Abstract
PURPOSE
This study aimed to compare the microshear bond strength (µSBS) of dual-cure resin cement in CAD-CAM zirconia after different cleaning techniques.
MATERIALS AND METHODS
Fifty discs of zirconia-based ceramic from Ivoclar Vivadent were embedded in acrylic resin. The discs were divided into five groups according to the cleaning methods used: Group 1: drying with spraying + sandblasting with Al2O3; Group 2: washed with water and dried with spraying + sandblasting with Al2O3; Group 3: washed with distilled water and dried with spraying + sandblasting with Al2O3 + zirconium oxide (Ivoclean); Group 4: washed with distilled water and dried with spraying + sandblasting with Al2O3 + potassium hydroxide (Zirclean); and Group 5: washed with distilled water and dried with spraying + sandblasting with Al2O3 + 1% NaClO. All of the groups were contaminated with artificial saliva for 1 minute and then cleaned. Statistical analyses were performed using ANOVA and Tukey's tests.
RESULTS
There were statistically significant differences among all groups for µSBS (P < .05). The group treated with zirconium oxide (Group 3) showed the highest µSBS (18.75 ± 0.23 MPa).
CONCLUSION
When applied to zirconia, the cleaning methods affected the bonding with resin cement differently.
Keywords: Zirconia, Ceramics, Dental cements, Cleaning, Mechanical test
INTRODUCTION
Metal-free dental prostheses are used widely due to their biocompatibility and superior aesthetic properties.1,2 Zirconia is one of the most commonly used materials for such prostheses, which can be used for bridge infrastructures, monolithic crowns, and implant abutments in dentistry.3,4 One of the most significant advantages imparted by metal-free prosthesis is the marginal adaptation, which avoids microleakage and increases retention.5 In this context, zirconia-based ceramics have shown suitable properties due to their aesthetic appearance and biocompatible properties compared to metal and porcelain restorations.3 The reduced laboratory costs for CAD-CAM metal-free restorations have assisted with their availability.6 All restorative materials, including zirconia-based materials, must be tested clinically to determine whether they have adequate marginal adaptation or require occlusal adjustment. Previous studies have shown that contamination of zirconia with saliva, blood, or silicone reduces the bond strength between the zirconia and the resin cement.7,8,9,10,11 The luting procedure, a cleaning process for zirconia, could be an effective method to improve the bonding and maintain the reliability of prosthetic treatment.12,13
Despite the excellent properties that zirconia offers to dentistry, this ceramic also displays significant challenges in its bonding ability. Zirconia offers lower adhesion compared to other ceramics, such as feldspathic porcelain and lithium disilicate, due to zirconia's higher crystalline phase content.14,15 The most commonly used method to improve the bond strength between resin cements and zirconia is with aluminum oxide (Al2O3, with 50 to 100 µm particles) by sandblasting.16,17,18 However, this process may produce cracks, making zirconia more susceptible to fractures.19 To overcome this issue, chemical bonds with zirconia have been proposed by incorporating-methacryloyloxydecyl dihydrogen phosphate (10-MDP) into primers and resin cements to promote ionic and hydrogen bonding to zirconia.4,20,21,22,23
Besides the concerns with bonding due to zirconia's high crystallinity phase, steps for cleaning zirconia prior to cementation have been investigated to eliminate saliva and organic contaminants and generate proper chemical adhesion.8,9,11 Some studies24,25,26,27,28 have examined the benefits of cleaning agents such as those with zirconium oxide (commercially available as Ivoclean) and sodium hypochlorite at 1% (NaClO). Other substances could be used to remove organic residue, such as potassium hydroxide. However, no studies have analyzed the effects of potassium hydroxide (commercially available as Zirclean) in this regard. After different cleaning techniques, this study compares the microshear bond strength (µSBS) of dual-cure resin cement in CAD-CAM zirconia. The null hypothesis to be tested is that using chemical agents for cleaning after sandblasting and posterior application of primer does not influence the µSBS to zirconia.
