Abstract
Background
Point‐of‐care ultrasound (POCUS) is a form of diagnostic ultrasonography, which has a defined role as a clinical adjunct in patient assessment and management. If it is to continue to develop as a core clinical skill, junior medical practitioners and trainees may benefit from dedicated ultrasound education and familiarisation early in their training. Controversy endures, however, as inappropriate use of this highly technical and operator‐dependent imaging modality has negative clinical implications.
Aims
A systematic review was performed to assess the ability of doctors in training to perform clinically appropriate and beneficial diagnostic ultrasound after undergoing a formal training programme.
Methods
Studies meeting pre‐defined inclusion criteria were identified in electronic databases MEDLINE, EMBASE, CINAHL, PUBMED and through Google Scholar. Methodological quality was assessed using an established series of indicators.
Results
Fifteen studies were included in the review. Ten of these were performed in the United States, and eight focused on emergency medicine trainees. After the teaching intervention, ten studies assessed overall ultrasound capacity by calculating the collective sensitivity and specificity of trainee‐performed ultrasound. Five studies used a standardised objective assessment tool to evaluate ultrasound skills and technique. Studies varied in terms of the specific ultrasound use investigated, teaching programmes used and methodological quality. Consistently identified areas for further research included the definition of the trainee learning curve and what constitutes competency in ultrasound.
Conclusions
Ultrasound can feasibly be incorporated into junior medical practitioner training, but more research is required to assess its effectiveness and appropriateness.
Keywords: education; internship, medical; point‐of‐care ultrasound; residency; ultrasonography
Introduction
Point‐of‐care ultrasound (POCUS) is a specific type of clinician‐performed diagnostic ultrasonography, which can assist in patient assessment and management. It is defined as ultrasound brought to the patient and performed in real time.1 POCUS has a number of established applications, especially in emergency departments, ranging from evaluation during the early management of trauma to confirmation of intrauterine pregnancy.2 Its use is limited by its operator‐dependent nature and the negative clinical impact associated with diagnostic error. For this reason, there is a clear need for medical practitioners to be adequately trained in its use. The Australasian College of Emergency Medicine recommends that all training programmes maintain processes allowing trainees to develop skills and experience in ultrasonography.3 It follows that establishing an effective framework for ultrasound skills development earlier rather than later in clinical training would be an opportunity to increase familiarity with this technical imaging modality. However, the overall feasibility and validity of establishing formal ultrasound education for junior medical practitioners and trainees are unclear, as is the clinical impact on patients.
As technological developments continue to improve the affordability, portability and quality of ultrasound machines, together with an increasing appreciation of the possible clinical applications, POCUS will remain a topical area of modern practice.4 The aim of this review is to establish whether doctors in training (trainees) can employ clinically beneficial and appropriate diagnostic ultrasound after undergoing a formal ultrasound education programme.
Methods
A systematic review was performed on literature from January 2000 to September 2015 using MEDLINE, PUBMED, EMBASE and CINAHL databases and Google Scholar. All relevant studies in the English language from these databases were considered. Medical Subject Headings and search strategy are described below – Table 1.
Table 1.
Medical subject headings and search strategy
| Medical subject heading | Entry terms |
|---|---|
| 1. Ultrasonography | Ultrasound Imaging |
| Imaging, Ultrasound | |
| Imagings, Ultrasound | |
| Ultrasound Imagings | |
| Sonography, Medical | |
| Medical Sonography | |
| Ultrasonic Imaging | |
| Imaging, Ultrasonic | |
| Echography | |
| Echotomography | |
| Echotomography, Computer | |
| Computer Echotomography | |
| Tomography, Ultrasonic | |
| Ultrasonic Tomography | |
| Diagnosis, Ultrasonic | |
| Diagnoses, Ultrasonic | |
| Ultrasonic Diagnoses | |
| Ultrasonic Diagnosis | |
| 2. Ultrasonography (subheading) | Ultrasonic diagnosis |
| Echography | |
| Echotomography | |
| 3. Ultrasonography, Doppler | Doppler Ultrasonography |
| Doppler Ultrasound Imaging | |
| Doppler Ultrasound Imagings | |
| Imaging, Doppler Ultrasound | |
| Imagings, Doppler Ultrasound | |
| Ultrasound Imaging, Doppler | |
| Ultrasound Imagings, Doppler | |
| Ultrasound | |
| 4. Education, medical, graduate | Education, Graduate Medical |
| Graduate Medical Education | |
| Medical Education, Graduate | |
| 5. Residency and Internship | Residency and Internship |
| Internship | |
| Internships | |
| Medical Residencies | |
| Residencies, Medical | |
| Residency, Medical | |
| Medical Residency | |
| Residency | |
| Residencies | |
| Residency, Dental | |
| Residencies, Dental | |
| Dental Residencies | |
| Dental Residency | |
| House Staff | |
| House Staffs | |
| Staff, House | |
| Staffs, House | |
| Internship, Dental | |
| Internships, Dental | |
| Dental Internship | |
| Dental Internships |
Searches: (1 or 2 or 3) and (4 or 5).
