Despite the undoubted progress achieved with the first vaccines against SARS-CoV-2 infection, the COVID-19 pandemic continues to affect thousands of people across the globe, particularly in those countries where vaccination is still incipient or the resources available to deal with the virus are scarce. In addition to this serious situation, we are faced with the challenge of managing new cases in subgroups of fully vaccinated people who have a high risk of developing severe COVID-19. As a result, the search for potential treatments against COVID-19 continues, seeking to identify therapies with antiviral activity or capable of modulating the increased, and not always predictable, inflammatory response observed in some patients. In this regard, the repurposing of drugs previously approved for other conditions remains a major strategy in the fight against the virus. This search should not only focus on safe and effective molecules, but also on those that are easy to administer, and whose manufacturing and distribution costs contribute to reducing resource inequities, especially in low-income countries, in order to preserve the health of the most disadvantaged patients.
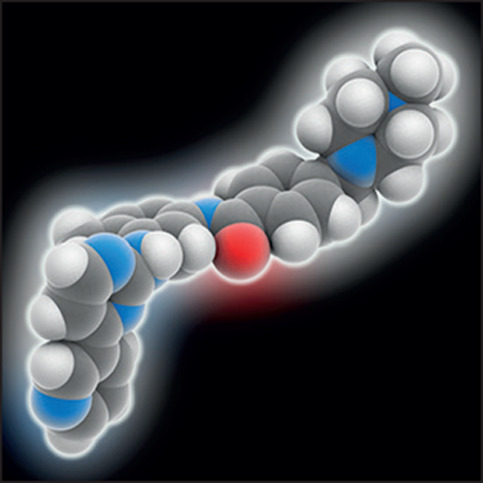
Imatinib mesilate, the main BCR–ABL tyrosine-kinase inhibitor, might fulfil these criteria. Although the potential of imatinib has scarcely been explored in COVID-19,1 this drug has been widely used as first-line therapy in chronic myeloid leukaemia and is also indicated for other conditions (eg, gastrointestinal stromal tumours), showing a safety profile that could be considered optimal since its first approval 20 years ago. During this time, other potential effects of imatinib have been identified, such as antiviral properties against other β-coronaviruses in vitro by hindering the early stages of the virus lifecycle.2 However, the precise effect of imatinib on SARS-CoV-2 viability remains controversial due to the inconsistent results of preclinical studies.3, 4 Additionally, the possibility that imatinib exerts antiviral effects through mechanisms not directly related to impairment of virus–cell interactions, such as the upregulation of genes involved in the response against viruses, cannot be ruled out.5 These unknowns represent some of many challenges to be clarified in relation to the use of this tyrosine-kinase inhibitor as an antiviral.
Imatinib has also been suggested as a possible immunomodulator capable of reducing pro-inflammatory cytokines, chemokines, and vascular adhesion molecules, according to preclinical models and observations in a small number of patients with chronic inflammatory diseases or chronic myeloid leukaemia.6, 7 However, the molecular mechanisms by which this drug might exert this immunomodulatory role are not completely clear and also need to be further elucidated.
Finally, imatinib has been linked to preventing pulmonary endothelial barrier dysfunction observed in some inflammatory conditions, which might lead to a mitigation of pulmonary capillary leak. In The Lancet Respiratory Medicine, Jurjan Aman and colleagues8 investigated this potential effect in the first randomised, double-blind, placebo-controlled clinical trial evaluating imatinib in hospitalised patients with COVID-19 requiring supplemental oxygen to maintain a peripheral oxygen saturation of greater than 94%. According to their results, treatment with imatinib did not change the time to discontinuation of supplemental oxygen and mechanical ventilation for more than 48 consecutive hours (unadjusted hazard ratio [HR] 0·95 [95% CI 0·76–1·20]; primary endpoint). However, compared with the placebo group, mortality at 28 days (unadjusted HR 0·51 [0·27–0·95], p=0·034), duration of mechanical ventilation (median duration 12 days [IQR 6–20] vs 7 days [3–13]; p=0·0080), and length of intensive care unit stay (median duration 15 days [7–21] vs 8 days [5–13]; p=0·025) were lower in patients in the imatinib group. Additionally, the safety profile of imatinib also appeared to be optimal after a thorough analysis of its side-effects, consistent with data available from its usual indications.