MATERIALS AND METHODS
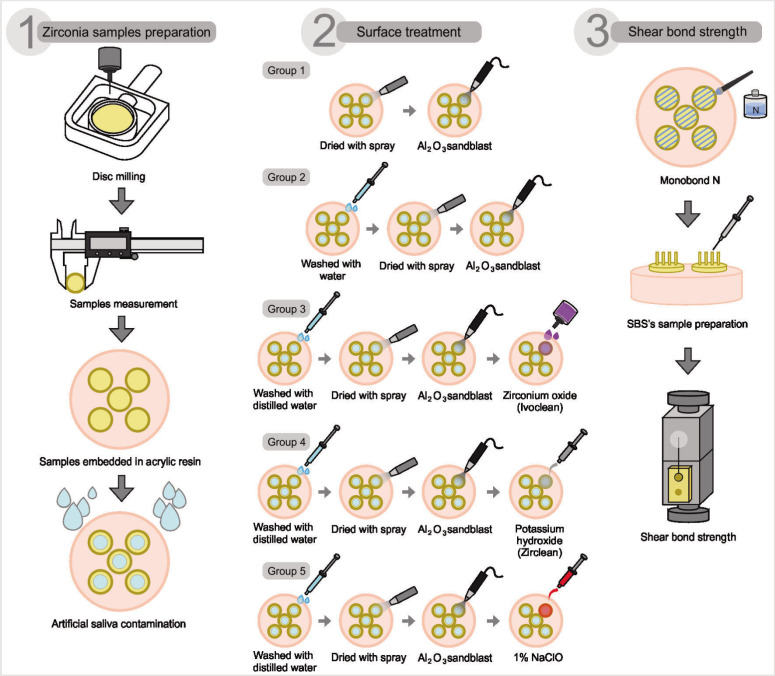
This study was performed in vitro, following the standards of and the guidance from the Ethics Committee of the Universidad Científica Del Sur, Perú. A pilot study was performed before the current study. A summarized flowchart of the study design is presented in Fig. 1.
Fig. 1. Flowchart of the study indicating the five groups tested via µSBS.
The Specimen preparation was fifty discs of zirconia (IPS MT A1, Ivoclar Vivadent AG, Schaan, Liechtenstein) measuring 11 mm in diameter and 3 mm thick were used in this study. The manufacturing process utilized a CAD/CAM milling machine (Wieland Dental ZENOTEC mini, Ivoclar Vivadent, Lindenstr.2,75175, Pfozheim, Germany). The sintering process was performed at 1500℃ to 1700℃ according to the manufacturer's instructions.29 One surface of each disc was tested and sandblasted with Al2O3 at 50 µm for 15 s at 10 mm and 2.5 bar. The samples were cleaned ultrasonically in isopropyl alcohol for 3 min, rinsed with distilled water, and dried.30 Subsequently, the ceramic surfaces were embedded in a polyvinyl chloride (PVC) tube (25 mm diameter and 40 mm height) using a self-cured acrylic resin.16 All of the materials tested in this study are shown in Table 1. The zirconia discs were divided into five groups (n = 10 per group). All of them were subjected to contamination with artificial saliva (Salival, LUSA laboratory, Lima, Perú). Artificial saliva was used due to its higher standardization compared to human saliva and no need for approval by an ethics committee. The artificial saliva used in this research has the same composition as previous studies.26,31 Afterward, all the samples for each group were prepared as follows (Fig. 2).
Table 1. Description of the commercial products materials name, composition, and manufacturers used in the study.