The databases were accessed by the lead researcher with results corroborated by an experienced coresearcher to maximise the search capability.
Study selection
The search was limited to English language articles to optimise the applicability of results to medical education in English‐speaking countries. The review focuses on published and peer‐reviewed studies, with informal education audits not included.
With these limits set, a study was included if it examined a study group comprised of1 interns/residents/registrars not enrolled in radiology training programmes who2 had no prior formal ultrasound training. This study group3 must then have been subjected to a structured ultrasound teaching programme followed by4 an objective evaluation of the participant's ability to perform ultrasound.
Studies were specifically excluded1 if they solely used non‐conventional ultrasound machines (e.g. low‐resolution hand‐held devices) or2 if they assessed non‐diagnostic uses of ultrasonography for procedures or interventional medicine.
Study abstracts were then examined, and the full text of all relevant papers was read by the lead researcher. The reference lists of all included articles were hand‐searched for further relevant studies that were then assessed for inclusion.
Raw data broadly covering the population, interventions, outcomes and conclusions of each study were extracted from the articles. Quality of included studies was assessed based on a series of 11 quality ‘indicators’ that had been developed by Buckley et al.5 (Table 2). The indicators related to the appropriateness of the study design, conduct, results analysis and conclusions. Evaluation of each study was conducted by two researchers and is presented in Table 3. There were no instances of disagreement requiring resolution. Study characteristics and findings were then compared and discussed.
Table 2.
Series of quality indicators
| Quality Indicator | Process |
|---|---|
| Research question | Assess for clarity |
| Study subjects | Note characteristics of study groups including number, demographics and homogeneity |
| Data collection | What types of data have been collected and does this fit the research question |
| Bias | Have confounding factors and biases been addressed |
| Results | Appropriateness of statistical analysis |
| Conclusions | Relation between conclusions and data presented |
| Reproducibility | What factors limit the study being repeated in another context |
| Study design | Prospective/retrospective |
| Ethical issues | Have ethical issues been adequately addressed |
| Data reliability and context | How do these findings fit with other sources |
Adapted from the series of 11 quality indicators developed by Buckley et al.5
Table 3.
Review table detailing study characteristics and relative rating of methodology and validity
| Origin | Study design | Demographics | Instrument | Results | Conclusions | Limitations | Study quality |
|---|---|---|---|---|---|---|---|
|
BuFstam et al.6 Malaysia 2014 |
Type: bedside echocardiography Setting: ED Teaching: Three‐hour web‐based didactic module, 3 h practical module Assessment: Trainee images compared with cardiologist views |
9 EM trainees with reported low baseline knowledge; series of 100 consecutive stable patients |
Ax: Technical and interpretive skills Measures: ‐Kappa coefficient for agreement |
Variable correlation depending on cardiac views Agreement: Quantitative and qualitative LV functional estimates: 93% Pericardial effusion: 98% IVC diameter assessment: 64.2% |
Able to interpret with reliable accuracy, feasibility of web‐based learning |
Observer effect noted; no control group; low participant numbers; unclear patient selection |
Biases affecting result; subjective diagnostic questions Rated 3/10 |
|
Caronia et al.8 USA 2014 |
Type: Focused vascular sonography Setting: ICU Teaching: 2‐h didactic and practical module Assessment: Trainee images compared with ultrasound technician views |
19 IM trainees; 143 studies on series of 75 consecutive patients with clinical features suggesting lower extremity DVT awaiting formal radiology |
Ax: Ability to achieve diagnosis of DVT Measures: ‐Kappa coefficient for agreement |
Substantial agreement for DVT diagnosis Above knee DVT: sn 97%; sp 63% Common femoral and popliteal DVT: sn 86%; sp 97% Agreement: Kappa: 0.70 No isolated superficial thromboses identified by residents Time from formal ultrasound to report: 14.7 h |
Residents can be trained to perform three‐step U/S examination; more subtle pathology not elucidated | Low number of DVT positive studies; Low number of participants; trainees not blinded to clinical context |
Simplistic diagnostic question; underpowered Rated 3/10 |
|
Caronia et al.7 USA 2013 |
Type: Renal sonography Setting: Inpatients – ICU, general ward, intermediate care Teaching: Five‐hour didactic module, three supervised examinations Assessment: Trainee images compared with formal radiology report |
