Abstract
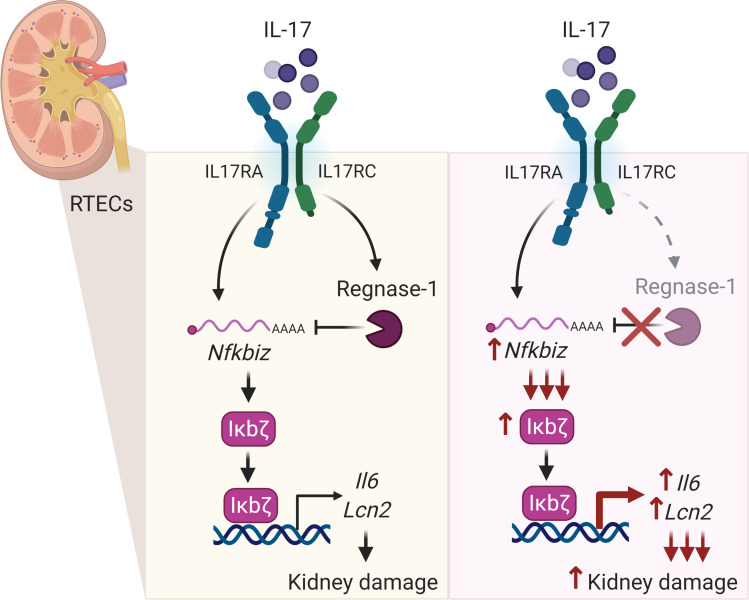
Antibody-mediated glomerulonephritis (AGN) is a clinical manifestation of many autoimmune kidney diseases for which few effective treatments exist. Chronic inflammatory circuits in renal glomerular and tubular cells lead to tissue damage in AGN. These cells are targeted by the cytokine IL-17, which has recently been shown to be a central driver of the pathogenesis of AGN. However, surprisingly little is known about the regulation of pathogenic IL-17 signaling in the kidney. Here, using a well-characterized mouse model of AGN, we show that IL-17 signaling in renal tubular epithelial cells (RTECs) is necessary for AGN development. We also show that Regnase-1, an RNA binding protein with endoribonuclease activity, is a negative regulator of IL-17 signaling in RTECs. Accordingly, mice with a selective Regnase-1 deficiency in RTECs exhibited exacerbated kidney dysfunction in AGN. Mechanistically, Regnase-1 inhibits IL-17–driven expression of the transcription factor IκBξ and, consequently, its downstream gene targets, including Il6 and Lcn2. Moreover, deletion of Regnase-1 in human RTECs reduced inflammatory gene expression in a IκBξ-dependent manner. Overall, these data identify an IL-17–driven inflammatory circuit in RTECs during AGN that is constrained by Regnase-1.
Keywords: Immunology, Inflammation
Keywords: Autoimmune diseases, Cytokines, Innate immunity
Introduction
Antibody-mediated glomerulonephritis (AGN) describes a heterogenous group of renal conditions caused by an inappropriate response to renal autoantigens, such as the glomerular basement membrane (GBM) (1, 2). The most severe form of human AGN is crescentic glomerulonephritis (GN), characterized by the formation of glomerular crescents and tubulointerstitial inflammation (3, 4). Although the initiators of AGN differ among diseases, the terminal events in end-organ kidney damage share common mechanisms that remain poorly understood. Even with the most aggressive immunosuppressive regimens, as many as approximately 30% of nephritic patients develop end-stage renal disease (5). To date, the best therapies are broad-acting immunosuppressants, namely cyclophosphamide with corticosteroids (5). Gaining a fundamental understanding of how pathogenic kidney inflammation is driven and amplified could help fill an unmet clinical need to achieve more specific and effective responses in AGN.
Typically, immune-mediated tissue pathology is viewed through the lens of hematopoietic lymphoid and myeloid cells. Less appreciated is the contribution of organ-specific tissue cells as amplifiers of inflammation that ultimately lead to chronic disease. In the kidney, glomerular and tubular inflammation are hallmark features of AGN (6). In fact, the majority of AGN patients progress to end-stage renal disease as a consequence of chronic tubular inflammation (7). Renal tubular epithelial cells (RTECs) comprise the major cell type of the tubular compartment (8). These cells actively contribute to the production of inflammatory mediators that propagate tissue injury locally by secreting cytokines and chemokines and undergoing apoptosis (7). Even so, our understanding of the inflammatory circuits operative in RTECs during chronic kidney disease is surprisingly rudimentary.
AGN has traditionally been considered a B cell–dependent disease because of the high autoantibody levels found in these patients (9). However, multiple studies also implicate IL-17, the signature cytokine of Th17 cells, as an essential driver of AGN pathology (10–15). IL-17 fuels an inflammatory response that damages renal podocytes, causing proteinuria. Loss of glomerular filtration is followed by IL-17–dominated tubular inflammation and damage of RTECs. Interestingly, IL-17 signaling in the nephritic kidney has no impact on the immunocomplex deposition in the glomeruli (10). While IL-17 is secreted almost exclusively by lymphocytes, its target cells are often but not always nonhematopoietic (16, 17). The specific IL-17 target cells in the context of renal autoimmunity remain unclear.
Although not well defined in the kidney, dysregulation of Th17 cells or IL-17 signaling causes pathology in other autoimmune conditions, such as psoriasis and psoriatic arthritis, where anti–IL-17 biologics are now standard therapies (18, 19). A landmark recent study showed that human Th17 cells specific for commensal microbes such as Staphylococcus aureus and Candida albicans contribute to AGN (20). These findings are consistent with prior work in preclinical models that IL-17 and its adaptor Act1 promote AGN in mice (10–14, 21–23). The downstream events operative in AGN have been presumed to occur through IL-17–mediated activation of the NF-κB signaling pathway, which is induced in response to a myriad of immune stimuli, including IL-17, TNF-α, TLR ligands, and T cell signaling (24, 25). NF-κB induces a panoply of genes that promote renal inflammation, including IL-6, neutrophil-attracting chemokines (CXCL1, CXCL5), and lipocalin 2 (LCN2, NGAL, 24p3), a major biomarker and driver of renal inflammation (26–28). NF-κB also upregulates the noncanonical NF-κB family member IκBξ (Nfkbiz), a transcription factor that regulates a more restricted subset of genes that includes both IL-6 and LCN2 (29, 30). In recent years, it has become evident that IL-17 regulates many genes posttranscriptionally, either by controlling mRNA stabilization and/or by influencing translation of downstream transcripts (31–33). Among these posttranscriptionally regulated targets are Il6 and Nfkbiz (IκBξ).
Autoimmune signaling must be sufficiently restrained in order to prevent hyperactivation of pathways that could contribute to immunomediated pathology. The endoribonuclease Regnase-1 (MCPIP1, encoded by Zc3h12a) is best recognized as an inhibitor of TLR and TCR signaling (34). In CD4+ T cells, loss of Regnase-1 leads to markedly elevated IL-6 levels and, consequently, elevated Th17 differentiation and exacerbated autoimmune disease, demonstrated in the experimental autoimmune encephalitis (EAE) model of multiple sclerosis (35). In cultured fibroblasts, Regnase-1 has been shown to restrict IL-17 signaling by degrading downstream target mRNAs such as Il6 (33). With respect to kidney, however, little is known, though a global deficiency of Regnase-1 enhances the immune response to disseminated C. albicans, a fungal infection that targets the kidney (33).
In this report, we show that RTECs are critical mediators of inflammatory damage in AGN by virtue of their sensitivity to IL-17 signaling. Conversely, Regnase-1 restricts AGN pathogenesis by limiting IL-17–driven renal-specific expression of the transcription factor IκBξ and, consequently, its downstream gene targets Il6 and Lcn2 within RTECs. These findings demonstrate a potent, kidney-intrinsic inflammation circuit that is potentiated by RTEC-specific IL-17 signaling and restrained by Regnase-1 in a highly cell type–specific manner.
Results
RTEC-intrinsic IL-17 signaling is critical for AGN pathology.