| Materials | Composition | Manufacturer | Lot no. |
|---|---|---|---|
| IPS e-max ZirCAD MT A1 - Ivoclar Vivadent AG | ZrO2 (86.0 – 93.5%), Y2O3 (> 6.5 % – ≤ 8.0 %), HF (≤ 5.0%), Al2O3 ≤ 1.0%, other oxides ≤ 1.0% | Ivoclar Vivadent, Schaan, Lichtenshtein | W31929 |
| Al2O3 | 50 μm aluminum oxide powder | Bio‑Art Equipamentos Odontológicos Ltda, São Carlos, SP, Brazil | 19-00586 |
| Ivoclean | Sodium hydroxide, ZrO2, water, polyethylene glycol, pigments | Ivoclar Vivadent, Schaan, Lichtenshtein | X36169 |
| Zirclean | Potassium hydroxide | Bisco, Schaumburg, IL, USA | REF B-7351 |
| Monobond N | Ethanol, 3-(trimethoxysilyl) propyl methacrylate, methacrylated phosphoric acid ester, disulfide methacrylate | Ivoclar Vivadent, Liechtenstein | Y19262 |
| SET PP Self-adhesive, self-etching, fluorine-releasing resin cement |
35% methacrylate 65% inorganic filler |
SeT PP, SDI, Victoria, Australia | S19031091 |
| Artificial Saliva | Sodium chloride 0.084 g, potassium chloride 0.120 g, calcium chloride dihydrate 0.015 g, magnesium chloride hexahydrate 0.005 g, carboxymethylcellulose sodium 0.375 g, propylene glycol 4,000 g, propylparaben 0.010 g, distilled water qs. 100.00 mL | Salival, LUSA laboratory, Lima, Perú | 1080218 |
Fig. 2. Illustration evidencing the step-by-step of the present study design.
Group 1 (control group): The samples were contaminated with artificial saliva for 1 min, then dried with a spray for 15 s and sandblasted with Al2O3 at 50 µm for 20 s at 10 mm at 2.5 bar.
Group 2: The samples were contaminated with artificial saliva for 1 min and then rinsed with water-spraying for 15 s, dried with a spray for 15 s, and sandblasted with Al2O3 at 50 µm for 20 s at 10 mm at 2.5 bar.
Group 3: The samples were contaminated with artificial saliva for 1 min and then rinsed with water-spraying for 15 s, dried with spray for 15 s, and sandblasted with Al2O3 at 50 µm for 20 s at a distance of 10 mm at 2.5 bar. Zirconium oxide (Ivoclean) was applied with a microbrush. It was allowed to react for 20 s on the surface, which then was rinsed with water spray for 30 s and air dried for another 10 s according to the manufacturer's instructions.
Group 4: Treated the same as Group 3 until sandblasting. Then, potassium hydroxide (Zirclean) was applied. The product was allowed to react for 20 s, after which rinsing with water spray continued for 30 s, followed by air-drying for 10 s according to the manufacturer's instructions.
Group 5: Treated the same way as Group 3 until sandblasting. Then, sodium hypochlorite (1% NaClO) was applied. The product was allowed to react for 20 s, and the samples were rinsed with water spray for 30 s and air dried for 10 s.
Immediately after all of the groups were prepared with their respective cleaning methods, Monobond Plus primer (Ivoclar Vivadent) was applied to all specimens with a microbrush for 60 s. Then, the surface was gently dried with air.32
After each cleaning and conditioning treatment, three Tygon plastic tubes (1 mm internal diameter and 3 mm thick) were filled with the resin cement SET PP SDI (dual-cure resin cement SeT PP, SDI, Victoria, Australia). The manipulation was performed according to the manufacturer's recommendation. The dual-cure resin cement was photoactivated for 20 s with 1100 mW/cm (Elipar™ DeepCure-L 3M™ Oral Care, St. Paul, MN, USA). After 10 min, the tubes were removed using a no. 11 scalpel blade to expose the cement cylinders. The specimens were stored in distilled water for 24 h at 37℃.33
The sample unit consisted of 10 disks per group (five total groups) of zirconia ceramics with three cement cylinders each (Tygon, Medical Accessories, Lima, Perú). Microshear bond strength (µSBS) was evaluated using a universal testing machine in all of the disks (Universal testing machine, LG CMT-5L number 7419, Seoul, South Korea). A steel hook was used to pull each resin cement cylinder, applying a shear force of 0.75 mm/min until fracture.26,34,35
After SBS testing, the debonded zirconia ceramic specimens were examined under microscopy (Andonstar ADSM201, Shenzhen Andonstar Technology Co. Ltd., Shenzhen, Guangdong, China) and magnification of 1600 ×. The failures were classified as adhesive failures between the zirconia disc and cement cylinders, cohesive failures in cement cylinders, or mixed failures. The failure pattern was calculated as percentages of each group.