17 IM trainees with no prior training in stated U/S modality; 125 studies on convenience series of 66 patients |
Ax: Rule out renal obstruction and identify sonographic findings of CKD Measures: ‐Sn and Sp ‐Kappa coefficient for agreement |
Variable agreement depending on renal pathology Hydronephrosis: sn 94%; sp 93% Renal atrophy: sn 100%; sp 83% Echogenicity: sn 40%; sp 98% Renal cysts: sn 60%; sp 96% |
Demonstration that basic skill can be taught | Selection/interest bias – trainees undertaking elective in critical care sonography; substantial variation in number of studies performed by trainees; Not powered to gauge proficiency; image acquisition skills not reported |
Small study; blinded; simplistic employment of U/S
Rated 4/10 |
|
Chalumeau‐Lemoine et al.9 France 2009 |
Type: ICU U/S Setting: ICU Teaching: 8.5‐h didactic teaching, staggered practical sessions Assessment: Trainee images compared with radiologist study |
8 ICU trainees; 129 clinical questions on convenience series of 77 patients; Patients included in series at discretion of intensivist |
Ax: Rule in/out pathology Measures ‐Kappa coefficient for agreement ‐Student's t‐test for time to imaging |
High agreement for immediately clinical relevant questions Most common clinical questions: presence of pleural effusion, presence of obstructive uropathy; signs of chronic renal insufficiency Agreement: Overall: 84.4% (kappa 0.66) Questions with a potential therapeutic implication (retrospective): 95% (kappa 0.86) Time to imaging Trainees vs. radiologists (37 ± 39mins vs. 296 ± 487mins, P = 0.004) |
Limited general u/s interpretation can be taught after brief training; need to better define learning curve and potential patient benefits | Selection bias – inclusion at discretion of intensivist; broad range of U/S uses; competency in ultrasound assessed only by diagnostic accuracy; low number of studies for each question subset |
Competency only assessed by diagnostic accuracy; underpowered Rated 3/10 |
|
Gaspari et al.10 USA 2009 |
Type: RUQ U/S Setting: ED Teaching: 9‐h didactic teaching; at least two practical sessions Assessment: Trainee images recorded and reviewed by expert |
37 EM trainees and 7 attendings (stratified); 352 patient series |
Ax: Identification of gallbladder pathology including image quality, presence of required images Measures ‐Kappa coefficient for agreement |
Interpretive and technical error rates decreasing with experience Agreement: Overall: kappa 0.917 ‐Number of poor‐quality ultrasounds decreasing after average of 7 scans ‐Performance of >25 (point of ‘credentialed’) ultrasound scans: increased agreement ‐Average number of scans before decrease in poor‐quality images: seven scans |
Agreement varied by experience level; supports performance of 25 U/S before clinical competency | Variable informal experience base; non‐specific patient enrolment; no comparison to images attained by experts |
Very specific focus on a very select group of patients limiting transferability of results Rated 5/10 |
|
Gulati et al.11 USA 2015 |
Type: MSK U/S Setting: Inpatients Teaching: web‐based learning, 2‐h didactic; unquantified practical session Assessment: OSCE |
15 IM residents; 3‐month unstructured practical experience |
Ax: Presence of knee effusion with assessment of theory, image acquisition and interpretation Measures: ‐Student's t‐test for pre‐/post‐intervention test scores ‐Descriptive statistics |
Significant improvement in proficiency post‐intervention Statistically significant increase in performance across all OSCE subcomponents Trainee survey: Experience reported as ‘very valuable’ Requested more training examinations
|
Can be feasibly incorporated but institution and educator dependent | Low number participants and focus; variability postulated to relate to individual learning curves; use of Likert scales to gauge trainee impressions; study did not produce expected numbers of positive and negative exams |
High degree of trainee variability in experience over study period; simplistic non‐acute modality of U/S Rated 4/10 |
|
Jacoby et al.12 USA 2007 |
Type: focused vascular sonography (two‐point DVT examination) Setting: ED Teaching: 90‐min mixed didactic and practical session, individual instruction not specified Assessment: Trainee images compared to blinded vascular technician |
Six EM trainees; series of 121 symptomatic extremities |
Ax: Presence of DVT in ‘femoral’ and ‘popliteal’ sties Measures: ‐sn and sp ‐Descriptive statistics
|
High degree of sn and sp Residents identified 8/9 positive cases of acute DVT within target area Overall prevalence of DVT within target area: 7% Overall sn 89% sp 97% |
Limited examination with considerable but not perfect sensitivity | Small sample size, no follow‐up on patient treatment or outcome, not consecutive patients presenting to ED, chronic DVT/partial occlusion counted as ‘no’; low prevalence of positive findings |