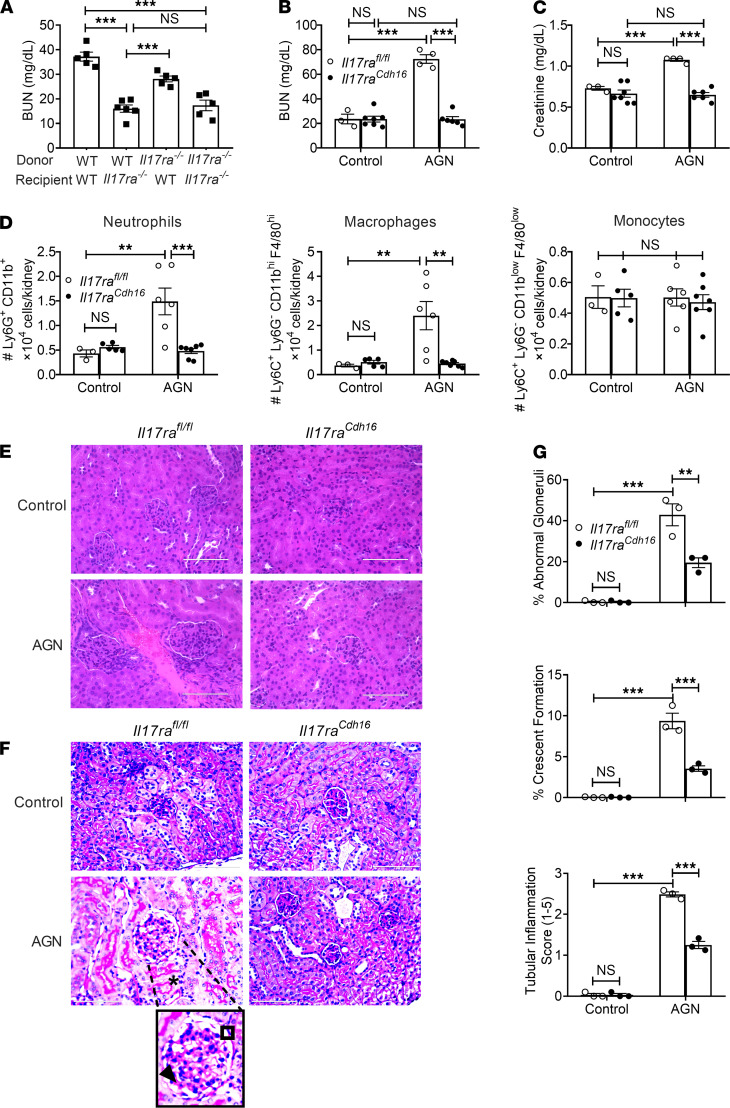
AGN is mediated by both kidney-infiltrating immune cells (hematopoietic) and kidney-resident nonhematopoietic cells. Several studies show that IL-17 and its receptor (IL-17RA), through the adaptor Act1, are essential for AGN (10–14, 21). However, the identity of IL-17 target cells in this setting is unknown. To define the contribution of IL-17RA in hematopoietic versus nonhematopoietic cells, we created BM chimeric mice in which Il17ra–/– or WT BM was adoptively transferred into irradiated reciprocal hosts. Successfully reconstituted recipients were then evaluated for susceptibility to AGN by injecting mice with rabbit IgG in complete Freund’s adjuvant (CFA), followed 3 days later by injection with rabbit anti-GBM serum (10, 36). As shown, WT hosts receiving Il17ra–/– BM showed identical susceptibility to AGN as WT mice, indicating that any activity of IL-17 in hematopoietic cells is dispensable for AGN pathology. Conversely, Il17ra–/– mice, regardless of BM source, were resistant to AGN (Figure 1A). Thus, IL-17RA signaling in nonhematopoietic cells is required for development of AGN.
Figure 1. IL-17RA signaling in RTECs is required for AGN.
(A) BM cells from Il17ra−/− (CD45.2+) and WT (CD45.1+) mice were adoptively transferred into sublethally irradiated Il17ra−/− or WT recipients (n = 5–6). Eight weeks later, successfully reconstituted mice were subjected to AGN and assessed for kidney dysfunction by measuring serum BUN levels. Il17rafl/fl and Il17raCdh16 mice (n = 3–7) were subjected to AGN. (B and C) At day 14 after anti-GBM serum injection, serum BUN (B) and serum creatinine (C) levels were measured by ELISA. (D) Neutrophil, macrophage, and monocyte infiltration in the kidney was quantified by flow cytometry at day 7 p.i. (E and F) Representative photographs of H&E-stained (E) and PAS-stained (F) renal histopathology were assessed. (G) Renal pathology was blindly evaluated and scored for percentages of abnormal glomeruli and crescent formation and for tubular inflammation. Data representative of 1 of 3 mice/group for E and F. A small part (as indicated by dotted lines) of the original image (total original magnification, ×400) was shown as inset panels. Open square, indicating entire glomerulus with mesangial and endocapillary hypercellularity; black arrow, GBM thickening; asterisk, tubular atrophy. Data pooled from at least 2 independent experiments. Statistical analysis by 1-way ANOVA (A) and 2-way ANOVA (B–D, G). **P < 0.01; ***P < 0.001.
The kidney-intrinsic nonhematopoietic cells thought to mediate AGN are RTECs. Prior studies showed that IL-17 can act on primary cultured RTECs to induce expression of cytokine and chemokine genes that are known to drive inflammation in AGN (24). Based on this, we sought to define the role of IL-17 signaling in RTECs in vivo. We took advantage of well-characterized Cdh16Cre mice, in which the Cre recombinase is expressed in the epithelial lining of proximal tubules, collecting ducts, loops of Henle, and distal tubules (37). We crossed Il17rafl/fl mice to Cdh16Cre mice (termed Il17raCdh16), which selectively and efficiently depleted IL-17RA in RTECs, as previously reported (38). Following AGN, Il17raCdh16 mice showed diminished levels of serum BUN and creatinine (Figure 1, B and C). Il17raCdh16 kidneys exhibited compromised renal infiltration of neutrophils and macrophages at day 7 after AGN (Figure 1D and Supplemental Figure 1; supplemental material available online with this article; https://doi.org/10.1172/jci.insight.147505DS1). Interestingly, the number of inflammatory monocytes, CD4+ T, CD8+ T, and B cells were comparable between the groups (Figure 1D, Supplemental Figures 1, and Supplemental Figure 2, A and B). When evaluated for kidney pathology, Il17raCdh16 kidneys showed reduced mesangial and endocapillary hypercellularity, thickening of GBM, crescents formation, tubular atrophy, and tubular inflammatory cell infiltration in comparison with controls, similar to Il17ra–/– or Act1–/– mice (10, 14) (Figure 1, E–G). These results, thus, demonstrate an RTEC-specific role of IL-17R signaling in AGN.
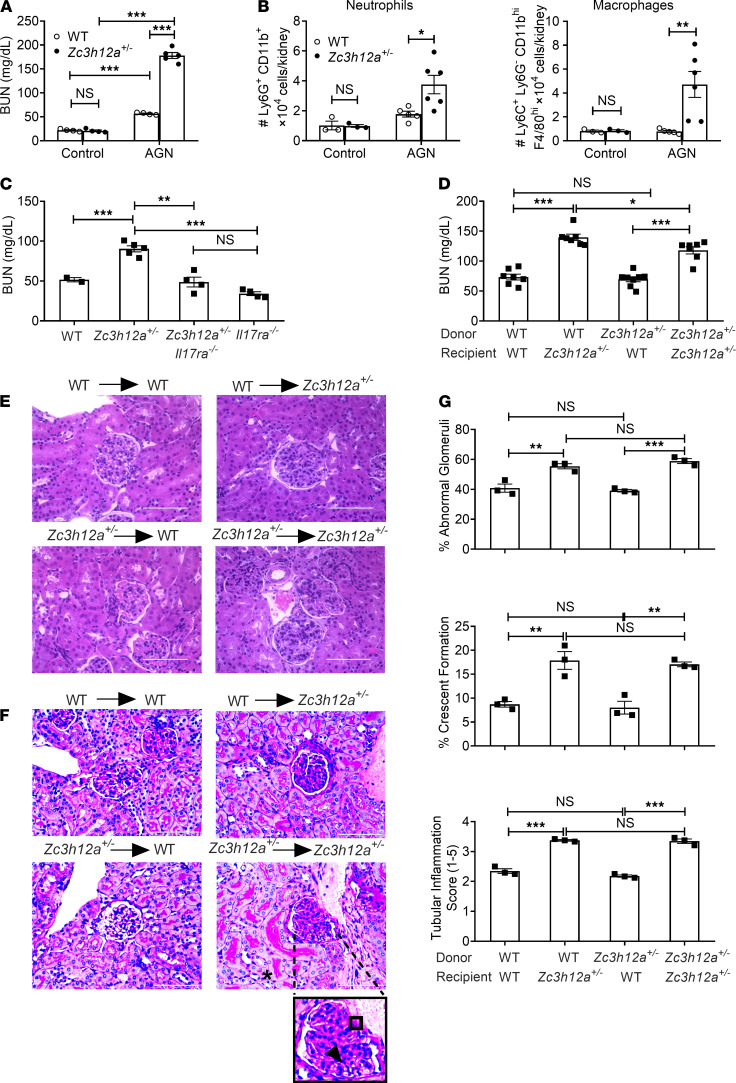
Regnase-1 haploinsufficient mice show exaggerated AGN.