All of the statistical analyses were performed using SPSS version 23 (SPSS Inc., Armonk, NY, USA). The data distributions were analyzed with the Shapiro-Wilk test, and the results of the µSBS tests were analyzed via a one-way analysis of variance (ANOVA) and Tukey post-hoc test. A 5% significance level was used.
RESULTS
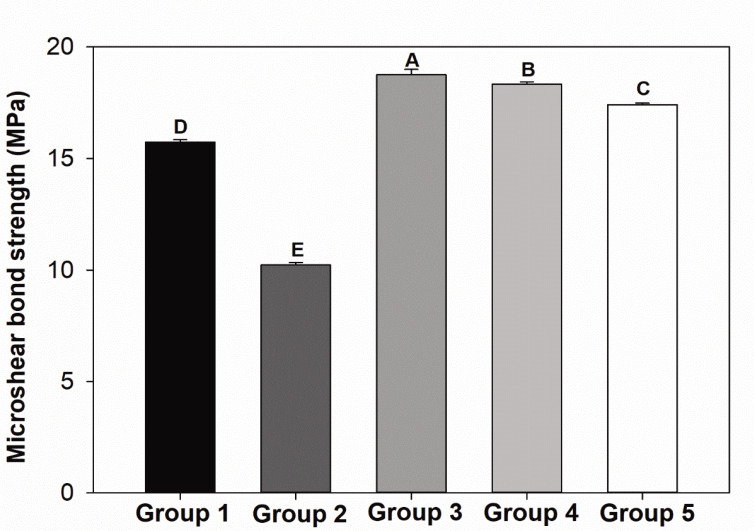
Fig. 3 shows the outcomes as mean and microshear values of MPa. The group treated with Ivoclean (Group 3) showed the highest µSBS (18.75 ± 0.23 MPa), while the group washed with water, dried with spray, and sandblasted (Group 2) showed the lowest value (10.22 ± 0.10 MPa) (P < .05).
Fig. 3. Results of µSBS of dual-cure resin cement on zirconia after treatment with one of the five cleaning techniques applied. The results are displayed in mean and standard deviation values of MPa. Different letters indicate a statistically significant difference among groups (P < .05).
The groups presented the following decreasing order of µSBS levels: Group 3, Group 4, Group 5, Group 1, and Group 2 (P < .05). The use of any cleaning agents tested (Groups 3, 4, and 5) increased the µSBS in comparison to only sandblasting (Group 1) or rinsing with water and sandblasting (Group 2) (P < .05).
The failure modes are presented in Table 2. Cohesive failure was observed among the most groups. Only one group showed a low incidence of adhesive failure. Mixed failures were not predominant for the zirconium ceramics.
Table 2. Failure pattern for tested specimens (in percentage).
| Group | Failure Model | ||
|---|---|---|---|
| Cohesive | Adhesive | Mixed | |
| Group 1: drying with spray + sandblast with Al2O3 | 88 | 9 | 3 |
| Group 2: washed with water and dried with spray + sandblast with Al2O3 | 40 | 50 | 10 |
| Group 3: washed with distilled water and dried with spray + sandblast with Al2O3 + zirconium oxide (Ivoclean) | 100 | 0 | 0 |
| Group 4: washed with distilled water and dried with spray + sandblast with Al2O3 + potassium hydroxide (Zirclean) | 100 | 0 | 0 |
| Group 5: washed with distilled water and dried with spray + sandblast with Al2O3 + 1% NaClO | 98 | 2 | 0 |
DISCUSSION
Previous studies investigated the effects of cleaning agents for zirconia, such as water, 37% phosphoric acid, and NaClO, because of the decreased bond strength when saliva contaminants are present on ceramic surfaces.8,9 Zirconia has strong adsorption potential for phosphorus, which is found in saliva. Consequently, it is adsorbed on the surface of zirconia. Due to this reason, saliva contamination is not removed only with a water wash.9 In the current research, the use of cleaning agents improved the µSBS compared to no cleaning agents. These agents are recommended to remove saliva contamination on the inner surface of restorations before cementation because they are able to eliminate and remove organic materials, magnesium, and carbonate ions from zirconia's surface.24,32 Thus, the null hypothesis must be rejected.