Diagnostic accuracy simplistic and underpowered for transferability of findings Rated 3/10 |
|
Jang et al.13 USA 2004 |
Type: compression U/S for proximal lower extremity DVT Setting: ED Teaching: One‐hour didactic teaching with demonstration, no practical component Assessment: Trainee provisional diagnosis vs. subsequently established DVT |
Eight EM trainees; non‐consecutive series of 72 patients |
Ax: presence/absence of proximal DVT Measures: ‐sn and sp
|
High rates of DVT detection 63/72 patients at 1 year follow‐up Overall sn 100% and sp 91.8%
|
High detection rates compromised by selection bias | Non‐consecutive series within less technically challenging patients included; optional participation – ‘US interest bias’; low number of study participants |
Select patient group limiting external validity Rated 4/10 |
|
Jones et al.14 USA 2003 |
Type: bedside echocardiography Setting: ED Teaching: 6‐h didactic course; one‐hour practical component Assessment: Performance on post‐intervention written and practical test |
30 EM residents with non‐cardiac ultrasound experience |
Ax: achieving specified goals and views; U/S theory Measures ‐Paired t‐test |
Statistically significant increase in test scores post‐intervention 9/30 residents excluded as did not attend all instructional material Written score: pre 54% vs. post 76% (P < 0.005) Practical score: pre 56% vs. post 94% (P < 0.005) Significant increase in scores on pre‐/post‐theory and practical |
Increasing scores indicating that minimal competency can be achieved in short time frame | Test not formally validated; practical element performed on healthy volunteers; no control; high dropout rate given voluntary nature of study; no period of knowledge consolidation |
High non‐completion rate affecting results implications of study limited by short time frame Rated 5/10 |
|
Kimura et al.15 USA 2012 |
Type: bedside echocardiography Setting: ICU, cardiology rooms Teaching: curriculum consisting of 10 supervised examinations with 12 h of lectures and 12 h of bedside tuition over each year of study Assessment: Standardised CLUE – clinical examination performed at end of each clinical year |
41 IM trainees assessed over 3‐year residency programme |
Ax: Diagnostic and technical skills; knowledge assessment Measures: ‐descriptive statistics ‐inferential statistics ‐Likert survey |
High rate of competency 8/41 trainees failed to achieve >80% competency in final CLUE assessment No correlation between CLUE pass rate and general academic performance, chief resident selection, gender Questionnaire finding self‐reported change in clinical behaviour |
U/S competency not linked to academic performance; feasibility in terms of costs when in‐hospital resources used | Resident experience and performance subjective; convenience series of studies; skillset development reliant on informal ad‐hoc learning |
Designed to rigorously test uptake and application of new skills; clear objective assessment Rated 7/10 |
|
MacVane et al.16 USA 2012 |
Type: TVUS for intra‐uterine pregnancy Setting: ED Teaching: one‐hour didactic lecture with theoretical competency examination; 10 observed TVUS attempts Assessment: Immediate diagnostic assessment with images videotaped and reviewed by expert |
22 EM trainees; 75 TVUS performed; Residents with established no prior experience in TVUS |
Ax: presence/absence of intrauterine pregnancy Measures: ‐Kappa coefficient for agreement |
High degree of correlation observed Correlation: Overall: 91.1% By PGY: PGY‐1 – 100%; PGY‐2 – 92.1%; PGY‐3 – 93.3% |
Concordance related to PGY; PGY‐1 outperformance suggesting level of experience no limitation to U/S training; supports early education in residency | Unquantified previous general ultrasound experience; small number in study; convenience sample; assumption that supervising clinician did not assist trainee |
Key biases discussed; technical modality of general U/S Rated 6/10 |
|
Poulsen et al.17 Denmark 2015 |
Type: abdominal U/S Setting: ED Teaching: 8‐h didactic lectures and practical sessions Assessment: Images saved and results correlated with definitive diagnosis post‐formal imaging/investigation |
Three general/intern trainees; series of 45 patients |
Ax: diagnosis of acute abdomen Measures ‐Descriptive statistics |
High proportion of images obtained clinically relevant 21/45 patients proceeded to specified definitive investigation and therefore included 14/21 patients had diagnostic agreement Qualitative image assessment: Useful images on all abdominal organs for all patients except large bowel and pancreas |
Junior trainees can correctly identify pathology and abdominal structures after short intervention | Participating intern potentially also the treating physician and not blinded to clinical presentation; education intervention details not provided (course not devised for project) |