These findings give reason for hope, as they point to a broadening of the therapeutic arsenal against COVID-19, but they should be interpreted with caution. In this regard, a study follow-up duration of longer than 28 days would have been more informative, allowing a clearer judgment on survival and the possible occurrence of hospital readmissions, which could have an unmeasured effect on the reported results. Similarly, other open questions to be investigated in further studies are related to the optimal dosage and duration of imatinib treatment, the best time to start treatment after symptom onset, and the possible interactions when taken in combination with other drugs, such as dexamethasone (given to 276 [72%] of 385 patients in the study8), which could decrease exposure to imatinib due to its CYP3A4-inducing action.9
Since the pandemic started approximately one and a half years ago, we have learned that we should temper our enthusiasm on receiving initial data for a potentially beneficial treatment in COVID-19, especially after witnessing unexpected results of randomised trials of previous therapeutic approaches involving sufficiently large numbers of patients. This fact will undoubtedly be conditioning our view of new therapies against SARS-CoV-2 infection until the inherent uncertainties can be resolved. In other words, we have also learned not to succumb to so-called optimism bias10 as easily as we did at the beginning of this unprecedented global health crisis. It is precisely this evolving view that calls again for a thoughtful judgment of promising data from well known drugs repurposed as treatments for new challenges, such as COVID-19.
DB-B is the principal investigator of a non-sponsored randomised trial investigating the role of imatinib and baricitinib in patients with COVID-19 (NCT04346147); AM-O, AIF-S, JGdT and JVSM-L are co-investigators in this project.
References
- 1.Morales-Ortega A, Rivas-Prado L, Frutos-Pérez B, et al. Early clinical experience with imatinib in COVID-19: searching for a dual effect. J Infect. 2021;82:186–230. doi: 10.1016/j.jinf.2021.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coleman CM, Sisk JM, Mingo RM, Nelson EA, White JM, Frieman MB. Abelson kinase inhibitors are potent inhibitors of severe acute respiratory syndrome coronavirus and Middle East respiratory syndrome coronavirus fusion. J Virol. 2016;90:8924–8933. doi: 10.1128/JVI.01429-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Han Y, Duan X, Yang L, et al. Identification of SARS-CoV-2 inhibitors using lung and colonic organoids. Nature. 2021;589:270–275. doi: 10.1038/s41586-020-2901-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao H, Mendenhall M, Deininger MW. Imatinib is not a potent anti-SARS-CoV-2 drug. Leukemia. 2020;34:3085–3087. doi: 10.1038/s41375-020-01045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galimberti S, Petrini M, Baratè C, et al. Tyrosine kinase inhibitors play an antiviral action in patients affected by chronic myeloid leukemia: a possible model supporting their use in the fight against SARS-CoV-2. Front Oncol. 2020;10 doi: 10.3389/fonc.2020.01428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ciarcia R, Vitiello MT, Galdiero M, et al. Imatinib treatment inhibit IL-6, IL-8, NF-KB and AP-1 production and modulate intracellular calcium in CML patients. J Cell Physiol. 2012;227:2798–2803. doi: 10.1002/jcp.23029. [DOI] [PubMed] [Google Scholar]
- 7.Hui KP, Cheung MC, Lai KL, et al. Role of epithelial-endothelial cell interaction in the pathogenesis of SARS-CoV-2 infection. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab406. https://doi.org//10.1093/cid/ciab406 published online May 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aman J, Duijvelaar E, Botros L, et al. Imatinib in patients with severe COVID-19: a randomised, double-blind, placebo-controlled, clinical trial. Lancet Respir Med. 2021 doi: 10.1016/S2213-2600(21)00237-X. published online June 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Récoché I, Rousseau V, Bourrel R, et al. Drug-drug interactions with imatinib: an observational study. Medicine (Baltimore) 2016;95 doi: 10.1097/MD.0000000000005076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chalmers I, Matthews R. What are the implications of optimism bias in clinical research? Lancet. 2006;367:449–450. doi: 10.1016/S0140-6736(06)68153-1. [DOI] [PubMed] [Google Scholar]


