Abstract
Esophagogastric junction (EGJ) barrier function is of fundamental importance in the pathophysiology of gastroesophageal reflux disease. Impaired EGJ barrier function leads to excessive distal esophageal acid exposure or, in severe cases, esophagitis. Hence, proposed high-resolution manometry (HRM) metrics assessing EGJ integrity are clinically important and were a focus of the Chicago Classification (CC) working group for inclusion in CC v4.0. However, the EGJ is a complex sphincter comprised of both a crural diaphragm (CD) and lower esophageal sphincter (LES) component, each of which is subject to independent physiological control mechanisms and pathophysiology. No single metric can capture all attributes of EGJ barrier function. The working group considered several potential metrics of EGJ integrity including LES-CD separation, the EGJ contractile integral (EGJ-CI), the respiratory inversion point (RIP) and intragastric pressure. Strong recommendations were made regarding LES-CD separation as indicative of hiatus hernia, although the numerical threshold for defining hiatal hernia was not agreed upon. There was no agreement on the significance of the RIP, only that it could localize either above the LES or between the LES and CD in cases of hiatus hernia. There was agreement on how to measure the EGJ-CI and that it should be referenced to gastric pressure in units of mmHg•cm, but the numerical threshold indicative of a hypotensive EGJ varied widely among reports and was not agreed upon. Intragastric pressure was endorsed as an important metric worthy of further study but there was no agreement on a numerical threshold indicative of abdominal obesity.
Introduction
The Chicago Classification (CC) v4.0 Working Group included 52 experts from 20 countries, representing six Neurogastroenterology and Motility societies from around the world. The Working Group was divided into seven subgroups, each tasked with developing statements specific to topics targeted for improvement or refinement based on the collective group experience with CCv3.0. This technical review summarizes the work of one of those seven subgroups tasked with developing statements regarding high-resolution manometry (HRM) metrics pertinent to EGJ barrier function (not formally addressed in CC v3.0). The formally validated RAND Appropriateness Method (RAM) was used through several on-line independent surveys to facilitate equal contribution among group members. Evidence supporting the statements was assessed according to GRADE by two CC Working Group members external to the EGJ subgroup when statement structure permitted. Although it was anticipated that the majority of the literature would be assessed as low or very low-level evidence by the GRADE construct (heavily weighted by randomized controlled trials and meta-analyses which are quite scarce in the field of HRM), the external expert review provided an additional unbiased evaluation.
EGJ Barrier Function
A fundamental abnormality in gastroesophageal reflux disease (GERD) is impairment of the esophagogastric junction (EGJ) as an antireflux barrier. The clinical consequence of this is excessive distal esophageal acid exposure as determined by ambulatory pH-metry or, in severe cases, unequivocal endoscopic esophagitis. Hence, proposed HRM metrics assessing EGJ integrity are appropriately tested by how predictive they are of abnormal pH-metry. However, the EGJ is a complex sphincter presenting unique challenges to that assessment. Among those challenges are: 1) EGJ pressure is comprised of both a crural diaphragm (CD) and lower esophageal sphincter (LES) component, each of which is subject to independent physiological control mechanisms and pathophysiology; 2) EGJ pressure morphology is heavily influenced by the anatomical integrity of the EGJ ranging from normal wherein the CD is completely superimposed on the LES to overt hiatus hernia wherein the two are spatially separated [1]; 3) EGJ pressure morphology can vary over time, even within a single patient study, transitioning between superimposed and separated CD and LES components [2]; 4) when the LES and CD are physiologically separated, the respiratory inversion point (RIP) where inspiratory pressure transitions from an augmentation to a reduction of intraluminal pressure can localize above the LES or between the CD and LES; and 5) there is extreme axial and radial asymmetry of EGJ pressure morphology attributable to both the “pinchcock” effect of CD contraction and the acute angle between the axis of the CD and that of the esophagus [3–5]. Clearly, no single HRM metric can capture all attributes of EGJ barrier function.
The recently published Lyon consensus grappled with the above as they sought to define manometric criteria for a diagnosis of GERD [6]. They proposed adopting two HRM metrics for quantifying EGJ functional integrity, one expressing the anatomical morphology of the EGJ and the other summarizing its contractile vigor. EGJ morphology, defined by the relationship between the LES and CD, is characterized as type I, II, or III as discussed in the Chicago Classification (CC) v3.0 [1, 7]; type 1 with superimposed LES and CD, type 2 with axially separated LES and CD pressure signals separated by less than 2 cm, and type 3 with a ≥2 cm separation between the LES and CD pressure signatures. The second HRM metric proposed by the Lyon consensus to quantify EGJ contractile vigor is the EGJ contractile integral (EGJ-CI) (Figure 1), calculated in a similar fashion to the distal contractile integral (DCI). With the DCI box set to encompass the LES and CD over exactly three respiratory cycles, the calculated “DCI” is then divided by the duration of the three respiratory cycles to make it independent of time and expressed in units of mmHg●cm, referenced to gastric pressure [8].
Figure 1.