Surprisingly little is known about the molecular signals that constrain inflammation in the context of AGN. Regnase-1 (encoded by Zc3h12a) is a negative feedback regulator of many inflammatory stimuli, including the TCR, TLR4, and IL-17 (33, 34). Mice lacking Zc3h12a entirely show systemic inflammation and early mortality, an effect that we previously found to be independent of IL-17 (39, 40). In contrast, Zc3h12a haploinsufficient (Zc3h12a+/–) mice have no peripheral inflammation in kidney or other visceral organs but exhibit enhanced susceptibility to IL-17–induced pathology in certain settings, including EAE (33, 41, 42). Consequently, we subjected Zc3h12a+/– mice to AGN to determine if this molecule influences outcomes in renal autoimmunity. As shown, Zc3h12a +/– mice were markedly more susceptible to AGN than control mice (Figure 2A). Mice lacking a single copy of the Zc3h12a gene demonstrated increased infiltration of neutrophils and macrophages but not monocytes, CD4+ T, CD8+ T, and B cells (Figure 2B, Supplemental Figure 1, and Supplemental Figure 3, A–C). Moreover, kidney dysfunction was reversed in Zc3h12a+/– Il17ra–/– mice, indicating that IL-17 signaling is essential for Regnase-1–mediated inhibitory signaling in the nephritic kidney (Figure 2C).
Figure 2. Zc3h12a+/– mice show exaggerated AGN.
(A) Zc3h12a+/+ (WT) and Zc3h12a+/– (n = 4–5) were subjected to AGN. Mice were evaluated for kidney dysfunction by measuring serum BUN at day 14 p.i. (B) Neutrophil and macrophage infiltration in the kidney was quantified by flow cytometry at day 7 p.i. (C) WT, Zc3h12a+/–, Zc3h12a+/–Il17ra–/–, and Il17ra–/– (n = 3–5) were subjected to AGN. Serum BUN level was measured at day 14 p.i. (D) BM cells from Zc3h12a+/− and WT mice were adoptively transferred into sublethally irradiated Zc3h12a+/− or WT recipients (n = 5–7). Eight weeks later, successfully reconstituted mice were subjected to AGN and assessed for serum BUN levels. (E and F) Representative photographs of H&E-stained (E) and PAS-stained (F) renal histopathology. Data representative 1 of 3 mice/group. A small part (as indicated by dotted lines) of the original image (total original magnification, ×400) was shown as inset panels. Open square, indicating entire glomerulus with mesangial and endocapillary hypercellularity; black arrow, GBM thickening; asterisk, tubular atrophy. (G) Renal pathology was blindly evaluated and scored for percentages of abnormal glomeruli and crescent formation, and for tubular inflammation. Data pooled from at least 2 independent experiments. Statistical analysis by 2-way ANOVA (A and B) and 1-way ANOVA (C, D, and G). *P < 0.05; **P < 0.01; ***P < 0.001.
Regnase-1 can also restrain Th17 cell differentiation; hence, mice lacking Regnase-1 in CD4+ T cells have exacerbated disease in EAE (35). Thus, the increased nephritis in Zc3h12a+/– could be due to enhanced IL-17 production from T cells or to unrestrained IL-17 signaling in responder cells — or potentially both. To distinguish among these possibilities, we created BM chimeric mice where Zc3h12a+/– or Zc3h12a+/+ BM from littermates were adoptively transferred into irradiated reciprocal hosts. Successfully reconstituted mice were subjected to AGN. These data show that Regnase-1 in nonhematopoietic cells was required for AGN development, evidenced by increased serum BUN and creatinine (Figure 2D and Supplemental Figure 3D). Zc3h12a+/– animals receiving either WT or Zc3h12a+/– BM showed evidence of increased glomerular pathology, as characterized by exaggerated crescents formation, mesangial hypercellularity, and increased GBM thickness. Additionally, these animals exhibited increased tubular atrophy and tubular inflammatory cell infiltration compared with WT recipients (Figure 2, E–G). These data indicate that Regnase-1 restricts AGN pathogenesis by acting in nonhematopoietic cells, with the caveat that mice still retained 1 intact copy of the Zc3h12a gene.
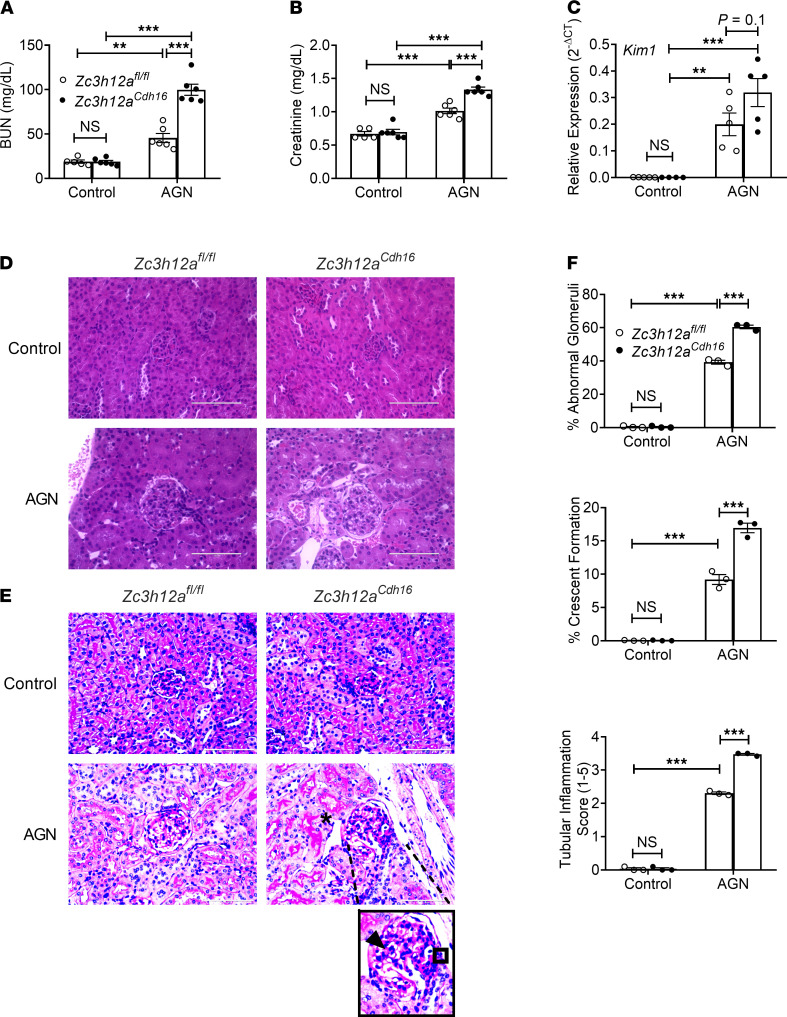
Regnase-1 restrains AGN severity in an RTEC-intrinsic manner.