The main components of saliva are water (99%), glycoproteins, mucins, enzymes, immunoglobulins, nitrogenous products, and electrolytes,36 which are similar to artificial saliva.31 Saliva is adsorbed onto zirconia easily, and other elements can contaminate the ceramic's surface, such as carbon compounds.12 Organic solvents (acetone or isopropanol) have already been tested as cleaning agents, but they have shown incomplete remotion of organic contaminants.12 Phosphoric acid at 37% showed a better cleaning effect but lower bond strength, in comparison to Ivoclean.32,37 Neither water nor phosphoric acid solution at 37% fully removes saliva contaminants because phosphoric acid has phosphates that are compatible with the phosphates in saliva, which bind with zirconia and decreases the adhesion force.9,24 Besides the sandblasting being essential for increasing the surface roughness, the best outcomes from luting zirconia involve combining physical (sandblasting) and chemical (chemical agents such as 10-MDP) approaches.38 However, sandblasting should be used with caution because excessive abrasion will weaken the zirconia. For this reason, it is reasonable to investigate how to improve the interactions between bonding agents and zirconia by removing improper elements from saliva contaminants.
Ceramics can be challenging materials for adhesion, depending on their composition and physicochemical surface properties. Contamination could occur at different steps, from the try-in procedures to the final luting of the restorations.11 In this context, few studies have compared cleaning agents, and no studies have evaluated the effect of potassium hydroxide on the zirconia's surfaces. According to the manufacturer (Bisco), Zirclean is a strong alkaline gel formulated with potassium hydroxide. It is a strong alkaline solution that can clean contaminants from restorations increasing the adhesive strength. NaClO also has been tested due to its well-known dissolution properties and consequent use as an endodontic irrigation solution. This solution has been used as an endodontic disinfectant due to its effective antimicrobial and tissue dissolving capabilities.39,40 Although all tested cleaning methods obtained better results than the group cleaned with water or sandblasting only, Ivoclean showed the highest µSBS, with a statistically significant difference. The rationale for the easy interaction between Ivoclean and the phosphorus is present in saliva.
There are different mechanisms of action to obtain a clean surface. According to manufacturer Ivoclar Vivadent, Ivoclean's main components are sodium hydroxide and ZrO2. This hyper-saturated solution of zirconium particles removes contaminants from saliva, which are attracted to the Ivoclean chemical solution.24,32 Therefore, the cleaning agent consists of an alkaline solution with a suspension of particles, a hydrophilic character, and a low contact angle on zirconia. The contaminants react with the sodium hydroxide and are removed after the Ivoclean is adsorbed on the surface.8,24 Even though the primary mechanism of all the tested commercial cleaning agents seems to be an acid-base reaction on the zirconia's surfaces, Ivoclean achieved the highest µSBS. This finding corroborates a previous study showing better outcomes for Ivoclean than common agents such as phosphoric acid at 37%.9 It was not possible to identify why Groups 1 and 2 showed a statistical difference, in that the only difference was the use of water before sandblasting for Group 2. However, it is possible to conclude that bond strength improved when a set of measures was used beyond just sandblasting or water and sandblasting
In the present study, the failure mode which was predominantly cohesive was found in a complementary way to the SBS test. It indicates that the stresses generated during the micro-shear test occurred at the level of the resin cement and not at the level of the materials' adhesion.
Further research could focus on the longitudinal effects of cleaning agents on the bonding to zirconia. Moreover, a more in-depth understanding of cleaning agents' mechanism on zirconia surfaces and chemical analyses of the cleaning agents, including pH analysis, are needed to determine why some commercially available materials provide better immediate outcomes.