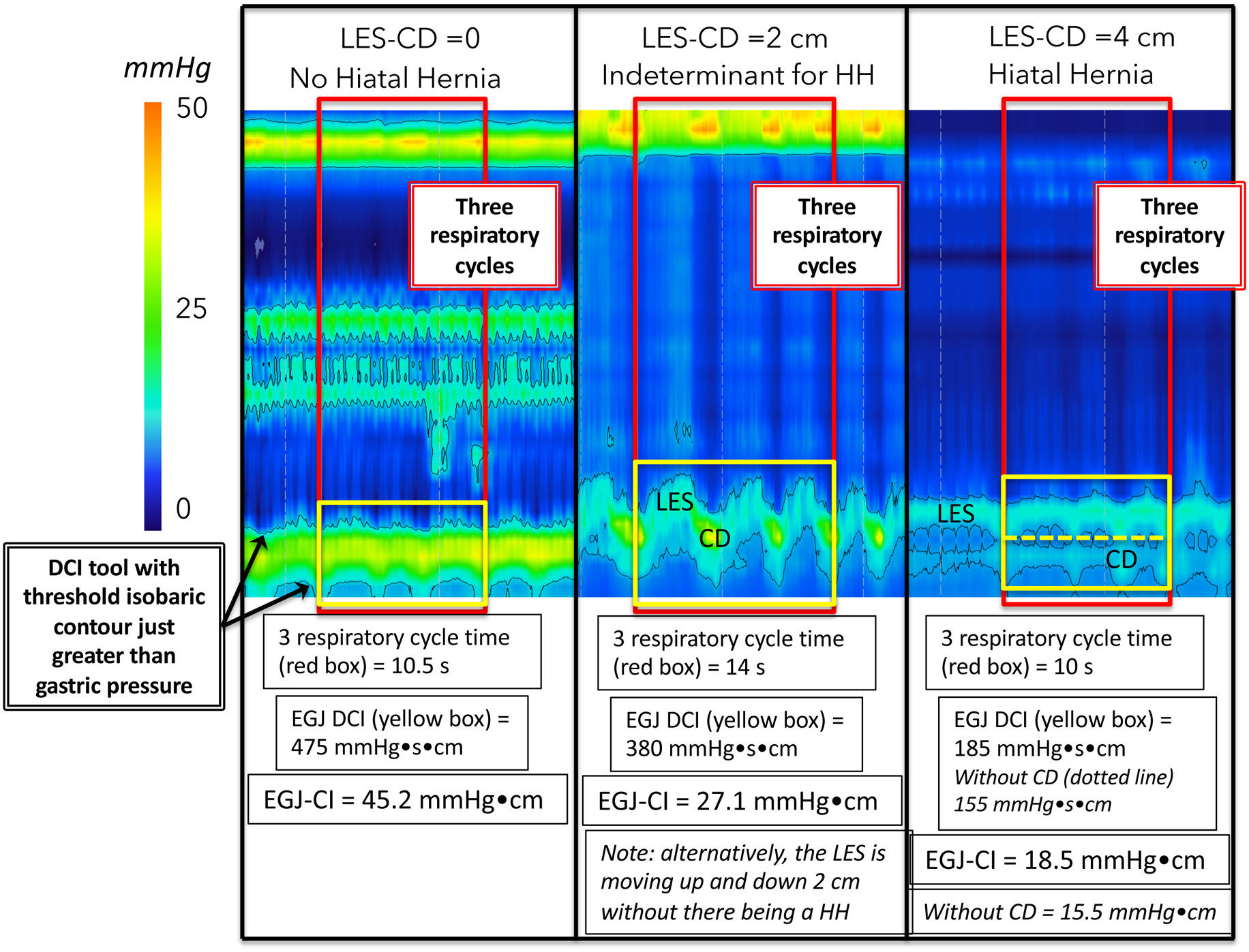
The esophagogastric junction contractile integral (EGJ-CI) measures vigor of the EGJ barrier using a software tool that encompasses length and vigor of the EGJ above the gastric baseline. The measurement is made over three respiratory cycles during rest and corrected for duration of respiration. Three examples are shown with progressive LES-CD separation and diminishing EGJ-CI values. Note that the middle panel is indeterminant for hiatal hernia because the sphincter complex may, alternatively, be moving up and down 2 cm with respiration with no axial LES-CD separation. Note also that some investigators restrict the EGJ-CI box to the LES component when LES-CD separation is complete; the effect of that is illustrated in the 4 cm LES-CD separation on the right. Figure used with permission from the Esophageal Center at Northwestern.
With these emerging concepts, EGJ barrier function was voted a priority area for modification in CC v4.0, especially since CC v3.0 did not provide specific guidance. Hence, in the CC v4.0 process, a subgroup was dedicated to developing statements regarding the assessment of EGJ barrier function in HRM. This working group, led by two co-chairs (PJK & RKM), was tasked with evaluating proposed HRM metrics related to EGJ barrier function based on literature review and expert consensus. As detailed in the main CCv4.0 document, each proposed statement underwent two rounds of independent ranking according to RAND UCLA Appropriateness Methodology. Statements achieving ≥85% agreement by the entire CC Working Group as being appropriate were considered strong recommendations, while those with 80–85% agreement were considered conditional recommendations. Statements not meeting these thresholds were discussed at working group meetings and in the text of this manuscript. Additionally, strong and conditional recommendations underwent further independent evaluation to assess the level of supportive evidence, using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) process, when possible [9]. Two experts external to the working subgroup independently evaluated the supportive literature provided by the subgroup. Some statements were not amenable to the GRADE process, either because of the structure of the statement or lack of published evidence.
LES-CD separation
Type I (sliding) hiatus hernia is of cardinal importance in the pathophysiology of reflux disease even though the precise criteria for differentiating a small hiatus hernia from normal are vague on account of the physiological mobility of the LES and definitional inconsistencies. HRM-defined LES-CD separation has been shown to correlate closely with the presence or absence and size of hiatus hernia as determined by endoscopy or barium x-ray with sensitivity and specificity of 88% and 95% respectively [10], although that analysis begs the question of which test is the appropriate reference standard. The unequivocal diagnosis of hiatus hernia is ultimately made intraoperatively wherein the spatial relationship between the EGJ and CD and presence or absence of a hernia sac are visually evident. A recent analysis compared the accuracy of HRM, endoscopy, and barium radiography to surgery in detecting and sizing hiatus hernia [11]. That analysis concluded that HRM, using the LES-CD metric, outperformed the other modalities with a sensitivity of 94%, specificity of 92% and kappa value of 0.85. In that analysis, HRM reached both optimal sensitivity and specificity for detecting hiatus hernia with a threshold LES–CD separation of 1.2 cm.