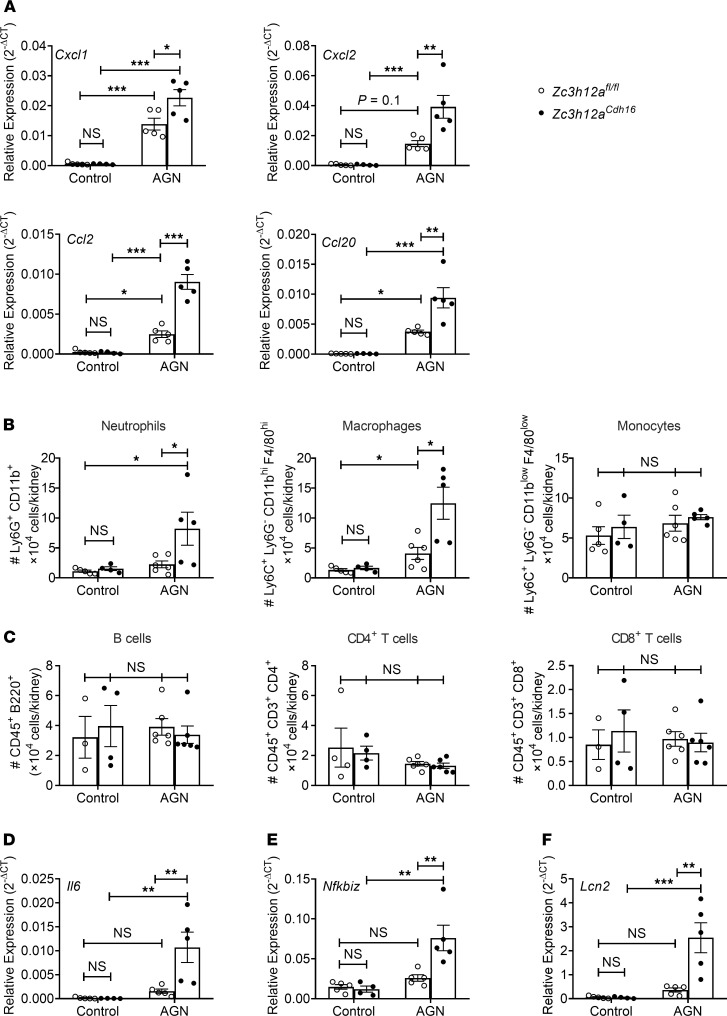
Given that Regnase-1 restricts IL-17 signaling and that Regnase-1 and IL-17RA both act in nonhematopoietic cells in AGN in an opposing manner, we predicted that loss of Regnase-1 in RTECs would exacerbate tissue pathology in AGN. We crossed Zc3h12afl/fl and Cdh16Cre mice to delete Regnase-1 in RTECs (Zc3h12aCdh16). Mice lacking Regnase-1 in RTECs breed normally and displayed normal serum BUN and kidney tissue architecture at baseline (Figure 3, A and D). After AGN induction, compared with Zc3h12afl/fl controls, Zc3h12aCdh16 mice showed more severe kidney dysfunction and a trend toward increased expression of the classical kidney injury marker Kim1 (43) (Figure 3, A–C). Moreover, Zc3h12aCdh16 mice exhibited more glomerular abnormality as characterized by increased mesangial and endocapillary hypercellularity, thickening of GBM, and crescents formation following AGN (Figure 3, D–F). Zc3h12aCdh16 kidneys demonstrated exaggerated tubular atrophy and inflammatory cell infiltration in the tubular space compared with control mice. Zc3h12aCdh16 kidney also showed increased expression of multiple chemokines implicated in AGN, including Cxcl1, Cxcl2, Ccl20, and Ccl2, that are known to recruit immune cells to diseased tissue (Figure 4A). Consequently, Zc3h12aCdh16 mice exhibited a trend of increased kidney-infiltrating CD45+ inflammatory cells (Supplemental Figure 1 and Supplemental Figure 4A). Although the number of neutrophils and macrophages were increased in Zc3h12aCdh16 mice, the frequencies of monocytes, CD4+ T, CD8+ T, and B cells were comparable among the nephritic groups (Figure 4, B and C, Supplemental Figure 1, and Supplemental Figure 4B). These results indicate a role for Regnase-1 as a negative regulator of renal inflammation.
Figure 3. RTEC-specific Regnase-1 deficiency exacerbates AGN.
Zc3h12afl/fl and Zc3h12aCdh16 mice (n = 5–6) were subjected to AGN. (A and B) At day 14 p.i., serum BUN (A) and serum creatinine (B) levels were assessed. (C) Kim1 transcript expression was assessed at day 7 p.i. Expression was normalized to Gapdh. (D and E) Representative photographs of H&E-stained (D) and PAS-stained (E) renal histopathology. (F) Renal pathology was blindly evaluated and scored for percentages of abnormal glomeruli and crescent formation and for tubular inflammation. Data representative of 1 of 3 mice/group for D and E. A small part (as indicated by dotted lines) of the original image (total original magnification, ×400) was shown as inset panels. Open square, indicating entire glomerulus with mesangial and endocapillary hypercellularity; black arrow, GBM thickening; asterisk, tubular atrophy. Data pooled from at least 2 independent experiments. Statistical analysis by 2-way ANOVA. **P < 0.01; ***P < 0.001.
Figure 4. Increased inflammatory gene expression and cell infiltration in the nephritic kidney of RTEC-specific Regnase-1 deficient mice.
Zc3h12afl/fl and Zc3h12aCdh16 mice (n = 3–6) were subjected to AGN. (A–F) At day 7 p.i., renal Cxcl1, Cxcl2, Ccl20 and Ccl2 mRNA (A) expression was measured by qPCR; neutrophil, macrophage, monocyte, B cell, CD4+ T cell, and CD8+ T cell infiltration in the kidney was quantified by flow cytometry (B and C); and Il6 (D), Nfkbiz (E), and Lcn2 (F) transcript expression was evaluated by qPCR. Expression was normalized to Gapdh (A, D, E, and F). The data is pooled from at least 2 independent experiments. Statistical analysis by 2-way ANOVA. *P < 0.05; **P < 0.01; ***P < 0.001.
Regnase-1 functions by binding to and degrading client mRNA transcripts (33). Some inflammatory transcripts are direct targets of Regnase-1, such as Il6, where Regnase-1 binds to a stem-loop sequence in Il6 the 3′ UTR to promote degradation. However, many mRNAs are indirectly influenced by Regnase-1 through its capacity to degrade mRNA, including the gene encoding the IκBξ transcription factor (Nfkbiz). A major example of IκBξ-dependent mRNA is Lcn2 (44). Therefore, we examined expression of known Regnase-1 client transcripts involved in AGN pathology in Zc3h12aCdh16 mice. There was no difference in the expression of Il6, Nfkbiz, or Lcn2 in kidney at baseline (Figure 4, D–F). However, following AGN, there was a marked increase in levels of Il6, Nfkbiz, and Lcn2 in Zc3h12aCdh16 kidneys compared with controls. Notably, all these genes are also known targets of IL-17 in AGN and are reduced in Il17ra–/– mice subjected to AGN (10). Collectively, these data suggest a role for Regnase-1 in restraining expression of pathogenic IL-17–dependent genes in an RTEC-specific manner during the inflammatory process of AGN.
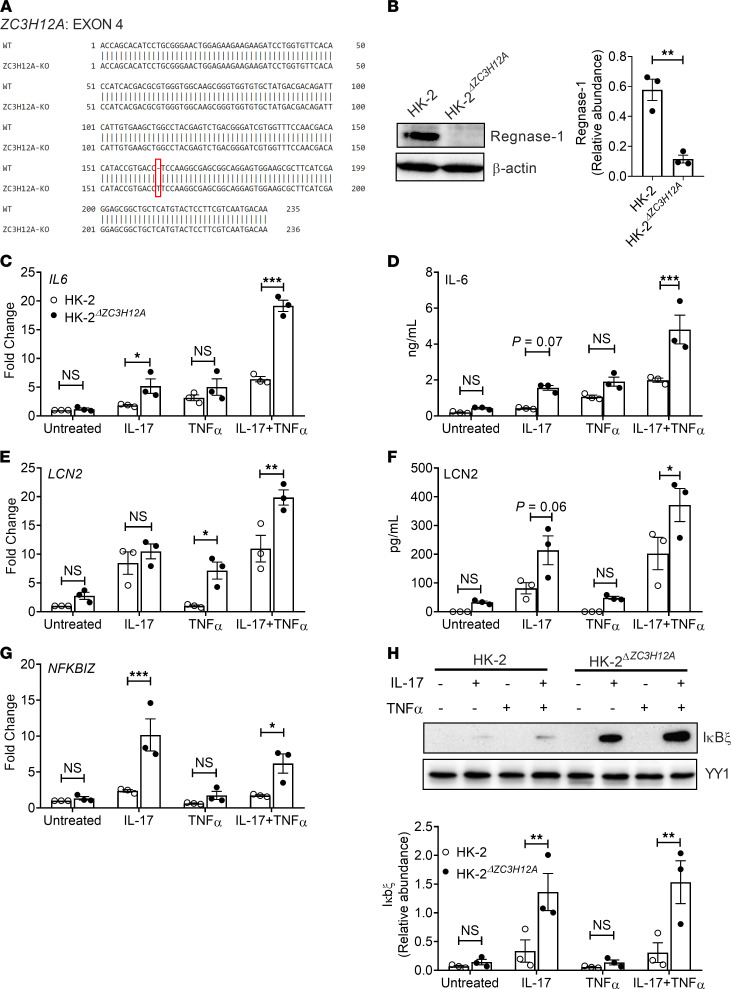
Regnase-1 in human RTECs drives inflammation via Iκbξ.
To determine in a more direct way how Regnase-1 functions in RTECs, we deleted the ZC3H12A gene in the human tubular kidney 2 (HK-2) cell line using CRISPR-Cas9 technology (henceforth referred to as HK-2ΔZC3H12A; Figure 5, A and B). HK-2 is a tubular epithelial cell line derived from normal kidney, and we found it to be highly responsive to IL-17 (Figure 5C). HK-2ΔZC3H12A and control HK-2 cells were stimulated with IL-17 and assessed for mRNA and protein expression of known IL-17 responsive genes, including IL6, LCN2, NFKBIZ, CEBPB, and CEBPD. We also performed stimulations in conjunction with TNF-α, since IL-17 and TNF-α often signal in a potently synergistic manner (45). IL-17 alone or in conjunction with TNF-α upregulated transcript (Figure 5, C and E) and protein (Figure 5, D and F) expression of IL6 and LCN2 in HK-2ΔZC3H12A cells. Notably, HK-2ZC3H12A cells demonstrated an increased expression of NFKBIZ transcript and Iκbξ expression following IL-17 treatment (Figure 5, G and H). The impact of IL-17 alone or IL-17 plus TNF-α on the mRNA and protein expression of CEBPB and CEBPD was variable (Supplemental Figure 5, A and B). Additionally, a luciferase assay revealed activation of Lcn2 promoter activity following IL-17 stimulation in human embryonic kidney 293 cells (HEK-293) (Supplemental Figure 5C). Overall, these results indicate that Regnase-1 is a negative regulator of IL-17 signaling in human RTECs.