Limited transferability of results; very low number of participants and scan rate Rated 3/10 |
|
Schnobrich et al.18 USA 2013 |
Type: general U/S Setting: no specific Teaching: 30 h of training over five‐day course – online, didactic and practical elements Assessment: Competency assessment pre‐/post‐teaching intervention |
32 IM trainees |
Ax: theoretical test; practical assessment on simulators and test subject Measures ‐Descriptive statistics ‐Paired t‐test ‐Likert survey |
Demonstrated increase in capability 29/32 trainees completed pre‐test and 25/32 completed post‐test Test scores: ‐Group 1: pre‐test A score 36% post‐test B score 73% (P < 0.001) ‐Group 2: pre‐test B score 43% post‐test A score: 75% (P < 0.001) Survey results: ‐pre/post: increased perceived skill in image acquisition, interpretation and clinical application (all P < 0.001) ‐Usefulness and relevancy rated 4.6/5; practicability of U/S rated 4.5/5 |
Successful in preparing interns to perform supervised scans; suggests that change in resident behaviour observed | Broad use of ultrasound assessed; no intervening clinical exposure for duration of study period; low number of participants |
Results in keeping with expected improvement after intervention; uncertain clinical relevance for trainees Rated 5/10 |
|
Tolsgaar et al.19 Denmark 2015 |
Type: TVUS Setting: Gynaecology clinics Teaching: participants randomised to intervention group receiving competency‐based simulation training in addition to clinical training – one‐hour didactic lecture followed by supervised practical sessions Assessment: Competency assessment involving expert review of recorded images 2 months post‐intervention |
33 O+G trainees completing on average 58 and 63 scans in intervention and control groups respectively |
Ax: image acquisition, interpretation, documentation and subsequent clinical decision making Measures ‐Descriptive statistics ‐Inferential statistics |
Simulation‐intervention group achieving higher assessment scores 26/33 randomised residents completing study requirements and analysed Assessment ‐Mean performance scores intervention group vs. control group (59.1% vs. 37.6%, P < 0.001) ‐Achievement of pre‐determined pass rate intervention group vs. control group (85.7% vs. 8.3%, P < 0.001) |
Simulation led to a substantial improvement in clinical performance at 2 months | Degree of patient variability in both consolidation phase and assessment; external factors not assessed ‐ monetary, time, transferability; pass/fail scoring on final assessment; unclear level of clinical supervision during study period for each participant |
Simulators and performance indicators validated in literature; poor external validity to other ultrasound modalities Rated 7/10 |
|
Unluer20 Turkey 2010 |
Type: Abdominal US Setting: ED Teaching: 3‐h didactic and 3‐h practical training Assessment: Trainee diagnosis compared with definitive investigation or patient follow‐up |
4 EM trainees; series of 174 patients |
Ax: presence/absence of SBO Measures ‐Descriptive statistics ‐sn and sp |
High degree of accuracy demonstrated Presence of SBO ‐Sn: 97.7% ‐Sp: 92.7% ‐PPV: 93.3% ‐NPV: 97.4% ‐LR: 13.4 84/90 true positives; 76/78 true negatives No significant difference between bedside ultrasonography and radiographer performed study |
Trainees consistently able to diagnose SBO on U/S | Clinical status of patient known to trainee; small number of trainee participants |
Results limited by key biases and low number Rated 3/10 |
U/S, Ultrasound; LV, left ventricle; ICU, intensive care unit; ED, emergency department; IM, internal medicine/physician; DVT, deep vein thrombosis; sp, specificity; sn, sensitivity; PPV, positive predictive value; NPV, negative predictive value; LR, likelihood ratio; Ax, assessment; OSCE, objective structured clinical examination; MSK, musculoskeletal; CLUE, cardiovascular limited ultrasound examination; TVUS, transvaginal ultrasound; PGY, postgraduate year; SBO, small bowel obstruction.
Results
The primary database search yielded a total of 630 articles after removal of duplicates.
The titles and abstracts were accessed for these papers with 603 not meeting inclusion criteria. In addition, three articles had no full text in English language and were therefore excluded. A single further study that met inclusion criteria was identified on review of reference lists.
The 25 articles were read in full and ten were excluded with 15 papers in total included in the review.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20 Of the excluded papers, five had heterogeneous study groups which included or focused on more senior clinicians, three did not objectively assess the study group post‐intervention, and two did not have a practical image acquisition component to the assessments. A study flowchart is provided in Figure 1.
Figure 1.
