Abstract
Introduction
Racial bias in health care is well documented. Research shows the presence of racial bias among health care providers. There is a paucity of workshops focused on racial bias effects in health professions educators.
Method
Two to three workshops were delivered to a diverse group of clinical educators from three programs at a major academic institution. Each workshop included a brief multimedia presentation followed by a facilitated group discussion. Participants completed the online Implicit Association Test (IAT), a baseline demographic questionnaire, and a brief post-then-pre questionnaire.
Results
Twenty-four faculty participated in the study (six physicians, eight nurse practitioners, 10 physician assistants). Nineteen (90%) were women, 18 (86%) were White, nine (43%) had more than 10 years of experience as educators, and seven (35%) had previously participated in a biases program. Seventeen completed the IAT. Sixteen educators agreed or strongly agreed that bias has a significant impact on patients' outcomes at the end of the workshop compared to 17 before the workshop. Seventeen educators agreed or strongly agreed that recognizing their own racial bias would positively alter their teaching practice after the workshop compared to 15 before the workshop.
Discussion
This series of workshops was created to fill a gap regarding the impact of racial bias on patient outcomes, health disparities, and health professions education. The impact of racial bias in health professions education and the long-term impact of awareness and knowledge of racial bias in education are areas needing further evaluation.
Keywords: Bias, Educators, Race, Awareness, Nurse/Nurse Practitioner, Physician, Physician Assistant, Anti-racism
Educational Objectives
By the end of this workshop, participants will be able to:
-
1.
Describe the impact of racial bias on patients' care, outcomes, health disparities, and health professions education.
-
2.
Recognize how educators' individual racial biases impact learners.
-
3.
Develop strategies to mitigate the impact of educators' personal racial bias in health professional education and teaching.
Introduction
Racial and ethnic health disparities are well documented in the health professions literature. The Institute of Medicine's Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care, published in 2003, led to increasing awareness and a national priority.1 This landmark report provided extensive evidence of racial and ethnic disparities in health outcomes and health care access. These disparities exist regardless of a patient's socioeconomic status, suggesting that other factors may be contributing to negative health care outcomes. One of the many factors contributing to health disparities is racism. Furthermore, implicit racial bias (also known as unconscious bias) is one of the contributing factors that has attracted considerable attention in the literature and is the focus of many articles and reports, including the proceedings of the Diversity and Inclusion Innovation Forum published by the Association of American Medical Colleges.2 The unconscious bias hypothesis, which is widely quoted in social psychology research, says that bias can occur without recognition and can affect how medical providers care for patients. Other studies have documented the impact of racial bias in health care delivery and demonstrated health care provider bias about patients' race/ethnicity.3–8
The biases described above influence health care professionals' behavior in unintentional but powerful and systematic ways, profoundly impacting clinical decision-making.9 Biases of educators also have a profound influence on students and trainees as they model their educators' behaviors and actions toward peers and students. Furthermore, research has demonstrated that nonverbal expressions of racial bias can be contagious.10 While there has been an increase in awareness and interventions regarding the impact of racial bias in patient care and medical education, the focus has mainly been on learners rather than educators.7,8,11–19 Few published studies and curricula on racial bias explicitly target health professional educators, making this an existing and significant gap.
Increasing awareness of racial and ethnic disparities in health care among physicians has been cited as an important step to decreasing health disparities.9–19 However, implicit bias in health professions needs to be addressed at all levels by increasing awareness and encouraging a continuous process of practice, feedback, and reflection.19
Health professions educators significantly influence learners through role modeling and direct instruction. Therefore, it is imperative to examine racial bias among interprofessional health professions educators. In 2015, with the support from the Duke University School of Medicine Academy for Health Professions Education and Academic Development (Duke AHEAD), a team of health professions educators developed a series of workshops. The goal of these workshops was to increase health care professions educators' awareness of their conscious and unconscious racial biases and how these could impact their patients' outcomes and education. The target audience was intentionally identified as an interdisciplinary group of health professions educators, a group not previously targeted in this type of work. Previous workshops, including those published in MedEdPORTAL, focused on students, faculty, and learners in clinical rounds, as well as search committees.15,16,20 Similar to our workshop, some of the previously published work utilized the Implicit Association Test (IAT) as a tool to increase awareness of participants' own biases through small-group discussions.15,16,21 Our workshop was unique compared to previously published work because our target audience was an interprofessional group of educators (physicians, nurse practitioners, and physician assistants), we used newly developed multimedia presentations, and we incorporated techniques to mitigate one's own racial bias in both the classroom and clinical settings.