Figure 5. Deletion of ZC3H12A gene elevates inflammatory mediator expression in the HK-2 cell line.
(A) Experimental strategy to delete ZC3H12A gene by CRISPR-Cas9 in the HK-2 cell line. (B) HK-2 and HK-2ΔZC3H12A cells were lysed and evaluated for Regnase-1 by Western blot. Protein relative abundance and representative image are shown. (C, E, and G) HK-2 and HK-2ΔZC3H12A cells were stimulated with IL-17 and/or TNF-α and mRNA expression of IL6, LCN2, and NFKBIZ was measured by qPCR (8 hours after stimulation), normalized to GAPDH. (D and F) Protein level of IL-6 (8 hours after stimulation) and LCN2 (24 hours after stimulation) in culture supernatant were measured by ELISA. (H) HK-2 and HK-2ΔZC3H12A cells were stimulated with IL-17 and/or TNF-α for 8 hours, and cell lysates were evaluated for IκBξ by Western blot. Protein relative abundance and representative image are shown. Data pooled from at least 3 independent experiments. Statistical analysis by 2-tailed unpaired t test (B) or 2-way ANOVA (C–H). *P < 0.05; **P < 0.01; ***P < 0.001.
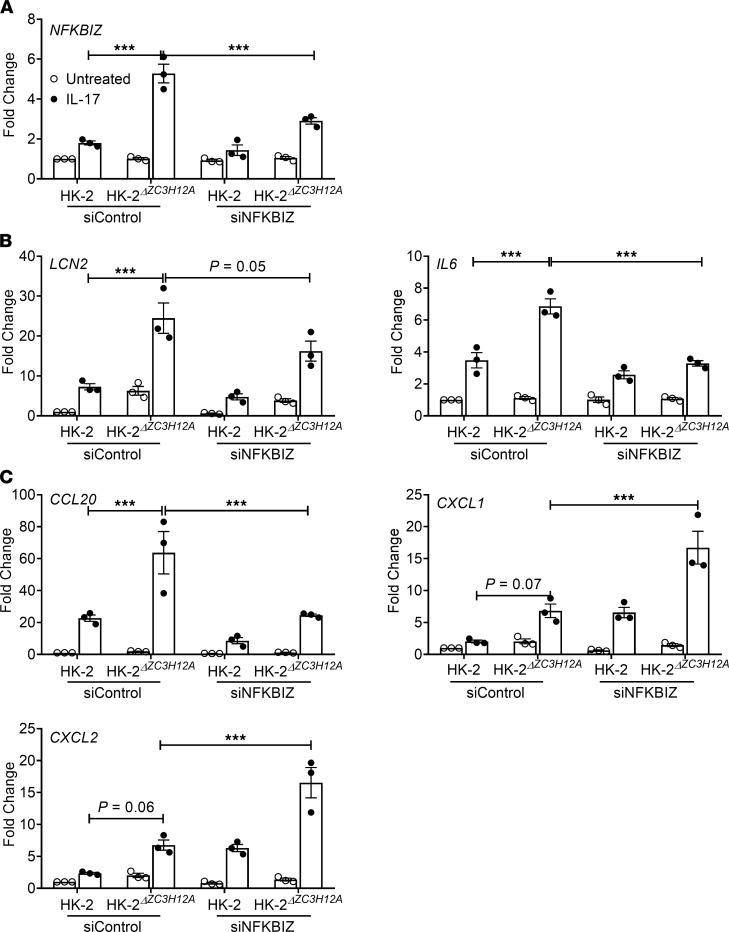
Since Regnase-1 restricts expression of the IκBξ transcription factor (NFKBIZ), which mediates expression of many of these characteristic downstream mRNAs, we evaluated the impact of IκBξ in HK-2 cells with respect to IL-17 signaling. To that end, we knocked down NFKBIZ by siRNA in HK-2ΔZC3H12A and control HK-2 cells, which resulted in 50%–60% reduction in NFKBIZ expression (Figure 6A). HK-2ΔZC3H12A cells in which NFKBIZ was silenced showed diminished levels of LCN2 and IL6 mRNA compared with controls (Figure 6B). Interestingly, while CCL20 levels were reduced upon NFKBIZ silencing, CXCL1 and CXCL2 were increased (Figure 6C). These results indicate that Regnase-1 selectively suppresses some IL-17 responsive genes that mediate kidney inflammation by increasing NFKBIZ in human RTECs.
Figure 6. Regnase-1 upregulates IL6 and LCN2 gene expression via NFKBIZ.
HK-2 and HK-2ΔZC3H12A cells were either treated with siRNA against NFKBIZ or control siRNA. (A) Efficiency of NFKBIZ gene silencing was measured by qPCR. (B and C) Cells were either stimulated with IL-17 or left untreated for 8 hours and analyzed for IL6, LCN2, CCL20, CXCL1, and CXCL2 gene expression by qPCR. Data pooled from at least 3 independent experiments. Statistical analysis by 2-way ANOVA. ***P < 0.001.
Discussion
Development of improved therapeutic approaches to treat AGN will require a more comprehensive understanding of the fundamental immune mechanisms in the kidney that drive this disease. The kidney is an immunologically distinct organ and is exquisitely sensitive to end-organ damage in numerous autoimmune diseases and infections. Indeed, renal injury caused by inappropriate immune responses is the most important predictor of mortality in AGN patients (7). Even so, our understanding of the fundamental immune processes in the kidney lags considerably behind that of other visceral organs, such as the gut or liver (1, 46). This is due to multiple kidney-specific factors, including poor regenerative capacity of nephrons, uremic toxins, hypoxia, and arterial blood pressure, which have confounding impacts on the ongoing immune response in the kidney. Defining how IL-17 mediates signals in target cell types in the nephritic kidney has important therapeutic implications, as specific targeting of the IL-17 pathway in these kidney-resident cells could spare other organs from unwanted side effects and potentially preserve important IL-17 host-defensive activities.
IL-17 is a critical contributor of autoinflammatory diseases (47). Antibodies that neutralize IL-17 were approved in 2016 and show efficacy in psoriasis, psoriatic arthritis, and ankylosing spondylitis (18, 19). In contrast, IL-17 blockade caused adverse outcomes in Crohn’s disease due to an unexpectedly strong tissue-reparative effect of intestinal epithelium (48–50). These dichotomous outcomes highlight the ramifications of tissue-specific mechanisms of IL-17 signaling. While there has been much research effort describing IL-17–producing cells and their generation, far less is known about how IL-17 mediates downstream signal transduction and mechanisms that regulate this process in responding cells. We showed that RTEC-specific activity of the IL-17 receptor subunit IL-17RA drives chronic inflammatory response in the nephritic kidney. Notably, IL-17RA acts as a shared receptor subunit for the related cytokines IL-17F and IL-17C (51). Hence, some of the effects seen here could be attributable to these cytokines, as well. Despite their emerging role in AGN, both IL-17F and IL-17C signaling mechanisms in the RTECs are almost entirely undefined, and no studies to date have focused on the regulation of IL-17F– and IL-17C–dependent signal transduction in these kidney-resident cell types (52, 53). Moreover, the type 2 cytokine IL-25 also signals via IL-17RA (51). To date, there is no evidence suggesting a pathogenic role of IL-25 in AGN development. The findings in this study, thus, set the stage for pursuing analysis of these related but poorly understood IL-17 family of cytokines.
The contribution of kidney-resident cells such as RTECs is often overlooked when considering the development of new therapeutic strategies in inflammatory kidney diseases. Although the IL-17R is ubiquitously expressed (51) and some studies indicated that IL-17 can act on immune cells including T cells, B cells, and NK cells (16, 17, 54), we show that the contribution of the hematopoietic system in AGN is, in fact, negligible. Rather, IL-17, produced locally in the nephritic kidney by Th17 and γδ T cells, signals directly on RTECs to drive production of pathogenic factors including cytokines, chemokines, and LCN2 (10). This finding is in line with other organ-specific autoimmune conditions, including collagen-induced arthritis and imiquimod-induced (IMQ-induced) dermatitis, where a tissue-dependent role for IL-17 signaling was similarly demonstrated. A limitation of BM chimeric mouse studies is that kidney harbors a radio-resistant tissue-resident population of macrophage (CX3CR1+), which are responsive to IL-17 (55). Hence, future studies will need to address the role of pathogenic IL-17 signaling in tissue-resident macrophages in AGN (e.g., by crossing Cx3cr1Cre mice to Il17rafl/fl animals).