CONCLUSION
The cleaning methods applied to zirconia affected the bonding with the dual-cure resin cement differently. The cleaning methods involving zirconium oxide led to the highest µSBS results, followed by potassium hydroxide.
ACKNOWLEDGEMENTS
To my mother Carmen my angel in heaven. In addition the authors gratefully acknowledge DDS Hernán Rodolfo Calle-Chávez for the experimental procedures, Daniel Valverde Angulo for the dental laboratory support, and Robert Eusebio Teheran for the technical support. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001 (scholarship of I.M.G.).
References
- 1.Zhang Y, Lawn BR. Novel zirconia materials in dentistry. J Dent Res. 2018;97:140–147. doi: 10.1177/0022034517737483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bavbek NC, Roulet JF, Ozcan M. Evaluation of microshear bond strength of orthodontic resin cement to monolithic zirconium oxide as a function of surface conditioning method. J Adhes Dent. 2014;16:473–480. doi: 10.3290/j.jad.a32812. [DOI] [PubMed] [Google Scholar]
- 3.Miyazaki T, Nakamura T, Matsumura H, Ban S, Kobayashi T. Current status of zirconia restoration. J Prosthodont Res. 2013;57:236–261. doi: 10.1016/j.jpor.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Koizumi H, Nakayama D, Komine F, Blatz MB, Matsumura H. Bonding of resin-based luting cements to zirconia with and without the use of ceramic priming agents. J Adhes Dent. 2012;14:385–392. doi: 10.3290/j.jad.a22711. [DOI] [PubMed] [Google Scholar]
- 5.Tabatabaian F. Color in zirconia-based restorations and related factors: a literature review. J Prosthodont. 2018;27:201–211. doi: 10.1111/jopr.12740. [DOI] [PubMed] [Google Scholar]
- 6.Baroudi K, Ibraheem SN. Assessment of chair-side computer-aided design and computer-aided manufacturing restorations: a review of the literature. J Int Oral Health. 2015;7:96–104. [PMC free article] [PubMed] [Google Scholar]
- 7.Nejatidanesh F, Savabi O, Savabi G, Razavi M. Effect of cleaning methods on retentive values of saliva-contaminated implant-supported zirconia copings. Clin Oral Implants Res. 2018;29:530–536. doi: 10.1111/clr.13150. [DOI] [PubMed] [Google Scholar]
- 8.Yoshida K. Influence of cleaning methods on resin bonding to saliva-contaminated zirconia. J Esthet Restor Dent. 2018;30:259–264. doi: 10.1111/jerd.12369. [DOI] [PubMed] [Google Scholar]
- 9.Takahashi A, Takagaki T, Wada T, Uo M, Nikaido T, Tagami J. The effect of different cleaning agents on saliva contamination for bonding performance of zirconia ceramics. Dent Mater J. 2018;37:734–739. doi: 10.4012/dmj.2017-376. [DOI] [PubMed] [Google Scholar]
- 10.Yang B, Wolfart S, Scharnberg M, Ludwig K, Adelung R, Kern M. Influence of contamination on zirconia ceramic bonding. J Dent Res. 2007;86:749–753. doi: 10.1177/154405910708600812. [DOI] [PubMed] [Google Scholar]
- 11.Angkasith P, Burgess JO, Bottino MC, Lawson NC. Cleaning methods for zirconia following salivary contamination. J Prosthodont. 2016;25:375–379. doi: 10.1111/jopr.12441. [DOI] [PubMed] [Google Scholar]
- 12.Yang B, Scharnberg M, Wolfart S, Quaas AC, Ludwig K, Adelung R, Kern M. Influence of contamination on bonding to zirconia ceramic. J Biomed Mater Res B Appl Biomater. 2007;81:283–290. doi: 10.1002/jbm.b.30664. [DOI] [PubMed] [Google Scholar]