Apart from being indicative of hiatus hernia, LES-CD separation also correlates with reflux severity as determined by pH-metry [1, 12, 13]. Furthermore, as the LES and CD become spatially separate there is the added issue of whether the RIP, the locus at which the inspiratory effect on intraluminal pressure transitions from augmentation (characteristic of the abdomen) to a reduction (characteristic of the chest) remains in its native position above the CD or not. Although the precise physiological meaning of the RIP is uncertain and its localization sometimes challenging, there can be general agreement regarding the observations that: 1) the RIP can never be below the diaphragm; 2) when the CD is superimposed on the LES (i.e LES-CD separation <1cm), the RIP localizes above the EGJ pressure complex placing the LES physiologically within and beneath the diaphragmatic hiatus; and 3) with spatial separation of the CD and LES, the RIP can localize either at or above the CD component (placing it within the hernia) or above the LES. Supporting the relevance of this distinction, a recent classification scheme subtyped individuals with LES-CD separation as ‘B’ or ‘C’ depending on whether the RIP localized above or below the LES respectively [14]. In that analysis, subtype B was less likely to exhibit pathological reflux on pH-metry than subtype C. The authors interpreted this to support the contention that subtype B was indicative of the LES remaining within the abdominal compartment and being advantageous. Viewed somewhat differently, with greater degrees of LES-CD separation, there is the additional factor of whether or not the CD is competent, in other words, does it effectively compartmentalize the stomach from the herniated stomach during inspiration? When it does, it is exhibiting greater sphincteric function than when it doesn’t, presumably because the hiatus is less dilated [15]. Although not precisely addressing this distinction, evidence supporting the relevance of CD competence comes from a logistic regression model of barrier function that simultaneously examined expiratory LES pressure, LES-CD separation, and inspiratory EGJ augmentation while controlling for age and body mass index (BMI). In that analysis, only inspiratory augmentation had a significant independent association with GERD as defined by pH-metry [1]. However, subsequent data from 3D-HRM studies clearly demonstrate that the inspiratory augmentation of EGJ pressure attributable to the CD is strongly correlated with the EGJ-CI (R=.84) [8] suggesting that this feature of EGJ barrier function is likely captured by the EGJ-CI.
Moving forward, accepting that the presence and size of hiatus hernia is a clinically relevant measurement, the working group concluded that there is compelling evidence in support of adopting LES-CD separation as an HRM metric for EGJ morphology. However, there was no agreement on the precise threshold value of LES-CD separation for defining a hiatal hernia or on what to do when variable degrees of LES-CD separation occurred within a study. The working group did not see reason to differentiate between type II and type III morphology as proposed by the Lyon consensus reasoning that there was insufficient evidence supporting the significance of that distinction. With respect to the