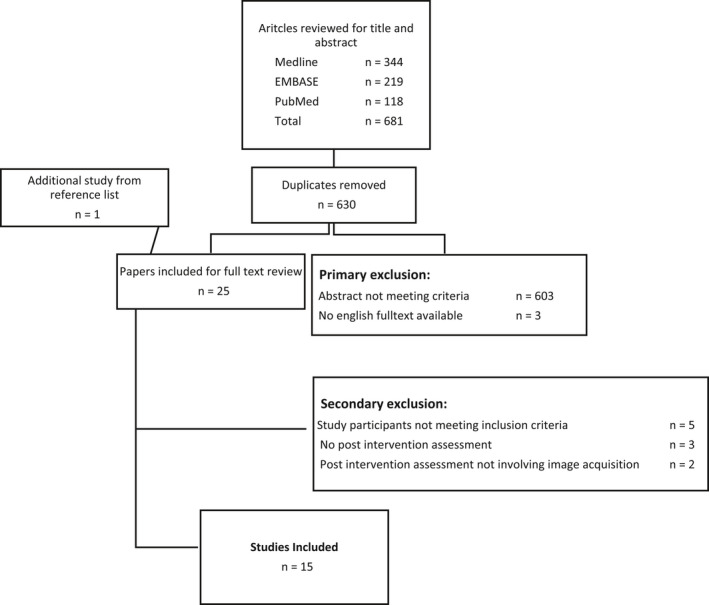
Study inclusion flowchart.
Study characteristics
Ten studies were performed in the United States, with two performed in Denmark and one each in France, Malaysia and Turkey. The type of ultrasound varied among studies, with four targeting abdominal ultrasound, three on deep venous thrombosis assessment, three on echocardiography, two on transvaginal ultrasound, one on focused renal sonography, one on intensive care ultrasonography and one on general abdominal and thoracic ultrasound. Eight studies had groups consisting of emergency medicine (EM) trainees. Of the remaining, four targeted internal medicine trainees, one obstetrics and gynaecology (O+G) trainees and one intensive care unit (ICU) trainees. The final study focused on first‐year postgraduate interns in a compulsory 6‐month emergency medicine rotation.
Type of teaching intervention
The teaching intervention provided to trainees varied between studies. All but one study included a clear practical component to the training programme and 13 further specified that participants were given individualised instruction and assistance during this practical teaching. The cumulative hours of didactic and practical teaching over the study period ranged from a single one‐hour course to 72 h staged and integrated over three years. Nine studies reported the total number of teaching hours at an average of 7.5 h. Five of the studies provided ultrasound instruction over a period of time, rather than in a continuous block of education, allowing for learning consolidation between education sessions.
Performance of trainees
Of the included studies, ten assessed the accuracy of trainee‐performed ultrasound in answering specific diagnostic questions by comparing the cohort's collective results to a ‘gold standard’ investigation. The remaining five studies evaluated trainee performance individually with an objective practical examination‐style assessment at the end of the study period.
For the former 10 studies, the number of trainees included ranged from three to 37 (average – 12.8) performing from 45 to 352 ultrasound scans (average – 133.6) during the study period. The overall sensitivity of trainee‐performed ultrasound ranged from 40% to 100% and the specificity ranged from 88% to 96%. Three studies focused on the rate of agreement between ultrasound images obtained by an ‘expert’ and those obtained by the trainees, with the degree of correlation ranging from 64.2% to 98% across a variety of views and diagnostic questions.
Of the five studies assessing trainees individually, all demonstrated statistically significant increases in trainee performance across pre‐specified domains following the education intervention. A high degree of study design variation was observed, and this precluded direct comparison of participant scores in the objective assessments.
Study quality
Overall, the methodological quality of available studies was poor. For the group of 10 studies defined above as those reporting sensitivity and specificity of trainee‐performed ultrasound, key biases introduced through patient selection were noted in seven. These included unclear selection processes, use of convenience samples of patients and inclusion at the discretion of study participants/assessors. It was also noted in six of the studies that there were low participation rates of trainees and a low proportion of positive ultrasound findings.
Generally, the remaining five studies which followed cohorts of trainees and assessed individual performance at an examination had higher methodological quality. Here, two studies cited low participation rates as a key weakness, with another two noting that ultrasound was not assessed in a way that reflected its broader clinical use. Three studies had a significant period of unstructured and unstandardised education occurring between the teaching intervention and the examination assessment which confounded results. Conversely, the two other studies which assessed trainees immediately after the teaching intervention could less convincingly demonstrate skill uptake and retention.