- 13.Yang B, Lange-Jansen HC, Scharnberg M, Wolfart S, Ludwig K, Adelung R, Kern M. Influence of saliva contamination on zirconia ceramic bonding. Dent Mater. 2008;24:508–513. doi: 10.1016/j.dental.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Quigley NP, Loo DSS, Choy C, Ha WN. Clinical efficacy of methods for bonding to zirconia: a systematic review. J Prosthet Dent. 2021;125:231–240. doi: 10.1016/j.prosdent.2019.12.017. [DOI] [PubMed] [Google Scholar]
- 15.Melo RM, Souza RO, Dursun E, Monteiro EB, Valandro LF, Bottino MA. Surface treatments of zirconia to enhance bonding durability. Oper Dent. 2015;40:636–643. doi: 10.2341/14-144-L. [DOI] [PubMed] [Google Scholar]
- 16.Petrauskas A, Novaes Olivieri KA, Pupo YM, Berger G, Gonçalves Betiol EÁ. Influence of different resin cements and surface treatments on microshear bond strength of zirconia-based ceramics. J Conserv Dent. 2018;21:198–204. doi: 10.4103/JCD.JCD_190_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shahin R, Kern M. Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent Mater. 2010;26:922–928. doi: 10.1016/j.dental.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 18.Cavalcanti AN, Foxton RM, Watson TF, Oliveira MT, Giannini M, Marchi GM. Bond strength of resin cements to a zirconia ceramic with different surface treatments. Oper Dent. 2009;34:280–287. doi: 10.2341/08-80. [DOI] [PubMed] [Google Scholar]
- 19.Ranjbar Omidi B, Karimi Yeganeh P, Oveisi S, Farahmandpour N, Nouri F. Comparison of micro-shear bond strength of resin cement to zirconia with different surface treatments using universal adhesive and zirconia primer. J Lasers Med Sci. 2018;9:200–206. doi: 10.15171/jlms.2018.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blatz MB, Alvarez M, Sawyer K, Brindis M. How to bond zirconia: the APC concept. Compend Contin Educ Dent. 2016;37:611–617. [PubMed] [Google Scholar]
- 21.Tanış MÇ, Akay C, Karakış D. Resin cementation of zirconia ceramics with different bonding agents. Biotechnol Biotechnol Equip. 2015;29:363–367. doi: 10.1080/13102818.2014.996606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stefani A, Brito RB, Jr, Kina S, Andrade OS, Ambrosano GM, Carvalho AA, Giannini M. Bond strength of resin cements to zirconia ceramic using adhesive primers. J Prosthodont. 2016;25:380–385. doi: 10.1111/jopr.12334. [DOI] [PubMed] [Google Scholar]
- 23.Chuang SF, Kang LL, Liu YC, Lin JC, Wang CC, Chen HM, Tai CK. Effects of silane- and MDP-based primers application orders on zirconia-resin adhesion-a ToF-SIMS study. Dent Mater. 2017;33:923–933. doi: 10.1016/j.dental.2017.04.027. [DOI] [PubMed] [Google Scholar]
- 24.Kim DH, Son JS, Jeong SH, Kim YK, Kim KH, Kwon TY. Efficacy of various cleaning solutions on saliva-contaminated zirconia for improved resin bonding. J Adv Prosthodont. 2015;7:85–92. doi: 10.4047/jap.2015.7.2.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Irmak Ö, Yaman BC, Orhan EO, Kılıçarslan MA, Mante FK, Ozer F. Influence of cleaning methods on bond strength to saliva contaminated zirconia. J Esthet Restor Dent. 2018;30:551–556. doi: 10.1111/jerd.12416. [DOI] [PubMed] [Google Scholar]