localization of the RIP, there was less agreement on its clinical significance, but it was concluded that in instances of the LES-CD separation it should be specified as to whether the RIP localized above or below the LES component. It was also highlighted that the PIP tool used to localize the RIP in Figures 2–4 is technically flawed in that with larger hernia, all of the relevant sensors are above the diaphragm and none is reflective of intra-abdominal pressure variations. In that circumstance the RIP localization becomes unreliable. Hence the three proposed morphologies are: 1) no hiatus hernia (LES-CD separation <1cm) with the RIP above the EGJ complex (Figure 2); 2) LES-CD separation >1 cm (indeterminant for hiatal hernia) with the RIP at the CD level (Figure 3); and 3) hiatus hernia with the RIP above the LES (Figure 4). However, apart from specifying the LES-CD separation and where the RIP localized, there was no consensus on a specific classification scheme.
Figure 2.
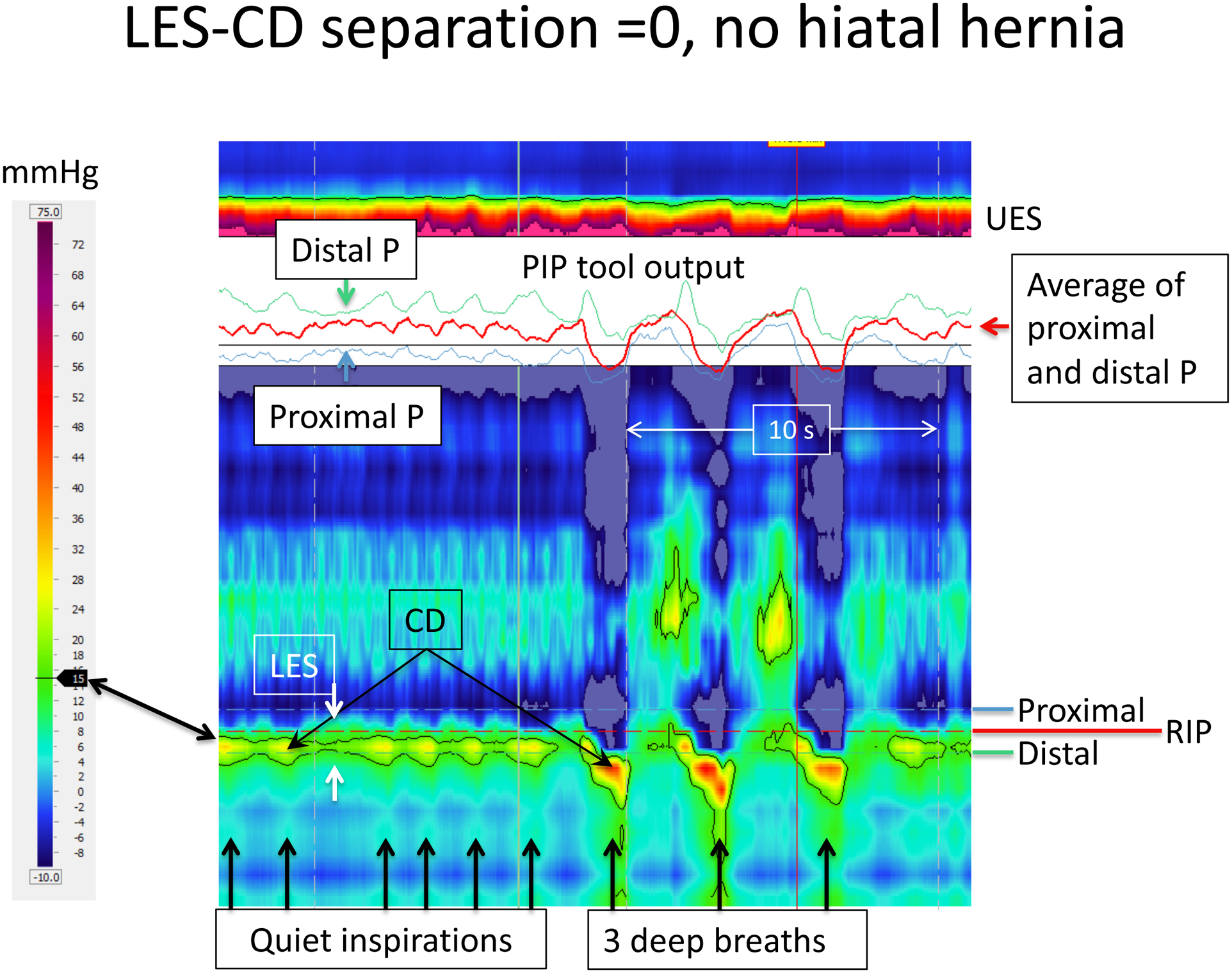
HRM recording of EGJ pressure in an individual without a hiatal hernia as evident by the CD-apex being completely superimposed on the LES pressure signature, i.e. the LES-CD separation is 0. Both during quiet respiration and deep breaths, the LES is only evident between inspirations when the CD signal is minimal. In this example, the PIP tool has been positioned to optimally isolate the RIP as evident by the PIP tool output shown as an insert. Barely visible on the pressure topography are a horizontal blue and green dashed lines indicating the locations of the proximal and distal pressure (P) recordings shown in the PIP tool output. The red line in the PIP tool output box is the computed average of those signals. In using the tool, the area of interrogation is scrolled up and down to find the location at which the red line in the output box is most nearly flat, indicative of the site at which the respiratory increases in pressure (green line) are offset by the respiratory decreases in pressure (blue line). The area of interest is during quiet respiration and the RIP is seen to localize toward the upper margin of the CD. This positions the majority of the LES signal within the hiatus, being pulled downward during the three deep breaths. Figure used with permission from the Esophageal Center at Northwestern.
Figure 4.
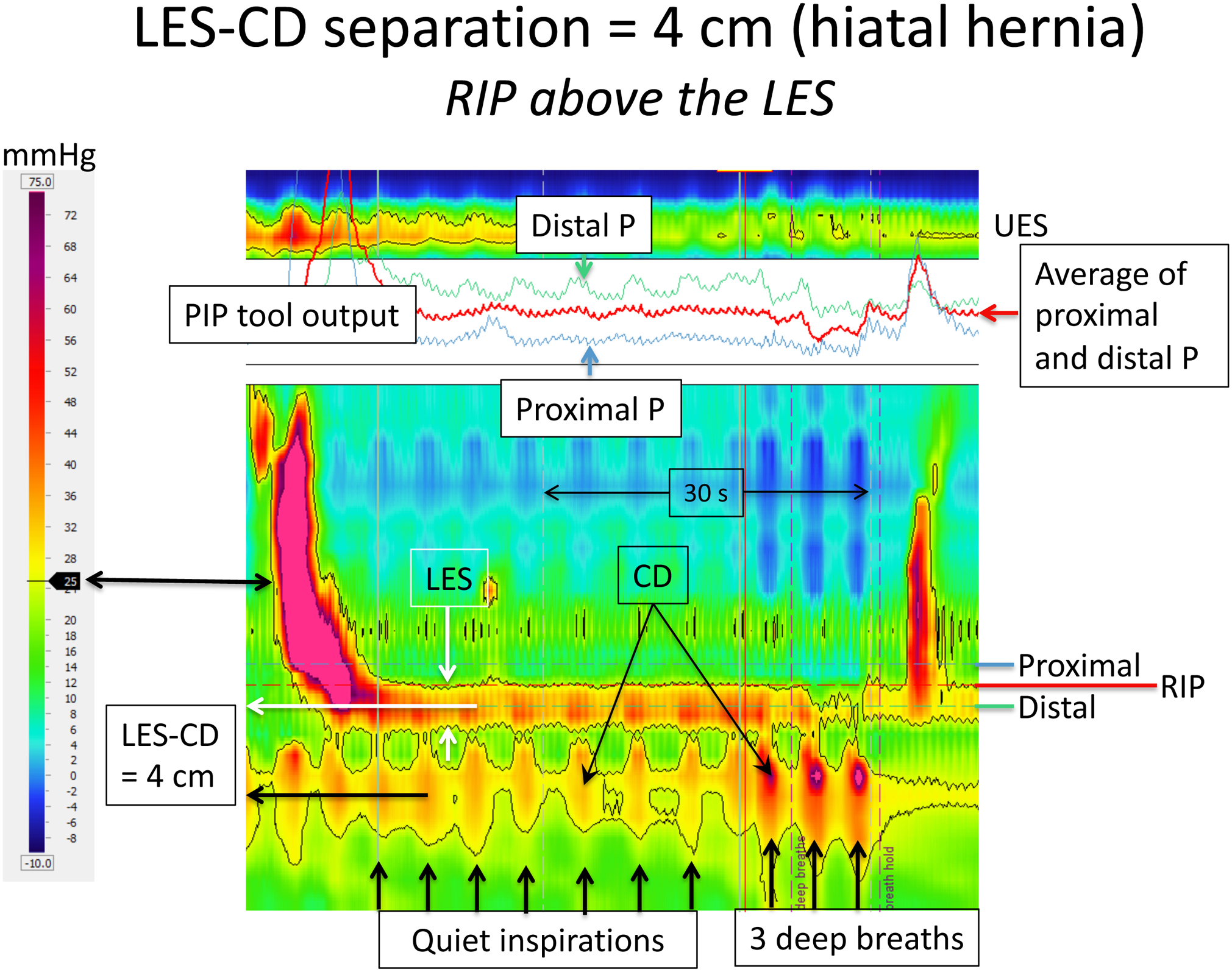
HRM recording of EGJ pressure in an individual with a moderate sized hiatal hernia as evident by the CD being isolated from the LES pressure signature; the LES-CD separation is 4 cm. Formatting of the figure is identical to that of Figures 2 and 3 with the dominant EGJ pressure profile highlighted by the black 25 mmHg isobaric contour and the PIP tool optimally positioned to isolate the RIP. However, in this example, the RIP no longer localizes the CD signal, instead localizing at the proximal margin of the LES. Even without the aid of the PIP tool, that is evident by the inspiratory bursts of red on the LES recording. In fact, the respiratory increases in pressure appear to extend into the distal esophagus in this example (evident by the three deep breaths) emphasizing how the RIP can be unreliable with greater degrees of LES-CD separation. Figure used with permission from the Esophageal Center at Northwestern.