Methods
Framework
This project used the Kern curriculum development framework, which included the following six steps: (1) identifying the existing gap by conducting a literature review; (2) targeting a needs assessment by reviewing prior work in racial biases in medical education; (3) developing the workshop learning objectives; (4) creating an educational strategy that included a multimedia presentation, facilitator guide, and facilitated group discussions; (5) developing an implementation strategy (i.e., obtaining financial support to develop the multimedia presentation, database, and deployment of the workshop); and (6) identifying measurable outcomes.22
Implementation
An interdisciplinary team of faculty and learners created and delivered the series of workshops. Learners participated in the development of multimedia presentations and surveys in order to incorporate their perspectives into the materials. We created three multimedia presentations to fit the learning objectives.
The first workshop provided the overall course goals and defined and explained the relationship between implicit bias, health disparities, and health professions education. The first multimedia presentation included the perspective of a medical student. The second workshop built upon the first and introduced Bennett's developmental model of intercultural sensitivity, a framework created to explain how people experience and engage with cultural differences.23–25 Grounded in theory and Bennett's observations, the model posited a continuum of cultural awareness that goes from ethnocentrism (denial and defense) to ethnorelativism (adaptation and integration). The third workshop relayed strategies and teaching techniques for health professions educators to mitigate the impact of racial biases in teaching in the classroom and clinical settings.
The target audience included health professions faculty with teaching responsibilities (physicians, nurse practitioners, and physician assistants) from the Duke School of Medicine (MD and physician assistant programs) and the School of Nursing (nurse practitioner program). Prior experience or training concerning racial bias was not required. All faculty members were invited to the workshop via email. To maximize learning and active participation, attendance was limited to no more than 20 participants per group. The workshops included three different cohorts with one for each group of educators (physicians, nurse practitioners, and physician assistants). Faculty who expressed interest were invited to one of the three groups based on their health professions program.
In preparation for the workshops, the facilitator and notetaker met to discuss their roles and the logistical plans for the session. These discussions included reviewing the participant list to become familiar with the participants/audience, materials needed, audiovisual needs, and room layout. The facilitator, who had prior experience, led the group discussions as an experienced facilitator was important due to the sensitive nature of the conversations and the current climate in this country. Before each workshop, we sent participants a reminder that included the date, time, and location of the workshop. We strongly encouraged participants to attend the complete workshop series.
Before the first session, we collected informed consent. We collected participants' demographic information using an online survey (Appendix A). All participants self-reported IAT results (Appendix A).26 The IAT was utilized to make participants aware of their own racial bias and preferences.
Each workshop lasted up to 90 minutes, allowing time for setup, multimedia presentation, discussion, and closing. The workshops were held in the corresponding school of each faculty group (medical school or health system building, nursing school, and physician assistant school).
The facilitated group discussions began with welcoming remarks, a review of the workshop objectives, a brief participants' introduction, and an icebreaking activity (Appendix B). The icebreaking activity asked participants, “Share with others one thing about yourself that others may not know just by looking at you.” The multimedia presentation immediately followed the icebreaking activity. After the multimedia presentation (Appendices C–E), the facilitator began the discussion with ground rules and guides. The group also generated additional ground rules. Then, the facilitator explained the need to create a safe space and a brave space during the discussion, reinforced how each participant's story was valuable, and stated the importance of acknowledging and being open to recognizing one's own racial biases. Facilitators used prompts to encourage group discussion and validated participants who expressed their thoughts even when it was uncomfortable for them to share.
In some instances, the facilitated group discussion was prolonged to a total of 90 minutes. The duration of the workshop was determined by group size, participant engagement, and participation.