Discussion
The literature consistently finds that a limited but potentially useful degree of proficiency in diagnostic ultrasound is attainable for junior trainees. Ultrasound repeatedly demonstrated high sensitivity and specificity in the hands of trainees. This was especially pronounced in studies which simplified the imaging goals to address specific clinical questions with binary outcomes (abnormality present/absent).
Trainee aptitude
Individual trainees differed in aptitude for ultrasound, potentially reflecting varying degrees of interest and willingness to pursue ad‐hoc teaching during the study period. Interestingly, several studies found that ultrasound performance did not relate to overall academic merit or even postgraduate year, but was simply correlated with the overall number of scans performed.10, 15, 16 This would support early implementation of ultrasound training for junior practitioners, and potentially even undergraduates.
Trainee perceptions and limitations
Studies which included participant surveys found a general willingness on the part of the trainees to learn ultrasound and reported that its benefits were appreciated. However, a distinction must be drawn between a formal ultrasound study performed by a qualified sonographer and one obtained by a trainee. Apprehensions do exist that the apparent benefits for trainees are muted by the potential for harm from over, under and misdiagnosis.21 It follows that the overall purpose of teaching ultrasound to trainees must be clearly defined. The benefits of POCUS rely on its judicious use as a clinical adjunct with formal validation of findings sought when appropriate. A study by Craig et al. found that in Australian Emergency Departments, clinicians with formal ultrasound training were more likely to seek independent confirmation of findings.22 Therefore, formalising ultrasound training for trainees could foreseeably be accompanied by a heightened awareness of the limitations.
Providing ultrasound education
The amount of training provided in the studies was variable, ranging from comprehensive education programmes integrated into residencies to a single short didactic session. In general, studies which assessed the cumulative diagnostic performance of a cohort of trainees on a series of patients had briefer educational programmes. These studies were also less likely to include quantitative endpoints, such as specific measurements of anatomical structures, in their assessment of trainee performance. Over‐simplification of the diagnostic process adds to concerns over the reliability of inexperienced users employing diagnostic ultrasound independently. In this way, the parameters for what constitutes proficiency and competency in ultrasound are yet to be convincingly defined. This complicates the development of a model education program for trainees. The feasibility of an ultrasound training programme is supported by the majority of studies, however, with its incorporation into junior practitioner training ideally guided by collaborative debate and application of education theory.23
Limitations of the study
It is acknowledged that small sample size, low prevalence of positive findings, heterogeneity of interventions and study outcome measures and selection bias all reduced the external validity of the included studies. In addition, the value of reporting cumulative sensitivity and specificity was reduced by the operator‐ and patient‐dependent nature of ultrasonography. These factors restricted the extent to which the clinical utility of trainee ultrasound could be explored. Many studies highlighted an assumed clinical benefit, but more research is required to establish this. Other key limitations are the inclusion of English language studies alone and the inability to comprehensively search for conference abstracts and reports, which may contain other experiences.
Conclusion
This review indicates that ultrasound training can feasibly be incorporated into junior medical practitioner training. However, the clinical impact of such training programmes could not be clearly defined. In this regard, the studies consistently called for further research, particularly into the point at which a trainee achieves competency. If competency is a function of experience, there is an impetus to develop a foundation for ultrasound proficiency early in clinical training. Ultimately, diagnostic ultrasound, and POCUS more specifically, is a patient assessment adjunct which has the potential to confer significant benefit by addressing important clinical questions. Its use is, however, firmly reliant on an appreciation and understanding of its limitations.
Acknowledgements
No funding was provided for this research.