Figure 3.
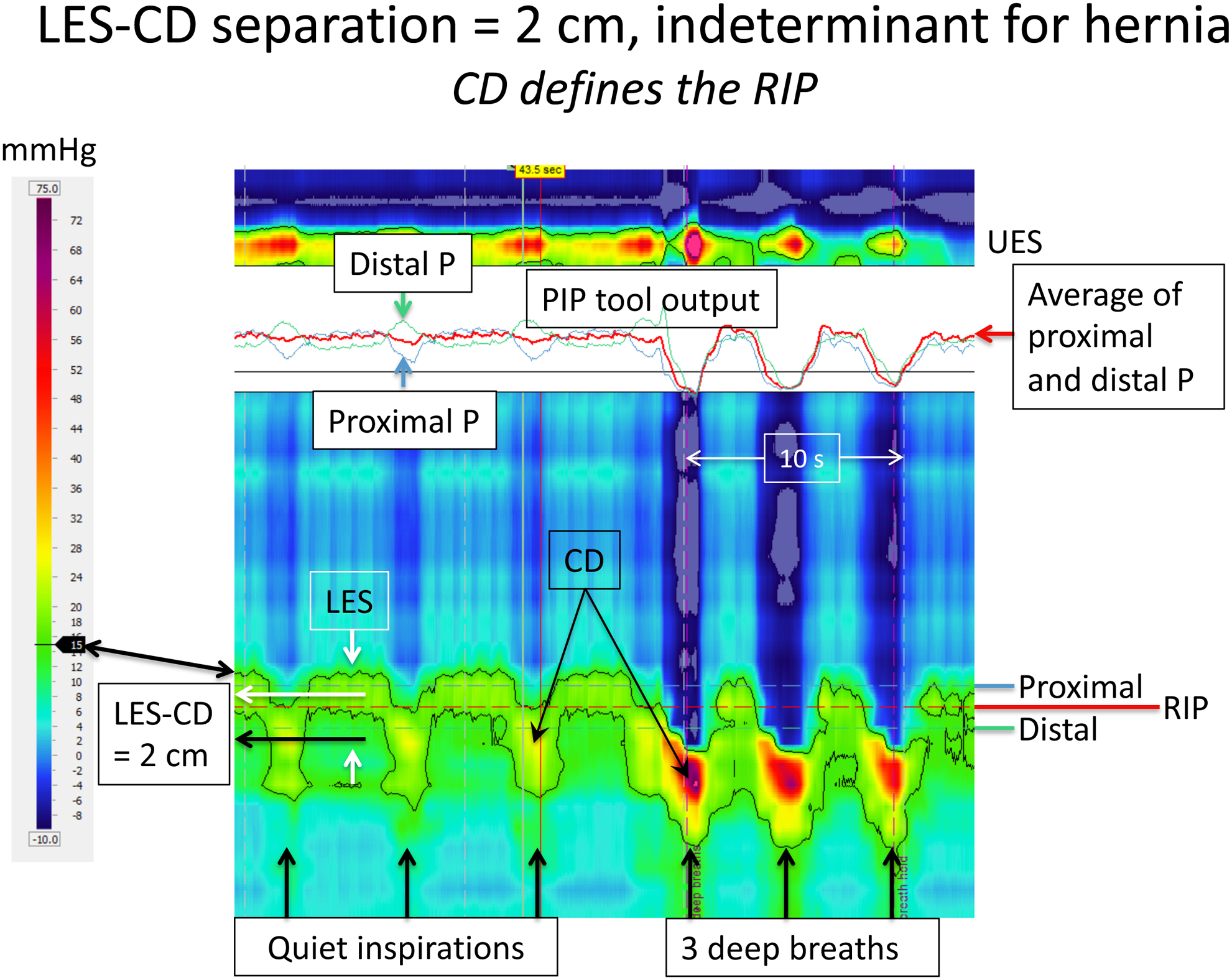
HRM recording of EGJ pressure in an individual with the CD being only partially superimposed on the LES pressure signature; the LES-CD separation is 2 cm. This is indeterminant for hiatus hernia as one cannot confidently localize the LES during inspiration necessitating that is position be defined during expiration. Formatting of the figure is identical to that of Figure 2 with the dominant EGJ pressure profile highlighted by the black line (the 15 mmHg isobaric contour) and the PIP tool optimally positioned to isolate the RIP. The center of the LES and CD high pressure zones (white and black horizontal arrows, respectively) are isolated with the help of the isobaric contour tool and the separation between the two rounded off to the nearest cm. In this example, the RIP continues to localize toward the upper margin of the CD signal. This is particularly evident during the three deep breaths where the strongly negative intrathoracic pressure (deep blue) is seen to abut directly on the CD signal negating whatever LES pressure signal may have been above it. Figure used with permission from the Esophageal Center at Northwestern.