The workshops were delivered and facilitated as follows:
-
•
Introduction of session's objectives and facilitators (Appendix B): 5 minutes.
-
•
Multimedia presentation, one video per session. Session 1's video (Appendix C) was 15:08 minutes, session 2's video (Appendix D) was 7:02 minutes, and session 3's video (Appendix E) was 5:36 minutes.
-
•
Facilitated group discussion (Appendix B): approximately 30–45 minutes.
-
•
Closing with debriefing and reminder of the next session date and time (only after sessions 1 and 2): 5 minutes.
Participants completed an end-of-the-program survey using a retrospective post-then-pre survey based on a design strategy endorsed by the University of Wisconsin.27 The four-question survey (Appendix F) was administered to participants to self-assess the impact of racial bias in patient outcomes and teaching styles. Participants ranked their knowledge as it stood after and then before participation in the program.
We created each survey using the REDCap platform, a secure, web-based application designed to support data capture.28 We obtained Institutional Review Board approval for this workshop.
Materials for in-person workshops included the following:
-
•
List of participants to record attendance.
-
•
Pens.
-
•
Audiovisual equipment, including computer and projector.
-
•
Chairs and tables to support approximately 10–20 participants.
-
•
Flip chart and markers to take notes and record the group discussion.
Although this workshop was deployed in person, it could also be implemented virtually using the modified implementation strategy outlined below.
-
•
The facilitator and participants gather on Zoom, Webex, or other online meeting platform.
-
•
Participants are encouraged to take notes using their preferred method (e.g., electronically or paper/pen).
-
•
After the multimedia presentation, the facilitator adjusts the virtual meeting room settings so they can view all participants.
-
•
Participants should keep their video on, if possible.
-
•
For the discussion, breakout rooms are used for larger groups, aiming for about 10 participants per breakout group. A facilitator is required for each breakout room.
-
•
During the discussion, the facilitator or notetaker takes notes using a virtual whiteboard.
Results
A total of three groups of health professions educators enrolled in 2015–2016. Two groups of participants completed the series of three workshops during two sessions. One group completed each session on three separate occasions.
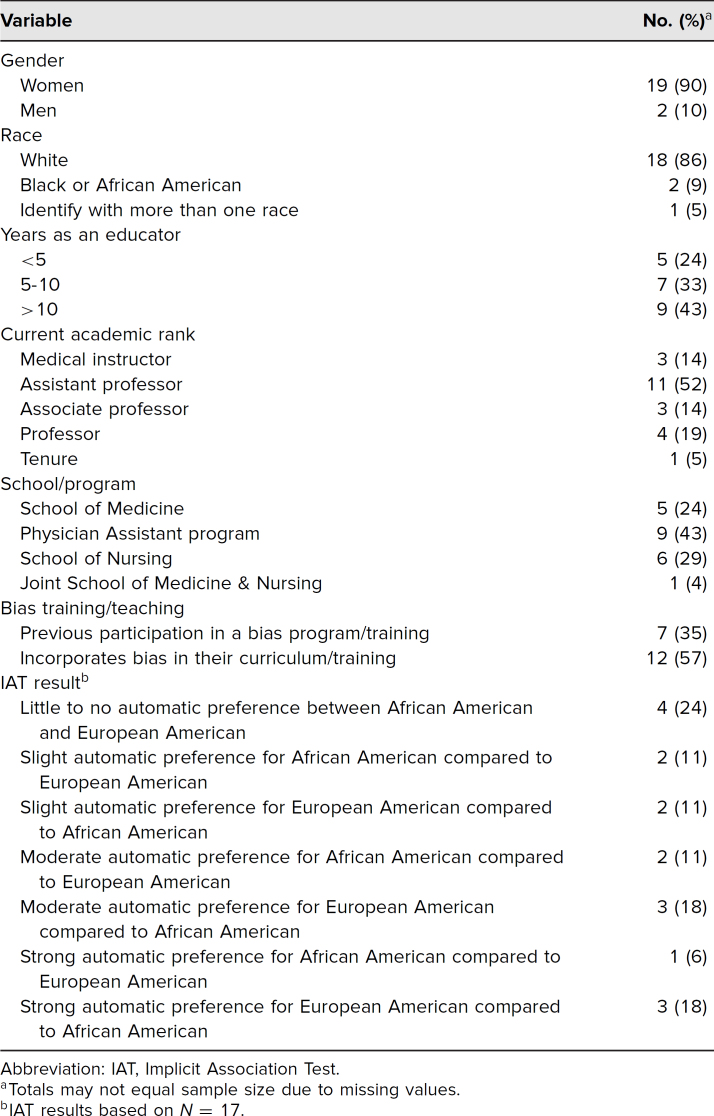