References
- 1.Moore CL, Copel JA. Current concepts: point‐of‐care ultrasongoraphy. New Engl J Med 2011; 364(8): 749–57. [DOI] [PubMed] [Google Scholar]
- 2.ACEM . Policy on the use of focussed ultrasound in emergency medicine. Melbourne, Victoria: Australasian College for Emergency Medicine; 2016. [Google Scholar]
- 3.ACEM . Policy on the use of bedside ultrasound by emergency physicians. Melbourne, Victoria: Australasian College for Emergency Medicine; 2012. Contract No.: P21. [Google Scholar]
- 4.Wilson S, Mackay A. Ultrasound in critical care. CEACP 2012; 12(4): 190–4. [Google Scholar]
- 5.Buckley S, Coleman J, Davison I, Khan KS, Zamora J, Malick S, et al. The educational effects of portfolios on undergraduate student learning: a Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 11. Med Teach 2009; 31(4): 282–98. [DOI] [PubMed] [Google Scholar]
- 6.Bustam A, Noor Azhar M, Singh Veriah R, Arumugam K, Loch A. Performance of emergency physicians in point‐of‐care echocardiography following limited training. EMJ 2014;31(5):369–73. [DOI] [PubMed] [Google Scholar]
- 7.Caronia J, Panagopoulos G, Devita M, Tofighi B, Mahdavi R, Levin B, et al. Focused renal sonography performed and interpreted by internal medicine residents. J Ultrasound Med 2013; 32(11): 2007–12. [DOI] [PubMed] [Google Scholar]
- 8.Caronia J, Sarzynski A, Tofighi B, Mahdavi R, Allred C, Panagopoulos G, et al. Resident performed two‐point compression ultrasound is inadequate for diagnosis of deep vein thrombosis in the critically III. J Thromb Thrombolysis 2014; 37(3): 298–302. [DOI] [PubMed] [Google Scholar]
- 9.Chalumeau‐Lemoine L, Baudel JL, Das V, Arrive L, Noblinski B, Guidet B, et al. Results of short‐term training of naive physicians in focused general ultrasonography in an intensive‐care unit. Intensive Care Med 2009; 35(10): 1767–71. [DOI] [PubMed] [Google Scholar]
- 10.Gaspari RJ, Dickman E, Blehar D. Learning curve of bedside ultrasound of the gallbladder. J Emerg Med 2009; 37(1): 51–6. [DOI] [PubMed] [Google Scholar]
- 11.Gulati G, Alweis R, George D. Musculoskeletal ultrasound in internal medicine residency – a feasibility study. J Community Hosp Intern Med Perspect 2015; 5(3): 27481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacoby J, Cesta M, Axelband J, Melanson S, Heller M, Reed J. Can emergency medicine residents detect acute deep venous thrombosis with a limited, two‐site ultrasound examination? J Emerg Med 2007; 32(2): 197–200. [DOI] [PubMed] [Google Scholar]
- 13.Jang T. Resident‐performed compression ultrasonography for the detection of proximal deep vein thrombosis: fast and accurate. Acad Emerg Med 2004; 11(3): 319–22. [DOI] [PubMed] [Google Scholar]
- 14.Jones AE. Focused training of emergency medicine residents in goal‐directed echocardiography: a prospective study. Acad Emerg Med 2003; 10(10): 1054–8. [DOI] [PubMed] [Google Scholar]
- 15.Kimura BJ, Amundson SA, Phan JN, Agan DL, Shaw DJ. Observations during development of an internal medicine residency training program in cardiovascular limited ultrasound examination. J Hosp Med 2012; 7(7): 537–42. [DOI] [PubMed] [Google Scholar]
- 16.MacVane CZ, Irish CB, Strout TD, Owens WB. Implementation of transvaginal ultrasound in an emergency department residency program: an analysis of resident interpretation. J Emerg Med 2012; 43(1): 124–8. [DOI] [PubMed] [Google Scholar]
- 17.Poulsen LlC, Bækgaard ES, Istre PG, Schmidt TA, Larsen T. Establishment of ultrasound as a diagnostic aid in the referral of patients with abdominal pain in an emergency department – a pilot study. Open Access Emerg Med 2015;00:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schnobrich DJ, Olson AP, Broccard A, Duran‐Nelson A. Feasibility and acceptability of a structured curriculum in teaching procedural and basic diagnostic ultrasound skills to internal medicine residents. J Grad Med Educ 2013; 5(3): 493–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tolsgaard MG, Ringsted C, Dreisler E, Norgaard LN, Petersen JH, Madsen ME, et al. Sustained effect of simulation‐based ultrasound training on clinical performance: a randomized trial. Ultrasound Obstet Gynecol 2015; 46(3): 312–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unluer EE, Yavasi O, Eroglu O, Yilmaz C, Akarca FK. Ultrasonography by emergency medicine and radiology residents for the diagnosis of small bowel obstruction. Eur J Emerg Med 2010; 17(5): 260–4. [DOI] [PubMed] [Google Scholar]
- 21.Solomon S, Saldana F. Point‐of‐care ultrasound in medical education – stop listening and look. N Engl J Med 2014; 370(12): 1083–5. [DOI] [PubMed] [Google Scholar]
- 22.Craig S, Egerton‐Warburton D, Mellett T. Ultrasound use in Australasian emergency departments: a survey of Australasian College for Emergency Medicine Fellows and Trainees. Emerg Med Australas 2014; 26(3): 268–73. [DOI] [PubMed] [Google Scholar]
- 23.Hayward M, Chan T, Healey A. Dedicated time for deliberate practice: one emergency medicine program's approach to point‐of‐care ultrasound (PoCUS) training. Can J Emerg Med 2015; 17(5): 558–61. [DOI] [PubMed] [Google Scholar]