Accepted Statements:
The EGJ complex should be measured during quiet respiration in the baseline recording in a segment relatively devoid of swallowing and/or recording artifacts. This also refers to measurement of intragastric pressure, which should be measured below the CD over three complete respiratory cycles, preferably the same segment as used to measure the EGJ-CI. (Strong Recommendation)
LES-CD separation should be scored as the distance between the center of the CD and LES signal during inspiration, unless obscured in which case the LES position should be scored at expiration. (Strong Recommendation)
The RIP is the axial location at which the inspiratory change in pressure transitions from an inspiratory increase, characteristic of intra-abdominal recordings, to an inspiratory decrease, characteristic of intrathoracic recordings. (Strong Recommendation)
There can be 3 subtypes of EGJ pressure topography: (1) No hiatal hernia: LES -CD separation < 1cm; (2) Hiatal hernia indeterminant, distal RIP: LES -CD separation >1 cm and RIP between the LES and CD; (3) Hiatal hernia, proximal RIP: complete LES -CD separation and RIP proximal to the LES. (Conditional Recommendation)
In the normal state (EGJ subtype 1) the RIP localizes at the proximal margin of the LES-CD (EGJ) complex. (Strong Recommendation)
With hiatus hernia the RIP can localize either between the LES and CD or proximal to the LES (Conditional Recommendation)
With an LES-CD >3 cm, the RIP location and relation to LES can be unreliable. However, these patients usually have an incompetent EGJ. (Conditional Recommendation)
EGJ-CI
Hoshino et al first proposed the concept of measuring a pressure integral of LES-CD complex using the DCI analysis tool. They measured over a 10 second recording, referenced the metric to 20 mmHg, called it the LES pressure integral, and reported increased distal esophageal acid exposure when this measured <400 mmHg•cm•s [16]. This concept was subsequently refined and standardized as the EGJ-CI, the HRM metric proposed by the Lyon consensus to quantify EGJ contractile vigor (Figure 1). Insight into the genesis of the EGJ-CI has been gleaned through studies using 3D-HRM [3] which, unlike “conventional” HRM which averages radial pressure at each axial locus, allows for both axial and radial pressure resolution. Radial resolution allows for isolation of the LES and CD pressure components within the EGJ complex because of the extreme asymmetry of the CD component. Studies quantifying the CD component within the composite EGJ signal on 3D-HRM concluded that across the entire respiratory cycle, approximately 85% of overall EGJ contractility was attributable to the CD [8, 17]. Furthermore, the CD signal in the 3D-HRM studies strongly correlated with acid exposure time on pH-metry (r =−0.42, p<0.01) suggesting the CD to be the dominant contractile component of the EGJ barrier [18]. Together, these studies provide physiological support for adopting the EGJ-CI as a metric of EGJ contractile vigor with the caveat that it is largely driven by the CD component.
Several groups of investigators have tested the performance of the EGJ-CI in segregating GERD populations (Table 1) [8, 12, 19–22] with general agreement that this metric differentiates GERD populations from control subjects. Studies that stratified GERD severity also generally suggest that a subset of patients with very low values of EGJ-CI are prone to either endoscopic esophagitis or unequivocally abnormal reflux testing. However, it is also evident from the spread of values reported among these studies that it is not possible to establish a firm threshold for abnormality. This is partly attributable to methodological differences among studies such as referencing the EGJ-CI to intragastric pressure versus a value slightly above intragastric pressure or including versus excluding the CD component in instances of complete LES-CD separation, but these differences are unlikely to explain the magnitude of differences reported among centers. Hence, the best one can do is to say that within laboratories lower EGJ-CI values correlated with increased severity of reflux and that the lower the EGJ-CI value, the more severe the EGJ dysfunction.
Table 1.
Studies that have compared the EGJ-CI among patient and control populations. Methods of EGJ-CI computation in instances of LES-CD separation were not uniform among these studies, with some including and some excluding the CD component. Functional patients were defied as having reflux symptoms, but normal physiological studies.
| Median [IQR] EGJ-CI in mmHg•cm | |||
|---|---|---|---|
| Study | Control Subjects | GERD | Functional |
| Nicodème 2014 | 39 [25–55] n=75 | 18* [8–30] n=7 | 45 [23–67] n=45 |
| Tolone 2015 | ----- | 11* [3–21] n=91 | 22 [10–41] n=39 |
| Jasper 2016 | 63 [50–90] n=63 | 50* [28–70] n=116 | ----- |
| Wang 2016 | 35 [26–58] n=21 | 30* [15–53] n=68 | ----- |
| Xie 2017 | 63 [38–83] n=21 | 22* [20–31] n=39† 26* [15–38] n=38§ |
30* [19–44] |
| Ham 2017 | 67 [27–79] n=23 | 28* [4–63] n=25† 26* [15–32] n=16§ |
51 [3–153] ¶ |
p<0.05 vs controls or comparator;
esophagitis patients;
Non-erosive reflux disease;
non-GERD
Moving forward, the working group concluded that, although imperfect, the EGJ-CI is currently the best validated metric of EGJ contractile vigor and should be adopted. To standardize the methodology for its computation, they recommend referencing the EGJ-CI measurement to gastric baseline pressure. However, there being poor agreement among laboratories, no threshold value of the EGJ-CI could be established to be conclusive evidence of EGJ dysfunction. There was also no consensus on whether or not to exclude the CD component from the computation in instances of LES-CD separation >2 cm when it is possible to exclusively isolate the LES.
Accepted Statement:
The EGJ-CI should be referenced to intragastric pressure and expressed in units of mmHg•cm. (Strong Recommendation)
Intra-abdominal Pressure
Irrespective of EGJ barrier function, gastroesophageal reflux is ultimately driven by the pressure within the abdomen. The more extreme the intra-abdominal pressure, the greater the demand on the EGJ to oppose it. Hence, going beyond the Lyon Consensus, the working group viewed it as important to consider intra-abdominal pressure as another clinically relevant aspect of EGJ barrier function. Increased BMI and abdominal girth are known to result in greater intragastric pressure [23, 24] and individuals with above-average BMIs are more likely to experience GERD [24, 25]. Similarly, in the special population of patients with end-stage lung disease, an increased abdominal to thoracic pressure gradient at inspiration was associated with worsening distal esophageal acid exposure on pH-metry [26]. Although there are clearly additional metabolic and mechanical variables affecting the relationship between obesity and GERD, intragastric pressure is an attractive HRM metric to adopt because of its simplicity and obvious relevance. Furthermore, it facilitates relating EGJ metrics that are referenced to intragastric pressure to atmospheric pressure as well. In HRM studies, the working group proposed that intragastric pressure be measured at expiration from an intragastric sensor relative free of artifact. As for defining what constitutes an elevated intragastric pressure, data relating intragastric pressure to obesity found that, on average, 8 mmHg correlates with a waist circumference of 36 inches or BMI of about 30 kg/m2 [23] suggesting that to be a reasonable indicator of abdominal obesity. However, the working group could not achieve consensus on what value of intragastric pressure was conclusive evidence of abnormality.