Twenty-four educators participated in the program (six physicians, eight nurse practitioners, and 10 physician assistants). Twenty-one (88%) completed the baseline questionnaire. Most participants (19, 90%) were women, 18 (86%) were White, nine (43%) were between the ages of 35 and 44, nine (43%) had more than 10 years of experience as educators, and 11 (52%) were assistant professors. Seven (35%) had previously participated in a racial bias program. Twelve (57%) reported incorporating racial bias into their curriculum or program. Seventeen participants (71%) completed the IAT (Table 1). Three participants (18%) did not answer the question regarding the IAT, one (6%) declined, and one (6%) answered “did not take the IAT.”
Table 1. Participants' Characteristics and IAT Results (N = 21).
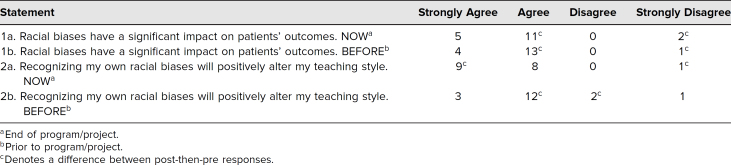
Eighteen participants (75%) completed the post-then-pre questionnaire. On the questionnaire, 16 participants (67%) agreed or strongly agreed that “racial biases have a significant impact on patients' outcomes” at the end of the program, compared with 17 (71%) who agreed or strongly agreed before the program. At the end of the program, 17 educators (71%) agreed or strongly agreed that recognizing their own bias would positively alter their teaching practice, compared with 15 (63%) before the program (Table 2).
Table 2. Post-Then-Pre Differences in Scores (N = 18).
Discussion
At the time these workshops were designed and implemented, very few curricula existed focusing on health professions educators. The goal of these workshops was to increase awareness of racial bias and its impact on patient care outcomes and to share strategies to mitigate the impact of racial bias in health professions education. While we cannot draw conclusions from the results, these workshops represent the first resource designed to recognize and address racial bias in health professions educators. The topics addressed in the workshops are more important than ever considering the recent events in our nation and the steps announced by many academic institutions regarding developing and implementing effective strategies focused on mitigating racism and the deployment of anti-racism training for all faculties.
Challenges and Lesson Learned
While this project yielded some success, we also had some challenges. The project had a small number of participants, and so, results cannot be generalizable. Additionally, the project was not sufficiently powered to determine a statistically significant change between participants' awareness before and after workshop attendance.
One of the lessons learned was the inability to measure and determine sustainable behavioral change, which would be useful as there is no current evidence, to date, that shows increasing awareness of racial bias leads to behavioral change. The presence of bias among health professions and its effects on patient care are of grave concern. Therefore, increasing awareness through successful workshops such as these is an essential first step in addressing and eliminating racial bias. Another lesson learned was that robust financial resources are necessary to allow for longitudinal follow-up and data acquisition from participants in order to assess change over time.