Regnase-1 has been shown to restrict many inflammatory signals, and IL-17 is just one of many. Based on our studies, we cannot rule out the roles for Regnase-1 in restricting other tissue-dependent inflammatory signals that use the IL-17RA subunit, including IL-17F, IL-17C, and IL-25 and non–IL-17 cytokines such as IL-1 family members. Since Regnase-1 acts on T cells and macrophages, it is also surprising that our BM chimera and RTEC-specific deletion studies indicated that the impact of Regnase-1 in AGN seemed to be so RTEC specific (35, 56). However, this finding does suggest that a major function of Regnase-1 is to restrain downstream IL-17R–mediated signals in the kidney. We previously reported that mice with a Regnase-1 deficiency have increased resistance to kidney infections caused by systemic Candida albicans infections (33). These data indicate that, while constraint of IL-17 signaling by Regnase-1 is beneficial in preventing autoimmunity, this same inhibition limits the efficacy of IL-17 in mediating renal host defense; thus, care will be needed when considering targeting this pathway pharmacologically. Although Cre-lox technology has enabled manipulation of gene expression in targeted tissues, off-target effects of Cre sometimes occur. However, Cdh16Cre mice are a well-characterized and extensively used mouse system with no reported off-target activity.
This work highlights an inflammatory signaling axis mediated by IL-17 and Regnase-1 and the transcription factor IκBζ. The gene encoding IκBζ (Nfkbiz) is transcriptionally induced by IL-17, thus acting as a feed-forward activator of IL-17 signaling (57, 58). IκBζ regulates transcription of Lcn2 and Il6 (58). Lcn2 is a well-known biomarker of kidney disease (27) and causes renal damage by inducing apoptosis of RTECs (26, 33, 59). This observation likely explains why we observed such a potent impact of negative regulatory mechanisms of IL-17 signaling in the development of nephritic pathology. We also observed that IL-17 synergizes with TNF-α in inducing NFKBIZ, IL6, and LCN2 in HK-2 cell lines lacking Regnase-1 (ZC3H12A). TNF-α on its own does not activate NFKBIZ (60); therefore, this result reveals a mechanism by which IL-17 and TNF-α together drive the expression of IκBζ and its responsive genes.
Understanding how IL-17 and its downstream signals are regulated is important from a basic science perspective and has potential translational applications. Currently, approximately 90 clinical trials are ongoing to test IL-17 blockade (clinicaltrials.gov; NCT01107457, NCT00966875, NCT01539213, NCT00936585, and NCT03073213). We previously showed that blocking IL-17 alleviates symptoms in mouse models of AGN (10). Antibodies against IL-23, the cytokine responsible for generating pathogenic type 17 cells, are showing promising results in clinical trials in number of inflammatory diseases (clinicaltrials.gov: accession nos. NCT01845987, NCT01947933, and NCT04630652). Hence, future studies will need to focus on conducting preclinical trials to assess the efficacy of anti–IL-23, anti–IL-6, and anti–IL-1 therapies, the upstream regulators of type 17 cells development, in mouse model of AGN. Here, we have identified a potentially novel role for the endoribonuclease Regnase-1 in restricting IL-17–mediated kidney inflammation through the transcription factor IκBζ. Since Regnase-1 negatively regulates pathogenic IL-17 activity in the nephritic kidney, these results may ultimately have the potential to provide new targets for therapies against AGN.
Methods
Mice.
C57BL/6NTac (WT) mice were from Taconic Biosciences Inc. Il17ra–/– mice were from Amgen and bred in-house. Il17rafl/fl mice were provided by Jay Kolls (Tulane University). Zc3h12afl/fl mice are under material transfer agreement (MTA) from University of Central Florida (Orlando, Florida, USA). Cdh16Cre (Ksp1.3Cre) mice and B6.SJL-Ptprc (B6 CD45.1) were from The Jackson Laboratory. All the experiments used age-matched controls of both sexes, housed in specific pathogen–free conditions.
AGN.
Mice are immunized i.p. with 0.2 mg of rabbit IgG (011-000-003, Jackson ImmunoResearch) in CFA (MilliporeSigma). Controls received CFA only. Three days later, mice were injected i.v. with heat-inactivated rabbit anti–mouse GBM serum (Custom-made, Lampire Biological Lab Inc.) at 5 mg/20 g body weight. Mice were sacrificed at day 7 or 14 after anti-GBM injection. Serum blood urea nitrogen (BUN) was measured using Blood Urea Nitrogen Enzymatic kit (Bioo Scientific Corp.) and creatinine with QuantiChrom Creatinine Assay kit (BioAssay Systems).
To create BM chimeras, mice were sublethally irradiated (9 Grey) and, 24 hours later, 5 × 106 to 10 × 106 donor BM cells (either CD45.1 or CD45.2) were injected i.v. After 6–8 weeks, peripheral blood of recipients was tested for reconstitution with donor BM cells by flow cytometry for CD45.1 and CD45.2.
Deletion of ZC3H12A in HK-2 cells.
KO of ZC3H12A in the HK-2 cell line was performed by SYNTHEGO Company using CRISPR-Cas9. Briefly, HK-2 cells were electroporated with Cas9 and a ZC3H12A-specific sgRNA (5′-GACACAUACCGUGACCUCCA-3′). Isogenic negative control HK-2 cells were electroporated with only Cas9. Editing efficiency was evaluated 48 hours after transfection. The cells were expanded to get a KO cell pool. Clonal ZC3H12A-KO cell lines were generated by limiting dilution. Genomic DNA from monoclonal populations were verified by PCR and Sanger sequencing using ZC3H12A specific primer (forward, 5′-TGACCTTGGCGTTAACCACTC -3′; reverse, 5′-GTGGACCCCAAGTCTGTCAG -3′). The sequencing results were analyzed using the Inference of CRISPR Edits (ICE) tool (https://ice.synthego.com/#/) and NCBI nucleotide blast tool.
Immunoblot analysis.
HK-2 cells (ATCC) were lysed in 1× NP-40 lysis buffer supplemented with protease inhibitor cocktail. Lysates were separated by SDS-PAGE, transferred to polyvinylidene difluoride membranes, and imaged with the enhanced chemiluminescence detection system (Thermo Fisher Scientific) and developed with a FluorChem E imager (ProteinSimple). Immunoblotting antibodies: human/mouse anti–Regnase-1 (MAB7875, R&D Systems), human anti–β actin (ab49900, Abcam), human anti-C/EBPδ (sc-365546, Santa Cruz Biotechnology Inc.), human/mouse anti-C/EBPβ (sc-7962, Santa Cruz Biotechnology Inc.), human anti-Iκbζ (9244, Cell Signaling Technology), and human/mouse anti-YY1 (sc-7341, Santa Cruz Biotechnology Inc.). The intensity of the protein band was measured by ImageJ software (NIH).
ELISA.
HK-2 cells (ATCC) were stimulated with IL-17 and/or TNF-α for different times. The supernatant was collected, and ELISA was performed to detect IL-6 (8 hours after stimulation, catalog 88-7066-22, Invitrogen) and LCN2 (24 hours after stimulation, catalog EHLCN2, Invitrogen).
Luciferase assay.
Luciferase assay was performed as previously described (61). Briefly, IL-17 Reporter HEK 293 cells were seeded in 12-well plates. In total, 100 ng of LCN2 promoter luciferase plasmid and 5 ng of Renilla luciferase plasmid were cotransfected. Cells were stimulated with 10 ng/mL of human IL-17 for 14 hours and then lysed for luciferase analyze by using GloMax Navigator Microplate Luminometer.
Histology and flow cytometry.
For IHC, kidneys were fixed with 10% buffered formaldehyde and embedded in paraffin. Slices of 4 μm thick were stained with H&E or periodic acid–Schiff (PAS) and observed on an EVOS microscope (Thermo Fisher Scientific). The slides were scored blindly by an expert with more than 10 years of experience with renal histopathology, as described previously (62). Briefly, severity of GN was assessed by mild to moderate increase in mesangial cellularity, thickening of the GBM, endocapillary hypercellularity, and crescents formation. The tubulointerstitial inflammation was measured by assessing tubular atrophy and tubulointerstitial inflammation.