Accepted Statement:
-
Intragastric pressure should be measured during quiet respiration in the baseline recording in a segment relatively devoid of swallowing and/or recording artifacts, preferably the same segment as used to measure the EGJ-CI.
Strength of recommendation: Strong (95%)
GRADE: Not applicable
Summary
The working group proposed metrics for EGJ barrier function in CC v4.0 characterizing its anatomical integrity and contractile vigor as well as for intra-abdominal pressure, the driving force behind reflux events. These are all new in CCv4.0. The fundamental metric defining EGJ anatomical integrity is LES-CD separation expressed in cm with a value >1 cm suggestive (but still inconclusive) of hiatus hernia. Hiatus hernia is further characterized as to whether or not the RIP localizes above or below the LES component although there was no consensus on which location was indicative of greater dysfunction and no consensus on a classification scheme for EGJ morphology. The EGJ-CI expressed in mmHg•cm is the metric proposed to assess the vigor of EGJ contractility at rest with lower values constituting a hypotensive EGJ. However, currently each laboratory needs to establish their own range of normal as there has been poor agreement among reports as to what threshold value constitutes conclusive evidence of a hypotensive EGJ. In fact, with the EGJ-CI being 85% driven by the magnitude of the inspiratory CD contraction, it is poorly reflective of LES contractility, the historical focus of EGJ barrier function analysis. This leaves open the possibility of developing a novel HRM metric in the future that best summarizes expiratory LES contractility, likely to be especially relevant with hiatus hernia. Finally, elevated intra-abdominal pressure referenced to atmospheric pressure is an indicator of abdominal obesity and should also be measured, but currently there is no consensus on the threshold value indicating conclusive evidence of an elevated intra-abdominal pressure. Accepted statements relative to EGJ barrier function are shown in Table 2.
Table 2.
EGJ Metrics of Barrier Integrity: Accepted Statements
| HRM Metrics for EGJ Barrier Integrity | |||
|---|---|---|---|
| Recommended Statement | Percent Agreement | Strength of Recommendation | Level of Evidence* |
| The EGJ complex should be measured during quiet respiration in the baseline recording in a segment relatively devoid of swallowing and/or recording artifacts. This also refers to measurement of intragastric pressure, which should be measured below the CD over three complete respiratory cycles, preferably in the same segment as used to measure the EGJ-CI | 95% | Strong | |
| LES-CD separation should be scored as the distance between the center of the CD and LES signal during inspiration, unless obscured in which case the LES position should be scored at expiration | 91% | Strong | |
| The RIP is the axial location at which the inspiratory change in pressure transitions from an inspiratory increase, characteristic of intra-abdominal recordings, to an inspiratory decrease, characteristic of intrathoracic recordings | 95% | Strong | Very Low |
There can be 3 subtypes of EGJ pressure topography
|
80% | Conditional | Low |
| In the normal state (EGJ subtype 1) the RIP localizes at the proximal margin of the LES-CD (EGJ) complex. | 88% | Strong | Low |
| With hiatus hernia the RIP can localize either between the LES and CD or proximal to the LES | 81% | Conditional | Low |
| With an LES-CD >3 cm, the RIP location and relation to LES can be unreliable. However, these patients usually have an incompetent EGJ. | 81% | Conditional | Low |
| The EGJ-CI should be referenced to intragastric pressure and expressed in units of mmHg•cm | 86% | Strong | |
| Intragastric pressure should be measured during quiet respiration in the baseline recording in a segment relatively devoid of swallowing and/or recording artifacts, preferably the same segment as used to measure the EGJ-CI. | 95% | Strong | |
GRADE process performed when applicable
In conclusion, while including EGJ barrier function metrics in CCv4.0 is clearly a step forward, it also highlighted the complexity of that task as there was remarkably little agreement among working group members on some rather fundamental issues. Nonetheless, sufficient consensus was achieved to develop uniform definitions of key metrics along with methodology for reporting them. This was an essential development that will foster future collaborative work among laboratories and hopefully iron out differences in the clinical measurement and characterization of EGJ barrier function.
Acknowledgements
Research Funding Support:
John E. Pandolfino and Peter J. Kahrilas are supported by P01 DK092217 (John E. Pandolfino) from the US Public Health Service. Ravinder K. Mittal is supported by NIH Grant R01 DK109376.
Abbreviations:
- BMI
body mass index
- CC
Chicago Classification
- CD
crural diaphragm
- DCI
distal contractile integral
- EGJ
esophagogastric junction
- EGJ-CI
esophagogastric junction contractile integral
- GERD
gastroesophageal reflux disease
- HRM
high-resolution manometry
- LES
lower esophageal sphincter
- RIP
respiratory inversion point
Footnotes
DISCLOSURES
Peter Kahrilas: Consulting: Ironwood, Bayer, Reckitt Benckiser
Ravinder K. Mittal: Nothing to disclose
Serhat Bor: Nothing to disclose
Geoffrey Kohn: Nothing to disclose
Johannes Lenglinger: Nothing to disclose
Sumeet K. Mittal: Nothing to disclose
John E. Pandolfino: Consultant: Medtronic, Ironwood Pharmaceuticals, DiversatekResearch support: Ironwood Pharmaceuticals, Takeda; Advisory Board: Medtronic, Diversatek; Stock Options: Crospon Inc
Jordi Serra: Consulting/speaker: AB-biotics, Allergan, Bayer, Norgine, Cassen-Recordati, Zespri and Reckitt Benckiser.