Recommendations
Our pilot workshops increased educators' awareness and furthered interest in pursuing opportunities to mitigate the impact of racial bias in health professional education and training. Therefore, we recommend that educators intentionally engage in opportunities to develop additional awareness and acquire the necessary skills and techniques to impact behaviors. This requires a long-term commitment from educators and conscious efforts to practice and implement strategies to mitigate the impact of their own biases in education and patient care. Others implementing these types of workshops should consider 6-, 12-, and 18-month postworkshop measures to determine the long-term impact of such workshops. Participants attending these workshops are likely to be faculty members who have an interest in exploring racial bias, who may have prior racial bias training, and who may already incorporate bias training into their teaching. Therefore, it is important to consider that the voluntary nature of the workshops can lead to participation bias that may underreport the impact the workshops might have on a group of less experienced participants. Flexibility in dates and times of sessions is important to consider when attempting to maximize participation as faculty from multiple health professions have competing demands, work schedules, and variable physical locations. Finally, facilitating these workshops takes a level of experience, and we highly recommend that those who facilitate these discussions be familiar with the topic and comfortable facilitating sensitive conversations about race, discrimination, and bias. Facilitators without prior experience can prepare by attending career development activities geared toward these topics. Subsequent workshops should focus on further increasing awareness, intentional behavior change, and implementation of newly acquired teaching strategies.
Appendices
- Participant Baseline Questionnaire.docx
- Facilitator Guide.docx
- Video Session 1.mp4
- Video Session 2.mp4
- Video Session 3.mp4
- Post-Then-Pre Questionnaire.docx
All appendices are peer reviewed as integral parts of the Original Publication.
Disclosures
None to report.
Funding/Support
Funded by a 2015 Duke University School of Medicine Academy for Health Professions Education and Academic Development (Duke AHEAD) grant.
Prior Presentations
Corsino L. The impact of racial bias in medical education: let's focus on the educator. Presented at: Duke AHEAD Education Day; September 13, 2016; Durham, NC.
Ethical Approval
The Duke University Institutional Review Board approved this project.
References
- 1.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Lewis D, Paulsen E, eds. Proceedings of the Diversity and Inclusion Innovation Forum: Unconscious Bias in Academic Medicine—How the Prejudices We Don't Know We Have Affect Medical Education, Medical Careers, and Patient Health. Association of American Medical Colleges, Kirwan Institute for the Study of Race and Ethnicity at The Ohio State University; 2017. Accessed July 27, 2020. https://store.aamc.org/downloadable/download/sample/sample_id/168/ [Google Scholar]
- 3.Williams DR, Wyatt R. Racial bias in health care and health: challenges and opportunities. JAMA. 2015;314(6):555–556. 10.1001/jama.2015.9260 [DOI] [PubMed] [Google Scholar]
- 4.Hall WJ, Chapman MV, Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105(12):e60–e76. 10.2105/AJPH.2015.302903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cooper LA, Beach MC, Johnson RL, Inui TS. Delving below the surface: understanding how race and ethnicity influence relationships in health care. J Gen Intern Med. 2006;21(suppl 1):S21–S27. 10.1111/j.1525-1497.2006.00305.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Green AR, Carney DR, Pallin DJ, et al. Implicit bias among physicians and its prediction of thrombolysis decisions for Black and White patients. J Gen Intern Med. 2007;22(9):1231–1238. 10.1007/s11606-007-0258-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gonzalez CM, Kim MY, Marantz PR. Implicit bias and its relation to health disparities: a teaching program and survey of medical students. Teach Learn Med. 2014;26(1):64–71. 10.1080/10401334.2013.857341 [DOI] [PubMed] [Google Scholar]