Kidneys were perfused with PBS containing EDTA (MilliporeSigma) before harvesting. Kidneys were digested at 37°C in 1 mg/mL collagenase IV (Worthington) in complete RPMI for 30 minutes, filtered through 70 mm strainers, and washed twice in PBS. For flow cytometry, the following antibodies were used: CD45 (30-F11, eBioscience), CD3 (145-2C11, BioLegend), CD4 (GK1.5, BioLegend), CD8 (53-6.7, BioLegend), CD45R/B220 (RA3-6B2, BioLegend), Ly6G (IA8, eBioscience), CD11b (M1/70, BioLegend), F4/80 (BM8, BioLegend), and Ly6C (HK1.4, eBioscience). Samples were acquired on BD LSRFortessa cytometer (BD Biosciences) and analyzed by FlowJo software (Tree Star Inc.).
RNA silencing and qPCR.
ON-TARGETplus SMARTpool siRNAs targeting human NFKBIZ were from Dharmacon. For RNA silencing, HK-2 cells were seeded overnight in antibiotic-free DMEM/F12 media (Thermo Fisher Scientific) with supplements. Transfection was performed 18 hours later with 50 nM siRNAs with DharmaFECT Reagent 1. Culture media was replaced after 24 hours. One day later, cells were treated with human IL-17 and human TNF-α (Peprotech) for 8 hours.
RNA was extracted using RNeasy kits (Qiagen). Complementary DNA was synthesized by SuperScript III First Strand Kits (Thermo Fisher Scientific). Quantitative PCR (qPCR) was performed with the PerfeCTa SYBR Green FastMix (Quanta BioSciences) and analyzed on an ABI 7300 real-time instrument. Primers were from QuantiTect Primer Assays (Qiagen). Expression was normalized to mouse or human Gapdh.
Statistics.
All data are shown as Mean ± SEM. Statistical analyses were performed using 1- or 2-tailed Student’s t test and 1- or 2-way ANOVA depending on the experiment using GraphPad Prism. A P value less than 0.05 was considered as statistically significant. *P < 0.05; **P < 0.01; ***P < 0.001. All experiments were performed at least twice in independent replicates.
Study approval.
All the experiments were conducted following NIH guidelines under protocols approved by the University of Pittsburgh IACUC (protocol no. 20087922).
Author contributions
DDL, JKK, SLG, and PSB designed the experiments; DDL, RB, KR, CVJ, YL, and PSB performed the experiments. JKK provided conditional KO mouse. DDL, SLG, and PSB analyzed and interpreted the data and wrote the manuscript.
Supplementary Material
Acknowledgments
This work was supported by a Rheumatology Research Foundation grant to SLG and PSB and NIH grants AI145242 (SLG and PSB), AI147383 (SLG), DK104680 (PSB), AI142354 (PSB), and R35 HL139930 (JKK). We thank P.K. Kollatukudy, M.J. McGeachy, K. Chen, S. Majumder, and G. Trevejo-Nunez for valuable input and B. Coleman and L. Lin for assistance with mouse breeding.
Version 1. 07/08/2021
Electronic publication
Footnotes
Conflict of interest: The authors have declared that no conflict of interest exists.
Copyright: © 2021, Li et al. This is an open access article published under the terms of the Creative Commons Attribution 4.0 International License.
Reference information: JCI Insight. 2021;6(13):e147505.https://doi.org/10.1172/jci.insight.147505.
Contributor Information
De-Dong Li, Email: del64@pitt.edu.
Rami Bechara, Email: rrb42@pitt.edu.
Kritika Ramani, Email: kritika.30@gmail.com.
Yang Li, Email: yal147@pitt.edu.
Jay K. Kolls, Email: jkolls1@tulane.edu.
Sarah L. Gaffen, Email: sig65@pitt.edu.
References
- 1.McAdoo SP, Pusey CD. Anti-glomerular basement membrane disease. Clin J Am Soc Nephrol. 2017;12(7):1162–1172. doi: 10.2215/CJN.01380217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Segelmark M, Hellmark T. Autoimmune kidney diseases. Autoimmun Rev. 2010;9(5):A366–A371. doi: 10.1016/j.autrev.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 3.Moroni G, Ponticelli C. Rapidly progressive crescentic glomerulonephritis: early treatment is a must. Autoimmun Rev. 2014;13(7):723–729. doi: 10.1016/j.autrev.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 4.Webster P, Pusey C. Glomerular disease: crescentic glomerulonephritis: beyond the immune system. Nat Rev Nephrol. 2017;13(4):198–200. doi: 10.1038/nrneph.2017.32. [DOI] [PubMed] [Google Scholar]
- 5.Waldman M, Appel GB. Update on the treatment of lupus nephritis. Kidney Int. 2006;70(8):1403–1412. doi: 10.1038/sj.ki.5001777. [DOI] [PubMed] [Google Scholar]
- 6.Davidson A. What is damaging the kidney in lupus nephritis? Nat Rev Rheumatol. 2016;12(3):143–153. doi: 10.1038/nrrheum.2015.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hodgkins KS, Schnaper HW. Tubulointerstitial injury and the progression of chronic kidney disease. Pediatr Nephrol. 2012;27(6):901–909. doi: 10.1007/s00467-011-1992-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Qi R, Yang C. Renal tubular epithelial cells: the neglected mediator of tubulointerstitial fibrosis after injury. Cell Death Dis. 2018;9(11):1126. doi: 10.1038/s41419-018-1157-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shlomchik MJ, et al. From T to B and back again: positive feedback in systemic autoimmune disease. Nat Rev Immunol. 2001;1(2):147–153. doi: 10.1038/35100573. [DOI] [PubMed] [Google Scholar]
- 10.Ramani K, et al. An essential role of interleukin-17 receptor signaling in the development of autoimmune glomerulonephritis. J Leukoc Biol. 2014;96(3):463–472. doi: 10.1189/jlb.3A0414-184R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Turner JE, et al. The Th17 immune response in renal inflammation. Kidney Int. 2010;77(12):1070–1075. doi: 10.1038/ki.2010.102. [DOI] [PubMed] [Google Scholar]
- 12.Turner JE, et al. IL-17A production by renal γδ T cells promotes kidney injury in crescentic GN. J Am Soc Nephrol. 2012;23(9):1486–1495. doi: 10.1681/ASN.2012010040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paust HJ, et al. The IL-23/Th17 axis contributes to renal injury in experimental glomerulonephritis. J Am Soc Nephrol. 2009;20(5):969–979. doi: 10.1681/ASN.2008050556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pisitkun P, et al. The adaptor protein CIKS/ACT1 is necessary for collagen-induced arthritis, and it contributes to the production of collagen-specific antibody. Arthritis Rheum. 2010;62(11):3334–3344. doi: 10.1002/art.27653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schmidt T, et al. Mechanisms and functions of IL-17 signaling in renal autoimmune diseases. Mol Immunol. 2018;104:90–99. doi: 10.1016/j.molimm.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 16.St Leger AJ, et al. STAT-3-independent production of IL-17 by mouse innate-like alphabeta T cells controls ocular infection. J Exp Med. 2018;215(4):1079–1090. doi: 10.1084/jem.20170369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mitsdoerffer M, et al. Proinflammatory T helper type 17 cells are effective B-cell helpers. Proc Natl Acad Sci U S A. 2010;107(32):14292–14297. doi: 10.1073/pnas.1009234107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bartlett HS, Million RP. Targeting the IL-17-T(H)17 pathway. Nat Rev Drug Discov. 2015;14(1):11–12. doi: 10.1038/nrd4518. [DOI] [PubMed] [Google Scholar]
- 19.Patel DD, et al. Effect of IL-17A blockade with secukinumab in autoimmune diseases. Ann Rheum Dis. 2013;72 Suppl 2:ii116–ii123. doi: 10.1136/annrheumdis-2012-202371. [DOI] [PubMed] [Google Scholar]
- 20.Krebs CF, et al. Pathogen-induced tissue-resident memory TH17 (TRM17) cells amplify autoimmune kidney disease. Sci Immunol. 2020;5(50):eaba4163. doi: 10.1126/sciimmunol.aba4163. [DOI] [PubMed] [Google Scholar]
- 21.Ooi JD, et al. IL-23, not IL-12, directs autoimmunity to the Goodpasture antigen. J Am Soc Nephrol. 2009;20(5):980–989. doi: 10.1681/ASN.2008080891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Z, et al. The role of IL-23/IL-17 axis in lupus nephritis. J Immunol. 2009;183(5):3160–3169. doi: 10.4049/jimmunol.0900385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koga T, et al. T cells and IL-17 in lupus nephritis. Clin Immunol. 2017;185:95–99. doi: 10.1016/j.clim.2016.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramani K, Biswas PS. Emerging roles of the Th17/IL-17-axis in glomerulonephritis. Cytokine. 2016;77:238–244. doi: 10.1016/j.cyto.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 25.Sonder SU, et al. IL-17-induced NF-kappaB activation via CIKS/Act1: physiologic significance and signaling mechanisms. J Biol Chem. 2011;286(15):12881–12890. doi: 10.1074/jbc.M110.199547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Viau A, et al. Lipocalin 2 is essential for chronic kidney disease progression in mice and humans. J Clin Invest. 2010;120(11):4065–4076. doi: 10.1172/JCI42004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Torres-Salido MT, et al. Neutrophil gelatinase-associated lipocalin as a biomarker for lupus nephritis. Nephrol Dial Transplant. 2014;29(9):1740–1749. doi: 10.1093/ndt/gfu062. [DOI] [PubMed] [Google Scholar]