- 26.Wattanasirmkit K, Charasseangpaisarn T. Effect of different cleansing agents and adhesive resins on bond strength of contaminated zirconia. J Prosthodont Res. 2019;63:271–276. doi: 10.1016/j.jpor.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 27.Negreiros WM, Ambrosano GMB, Giannini M. Effect of cleaning agent, primer application and their combination on the bond strength of a resin cement to two yttrium-tetragonal zirconia polycrystal zirconia ceramics. Eur J Dent. 2017;11:6–11. doi: 10.4103/ejd.ejd_276_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Charasseangpaisarn T, Wiwatwarrapan C, Siriwant N, Khochachan P, Mangkorn P, Yenthuam P, Thatphet P. Different cleasing methods effect to bond strength of contaminated zirconia. J Dent Assoc Thailand. 2018;68:28–35. [Google Scholar]
- 29.Zandparsa R, Talua NA, Finkelman MD, Schaus SE. An in vitro comparison of shear bond strength of zirconia to enamel using different surface treatments. J Prosthodont. 2014;23:117–123. doi: 10.1111/jopr.12075. [DOI] [PubMed] [Google Scholar]
- 30.Kim MJ, Kim YK, Kim KH, Kwon TY. Shear bond strengths of various luting cements to zirconia ceramic: surface chemical aspects. J Dent. 2011;39:795–803. doi: 10.1016/j.jdent.2011.08.012. [DOI] [PubMed] [Google Scholar]
- 31.J Pytko-Polonczyk J, Jakubik A, Przeklasa-Bierowiec A, Muszynska B. Artificial saliva and its use in biological experiments. J Physiol Pharmacol. 2017;68:807–813. [PubMed] [Google Scholar]
- 32.Feitosa SA, Patel D, Borges AL, Alshehri EZ, Bottino MA, Özcan M, Valandro LF, Bottino MC. Effect of cleansing methods on saliva-contaminated zirconia-an evaluation of resin bond durability. Oper Dent. 2015;40:163–171. doi: 10.2341/13-323-L. [DOI] [PubMed] [Google Scholar]
- 33.Flores-Ferreyra BI, Scougall-Vilchis RJ, Velazquez-Enriquez U, Garcia-Contreras R, Aguillon-Sol L, Olea-Mejia OF. Effect of airborne-particle abrasion and, acid and alkaline treatments on shear bond strength of dental zirconia. Dent Mater J. 2019;38:182–188. doi: 10.4012/dmj.2018-078. [DOI] [PubMed] [Google Scholar]
- 34.Zeidan LC, Esteves CM, Oliveira JA, Brugnera A, Jr, Cassoni A, Rodrigues JA. Effect of different power settings of Er,Cr:YSGG laser before or after tribosilicatization on the microshear bond strength between zirconia and two types of cements. Lasers Med Sci. 2018;33:233–240. doi: 10.1007/s10103-017-2343-2. [DOI] [PubMed] [Google Scholar]
- 35.Milleding P, Carlén A, Wennerberg A, Karlsson S. Protein characterisation of salivary and plasma biofilms formed in vitro on non-corroded and corroded dental ceramic materials. Biomaterials. 2001;22:2545–2555. doi: 10.1016/s0142-9612(00)00445-2. [DOI] [PubMed] [Google Scholar]
- 36.Humphrey SP, Williamson RT. A review of saliva: normal composition, flow, and function. J Prosthet Dent. 2001;85:162–169. doi: 10.1067/mpr.2001.113778. [DOI] [PubMed] [Google Scholar]
- 37.Quaas AC, Yang B, Kern M. Panavia F 2.0 bonding to contaminated zirconia ceramic after different cleaning procedures. Dent Mater. 2007;23:506–512. doi: 10.1016/j.dental.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 38.Özcan M, Bernasconi M. Adhesion to zirconia used for dental restorations: a systematic review and meta-analysis. J Adhes Dent. 2015;17:7–26. doi: 10.3290/j.jad.a33525. [DOI] [PubMed] [Google Scholar]
- 39.Spencer HR, Ike V, Brennan PA. Review: the use of sodium hypochlorite in endodontics-potential complications and their management. Br Dent J. 2007;202:555–559. doi: 10.1038/bdj.2007.374. [DOI] [PubMed] [Google Scholar]
- 40.Tanaka J, Nakai H. Application of root canal cleaning agents having dissolving abilities of collagen to the surface treatment for enhanced bonding of resin to dentin. Dent Mater J. 1993;12:196–208. doi: 10.4012/dmj.12.196. [DOI] [PubMed] [Google Scholar]