis AJ, Nalos M, Sue KH, Hruby J, Campbell DM, Braham RM, et al. Bedside lung ultrasound, mobile radiography and physical examination: a comparative analysis of diagnostic tools in the critically ill. Crit Care Resuscit 2016; 18(2): 124. [PubMed] [Google Scholar]
- 3.Abdalla W, Elgendy M, Abdelaziz AA, Ammar MA. Lung ultrasound versus chest radiography for the diagnosis of pneumothorax in critically ill patients: a prospective, single‐blind study. Saudi J Anaesth 2016; 10(3): 265–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bouhemad B, Mongodi S, Via G, Rouquette I. Ultrasound for “lung monitoring” of ventilated patients. Anesthesiology 2015; 122(2): 437–47. [DOI] [PubMed] [Google Scholar]
- 5.Xirouchaki N, Kondili E, Prinianakis G, Malliotakis P, Georgopoulos D. Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med 2014; 40(1): 57–65. [DOI] [PubMed] [Google Scholar]
- 6.Ntoumenopoulos G, Ong HK, Toh HC, Saclolo RP, Sewa WD. Evaluation of a pilot programme on diagnostic thoracic ultrasound curriculum for acute care physiotherapists. Australasian J Ultrasound Med 2017; 20(4): 147–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Parry SM, El‐Ansary D, Cartwright MS, Sarwal A, Berney S, Koopman R, et al. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J Crit Care 2015; 30(5): 1151–e9. [DOI] [PubMed] [Google Scholar]
- 8.Mourtzakis M, Parry S, Connolly B, Puthucheary Z. Skeletal muscle ultrasound in critical care: a tool in need of translation. Ann Am Thorac Soc 2017; 14(10): 1495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cartwright MS, Kwayisi G, Griffin LP, Griffin LP, Sarwal A, Walker FO, et al. Quantitative neuromuscular ultrasound in the intensive care unit. Muscle Nerve 2013; 47(2): 255–9. [DOI] [PubMed] [Google Scholar]
- 10.McKiernan K, Chiarelli P, Warren‐Forward H. Diagnostic ultrasound use in physiotherapy, emergency medicine and anaesthesiology. Radiography 2010; 16: 154–9. [Google Scholar]
- 11.Arntfield RT. The utility of remote supervision with feedback as a method to deliver high‐volume critical care ultrasound training. J Crit Care 2015; 30: 441–e1. [DOI] [PubMed] [Google Scholar]
- 12.Dinh VA, Giri PC, Rathinavel I, Nguyen E, Hecht D, Dorotta I, et al. Impact of a 2‐day critical care ultrasound course during fellowship training: a pilot study. Critical Care Res Pract 2015; 215: 675041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Edrich T, Stopfkuchen‐Evans M, Scheiermann P, Heim M, Chan W, Stone MB, et al. A comparison of web‐based with traditional classroom‐based training of lung ultrasound for the exclusion of Pneumothorax. Anest Analg 2016; 123(1): 123–8. [DOI] [PubMed] [Google Scholar]
- 14.Heiberg J, Hansen LS, Wemmelund K, Sorensen AH, Ilkjaer C, Cloete E, et al. Point‐of‐care clinical ultrasound for medical students. Ultrasound Int Open 2015; 1(2): E58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hulett CS, Pathak V, Katz JN, Montgomery SP, Chang LH. Development and preliminary assessment of a critical care ultrasound course in an adult pulmonary and critical care fellowship program. Ann Am Thorac Soc 2014;6621(2325‐6621(Electronic)):784–8. [DOI] [PubMed] [Google Scholar]
- 16.Neri L, Storti E, Lichtenstein D. Toward an ultrasound curriculum for critical care medicine. Crit Care Med 2007; 35(5 Suppl): S290–304. [DOI] [PubMed] [Google Scholar]
- 17.Silva JA‐O, Plescia TA‐O, Molina NA‐O, Tonelli AA‐O, Langdorf MA‐O, Fox JA‐OX. Randomized study of effectiveness of computerized ultrasound simulators for an introductory course for residents in Brazil. J Educ Eval Health Prof 2016;13(1975‐5937 (Electronic)):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turner EE, Fox JC, Rosen M, Allen A, Rosen S, Anderson C. Implementation and assessment of a curriculum for bedside ultrasound training. J Ultrasound Med 2015;9613(1550‐9613 (Electronic)):823–8. [DOI] [PubMed] [Google Scholar]
- 19.Expert Round Table on Ultrasound in ICU . International expert statement on training standards for critical care ultrasonography. Intensive Care Med 2011; 37(7): 1077–83. [DOI] [PubMed] [Google Scholar]
- 20.Mayo PH, Beaulieu Y, Doelken P, Feller‐Kopman D, Harrod C, Kaplan A, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest 2009;3543(1931‐3543 (Electronic)):1050–60. [DOI] [PubMed] [Google Scholar]
- 21.Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence‐based recommendations for point‐of‐care lung ultrasound. Intensive Care Med 2012; 38(4): 577–91. [DOI] [PubMed] [Google Scholar]
- 22.Leech M, Bissett B, Kot M, Ntoumenopoulos G. Lung ultrasound for critical care physiotherapists: a narrative review. Physiotherapy Res Int 2015; 20: 69–76. [DOI] [PubMed] [Google Scholar]
- 23.Xirouchaki N, Georgopoulos D. Impact of lung ultrasound on clinical decision making in critically ill patients: response to O'Connor et al. Intensive Care Med 2014;40(7):1063. [DOI] [PubMed] [Google Scholar]
- 24.Ntoumenopoulos G, Hough J. Diagnostic thoracic ultrasound within critical care. J Physiotherapy 2014; 60(2): 112. [DOI] [PubMed] [Google Scholar]
- 25.Llamas‐Alvarez AM, Tenza‐Lozano EM, Latour‐Perez J. Diaphragm and lung ultrasound to predict weaning outcome: systematic review and meta‐analysis. Chest 2017; 152: 1140–50. [DOI] [PubMed] [Google Scholar]
- 26.Via G, Storti E, Gulati G, Neri L, Mojoli F, Braschi A. Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol 2012; 78(11): 1282–96. [PubMed] [Google Scholar]
- 27.Arts IM, Pillen S, Schelhaas HJ, Overeem S, Zwarts MJ. Normal values for quantitative muscle ultrasonography in adults. Muscle Nerve 2010; 41(1): 32–41. [DOI] [PubMed] [Google Scholar]
- 28.Greenstein YY, Littauer R, Narasimhan M, Mayo PH, Koenig SJ. Effectiveness of a critical care ultrasonography course. Chest 2017; 151(1): 34–40. [DOI] [PubMed] [Google Scholar]
- 29.Rippey J, Gawthrope I. Creating thoracic phantoms for diagnostic and procedural ultrasound training. Australasian J Ultrasound Med 2012; 15(2): 43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reissig A, Copetti R, Mathis G, Mempel C, Schuler A, Zechner P, et al. Lung ultrasound in the diagnosis and follow‐up of community‐acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest 2012; 142(4): 965–72. [DOI] [PubMed] [Google Scholar]
- 31.Tutino L, Cianchi G, Barbani F, Batacchi S, Cammelli R, Peris A. Time needed to achieve completeness and accuracy in bedside lung ultrasound reporting in intensive care unit. Scand J Trauma Resusc Emerg Med 2010; 18: 44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: Bedside lung ultrasound in critical care practice. Crit Care 2007; 11(1): 205. [DOI] [PMC free article] [PubMed] [Google Scholar]