Roger Tatum: Nothing to disclose
Rena Yadlapati: Institutional Consulting Agreement: Medtronic, Ironwood Pharmaceuticals, Diversatek; Research support: Ironwood Pharmaceuticals; Advisory Board: Phatom Pharmaceuticals
Writing Assistance: None
REFERENCES
- 1.Pandolfino JE, Kim H, Ghosh SK, et al. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 2007;102:1056–63. [DOI] [PubMed] [Google Scholar]
- 2.Bredenoord AJ, Weusten BL, Timmer R, et al. Intermittent spatial separation of diaphragm and lower esophageal sphincter favors acidic and weakly acidic reflux. Gastroenterology 2006;130:334–40. [DOI] [PubMed] [Google Scholar]
- 3.Kwiatek MA, Pandolfino JE, Kahrilas PJ. 3D-high resolution manometry of the esophagogastric junction. Neurogastroenterol Motil 2011;23:e461–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicodème F, Lin Z, Pandolfino JE, Kahrilas PJ. Esophagogastric junction pressure morphology: comparison between a station pull-through and real-time 3D-HRM representation. Neurogastroenterol Motil 2013;25:e591–e598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mittal RK, Zifan A, Kumar D, et al. Functional morphology of the lower esophageal sphincter and crural diaphragm determined by three-dimensional high-resolution esophago-gastric junction pressure profile and CT imaging. Am J Physiol 2017;313:G212–G219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gyawali CP, Kahrilas PJ, Savarino E, et al. Modern diagnosis of GERD: the Lyon Consensus. Gut 2018. July;67(7):1351–1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nicodème F, Pipa-Muniz M, Khanna K, et al. Quantifying esophagogastric junction contractility with a novel HRM topographic metric, the EGJ-Contractile Integral: normative values and preliminary evaluation in PPI non-responders. Neurogastroenterol Motil 2014;26:353–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 2011;64:401–6. [DOI] [PubMed] [Google Scholar]
- 10.Weijenborg PW, Van Hoeij FB, Smout AJPM, AJ Bredenoord. Accuracy of hiatal hernia detection with esophageal high-resolution manometry. Neurogastroenterol Motil 2015;27(2):293–299. [DOI] [PubMed] [Google Scholar]
- 11.Tolone S, Savarino E, Zaninotto G, et al. High-resolution manometry is superior to endoscopy and radiology in assessing and grading sliding hiatal hernia: a comparison with surgical in vivo evaluation. United European Gastroenterol J 2018;6(7):981–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ham H, Cho YK, Lee HH, et al. Esophagogastric junction contractile integral and morphology: Two high-resolution manometry metrics of the anti-reflux barrier. J Gastroenterol Hepatol 2017;32:1443–1449. [DOI] [PubMed] [Google Scholar]
- 13.Tolone S, de Cassan C, de Bortoli N, et al. Esophagogastric junction morphology is associated with a positive impedance-pH monitoring in patients with GERD. Neurogastroenterol Motil 2015;27:1175–82. [DOI] [PubMed] [Google Scholar]
- 14.Akimoto S, Singhal S, Masuda T, Mittal SK. Classification for esophagogastric junction (EGJ) complex based on physiology. Dis Esoph 2017;30:1–6. [DOI] [PubMed] [Google Scholar]
- 15.Kumar D, Zifan A, Ghahremani G, et al. Morphology of the esophageal hiatus; is it different in 3 types of hiatus hernia? J Neurogastroenterol Motil 2020;26(1):51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoshino M, Sundaram A, Mittal SK. Role of the lower esophageal sphincter on acid exposure revisited with high-resolution manometry. J Am Coll Surg 2011;213:743–750. [DOI] [PubMed] [Google Scholar]
- 17.Lin Z, Xiao Y, Li Y, et al. Novel 3D high-resolution manometry metrics for quantifying esophagogastric junction contractility. Neurogastroenterol Motil 2017;29: e13054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao Y, Lin Z, Li Y, et al. Correlation between novel 3D high-resolution manometry esophagogastric junction metrics and pH-metry in reflux disease patients. Neurogastroenterol Mot 2018; 30 e 13344. [DOI] [PubMed] [Google Scholar]
- 19.Tolone S, De Bortoli N, Marabotto E, et al. Esophagogastric junction contractility for clinical assessment in patients with GERD: a real added value? Neurogastroenterol Motil 2015;27:1423–31. [DOI] [PubMed] [Google Scholar]
- 20.Jasper D, Freitas-Queiroz N, Hollenstein M, et al. Prolonged measurement improves the assessment of the barrier function of the esophago-gastric junction by high-resolution manometry. Neurogastroenterol Motil 2016;29: e12925. [DOI] [PubMed] [Google Scholar]
- 21.Wang D, Patel A, Mello M, et al. Esophagogastric junction contractile integral (EGJ-CI) quantifies changes in EGJ barrier function with surgical intervention. Neurogastroenterol Motil 2016;28:639–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xie C, Wang J, Li Y, et al. Esophagogastric junction contractility integral reflected the anti-reflux barrier dysfunction in GERD patients. J Neurogastroenterol Motil 2017; 23:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pandolfino JE, El-Serag HB, Zhang Q, et al. Obesity: a challenge to esophagogastric junction integrity. Gastroenterology 2006;130:639–649. [DOI] [PubMed] [Google Scholar]
- 24.de Vries DR, van Herwaarden MA, Smout AJ, Samsom M. Gastroesophageal pressure gradients in gastroesophageal reflux disease: relations with hiatal hernia, body mass index, and esophageal acid exposure. Am J Gastroenterol 2008;103:1349–54. [DOI] [PubMed] [Google Scholar]
- 25.Derakhshan MH, Robertson EV, Fletcher J, et al. Mechanism of association between BMI and dysfunction of the gastro-oesophageal barrier in patients with normal endoscopy. Gut 2012;61:337–343. [DOI] [PubMed] [Google Scholar]
- 26.Masuda T, Mittal SK, Kovacs B, et al. Thoracoabdominal pressure gradient and gastroesophageal reflux: insights from lung transplant candidates. Dis Esoph 2018. October 1;31(10). doi: 10.1093/dote/doy025. [DOI] [PubMed] [Google Scholar]