- 8.Schnierle J, Christian-Brathwaite N, Louisias M. Implicit bias: what every pediatrician should know about the effect of bias on health and future directions. Curr Probl Pediatr Adolesc Health Care. 2019;49(2):34–44. 10.1016/j.cppeds.2019.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Betancourt JR. Eliminating racial and ethnic disparities in health care: what is the role of academic medicine? Acad Med. 2006;81(9):788–792. 10.1097/00001888-200609000-00004 [DOI] [PubMed] [Google Scholar]
- 10.Willard G, Isaac KJ, Carney DR. Some evidence for the nonverbal contagion of racial bias. Organ Behav Hum Decis Process. 2015;128:96–107. 10.1016/j.obhdp.2015.04.002 [DOI] [Google Scholar]
- 11.van Ryn M, Hardeman R, Phelan SM, et al. Medical school experiences associated with change in implicit racial bias among 3547 students: a Medical Student CHANGES study report. J Gen Intern Med. 2015;30(12):1748–1756. 10.1007/s11606-015-3447-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teal CR, Gill AC, Green AR, Crandall S. Helping medical learners recognise and manage unconscious bias toward certain patient groups. Med Educ. 2012;46(1):80–88. 10.1111/j.1365-2923.2011.04101.x [DOI] [PubMed] [Google Scholar]
- 13.White AA III, Logghe HJ, Goodenough DA, et al. Self-awareness and cultural identity as an effort to reduce bias in medicine. J Racial Ethn Health Disparities. 2018;5(1):34–49. 10.1007/s40615-017-0340-6 [DOI] [PubMed] [Google Scholar]
- 14.DallaPiazza M, Padilla-Register M, Dwarakanath M, Obamedo E, Hill J, Soto-Greene ML. Exploring racism and health: an intensive interactive session for medical students. MedEdPORTAL. 2018;14:10783. 10.15766/mep_2374-8265.10783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brooks KC, Rougas S, George P. When race matters on the wards: talking about racial health disparities and racism in the clinical setting. MedEdPORTAL. 2016;12:10523. 10.15766/mep_2374-8265.10523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perdomo J, Tolliver D, Hsu H, et al. Health Equity Rounds: an interdisciplinary case conference to address implicit bias and structural racism for faculty and trainees. MedEdPORTAL. 2019;15:10858. 10.15766/mep_2374-8265.10858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–887. 10.1007/s11606-007-0160-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith WR, Betancourt JR, Wynia MK, et al. Recommendations for teaching about racial and ethnic disparities in health and health care. Ann Intern Med. 2007;147(9):654–665. 10.7326/0003-4819-147-9-200711060-00010 [DOI] [PubMed] [Google Scholar]
- 19.Byrne A, Tanesini A. Instilling new habits: addressing implicit bias in healthcare professionals. Adv Health Sci Educ Theory Pract. 2015;20(5):1255–1262. 10.1007/s10459-015-9600-6 [DOI] [PubMed] [Google Scholar]
- 20.Cahn PS. Recognizing and reckoning with unconscious bias: a workshop for health professions faculty search committees. MedEdPORTAL. 2017;13:10544. 10.15766/mep_2374-8265.10544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gill A, Thompson B, Teal C, et al. Best intentions: using the Implicit Associations Test to promote reflection about personal bias. MedEdPORTAL. 2010;6:7792. 10.15766/mep_2374-8265.7792 [DOI] [Google Scholar]
- 22.Thomas PA, Kern DE, Hughes MT, Chen BY, eds. Curriculum Development for Medical Education: A Six-Step Approach. 3rd ed.Johns Hopkins University Press; 2016. [Google Scholar]
- 23.Bennett M. Becoming interculturally competent. In: Wurzel JS, ed. Toward Multiculturalism: A Reader in Multicultural Education. 2nd ed. Intercultural Resource Corporation; 2004:62–77. [Google Scholar]
- 24.Bennett MJ. Towards ethnorelativism: a developmental model of intercultural sensitivity. In: Paige RM, ed. Education for the Intercultural Experience. Intercultural Press; 1993:21–71. [Google Scholar]
- 25.Bennett MJ. A developmental approach to training for intercultural sensitivity. Int J Intercult Relat. 1986;10(2):179–196. 10.1016/0147-1767(86)90005-2 [DOI] [Google Scholar]
- 26.Preliminary information. Project Implicit. Accessed July 8, 2021. https://implicit.harvard.edu/implicit/takeatest.html [Google Scholar]
- 27.Program Development and Evaluation. Using the Retrospective Post-Then-Pre Design. University of Wisconsin-Extension; 2005. Quick Tips no. 27. Accessed July 27, 2020. https://fyi.extension.wisc.edu/programdevelopment/files/2016/04/Tipsheet27.pdf [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- Participant Baseline Questionnaire.docx
- Facilitator Guide.docx
- Video Session 1.mp4
- Video Session 2.mp4
- Video Session 3.mp4
- Post-Then-Pre Questionnaire.docx
All appendices are peer reviewed as integral parts of the Original Publication.