- 28.Haase M, et al. Neutrophil gelatinase-associated lipocalin: a superior biomarker for detection of subclinical acute kidney injury and poor prognosis. Biomark Med. 2011;5(4):415–417. doi: 10.2217/bmm.11.49. [DOI] [PubMed] [Google Scholar]
- 29.Qian Y, et al. The adaptor Act1 is required for interleukin 17-dependent signaling associated with autoimmune and inflammatory disease. Nat Immunol. 2007;8(3):247–256. doi: 10.1038/ni1439. [DOI] [PubMed] [Google Scholar]
- 30.Chang SH, et al. Act1 adaptor protein is an immediate and essential signaling component of interleukin-17 receptor. J Biol Chem. 2006;281(47):35603–35607. doi: 10.1074/jbc.C600256200. [DOI] [PubMed] [Google Scholar]
- 31.Anderson P. Post-transcriptional regulons coordinate the initiation and resolution of inflammation. Nat Rev Immunol. 2010;10(1):24–35. doi: 10.1038/nri2685. [DOI] [PubMed] [Google Scholar]
- 32.O’Connell RM, et al. MicroRNA-155 promotes autoimmune inflammation by enhancing inflammatory T cell development. Immunity. 2010;33(4):607–619. doi: 10.1016/j.immuni.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Garg AV, et al. MCPIP1 endoribonuclease activity negatively regulates interleukin-17-mediated signaling and inflammation. Immunity. 2015;43(3):475–487. doi: 10.1016/j.immuni.2015.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mao R, et al. Regnase-1, a rapid response ribonuclease regulating inflammation and stress responses. Cell Mol Immunol. 2017;14(5):412–422. doi: 10.1038/cmi.2016.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jeltsch KM, et al. Cleavage of roquin and regnase-1 by the paracaspase MALT1 releases their cooperatively repressed targets to promote T(H)17 differentiation. Nat Immunol. 2014;15(11):1079–1089. doi: 10.1038/ni.3008. [DOI] [PubMed] [Google Scholar]
- 36.Du Y, et al. Experimental anti-GBM nephritis as an analytical tool for studying spontaneous lupus nephritis. Arch Immunol Ther Exp (Warsz) 2008;56(1):31–40. doi: 10.1007/s00005-008-0007-4. [DOI] [PubMed] [Google Scholar]
- 37.Shao X, et al. Epithelial-specific Cre/lox recombination in the developing kidney and genitourinary tract. J Am Soc Nephrol. 2002;13(7):1837–1846. doi: 10.1097/01.ASN.0000016444.90348.50. [DOI] [PubMed] [Google Scholar]
- 38.Ramani K, et al. Unexpected kidney-restricted role for IL-17 receptor signaling in defense against systemic Candida albicans infection. JCI Insight. 2018;3(9):e98241. doi: 10.1172/jci.insight.98241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liang J, et al. MCP-induced protein 1 deubiquitinates TRAF proteins and negatively regulates JNK and NF-kappaB signaling. J Exp Med. 2010;207(13):2959–2973. doi: 10.1084/jem.20092641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miao R, et al. Targeted disruption of MCPIP1/Zc3h12a results in fatal inflammatory disease. Immunol Cell Biol. 2013;91(5):368–376. doi: 10.1038/icb.2013.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Monin L, et al. MCPIP1/Regnase-1 restricts IL-17A- and IL-17C-dependent skin inflammation. J Immunol. 2017;198(2):767–775. doi: 10.4049/jimmunol.1601551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ruiz-Romeu E, et al. MCPIP1 RNase is aberrantly distributed in psoriatic epidermis and rapidly induced by IL-17A. J Invest Dermatol. 2016;136(8):1599–1607. doi: 10.1016/j.jid.2016.04.030. [DOI] [PubMed] [Google Scholar]
- 43.Han WK, et al. Kidney injury molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int. 2002;62(1):237–244. doi: 10.1046/j.1523-1755.2002.00433.x. [DOI] [PubMed] [Google Scholar]
- 44.Karlsen JR, et al. Induction of neutrophil gelatinase-associated lipocalin expression by co-stimulation with interleukin-17 and tumor necrosis factor-alpha is controlled by IkappaB-zeta but neither by C/EBP-beta nor C/EBP-delta. J Biol Chem. 2010;285(19):14088–14100. doi: 10.1074/jbc.M109.017129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ruddy MJ, et al. Functional cooperation between interleukin-17 and tumor necrosis factor-alpha is mediated by CCAAT/enhancer-binding protein family members. J Biol Chem. 2004;279(4):2559–2567. doi: 10.1074/jbc.M308809200. [DOI] [PubMed] [Google Scholar]
- 46.Kurts C, et al. The immune system and kidney disease: basic concepts and clinical implications. Nat Rev Immunol. 2013;13(10):738–753. doi: 10.1038/nri3523. [DOI] [PubMed] [Google Scholar]
- 47.Korn T, et al. IL-17 and Th17 Cells. Annu Rev Immunol. 2009;27:485–517. doi: 10.1146/annurev.immunol.021908.132710. [DOI] [PubMed] [Google Scholar]
- 48.Targan SR, et al. A randomized, double-blind, placebo-controlled phase 2 study of brodalumab in patients with moderate-to-severe crohn’s disease. Am J Gastroenterol. 2016;111(11):1599–1607. doi: 10.1038/ajg.2016.298. [DOI] [PubMed] [Google Scholar]
- 49.Lee JS, et al. Interleukin-23-independent IL-17 production regulates intestinal epithelial permeability. Immunity. 2015;43(4):727–738. doi: 10.1016/j.immuni.2015.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maxwell JR, et al. Differential roles for interleukin-23 and interleukin-17 in intestinal immunoregulation. Immunity. 2015;43(4):739–750. doi: 10.1016/j.immuni.2015.08.019. [DOI] [PubMed] [Google Scholar]
- 51.McGeachy MJ, et al. The IL-17 family of cytokines in health and disease. Immunity. 2019;50(4):892–906. doi: 10.1016/j.immuni.2019.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Riedel JH, et al. IL-17F promotes tissue injury in autoimmune kidney diseases. J Am Soc Nephrol. 2016;27(12):3666–3677. doi: 10.1681/ASN.2015101077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Krohn S, et al. IL-17C/IL-17 receptor E signaling in CD4+ T cells promotes TH17 cell-driven glomerular inflammation. J Am Soc Nephrol. 2018;29(4):1210–1222. doi: 10.1681/ASN.2017090949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bar E, et al. IL-17 regulates systemic fungal immunity by controlling the functional competence of NK cells. Immunity. 2014;40(1):117–127. doi: 10.1016/j.immuni.2013.12.002. [DOI] [PubMed] [Google Scholar]
- 55.Liu F, et al. Distinct fate, dynamics and niches of renal macrophages of bone marrow or embryonic origins. Nat Commun. 2020;11(1):2280. doi: 10.1038/s41467-020-16158-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Akira S. Regnase-1, a ribonuclease involved in the regulation of immune responses. Cold Spring Harb Symp Quant Biol. 2013;78:51–60. doi: 10.1101/sqb.2013.78.019877. [DOI] [PubMed] [Google Scholar]
- 57.Annemann M, et al. Atypical IκB proteins in immune cell differentiation and function. Immunol Lett. 2016;171:26–35. doi: 10.1016/j.imlet.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 58.Sun SC. The non-canonical NF-κB pathway in immunity and inflammation. Nat Rev Immunol. 2017;17(9):545–558. doi: 10.1038/nri.2017.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Onishi RM, Gaffen SL. Interleukin-17 and its target genes: mechanisms of interleukin-17 function in disease. Immunology. 2010;129(3):311–321. doi: 10.1111/j.1365-2567.2009.03240.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Willems M, et al. IκBζ: an emerging player in cancer. Oncotarget. 2016;7(40):66310–66322. doi: 10.18632/oncotarget.11624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shen F, et al. Identification of common transcriptional regulatory elements in interleukin-17 target genes. J Biol Chem. 2006;281(34):24138–24148. doi: 10.1074/jbc.M604597200. [DOI] [PubMed] [Google Scholar]
- 62.Li QZ, et al. The lupus-susceptibility gene kallikrein downmodulates antibody-mediated glomerulonephritis. Genes Immun. 2009;10(5):503–508. doi: 10.1038/gene.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.